Abstract
Objective
To assess the prognostic value of absolute and sex-specific, age-specific and race/ethnicity-specific (Multi-Ethnic Study of Atherosclerosis, MESA) percentiles of coronary artery calcification in symptomatic women and men.
Methods
The study population consisted of 4985 symptomatic patients (2793 women, 56%) visiting a diagnostic outpatient cardiology clinic between 2009 and 2018 who were referred for cardiac CT to determine Coronary Artery Calcium Score (CACS). Regular care data were used and these data were linked to the databases of Statistics Netherlands for all-cause mortality data. Kaplan-Meier curves, multivariate Cox proportional hazards regression and concordance statistics were used to evaluate the prognostic value of CACS and MESA percentiles. Women were older compared with men (60 vs 59 years).
Results
Median CACS was 0 (IQR: 0–54) in women and 42 (IQR: 0–54) in men. After a median follow-up of 4.4 years (IQR: 3.1–6.3), 116 (2.3%; 53 women and 63 men) patients died. MESA percentiles did not perform better compared with absolute CACS (C-statistic 0.65, 95% CI 0.57 to 0.73, vs 0.66, 95% CI 0.58 to 0.74, in women and 0.59, 95% CI 0.51 to 0.67, vs 0.62, 95% CI 0.55 to 0.69, in men, for the percentiles and absolute CACS, respectively).
Conclusions
In symptomatic individuals absolute CACS predicts mortality with a moderately good performance. MESA percentiles did not perform better compared with absolute CACS, thus there is no need to use them. Including degree of stenosis in the model might slightly improve mortality risk prediction in women, but not in men.
Keywords: CORONARY ARTERY DISEASE, Computed Tomography Angiography, Coronary Stenosis, Electronic Health Records
WHAT IS ALREADY KNOWN ON THIS TOPIC
In asymptomatic women and men, calcification of the coronary arteries is a strong predictor for mortality.
WHAT THIS STUDY ADDS
Validation of commonly used calcification measures in a large real-word patient population.
In symptomatic patients at cardiac outpatient clinics, absolute and Multi-Ethnic Study of Atherosclerosis (MESA) percentiles of Coronary Artery Calcium Score (CACS) predict mortality equally well.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
In symptomatic patients, simple absolute CACS can be used instead of additional calculation of MESA percentiles.
In this study, the hypothesis was generated that in future studies the focus should be broadened from CACS only to non-calcified plaques as well to further improve risk prediction in symptomatic women and men.
Introduction
In asymptomatic women and men, calcification of the coronary arteries is proven to be a strong predictor for mortality.1 In individuals with symptoms suspicious for cardiac disease, but without coronary artery calcification, the presence of obstructive coronary artery disease (CAD) is low, and their long-term prognosis is good.2 However, the value of coronary artery calcification in these symptomatic individuals is not well established.3
Non-contrast-enhanced CT and coronary CT angiography are used to evaluate the calcification of the coronary arteries. Based on the results of this diagnostic assessment, the amount of coronary artery calcium (CAC) is quantified by the CAC Score (CACS) according to Agatston.4 CACS, as a continuous variable, is often categorised for clinical use.5–7
Several studies demonstrated sex differences in the amount and type of atherosclerotic plaques in symptomatic patients. Development of coronary artery calcification is on average delayed by 10 years in symptomatic women compared with men and onset of coronary artery calcification starts at an earlier age in men than in women.5 8 Furthermore, symptomatic men mostly have calcified plaques while women predominantly have mixed or non-calcified plaques.9 10 Therefore, use of absolute CACS to estimate mortality risk may lead to false reassurance in women with low CACS, as symptomatic women might have CAD caused by non-calcified plaques.11 Thus, CACS may have a different prognostic value in symptomatic women compared with men,12 13 although literature is not consistent.14
The presence of coronary artery calcification also differs between ethnicities15 16 and increases with age.5 6 8 17 Therefore, the Multi-Ethnic Study of Atherosclerosis (MESA) reported sex-specific, age-specific and race/ethnicity-specific percentiles for CACS in the general and asymptomatic population.18 19 However, the question remains if these percentiles are a better discriminator of risk compared with absolute CACS in symptomatic patients in a real-world cardiology setting.
To address these issues, we first studied the prognostic value of coronary artery calcification measures in a symptomatic population in a sex-stratified manner, as CACS is mainly assessed and used as a risk marker in these symptomatic women and men.20–22 Both absolute measures, as reflected by CACS, and MESA percentiles,18 were evaluated as measures to reflect the amount of calcification. Second, we evaluated whether degree of coronary stenosis at CT angiography increases the discriminative prognostic value when added to the model based on CACS.
