Abstract
Objective:
To compare the effects of low-level laser therapy, kinesio-taping and manual lymphatic drainage (MLD) on the affected arm volume, quality of life, arm function, neuropathic pain and shoulder mobility in patients with stage II breast cancer-related lymphedema.
Materials and Methods:
Forty-five breast cancer patients with stage II lymphedema were included. The patients were randomized to three groups and treated with MLD, kinesio-taping or low-level laser therapy. After these different therapeutic modalities, all patients received multilayer compression bandaging, lymphedema remedial exercises, skin care, and a patient education program by the same lymphedema therapist. All treatments were applied 5-days a week for three weeks. The lymphedema compression garments were prescribed to all patients and follow-up visits were planned at the end of the treatment, and at four and 12 weeks. The efficacy of the treatments was evaluated by volumetric calculations based on circumferential measurements using the formula for a truncated cone, in addition to goniometric assessments for shoulder joint ROM, and questionnaires: Quick-disability of arm, shoulder and hand for arm disability; pain-detect for neuropathic pain; and quality of life for arm lymphedema (LYMQOL-arm).
Results:
The baseline patient and disease characteristics, and outcome measures were similar between groups. All treatment modalities were found to be effective in decreasing arm volume, and improving quality of life, upper extremity disability and neuropathic pain. The percentage of decreased arm volume or treatment success was better in kinesio-taping group than in the MLD group at the end of the treatment, and at four and 12 weeks after treatment (p = 0.009, p = 0.039, and p = 0.042, respectively).
Conclusion:
Kinesio-taping led to better results than MLD and was similarly effective compared with low-level laser in stage II breast cancer-related lymphedema at the twelfth week of follow-up. Kinesio-taping and low-level laser should be considered as alternative treatments in early-moderate stages of lymphedema. After these modalities, multi-layer compression and compression bandaging remain cornerstones of lymphedema treatment.
Keywords: Lymphedema, breast cancer, low level laser therapy, kinesio-taping, manual lymphatic drainage, complex decongestive treatment
Key Points
• Lymphedema is chronic, progressive and disabling disease needed self-management including skin care, self-manual lymphatic drainage massage, compressive garments, and exercises. Since manual lymphatic drain age is time-consuming and tiresome technique, alternative treatments such as kinesio-taping and LLLT should be considered because of similar effectivity in early stage of lymphedema.
Introduction
Lymphedema is a chronic, progressive and sometimes disabling disease if it has been not treated until end stage. Breast cancer (BC) related lymphedema (BCRL) is the most common cause of lymphedema in developed countries with an incidence ranging from 6–30% (1, 2, 3, 4).
The main risk factors for BCRL are the number of removed axillary lymph nodes, the number of metastatic lymph nodes, axillary radiotherapy, taxane type chemotherapy, obesity, advanced age, lack of physical activity, and the presence of hematoma, seroma or infection in the affected quadrant (4, 5, 6).
Lymphedema patients need life-long care, medical and psychosocial support (2). For optimal benefits, it is important to diagnose early, start treatment early and customize the treatment (2). Complex decongestive therapy (CDT) is the internationally accepted gold standard treatment method consisting of two-phases (2). The first phase of CDT is intensive and is performed by health professionals; this phase includes skin care, manual lymphatic drainage (MLD), compression therapies, such as multi-layer low-stretch bandaging, and specialized exercises (2). The second phase is for maintenance and is performed by the patient, caregiver, or family and consists of the same components, and compression garments.
MLD is a unique gentle massage technique intended to increase lymphatic circulation using lymphatic anastomoses and territories in addition to diaphragmatic breathing. MLD can be applied by health professionals or by patients themselves (self MLD). Since MLD is a time-consuming technique and costly to implement, there were some recent studies that investigated the effectiveness of combining alternative techniques. However, there were a limited number of randomized controlled studies investigating the efficacies of MLD (7, 8), low-level laser therapy (LLLT) (9, 10, 11), and kinesio-taping (12, 13, 14). Moreover, there was no direct comparative study of these treatment modalities.
