Abstract
Haemophilia treatment has seen great advances in recent years with an accompanied reduced risk of physical activity (PA) related bleeds. Based on its known health benefits, people with haemophilia (PWH) are currently encouraged to regularly engage in PA. However, this may not always translate to increased levels of PA. In this narrative review we aim to provide a brief overview of what is currently understood regarding PA levels and influences for the three broad age groups of children and adolescents, adults and older adults. We also provide recommendations for members of the haemophilia team on important aspects related to promotion of PA in their clinical practice. We highlight that PA behaviour is multifactorial and that many PWH still have limited access to adequate care. Whilst some still face unique challenges to being more physically active, overall, the barriers and facilitators to activity are very similar to that of the general population.
Keywords: behaviour, haemophilia, life stages, physical activity, physical activity promotion
1. INTRODUCTION
People with haemophilia (PWH) have previously been discouraged from leading physically active lifestyles due to the associated increased risk of bleeding. 1 This started to change with the introduction of clotting factor replacement therapy in the 1950′s 2 and the subsequent increased access to regular treatment and implementation of prophylactic treatment to prevent bleeds from the 1970′s onwards. 3 , 4 Currently, PWH are encouraged to participate in regular physical activity (PA), 4 in accordance with the World Health Organization (WHO) recommendations, which now also specifically include people living with chronic conditions. 5 There have been significant advances in haemophilia treatment in recent years, with several extended half‐life products now available and non‐replacement therapies emerging. Gene therapy is also in late‐stage development for those with severe haemophilia, 6 and was just granted conditional marketing approval in the European Union for those with severe haemophilia A without inhibitors. 7
Whilst advancements in haemostatic therapies for PWH may encourage enhanced levels of PA, this may not always translate into actual changes in the day‐to‐day life or behaviours of PWH. 8 Co‐morbid musculoskeletal issues exist on a spectrum from minimal to very high, depending on age, previous and current access to healthcare and people's behaviours. Strict adherence to continuous prophylaxis in severe haemophilia is still required to avoid deterioration of joint status despite low bleeding rates, and to allow for higher levels of PA with minimal risk of bleeding.
Physical inactivity is considered the fourth leading risk factor for all‐cause mortality and a major public‐health issue. 5 Enabling more and better PA in all age groups regardless of the underlying health condition is a pressing public health issue, and perhaps even more so within those with haemophilia. Bleeds, pain, arthropathy and fear of new bleeds may cause PWH to get trapped in a vicious circle of inactivity: Reduced PA may, in turn, lead to weight gain and increased load on joints, followed by further bleeds and mobility problems. 4 , 9 , 10 This paper aims to present an overview of current understanding of PA and conceptualise it within a lifespan model of those living with haemophilia.
2. PHYSICAL ACTIVITY: STATUS, INFLUENCES AND RECOMMENDATIONS
PA is defined as ‘any bodily movement, produced by skeletal muscles, requiring energy expenditure’. 11 It includes all types of activity, including everyday activities (work, play, active transport, shopping, etc.), active hobbies (walking, dancing, swimming, gym‐based exercise, etc.) and competitive sports (e.g., football, cycling, tennis). Clinicians should remember that people's perceptions of what PA is can vary between individuals, based on their personal experience and knowledge and should adapt their consultation strategies accordingly.
It is well established that PA has numerous health benefits, including contributions to the prevention and management of non‐communicable diseases such as cardiovascular disease, diabetes and several cancers, improvements in sleep, mental and cognitive health, as well as preventing overweight, functional decline, falls and fall‐related injuries. 5 , 12 The WHO recommends people of all ages undertake regular and adequate moderate to vigorous intensity PA to achieve such health benefits. 5 , 13 PWH can achieve the same health benefits of PA as seen in the general population, and may also experience reduced joint and muscle bleeds via improvements in muscle strength, proprioception, balance, joint mobility, stability and function. 14 , 15 Furthermore, benefits of PA generally outweigh the risks, including for people living with musculoskeletal pain and frailty. 16
Several models and approaches have been developed to promote positive behaviour change and have been used to enhance interventions based on modifying PA (e.g. ‘The Transtheoretical Model of Health Behaviour Change’, 17 the ‘Theory of Planned Behaviour’, 18 the ‘Behaviour Change Wheel 19 ’ and ‘Therapeutic Education 20 ’). It is not the aim of this paper to advocate for or recommend one behaviour change theory over another, and readers are encouraged to develop their own knowledge and understanding of these and/or other models and approaches for the use in PA promotion within their clinical practice.
