Abstract
Background
The fracture of a Morse tapered abutment connection in an osseointegrated implant is one of the most serious mechanical complications, and it is extremely hard to deal with this complication in clinical practice.
Purpose
The aim of this study was to explore the cumulative mechanical complications focus on abutment of a platform switching Morse taper connection implant system after loading, and to perform a retrospective, approximately 1‐ to 9‐year follow‐up study to identify the predisposing factors.
Materials and Methods
A total of 495 patients with 945 fitted implants were enrolled in this study with a follow‐up from January 2012 to January 2020. The data of mechanical complications of the abutment, including abutment fracture (AF) and abutment screw loosening (ASL), and possible causative factors were extracted and evaluated statistically.
Results
A total of 25 out of 945 (2.65%) cumulative abutment mechanical complications occurred. AF was the most common complication (n = 13, 1.38%), followed by ASL (n = 12, 1.27%). For AF, gender, type of prosthesis, abutment design, and implant diameter were identified as the causative factors. AF was mostly observed in the single crown of males in molar areas, while ASL was more likely to occur on an angled abutment than on a non‐angled abutment. Moreover, the abutment with the positioning index (/X) had a higher incidence of fracture than the abutment without the positioning index (C/).
Conclusions
This study shows that the Morse taper connection is a safe abutment connection. AF occurs more frequently within single crowns in molar area of males, especially with the positioning index (/X), while ASL is more likely to occur in an angled abutment.
Keywords: dental abutment, dental implants, mechanical complication, Morse taper connection, positioning index
Summary box.
What is known
The implant‐abutment connection represents the weakest part of dental implant fixtures. A prosthetic index has been added to some Morse taper abutments. To date, there have been no retrospective clinical studies on the long‐term survival rate of this structure.
What this study adds
We showed that Morse taper connection is a safe abutment connection. Abutment fracture occurs more frequently within single crowns in molar area of males, while abutment screw loosing was more likely to occur in angled abutment. Moreover, abutment with positioning index had a higher incidence of fracture than without positioning index.
1. INTRODUCTION
An osseointegrated implant is considered the first choice for a loose tooth due to its high long‐term survival rates and predictable outcomes. 1 , 2 However, the implant‐abutment connection represents the weakest part of dental implant fixtures, and the biomechanical stability of the implant‐abutment connection is critical for the success of implant‐supported restorations. 3 The most frequent mechanical complications include implant fracture, abutment fracture (AF), abutment screw loosening (ASL), deformations at the different interfaces, and bacterial microleakage, and they are serious after long‐term function loading in clinical practice. 4 A systematic review reported an incidence of 5.3% for abutment or screw loosening during a 5‐year follow‐up period. 5 Studies have suggested that various causative factors, such as different abutment connections, bruxism, large occlusal force, superstructure design, implant position, diameter, age, gender, and crown‐implant ratio, might be associated with the incidence of abutment mechanical complications. 6 , 7
Different implant‐abutment connections, including external connection, internal parallel connection, and internal conical connection, have been developed to reduce the mechanical and biological complications. 4 , 8 Compared with external connections, internal connections have advantages, such as stability, better resistance of torque loss, and less screw loosening. 9 , 10 The internal conical abutments provide greater resistance to deformation and fracture under oblique compressive loading than internal hex abutments do. 11 Moreover, the conical Morse taper connection appears to be more efficient in abutment fit and seal performance, presents a high long‐term survival rate, is associated with less marginal bone resorption and a lower incidence of mechanical complications, significantly reduces the occurrence of implant fracture to nearly 0% or <1%, and the rate of screw loosening is only 1.3%. 3 , 4 , 12 , 13 , 14
Furthermore, a prosthetic index has been added to the abutment to guide the prosthetic components into the implants in some Morse taper implant systems. However, the influence of the prosthetic index inside Morse taper implants on fracture resistance compared with non‐indexed ones is still unclear. A previous study showed that in a 11.5‐degree angulation of the internal conical portion, the presence of a prosthetic index on Morse taper abutments did not decrease its resistance to fracture. 15 , 16 However, another study showed that indexed tapered abutments for single crown restorations might represent a greater biomechanical risk under function. 17 Moreover, reduction in the conical area of abutments with an internal hexagonal index may result in a biomechanical disadvantage for Morse taper connections. 18
The Ankylos implant (Dentsply Implants Manufacturing GmbH) offers a precisely machined platform switching for the Morse tapered abutment connection, 19 and a new Morse tapered abutment connection with an internal positioning index was fabricated in 2008. The internal geometry apical to the tapered portion was changed while leaving the dimensions of the conical internal connection unchanged. The abutment without the positioning index (C/) can be freely turned in the implant, whereas the positioning indexed abutment (/X) may facilitate the positioning of abutment and cannot rotate freely (Figure 1). This design gives the clinicians the option of working with either an indexed or non‐indexed abutment. 14 Both types of abutments can form a friction‐locked connection and the conical friction area of the two abutments is same.
FIGURE 1.
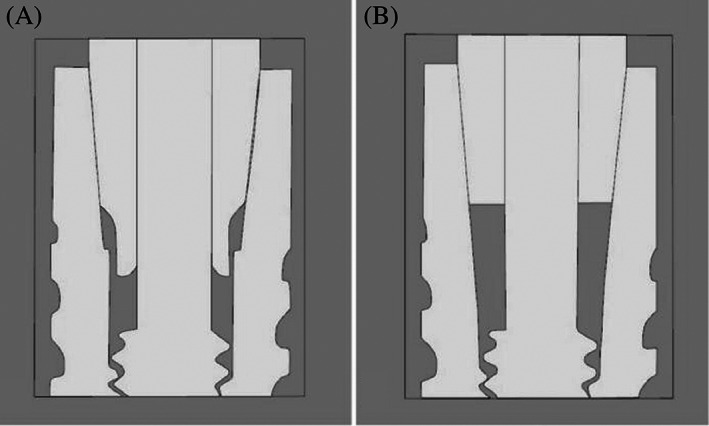
Schematic representation of the two types of abutments, A: with positioning index (/X) which is not freely rotatable; B: without positioning index (C/) which can be freely turned in the implant
To date, it is unclear whether this prosthetic index construction could decrease the mechanical strength of Morse taper connection and there are no clinical studies assessing whether there is any difference in the mechanical complication rate between the indexed and non‐indexed abutments. Therefore, the aim of this study was to evaluate the clinical outcome of this Morse taper implant‐abutment connection with or without the positioning index in the Ankylos implant system over a 1‐ to 9‐year follow‐up, and to identify the predisposing factors.
