Abstract
Background:
In the treatment and abstinence of alcoholism, especially in abstinence after treatment, "Craving" has an essential role. Thus, our aim was to examine the effect of cue-exposure therapy on alcohol craving in virtual environment based on the habit loop.
Methods:
The present investigation was a case-control experimental study with a pretest–posttest–5 weeks follow–up design. Research population were alcohol-addicted people hospitalized in a psychiatric hospital. We had 62 subjects who had abstained from alcohol consumption. The sampling method was convenience sampling and the sample allocation was randomized and matched. The intervention was VR-CET that was implemented in eight sessions. Penn Alcohol Craving Scale, Alcohol Urge Questionnaire, and Obsessive-Compulsive Drinking Scale were used to collect the data. In order to analyze the data, analysis of covariance (ANCOVA) in SPSS V.23 was performed.
Findings:
Our results showed that after implementation of VR-CET program the rate of PACS reduced significantly in posttest stage (p = 0.01) and follow up stage (p= 0.05). Also, the rate of AUQ and OCDS after exposure to VR-CET program declined significantly. The significant level of AUQ and OCDS in posttest and follow up stages were set at p- value < 0.01 and p-value <0.05 respectively.
Conclusion:
VR-CET program can reduce alcohol craving by paying attention to various cues and contexts. In fact, it would be more beneficial if the treatment environment resembles a conditioned context and contains as many related cues as possible.
Keywords: Exposure Therapy, Alcoholism, Craving, Virtual Environment, Habit
Introduction
Craving is one of the most important concepts in post-treatment abstinence from drug abuse and alcohol consumption.1 Pavlovian conditioning theory supplies explanations for craving. When certain situations or objects are repeatedly paired with addictive substances (unconditioned stimuli: US), the contexts or objects become conditioned stimuli (CS) that can elicit the addict's desire to use (conditioned response: CR), much like an unconditioned response (UR) to addictive substances. When an addict confronts the CS, he or she feels the craving.2,3 In other words, these conditions occur in four phases that are called a habit loop; cue, craving, response, and reward 4 (Figure 1). Also, we can divide these four steps into two phases: the problem phase and the solution phase. The problem phase includes the cue and the craving, and it is when an individual understands that something needs to change. The solution phase includes the response and the reward, and it is when he/she takes an action and attains the desired changes.4
Figure 1.
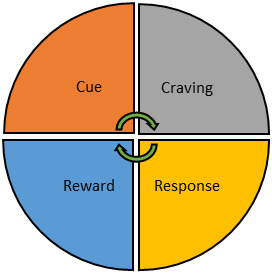
The habit loop: The process of forming an addictive behavior can be divided into four steps: cue, craving, response, and reward
Based on the habit loop, Cue evokes Craving. Indeed, Cue is regarded as a trigger of addictive behaviors.4,5 For instance, if a person goes to the supermarket and buys alcohol and drinks whenever he wants, even while he is abstinent, the person would buy alcohol and use it automatically after encountering the same brand of alcohol in a shop.6 In fact, cues of drug use create a state that is called "Wanting".7 Opposite to “liking”, wanting is related to the dopaminergic system.8 In summary the cue begins a craving, which urges a response, the response supplies a reward and it satisfies the craving and, ultimately, becomes associated with the cue.9,10
As cues correlate to relapse, many researchers suggest cue-exposure therapy (CET) to decrease cue reactivity. The purpose of CET is to extinguish conditioned responses (CR) by repeated exposure to addictive substances cues without the use of the unconditioned stimuli.11,12 In this regard, Hone-Blanchet et al13. showed that VR can decrease craving for substance use. Lee et al.14 also showed that CET can be a useful tool to reduce cravings for people who are nicotine dependent.
We aimed to employ VR technology and 3D animation techniques to apply CET since these approaches can prepare a wide range of settings and stimuli.14 Also, give the impression that the participant is in a pub rather than a clinic. Indeed, it's a virtual environment.
