Abstract
Objective
To present an approach to build capacity for the use of systems science to support local communities in municipal public health and well-being planning.
Design
Case study.
Setting
Local government authorities participating in the VicHealth Local Government Partnership in Victoria, Australia.
Participants
Local government staff members were trained in community-based system dynamics (CBSD), and group model building (GMB) techniques to mobilise local community efforts. The trained local government facilitation teams then delivered GMB workshops to community stakeholder groups from 13 local government areas (LGA)s.
Main outcomes
Training in CBSD was conducted with council facilitation teams in 13 LGAs, followed by the local delivery of GMB workshops 1–3 to community stakeholders. Causal loop diagrams (CLD) representing localised drivers of mental well-being, healthy eating, active living or general health and well-being of children and young people were developed by community stakeholders. Locally tailored action ideas were generated such as well-being classes in school, faster active transport and access to free and low-cost sporting programmes
Results
Overall, 111 local government staff participated in CBSD training. Thirteen CLDs were developed, with the stakeholders that included children, young people and community members, who had participated in the GMB workshops across all 13 council sites. Workshop 3 had the highest total number of participants (n=301), followed by workshop 1 (n=287) and workshop 2 (n=171).
Conclusions
Local facilitation of the CBSD process has developed community informed and locally relevant CLDs that will be used to lead local action to improve the well-being of children and young people. Training employees in CBSD is one approach to increase systems thinking capacity within local government.
Keywords: public health, qualitative research, community child health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
We trained a labour force to become systems thinkers to develop community stakeholder informed actions to improve the health and well-being of children and young people.
We used a systems mapping software programme that enabled participants to develop Causal Loop Diagrams (CLDs) online and to observe the interconnected determinants of health and well-being.
It is unknown if there were gaps in council facilitation teams’ knowledge as they progressed from workshop training to systems thinking facilitation.
The utility of the systems mapping software used to develop CLDs was not measured.
Introduction
Obesity is a worldwide health priority.1 Obesity prevalence has continued to increase over recent decades and is conservatively estimated to cost US$2 trillion per year or 2.8% of global Gross Domestic Product (GDP).2 In Australia, 25% of children (aged 5–17 years of age) are overweight or obese3 and are at greater risk of lower self-rated health-related quality of life (HRQol), depression,4–6 and experience comorbidities such as type 2 diabetes and hypertension.7 Obesity prevention among children is critical as obesity strongly tracks into adulthood, highlighting the need for early intervention.8
A key challenge for chronic disease prevention is to address the complex relationships between the societal causes of preventable disease.9 Historically, prevention efforts have centred on small groups of actors in single sectors targeting individualistic behavioural outcomes with limited success.9 Implementation at scale has been further challenged by the need for adaption across settings, without which intervention effects are reduced by inflexibility to heterogeneity in community resources, readiness and environments, among other potential reasons.10 11
Whole-of-community approaches12 to prevention are more likely to succeed and be sustained where systems-based methods support understanding the community, environmental, social and economic drivers of disease, and by focusing on capacity-building within communities to address this challenge.13 14 Methods from system science, like Group Model Building (GMB) and causal loop diagramming (CLD), provide means to understand the complex drivers of preventable disease by describing non-linear relationships of cause and effect, feedback loops and adaption.14 15 Several examples of whole-of-community systems-based prevention trials (eg, communities randomised to intervention or control12) exist in the literature at a multi-community scale.16–18 Scaling and embedding these methods at the local government level, to support regulatory intervention and build capacity to support government health planning remains an important next step.18 Local government is a particularly desirable setting for systems-based approaches due to council’s regulatory remit over a range of environmental and policy levers, and the potential for regulatory interventions to create sustainable, equitable changes and to ameliorate the impacts of harmful system drivers (eg, the built environment and marketing).13 18
Development of frameworks to embed these methods within local government are emerging internationally, examples include Public Health England’s (PHE) local government whole systems approach to address obesity.19 Several councils and boroughs across England have utilised the programme to operationalise local-led approaches to obesity by engaging with their local stakeholders to implement systems change across the community.19 In 2019, PHE launched the Whole Systems Approach to Obesity: a guide to support local approaches to promoting a healthy weight programme for local governments across England, which includes systems mapping of obesity drivers with community stakeholders as a central tool.19
In 2020, VicHealth initiated the ‘VicHealth Local Government Partnership:Young people leading healthier communities’ (VLGP). The partnership aims to create community environments where children and young people aged 0–25 years could become physically active, socially connected and mentally healthy.20 The VLGP currently includes 13 metropolitan, regional and rural Victorian Local Governments, using systems thinking methods to direct, and guide municipal chronic disease prevention in young people.20
This paper describes the design of a framework to embed systems thinking as a guiding principle for the delivery of municipal prevention of chronic disease in children and young people. The specific approach to systems dynamics is outlined, alongside the processes used to initially build councils’ capacity, and ongoing support mechanisms to guide continued use of the systems thinking methods. Some results reflecting early outcomes from the local communities are provided.
