Abstract
Objective
To describe the demographics and outcomes of sports‐related ocular injuries in an Australian tertiary eye hospital setting.
Methods
Retrospective descriptive study from the Royal Victorian Eye and Ear Hospital from 2015 to 2020. Patient demographics, diagnosis and injury causation were recorded from baseline and follow‐up. Outcomes included visual acuity (VA), intraocular pressure (IOP), ocular injury diagnosis, investigations and management performed.
Results
A total of 1793 individuals (mean age 28.67 ± 15.65 years; 80.42% males and 19.58% females) presented with sports‐related ocular trauma. The top three injury‐causing sports were soccer (n = 327, 18.24%), Australian rules football (AFL) (n = 306, 17.07%) and basketball (n = 215, 11.99%). The top injury mechanisms were projectile (n = 976, 54.43%) and incidental body contact (n = 506, 28.22%). The most frequent diagnosis was traumatic hyphaema (n = 725). Best documented VA was ≥6/12 at baseline in 84.8% and at follow‐up in 95.0% of cases.
The greatest risk of globe rupture/penetration was associated with martial arts (odds ratio [OR] 16.22); orbital blow‐out fracture with skiing (OR 14.42); and hyphaema with squash (OR 4.18): P < 0.05 for all. Topical steroids were the most common treatment (n = 693, 38.7%). Computed tomography orbits/facial bones were the most common investigation (n = 184, 10.3%). The mean IOP was 16.1 mmHg; 103 (5.7%) cases required topical anti‐ocular hypertensives. Twenty‐six individuals (1.45%) required surgery with AFL contributing the most surgical cases (n = 5, 19.23%).
Conclusion
The top three ocular injury causing sports were soccer, AFL and basketball. The most frequent injury was traumatic hyphaema. Projectiles posed the greatest risk.
Keywords: eye, injury, ocular, sports, trauma
To describe the demographics and outcomes of sports‐related ocular injuries in an Australian tertiary eye hospital setting.

Key findings.
The most frequent sports associated with ocular trauma over a 5‐year period in a tertiary eye hospital in Melbourne were soccer, Australian rules football, and basketball. With the most common injuries sustained to the eye in sports‐related trauma are traumatic hyphaema and uveitis, commotio retinae, and superficial injury to the cornea and conjunctiva. Projectile was the most common causative mechanism contributing to 54.43% of injuries.
Mean patient age was 28.67 years and there was a downward trend in number of cases in each age group above the age of 30. The percentage of paediatric patients was 30.56%. The study identified that paediatric age patients were more likely to have retinal tears.
The study observed that only 1.45% of patients require surgical management to the eye. However, a large number of patients required anti‐ocular hypertensive, anti‐inflammatory and cycloplegic drops to treat the immediate consequences of blunt trauma. This suggests that while majority of patients had excellent VA upon presentation, this does not necessarily exclude the potential for significant ocular injuries and the imperative upon timely review.
Introduction
Sport‐related injuries contribute a large number of healthcare presentations each year. 1 Although musculoskeletal injuries are a common presentation of these injuries, studies have also explored the incidence of sport‐related ocular trauma. 2 , 3 Ocular injuries are an important cause of visual morbidity and loss of quality of life. 4 The Australian Institute of Health and Welfare reported that among 52 000 admissions of eye injuries to hospitals, sports‐related eye injuries accounted for 3886 presentations (7.5%). 5 This compares to 3.3% of all ocular trauma presenting to the ED in the United States, 6 and 12.5% of all ocular trauma requiring inpatient care in Scotland. 2 Sports‐related ocular trauma has shown a predilection for young people, particularly those aged 25–44 years, with a strong prevalence among males.
