Abstract
A literature search was conducted to systematically review and meta‐analyze time‐loss and recurrence rate of lateral ankle sprains (LAS) in male professional football players. Six electronic databases (PubMed, Scopus, Web of Science, PEDRO, CINAHL, and Cochrane) were searched independently, separately both for time‐loss and recurrence from inception until April 30, 2021. In addition, reference lists were screened manually to find additional literature. Cohort studies, case reports, case–control studies and RCT in English language of male professional football players (aged more than 16 years) for which data on time‐loss or recurrence rates of LAS were available were included. A total of 13 (recurrence) and 12 (time‐loss) studies met the inclusion criteria. The total sample size of the recurrence studies was 36,201 participants (44,404 overall initial injuries; 7944 initial ankle sprain [AS] injuries, 1193 recurrent AS injuries). 16,442 professional football players (4893 initial AS injuries; 748 recurrent AS injuries) were meta‐analyzed. A recurrence rate of 17.11% (95% CI: 13.31–20.92%; df = 12; Q = 19.53; I2 = 38.57%) based on the random‐effects model was determined. A total of 7736 participants were part of the time‐loss studies (35,888 total injuries; 4848 total ankle injuries; 3370 AS injuries). Out of the 7736 participants, 7337 participants met the inclusion criteria with a total of 3346 AS injuries. The average time‐loss was 15 days (weighted mean: 15.92; median: 14.95; min: 9.55; max: 52.9). We determined a priori considerable heterogeneity (CI: 18.15–22.08; df = 11; Q = 158; I2 = 93%), so that the data on time‐loss are only presented descriptively. There is an average time‐loss of 15 days per LAS and a recurrence rate of 17%. LAS is one of the most common types of injury with higher recurrence rates than ACL injuries (9%–12%) in professional football players. Nevertheless, the focus of research in recent years has been mostly on ACL injuries. However, the high recurrence rates and long‐term consequences show the necessity for research in the field of LAS in elite football. Yet, heterogeneous data lead to difficulties concerning the aspect of comparability.
Keywords: ankle, football, rehabilitation, sporting injuries, sprains
1. INTRODUCTION
Ligamentous injuries of the ankle are among the most common types of injuries in sports, 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 especially in sports with multi‐directional movement patterns. 10 , 11 , 12 , 13 Along with muscle (33–35%) 14 , 15 , 16 , 17 and knee joint injuries (15%–21%), 14 , 16 , 17 , 18 , 19 , 20 trauma to the ankle is the third most common type of injury in professional football. 17 , 21 , 22 , 23 The injury rate is still high despite a decreasing trend in the injury frequency of ligamentous ankle injuries in professional soccer 24 : 10–18% of the occurring injuries in professional football involve the ankle. 15 , 17 , 19 , 21 , 25 , 26 , 27 , 28 , 29 Of this, ligamentous injuries (ankle sprains) account for a large proportion of occurring ankle injuries, with 62–69%. 24 , 25 , 26 More than 75% of ankle sprains involve the lateral ligaments. 24 , 25 , 26
Previous injuries and inadequate rehabilitation are considered the greatest risk factors for recurrent injuries 14 , 30 , 31 , 32 : the re‐injury rate of ligamentous ankle injuries in sports is increased two‐ to fivefold, 13 , 33 , 34 and especially in soccer up to fivefold. 31 , 35 , 36 , 37 , 38 , 39 Persistent symptoms such as feelings of instability, persistent swelling, continuous pain conditions, limited mobility, or cartilage defects can have serious long‐term consequences for athletes, and in the worst case, lead to early career dropout. 34 , 40
Injury‐related time‐loss due to initial or recurrent injuries can have significant consequences from many perspectives for various stakeholders (clubs, teams, players, insurances): The team's success depends largely on player availability. 41 , 42 Long periods of time‐loss can therefore have a negative impact on the success of a team and, as a consequence, can be decisive for its performance in the league table and for promotion and relegation. In turn, poor table performance can have important consequences for clubs and indirectly causes high costs. 43 Medical treatment costs directly affect insurance companies. Players, especially elite junior athletes, can be hindered in their athletic development by injury‐related time‐loss. In addition, an inadequately rehabilitated initial injury, especially in adolescence, is often the beginning of a persistent “injury career”. 30
Lateral ankle ligament injury is still trivialized. Often, the time‐loss is less than the time of physiological wound healing. 44 An injury that has not completely healed can have long‐lasting consequences (e.g., CAI) and can be a major risk factor for re‐injury. Due to differences in study designs, current data on time‐loss and recurrence rates of ligamentous ankle injuries in professional football are very heterogeneous. Therefore, this review aimed to systematically compile data on time‐loss and recurrence rates of lateral ligamentous ankle injuries in male professional football (soccer). Data on time‐loss and recurrence rate can be used as outcome parameters both for practitioners to evaluate the effectiveness of existing concepts and for researchers to evaluate future return to sports approaches.
2. MATERIAL AND METHODS
All procedures were performed in accordance with the latest PRISMA statement. 45
2.1. Search strategy
We conducted a systematic literature search on time‐loss and recurrence rates of ligamentous lateral ankle injuries in male professional football players from inception until April 30, 2021 (PROSPERO: CRD42020201577).
2.2. Study selection and eligibility criteria
Studies had to meet the following inclusion criteria: (1) peer‐reviewed; (2) availability of epidemiological data; (3) study type: case reports, case–control studies, case‐cohort studies, randomized controlled trials; (4) sex: male; (5) age: >16 years; (6) Level of play: professionals; (7) sports: football (soccer); and (8) injury: lateral ligamentous ankle injuries.
2.3. Databases and reference lists
We scanned six electronic databases (PubMed, CINAHL, Cochrane, PEDro, Scopus, and Web of Science) during August–September 2020 with the following search terms in Boolean search strategy both for time‐loss (football OR soccer) AND (elite OR professional) AND (ankle injuries OR ankle sprains OR lateral ligamentous ankle injuries OR lateral ligamentous ankle sprains) AND (time‐loss OR time lost injury OR time* OR return*) and recurrence rate (football OR soccer) AND (elite OR professional) AND (ankle injuries OR ankle sprains OR lateral ligamentous ankle injuries OR lateral ligamentous ankle sprains) AND (recurrence* OR reinjur* OR recurrent* OR repeat* OR second*). Reference lists were manually scanned to find additional relevant studies that had not been identified in the electronic databases.
2.4. Screening process
2.4.1. Abstract screening
Two independent examiners (ZF, KH) screened title and abstracts. Titles were transferred into an Excel list and were reviewed by the first author (ZF) for accordance. A third author (KDC) was contacted in case of disagreement and decided whether to include the abstract in the full‐text screening.
2.4.2. Full‐text screening
ZF screened all of the relevant articles (October/November 2020) for meeting the inclusion criteria using a codebook (Excel file). Relevant articles were screened in a two‐step procedure: in a pre‐final analysis, evidently irrelevant articles were excluded. In a further final analysis, the remaining articles were screened again. This two‐step analysis approach ensured meeting the inclusion criteria. Before data extraction, the second author (KH) screened the articles that passed the final analysis (Appendix S1 and S2).
2.4.3. Data extraction
Relevant articles for both time‐loss and recurrence rate were tabulated by the first author (ZF) in three categories (1) characteristics of included studies; (2) subgroup analysis; (3) results. Subsequently, data were compiled from relevant articles.
2.5. Quality assessment of reporting quality
A modified version of the STROBE guidelines 46 was used to assess methodological quality and was systematically evaluated using a checklist and data sheet (Appendix S3 and S4). We extracted 11 of the 22 items (Methods: Items 4–9; Results: Items 15, 16; Discussion: 18–20). One point could be given for each item. We defined sub‐items as necessary (N) or facultative (F), respectively. To evaluate an item as 1, all necessary sub‐items (N) must be met. We used a range system. Studies within a range of 8–11 points were defined as high quality, 4–7 points as moderate, and 0–3 points as low quality. Two examiners (ZF, KH) evaluated each study independently. In case of disagreement, a third author (KDC) made the final assessment. Modifications of the STROBE guidelines have already been applied in previous reviews. 22 , 23 , 47
2.6. Dealing with missing data
Data could be calculated if other data were available that allowed an unambiguous calculation. Missing data were requested from the author via e‐mail if studies seemed to have useful but not clear reported data. The authors had to respond on request within four weeks. This approach could potentially raise the number of included studies.
2.7. Data extraction: Systematic review
Separate data extraction sheets were prepared for both outcome parameters of interest (time‐loss and recurrence rate). Relevant data on the time of recurrence (early/late) for the outcome parameters were extracted from the studies and entered into these data sheets. The data relevant for time‐loss are type of ankle injury, frequency of ankle injury (n+%), frequency of ankle injury in different age‐groups (n+%), time‐loss (days) in different age groups (n+%), and severity (n+%). The following data of recurrence rate were of interest: type of injury, frequency of ankle injury initial and recurrence (n+%), frequency of ankle injuries in different age groups (n+%), frequency of recurrence in different age groups (n+%), on the time of recurrence (early/late) for the outcome parameters were extracted from the studies and entered into these data sheets.
2.8. Data extraction and statistical analysis: Meta‐analysis
Data on the relevant outcome parameters (time‐loss: overall sample size; number of injuries; lost time in days, age; recurrence rate: overall sample size, number of injuries), number of recurrences (n+%) were statistically evaluated.
