Abstract
Background:
Patients with sleep disturbances have gastrointestinal symptoms. Breath hydrogen (H2) and methane (CH4) indicating small intestinal bacterial overgrowth (SIBO) might be related with these symptoms. The study was conducted to assess the link between breath profiles and untreated obstructive sleep apnea (OSA).
Methods:
This prospective study enrolled consecutive patients with OSA using polysomnography. Heart rate variability (HRV) was used as a measurement for the balance of autonomic nervous system during polysomnography. Glucose breath test (GBT) to evaluate breath H2 and CH4 and bowel symptom questionnaire to investigate associated intestinal symptoms were performed.
Results:
Among 52 patients with OSA, 16 (30.8%) showed positivity to GBT. Although no significant difference was shown in GBT positivity between patients with healthy controls and patients with OSA (13.3% vs 30.8%, P = 0.109), breath H2 and CH4 levels in the OSA group were significantly higher than those in controls (P < 0.05). Flatulence was significantly common in OSA groups with GBT positivity than those without GBT positivity. Multivariate analysis demonstrated that waist-to-hip ratio (odds ratio = 12.889; 95% confidence interval (CI): 1.257–132.200; P = 0.031) and low-to-high-frequency ratio of HRV (odds ratio = 1.476; 95% CI: 1.013–2.151, P = 0.042) are independently related to GBT positivity in patients with OSA.
Conclusion:
Elevated breath H2 or CH4 after glucose load might not be an uncommon finding in patients with untreated OSA. Abdominal obesity and autonomic imbalance dysfunction are significantly associated with GBT positivity in OSA patients. SIBO could be considered as target for therapeutic management in OSA patients.
Keywords: Glucose breath test, heart rate variability, obstructive sleep apnea, small intestinal bacterial overgrowth
INTRODUCTION
Small intestinal bacterial overgrowth (SIBO) is defined as an increase in the number of bacteria in the small bowel, causing intestinal symptoms of chronic abdominal pain, bloating, diarrhea, flatulence and/or constipation. It could be related with several gastrointestinal disorders, such as celiac disease, inflammatory bowel disease like Crohn's disease, chronic liver disease, or functional gastrointestinal disorder (FGID) with irritable bowel syndrome (IBS).[1,2,3] An underlying pathophysiologic condition that alters the intestinal transit or loss of defense mechanism against bacteria can predispose patients to SIBO.[4] Recently, a non-invasive hydrogen (H2) and methane (CH4) breath test has been preferred for diagnosis of SIBO because of its simplicity and lower expense.
The characteristics of obstructive sleep apnea (OSA) are recurrent upper airway obstruction while sleeping, which causes fragmentation of sleep, recurrent hypoxia, and dysfunction of the autonomic nervous system (ANS). Because obstructive sleep apnea syndrome (OSAS), defined as an apnea–hypopnea index (AHI) of >5 and excessive daytime sleepiness was reported to occur in 6% of men and 4% of women, it is regarded as a significant public health issue.[5] Emotional and physiological stress from repetitive respiratory events during sleep, intermittent hypoxia, desaturation, fragmented sleep and altered autonomic balance might be associated with uncontrolled hypertension, type 2 diabetes, heart failure and stroke or functional bowel disorders including IBS, in patients with OSA.[6,7,8]
Recently intestinal dysbiosis has been reported to be linked to OSA.[9,10,11,12] Patients with restless leg syndrome, which leads to disrupted sleep, showed a higher prevalence of SIBO,[11,12] which is closely associated with functional gastrointestinal disorders, including IBS. Although the evidence of pathophysiology in human studies is still limited, an animal model of sleep apnea postulated that the mechanism is believed to be hypoxia-induced inflammation.[10] Because OSA can also affect the ANS to modulate the gastrointestinal motility, it might play a pivotal role in brain-gut-microbiome axis.
The association between SIBO and OSA is rarely reported. We hypothesize that ANS and desaturation/hypoxia from the respiratory events in OSA patients could be related to the presence of SIBO. We endeavored to prospectively survey the characteristics of patients with OSA and the risk factors of the SIBO in patients with OSA using physical examination, polysomnography (PSG), and glucose breath test (GBT).
PATIENTS AND METHODS
The protocol was approved by the Institutional Review Boards of St. Vincent's hospital, Catholic University of Korea (VC18OESI0079) on 24th April 2018. The study was conducted in compliance with the Declaration of Helsinki. A written informed consent was received from all the participants before inclusion in the study.