Sports‐related ocular injuries have generated considerable interest and research. Although key papers were published many years ago, as rules and regulations in sport are frequently updated, it is important for recommendations to be guided by up‐to‐date evidence. 7 , 8 , 9 , 10 Although there are more recent papers, some of these have only focused on single sports rather than providing a broader overview of ocular injuries in sport. 11 , 12 , 13 , 14 Of the articles that have investigated multiple sports, some of these papers generated data from statistical coding databases as opposed to individually assessing case presentations thereby being unable to provide descriptive information regarding characteristics and impact of the injury. 3 , 15 Furthermore, not all studies assessed long‐term follow‐up of these injuries. 3 , 15 , 16 Therefore, there is a paucity of understanding of the nature and severity of specific ocular injuries, complications, treatments and follow‐up outcomes. This retrospective descriptive study sought to characterise the nature, mechanisms, severity, complications and visual outcomes associated with sports‐related eye injuries in a tertiary eye hospital across a 5‐year period.
Methods
Patients presenting to or referred with sports‐related ocular injuries to The Royal Victorian Eye and Ear Hospital (RVEEH) ED, East Melbourne, Victoria, Australia, were recruited based upon search terms identified from medical record coding (Appendix S1). The RVEEH is the largest tertiary eye care hospital in Australia with over 40 000 presentations to the ED annually. 17 To be consistent with the published literature, ocular trauma was defined as a ‘diagnosis of either blow‐out fracture of the orbit, open wounds of the ocular adnexa or eye, superficial injury or contusion to the eye and/or adnexa, foreign body either intraocular or external to the eye, or injury to the optic nerve or cranial nerves’ where the primary mechanism was in the context of sports‐related trauma. 3 Terminology used for analysis was based upon the Birmingham Eye Trauma Terminology classification. 18 The search was performed for a 5‐year period between 1 June 2015 and 31 May 2020. Inclusion criteria encompassed ocular injury related to sport and that this was the first presentation for that injury. Variables were extracted from patient records and included baseline as well as most recent follow‐up data.
The present study was approved by the Human Research Ethics Committee of the RVEEH (Approval number: 09/886H/14) and all patient information was de‐identified. The study was conducted in accordance with the International Conference on Harmonization Guidelines for Good Clinical Practice and tenets of the Declaration of Helsinki.
Data examined included patient demographics (age, sex), injury mechanism (sport, mechanism, bilateral or unilateral involvement), injury characteristics (visual acuity [VA], intraocular pressure [IOP], diagnosis), investigations (orbital imaging) and medical and surgical management performed. VA was recorded in both the affected and unaffected eye at initial presentation and the latest follow‐up appointment. Best corrected VA was measured either with glasses or pinhole. Both unaided and best corrected VA were documented where possible. The better of these two values was recorded as best documented VA.
Statistical analyses were conducted using Stata/IC 16.0 software (StataCorp, College Station, TX, USA). Descriptive statistics included measurements such as means with standard deviations (SD), frequencies, percentages and distributions plotted using bar graphs. Multivariate logistic regression was used to analyse the sports and activities which had an increased risk of leading to an ocular injury that warrants a visit to the ED. Australian rules football (AFL) was used as the base reference. Statistical significance threshold was P < 0.05.
Results
The search yielded 3287 presentations, of which 1494 were excluded as they did not meet inclusion criteria. Thus, 1793 cases were included for analysis. Of these, 878 (48.97%) cases were followed up at the RVEEH. Given that data from the latest follow‐up appointment was included, this meant follow‐up period differed for each case based on individual injury and severity. Median follow‐up period was 24 days (interquartile range 43 days). These 1793 patient presentations accounted for approximately 0.86% of all 208 000 patients presenting to the RVEEH ED during the study period. The majority of patients were male with 1442 (80.42%) cases.
Mean patient age was 28.67 ± 15.65 years (95% confidence interval 27.95–29.40). Age‐specific rates of injury are shown in Figure 1. More than half of the patients (59.56%) were below the age of 30, with the most common age groups being 20–29 (27.11%), 10–19 (26.99%) and 30–39 (19.19%), respectively. Above the age of 30, there was a downward trend in number of cases in each age group. Winter was the most common season for injuries with 516 (28.78%) cases followed by spring, autumn and summer with 473 (26.38%), 440 (24.54%) and 364 (20.30%) cases, respectively.