PA is a behaviour influenced by a variety of factors at individual, social, environmental and policy levels. 21 The significance of these factors varies between age groups, life stages and physical function, and must be taken into consideration by clinicians promoting PA. Physical literacy, that is, the motivation, confidence, physical competence, knowledge and understanding to value and take responsibility for engagement in physical activities for life is particularly important. 22 , 23 The many and varied potential competing influences on an individual's choice to be active need to be acknowledged and understood by all healthcare professionals. Such an approach may help inform any intervention that aims to encourage changes to PA, particularly in relation to the additional barriers PWH may face. Examples of such factors are shown in Figure 1.
FIGURE 1.
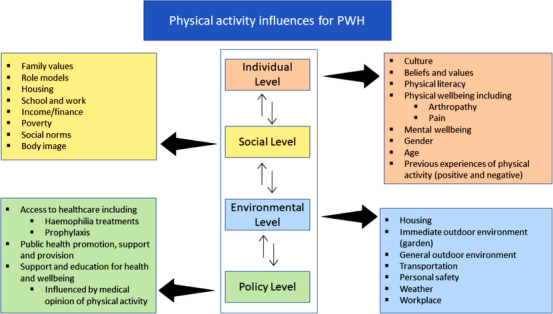
Physical activity influences for PWH
In the following section, we discuss what is currently understood about PA in three broad age groups of children and adolescents, adults and older adults, as well as provide general recommendations for practice working with PA promotion for PWH.
2.1. Children and adolescents
For children and adolescents aged 5–17 years, the WHO recommends at least an average of 60 min of moderate to vigorous physical activity (MVPA) per day and to incorporate activities that strengthen muscle and bone on at least 3 days per week. 5 In the general population it is estimated that 81% of adolescents (aged 11–17 years) do not meet recommendations for aerobic PA. 24 There is almost no data on global PA levels of the youngest children (ages 0–4 years) and very little data on those < 10 years. 25 However, contrary to these figures in the general population, a recent systematic review demonstrates that children with haemophilia are now close to reaching the recommended 60 min of MVPA per day and that a large proportion are as engaged in sports as the general population. 26 Why such a difference between the general population and children with haemophilia may exist is unclear though it remains a positively encouraging observation. We speculate that this could be related to regular encouragement and reassurance by the multidisciplinary haemophilia teams of the benefits and safety of PA for PWH on prophylaxis.
In the general population, the individual and social factors that have been shown to be positively associated with PA for children and adolescents are male gender, previous PA and self‐efficacy, the latter meaning confidence in the ability to be physically active in specific situations. 21 Perceived behavioural control, that is, general perceptions of ability to be physically active, family and social support are also of importance for adolescents. Regarding environmental factors, the most important are walkability, lower traffic speed and volume, residential density, proximity of homes and shops and access or proximity to recreation facilities. 21
For children with haemophilia, the main facilitators of PA are that the activity is fun and an opportunity to be with friends, which in turn can help develop self‐efficacy for PA which will promote this positive behaviour even more. 27 , 28 For young children, one barrier to PA may be caregivers’ fear of PA related bleeds, 29 and the importance of feeling safe has also been highlighted by adolescents and young adults (aged 14–25 years). 30 Safety depends on several factors, including the person's developmental status, functional level and fitness, as well as type, intensity and volume of PA together with the availability, level of and adherence to recommended treatments. 31 , 32 , 33
2.1.1. Recommendations
Clinicians should:
Be knowledgeable of the risks and benefits of PA for PWH and reassure children and parents of the safety that comes with adequate medical treatment. 34 , 35 , 36
Be able to advise PWH regarding appropriate types, intensity and frequency of activity, depending on the child's psychomotor development, health status, bleeding tendency, access and adherence to treatment, and not least based on the young person's motivation. 37
Ensure they have an understanding of the values that parents of children with haemophilia attribute to PA, and be prepared to engage on a family level as well as an individual level when discussing the risks and benefits of PA.
