Abstract
Objective
This study aimed to investigate the effects of clinical Pilates exercises in patients with fibromyalgia (FM) and to compare the effects of one-to-one and group-based exercise methods.
Methods
A total of 42 women (mean age, 50.90±7.78 years) with FM were included. The participants were randomly divided into 2 groups (one-to-one exercise, n=16; group-based exercise, n=26). Disease impact was evaluated with the FM Impact Questionnaire, functional status with the Health Assessment Questionnaire, anxiety with the Beck Anxiety Inventory, quality of life with short form-36, and biopsychosocial status with the Bilişsel Egzersiz Terapi Yaklaşımı-biopsychosocial questionnaire. All the evaluations were performed pre- and post-treatment. Clinical Pilates exercises were carried out 2 days a week for 6 weeks.
Results
When the pre- and post-treatment data were compared, significant improvement was seen in all parameters in the group-based exercise group; in the one-to-one exercise group, improvement was noted in disease impact, quality of life, and biopsychosocial status. When post-treatment data were compared, only disease impact was significant for the one-to-one exercise group. Effect size results were found to be moderate and high for both methods.
Conclusion
For clinical Pilates exercise in FM, one-to-one method was suggested to have high disease impact and low quality of life, whereas group-based exercise method showed high anxiety.
Keywords: Fibromyalgia, exercise, quality of life, anxiety
Introduction
Fibromyalgia (FM) is a chronic disease characterized by widespread pain in the body accompanied by other symptoms, including fatigue, sleep disturbances, depression, cognitive dysfunction, irritable bowel syndrome, and headache (1, 2). The pain, which is the most common symptom of FM, is variable (hyperalgesia or allodynia) and is associated with physical and emotional stress and therefore causes psychological problems, such as depression and anxiety, and decreases the quality of life (3, 4). It has been estimated that FM affects 2.7% of the population and occurs more often in women than in men (5).
The management of FM usually aims to reduce pain and fatigue and improve sleep quality and functionality. A multidisciplinary approach with the combination of non-pharmacologic and pharmacologic treatments according to symptoms is often suggested (6). Furthermore, it has been seen that exercise, which is one of the non-pharmacologic treatment methods, is particularly emphasized (7, 8).
Pilates, originally known as “Contrology,” was developed in the early 1900s by Joseph H. Pilates and has become quite popular in the recent years. In the early 2000s, Pilates exercises were adapted to the clinic by Australian physiotherapists, and this method was called the “clinical Pilates” or “modified Pilates” method The clinical Pilates method can be used as an exercise method for healthy people as well as for various patient populations (9).
The clinical Pilates method is a form of mind-body exercises, based on 6 principles— centering, concentration, control, precision, breath, and flow. It aims to coordinate the quality of movement along with breathing and active movement. Pilates exercises focus on spinal stabilization and are designed to ensure muscular strength, flexibility, balance, proprioception, and body awareness. These are low-impact exercises that can be performed in various positions, including standing, supine, prone, or sitting. During these exercises, breathing and muscular control reduce pain and enhance posture (10–12). These exercises are often used as a treatment method in patients with low-back pain (13). There are only 4 pilot studies on the effects of Pilates exercises in individuals with FM. In these studies, Pilates was found to be better than short-term home exercises and connective tissue massage on pain-pressure threshold and anxiety, similar to yoga with no intervention in the control group (11, 14–16). Although the modified Pilates method was preferred to aerobic training in 1 of the 2 most recent protocol studies on the effectiveness of Pilates (17), another study has reported that mat Pilates and aquatic aerobic exercise had similar effects, in terms of pain and disability in individuals with FM (18). Beltrán-Carrillo et al. (19) also indicated that taking part in a group-based exercise program of individuals with FM may be effective in coping with FM and provide psychosocial benefits in addition to its physical benefits.
Although some studies have highlighted that Pilates is an effective method in reducing disease-related findings, there is a lack of information on whether one-to-one and group-based exercise methods for clinical Pilates have superiority over each other and which exercise method (one-to-one or group-based exercise) should be preferred when the possibilities are favorable. This study aimed to investigate the effectiveness of clinical Pilates exercises in patients with FM and to compare the effects of one-to-one and group-based exercise methods.