Figure 1.
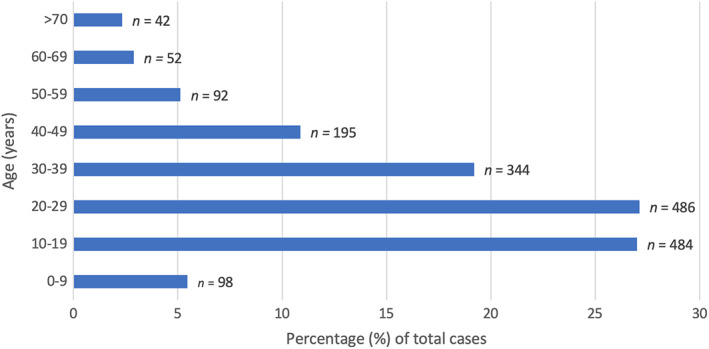
Rates of injury by age.
The majority of injuries were unilateral with 1779 (99.22%) cases and 14 (0.78%) cases with bilateral injury. Of the unilateral cases, the distribution between left and right eye was almost symmetrical at 857 (48.17%) cases and 922 (51.83%) cases, respectively.
Soccer was the leading sport to cause injuries with 327 (18.24%) cases, followed by AFL with 306 (17.07%), basketball with 215 (11.99%), tennis with 157 (8.76%) and cricket with 149 (8.31%) cases, respectively. All sports causing ocular injury are classified in Figure 2. A detailed breakdown of which sports is included in groups such as ‘water sports’ and ‘unspecified’ can be found in Appendix S1.
Figure 2.
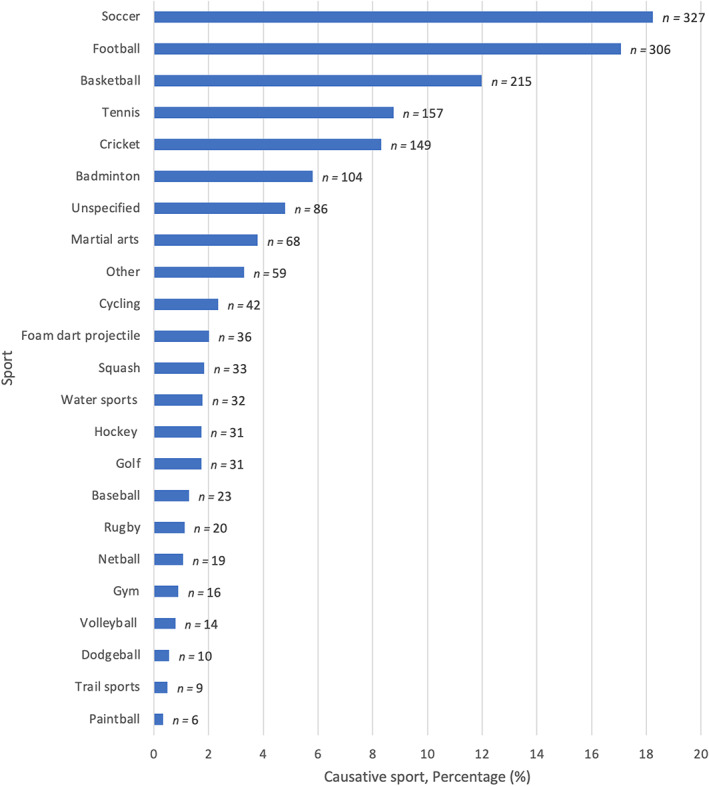
Classification of injuries by causative sport.
There were 548 paediatric patients (ages 0–18 years), contributing to 30.56% of the entire patient cohort. The leading sports to cause injury for paediatric patients were also soccer, AFL and basketball.
As shown in Table 1, the most common mechanism of injury was projectile with 976 (54.43%) cases, followed by incidental body contact with 506 (28.22%) cases and sporting equipment with 104 (5.80%) cases.
TABLE 1.
