Abstract
Facial seborrheic dermatitis is a chronic skin condition that presents as erythematous scaly dermatitis and has a detrimental effect on the patient's quality of life. The purpose of this article is to present successful treatment of two male patients with face seborrheic dermatitis, one aged 50 and the other aged 56, who developed facial seborrheic dermatitis following facial erythema eruptions. We diagnosed it as face seborrheic dermatitis based on the patients' initial appearances and the location of the erythema during the episode. The previous doctor diagnosed the patients' facial symptoms as related to allergies or infections; therefore, they were treated with long-term anti-inflammatory (tacrolimus) and antiallergic medications (loratadine) throughout the disease's early stages. Erythema of the face was recurring and recalcitrant. Their facial skin lesions vanished after one week of Chinese herbal medicine treatment along with warming yang therapy. The application of the principle of warming the kidney yang to the treatment of face seborrheic dermatitis produced favorable results. This may be an advantageous adjunct to the treatment of recurrent seborrheic dermatitis of the face. High-performance liquid chromatography coupled with electrospray mass spectrometry (HPLC/ESI-MS) was used to determine the primary components of the Chinese herbal formula "adjusted Shen-Liu-Wei (ASLW)," which has six natural substances as its primary components. As a result, we believe that the Chinese herbal compound ASLW might be a viable alternative for symptom relief and successful treatment of face seborrheic dermatitis.
Keywords: Facial seborrheic dermatitis (FSD), Traditional Chinese medicine (TCM), Warming yang therapy, Case report
Facial seborrheic dermatitis (FSD); Traditional Chinese medicine (TCM); Warming yang therapy; Case report.
1. Introduction
Facial seborrheic dermatitis (FSD) is a chronic and recurrent inflammatory skin disorder occurring in sebaceous gland-rich areas of the face [1]. These are erythematous macules or plaques on the face with variable degrees of scaling and pruritus, and the skin is covered with scales and erythema that do not denote normal skin [2]. Numerous factors contribute to the development of seborrheic dermatitis. As far as we are aware, the cause of FSD is unknown. Malassezia yeast and nonspecific immune responses have been implicated in the development of this infection. Antifungal agents (e.g., ketoconazole) are frequently used in therapy to lower the amount of Malassezia yeast, while anti-inflammatory agents such as corticosteroids help alleviate inflammation. Due to the strong effect on specific individuals, antifungal medications such as topical ketoconazole are presently the basis of treatment for seborrheic dermatitis on the face. However, due to the possibility of adverse effects, these anti-inflammatory and antifungal medications should only be taken in the short term.
Traditional Chinese medicine (TCM) sees the human body as an organic organism comprised of several organs, each of which carries its own yin or yang character and functions in a mutually restrictive manner. The yin-yang theory is a TCM conceptual framework that developed from a philosophical notion. Generally, it is believed that the dynamic balance of yin and yang defines a body's condition of coordination and harmony. TCM uses the yin-yang principle to classify bodily structures, explain clinical symptoms, and guide illness therapy [3]. TCM considers that yang represents warmth and the promotion of beneficial functions, and functional activities of the body such as “qi” are classified as yang. However, cold and the material basis of vital functions belong to yin. Concepts such as “essence”, “blood”, and “body fluid” are classified as yin [4]. According to the basic characteristics of Traditional Chinese Medicine theory, some diseases arise from the relative decline of yin or yang of the five Zang-organs. Kidney yang deficiency is one of the classic syndrome patterns in TCM and is characterized by disorders in multiple metabolic pathways.
