Abstract
Introduction
The prevalence of food allergy (FA) in the Makkah region has received little attention, so we conducted this study to estimate the prevalence of FA in adults.
Methods
This descriptive, cross-sectional, survey-based study was conducted online among 531 participants with or without a prior diagnosis of FA. The collected data related to socio-demographics (age and gender), whether the participant had been medically diagnosed with any food allergens, and assessing the prevalence of different food allergens.
Results
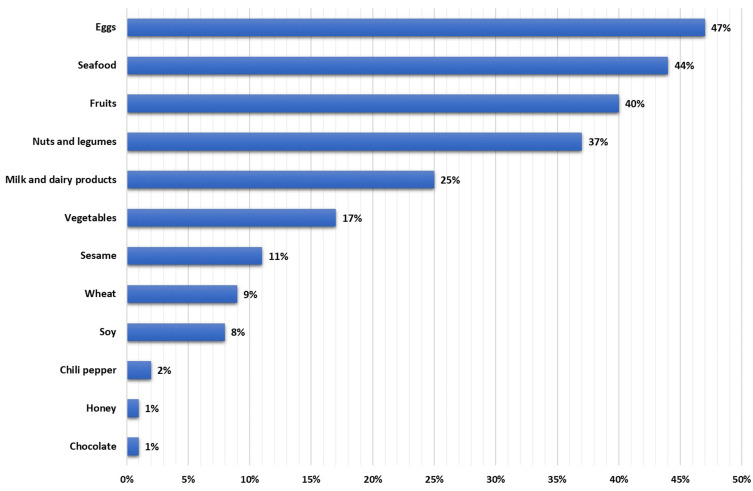
Only 93 (17.5%) of the 531 people screened positive for FA; females (65.6%) predominated, with 37.6% aged 40–59. The type of food for allergy was: eggs (47%), seafood (44%), fruits (40%), nuts and legumes (37%), milk and dairy products (25%), vegetables (17%), sesame (11%), wheat (9%), soy (8%), 2% to chili peppers, and only 1% honey and chocolate.
Conclusion
Both genders were allergic to eggs, followed by seafood, fruits, nuts, and legumes, and milk and dairy products, respectively.
Keywords: food allergy, Makkah, food allergen, eggs, seafood
Introduction
A food allergy (FA) is a set of immunological responses that appears to happen when a person shows a particular interaction with some food items.1 FA is classified into three types based on the immune-mediated response: immunoglobulin (IgE)-mediated and non-IgE mediated or a combination of both. IgE-mediated food allergies (4–7% in children and 1–2% in adults) require prior sensitization to food allergens and produce allergic symptoms upon reexposure to that food.2 The number of people who suffer from FA is rising all over the world, and there are approximately 2–10% of people in the world suffer from FA.3 The reasoning behind this increase is not entirely clear; however, changes in lifestyle, environmental factors, and modernization are to blame.4
The FA has been found to affect various body organs, including the respiratory tract, the digestive tract, the skin, and the cardiovascular system.3 Several symptoms point to the presence of the FA, and their severities are associated with its type.3,5 In the IgE-mediated FA where the IgE antibodies are involved, the symptoms will appear immediately after the food ingestion. These symptoms are typically mild, but they occasionally can lead to severe reactions that could cause life-threatening events. Most of these signs include rash, hives, swelling, tingling of the lips and tongue, vomiting, and in severe cases, difficulty breathing and anaphylactic shock.6 However, the non-IgE mediated FA is a late immune reaction that results from an immune cell-mediated response which can cause inflammation in the gastrointestinal tract indicated by some manifestations such as vomiting, diarrhea, and bloating. Unlike the IgE type, these symptoms appear after hours or weeks after ingestion.7 In the combination FA, where both IgE antibodies and cell-mediated immune response are involved, the most common FA symptoms are atopic eczema, abdominal pain, nausea, vomiting, diarrhea, and in some cases, weight loss in adults and failure to thrive in young children.8,9
The prevalence of FA varies from country to country because estimates are affected by several factors, including genetic factors (race and gender) and environmental factors, such as the frequency of dietary intake and the preparation method.10 In Europe, from 2011 to 2012, the number was estimated to be between 11 and 26 million, while in Malaysia, the percentage of affected children increased to 10–15 of the total population.11 Approxmailty 877 of FA patients with severe symptoms were reported in Norway from 2000 to 2010, and this population has kept increasing.12 In the United States, FA affects 10.8% of US adults while it presents 7.6% of US children,13 while in the United Kingdom, only 1–2% of adults and 5–8% of children were affected by the condition.14 According to estimates in 2012, approximately 2.108 people out of a total population of 30,018 in Taiwan suffered from FA.15 According to a study conducted among Japanese nursery schools in 2019, approximately 45,807 children in Japan suffer from FA, and 3499 have experienced an allergic reaction to food.16 Many people are susceptible to developing FA at any point in their lives, possibly between childhood and old age.17
To date, the adult FA examination has concentrated on a small number of specific allergens.13 Recent studies have shown that the prevalence of allergic diseases in the Middle East Region is rapidly increasing.18 Only one Tayeb et al study has attempted to quantify the types of food allergens present in Makkah.19 However, this research was conducted solely on people with a diagnosis of FA and not in a community setting of any kind. In addition, a recent investigation into the prevalence of FA among adults in Saudi Arabia was carried out in a community-based study.20 However, there were only 70 participants from the Makkah region, a relatively small number compared to the other Saudi regions; this could be a limitation of the study. Hence this study aims to investigate the prevalence of self-reported FA and specific food allergens among adults in the Makkah region of Saudi Arabia. In addition, one of our goals is to investigate the relationship between the most common food allergens and age and gender.