Methods
Patient selection
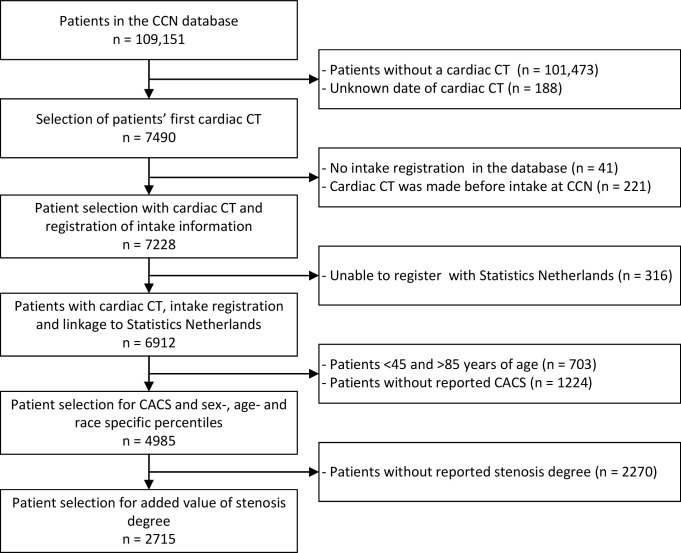
Individual patient data from electronic health records (CardioPortal, Cardiology Centers of the Netherlands (CCN) proprietary electronic health records, EHR) was retrieved from thirteen Dutch outpatient cardiology clinics (CCN) between 2007 and 2018. A detailed description of this database has been previously published.23 All included patients were symptomatic, that is, they had cardiovascular complaints and were referred by the general practitioner to a cardiovascular screening centre. We analysed a selection of patients that underwent cardiac CT as part of clinical care, resulting in a study population of 4985 women and men, aged between 45 and 85 years (figure 1). Standardised cardiovascular workup was performed and documented for these patients.23
Figure 1.
Patient selection for CACS and sex-specific, age-specific and race/ethnicity-specific analysis and for analysis of addition of stenosis degree. CACS, Coronary Artery Calcium Score; CCN, Cardiology Centers of the Netherlands.
Calcium score, MESA percentiles and degree of stenosis assessment
The cardiac CT scanning protocol consisted of a non-contrast enhanced scan to evaluate CACS and a contrast-enhanced protocol for coronary angiography. Type of CT-scanner was determined by availability in the referred centres. Results of diagnostic imaging were reported in free text, which was transformed into different features, for example, CACS and degree of stenosis in one of the main coronary arteries. Sex-specific, age-specific and race/ethnicity-specific percentiles were based on retrieved absolute CACS using the previously reported percentile tables from the MESA.19 As race/ethnicity was not structurally reported in the database, we used Caucasian percentiles in the main analysis.
As CACS is clinically used in different categories, we categorised CACS into the following groups: zero CACS, CACS 1–100, CACS 101–400 and CACS>400. For the MESA percentiles the following categories were used: no CAC, ≤75th percentile, 75th–90th percentile and >90th percentile. In 2715 (54%) of these patients, degree of stenosis determined by CT angiography was also documented in free text. A comparison was made for baseline characteristics of the complete CT population in which CACS was reported and the CT population in whom degree of stenosis was additionally documented. The available CT angiography results were classified into grades of stenosis, namely 0%, 1%–24%, 25%–49%, 50%–70%, 71%–99% and 100% stenosis.24 Qualitative indications of degree of stenosis were discussed with two cardiologists to enable quantification of stenosis degree. This resulted in the following conversion from qualitative to quantative; for 1%–24% any, minimal, minor, for 25–49% partial, diffuse, mild, not-significant, non-significant, for 50%–70% important, clear, significant, intermediate, for 71%–99% severe, high grade and for 100% occlusion. As (high-risk) plaque characteristics were irregularly and unstructured mentioned in free text, these features were not taken into account for analysis.
Outcome assessment
Information on a patient’s country of origin, mortality and cause of death was obtained by linkage to the population registry of Statistics Netherlands. Event rates are only exactly reported when 10 or more events were included, following regulations of Statistics Netherlands to avoid risk of personal disclosure. In all other cases, the number of events and percentages were reported as ‘<10’ with the corresponding percentage.
Statistical analyses
The baseline characteristics of the datasets were described as mean±standard deviation (SD) or median with interquartile range (IQR) when appropriate. We estimated survival functions using Kaplan-Meier curves. Cox proportional hazards regression analysis was performed to study the predictive value of coronary artery calcification (absolute CACS as calculated by the Agatston score and MESA percentiles) and mortality. For the model based on the MESA percentiles, a binary variable was added to indicate whether CACS was positive (>0) at baseline. The addition of a variable to indicate the presence or absence of CACS is needed to correct for the possible discontinuity in the MESA percentiles between individuals with a CACS of zero or any positive continuous CACS. We first constructed models including CACS or MESA percentiles as continuous variables. Subsequently, we constructed models with the previously described categorised CACS and MESA percentiles. The concordance statistic (C-statistic) with 95% confidence interval (CI) was used to assess the ability of these models to discriminate patients at risk for mortality. A higher C-statistic indicates a better fit and higher prognostic power. Subsequently, we evaluated whether addition of degree of stenosis on top of absolute CACS improved the prognostic power of the Cox proportional hazards model. All analyses were stratified by sex. Statistical analyses were performed in R (V.4.0.2).
Sensitivity analyses
The race groups within the MESA percentiles as defined by the MESA19 were not transferable to a patient’s country of origin as documented in the population registry of Statistics Netherlands. In our primary analyses, we calculated MESA percentiles based on the Caucasian race. In a sensitivity analysis, we excluded all patients born outside Europe, using this individual’s characteristic as a surrogate for a different race.
Patient and public involvement
Patients were not involved in any stage of this research process.