There were also some controlled studies including intermittent pneumatic compression devices (15), low-level laser treatment (9, 10, 11), electrotherapy (16), extra-corporal shock wave therapy (17), and kinesio-taping (2, 7).
The aim of this study was to compare the effectiveness and tolerability of LLLT, and kinesio-taping, as alternative treatment options for MLD, in patients with stage II BCRL.
Materials and Methods
Patients with BCRL attending the University of Health Sciences Turkey, Ankara Training and Research Hospital, Department of Physical Medicine and Rehabilitation, Division of Oncological Rehabilitation and Lymphedema were evaluated in this study. Ethical approval was obtained to conduct this study from the Institutional Review Board for Human Subjects (approval number: E-18-2025, date: 26.06.2018).
Patients were eligible if they had unilateral, stage I-III BC, unilateral stage II arm lymphedema and arm volume difference of 5–20% on the affected side after BC surgery. Exclusion criteria were: Patients with stage IV BC; bilateral BC; bilateral lymphedema; stage I (spontaneous reversible), late stage II (spontaneous irreversible with fibrotic changes) or stage III lymphedema; skin infection or lesion in the arms; diseases of the cardiovascular, pulmonary, renal, hepatic, other skin and allergic diseases; and patients who had received lymphedema treatment in the last six months. Patients were also excluded if there was a history of band-aid or skin allergy.
The study was performed with 60 patients who reed to participate in the study. Six of the patients did not meet the study criteria, the other 6 patients were not included in the study due to transportation problems. The participating patients were randomly divided into three groups using numbered envelopes with the shooting method. The patients were divided into groups of 15, 18 and 15 people according to the treatment protocol in the envelope they took. Before the treatment of patients in the kinesio-taping group, a 4x1 cm-sized kinesio-tape was applied to the volar surface of the forearm to test for kinesio-tape allergy. After the tape was removed the next day, the skin was examined and three patients with allergic skin reactions were excluded from the study. The flowchart of the study was shown in Figure 1.
Figure 1.
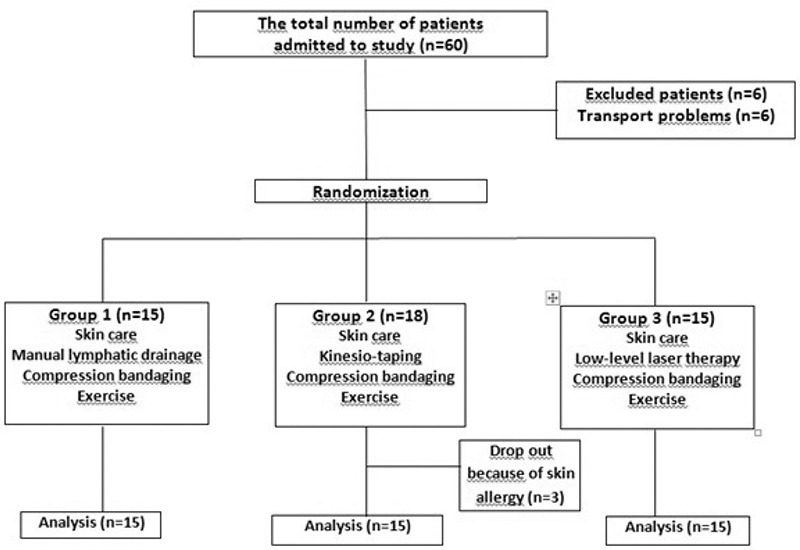
The flowchart of the study
Each physical therapy session was performed by the same therapist, for five days a week for three weeks. All patients were educated about self-massage, skin care and precautions for lymphedema using both face-to-face information and printed materials. At the end of the each physical therapy session, multi-layer bandaging was performed in all groups (Figure 2). Patients were informed about wearing bandages for 23–24 hours daily. After bandaging, supervised lymphedema exercises, including hand squeezing using green egg soft-ball (Erlegen, Turkey), and active resistive exercises for shoulder, elbow and wrist joints using green resistance tape (Thera-band®, Germany) were administered to all patients.