Methodology
Study Design and Population
This was a descriptive, cross-sectional, survey-based research carried out online and disseminated to the general public in the Makkah area, with or without a prior diagnosis of FA. The research was carried out between April and June of 2021. It covered all adults over 18 who lived in the Makkah area. Participants were excluded if they were under 18 or did not live in the Makkah areas. On the first page, there was an online informed consent form. It was also stated that participation in this research was completely voluntary. The questionnaire was then distributed to the participants. OpenEpi version 3.0 computed the minimal sample size needed in sample size computation. Compared to the Makkah area’s total population, around 8.8 million people,21 the estimated sample size was 385 participants. This estimate was derived using a confidence level of 95% and a margin of error of 5%; nevertheless, 531 individuals were included in the study.
Measurement Tool
Previous research that was published served as the basis for a revised questionnaire.13,19,20 Three experts in medical immunology, family medicine, and clinical nutrition assessed the questionnaire’s style and content to assess its appropriateness, relevance, clarity, and adequacy. The questionnaire was written in English and translated into Arabic (the native language of the participants). The final Arabic questionnaire was pre-tested with three specialists (native Arabic speakers) and ten general population participants. Based on the comments, the final questionnaire was updated. The questionnaire was then sent to the general Saudi populace through social media sites (Twitter, WhatsApp, and Snapchat). The questionnaire had six questions divided into two parts. Section one consisted of yes and no questions evaluating the prevalence of FA allergy in all subjects. Then, if the participants were food-allergic individuals, they were moved to the second part of the question, which asked them about their personal information, such as age, gender, education, food allergen, and whether or not a doctor diagnosed their conditions, Supplementary Figure 1.
Data Analysis
The information was gathered, evaluated, and entered into the Statistical Package for Social Sciences version 21. (SPSS: An IBM Company). All statistical procedures were two-tailed with an alpha level of 0.05, and significance was determined if the P value was less than or equal to 0.05. Descriptive analysis was performed using frequency distribution and percentage for research variables such as adults’ food allergy history, age, gender, food allergens, and a physician’s diagnosis as a food allergy patient. Due to the narrow frequency distributions, cross tabulation was used to depict the distribution of adults’ reported food allergies by age and gender data, with an exact probability test for significance.
Results
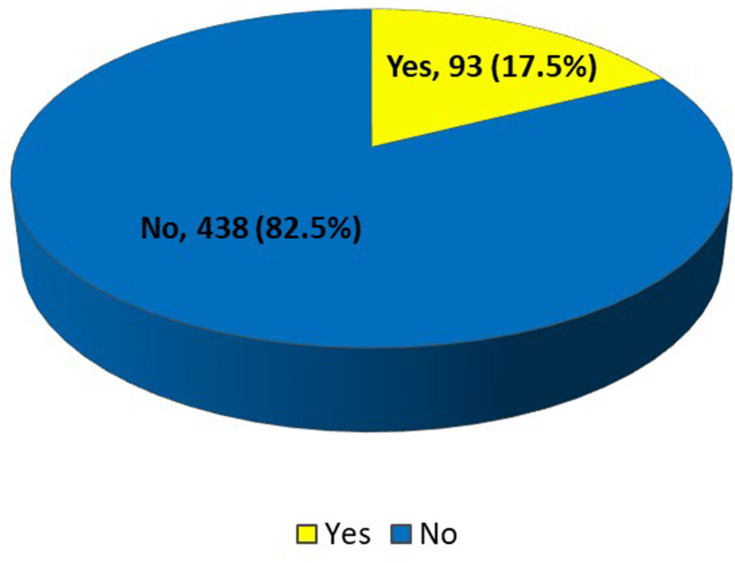
The study aims to assess the subjects’ most prevalent food allergies. The questionnaire was used to gather primary data; only 93 (17.5%) of the 531 sample collection had a food allergy, while 438 (82.5%) did not; more details about the socio-demographic characteristics of study participants can be seen in Table 1. Because only patients with food allergies were chosen for further research, a total sample size of 93 was used. SPSS version 21 was used to analyze the gathered data. The frequency and percentage of the variables were evaluated using descriptive statistics, and the link between the variables was discovered using the cross-tabs approach.
