Abstract
Introduction
Tele-rehabilitation is a method of delivering rehabilitation services using information, technology and communication to everyone, irrespective of their geographic location. National zeal for competitive sports and COVID pandemic has led to an increase in its demand and popularity worldwide. The athletes need immediate treatment and correct rehabilitation to keep them in their game. This review aims to bring into perspective the importance of telemedicine and telerehabilitation in orthopaedics and sports medicine with a focus on virtual reality.
Methods
Articles were searched based on suitable keywords ‘telemedicine’, ‘telerehabilitation’ ‘orthopedics’, ‘orthopaedics’, ‘sports’ and ‘India*’ which were combined using suitable boolean operators in PubMed, Scopus and Web of Science. Government guidelines and laws were also reviewed in view of telehealth and telemedicine.
Conclusion
Tele-rehabilitation and virtual physical therapy are innovative and cost-effective ways to provide the best rehabilitative services to the patients at their doorstep. Virtual reality should be incorporated into the Indian telehealth delivering system with a special focus on the remote athlete population.
Keywords: Telerehabilitation, Remote rehabilitation, Virtual rehabilitation, Sports medicine, Orthopedics, Virtual reality, Psychology, Nutrition, Telemedicine, eHealth
Introduction
In 2017, an executive boardroom meeting was organized by the World Health Organization. The meeting was—Rehabilitation 2030: A call for action. They acknowledged the unmet rehabilitation needs and also the importance of greater access to rehabilitation services throughout the globe [1]. Tele-rehabilitation is one of the methods of providing these much needed rehabilitation services through the use of information and communication technologies, as established by the American Telemedicine Association [2]. Knowing and understanding the functioning of telerehabilitation is the need of the hour, not only to achieve a sustainable developmental goal but also to bring a necessary health service to the doorstep of the patients.
Rehabilitation is the act of restoring someone to a healthy or a normal life. Another dimension in rehabilitation is—the return to play/sport. With the ever-increasing popularity of sports worldwide, various sports have become more competitive and less forgiving to those with an injury. An important factor in early return to play is early and correct rehabilitation [3]. This has also led to the launch of a Centralised Athlete Injury Management System (CAIMS) in India in June 2021. The aim of this online athlete management system is to provide them with correct rehabilitation on time [4].
This review aims to bring into perspective as per the available literature, the importance and effectiveness of telerehabilitation in sports and exercise medicine.
Methods
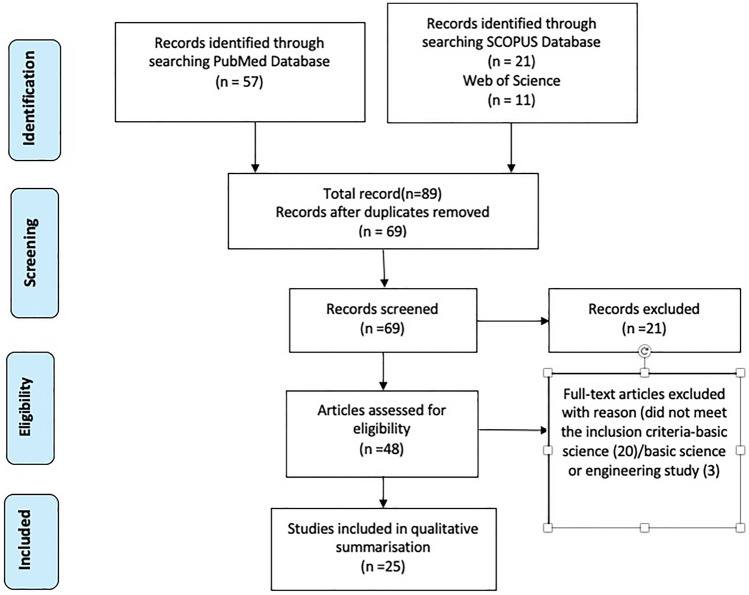
A systematic search of the PubMed, Scopus, and Web of Science databases was performed using the search terms combined with suitable boolean operators[(telemedicine OR telerehabilitation) AND (orthopedics OR orthopaedics OR sports) AND India*] Reference lists of the articles were also screened. Bibliographic references were then fed into the EndNote software application to check for duplication, compilation and subsequent manual selection. The last date searched was 25th July 2022. This search led to 25 relevant papers (Fig. 1). We did not contact the authors for any additional information. Apart from online databases, WHO and various government websites were also searched in view of guidelines laid by them to practice tele-based health services.
Fig. 1.
PRISMA Flowchart showing methodology and selection of papers
Results
The key messages and recommendations from these articles have been summarised in Table 1 [5–37]. The research papers showed that there is evidence regarding the effectiveness of telerehabilitation as a method of providing health care [5–9]. Various papers gave guidelines on conducting a teleconsultation for rehabilitation [12, 13]. Post-operative wound care, suture removal and drain removal could also be done using telecommunication [11]. Devices such as smart watch [17–19], accelerometer [20–23], and other movement sensors [34] could be used along with telerehabilitation The use of virtual reality for rehabilitation was also explored and had a positive review [15, 16, 24–26]. Based on these papers it can be concluded that telerehabilitation and virtual reality should be incorporated into the Indian telehealth delivering system with a special focus on the remote athlete population.
Table 1.