Results
Baseline characteristics
Baseline characteristics of the selected population are displayed in table 1. Of the 4985 patients, 2793 (56%) patients were women. On average, women were 1 year older compared with men (60 vs 59). Other cardiovascular risk factors were similar between women and men. Both sexes primarily presented with chest pain or discomfort. Median CACS in women was 0 (IQR: 0–54), and 42 (IQR: 0–54) in men. CACS categories of 0, 1–100, 100–400 and >400 were, respectively, present in 1387 (50%), 899 (32%), 340 (12%) and 167 (6%) women in this study. In men, this distribution was 569 (26%), 774 (35%), 436 (20%) and 413 (19%), respectively. Higher CACS was seen in individuals with higher age and a higher prevalence of hypertension and dyslipidaemia in both sexes (online supplemental table 1).
Table 1.
Baseline characteristics of study population stratified by sex
| Overall | Women | Men | |
| n | 4985 | 2793 | 2192 |
| Age in years (mean (SD)) | 59 (8) | 60 (8) | 59 (8) |
| Body mass index (mean (SD)) | 27 (5) | 27 (5) | 27 (4) |
| Originated from Europe, n (%) | 4309 (86) | 2411 (86) | 1898 (87) |
| Complaints, n (%) | |||
| Chest pain or discomfort | 2683 (54) | 1585 (57) | 1098 (50) |
| Dyspnoea | 538 (11) | 329 (12) | 209 (10) |
| Fatigue | 172 (4) | 85 (3) | 87 (4) |
| Palpitations | 463 (9) | 290 (10) | 173 (8) |
| Collapse | 27 (1) | <10 | >10 |
| Smoking status, n (%) | |||
| Current | 1476 (32) | 859 (33) | 617 (30) |
| Former | 1650 (36) | 875 (34) | 775 (38) |
| Never | 1504 (33) | 854 (33) | 650 (32) |
| Diabetes mellitus, n (%) | 396 (8) | 213 (8) | 183 (8) |
| Hypertension, n (%) | 1581 (32) | 954 (34) | 627 (29) |
| Dyslipidaemia, n (%) | 850 (17) | 477 (17) | 373 (17) |
| CACS score (median (IQR)) | 8 (0, 121) | 0 (0, 54) | 42 (0, 278) |
| CACS category, n (%) | |||
| 0 | 1956 (39) | 1387 (50) | 569 (26) |
| 1–100 | 1673 (34) | 899 (32) | 774 (35) |
| 101–400 | 776 (16) | 340 (12) | 436 (20) |
| >400 | 580 (12) | 167 (6) | 413 (19) |
| Examinations during follow-up, n (%) | |||
| At least one CAG | 812 (16) | 309 (11) | 503 (23) |
| At least one PCI or CABG | 307 (6) | 89 (3) | 218 (10) |
| All-cause mortality | 116 (2) | 53 (2) | 63 (3) |
| Years of follow-up (median (IQR)) | 4.5 (3.1, 6.3) | 4.5 (3.1, 6.3) | 4.5 (3.1, 6.3) |