2. MATERIALS AND METHODS
This retrospective study was conducted in the dental department of Zhejiang Provincial People's Hospital and was approved by the Ethics Committee of Human Research at the hospital (no. 2021QT331). The study enrolled all patients treated with the Ankylos implant system between January 2012 and January 2020. The exclusion criteria included cases of non‐Ankylos implant restoration, non‐original abutments, implant failure due to preload loss, and cases loss during follow‐up. The implants were inserted by a single experienced dentist in accordance with the manufacturer's protocol. All implants were restored with a cemented implant‐supported single crown (ISC) or implant‐supported fixed partial denture (IFPD). Three types of abutments with a Morse taper were used for the prosthesis, including regular abutment, balanced posterior abutment, and Ti‐base abutment. The screws of the abutment were tightened according to the manufacturer's recommendations with a force of 15 N. X‐rays were taken immediately after fixation of the final restoration to ensure that there was a fit of the abutment and crown. All patients were asked to return for a routine annual follow‐up visit or any time if they experienced any discomfort or any other problem. All clinical problems were checked and recorded in an electronic medical recording system.
Data were collected from the electronic medical recording system, and dropouts occurred when the patients died or stopped coming for recall appointments. All implants were placed by a single experienced dentist and the prosthetic treatment was performed with the same person. The mechanical complications of the abutment were analyzed, including AF and ASL. Factors, including gender, age, arch, position, type of the prosthesis, cantilever, abutment design, abutment angulation, opposite jaw, implant length, diameter, bone graft, and functional loading time were analyzed to identify the causative factor.
The time between prosthesis placement and failure was defined as the survival time. If no failure occurred, the time from prosthesis placement to last visit was defined as the censored survival time. All data analyses were performed using SPSS statistical software (version 21.0; SPSS Inc.). Cox models were performed using the Stata software version 15 (StataCorp LLC). Notably, the analysis was performed at the implant level rather than at the patient level. Chi‐squared (χ 2 ) test, Fisher's precise test, Student's t‐test, and the Mann–Whitney U test were conducted to compare the variables between the two groups of categorical variables where appropriate. Univariate and multivariate Cox regression were used to analyze the influencing factors of the 9‐year cumulative fracture rate (CFR) and the associations between clinical covariates and AF. In addition, Kaplan–Meier analysis was used to estimate the cumulative survival rates (CSR) and CFR, and p < 0.05 was considered statistically significant.
3. RESULTS
A total of 582 patients with a total of 1086 implants were tracked, and 87 patients who received 141 dental implants were excluded due to the following reasons: dropped out during the follow‐up period, early osseointegration failure, late failure due to peri‐implantitis, and short follow‐up time (<12 months). Thus, 495 patients with 945 Ankylos implants were included in this study. Of these patients, 500 implants were obtained from 255 men and 445 implants from 240 women, with a mean age of 52.42 ± 14.09 years (range 18–85 years), and 40.21% subjects were ≤50 years, 59.79% subjects were >50 years at the time of implant placement. The mean duration of functional loading time was 48.86 ± 23.37 months (range 12–108 months). A total of 25 abutment mechanical complications were observed among the 945 Ankylos implants (2.65%). AF was the most common complication (n = 13, 1.38%), followed by ASL (n = 12, 1.27%).
Table 1 shows the results of the rate of abutment mechanical complications with possible relevant factors, including gender, age, arch, position, type of the prosthesis, cantilever, abutment design, abutment angulation, opposite jaw, implant length, diameter, bone graft, and duration of loading time. In cases with abutment mechanical complications, including AF and ASL, there was a significant difference between various clinical factors, including gender, position, and implant length and diameter (p < 0.05). Males (20/500, 4.00%) had a higher rate of mechanical complications than females (5/445, 1.12%). The molar position (20/541, 3.70%) had a higher complication rate than the premolar position (5/207, 2.42%) and anterior position (0/197, 0%). A short implant (8 mm, 7/99, 7.07%) had a significant higher risk than the other implants (9.5, 11, and 14 mm). The rate of complications with a large diameter (4.5 mm, 16/317, 5.05%) was significantly higher than that with a small diameter (3.5 mm, 9/628, 1.43%).
TABLE 1.
Baseline data and abutment mechanical complication rate (AF, ASL) of gender, age, arch, position, type of the prosthesis, abutment design, implant length or diameter, bone graft, type of the abutments, and duration time in Ankylos implants (n = 945)
| n (%) | Abutment mechanical complication | p value | ||||
|---|---|---|---|---|---|---|
| ASL | AF | N (%) | ||||
| Gender | Male | 500 (52.91) | 9 | 11 | 20 (4.00) | 0.006 a |
| Female | 445 (47.09) | 3 | 2 | 5 (1.12) | ||
| Age | ≤50 years | 380 (40.21) | 12 | 13 | 8 (2.11) | 0.396 a |
| >50 years | 565 (59.79) | 9 | 8 | 17 (3.00) | ||
| Arch | Maxillary | 477 (50.48) | 5 | 4 | 9 (1.89) | 0.142 a |
| Mandible | 468 (49.52) | 7 | 9 | 16 (3.42) | ||
| Position | Anterior | 197 (20.85) | 0 | 0 | 0 (0.00) | 0.021 a |
| Premolar | 207 (21.90) | 4 | 1 | 5 (2.42) | ||
| Molar | 541 (57.25) | 8 | 12 | 20 (3.70) | ||
| Type of the prosthesis | ISC | 475 (50.26) | 5 | 11 | 16 (3.37) | 0.164 a |
| IFDP | 470 (49.74) | 7 | 2 | 9 (1.91) | ||
| Cantilever | Yes | 19 (2.01) | 0 | 0 | 0 (0.00) | 1.000 b |
| No | 926 (97.99) | 12 | 13 | 25 (2.70) | ||
| Abutment design | Indexed (/X) | 441 (46.67) | 4 | 10 | 14 (3.17) | 0.343 a |
| Without index(C/) | 504 (53.33) | 8 | 3 | 11 (2.18) | ||
| Abutment angulation | Yes | 270 (28.57) | 8 | 2 | 10 (3.70) | 0.200 a |
| No | 675 (71.43) | 4 | 11 | 15 (2.22) | ||
| Opposing jaw | Natural tooth | 806 (85.29) | 11 | 13 | 24 (2.98) | 0.161 b |
| Implant tooth | 106 (11.22) | 0 | 0 | 0 (0.00) | ||
| Others | 33 (3.49) | 1 | 0 | 1 (3.03) | ||
| Length | 8 mm | 99 (10.48) | 3 | 4 | 7 (7.07) | 0.038 b |
| 9.5 mm | 232 (24.55) | 3 | 1 | 4 (1.72) | ||
| 11 mm | 555 (58.73) | 6 | 8 | 14 (2.52) | ||
| 14 mm | 59 (6.24) | 0 | 0 | 0 (0.00%) | ||
| Diameter | 3.5 mm | 628 (66.46) | 6 | 3 | 9 (1.43) | 0.001 a |
| 4.5 mm | 317 (33.54) | 6 | 10 | 16 (5.05) | ||
| Bone graft | Yes | 304 (32.17) | 3 | 1 | 4 (1.32) | 0.079 a |
| No | 641 (67.83) | 9 | 12 | 21 (3.28) | ||
| Duration time | 1–2 years | 185 (19.58) | 4 | 1 | 5 (2.70) | |
| 2–3 years | 154 (16.30) | 4 | 3 | 7 (4.55) | 0.276 | |
| 3–4 years | 161 (17.04) | 2 | 6 | 8 (4.97) | ||
| 4–5 years | 124 (13.12) | 0 | 2 | 2 (1.61) | ||
| >5 years | 321 (33.97) | 2 | 1 | 3 (0.93) | ||
Chi‐square test.