Summary on tele-rehabilitation and recommendations by various authors
| Is it a satisfactory and effective mode of providing treatment? | Yes [5–9], functional MRI shows the same cortical activation in patients undergoing telerehabilitation as in traditional rehabilitation [10] |
| What does telerehabilitation include? | Home physiotherapy training on ROM exercises, strength, balance, gait retraining, rehabilitation for RTP and RTP assessment [11] |
| How to identify and take consent of a patient? | Using UID verification and Google forms etc. [12, 13] |
| Is telemedicine accurate in diagnosing musculoskeletal conditions? | Yes, spine conditions can be diagnosed highly accurately [14]; in 94% of patients’ telemedicine diagnosis and surgical plan remained unchanged on subsequent hospital visits. Radiculopathy, myelopathy and neurogenic claudication conditions were more easy to diagnose. However deformity, tumor surgery or revision surgeries of the spine needed an in-patient visit before confirmation of diagnosis [14] |
| Can post-operative care be given using telecommunication? |
Yes; post-operative dressings, wound care, suture removal with or without assistance (interactive video instructions), drain removal. Figure eight sutures are more easy to remove than mattress sutures (horizontal) Jackson Pratt drains are easier to remove [11] |
| How to teach exercises? |
Patient to be taught using video demonstration at least 2 angles using teach back method [7, 11] VR based digital trainer—Exer-gaming [15] Example: Xbox KINECT system—table tennis (improving hand–eye coordination), golf, boxing (These can help in improving reaction time), soccer (weight-shifting and weight-bearing training), ski, football (balance training) [15]; Nintendo Wii Fit (balance training) [16] |
| What are the devices that can be used for telerehabilitation? | Smart wristwatches connected to apps like Zepp/Google fit [17–19]; Belt strap with sensor for HRM connected to apps via bluetooth [17]; Accelerometer [20–23]; APECS |
| What is the latest, is VR effective and how can it be used in sportsmen specifically? | Virtual reality (VR). Yes [24–27] VR based games like boxing can help in non-contact training before returning to training in the ring and RTP. Games like table tennis (improving hand–eye coordination), golf (improving trunk rotation and lumbopelvic control), boxing (improving reaction time) [15, 16] |
| How does VR help in improving the quality of rehabilitation? | VR system provides feedback and evaluation for rehabilitation training using sensors like accelerometer, gyroscope, magnetometer and constellation tracking camera, thereby improving the quality of rehabilitation [28] |
| Has telemedicine or telerehabilitation been tested clinically? | Yes [29]. Clinical efficacy of VR was demonstrated in terms of motor intention recognition rate, completion of task and average total time [29] |
| Has VR-based rehabilitation been used clinically and where? | Yes [28, 30]. It has been used for ankle instability, focusing on improving balance, proprioception and decreasing muscle imbalance. [31] Also used in upper limb rehabilitation training [28] |
| How can VR be used in post-operative follow-up in orthopedics? | Improves early functional outcomes [11]; Multimodal stimuli is provided to the patient and he is fully immersed in that simulation. VR-based rehab done in TKR patients [26, 32]. Example: Nintendo Wii Fit [15], VERA system [33] |
| What to do in telemonitoring/follow-up? | Patient’s pain, swelling, ROM, muscle strength, balance and proprioception can be reassessed |
| How can you assess the quality of exercises done during rehab? | Sensor-based assessment [20–23]. Example: VERITAS system [33], Force-based and speed-based sensors (eFisioTrack virtual PT) [34] |
| What is biometric data that is to be monitored during tele-rehab and how to measure it? | Physiological data—heart rate (HR), heart rate variability (HRV), blood pressure (BP), temperature, oxygen saturation, electrocardiogram (ECG), SpO2 (oxygen saturation), sleep parameters—which can be measured through smart-watches, chest strap HR monitor and similar devices [17–19] |
| What other biomechanical data can be obtained? | Electromyography, range of motion, motor control, force, tone, torque, displacement, etc.—can also be measured and can be used in better virtual assessment of an individual [17–19] |
| What alternatives can be used to make telerehabilitation more effective and not monotonous? | Virtual yoga [11], interactive group sessions for integrative rehabilitation, telenutrition [35], telepsychology [36, 37] |
| How to make telerehabilitation more holistic? | Tele-nutrition [35], tele-psychology [36, 37], awareness about doping |
MRI Magnetic resonance imaging, ROM Range of motion, RTP Return to play, UID Unique identification numbers, VR Virtual reality, HRM Heart rate monitoring, APECS Artificial intelligence-based posture evaluation and correction system, TKR Total knee replacement, VERA system Virtual exercise rehabilitation assistant
Discussion
India’s digital policy advocates for the use of digital tools for improving the delivery of various healthcare facilities. The Ministry of Health and Family Welfare of India brought out telemedicine practice guidelines in partnership with NITI Aayog. They mentioned 4 modes of communication and discussed the strengths and limitations of each, these modes included—video (telemedicine facility, video-chat platforms), audio (phone), text-based/chat-based platforms (WhatsApp messenger, facebook messenger, SMS, other similar smartphone apps) and asynchronous modes (emails, fax, recordings, etc.) [13, 38–42]. The telemedicine network of India has come a long way since it was first started as a pilot project by the Indian Space Research Organization (ISRO) in 2001 [43]. These advances in communications /internet network allow us to deliver quality health and rehabilitation services at any place including the patient’s home or a low-resource setting via various telecommunication technologies [44–49].
In a population of 1.39 billion [50], sports literacy in India is only 5.56% of the total population [51]. This could be due to the very high dropout rate of young athletes; one of the reasons for this is their injury and its inadequate rehabilitation [52]. Tele-rehabilitation could help in the proper treatment of an injured athlete irrespective of his location and thereby help in early return to play, decrease in dropout rates and increased participation in sports.
The advantages of telerehabilitation have been well documented in literature; it is cost effective, has good adherence and low drop-out rate. It is easily accessible, the travel time is decreased (even possible in the comfort of home), it involves decreased dependence on others to receive care. Hence there is a decrease in loss of training time, continuity of care is maintained across different locations and training centres. The main advantage is an increase in the chances of getting specialty/quality care with an interdisciplinary team (orthopaedic and sports medicine specialists, physiotherapist, sports nutritionist and psychologist and the coaches). The ease of conducting group-based rehabilitation (such as postoperative physiotherapy sessions, yoga, Tai Chi, and pilates) makes it less monotonous and more engrossing for the patient. He can compare and assess himself while performing the exercises in a group. The pictographic memory associated with it also lasts longer [10, 18, 53].