Methods
In this study, which was planned as a randomized controlled parallel group, one-toone and group-based exercise methods were evaluated. Randomization was carried out by a researcher through a computer program, IBM Statistical Package for the Social Sciences version 22 (IBM SPSS Corp.; Armonk, NY, USA) in charge of allocation. Assessments (pre- and post-treatment) and training were carried out by different physiotherapists. The study was planned as single-blind, and the physiotherapist performing the evaluation was blinded to the study. Clinical Pilates exercises were performed by an experienced and certified physiotherapist in this field.
Participants
A total of 42 volunteers (women with mean age 50.90±7.78 years) were included in the study. They were diagnosed with FM by the same rheumatologist according to the American College of Rheumatology (ACR) 2016 criteria and referred to the Rheumatologic Physiotherapy and Rehabilitation clinic and were screened for eligibility. The one-to-one exercise group had 16 participants (mean age, 55.93±8.03 years), and the group-based exercise group had 26 participants (mean age, 47.80±5.87 years).
Demographic data of the participants were recorded before the evaluations. Demographic data are shown in Table 1.
Table 1.
Demographic characteristics of the patients.
| Variables | One-to-one exercise group (n=16) M±SD | Group-based exercise group (n=26) M±SD | p* |
|---|---|---|---|
| Age (years) | 55.93±8.03 | 47.80±5.87 | 0.001 |
| Body weight (kg) | 75.62±13.61 | 78.15±13.22 | 0.555 |
| Height (m) | 1.57±0.068 | 1.60±0.65 | 0.159 |
| BMI (kg/m2) | 30.76±6.15 | 30.50±5.03 | 0.883 |
Independent samples test.
M: mean; SD: standard deviation; BMI: body-mass index.
The inclusion criteria were as follows: (a) having FM diagnosis according to the ACR 2016 criteria; (b) aged 20–65 years; (c) stable drug use for at least 3 months or more; and (d) volunteering to participate in this study.
The exclusion criteria were as follows orthopedic and cardiopulmonary diseases (which would prevent patients from doing exercise); neurological disorders; unstable endocrine system diseases; malignancy; pregnancy; and severe psychological diseases.
This study was approved by the Ethics Committee for Non-Interventional Clinical Research of Pamukkale University (Approval Date: September 10, 2019; Approval Number: 60116787-020/62191).
All the participants were informed verbally, and informed consent forms were signed.
Assessments
All individuals were evaluated by the same physiotherapist according to standardized test protocols and in the same conditions at baseline and at the end of the 6th week. Disease impact was evaluated with the FM Impact Questionnaire (FIQ), functional status with the Health Assessment Questionnaire (HAQ), anxiety with the Beck anxiety inventory (BAI), quality of life with the short form-36 (SF-36), and biopsychosocial status with the Bilişsel Egzersiz Terapi Yaklaşımı-biopsychosocial questionnaire (BETY-BQ).
FIQ
FIQ is a questionnaire that includes 10 items (physical impairment, days felt good, work missed, work impairment, pain, fatigue, morning tiredness, stiffness, anxiety, and depression), ranging from 0 to 10, evaluating the health status and physical function of the individuals diagnosed with FM. Higher scores indicate a lower functionality on the disease (20, 21).
HAQ
Functional status of patients is evaluated with HAQ, which includes 20 questions and 8 subscales, such as dressing, grooming, rising, eating, hygiene, reach, grip, and activity. Each question is scored from 0 (without difficulty) to 3 (unable to do), and the highest score of each subscales is added (22, 23).
BAI
This questionnaire, developed by Aeron Beck that includes 21 questions, is used to evaluate the level of anxiety. Each question is rated between 0 (not at all) and 3 (severely). Higher scores indicate a severe anxiety level in patients (24, 25).
SF-36
This is the most commonly used quality of life scale and includes 36 questions on 8 subscales; physical functioning, role limitations because of physical health, body pain, social functioning, role limitation owing to emotional health, vitality, mental health, and general health perceptions. The total score ranges from 0 to 100. Higher scores indicate that the quality of life is good (26, 27).
BETY-BQ
BETY-BQ is an original questionnaire that was developed by Unal et al. (28) in 2017 to evaluate the biopsychosocial status of patients with rheumatic diseases. It includes 30 questions that are answered using a 5-point Likert-type scale. Higher scores indicate “bad” biopsychosocial status of the patients.