Only data from the target group (male, age > 16 years–professionals) were calculated in the meta‐analysis. The meta‐analysis was conducted based on the random‐effects model 48 : Heterogeneity was both determined by using the Cochran's Q and I 2 test and in addition visually checked by the funnel plot. The following thresholds were set to guide the interpretation of heterogeneity: 0%–40% (not important), 30%–60% (moderate), 50%–90% (substantial), and 75%–100% (considerable).
2.9. Deviations from the PROSPERO protocol
Only minor changes were made to the PROSPERO protocol. Deviating from the previously defined inclusion criteria, we also included studies that did not include a clear definition of recurrence rate.
3. SYSTEMATIC REVIEW
3.1. Results
3.1.1. Search process
Time‐loss
A total of 412 records were identified in six electronic databases whose abstracts and titles were screened. After removing irrelevant studies, a total of 12 studies for time‐loss were included in the analysis. The process is shown in Figure 1.
FIGURE 1.
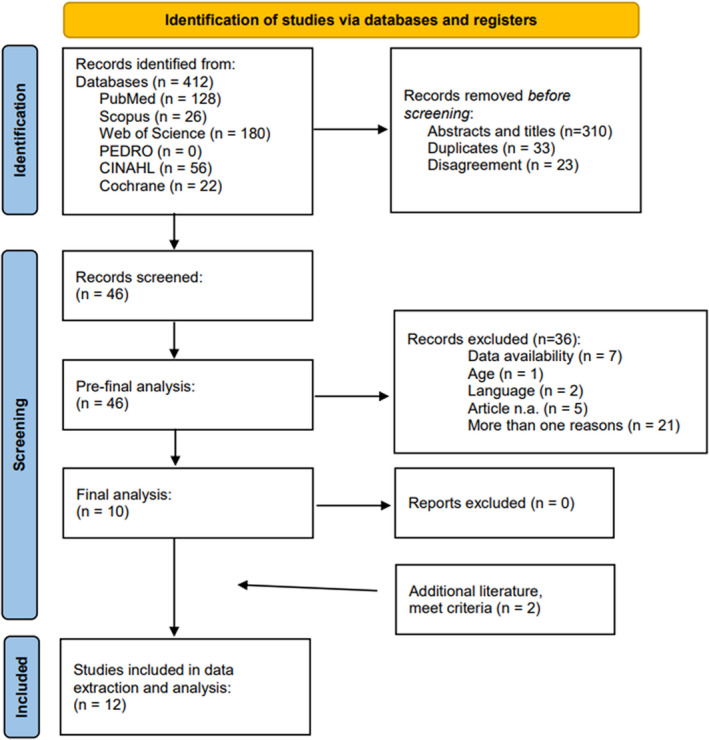
Flow‐Chart time‐loss
Recurrence rate
In sum, 516 records were identified for recurrence rate. At the end of the screening procedure, a total of 13 studies met the inclusion criteria and were analyzed for recurrence rate (Figure 2).
FIGURE 2.
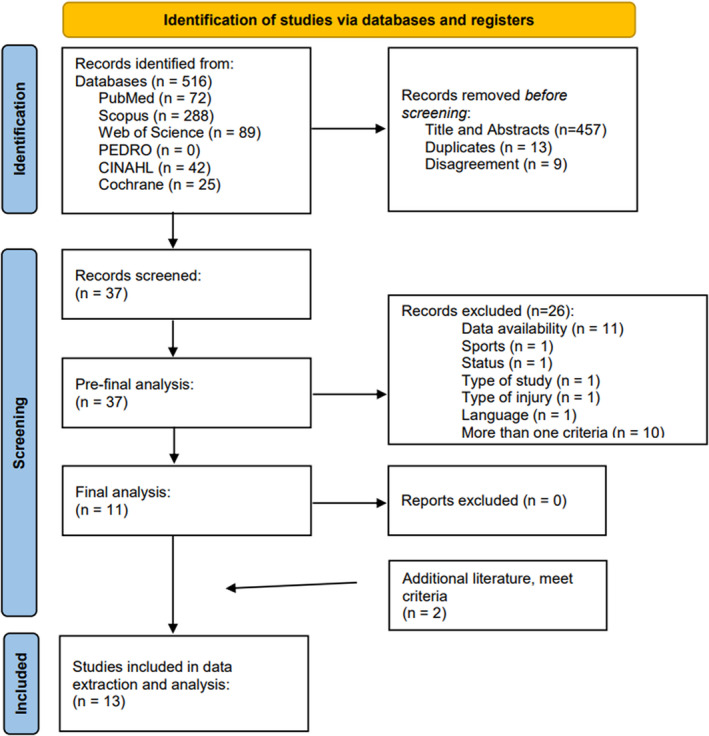
Flow‐Chart recurrence rate
3.2. Characteristics of included studies
3.2.1. Time‐loss
Twelve studies from 8 different countries (England (3), EU (3), Brazil (1), Netherlands (1), Spain (1), Turkey (1), Australia (1), and Germany (1)) were analyzed (Table 1). One out of 12 studies examined elite youth players only 49 ; two out of 12 studies examined both elite youth and professional players. 50 , 51 9 out of 12 studies examined only professionals. Six out of 12 studies made differentiated age statements. Eleven out of 12 studies examined exclusively male football players; one out of 12 studies examined other sports and women in addition to male football players. Data were extractable. All studies included a clear definition of time‐loss.
TABLE 1.
Characteristics of included studies. Recurrence rate
| General study descriptors | Definition of investigated ankle injury | Definition recurrence | Distinction between early and late recurrence (yes/no) | Follow‐up time | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study (Author, Year) | Study Type (Design) | Status | Country | Participants | |||||||
| Number (n) | Sex | Age (years) | |||||||||
| Mean + SD | Range | ||||||||||
| Amer (2020) | Cross‐sectional Study | Professionals + Amateur | Saudi Arabia |
N = 400 (4 Clubs) N = 87 Prof. N = 313 Amateur |
male | 23,2 ± 5,9 | 18–40 (inclusion criteria) | “Ankle Sprain” | n.a. | no | The results of this study (…) reporting ankle sprain once and more than once within the prior 12 months, respectively. |
| Fransz (2018) |
Case Control Study Level of evidence: 3 |
Prof. + Elite Youth | Netherlands | n = 190 | male |
U13: 11,8 ± 0,6 U15: 13,9 ± 0,6 U17: 15,7 ± 0,8 U19: 17,7 ± 0,7 Prof.: 23,2 ± 3,2 |
n.a. | “Ankle Sprains” | n.a. | no | 36 months |
| Gulbrandsen (2019) | Descriptive epidemiological study | College | USA | 17.025 a | male and female | n.a. (“college”) | n.a. | “lateral ligament complex tear” | n.a. | no | 10 year investigation (survey) |
| Hawkins (1999) | Prospective epidemiological study |
Elite Youth Professionals |
England | ? | male | n.a. | n.a. | “ankle / sprain” (data calculated) | n.a. | no | n.a. |
| Jain(2014) | Observational cohort study | Professionals Elite Youth | England |
Overall: n = 67 Prof.: n = 28 |
male |
Youth: n.a. Prof.: 25,1 |
Youth: n.a. Prof.: 19–35 |
“ATFL” | n.a. | no | 4 year period (2007–2011) |
| Pourharib‐Shai (2020) |
Prospective cohort study Level of evidence: 2 |
Professionals | Iran |
Overall: n = 106 N = 58 (football) N = 48 (basketball) |
male | 19,8 ± 4,5 | 15–40 | “Lateral Ankle Sprain” | n.a. | no | Requestion of injury history of the past two years (Risk of bias: self‐reporting) |
| Price (2004) | Prospective epidemiological study | Elite Youth | England | N = 4773 (38 academies) | male | n.a. | 9–19 | “Ankle” (location) and ligamentous sprains “ATFL” | n.a. | no | |
| Roos (2016) | Descriptive epidemiology study | College | USA |
? n.a. |
Male and female |
n.a. (“college”) |
n.a. | “LLC sprains” | n.a. | no | 6 year investigation period (2009–2015) |
| Waldén (2005) | Prospective cohort study | Professionals | Sweden | N = 310 | male | 25 | 17–38 | “Ankle sprain” | “A re‐injury was defined as the same type of injury to the same side and location within 2 months after the final rehabilitation day of the previous injury.” | no | 1 season |
| Waldén (2013) | Prospective cohort study | Professionals | Europe | N = 1743 | male | n.a. | n.a. | “Sprain/ligament injury, lateral” | “Injury of the same type and the same site as an index injury occurring within 2 months after return to full participation from the index injury.” | no | Teams from varying number of seasons from 2001–2012 |
| Woods (2003) | Cohort study | Professionals | England | N = 2376 | male | n.a. | 17–35 | “Anterior talofibular ligament” | n.a. | no | Two competitive seasons (1997–1999) |
| Hägglund (2016) | Cohort study |
EU Top Elite Elite (Prof.) Amateur |
EU + Sweden |
N = 6956 player seasons (Top Elite) N = 2014 player seasons (Elite) N = 241 player seasons (Amateur) |
male |
Top Elite 25,4 ± 4,6 Elite 25,2 ± 4,8 |
n.a. | “Lateral Ankle Sprains” | “Recurrent injury of the same type and at the same side…” |
Yes (not for ankle sprains) |
Top Elite: 14 years (2001–2015) Elite: 9 years (2001–2011) |
| Ekstrand (2020) | Cohort study | Professionals | EU + Sweden, Denmark, England, Norway |
N =? 116 teams (24 countries) |
male | n.a. | n.a. | “Ankle lateral ligament injury” | “A re‐injury was defined as an injury of the same type and location as a previous injury.” | no | 16 years (2001–2017) |
3.2.2. Recurrence rate
Thirteen studies from seven different countries (England (4), Saudi Arabia (1), Netherlands (1), USA (2), Iran (1), Sweden (1), and EU (3)) were analyzed (Table 2). One study 52 examined elite youth players only. 2 of 12 studies included both elite youth players and professional players. Only 2 of 13 studies provided differentiated age data. One study 53 included both professionals and amateurs. 3 of 12 studies 54 , 55 , 56 included other sports: of these, 2 of 3 included women. 54 , 55 Relevant data were extractable from all studies.