Methods
The present study is a pretest-posttest experiment with the control group and a follow-up (5 weeks) period. The research population were alcohol-addicted people that were hospitalized in a psychiatric hospital. 62 subjects who had abstained from alcohol consumption were included. The convenience sampling method was used in this study, and the sample allocation to the groups was randomized and matched.
Participants signed informed consent after being told of the study's goals. The technique of implementation was then explained to the participants. Inclusion criteria included diagnosing alcoholism by a psychiatrist, being hospitalized in a psychiatric hospital, and signing informed consent for taking part in the study. The exclusion criteria were being absent for more than two treatment sessions. University of Tabriz Ethics Committee approved the ethics of this study (IR.UTBZ.REC.1400.176).
Measurement and VR instrument: Penn Alcohol Craving Scale15 (PACS): The PACS is a five-item self-administered instrument for measuring craving. Frequency, intensity, and duration of thoughts about drinking are assessed along with the ability to resist drinking. The final item asks the responder to provide an average rating of his/her craving over the course of the past week, using a 7-point scale. Flannery et al.15 reported the reliability of this scale 0.92 by using Cronbach’s α. Also, they reported the validity of PACS by correlation between total PACS score and total Obsessive-Compulsive Drinking Scale (OCDS) score (r = 0.55, df = 146, p <0.00l) and Alcohol Urge Questionnaire (AUQ) scores (r = 0.39, df = 146, p < 0.001), which are great evidence for concurrent validity.
Alcohol Urge Questionnaire16 (AUQ): AUQ is an eight-item self-administered questionnaire including three items of drinking urges: 1. The desire for a drink (four items); 2. The expectation of positive effect from drinking (two items); and 3. Failure to abstain from drinking if alcohol was accessible (two items). Participants answer to AUQ with a 7-point scale. Bohn et al.16 reported the internal consistency of AUQ for 8-items 0.91 that was measured by Cronbach’s α. In addition, to assess the validity, they used a correlation between AUQ scores and Alcohol Dependence Scale (ADS) scores that were significantly related (R2 = 0.22, F = 8.57, p < 0.005).
Obsessive-Compulsive Drinking Scale17 (OCDS): The Obsessive-Compulsive Drinking Scale (OCDS) is a 14-item questionnaire that measures an individual’s alcohol use and his/her attempts to control his/her drinking and it uses a 5-point scale. Anton et al.17 reported the internal consistency of this scale 0.86 by using Cronbach’s α. Besides, to assess the validity of this scale they used a correlation between obsessive thoughts about alcohol subscale with the compulsive drinking subscale (r =0. 62, < 0.001) and with the total score (r = 0.92, p < 0.001).
We also used a Pentium IV PC, an Open GL Accelerator VGA card, a 2.4m 1.8m beam projector, and surround speakers. At the start of the VR simulation, the doors to two bars in the middle of a hallway were visible. A bartender and a few individuals drinking at tables would greet a user as they entered a tavern. Some folks drank alone, while others drank with their buddies. On the tables were bottles of beer, Soju, and bourbon, as well as side dishes, and the usual bar hubbub could be heard. Also, there was an advertisement for booze.
Statistical method: We used the analysis of covariance (ANCOVA) by SPSS Ver.23.
Procedure: The VR-CET was conducted in a group session with all of the participants and a clinical psychologist. For four weeks, participants underwent eight VR-CET sessions (i.e., two sessions a week).