Due to privacy constraints, numbers of individuals fewer than 10 are not allowed to be exported from statistics Netherlands. These numbers are represented as ‘<10’ with the corresponding percentage.
CABG, coronary artery bypass graft; CAC, coronary artery calcium; CACS, coronary artery calcium score CAG, coronary angiography; PCI, percutaneous coronary intervention.
openhrt-2022-002005supp001.pdf (104.7KB, pdf)
The predictive value of coronary calcification for all-cause mortality
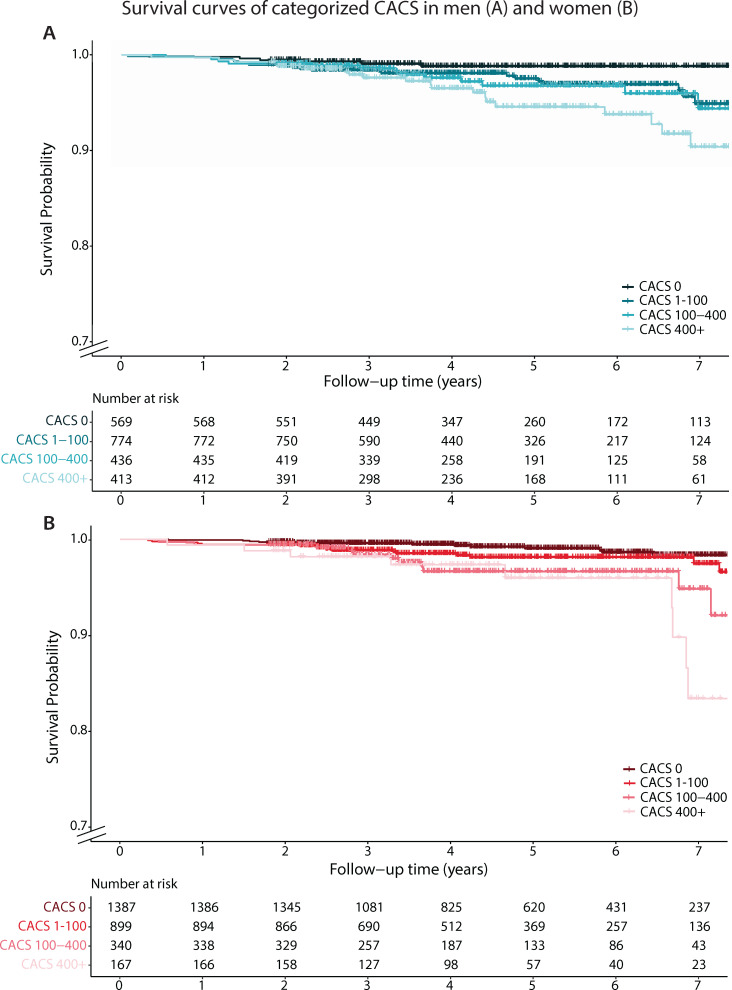
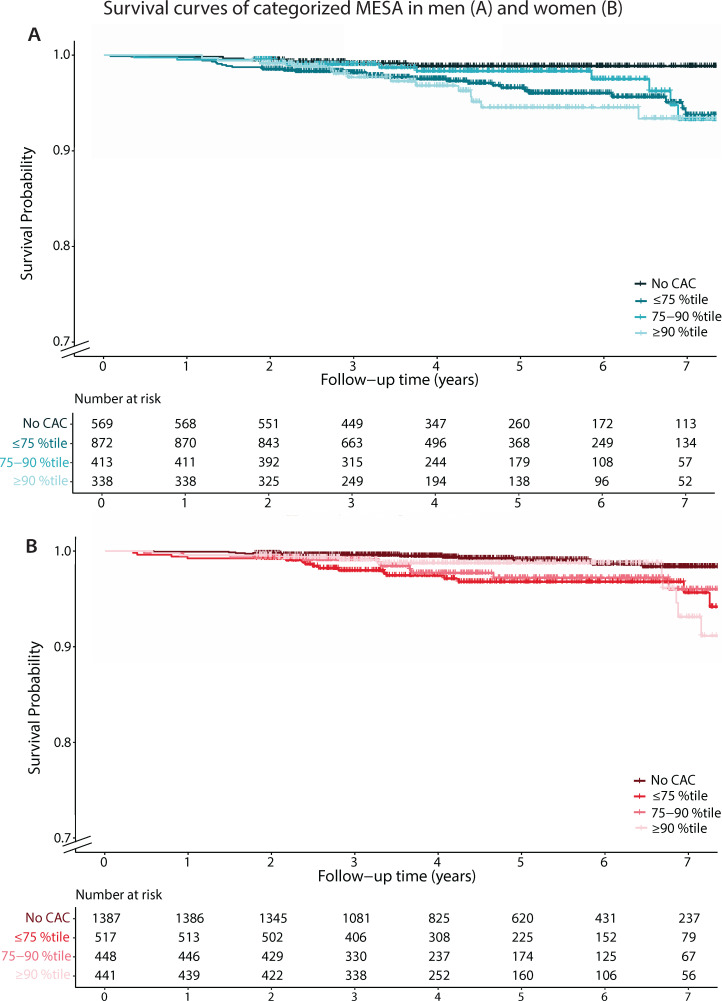
After a median follow-up of 4 years (IQR: 3–6), 116 (53 women and 63 men) patients died, of which 22 were attributed to cardiovascular mortality. Mortality rate was higher in individuals who had higher CACS (women: 1%, 2%, 4% and <6%, men: <2%, 3%, 3% and 5%, for, respectively CACS categories of 0, 1–100, 100–400 and >400, online supplemental table 1). Figure 2 shows the survival over time per absolute CACS category for women and men. Survival over time for categorised MESA percentiles is shown in figure 3. Overall, women had a better survival. Individuals with higher levels of absolute CACS showed lower survival rates compared with low CACS levels. This relation was also seen with higher MESA percentiles, although less strong. However, differences were small.
Figure 2.
Survival of women and men by absolute CACS. CACS, Coronary Artery Calcium Score.
Figure 3.
Survival of women and men by age-specific, sex-specific and race/ethnicity-specific percentiles (MESA). CAC, coronary artery calcium; MESA, Multi-Ethnic Study of Atherosclerosis.
Mortality rates, hazard ratios (HR) and C-statistics are displayed in table 2 for women and men. For continuous calcification measures, the discriminative ability of absolute CACS was moderate in both women and men (C-statistic 0.66, 95% CI 0.58 to 0.74 in women, and 0.62, 95% CI 0.55 to 0.69, in men). The discriminative ability of absolute CACS was similar to models based on MESA percentiles (0.65, 95% CI 0.57 to 0.73 in women, 0.59, 95% CI 0.51 to 0.67 in men). Results were similar for the models that used categorical classifications of CACS and MESA percentiles instead of continuous measures (CACS C-statistic 0.65, 95% CI 0.57 to 0.73 and 0.60, 95% CI 0.53 to 0.67, in women and men, respectively, MESA percentiles C-statistic 0.64, 95% CI 0.57 to 0.73 and 0.61, 95% CI 0.54 to 0.67 in women and men, respectively).
Table 2.