Study population
This prospective study was performed from January 2019 to December 2019, at a teaching hospital of St. Vincent's Hospital, the Catholic University School of Medicine. We enrolled symptomatic OSA patients diagnosed using full-attended PSG with the patients undergoing the Berlin questionnaire, Epworth sleepiness scale, and examination of the ear, nose, and throat. The subjects voluntarily participated in the study, and all were ≥18 years of age, without any history of organic gastrointestinal diseases. The patients who were treated with antisecretory agents such as histamine (H)2 receptor blockers or proton pump inhibitors, antibiotics, probiotics, prokinetics, narcotics, laxatives, bulking agents, or antidiarrheal agents within the previous four weeks; and those with renal insufficiency, major psychiatric problem, liver disease, connective tissue disease, hearing disturbance, thyroid disease, gastrointestinal disease, masticatory dysfunction, and incomplete data, or those who had underwent colonoscopy within the last three months, were also excluded. In addition, the subjects with previous history of gastrointestinal and gynecologic surgery except appendectomy using laparoscopy were excluded.[3]
Study design
All patients were surveyed for demographics, bowel symptom questionnaire, and GBT, immediately followed by the PSG study.
Polysomnography
Overnight, full-attended PSG was performed with the help of RemLogic-E version 3.4.1 software and Embla N7000/S7000 hardware (Embla Systems, Inc., Brawfield, CO, USA) in the hospital. During the PSG test, 13 sensors were used to measure the biological signals: six electroencephalogram (EEG) electrodes (F3, F4, C3, C4, O1, O2), two electrodes for electrooculogram, a single electrocardiography lead II and torso electrode, three electrodes on chin for electromyogram, two electrode sensors on both anterior tibial muscles for leg movements, on the left and right sides and body position sensors. An oral thermistor, a nasal pressure transducer, a pulse oximeter, belts for thoracic and abdominal respiratory plethysmography and a sensor for snoring were used to monitor respiratory events during sleep. Two sleep technicians initially scored data for PSG, and subsequently, a sleep specialist reviewed the data. The data for respiratory events, movements, arousals, sleep stages and sleep-related events index were evaluated based on the criteria of the American Academy of Sleep Medicine (AASM) Scoring Manual version 2.4.[13] Respiration events were scored as follows: Apnea was defined as the decrease in peak signal excursion by ≥90% of the pre-event baseline for ≥10 seconds through an oronasal thermal sensor or nasal cannula pressure transducer; hypopnea was defined as the decrease in the peak signal excursions by ≥ 30% of the pre-event baseline for ≥10 seconds through a nasal cannula pressure transducer with a desaturation of ≥3% or EEG arousal. The AHI was stated as the number of hypopneas and apneas per hour during total sleep time. OSA was stated as an AHI score of >5 and the presence of clinical symptoms, or an AHI score of >15.
Glucose breath test
Glucose H2–CH4 breath test was used for the diagnosis of SIBO. The patients were presented to the gastroenterology clinic after a minimum of 12 hours of fasting before the test. Physical exercise was not allowed during the test, starting two hours before the test. Patients were recommended to wash their mouth with 20 mL of 0.05% chlorhexidine 30 minutes before the breath test. The end expiratory breath samples were collected at baseline after ingestion of 75 gm of oral glucose solution (DIASOL-S SOLN, Tae Joon Pharma, Seoul, Korea) and then for 120 minutes at every 10-minute interval. Breath tests of the samples were performed each time by gas chromatography equipment (Quintron BreathTracker SC; Quintron Instrument Company, Milwaukee, WI, USA).
Definition of SIBO and assessment of intestinal symptoms
A positive GBT was defined and classified as follows[14]: (1) an increase in H2 concentration of more than 12 ppm above baseline within 90 minutes or baseline H2 ≥ 20 ppm (GBT (H2) + group), and (2) an increase in CH4 concentration of more than 12 ppm above baseline within 90 minutes or baseline CH4 level ≥20 ppm (GBT (CH4) + group). The GBT (mixed) + group was defined when both conditions (1) and (2) were met. All participants completed the bowel symptom questionnaire. The validated version of the IBS Quality of Life questionnaire was based on Rome IV criteria, together with additional questions about gastrointestinal symptoms.[15,16] Besides, 13 questions related to various gastrointestinal symptoms experienced in the last four weeks were included. Information on bowel symptoms of discomfort, pain, hard or lumpy stools, loose or watery stools, straining during bowel movements, bowel urgency, mucus passing during bowel movements, abdominal fullness and bloating or swelling, flatus, chest pain or heartburn, the feeling of being full soon after a meal, urinary frequency, and nausea was collected. The severity of symptoms was estimated by the total symptom score, defined by the cumulative scores of event frequency and intrusiveness. The frequency and intrusiveness of each symptom were evaluated by each patient using a seven-point scale from 0 to 6. Since the total symptom score was defined as the sum of the symptom frequency and intrusiveness scores, the range of a score by each symptom was 0–12.