Classification of injuries by causative mechanism
| Mechanism of injury | Frequency | Percentage (%) of total cases |
|---|---|---|
| Projectile | 976 | 54.43 |
| Incidental body contact | 506 | 28.22 |
| Sporting equipment | 104 | 5.80 |
| Foreign body | 78 | 4.35 |
| Unspecified | 71 | 3.96 |
| Natural element | 33 | 1.84 |
| Fall | 14 | 0.78 |
| Other | 7 | 0.40 |
| Protective clothing | 4 | 0.22 |
| Total | 1793 | 100.00 |
In relation to VA, data for the 14 cases where injury occurred to both eyes were analysed separately. For a further 25 cases, data were not included as VA was unavailable, in most cases because the patient did not wait for completion of their vision assessment.
Best corrected VA in the affected eye at initial presentation was documented in only 793 (45.21%) cases. Of the remaining 961 (54.79%) cases, 899 (93.55%) had unaided VA greater than 20/40, which might explain why further efforts to document subjective best corrected VA in an emergency setting was not performed. Only 62 (6.45%) cases had VA less than 20/40 and no corrected VA recorded.
VA at latest follow‐up appointment was recorded in 836 (46.63%) cases. In total, 558 (67.88%) cases had only unaided VA without best corrected VA documented. Of these, 534 (95.70%) cases had a VA greater than or equal to 20/40, which might explain why the clinician did not also record best corrected vision. For the remainder of cases where VA at latest follow up was not recorded, 722 (40.27%) cases had no follow‐up appointment scheduled, either because this was deemed unnecessary or follow up was arranged at a different setting. A total of 193 (10.76%) patients did not attend the scheduled appointment and 42 (2.34%) cases had no recorded VA, mostly because the appointment was conducted via telehealth where VA assessment was not possible.
The injuries were categorised by their diagnosis based on anatomical region, as shown in Figure 3, which is similar to the Birmingham Eye Trauma Terminology (BETT) system. 18 Hyphaema and traumatic uveitis were grouped together as they are often concomitantly present in trauma. The most common pathology observed was hyphaema and traumatic uveitis with 725 cases, followed by commotio retinae with 519 cases, corneal injuries (including abrasion, erosion, laceration, dry eye, blepharitis and microbial keratitis) with 351 cases and conjunctival injuries (including laceration, conjunctivitis and subconjunctival haemorrhage) with 224 cases.
Figure 3.
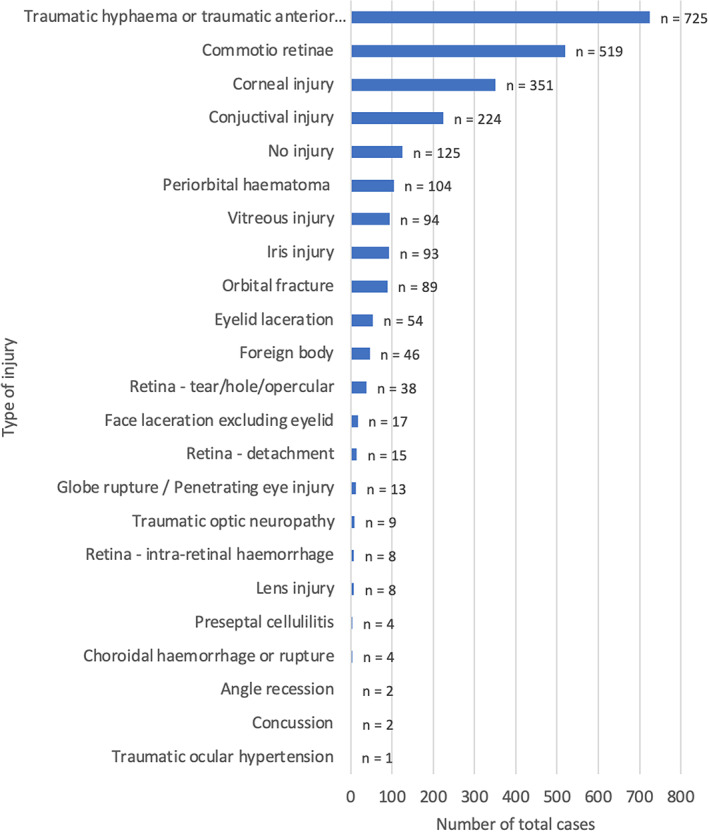
Classification of injuries by diagnosis.