Table 1.
Socio-Demographic Characteristics of Study Participants in Makkah Region (n=531)
| Variables | No | % | |
|---|---|---|---|
| Gender | Female | 267 | 50.3% |
| Male | 264 | 49.7% | |
| Age (in years) | 18–28 years | 114 | 21.5% |
| 29–39 years | 95 | 17.9% | |
| 40–59 years | 240 | 45.2% | |
| 60–80 years | 82 | 15.4% | |
| Level of education | Under high school | 17 | 3.2% |
| High school/ diploma | 88 | 16.6% | |
| Bachelor’s degree | 330 | 62.1% | |
| Postgraduate studies | 96 | 18.1% | |
| Are you Food Allergy patient? | Yes | 93 | 17.5% |
| No | 438 | 82.5% |
Figure 1 illustrates the prevalence of food allergy among Saudi Adults in Makkah Region, among the 531 collected samples; only 93 of the participants had a food allergy while the remaining 438 participants did not have a food allergy.
Figure 1.
Prevalence of food allergy among Saudi Adults in Makkah Region, Saudi Arabia. Between the 531 participants, only 93 (17.5%) had a food allergy, whereas the rest (438=82.5%) were healthy, as they reported.
Table 2 displays the frequency values for the demographic variables of patients with food allergy in Makkah region. The ages of the participants (in years) were divided into four categories: 28% between the ages of 18 and 28, 18.3% between the ages of 29 and 39, 37.6% between the ages of 40 and 59, and 16.1% between the ages of 60 and 80. Furthermore, the majority of participants (65.6%) were female, with 34.4% being male. Only 62.4% of the 93 participants with food allergies had their allergy confirmed by a clinician, while 37.6% self-reported their allergy.
Table 2.
Socio-Demographic Characteristics of Patients with Food Allergy in Makkah Region, Saudi Arabia (n=93)
| Variables | No | % | |
|---|---|---|---|
| Gender | Female | 61 | 65.6 |
| Male | 32 | 34.4 | |
| Age (in years) | 18–28 years | 26 | 28 |
| 29–39 years | 17 | 18.3 | |
| 40–59 years | 35 | 37.6 | |
| 60–80 years | 15 | 16.1 | |
| Level of education | Under high school | 3 | 3.2 |
| High school/ diploma | 9 | 9.7 | |
| Bachelor’s degree | 59 | 63.4 | |
| Postgraduate studies | 22 | 23.7 | |
| Diagnosed with food allergy by a doctor | Yes | 58 | 62.4 |
| No | 35 | 37.6 |
Figure 2 depicts the distribution of the most common food allergens among the participants. The majority of the participants, 47% (44), had an allergy to eggs, followed by 44% (41) having an allergy to seafood and 40% (37) having an allergy to fruits. In addition, 37% (34) of the participants had an allergy to nuts and legumes, 25% (23) had an allergy to milk and dairy products, 17% (16) of the participants had an allergy to vegetables, 11% (10) of them had an allergy to sesame, and 9% (8) and 8% (7) of the participants were allergic to wheat and soy respectively. Only 2% (2) of the participants were allergic to chilli peppers, and only 1% (1) were allergic to honey and chocolate.
Figure 2.
Most common Food Allergen among Saudi Adults in Makkah Region, Saudi Arabia.
Table 3 depicts the distribution of food allergens by adult age groups and the relationship between age groups and the most common allergic food. Among them, 46.2% of the participants were allergic to both nuts and legumes and fruits between the ages of 18 and 28, 76.5% of the participants were allergic to seafood between the ages of 29 and 39, 54.3% of the participants were allergic to eggs between the ages of 40 and 59, and 53.3% are allergic to eggs, seafood, and fruits between the ages of 60 and 80. All these differences were found to be statistically significant (P=0.001).