Figure 2.

Finger wrap, tubular stockinette, cotton wrap, forearmshort-stretch
Bandage, arm short-stretch bandage of multi-layer bandaging were applied to all groups
In the MLD group, MLD using Vodder’s massage technique was applied to the patients approximately 30–45 minutes by the same certified lymphedema therapist (18). After MLD, multi-layer bandaging was applied to these patients.
Kinesio-taping and multilayer bandaging was performed in the second group of patients. Diagonal direction of fan-cut kinesio-tape was applied from proximal to distal using the lymphedema kinesio-taping technique of paper-off tension (19, 20, 21). The anchor for the first kinesio-tape on the volar arm was placed to front side of the shoulder. The fan-like ends of the first kinesio-tape were directed to the elbow towards the lateral epicondyle. The rear of the shoulder was used as the anchor point for the second kinesio-tape for the dorsal arm. After the anchor was positioned, the arm kinesio-tape was fixed to the back of the shoulder, the fan-like ends were directed towards the medial epicondyle. The third kinesio-tape for the forearm was anchored to the end of the first kinesio-tape, that is, the lateral epicondyle, and the fan-like ends were directed towards the dorsal forearm and adhered to the medial side of the wrist. Then, the fourth kinesio-tape for the forearm was applied with the anchor starting from the medial epicondyle, with the fan-like ends directed towards the volar forearm to the lateral side of the wrist. Finally, the fifth and sixth kinesio-tapes for the hand were started on the ulnar and radial side of the wrist and the fan-like ends were terminated through the dorsum of the hand to between the fingers. The kinesio-taping applications of the patients were performed by the same therapist and were renewed twice a week (Figure 3a and 3b). After kinesio-taping, multilayer bandaging was also applied to the patients in the kinesio-tape group.
Figure 3.

Kinesio-taping with lymphedema teqnique
Patients in the low-level laser group received LLLT and multilayer bandaging by the same therapist. A power density of 30 mW/cm2 and a square centimeter density of 1.5 J/cm2 for 1 minute Gallium-Aluminum-Arsenid laser (Ga-Al-As) (BTL-5000®, BTL industries Ltd. Hertfordshire, UK) was applied directly using a grid technique. Patients were placed in the supine position with the arm in 90 degrees abduction. LLLT was applied to a total of 12 points in the axillary lymphatics or armpit region and eight points in the cubital lymphatics or volar elbow area, to be applied to each point for one minute, the whole procedure taking 20 minutes (22, 23). After LLLT, multilayer bandaging was also applied to the patients in LLLT group.
After 15 sessions of the different treatments detailed, flat-knitted lymphedema garments with pressure level of CCL2 (30–40 mmHg) (Medi GmbH®, Bayreuth, Germany) were prescribed to all patients for the maintenance phase. Patients regularly performed skin care, self-massage, day-worn compression garments and lymphedema exercises in the maintenance phase.
Patients
Demographic data of the patients, including personal information, such as age, sex, height (m), weight (kg), body-mass index (kg/m2), occupation, marital status, education level, caregiver support, and co-morbidities, and disease characteristics and lymphedema history were recorded.
Outcomes
Patients were evaluated at four time-points: Baseline; end of the treatment; and four and 12 weeks after the end of the treatment by the same physician. Volumetric measurements of arms were calculated from circumferential measurements using the formula for a truncated cone. Patients completed three questionnaires: Lymphedema Quality of Life Tool (LYM-QoL ARM); Quick DASH for assessment of upper extremity disability; and neuropathic pain was assessed with the pain detect questionnaire (PDQ). Joint range of motion (ROM) was assessed using plastic goniometer in shoulder joint.
Circumferential Measurement and Volume Calculation
Circumferential tape measurements of both arms were taken in 4-cm intervals starting from the ulnar styloid to the axilla while the patient was sitting in a sturdy chair with shoulder flexed at 90 degrees by a single physician. Circumferential measurements were made at every point with zero tension and without compression using non-flexible measuring tape.