Methods
Study design and data collection
Study context
The state of Victoria, south-eastern Australia, has a population of ~6.7 million people and is composed of 79 local government areas (LGA).21 Individual LGAs vary broadly across various measures including geographical size, population density, rurality and cultural and linguistic diversity.21 Overall, 28% of Victorians were born overseas and 26% speak a language other than English.21
VLGP overview and modules
The VLGP represents a partnership approach to building capacity for evidence-based prevention at the local government level. Councils were invited to apply to join the VLGP through a competitive process, initially open to the 39 Victorian councils with an Index of Relative Social Disadvantage (IRSD) of 1–5 and with health and well-being needs, between the lower and higher IRSD LGAs.22 The 21 submitted applications then underwent a scoring process, followed by an assessment panel discussion. Of the 21 council applications, 16 were selected to take part in the partnership, with 3 in a modified partnership arrangement, which allowed for 1 of the VLGP foundation modules to be omitted from their programme.
The VLGP provides support to the 13 partner councils to develop and deliver evidence-based action to improve children and young people’s health and well-being through the mechanism of councils’ Municipal Public Health and Wellbeing Plans (MPHWP).20 In Victoria, the state government mandates that councils develop 4-year MPHWP, that guide strategic direction and priorities for municipal health promotion relative to a locally tailored set of priorities, taken from identified state-level drivers of poor health and health inequity.23
The key outcomes of the VLGP are to foster improvements in the capacity of councils to deliver evidence-based action in the implementation of their MPHWP, the promotion of the voices of children and young people into local government policy decisions and action, and improved rates of healthy eating, physical activity and social connectedness among young people aged 0–25 by the end of 2025.20
Eight evidenced-informed health promotion modules were developed to serve as a series of practical, ‘how-to guides’ for policy, programme development/delivery and practice change. These guides were devised to support councils to implement action at the local level to create healthier communities for children and young people.20 The eight modules were designed to consolidate the practice knowledge, experience and research developed from the close collaboration between VicHealth, local governments and expert partners. Each module included several impact streams, each of which included a number of evidence-informed implementation actions or key policy, programme and practice changes relative to the theme of the module. The modules were divided into three categories, namely: Foundation, Core and Stretch (table 1).20
Table 1.
The VicHealth Local Government Partnership (VLGP) modules and impact streams20
| Modules and impact streams | |
| Foundation modules: Compulsory modules that provided the basic building blocks to develop staff capabilities and skills in systems-thinking and engagement with children and young people in planning, policies and programmes | Connecting the Dots—creating solutions for lasting change Big picture thinking for better solutions Leading the Way—engaging young voices for change: Including children and young people in policy creation; Including children and young people in planning |
| Core modules: Evidence-based activities, designed to address childhood obesity | Building active communities: Increasing active travel to and from school; Increasing walking and bike riding in council strategies; Creating opportunities for all Victorians to be active; Including gender equity in council sport and recreation policy; Empowering and enabling women to get active through local promotion of ‘This Girl Can-Victoria’ Creating connected and supportive communities: Co-designing with young people for better community well-being; Building proud and inclusive communities; Addressing social determinants of mental well-being Building better food systems for healthier communities: Creating thriving local food systems; Embedding healthy food and drink options in council owned and operated places; Using healthy rewards and sponsorships in community activities; Enabling healthy partnerships |
| Stretch modules: Optional modules that built on essential health policy priorities to promote healthy environments for children and young people | Increasing alcohol harm prevention at a local level: Adopting alcohol harm prevention actions to protect children and young people Strengthening tobacco control at a local level: Adopting tobacco control actions to protect children and young people Promoting everyday creativity at a local level: Increasing equity in creative strategies; Embracing opportunities for children to inform creative programmes; Improving opportunities for young people to lead creative programmes |
Connecting the Dots
The Connecting the Dots (CtD) foundation module contained one impact stream with two required implementation actions, which consisted of structured training workshops (block 1) and the delivery of systems thinking approaches (block 2) (table 2).20
Table 2.
