Abstract
The extracellular matrix (ECM), a complex set of fibrillar proteins and proteoglycans, supports the renal parenchyma and provides biomechanical and biochemical cues critical for spatial-temporal patterning of cell development and acquisition of specialized functions. As in vitro models progress towards biomimicry, more attention is paid to reproducing ECM-mediated stimuli. ECM’s role in in vitro models of renal function and disease used to investigate kidney injury and regeneration is discussed. Availability, affordability, and lot-to-lot consistency are the main factors determining the selection of materials to recreate ECM in vitro. While simpler components can be synthesized in vitro, others must be isolated from animal or human tissues, either as single isolated components or as complex mixtures, such as Matrigel or decellularized formulations. Synthetic polymeric materials with dynamic and instructive capacities are also being explored for cell mechanical support to overcome the issues with natural products. ECM components can be used as simple 2D coatings or complex 3D scaffolds combining natural and synthetic materials. The goal is to recreate the biochemical signals provided by glycosaminoglycans and other signaling molecules, together with the stiffness, elasticity, segmentation, and dimensionality of the original kidney tissue, to support the specialized functions of glomerular, tubular, and vascular compartments. ECM mimicking also plays a central role in recent developments aiming to reproduce renal tissue in vitro or even in therapeutical strategies to regenerate renal function. Bioprinting of renal tubules, recellularization of kidney ECM scaffolds, and development of kidney organoids are examples. Future solutions will probably combine these technologies.
Keywords: extracellular matrix, matrigel, kidney, bioprinting, scaffolds, microfluidics, organoids
Introduction
Extracellular matrix components provide critical cues for renal cell and tissue functions
The extracellular matrix (ECM) is a biological scaffold holding all cellular tissue components together (Supplementary Figure 1). The main components of kidney ECM are collagen I, proteoglycans, and glycosaminoglycans. The basal membrane (BM) surrounding the renal tubules contains collagen IV, laminins, and fibronectin (Theocharis et al., 2016). ECM composition and dimensionality establish biomechanical and biochemical signals essential for kidney’s development (Clause and Barker, 2013; Loganathan et al., 2020), tissue growth, differentiation (Muncie and Weaver, 2018), and function (Frantz et al., 2010; Manninen, 2015; Loganathan et al., 2020).
The stiffness of the ECM influences organ or tissue differentiation and morphogenesis. ECM stiffness is determined by the material’s elasticity, as measured by the Young’s elastic modulus. Conventional plastic cell culture containers (109 Pa) are stiffer than bone (15–20 106 Pa) and the kidney (5–10 103 Pa). The substrate mechanical properties affect cell adhesion, migration, proliferation, and differentiation (Chen et al., 2014; Melica et al., 2019). Topography and dimensionality, which identify ECM forms, features, and distribution, are linked to cell polarization, actin bundle alignment, cell adhesion, orientation, migration, and morphology (Nur-E-Kamal et al., 2006; Kim et al., 2014; Sciancalepore et al., 2016; Hulshof et al., 2018; Bosch-Fortea et al., 2019) and renal progenitors’ fate (Nur-E-Kamal et al., 2006; Kim et al., 2014; Bosch-Fortea et al., 2019; Walma and Yamada, 2020). Microfabrication methods can reproduce ECM mechanical and physical properties and architectural features, but resolution and complexity are still rudimentary (Le Digabel et al., 2010). Engineered ECM can be tailored to meet cell or tissue-specific needs (Beamish et al., 2017).
ECM components, particularly glycosaminoglycans (GAGs), provide biochemical signals that regulate cell functions and the organization of the ECM itself (Weber et al., 2017) (Table 1). Hyaluronan, the most abundant GAG (Iozzo and Schaefer, 2015; Theocharis et al., 2016), heparan sulphate or chondroitin sulphate (Lelongt and Ronco, 2003) are involved in tissue development, by displaying growth factors spatial-temporal distribution during epithelial branching (Nigam and Bush, 2014). ECM-renal cells interact through ECM-binding transmembrane receptors such as integrins (Chen et al., 2004; Clause and Barker, 2013; Handorf et al., 2015; Bülow and Boor, 2019) or polycystins (Nickel et al., 2002) that translate ECM biomechanical features into intracellular signals (Hagelaars et al., 2022). In diabetic nephropathy (Kolset et al., 2012) or autosomal dominant polycystic kidney disease (ADPKD) (Zhang et al., 2020), ECM disruptions result in alterations in kidney function. Changes in ECM synthesis and turnover of laminin, heparan sulphate, and chondroitin sulphate proteoglycans contribute to disease pathogenesis (Zhang et al., 2020). Unresolved renal parenchyma damage causes scarring by abnormal deposition of ECM. Chronic damage or excessive scarring leads to fibrosis, a hallmark of chronic kidney disease (Clause and Barker, 2013; Bülow and Boor, 2019). Any in vitro model aiming to accurately represent kidney function, damage, and regeneration should incorporate the ECM compartment. We review ECM’s role in in vitro kidney models. Established models are briefly discussed to better understand the advantages of new methodological developments.
TABLE 1.
Role of ECM in in vitro models of renal function and disease.
| 2D models | |||||
|---|---|---|---|---|---|
| Culture architecture | ECM surrogate | Cells | Biological structure | Application | References |
| Coated PS plates | Fibronectin, laminin, collagen type IV and Matrigel | hESCs | Differentiated PT-like cells monolayer | Induced Differentiation to PT | Narayanan et al. (2013) |
| Coated glass plates and electrospun PCL-BU membranes | PCL-BU vs Collagens, laminin, MG, L-Dopa | HK-2, RPTEC | Differentiated PT-like cells monolayer | Synthetic membrane for BAK | van Gaal et al. (2021) |
| Coated PES/PVP/PSF-FC membranes | Collagen I, collagen IV, Laminin, L-DOPA | HPTCs, HK-2 | Differentiated PT-like cells monolayer | Synthetic membrane for BAK | Ni et al. (2011) |
| Coated PS- and PES-microstructured substrates | L-DOPA, collagen IV | ciPTEC | Monolayer of differentiated PT-like cells | Synthetic membrane for BAK | Hulshof et al. (2018) |
| Coated microPES hollow fiber membrane | L-DOPA, collagen IV | ciPTEC | Monolayer of differentiated PT-like cells | Synthetic membrane for BAK | Jansen et al. (2015) |
| Coated PE and PES-50 transwell membrane | L-DOPA, collagen IV | ciPTEC | Monolayer of differentiated PT-like cells | Synthetic membrane for BAK | Schophuizen et al. (2015) |
| Hydrogel bioprinted onto polyester Transwell membrane | Organovo’s NovoGel Bio-Ink | RPTEC Renal fibroblasts and HUVEC | RPTEC monolayer on top of hydrogel with HUVEC and fibroblasts | Differentiation CTX Fibrosis | King et al. (2017) |
| Coated Polycarbonate porous membrane within a microchip | Matrigel | RPTECs | Monolayer of differentiated PT-like cells | Synthetic membrane for BAK | Gao et al. (2011) |
| 2.5D Models | |||||
| Culture architecture | ECM surrogate | Cells | Biological structure | Application | References |
| Coated Micropatterned Silicon-PDMS surfaces | Fibronectin, laminin, matrigel. Matrigel in medium | MDCK, RPTEC, LLC-PK1 | Cysts and tubules (PT) | Morphogenesis Nephrotoxicity | Bosch-Fortea et al. (2019) |
| Hydrogels Coated PS plates | Matrigel | HPTCs | Tubules (PT) | Morphogenesis | Zhang et al. (2011) |
| 3D Models | |||||
| Culture architecture | ECM surrogate | Cells | Biological structure | Application | References |
| Hydrogel | 20% Growth factor-depleted Matrigel 80%Collagen I | Mouse embryonic UB and BSN primary cells mIMCD3 | Cysts and tubules (UB) | Tubulogenesis Development | Sakurai et al. (1997) |
| Hydrogel | Matrigel | Primary baby mouse kidney epithelial cells | Tubules | Tubulogenesis | Taub et al. (1990) |
| Hydrogel | Rat tail collagen type I | Primary murine renal cells | Tubule- and glomerulus-like structures | Morphogenesis | Joraku et al. (2009) |
| 0.4 µm Polyester Transwell membranes | Matrigel and collagen I (1:1) | RPTEC | Tubules (PT) | Tubulogenesis | Miya et al. (2011) |
| 0.4 µm polycarbonate Transwell membranes | Matrigel and rat tail collagen I (1:1) | NKi-2 | Tubules | Morphogenesis Nephrotoxicity | DesRochers et al. (2013) |
| Hydrogel | Collagen | MDCK co-cultured with Swiss 3T3 | Tubules (Distal nephron) | Morphogenesis | Montesano et al. (1991a) |
| Hydrogel | Collagen | MDCK and co-cultured with MRC-5 | Tubules (Distal nephron) | Morphogenesis | Montesano et al. (1991b) |
| Hydrogel | Collagen | HK-2 | Tubules (PT) | Morphogenesis | Kher et al. (2011) |
| Hydrogel | Matrigel | Mouse renal tubule fragments | Cysts and tubules (Collecting Duct) | Genetic disease (ADPKD) | Dixon et al. (2020) |
| Hydrogel | Growth factor reduced, phenol red-free Matrigel | RPTEC/TERT1 | Tubules (PT) | Nephrotoxicity | Secker et al. (2018) |
| Casting molds in 12-well plate | Collagen-Matrigel | Neonatal rat renal cells | Tubule- and glomerulus-like structures | Morphogenesis | Lü et al. (2012) |
| Round bottom microwell plate | GFR-Matrigel | MDCK | Tubules (distal nephron) | Morphogenesis | Hirashima et al. (2017) |