The circumference measurement of both arms was recorded in each examination for volumetric calculations using the truncated cone formula. This technique is a valid and reliable method correlated with volumetric measurements (24, 25). Excess volume was defined as the difference between pre-treatment lymphedematous arm volume (LV) and pre-treatment healthy arm volume (HV) and the percentage of volume difference was preferred in evaluating the severity of lymphedema because the percentage of volume difference (PVD) showed the severity of lymphedema better than volume excess (24). The PVD formula was used to calculate the percentage of volume difference, which is an indicator of lymphedema severity (24, 25).
PVD = 100 x (LV-HV)/HV
(PVD: The percentage of volume difference or the severity of lymphedema) (24). The treatment success or response to lymphedema treatment was evaluated with the PDV as summarized below: PDV = 100 x (Pre-treatment arm volume – Post-treatment arm volume)/(Pre-treatment arm volume)
[PDV: The percentage of decreased volume (PDV) or the treatment success]
Functional Status of the Upper Extremity
In order to determine the functional level of the upper extremity, the 11-item Quick-DASH (disability of arm, shoulder and hand) questionnaire, which measures physical function and symptoms and is self-completed, was used. Each item offers can be scored on a5-point scale and at least 10 out of 11 questions must be answered in order to calculate the Quick DASH score (26, 27).
Quality of Life
LYM-QoL-Arm questions are grouped under four areas: Function, appearance, symptom and mood. It consists of 21 questions and the last question consists of the “general quality of life” scale (QoL). The item scoring in each area is: Nothing = 1, a little = 2, much = 3, a lot = 4. The total score for each area is calculated by adding all scores together and dividing by the total number of questions answered. Higher scores indicate lower quality of life. The final question on general quality of life (QoL) is scored between 0 and 10. Higher scores for the final question indicate a better overall quality of life (28, 29).
Neuropathic Pain
The PDQ is a patient-based, easy-to-use, 4-item questionnaire originally developed in German. The final score is scored between 0 and 38 points. Below 13 means no neuropathic pain, between 13 and 19 indicates uncertainty for neuropathic pain, and a score of more than 19 indicates possible neuropathic pain component (30, 31).
Shoulder Range of Motion
A standard plastic goniometer was used to measure ROMs for active shoulder flexion, abduction, and external rotation. The measurement was made on the examination table while the patient was lying down in the supine position. The reliability of the goniometric measurement technique for evaluating shoulder ROM has been previously demonstrated (32).
Power Analysis
After the criteria of the study were determined, the change in power analysis using G-power 3.1 version was taken as 5%, 6%, and 7% for each group, respectively, and the effect size was 0.56. In a study comparing the difference between three independent averages using the ANOVA test when the alpha error rate was 0.05 and the power was 0.91 (1-beta), the size of the groups was determined as 15 (33). A total of 60 patients with upper extremity lymphedema were included in the study by calculating 30% more than the specified group size.
Statistical Analysis
The data collected from the patients were entered into the SPSS 21.0 package program (IBM Inc., Armonk, NY, USA), a data set was created and statistical analysis was performed. Descriptive statistics [frequency, percentages, means ± standard deviations, median (range between quarters)] of the variables were indicated with tables. Conformity to normal distribution was determined by Kolmogorov–Smirnov and Shapiro–Wilk tests in order to determine whether the variables met the parametric test assumptions.
After determining that the variables fit the normal distribution, for pairs Student’s t–test and ANOVA test were used for more than two groups. ANOVA test if the difference between the groups was found to be significant after the post-hoc comparisons were made in order to determine that it originated from the group Bonferoni paired comparison test was continued. Repeated measures ANOVA test was performed for repeated measures for parametric variables. If significance was found after performing the ANOVA test in repeated measurements Bonferoni to determine at what time the difference is due to the measurement corrected Bonferoni corrected paired Sample t–test was performed.