TABLE 2.
Characteristics of included studies—Time‐loss
| General study descriptor | Definition of investigated ankle injury | Definition of time‐loss | Definition of severity | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study (Author, Year) | Study Type (Design) | Status | Country | Participants | ||||||
| Number (n) | Sex | Age (years) | ||||||||
| Mean ± SD | Range | |||||||||
| Cezarino (2020) | Descriptive epidemiology study / prospective cohort study | Elite Youth | Brazilian |
N = 228 (total) U11: 23 U12: 22 U13: 25 U14: 28 U15: 28 U16: 25 U17: 28 U18: 16 U20: 33 |
male |
Total: 16.51 ± 2.59 U11: 11.23 ± 0.11 U12: 12.17 ± 0.62 U13: 13.20 ± 0.55 U14: 13.73 ± 3.16 U15: 15.33 ± 0.38 U16: 16.35 ± 0.36 U17: 17.19 ± 0.54 U18: 18.05 ± 0.49 U20: 18.31 ± 2.59 |
n.a. | “Foot / ankle sprain” | “A player was considered injured until the team's medical staff indicated that he could be fully involved in training and was available for match selection.” | “Injury severity was defined according to the number of days lost by the player between the day of the injury and return to full participation in team training and match play. For different categories were used: minimal (o‐1 days lost), mild (4–7 days lost), mild (4–7 days lost), moderate (8–28 days lost) or severe (>28 days lost).” |
| Fuller (2006) | Cohort study | Professionals | England | N = 55 | male | n.a. | 20–34 | “Ankle Sprains” | “Players were considered to be fit to return to normal team training and competition when they had achieved a 100% recovery score.” | n.a. |
| Fransz (2018) |
Case control study Level of evidence: 3 |
Professionals Elite Youth |
Netherlands | N = 190 | male |
U13: 11.8 ± 0.6 U15: 13.9 ± 0.6 U17: 15.7 ± 0.8 U19: 17.7 ± 0.7 Prof.: 23.2 ± 3.2 |
n.a. | “Ankle Sprains” | “… we considered the number of days that the player was unfit to participate in training or matches after the sprain as a measure of injury severity.” | “… we considered the number of days that the player was unfit to participate in training or matches after the sprain as a measure of injury severity.” |
| Larruskain (2017) | Prospective cohort study | Professionals (First Division) | Spain |
Male: n = 50 Female: n = 35 |
male and female |
Male: 25 ± 4 Female: 25 ± 5 |
n.a. |
“Ligament injury” “Lateral sprain” |
“…unable to participate in future training session or match due to a physical complaint resulting from football training or match play and was considered injured until the medical staff cleared the player for full participation in training and match play.” | “According to the number of days lost, injury severity was recorded as minimal (1–3 days), mild (4–7 days), moderate (8–28 days) and severe (>28 days.” |
| Oztekin (2009) | Retrospective cohort study | Professionals (registered with the National Football Association of Turkey) | Turkey | N = 200 (n = 66 ankle injuries) | male | 23 | 17–31 |
“ATFL sprain” “C/F ligament sprain” |
“Time lost from participation was calculated from our own medical records and confirmed by telephone interviews.” | “Injury severity was defined as days unable to play, and was classified as minor (1–7 days absent from play), moderate (8–28 days absent from play) and severe (>28 days absent from play.)” |
| Whalan (2019) | Descriptive epidemiological study/Prospective cohort study | Sub‐elite | Australia |
N = 1049 (n = 25 sub‐elite Clubs) |
male | 24.3 ± 6.2 | n.a. | “Ankle ligament sprain” |
“Injury that results in a player being unable to fully participate in matches or training. Payers were deemed to have recovered from injury once they had returned to full training / match participation or were considered eligible for team selection.” |
n.a. |
| Waldén (2013) | Prospective cohort study | Professionals | Europe | N = 1743 | male | n.a. | n.a. | “Sprain/ligament injury, lateral” | “…players were considered injured until the club medical staff allowed full participation in training and availability for match selection.” |
Slight / minimal: Injury causing 0–3 days lay‐off Mild injury: Injury causing 4–7 days lay‐off Moderate injury: Injury causing 8–28 days lay‐off Severe injury: Injury causing >28 days lay‐off |
| Jain (2014) | Observational cohort study |
Professionals Elite Youth |
England |
Overall: n = 67 Prof.: n = 28 2nd team: n = 18 Youth: n = 21 |
male |
Youth: n.a. Prof.: 25.1 |
Youth: n.a. Prof.: 19–35 |
“ATFL” |
“Injuries defined as an injury that prevented a player being available for selection for at least 5 days. The end oft he injury episode was taken when player was declared as fit for full training or for selection in a match by the medical staff.” | n.a. |
| Woods (2003) | Cohort study | Professionals | England | N = 2376 | male | n.a. | 17–35+ |
“Anterior talofibular” |
“A recordable injury was defined as one sustained during training or competition and which prevented player from participation in normal training or competition for more than 48 hours (not including the day of injury).” | n.a. |
| Ekstrand (2013) | Prospective cohort study | Professionals |
Europe (10 countries) |
N = 1743 (27 teams) |
male | n.a. | n.a. | “Ankle sprain, lateral” | “The payer was considered injured until the team medical staff allowed full participation in training and availability for match selection.” |
“Injuries were categorized under four degrees of severity based on the number of days absent. All injuries were followed until the final day of rehabilitation.” Sligh / minimal injury: Injury causing 0–3 days´ absence from training and match play. Mild injury: Injury causing 4–7 days´ absence from training and match play. Moderate injury: Injury causing 8–28 days´ absence from training and match play. Severe injury: Injury causing more than 28 days´ absence from training and match play. |
| Ekstrand (2020) | Cohort study | Professionals | EU + England, Sweden, Denmark Norway |
N =? 116 teams 449 team‐seasons |
male | n.a. | n.a. | “Ankle lateral ligament injury” | “A player's period of absence following an injury constituted the full period (number of days) between the when he the player was forced to discontinue his football participation due to an injury until the date when the medical team allowed the player to return to full participation.” | “… mild (leading to a median absence of 7 days or less)… or moderate (median absence: 7–28 days)…severe (median absence >28 days.” |
| Krutsch (2021) |
Prospective cohort study Level of evidence: 2 |
Professionals |
Germany (1st Bundesliga) | N = 660 | male |
At injury: 26.3 ± 4.0 |
17.6–38.6 | “Lateral ligament rupture, ankle” | n.a. | “…The analysis of included injury types that resulted in absence from official football matches of at least 28 days and were therefore categorized as ‘severe’…” |
3.3. Results of individual studies for all outcome parameters
3.3.1. Time‐loss
The overall sample size derived from 12 studies is 7736 participants. Two studies do not provide clear information on the sample size. 57 , 58 Of the 7736 participants, 7701 were male, 35 were female. 6054 participants were professionals (male: 6019; female: 35), 443 elite youth players and 1049 semi‐professionals (Table S1).
35,888 overall injuries were recorded of which 4848 (13.5%) were ankle injuries. Of these 4848 overall ankle injuries, 3370 were ankle sprains (69.5%): 3299 ankle sprains occurred in professionals, 71 ankle sprains in elite youth players (47 ankle sprains in the target older age groups). Therefore, a total of 3346 ankle sprain injuries were included in the statistical calculation.
All studies indicate the time‐loss as “mean”. Five of 12 studies report both mean and median. No study reports only the median, one study reports “average”. Each study clearly defines time‐loss. In two of 12 studies, 57 , 58 no clearly differentiated age information is given.
3.3.2. Recurrence rate
The overall sample size of the 13 studies is 36,201 participants (male: 29,941; female: 9260). Of these, 30,669 were professionals (84.7%), 4979 elite youth players (13.7%) and 554 amateurs (1.5%).
44,404 initial injuries of all anatomical areas were registered, of which 6587 were recurrences (14.8%). Of 40,905 initial injuries, 5966 recurrences occurred in male athletes. 158 recurrences of 1756 initial injuries were recorded in female athletes.
27,174 injuries and 3496 recurrences occurred in professionals (12.8%), 780 initial injuries and 137 recurrences in elite youth players (17.5%) and 7 initial in amateurs. Data on recurrence for amateurs were not available. A total of 7944 initial ankle sprain injuries and 1193 ankle sprain recurrences were identified from all groups, genders, and age groups. Of these, 4893 initial and 748 recurrences were meta‐analytically calculated in 16,442 football players (Table 3).
TABLE 3.