| Hydrogel | Collagen I, GRF-Matrigel | RPTEC, renal fibroblasts and HUVEC | Tubules (PT) and endothelial unit | Tubulo-vascular interactions | Wang et al. (2020) |
| Printed silicon gasket | Gelatin, Fibrinogen | PTECT-TERT1, GMECs | Tubules (PT) and endothelial unit | Epithelial transport Tubulo-vascular interactions | Lin et al. (2019) |
| Hydrogel | Collagen I | HKC-8 and WS-1 | HKC-8 monolayer on top of WS-1 embeded hydrogel | Fibrosis Nephrotoxicity | Moll et al. (2013) |
| Polystyrene multiwell plate | Covalent polymer networks of heparin and/or starPEG | HK-2 | Tubules (PT) | Tubulogenesis | Weber et al. (2017) |
| PEGDA Hydrogel | HA | Mouse proximal tubule cells | Tubules (PT) | Nephrotoxicity | Astashkina et al. (2012); Astashkina et al. (2014) |
| Hydrogel | HA Matrigel | Embryonic rat UB | Tubules (UB) | Morphogenesis | Rosines et al. (2007) |
| PEG hydrogel | PEG functionalized with RGD peptide, laminin-1 | MDCK | Cysts | Epithelial morphogenesis | Chung et al. (2008) |
| Scaffold | Silk | hiPSCs | Organoids | Development Differentiation | Gupta et al. (2019) |
| Scaffold | Thiol-ene crosslinked alginate | hiPSCs | Organoids | Development Differentiation | Geuens et al. (2021); Ruiter et al. (2022) |
| Scaffold | PLA Matrigel-Geltrex | HRECs | Monolayer- | ECM biomechanical properties | Love et al. (2019) |
| Hydrogel | PEG-4-MAL | MDCK | Cysts | ECM biomechanical properties | Enemchukwu et al. (2016) |
| PCLdi (u-UPy) electro-spun HFM | Collagen I, IV, fibronectin, laminin | hRPTECs | Monolayer | Bioactive membranes for BAKs | Dankers et al. (2011) |
| Electrospun transwell membrane | 1:1 dKECM-PLC | hRPCs HUVEC | Monolayer | Differentiation Tubule-Vascular unit Nephrotoxicity | Sobreiro-Almeida et al. (2019); Sobreiro-Almeida et al. (2020) |
| Melt-electrowritten tubular scaffold | PCL | ciPTEC HUVEC | Monolayer Self-produced ECM | Tubule-Vascular unit Bioactive membranes for BAKs | van Genderen et al. (2021) |
| Silk-based porous scaffold | Matrigel and Collagen-Matrigel | MEK | Tubules and cysts | Genetic disease (ADPKD) | Subramanian et al. (2010) |
| Silk-based porous scaffold | Collagen type I and Matrigel (1:1) | mIMCD | Cysts | Genetic disease (ADPKD) | Subramanian et al. (2012) |
| Hollow tubes insidehydrogel | Collagen I | MDCK Primary PCT from transgenic mice | Tubules | Genetic disease (ADPKD) | Myram et al. (2021) |
| Extruded topographic hollow fiber (h- FIBER) | RGD-conjugated alginate | Podocytes and endothelial cells | Tubules Glomerulus-like structure | Glomerular filtration studies | Xie et al. (2020) |
| EDC hollow fibers | Collagen IV | HK-2 | Tubules (PT) | Bioengineering renal tubules | Shen et al. (2015) |
| MicroPES HFM | Collagen IV and L-DOPA | ciPTEC | Tubules (PT) | Bioactive membranes for BAKs | Chevtchik et al. (2016) |
| PCL tubular nanofiber scaffold | Collagen IV and L-DOPA | ciPTEC-OAT1 | Tubules (PT) | Bioactive membranes for BAKs Nephrotoxicity | Jansen et al. (2019) |
| Bioprinted Scaffolds | |||||
| Culture architecture | ECM surrogate | Cells | Biological structure | Application | References |
| Bioprinted renal constructs | dKECMMA | Human primary kidney cells | Tubular Glomerular-like structures | Tissue bioengineering | Ali et al. (2019) |
| Bioprinted renal construct | dKECM Gelatin | hRPCs HUVEC, podocytes | 3D glomerular model | Regenerative medicine | Sobreiro-Almeida et al. (2021) |
| Bioprinted hollow tubules | dECM and alginate | RPTEC, HUVEC, hBMMSCs | Perfused Tubules and capillaries | Regenerative medicine | Singh et al. (2020) |
| Bioprinted hollow tubules | Gelatin-fibrin hydrogel | RPTEC/TERT1, GMECs | Perfused Tubules and capillaries | Tubule-Vascular unit Nephrotoxicity | Homan et al. (2016); Lin et al. (2019); Aceves et al. (2022) |
| Hydrogel-sandwiched, bioprinted tubular structure | Collagen I, Matrigel, Fibrin | RPTEC/TERT1, iRECs | Perfused Tubules | Bioengineering renal tubules | Tröndle et al. (2021) |
Natural polymers: HA: hyaluronic acid, FMB: fibrin microbreads, dKECMMA: photo-crosslinable kidney ECM-derived bioink.
Synthetic polymers: EDC: 1-ethyl-3-(3- (dimethylamino)propyl) carbodiimide hydrochloride, PA: polyacrylamide.
Cell lines: HUTECs: Primary human tubular epithelial cells, HK-2: Human kidney-2, HPTCs: Human primary renal proximal tubule cells, RPTECs: renal proximal tubular epithelial cells, hESCs: embryonic stem cells, HUVEC: human umbilical vein endothelial cells, NKi-2: human renal epithelial cells, MDCK: Madin-Darby canine kidney, MRC-5: human fibroblasts, MEK: mouse embryonic kidney, HK-2: human immortalized proximal tubule epithelial cells, ciPTECs: Conditionally immortalized proximal tubule epithelial cells, HRECs: Human renal epithelial cells, LLC-PK1: pig kidney epithelial cells, 3T3: fibroblasts, UB: ureteric bud,HEK-293: Human embryonic kidney cell line, CaKi-1: human renal cancer cells, mIMCD: mouse inner medullary collecting duct, GMECs: glomerular microvascular endothelial cells, HKC-8: human proximal tubular epithelial cells, WS-1: human dermal fibroblasts, hBMMSCs: human bone marrow-derived mesenchymal stem cells, GMECs: glomerular microvascular endothelial cells, iRECs: induced renal tubular epithelial cells.
Extracellular matrix sources for in vitro models
In vivo, stromal cells (fibroblasts) produce ECM, and renal epithelial cells contribute themselves to BM synthesis, which can be exploited in in vitro models (Satyam et al., 2020). Simple ECM proteins like laminins are commercially available as recombinant proteins with proven utility for in vitro kidney models (Karamessinis et al., 2002; Chung et al., 2008; Zhang et al., 2009; Sebinger et al., 2013; Homan et al., 2019; Adelfio et al., 2020). However, most in vitro research uses ECM extracts from animal tissues because it is difficult to make complex macromolecular GAGs and large proteoglycans (Petkau-Milroy and Brunsveld, 2013; Aisenbrey and Murphy, 2020; Xing et al., 2020). Stroma-rich tissues like bone or cartilage can yield large quantities of pure ECM components. Commercial sources for human and animal collagen in various isoforms, hyaluronic acid, and fibronectin are available.
The biochemical complexity present in the original tissue is required to induce or maintain a specific phenotype. Here it is best to use complex, unfractionated tissue extracts containing a complex mix of glycosaminoglycans and other signaling molecules. Several commercial products, the best known being Matrigel (Kleinman and Martin, 2005; Passaniti et al., 2021), are readily available in different formulations (e.g., reduced growth factors). There are many examples of in vitro renal models employing such extracts (Zhang et al., 2009; Lam et al., 2014; Takasato et al., 2015; Figliuzzi et al., 2017; King et al., 2017; Hiraki et al., 2018; Howden et al., 2019; Otero et al., 2020) (Supplementary Table S1). Matrigel complexity (contains laminin, collagen IV, entactin, heparan sulfate proteoglycan and bound growth factors) yields better results than gelatin, collagen I, poly-L-lysine, and laminin alone (Hughes et al., 2010; Gao et al., 2011; Passaniti et al., 2021).
Matrigel-like products are expensive, batch-variable, ethically questionable (made from tumors grown in animals) and cannot be employed in human cell-therapy downstream applications. To solve recent availability and ethics-related issues, JellaGel, made from jellyfish Collagen 0 isolates, has recently become available. However, this formulation does not fully mimic the kidney ECM’s specific proteomic signature. ECM extracts from decellularized human kidneys can capture this specificity (Figliuzzi et al., 2017; Hiraki et al., 2018).
In recent years, artificial ECMs have been designed to replace natural ECM for renal epithelium scaffolding to reduce batch variability and degradation. This alternative allows more control over biochemical and mechanical properties and functionalization with instructive biomolecular tags to enhance cell attachment, proliferation, and differentiation (Aisenbrey and Murphy, 2020). Synthetic ECMs can be formed as hydrogels (Minuth et al., 2004; Chung et al., 2008; Astashkina et al., 2012) or hollow fibers (Dankers et al., 2011; Jansen et al., 2015; Shen et al., 2015; Chevtchik et al., 2016; Jansen et al., 2019; Xie et al., 2020; Myram et al., 2021) (Supplementary Table S1). The goal is to obtain a material whose composition can be tailored to control physiochemical matrix properties such as elasticity (Love et al., 2019), density, and stiffness, while ensuring low degradation under specific conditions (Petkau-Milroy and Brunsveld, 2013; Cruz-Acuña et al., 2019).
Conventional models of kidney function and disease
Two-dimensional renal cell culture on extracellular matrix-Coated surfaces
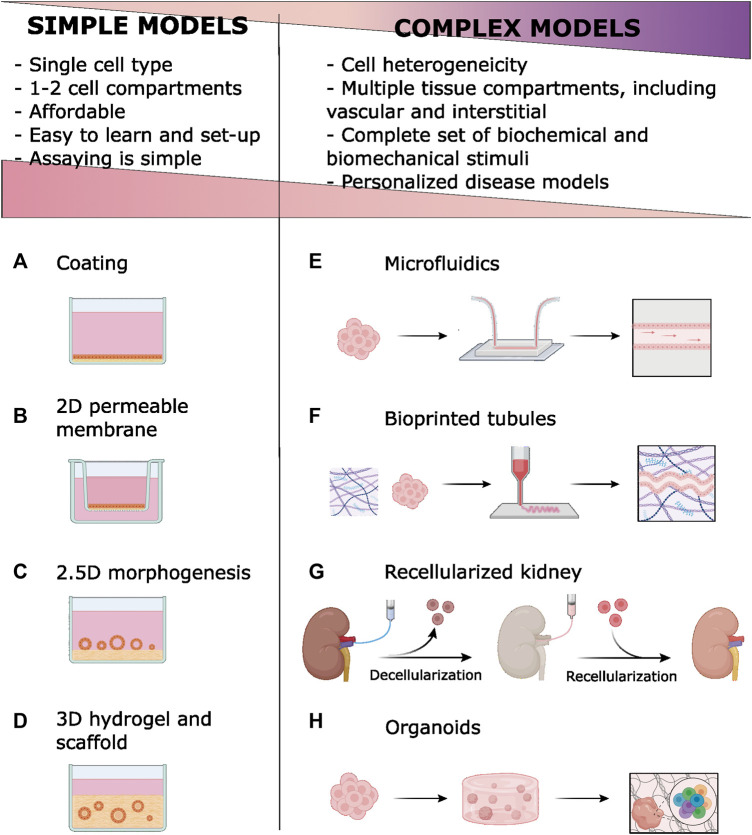
In the simplest culture configuration, renal cells grew directly on plastic surfaces as two-dimensional (2D) epithelial monolayers (Figure 1A). Adsorbing (coating) ECM components on plastic surfaces enhances renal cell adhesion, proliferation, and differentiation (Narayanan et al., 2013; van Gaal et al., 2021). Matrigel’s complex set of biochemical signals is used when cell differentiation is the goal (Narayanan et al., 2013). ECM coatings are also used to functionalize synthetic scaffolds (Chung et al., 2008; Ni et al., 2011). Relevant examples of 2D in vitro kidney models are provided in Table 1. However, lack of complex cell interactions can lead to undesired effects, such as epithelial-to-mesenchymal transition (EMT) (Forino et al., 2006).