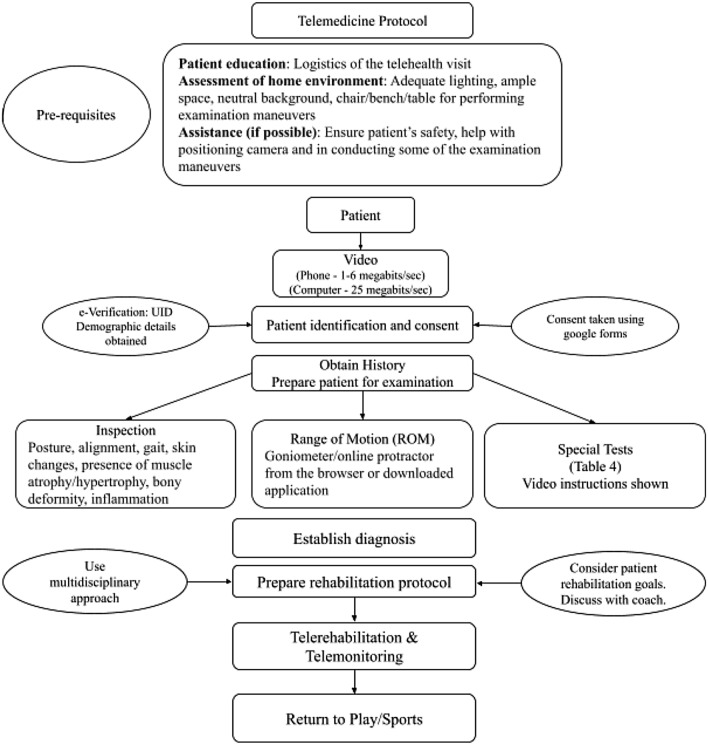
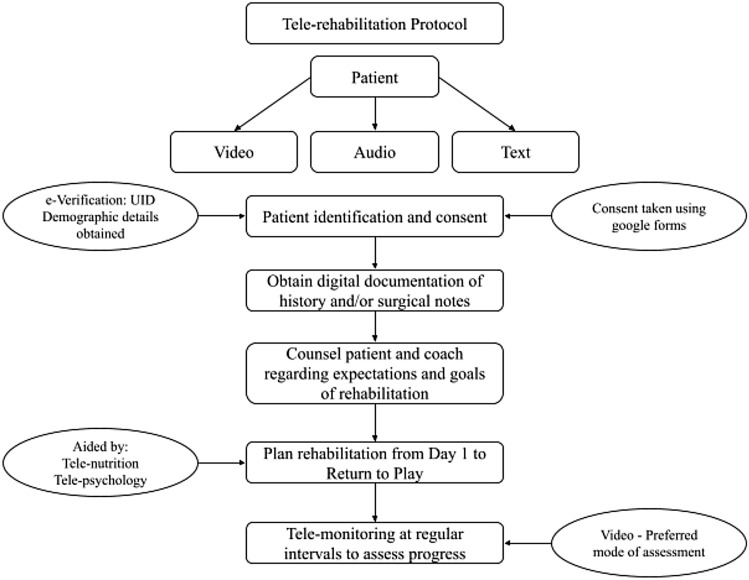
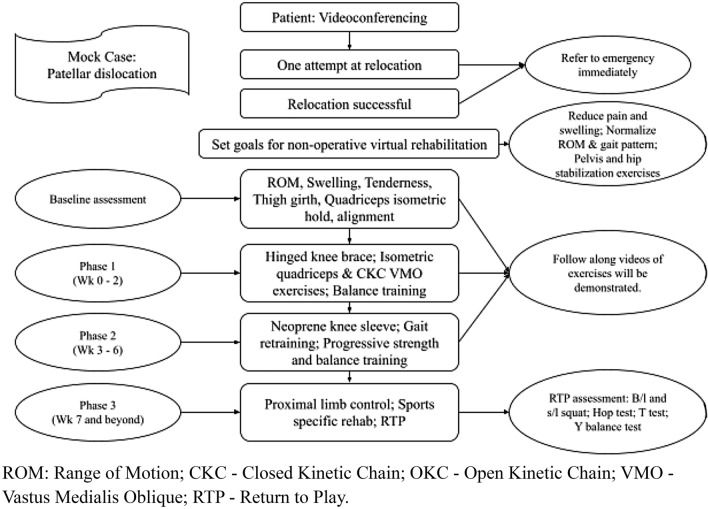
Figures 2, 3, 4, 5, 6 represents essential elements of telerehabilitation and how it can bridge a gap between patients in remote area and an apex health facility. The patient can contact his nearest health facility to get his physical assessment done, the specialists in the central institutes could assess him and manage him using a team approach. Similarly, the specialists can also follow up cases of orthopaedic surgeries so as to provide the best course of action in future-tele-follow-up.
Fig. 2.
Tele-rehabilitation could bridge a gap between the patients in the remote area and the quality services that are provided at an apex centre. Telemedicine Flowchart
Fig. 3.
Tele-rehabilitation Protocol
Fig. 4.
Mock Case Tele-rehabilitation of 1st time Patellar Dislocation
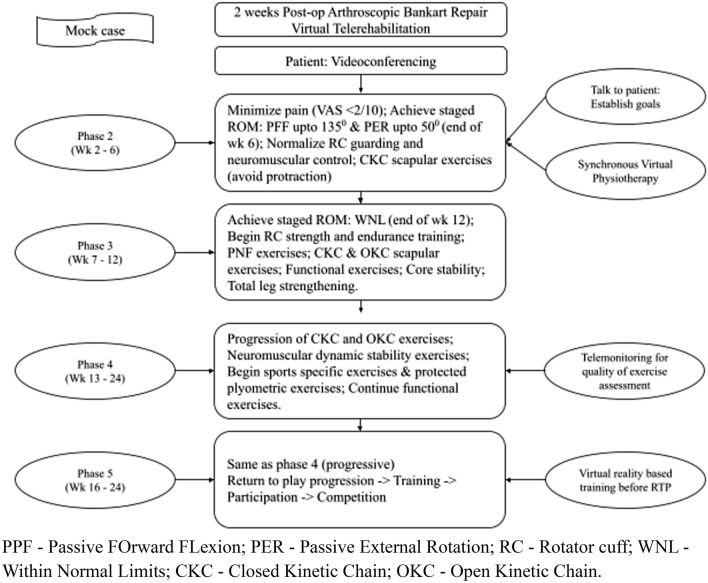
Fig. 5.
Mock Case Tele-rehabilitation 2-week post-operative arthroscopic Bankart Repair
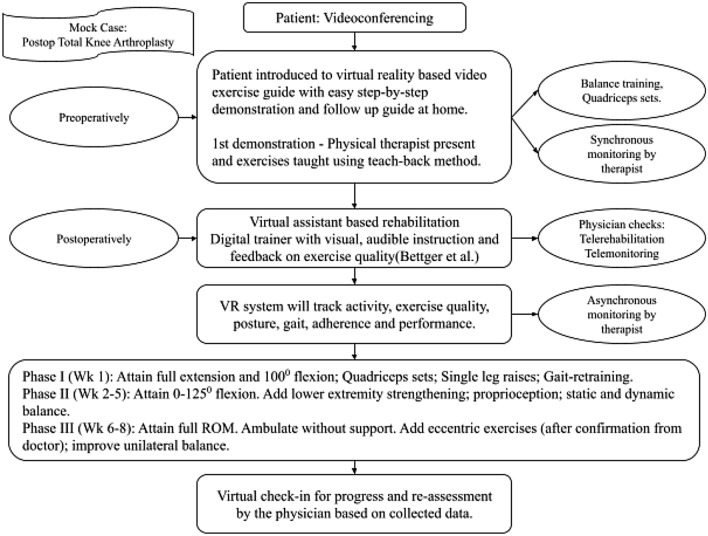
Fig. 6.
Mock Case Tele-rehabilitation of Total Knee Arthroplasty
The prerequisites for a telemedicine or telerehabilitation visit by a sports person/orthopaedic patient are: [11].
Good internet connection.18 Telecommuting requires 5—25 Mbps download speed. HD video teleconferencing requires a minimum download speed of 6 Mbps whereas HD personal video call (example: skype) requires 1.5 Mbps [54, 55].