The most common investigation was computed tomography orbits and facial bones with 184 (10.26%) cases followed by ophthalmic ultrasound (B scan) with 52 (2.90%) cases. The most common non‐surgical management was steroids with 693 (38.65%) cases and cycloplegics with 585 (32.63%) cases, respectively.
The mean IOP in the injured eye at presentation was 16.05 mmHg with an SD of 7.1 mmHg. One hundred and three (5.74%) cases required anti‐ocular hypertensive medications. The mean IOP for these cases at initial presentation was 33.47 mmHg and 16.70 mmHg at follow up. For these cases requiring anti‐ocular hypertensive medications, the most common causative sports were soccer, AFL and badminton with 35, 17 and 15 cases, respectively.
Of the presenting cases, 27 (1.51%) were recorded as being admitted from the ED to hospital and 26 (1.45%) cases required surgery. The most common sport contributing to surgical cases was AFL with five cases (19.23% of cases requiring surgery) followed by basketball, cricket, golf and hockey all with three cases (11.54% of cases requiring surgery) each. As can be seen in Table 2, the most common injury requiring surgery was globe rupture/penetration with 10 cases.
TABLE 2.
Type of injury requiring surgery
| Injury | Frequency | Percentage (%) of injuries requiring surgery |
|---|---|---|
| Globe rupture/penetration | 10 | 25.64 |
| Eyelid laceration | 6 | 15.38 |
| Traumatic hyphaemia | 4 | 10.26 |
| Retinal detachment | 4 | 10.26 |
| Facial (non‐eyelid) laceration | 4 | 10.26 |
| Commotio retinae | 3 | 7.70 |
| Conjunctival laceration | 2 | 5.13 |
| Orbital blow out fracture | 2 | 5.13 |
| Subconjunctival haemorrhage | 1 | 2.56 |
| Traumatic mydriasis | 1 | 2.56 |
| Ptosis | 1 | 2.56 |
| Neuro‐ophthalmology | 1 | 2.56 |
| Total | 39 | 100.00 |
The 10 sports associated with globe rupture included two cases of golf, two cases of football and one case each of badminton, hockey, crick, tennis, martial arts and an unspecified case.
Using AFL as the base reference, multivariate logistic regression showed that the greatest risks of globe rupture or penetration were associated with martial arts (odds ratio [OR] 16.22) and golf (OR 10.43); orbital blow‐out fracture with skiing (OR 14.42), hockey (OR 4.39) and cricket (OR 2.35); hyphaema with squash (OR 4.18), badminton (OR 3.87) and cricket (OR 2.39); and retinal tears with foam dart projectiles (OR 5.59). All associations were statistically significant (P < 0.05).
Discussion
Soccer, AFL and basketball were the leading sports to cause injuries, accounting for a total of 47.30% of all cases. It is important to keep in mind the relative popularity of these sports in the study's catchment area. For example, AFL is a popular sport in the state of Victoria, likely contributing to the higher number of cases. This is in keeping with a similar study performed by Fong at the RVEEH between 1989 and 1991 which also found that football was the most common sport contributing to ocular trauma. 8 It is interesting to note that the leading sports to cause ocular injury in our study did not necessarily align with sports considered high‐risk for eye trauma by Sports Medicine Australia. 19 For example, soccer and AFL were the most common sports to cause injuries in our study; however, they are only considered moderate risk for eye trauma by Sports Medicine Australia. Our study is the most comprehensive in Australia to date in this field, and its findings may inform updated guidelines and policy changes.