FIGURE 1.
Simple models in vitro of renal epithelia employ ECM components of basal membrane (BM) and extracellular matrix (ECM) Coatings are simply ECM materials, usually collagen, adsorbed to the plastic (A) or permeable membrane (B). Permeable membranes and scaffold-based models improve epithelial polarity by offering two fluid compartments. Tubulogenesis is stimulated by growing renal epithelial cells onto (C) or within (D) hydrogels. New technologies [microfluidics (E), bioprinting (F), ECM decellularization (G) and organoids development (H)] enable complex models that introduce cell heterogeneity, vascular and interstitial compartments, and biomechanical stimuli. Compared to simpler, conventional models, these models have disadvantages related to their complexity. However, complex models allow for more faithful modeling of kidney function and disease. A licensed version of BioRender was used to prepare this figure.
Epithelial 2D monolayers are frequently grown on permeable supports, like the Transwell system, to promote cell polarization (Gao et al., 2011; Ni et al., 2011; Shamir and Ewald, 2014; Schophuizen et al., 2015; Hulshof et al., 2018) (Figure 1B). Porous membranes can be coated with ECM (Ni et al., 2011; Shamir and Ewald, 2014) or used as scaffolds for thin hydrogels to improve mechanical properties (Shamir and Ewald, 2014) (Table 1). This configuration also facilitates co-culture with other kidney-relevant components (King et al., 2017).
When grown on top of hydrogels, kidney primary cells (Zhang et al., 2011) and most renal cell lines form tubular structures (tubulogenesis; termed 2.5D architecture; Figure 1C). Formation of tubules requires adding Matrigel to the hydrogel and/or to the medium, stressing the need for specific ECM chemical signals (Shamir and Ewald, 2014; Bosch-Fortea et al., 2019). Tubulogenesis studies on the MDCK cell line have been instrumental for understanding molecular the processes involved in epithelial differentiation and polarization (Bosch-Fortea et al., 2019). Hagelaars et al. have recently used this model to show cellular differences in how matrix stiffness affects integrin-mediated cell-ECM attachment and cell polarization (Hagelaars et al., 2022). Better differentiation can happen when the tubule is fully embedded in the ECM (3D architecture, discussed below), however, direct exposure to culture medium in 2.5D structures facilitates imaging and biochemical treatments and assays.
Three-dimensional renal cell culture in hydrogel and scaffolds
Primary or continuous renal cell lines grown within collagen I or Matrigel hydrogels spontaneously form tubule-like structures (Taub et al., 1990; Sakurai et al., 1997; Zegers et al., 2003; Joraku et al., 2009; Schlüter and Margolis, 2009) (Figure 1D). Dissociated cells are mixed with biocompatible hydrogels in liquid form and allowed to polymerize (Miya et al., 2011; DesRochers et al., 2013). Alternatively, cells can be sandwiched between two ECM layers (Montesano et al., 1991a; Montesano et al., 1991b; Kher et al., 2011; Secker et al., 2018; Dixon et al., 2020) In the presence of appropriate factors, cells form hollow cysts (Zegers et al., 2003; Schlüter and Margolis, 2009) and continue to differentiate by elongation (Joraku et al., 2009) and tubule branching. Different nephron segments, including the glomerulus, have been modeled in 3D hydrogels (Joraku et al., 2009; Lü et al., 2012; Hirashima et al., 2017).
3D-culture allows co-culturing of different renal cell lineages, introducing complexity in kidney models (Montesano et al., 1991a; Montesano et al., 1991b; Secker et al., 2018). Wang et al. showed that using a sandwich 3D co-culture model is possible to recreate in vitro the tubule-interstitial-vascular unit, with more tubular cell polarity and enhanced functional gene expression (Wang et al., 2020). Gelatin-fibrin hydrogels outperformed conventional Transwell co-culture in modeling the proximal tubule-vascular unit in vitro (Lin et al., 2019). Tubulointerstitial fibrosis, a common feature in chronic kidney disease, has been modeled in 3D co-cultures (Moll et al., 2013).
Collagen I and Matrigel-like ECM extracts are often used, alone, mixed, or combined with other ECM components like collagen IV, fibronectin, or laminins (Weber et al., 2017). Functionality depends on the 3D hydrogel’s composition, protein concentration, and stiffness (Shamir and Ewald, 2014; Hirashima et al., 2017; Hiraki et al., 2018). Hyaluronic acid is an interesting alternative to tissue extracts because it provides good mechanical and biochemical stimuli. 3D organoids containing proximal tubule structures were generated from mouse kidney explants by prolonged (6 weeks) culture in hyaluronic acid hydrogels resembling in vivo environment (Astashkina et al., 2012). This model has been successfully employed in the preclinical evaluation of nanoparticle nephrotoxicity (Astashkina et al., 2014). Hyaluronic acid modulated ureteric bud branching and promoted mesenchymal-to-epithelial transition (Rosines et al., 2007). The polarity of tubular structures obtained by growing human renal cells (HK-2, ciPTEC, and primary proximal tubule cells) in glycosaminoglycan-based hydrogels was found to depend on sulphated GAGs (Weber et al., 2017). Matrix stiffness strongly affects tubulogenesis in MDCK cells (Hirashima et al., 2017). Such studies (Table 1) exemplify how morphogenesis and function can be modulated by adjusting hydrogel degradability, growth factor signaling, and mechanics.
ECM-derived hydrogels have low resistance to mechanical stress, partly a consequence of active cell remodeling, limiting their use. A potential solution is to exploit the mechanical properties of natural (silk, alginate) or synthetic (PEG, PCL, PLA) polymers to complement natural ECM components (Chung et al., 2008; Enemchukwu et al., 2016; Gupta et al., 2019) (Supplementary Table S2). Plastic materials are easily deposited in 2D or 3D structures by electrospinning or printing techniques (Dankers et al., 2011; Sobreiro-Almeida et al., 2020; van Genderen et al., 2021). Murine PKD1 knockout renal tubular cells seeded in silk-scaffolds filled with Matrigel and collagen hydrogels has been shown to reproduce morphological and functional abnormalities present in Autosomal Dominant Polycystic Kidney disease (ADPKD) (Subramanian et al., 2010; Subramanian et al., 2012).
Recently, 3D models have gained momentum with microfabrication techniques. The organ-on-a-chip technology aims to mimic in vivo tissue architecture by providing independent but connected compartments (Rayner et al., 2018) (Figure 1E). Models based on microfabricated devices recapitulate intercellular and cell-ECM interactions at the microscale. Microfluidics integration adds flow-mediated shear stress, a critical mechanical stimulus for the renal tubule (Jang et al., 2013). Mimetas Organoplate allows for a high throughput culture and analysis of 3D tissue units under fluidic stimulus (Schutgens et al., 2019) and it has proven useful in modeling nephrotoxicity (Vormann et al., 2021) and acute kidney injury (Vormann et al., 2022). Commercial organ-on-chip solutions are listed in Supplementary Table S2.
3D models of tubulogenesis have been instrumental in defining chemical and mechanical stimuli involved in ECM-cell interactions and their role in kidney development and function. Lumen access, high-resolution imaging, biochemical studies, and manipulation for functional or nephrotoxicity assays are, however, limited in their architecture.
New strategies in in vitro modeling of kidney function and disease
Bioprinted scaffolds
Bioprinting has recently emerged as a tool for building complex tissue structures. Biocompatible polymers (bioinks) are layered to create 3D structures (Figure 1F). Cells are seeded on these 3D scaffolds or directly mixed in the bioink. Bioprinting offers unprecedented flexibility and versatility to recreate in vivo environments at the microscale through stereotaxic control of bioink deposition (Fransen et al., 2021).
Bioinks are chosen for their rheological properties and printing device compatibility. As technology evolves, the use of bioinks derived from native tissue like collagen and decellularized ECM is favored (Garreta et al., 2017; Ali et al., 2019; Dzobo et al., 2019; Sobreiro-Almeida et al., 2021). This enhances kidney-specific gene expression by providing tissue-specific biochemical cues (Singh et al., 2020). However, because ECM bioinks exhibit poor mechanical stability, they are often combined with other polymers like methacrylate (Ali et al., 2019).
Using bioprinting, perfused renal tubules have been successfully made. Lewis’s group used fugitive ink to cast tubular conduits within hydrogels, which they populated with proximal tubule cells or endothelial cells and perfused in a closed circuit for days. These tubular-vascular units expressed differentiated phenotypes, and their response to pathogenic insults mimicked those observed in native human tissues (Homan et al., 2016; Lin et al., 2019; Aceves et al., 2022). Tröndle et al. recently reported a modified 3D sandwich model in which renal cells were bioprinted as clusters at a controlled topography on a collagen and Matrigel substrate gel. Cell clusters formed lumen-containing spheroids, which coalesced into tubular structures that could be connected to fluidic systems (Tröndle et al., 2021). Both strategies use fibrin polymers to improve hydrogel biomechanics. A third strategy used a proprietary bioprinting technology (the Organovo 3D printing platform) to sequentially print epithelial tubule, fibroblast-containing ECM, and endothelial vessels (King et al., 2017). A glomerular functional unit was successfully recreated by printing hollow tubules from a functional hybrid bioink (alginate plus decellularized ECM) (Singh et al., 2020).
Bioprinting’s flexibility and automatization capabilities make it a promising method for in vitro modeling of the kidney’s basic functional unit. An immediate challenge is to make it affordable for the general laboratory.
Decellularized kidney as a tissue-specific scaffold
Regenerative medicine has long sought to fabricate a functional kidney using a donor’s decellularized ECM scaffold repopulated with host cells to mitigate the shortage of organs available for transplant (Sullivan et al., 2012). The technique involves perfusing whole kidneys with detergent solutions to remove cells and preserve ECM microscopic architecture and tissue-specific ECM components like collagens and laminins, as well as basement membranes (Song et al., 2013) (Figure 1G). Conservation of signaling molecules, namely glycosaminoglycans, requires proper detergent composition and perfusion rates and timing (Caralt et al., 2015; Poornejad et al., 2016; He et al., 2017; Kajbafzadeh et al., 2019; Zhou et al., 2020; Shahraki et al., 2022). Decellularization can be successfully applied to stored frozen tissues (Chani et al., 2017). Decellularized scaffolds have been successfully repopulated with pluripotent, progenitor, epithelial, or endothelial cells. When implanted in animal models, this bioengineered tissue integrates with host structures and shows some kidney functions (Bonandrini et al., 2014; Caralt et al., 2015; Figliuzzi et al., 2017; Ciampi et al., 2019; Han et al., 2019; Zhang et al., 2019) or helps to revert EMT and fibrosis (Hu et al., 2020).