VicHealth Local Government Partnership (VLGP) Connecting the Dots foundation module20
| Connecting the Dots—creating solutions for lasting change | ||
| Impact stream | Implementation action | Formal training & support |
| Big picture thinking for better solutions | Understanding systems thinking approaches | Block 1—Fundamentals in systems thinking and facilitation |
| Actioning new systems thinking approaches | Block 2—Workshop preparation and delivery support | |
Understanding systems thinking approaches: fundamentals in systems thinking and facilitation
This stream consisted of a series of training sessions (block 1) designed to quickly upskill (~10 hours pivoted to online learning in some cases due to COVID-19, work from home and travel restrictions) council core facilitation teams on: (1) the basics of systems thinking including the fundamental skills around concepts and language and (2) community-based systems dynamics (CBSD) and GMB workshop facilitation process via participation in facilitated demonstrations and guided facilitation practice.20
Initial plans for local delivery of the workshop process, including context/framing, facilitation team membership, key participant groups and engagement/workshop timelines were also covered. The use of the Systems Thinking in Community Knowledge Exchange (STICKE) systems mapping software program (STICKE Version 3 Deakin University) was used throughout the training as it allows council and community members to build CLDs using a supported online process24
Regional advisors and a central coordination team comprising academic and practitioner experts in systems thinking methodologies from Deakin University and local government representatives comprised the CtD team. The regional advisors worked closely with their nominated councils (2–3 councils each) to deliver training and provide continued implementation support and guidance. Partner councils established core facilitation teams to lead and deliver the actioning of new systems thinking approaches. Each team consisted of a VicHealth funded project officer based at the local councils and other council employees overseeing the MPHWP. Additional staff involved in child/youth health and community engagement and non-council staff were also nominated for training. Approximately, 2–10 persons undertook the training sessions within each council. The Fundamentals in Systems Thinking & Facilitation impact stream was completed in full before councils began delivering participatory GMB workshops with the community.
Actioning new systems thinking approaches: workshop preparation and delivery
This impact stream included a series of online seminars (~10 hours) designed to support council teams scheduled alongside the delivery of community based GMB workshops (block 2). The preparation seminars covered various topics and focused closely on supporting council teams as they negotiated the tasks and preparations relative to the stages of GMB workshop delivery.20
Council core facilitation teams delivered at least three participatory GMB workshops of ~1–3 hours to groups of community stakeholders from each of the 13 partner LGAs (table 3). Stakeholders included young people, children, community leaders and diverse community members drawn from across all sectors including local government, non-government organisations, small business, commercial sector, education, community organisations and healthcare providers. Stakeholders were recruited by partner councils through existing networks, emails, expressions of interest and advertisements.
Table 3.