After determining that the variables do not fit the normal distribution binary groups the Mann–Whitney U test was used for each group, and the Kruskal–Wallis H test for more than two groups. If the difference between the groups was found to be significant after the Kruskal–Wallis H test, Pairwise comparisons were made to determine which group the difference originated from. Dunn–Bonferoni pairwise comparison test was used.
Friedman test was used for non-parametric repeated variables. Significance after Friedman test determined, to determine at what time the difference was due to measurement. Wilcoxon test with Bonferoni correction was performed. The chi-square test was used for the comparison of categorical variables. A p value of <0.05 was considered statistically significant.
Results
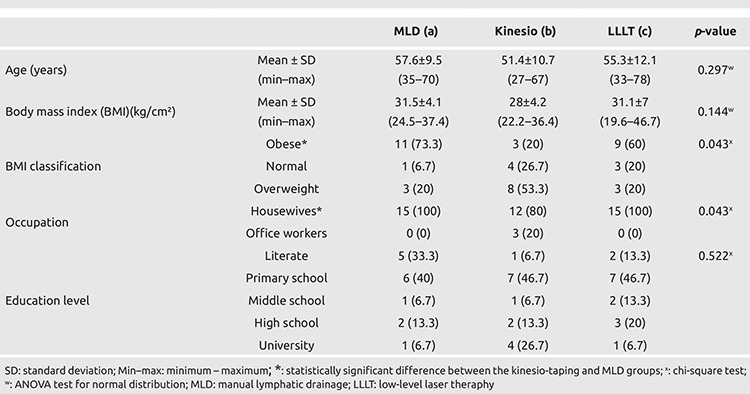
Demographic characteristics of patients are shown in Table 1. There were no significant differences between groups in terms of age (p = 0.297) and body mass index (BMI) (p = 0.144). Distribution of obese, overweight, and normal BMI patients were different between groups (p = 0.043). The frequency of obese patients was n = 11 (73.3%) in the MLD Group, n = 3 (20%) in the kinesio-taping group, and n = 9 (60%) in the LLLT group. This was significantly different between the kinesio-tape and the MLD groups (p = 0.01).
Table 1. The comparison of demographics of patients in the three treatment groups. Data are given as n (%) unless otherwise stated.
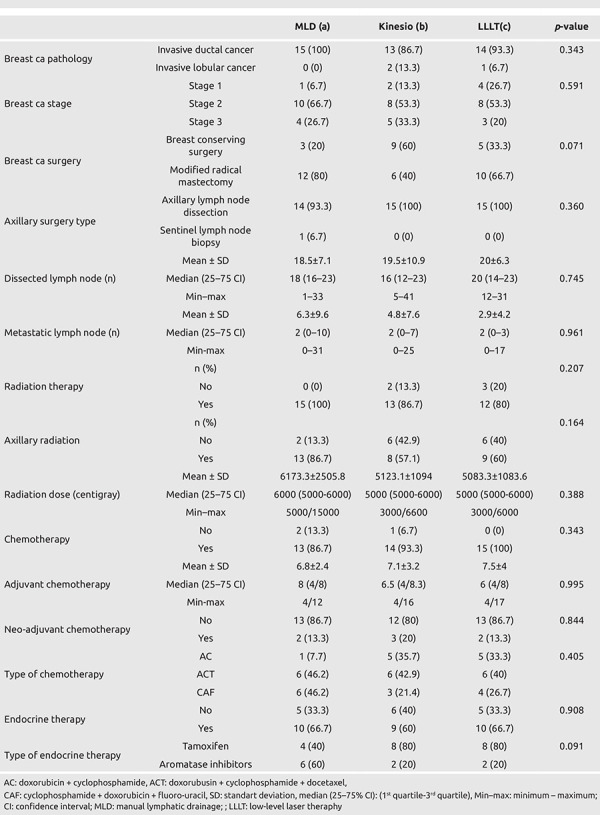
There was no difference between the treatment groups in terms of regarding lymphedema characteristics, BC surgery and BC-related treatments (see Table 2 and Table 3).