Statistical analyses
Clinical demographic evaluations included were according to the presence of SIBO. The profiles of breath H2 and CH4 in patients with OSA were compared with those of historically healthy controls without any functional gastrointestinal symptoms or organic diseases who were previously registered in the determination of normal GBT value at the Catholic University of Korea, School of Medicine.[2] During the study, we confirmed by phone that controls had no history of sleep disturbances. Statistical Package for the Social Sciences (SPSS) version 20.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical analyses. Categorical variables are expressed as quantities and analyzed using χ2 tests or Fisher's exact test, whereas continuous variables are presented as mean ± standard deviation (SD) and were analyzed using student's t-test. Multiple stepwise logistic regression analysis was used to identify independent factors correlated with the existence of SIBO. A P value of less than 0.05 was considered significant for all tests. The risk factors with P value less than 0.15 in univariate analysis were used for variables in multivariate analysis.
RESULTS
Study population
Fifty-six patients with OSA were enrolled in the study. Four subjects were excluded from the analysis due to a sample error. Finally, 52 patients were included in this study. Among the participants, the mean age was 49.9 (range, 24–75) years, and 11 patients (21.2%) were women. Twelve patients (23.1%) were diagnosed with IBS.
Comparison of GBT and SIBO in OSA patients and healthy controls
Among 52 patients with OSA, 16 (30.8%) were included in the positivity to GBT; 10 (62.5%) with H2 excretors, 2 (12.5%) with CH4 excretors, and 4 (25.0%) with mixed excretors. The significant differences were shown in the exhaled H2 or CH4 at all the time points, between patients with OSA and controls [Figure 1]. There was no significant difference except a trend in GBT positivity between patients with OSA and controls (30.8% vs 13.3%, P = 0.109).
Figure 1.
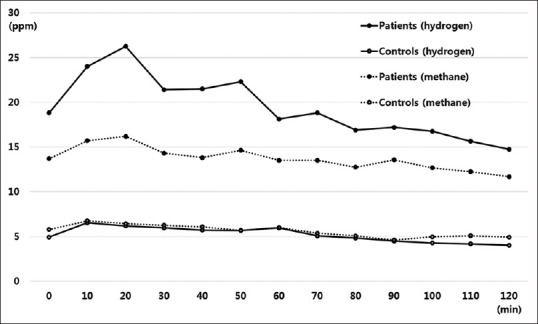
Flowchart of breath hydrogen and methane profiles during glucose breath test in patients with obstructive sleep apnea and controls
Clinical characteristics and bowel symptoms according to the presence of SIBO
There were no differences between GBT-positive and GBT-negative groups with regard to demographics except for the waist-to-hip ratio (WHR) (P = 0.043) [Table 1]. Among bowel symptoms score, the total symptom score of flatulence alone was significantly higher in the GBT-positive group than in the GBT-negative group (5.75 ± 2.11 vs 3.83 ± 2.74, P = 0.016) [Figure 2].
Table 1.
Clinical characteristics according to the presence of SIBO
| Variable | SIBO (n=16) | Non-SIBO (n=36) | P |
|---|---|---|---|
| Age, yrs | 50.6±11.2 | 49.5±11.8 | 0.755 |
| Male, n (%) | 13 (81.3) | 29 (77.8) | 0.777 |
| BMI, kg/m2 | 28.7±6.3 | 27.0±4.2 | 0.246 |
| Body fat percentage | 30.8±8.4 | 28.4±6.7 | 0.288 |
| WHR | |||
| M≤0.9, F≤0.85 | 2 | 15 | 0.043 |
| M>0.9, F>0.85 | 13 | 20 | |
| Visceral fat area | 120.3±48.3 | 98.9±38.0 | 0.099 |
| Diabetes, n (%) | 2 (12.5) | 5 (13.9) | 0.892 |
| Hypertension, n (%) | 3 (18.8) | 12 (33.3) | 0.284 |
| Smoking, n (%) | 2 (12.5) | 12 (30.6) | 0.165 |
| Alcohol, n (%) | 7 (43.8) | 21 (58.3) | 0.330 |
| IBS, n (%) | 4 (25.0) | 8 (22.2) | 0.826 |
SIBO, Small intestinal bacterial overgrowth; BMI, Body mass index; WHR, Waist-to-hip ratio; IBS, Irritable bowel syndrome. *Data are expressed as mean±SD or number (%)
Figure 2.