Summary of the Victorian Local Government Partnership (VLGP) Group Model Building (GMB) workshop process
| GMB workshop | Duration (minutes) | Participant capacity | Objectives |
| 1 | 120 | 5–25 participants | Orientation of participants to VLGP project, local context for work and GMB process to be undertaken. Development of initial systems map. |
| 2 | 120 | 5–25 participants | Refinement of systems map based on revisions since workshop 1 and further conversation and consideration of health and well-being determinants. Optionally: Discussion of preliminary insights on potential focal points on systems map for community-led action and potential additional invitees and recruitment strategies for workshop 3. |
| 3 | 180 | 5–25 participants (with option to extend up to 100 participants) | Introduction and orientation to systems map for new participants if required. Further discussion of if required. Further discussion of workshop 2. Facilitated discussion and prioritisation of potential community-led actions identified in response to insights from systems map. |
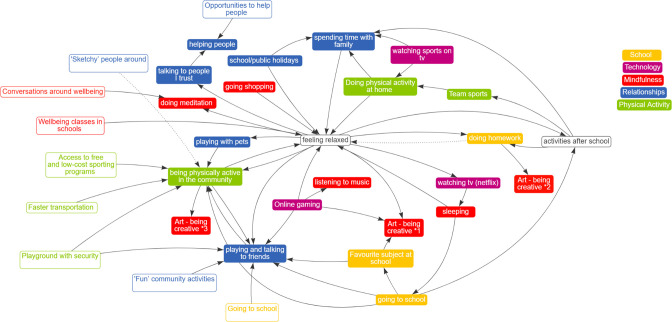
Together, council core facilitation teams and workshop participants created a CLD of the locally relevant drivers of health and well-being of children and/or young people in their community and determined the highest-priority leverage points for action. The method used to generate the systems map in the form of a CLD was the GMB technique, which is a structured collaborative CBSD methodology, designed to guide participants through developing hypotheses about the connections between various contributing factors in complex problems.14 A set of scripts used in the GMB workshops (graphs over time, connection circles and action ideas) were used to guide workshop content and help stakeholders develop CLDs25 The CLDs highlighted drivers of childhood health and the complex, non-linear relationships between those drivers. The structured workshop process resulted in a CLD which represented a view on the systems components, relationships and boundaries (figure 1)14 (see online supplemental file 1 for a summary of CtD framework).
Figure 1.
An example of a casual loop diagram showing the variables, themes and the actions ideas generated by stakeholders from one of the VicHealth Local Government Partnership councils.
bmjopen-2022-068190supp001.pdf (24.4KB, pdf)
Following the completion of the participatory systems mapping and community engagement process, council facilitation teams were supported by the CtD team to use the CLD developed by the group to guide the identification and prioritisation of stakeholder informed actions ideas that can be applied in the community to support children and young people’s health during 2022–2025. These will be driven by their own CLD and informed by evidence including case studies from previous successful interventions.26 Community actions will be recorded throughout the duration of the project, including tracking against the systems map in STICKE. Forthcoming publications will examine the implications of local community contexts and priorities on the precise adaptations to process undertaken by individual councils.
Patient and public involvement
None.
Results
All 13 partner councils had participated in the initial systems training, with 111 total staff (>18 years of age) attending the training across all councils. Individual facilitation teams based at the councils included a funded project officer and between 3 and 12 additional staff including council employees involved in child/youth health and community engagement, and staff from external community organisations collaborating with councils, such as sports facilities or health services. All 13 partner councils delivered GMB workshops 1–3 face to face and online (due to COVID-19 and travel restrictions). In some instances, workshops were combined, for example, workshop 1 was combined with workshop 2 and delivered together as one session (due to time constraints and capacity of council staff). The workshop participants included either young people or stakeholders with the exception of workshop 3, which included young people and stakeholders together (conducted by three councils) (table 4).
Table 4.
Total number of participants who attended the Group Model Building workshops from the 13 partner local government authorities
| Workshop 1 | Workshop 2 | Workshop 3 | Combined workshop 1 and 2 | Combined workshop 2 and 3 | |
| Participants (n) | |||||
| Young people | 174 | 99 | 128 | 52 | 9 |
| Stakeholders | 113 | 72 | 90 | 7 | 20 |
| Combination of both young people and stakeholders | − | − | 83 | − | − |
| Total participants | 287 | 171 | 301 | 59 | 29 |
All councils successfully created CLDs, with community stakeholders including: children and young people, the local prevention workforce, service providers, policy and decision-makers, and grass-roots community members from sectors including local government, non-government organisations, small business, education, community organisations and healthcare providers. The diagrams resulting from the workshop process were similar in range and scope to other prevention efforts which have used these methods across multiple community sites in Victoria.26 For example, each council’s diagram included the typical elements of a CLD: variables (determined by stakeholders as influencing the health and well-being of children and young people in the community, eg, junk food), the connections between the variables, actions (eg, banning sugary drinks from sporting clubs) and overarching themes. An example of a council CLD with five themes (eg, relationships, physical activity) and nine action ideas (eg, well-being classes in school, faster transportation, access to free and low-cost sporting programmes) identified by stakeholders is shown in figure 1.