Fisher's precise test.
Then we carried out further analysis on AF and ASL. The results are shown in Table 2. Males (11/500, 2.20%) had a significant higher rate of AF than females (2/445, 0.45%) with a 9‐year abutment CFR of 4.0%, while only 0.5% of females developed this condition. The molar position (12/541, 2.20%) had a higher AF rate than the premolar position (1/207, 0.48%) and anterior position (0/197, 0%). The ISC (11/475, 2.32%) had a significantly higher failure AF rate than the IFPD (2/470, 0.43%), and the 9‐year CFR of the abutment in ISC was 4.7% while it was only 0.7% in IFPD. AF occurred in 10 (2.27%) out of the 441 abutments with the positioning index (/X), and it occurred in only 3 (0.60%) out of the 504 implants without the index (C/). The 9‐year CFR of the indexed abutment was 5.4%, while it was only 1.0% in the non‐indexed abutment. The 3.5‐mm diameter implant (3/628, 0.48%) had a significantly lower AF rate than the 4.5‐mm diameter implant (10/317, 3.15%); and the 9‐year CFR of the abutment with the 3.5‐mm diameter was 1.0%, while it was 4.8% for the abutment with 4.5‐mm diameter. In addition, the angled abutment (8/270, 2.96%) had a significant higher ASL rate than the non‐angled abutment (4/675, 0.59%), while there was no significant difference in the AF rate between the angled and non‐angled abutments. The median time of ASL occurrence was 34.67 ± 19.80 months after functional loading. No difference was found with respect to age, arch, cantilever, opposite jaw, implant length, and bone graft between AF and ASL.
TABLE 2.
Abutment mechanical complication rate (AF and ASL) of gender, age, arch, position, type of the prosthesis, cantilever, abutment design, implant length or diameter, bone graft, type of the abutments, and duration time in Ankylos implants (n = 945)
| Factor | Abutment screw loosening (%) | p value | Abutment fracture (%) | p value | |||
|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | 9 year CFR | |||
| Gender | |||||||
| Male | 491 (98.20) | 9 (1.80) | 0.123 a | 489 (97.80) | 11 (2.20) | 4.0 | 0.021 a |
| Female | 442 (99.33) | 3 (0.67) | 443 (99.55) | 2 (0.45) | 0.5 | ||
| Age: mean ± SD (years) | 52.41 ± 14.07 | 53.58 ± 17.26 | 0.447 b | 52.41 ± 14.16 | 53.69 ± 9.06 | 0.744 b | |
| Arch | |||||||
| Maxillary | 472 (98.95) | 5 (1.05) | 0.539 a | 473 (99.16) | 4 (0.84) | 1.3 | 0.152 a |
| Mandible | 461 (98.50) | 7 (1.50) | 459 (98.08) | 9 (1.92) | 3.7 | ||
| Position | |||||||
| Anterior | 197 (100) | 0 (0) | 0.147 c | 197 (100) | 0 (0) | 0 | 0.039 c |
| Premolar | 203 (98.07) | 4 (1.93) | 206 (99.52) | 1 (0.48) | 0.9 | ||
| Molar | 533 (98.52) | 8 (1.48) | 529 (97.78) | 12 (2.22) | 3.7 | ||
| Type of the prosthesis | |||||||
| ISC | 470 (98.95) | 5 (1.05) | 0.549 a | 464 (97.68) | 11 (2.32) | 4.7 | 0.013 a |
| IFPD | 463 (98.51) | 7 (1.49) | 468 (99.57) | 2 (0.43) | 0.7 | ||
| Cantilever | |||||||
| Yes | 19 (100) | 0 (0) | 19 (100) | 0 (0) | 0 | 1.000 c | |
| No | 914 (98.70) | 12 (1.30) | 1.000 c | 913 (98.60) | 13 (1.40) | 2.6 | |
| Abutment design | |||||||
| Indexed (/X) | 437 (99.01) | 4 (0.91) | 431 (97.73) | 10 (2.27) | 5.4 | 0.027 a | |
| Without index(C/) | 496 (98.41) | 8 (1.59) | 0.351 a | 501 (99.40) | 3 (0.60) | 1.0 | |
| Abutment angulation | |||||||
| Yes | 262 (97.04) | 8 (2.96) | 268 (99.26) | 2 (0.74) | 1.0 | 0.369 a | |
| No | 671 (99.41) | 4 (0.59) | 0.007 c | 664 (98.37) | 11 (1.63) | 2.7 | |
| Opposing jaw | |||||||
| Natural tooth | 795 (98.64) | 11 (1.36) | 0.269 c | 793 (98.39) | 13 (1.61) | 3.0 | 0.612 c |
| Implant tooth | 106 (100) | 0 (0) | 106 (100) | 0 (0) | 0.0 | ||
| Other conditions | 32 (96.97) | 1 (3.03) | 33 (100) | 0 (0) | 0.0 | ||
| Length | |||||||
| 8 mm | 96 (96.97) | 3 (3.03) | 0.346 c | 95 (95.96) | 4 (4.04) | 8.8 | 0.087 c |
| 9.5 mm | 229 (98.71) | 3 (1.29) | 231 (99.57) | 1 (0.43) | 0.5 | ||
| 11 mm | 549 (98.92) | 6 (1.08) | 547 (98.56) | 8 (1.44) | 2.8 | ||
| 14 mm | 59 (100) | 0 (0) | 59 (100) | 0 (0) | 0.0 | ||
| Diameter | |||||||
| 3.5 mm | 622 (99.04) | 6 (0.96) | 0.232 c | 625 (99.52) | 3 (0.48) | 1.0 | 0.002 a |
| 4.5 mm | 311 (98.11) | 6 (1.89) | 307 (96.85) | 10 (3.15) | 4.8 | ||
| Bone graft | |||||||
| Yes | 301 (99.01) | 3 (0.99) | 303 (99.67) | 1 (0.33) | 0.7 | ||
| No | 632 (98.60) | 9 (1.40) | 0.761 c | 629 (98.13) | 12 (1.87) | 3.2 | 0.072 c |
| Duration time: mean ± SD (months) | 49.04 ± 23.37 | 34.67 ± 19.80 | 0.028 d | 48.96 ± 23.47 | 41.85 ± 12.73 | 0.276 b | |
Chi‐square test.