Table 2. Lymphedema characteristics of patients.
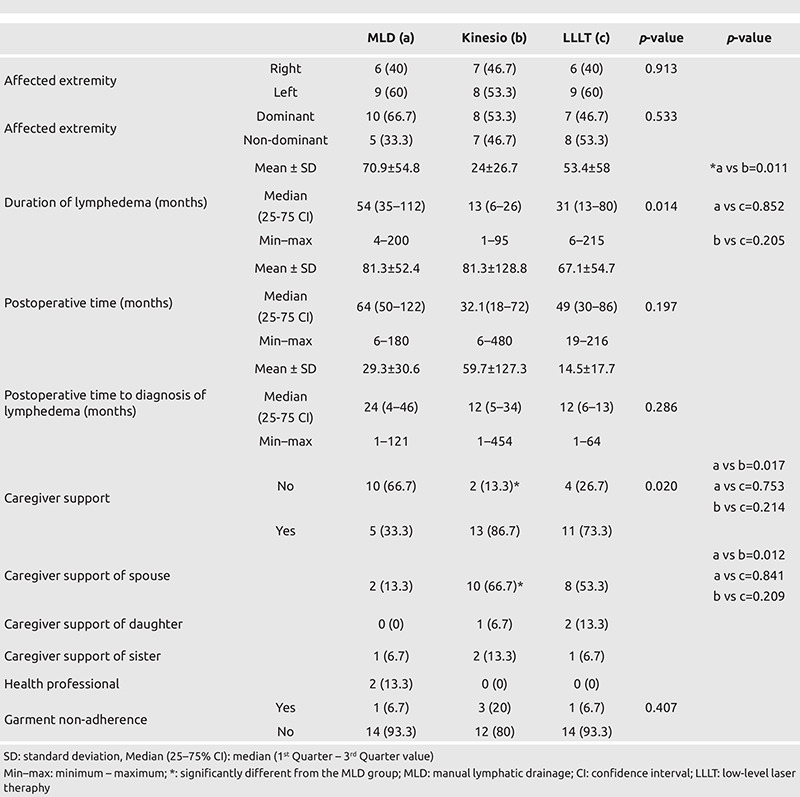
Table 3. Breast ca surgery and related treatment characteristics of patients.
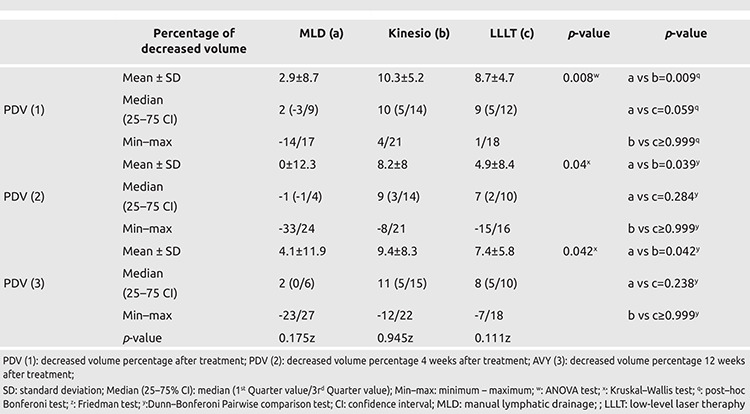
The improvement in the lymphedema arm volume or treatment success was determined by calculating the percentage of decreased volume (PDV). The percentage of improvement and subsequent change in the lymphedema arms of patients is summarized in Table 4. Compared the three groups, the PDV or treatment success was significantly higher in the kinesio-taping group than the MLD group at the end of the treatment, and four weeks and 12 weeks after treatment (p = 0.009, p = 0.039, and p = 0.042, respectively).
Table 4. Percentage of decreased volume (PDV) and subsequent changesat follow-up of end of the treatment (1), 4th weeks (2) and 12th weeks (3).