Set tailored and appropriate PA goals to avoid discouragement.
2.2. Adults
For adults aged 18–64, the WHO recommends at least 150–300 min of moderate intensity (MPA) or 75–150 min of vigorous‐intensity PA (VPA) per week, or a combination of the two, as well as muscle‐strengthening activities at least 2 days per week. 5 In the general population it is estimated that 27.5% of adults (≥18 years) globally do not meet recommendations for aerobic PA, 38 and this appears to be similar for many adults with haemophilia, where a recent systematic review of PWH's habitual PA showed that most are classified as sedentary. 26 There is, however, presumably a spectrum of PA levels within this broad age category, reflecting various life situations, functional levels and heterogeneous perceptions of PA. Notably and encouragingly, it seems that those younger adult PWH using long‐term prophylaxis and/or exhibiting a mild/moderate bleeding phenotype who have a supportive social environment are as active as their healthy peers. 39 , 40 , 41
In the general adult population, health status and self‐efficacy are the most important individual factors for being physically active, followed by previous PA and intention to exercise. 21 Younger age, male sex, social support, education level, ethnic origin, not being overweight, low perceived effort of PA, availability of recreation facilities, transportation environment, and aesthetic pleasantness of the environment are other factors associated with PA for adults. 21 For PWH, facilitators of PA are self‐efficacy, 27 fun and social aspects, 28 and motivation to participate in sport appears to depend upon enthusiasm and interest. 42 Having positive role models is also valuable. 43 , 44 Personal barriers to PA may include family responsibilities, job strain, stress, lack of time, motivation, support and resources, as well as pain, fair of injury, lack of energy and a perception that it is too difficult. 45 , 46 , 47 , 48 , 49 The challenges of being physically active for those PWH in the older age range within this category or those who have had limited access to treatment are probably greater than for many other PWH. It is likely that they grew up with advice to avoid PA, have had negative experiences with PA‐related bleeds, and are now living with sequelae of haemophilic arthropathy, pain and functional limitations. 50 , 51 This may contribute to a perception that PA is associated with the development of bleeds, injuries and joint damage. 46 , 47 , 52 For this group, lack of accessible equipment and transportation and unqualified personnel who are unable to adapt exercises for people with disabilities may be important environmental barriers. 48
2.2.1. Recommendations
Clinicians should:
Provide support and advice according to the life situation, health status, pain, functional levels and previous PA experiences of adult PWH.
Assist in the selection of appropriate PA that minimises the risk of injury and matches the individual's interests, skills and needs. 31
2.3. Older adults
For older adults aged over 65, the WHO recommends at least 150–300 min of MPA or 75–150 min of VPA per week, or a combination of the two, as well as muscle strengthening activities at least two days per week and multicomponent PA with emphasis on functional balance and strength at least 3 times per week. 5 In European older adults (> 55 years) an overall of 12.5% (range 5%–29%) appear to be physically inactive. 53 PA levels of older PWH specifically, does not seem to have been studied or analysed separately from adults in general. Results from studies including also those over 65 suggest that this age group is less active than the younger. 1 , 54 , 55
In the general population, the most consistent personal factors facilitating PA for this age group appear to be health status, self‐efficacy, personal history of PA during adulthood and intention to exercise. 21 Consistent environmental barriers or facilitators of PA among older adults have not been reported to date. 21 For older PWH, barriers to PA include pain, fear of falls and injury, lack of energy, motivation, support, resources, confidence and transport. 45 , 46 , 47 , 48 , 56
When considering PA levels in older adults in the general population, three categories, which are also relevant for older PWH, are suggested: ‘Active Older Adults’ (those who are already active), ‘Active Older Adults in Transition’ (those who demonstrate declining function, possibly with lower levels of activity and significant sedentary time) and ‘Frailer Older Adults’ (representing those with low physical or cognitive function as a result of chronic disease, dementia or advanced old age). 57 Although some highly motivated older PWH may manage to maintain high levels of PA, clinicians should keep in mind that PA generally requires elements of strength, endurance, balance, and coordination that is often taken for granted. 48 For older PWH, such physical attributes may be impaired because of a combination of multi‐joint arthropathy, lower levels of fitness or functional capacity, and a history of extended periods of inactivity associated with bleeds or fear of bleeding, that may limit their access to PA.