Results—Recurrence rate
| Study | Participants | Injuries |
Data (extracted) for Meta‐Analysis |
|||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size (n) (overall) | Sex | Status / Age | Number of injuries (overall) | Number of AS (overall) | Sex (overall) | Status / Age (overall) | Status / Age (only AS injury) | |||||||||||||||||||
| male | Fem. | Prof. (n) | EY (n) | Am. | Prof. (n) | EY (n) | ||||||||||||||||||||
| Male (n) | Fem. (n) | Prof. (n) | EY (n) | Am (n) | Init. | Rec. | Init. | Rec. | Init. | rec | Init. | Rec. | Init. | Rec. | Init. | Rec. | Init. | Rec. | Init. | Rec. | Init. | Rec. | Init. | Rec. | ||
| Amer (2020) | 400 | 400 | 0 | 87 | 0 | 313 | 87 | 36 | 87 | 36 | 87 | 36 | 0 | 0 | 87 | 36 | 0 | 0 | n.a. | n.a. | 87 | 36 | 0 | 0 | 87 | 36 |
| Fransz (2018) | 190 | 190 | 0 | 24 | 166 | 0 | 45 | 10 | 45 | 10 | 45 | 10 | 0 | 0 | 0 | 0 | 45 | 10 | 0 | 0 | 3 | 0 | 18 | 6 | 21 | 6 |
| Gulbrandsen (2019) | 17,025 | 7765 | 9260 | 17,025 | 0 | 0 | 2068 | 297 | 1358 | 297 | 984 | 139 | 1084 | 158 | 984 | 139 | 0 | 0 | 0 | 0 | 617 | 137 | 0 | 0 | 617 | 139 |
| Hawkins (1999) a | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | 125 | 31 | 95 | 31 | 95 b | 31 | 0 | 0 | 23 | n.a. | 8 | n.a. | 0 | 0 | n.a. | n.a. | n.a. | n.a. | 95 | 31 |
| Jain (2014) | 67 | 67 | 0 | 28 | 40 | 0 | 45 | 11 | 14 | 4 | 45 | 11 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | n.a. | n.a. | n.a. | n.a. | 14 | 4 |
| Pourgharib‐Shai (2020) | 106 | 106 | 0 | 106 | 0 | 0 | 30 | 20 | 30 | 20 | 30 | 20 | 0 | 0 | 30 | 20 | 0 | 0 | 0 | 0 | 30 | 6 | 0 | 0 | 30 | 6 |
| Price (2004) a | 4773 | 4773 | 0 | 0 | 4773 | 0 | 727 c | 127 | 523 c | 91 c | 727 | 127 | 0 | 0 | 0 | 0 | 727 | 127 | 0 | 0 | 0 | 0 | 523 | 91 | 523 | 91 |
| Roos (2016) a | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | 2429 | 289 | 2429 | 289 | 756 | n.a. | 672 | n.a. | 143 | 20 d | 0 | 0 | 0 | 0 | 143 | 20 | 0 | 0 | 143 | 20 |
| Waldén (2005) | 310 | 310 | 0 | 310 | 0 | 0 | 765 | 180 | 53 e | 6 e | 53 | 6 | 0 | 0 | 53 | 6 | 0 | 0 | 0 | 0 | 53 | 6 | 0 | 0 | 53 | 6 |
| Waldén (2013) | 1743 | 1743 | 0 | 1743 | 0 | 0 | 1080 | 121 | 552 | 38 | 1080 | 121 | 0 | 0 | 1080 | 121 | 0 | 0 | 0 | 0 | 552 | 38 | 0 | 0 | 552 | 38 |
| Woods (2003) a | 2376 | 2376 | 0 | 2376 | 0 | 0 | 1011 | n.a. | 677 | 61 f | 1011 | n.a. | 0 | 0 | 1011 | n.a. | 0 | 0 | 0 | 0 | 677 | 61 | 0 | 0 | 677 | 61 |
| Hägglund (2016) | 9211 | 9211 | 0 | 8970 | 0 | 241 | 13,050 | 2449 | 821 | 138 | 13,050 | 2449 | 0 | 0 | 821 | 138 | 0 | 0 | 7 | n.a. | 821 | 138 | 0 | 0 | 821 | 138 |
| Ekstrand (2020) |
n.a. (116 teams) |
n.a. | n.a. | n.a. | n.a. | n.a. | 22,942 | 3016 | 1260 | 172 (13.7%) | 22,942 | 3016 | 0 | 0 | 22,942 | 3016 | 0 | 0 | 0 | 0 | 1260 | 172 | 0 | 0 | 1260 | 172 |
| Total | 36,201 | 26,941 | 9260 | 30,669 | 4979 | 554 | 44,404 | 6587 | 7944 | 1193 | 40,905 | 5966 | 1756 | 158 | 27,174 | 3496 | 780 | 137 | 7 | n.a. | 4243 | 614 | 541 | 97 | 4893 | 748 |
Abbreviations: Am, Amateur; AS, Ankle Sprain; EY, Elite Youth; Fem., female; Init., initial; n.a., not available; Prof., Professionals; rec., recurrence.
Missing data were calculated.
Hawkins (1999): 76% out of 125 = 95.
Price (2004): 19% out of all injuries = 727; 72% out of 727 = 523 ankle sprains; 72% out of 127 re‐injuries = 91 re‐injuries (ankle sprains).
Roos (2016): 14% out of 143 = 20; only includes sports in which both sexes participated.
Waldén (2005): 99 sprains; out of 99 sprains were 54% ankle sprains (=53 ankle sprains); 11% out of 53 were recurrent (n = 6).
Woods (2003): “re‐injury rate of AS was 9%”; 9% out of 677 = 61.
Four of 13 studies clearly define the “recurrence rate”. Only one of 13 studies distinguishes between “early” and “late” recurrence. No study distinguishes between “recurrence rate” and “exacerbation”.
3.4. Risk of bias/quality assessment
3.4.1. Time‐loss
None of the included studies were of low quality. While 4 out of 12 (33%) were of moderate quality, 25 , 50 , 59 , 60 8 out of 12 (66%) were of high quality. 24 , 49 , 51 , 57 , 58 , 61 , 62 , 63
3.4.2. Recurrence rate
Four out of 13 (31%) of the studies were of moderate quality. 26 , 50 , 52 , 53 Eight out of 13 (61%) showed high quality. 24 , 27 , 31 , 51 , 54 , 55 , 56 , 57 For one study (1 out of 13, 8%) no agreement could be reached on the assessment. 25
There is a trend towards improved quality assessment through the introduction of recording recommendations. Appendix S5 summarizes the results of the methodological quality assessment.
4. META‐ANALYSIS
4.1. Statistical analysis
4.1.1. Data extraction
Recurrence rate
Thirteen studies were included in the meta‐analysis as shown in Figures 3 and 4. A sample size of 16,442 players (male, age > 16 years – professionals) was determined in these 13 studies. Four of the 13 studies provide accurate age data for a total of 9587 players. The mean age of this sample is 25.12 (SD = 4.67) years. These 13 studies included a total of 4893 ligament ankle sprains, of which 748 were recurrent injuries. Meta‐analytically, a mean and pooled weighted recurrence rate based on the random‐effects model of 17.11% (95% CI: 13.31%–20.92%; df = 12; Q = 19.53; I2 = 38.57%) was calculated. We found moderate heterogeneity (I2 = 38.57%).
FIGURE 3.
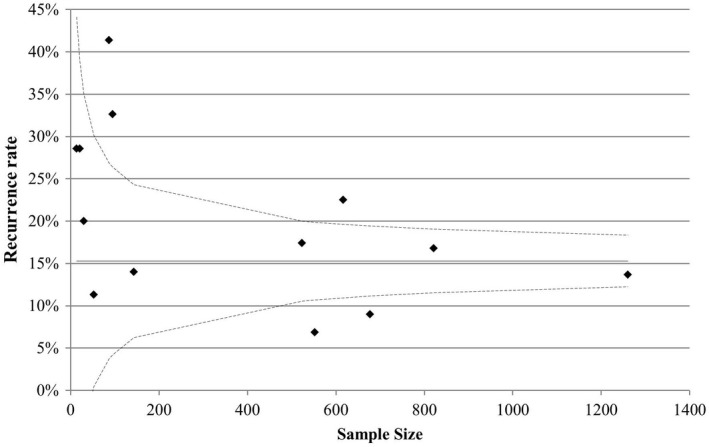
Funnel Plot Recurrence rate
FIGURE 4.
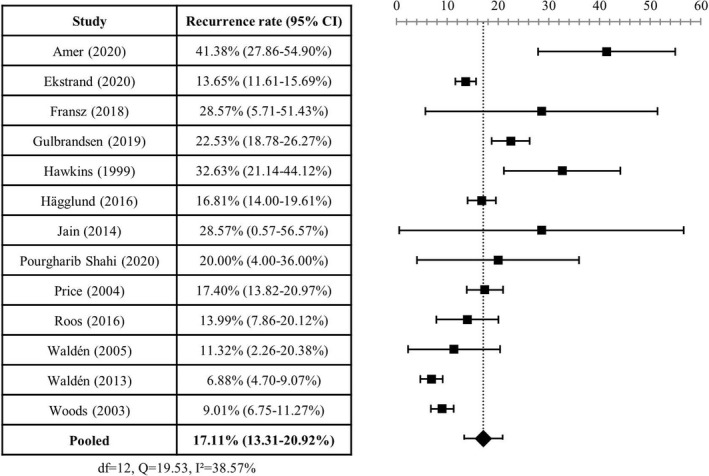
Forrest Plot Recurrence rate
Time‐Loss
Twelve studies were included in the meta‐analysis. A sample size of 7293 players (male, age > 16 years – professionals) was determined in these 12 studies. Six of 12 studies included specific age data for a total of 2013 (1849 professional; 164 elite youth) players. The average age determined is 23.91 (SD = 4.99) years. An a priori assessment of heterogeneity found “considerable heterogeneity” (20.11 days; 95%CI 18.15–22.08; df = 11; Q = 158.19; I2 = 93.05%). Due to “considerable heterogeneity” we decided to perform descriptive statistics for the time‐loss outcome parameter. There were 3346 ankle sprains (Professionals: 3299; Elite Youth: 47) in the 12 included studies. We found the weighted mean time‐loss is 15.92 days (median: 14.95; minimum: 9.55; maximum: 52.9).