Intervention
Clinical Pilates exercises were performed by a certified and experienced physiotherapist in 2 different methods (one-to-one and group-based) 2 times a week for 6 weeks.
One-to-one exercise group
Before starting the clinical Pilates exercise program, 5 key elements of clinical Pilates exercises were taught to all the patients breathing; focus; and placement of the rib cage, shoulder, head, and neck. Patients were encouraged to use these 5 key elements not only during exercises but also in their daily routines and activities. During clinical Pilates sessions, exercises were repeated until the correct posture was achieved in different positions according to the key elements taught on the 1st day. First, the physiotherapist demonstrated the exercises and then asked the patients to perform the exercise correctly. In addition, the aim of each exercise was explained to the patients, and they were asked to try to make it functional in their daily life. Each exercise was performed for 8–10 repetitions and was performed on a mat in the supine/side-lying/prone and sitting positions. Increasing the number of repetitions, changing the position to level, stability balls, and therabands were used for the progression of exercises. Each patient’s stabilization ball was personal, and it was 55–65 cm in height so as to achieve a 90° angle at the hips and knees (29). The program for both the methods lasted 60 minutes, including warm up (10 minutes), clinical Pilates exercises (40 minutes), and cool down (10 minutes).
Group-based exercise group
The group-based exercise program was the same as the exercise program applied to the one-to-one exercise group. However, it was performed in the form of group sessions with 6–8 people together.
Statistical analysis
Through power analysis, it was calculated that 32 patients enrolled in this study (16 patients in each group) would have 80% power with 95% confidence interval. Data were assessed using the IBM Statistical Package for the Social Sciences version 21.0 (IBM SPSS Corp.; Armonk, NY, USA). Continuous variables were stated as average, standard deviation, and percentage. The Kolmogorov-Smirnov test was used to determine whether the continuous variables showed normal distributions. P value <0.05 was considered as statistically significant. Effect size was measured with the Cohen’s d coefficient. An effect size greater than 0.8 was considered as large, approximately 0.5 as moderate, and less than 0.2 as small (30).
Results
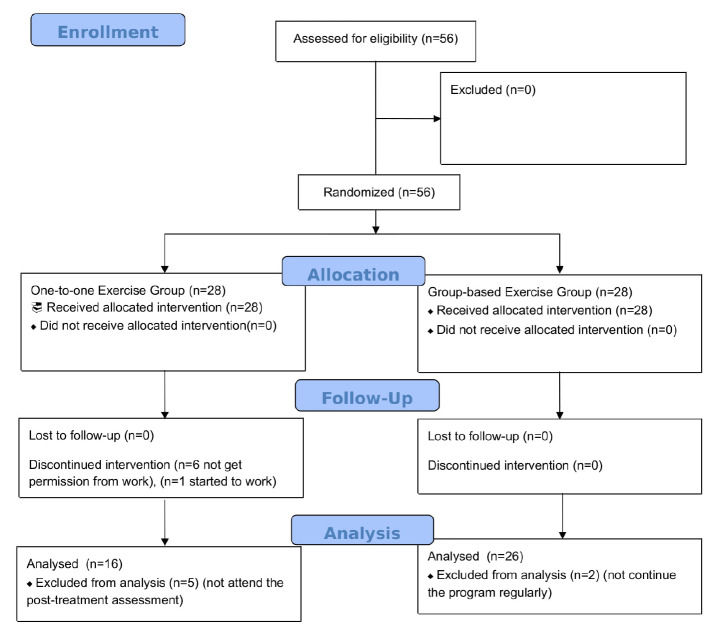
A total of 56 volunteers who met the inclusion criteria were randomly divided into 2 groups; the one-to-one exercise group (n=28) and the group-based exercise group (n=28) with SPSS 21.0 package program. In the one-toone exercise group, 6 people left the training because they could not get permission from work, 3 people did not continue the program regularly, 2 people did not attend the post-treatment assessment, and 1 person could not continue the program because she started work after starting treatment. In the group-based exercise group, 2 people did not continue the program regularly, thus all these patients’ data were excluded. This study was completed with a total of 42 participants; 16 women (mean age, 55.93±8.03 years) in the one-to-one exercise group and 26 women (mean age, 47.80±5.87 years) in the group-based exercise group. Figure 1 shows a flowchart of the study design. There were no adverse events reported with the program. The rate of participation in the treatment sessions was 90%. The demographic data are shown in Table 1. When pre-treatment data of outcome measures were compared statistically, there was no difference (p>0.05).