Mortality prediction as a function of absolute and age-specific, sex-specific and race/ethnicity-specific percentiles of CACS in women (above) and men (below)
| Model | n | Events | HR (95% CI) | C-statistic (95% CI) | |
| Women | Absolute CACS | ||||
| Continuous | 2793 | 53 | 1.0 (1.0 to 1.0) | 0.66 (0.58 to 0.74) | |
| Categorised | |||||
| CACS 0 | 1387 | 14 | Reference | 0.65 (0.57 to 0.73) | |
| CACS 1–100 | 899 | 18 | 2.1 (1.0 to 2.1) | ||
| CACS 101–400 | 340 | 12 | 4.0 (1.8 to 8.6) | ||
| CACS >400 | 167 | <10 | 5.7 (2.5 to 13.2) | ||
| MESA percentiles | |||||
| Continuous, adjusted for any calcification | |||||
| MESA percentile | 2793 | 53 | 0.4 (0.1 to 1.5) | 0.65 (0.57 to 0.73) | |
| Any calcification | 6.1 (1.9 to 19.1) | ||||
| Categorised | |||||
| No calcification | 1387 | 14 | Reference | 0.64 (0.57 to 0.72) | |
| <75th percentile | 517 | 18 | 3.5 (1.8 to 7.1) | ||
| 75th–90th percentile | 448 | 11 | 2.7 (1.2 to 5.9) | ||
| >90th percentile | 441 | 10 | 2.5 (1.1 to 5.6) | ||
| Men | Absolute CACS | ||||
| Continuous | 2192 | 63 | 1.0 (1.0 to 1.0) | 0.62 (0.55 to 0.69) | |
| Categorised | |||||
| CACS 0 | 569 | <10 | Reference | 0.60 (0.53 to 0.67) | |
| CACS 1–100 | 774 | 23 | 3.0 (1.2 to 7.5) | ||
| CACS 101–400 | 436 | 14 | 3.3 (1.3 to 8.7) | ||
| CACS >400 | 413 | 20 | 5.1 (2.0 to 12.7) | ||
| MESA percentiles | |||||
| Continuous, adjusted for any calcification | |||||
| MESA percentile | 2192 | 63 | 0.5 (0.2 to 1.5) | 0.59 (0.51 to 0.67) | |
| Any calcification | 5.7 (1.9 to 16.8) | ||||
| Categorised | |||||
| No calcification | 569 | <10 | Reference | 0.61 (0.54 to 0.67) | |
| <75th percentile | 872 | 33 | 3.9 (1.6 to 9.3) | ||
| 75th–90th percentile | 413 | 10 | 2.5 (0.9 to 7.0) | ||
| >90th percentile | 338 | 14 | 4.3 (1.6 to 11.1) | ||
CACS, Coronary Artery Calcium Score; MESA, Multi-Ethnic Study of Atherosclerosis.
The sensitivity analysis in which we excluded all patients in whom the country of birth was documented to be outside Europe (n=676, 13.5%), as a surrogate for a different race, showed similar results. The European population comprised 2411 women and 1898 men. The C-statistic for absolute CACS was comparable to MESA percentiles (in women, 0.67, 95% CI 0.59 to 0.76, vs 0.66, 95% CI 0.58 to 0.75, and in men 0.64, 95% CI 0.55 to 0.72, vs 0.59, 95% CI 0.51 to 0.67). Results of the sensitivity analysis are displayed in online supplemental table 2.
Stenosis degree and the relation between coronary calcification and mortality
Stenosis severity by CT angiography was documented for 1330 (60.7%) men and 1385 (49.6%) women. Baseline characteristics of these women and men are depicted in table 3. Online supplemental table 3 shows the baseline characteristics of the CT population in which CACS was reported and the CT population in whom degree of stenosis was additionally documented. During a median follow-up of 5 years (IQR: 3–6 years), 46 (3.5%) men and 22 (1.5%) women died. Compared with the population in which only CACS was available, these women and men did not differ in baseline characteristics (for direct comparison and baseline characteristics per CACS category, see online supplemental tables 3,4, respectively). In the population in whom both CACS and information on stenosis degree was available, the relation between calcification measures and mortality was comparable to the relation found in the total population (table 4). In men, the discriminative power of the model did not improve when degree of stenosis was added (C-statistic changed from 0.63, 95% CI 0.55 to 0.71 based on CACS to 0.59, 95% CI 0.51 to 0.67 after addition of stenosis to the model). In women, the performance to predict mortality improved slightly (C-statistic 0.68, 95% CI 0.58 to 0.78 and 0.72, 95% CI 0.61 to 0.83, respectively). However, this improvement was not significant, and thus, no hard conclusions can be drawn.
Table 3.
Baseline characteristics of women and men that underwent cardiac CT angiography
| Overall | Women | Men | |
| n | 2715 | 1385 | 1330 |
| Age in years (mean (SD)) | 60 (8) | 60 (8) | 59 (8) |
| Body mass index (mean (SD)) | 27 (4) | 27 (5) | 27 (4) |
| Complaints, n (%) | |||
| Chest pain or discomfort | 1499 (55) | 801 (58) | 698 (53) |
| Dyspnoea | 295 (11) | 167 (12) | 128 (10) |
| Fatigue | 93 (3) | 47 (3) | 46 (4) |
| Palpitations | 272 (10) | 163 (12) | 109 (8) |
| Collapse | 18 (1) | <10 | >10 |
| Smoking status, n (%) | |||
| Current | 809 (32) | 428 (34) | 381 (31) |
| Former | 936 (37) | 461 (36) | 475 (38) |
| Never | 765 (31) | 380 (30) | 385 (31) |
| Diabetes mellitus, n (%) | 211 (8) | 97 (7) | 114 (9) |
| Hypertension, n (%) | 885 (33) | 518 (38) | 367 (28) |
| Dyslipidaemia, n (%) | 497 (18) | 263 (19) | 234 (18) |
| CACS score (median (IQR)) | 34 (0–162) | 14 (0–92) | 67 (6–267) |
| CACS category, n (%) | |||
| 0 | 682 (25) | 472 (34) | 210 (16) |
| 1–100 | 1150 (42) | 585 (42) | 565 (43) |
| 101–400 | 598 (22) | 251 (18) | 347 (26) |
| >400 | 285 (11) | 77 (6) | 208 (16) |
| Degree of stenosis, n (%) | |||
| 0 % | 792 (29) | 527 (38) | 265 (20) |
| 1%–49% | 1114 (41) | 563 (41) | 551 (41) |
| 50%–70% | 431 (16) | 168 (12) | 263 (20) |
| >70% | 378 (14) | 127 (9) | 251 (19) |
| Examinations during follow-up, n (%) | |||
| At least one CAG | 553 (20) | 205 (15) | 348 (26) |
| At least one PCI or CABG | 234 (9) | 66 (5) | 168 (13) |
| All-cause mortality | 68 (3) | 22 (2) | 46 (4) |
| Cardiovascular mortality | 10 (0.4) | <10 | <10 |
| Years of follow-up (median (IQR)) | 4.6 (3.2–6.3) | 4.6 (3.2–6.3) | 4.7 (3.2–6.4) |
Due to privacy constraints, numbers of individuals fewer than 10 are not allowed to be exported from statistics Netherlands. These numbers are represented as ‘<10’ with the corresponding percentage.