Student's t‐test.
Fisher's precise test.
Mann–Whitney U test.
A comparison according to different factors of the 9‐year cumulative abutment fracture rate and the associations between clinical covariates were evaluated by the univariate Cox regression models, and the results are shown in Table 3. The variables with p < 0.20 in the univariate analysis, including gender, position, type of prosthesis, abutment design, implant length, implant diameter, and bone graft or not, were further considered as the independent variables for final multivariate Cox regression models. The multivariate regression results showed that gender, type of prosthesis, abutment design, and implant diameter were incorporated into the model. Gender, abutment design, type of prosthesis, and implant diameter were the factors that continued to present a statistically significant HR in the multivariate Cox regression model (Table 4). Considering the abutment without the positioning index as the reference group, the 9‐year CFR of the abutment with the index was 4.89 times that of the abutment without the index. In addition, the 9‐year CFR of males was 5.41 times higher than that of females. With ISC as the reference group, the 9‐year cumulative fracture rate of ISC was 4.42 times higher than that of IFPD. In contrast, the CFR of the 3.5‐mm diameter implant was 0.21 times of that of the 4.5‐mm diameter implant.
TABLE 3.
Comparison of cumulative abutment fracture rate according to different factors, and hazard ratio estimated from univariate Cox proportional hazard models at 9 years
| Factors | Univariate | |
|---|---|---|
| HR (95% CI) | p‐value | |
| Gender | ||
| Male | 1 | 0.047* |
| Female | 0.217 (0.048 ~ 0981) | |
| Age | ||
| Step by one | 1.007 (0.968 1.048) | 0.724 |
| Arch | ||
| Maxillary | 1 | 0.211 |
| Mandible | 2.120 (0.653 ~ 6.886) | |
| Position | ||
| Anterior | <0.001 (<0.001 ~ 107300) | 0.967 |
| Premolar | 0.251 (0.033 ~ 1.932) | 0.184 |
| Molar | 1 | |
| Type of prosthesis | ||
| ISC | 1 | 0.016* |
| IFPD | 0.156 (0.035 ~ 0.705) | |
| Cantilever | ||
| Yes | 0.048 (<0.001 ~ 292 939.886) | |
| No | 1 | 0.703 |
| Abutment design | ||
| Indexed (/X) | 5.855 (1.566 ~ 21.893) | 0.009* |
| Without indexed (C/) | 1 | |
| Abutment angulation | ||
| Yes | 0.863 (0.189 ~ 3.938) | 0.849 |
| No | 1 | |
| Opposing jaw | ||
| Natural tooth | 26.347 (<0.001 ~ 44 68 485.545) | 0.594 |
| Implant crown | 1.000 (<0.001 ~ 14 70 558.607) | 1.000 |
| Others | 1 | |
| Length | ||
| 8 mm | 1 | |
| 9.5 mm | 0.075 (0.008 ~ 0.679) | 0.021 |
| 11 mm | 0.264 (0.079 0.885) | 0.031 |
| 14 mm | <0.001 (<0.001 ~ −) | 0.980 |
| Diameter | ||
| 3.5 mm | 0.196 (0.054 ~ 0.714) | 0.013* |
| 4.5 mm | 1 | |
| Bone graft | ||
| Yes | 0.218 (0.028 ~ 1.676) | 0.143 |
| No | 1 | |
Abbreviations: CI, confidence interval; HR, hazard ratio.
p < 0.05.
TABLE 4.
Comparison of cumulative abutment fracture rate according to different factors, and hazard ratio estimated from Multivariate Cox proportional hazard models at 9 years
| Factors | HR (95% CI) | p‐vaule |
|---|---|---|
| Gender | ||
| Male | 1 | 0.029* |
| Female | 0.185 (0.041 ~ 0.838) | |
| Type of the prosthesis | ||
| ISC | 1 | 0.049* |
| IFPD | 0.226 (0.048 ~ 1.074) | |
| Abutment design | ||
| Without index(C/) | 1 | 0.023* |
| Indexed (/X) | 4.887 (1.240 ~ 19.268) | |
| Diameter | ||
| 3.5 mm | 0.208 (0.057–0.758) | 0.017* |
| 4.5 mm | 1 | |
Note: Only the factors that were considered statistically significant (p < 0.05) in the univariate model and did not present multicollinearity were included in the multivariate model.
Abbreviations: CI, confidence interval; HR, hazard ratio.
p < 0.05.
Furthermore, the cumulative abutment survival rates of the abutment to different factors, including gender, type of prosthesis, abutment design, and implant diameter, were analyzed. The result showed that the CSRs for male patients (96.0%, 9 years) were significantly lower than those for female patients (99.5%, 9 years) (Figure 2). The CSRs for ISC (95.3%, 9 years) were significantly lower than those for IFDP (99.3%, 9 years) (Figure 3). The CSRs for the 4.5‐mm implant (95.2%, 9 years) were significantly lower than those for the 3.5‐mm implant (99.0%, 9 years) (Figure 4). The CSRs for the indexed abutment (94.6%, 9 years) were significantly lower than those for the abutment without the index (99.0%, 9 years) (Figure 5).
FIGURE 2.
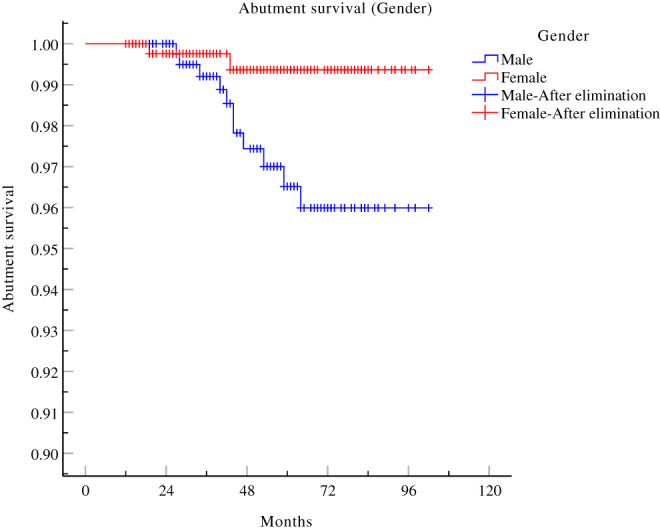
Kaplan–Meier abutment cumulative survival curve of different gender
FIGURE 3.