Figure 1.
Flowchart of the progress through the phases of the study according to the Consolidated Standards of Reporting Trials.
Statistically significant improvement was observed in FIQ, physical and mental components of SF-36, and BETY-BQ scale in both the groups when pre- and post-treatment outcomes were compared (p=0.001, p=0.000; p=0.003, p=0.000; p=0.022, p=0.004; and p=0.038, p=0.001, respectively). There was also a significant improvement in the HAQ (p=0.006) and BAI (p=0.004) scores of the group-based exercise group (Table 2).
Table 2.
Pre-treatment and post-treatment results within groups.
| Variables | One-to-one exercise group (n=16) | Group-based exercise group (n=26) | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Pre-treatment M±SD |
Post-treatment M±SD |
p* | Pre-treatment M±SD |
Post-treatment M±SD |
p* | |
| Fibromyalgia Impact Questionnaire | 55.04±18.48 | 32.80±22.19 | 0.001 | 62.44±17.80 | 46.39±22.26 | 0.000 |
| Health Assessment Questionnaire | 0.85±0.70 | 0.58±0.66 | 0.063 | 1.02±0.63 | 0.67±0.55 | 0.006 |
| Beck Anxiety Inventory | 21.12±12.85 | 16.75±13.41 | 0.108 | 26.57±12.54 | 20.88±10.09 | 0.004 |
| Short form-36 | ||||||
| Physical component | 145.83±67.39 | 196.50±95.37 | 0.003 | 138.07±74.46 | 196.82±81.94 | 0.000 |
| Mental component | 177.33±96.07 | 231.77±109.07 | 0.022 | 159.22±79.61 | 208.98±95.69 | 0.004 |
| Bilisşel Egzersiz Terapi Yaklaşı-mıbiopsychosocial questionnaire (0–120) | 35.60±20.03 | 25.62±17.67 | 0.038 | 41.88±19.64 | 31.53±19.90 | 0.001 |
Wilcoxon test.
M: mean; SD: standard deviation.
When the pre-treatment data were compared, there was no difference between the groups (p>0.05). When both the groups were compared post-treatment, only FIQ was significantly in favor of the one-to-one exercise group (p=0.041) (Table 3).
Table 3.
Comparison of post-treatment and effect size results with groups.
| Variables | p* | One-to-one exercise group (n=16) | Group-based exercise group (n=26) |
|---|---|---|---|
|
|
|
||
| Cohen’s d | Cohen’s d | ||
| Fibromyalgia Impact Questionnaire | 0.041 | 1.385300659 | 1.140676071 |
| Health Assessment Questionnaire | 0.491 | 0.518116833 | 0.686457102 |
| Beck Anxiety Inventory | 0.186 | 0.465364091 | 0.633333277 |
| Short form-36 | |||
| Physical component | 0.935 | −1.061124271 | −0.964980518 |
| Mental component | 0.516 | −0.662695446 | −0.625877193 |
| Bilisşel Egzersiz Terapi Yaklaşımı-biopsychosocial questionnaire (0–120) | 0.437 | 0.772958735 | 0.760591624 |
Mann-Whitney U test.
Both the exercise methods had moderate and high levels of effect for all parameters (0.46≤d≤1.38). FIQ (d=1.38), SF-36 physical component (d=1.06), and SF-36 mental component (d=0.66) in the one-to-one exercise method and HAQ (d=0.68) and BAI (d=0.63) in the group-based exercise method had a greater effect; the 2 groups had a similar effect in terms of BETY-BQ (d=0.77, d=0.76) (Table 3).