5. DISCUSSION
To our knowledge, this is the first systematic review to explicitly examine the time‐loss and recurrence rate after lateral ankle ligament injuries in professional football players. The overall aim of this systematic review was to determine time‐loss and recurrence rates after LAS in elite football players. Among other things, these can serve as outcome parameters for testing the effectiveness of future rehabilitation concepts.
5.1. Main findings
5.1.1. Time‐loss
We determined an average time‐loss of 15.92 days (MD: 14.95; Min: 9.55; Max: 52.9) following lateral ankle ligament injury. Even though only one of the included studies 58 explicitly investigated severe injuries (ruptures), it should be critically noted that wound healing of the ligaments is still incomplete with time losses of about 15 days, 44 especially for higher grade ankle sprains with structural damage. Ligaments need adequate tissue loading in rehabilitation training sessions for remodeling and maturation to attain adequate stability. 64 On the one hand, this physiological process is time‐based and unlikely to be complete with time‐loss of 15 days leading to professional football players returning to competitive sport with incomplete healing of the ligament structures. On the other hand, this highlights the need for criteria‐based functional rehabilitation which should be independent of time. Time‐loss of 15 days raises doubts as to whether the duration of the rehabilitation period is sufficient to gradually restore sport‐specific function to pre‐injury levels. Athletes should not return to sport until specific criteria are met and original movement patterns are restored. Compensatory movement behavior due to unhealed injuries by an insufficient rehabilitation period are risk factors for secondary injuries. 65
Therefore, approaches to functional rehabilitation based on specific criteria fulfillment for RTC were developed for knee and muscle injuries. 66 , 67 , 68 , 69 Such approaches are still lacking for ankle injuries. 70 , 71 In this context, the use of pain‐relieving drugs for the fastest possible RTC should also be critically discussed. Neither subjectively reported absence of pain nor time should be decisive factors in determining RTC.
5.1.2. Recurrence rate
We determined a recurrence rate of lateral ankle ligament injury in competitive football players of 17%. Even though this is a higher recurrence rate of ACL injuries (9%–12%) in professional football, 27 , 72 , 73 a major focus of research was on ACL injuries in the past. Thus, there is a need to fill the gap in research of LAS, especially in the question of reasons for the high rate of recurrent ankle injuries in professional football players. In addition to a possible insufficient healing time (cf. time‐loss), healing and tissue stability, the causes of high recurrence rates can be suspected in neuro‐plastic alterations. Injuries change the movement pattern at the cortico‐spinal level and influence postural control mechanisms. 74 , 75 , 76 This could affect protective mechanisms to prevent further trauma (e.g., prolonged latency). 77 , 78 This could explain why a previous injury is one of the greatest risk factors for a subsequent injury. 30 We could not identify in this review whether the recurrences occurred at an early or late time point. However, morphologic alterations in axons at early time points after injury have been described. 75 Thus, with knowledge of the timing of recurrent injuries, more specific prevention programs could be developed based on neuroplastic research findings. Longer rehabilitation periods after ACL injuries, however, offer the possibility to gradually eliminate deficits and to restore original movement pattern.
Ankle injuries are often trivialized. 79 Financial pressures can lead to athletes and medical staff encounter severe pressure from the club's management and coaching staff to return athletes to play as quick but may not be as safe as possible. Coaching staff is pressured to succeed and to win titles. Thus, coaches may put pressure on athletes to risk their own health and long‐term consequences for short‐term success. 80 This often leads to conflicting situations between medical staff and head coaches. 81 Head coach’s leadership style and trustworthy internal communication between the medical team and the head coach are important factors in reducing injury risk. Teams with high internal communication quality had lower injury rates and higher player availability than teams with low communication quality. 82 This could explain the connection between the short duration of absence and the increased recurrence rate for these injuries, especially since every form of injury must be considered a “systemic injury” with consequences at the cortical level (e.g., altered movement pattern).
On the one hand, Ekstrand 63 , 83 describes a decreasing trend in the occurrence and recurrence rate for all types of injuries as well as for ligament injuries in elite football players. However, our review could not confirm this decreasing trend for ankle ligament injuries. The authors attribute the decreasing trend, among other things, to improved treatment and rehabilitation concepts. Nevertheless, the recurrence rate of 17% after LAS appears high. Recurrence rates above the initial injury rate should give rise to discussion and, despite improved rehabilitation measures, the effectiveness of current rehabilitation concepts should be questioned especially in supposedly minor low‐grade ankle sprains. Malliaropooulos 84 shows in his study that in particular low‐grade ankle sprains show high recurrence rates. They ascribe this, among other things, to the trivialization of the injury and the insufficient duration of rehabilitation. Rehabilitation is mostly still time‐based and controlled by the experience of the physician and therapist. Although guidelines for RTC decisions have been developed in the past, 85 there are currently few criteria‐based step‐by‐step approaches to guide the rehabilitation.
Reducing recurrence rates after LAS has benefits for many stakeholders (player, team, club): injury‐free teams are proven to be more successful. 41 The availability of key players, in particular, can determine matches, and thus, the outcome of the standings (table position) and, ultimately, promotion or relegation. A correlation between injury‐related time‐loss and costs incurred has been identified both globally 43 and specifically in relation to ankle injury. 86 For professional players, a repeatedly long period of time‐loss often means fewer practice and a possible loss of their regular place, which is often accompanied by significant decrease of their market value and may put players into disadvantageous negotiating positions for new contracts.
5.2. Reporting quality/reporting bias
We used a modified form of the STROBE guidelines to assess the reporting quality of included studies. 46 , 87 The majority of studies were of moderate to high reporting quality. More recent studies published after the establishment of consensus agreements on data recording tended to have better reporting quality. This could indicate the successful establishment of uniform recording recommendations through consensus statements. Nevertheless, the original STROBE assessment appears to be suitable only to a limited extent, since not all of the 22 items or their sub‐items appear to be suitable for assessing the reporting quality of individual questions of systematic reviews. The use of a pure sum score to assess the quality of reporting seems unsuitable, as individual items can have different importance. This approach is quite imprecise. Nevertheless, it offers an approximation for assessing the reporting quality of included studies. Critically, it should be noted that the procedure refers purely to the assessment of reporting and does not represent a report on the methodological quality of the study itself. 88 , 89 Even methodologically poorly conducted studies can be well reported, and vice versa. Nevertheless, modified STROBE guidelines are obviously also indirectly suitable for assessing study quality. 89 The lack of a quality assessment for observational studies led us to develop our own approach. Therefore, we decided on a “range‐solution”. Various systematic reviews use modified versions for quality assessment. 22 , 23 , 47 This indicates the need for future development of specific assessment methods to assess quality of observational studies.
5.2.1. Confounder of reporting
We were able to identify only a few studies from which we could determine the time‐loss or recurrence rates after lateral ligament injuries of the ankle in professional football players. This finding confirms the results of Lopez‐Valenciano et al., 23 who found it was not feasible to conduct a subgroup analysis on the time‐loss of different types of injuries in professional football due to a lack of data. In addition, the heterogeneous data situation of non‐uniform recording methods makes the comparability of individual study results difficult. For this reason, eleven consensus papers on processes of homogeneous data collection have been produced since 2005 in order to establish better reporting standards for epidemiological studies in the future. 90 , 91
Subgroup analysis
Only a few of the included studies (time‐loss 6/12; recurrence rate 2/13) provide specific age information, so that we could not conduct a subgroup analysis of the outcome parameters (time‐loss; recurrence rate) between professionals and elite youth players. Thus, future studies should present differentiated information on age. An overview of injury occurrence (e.g., exposure, prevalence, incidence, recurrence rate, time‐loss, and severity) of different age cohorts can help to detect injury patterns at certain career points and to develop target‐oriented prevention programs. Originally, we planned a differentiated subgroup analysis of different ankle ligaments. However, only a few studies (recurrence: 2/13; time‐loss: 3/12) present data of interest of different lateral ligamentous structures, so we could not perform a subgroup analysis of specific ligament structures. Future studies should also provide information on anatomical structures to specific time‐loss for individual ligaments to improve prevention for reduction of recurrence rates.
Inconsistent definitions
Inconsistent definitions make it difficult to compare study results: while 12 out of 12 studies described a clear definition for time‐loss, only 4 of 13 studies clearly defined “recurrence”. This reporting bias can lead to inconsistent results and should be taken into account when interpreting the results of this review. This finding highlights the need for uniform definitions in the future for comparability of results. Similarly, only one study 31 differentiate between “early” and “late” recurrence: by knowing more precisely the timing of recurrence, more effective prevention strategies could be developed that take into account vulnerable phases. The timing of vulnerable phases for recurrence appears to be better researched in ACL injuries, among others. 92 , 93 , 94
Exacerbation versus recurrence
No study differentiates between “exacerbation” or “recurrence”: future studies focusing on issues of recurrent injury causation should also include sub‐categories of recurrence and exacerbation to ultimately establish better RTC decision models. 95 Inclusion of exacerbation‐category specified data. Accordingly, a re‐injury suffered during rehabilitation before the RTC would not be recorded as a “recurrence” but as an “exacerbation”. This definition implies a possible prolonged time‐loss and should be critically considered under this aspect. Nevertheless, an integration of this sub‐category (“exacerbation”) seems advisable. This should initially be integrated additionally in future studies so that the data on existing studies remain comparable.