Regenerating a fully functional organ from a decellularized scaffold is a formidable challenge because of the kidney’s high structural and functional complexity. Nevertheless, studies on kidney decellularization have provided valuable information on cell-ECM interactions, supporting GAGs’ critical role (Louzao-Martinez et al., 2019; Ullah et al., 2020). Moreover, decellularized scaffolds are useful for in vitro method development. Decellularized kidney sections serve as scaffolds for growing renal cells in nephrotoxicity models (Fedecostante et al., 2018). These scaffolds allow for the investigation of cell-ECM interactions in specific organ or tissue microdomains. For example, the fate of pluripotent or progenitor cells in a recellularized scaffold can be followed to learn about specific cell differentiation determinants (Du et al., 2016; Bombelli et al., 2018; Zhang et al., 2019; Bombelli et al., 2020; Ullah et al., 2020).
An acid hydrolysate of decellularized kidney scaffolds, termed dKECM, can be used as a source of tissue-specific ECM materials for surface coating and hydrogel fabrication (Hiraki et al., 2018; Zhou et al., 2020; Shen et al., 2021; Lee et al., 2022). Combining dKECM with other natural or synthetic compounds can enhance their rheological or biophysical properties (Lih et al., 2019; Sobreiro-Almeida et al., 2019; Sobreiro-Almeida et al., 2020; Geng et al., 2021; Ko et al., 2021; Sobreiro-Almeida et al., 2021). Accordingly, dKECM is becoming a favorite bioink in bioprinting applications (Ali et al., 2019; Han et al., 2019). The undesired effects observed when growing human glomerular endothelial cells within hydrogels made of porcine dKECM (Su et al., 2018) illustrates the remarkable specificity of biochemical signals delivered by ECM.
Role of ECM in kidney organoids development
Two strategies are currently used to develop 3D renal structures from progenitor or pluripotent cells by exploiting kidney development programs. Tubuloids are generated from primary cells and kidney organoids from pluripotent stem cells. Both situations require ECM components. Tubuloid culture is a refined version of 3D culture in Matrigel hydrogels where specific biochemical factors are added to stimulate progenitor cell proliferation and differentiation (Schutgens et al., 2019; Wiraja et al., 2021). Human tubuloid culture allows for long-term propagation of donor-specific primary kidney epithelium without requiring immortalization or genetic modification. A recent study comparing the polarization of tubuloid-derived cells and MDCK cells in response to substrate stiffness demonstrated tubuloid-derived cells appear to have different requirements and use different polarization mechanisms (Hagelaars et al., 2022). Unlike tubuloids, immortalized, well-established cell lines have been selected to grow on plastic substrates. By skipping the phase of culture on a stiff substrate, tubuloids might retain more of their physiological responses to ECM. This makes them a simple and affordable alternative cell source for in vitro models.
In the organoid technique (Figure 1H), Matrigel (Xia et al., 2013; Kang and Han, 2014; Takasato et al., 2015; Takasato and Little, 2017; Howden et al., 2019; Low et al., 2019) or Geltrex (Lam et al., 2014; Morizane et al., 2015; Morizane and Bonventre, 2017) coatings or hydrogels are used in feeder-free culture of stem cells or at several differentiation steps. For instance, Taguchi et al. used a 50% Matrigel culture medium to stimulate branching morphogenesis in ureteric buds and to induce interactions with nephron progenitors (Taguchi and Nishinakamura, 2017). Freedman et al. induced epiblast spheroids differentiation by sandwiching hPSC between two layers of diluted Matrigel (Freedman et al., 2015). Under the appropriate concentration and timing of specific biochemical inducers, complex self-organized 3D structures develop.
Organoids contain kidney parenchyma and stroma components, and the synthesis of ECM has been observed (Lam et al., 2014; Takasato et al., 2015; Howden et al., 2019). Given the complexity and animal origin of Matrigel and similar products, there have been efforts to replace it with recombinant ECM proteins, such as laminins (Howden et al., 2019; Mae et al., 2020) or vitronectin (van den Berg et al., 2018), or synthetic products like Synthemax (Toyohara et al., 2015). Recently, Geunes et al. cultured kidney organoids in thiol-ene cross-linked alginate hydrogels and showed a reduction in the onset of aberrant ECM expression and off-target cell populations (Geuens et al., 2021). By engineering gel mechanics and dynamics, ECM deposition and organoid maturation could be tuned, highlighting the role of engineered matrices in stirring organoid commitment (Ruiter et al., 2022).
Incomplete maturation and lack of vascularization are unsolved issues in organoid development where a proper selection and use of ECM components could help. Garreta et al. demonstrated that ECM biophysical properties modulate hPSC proliferation and differentiation (Garreta et al., 2019). Soft hydrogels with stiffness in the physiological range better mimic the early stages of embryonic development. Vascular compartment expression improved when organoids were grown in hydrogels made from decellularized human kidney extracellular matrix (Kim et al., 2022). Bioprinting cellular bioinks allows for precise and reproducible manipulation of organoid size and more differentiated cells (Howden et al., 2019; Lawlor et al., 2021). Perfusion of organoids in microfluidic devices induces higher expression of vascular and podocyte compartments (Homan et al., 2016; Lee et al., 2021). High levels of structural and functional complexity in bioprinted, perfused organoids model more faithfully renal function and disease, as shown recently for APKD (Howden et al., 2021; Hiratsuka et al., 2022).
Relevance of ECM-based in vitro models of renal disease for studies of renoprotection and kidney regeneration
Increasing rates of chronic kidney disease (CKD) represent a major burden for social and healthcare systems worldwide. Fighting underlying causes (diabetes, obesity, cardiovascular disease, etc.) is key. But it is equally important to prevent, slow down, or reverse CKD progression, which very often results from maladaptive responses to acute kidney injury.
Shortcomings of traditional preclinical models (animal experimentation and conventional cell culture) have fueled the development of sophisticated in vitro kidney models that take advantage of recent technological advances (Morizane et al., 2015). Only through such complex models is it possible, for instance, to recreate the delicate glomerular filtration barrier, allowing for the investigation of the varied glomerulopathies (Lü et al., 2012; Du et al., 2016; Xie et al., 2020). Sophisticated models, such as organoids, are already being used successfully to study genetic (e.g., ADPKD (Subramanian et al., 2010; Freedman et al., 2015; Dixon et al., 2020; Zhang et al., 2020; Howden et al., 2021; Myram et al., 2021; Hiratsuka et al., 2022)) or metabolic tubulopathies (Fabry’s disease (Kim et al., 2022)). Investigating the mechanisms of drug-related nephrotoxicity and discovering ways to prevent it is frequently the goal behind model design or validation (Astashkina et al., 2012; DesRochers et al., 2013; King et al., 2017; Fedecostante et al., 2018; Vormann et al., 2021; Tröndle et al., 2022). Research on common mechanisms underlying CKD progression, irrespective of its cause, such as epithelial-to-mesenchymal transition (Forino et al., 2006) or fibrosis (Moll et al., 2013; Hu et al., 2020; Li et al., 2022), requires the presence of all participants in such complex processes. Studying tubulogenesis or cell-repair mechanisms in complex in vitro models helps identification of signals needed for kidney regeneration (Miya et al., 2011). These processes, which involve multiple actors from distinct compartments, cannot be studied adequately with conventional in vitro models. Some bioengineering strategies are originally aimed at fabricating tissue-like structures for regenerative techniques, based on the concept of regenerating an entire organ from a decellularized scaffold (Song et al., 2013; Du et al., 2016; Figliuzzi et al., 2017; Ciampi et al., 2019) or by stimulating regeneration in vivo via cell or tissue implants (Lih et al., 2019; Ko et al., 2021; van den Berg et al., 2018; Garreta et al., 2019; Kim et al., 2022).
We have summarized the essential roles of ECM in in vitro kidney function and disease modeling. ECM provides the biochemical and mechanical stimuli required for promoting and maintaining cell differentiation. A proper 3D architecture also permits cell-cell interactions and facilitates the presence of all necessary compartments, including fluid convection, to faithfully mimic in vivo kidney function. More efforts are needed to make the technical skills required simpler and to lower the costs associated with using such models, which would increase their adoption in kidney translational research.
Acknowledgments
We would like to thank all the excellent technical assistance provided by the people at our institutions that make possible working with complex and sophisticated cell culture models.
Author contributions
All authors: conceptual design, data adquisition and interpretation, critical revision, final approval of the version to be published.