Table 3.
Distribution of Food Allergens by Adult’s Age, Makkah Region, Saudi Arabia
| Allergens | Total | Age in Years | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 18–28 | 29–39 | 40–59 | 60–80 | |||||||
| N | % | N | % | N | % | N | % | |||
| Nuts and legumes | 34 | 12 | 46.2% | 7 | 41.2% | 12 | 34.3% | 3 | 20.0% | 0.001* |
| Eggs | 44 | 9 | 34.6% | 8 | 47.1% | 19 | 54.3% | 8 | 53.3% | |
| Milk and dairy products | 23 | 6 | 23.1% | 7 | 41.2% | 9 | 25.7% | 1 | 6.7% | |
| Wheat | 8 | 0 | 0.0% | 2 | 11.8% | 3 | 8.6% | 3 | 20.0% | |
| Soy | 7 | 2 | 7.7% | 3 | 17.6% | 1 | 2.9% | 1 | 6.7% | |
| Sesame | 10 | 3 | 11.5% | 5 | 29.4% | 0 | 0.0% | 2 | 13.3% | |
| Seafood | 41 | 4 | 15.4% | 13 | 76.5% | 16 | 45.7% | 8 | 53.3% | |
| Fruits | 37 | 12 | 46.2% | 8 | 47.1% | 9 | 25.7% | 8 | 53.3% | |
| Vegetables | 16 | 2 | 7.7% | 5 | 29.4% | 6 | 17.1% | 3 | 20.0% | |
| Chilli pepper | 2 | 1 | 3.8% | 1 | 5.9% | 0 | 0.0% | 0 | 0.0% | |
| Chocolate | 1 | 1 | 3.8% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | |
| Honey | 1 | 0 | 0.0% | 0 | 0.0% | 1 | 2.9% | 0 | 0.0% | |
Notes: p: Exact probability test, * p < 0.05 (significant). %: The percentage calculated from the total population for each age group, for example, the number of allergic participants with age 18–28 was 12, and the total number of these participants was 26: 12/26x100=46.2%.
Table 4 displays the frequency of food allergens by gender and the relationship between gender variables and the most common allergic food. The most reported food allergens among male adults were eggs (56.3%) compared to 42.6% for females, followed by sea food (50% vs 41% respectively), fruits (40.6% vs 39.3%, respectively), and nuts and legumes (31.3% vs 39.3%, respectively). All differences were statistically insignificant (P=0.062).
Table 4.
Distribution of Food Allergens by Gender, Makkah Region, Saudi Arabia
| Allergens | Gender | p-value | |||
|---|---|---|---|---|---|
| Male | Female | ||||
| N | % | N | % | ||
| Nuts and legumes | 10 | 31.3% | 24 | 39.3% | 0.062 |
| Eggs | 18 | 56.3% | 26 | 42.6% | |
| Milk and dairy products | 4 | 12.5% | 19 | 31.1% | |
| Wheat | 6 | 18.8% | 2 | 3.3% | |
| Soy | 2 | 6.3% | 5 | 8.2% | |
| Sesame | 4 | 12.5% | 6 | 9.8% | |
| Seafood | 16 | 50.0% | 25 | 41.0% | |
| Fruits | 13 | 40.6% | 24 | 39.3% | |
| Vegetables | 7 | 21.9% | 9 | 14.8% | |
| Chilli pepper | 0 | 0.0% | 2 | 3.3% | |
| Chocolate | 0 | 0.0% | 1 | 1.6% | |
| Honey | 1 | 3.1% | 0 | 0.0% | |
Notes: p: Exact probability test. %: The percentage is calculated from the total population for each gender. For example, the number of females allergic to Nuts and legumes is 24, and the total of FA females is 61; therefore, the percentage will be 24/61x100=39.3%.
Discussion
There is a paucity of information on the prevalence of FA in the Saudi population living in the Makkah Region. To the best of our knowledge, this is the first study to investigate the prevalence of FA among adults in the Makkah region since Tayeb et al study in 2009.19 In our study, we found only 17% of participants had FA, and most of them were females. Regarding the common FA allergens, egg presents the most common allergen, while chocolate and honey present the lowest in the list.