6. STRENGTHS
This systematic review followed a clear methodological approach based on the current PRISMA guidelines, 45 it was registered on PROSPERO prior to literature searching and at least two authors (ZF, KH) assessed relevant data independently.
A strength of this systematic review lies in the specificity: we included only studies that provide data on time‐loss and recurrence rates of lateral ankle ligament injuries in male professional football players. Many studies present the data non‐specifically by location (“ankle”). Based on the aim to specifically investigate lateral ligament injuries, we excluded studies of a global presentation (“ankle”).
Another strength is the large sample size of participants and injuries examined for both time‐loss and recurrence rate, which makes the results of this systematic review very robust.
7. LIMITATIONS
Despite following the latest PRISMA guidelines and PROSPERO registration, there were still some limitations of our systematic review. Firstly, we included some studies that did not clearly define age or status. Data on elite or professionals classified participants as “adults”. We also classified college athletes as “professionals”. Secondly, as it is often not possible to differentiate between different ligamentous ankle injuries from the study data, we included all types of ankle sprains based on the knowledge that approximately 75%–90% of all ankle sprains affect the lateral ligaments. 24 , 25 , 26 In contrast to what was registered on PROSPERO, we also included studies that did not (or did not clearly) define “recurrence”. Adhering to this criterion would have drastically reduced the number of studies for the analysis. On a rather critical note, the overall comparability is limited due to the lacking definition of “recurrence”. It should also be considered that we only included study data from male professional football players, so that our results are not generalizable to other cohorts (e.g., female, amateur, non‐elite, younger age) and the results must be interpreted within this context.
8. PERSPECTIVE
The results of this systematic review on time‐loss and recurrence rate can be used as outcome parameters to evaluate the effectiveness of existing concepts. On the one hand, practitioners can use them as “guideline values” to evaluate their own approaches. On the other hand, the results can be helpful in convincing athletes and especially coaches of the need for adequate function‐based rehabilitation, even though this may mean a potentially longer rehabilitation period. In particular, coaches are pushing for an early return of their key players. The risk of re‐injury with the knowledge that a subsequent injury means not only a renewed but mostly also prolonged time‐loss, can be a strong argument towards coaches for accepting a longer rehabilitation period, especially if they push (also being under external pressure) for an early RTC. Elite youth players in particular should not return to competition with physiologically unhealed ligament structures, which is a major responsibility for medical teams.
Finally, researchers can use the results of this systematic review of the outcome parameters as a basis for prospective planning and evaluation of the effectiveness of future rehabilitation concepts.
9. CONCLUSION
Lateral ankle ligament injuries are one of the most common types of injury in professional football. The time‐loss averages 15 days and is thus below the necessary time for physiological wound healing. The high recurrence rate of 17% raises the question whether the duration of the rehabilitation period is sufficient to gradually restore sport‐specific function to pre‐injury levels. These findings highlight the need for criteria‐based rehabilitation concepts. Data on time‐loss and recurrence rate can be used as outcome parameters to evaluate the effectiveness of rehabilitation algorithms, based on this systematic review's result. Nevertheless, the heterogenous data recording of individual studies complicates the general comparability of the study results which highlights the need for future homogenous data recording in football injury studies.
AUTHOR CONTRIBUTIONS
ZF and KH selected the studies. KDC decided in case of disagreements. ZF extracted and analyzed the data, was responsible for conception and design, and drafted the manuscript. KH and KDC revised the manuscript. All authors commented on the paper and approved the final version.
FUNDING INFORMATION
There are no funders to report for this submission.
CONFLICT OF INTEREST
There are no competing interests for any author.
PATIENT INVOLVEMENT
The study does not involve identifiable patients.
Supporting information
Appendix S1
Appendix S2
Appendix S3
Appendix S4
Appendix S5
Table S1
ACKNOWLEDGMENTS
There is no special acknowledgment to mention.
Flore Z, Hambly K, De Coninck K, Welsch G. Time‐loss and recurrence of lateral ligament ankle sprains in male elite football: A systematic review and meta‐analysis. Scand J Med Sci Sports. 2022;32:1690‐1709. doi: 10.1111/sms.14217
PROSPERO: CRD42020201577.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Clark RC, Saxion CE, Cameron KL, Gerber JP. Associations between three clinical assessment tools for postural stability. N Am J Sports Phys Ther. 2010;5(3):122‐130. [PMC free article] [PubMed] [Google Scholar]
- 2. Zech A, Hübscher M. Sensomotorisches training zur prävention von sprunggelenksverletzungen. Dtsch Z Sportmed. 2012;63:5‐8. doi: 10.5960/dzsm.2011.060 [DOI] [Google Scholar]
- 3. Richie D, Izadi F. Return to play after an ankle sprain: guidelines for the podiatric physician. Clin Podiatr Med Surg. 2015;32(2):195‐215. doi: 10.1016/j.cpm.2014.11.003 [DOI] [PubMed] [Google Scholar]
- 4. Hertel J, Corbett R. An updated model of chronic ankle instability. J Athl Train. 2019;54(6):572‐588. doi: 10.4085/1062-6050-344-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sman A, Hiller C, Rae K, et al. Predictive factors for ankle syndesmosis injury in football players: a prospective study. J Sci Med Sport. 2014;17(6):586‐590. doi: 10.1016/j.jsams.2013.12.009 [DOI] [PubMed] [Google Scholar]
- 6. Fong DT, Chan YY, Mok KM, Yung PS, Chan KM. Understanding acute ankle ligamentous sprain injury in sports. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:14. doi: 10.1186/1758-2555-1-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Petersen W, Rembitzki IV, Koppenburg AG, et al. Treatment of acute ankle ligament injuries: a systematic review. Arch Orthop Trauma Surg. 2013;133(8):1129‐1141. doi: 10.1007/s00402-013-1742-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kaminski TW, Hertel J, Amendola N, et al. National Athletic Trainers' association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013;48(4):528‐545. doi: 10.4085/1062-6050-48.4.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains [published correction appears in am fam physician 2001 Aug 1;64(3):386]. Am Fam Physician. 2001;63(1):93‐104. [PubMed] [Google Scholar]
- 10. Melam G, Alhusaini A, Perumal V, Buragadda S, Kaur K. Comparison of static and dynamic balance between football and basketball players with chronic ankle instability. Saudi J Sports Med. 2016;16:199‐204. [Google Scholar]
- 11. Brunner R, Friesenbichler B, Casartelli NC, Bizzini M, Maffiuletti NA, Niedermann K. Effectiveness of multicomponent lower extremity injury prevention programmes in team‐sport athletes: an umbrella review. Br J Sports Med. 2019;53(5):282‐288. doi: 10.1136/bjsports-2017-098944 [DOI] [PubMed] [Google Scholar]
- 12. Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73‐94. doi: 10.2165/00007256-200737010-00006 [DOI] [PubMed] [Google Scholar]
- 13. Steib S, Pfeifer K. Beeinträchtigungen der sensomotorischen Kontrolle bei funktioneller Sprunggelenkinstabilität [sensorimotor deficits in functional ankle instability]. Z Orthop Unfall. 2015;153(3):253‐258. doi: 10.1055/s-0034-1396293 [DOI] [PubMed] [Google Scholar]
- 14. Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553‐558. doi: 10.1136/bjsm.2009.060582 [DOI] [PubMed] [Google Scholar]
- 15. Hägglund M, Waldén M, Ekstrand J. Injuries among male and female elite football players. Scand J Med Sci Sports. 2009;19(6):819‐827. doi: 10.1111/j.1600-0838.2008.00861.x [DOI] [PubMed] [Google Scholar]
- 16. Stubbe JH, van Beijsterveldt AM, van der Knaap S, et al. Injuries in professional male soccer players in The Netherlands: a prospective cohort study. J Athl Train. 2015;50(2):211‐216. doi: 10.4085/1062-6050-49.3.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Luig P, Bloch H, Burkhardt K, Klein C, Kühn N. VBG‐Sportreport 2018 – Analyse des Unfallgeschehens in den zwei höchsten Ligen der Männer: Basketball, Eishockey, Fußball und Handball. VBG; 2018. [Google Scholar]
- 18. Hawkins RD, Hulse MA, Wilkinson C, Hodson A, Gibson M. The association football medical research programme: an audit of injuries in professional football. Br J Sports Med. 2001;35(1):43‐47. doi: 10.1136/bjsm.35.1.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Morgan B, Oberlander M. An examination of injuries in major league soccer. The inaugural season. Am J Sports Med 2001;29(4):426–30. doi: 10.1177/03635465010290040701, 430. [DOI] [PubMed] [Google Scholar]