Discussion
This paper describes the capacity building of local councils to use systems thinking and participatory methods within local governments to inform the implementation of MPHWP. The council facilitation teams demonstrated complex systems science practice to develop CLDs with community stakeholders (with an understanding of systems theory) which can then act as basic logic models for community led action and implementation.
The logic underpinning the approach used in CtD has been published previously and posits that building and sustaining capacity for work informed by CBSD methods increases leadership and organisational engagement with prevention, and collaboration across community organisations, which generates higher quality, more sustainable outcomes within communities.27 We observed that local stakeholder informed prevention designs allowed for differences between communities and adaption to the local context rather than a predefined programme of work. The effectiveness of this locally informed prevention approach and community capacity building has been reported in previous trials, for example, Whole of Systems Trial of Prevention Strategies for Childhood Obesity (WHO STOPS),26 Romp and Chomp,28 It’s Your Move,29 Be Active Eat Well.30
There is an increased focus using systems thinking at local community level to improve population health. Recent examples include PHE’s support for whole of systems change, given to all 408 UK local authorities and potentially impacting 55M people.19 The UK’s guidance also calls for action at local communities and emphasises the development of shared models of the complexity within community, using a range of techniques from GMB. Our systems guidance incorporated into the CtD module has arisen from several trials of systems thinking in obesity prevention results, notably trials in schools (eg, ‘It’s Your Move 231) and local communities.32 These trials began with a heavy investment of researcher support in assisting doing systems science12 and then moved to building capacity and supporting people within local communities to deliver and evolve systems thinking in situ.32 These types of systems thinking approaches may also support First Nation rural communities.33
Our results, and these implications for practice, parallel early trials of systems thinking in health. For example, Healthy Together Victoria (HTV), was a large-scale initiative that applied a ‘complex whole of systems approach’ to the prevention of chronic disease.34 HTV provides many pointers to future practice and built a workforce of system thinkers from across the state in local government, community health and non-government organisations to implement a range of actions at the community and state level.34 35 The VLGP builds on one of the key lessons from HTV: the challenge to identify the most effective ways to support communities to deliver a systems approach at a local level.34–36 This project shows that providing capacity building in systems thinking, can support council staff to access and apply knowledge from Deakin University’s >20 years’ experience in complex systems thinking and community-based obesity prevention.26 28–30 We observed that the strong organisational and structural factors such as researcher support and regional advisors who provided continued support allowed the novice council facilitation teams to build confidence while developing their practical know-how for systems thinking in the community setting.
Building local capacity likely creates positive change within communities. This is shown in outcomes of previous trials like WHO STOPS, which catalysed >300 community members to drive >400 actions ranging from council food policy, soft drink bans and active transport strategies.26 As a result, WHO STOPS showed initial reductions in overweight and obesity in the first 2 years of intervention, compared with no change in the control group,26 however, these were not sustained. The longer-term outcomes (4 years) demonstrated significant maintenance of HRQol, reduced takeaway, nutrient-poor snack consumption (boys only) and water consumption (girls only) favouring intervention children compared with controls. Highlighting for the first time that long-term behavioural and HRQol improvements are possible using a whole of community systems approach to childhood obesity.26
The CtD module represents one of the first efforts to build systems thinking capacity among local government staff, which provided the opportunity for the trained labour force to become systems thinkers and identified stakeholder informed actions for their communities to enhance the health and well-being of children and young people. This was demonstrated by their ability to observe the interconnected determinants of health and well-being through the use of CLDs. A well-scripted systematic and rigorous approach to using systems science was applied during the CtD workshops and GMB sessions. A well-structured training manual written by our CtD team and based on a similar format to our previous community-based interventions allowed for the training to be standardised across the 13 partner councils.