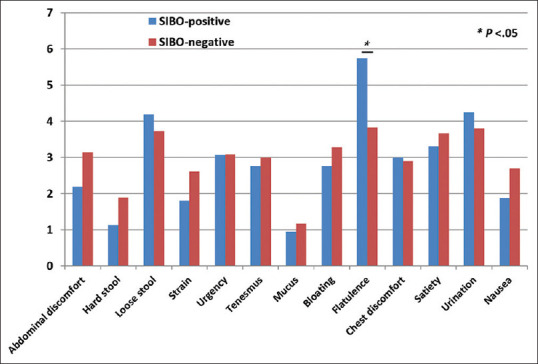
Total symptom scores of individual intestinal symptoms according to small intestinal bacterial overgrowth
Parameters of PSG and heart rate variability according to the positivity to GBT
Among PSG parameters, only the parameter of rapid eye movement (REM) (%) was significantly lower in GBT-positive patients than in GBT-negative patients [Table 2]. After the patients were divided into four subgroups according to GBT positivity and REM20 (the number of subjects ≤20%, or >20% of their REM sleep duration), there was no significant difference among the four subgroups, although there was a trend based on GBT positivity (P = 0.105). For parameters of heart rate variability (HRV), significant differences were shown in the value of SD of N–N intervals (SDNN), mean of the SDs of all the N–N intervals for each five-minute segment (SDNN index) or low frequency (LF), and a trend was observed in the ratio of low frequency to high frequency (LF/HF) between GBT-negative and -positive subjects, respectively [Table 3]. Multivariate analysis with covariates such as WHR, REM (%), flatulence, SDNN, and LF (or LF/HF) showed that WHR and LF/HF were significant independent factors for GBT positivity in patients with OSA [Table 4].
Table 2.
The parameters of polysomnography according to the presence of SIBO
| Variable | SIBO (n=16) | Non-SIBO (n=36) | P |
|---|---|---|---|
| AHI | 43.8±29.7 | 44.2±24.9 | 0.961 |
| RDI | 44.1±29.4 | 44.5±24.8 | 0.957 |
| Apnea index | 20.2±25.3 | 21.3±24.1 | 0.883 |
| Hypopnea index | 23.6±20.2 | 24.1±15.1 | 0.919 |
| Oxygen desaturation events | 38.6±31.3 | 55.6±115.8 | 0.568 |
| Supine RDI | 41.2±24.7 | 46.6±26.3 | 0.489 |
| REM (%) | 14.7±8.7 | 20.2±7.1 | 0.021 |
| REM20, n (%) | |||
| ≤20 | 11 (68.8) | 16 (44.4) | 0.105 |
| >20 | 5 (31.2) | 20 (55.6) | |
| AHI REM index | 42.7±23.6 | 44.1±24.6 | 0.853 |
| Mean oxygen saturation | 93.5±3.4 | 94.3±2.7 | 0.333 |
| Lowest oxygen saturation | 78.6±9.7 | 79.2±7.9 | 0.797 |
| T90 (min) | 56.8±89.4 | 42.2±61.5 | 0.498 |
| AD/TST (%) | 16.2±24.0 | 15.9±19.0 | 0.964 |
| HD/TST (%) | 16.0±12.5 | 17.7±11.0 | 0.619 |
| Respiratory arousals | 2.6±2.8 | 3.3±3.9 | 0.516 |
| Spontaneous arousals | 6.4±6.5 | 4.4±3.3 | 0.246 |
| Total arousals index | 46.9±20.9 | 42.9±21.3 | 0.527 |
SIBO, Small intestinal bacterial overgrowth; AHI, Apnea–hypopnea index; RDI, Respiratory disturbance index; REM, Rapid eye movement sleep; REM20, A number of subjects below their REM sleep duration percentage of 20%; T90, Total sleep time in oxygen saturation <90%; AD, Apnea duration; TST, Total sleep time; HD, Hypopnea duration. Data are expressed as mean±SD or number (%)
Table 3.