2. Case presentation
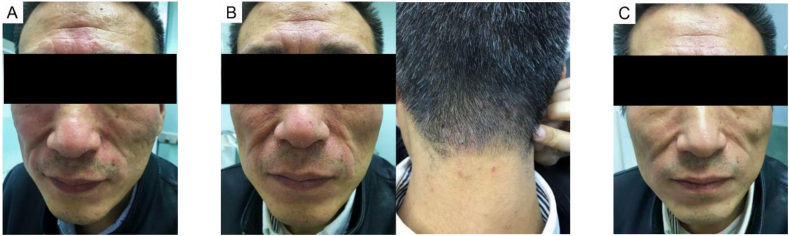
Case 1 is a 50-year-old man who appeared with recurring red spots on the face and rashes for five years. Around his nose and forehead, the patient exhibited noticeable oil discharge, which was found to be red, spotty, and coated with scales (Figure 1A). Since the patient attended another hospital when his early symptoms appeared and the doctors there considered that the facial symptoms were caused by allergy, the patient had previously been treated with antiallergic medications (loratadine, oral 10 mg/d). Subsequent laboratory tests were negative for allergy-related indicators, which was consistent with the finding that antiallergy therapy did not improve the patient's symptoms. However, with tacrolimus (applied evenly to the face twice a day) and other antifungal medications, the patient's erythema subsided. However, with previous treatments the patient still experienced frequent reoccurrence of symptomatic episodes. Meanwhile, we discovered that the patient suffered from additional bodily ailments in addition to face symptoms, including chills (particularly in the early morning), and that eating ice cream made him feel uneasy. The patient's tongue was crimson with white hairs and his pulse was feeble, indicating renal yang insufficiency. We administered the components in the traditional Chinese medicine (TCM) "Shen-Qi-Wan (SQW)" to warm the kidney yang based on the diagnosis. SQW is composed of ten different Chinese herbs (Table 1). The therapeutic result was not as predicted, as we observed several miliary red papules on his neck (Figure 1B), even though the facial erythema resolved after one week of therapy. We noted that the patient did not experience any loss of bodily fluid or feelings of dryness or heat after taking the hot-natured medications, which was uncommon. We believe that the prescription SQW was effective at warming the kidney yang and transmitting yang-qi to the body surface, but it was insufficiently potent to adjust the body's yin-yang balance, so we changed the Chinese herbal formulas to "adjusted Shen-Liu-Wei (ASLW)" (Table 2), which could further warm the yang and invigorate the yang-qi. Two days after taking the decoction "ASLW," the patient's facial erythema subsided and nearly vanished after one week of monotherapy with ASLW (Figure 1C).
Figure 1.
Changes in cutaneous symptoms during the first patient's therapy (A) Severe FSD lesions on the skin that did not improve despite tacrolimus treatment (B) After using SQW, red patches formed on the neck, but the facial symptoms improved (C) After taking another ASLW formula, the face erythema nearly vanished.
Table 1.
Ingredients of the Chinese herbal formula “Shen-Qi-Wan”.
| Traditional Chinese herb | Daily dose (g) |
|---|---|
| Shudihuang (Rehmanniae Radix Praeparata) | 10 |
| Shanyao (Dioscoreae Rhizoma) | 15 |
| Shanzhuyu (Corni Fructus) | 10 |
| Mudanpi (Moutan Cortex) | 15 |
| Fuling (Poria) | 15 |
| Zexie (Alismatis Rhizoma) | 10 |
| Rougui (Cinnamomi Cortex) | 3 |
| Guizhi (Cinnamomi Ramulus) | 10 |
| Shengma (Cimicifugae Rhizoma) | 10 |
| Dazao (Jujubae Fructus) | 10 |
Table 2.
Ingredients of the Chinese herbal formula “adjusted Shen-Liu-Wei”.
| Traditional Chinese herb | Daily dose (g) |
|---|---|
| Yinchaihu (Stellariea Radix) | 6 |
| Fangfeng (Saposhnikoviae Radix) | 10 |
| Wumei (Mume Fructus) | 10 |
| Wuweizi (Schisandrae Chinensis Fructus) | 10 |
| Gouqizi (Lycii Fructus) | 10 |
| Tusizi (Cuscutae Semen) | 10 |
| Buguzhi (Psoraleae Fructus) | 10 |
| Yinyanghuo (Epimedii Folium) | 10 |
| Rougui (Cinnamomi Cortex) | 6 |
| Shufupian (Aconiti Lateralis Radix Praeparata) | 10 |
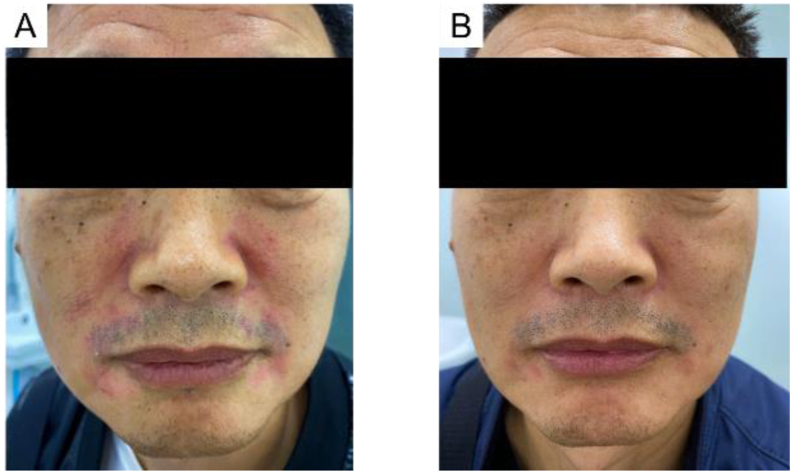
Case 2 is a 56-year-old male who had the same symptoms as Case 1 and was diagnosed with FSD. As in the last case, he had the same facial symptoms that were diagnosed to be caused by allergy in another hospital and treated with tacrolimus and antiallergic medications (loratadine, oral 10 mg/d). However, the treatment had little impact, and he had recurrent erythema. When he arrived at our hospital, the erythema around his nose and on his forehead persisted (Figure 2A). His symptoms were nearly identical to those described in the preceding example (case 1), confirming the diagnosis of FSD. As a result, we tended to treat with the warming yang prescription ASLW. After one week of therapy, the patient's erythema on the back was also greatly decreased (Figure 2B).