High-quality camera and microphone. 51, 52:Some digital examination cameras that can be used for telemedicine have been mentioned by Baker J et al. (2018) [56]. Chris Patricoski et al. described 10 considerations for digital camera selection include: (1) camera user experience, (2) clinical application, (3) image quality, (4) advanced settings that may be needed, (5) ease of usage, (6) macro setting, (7) power source, (8) image transfer, (9) docking station requirement and (10) price. After these considerations, they found that Kodak V1233, Fuji F40 and EX-Z1200 were a good choice for telemedicine (57).
Adequate room lighting
Adequate space to stand and move about in front of the camera
Availability of sturdy chair, bench and table for performing various tests
Determine correct laterality [58]. Patient should be wearing comfortable and loose clothing.
Tools (from provider/freeware) for teleconsultation should be downloaded and pre-installed in the computer/laptop like the consultation application, online protractor or goniometer websites or apps etc. [18].
It is essential that the patient sees a video guide on do's & don'ts of teleconsultation including a demonstration of various physical examination tests prior to his/her telehealth visit. (11) (Table 2) [11, 59–61]
Table 2.
| Anatomical Region | Examination (Ask patient to look into camera, turn with back to camera and turn to side pose). Palpation with opposite limb (O)/rarely assistant (A). ALL COMMUNICATED BY PRERECORDED VIDEO | Special Tests | PROM/History using google forms etc. prepared by clinician | Home-based tele-rehabilitation exercises (Pre-recorded Video/Virtual reality based) |
| Shoulder: 3 bony points to be palpated and compared: acromion, greater tuberosity and coracoid. (O/A) | Inspection and ROM (in telemedicine assess range of motion during inspection) Don’t miss pain/patient grimace during range of motion, scapular dyskinesis. Palpation- Don’t miss hot joints (temperature), bony deformity/hollowness/bony tenderness/distal sensory or motor loss—red flags − > suggest clinic visit; temperature (with opposite hand—O); tenderness (O) | Impingement tests:painful arc, Hawkins(A-assist) and Neers. Rotator cuff tests:empty can, belly press,drop arm; Biceps pathology: Uppercut test#; Yergason test; Speed test; Instability: Dugas, Sulcus sign; Cross body adduction test; AC traction test Voluntary dislocation | VAS; QuickDASH ASES; OSS | ROM exercises; Isometric (press against wall) − > Concentric − > Eccentric RC strengthening using resistance bands; Thrower’s 10 program; MPSSEs; Doorway stretch (Pectoralis major, minor), Table stretch(Latissimus dorsi); Exercise promoting truck rotation |
| Elbow: 3 bony points with back to camera; epicondyles; olecranon | As above. Don’t miss capillary filling, distal sensory or motor loss—red flags − > abort tele visit | Springing the radius; Tinel test; Cozen test; Tests for medial epicondylitis (A/O) | VAS; ASES | ROM exercises; Wrist stretches; Graduated exercise with weights or resistance bands; Coordination exercise with rod/body blade for pronation and supination |
| Hand And Wrist: 3 bony points; styloids; anatomical snuff box | As above Don’t miss capillary filling, distal sensory or motor loss—red flags − > abort tele visit | Bench press test Tinel test; Phalen test; Finkelstein test; Froment sign; Ok Sign; Cross Finger; Pointing Index; Hand Grip | VAS; PRWE; Michigan Hand Outcome Questionnaire | ROM exercises; Functional wrist strengthening and neuromuscular training using ball, towel stretch on table, slosh pipe, wrist weights; Tendon gliding exercises; Strengthening of fingers using putty, grippers and stress balls |
| Hip: 3 bony points: ASIS, GT, ISCH. T | Don’t miss: Typical attitudes—FABER, FADIR, FD hip from side camera; Limb length discrepancy—galeazzi sign; GAIT—abnormal gait − > red flag. Groin tenderness versus hip joint tenderness Trochanteric tenderness often with ITB tenderness/tight distally | Active SLR/internal rotation. Trendelenburg test; Thomas test(A) | OHS; HHS; WOMAC | ROM exercises; Deep hip stabilizer strengthening exercises in 4-point kneel with resistance band; gluteus maximus retraining exercises; trunk muscle strengthening; retraining of functional activities—s/l hop for distance; landing training; avoid sit ups |
| Knee: 3 bony landmarks—patella, femur condyles & tibial tuberosity | Don’t miss: Locked knee; Extensor lag; Suprapatellar fullness; Parapatellar fullness; Swelling over pes anserine bursa, tibial tuberosity; Popliteal fossa fullness; Position of the patella; J sign,Sag sign, abnormal varus valgus hyperextension thrust in gait. Don't miss distal sensory motor loss; capillary filling | Springing of fibula. Patella grinding; Thessaly test; Strength test; Drawer tests (ADT, PDT-A) Gower sign climb/down climb stairs, cinema sign | Lysholm score; IKDC (subjective); Tegner activity level rating scale | ROM exercises; Isometric quadriceps, hamstrings, VMO exercises using towel; body weight exercises like squats, lunges; Nordic hamstring curls; L-protocol for hamstring; Balance and proprioception on wobble board/pillow; carioca exercises; Nintendo Wii Fit for TKR patients [15] |
| Ankle, Foot: 3 bony points—malleoli and point of heel | Walk without footwear; Foot drop; Foot slapping Foot pronation or supination; stand on toes—achilles tendon injury, flexible pes planus | Tiptoe walking Tinel test at medial ankle; Thompson test; Metatarsal squeeze test; Thumb index squeeze test | VAS; FAOS; FFI | ROM exercises; Heel raises; intrinsic foot muscle strengthening using towel; plantar fascia stretches; skipping; fast stairs climbing |
| Spine and SI Joint Neurological assess Gait | Don’t miss red flag—> unstable spine—spinous process tenderness/ deformity or swelling with neurological deficit. Active Straight Leg Raise test; Don’t miss to compare with other limb. Don’t miss myelopathy—Close and open your hand rapidly for 10 s. Although the rate varies with gender and age, inability to perform at least 20 repetitions in 10 s suggests weakness/incoordination of gait. Do finger nose test. Inspect for any gait abnormality: antalgic gait, trendelenberg, stiff hip gait, scissoring gait, pelvic tilt, trunk sway, foot drag | Holdswath test—(A/O). Spurling*; Slump Test#; Roos test FABER test (Patrick test) on chair Lower extremity strength testing; Walk on toes, heels Perform repeated heel raises. Unilateral sit-to-stand maneuver. Upper extremity strength testing: Grip a weighted object, such as a water bottle. Active SAR. Limited sensory testing—soft cloth, cotton ball, make-up brush, toothpick, pen, paper clip | VAS; HOOS; Mayo Hip Score; Hip Outcome Score | ROM exercises; Rotational and bending exercises in a direction away from pain; Virtual reality-based demonstration of correct active and passive movement patterns to offload the affected musculature; self-static stretching for erector spinae, psoas, ITB, hip external rotators, hamstrings, rectus femoris; cat and camel pose; cobra pose. Glute bridge with progressing difficulty level. Gait-retraining, balance and posture correction using virtual reality-based trainers, feedback and exercises |
*These tests need to be done under caution. A quick response team may need to be dispatched in case of an emergency. Inspection is to be done by a physician. Instruct the patient to walk towards and away from the camera. Assess in standing and supine position from all sides. Assess for posture; attitude; alignment; symmetry; skin discoloration; redness; scars; sinuses; swelling; deformity; muscle atrophy; range of motion. Palpation can be done by the patient himself, however, it would be advisable to have assistance. Neurovascular status can be assessed using capillary refill time and SpO2 probe