The parameters of heart rate variability during polysomnography according to the presence of SIBO
| Variable | SIBO (n=16) | Non-SIBO (n=36) | P |
|---|---|---|---|
| HRV | 28.9±36.0 | 15.0±5.5 | 0.175 |
| SDNN | 101.7±33.8 | 76.4±20.0 | 0.025 |
| SDNN index | 76.5±31.8 | 55.0±18.2 | 0.039 |
| RMSSD | 62.4±49.9 | 40.6±25.5 | 0.162 |
| pNN50 | 12.3±12.8 | 7.5±6.3 | 0.221 |
| VLF | 22,719.4±15,892.0 | 16,273.9±11,227.6 | 0.157 |
| LF | 16,543.2±12,452.3 | 9248.8±6934.5 | 0.041 |
| HF | 4424.1±2367.0 | 4823.2±4064.2 | 0.717 |
| LF/HF | 4.3±4.6 | 2.4±1.5 | 0.118 |
SIBO, Small intestinal bacterial overgrowth; HRV, Heart rate variability; SDNN, Standard deviation of N–N intervals; SDNN index, Mean of the standard deviations of all the N–N intervals for each five-minute segment; RMSSD, Square root of the mean of the squared differences of adjacent N–N intervals; NN50 count, Number of pairs of adjacent N–N intervals more than 50 ms; pNN50, Rate of NN50 in total number of N–N intervals; VLF, Very low frequency; LF, Low frequency; HF, High frequency; LF/HF, Ratio of low frequency to high frequency. Data are expressed as mean±SD
Table 4.
Factors associated with small intestinal bacterial overgrowth on multivariate analysis
| Beta | SE beta | Odd ratio (95% CI) | P | |
|---|---|---|---|---|
| Waist-to-hip ratio | 2.556 | 1.188 | 12.889 (1.257–132.200) | 0.031 |
| LF/HF | 0.390 | 0.192 | 1.48 (1.013–2.151) | 0.042 |
WHR, Waist-to-hip ratio; LF/HF, Ratio of low frequency to high frequency
DISCUSSION
The current study showed that elevated breath H2 or CH4 after glucose load might be related to untreated OSA patients. It appears to be closely related to the reduced REM sleep duration and the affected HRV seen in OSA patients. To our knowledge, this is the first study to evaluate the effects of OSA or sleep on the result of GBT indicating the status of SIBO.
In the present study, 30.8% of patients with untreated OSA had positivity to GBT. SIBO is defined as the excessive amounts of bacteria in the small intestine. The small bowel shows an inherent defense mechanism against bacterial overgrowth that sweeps the bacteria from the small bowel to the colon. Motility disorders secondary to inflammation, neuropathy and autonomic nervous system alterations may disrupt this protective mechanism and serve as important contributors to SIBO. Although the exact mechanism is not well known, sleep disturbance might affect the enteric nervous system and immune system. Sleep is related to the enteric nervous system that controls gastrointestinal transit and pro-inflammatory cytokines that affect the sleep–wake cycle, which has been associated with gastrointestinal motility disorders such as IBS.[17,18,19] IBS is a representative disease which is considered to be a partial cause of SIBO.[20,21] Therefore, it can be cautiously inferred that SIBO is associated with sleep disorders. Furthermore, future research is expected to reveal what specific effects OSA and SIBO have on each other, and which causes and effects, through pathophysiological studies. The positivity to GBT did not differ between controls and OSA patients. A potential limitation of this study was the use of historical controls. This is not a well-matched case–control study with small number of historical controls. The number of historical controls, which is less than the cases, may affect the result. However, the positivity to GBT in historic controls is consistent with that in other studies,[22,23,25] and the positivity to GBT of 30.8% in OSA patients were similar to that of 31.9% in patients with functional gastrointestinal disorders known to be related with enteric bacteria in its pathogenesis.[26,27] In addition, intestinal bacteria may be associated with OSA based on significantly higher profiles of both breath H2 and CH4 during GBT in patients with OSA. The failure to accurately evaluate OSA by PSG and to perform detailed demographic investigation in controls surveyed in the past should possibly be considered to interpret the above result. However, there are many reports that state that the prevalence of OSA is 2%–4%,[28,29] so even if there were OSA in controls, only a small percentage of OSA patients would have been in the control group, and we confirmed by phone that controls had no clinical history of sleep disturbance. Nevertheless, further research is needed to verify the diagnosis of bacterial overgrowth by GBT using well-designed controls.
WHR, known as a relevant obesity index, is an independent factor for GBT positivity in patients with untreated OSA. Although it is debatable, there is a link between SIBO and obesity.[30,31] Generally, body mass index (BMI) is a valid indicator of global obesity, although WHR is used to assess central obesity. Interestingly, GBT positivity was not associated with BMI, though it was independently associated with WHR, indicating regional central obesity in the study. Recent reports[31,32] revealed that IBS or SIBO correlated with obesity, with altered bowel motility as a suggested pathophysiology, but was not associated with BMI, consistent with the result of this study. It is already well known that OSA is associated with obesity.[33] Flatulence was associated with SIBO in the study. Flatulence, together with signs of abdominal distension, might affect increased WHR in SIBO-positive patients. We need to study it further to determine the direct correlation between GBT positivity and WHR in a large number of enrolled subjects with obesity.