The entire VR environment was implemented in Session 1. Every cue exposure in Sessions 2, 3, and 4 was based on a different theme, as determined by preliminary survey results: Session 2 focused on cravings elicited by other individuals, while Session 3 focused on cravings elicited by the environment. The fourth session concentrated on cravings that are elicited by a particular circumstance. Sessions 5, 6, and 7 employed a mixture of these three types of sessions. Finally, Session 8 focused on how to avoid relapse. Table 1 summarizes the topics of each session in a concise manner. Participants were asked for their demographic information and medical background before the first VR-CET session. They were asked to complete a survey about their drinking habits (e.g., frequency of getting drunk and history of alcohol-related injury) and to rate their desire for alcohol on the three scales. The AUQ was used to measure participants' responses to the VR-CET immediately after each session, and the three scales were retested at the end of the eighth session because it includes questions concerning the immediate desire to drink (i.e., it allows to assess "craving" elicited by alcohol-related cues even though the name that AUQ uses is the word "urge"). Each of the eight sessions lasted 30 minutes and consisted of three parts: a 5-minute introduction and immersion; a 20-minute VR navigation and interview (about the participants' feelings and ideas); and a 5-minute self-report questionnaire completion.
Table 1. Contents of the VR-CET program sessions6 .
| Session | Theme | VR-CET program content |
| 1 | Initial navigation | During the first session, the individual was free to move about. 1. Have you gotten a good feel for VR?? 2. Tell us how you felt and what you thought after experiencing virtual reality. 3. What emotions and thoughts do you have about the objects and situations in the VR? |
| 2 | Person-elicited craving | To understand more about the person who makes them want something, conduct an interview with them (open-ended). 1. How do you feel when you see a man in a virtual bar drinking alone? 2. How do you feel when you see a woman at a virtual bar drinking alone? 3. How do you feel when you observe a group of individuals drinking? |
| 3 | Object-elicited craving | Interview the client to discover more about the item that piques their interest (open-ended). 1. Which bottle tempts you to take a sip of something? 2. Which of the following side dishes makes you crave a glass of water? 3. When you see a commercial, what makes you want to drink? |
| 4 | Situation-elicited craving | Interview the client to learn more about the situation that has triggered their need for something (open-ended). 1. When you see someone drinking at a western pub, how strongly do you desire to drink? 2. When you see someone drinking in a Japanese bar, how strongly do you want to drink? 3. Would you like more booze if you ran out? What would you do if you drank more alcohol? |
| 5 6 7 8 |
Person-elicited craving
Object-elicited craving Situation-elicited craving Final navigation |
Rep all of the prior session's questions. Rep the questions from the third session. Rep the questions from the fourth session. The individual was free to walk about throughout the last session. 1. How do you feel and think now that you've spent so much time in virtual reality? (For a contrast, see the first session.) 2. How do the virtual reality objects and scenarios make you feel and think now, and what do they make you want to do? 3. What would you do if you were to have a VR experience in real life? |
Results
Based on the contents of table 2, demographic variables including age, sex, marital state, and educational level were measured in both case and control groups. The results showed that there is no significant difference between the groups.
Table 2. Comparison of participants' distribution based on qualitative demographic variable .
| Variable |
casegroup
N= 31 |
control group
N= 31 |
P |
| Age (Mean & SD) | 44.88 (89. 02) | 41.32 (7.66) | 0.9 |
|
Sex (N & %)
Male Female |
50 (80%) 12 (20%) |
43 (78%) 13 (22%) |
0.19 |
|
Marital status (N & %)
Single Married Divorced |
16 (25%) 6 (10%) 40 (65%) |
6 (10%) 17 (30%) 33 (60%) |
0.13 |
|
Educational level (N & %)
HS B.S M.Sc. and higher |
25 (40%) 19 (31%) 18 (29%) |
19 (35%) 14 (25%) 23 (40%) |
0.16 |
Based on table 3, the mean and standard deviation of scores in three variables (PACS, AUQ, and OCDS) in groups and in pre-test, posttest and follow up stages were assessed. The results showed that the mean of variables in three stage was different. In the case group, the mean of PACS in pre-test stage was 21.33, this amount decreased to 13.44 after implementation of the treatment sessions in posttest stage. Additionally, in the follow-up phase, this decreasing trend was almost maintained (16.42). Similarly, the mean of AUQ before implementation of treatment sessions was 19.89 and in posttest and follow up stages it decreased to 14.63, 16.1 respectively. Furthermore, the mean of OCDS in posttest and follow up stages after treatment sessions decreased to 15.6 and 17.2 respectively.