In our samples, we reported that females were substantially more allergic to food (65.6%) than men (34.4%), consistent with the previous study.19 However, in the Iranian population, males were substantially more allergic to food than females.22 Gender differences in allergy prevalence exist. Before puberty, males are more likely than girls to have general atopic symptoms such as skin responses to one or more allergens, asthma, and food allergies.23 Females are much more impacted by food-induced complaints later in life (13–21 years) Marklund et al;24 other research reveals that the ratio of food intolerance between females and males after puberty is 60:40,25 1: 1.8 (female: male).26 In Saudi Arabian research, males were at greater risk for anaphylactic responses (61.2%) in the pediatric group (17 years) with food.27 In Mongolia, self-reported FA was 18.% among 4441 completed surveys, with 15.2% of males and 20.6% of women afflicted.28 This gender discrepancy decreased at the age of 55. The gender difference in response to metabolic variables may impact immunological function. A high body mass index is connected with atopy in sexually mature females,29 allergy,30 and asthma.31 This might imply that leptin or other adipokines have a role in allergy illness susceptibility.32–34 In one research, rats given leptin at levels comparable to mild obesity had more significant blood IgE levels, suggesting a probable direct relationship between leptin and allergy illness.35 The higher reported FA among prepubescent-age males might be explained by genetic susceptibility. The foundation of sex differences is the sexual genotype (XX in females and XY in men). Thus, an X-linked recessive trait related to allergy illness would be more likely to be exposed in males. It might explain why FA predominates in men at such an early age.36 Male cord blood has higher amounts of total IgE than female cord blood37 and remains elevated throughout the lifetime, despite female atopy after puberty.38
The most reported allergy foods in the current research were eggs, seafood, fruits, nuts and legumes, milk, and dairy products, and the less reported were vegetables, sesame, wheat, and soy. Furthermore, the least reported food products were chili pepper, honey, and chocolate. According to Althumiri, N.A. et al 2021, the most common dietary allergens among Saudis are milk (61.96%), egg whites (59.78%), wheat (45.65%), and peanuts (38.04%).20 Tayeb et al did similar research in 2009 and listed the top five food allergies: chocolate, peanuts, egg white, milk, and strawberry.19 In 2017, Fatima Ali revealed that eggs, milk, and nuts were the most common dietary allergies.39 We are unable to do additional comparison research since there is a lack of data on the dietary allergies that occur most often in Makkah city.
The most common allergens found in adults were found to be shellfish (1.9%), vegetables (1.3%), and fruits (1.6%), according to another research that was conducted by Sicherer et al and assessed 9667 individuals.5 Acker et al researched a number of different Ethnic groups, and they discovered that females of Asian race have a greater propensity to be allergic to food than other groups.40 It was shown that shellfish allergy affected the most persons (0.9% of cases), followed by fruit or vegetable allergy (0.7%), dairy allergy (0.5%), and peanut allergy (0.5%). FA is estimated to affect 4% of children and 1% of adults globally, with a rise in frequency over the last two decades.41,42 Differences in reported prevalence are because FA is not entirely understood, and some unpleasant food responses are not allergic. However, it is estimated that roughly 25% of persons in the western world have a FA.43
According to recent research conducted in the United Arab Emirates, seafood and nuts were the most prevalent dietary allergens.44 Another research found that the most common food-specific IgE responses are to hazelnuts and peanuts, with a significant increase in reactivity to hazelnuts.12 A study conducted in Turkey was shown that tree nut allergy was the highest on the list, then milk, seeds, and egg.45 According to Seth D’s analysis in 2020, the eight most prevalent food allergens are eggs, milk, peanuts, tree nuts, soy, wheat, crustacean shellfish, and fish, all of which are often eaten in the United States.46 In addition to these foods, other significant foods that contributed to the development of the allergy include beef in China, rice in Thailand, sesame in Singapore, pork, seafood, and peaches in Korea, bananas in Saudi Arabia and Egypt, apples, tomatoes, and crab in Zimbabwe, peanuts and pineapples in Ghana, shrimp and oranges in Mexico, and corn in Brazil. All of these foods were consumed in the respective countries.47 The prevalence of foods that trigger allergic reactions might vary from country to country depending on the eating customs, genetic variables, and cultural norms of the people who live there.48
Conclusion
Public knowledge of FA is regarded as low because people underestimate its effect on food allergy patients until they experience the severity of the condition. FA patients experience great difficulties since they are exposed to risks that might endanger their lives. In conclusion, it is essential to do research on FA among those who suffer from FA. Patients may use this information to pinpoint the meals that bring on their symptoms and steer clear of them. Because of this, they will not have allergic responses if the trigger is removed from the environment. The findings of an investigation on FA among adults in Makkah city should assist the government in making informed decisions about the components of meal planning.