#Upper cut test: Shoulder in a neutral position, elbow flexed to 900, fist clenched, and wrist supinated. The patient moves the wrist toward the chin while the other hand is placed over the fist to resist this
#Slump Test: In seated position extend the knee and passively dorsiflex the ankle using a towel or cloth. In the supine position, with the knee extended, the leg can be raised using a towel. Positive test: Pain reproduction
#Patrick Test: While lying supine or seated, flex the knee, externally rotate the hip, and place the ankle just above the contralateral knee. Then apply downward pressure on the flexed knee while stabilizing the contralateral pelvis. Positive test: pain in the lower back is exacerbated, suggesting sacroiliac joint pathology
O use opposite hand for examination, A assistant helps; MPSSEs Modified posterior shoulder stretching exercises, FABER Flexion, abduction, external rotation, FADIR Flexion, adduction, internal rotation, MFC medial femoral condyle, LFC Lateral femoral condyle, MTP Medial tibial plateau, LTP Lateral tibial plateau; VAS Visual analogue scale, quickDASH Quick disabilities of the arm, shoulder and hand, ASES American shoulder and elbow surgeons shoulder score, OSS Oxford shoulder score, PRWE Patient rated wrist/hand evaluation, OHS Oxford hip score, HHS Harris hip score, IKDC International knee documentation committee, FAOS Foot and ankle outcome score, FFI Foot function index
The additional set-up/accessories that can be used to improve the quality of telerehabilitation are:
Wearable technology like smart-watches/chest strap HR monitor/portable pulse oximeters can help in collecting certain parameters of health (like HR, HR variability, sleep patterns, etc.) which can help in assessing the performance of the athlete and thereby can help in the improvement of the performance [17–19].
There are technologies which can potentially compensate for the deficit in the virtual examination of the musculoskeletal system like motion sensing input devices etc.
Use of mobile apps like—APECS could also be used by the physician as well as patients. APECS stands for Artificial Intelligence-based Posture Evaluation and Correction System. It is an app developed by doctors. It was first released on Jul 27, 2018 on the google play store, offered by New Body Technology. It has photo-grammetric algorithms which could help in accurate posture assessments preventing low backache etc.
Virtual reality; a technology that can help in revolutionizing the delivery of telehealth, telemedicine and telerehabilitation [62].
Virtual reality (VR) is an advanced communication interface that assists in the biomechanical assessment (posture, alignment), balance, coordination, reaction time training, strength and endurance of the athlete in telemedicine and telerehabilitation.
Essentials of a VR system—Head-mounted display (fully immersive) or monitor display device (partially immersive) like desktop monitor; interactive input device like mouse, joystick; PC (personal computer) engines; 3D accelerator cards for real time 3D simulation display [62].
VR devices could be PC (personal computer) based, mobile-based, console-based or standalone.
In a PC-based device the system includes Oculus Rift S, HTC COsmos/Vive Pro/Pro Eye, Valve Index or HP Reverb G2. For these systems, the specifications are as follows: Video card—NVIDIA GTX 1060/AMD Redeon RX 480 or greater; CPU—Intel i5-4590/AMD Ryzen 51500X or greater; Memory—8 GB RAM or greater; Video Output—DisplayPort; USB Ports: 1 × USB 3.0 port; OS—Windows 10. Sensors include—Accelerometer, gyroscope, magnetometer and constellation tracking camera. [63] The resolutions should be 2560 × 1440 or above, with a refresh rate ranging between 90–120 Hz. They should also have high body tracking with high user interaction using controllers [62, 63].
In a mobile-based device, the system includes Samsung Gear VR, Google Cardboard or Google Daydream. The minimum resolution required is 1024 × 768 with a refresh rate ranging from 60 to 90 Hz. Body tracking should also be available with low to medium user interaction using gaze or joystick or built-in pad [62].
In console-based and standalone devices have similar specifications. These systems include PlayStation VR, Xiaomi MI XR, Oculus Quest 2, Lenovo VR Classroom 2 [64]. Exergaming is a blend word which can be defined as a technology-driven physical activity. A preliminary study conducted on stroke survivors found that virtual reality-augmented rehabilitation has significantly better outcomes than conventional therapy. This virtual reality environment was provided using the video game—XBox Kinect system. Kinect system uses infrared depth sensor and RGB camera to capture data for creating 3D human body model in real-time and for body position and motion assessment [15].
The advantages of VR includes: increase in activation of the primary sensorimotor cortex, the supplementary motor area and cerebellum while performing hand clenching tasks; it reduces health staff time and increases patient motivation towards rehabilitation [15]. The kinect-based VR training includes auditory and visual stimulation; further feedback information about winning or losing and repetitions of the same motion provides a variable engrossing (versus performed in front of a mirror in conventional physical therapy) and barrier-free tool for rehabilitation exercises [15]. In-built logging-in tracking system of VR provides information about compliance. Despite sparse evidence, functional improvements observed by combining VR and tele-rehab seem to be comparable to traditional rehabilitation [30].
Tele-Integrative Medicine for Athletes: Complementary and various integrative health techniques like yoga, tai chi, self-massage, mindfulness meditation have been used for managing chronic pain and can be easily incorporated into telemedicine as supportive rehabilitative care for athletes [64].
Tele-Psychology for Athletes: The mental health of elite athletes impacts their physical performance [65] and we need to address this issue through telepsychiatry while we address their physical symptoms through telerehabilitation. Various studies have shown that in-person treatment is comparable to telehealth services for mental health conditions like PTS, anxiety and depression [66].
Tele-Nutrition for Athletes: Nutrition also plays an important role in the rehabilitation and general well being of the athlete. Need for education about nutrition is essential to improve performance by promoting healthy weight gain or loss and adequate energy intake [67]. Not only is nutrition essential for recovery, it is also essential for maintaining the correct body composition and anthropometric parameters for the athletes according to their respective sports. Tele-nutrition can help increase awareness regarding the relative energy deficiency in sports and to help the athletes have a healthy outlook towards food and calorie intake.
Current research and various clinical studies have suggested that using biometric data for telerehabilitation (Table 1) enhances performance and makes individualized telerehabilitation protocol. It can also help in improved virtual physical assessment & improves the adherence of the patients to the rehabilitation program thereby improving outcomes [17].