Figure 2.
Changes in cutaneous symptoms during the treatment of the second patient (A) Condition of the patient when he came to our department (B) After 1 week of ASLW medication, the patient's cutaneous symptoms were relieved.
When these two patients returned to our hospital for additional consultations after 1 week of herbal medicine, we found that they did not have any adverse reactions to ASLW. The patient in Case 1 had no relapse with regular medication, but the patient in Case 2 developed intermittent mild erythema on the face within 2 months of further consultation. This patient came to us for further consultation for 1 year. He visited us 3 times for intermittent facial symptoms, and each time he was relieved with the same herbal treatment. According to further follow-up with patients, patients' symptoms largely improved during the use of ASLW. Therefore, we considered that no further treatment or follow-up was needed.
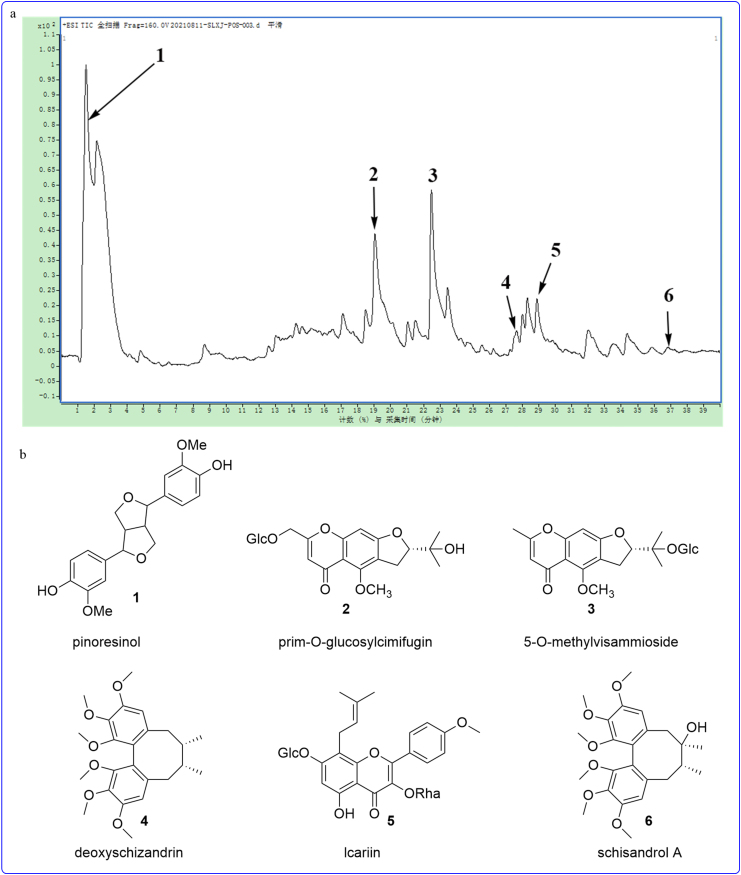
The aqueous extract of the Chinese herbal formula ASLW was analyzed by HPLC/ESI-MS in positive-ion mode (Figure 3A). Compounds 1–6 with retention times of 1.50 min, 19.11 min, 22.50 min, 27.62 min, 28.91 min, and 34.40 min were identified as pinoresinol (1), prim-O-glucosylcimifugin (2), 5-O-methylvisammioside (3), deoxyschizandrin (4), lcariin (5), and schisandrol A (6) on the basis of the observation of the pseudomolecular ion peaks at m/z 381.0795 [M + Na]+ (1), m/z 469.1714 [M + Na]+ (2), m/z 453.1772 [M + H]+ (3), m/z 439.1610 [M + Na]+ (4), m/z 677.2429 [M + H]+ (5), and m/z 433.2205 [M + H]+ (6), respectively, in HPLC/ESI-MS chromatograms, in accordance with the molecular weights of the six compounds (Figure 3B). In this case, six compounds were clearly identified by looking at the retention times and the MS data with the reference standards that were used in the study.