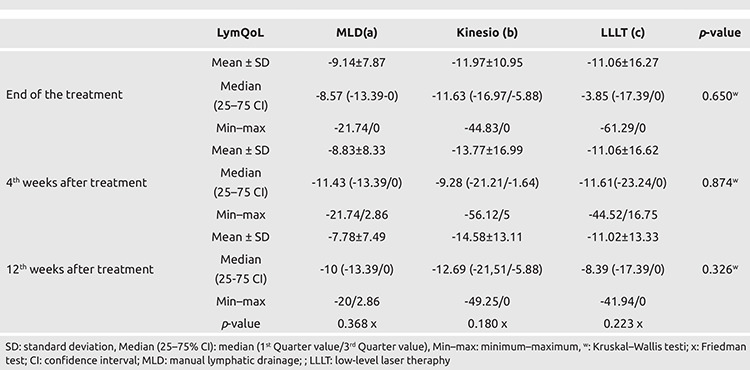
All LYM-QoL measures at follow-up showed significant improvement in the kinesio-taping group (p = 0.007, p = 0.005, and p = 0.002, respectively). Change in LYM-QoL values showed a significant decrease at the end of the treatment and 4 weeks after treatment (p = 0.022 and p = 0.043, respectively) in the MLD group. A significant decrease was found only at the end of treatment when compared to before treatment in the LLLT group (p = 0.043).
No significant differences were found in intergroup comparisons of LymQoL values at the end of the treatment, and at the fourth and twelfth weeks after treatment (p = 0.650, p = 0.874, and p = 0.326, respectively) (Table 5).
Table 5. Inter- and intra-group comparisons for LymQoL change (%).
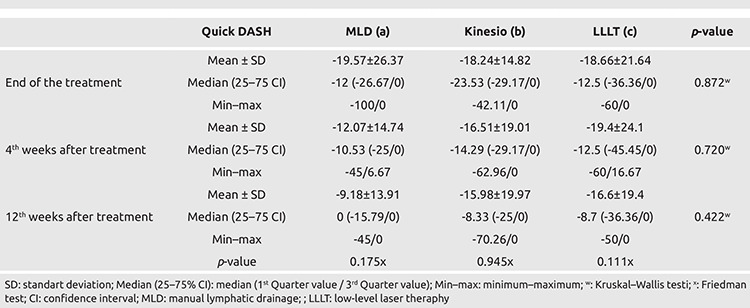
There were significant improvement in Quick-DASH scores in both the kinesio-taping and LLLT groups at the end of the treatment, and at the fourth and twelfth weeks after treatment (p = 0.003, p = 0.016, respectively). A significant decrease was found at the end of the treatment in quick-DASH scores in the MLD group (p = 0.008).
No statistically significant intra-group and inter-group differences were found in the improvement of Quick DASH scores between groups at follow-up periods including end of the treatment, and fourth and twelfth weeks after treatment (p = 0.872, p = 0.720, p = 0.422, respectively) (Table 6).
Table 6. Inter-group comparison of Quick DASH changes (%).
PDQ scores at baseline were 17±13.9 in the MLD group, 18.5±11.6 in the kinesio-taping group, and 16±13.1 in the LLLT group (p = 0.871). When the groups were evaluated within themselves, a significant decrease was found in all three groups only end of the treatment compared to baseline (p = 0.011, p = 0.028, p = 0.007, respectively).
No significant differences were found in the improvement in PDQ scores of groups at the end of the treatment, and fourth and twelfth weeks after treatment between groups (p = 0.475, p = 0.600, p = 0.601, respectively).
No significant limitation was found in shoulder ROM both at the beginning and follow-up in any patients.
Discussion and Conclusion
The results showed that all treatment modalities, including MLD, kinesio-taping and LLLT, were safe and effective in the treatment of stage II breast-cancer related lymphedema at follow-up until 12 weeks after treatment. Kinesio-taping was similarly effective as LLLT and more effective on PDV compared to MLD in the present study. All of these treatment methods were similarly effective on quality of life, upper extremity disability and neuropathic pain. In addition, we observed that the treatment success was greater in patients who did not receive adjuvant chemotherapy compared to those who received it.