- 20. Hägglund M, Waldén M, Ekstrand J. Injury incidence and distribution in elite football‐‐a prospective study of the Danish and the Swedish top divisions. Scand J Med Sci Sports. 2005;15(1):21‐28. doi: 10.1111/j.1600-0838.2004.00395.x [DOI] [PubMed] [Google Scholar]
- 21. Luig P, Bloch H, Burkhardt K, et al. VBG‐Sportreport 2016 – Analyse des Unfallgeschehens in den zwei höchsten Ligen der Männer: Basketball, Eishockey, Fußball und Handball. VBG; 2016. [Google Scholar]
- 22. Klein C, Henke T, Platen P. Injuries in football (soccer)—a systematic review of epidemiology and aetiological aspects. Ger J Exerc Sport Res. 2018;48:309‐322. doi: 10.1007/s12662-018-0530-3 [DOI] [Google Scholar]
- 23. López‐Valenciano A, Ruiz‐Pérez I, Garcia‐Gómez A, et al. Epidemiology of injuries in professional football: a systematic review and meta‐analysis. Br J Sports Med. 2020;54(12):711‐718. doi: 10.1136/bjsports-2018-099577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Waldén M, Hägglund M, Ekstrand J. Time‐trends and circumstances surrounding ankle injuries in men's professional football: an 11‐year follow‐up of the UEFA champions league injury study. Br J Sports Med. 2013;47(12):748‐753. doi: 10.1136/bjsports-2013-092223 [DOI] [PubMed] [Google Scholar]
- 25. Woods C, Hawkins R, Hulse M, Hodson A. The football association medical research programme: an audit of injuries in professional football: an analysis of ankle sprains. Br J Sports Med. 2003;37(3):233‐238. doi: 10.1136/bjsm.37.3.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hawkins R, Fuller C. A prospective epidemiological study of injuries in four English professional football clubs. Br J Sports Med. 1999;33(3):196‐203. doi: 10.1136/bjsm.33.3.196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Waldén M, Hägglund M, Ekstrand J. Injuries in Swedish elite football‐a prospective study on injury definitions, risk for injury and injury pattern during 2001. Scand J Med Sci Sports. 2005;15(2):118‐125. doi: 10.1111/j.1600-0838.2004.00393.x [DOI] [PubMed] [Google Scholar]
- 28. Waldén M, Hägglund M, Ekstrand J. UEFA champions league study: a prospective study of injuries in professional football during the 2001‐2002 season. Br J Sports Med. 2005;39(8):542‐546. doi: 10.1136/bjsm.2004.014571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lüthje P, Nurmi I, Kataja M, et al. Epidemiology and traumatology of injuries in elite soccer: a prospective study in Finland. Scand J Med Sci Sports. 1996;6(3):180‐185. doi: 10.1111/j.1600-0838.1996.tb00087.x [DOI] [PubMed] [Google Scholar]
- 30. Hägglund M, Waldén M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40(9):767‐772. doi: 10.1136/bjsm.2006.026609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hägglund M, Waldén M, Ekstrand J. Injury recurrence is lower at the highest professional football level than at national and amateur levels: does sports medicine and sports physiotherapy deliver? Br J Sports Med. 2016;50(12):751‐758. doi: 10.1136/bjsports-2015-095951 [DOI] [PubMed] [Google Scholar]
- 32. Hägglund M, Waldén M, Ekstrand J. Lower reinjury rate with a coach‐controlled rehabilitation program in amateur male soccer: a randomized controlled trial. Am J Sports Med. 2007;35(9):1433‐1442. doi: 10.1177/0363546507300063 [DOI] [PubMed] [Google Scholar]
- 33. McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103‐108. doi: 10.1136/bjsm.35.2.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Delahunt E, Remus A. Risk factors for lateral ankle sprains and chronic ankle instability. J Athl Train. 2019;54(6):611‐616. doi: 10.4085/1062-6050-44-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Arnason A, Sigurdsson SB, Gudmundsson A, Holme I, Engebretsen L, Bahr R. Risk factors for injuries in football. Am J Sports Med. 2004;32(1 suppl):5S‐16S. doi: 10.1177/0363546503258912 [DOI] [PubMed] [Google Scholar]
- 36. Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for acute ankle injuries among male soccer players: a prospective cohort study. Scand J Med Sci Sports. 2010;20(3):403‐410. doi: 10.1111/j.1600-0838.2009.00971.x [DOI] [PubMed] [Google Scholar]
- 37. Ekstrand J, Gillquist J, Liljedahl SO. Prevention of soccer injuries. Supervision by doctor and physiotherapist. Am J Sports Med. 1983;11(3):116‐120. doi: 10.1177/036354658301100302 [DOI] [PubMed] [Google Scholar]
- 38. Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med 1985;13(4):259–62. doi: 10.1177/036354658501300408, 262. [DOI] [PubMed] [Google Scholar]
- 39. Kofotolis N, Kellis E, Vlachopoulos S. Ankle sprain injuries and risk factors in amateur soccer players during a 2‐year period. Am J Sports Med. 2007;35(3):458‐466. doi: 10.1177/0363546506294857 [DOI] [PubMed] [Google Scholar]
- 40. Delahunt E, Bleakley CM, Bossard DS, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the international ankle consortium. Br J Sports Med. 2018;52(20):1304‐1310. doi: 10.1136/bjsports-2017-098885 [DOI] [PubMed] [Google Scholar]
- 41. Hägglund M, Waldén M, Magnusson H, Kristenson K, Bengtsson H, Ekstrand J. Injuries affect team performance negatively in professional football: an 11‐year follow‐up of the UEFA champions league injury study. Br J Sports Med. 2013;47(12):738‐742. doi: 10.1136/bjsports-2013-092215 [DOI] [PubMed] [Google Scholar]
- 42. Eirale C, Tol JL, Farooq A, Smiley F, Chalabi H. Low injury rate strongly correlates with team success in Qatari professional football. Br J Sports Med. 2013;47(12):807‐808. doi: 10.1136/bjsports-2012-091040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Eliakim E, Morgulev E, Lidor R, Meckel Y. Estimation of injury costs: financial damage of English premier league teams' underachievement due to injuries. BMJ Open Sport Exerc Med. 2020;6(1):e000675. doi: 10.1136/bmjsem-2019-000675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Houglum P. Soft tissue healing and its impact on rehabilitation. J Sport Rehabil. 1992;1(1):19‐39. [Google Scholar]
- 45. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344‐349. doi: 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 47. Waldén M, Hägglund M, Ekstrand J. The epidemiology of groin injury in senior football: a systematic review of prospective studies. Br J Sports Med. 2015;49(12):792‐797. doi: 10.1136/bjsports-2015-094705 [DOI] [PubMed] [Google Scholar]
- 48. Neyeloff J, Fuchs S, Moreira L. Meta‐analyses and forest plots using a microsoft excel spreadsheet: step‐by‐step guide focusing on descriptive data analysis. BMC Res Notes. 2012;20(5):52. doi: 10.1186/1756-0500-5-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cezarino L, Grüninger B, Silva R. Injury profile in a Brazilian first‐division youth SoccerTeam: a prospective study. J Athl Train. 2020;55(3):295‐302. doi: 10.4085/1062-6050-449-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Jain N, Murray D, Kemp S, Calder J. Frequency and trends in foot and ankle injuries within an English premier league football club using a new impact factor of injury to identify a focus for injury prevention. Foot Ankle Surg. 2014;20(4):237‐240. doi: 10.1016/j.fas.2014.05.004 [DOI] [PubMed] [Google Scholar]
- 51. Fransz DP, Huurnink A, Kingma I, de Boode VA, Heyligers IC, van Dieën JH. Performance on a single‐legged drop‐jump landing test is related to increased risk of lateral ankle sprains among male elite soccer players: a 3‐year prospective cohort study. Am J Sports Med. 2018;46(14):3454‐3462. doi: 10.1177/0363546518808027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Price RJ, Hawkins RD, Hulse MA, Hodson A. The football association medical research programme: an audit of injuries in academy youth football. Br J Sports Med. 2004;38(4):466‐471. doi: 10.1136/bjsm.2003.005165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Amer H, Mohamed S. Prevalence and risk factors of ankle sprain among male soccer players in Tabuk, Saudi Arabia: a cross‐sectional study. Open Sports Sci J. 2020;13:27‐33. doi: 10.2174/1875399X02013010027 [DOI] [Google Scholar]
- 54. Gulbrandsen M, Hartigan DE, Patel KA, Makovicka JL, Tummala SV, Chhabra A. Ten‐year epidemiology of ankle injuries in Men's and Women's collegiate soccer players. J Athl Train. 2019;54(8):881‐888. doi: 10.4085/1062-6050-144-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wikstrom EA. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association Sports. Am J Sports Med. 2017;45(1):201‐209. doi: 10.1177/0363546516660980 [DOI] [PubMed] [Google Scholar]
- 56. Pourgharib Shahi MH, Selk Ghaffari M, Mansournia MA, Halabchi F. Risk factors influencing the incidence of ankle sprain among elite football and basketball players: a prospective study. Foot Ankle Spec. 2021;14(6):482‐488. doi: 10.1177/1938640020921251 [DOI] [PubMed] [Google Scholar]
- 57. Ekstrand J, Krutsch W, Spreco A, et al. Time before return to play for the most common injuries in professional football: a 16‐year follow‐up of the UEFA elite Club injury study. Br J Sports Med. 2020;54(7):421‐426. doi: 10.1136/bjsports-2019-100666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Krutsch W, Memmel C, Alt V, et al. Timing return‐to‐competition: a prospective registration of 45 different types of severe injuries in Germany's highest football league. Arch Orthop Trauma Surg. 2022;142(3):455‐463. doi: 10.1007/s00402-021-03854-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Oztekin HH, Boya H, Ozcan O, Zeren B, Pinar P. Foot and ankle injuries and time lost from play in professional soccer players. Foot (Edinb). 2009;19(1):22‐28. doi: 10.1016/j.foot.2008.07.003 [DOI] [PubMed] [Google Scholar]