Table 3. The mean and standard deviation of scores .
| Group | Variable |
Pre-test
Mean (SD) |
Post-test
Mean (SD) |
Follow-up (5 weeks)
Mean (SD) |
| Case | ||||
| PACS | 21.23 (8.1) | 13.44 (2.6) | 16.42 (2.9) | |
| AUQ | 19.89 (6.2) | 14.63 (3.3) | 16.1 (4.1) | |
| OCDS | 23.8 (5.5) | 15.6 (4.4) | 17.2 (4.7) | |
| Control | ||||
| PACS | 22.6 (8.6) | 22.8 (4.3) | 23.2 (4.5) | |
| AUQ | 20.41 (7.2) | 23.5 (3.6) | 22.1 (5.1) | |
| OCDS | 18.3 (4.3) | 19.9 (5.1) | 21.1 (4.4) |
In addition, we used the covariance analysis test to examine the means more closely (Table 4). Contents of table 4 show that VR-CET program was effective. In other words, the rate of PACS after implementation of VR-CET program reduced significantly in posttest stage (p = 0.01) and follow up stage (p= 0.05). Also, the rate of AUQ and OCDS after exposure to VR-CET program declined significantly. The significant level of AUQ and OCDS in posttest and follow up stages were set at p- value < 0.01 and p-value <0.05 respectively. All in all, the results of present study showed that Cue-exposure therapy is effective on alcohol craving in virtual environment among people addicted to alcohol.
Table 4. Results of the covariance analysis test .
| Scale | Stages | Variable index | df | F | P-Value | Effectiveness | Statistical power |
| PACS | Post-test | Pre-test | 1 | 25.1 | 0.01 | 0.50 | 0.997 |
| Intervention | 1 | 19.5 | 0.01 | 0.48 | 0.998 | ||
| Follow-up | Pre-test | 1 | 9.52 | 0.006 | 0.31 | 0.83 | |
| Intervention | 1 | 12.34 | 0.02 | 0.37 | 0.91 | ||
| AUQ | |||||||
| Post-test | Pre-test | 1 | 7.5 | 0.08 | 0.15 | 0.388 | |
| Intervention | 1 | 23.1 | 0.01 | 0.16 | 0.396 | ||
| Follow-up | Pre-test | 1 | 6.43 | 0.09 | 0.13 | 0.377 | |
| Intervention | 1 | 13.68 | 0.03 | 0.39 | 0.84 | ||
| OCDS | |||||||
| Post-test | Pre-test | 1 | 12.3 | 0.002 | 0.39 | 0.91 | |
| Intervention | 1 | 19.3 | 0.01 | 0.48 | 0.98 | ||
| Follow-up | Pre-test | 1 | 3.15 | 0.09 | 0.13 | 0.39 | |
| Intervention | 1 | 13.6 | 0.02 | 0.38 | 0.33 |
Discussion
In the present study, we aimed to examine the effect of cue-exposure therapy on alcohol craving in virtual environment based on the habit loop.
Our results showed that VR-CET program decreased alcohol craving effectively. In accordance with our results Lee et al.6, Mellentin et al.18, Monti et al.19, and Byrne et al.14showed that CET program was effective in reducing alcohol craving. Although, CET has been used to treat a variety of substance addictions, including cigarettes, alcohol, and illicit drugs; the impact of CET has been inconsistent. In this regard, Tiffany and Conklin20 believed that in some CET studies that only used one cue, extinction of a CR to one cue could not be generalized to the others, and some CET studies failed to avoid relapse. Therefore, drug administration should be considered in conjunction with a variety of items and contexts.