2.3.1. Recommendations
Clinicians should:
Consider the life situation, health status, pain, PA and functional levels and previous experiences of PA of older PWH and provide support and advice accordingly.
Address pain and fatigue management and how to gradually build up PA levels.
Keep in mind that frailty is not a contraindication to exercise, but conversely one of the most important reasons to prescribe it. 58
2.4. General clinical practice key points
Although PA is recommended and has numerous benefits, clinicians cannot expect that simply advising PWH to increase their PA levels will be effective. Although recent advances in the treatment of haemophilia have been substantial, there is still great variability in access to adequate medical treatment and care for PWH. We also know that multiple factors impact PA to various degrees for people in different life stages. Additional challenges for clinicians are to operationalise effective PA advice, 16 variability in knowledge and perceptions about PA between health care professions, 59 and lack of education and resources to promote PA. 60 With these challenges in mind, we here present some clinical practice key points related to PA promotion for members of the haemophilia team:
Clinicians should be up to date on PA recommendations.
There should be a coherent approach across clinical teams in their communication about PA.
An understanding of individual, social and environmental factors influencing PA in various age groups is important to tailor successful advice and interventions. This includes general factors as well as those specific for PWH, such as bleeding phenotype, intensity of‐, access to‐ and adherence to treatment.
Rather than recommending ‘population norm PA’ clinicians should seek to understand the needs of each person in their care, their unique thoughts and beliefs around PA, and communicate in a collaborative and consistent way about PA benefits.
Clinicians need to identify each individual's starting point and motivation for PA, begin there and advise each person on how to build up PA frequency, intensity and duration gradually.
Injuries in PWH should be closely monitored and treated in close cooperation between patients and clinicians.
3. CONCLUSION
Although haemophilia treatment has seen great advances in recent years with concomitant reduced risk of PA related bleeds, this may not automatically translate into increased PA in PWH. Many PWH still have limited access to adequate care and PA is a behaviour influenced by numerous factors. Physical inactivity is a global public health concern, and in addition to general barriers to being physically active PWH face some unique challenges. Haemophilia treaters need to be able to confidently support PWH in making positive decisions and behaviour changes relating to PA. In order to do so, clinicians need to provide individualised advice and support based on up‐to‐date information on barriers and motivators for PA combined with the person's unique physical, cognitive and emotional characteristics.
CONFLICT OF INTERESTS
The authors stated that they had no interests which may be perceived as posing a conflict or bias.
AUTHOR CONTRIBUTIONS
All authors contributed to the conceptualisation, writing, revision and final approval of the paper.
ACKNOWLEDGEMENT
This paper was written on behalf of the EAHAD Physiotherapists Committee.
Matlary RED, Grinda N, Sayers F, Versloot O, McLaughlin P. Promoting physical activity for people with haemophilia in the age of new treatments. Haemophilia. 2022;28:885–890. 10.1111/hae.14641
DATA AVAILABILITY STATEMENT
Data sharing not applicable ‐ no new data generated.