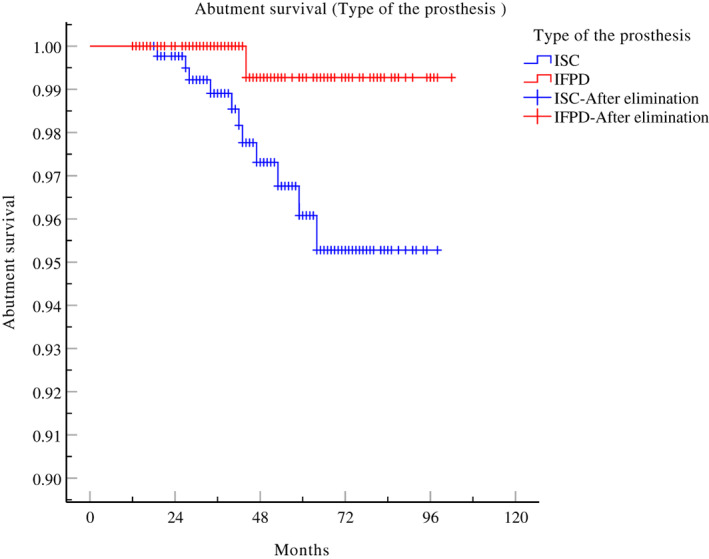
Kaplan–Meier abutment cumulative survival curve concerning type of the prosthesis
FIGURE 4.
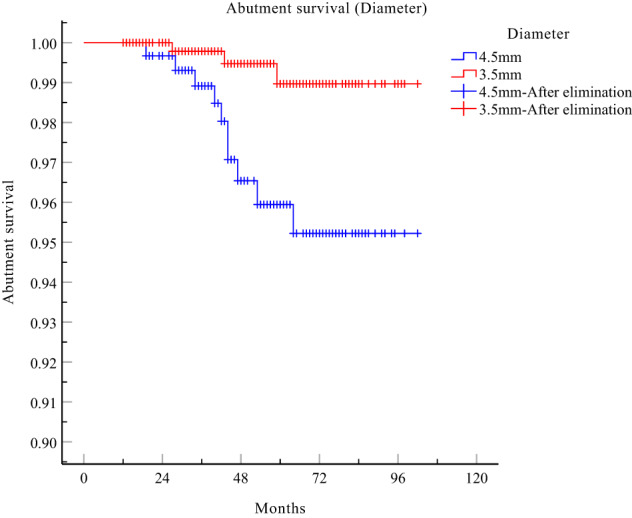
Kaplan–Meier abutment cumulative survival curve concerning implant diameter
FIGURE 5.
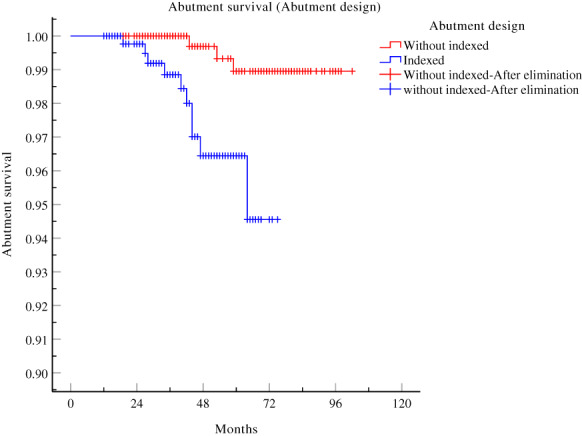
Kaplan–Meier abutment cumulative survival curve concerning abutment design (indexed or non‐indexed)
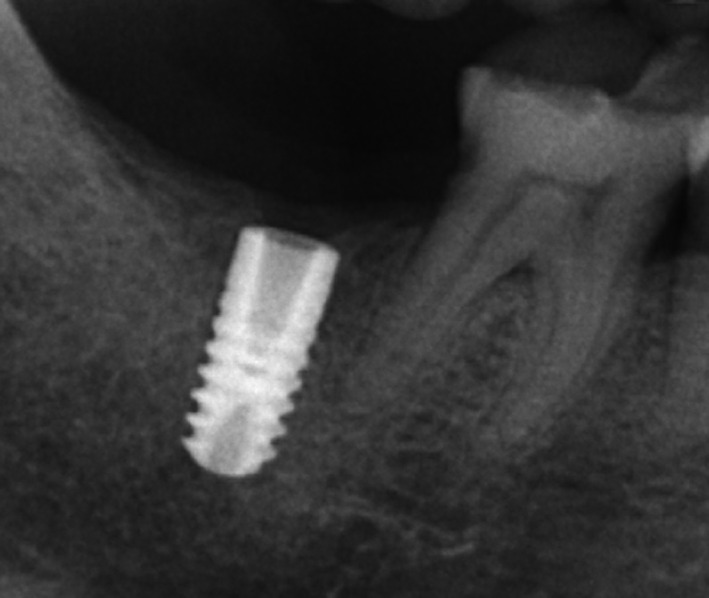
Moreover, 10 out of the 13 fractured abutments exhibited AF at the neck of the abutment with fracture of the central screw at the same time (Figures 6 and 7), 2 had fractures only at the neck of the abutment with a complete central screw, and 1 exhibited fracture at the end of the central screw (Figures 8 and 9). Notably, the opposing jaw in all of them was a natural tooth. Moreover, 11 out of the 13 abutment fractures occurred in the molar area with single crown restoration. Table 5 shows detailed information about the 13 AF cases.
FIGURE 6.

X‐ray of fracture both at the neck of abutment and at the screw
FIGURE 7.

View of fracture both at the neck of abutment and at the screw
FIGURE 8.
X‐ray of fracture at the end of the central screw
FIGURE 9.

View of fracture only at the end of the central screw
TABLE 5.