Figure 3.
(A) HPLC/ESI-MS chromatogram of the aqueous extract from “ASLW” in positive mode (B) Identification of chemical structures of six compounds in “ASLW”.
3. Discussion
FSD is characterized by erythematous macules, patches and plaques of varying degrees of scale on the face, which are accompanied by pruritus. In extreme cases, the skin lesion begins as a tiny region on the forehead or around the nose and rapidly develops and merges into dark red or yellow-red areas coated in oily scales or scabs. Certain beneficial compounds, such as piroctone olamine, stearyl glycyrrhetinate, dihydroavenanthramide, zinc pidolate, and acetamide MEA, may arrest or reverse FSD [5]. When erythema and scales emerge on a limited region of the face, topical antifungal and anti-inflammatory medications are the mainstays of therapy [6, 7]. However, continuous usage of some of them is prohibited due to the possibility of adverse effects such as skin thinning and striae. Traditional Chinese remedies have progressively extended to 183 countries and regions worldwide over the last decade as health goods and alternative medicines [8, 9]; technologies such as acupuncture and moxibustion have also increased in popularity in select countries. As a result, we feel that Chinese medicine provides several benefits in the treatment of some resistant disorders.
TCM is often used in the treatment of diseases based on pattern differentiation and emphasizes personalized diagnosis and treatment. Although there are many controlled clinical studies on the treatment of FSD with TCM, the therapies and medications are different. A meta-analysis evaluated the safety and effectiveness of tanshinone capsules combined with prednisone in the treatment of facial seborrheic dermatitis. In comparison to prednisone, tanshinone capsules combined with prednisone may be more effective in the treatment of facial seborrheic dermatitis [10]. Another meta-analysis indicated that the treatment of FSD with the comedication of Chinese and Western medicines was significantly more effective than single use of Western medicine in terms of symptom score, skin physiological parameters, recurrence rate and incidence of adverse effects [11]. Similarly, there are studies of Chinese herbal formulas (Chushi Xiaozhi Decoction, Qingre Chushi Decoction, Qingre Lishi Decoction) combined with Western medicine for the treatment of FSD, but the principle of treatment used in most of these formulas is clearing heat and dampness as the treatment [12, 13, 14], which is different from the principle of warming yang in ASLW and SQW, which also reflects that TCM emphasizes personalized diagnosis and treatment.
These two patients' symptoms did not improve despite a year of antiallergic, antifungal, and anti-inflammatory medicine therapy. As a result, they sought TCM therapy as a substitute. Within one week of therapy, the patient's facial problems had improved significantly, and other symptoms of pain had also improved. Unfortunately, we evaluated the effect by the patients' own description of itching and the observed extent of facial erythema instead of using the Erythema Index and Itch Severity Scale, which was somewhat less objective. In example 1, the patient was able to enjoy ice cream that he had previously avoided due to the relief of chills, which is considered an improvement of yang deficiency symptoms in TCM theory. Additionally, conventional therapies showed adverse consequences such as drug resistance and local dermatitis, but Chinese herbal remedies had minimal reported adverse effects. This is because herbals originating from natural resources have been treated to eliminate the majority of hazardous components, ensuring their safety. All of the prescriptions we write for patients are standard formulas that have been studied extensively in clinical studies.