Limitations of Tele-Rehabilitation include: difficulty in performing a comprehensive physical examination, technical difficulties, patient confidentiality problems, patients considering online interactions as impersonal and dangerous, decreased satisfaction in asynchronous telerehabilitation; increased chances of misdiagnosis, and potential medico-legal risks [68].
Limitations of virtual reality-based rehabilitation include: high cost of establishing a setup, cybersickness/simulation sickness (headache, eye strain, nausea, vomiting, dizziness, ataxia, etc.), perceptuomotor after-effects, sleepiness, fatigue, etc. [61, 69].
The authors suggest and propose that the versatility of telemedicine and telerehab can only be exploited fully if we start early, that is incorporate it in school/colleges physical education curriculum, connect schools/colleges to remote telemedicine centres. This will help in catching the youth interested in sports (talent identification) and giving proper, adequate injury care and rehabilitation when necessary. Even the existing Primary Health Centre network in India established as part of the National Health Mission could help in setting up a common telerehabilitation consultation office for the rural population that the PHC caters to. Health workers in the 23,391 PHCs all over India could be trained to perform the various physical examination tests that need to be performed to reach a particular diagnosis. Coaches should also be involved in the rehabilitation of these athletes to ensure compliance with telerehabilitation.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethical standard
This article does not contain any studies with human or animal subjects performed by any of the authors
Informed consent
For this type of study informed consent is not required
Footnotes
In this article the author name of Himanshu Kataria was incorrectly written as Himansu Kataria.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/15/2023
A Correction to this paper has been published: 10.1007/s43465-023-00918-2
References
- 1.Rehabilitation 2030: A call for action. Available online at : https://www.who.int/publications/m/item/rehabilitation-2030-a-call-for-action, last assessed on 1st May 2022
- 2.Maresca G, Maggio MG, De Luca R, Manuli A, Tonin P, Pignolo L, et al. Tele-neuro-rehabilitation in italy: state of the art and future perspectives. Frontiers in Neurology. 2020;30(11):563375. doi: 10.3389/fneur.2020.563375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhillon H, Dhilllon S, Dhillon MS. Current concepts in sports injury rehabilitation. Indian J Orthop. 2017;51(5):529–536. doi: 10.4103/ortho.IJOrtho_226_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Times of India. Sports Minister Rijiju launches an athlete injury management system. Available online at : https://timesofindia.indiatimes.com/sports/more-sports/others/sports-minister-rijiju-launches-athlete-injury-management-system/articleshow/83430543.cms. , last assessed on 1st May 2022
- 5.Kumar S, Kumar A, Kumar M, Kumar A, Arora R, Sehrawat R. Feasibility of telemedicine in maintaining follow-up of orthopaedic patients and their satisfaction: a preliminary study. J Clin Orthop Trauma. 2020;11(5):S704–S710. doi: 10.1016/j.jcot.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iyengar KP, Garg R, Jain VK, Malhotra N, Ish P. Electronic intensive care unit: a perspective amid the COVID-19 era—Need of the day! Lung India. 2021;38(Supplement):S97–S100. doi: 10.4103/lungindia.lungindia_663_20.PMID:33686991;PMCID:PMC8104336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeyaraman M, Muthu S, Shyam A. Indian paradigm of orthopedic care in post-COVID-19 era. J Orthop Case Rep. 2021;11(4):110–116. doi: 10.13107/jocr.2021.v11.i04.2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sahu D, Rathod V, Phadnis A, Bansal SS. Telehealth for consultation and shoulder rehabilitation: a preliminary study on the perspectives of 30 patients during the COVID-19 lockdown. Clin Shoulder Elb. 2021;24(3):156–165. doi: 10.5397/cise.2021.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Q, Lee RLT, Hunter S, Chan SW-C. The effectiveness of internet-based telerehabilitation among patients after total joint arthroplasty: An integrative review. International Journal of Nursing Studies. 2021;115:103845. doi: 10.1016/j.ijnurstu.2020.103845. [DOI] [PubMed] [Google Scholar]
- 10.Maresca G, Maggio MG, De Luca R, Manuli A, Tonin P, Pignolo L, et al. Tele-neuro-rehabilitation in Italy: State of the art and future perspectives. Frontiers in Neurology. 2020;11:563375. doi: 10.3389/fneur.2020.563375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phuphanich ME, Sinha KR, Truong M, Pham QG. Telemedicine for musculoskeletal rehabilitation and orthopedic postoperative rehabilitation. Phys Med Rehabilit Clin North Am. 2021;32(2):319–353. doi: 10.1016/j.pmr.2020.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Iyengar K, Jain VK, Vaishya R. Pitfalls in telemedicine consultations in the era of COVID 19 and how to avoid them. Diabet Metab Syndr. 2020;14(5):797–799. doi: 10.1016/j.dsx.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lal H, Sharma DK, Patralekh MK, Jain VK, Maini L. Out Patient Department practices in orthopaedics amidst COVID-19: The evolving model. J Clin Orthop Trauma. 2020;11(4):700–712. doi: 10.1016/j.jcot.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bovonratwet P, Song J, Kim YE, Shinn D, Morse KW, Dowdell JE, et al. Telemedicine visits can generate highly accurate diagnoses and surgical plans for spine patients. Spine. 2022;47(17):1194–1202. doi: 10.1097/BRS.0000000000004387. [DOI] [PubMed] [Google Scholar]
- 15.Park D-S, Lee D-G, Lee K, Lee G. Effects of virtual reality training using xbox kinect on motor function in stroke survivors: a preliminary study. J Stroke Cerebrovascul Dis. 2017;26(10):2313–2319. doi: 10.1016/j.jstrokecerebrovasdis.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 16.Nicholson VP, McKean M, Lowe J, Fawcett C, Burkett B. Six weeks of unsupervised Nintendo Wii Fit gaming is effective at improving balance in independent older adults. Journal of Aging and Physical Activity. 2015;23(1):153–158. doi: 10.1123/JAPA.2013-0148. [DOI] [PubMed] [Google Scholar]
- 17.Annaswamy TM, Pradhan GN, Chakka K, Khargonkar N, Borresen A, Prabhakaran B. Using biometric technology for telehealth and telerehabilitation. Phy Med Rehabilit Clin North Am. 2021;32(2):437–449. doi: 10.1016/j.pmr.2020.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Matsumoto ME, Wilske GC, Tapia R. Innovative approaches to delivering telehealth. Phy Med Rehabilit Clin North Am. 2021;32(2):451–465. doi: 10.1016/j.pmr.2020.12.008. [DOI] [PubMed] [Google Scholar]