Detailed information about the 13 AF cases
| Gender | Age | Site | Type of the prosthesis | Length | Diameter | Abutment angulation | Type of the abutments | Periods (months) | Abutment fracture site | Re‐restoration | Opposing jaw | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 39 | 36 | ISC | 11 mm | 4.5 mm | No | Balance abutment C/ | 53 | Abutment neck with screw | Yes | Natural tooth |
| 2 | Female | 50 | 36 | ISC | 9.5 mm | 4.5 mm | Yes | Regular abutment /X | 19 | Abutment neck | Yes | Natural tooth |
| 3 | Male | 54 | 36 | ISC | 11 mm | 4.5 mm | No | Regular abutment /X | 40 | Abutment neck with screw | Yes | Natural tooth |
| 4 | Male | 44 | 37 | ISC | 8 mm | 4.5 mm | No | Regular abutment /X | 34 | Abutment neck with screw | Yes | Natural tooth |
| 5 | Male | 44 | 26 | ISC | 11 mm | 4.5 mm | No | Regular abutment/X | 28 | Abutment neck | Yes | Natural tooth |
| 6 | Male | 67 | 26 | ISC | 8 mm | 4.5 mm | No | Regular abutment/X | 42 | Abutment neck with screw | Yes | Natural tooth |
| 7 | Male | 60 | 46 | ISC | 11 mm | 3.5 mm | No | Balance abutment C/ | 59 | Abutment neck with screw | Yes | Natural tooth |
| 8 | Male | 61 | 37 | ISC | 11 mm | 4.5 mm | No | Regular abutment /X | 47 | Abutment neck with screw | Yes | natural tooth |
| 9 | Male | 42 | 26 | ISC | 11 mm | 3.5 mm | Yes | Regular abutment/X | 27 | Abutment neck with screw | No | Natural tooth |
| 10 | Male | 54 | 46 | ISC | 11 mm | 4.5 mm | No | Regular abutment/X | 64 | Abutment screw desoldering | Yes | Natural tooth |
| 11 | Female | 61 | 46 | ISC | 11 mm | 3.5 mm | No | Balance abutment C/ | 43 | Abutment neck with screw | Yes | Natural tooth |
| 12 | Male | 61 | 36 | IFPD | 8 mm | 4.5 mm | No | Regular abutment/X | 44 | Abutment neck with screw | No | Natural tooth |
| 13 | Male | 61 | 37 | IFPD | 8 mm | 4.5 mm | No | Regular abutment/X | 44 | Abutment neck with screw | No | Natural tooth |
4. DISCUSSION
This retrospective clinical study explored the cumulative abutment mechanical complications of the Morse taper connection implant system and its causative factors, and it is the first to identify the relationship between abutment design and mechanical complications in detail which has not been reported so far. A total of 25 (2.65%, n = 945) abutment mechanical complications were recorded, including 13 cases of AF and 12 cases of ASL. The abutment fracture rate was 1.38%, which was similar to that in a previous study (mainly focused on gonial angle and splinting status of the superstructure without distinction of abutment classification) involving 1126 Ankylos implants in 430 patients with a fracture rate of 1.6% after follow‐up for approximately 10 years, 6 and significant lower than some other non‐Morse tapered connection implant systems as previous reported. 5 , 20 Moreover, the abutment with positioning index had a significant higher incidence of fracture (10/441, 2.27%) than without positioning index (3/504, 0.60%). The predisposing factors associated with AF including gender, type of prosthesis, abutment design, and implant diameter.
Three designs of abutments were used in this study, including regular abutments, balanced posterior teeth, and titanium base abutments. Notably, the implants had the central screw and the abutment two relatively independent parts. The central screw could not be pulled out of the abutment because the thread of the central screw underwent laser welding to the end of the central rod after inserting the central rod into the abutment in accordance with the manufacturer's instructions. Only one case (0.11%) presented a thread desoldered from the central screw. Assessment of possible deformations at different interfaces after repeated application of tightening torque using a scanning electron microscope (SEM) showed that damage was observed in the threads of the abutment screws before and after loading in the internal and external connections. 4 Tsuge et al. 21 observed damage on the threads of the abutment screws and the screw surfaces on the upper and lower flanks, which was probably due to screw tightening. According to our results, the non‐integral structure and the laser‐welded screw slot structure is safe and does not fall off easily from the rod of the abutment screw.
AF is a very frustrating problem especially in Morse tapered abutment and it is difficult to deal with, approximately 40% of abutment fractures resulted in implant failures due to the failed extraction of broken fragments. 22 To the best of our knowledge, this is the first clinical study to explore the mechanical complications of the Ankylos abutment with or without the positioning index. Among the 13 AF cases, 10 (10/441, 2.27%) were indexed whereas 3 (3/504, 0.60%) were non‐indexed, and the difference was statistically significant. Adding a positioning index structure could provide an anti‐rotational function but could compromise the anti‐bending strength of the abutment within the ITI implant system, and the internal hexagonal index may influence the mechanical stability of the implant‐abutment assembly because it reduces the area of conical contact and may thus diminish friction between the components, which may be attributed to the stress concentration on the index. 23 A previous in vitro study investigated the effect of a positioning index on the abutment screw preload values of tapered connection implants, and the result suggested that indexed tapered abutments for single‐crown restorations might represent a greater biomechanical risk under function. 17 Moreover, presence of the internal hexagonal index of the Morse tapered abutment might significantly reduce the force necessary to dislodge the abutment from the implant. 18 A previous experimental study assessed the reverse torque of an indexed and non‐indexed Morse taper abutment in a mechanical fatigue test, the result showed the indexed abutment presented a greater loosening of the retaining screw and failed to show good outcomes related to the cold‐welding effect. 24 Importantly, our results are consistent with the conclusions reported in the above‐mentioned studies. From a clinical viewpoint, loading conditions should be taken into consideration when choosing abutments and this conclusion can provide engineers with new ideas to improve the existing designs during the manufacturing process.