REFERENCES
- 1. Von Mackensen S. Quality of life and sports activities in patients with haemophilia. Haemophilia. 2007;13:38‐43. [DOI] [PubMed] [Google Scholar]
- 2. Steen Carlsson K, Höjgård S, Glomstein A, et al. On‐demand vs prophylactic treatment for severe haemophilia in Norway and Sweden. Haemophilia. 2003;9:555‐566. [DOI] [PubMed] [Google Scholar]
- 3. Oldenburg J. Optimal treatment strategies for hemophilia: achievements and limitations of current prophylactic regimens. Blood. 2015;125(13):2038‐2044. [DOI] [PubMed] [Google Scholar]
- 4. Srivastava A, Santagostino E, Dougall A, et al. WFH guidelines for the management of hemophilia, 3rd edition. Haemophilia. 2020;26(S6):1‐158. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization. 2020.
- 6. Arruda VR, Doshi BS, Samelson‐Jones BJ. Novel approaches to hemophilia therapy: successes and challenges. Blood. 2017;130(21):2251‐2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. European Medicines Agency. First gene therapy to treat severe haemophilia A 2022; https://www.ema.europa.eu/en/news/first‐gene‐therapy‐treat‐severe‐haemophilia Accessed July, 2022.
- 8. Lobet S, Timmer M, Königs C, et al. The role of physiotherapy in the new treatment landscape for haemophilia. J Clin Med. 2021;10(13):2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wong TE, Majumdar S, Adams E, et al. Overweight and obesity in hemophilia: a systematic review of the literature. Am J Prev Med. 2011;41:S369‐375. 6 Suppl 4. [DOI] [PubMed] [Google Scholar]
- 10. Lim MY, Wei G, Presson AP, Bray P, Rodgers GM. High prevalence of overweight/obesity in adult persons with hemophilia in Utah and a review of the literature. Blood Coagul Fibrinolysis. 2020;31(8):522‐529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health‐related research. Public Health Rep. 1985;100(2):126. [PMC free article] [PubMed] [Google Scholar]
- 12. Crimmins EM. Lifespan and healthspan: past, present, and promise. Gerontologist. 2015;55(6):901‐911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bull FC, Al‐Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451‐1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang M, Álvarez‐Román MT, Chowdary P, Quon DV, Schafer K. Physical activity in individuals with haemophilia and experience with recombinant factor VIII Fc fusion protein and recombinant factor IX Fc fusion protein for the treatment of active patients. Blood Coagul Fibrinolysis. 2016;27(7):737‐744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harris S, Boggio LN. Exercise may decrease further destruction in the adult haemophilic joint. Haemophilia. 2006;12(3):237‐240. [DOI] [PubMed] [Google Scholar]
- 16. Reid H, Ridout AJ, Tomaz SA, Kelly P, Jones N; Physical Activity Risk Consensus group . Benefits outweigh the risks: a consensus statement on the risks of physical activity for people living with long‐term conditions. Br J Sports Med. 2022;56(8):427‐438. 10.1136/bjsports-2021-104281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38‐48. [DOI] [PubMed] [Google Scholar]
- 18. Ajzen I, From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckmann J, eds. Action control: from cognition to behavior. Springer Berlin Heidelberg; 1985:11‐39. [Google Scholar]
- 19. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(42). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Boiché J, Perrin C, Ninot G, Varray A, Barriers to exercise: statement and motivational strategies. 2020.