Funding
Publication of this review has been made possible through funds provided by the Government of Spain (RTI2018-0099946-B-100 to I.G.) and a “2017 Research Fellowship” from Sociedad Española de Nefrología.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2022.1048738/full#supplementary-material
References
- Aceves J. O., Heja S., Kobayashi K., Robinson S. S., Miyoshi T., Matsumoto T., et al. (2022). 3D proximal tubule-on-chip model derived from kidney organoids with improved drug uptake. Sci. Rep. 12 (1), 14997. 10.1038/s41598-022-19293-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adelfio M., Szymkowiak S., Kaplan D. L. (2020). Matrigel-free laminin-entactin matrix to induce human renal proximal tubule structure formation in vitro . ACS Biomater. Sci. Eng. 6 (12), 6618–6625. 10.1021/acsbiomaterials.0c01385 [DOI] [PubMed] [Google Scholar]
- Aisenbrey E. A., Murphy W. L. (2020). Synthetic alternatives to matrigel. Nat. Rev. Mat. 5 (7), 539–551. 10.1038/s41578-020-0199-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali M., Pr A. K., Yoo J. J., Zahran F., Atala A., Lee S. J. (2019). A photo-crosslinkable kidney ECM-derived bioink accelerates renal tissue formation. Adv. Healthc. Mat. 8 (7), e1800992. 10.1002/adhm.201800992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astashkina A. I., Jones C. F., Thiagarajan G., Kurtzeborn K., Ghandehari H., Brooks B. D., et al. (2014). Nanoparticle toxicity assessment using an invitro 3-D kidney organoid culture model. Biomaterials 35 (24), 6323–6331. 10.1016/j.biomaterials.2014.04.060 [DOI] [PubMed] [Google Scholar]
- Astashkina A. I., Mann B. K., Prestwich G. D., Grainger D. W. (2012). A 3-D organoid kidney culture model engineered for high-throughput nephrotoxicity assays. Biomaterials 33 (18), 4700–4711. 10.1016/j.biomaterials.2012.02.063 [DOI] [PubMed] [Google Scholar]
- Beamish J. A., Chen E., Putnam A. J. (2017). Engineered extracellular matrices with controlled mechanics modulate renal proximal tubular cell epithelialization. PLoS One 12 (7), e0181085. 10.1371/journal.pone.0181085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bombelli S., Meregalli C., Grasselli C., Bolognesi M. M., Bruno A., Eriani S., et al. (2020). PKHhigh/CD133+/CD24- renal stem-like cells isolated from human nephrospheres exhibit in vitro multipotency. Cells 9 (8), E1805. 10.3390/cells9081805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bombelli S., Meregalli C., Scalia C., Bovo G., Torsello B., De Marco S., et al. (2018). Nephrosphere-derived cells are induced to multilineage differentiation when cultured on human decellularized kidney scaffolds. Am. J. Pathol. 188 (1), 184–195. 10.1016/j.ajpath.2017.09.012 [DOI] [PubMed] [Google Scholar]
- Bonandrini B., Figliuzzi M., Papadimou E., Morigi M., Perico N., Casiraghi F., et al. (2014). Recellularization of well-preserved acellular kidney scaffold using embryonic stem cells. Tissue Eng. Part A 20 (9–10), 1486–1498. 10.1089/ten.TEA.2013.0269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosch-Fortea M., Rodriguez-Fraticelli A. E., Herranz G., Hachimi M., Barea M. D., Young J., et al. (2019). Micropattern-based platform as a physiologically relevant model to study epithelial morphogenesis and nephrotoxicity. Biomaterials 218, 119339. 10.1016/j.biomaterials.2019.119339 [DOI] [PubMed] [Google Scholar]
- Bülow R. D., Boor P. (2019). Extracellular matrix in kidney fibrosis: More than just a scaffold. J. Histochem. Cytochem. 67 (9), 643–661. 10.1369/0022155419849388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caralt M., Uzarski J. S., Iacob S., Obergfell K. P., Berg N., Bijonowski B. M., et al. (2015). Optimization and critical evaluation of decellularization strategies to develop renal extracellular matrix scaffolds as biological templates for organ engineering and transplantation. Am. J. Transpl. 15 (1), 64–75. 10.1111/ajt.12999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chani B., Puri V., Sobti R. C., Jha V., Puri S. (2017). Decellularized scaffold of cryopreserved rat kidney retains its recellularization potential. PLoS One 12 (3), 01730400–e173120. 10.1371/journal.pone.0173040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D., Roberts R., Pohl M., Nigam S., Kreidberg J., Wang Z., et al. (2004). Differential expression of collagen- and laminin-binding integrins mediates ureteric bud and inner medullary collecting duct cell tubulogenesis. Am. J. Physiol. Ren. Physiol. 287 (4 56-4), 602–611. 10.1152/ajprenal.00015.2004 [DOI] [PubMed] [Google Scholar]
- Chen W. C., Lin H. H., Tang M. J. (2014). Regulation of proximal tubular cell differentiation and proliferation in primary culture by matrix stiffness and ECM components. Am. J. Physiol. Ren. Physiol. 307 (6), F695–F707. 10.1152/ajprenal.00684.2013 [DOI] [PubMed] [Google Scholar]
- Chevtchik N. V., Fedecostante M., Jansen J., Mihajlovic M., Wilmer M., Rüth M., et al. (2016). Upscaling of a living membrane for bioartificial kidney device. Eur. J. Pharmacol. 790, 28–35. 10.1016/j.ejphar.2016.07.009 [DOI] [PubMed] [Google Scholar]
- Chung I. M., Enemchukwu N. O., Khaja S. D., Murthy N., Mantalaris A., García A. J. (2008). Bioadhesive hydrogel microenvironments to modulate epithelial morphogenesis. Biomaterials 29 (17), 2637–2645. 10.1016/j.biomaterials.2008.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciampi O., Bonandrini B., Derosas M., Conti S., Rizzo P., Benedetti V., et al. (2019). Engineering the vasculature of decellularized rat kidney scaffolds using human induced pluripotent stem cell-derived endothelial cells. Sci. Rep. 9 (1), 8001. 10.1038/s41598-019-44393-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clause K. C., Barker T. H. (2013). Extracellular matrix signaling in morphogenesis and repair. Curr. Opin. Biotechnol. 24 (5), 830–833. 10.1016/j.copbio.2013.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Acuña R., Mulero-Russe A., Clark A. Y., Zent R., García A. J. (2019). Identification of matrix physicochemical properties required for renal epithelial cell tubulogenesis by using synthetic hydrogels. J. Cell Sci. 132 (20), jcs226639. 10.1242/jcs.226639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dankers P. Y. W., Boomker J. M., Huizinga-van der Vlag A., Wisse E., Appel W. P. J., Smedts F. M. M., et al. (2011). Bioengineering of living renal membranes consisting of hierarchical, bioactive supramolecular meshes and human tubular cells. Biomaterials 32 (3), 723–733. 10.1016/j.biomaterials.2010.09.020 [DOI] [PubMed] [Google Scholar]
- DesRochers T. M., Suter L., Roth A., Kaplan D. L. (2013). Bioengineered 3D human kidney tissue, a platform for the determination of nephrotoxicity. PLoS One 8 (3), e59219. 10.1371/journal.pone.0059219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon E. E., Maxim D. S., Halperin Kuhns V. L., Lane-Harris A. C., Outeda P., Ewald A. J., et al. (2020). GDNF drives rapid tubule morphogenesis in a novel 3D in vitro model for ADPKD. J. Cell Sci. 133 (14), jcs249557. 10.1242/jcs.249557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du C., Narayanan K., Leong M. F., Ibrahim M. S., Chua Y. P., Khoo V. M. H., et al. (2016). Functional kidney bioengineering with pluripotent stem-cell-derived renal progenitor cells and decellularized kidney scaffolds. Adv. Healthc. Mat. 5 (16), 2080–2091. 10.1002/adhm.201600120 [DOI] [PubMed] [Google Scholar]
- Dzobo K., Motaung K. S. C. M., Adesida A. (2019). Recent trends in decellularized extracellular matrix bioinks for 3D printing: An updated review. Int. J. Mol. Sci. 20 (18), E4628. 10.3390/ijms20184628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enemchukwu N. O., Cruz-Acuña R., Bongiorno T., Johnson C. T., García J. R., Sulchek T., et al. (2016). Synthetic matrices reveal contributions of ECM biophysical and biochemical properties to epithelial morphogenesis. J. Cell Biol. 212 (1), 113–124. 10.1083/jcb.201506055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedecostante M., Westphal K. G. C., Buono M. F., Romero N. S., Wilmer M. J., Kerkering J., et al. (2018). Recellularized native kidney scaffolds as a novel tool in nephrotoxicity screening. Drug Metab. Dispos. 46 (9), 1338–1350. 10.1124/dmd.118.080721 [DOI] [PubMed] [Google Scholar]
- Figliuzzi M., Bonandrini B., Remuzzi A. (2017). Decellularized kidney matrix as functional material for whole organ tissue engineering. J. Appl. Biomater. Funct. Mat. 15 (4), e326–e333. 10.5301/jabfm.5000393 [DOI] [PubMed] [Google Scholar]
- Forino M., Torregrossa R., Ceol M., Murer L., Della Vella M., Del Prete D., et al. (2006). TGFbeta1 induces epithelial-mesenchymal transition, but not myofibroblast transdifferentiation of human kidney tubular epithelial cells in primary culture. Int. J. Exp. Pathol. 87 (3), 197–208. 10.1111/j.1365-2613.2006.00479.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fransen M. F. J., Addario G., Bouten C. V. C., Halary F., Moroni L., Mota C. (2021). Bioprinting of kidney in vitro models: Cells, biomaterials, and manufacturing techniques. Essays Biochem. 65 (3), 587–602. 10.1042/EBC20200158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frantz C., Stewart K. M., Weaver V. M. (2010). The extracellular matrix at a glance. J. Cell Sci. 123 (24), 4195–4200. 10.1242/jcs.023820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman B. S., Brooks C. R., Lam A. Q., Fu H., Morizane R., Agrawal V., et al. (2015). Modelling kidney disease with CRISPR-mutant kidney organoids derived from human pluripotent epiblast spheroids. Nat. Commun. 6, 8715. 10.1038/ncomms9715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao X., Tanaka Y., Sugii Y., Mawatari K., Kitamori T. (2011). Basic structure and cell culture condition of a bioartificial renal tubule on chip towards a cell-based separation microdevice. Anal. Sci. 27 (9), 907–912. 10.2116/analsci.27.907 [DOI] [PubMed] [Google Scholar]
- Garreta E., Oria R., Tarantino C., Pla-Roca M., Prado P., Fernández-Avilés F., et al. (2017). Tissue engineering by decellularization and 3D bioprinting. Mat. TodayKidlingt. 20 (4), 166–178. 10.1016/j.mattod.2016.12.005 [DOI] [Google Scholar]
- Garreta E., Prado P., Tarantino C., Oria R., Fanlo L., Martí E., et al. (2019). Fine tuning the extracellular environment accelerates the derivation of kidney organoids from human pluripotent stem cells. Nat. Mat. 18 (4), 397–405. 10.1038/s41563-019-0287-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geng G., Xiao Y., Shang Y., Zhang Y., Zhu F., Tang L., et al. (2021). Naphthalenephenylalanine-phenylalanine-glycine-arginine-glycine-aspartic promotes self-assembly of nephron progenitor cells in decellularized scaffolds to construct bioengineered kidneys. Biomater. Adv. 134, 112590. 10.1016/j.msec.2021.112590 [DOI] [PubMed] [Google Scholar]