Shen-Qi-Wan (SQW) is a traditional prescription found in the Jin Gui Yao Lue (Synopsis of the Golden Chamber's Prescriptions) that has the function of feeding and warming the kidney yang. SQW's effectiveness in tonifying renal yang has been demonstrated through millennia of therapeutic use in China. Adjusted Shen-Liu-Wei comprises two prescriptions: Guo-Min-Jian (GMJ) is a formula from the "A Collection by Zhu Chenyu" collection established by a well-known Chinese physician in modern times. It is frequently used to treat allergic asthma, allergic rhinitis, and urticaria. GMJ is a combination of four traditional Chinese medicines: Yinchaihu (Stellariea Radix), Fangfeng (Saposhnikoviae Radix), Wumei (Mume Fructus), and Wuweizi (Mume Fructus) (Schisandrae Chinensis Fructus). Shen-Liu-Wei (SLW) is derived from Li Ke's "A Collection of Emergency and Severe Cases" and is given by Li Ke, a well-known TCM physician. It is primarily utilized to warm and regenerate the kidney yang while also nourishing the renal yin. SLW is a combination of six traditional Chinese medicines: Gouqizi (Lycii Fructus), Tusizi (Cuscutae Semen), Buguzhi (Psoraleae Fructus), Yinyanghuo (Epimedii Folium), Rougui (Cinnamomi Cortex), and Shufupian (Cinnamomi Cortex) (Aconiti Lateralis Radix Praeparata). In two instances, we combined the GMJ and SLW formulas to create a new formula termed ASLW. Although the Chinese herbs present in ASLW did not appear to be poisonous, we employed HPLC/ESI-MS to perform a detailed study.
HPLC/ESI-MS showed six main compounds in ASLW: pinoresinol (1), prim-O-glucosylcimifugin (2), 5-O-methylvisammioside (3), deoxyschizandrin (4), lcariin (5), and schisandrol A (6). It has been reported in the literature that some of these compounds have anti-inflammatory activity. Compound (1) possesses fungicidal activities as an antifungal effect by causing damage to the fungal plasma membrane [15]. Compound (2) exerts anti-inflammatory effects by inhibiting the phosphorylation of JAK2/STAT3 [16], and compound (2) exhibits significant anti-inflammatory functions in mouse ear inflammation [17]. Compound (4) suppressed the cleavage of pro-caspase-1 and inhibited the activity of the NLRP3 inflammatory proteasome, thereby reducing the inflammatory response [18]. Compound (5) exerts diversified effects on lymphocyte balance, anti-inflammatory/inflammatory cytokines and NF-κB in the treatment of different diseases [19].
In summary, we used HPLC/ESI-MS to analyze the highly expressed compounds obtained after analyzing ASLW that have shown noticeable anti-inflammatory effects in many studies, but this analysis method may have certain deficiencies, being unable to thoroughly analyze all components, and may be expressed for compounds that are effective for FSD. Because the quantity is not the most critical factor, the effectiveness of the substances must be confirmed.
4. Conclusion
FSD is clinically difficult to treat with anti-allergic and anti-infla-mmatory Western medicines. The results of this study have demonstrated that warming yang therapy with the Chinese medicine prescription ALSW could be a safe and effective option for the treatment of FSD; it might be considered an alternative treatment for FSD. Further comprehensive studies are necessary to determine the therapeutic effects of FSD since this study only consists of two case reports.
Declarations
Author contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Funding statement
Yanjuan Duan was supported by Training Program of the Seventh People's Hospital, Shanghai University of Traditional Chinese Medicine [QMX2021-05], National Natural Science Foundation of China [82004366], Clinical Research Plan of SHDC [SHDC2020CR4041]. Jianyong Zhu was supported by Innovative Team Projects of Shanghai Municipal Commission of Health (No.2022CX011). Yi Wang was supported by Clinical Research Plan of SHDC (No. SHDC2020CR4041). Xiaoxiang Zhai was supported by The Clinical Chinese Medicine Plateau Discipline Construction Project of Shanghai Pudong New Area Health Committee (PDZY-2018-0604).
Data availability statement
Data included in article/supp. material/referenced in article.
Declaration of interest's statement
The authors declare no competing interests.
Additional information
No additional information is available for this paper.
Ethics statement
Informed written consent was obtained from the patient for publication of this case report with associated images.