Also, extinction in one context (a hospital, for example) has no effect in another. This explanation is based on classical conditioning research's "renewal effect."21 As a result, it will be more useful if the treatment environment is similar to the conditional context and includes most related symptoms as much as possible. Previous experiments have drawbacks in terms of the different associations of substance use: most studies have been performed using one or two stimuli in a therapy environment, such as a hospital or laboratory. Virtual reality (VR) and 3D animation techniques, on the other hand, can include a wide variety of scenarios and sensations, as well as the sensation of being in a bar rather than a hospital. These strategies would elicit cravings more efficiently than conventional approaches.22
CET mechanism was designed based on classical conditioning and habit loop. Indeed, based on reinforcement-learning models, the basic goal of an organism is to increase future rewards and decrease future punishments.23 But because the rewards are related to the dopaminergic system, they are pursued and can become addiction and habit.24,25 What separates habits and addictive behaviors from other behaviors are two competing neural systems; bottom-up system and top-down system. Bottom-up system, impulsive, or reactive system utilizes subcortical brain areas (amygdala and reward-sensitive dopamine-rich areas in the midbrain).26 Unlike Top-down system, this system tends to elevate rewarding and habitual behaviors and responds rapidly to accessible cues, without paying attention to the outcomes.26 In reality, addictive and habitual behaviors are processed unconsciously.27
As a result, they are result, they are controlled by an impulsive process and can be induced with little cognitive effort, knowledge, control, or intention.28 It seems that in this process primary memory is related to cues and craving29. In the other words, cue and craving urge the addictive and habitual behaviors (problem phase) until the organism reduces the tension by responding and gaining rewards (solution phase).4 According to the habit loop and classical conditioning, CET tries to put the consumer to frequent exposure with cues. Indeed, an alcohol addict becomes sensitive to cues of alcohol in elementary stages of his consumption and looks for a way to decrease alcohol craving by earning reward and response repeatedly (Sensitivity phase). However, in CET program due to repeated exposure to the cues, habituation is formed. As a result, the person does not respond to the cues (habituation phase).30-32
It should be noted that self-report instruments were used to collect data in this analysis, which could make the accuracy of the data difficult. Thus, it is proposed that common cognitive neuroscience techniques be used in future studies.
Conclusion
By paying attention to various cues and contexts (Generalizability), VR-CET program can decrease alcohol craving. Unlike traditional ways, it seems this method can elicit the craving more substantially. Indeed, it would be lucrative if the treatment environment was as similar to the conditional context as possible and provided as many related symptoms as possible. Therefore, mental health specialists can use this treatment program for the treatment of alcoholism.
Acknowledgments
We are grateful to all participants who helped us with this research. Under the code number IR.UTBZ.REC.1400.176, the study was authorized by the regional ethics committee. No. 894 of the project.
Citation: Karimpour Vazifehkhorani A, Attaran A, Karimi Saraskandrud A, Faghih H, Yeganeh N. Effectiveness of Cue-Exposure Therapy on Alcohol Craving in Virtual Environment: Based on habit loop. Addict Health 2022; 41(2): 78-86.
Footnotes
Conflict of Interests
The authors declare no conflict of interest in this study.
Authors’ Contribution
Main investigator, designed the study: AKV. Collected the data, performed analysis and wrote the first draft: NY, AA, AK and HF. All authors read and approved the final revision of the manuscript.
References
- 1.Stohs ME, Schneekloth TD, Geske JR, Biernacka JM, Karpyak VM. Alcohol craving predicts relapse after residential addiction treatment. Alcohol Alcohol. 2019;54(2):167–72. doi: 10.1093/alcalc/agy093. [DOI] [PubMed] [Google Scholar]
- 2.Heinz A, Beck A, Halil MG, Pilhatsch M, Smolka MN, Liu S. Addiction as learned behavior patterns. J Clin Med. 2019;8(8):1086. doi: 10.3390/jcm8081086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Doñamayor N, Ebrahimi C, Garbusow M, Wedemeyer F, Schlagenhauf F, Heinz A. Instrumental and Pavlovian Mechanisms in Alcohol Use Disorder. Current Addiction Reports 2020:1-25.