There is limited evidence about the sustainability of health and well-being, community-led change. As noted with the 4-year WHOSTOPS trial, which positively impacted children’s health, the long-term (>2 years) sustainability of community-based action is still understudied.26 A key limitation is the assessment of the quality and effectiveness of the training materials used in the delivery of systems thinking facilitation, teaching of specific skills and knowledge, the training methods and participant’s use of the online platform. For example, it is unknown if there were gaps in participants’ knowledge as they progressed from workshop training to systems thinking facilitation. The use of STICKE enabled participants to create CLDs online and has been considered to be useful by participants.24 However, we did not measure the utility of the STICKE software. It is possible that the functionality of the STICKE software requires updating to accommodate upscaling to larger interventions across numerous geographical areas. Pivoting to online learning (following COVID-19 restrictions), for the staff training ensured good participation and appears to be efficient in facilitating GMB rather than in person delivery, although this may differ across the metropolitan, regional and rural LGAs. However, we did not gather evidence to support this approach.
Future research
The future of chronic disease prevention is pointing to the cocreation of systemic change supporting communities using techniques to address complexity; a move from single behaviour, individual focus to a consideration of wholistic relations of cause and effect across multiple levels of community action.11 As the Lancet Commission on Obesity shows, this has implications for science, as the approach is less amenable to randomised controlled trials and more suited to implementation and hybrid studies, as it places the control of the effort in the hands of communities, at the agreed expense of intervention fidelity and generalisability.11
This paper and our broader community behaviour intervention research26 30–32 raises some questions for future studies: What should the user interface and user experience look like? For example, could gamification, where the use of game thinking in a non-game context to engage users and to solve problems, be included as part of the systems thinking toolkit? Could an accreditation system where the recognition of communities that meet the requirements of certain standards be applied? Does this systems approach improve health? Can this approach be transferred to tackle other complex issues beyond obesity prevention? Can prior experience with community-based action on childhood obesity provide communities with the fundamentals to apply systems science thinking to other areas of community concern such as recovery plans from major disasters such as bushfire, floods and COVID-19 and the development of strategies for climate change resilience?
Conclusion
This paper has provided an example of establishing the capacity of a government workforce by developing their knowledge and understanding of systems theories tools and practice. An emphasis on the process to create change, but not at the expense of local empowerment and adaptability should be considered when planning the implementation of systems science at the local government level.
Supplementary Material
Acknowledgments
We wish to acknowledge the Victorian Health Promotion Foundation (VicHealth), which funded the VicHealth Local Government Partnership.
Footnotes
Twitter: @OhSiobhan
Contributors: SO'H, SA and JH conceptualised the study. SO'H conducted the literature search, led the drafting and the revision of the manuscript and prepared the manuscript for publication. SO'H accepted full responsibility for the work of the study, had access to the data and controlled the decision to publish as guarantor. SA supervised the study and provided overall guidance. JH contributed significantly to the revision of the manuscript with inputs from SA, TF, CN, SK, ER, JP, PF, AD, CS. All authors contributed to subsequent revisions and approved the manuscript prior to submission.
Funding: SO'H, JH, JP, TF, CN, PF, SK, ER and AD are supported by VicHealth N/A award/grant number. CS was a researcher within a NHMRC Centre for Research Excellence in Obesity Policy and Food Systems (GNT1114118). SA is a lead investigator receiving funding from VicHealth and Australian National Health and Medical Research Council grant (GNT1133090).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Deakin University Human Research Ethics Committee HEAG-H-121_2022. Participants gave informed consent to participate in the study before taking part.
References
- 1.Lobstein T, Jackson-Leach R, Moodie ML, et al. Child and adolescent obesity: part of a bigger picture. Lancet 2015;385:2510–20. 10.1016/S0140-6736(14)61746-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dobbs R, Sawers C, Thompson F, et al. A. overcoming obesity: an initial economic analysis. Jakarta, Indonesia: McKinsey Global Institute, 2014. [Google Scholar]
- 3.Australian Bureau of Statistics . 4364.0.55.001National health survey: first results, 2017–18, 2018. Available: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/latest-release [Accessed 15 Feb 2022].