The most common mechanisms of injury for the top three sports were projectile and incidental body contact. The use of protective eyewear is not mandatory in any of these sports, likely contributing to the high number of presentations. In contrast, paintball, where the use of a face shield in Australia is mandatory, was the sport to cause the least number of injuries, contributing only 0.33% of cases. This is despite its classification as high risk by Sports Medicine Australia, highlighting the positive impact of protective eyewear in decreasing ocular injuries.
The data also provided an insight into eye injuries among a broad age demographic including paediatric patients. Mean patient age was 28.67 years and there was a downward trend in number of cases in each age group above the age of 30. Paediatric patients accounted for 30.56% of eye injuries in this study cohort. The study identified that paediatric age patients were more likely to have retinal tears. These were most associated with foam dart projectiles which are popular among younger age groups.
The mean age of 37.15 years for the cases requiring surgery further emphasises the implication of long‐term impact of serious injuries on the younger population, with the potential risk for long‐term vision‐related quality of life. Further research is required to explore the nature of this observation and may target interventions for particular high‐risk sports among children participating at school and community level sport. For example, Hoskin et al. explored the incidence of paediatric ocular trauma at a tertiary hospital in Western Australia, with both studies including soccer, AFL and tennis in their top four causative sports – perhaps highlighting a pattern of higher risk sports requiring targeted intervention. 20 Such information would be useful for healthcare providers and patients to improve awareness of high‐risk sports, and sequelae that can lead to long‐term ocular morbidity. This might also facilitate greater awareness and education among sporting organisations in considering preventative strategies to reduce the burden of ocular injury.
The main ocular injuries were traumatic hyphaema and traumatic anterior uveitis. This in keeping with Fong's study who reported that hyphaema was the most common injury occurring in 46% of all presentations. 8 Projectile was the most common causative mechanism contributing to 54.43% of injuries. The greatest risk of hyphaema was associated with squash (OR 4.18), badminton (OR 3.87) and cricket (OR 2.39), all of which involve a projectile. This finding is relevant given that these injuries can lead to ocular hypertension, and later, sequelae of chronic uveitis such as cataract, glaucoma and macular oedema. Although our study follow‐up period was not long enough to capture the longer term outcomes of the aforementioned complications, the potential development of these complications following an acute injury should not be ignored.
The greatest risk of globe rupture or penetration in the present study was associated with martial arts (OR 16.22) and golf (OR 10.43). Globe rupture or penetration is one of the most serious ophthalmic injuries, highlighted by the fact that of the 13 cases presenting with globe rupture, 10 required surgery. When planning targeted prevention strategies for specific sports, it is not only important to consider the relative frequency of injuries caused by a specific sport, but also the relative severity of injuries caused by that sport. For example, AFL was the sport to contribute one of the highest numbers of injuries, as well contributing the most surgical cases, therefore highlighting the potential substantial impact of introducing interventions such as mandatory protective eyewear in AFL.
The study observed that most patients required non‐surgical management. However, a large number of patients required anti‐ocular hypertensive, anti‐inflammatory and cycloplegic drops to treat the immediate consequences of blunt trauma. Among patients with acute ocular hypertension the mean IOP was 33.47 mmHg. This suggests although 85% of patients had excellent VA upon presentation, this does not necessarily exclude the potential for significant ocular injuries and the imperative upon timely review.
The study was also important in highlighting challenges improving awareness of sports‐related eye trauma. The frequency of the use of protective eyewear was not calculated in study participants as this information was not documented in the majority of cases. This is an important observation and warrants ongoing education of clinical staff with regards to careful documentation in eye trauma. It has been repeatedly demonstrated that appropriate protective eyewear can reduce the incidence of sports‐related ocular injury. The Helsinki University Eye Hospital, Helsinki, Finland, showed that hockey‐related eye injuries declined by 90.91% in the under‐14 age group as a direct consequence of the introduction of mandatory protective eyewear. 16 Dain published a recent review outlining sports eyewear protective standards, explaining that Australia has several sports eyewear protective standards – including for squash, tennis and cricket – but there is no general sports eyewear protective standard. 21 A further three standards for protective eyewear in specific sports are currently being reviewed for adoption in Australia. These focus on eye protection in three areas including skiing and snowboarding, racquetball and squash, and swimming. 22 An Australian standard for general sports eye protection was approved in 2014 by Standards Australia but has not yet been published. 19 It would be useful for a future study to investigate the impact of this standard on the incidence of sport related eye injuries to guide further standards and legislation.