References
- 1.Naldi L., Rebora A. Clinical practice. Seborrheic dermatitis. N. Engl. J. Med. 2009;360:387–396. doi: 10.1056/NEJMcp0806464. [DOI] [PubMed] [Google Scholar]
- 2.Tucker D., Masood S. StatPearls; Treasure Island (FL): 2021. Seborrheic Dermatitis. [PubMed] [Google Scholar]
- 3.O'Brien K.A., Xue C. A Comprehensive Guide To Chinese Medicine; 2016. The Theoretical Framework of Chinese Medicine. [Google Scholar]
- 4.Liu Z. Essentials of Chinese Medicine; 2009. Essentials of Chinese Medicine. [Google Scholar]
- 5.Borda L.J., Perper M., Keri J.E. Treatment of seborrheic dermatitis: a comprehensive review. J. Dermatol. Treat. 2019;30:158–169. doi: 10.1080/09546634.2018.1473554. [DOI] [PubMed] [Google Scholar]
- 6.Piquero-Casals J., La Rotta-Higuera E., Francisco Mir-Bonafé J., et al. Non-steroidal topical therapy for facial seborrheic dermatitis. J Drugs Dermatol. 2020;19:658–660. doi: 10.36849/JDD.2020.10.36849/JDD.2020.5121. [DOI] [PubMed] [Google Scholar]
- 7.Kim H.O., Yang Y.S., Ko H.C., et al. Maintenance therapy of facial seborrheic dermatitis with 0.1% tacrolimus ointment. Ann. Dermatol. 2015;27:523–530. doi: 10.5021/ad.2015.27.5.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang-hua W. Effect of integrated traditional on facial seborrhea dermatitis and its effect on skin barrier function:a-mate-analysis. Journal Of Diseases Monitor & Control. 2020;14:341–348. [Google Scholar]
- 9.Qi W., Jie Y., Qian C., et al. Meta-analysis of the efficacy and safety of traditional Chinese medicine in the treatment of seborrheic dermatitis of the head. China Medical Cosmetology. 2021;11:90–3+103. [Google Scholar]
- 10.Fu Q., Huang M., Tang L., et al. Tanshinone capsules combined with prednisone for facial seborrheic dermatitis: a systematic review and meta-analysis of randomized clinical trials. Front. Med. 2022;9 doi: 10.3389/fmed.2022.816419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang CJ. Effect of integrated traditional in facial seborrhea dermatitis and its effect on skin barrier function:A- meta-analysis.
- 12.Zeng G.S., Zhu K., Han J.D., et al. Clinical observation of recipe for clearing heat and removing dampness combined with butyl flufenamate ointment in treating Facial Seborrheic Dermatitis. Journal of Guangzhou University of Traditional Chinese Medicine. 2018:35. 5. [Google Scholar]
- 13.Mao Y. Clinical observation of using Chushi Xiaozhi Decoction combined with tacrolimus in the treatment of gastroin- testinal damp-heat type Seborrheic Dermatitis of face. Journal of Sichuan of Traditional Chinese Medicine. 2020:38. 4. [Google Scholar]
- 14.Lyu J.J., Chen ZhX., Xu J.N., et al. Evaluation on the clinical effect of Qingre Chushi decoction and piyan decoction on facial seborrheic dermatitis. Chinese Medicine Modern Distance Education of China. 2018;16:250. 18. [Google Scholar]
- 15.Hwang B., Lee J., Liu Q.H., et al. Antifungal effect of (+)-pinoresinol isolated from Sambucus williamsii. Molecules. 2010;15:3507–3516. doi: 10.3390/molecules15053507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou J., Sun Y.Y., Sun M.Y., et al. Prim-O-glucosylcimifugin attenuates lipopolysaccharideinduced inflammatory response in RAW 264.7 macrophages. Pharmacogn Mag. 2017;13:378–384. doi: 10.4103/pm.pm_323_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xue B.Y., Li W., Li L., et al. A pharmacodynamic research on chromone glucosides of fangfeng. Zhongguo Zhongyao Zazhi. 2000;25:297–299. [PubMed] [Google Scholar]
- 18.Cui H.R., Li P.Y., Li Y.M., et al. Inhibitory effect and mechanism of deoxyschizandrin on NLRP3 inflammasome. Yao Xue Xue Bao. 2017;52:80–85. [PubMed] [Google Scholar]
- 19.Shen R., Wang J.H. The effect of icariin on immunity and its potential application. Afr. J. Clin. Exp. Immunol. 2018;7:50–56. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supp. material/referenced in article.