- 19.Meinhart F, Stütz T, Sareban M, Kulnik ST, Niebauer J. Mobile technologies to promote physical activity during cardiac rehabilitation: a scoping review. Sensors (Basel). 2020;21(1):65. doi: 10.3390/s21010065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Porciuncula F, Roto AV, Kumar D, Davis I, Roy S, Walsh CJ, et al. Wearable movement sensors for rehabilitation: A focused review of technological and clinical advances. PM & R : The Journal of Injury, Function, and Rehabilitation. 2018;10(9 Suppl 2):S220–S232. doi: 10.1016/j.pmrj.2018.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anton D, Berges I, Bermúdez J, Goñi A, Illarramendi A. A telerehabilitation system for the selection, evaluation and remote management of therapies. Sensors (Basel). 2018;18(5):1459. doi: 10.3390/s18051459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Dijk-Huisman HC, Weemaes ATR, Boymans TAEJ, Lenssen AF, de Bie RA. Smartphone app with an accelerometer enhances patients’ physical activity following elective orthopedic surgery: a pilot study. Sensors (Basel). 2020;20(15):4317. doi: 10.3390/s20154317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Komaris D-S, Tarfali G, O’Flynn B, Tedesco S. Unsupervised IMU-based evaluation of at-home exercise programmes: a feasibility study. BMC Sports Science, Medicine and Rehabilitation. 2022;14(1):28. doi: 10.1186/s13102-022-00417-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peng Q-C, Yin L, Cao Y. Effectiveness of virtual reality in the rehabilitation of motor function of patients with subacute stroke: a meta-analysis. Frontiers in Neurology. 2021;12:639535. doi: 10.3389/fneur.2021.639535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Asadzadeh A, Samad-Soltani T, Salahzadeh Z, Rezaei-Hachesu P. Effectiveness of virtual reality-based exercise therapy in rehabilitation: a scoping review. Inform Med Unlocked. 2021;24(100562):100562. doi: 10.1016/j.imu.2021.100562. [DOI] [Google Scholar]
- 26.Peng L, Zeng Y, Wu Y, Si H, Shen B. Virtual reality-based rehabilitation in patients following total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials: a systematic review and meta-analysis of randomized controlled trials. Chinese Medical Journal (Engl) 2021;135(2):153–163. doi: 10.1097/CM9.0000000000001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gazendam A, Zhu M, Chang Y, Phillips S, Bhandari M. Virtual reality rehabilitation following total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. Knee Surgery, Sports Traumatology, Arthroscopy. 2022;30(8):2548–2555. doi: 10.1007/s00167-022-06910-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen J. Clinical effect of virtual reality technology on rehabilitation training of sports injury. J Healthc Eng. 2021;2021:1361851. doi: 10.1155/2021/1361851. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 29.Han Y. A virtual reality algorithm for the study of clinical efficacy of sports injury rehabilitation training. J Healthc Eng. 2021;2021:6725625. doi: 10.1155/2021/6725625. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 30.Schröder J, van Criekinge T, Embrechts E, Celis X, Van Schuppen J, Truijen S, et al. Combining the benefits of tele-rehabilitation and virtual reality-based balance training: a systematic review on feasibility and effectiveness. Disability and Rehabilitation. Assistive Technology. 2019;14(1):2–11. doi: 10.1080/17483107.2018.1503738. [DOI] [PubMed] [Google Scholar]
- 31.Lin H, Han K, Ruan B. Effect of virtual reality on functional ankle instability rehabilitation: a systematic review. J Healthc Eng. 2021;2021:7363403. doi: 10.1155/2021/7363403. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 32.Blasco J, Igual-Camacho C, Blasco M, Antón-Antón V, Ortiz-Llueca L, Roig-Casasús S. The efficacy of virtual reality tools for total knee replacement rehabilitation: a systematic review. Physiotherapy Theory and Practice. 2021;37(6):682–692. doi: 10.1080/09593985.2019.1641865. [DOI] [PubMed] [Google Scholar]
- 33.Prvu Bettger J, Green CL, Holmes DN, Chokshi A, Mather RC, 3rd, Hoch BT, et al. Effects of virtual exercise rehabilitation in-home therapy compared with traditional care after total knee arthroplasty: VERITAS, a randomized controlled trial: VERITAS, a randomized controlled trial. Journal of Bone and Joint Surgery. American Volume. 2020;102(2):101–109. doi: 10.2106/JBJS.19.00695. [DOI] [PubMed] [Google Scholar]
- 34.Ruiz-Fernandez D, Marín-Alonso O, Soriano-Paya A, García-Pérez JD. eFisioTrack: a telerehabilitation environment based on motion recognition using accelerometry. ScientificWorldJournal. 2014;2014:495391. doi: 10.1155/2014/495391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gnagnarella P, Ferro Y, Monge T, Troiano E, Montalcini T, Pujia A, et al. Telenutrition: Changes in professional practice and in the nutritional assessments of Italian dietitian nutritionists in the COVID-19 era. Nutrients. 2022;14(7):1359. doi: 10.3390/nu14071359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nelson E-L, Bui TN, Velasquez SE. Telepsychology: research and practice overview. Child and Adolescent Psychiatric Clinics of North America. 2011;20(1):67–79. doi: 10.1016/j.chc.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 37.Alqahtani MMJ, Alkhamees HA, Alkhalaf AM, Alarjan SS, Alzahrani HS, AlSaad GF, et al. Toward establishing telepsychology guideline. Turning the challenges of COVID-19 into opportunity. Ethics Med Public Health. 2021;16(100612):100612. doi: 10.1016/j.jemep.2020.100612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Board of Governors in supersession of the Medical Council of India, Ministry of Health and Family Welfare, Government of India and Niti Aayog; Telemedicine practice guidelines - MoHFW [Internet]; 2020 [cited 2022 May 28]; Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf
- 39.Iyengar K, Upadhyaya GK, Vaishya R, Jain V. COVID-19 and applications of smartphone technology in the current pandemic. Diabetes and Metabolic Syndrome: Clinical Research and Reviews. 2020;14(5):733–737. doi: 10.1016/j.dsx.2020.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Iyengar K, Mabrouk A, Jain VK, Venkatesan A, Vaishya R. Learning opportunities from COVID-19 and future effects on health care system. Diabetes and Metabolic Syndrome: Clinical Research and Reviews. 2020;14(5):943–946. doi: 10.1016/j.dsx.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jain VK, Vaishya R. COVID-19 and orthopaedic surgeons: the Indian scenario. Tropical Doctor. 2020;50(2):108–110. doi: 10.1177/0049475520921616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singhal A, Kapoor A, Gupta R. Sports medicine in COVID Era. J Arthrosc Jt Surg. 2020;7(3):103–104. doi: 10.1016/j.jajs.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chellaiyan VG, Nirupama AY, Taneja N. Telemedicine in India: where do we stand? J Family Med Prim Care. 2019;8(6):1872–1876. doi: 10.4103/jfmpc.jfmpc_264_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ganapathy K, Das S, Reddy S, Thaploo V, Nazneen A, Kosuru A, Shankar NU. Digital health care in public private partnership mode. Telemed J E-Health. 2021 doi: 10.1089/tmj.2020.0499. [DOI] [PubMed] [Google Scholar]
- 45.Iyengar K, Vaish A, Toh E, Vaishya R. COVID-19 and remote consulting strategies in managing trauma and orthopaedics. Postgraduate Medical Journal. 2020;96(1137):438–439. doi: 10.1136/postgradmedj-2020-137917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jaly I, Iyengar K, Bahl S, Hughes T, Vaishya R. Redefining diabetic foot disease management service during COVID-19 pandemic. Diabet Metabolic Synd Clin Res Rev. 2020;14(5):833–838. doi: 10.1016/j.dsx.2020.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jerome JTJ, Mercier F, Mudgal CS, Arenas-Prat J, et al. Perspectives and consensus among international orthopaedic surgeons during initial and mid-lockdown phases of coronavirus disease. Journal of Hand and Microsurgery. 2020;12(3):135–162. doi: 10.1055/s-0040-1713964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lakhani A, Sharma E. Corona virus (Covid-19)—ITS implications in pediatric orthopedic care. J Orthopaed. 2020;13(21):326–330. doi: 10.1016/j.jor.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morreale PA. 2007 Wireless Sensor Network Applications in Urban Telehealth. In: 21st International Conference on Advanced Information Networking and Applications Workshops (AINAW’07). 810–4.