The strength of the study is that data were obtained from the ED of the largest tertiary eye referral centre in Australia and New Zealand, the catchment population of which is approximately 5 million. Fong also explored sports‐related injury at the RVEEH; however, the present study assessed presentations between 1989 and 1991. Since this date, Hoskin et al. also published a study that focused on a paediatric population in Western Australia. It is important to acknowledge that our retrospective study does not encompass all patients with sports‐related eye trauma in Victoria during the study period. Although many patients with ocular injuries are referred from other hospitals to RVEEH, this is not always feasible. Furthermore, patients with more extensive life‐threatening injuries are typically more suited for management at other general metropolitan hospitals with medical infrastructure beyond that of a dedicated eye hospital. Second, follow‐up data were only included for patients with follow up at RVEEH. Therefore, the study did not include follow‐up data for patients who were examined in other local or private healthcare settings. Furthermore, as this was a retrospective study with study follow‐up period was based on latest follow‐up data available, for some cases which presented more recently, latest follow‐up appointment available was not reflective of the final follow‐up appointment for the patient.
Further research is required to expand on the present study and further explore the prevalence and impact of sports‐related ocular injuries. In particular, a subsequent study examining longitudinal follow‐up data would provide information on long‐term ophthalmic complications. Furthermore, a multi‐centre dataset would provide a more complete perspective of eye trauma presentations nation‐wide. Given the prevalence of sporting activities in younger age groups, a separate paediatric eye trauma study would also be valuable. Most importantly, the result of all further studies should be aimed at advocating for increased protective eyewear, especially at school and community level sports.
Conclusion
Ocular injuries and their sequelae can predispose patients to long‐term physical, psychosocial and health‐economic impacts. The present study captured the demographic, nature and extent of ocular injuries, treatment and short‐term follow up outcomes of sports‐related eye trauma. In addition, it offers insight into understanding the sports and mechanisms associated with severe eye injuries.
Sports‐related trauma disproportionately impacts younger individuals. The most common sports linked to ocular injury are popular sports that individuals participate in at recreational, amateur and professional levels. The most common mechanisms of injury are projectile and incidental physical contact. Although the majority of injuries result in blunt trauma with overall good visual outcomes, there are still a number of patients with blunt trauma that have intraocular sequelae, which require follow up and management.
The reduction of ocular injury requires a coordinated effort from the community including public health professionals, policy makers and role model athletes to encourage a safer sporting culture. Although elimination of hazards remains the most effective way to prevent injuries, for example prohibiting the use of hockey sticks above shoulder‐height, it is also important to educate children regarding hazard awareness and safe play, as well as encouraging the use of standardised protective eyewear. 20 Not only is further research required to identify areas for intervention, but health professionals treating sports‐related ocular injuries should also be encouraged to document whether there was use of protective eyewear so that we are able to examine the impact of the changes we make.
Supporting information
Appendix S1. Supporting information.
Acknowledgement
Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
Author contributions
Study conception and design: GA, JA, CC, RC. Data collection: GA. Analysis and interpretation of results: GA, JA. Draft manuscript preparation: GA, RC. All authors reviewed the results and approved the final version of the manuscript.