- 60. Fuller CW, Walker J. Quantifying the functional rehabilitation of injured football players. Br J Sports Med. 2006;40(2):151‐157. doi: 10.1136/bjsm.2005.021048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Whalan M, Lovell R, McCunn R, Sampson JA. The incidence and burden of time loss injury in Australian men's sub‐elite football (soccer): a single season prospective cohort study. J Sci Med Sport. 2019;22(1):42‐47. doi: 10.1016/j.jsams.2018.05.024 [DOI] [PubMed] [Google Scholar]
- 62. Larruskain J, Lekue JA, Diaz N, Odriozola A, Gil SM. A comparison of injuries in elite male and female football players: a five‐season prospective study. Scand J Med Sci Sports. 2018;28(1):237‐245. doi: 10.1111/sms.12860 [DOI] [PubMed] [Google Scholar]
- 63. Ekstrand J, Hägglund M, Kristenson K, Magnusson H, Waldén M. Fewer ligament injuries but no preventive effect on muscle injuries and severe injuries: an 11‐year follow‐up of the UEFA champions league injury study. Br J Sports Med. 2013;47(12):732‐737. doi: 10.1136/bjsports-2013-092394 [DOI] [PubMed] [Google Scholar]
- 64. Logerstedt DS, Ebert JR, MacLeod TD, Heiderscheit BC, Gabbett TJ, Eckenrode BJ. Effects of and response to mechanical loading on the knee. Sports Med. 2022;52(2):201‐235. doi: 10.1007/s40279-021-01579-7 [DOI] [PubMed] [Google Scholar]
- 65. Hägglund M, Waldén M, Ekstrand J. Risk factors for lower extremity muscle injury in professional soccer: the UEFA injury study. Am J Sports Med. 2013;41(2):327‐335. doi: 10.1177/0363546512470634 [DOI] [PubMed] [Google Scholar]
- 66. Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria‐based progression through the return‐to‐sport phase. J Orthop Sports Phys Ther. 2006;36(6):385‐402. doi: 10.2519/jospt.2006.2222 [DOI] [PubMed] [Google Scholar]
- 67. Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):192‐199. doi: 10.1007/s00167-016-4246-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. van der Horst N, van de Hoef S, Reurink G, Huisstede B, Backx F. Return to play after hamstring injuries: a qualitative systematic review of definitions and criteria. Sports Med. 2016;46(6):899‐912. doi: 10.1007/s40279-015-0468-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Tassignon B, Verschueren J, Delahunt E, et al. Criteria‐based return to sport decision‐making following lateral ankle sprain injury: a systematic review and narrative synthesis. Sports Med. 2019;49(4):601‐619. doi: 10.1007/s40279-019-01071-3 [DOI] [PubMed] [Google Scholar]
- 70. Wikstrom EA, Mueller C, Cain MS. Lack of consensus on return‐to‐sport criteria following lateral ankle sprain: a systematic review of expert opinions. J Sport Rehabil. 2020;29(2):231‐237. doi: 10.1123/jsr.2019-0038 [DOI] [PubMed] [Google Scholar]
- 71. Serner A, Hölmich P, Tol JL, et al. Progression of strength, flexibility, and palpation pain during rehabilitation of athletes with acute adductor injuries: a prospective cohort study. J Orthop Sports Phys Ther. 2021;51(3):126‐134. doi: 10.2519/jospt.2021.9951 [DOI] [PubMed] [Google Scholar]
- 72. Della Villa F, Hägglund M, Della Villa S, Ekstrand J, Waldén M. High rate of second ACL injury following ACL reconstruction in male professional footballers: an updated longitudinal analysis from 118 players in the UEFA elite Club injury study. Br J Sports Med. 2021;55(23):1350‐1356. doi: 10.1136/bjsports-2020-103555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Forsythe B, Lavoie‐Gagne OZ, Forlenza EM, Diaz CC, Mascarenhas R. Return‐to‐play times and player performance after ACL reconstruction in elite UEFA professional soccer players: a matched‐cohort analysis from 1999 to 2019. Orthop J Sports Med. 2021;9(5):23259671211008892. doi: 10.1177/23259671211008892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Grooms DR, Page SJ, Nichols‐Larsen DS, Chaudhari AM, White SE, Onate JA. Neuroplasticity associated with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2017;47(3):180‐189. doi: 10.2519/jospt.2017.7003 [DOI] [PubMed] [Google Scholar]
- 75. Terada M, Johnson N, Kosik K, Gribble P. Quantifying brain White matter microstructure of people with lateral ankle sprain. Med Sci Sports Exerc. 2019;51(4):640‐646. doi: 10.1249/MSS.0000000000001848 [DOI] [PubMed] [Google Scholar]
- 76. Needle AR, Lepley AS, Grooms DR. Central nervous system adaptation after ligamentous injury: a summary of theories, evidence, and clinical interpretation. Sports Med. 2017;47(7):1271‐1288. doi: 10.1007/s40279-016-0666-y [DOI] [PubMed] [Google Scholar]
- 77. Pietrosimone BG, Gribble PA. Chronic ankle instability and corticomotor excitability of the fibularis longus muscle. J Athl Train. 2012;47(6):621‐626. doi: 10.4085/1062-6050-47.6.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Terada M, Bowker S, Thomas AC, Pietrosimone B, Hiller CE, Gribble PA. Corticospinal excitability and inhibition of the soleus in individuals with chronic ankle instability. Pm R. 2016;8(11):1090‐1096. doi: 10.1016/j.pmrj.2016.04.006 [DOI] [PubMed] [Google Scholar]
- 79. Lohrer H, Nauck T, Gehring D, Gollhofer A. Sprunggelenkarthrometrie zur Diagnostik der mechanischen Komponente der chronischen Sprunggelenkinstabilität [ankle arthrometry for evaluation of the mechanical component in chronic ankle instability]. Sportverletz Sportschaden. 2013;27(2):85‐90. doi: 10.1055/s-0032-1330768 [DOI] [PubMed] [Google Scholar]
- 80. Polsky S. Winning medicine: professional sports team doctors' conflicts of interest. J Contemp Health Law Policy. 1998;14(2):503‐529. [PubMed] [Google Scholar]
- 81. Pike Lacy AM, Singe SM, Bowman TG. Collegiate athletic Trainers' experiences with external pressures faced during decision making. J Athl Train. 2020;55(4):409‐415. doi: 10.4085/1062-6050-165-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ekstrand J, Lundqvist D, Davison M, D'Hooghe M, Pensgaard AM. Communication quality between the medical team and the head coach/manager is associated with injury burden and player availability in elite football clubs. Br J Sports Med. 2019;53(5):304‐308. doi: 10.1136/bjsports-2018-099411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Ekstrand J, Spreco A, Bengtsson H, Bahr R. Injury rates decreased in men's professional football: an 18‐year prospective cohort study of almost 12 000 injuries sustained during 1.8 million hours of play. Br J Sports Med. 2021;55(19):1084‐1091. doi: 10.1136/bjsports-2020-103159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Malliaropoulos N, Ntessalen M, Papacostas E, Longo UG, Maffulli N. Reinjury after acute lateral ankle sprains in elite track and field athletes. Am J Sports Med. 2009;37(9):1755‐1761. doi: 10.1177/0363546509338107 [DOI] [PubMed] [Google Scholar]
- 85. Smith MD, Vicenzino B, Bahr R, et al. Return to sport decisions after an acute lateral ankle sprain injury: introducing the PAASS framework‐an international multidisciplinary consensus. Br J Sports Med. 2021;55(22):1270‐1276. doi: 10.1136/bjsports-2021-104087 [DOI] [PubMed] [Google Scholar]
- 86. Alhdad T, Gavrilović P, Životić D. Economic effects of injuries in elite soccer players with regard to ankle injury. Physical Education and Sport. 2020;18(1):83‐92. doi: 10.22190/FUPES190918008A [DOI] [Google Scholar]
- 87. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500‐1524. doi: 10.1016/j.ijsu.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 88. Ramke J, Palagyi A, Jordan V, Petkovic J, Gilbert CE. Using the STROBE statement to assess reporting in blindness prevalence surveys in low and middle income countries. PLoS One. 2017;12(5):e0176178. doi: 10.1371/journal.pone.0176178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Limaye D, Pitani R, Limaye V, et al. Development of a quantitative scoring method for strobe checklist. Acta Pol Pharm Drug Res. 2018;5:1095‐1106. doi: 10.32383/appdr/84804 [DOI] [Google Scholar]
- 90. International Olympic Committee Injury , Illness Epidemiology Consensus Group , Bahr R, Clarsen B, Derman W, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sports 2020 (including the STROBE extension for sports injury and illness surveillance [STROBE‐SIIS]). Orthop J Sports Med. 2020;8(2):2325967120902908. doi: 10.1177/2325967120902908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Br J Sports Med. 2006;40(3):193‐201. doi: 10.1136/bjsm.2005.025270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta‐analysis. Am J Sports Med. 2016;44(7):1861‐1876. doi: 10.1177/0363546515621554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116‐121. doi: 10.1097/JSM.0b013e318246ef9e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567‐1573. doi: 10.1177/0363546514530088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Fuller CW, Bahr R, Dick RW, Meeuwisse WH. A framework for recording recurrences, reinjuries, and exacerbations in injury surveillance. Clin J Sport Med. 2007;17(3):197‐200. doi: 10.1097/JSM.0b013e3180471b89 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Appendix S2
Appendix S3
Appendix S4
Appendix S5
Table S1
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