- 21. Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380(9838):258‐271. [DOI] [PubMed] [Google Scholar]
- 22. Tremblay MS, Costas‐Bradstreet C, Barnes JD, et al. Canada's physical literacy consensus statement: process and outcome. BMC Public Health. 2018;18(Suppl 2):1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Whitehead M. The concept of physical literacy. Eur J Phys Educ. 2006;6(2):127‐138. [Google Scholar]
- 24. Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population‐based surveys with 1·6 million participants. Lancet Child Adolesc Health. 2020;4(1):23‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Aubert S, Brazo‐Sayavera J, Gonzalez SA, et al. Global prevalence of physical activity for children and adolescents; inconsistencies, research gaps, and recommendations: a narrative review. Int J Behav Nutr Phys Act. 2021;18(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kennedy M, O'Gorman P, Monaghan A, et al. A systematic review of physical activity in people with haemophilia and its relationship with bleeding phenotype and treatment regimen. Haemophilia. 2021;27(4):544‐562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bandura A. Self‐efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;88(2):191‐215. [DOI] [PubMed] [Google Scholar]
- 28. Fromme A, Dreeskamp K, Pollmann H, Thorwesten L, Mooren F, Völker K. Participation in sports and physical activity of haemophilia patients. Haemophilia. 2007;13(3):323‐327. [DOI] [PubMed] [Google Scholar]
- 29. Rosso N, Guillaume Y, Roche M, et al. Dispositif pluridisciplinaire d'accompagnement des enfants et de leur famille depuis l'annonce diagnostique d'une forme sévère d'hémophilie. Revue d'Oncologie Hématologie Pédiatrique. 2016;4(3):156‐161. [Google Scholar]
- 30. Hoefnagels JW, Kars MC, Fischer K, Schutgens R, Schrijvers LH. The Perspectives of adolescents and young adults on adherence to prophylaxis in hemophilia: a qualitative study. Patient Prefer Adherence. 2020;14:163‐171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Petrini P, Seuser A. Haemophilia care in adolescents compliance and lifestyle issues. Haemophilia. 2008;15:15‐19. [DOI] [PubMed] [Google Scholar]
- 32. Seuser A, Boehm P, Kurme A, Schumpe G, Kurnik K. Orthopaedic issues in sports for persons with haemophilia. Haemophilia. 2007;13:47‐52. [DOI] [PubMed] [Google Scholar]
- 33. Seuser A, Böhm P, Wermes C. Early orthopaedic challenges in haemophilia patients and therapeutic approach. Thromb Res. 2014;134:61‐67. [DOI] [PubMed] [Google Scholar]
- 34. Manco‐Johnson MJ. Collision sports and risk of bleeding in children with hemophilia. JAMA. 2012;308:1480‐1481. [DOI] [PubMed] [Google Scholar]
- 35. Ross C, Goldenberg NA, Hund D, Manco‐Johnson MJ. Athletic participation in severe hemophilia: bleeding and joint outcomes in children on prophylaxis. Pediatrics. 2009;124(5):1267‐1272. [DOI] [PubMed] [Google Scholar]
- 36. Broderick CR, Herbert RD, Latimer J, et al. Association between physical activity and risk of bleeding in children with hemophilia. JAMA. 2012;308(14):1452. [DOI] [PubMed] [Google Scholar]
- 37. Howell C, Scott K, Patel DR. Sports participation recommendations for patients with bleeding disorders. Transl Pediatr. 2017;6(3):174‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population‐based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077‐e1086. [DOI] [PubMed] [Google Scholar]
- 39. Negrier C, Seuser A, Forsyth A, et al. The benefits of exercise for patients with haemophilia and recommendations for safe and effective physical activity. Haemophilia. 2013;19(4):487‐498. [DOI] [PubMed] [Google Scholar]
- 40. Buxbaum NP, Ponce M, Saidi P, Michaels LA. Psychosocial correlates of physical activity in adolescents with haemophilia. Haemophilia. 2010;16:656‐661. [DOI] [PubMed] [Google Scholar]
- 41. Versloot O, Balen EC, Hassan S, et al. Similar sports participation as the general population in Dutch persons with haemophilia; results from a nationwide study. Haemophilia. 2021;27:876‐885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Koiter J, van Genderen FR, Brons PP, Nijhuis‐van der Sanden MW. Participation and risk‐taking behaviour in sports in children with haemophilia. Haemophilia. 2009;15(3):686‐694. [DOI] [PubMed] [Google Scholar]