Competing interests
None declared.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
- 1. Kreisfeld R, Harrison J. Hospitalised sports injury in Australia, 2016–17. In: Injury Research and Statistics, Series no. 131. Canberra: Australian Institute of Health and Welfare, 2020. [Google Scholar]
- 2. Barr A, Baines PS, Desai P, MacEwen CJ. Ocular sports injuries: the current picture. Br. J. Sports Med. 2000; 34: 456–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Haring RS, Sheffield ID, Canner JK, Schneider EB. Epidemiology of sports‐related eye injuries in the United States. JAMA Ophthalmol. 2016; 134: 1382–90. [DOI] [PubMed] [Google Scholar]
- 4. Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998; 5: 143–69. [DOI] [PubMed] [Google Scholar]
- 5. Tovell A, McKenna K. Eye injuries in Australia, 2010–11 to 2014–15. In: Injury Research and Statistics Series no 194 Cat no INJCAT 114. Canberra: Australian Institute of Health and Welfare, 2018. [Google Scholar]
- 6. Zafar S, Canner JK, Mir T et al. Epidemiology of hyphema‐related emergency department visits in the United States between 2006 and 2015. Ophthalmic Epidemiol. 2019; 26: 208–15. [DOI] [PubMed] [Google Scholar]
- 7. Larrison WI, Hersh PS, Kunzweiler T, Shingleton BJ. Sports‐related ocular trauma. Ophthalmology 1990; 97: 1265–9. [DOI] [PubMed] [Google Scholar]
- 8. Fong LP. Sports‐related eye injuries. Med. J. Aust. 1994; 160: 743–50. [DOI] [PubMed] [Google Scholar]
- 9. MacEwen CJ. Sport associated eye injury: a casualty department survey. Br. J. Ophthalmol. 1987; 71: 701–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pardhan S, Shacklock P, Weatherill J. Sport‐related eye trauma: a survey of the presentation of eye injuries to a casualty clinic and the use of protective eye‐wear. Eye 1995; 9: 50–3. [PubMed] [Google Scholar]
- 11. Capão Filipe JA, Fernandes VL, Barros H, Falcão‐Reis F, Castro‐Correia J. Soccer‐related ocular injuries. Arch. Ophthalmol. 2003; 121: 687–94. [DOI] [PubMed] [Google Scholar]
- 12. Park SJ, Park KH, Heo JW, Woo SJ. Visual and anatomic outcomes of golf ball‐related ocular injuries. Eye 2014; 28: 312–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gardner EC. Head, face, and eye injuries in collegiate women's field hockey. Am. J. Sports Med. 2015; 43: 2027–34. [DOI] [PubMed] [Google Scholar]
- 14. Leivo T, Puusaari I, Mäkitie T. Sports‐related eye injuries: floorball endangers the eyes of young players. Scand. J. Med. Sci. Sports 2007; 17: 556–63. [DOI] [PubMed] [Google Scholar]
- 15. Matsa E, Shi J, Wheeler KK, McCarthy T, McGregor ML, Leonard JC. Trends in US emergency department visits for pediatric acute ocular injury. JAMA Ophthalmol. 2018; 136: 895–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhang J, Zhu X, Sun Z et al. Epidemiology of sports‐related eye injuries among athletes in Tianjin, China. Front. Med. 2021; 8: 690528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. The Royal Victorian Eye and Ear Hospital . Annual Report 2019–2020. Melbourne: The Royal Victorian Eye and Ear Hospital, 2020.
- 18. Kuhn F, Morris R, Witherspoon CD, Mester V. The Birmingham eye trauma terminology system (BETT). J. Fr. Ophtalmol. 2004; 27: 206–10. [DOI] [PubMed] [Google Scholar]
- 19. Sports‐Medicine‐Australia . Eye injuries, 2021. Available from URL: https://sma.org.au/resources-advice/injury-fact-sheets/eye-injuries/
- 20. Hoskin AK, Yardley A‐ME, Hanman K, Lam G, Mackey DA. Sports‐related eye and adnexal injuries in the Western Australian paediatric population. Acta Ophthalmol. 2016; 94: e407–10. [DOI] [PubMed] [Google Scholar]
- 21. Dain SJ. Sports eyewear protective standards. Clin. Exp. Optom. 2016; 99: 4–23. [DOI] [PubMed] [Google Scholar]
- 22. Standards: Standards Australia. 2021. Available from URL: https://www.standards.org.au/search?q=sport+eye+protection&mode=allwords&sort=relevance
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting information.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