The changes in sleep could occur with age, although REM sleep is usually 20%–25% of total sleep in healthy young adults and is well maintained in the healthy elderly.[34] However, patients with untreated OSA usually show distinct characteristics such as fragmented sleep architecture, reduced REM or slow wave sleep, abnormal HRV and increases in respiratory index such as AHI, RDI and lowest oxygen saturation. These abnormalities in respiration, sleep architecture and autonomic nervous systems improve with continuous positive airway pressure. A meta-analysis showed that a significant increase in the percentage of REM sleep duration was shown during titration of continuous positive airway pressure compared with baseline sleep study in 11 of 14 studies.[35] This could suggest that reduced REM sleep in patients with untreated OSA may be associated with respiratory events, fragmented sleep and repetitive arousals due to respiratory events.
There have been some studies on the relationship between sleep and gastrointestinal motility disorders, which has shown inconsistent results.[36,37] The percentage of REM sleep was prominently increased in IBS patients compared with that in controls,[38] which was contrary to our results that reduced REM was closely associated with the presence of SIBO. This might be because most participants in the previous study were non-OSA status, contrary to this study with OSA patients, which could show contradictory expression of REM. No significant difference was found in AHI during REM sleep (REM AHI) between GBT-positive and -negative groups, whereas there were statistically significant differences in REM (%) or trend in REM20 in univariate analysis. Moreover, multivariate logistical analysis showed that reduced REM sleep duration percentage was independently related to GBT positivity. One can speculate that the percentage of REM sleep might be a more important factor to the presence of SIBO than hypoxia during REM sleep.
The pathophysiological mechanism for the correlation between SIBO and sleep deprivation is not clear, although it could be deduced from research on the role of dominant sympathetic functioning in IBS. The evaluation of beat-to-beat variation of heart rate has been known to be an indicator of the function of the autonomic nervous system to control HRV by both vagal and sympathetic activity.[39,40] Thompson et al.[36] reported that IBS patients had increased LF levels, greater sympathetic dominance with elevated LF/HF ratio, and greater sympathetic dominance because of vagal withdrawal. Our results demonstrate that SDNN, SDNN index and LF were higher in GBT-positive patients in univariate analysis. Moreover, we found a relationship between LF/HF and GBT positivity in the multivariate analysis. Accordingly, SIBO might be associated with altered autonomic balance with sympathetic dominance, represented by HRV in OSA patients. Nevertheless, we need to study further with a larger number of patients to validate this data.
In conclusion, elevated breath H2 or CH4 after glucose load might not be an uncommon finding in patients with untreated OSA. Central obesity and autonomic dysfunctions with increased sympathetic dominance, which are common findings in patients with OSA, might increase the risk of SIBO. Further studies are needed to elucidate the role of SIBO in patients diagnosed with untreated OSA by demonstrating the potential response to pharmacological treatment for SIBO.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors wish to acknowledge the support of the Catholic Medical Center Research Foundation made in the program year of 2018.
REFERENCES
- 1.Rao SSC, Bhagatwala J. Small intestinal bacterial overgrowth: Clinical features and therapeutic management. Clin Transl Gastroenterol. 2019;10:e00078. doi: 10.14309/ctg.0000000000000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee JM, Lee KM, Chung YY, Lee YW, Kim DB, Sung HJ, et al. Clinical significance of the glucose breath test in patients with inflammatory bowel disease. J Gastroenterol Hepatol. 2015;30:990–4. doi: 10.1111/jgh.12908. [DOI] [PubMed] [Google Scholar]
- 3.Lee KM, Paik CN, Chung WC, Yang JM, Choi MG. Breath methane positivity is more common and higher in patients with objectively proven delayed transit constipation. Eur J Gastroenterol Hepatol. 2013;25:726–2. doi: 10.1097/MEG.0b013e32835eb916. [DOI] [PubMed] [Google Scholar]