- 50.Kumar M 2021 flashback: The “Super Seven” who gave India its best ever medal haul at the Olympics [Internet]. Times Of India. 2021 [cited 2022 Jul 9]. Available from: https://timesofindia.indiatimes.com/sports/more-sports/others/2021-flashback-the-super-seven-who-gave-india-its-best-ever-medal-haul-at-the-olympics/articleshow/88584587.cms
- 51.The Bridge Desk. Only 5.56% of Indian population is sports literate [Internet]. The Bridge—Home of Indian Sports. 2019 [cited 2022 Jul 9]. Available from: https://thebridge.in/news/only-5-56-of-indian-population-is-sports-literate
- 52.Sáez I, Solabarrieta J, Rubio I. Reasons for sports-based physical activity dropouts in university students. Intern J Environ Res Pub Health. 2021;18(11):5721. doi: 10.3390/ijerph18115721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuroda Y, Young M, Shoman H, Punnoose A, Norrish AR, Khanduja V. Advanced rehabilitation technology in orthopaedics—a narrative review. Intern Orthopaed. 2021;45(8):1933–1940. doi: 10.1007/s00264-020-04814-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Telecom Regulatory Authority of India. Recommendations on Roadmap to Promote Broadband Connectivity and Enhanced Broadband Speed. New Delhi, India; 31–08–2021; 28. Available from: https://www.trai.gov.in/sites/default/files/Recommendations_31082021.pdf
- 55.Baker J, Stanley A. Telemedicine technology: a review of services, equipment, and other aspects. Current Allergy Asthma Rep. 2018;18(11):60. doi: 10.1007/s11882-018-0814-6. [DOI] [PubMed] [Google Scholar]
- 56.Patricoski C, Ferguson AS. Selecting a digital camera for telemedicine. Telemed J E Health [Internet]. 2009;15(5):465–475. doi: 10.1089/tmj.2008.0166. [DOI] [PubMed] [Google Scholar]
- 57.Nanda U, Luo J, Wonders Q, Pangarkar S. Telerehabilitation for pain management. Phy Med Rehabilit Clin North Am. 2021;32(2):355–372. doi: 10.1016/j.pmr.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Das S. A manual on clinical surgery. 15. Das Publications; 2021. [Google Scholar]
- 59.Brukner P, Khan K. Clinical sports medicine. 5. McGraw Hill; 2017. [Google Scholar]
- 60.Brotzman SB, Giangara CE, Manske RC. Clinical orthopaedic rehabilitation. 4. Amserdam: Elsevier; 2017. [Google Scholar]
- 61.Riva G, Gamberini L. Virtual reality in telemedicine. Telemedicine Journal and E-Health. 2000;6(3):327–340. doi: 10.1089/153056200750040183. [DOI] [PubMed] [Google Scholar]
- 62.PSCC libraries: Virtual reality: VR equipment and specs [Internet]. 2018 [cited 2022 Aug 14]; Available from: https://lib.pstcc.edu/vr/about
- 63.Riva G, Serino S. Virtual reality in the assessment, understanding and treatment of mental health disorders. Journal of Clinical Medicine. 2020;9(11):3434. doi: 10.3390/jcm9113434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mullur RS, Kaur Cheema SP, Alano RE, Chang LE. Tele-integrative medicine to support rehabilitative care. Phy Med Rehabilit Clin North Am. 2021;32(2):393–403. doi: 10.1016/j.pmr.2020.12.006. [DOI] [PubMed] [Google Scholar]
- 65.Rice SM, Purcell R, De Silva S, Mawren D, McGorry PD, Parker AG. The mental health of elite athletes: a narrative systematic review. Sports Med Auckl NZ. 2016;46(9):1333–1353. doi: 10.1007/s40279-016-0492-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wells MJ, Dukarm P, Mills A. Telehealth in rehabilitation psychology and neuropsychology. Phy Med Rehabilit Clin North Am. 2021;32(2):405–418. doi: 10.1016/j.pmr.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Folasire OF, Akomolafe AA, Sanusi RA. Does nutrition knowledge and practice of athletes translate to enhanced athletic performance? Cross-sectional study amongst nigerian undergraduate athletes. Glob J Health Sci. 2015;7(5):215–225. doi: 10.5539/gjhs.v7n5p215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gajarawala SN, Pelkowski JN. Telehealth benefits and barriers. J Nurse Pract. 2021;17(2):218–221. doi: 10.1016/j.nurpra.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Baniasadi T, Ayyoubzadeh SM, Mohammadzadeh N. Challenges and practical considerations in applying virtual reality in medical education and treatment. Oman Medical Journal. 2020;35(3):e125. doi: 10.5001/omj.2020.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Havran MA, Bidelspach DE. Virtual physical therapy and telerehabilitation. Phy Med Rehabilit Clin North Am. 2021;32:419–428. doi: 10.1016/j.pmr.2020.12.005. [DOI] [PubMed] [Google Scholar]
- 71.Petersen W, Karpinski K, Backhaus L, Bierke S, Haner M. A systematic review about telemedicine in orthopedics. Archiv Orthopaed Trauma Surg. 2021;141:1731–1739. doi: 10.1007/s00402-021-03788-1. [DOI] [PMC free article] [PubMed] [Google Scholar]