While the loosening of the abutment screw is one of the most common complications in implant‐supported restorations, the factors associated with ASL were also analyzed. As reported previously, the internal connection and abutments with anti‐rotational and conical designs have better resistance to screw loosening. 25 The ASL rate is significantly lower than that of the external hexagon connection between 6% and 48%, as reported in the literature. 20 In our presented study, the total ASL rate was 1.27% and a significant difference in ASL occurrence was found between the angled abutment with 8 of 504 abutments (2.96%) and that of the non‐angled abutment with only 4 out of 675 abutments (0.59%). This result is consistent with a recent in vitro research, which measured the screw loosening values of prosthetic abutments with internal conical connections (indexed and non‐indexed) with different angles under mechanical cycling. A decrease in detorque values in the indexed abutments related to their inclination was found under mechanical cycling; the prosthetic abutments with 30 degrees of angulation had the lowest values, whereas no decrease was found in the non‐indexed abutments. 26 ASL increases with increasing abutment angulations and collar lengths after dynamic cyclic loading. 27 However, in some clinical cases, it is difficult to perceive loosening of the abutment screw due to the adequately strong friction between the abutment and internal wall of the implant, which is well known due to the internal conical Morse tapered connection of the Ankylos implant. Specifically, locking the wall of the abutment and the implant by mechanical friction results in formation of a “cold welding” effect between the lateral wall of the implant and the abutment by the Morse taper connection based on high contact pressure, which eliminates any strain on the central abutment screw. 28 As a result, the crown will not fall off even if the abutment screw is loosened, and thus the abutment often remains stably fixed even with a loosened screw. 6 This may be one of the reasons why ASL is rare after the use of this system. In addition, there was no significant difference in ASL between the indexed and non‐indexed abutments. So far, there is still limited consensus on the factors due to ASL in implants and more studies are needed to derive clear conclusions regarding the methodologies to abolish screw loosening. 29
Herein, the results suggested that the type of prosthesis is an important factor for AFs. This result is consistent with the findings reported in a previous study, which evaluated the long‐term cumulative mechanical complications with a focus on the abutment neck fractures of the Ankylos implant for single‐tooth restorations in Koreans. They observed a 2.2% (10/450) rate of AFs, and found that middle‐aged patients, the molar position, and a large implant diameter were associated with a high incidence of AF. 22 Results obtained in this study indicated that patients with a single crown had a significantly higher rate of AF complications (11/475, 2.32%) than patients with IFPD (2/470, 0.43%), and all prosthetic AFs occurred on single crown restorations in the molar area. With respect to the abutment mechanical complications of IFPD, a previous retrospective study with a 1‐ to 12‐year follow‐up showed a 0.3% fracture rate of the occlusal screw, but it did not describe the rate of AF. 30 In another 9‐year follow‐up retrospective clinical evaluation of 2‐ to 6‐unit IFPD, the deformation and fracture rate of the prosthetic abutment was 1.1% (10/876). 31
In addition, we found that the molar position was a predisposing factor for fractures. According to the results, AF in male patients occurred most often in the molar position and with a large‐diameter implant. Notably, the molar is fractured more frequently than anterior or premolar teeth because the molar region is subjected to the greatest masticatory forces. 32 Evidence suggests that the occlusal force is significantly stronger in men than in women. 33 Interestingly, we also found that larger‐diameter (4.5 mm) Ankylos implants had a significantly higher AF rate compared to the small‐diameter (3.5 mm) implants, which is consistent with the results reported by Shim et al. 22 A previous study also identified implant diameter as another factor associated with the rate of implant fracture. 34 All abutments of Ankylos implants have the same diameter of approximately 2.5 mm at the implant platform, regardless of the implant diameter. It is speculated that the causal relationship between the diameter of the implant and AF may be attributed to the fact that larger‐diameter implants are usually used in the molar areas (with a greater bite force), whereas small‐diameter implants are used more often in the anterior areas. Relatively small‐diameter implants are more likely to fracture than large‐diameter implants, but this does not apply to fracture of the abutment. However, further studies should be conducted in the future to validate this hypothesis.
This study is not without its limitations. First, since it is a retrospective study and it was difficult to accurately investigate all risk factors involved in the mechanical complications of abutments, thus, 13 factors were included, while others such as parafunctional activity, occlusion, crown‐implant ratio and so on, 6 , 35 were not discussed in the present study. Therefore, well‐designed prospective studies are required in the future. Second, the follow‐up time of this study is 1–9 years, since the abutment with positioning index of Ankylos was fabricated in 2008, longer follow‐up time are required to corroborate more impactful results in the future.
5. CONCLUSIONS
In conclusion, our data demonstrate that the Morse taper connection of the Ankylos implant is a safe abutment connection. The abutment with the positioning index has a higher incidence of fracture than the abutment without the index. Fracture of the abutment occurs more frequently within the single crown of males in molar areas.
AUTHOR CONTRIBUTIONS
Fan Yang: Concept, Design, Analysis or interpretation of data, Drafting article, Critical revision of article. Yan Ruan: Data collection, Analysis and interpretation of data. Yunqing Liu: Statistics, Data analysis, Critical revision of article. Jianping Chen: Data collection, Supervision, Resources. Yunfang Chen: Research design, Methodology, Project administration. Wentao Zhang: Data analysis, Validation, Approval of article. Yude Ding: Conceptualization, Validation. Linhong Wang: Conceptualization, Data interpretation, Writing draft, Approval of the submitted and final versions.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest related to this study.
ACKNOWLEDGMENTS
This work was supported by the Zhejiang Provincial Natural Science Foundation of China (no. LGF20H140010). We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Yang F, Ruan Y, Liu Y, et al. Abutment mechanical complications of a Morse taper connection implant system: A 1‐ to 9‐year retrospective study. Clin Implant Dent Relat Res. 2022;24(5):683‐695. doi: 10.1111/cid.13115
Funding information Zhejiang Provincial Natural Science Foundation, Grant/Award Number: no.LGF20H140010
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Albrektsson T, Donos N. Implant survival and complications. The third EAO consensus conference 2012. Clin Oral Implants Res. 2012;23(Suppl 6):63‐65. [DOI] [PubMed] [Google Scholar]