- 4. Clear J. Atomic Habits: An Easy & Proven Way to Build Good Habits & Break Bad Ones. New York: Avery; 2018.
- 5.Starcke K, Antons S, Trotzke P, Brand M. Cue-reactivity in behavioral addictions: A meta-analysis and methodological considerations. J Behav Addict. 2018;7(2):227–38. doi: 10.1556/2006.7.2018.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee JH, Kwon H, Choi J, Yang BH. Cue-exposure therapy to decrease alcohol craving in virtual environment. Cyberpsychol Behav. 2007;10(5):617–23. doi: 10.1089/cpb.2007.9978. [DOI] [PubMed] [Google Scholar]
- 7.Morales I, Berridge KC. ‘Liking’and ‘wanting’in eating and food reward: Brain mechanisms and clinical implications. Physiol Behav. 2020;227:113152. doi: 10.1016/j.physbeh.2020.113152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuypers KP, Perna ED, Dolder PC, Toennes SW, Theunissen EL, Mason NL, et al. Drug liking and wanting, not impulsive action or reflection is increased by 4-fluoroamphetamine. Psychopharmacology (Berl) 2018;235(8):2349–56. doi: 10.1007/s00213-018-4931-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen D, Naffziger EE, Berridge KC. Positive affect: nature and brain bases of liking and wanting. Curr Opin Behav Sci. 2021;39:72–78. doi: 10.1016/j.cobeha.2021.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Becker GS. Habits, addictions, and traditions. Chicago – Economics: University of Chicago - Economics Research Center 91- 8; 1991.
- 11.Loeber S, Croissant B, Heinz A, Mann K, Flor H. Cue exposure in the treatment of alcohol dependence: Effects on drinking outcome, craving and self‐efficacy. Br J Clin Psychol. 2006;45(Pt 4):515–29. doi: 10.1348/014466505X82586. [DOI] [PubMed] [Google Scholar]
- 12.Byrne SP, Haber P, Baillie A, Giannopolous V, Morley K. Cue Exposure Therapy for Alcohol Use Disorders: What Can Be Learned from Exposure Therapy for Anxiety Disorders? Subst Use Misuse. 2019;54(12):2053–63. doi: 10.1080/10826084.2019.1618328. [DOI] [PubMed] [Google Scholar]
- 13.Hone-Blanchet A, Wensing T, Fecteau S. The use of virtual reality in craving assessment and cue-exposure therapy in substance use disorders. Front Hum Neurosci. 2014;8:844. doi: 10.3389/fnhum.2014.00844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee J, Lim Y, Graham SJ, Kim G, Wiederhold BK, Wiederhold MD, et al. Nicotine craving and cue exposure therapy by using virtual environments. Cyberpsychol Behav. 2004;7(6):705–13. doi: 10.1089/cpb.2004.7.705. [DOI] [PubMed] [Google Scholar]
- 15.Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn alcohol craving scale. Alcohol Clin Exp Res. 1999;23(8):1289–95. [PubMed] [Google Scholar]
- 16.Bohn MJ, Krahn DD, Staehler BA. Development and initial validation of a measure of drinking urges in abstinent alcoholics. Alcohol Clin Exp Res. 1995;19(3):600–6. doi: 10.1111/j.1530-0277.1995.tb01554.x. [DOI] [PubMed] [Google Scholar]
- 17.Anton RF, Moak DH, Latham P. The Obsessive-Compulsive Drinking Scale: a self‐rated instrument for the quantification of thoughts about alcohol and drinking behavior. Alcohol Clin Exp Res. 1995;19(1):92–9. doi: 10.1111/j.1530-0277.1995.tb01475.x. [DOI] [PubMed] [Google Scholar]
- 18.Mellentin AI, Skøt L, Nielsen B, Schippers GM, Nielsen AS, Stenager E, Juhl C. Cue exposure therapy for the treatment of alcohol use disorders: a meta-analytic review. Clin Psychol Rev. 2017;57:195–207. doi: 10.1016/j.cpr.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Monti PM, Rohsenow DJ. Coping-skills training and cue-exposure therapy in the treatment of alcoholism. Alcohol Res Health. 1999;23(2):107–15. [PMC free article] [PubMed] [Google Scholar]
- 20.Tiffany ST, Conklin CA. A cognitive processing model of alcohol craving and compulsive alcohol use. Addiction. 2000;95(8 Suppl 2):145–53. doi: 10.1080/09652140050111717. [DOI] [PubMed] [Google Scholar]
- 21. Olive MF, Kalivas PW. Conditioning of Addiction. New York, NY. Springer; 2010. p. 159-78.