- 4.Pimentel M, Saad RJ, Long MD, Rao SSC. ACG clinical guideline: Small intestinal bacterial overgrowth. Am J Gastroenterol. 2020;115:165–78. doi: 10.14309/ajg.0000000000000501. [DOI] [PubMed] [Google Scholar]
- 5.Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev. 2017;34:70–81. doi: 10.1016/j.smrv.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Nieto FJ, et al. Sleep-disordered breathing and cardiovascular disease: Cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 7.Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, et al. Association of nocturnal arrhythmias with sleep-disordered breathing: The sleep heart health study. Am J Respir Crit Care Med. 2006;173:910–6. doi: 10.1164/rccm.200509-1442OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeng YM, Hu AK, Su HZ, Ko CY. A review of the association between oral bacterial flora and obstructive sleep apnea-hypopnea syndrome comorbid with cardiovascular disease. Sleep Breath. 2020;24:1261–6. doi: 10.1007/s11325-019-01962-9. [DOI] [PubMed] [Google Scholar]
- 9.Ko CY, Liu QQ, Su HZ, Zhang HP, Fan JM, Yang JH, et al. Gut microbiota in obstructive sleep apnea-hypopnea syndrome: Disease-related dysbiosis and metabolic comorbidities. Clin Sci (Lond) 2019;133:905–17. doi: 10.1042/CS20180891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tripathi A, Melnik AV, Xue J, Poulsen O, Meehan MJ, Humphrey G, et al. Intermittent hypoxia and hypercapnia, a hallmark of obstructive sleep apnea, alters the gut microbiome and metabolome. mSystems. 2018;3:e00020–18. doi: 10.1128/mSystems.00020-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weinstock LB, Walters AS. Restless legs syndrome is associated with irritable bowel syndrome and small intestinal bacterial overgrowth. Sleep Med. 2011;12:610–3. doi: 10.1016/j.sleep.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Weinstock LB, Fern SE, Duntley SP. Restless legs syndrome in patients with irritable bowel syndrome: Response to small intestinal bacterial overgrowth therapy. Dig Dis Sci. 2008;53:1252–6. doi: 10.1007/s10620-007-0021-0. [DOI] [PubMed] [Google Scholar]
- 13.Berry RB, Brooks R, Gamaldo C, Harding SM, Lloyd RM, Quan SF, et al. AASM scoring manual updates for 2017 (Version 2.4) J Clin Sleep Med. 2017;13:665–6. doi: 10.5664/jcsm.6576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saad RJ, Chey WD. Breath testing for small intestinal bacterial overgrowth: Maximizing test accuracy. Clin Gastroenterol Hepatol. 2014;12:1964–72. doi: 10.1016/j.cgh.2013.09.055. [DOI] [PubMed] [Google Scholar]
- 15.Park JM, Choi MG, Oh JH, Cho YK, Lee IS, Kim SW, et al. Cross-cultural validation of irritable bowel syndrome quality of life in Korea. Dig Dis Sci. 2006;51:1478–84. doi: 10.1007/s10620-006-9084-6. [DOI] [PubMed] [Google Scholar]
- 16.Park JM, Choi MG, Kim YS, Choi CH, Choi SC, Hong SJ, et al. Quality of life of patients with irritable bowel syndrome in Korea. Qual Life Res. 2009;18:435–46. doi: 10.1007/s11136-009-9461-7. [DOI] [PubMed] [Google Scholar]
- 17.Ghiasi F, Amra B, Sebghatollahi V, Azimian F. Association of irritable bowel syndrome and sleep apnea in patients referred to sleep laboratory. J Res Med Sci. 2017;22:72. doi: 10.4103/jrms.JRMS_523_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rotem AY, Sperber AD, Krugliak P, Freidman B, Tal A, Tarasiuk A. Polysomnographic and actigraphic evidence of sleep fragmentation in patients with irritable bowel syndrome. Sleep. 2003;26:747–52. doi: 10.1093/sleep/26.6.747. [DOI] [PubMed] [Google Scholar]
- 19.Amin MM, Belisova Z, Hossain S, Gold MS, Broderick JE, Gold AR. Inspiratory airflow dynamics during sleep in veterans with Gulf War illness: A controlled study. Sleep Breath. 2011;15:333–9. doi: 10.1007/s11325-010-0386-8. [DOI] [PubMed] [Google Scholar]
- 20.Pimentel M, Chow EJ, Lin HC. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol. 2000;95:3503–6. doi: 10.1111/j.1572-0241.2000.03368.x. [DOI] [PubMed] [Google Scholar]