Discussion
In this study, clinical Pilates exercises were performed as one-to-one and group-based methods in patients with FM. Our results have shown that after treatment, group-based exercise methods improved all parameters, whereas one-toone exercise method improved all parameters, except functional status and anxiety. When the post-treatment data were compared, the groups did not show superiority to each other in any other parameters. Therefore, effect size analysis was performed, which showed that one-to-one exercise method had a greater effect on disease impact and quality of life, whereas group-based exercise method had a greater effect on functional status and anxiety, and both the methods had a similar effect on biopsychosocial status. Consequently, one-to-one exercise method has helped individuals to improve disease impact and quality of life by solving individual physical problems. Group-based exercise method helps the participants to get together and socialize. Furthermore, it helps them psychologically by seeing other individuals who have similar problems as their own, thus improving the anxiety score. Moreover, we believe that group-based exercise motivates the participants by them seeing another person being able to perform the exercises and hence supports functionality.
It has been reported in the literature that physical exercise is a low-cost, safe, and effective method in patients with FM that plays a role in reducing the pain severity and number of painful tender points, improving the quality of sleep and life, as well as reducing the symptoms of depression by supporting them psychologically (31–34).
Modified Pilates is a different and useful exercise method that increases spinal mobility, flexibility, and muscle strength in the treatment of FM (17). It has been reported that Pilates can lead to good adherence because it uses equipment and exercises divided into levels of progression (35). It has been indicated that Pilates exercises may cause less muscle pain, may be more enjoyable and stimulating and could be an easy and alternative method in patients with FM who tend to be resistant to exercise (17).
Some studies have been performed on Pilates and examined its effect in patients with FM. In the first clinical trial by Altan et al. (14), Pilates, performed as a group method, was found to be more effective on pain and disease impact than home-based relaxation/stretching exercises in patients with FM. In parallel with this study, our study has shown that the exercise of both groups, which were performed as supervised by the physiotherapist, increased adherence of individuals and had a positive effect on quality of life, biopsychosocial status, functional status, and anxiety in addition to disease impact. Korkmaz (16) has reported that the 12-week Pilates program had a positive effect on weight control, anthropometric parameters, social-physical concern, pain, and depression in patients with FM. Ekici et al. (11) have shown that group-based Pilates exercises were more effective on anxiety and pain-pressure threshold than connective tissue massage in patients with FM. In our study, the group-based exercise method was found to have a greater effect on anxiety and functional level. We believe that this may be owing to the group-based method providing social interaction and motivation within the groups. This motivation has also contributed to the improvement of functional outcomes by increasing the individual’s willingness to exercise and by continuing the exercise as seen numerically in the flowchart. The group-based exercise method showed a higher impact on anxiety; therefore, in future studies, it could be of interest to compare the 2 group of patients in terms of other factors that may influence this aspect, such as specific drugs intake, psychotherapy, duration of the disease, and so on, or to evaluate the effect of group-based exercises on anxiety in patients previously treated with one-to-one exercise method. In the protocol study by Silva et al. (18), which compared 12-week group-based mat Pilates exercises with aquatic aerobic exercises in patients with FM, both methods have shown beneficial effects on pain and disability but did not show superiority over each other. In another protocol study, which compared the effects of modified Pilates exercises with aerobic exercises, modified Pilates has been reported to be more effective than aerobic exercises in improving symptoms and this improvement could be sustained in the medium and long term (17). In our study, clinical Pilates was performed instead of traditional Pilates. In clinical Pilates exercise, all movements are under the patient’s control. The exercises are protective against injury and proceed to an upper level only when the patients adapt to the key elements, which is why we chose it as clinical Pilates would be safer and more practical for our patients with FM.
In the literature, there are some studies that have compared different treatment methods in different patient populations. A systematic review by Robertson and Harding (36) has shown that both group-based and one-to-one treatment methods had a similar effect on the quality of life, functional disability, and low-back pain. Furthermore, both the methods had a similar effect on incontinence severity and amount of loss of urine in urinary incontinence. Allen et al. (37) have reported that group-based therapy was not superior to one-on-one treatment in terms of pain, function, and performance in patients with knee osteoarthritis. In a study in which constraint-induced movement therapy was applied in patients with stroke, it has been reported that group-based treatment showed a more significant improvement in upper limb function and a longer lasting effect than individual treatment (38). In the studies comparing the effectiveness of the Pilates method in individuals with FM, it has been observed that group-based exercise method was often preferred (11, 14–18). However, our study compared whether clinical Pilates exercises made a difference when performed as one-toone and group-based methods. We observed that clinical Pilates performed as group-based and one-to-one methods had beneficial effects in patients with FM, but these 2 different methods were not superior to each other.