CABG, coronary artery bypass graft; CAC, coronary artery calcium; CACS, Coronary Artery Calcium Score; CAG, coronary angiography; PCI, percutaneous coronary intervention.
Table 4.
Mortality prediction as a function of absolute CACS and degree of stenosis in women (above) and men (below)
| Model | n | Events | HR (95% CI) | C-statistic (95% CI) | |
| Women | Absolute CACS | ||||
| Continuous | 1385 | 22 | 1.0 (1.0 to 1.0) | 0.68 (0.58 to 0.78) | |
| + Degree of stenosis | 0.72 (0.61 to 0.83) | ||||
| 0% | 527 | <10 | Reference | ||
| 1%–49% | 563 | 14 | 6.9 (1.6 to 30.6) | ||
| 50%–70% | 168 | <10 | 4.9 (0.9 to 28.6) | ||
| >70% | 127 | <10 | 2.8 (0.3 to 22.4) | ||
| Men | Absolute CACS | ||||
| Continuous | 1330 | 46 | 1.0 (1.0 to 1.0) | 0.63 (0.55 to 0.71) | |
| + Degree of stenosis | 0.59 (0.51 to 0.67) | ||||
| 0% | 265 | <10 | Reference | ||
| 1%–49% | 551 | 22 | 4.5 (1.3 to 15.3) | ||
| 50%–70% | 263 | 10 | 3.9 (1.1 to 14.7) | ||
| >70% | 251 | 11 | 4.2 (1.1 to 16.3) |
CACS, Coronary Artery Calcium Score.
Discussion
Our data showed that absolute CACS and MESA percentiles perform equally well in predicting mortality in symptomatic women and men who visit outpatient cardiology clinics in a real-world setting. Hence, for discrimination of mortality in symptomatic individuals, there is no need for MESA percentiles to quantify coronary artery calcification. Absolute CACS predicts mortality with moderate performance, comparable to performance in asymptomatic inidivuals.19 Finally, the data hint that in women, the discriminative power of CACS for mortality might be higher when degree of stenosis was included in the model. However, these results should be interpreted with caution, as improvement was not significant. In men, addition of degree of stenosis did not result in better prediction of mortality. This subtle sex-difference might be due to the presence of non-calcified plaques causing symptoms in women.9 This type of plaques remains (partly) unappreciated when using CACS only for mortality prediction.
When comparing the results of the result of the prognostic value of CACS to other publications, a similar result was presented by Engbers et al14 in which they sought to evaluate gender-specific (n=3705, 61% women) prognostic value of CACS on top of SPECT myocardial perfusion imaging. No gender-specific differences were found and the HRs described in this study are similar to the HRs for the CACS categories in both sexes in our study. Another study that focused on symptomatic individuals (n=3840, 51% women) suspected of CAD showed that a high prognostic value of CACS, which further increased after addition of stenosis degree.3 More variables, that is, degree of stenosis, specific (high risk) plaque characteristics, were incorporated in prognostic models. However, their analysis was not stratified by sex, hampering any comparison to our data and impeding analysis of sex differences. They also showed that the recently developed CAD Reporting and Data System24 classification provides the highest prognostic value for cardiovascular events.3
Our results in symptomatic women and men are in line with results of the MESA, which was conducted in non-symptomatic individuals from the general population. The MESA demonstrated that absolute CACS outperforms MESA percentiles for event prediction.19 We also found that the discriminative capacity remains intact when categorising CACS. This finding is valuable for clinical use, as HRs derived from categories are easier to interpret than continuous values. Furthermore, studies in asymptomatic individuals concluded that CACS predicted mortality risk equally well for both sexes,1 12 despite the findings that women had lower CACS compared with men1 and that significant sex differences were present in cumulative mortality.12 Most studies reported that CACS may be a better predictor for mortality in women compared with men.12 21 22 This suggestion is in line with the slightly higher C-statistic for the CACS-model we described in women. In addition, sex-specific CACS percentiles tend to better stratify risk in women than men as opposed to absolute scores.21 The reason for discrepancy between results might be the inclusion of an asymptomatic older population in the study by Wang et al.21
Strengths and limitations
A strength of the presented study is the use of a real-world population in whom cardiac CT is often used as a primary diagnostic, yet its power is not often studied. This population is best described as a symptomatic population, referred to a specialised cardiac screening centre, which is positioned between general practitioners and hospital care. Furthermore, linkage to the database of Statistics Netherlands provided long-term follow-up data on mortality and information on country of birth.