- 43. Morgenroth T, Ryan MK, Peters K. The motivational theory of role modeling: how role models influence role aspirants’ goals. Rev Gen Psychol. 2015;19(4):465‐483. [Google Scholar]
- 44. Willis C, Girdler S, Thompson M, Rosenberg M, Reid S, Elliott C. Elements contributing to meaningful participation for children and youth with disabilities: a scoping review. Disabil Rehabil. 2017;39(17):1771‐1784. [DOI] [PubMed] [Google Scholar]
- 45. Taylor S, Toye F, Donovan‐Hall M, Barker K. Past the tipping point: a qualitative study of the views and experiences of men with haemophilia regarding mobility, balance, and falls. Disabil Rehabil. 2021:1‐9. [DOI] [PubMed] [Google Scholar]
- 46. Flaherty LM, Schoeppe J, Kruse‐Jarres R, Konkle BA. Balance, falls, and exercise: beliefs and experiences in people with hemophilia: a qualitative study. Res Pract Thromb Haemost. 2018;2(1):147‐154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Baumann K, Hernandez G, Witkop M, et al. Impact of mild to severe hemophilia on engagement in recreational activities by US men, women, and children with hemophilia B: the Bridging Hemophilia B Experiences, Results and Opportunities into Solutions (B‐HERO‐S) study. Eur J Haematol. 2017;98(Suppl 86):25‐34. [DOI] [PubMed] [Google Scholar]
- 48. Rimmer JH, Marques AC. Physical activity for people with disabilities. Lancet. 2012;380(9838):193‐195. [DOI] [PubMed] [Google Scholar]
- 49. Kennedy M, Monaghan A, Roche S, et al. Barriers to physical activity amongst adults with moderate and severe haemophilia in Ireland: the Irish Personalised Approach to the Treatment of Haemophilia (iPATH) Study. Haemophilia. 2019;25(S1):35‐188. [Google Scholar]
- 50. Knobe K, Berntorp E. Haemophilia and joint disease: pathophysiology, evaluation, and management. J Comorb. 2011;1(1):51‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kennedy M, O' Mahony B, Roche S, et al. Pain and functional disability amongst adults with moderate and severe haemophilia from the Irish personalised approach to the treatment of haemophilia (iPATH) study. Eur J Haematol. 2022;108(6):518‐527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. McLaughlin P, Hurley M, Chowdary P, Stephensen D, Khair K. How does a lifetime of painful experiences influence sensations and beliefs about pain in adults with severe haemophilia? A qualitative study. 2021:1‐8. [DOI] [PubMed]
- 53. Gomes M, Figueiredo D, Teixeira L, et al. Physical inactivity among older adults across Europe based on the SHARE database. Age Ageing. 2017;46(1):71‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Taylor S, Room J, Barker K. Physical activity levels in men with Haemophilia—a single centre UK survey. Haemophilia. 2020;26(4):718‐725. [DOI] [PubMed] [Google Scholar]
- 55. Baumgardner J, Elon L, Antun A, et al. Physical activity and functional abilities in adult males with haemophilia: a cross‐sectional survey from a single US haemophilia treatment centre. Haemophilia. 2013;19(4):551‐557. [DOI] [PubMed] [Google Scholar]
- 56. McLaughlin P, Hurley M, Chowdary P, Stephensen D, Khair K. The experiences and beliefs of people with severe haemophilia and healthcare professionals on pain management, and their views of using exercise as an aspect of intervention: a qualitative study. Disabil Rehabil. 2021:1‐9. [DOI] [PubMed] [Google Scholar]
- 57. UK Chief Medical Officers . UK Chief Medical Officers' Physical Activity Guidelines. 2019.
- 58. Bauman A, Merom D, Bull FC, Buchner DM, Fiatarone Singh MA. Updating the evidence for physical activity: summative reviews of the epidemiological evidence, prevalence, and interventions to promote “Active Aging”. Gerontologist. 2016;56(S2):S268‐280. [DOI] [PubMed] [Google Scholar]
- 59. Douglas F, Torrance N, van Teijlingen E, Meloni S, Kerr A. Primary care staff's views and experiences related to routinely advising patients about physical activity. A questionnaire survey. BMC Public Health. 2006;6:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Huijg JM, Gebhardt WA, Verheijden MW, et al. Factors influencing primary health care professionals' physical activity promotion behaviors: a systematic review. Int J Behav Med. 2015;22(1):32‐50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable ‐ no new data generated.