- Geuens T., Ruiter F. A. A., Schumacher A., Morgan F. L. C., Rademakers T., Wiersma L. E., et al. (2021). Thiol-ene cross-linked alginate hydrogel encapsulation modulates the extracellular matrix of kidney organoids by reducing abnormal type 1a1 collagen deposition. Biomaterials 275, 120976. 10.1016/j.biomaterials.2021.120976 [DOI] [PubMed] [Google Scholar]
- Gupta A. K., Coburn J. M., Davis-Knowlton J., Kimmerling E., Kaplan D. L., Oxburgh L. (2019). Scaffolding kidney organoids on silk. J. Tissue Eng. Regen. Med. 13 (5), 812–822. 10.1002/term.2830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagelaars M. J., Yousef Yengej F. A., Verhaar M. C., Rookmaaker M. B., Loerakker S., Bouten C. V. C. (2022). Substrate stiffness determines the establishment of apical-basal polarization in renal epithelial cells but not in tubuloid-derived cells. Front. Bioeng. Biotechnol. 10, 820930. 10.3389/fbioe.2022.820930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han W., Singh N. K., Kim J. J., Kim H., Kim B. S., Park J. Y., et al. (2019). Directed differential behaviors of multipotent adult stem cells from decellularized tissue/organ extracellular matrix bioinks. Biomaterials 224, 119496. 10.1016/j.biomaterials.2019.119496 [DOI] [PubMed] [Google Scholar]
- Handorf A. M., Zhou Y., Halanski M. A., Li W. J. (2015). Tissue stiffness dictates development, homeostasis, and disease progression. Organogenesis, 11 (1), 1–15. 10.1080/15476278.2015.1019687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He M., Callanan A., Lagaras K., Steele J. A. M., Stevens M. M. (2017). Optimization of SDS exposure on preservation of ECM characteristics in whole organ decellularization of rat kidneys. J. Biomed. Mat. Res. B Appl. Biomater. 105 (6), 1352–1360. 10.1002/jbm.b.33668 [DOI] [PubMed] [Google Scholar]
- Hiraki H. L., Nagao R. J., Himmelfarb J., Zheng Y. (2018). Fabricating a kidney cortex extracellular matrix-derived hydrogel. J. Vis. Exp. 140, e58314. 10.3791/58314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirashima T., Hoshuyama M., Adachi T. (2017). In vitro tubulogenesis of Madin–Darby canine kidney (MDCK) spheroids occurs depending on constituent cell number and scaffold gel concentration. J. Theor. Biol. 435, 110–115. 10.1016/j.jtbi.2017.09.009 [DOI] [PubMed] [Google Scholar]
- Hiratsuka K., Miyoshi T., Kroll K. T., Gupta N. R., Valerius M. T., Ferrante T., et al. (2022). Organoid-on-a-chip model of human ARPKD reveals mechanosensing pathomechanisms for drug discovery. Sci. Adv. 8 (38), eabq0866. 10.1126/sciadv.abq0866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan K. A., Gupta N., Kroll K. T., Kolesky D. B., Skylar-Scott M., Miyoshi T., et al. (2019). Flow-enhanced vascularization and maturation of kidney organoids in vitro . Nat. Methods 16 (3), 255–262. 10.1038/s41592-019-0325-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan K. A., Kolesky D. B., Skylar-Scott M. A., Herrmann J., Obuobi H., Moisan A., et al. (2016). Bioprinting of 3D convoluted renal proximal tubules on perfusable chips. Sci. Rep. 6, 34845. 10.1038/srep34845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howden S. E., Vanslambrouck J. M., Wilson S. B., Tan K. S., Little M. H. (2019). Reporter‐based fate mapping in human kidney organoids confirms nephron lineage relationships and reveals synchronous nephron formation. EMBO Rep. 20 (4), 474833–e47513. 10.15252/embr.201847483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howden S. E., Wilson S. B., Groenewegen E., Starks L., Forbes T. A., Tan K. S., et al. (2021). Plasticity of distal nephron epithelia from human kidney organoids enables the induction of ureteric tip and stalk. Cell Stem Cell 28 (4), 671–684.e6. e6. 10.1016/j.stem.2020.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu D., Zhang D., Liu B., Liu Y., Zhou Y., Yu Y., et al. (2020). Human ucMSCs seeded in a decellularized kidney scaffold attenuate renal fibrosis by reducing epithelial-mesenchymal transition via the TGF-β/Smad signaling pathway. Pediatr. Res. 88 (2), 192–201. 10.1038/s41390-019-0736-6 [DOI] [PubMed] [Google Scholar]
- Hughes C. S., Postovit L. M., Lajoie G. A. (2010). Matrigel: A complex protein mixture required for optimal growth of cell culture. Proteomics 10 (9), 1886–1890. 10.1002/pmic.200900758 [DOI] [PubMed] [Google Scholar]
- Hulshof F., Schophuizen C., Mihajlovic M., van Blitterswijk C., Masereeuw R., de Boer J., et al. (2018). New insights into the effects of biomaterial chemistry and topography on the morphology of kidney epithelial cells. J. Tissue Eng. Regen. Med. 12 (2), e817–e827. 10.1002/term.2387 [DOI] [PubMed] [Google Scholar]
- Iozzo R. V., Schaefer L. (2015). Matrix biology. Proteoglycan Funct. A Compr. Nomencl. proteoglycans 42, 11–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang K. J., Mehr A. P., Hamilton G. A., McPartlin L. A., Chung S., Suh K. Y., et al. (2013). Human kidney proximal tubule-on-a-chip for drug transport and nephrotoxicity assessment. Integr. Biol. 5 (9), 1119–1129. 10.1039/c3ib40049b [DOI] [PubMed] [Google Scholar]
- Jansen J., De Napoli I. E., Fedecostante M., Schophuizen C. M. S., Chevtchik N. V., Wilmer M. J., et al. (2015). Human proximal tubule epithelial cells cultured on hollow fibers: Living membranes that actively transport organic cations. Sci. Rep. 5 (1), 16702. 10.1038/srep16702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen K., Castilho M., Aarts S., Kaminski M. M., Lienkamp S. S., Pichler R., et al. (2019). Fabrication of kidney proximal tubule grafts using biofunctionalized electrospun polymer scaffolds. Macromol. Biosci. 19 (2), e1800412–e1800419. 10.1002/mabi.201800412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joraku A., Stern K. A., Atala A., Yoo J. J. (2009). In vitro generation of three-dimensional renal structures. Methods 47 (2), 129–133. 10.1016/j.ymeth.2008.09.005 [DOI] [PubMed] [Google Scholar]
- Kajbafzadeh A. M., Khorramirouz R., Nabavizadeh B., Ladi Seyedian S. S., Akbarzadeh A., Heidari R., et al. (2019). Whole organ sheep kidney tissue engineering and in vivo transplantation: Effects of perfusion-based decellularization on vascular integrity. Mat. Sci. Eng. C Mat. Biol. Appl. 98, 392–400. 10.1016/j.msec.2019.01.018 [DOI] [PubMed] [Google Scholar]
- Kang M., Han Y. M. (2014). Differentiation of human pluripotent stem cells into nephron progenitor cells in a serum and feeder free system. PLoS One 9 (4), e94888. 10.1371/journal.pone.0094888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karamessinis P. M., Tzinia A. K., Kitsiou P. V., Stetler-Stevenson W. G., Michael A. F., Fan W-W., et al. (2002). Proximal tubular epithelial cell integrins respond to high glucose by altered cell-matrix interactions and differentially regulate matrixin expression. Lab. Invest. 82 (8), 1081–1093. 10.1097/01.lab.0000022224.86237.31 [DOI] [PubMed] [Google Scholar]
- Kher R., Sha E. C., Escobar M. R., Andreoli E. M., Wang P., Xu W. M., et al. (2011). Ectopic expression of cadherin 8 is sufficient to cause cyst formation in a novel 3D collagen matrix renal tubule culture. Am. J. Physiol. Cell Physiol. 301 (1), C99–C105. 10.1152/ajpcell.00151.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J. W., Nam S. A., Yi J., Kim J. Y., Lee J. Y., Park S. Y., et al. (2022). Kidney decellularized extracellular matrix enhanced the vascularization and maturation of human kidney organoids. Adv. Sci. 9 (15), e2103526. 10.1002/advs.202103526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M-H., Sawada Y., Taya M., Kino-Oka M. (2014). Influence of surface topography on the human epithelial cell response to micropatterned substrates with convex and concave architectures. J. Biol. Eng. 8 (1), 13. 10.1186/1754-1611-8-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King S. M., Higgins J. W., Nino C. R., Smith T. R., Paffenroth E. H., Fairbairn C. E., et al. (2017). 3D proximal tubule tissues recapitulate key aspects of renal physiology to enable nephrotoxicity testing. Front. Physiol. 8 (MAR), 123. 10.3389/fphys.2017.00123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman H. K., Martin G. R. (2005). Matrigel: Basement membrane matrix with biological activity. Semin. Cancer Biol. 15 (5), 378–386. 10.1016/j.semcancer.2005.05.004 [DOI] [PubMed] [Google Scholar]
- Ko K. W., Park S. Y., Lee E. H., Yoo Y. I., Kim D. S., Kim J. Y., et al. (2021). Integrated bioactive scaffold with polydeoxyribonucleotide and stem-cell-derived extracellular vesicles for kidney regeneration. ACS Nano 15 (4), 7575–7585. 10.1021/acsnano.1c01098 [DOI] [PubMed] [Google Scholar]
- Kolset S. O., Reinholt F. P., Jenssen T. (2012). Diabetic nephropathy and extracellular matrix. J. Histochem. Cytochem. 60 (12), 976–986. 10.1369/0022155412465073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam A. Q., Freedman B. S., Morizane R., Lerou P. H., Valerius M. T., Bonventre J. V. (2014). Rapid and efficient differentiation of human pluripotent stem cells into intermediate mesoderm that forms tubules expressing kidney proximal tubular markers. J. Am. Soc. Nephrol. 25 (6), 1211–1225. 10.1681/ASN.2013080831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawlor K. T., Vanslambrouck J. M., Higgins J. W., Chambon A., Bishard K., Arndt D., et al. (2021). Cellular extrusion bioprinting improves kidney organoid reproducibility and conformation. Nat. Mat. 20 (2), 260–271. 10.1038/s41563-020-00853-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Digabel J., Ghibaudo M., Trichet L., Richert A., Ladoux B. (2010). Microfabricated substrates as a tool to study cell mechanotransduction. Med. Biol. Eng. Comput. 48 (10), 965–976. 10.1007/s11517-010-0619-9 [DOI] [PubMed] [Google Scholar]
- Lee E. H., Chun S. Y., Yoon B. H., Kim H. T., Chung J-W., Lee J. N., et al. (2022). Application of porcine kidney-derived extracellular matrix as coating, hydrogel, and scaffold material for renal proximal tubular epithelial cell. Biomed. Res. Int. 2022, 2220641. 10.1155/2022/2220641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H. N., Choi Y. Y., Kim J. W., Lee Y. S., Choi J. W., Kang T., et al. (2021). Effect of biochemical and biomechanical factors on vascularization of kidney organoid-on-a-chip. Nano Converg. 8 (1), 35. 10.1186/s40580-021-00285-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelongt B., Ronco P. (2003). Role of extracellular matrix in kidney development and repair. Pediatr. Nephrol. 18, 731–742. 10.1007/s00467-003-1153-x [DOI] [PubMed] [Google Scholar]
- Li L., Fu H., Liu Y. (2022). The fibrogenic niche in kidney fibrosis: Components and mechanisms. Nat. Rev. Nephrol. 18 (9), 545–557. 10.1038/s41581-022-00590-z [DOI] [PubMed] [Google Scholar]