In our study, clinical Pilates exercises were performed by a certified clinical Pilates instructor and a physiotherapist experienced in rheumatology. This was the strength of our study. The limitation of this study was the lack of long-term follow-up to obtain the effectiveness of clinical Pilates exercises in individuals with FM. Another limitation was the difference between the groups in terms of age at baseline because we did not use a stratified randomization technique. Although the average age of the group-based exercise participants was lower, pre-treatment data were similar in terms of outcome measures. Hence, we think that negative situations that could occur owing to age differences did not affect the results of our study.
The sample loss was 25% in our study. The reason for the participants not continuing the exercise program was related to their private life; therefore, we did not examine it in detail. In future studies, we recommend that the effect of FM on the individual’s life should be examined in more detail in terms of adaptation to exercise.
Another detail in this study was that the participants’ body-mass index (BMI) values were high, which is a common problem in individuals with FM. The increased BMI leads to a decreased pain threshold and an increased sensitivity and causes pain to be felt more (39). We also think that the relationship between obesity and exercise will be detailed in future studies.
In conclusion, we found that the one-to-one method of the clinical Pilates exercises helped the patients with FM who had high disease impact and low quality of life, whereas the group-based method helped those with a high anxiety level. It is important to know which exercise method (one-on-one or group-based exercise) should be preferred according to pre-treatment evaluation data for effectiveness of treatment. Therefore, the results of our study are quite remarkable in terms of comparing these 2 methods. When treating FM, 1 of the 2 treatment methods deemed appropriate by the physiotherapist per the patient’s needs and wishes can be chosen.
Main Points.
The one-to-one exercise method had a greater effect on disease impact and quality of life.
The group-based exercise method had a greater effect on functional status and anxiety.
Both methods had a similar effect on biopsychosocial status.
Footnotes
The abstract of this article was presented at the Annual European Congress of Rheumatology (EULAR) 2019 and the abstract of congress were published in journal of Annals of Rheumatic Diseases.
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee for Non-Interventional Clinical Research of Pamukkale University (Approval Date: September 10, 2019; Approval Number: 60116787-020/62191).
Informed Consent: Informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - B.B.Ç., E.G.K.; Design - B.B.Ç., E.G.K.; Supervision - U.B.A., B.B.Ç., U.K.; Data Collection and/or Processing - E.G.K., B.Ç.Ç., A.K.; Analysis and/or Interpretation - E.G.K., B.Ç.Ç.; Literature Search - B.Ç.Ç., A.K.; Writing Manuscript - B.Ç.Ç., E.G.K.; Critical Review - B.B.Ç., E.G.K., U.B.A., U.K.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1. Clauw DJ. Fibromyalgia and related conditions. Mayo Clin Proc. 2015;90:680–92. doi: 10.1016/j.mayocp.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 2. Arnold LM, Gebke KB, Choy EH. Fibromyalgia: Management strategies for primary care providers. Int J Clin Pract. 2016;70:99–112. doi: 10.1111/ijcp.12757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Henriksson KG. Fibromyalgia-from syndrome to disease. Overview of pathogenetic mechanisms. J Rehabil Med. 2003;41:89–93. doi: 10.1080/16501960310010215. [DOI] [PubMed] [Google Scholar]
- 4. Cassisi G, Sarzi-Puttini P, Casale R, Cazzola M, Boccassini L, Atzeni F, et al. Pain in fibromyalgia and related conditions. Reumatismo. 2014;66:72–86. doi: 10.4081/reumatismo.2014.767. [DOI] [PubMed] [Google Scholar]
- 5. Queiroz LP. Worldwide epidemiology of fibromyalgia. Curr Pain Headache Rep. 2013;17:356. doi: 10.1007/s11916-013-0356-5. [DOI] [PubMed] [Google Scholar]