Use of EHR data also has inherent limitations. First, data were not primarily collected for study purposes. Therefore, part of the population that underwent cardiac CT could not be included, due to insufficient documentation of CT results. Second, as CT angiography was only performed based on referral by the cardiologist and/or local scan protocol, not all patients underwent CT angiography. Thus, the subanalysis focusing on degree of stenosis, based on CT angiography results, was only performed in a subset of patients. This significantly reduced the power of our statistical analysis and might have led to selection bias. To evaluate this bias, we compared the overall and subpopulation and repeated the analyses in the subpopulation. The populations were comparable on known baseline characteristics. Moreover, the results of the use of CACS and MESA percentiles for risk stratification did not significantly differ. This suggests that increased discriminative power of CACS when degree of stenosis was added to the model is generalisable. Third, as stenosis severity was retrieved from text reports in which the degree of stenosis was not always quantified, the interpretation of the grade of stenosis could lead to uncertainty in our data. Fourth, we did not take treatment differences into account between different groups. These differences may explain the decreasing HR with an increasing degree of coronary stenosis, although this decrease was not significant. Finally, as we have used country of origin as a surrogate for race/ethnicity, the categories used in the original MESA calculations and our study population were not identical. To assess whether this has influenced our results, we performed a sensitivity analysis in which we included women and men who originated from Europe, assuming they all have the Caucasian race. These results were not significantly different from the main analyses. Moreover, as our population was primarily coming from Europe, our results might not be applicable to individuals of other ethnic populations.
We found that adding degree of stenosis to the survival model slightly improved the discriminative power in women, but not in men. However, this improvement in women was not statistically significant and confidence intervals largely overlapped. Even though we showed a moderate prognostic value of CACS in both symptomatic women and men, our results warrant evaluation beyond CACS alone for optimal risk prediction as C-statistics were below 0.70. This might be especially relevant in women, in whom information on the degree of stenosis potentially has added value due to presence of non-calcified plaques. We were unable to assess the added value of degree of stenosis properly due to incomplete data. Nevertheless, the difference between women and men we found after degree of stenosis was added to the model stresses the importance of a sex-specific view on CAD. Replication of this study in larger trials or populations is going to contribute to confirm these hypotheses, regarding the importance of non-calcified plaques in women for mortality risk.
Conclusion
In symptomatic individuals, absolute CACS predicts mortality with a moderately good performance. MESA percentiles did not perform better compared with absolute CACS, thus, there is no need to use them. Including degree of stenosis in the model might slightly improve mortality risk prediction in women, but not in men.
Acknowledgments
Results are based on calculations by the authors using non-public microdata from Statistics Netherlands.
Footnotes
Twitter: @Klaskeeee
Contributors: KRS, FG, ALME, CO-M and HMdR designed the study and study methods. KRS cleaned the raw data, KRS and FG performed data analyses and wrote the manuscript. WJodB provided extensive literature search. IIT, LH and GAS collected the raw data and reviewed the manuscript. TL, YA, CO-M and HMdR critically reviewed the manuscript. HMdR acts as the guarantor and accepts full responsibility for the work and conduct of the study, had access to the data and controlled the decision to publish.
Funding: This study was funded by the Dutch Heart Foundation (CVON-AI: 2018B017 and CVON ARGUS: 2017–22).
Competing interests: LH, IIT and GAS are employed by Cardiology Centers of the Netherlands. All other authors declare no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. The CCN database is not publicly available due to ethical and data protection constraints, but is available from the corresponding author on reasonable request. The results of presented survival analyses are based on calculations by the authors using non-public microdata from Statistics Netherlands. Under certain conditions, these microdata are accessible for statistical and scientific research. For further information: microdata@cbs.nl.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The Medical Research Ethics Committee of the University Medical Center Utrecht declared that research with the CCN database does not meet the Dutch Medical Research Involving Human Subjects Act (proposal number 17/359).