- 21.Chen B, Kim JJ, Zhang Y, Du L, Dai N. Prevalence and predictors of small intestinal bacterial overgrowth in irritable bowel syndrome: A systematic review and meta-analysis. J Gastroenterol. 2018;53:807–18. doi: 10.1007/s00535-018-1476-9. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Liu G, Duan Y, Dong H, Geng J. Prevalence of small intestinal bacterial overgrowth in multiple sclerosis: A case-control study from China. J Neuroimmunol. 2016;301:83–7. doi: 10.1016/j.jneuroim.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Lasa JS, Zubiaurre I, Fanjul I, Olivera P, Soifer L. Small intestinal bacterial overgrowth prevalence in celiac disease patients is similar in healthy subjects and lower in irritable bowel syndrome patients. Rev Gastroenterol Mex. 2015;80:171–4. doi: 10.1016/j.rgmx.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 24.Niu XL, Liu L, Song ZX, Li Q, Wang ZH, Zhang JL, et al. Prevalence of small intestinal bacterial overgrowth in Chinese patients with Parkinson's disease. J Neural Transm (Vienna) 2016;123:1381–6. doi: 10.1007/s00702-016-1612-8. [DOI] [PubMed] [Google Scholar]
- 25.Gabrielli M, Bonazzi P, Scarpellini E, Bendia E, Lauritano EC, Fasano A, et al. Prevalence of small intestinal bacterial overgrowth in Parkinson's disease. Mov Disord. 2011;26:889–92. doi: 10.1002/mds.23566. [DOI] [PubMed] [Google Scholar]
- 26.Saffouri GB, Shields-Cutler RR, Chen J, Yang Y, Lekatz HR, Hale VL, et al. Small intestinal microbial dysbiosis underlies symptoms associated with functional gastrointestinal disorders. Nat Commun. 2019;10:2012. doi: 10.1038/s41467-019-09964-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim DB, Paik CN, Kim YJ, Lee JM, Jun KH, Chung WC, et al. , Positive glucose breath tests in patients with hysterectomy, gastrectomy, and cholecystectomy. Gut Liver. 2017;11:237–42. doi: 10.5009/gnl16132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–43. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim J, In K, Kim J, You S, Kang K, Shim J, et al. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004;170:1108–13. doi: 10.1164/rccm.200404-519OC. [DOI] [PubMed] [Google Scholar]
- 30.Wijarnpreecha K, Werlang ME, Watthanasuntorn K, Panjawatanan P, Cheungpasitporn W, Gomez V, et al. Obesity and risk of small intestine bacterial overgrowth: A systematic review and meta-analysis. Dig Dis Sci. 2020;65:1414–22. doi: 10.1007/s10620-019-05887-x. [DOI] [PubMed] [Google Scholar]
- 31.Madrid AM, Poniachik J, Quera R, Defilippi C. Small intestinal clustered contractions and bacterial overgrowth: A frequent finding in obese patients. Dig Dis Sci. 2011;56:155–60. doi: 10.1007/s10620-010-1239-9. [DOI] [PubMed] [Google Scholar]
- 32.Lee CG, Lee JK, Kang YS, Shin S, Kim JH, Lim YJ. Visceral abdominal obesity is associated with an increased risk of irritable bowel syndrome. Am J Gastroenterol. 2015;110:310–9. doi: 10.1038/ajg.2014.422. [DOI] [PubMed] [Google Scholar]
- 33.Sekizuka H, Ono Y, Saitoh T, Ono Y. Visceral fat area by abdominal bioelectrical impedance analysis as a risk of obstructive sleep apnea. Int Heart J. 2021;62:1091–5. doi: 10.1536/ihj.21-219. [DOI] [PubMed] [Google Scholar]
- 34.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 35.Nigam G, Camacho M, Riaz M. Rapid Eye Movement (REM) rebound on initial exposure to CPAP therapy: A systematic review and meta-analysis. Sleep Sci Pract. 2017;1:13. [Google Scholar]
- 36.Thompson JJ, Elsenbruch S, Harnish MJ, Orr WC. Autonomic functioning during REM sleep differentiates IBS symptom subgroups. Am J Gastroenterol. 2002;97:3147–53. doi: 10.1111/j.1572-0241.2002.07112.x. [DOI] [PubMed] [Google Scholar]
- 37.Fass R, Fullerton S, Tung S, Mayer EA. Sleep disturbances in clinic patients with functional bowel disorders. Am J Gastroenterol. 2000;95:1195–2000. doi: 10.1111/j.1572-0241.2000.02009.x. [DOI] [PubMed] [Google Scholar]
- 38.Kumar D, Thompson PD, Wingate DL, Vesselinova-Jenkins CK, Libby G. Abnormal REM sleep in the irritable bowel syndrome. Gastroenterology. 1992;103:12–7. doi: 10.1016/0016-5085(92)91089-m. [DOI] [PubMed] [Google Scholar]
- 39.Kamath MV, Fallen EL. Power spectral analysis of heart rate variability: A noninvasive signature of cardiac autonomic function. Crit Rev Biomed Eng. 1993;21:245–311. [PubMed] [Google Scholar]
- 40.Berntson GG, Bigger JT Jr, Eckberg DL, Grossman P, Kaufmann PG, Malik M, et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology. 1997;34:623–48. doi: 10.1111/j.1469-8986.1997.tb02140.x. [DOI] [PubMed] [Google Scholar]