Strength, Limitations, and Future Studies
Although the current study represents one of the first assessments of the prevalence of FA, the common food allergen, the relationship between food allergens and age, and gender among Saudi adults in the Makkah region, there are some limitations. The most important limitation is the restriction of the result in one region (Makkah) and to people who had access to the online questionnaire, which may prevent the generalization of the current study results. Therefore, a comprehensive study is suggested to be applied at a national level, including all Saudi regions. In addition, the current study was a self-reported online questionnaire which may bias the result as the patients’ understanding, standards, and feelings might influence it. Hence, the authors recommended a qualitative approach to future studies with a semi-structured interview that would significantly contribute to verifying the present study’s findings.
Acknowledgments
The authors would like to acknowledge all the participants for their generous participation in this study.
Funding Statement
The authors received no financial support for the research, authorship, and/or publication of this article.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethical Approval
The Biomedical Ethics Committee, College of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia, granted ethical permission with approval No (HAPO-02-K-012-2021-03-631), and we conducted it in accordance with the Declaration of Helsinki.
Author Contributions
All authors made substantial contributions to the conception, design, acquisition of data, analysis, and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit it to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declared no potential conflicts of interest.
References
- 1.Phan NHD, Nguyen TT, Tran TBH., et al. Exploring the PCR assay for detecting tropomyosin: major allergen in shrimp-derived ingredient in food. Pharmacophore. 2020;11(2):53–57. [Google Scholar]
- 2.Turnbull JL, Adams HN, Gorard DA. The diagnosis and management of food allergy and food intolerances. Aliment Pharmacol Ther. 2015;41(1):3–25. doi: 10.1111/apt.12984 [DOI] [PubMed] [Google Scholar]
- 3.Sicherer SH, Sampson HA. Food allergy: epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014;133(2):291–307.e5. doi: 10.1016/j.jaci.2013.11.020 [DOI] [PubMed] [Google Scholar]
- 4.Tang MLK, Mullins RJ. Food allergy: is prevalence increasing? Intern Med J. 2017;47(3):256–261. doi: 10.1111/imj.13362 [DOI] [PubMed] [Google Scholar]
- 5.Sicherer SH, Wood RA, Vickery BP, et al. Impact of Allergic Reactions on Food-Specific IgE Concentrations and Skin Test Results. J Allergy Clin Immunol Pract. 2016;4(2):239–45.e4. doi: 10.1016/j.jaip.2015.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sicherer SH, Sampson HA. Food allergy. J Allergy Clin Immunol. 2010;125(2):S116–S125. doi: 10.1016/j.jaci.2009.08.028 [DOI] [PubMed] [Google Scholar]
- 7.Connors L, O’Keefe A, Rosenfield L, Kim H. Non-IgE-mediated food hypersensitivity. Allergy Asthma Clin Immunol. 2018;14(S2):56. doi: 10.1186/s13223-018-0285-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Furuta GT, Katzka DA. Eosinophilic Esophagitis. N Eng J Med. 2015;373(17):1640–1648. doi: 10.1056/NEJMra1502863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roerdink EM, Flokstra-de Blok BMJ, Blok JL, et al. Association of food allergy and atopic dermatitis exacerbations. Ann Allergy Asthma Immunol. 2016;116(4):334–338. doi: 10.1016/j.anai.2016.01.022 [DOI] [PubMed] [Google Scholar]
- 10.Kim M, Lee JY, Jeon H-Y. Prevalence of immediate-type food allergy in Korean schoolchildren in 2015: a nationwide, population-based study. Allergy Asthma Immunol Res. 2017;9(5):410–416. doi: 10.4168/aair.2017.9.5.410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pawankar R, Canonica GW, Holgate ST, Lockey RF, Blaiss MS. WAO white book on allergy. World Allergy Org. 2011;3:156–157. [Google Scholar]