- 6. Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Fluß E, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76:318–28. doi: 10.1136/annrheumdis-2017-211587. [DOI] [PubMed] [Google Scholar]
- 7. Sosa-Reina MD, Nunez-Nagy S, Gallego-Izquierdo T, Pecos-Martín D, Monserrat J, Álvarez-Mon M. Effectiveness of therapeutic exercise in fibromyalgia syndrome: A systematic review and meta-analysis of randomized clinical trials. Biomed Res Int. 2017;2017:2356346. doi: 10.1155/2017/2356346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Busch AJ, Webber SC, Brachaniec M, Bidonde J, Dal Bello-Haas V, Danyliw AD, et al. Exercise therapy for fibromyalgia. Curr Pain Headache Rep. 2011;15:358. doi: 10.1007/s11916-011-0214-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Owsley A. An introduction to clinical Pilates. Athletic Therapy Today. 2005;10:19–25. doi: 10.1123/att.10.4.19. [DOI] [Google Scholar]
- 10.Frank R, Edwards K, Larimore J. Yoga and pilates as methods of symptom management in multiple sclerosis. In: Watson RR, Killgore WDS, editors. Nutrition and Lifestyle in Neurological Autoimmune Diseases Massachusetts. Academic Press; 2017. pp. 189–94. [DOI] [Google Scholar]
- 11. Ekici G, Unal E, Akbayrak T, Vardar-Yagli N, Yakut Y, Karabulut E. Effects of active/passive interventions on pain, anxiety, and quality of life in women with fibromyalgia: Randomized controlled pilot trial. Women Health. 2017;57:88–107. doi: 10.1080/03630242.2016.1153017. [DOI] [PubMed] [Google Scholar]
- 12. Basakcı Calık B, Gür Kabul E, Bas Aslan U, Çobankara V. The effects of clinical pilates exercises on functional level and quality of life in women with fibromiyalgia: A preliminary study. IJMAS. 2018;4:75–7. [Google Scholar]
- 13. Patti A, Bianco A, Paoli A, Messina G, Montalto MA, Bellafiore M, et al. Effects of Pilates exercise programs in people with chronic low back pain: A systematic review. Medicine. 2015;94:e383. doi: 10.1097/MD.0000000000000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Altan L, Korkmaz N, Bingol U, Gunay B. Effect of pilates training on people with fibromyalgia syndrome: A pilot study. Arch Phys Med Rehabil. 2009;90:1983–8. doi: 10.1016/j.apmr.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 15. Palekar TJ, Basu S. Comparative study of pilates exercise verses yogasana in the treatment of fibromyalgia syndrome: A pilot study. Int J Pharm Bio Sci. 2014;5:B410–20. [Google Scholar]
- 16. Korkmaz N. Effects of Pilates exercises on the social physical concern of patients with Fibromyalgia syndrome: A pilot study. Arch Rheumatol. 2010;25:201–7. doi: 10.5152/tjr.2010.29. [DOI] [Google Scholar]
- 17. Franco KFM, dos Santos Franco YR, Santo Salvador EME, do Nascimento BCB, Miyamoto GC, Cabral CMN. Effectiveness and cost-effectiveness of the modified Pilates method versus aerobic exercise in the treatment of patients with fibromyalgia: Protocol for a randomized controlled trial. BMC Rheumatol. 2019;3:2. doi: 10.1186/s41927-018-0051-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. de Almeida Silva HJ, de Almeida Lins CA, Nobre TTX, de Sousa VPS, Caldas RTJ, de Souza MC. Mat Pilates and aquatic aerobic exercises for women with fibromyalgia: A protocol for a randomised controlled blind study. BMJ Open. 2019;9:e022306. doi: 10.1136/bmjopen-2018-022306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Beltrán-Carrillo VJ, Tortosa-Martínez J, Jennings G, Sánchez ES. Contributions of a group-based exercise program for coping with fibromyalgia: A qualitative study giving voice to female patients. Women Health. 2013;53:612–29. doi: 10.1080/03630242.2013.819399. [DOI] [PubMed] [Google Scholar]
- 20. Bennett R. The Fibromyalgia Impact Questionnaire (FIQ): A review of its development, current version, operating characteristics and uses. Clin Exp Rheumatol. 2005;23:S154. [PubMed] [Google Scholar]
- 21. Sarmer S, Ergin S, Yavuzer G. The validity and reliability of the Turkish version of the Fibromyalgia Impact Questionnaire. Rheumatol Int. 2000;20:9–12. doi: 10.1007/s002960000077. [DOI] [PubMed] [Google Scholar]