- 2. Del FM, Testori T, Kekovic V, Goker F, Tumedei M, Wang HL. A systematic review of survival rates of osseointegrated implants in fully and partially edentulous patients following immediate loading. J Clin Med. 2019;8(12):2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schmitt CM, Nogueira‐Filho G, Tenenbaum HC, et al. Performance of conical abutment (Morse taper) connection implants: a systematic review. J Biomed Mater Res A. 2014;102(2):552‐574. [DOI] [PubMed] [Google Scholar]
- 4. Vinhas AS, Aroso C, Salazar F, Lopez‐Jarana P, Rios‐Santos JV, Herrero‐Climent M. Review of the mechanical behavior of different implant‐abutment connections. Int J Environ Res Public Health. 2020;17(22):8685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pjetursson BE, Thoma D, Jung R, Zwahlen M, Zembic A. A systematic review of the survival and complication rates of implant‐supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implan Res. 2012;23:22‐38. [DOI] [PubMed] [Google Scholar]
- 6. Murakami H, Igarashi K, Fuse M, et al. Risk factors for abutment and implant fracture after loading. J Oral Sci. 2021;63(1):92‐97. [DOI] [PubMed] [Google Scholar]
- 7. Huang HM, Tsai CM, Chang CC, Lin CT, Lee SY. Evaluation of loading conditions on fatigue‐failed implants by fracture surface analysis. Int J Oral Maxillofac Implants. 2005;20(6):854‐859. [PubMed] [Google Scholar]
- 8. Freitas‐Junior AC, Almeida EO, Bonfante EA, Silva NR, Coelho PG. Reliability and failure modes of internal conical dental implant connections. Clin Oral Implants Res. 2013;24(2):197‐202. [DOI] [PubMed] [Google Scholar]
- 9. Gracis S, Michalakis K, Vigolo P, Vult VSP, Zwahlen M, Sailer I. Internal vs. external connections for abutments/reconstructions: a systematic review. Clin Oral Implants Res. 2012;23(Suppl 6):202‐216. [DOI] [PubMed] [Google Scholar]
- 10. Vetromilla BM, Brondani LP, Pereira‐Cenci T, Bergoli CD. Influence of different implant‐abutment connection designs on the mechanical and biological behavior of single‐tooth implants in the maxillary esthetic zone: a systematic review. J Prosthet Dent. 2019;121(3):398‐403. [DOI] [PubMed] [Google Scholar]
- 11. Coppede AR, Bersani E, de Mattos MG, Rodrigues RC, Sartori IA, Ribeiro RF. Fracture resistance of the implant‐abutment connection in implants with internal hex and internal conical connections under oblique compressive loading: an in vitro study. Int J Prosthodont. 2009;22(3):283‐286. [PubMed] [Google Scholar]
- 12. Doring K, Eisenmann E, Stiller M. Functional and esthetic considerations for single‐tooth Ankylos implant‐crowns: 8 years of clinical performance. J Oral Implantol. 2004;30(3):198‐209. [DOI] [PubMed] [Google Scholar]
- 13. Morris HF, Ochi S, Crum P, Orenstein IH, Winkler S. AICRG, part I: a 6‐year multicentered, multidisciplinary clinical study of a new and innovative implant design. J Oral Implantol. 2004;30(3):125‐133. [DOI] [PubMed] [Google Scholar]
- 14. Krebs M, Schmenger K, Neumann K, Weigl P, Moser W, Nentwig GH. Long‐term evaluation of ANKYLOS(R) dental implants, part I: 20‐year life table analysis of a longitudinal study of more than 12,500 implants. Clin Implant Dent Relat Res. 2015;17(Suppl 1):e275‐e286. [DOI] [PubMed] [Google Scholar]
- 15. Zancope K, Dias RC, Castro CG, Salatti RC, Domingues DNF. Influence of the prosthetic index on fracture resistance of Morse taper dental implants. Int J Oral Maxillofac Implants. 2017;32(6):1333‐1337. [DOI] [PubMed] [Google Scholar]
- 16. Zancope K, Resende CC, Tavares LN, Neves FD. Influence of indexed abutments on the fracture resistance of internal conical dental implants. Gen Dent. 2017;65(1):e14‐e16. [PubMed] [Google Scholar]
- 17. Villarinho EA, Cervieri A, Shinkai RS, Grossi ML, Teixeira ER. The effect of a positioning index on the biomechanical stability of tapered implant‐abutment connections. J Oral Implantol. 2015;41(2):139‐143. [DOI] [PubMed] [Google Scholar]
- 18. de Oliveira ST, Mendes AS, Da SVV, de Moura C. Effect of internal hexagonal index on removal torque and tensile removal force of different Morse taper connection abutments. J Prosthet Dent. 2017;117(5):621‐627. [DOI] [PubMed] [Google Scholar]
- 19. Weigl P. New prosthetic restorative features of Ankylos implant system. J Oral Implantol. 2004;30(3):178‐188. [DOI] [PubMed] [Google Scholar]
- 20. Pardal‐Pelaez B, Montero J. Preload loss of abutment screws after dynamic fatigue in single implant‐supported restorations. A systematic review. J Clin Exp Dent. 2017;9(11):e1355‐e1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tsuge T, Hagiwara Y. Influence of lateral‐oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent Mater J. 2009;28(4):373‐381. [DOI] [PubMed] [Google Scholar]
- 22. Shim HW, Yang B. Long‐term cumulative survival and mechanical complications of single‐tooth Ankylos implants: focus on the abutment neck fractures. J Adv Prosthodont. 2015;7(6):423‐430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ding TA, Woody RD, Higginbottom FL, Miller BH. Evaluation of the ITI Morse taper implant/abutment design with an internal modification. Int J Oral Maxillofac Implants. 2003;18(6):865‐872. [PubMed] [Google Scholar]
- 24. Martins CM, Ramos EV, Kreve S, et al. Reverse torque evaluation in indexed and nonindexed abutments of Morse taper implants in a mechanical fatigue test. Dent Res J (Isfahan). 2019;16(2):110‐116. [PMC free article] [PubMed] [Google Scholar]
- 25. Huang Y, Wang J. Mechanism of and factors associated with the loosening of the implant abutment screw: a review. J Esthet Restor Dent. 2019;31(4):338‐345. [DOI] [PubMed] [Google Scholar]
- 26. Hein D, Joly JC, Napimoga MH, Peruzzo DC, Martinez EF. Influence of abutment angulation on loss of prosthetic abutment torque under mechanical cycling. J Prosthet Dent. 2021;125(2):341‐349. [DOI] [PubMed] [Google Scholar]
- 27. El‐Sheikh M, Mostafa T, El‐Sheikh MM. Effect of different angulations and collar lengths of conical hybrid implant abutment on screw loosening after dynamic cyclic loading. Int J Implant Dent. 2018;4(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Merz BR, Hunenbart S, Belser UC. Mechanics of the implant‐abutment connection: an 8‐degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants. 2000;15(4):519‐526. [PubMed] [Google Scholar]
- 29. Alsubaiy EF. Abutment screw loosening in implants: a literature review. J Family Med Prim Care. 2020;9(11):5490‐5494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Papaspyridakos P, Bordin TB, Kim YJ, et al. Technical complications and prosthesis survival rates with implant‐supported fixed complete dental prostheses: a retrospective study with 1‐ to 12‐year follow‐up. J Prosthodont. 2020;29(1):3‐11. [DOI] [PubMed] [Google Scholar]
- 31. Chrcanovic BR, Kisch J, Larsson C. Retrospective clinical evaluation of 2‐ to 6‐unit implant‐supported fixed partial dentures: mean follow‐up of 9 years. Clin Implant Dent Relat Res. 2020;22(2):201‐212. [DOI] [PubMed] [Google Scholar]
- 32. Gealh WC, Mazzo V, Barbi F, Camarini ET. Osseointegrated implant fracture: causes and treatment. J Oral Implantol. 2011;37(4):499‐503. [DOI] [PubMed] [Google Scholar]
- 33. Miwa S, Wada M, Murakami S, Suganami T, Ikebe K, Maeda Y. Gonial angle measured by Orthopantomography as a predictor of maximum occlusal force. J Prosthodont. 2019;28(1):e426‐e430. [DOI] [PubMed] [Google Scholar]
- 34. Shemtov‐Yona K, Rittel D, Machtei EE, Levin L. Effect of dental implant diameter on fatigue performance. Part II: failure analysis. Clin Implant Dent Relat Res. 2014;16(2):178‐184. [DOI] [PubMed] [Google Scholar]
- 35. Stoichkov B, Kirov D. Analysis of the causes of dental implant fracture: a retrospective clinical study. Quintessence Int. 2018;49(4):279‐286. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