- 12.Namork E, Fæste CK, Stensby BA, Egaas E, Løvik M. Severe Allergic Reactions to Food in Norway: a Ten Year Survey of Cases Reported to the Food Allergy Register. Int J Environ Res Public Health. 2011;8(8):3144–3155. doi: 10.3390/ijerph8083144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta RS, Warren CM, Smith BM, et al. Prevalence and Severity of Food Allergies Among US Adults. JAMA Netw Open. 2019;2(1):e185630–e185630. doi: 10.1001/jamanetworkopen.2018.5630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buck J, Hattersley S, Kimber I. Food allergy science and policy needs the UK Food Standards Agency research programme. Toxicology. 2010;278(3):319–325. doi: 10.1016/j.tox.2010.08.007 [DOI] [PubMed] [Google Scholar]
- 15.Wu TC, Tsai TC, Huang CF, et al. Prevalence of food allergy in Taiwan: a questionnaire-based survey. Intern Med J. 2012;42(12):1310–1315. doi: 10.1111/j.1445-5994.2012.02820.x [DOI] [PubMed] [Google Scholar]
- 16.Yanagida N, Katsunuma T, Ebisawa M, Yoshizawa J. Risk factors of severe accidental ingestion in nursery school: a nationwide survey. J Allergy Clin Immunol. 2019;143(2):AB148. doi: 10.1016/j.jaci.2018.12.450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grabenhenrich LB, Dölle S, Moneret-Vautrin A, et al. Anaphylaxis in children and adolescents: the European Anaphylaxis Registry. J Allergy Clin Immunol. 2016;137(4):1128–1137.e1. doi: 10.1016/j.jaci.2015.11.015 [DOI] [PubMed] [Google Scholar]
- 18.Pazoki N, Ahmadi A, Onsori F, Mosavi Khorshidi M, Mansori M, Salimian J. Prevalence of aeroallergens and food allergens in allergic patients in Tehran, Iran. Int J Med Lab. 2018;5(4):246–254. [Google Scholar]
- 19.Tayeb MMS, Koshak EA, Qutub MMA. Sensitization to Common Food Allergens in Makkah City. Egypt J Hosp Med. 2009;35(1):288–294. doi: 10.21608/ejhm.2009.17575 [DOI] [Google Scholar]
- 20.Althumiri NA, Basyouni MH, AlMousa N, AlJuwaysim MF, BinDhim NF, Alqahtani SA. Prevalence of Self-Reported Food Allergies and Their Association with Other Health Conditions among Adults in Saudi Arabia. Int J Environ Res Public Health. 2021;18(1):347. doi: 10.3390/ijerph18010347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arabia S. General Authority for Statistics. General Population Housing Census. 2016;26:548. [Google Scholar]
- 22.Ahanchian H, Jafari S, Behmanesh F, et al. Epidemiological survey of pediatric food allergy in Mashhad in Northeast Iran. Electron Phys. 2016;8(1):1727. doi: 10.19082/1727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Becklake MR, Kauffmann F. Gender differences in airway behaviour over the human life span. Thorax. 1999;54(12):1119–1138. doi: 10.1136/thx.54.12.1119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marklund B, Ahlstedt S, Nordstrm G. Health-related quality of life among adolescents with allergy-like conditions with emphasis on food hypersensitivity. Health Qual Life Outcomes. 2004;2(1):1–12. doi: 10.1186/1477-7525-2-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lovik M, Namork E, Foste C, Egaas E. The Norwegian national reporting system and register of severe allergic reactions to food. Norsk epidemiol. 2004;14(2):6598. [Google Scholar]
- 26.Kelly C, Gangur V. Sex disparity in food allergy: evidence from the PubMed database. J Allergy (Cairo). 2009;2009. doi: 10.1155/2009/159845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alkanhal R, Alhoshan I, Aldakhil S, et al. Prevalence triggers and clinical severity associated with anaphylaxis at a tertiary care facility in Saudi Arabia: a cross-sectional study. Medicine. 2018;97(31):e11582. doi: 10.1097/MD.0000000000011582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang XY, Zhuang Y, Ma TT, Zhang B, Wang XY. Prevalence of self-reported food allergy in six regions of inner Mongolia, northern China: a population-based survey. Med Sci Monit. 2018;24:1902. doi: 10.12659/MSM.908365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vieira VJ, Ronan AM, Windt MR, Tagliaferro AR. Elevated atopy in healthy obese women. Am J Clin Nutr. 2005;82(3):504–509. doi: 10.1093/ajcn/82.3.504 [DOI] [PubMed] [Google Scholar]
- 30.Huang SL, Shiao G, Chou P. Association between body mass index and allergy in teenage girls in Taiwan. Clin Exp Allergy. 1999;29(3):323–329. doi: 10.1046/j.1365-2222.1999.00455.x [DOI] [PubMed] [Google Scholar]