- Lih E., Park W., Park K. W., Chun S. Y., Kim H., Joung Y. K., et al. (2019). A bioinspired scaffold with anti-inflammatory magnesium hydroxide and decellularized extracellular matrix for renal tissue regeneration. ACS Cent. Sci. 5 (3), 458–467. 10.1021/acscentsci.8b00812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin N. Y. C., Homan K. A., Robinson S. S., Kolesky D. B., Duarte N., Moisan A., et al. (2019). Renal reabsorption in 3D vascularized proximal tubule models. Proc. Natl. Acad. Sci. U. S. A. 116 (12), 5399–5404. 10.1073/pnas.1815208116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loganathan R., Little C. D., Rongish B. J. (2020). Extracellular matrix dynamics in tubulogenesis. Cell. Signal. 72, 109619. 10.1016/j.cellsig.2020.109619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louzao-Martinez L., van Dijk C. G. M., Xu Y. J., Korn A., Bekker N. J., Brouwhuis R., et al. (2019). A proteome comparison between human fetal and mature renal extracellular matrix identifies EMILIN1 as a regulator of renal epithelial cell adhesion. Matrix Biol. Plus 4, 100011. 10.1016/j.mbplus.2019.100011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Love H. D., Ao M., Jorgensen S., Swearingen L., Ferrell N., Evans R., et al. (2019). Substrate elasticity governs differentiation of renal tubule cells in prolonged culture. Tissue Eng. Part A 25 (13–14), 1013–1022. 10.1089/ten.TEA.2018.0182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low J. H., Li P., Chew E. G. Y., Zhou B., Suzuki K., Zhang T., et al. (2019). Generation of human PSC-derived kidney organoids with patterned nephron segments and a de novo vascular network. Cell Stem Cell 25 (3), 373–387. e9. 10.1016/j.stem.2019.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lü S. H., Lin Q., Liu Y. N., Gao Q., Hao T., Wang Y., et al. (2012). Self-assembly of renal cells into engineered renal tissues in collagen/Matrigel scaffold in vitro . J. Tissue Eng. Regen. Med. 6 (10), 786–792. 10.1002/term.484 [DOI] [PubMed] [Google Scholar]
- Mae S-I., Ryosaka M., Sakamoto S., Matsuse K., Nozaki A., Igami M., et al. (2020). Expansion of human iPSC-derived ureteric bud organoids with repeated branching potential. Cell Rep. 32 (4), 107963. 10.1016/j.celrep.2020.107963 [DOI] [PubMed] [Google Scholar]
- Manninen A. (2015). Epithelial polarity - generating and integrating signals from the ECM with integrins. Exp. Cell Res. 334 (2), 337–349. 10.1016/j.yexcr.2015.01.003 [DOI] [PubMed] [Google Scholar]
- Melica M. E., La Regina G. L., Parri M., Peired A. J., Romagnani P., Lasagni L. (2019). Substrate stiffness modulates renal progenitor cell properties via a ROCK-mediated mechanotransduction mechanism. Cells 8 (12), E1561. 10.3390/cells8121561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minuth W. W., Sorokin L., Schumacher K. (2004). Generation of renal tubules at the interface of an artificial interstitium. Cell. Physiol. biochem. 14 (4–6), 387–394. 10.1159/000080348 [DOI] [PubMed] [Google Scholar]
- Miya M., Maeshima A., Mishima K., Sakurai N., Ikeuchi H., Kuroiwa T., et al. (2011). Enhancement of in vitro human tubulogenesis by endothelial cell-derived factors: Implications for in vivo tubular regeneration after injury. Am. J. Physiol. Ren. Physiol. 301 (2), 387–395. 10.1152/ajprenal.00619.2010 [DOI] [PubMed] [Google Scholar]
- Moll S., Ebeling M., Weibel F., Farina A., Araujo Del Rosario A., Hoflack J. C., et al. (2013). Epithelial cells as active player in fibrosis: Findings from an in vitro model. PLoS One 8 (2), e56575. 10.1371/journal.pone.0056575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montesano R., Matsumoto K., Nakamura T., Orci L. (1991). Identification of a fibroblast-derived epithelial morphogen as hepatocyte growth factor. Cell 67 (5), 901–908. 10.1016/0092-8674(91)90363-4 [DOI] [PubMed] [Google Scholar]
- Montesano R., Schaller G., Orci L. (1991). Induction of epithelial tubular morphogenesis in vitro by fibroblast-derived soluble factors. Cell 66 (4), 697–711. 10.1016/0092-8674(91)90115-f [DOI] [PubMed] [Google Scholar]
- Morizane R., Bonventre J. V. (2017). Generation of nephron progenitor cells and kidney organoids from human pluripotent stem cells. Nat. Protoc. 12 (1), 195–207. 10.1038/nprot.2016.170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morizane R., Lam A. Q., Freedman B. S., Kishi S., Valerius M. T., Bonventre J. V. (2015). Nephron organoids derived from human pluripotent stem cells model kidney development and injury. Nat. Biotechnol. 33 (11), 1193–1200. 10.1038/nbt.3392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muncie J. M., Weaver V. M. (2018). The physical and biochemical properties of the extracellular matrix regulate cell fate. Curr. Top. Dev. Biol. 130, 1–37. 10.1016/bs.ctdb.2018.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myram S., Venzac B., Lapin B., Battistella A., Cayrac F., Cinquin B., et al. (2021). A multitubular kidney-on-chip to decipher pathophysiological mechanisms in renal cystic diseases. Front. Bioeng. Biotechnol. 9, 624553. 10.3389/fbioe.2021.624553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayanan K., Schumacher K. M., Tasnim F., Kandasamy K., Schumacher A., Ni M., et al. (2013). Human embryonic stem cells differentiate into functional renal proximal tubular-like cells. Kidney Int. 83 (4), 593–603. 10.1038/ki.2012.442 [DOI] [PubMed] [Google Scholar]
- Ni M., Teo J. C. M., Ibrahim M. S., Zhang K., Tasnim F., Chow P-Y., et al. (2011). Characterization of membrane materials and membrane coatings for bioreactor units of bioartificial kidneys. Biomaterials 32 (6), 1465–1476. 10.1016/j.biomaterials.2010.10.061 [DOI] [PubMed] [Google Scholar]
- Nickel C., Benzing T., Sellin L., Gerke P., Karihaloo A., Liu Z-X., et al. (2002). The polycystin-1 C-terminal fragment triggers branching morphogenesis and migration of tubular kidney epithelial cells. J. Clin. Invest. 109 (4), 481–489. 10.1172/JCI12867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigam S. K., Bush K. T. (2014). Growth factor-heparan sulfate “switches” regulating stages of branching morphogenesis. Pediatr. Nephrol. 29 (4), 727–735. 10.1007/s00467-013-2725-z [DOI] [PubMed] [Google Scholar]
- Nur-E-Kamal A., Ahmed I., Kamal J., Schindler M., Meiners S. (2006). Three-dimensional nanofibrillar surfaces promote self-renewal in mouse embryonic stem cells. Stem Cells 24 (2), 426–433. 10.1634/stemcells.2005-0170 [DOI] [PubMed] [Google Scholar]
- Otero J., Navajas D., Alcaraz J. (2020). Characterization of the elastic properties of extracellular matrix models by atomic force microscopy. Methods Cell Biol. 156, 59–83. 10.1016/bs.mcb.2019.11.016 [DOI] [PubMed] [Google Scholar]
- Passaniti A., Kleinman H. K., Martin G. R. (2021). Matrigel: History/background, uses, and future applications. J. Cell Commun. Signal. 10.1007/s12079-021-00643-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petkau-Milroy K., Brunsveld L. (2013). Supramolecular chemical biology; bioactive synthetic self-assemblies. Org. Biomol. Chem. 11 (2), 219–232. 10.1039/c2ob26790j [DOI] [PubMed] [Google Scholar]
- Poornejad N., Schaumann L. B., Buckmiller E. M., Momtahan N., Gassman J. R., Ma H. H., et al. (2016). The impact of decellularization agents on renal tissue extracellular matrix. J. Biomater. Appl. 31 (4), 521–533. 10.1177/0885328216656099 [DOI] [PubMed] [Google Scholar]
- Rayner S. G., Phong K. T., Xue J., Lih D., Shankland S. J., Kelly E. J., et al. (2018). Reconstructing the human renal vascular–tubular unit in vitro . Adv. Healthc. Mat. 7 (23), e1801120. 10.1002/adhm.201801120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosines E., Schmidt H. J., Nigam S. K. (2007). The effect of hyaluronic acid size and concentration on branching morphogenesis and tubule differentiation in developing kidney culture systems: Potential applications to engineering of renal tissues. Biomaterials 28 (32), 4806–4817. 10.1016/j.biomaterials.2007.07.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiter F. A. A., Morgan F. L. C., Roumans N., Schumacher A., Slaats G. G., Moroni L., et al. (2022). Soft, dynamic hydrogel confinement improves kidney organoid lumen morphology and reduces epithelial-mesenchymal transition in culture. Adv. Sci. 9 (20), e2200543. 10.1002/advs.202200543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakurai H., Barros E. J., Tsukamoto T., Barasch J., Nigam S. K. (1997). An in vitro tubulogenesis system using cell lines derived from the embryonic kidney shows dependence on multiple soluble growth factors. Proc. Natl. Acad. Sci. U. S. A. 94 (12), 6279–6284. 10.1073/pnas.94.12.6279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satyam A., Tsokos M. G., Tresback J. S., Zeugolis D. I., Tsokos G. C. (2020). Cell derived extracellular matrix-rich biomimetic substrate supports podocyte proliferation, differentiation and maintenance of native phenotype. Adv. Funct. Mat. 30 (44), 1908752. 10.1002/adfm.201908752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlüter M. A., Margolis B. (2009). Apical lumen formation in renal epithelia. J. Am. Soc. Nephrol. 20 (7), 1444–1452. 10.1681/ASN.2008090949 [DOI] [PubMed] [Google Scholar]
- Schophuizen C. M. S., De Napoli I. E., Jansen J., Teixeira S., Wilmer M. J., Hoenderop J. G. J., et al. (2015). Development of a living membrane comprising a functional human renal proximal tubule cell monolayer on polyethersulfone polymeric membrane. Acta Biomater. 14, 22–32. 10.1016/j.actbio.2014.12.002 [DOI] [PubMed] [Google Scholar]
- Schutgens F., Rookmaaker M. B., Margaritis T., Rios A., Ammerlaan C., Jansen J., et al. (2019). Tubuloids derived from human adult kidney and urine for personalized disease modeling. Nat. Biotechnol. 37 (3), 303–313. 10.1038/s41587-019-0048-8 [DOI] [PubMed] [Google Scholar]
- Sciancalepore A. G., Portone A., Moffa M., Persano L., De Luca M., Paiano A., et al. (2016). Micropatterning control of tubular commitment in human adult renal stem cells. Biomaterials 94, 57–69. 10.1016/j.biomaterials.2016.03.042 [DOI] [PubMed] [Google Scholar]
- Sebinger D. D. R., Ofenbauer A., Gruber P., Malik S., Werner C. (2013). ECM modulated early kidney development in embryonic organ culture. Biomaterials 34 (28), 6670–6682. 10.1016/j.biomaterials.2013.05.031 [DOI] [PubMed] [Google Scholar]
- Secker P. F., Luks L., Schlichenmaier N., Dietrich D. R. (2018). RPTEC/TERT1 cells form highly differentiated tubules when cultured in a 3D matrix. ALTEX 35 (2), 223–234. 10.14573/altex.1710181 [DOI] [PubMed] [Google Scholar]
- Shahraki S., Bideskan A. E., Aslzare M., Tavakkoli M., Bahrami A. R., Hosseinian S., et al. (2022). Decellularization with triton X-100 provides a suitable model for human kidney bioengineering using human mesenchymal stem cells. Life Sci. 295, 120167. 10.1016/j.lfs.2021.120167 [DOI] [PubMed] [Google Scholar]