- 22.Ghiţă A, Teixidor L, Monras M, Ortega L, Mondon S, Gual A, et al. Identifying triggers of alcohol craving to develop effective virtual environments for cue exposure therapy. Front Psychol. 2019;10:74. doi: 10.3389/fpsyg.2019.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karimpour-Vazifehkhorani A, Rudsari AB, Rezvanizadeh A, Kehtary-Harzang L, Hasanzadeh K. Behavioral Activation Therapy on Reward Seeking Behaviors in Depressed People: An Experimental study. J Caring Sci. 2020;9(4):195–202. doi: 10.34172/jcs.2020.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mahmood Aliloo M, Hashemi Nosratabad T, Karimpour Vazifehkhorani A. The role of impulsivity, sensitivity to reward and anhedonia in distinction people with symptoms of borderline personality disorder from ordinary people Iran. Journal of Psychiatry and Clinical Psychology. 2018;24(2):136–47. [Google Scholar]
- 25.Stevens L, Verdejo-García A, Goudriaan AE, Roeyers H, Dom G, Vanderplasschen W. Impulsivity as a vulnerability factor for poor addiction treatment outcomes: a review of neurocognitive findings among individuals with substance use disorders. J Subst Abuse Treat. 2014;47(1):58–72. doi: 10.1016/j.jsat.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 26.Yin HH, Knowlton BJ. The role of the basal ganglia in habit formation. Nat Rev Neurosci. 2006;7(6):464–76. doi: 10.1038/nrn1919. [DOI] [PubMed] [Google Scholar]
- 27.Lewis M. Addiction and the brain: development, not disease. Neuroethics. 2017;10(1):7–18. doi: 10.1007/s12152-016-9293-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carmack SA, Koob GF, Anagnostaras SG. Learning and Memory in Addiction. Netherlands: Elsevier; 2017. 10.1016/B978-0-12-809324-5.21101-2. [DOI]
- 29.Benito KG, Walther M. Therapeutic process during exposure: Habituation model. J Obsessive Compuls Relat Disord. 2015;6:147–57. doi: 10.1016/j.jocrd.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kavanagh DJ, Sitharthan G, Young RM, Sitharthan T, Saunders JB, Shockley N, et al. Addition of cue exposure to cognitive‐behaviour therapy for alcohol misuse: a randomized trial with dysphoric drinkers. Addiction. 2006;101(8):1106–16. doi: 10.1111/j.1360-0443.2006.01488.x. [DOI] [PubMed] [Google Scholar]
- 31.Bakhshipour-Rudsari A, Karimpour-Vazifehkhorani A. The Role of Impulsivity and Sensitivity to Reward in Dropout of Addiction Treatment in Heroin Addicts. Addict Health. 2021;13(1):45–51. doi: 10.22122/ahj.v13i1.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Iranpour A, Nakhaee N. A review of alcohol-related harms: a recent update. Addict Health. 2019;11(2):129–37. doi: 10.22122/ahj.v11i2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]