- 31.Chen Y, Dales R, Tang M, Krewski D. Obesity may increase the incidence of asthma in women but not in men: longitudinal observations from the Canadian National Population Health Surveys. Am J Epidemiol. 2002;155(3):191–197. doi: 10.1093/aje/155.3.191 [DOI] [PubMed] [Google Scholar]
- 32.Hersoug LG, Linneberg A. The link between the epidemics of obesity and allergic diseases: does obesity induce decreased immune tolerance? Allergy. 2007;62(10):1205–1213. doi: 10.1111/j.1398-9995.2007.01506.x [DOI] [PubMed] [Google Scholar]
- 33.Guler N, Kirerleri E, Ones U, Tamay Z, Salmayenli N, Darendeliler F. Leptin: does it have any role in childhood asthma? J Allergy Clin Immunol. 2004;114(2):254–259. doi: 10.1016/j.jaci.2004.03.053 [DOI] [PubMed] [Google Scholar]
- 34.Sood A, Ford ES, Camargo CA. Association between leptin and asthma in adults. Thorax. 2006;61(4):300–305. doi: 10.1136/thx.2004.031468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shore SA, Schwartzman IN, Mellema MS, Flynt L, Imrich A, Johnston RA. Effect of leptin on allergic airway responses in mice. J Allergy Clin Immunol. 2005;115(1):103–109. doi: 10.1016/j.jaci.2004.10.007 [DOI] [PubMed] [Google Scholar]
- 36.Melen E, Kere J, Pershagen G, Svartengren M, Wickman M. Influence of male sex and parental allergic disease on childhood wheezing: role of interactions. Clin Exp Allergy. 2004;34(6):839–844. doi: 10.1111/j.1365-2222.2004.01957.x [DOI] [PubMed] [Google Scholar]
- 37.Halonen M, Stern D, Lyle S, Wright A, Taussig L, Martinez FD. Relationship of total serum IgE levels in cord and 9 month sera of infants. Clin Exp Allergy. 1991;21(2):235–241. doi: 10.1111/j.1365-2222.1991.tb00836.x [DOI] [PubMed] [Google Scholar]
- 38.Burney P, Malmberg E, Chinn S, et al. The distribution of total and specific serum IgE in the European Community Respiratory Health Survey. J Allergy Clin Immunol. 1997;99(3):314–322. doi: 10.1016/S0091-6749(97)70048-4 [DOI] [PubMed] [Google Scholar]
- 39.Ali F. A survey of self-reported food allergy and food-related anaphylaxis among young adult students at Kuwait University, Kuwait. Med Principles Practice. 2017;26(3):229–234. doi: 10.1159/000464361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Acker WW, Plasek JM, Blumenthal KG, et al. Prevalence of food allergies and intolerances documented in electronic health records. J Allergy Clin Immunol. 2017;140(6):1587–1591.e1. doi: 10.1016/j.jaci.2017.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boyce JA, Assa’ad A, Burks AW. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 Suppl):S1–58. doi: 10.1016/j.jaci.2010.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gupta RS, Springston EE, Warrier MR, et al. The Prevalence, Severity, and Distribution of Childhood Food Allergy in the United States. Pediatrics. 2011;128(1):e9–e17. doi: 10.1542/peds.2011-0204 [DOI] [PubMed] [Google Scholar]
- 43.Elghoudi A, Narchi H. Food allergy in children—the current status and the way forward. World J Clin Pediatr. 2022;11(3):253–269. doi: 10.5409/wjcp.v11.i3.253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Irani C, Maalouly G. Prevalence of self-reported food allergy in Lebanon: a Middle-Eastern taste. Int Sch Res Notices. 2015;2015. doi: 10.1155/2015/639796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Akarsu A, Ocak M, Köken G, Şahiner ÜM, Soyer Ö, Şekerel BE. Ige mediated food allergy in Turkey: different spectrum, similar outcome. Turk J Pediatr. 2021;63(4):554. doi: 10.24953/turkjped.2021.04.002 [DOI] [PubMed] [Google Scholar]
- 46.Seth D, Poowutikul P, Pansare M, Kamat D. Food allergy: a review. Pediatr Ann. 2020;49(1):e50–e58. doi: 10.3928/19382359-20191206-01 [DOI] [PubMed] [Google Scholar]
- 47.Dey D, Ghosh N, Pandey N, Bhattacharya SG. A hospital-based survey on food allergy in the population of Kolkata, India. Int Arch Allergy Immunol. 2014;164(3):218–221. doi: 10.1159/000365629 [DOI] [PubMed] [Google Scholar]
- 48.Mandal J, Das M, Roy I, Chatterjee S, Barui NC, Gupta-Bhattacharya S. Immediate hypersensitivity to common food allergens: an investigation on food sensitization in respiratory allergic patients of Calcutta, India. World Allergy Org J. 2009;2(1):9–12. doi: 10.1097/WOX.0b013e318194c0de [DOI] [PMC free article] [PubMed] [Google Scholar]