- Shamir E. R., Ewald A. J. (2014). Three-dimensional organotypic culture: Experimental models of mammalian biology and disease. Nat. Rev. Mol. Cell Biol. 15 (10), 647–664. 10.1038/nrm3873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen C., Zhang G., Wang Q., Meng Q. (2015). Fabrication of collagen gel hollow fibers by covalent cross-linking for construction of bioengineering renal tubules. ACS Appl. Mat. Interfaces 7 (35), 19789–19797. 10.1021/acsami.5b05809 [DOI] [PubMed] [Google Scholar]
- Shen L., Song X., Xu Y., Tian R., Wang Y., Li P., et al. (2021). Patterned vascularization in a directional ice-templated scaffold of decellularized matrix. Eng. Life Sci. 21 (10), 683–692. 10.1002/elsc.202100034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh N. K., Han W., Nam S. A., Kim J. W., Kim J. Y., Kim Y. K., et al. (2020201911973). Three-dimensional cell-printing of advanced renal tubular tissue analogue. Biomaterials 232, 119734. 10.1016/j.biomaterials.2019.119734 [DOI] [PubMed] [Google Scholar]
- Sobreiro-Almeida R., Fonseca D. R., Neves N. M. (2019). Extracellular matrix electrospun membranes for mimicking natural renal filtration barriers. Mat. Sci. Eng. C Mat. Biol. Appl. 103, 109866. 10.1016/j.msec.2019.109866 [DOI] [PubMed] [Google Scholar]
- Sobreiro-Almeida R., Gómez-Florit M., Quinteira R., Reis R. L., Gomes M. E., Neves N. M. (2021). Decellularized kidney extracellular matrix bioinks recapitulate renal 3D microenvironment in vitro . Biofabrication 13 (4), 045006. 10.1088/1758-5090/ac0fca [DOI] [PubMed] [Google Scholar]
- Sobreiro-Almeida R., Melica M. E., Lasagni L., Romagnani P., Neves N. M. (2020). Co-cultures of renal progenitors and endothelial cells on kidney decellularized matrices replicate the renal tubular environment in vitro . Acta Physiol. 230 (1), e13491. 10.1111/apha.13491 [DOI] [PubMed] [Google Scholar]
- Song J. J., Guyette J. P., Gilpin S. E., Gonzalez G., Vacanti J. P., Ott H. C. (2013). Regeneration and experimental orthotopic transplantation of a bioengineered kidney. Nat. Med. 19 (5), 646–651. 10.1038/nm.3154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su J., Satchell S. C., Shah R. N., Wertheim J. A. (2018). Kidney decellularized extracellular matrix hydrogels: Rheological characterization and human glomerular endothelial cell response to encapsulation. J. Biomed. Mat. Res. A 106 (9), 2448–2462. 10.1002/jbm.a.36439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian B., Ko W. C., Yadav V., DesRochers T. M., Perrone R. D., Zhou J., et al. (2012). The regulation of cystogenesis in a tissue engineered kidney disease system by abnormal matrix interactions. Biomaterials 33 (33), 8383–8394. 10.1016/j.biomaterials.2012.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian B., Rudym D., Cannizzaro C., Perrone R., Zhou J., Kaplan D. L. (2010). Tissue-engineered three-dimensional in vitro models for normal and diseased kidney. Tissue Eng. Part A 16 (9), 2821–2831. 10.1089/ten.tea.2009.0595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan D. C., Mirmalek-Sani S. H., Deegan D. B., Baptista P. M., Aboushwareb T., Atala A., et al. (2012). Decellularization methods of porcine kidneys for whole organ engineering using a high-throughput system. Biomaterials 33 (31), 7756–7764. 10.1016/j.biomaterials.2012.07.023 [DOI] [PubMed] [Google Scholar]
- Taguchi A., Nishinakamura R. (2017). Higher-order kidney organogenesis from pluripotent stem cells. Cell Stem Cell 21 (6), 730–746. e6. 10.1016/j.stem.2017.10.011 [DOI] [PubMed] [Google Scholar]
- Takasato M., Er P. X., Chiu H. S., Maier B., Baillie G. J., Ferguson C., et al. (2015). Kidney organoids from human iPS cells contain multiple lineages and model human nephrogenesis. Nature 526 (7574), 564–568. 10.1038/nature15695 [DOI] [PubMed] [Google Scholar]
- Takasato M., Little M. H. (2017). Making a kidney organoid using the directed differentiation of human pluripotent stem cells. Methods Mol. Biol. 1597, 195–206. 10.1007/978-1-4939-6949-4_14 [DOI] [PubMed] [Google Scholar]
- Taub M., Wang Y., Szczesny T. M., Kleinman H. K. (1990). Epidermal growth factor or transforming growth factor α is required for kidney tubulogenesis in matrigel cultures in serum-free medium. Proc. Natl. Acad. Sci. U. S. A. 87 (10), 4002–4006. 10.1073/pnas.87.10.4002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theocharis A. D., Skandalis S. S., Gialeli C., Karamanos N. K. (2016). Extracellular matrix structure. Adv. Drug Deliv. Rev. 97, 4–27. 10.1016/j.addr.2015.11.001 [DOI] [PubMed] [Google Scholar]
- Toyohara T., Mae S-I., Sueta S-I., Inoue T., Yamagishi Y., Kawamoto T., et al. (2015). Cell therapy using human induced pluripotent stem cell-derived renal progenitors ameliorates acute kidney injury in mice. Stem Cells Transl. Med. 4 (9), 980–992. 10.5966/sctm.2014-0219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tröndle K., Miotto G., Rizzo L., Pichler R., Koch F., Koltay P., et al. (2022). Deep learning-assisted nephrotoxicity testing with bioprinted renal spheroids. Int. J. Bioprint. 8 (2), 528. 10.18063/ijb.v8i2.528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tröndle K., Rizzo L., Pichler R., Koch F., Itani A., Zengerle R., et al. (2021). Scalable fabrication of renal spheroids and nephron-like tubules by bioprinting and controlled self-assembly of epithelial cells. Biofabrication 13 (3), 035019. 10.1088/1758-5090/abe185 [DOI] [PubMed] [Google Scholar]
- Ullah I., Busch J. F., Rabien A., Ergün B., Stamm C., Knosalla C., et al. (2020). Adult tissue extracellular matrix determines tissue specification of human iPSC-derived embryonic stage mesodermal precursor cells. Adv. Sci. 7 (5), 1901198. 10.1002/advs.201901198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Berg C. W., Ritsma L., Avramut M. C., Wiersma L. E., van den Berg B. M., Leuning D. G., et al. (2018). Renal subcapsular transplantation of PSC-derived kidney organoids induces neo-vasculogenesis and significant glomerular and tubular maturation in vivo . Stem Cell Rep. 10 (3), 751–765. 10.1016/j.stemcr.2018.01.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Gaal R. C., Vrehen A. F., van Sprang J. F., Fransen P-P. K. H., van Turnhout M. C., Dankers P. Y. W. (2021). Biomaterial screening of protein coatings and peptide additives: Towards a simple synthetic mimic of a complex natural coating for a bio-artificial kidney. Biomater. Sci. 9 (6), 2209–2220. 10.1039/d0bm01930e [DOI] [PubMed] [Google Scholar]
- van Genderen A. M., Jansen K., Kristen M., van Duijn J., Li Y., Schuurmans C. C. L., et al. (2021). Topographic guidance in melt-electrowritten tubular scaffolds enhances engineered kidney tubule performance. Front. Bioeng. Biotechnol. 8, 617364. 10.3389/fbioe.2020.617364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vormann M. K., Tool L. M., Ohbuchi M., Gijzen L., van Vught R., Hankemeier T., et al. (2022). Modelling and prevention of acute kidney injury through ischemia and reperfusion in a combined human renal proximal tubule/blood vessel-on-a-chip. Kidney360 3 (2), 217–231. 10.34067/KID.0003622021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vormann M. K., Vriend J., Lanz H. L., Gijzen L., van den Heuvel A., Hutter S., et al. (2021). Implementation of a human renal proximal tubule on a chip for nephrotoxicity and drug interaction studies. J. Pharm. Sci. 110 (4), 1601–1614. 10.1016/j.xphs.2021.01.028 [DOI] [PubMed] [Google Scholar]
- Walma D. A. C., Yamada K. M. (2020). The extracellular matrix in development. Development 147 (10), dev175596–9. 10.1242/dev.175596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Guo C., Chen Y., Tozzi L., Szymkowiak S., Li C., et al. (2020). Developing a self-organized tubulogenesis model of human renal proximal tubular epithelial cells in vitro . J. Biomed. Mat. Res. A 108 (3), 795–804. 10.1002/jbm.a.36858 [DOI] [PubMed] [Google Scholar]
- Weber H. M., Tsurkan M. V., Magno V., Freudenberg U., Werner C. (2017). Heparin-based hydrogels induce human renal tubulogenesis in vitro . Acta Biomater. 57, 59–69. 10.1016/j.actbio.2017.05.035 [DOI] [PubMed] [Google Scholar]
- Wiraja C., Mori Y., Ichimura T., Hwang J., Xu C., Bonventre J. V. (2021). Nephrotoxicity assessment with human kidney tubuloids using spherical nucleic acid-based mRNA nanoflares. Nano Lett. 21 (13), 5850–5858. 10.1021/acs.nanolett.1c01840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia Y., Nivet E., Sancho-Martinez I., Gallegos T., Suzuki K., Okamura D., et al. (2013). Directed differentiation of human pluripotent cells to ureteric bud kidney progenitor-like cells. Nat. Cell Biol. 15 (12), 1507–1515. 10.1038/ncb2872 [DOI] [PubMed] [Google Scholar]
- Xie R., Korolj A., Liu C., Song X., Lu R. X. Z., Zhang B., et al. (2020). h-FIBER: Microfluidic topographical hollow fiber for studies of glomerular filtration barrier. ACS Cent. Sci. 6 (6), 903–912. 10.1021/acscentsci.9b01097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing H., Lee H., Luo L., Kyriakides T. R. (2020). Extracellular matrix-derived biomaterials in engineering cell function. Biotechnol. Adv. 42, 107421. 10.1016/j.biotechadv.2019.107421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zegers M. M. P., O’Brien L. E., Yu W., Datta A., Mostov K. E. (2003). Epithelial polarity and tubulogenesis in vitro . Trends Cell Biol. 13 (4), 169–176. 10.1016/s0962-8924(03)00036-9 [DOI] [PubMed] [Google Scholar]
- Zhang H., Lau S. F-T., Heng B. F., Teo P. Y., Alahakoon P. K. D. T., Ni M., et al. (2011). Generation of easily accessible human kidney tubules on two-dimensional surfaces in vitro . J. Cell. Mol. Med. 15 (6), 1287–1298. 10.1111/j.1582-4934.2010.01113.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Tasnim F., Ying J. Y., Zink D. (2009). The impact of extracellular matrix coatings on the performance of human renal cells applied in bioartificial kidneys. Biomaterials 30 (15), 2899–2911. 10.1016/j.biomaterials.2009.01.046 [DOI] [PubMed] [Google Scholar]
- Zhang J., Li K., Kong F., Sun C., Zhang D., Yu X., et al. (2019). Induced intermediate mesoderm combined with decellularized kidney scaffolds for functional engineering kidney. Tissue Eng. Regen. Med. 16 (5), 501–512. 10.1007/s13770-019-00197-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Reif G., Wallace D. P. (2020). Extracellular matrix, integrins, and focal adhesion signaling in polycystic kidney disease. Cell. Signal. 72, 109646. 10.1016/j.cellsig.2020.109646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou C., Zhou L., Liu J., Xu L., Xu Z., Chen Z., et al. (2020). Kidney extracellular matrix hydrogel enhances therapeutic potential of adipose-derived mesenchymal stem cells for renal ischemia reperfusion injury. Acta Biomater. 115, 250–263. 10.1016/j.actbio.2020.07.056 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.