References
- 1.Nakanishi R, Li D, Blaha MJ, et al. All-cause mortality by age and gender based on coronary artery calcium scores. Eur Heart J Cardiovasc Imaging 2016;17:1305–14. 10.1093/ehjci/jev328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mittal TK, Pottle A, Nicol E, et al. Prevalence of obstructive coronary artery disease and prognosis in patients with stable symptoms and a zero-coronary calcium score. Eur Heart J Cardiovasc Imaging 2017;18:922–9. 10.1093/ehjci/jex037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bittner DO, Mayrhofer T, Budoff M, et al. Prognostic value of coronary CTA in Stable stable chest pain: CAD-RADS, CAC, and cardiovascular events in promise. JACC Cardiovasc Imaging 2020;13:1534–45. 10.1016/j.jcmg.2019.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32. 10.1016/0735-1097(90)90282-T [DOI] [PubMed] [Google Scholar]
- 5.Nicoll R, Wiklund U, Zhao Y, et al. Gender and age effects on risk factor-based prediction of coronary artery calcium in symptomatic patients: a Euro-CCAD study. Atherosclerosis 2016;252:32–9. 10.1016/j.atherosclerosis.2016.07.906 [DOI] [PubMed] [Google Scholar]
- 6.Raggi P, Gongora MC, Gopal A, et al. Coronary artery calcium to predict all-cause mortality in elderly men and women. J Am Coll Cardiol 2008;52:17–23. 10.1016/j.jacc.2008.04.004 [DOI] [PubMed] [Google Scholar]
- 7.Rumberger JA, Brundage BH, Rader DJ. Electron beam CT CAC scanning-a review and guidleins for use in asymptomatic persons. Mayo Clin Proc 1999;74:243–52. [DOI] [PubMed] [Google Scholar]
- 8.Kim BS, Chan N, Hsu G. Sex differences in coronary arterial calcification in symptomatic patients. Am J Cardiol 2016;2021:16–20. [DOI] [PubMed] [Google Scholar]
- 9.Plank F, Beyer C, Friedrich G, et al. Sex differences in coronary artery plaque composition detected by coronary computed tomography: quantitative and qualitative analysis. Neth Heart J 2019;27:272–80. 10.1007/s12471-019-1234-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams MC, Kwiecinski J, Doris M, et al. Sex-Specific computed tomography coronary plaque characterization and risk of myocardial infarction. JACC Cardiovasc Imaging 2021;14:1804–14. 10.1016/j.jcmg.2021.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussain A, Ballantyne CM, Nambi V. Zero coronary artery calcium score: desirable, but enough? Circulation 2020;142:917–9. 10.1161/CIRCULATIONAHA.119.045026 [DOI] [PubMed] [Google Scholar]
- 12.Raggi P, Shaw LJ, Berman DS, et al. Gender-Based differences in the prognostic value of coronary calcification. J Womens Health 2004;13:273–83. 10.1089/154099904323016437 [DOI] [PubMed] [Google Scholar]
- 13.Bellasi A, Lacey C, Taylor AJ, et al. Comparison of prognostic usefulness of coronary artery calcium in men versus women (results from a meta- and pooled analysis estimating all-cause mortality and coronary heart disease death or myocardial infarction). Am J Cardiol 2007;100:409–14. 10.1016/j.amjcard.2007.03.037 [DOI] [PubMed] [Google Scholar]
- 14.Engbers EM, Timmer JR, Ottervanger JP, et al. Impact of gender on the prognostic value of coronary artery calcium in symptomatic patients with normal single-photon emission computed tomography myocardial perfusion. Am J Cardiol 2016;118:1611–5. 10.1016/j.amjcard.2016.08.037 [DOI] [PubMed] [Google Scholar]
- 15.Bild DE, Detrano R, Peterson D. Ethnic differences in coronary calcification: the multi-ethnic study of atherosclerosis (MESA). Circulation 2005;111:1313–20. [DOI] [PubMed] [Google Scholar]
- 16.Nasir K, Shaw LJ, Liu ST, et al. Ethnic differences in the prognostic value of coronary artery calcification for all-cause mortality. J Am Coll Cardiol 2007;50:953–60. 10.1016/j.jacc.2007.03.066 [DOI] [PubMed] [Google Scholar]
- 17.Hoff JA, Chomka EV, Krainik AJ, et al. Age and gender distributions of coronary artery calcium detected by electron beam tomography in 35,246 adults. Am J Cardiol 2001;87:1335–9. 10.1016/S0002-9149(01)01548-X [DOI] [PubMed] [Google Scholar]
- 18.Budoff MJ, Nasir K, McClelland RL. Coronary calcium predicts events better with absolute calcium scores than Age-Sex-Race/Ethnicity percentiles. MESA (multi-ethnic study of atherosclerosis). J Am Coll Cardiol 2009;53:345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McClelland RL, Chung H, Detrano R. Distribution of coronary artery calcium by race, gender, and age: results from the multi-ethnic study of atherosclerosis (MESA). Circulation 2006;113:30–7. [DOI] [PubMed] [Google Scholar]
- 20.Shaw LJ, Min JK, Nasir K, et al. Sex differences in calcified plaque and long-term cardiovascular mortality: observations from the CAC Consortium. Eur Heart J 2018;39:3727–35. 10.1093/eurheartj/ehy534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang FM, Rozanski A, Arnson Y, et al. Cardiovascular and all-cause mortality risk by coronary artery calcium scores and percentiles among older adult males and females. Am J Med 2021;134:341–50. 10.1016/j.amjmed.2020.07.024 [DOI] [PubMed] [Google Scholar]
- 22.Kelkar AA, Schultz WM, Khosa F. Long-term prognosis after coronary artery calcium scoring among Low-Intermediate risk women and men. Circulation 2016;9:1–7. [DOI] [PubMed] [Google Scholar]
- 23.Bots SH, Siegersma KR, Onland-Moret NC, et al. Routine clinical care data from thirteen cardiac outpatient clinics: design of the cardiology centers of the Netherlands (CCN) database. BMC Cardiovasc Disord 2021;21:1–9. 10.1186/s12872-021-02020-7 10.1186/s12872-021-02020-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Foldyna B, Szilveszter B, Scholtz J-E, et al. CAD-RADS - a new clinical decision support tool for coronary computed tomography angiography. Eur Radiol 2018;28:1365–72. 10.1007/s00330-017-5105-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2022-002005supp001.pdf (104.7KB, pdf)
Data Availability Statement
Data are available on reasonable request. The CCN database is not publicly available due to ethical and data protection constraints, but is available from the corresponding author on reasonable request. The results of presented survival analyses are based on calculations by the authors using non-public microdata from Statistics Netherlands. Under certain conditions, these microdata are accessible for statistical and scientific research. For further information: microdata@cbs.nl.