- 4.Goldfield GS, Moore C, Henderson K, et al. Body dissatisfaction, dietary restraint, depression, and weight status in adolescents. J Sch Health 2010;80:186–92. 10.1111/j.1746-1561.2009.00485.x [DOI] [PubMed] [Google Scholar]
- 5.Hoare E, Crooks N, Hayward J, et al. Associations between combined overweight and obesity, lifestyle behavioural risk and quality of life among Australian regional school children: baseline findings of the Goulburn Valley health behaviours monitoring study. Health Qual Life Outcomes 2019;17:16. 10.1186/s12955-019-1086-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanders RH, Han A, Baker JS, et al. Childhood obesity and its physical and psychological co-morbidities: a systematic review of Australian children and adolescents. Eur J Pediatr 2015;174:715–46. 10.1007/s00431-015-2551-3 [DOI] [PubMed] [Google Scholar]
- 7.Lobstein T, Jackson-Leach R. Planning for the worst: estimates of obesity and comorbidities in school-age children in 2025. Pediatr Obes 2016;11:321–5. 10.1111/ijpo.12185 [DOI] [PubMed] [Google Scholar]
- 8.Singh AS, Mulder C, Twisk JWR, et al. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008;9:474–88. 10.1111/j.1467-789X.2008.00475.x [DOI] [PubMed] [Google Scholar]
- 9.Finegood DT, Merth TDN, Rutter H. Implications of the Foresight obesity system map for solutions to childhood obesity. Obesity 2010;18 Suppl 1:S13–16. 10.1038/oby.2009.426 [DOI] [PubMed] [Google Scholar]
- 10.McCrabb S, Lane C, Hall A, et al. Scaling-up evidence-based obesity interventions: a systematic review assessing intervention adaptations and effectiveness and quantifying the scale-up penalty. Obes Rev 2019;20:964–82. 10.1111/obr.12845 [DOI] [PubMed] [Google Scholar]
- 11.Swinburn BA, Kraak VI, Allender S, et al. The global Syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet 2019;393:791–846. 10.1016/S0140-6736(18)32822-8 [DOI] [PubMed] [Google Scholar]
- 12.Allender S, Millar L, Hovmand P, et al. Whole of systems trial of prevention strategies for childhood obesity: who stops childhood obesity. Int J Environ Res Public Health 2016;13:1143. 10.3390/ijerph13111143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet 2011;378:804–14. 10.1016/S0140-6736(11)60813-1 [DOI] [PubMed] [Google Scholar]
- 14.Hovmand PS. Group Model Building and Community-Based System Dynamics Process. In: Community based system dynamics. New York: Springer, 2014: 163–96. [Google Scholar]
- 15.World Health Organization . Systems thinking for noncommunicable disease prevention policy:guidance to bring systems approaches into practice, 2022. Available: https://www.who.int/europe/publications/i/item/WHO-EURO-2022-4195-43954-61946 [Accessed 10 Nov 2022].
- 16.Brennan LK, Sabounchi NS, Kemner AL, et al. Systems thinking in 49 communities related to healthy eating, active living, and childhood obesity. J Public Health Manag Pract 2015;21 Suppl 3:S55–69. 10.1097/PHH.0000000000000248 [DOI] [PubMed] [Google Scholar]
- 17.Sawyer A, den Hertog K, Verhoeff AP, et al. Developing the logic framework underpinning a whole-systems approach to childhood overweight and obesity prevention: Amsterdam healthy weight approach. Obes Sci Pract 2021;7:591–605. 10.1002/osp4.505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allender S, Gleeson E, Crammond B, et al. Moving beyond 'rates, roads and rubbish': How do local governments make choices about healthy public policy to prevent obesity? Aust New Zealand Health Policy 2009;6:20. 10.1186/1743-8462-6-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Public Health England . Whole systems approach to obesity: a guide to support local approaches to promoting a healthy weight, 2019. Available: https://www.gov.uk/government/publications/whole-systems-approach-to-obesity [Accessed 23 Mar 2022].