- 22. Ramey DR, Raynauld JP, Fries JF. The health assessment questionnaire 1992. Status and review. Arthritis Care Res. 1992;5:119–29. doi: 10.1002/art.1790050303. [DOI] [PubMed] [Google Scholar]
- 23. Küçükdeveci AA, Sahin H, Ataman S, Griffiths B, Tennant A. Issues in cross-cultural validity: Example from the adaptation, reliability, and validity testing of a Turkish version of the Stanford Health Assessment Questionnaire. Arthritis Care Res. 2004;51:14–9. doi: 10.1002/art.20091. [DOI] [PubMed] [Google Scholar]
- 24. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. 1988;56:893. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- 25. Eren I, Sahin M, Tunc SE, Cure E, Civi II. Psychiatric symptoms and quality of life in patients with Behcet’s disease. Neurol Psychiatry Brain Res. 2006;13:169–74. [Google Scholar]
- 26. Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 27. Koçyiğit H, Aydemir O, Fişek G, Olmez N, Memiş A. Short Form-36’s reliability and validity of the Turkish version. İlaç ve Tedavi Derg. 1999;12:102–6. [Google Scholar]
- 28. Unal E, Arın G, Karaca NB, Kiraz S, Akdoğan A, Kalyoncu U, et al. Development of a quality of life measurement for rheumatic patients: Item pool construction. JETR. 2017;4:67–75. [Google Scholar]
- 29.Morris M, Morris S, Resistaball CORE. Instructor Certification. Destin, Florida: Resistaball, Inc; 2001. [Google Scholar]
- 30.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 31. Busch AJ, Webber SC, Brachaniec M, Bidonde J, Dal Bello-Haas V, Danyliw AD, et al. Exercise therapy for fibromyalgia. Curr Pain Headache Rep. 2011;15:358. doi: 10.1007/s11916-011-0214-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sieczkowska SM, Vilarino GT, de Souza LC, Andrade A. Does physical exercise improve quality of life in patients with fibromyalgia? Ir J Med Sci. 2020;189:341–7. doi: 10.1007/s11845-019-02038-z. [DOI] [PubMed] [Google Scholar]
- 33. Andrade A, Steffens RDAK, Vilarino GT, Sieczkowska SM, Coimbra DR. Does volume of physical exercise have an effect on depression in patients with fibromyalgia? J Affect Disord. 2017;208:214–7. doi: 10.1016/j.jad.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 34. Andrade A, Vilarino GT, Bevilacqua GG. What is the effect of strength training on pain and sleep in patients with fibromyalgia? Am J Phys Med Rehabil. 2017;96:889–93. doi: 10.1097/PHM.0000000000000782. [DOI] [PubMed] [Google Scholar]
- 35. Franco KM, dos Santos Franco Y, de Oliveira NB, Miyamoto GC, Santos MO, Liebano RE, et al. Is Interferential current before pilates exercises more effective than placebo in patients with chronic nonspecific low back pain?: A randomized controlled trial. Arch Phys Med Rehabil. 2017;98:320–8. doi: 10.1016/j.apmr.2016.08.485. [DOI] [PubMed] [Google Scholar]
- 36. Robertson B, Harding KE. Outcomes with individual versus group physical therapy for treating urinary incontinence and low back pain: A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2014;95:2187–98. doi: 10.1016/j.apmr.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 37. Allen KD, Bongiorni D, Bosworth HB, Coffman CJ, Datta SK, Edelman D, et al. Group versus individual physical therapy for veterans with knee osteoarthritis: Randomized clinical trial. Phys Ther. 2016;96:597–608. doi: 10.2522/ptj.20150194. [DOI] [PubMed] [Google Scholar]
- 38. Doussoulin A, Rivas C, Rivas R, Saiz J. Effects of modified constraint-induced movement therapy in the recovery of upper extremity function affected by a stroke: A single-blind randomized parallel trial-comparing group versus individual intervention. Int J Rehabil Res. 2018;41:35–40. doi: 10.1097/MRR.0000000000000257. [DOI] [PubMed] [Google Scholar]
- 39. Okifuji A, Donaldson GW, Barck L, Fine PG. Relationship between fibromyalgia and obesity in pain, function, mood and sleep. J Pain. 2010;11:1329–37. doi: 10.1016/j.jpain.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]