- 20.VicHealth . VicHealth Local Government Partnerships, 2022. Available: https://www.vichealth.vic.gov.au/programs-and-projects/local-government-partnership [Accessed 01 Feb 2022].
- 21.Australian Bureau of Statistics. Available: https://www.abs.gov.au/ [Accessed 22 Feb 2022].
- 22.Australian Bureau of Statistics . Socio-Economic Indexes for Areas (SEIFA) - Technical Paper, 2006. Canberra: Australian Bureau of Statistics, 2008. [Google Scholar]
- 23.Victorian Government Department of Health . Public Health and Wellbeing Planning. Available: https://www.health.vic.gov.au/health-strategies/public-health-and-wellbeing-planning [Accessed 02 Mar 2022].
- 24.Hayward J, Morton S, Johnstone M, et al. Tools and analytic techniques to synthesise community knowledge in CBPR using computer-mediated participatory system modelling. NPJ Digit Med 2020;3:22. 10.1038/s41746-020-0230-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hovmand PS, Andersen DF, Rouwette E. Group Model-Building ‘Scripts’ as a Collaborative Planning Tool. Syst Res Behav Sci 2012;29:179–93. 10.1002/sres.2105 [DOI] [Google Scholar]
- 26.Allender S, Orellana L, Crooks N, et al. Four-Year behavioral, health-related quality of life, and BMI outcomes from a cluster randomized whole of systems trial of prevention strategies for childhood obesity. Obesity 2021;29:1022–35. 10.1002/oby.23130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown AD, Whelan J, Bolton KA, et al. A theory of change for community-based systems interventions to prevent obesity. Am J Prev Med 2022;62:786–94. 10.1016/j.amepre.2021.10.006 [DOI] [PubMed] [Google Scholar]
- 28.de Silva-Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr 2010;91:831–40. 10.3945/ajcn.2009.28826 [DOI] [PubMed] [Google Scholar]
- 29.Millar L, Kremer P, de Silva-Sanigorski A, et al. Reduction in overweight and obesity from a 3-year community-based intervention in Australia: the 'It's Your Move!' project. Obes Rev 2011;12 Suppl 2:20–8. 10.1111/j.1467-789X.2011.00904.x [DOI] [PubMed] [Google Scholar]
- 30.Sanigorski AM, Bell AC, Kremer PJ, et al. Reducing unhealthy weight gain in children through community capacity-building: results of a quasi-experimental intervention program, be active eat well. Int J Obes 2008;32:1060–7. 10.1038/ijo.2008.79 [DOI] [PubMed] [Google Scholar]
- 31.Malakellis M, Hoare E, Sanigorski A, et al. School-based systems change for obesity prevention in adolescents: outcomes of the Australian Capital Territory 'It's Your Move!'. Aust N Z J Public Health 2017;41:490–6. 10.1111/1753-6405.12696 [DOI] [PubMed] [Google Scholar]
- 32.Bolton KA, Fraser P, Lowe J, et al. Generating change through collective impact and systems science for childhood obesity prevention: the GenR8 change case study. PLoS One 2022;17:e0266654. 10.1371/journal.pone.0266654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beks H, Amos T, Bell J, et al. Participatory research with a rural aboriginal community controlled health organisation: lessons learned using the consider statement. Rural Remote Health 2022;22:6740. 10.22605/RRH6740 [DOI] [PubMed] [Google Scholar]
- 34.Strugnell C, Millar L, Churchill A, et al. Healthy together Victoria and childhood obesity-a methodology for measuring changes in childhood obesity in response to a community-based, whole of system cluster randomized control trial. Arch Public Health 2016;74:16. 10.1186/s13690-016-0127-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bensberg M, Allender S, Sacks G. Building a systems thinking prevention workforce. Health Promot J Austr 2020;31:436–46. 10.1002/hpja.325 [DOI] [PubMed] [Google Scholar]
- 36.Bensberg M. Developing a systems Mindset in community-based prevention. Health Promot Pract 2021;22:82–90. 10.1177/1524839919897266 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-068190supp001.pdf (24.4KB, pdf)
Data Availability Statement
Data are available on reasonable request.