There is no head-to-head comparison study for these three treatment methods in the literature. However, there are some studies evaluating the effectiveness of each treatment methods (7, 8, 9, 10, 11, 12, 13, 14). In a cochrane review, it was shown that compression therapies (multilayer bandaging, compression garments, intermittant pneumatic compression) should be used in all stages of lymphedema treatment (34). It was reported that MLD contributed 7% to compression treatments in this review. In another systematic review conducted in 2018, it was stated that the effects of MLD on the quality of life were not clear but it was effective in volume reduction (35).
The kinesio-taping technique used to support lymphatic drainage is a relatively new option in the field of physical therapy (14). Although kinesio-taping is a relatively new treatment modality, its use for lymphedema control is becoming more common. Kinesio-tape has some physiological effects, such as reducing pain and abnormal sensory sensitivity, supporting the movement of muscles, and preventing congestion of lymphatic fluid or hemorrhages under the skin. After kinesiotape is applied, the kinesio-taped area creates convolutions and increases the space between the skin and muscles (36). With the lymphatic application technique of kinesio-taping, the skin is removed and the area between the dermis and fascia is opened, so that the lymphatic drainage effect continues for 24 hours (13). When the physiological effects, such as capillary filtration reduction are analyzed, it has been suggested that kinesio-taping is more similar to compression therapy (13). In our study, it was seen that kinesio-taping was obviously effective in volume reduction. When we look at the treatment success measured by PDV in the affected limb, it was found to be significantly more effective than MLD, causing improvement immediate after treatment, and at four and twelve weeks after treatment. However, the patient characteristics, such as longer duration of lymphedema, lesser spouse support, more obesity and more houewive profiles in the MLD group compared to the those of kinesio-taping group are confounders and might explain the worse response to treatment.
In a meta-analysis examining the effectiveness of kinesiotape in BCRL, studies conducted between 2009 and 2016 were evaluated. In total, seven studies met the criteria and it was stated that kinesio-taping was effective in the treatment of lymphedema due to breast cancer, but it was not superior to other treatments (37).
A meta-analysis investigating the effectiveness and safety of kinesio-taping in cancer-related lymphedema reported that the frequency of kinesio-tape related skin reactions was between 10% and 21%. It has been stated that the quality of life is better and kinesio-taping is not more comfortable in those who have made multilayer short-stretch bandaging (38). In our study, skin reaction due to kinesio-tape was observed in 3 (16.6%) of 18 patients. This relatively common occurrence of skin reactions in patients is in keeping with previous reports. This type of common reaction might limit the use of kinesio-taping for treatment of BCRL.
LLLT has been used worldwide since 1995 and was approved by the FDA in 2007. Laser therapy is believed to increase the contractility of lymphatics, which allows the transport of lymph fluid by stimulating lymphangiogenesis and lymphatic motoricity, softening fibrotic tissues, and increasing macrophage activity. By these mechanisms, it allows the flow of fluid into the extracellular space (10, 11). Its effects are considered to be chronic rather than short term (39).
In a meta-analysis published in 2017, where the effectiveness of LLLT in BCRL was investigated, it was reported that LLLT is more effective than sham laser treatment in reducing the limb volume and its effect on pain is also greater than sham laser therapy, in the short term (23). Another meta-analysis of LLLT in BCRL reported that the decrease in the limb volume was statistically and clinically significant in the groups in which low-dose laser therapy was added, and there was a some decrease in pain with low-dose laser therapy, but the evidence that it provided an additional effect to other treatments was not sufficient (40). A systematic review showed that LLLT may offer additional benefits compared to compression therapies (pneumatic compression or compression bandage), a placebo laser, or no treatment for patients with BCRL. However, LLLT did not appear to significantly improve outcomes when compared to with other types of active interventions (11).
Although there are some studies in the literature comparing the components of CDT, the standard treatment method in lymphedema, to the best of our knowledge, there is no study comparing LLLT, kinesio-taping and MLD in a single study. Thus we belive this is the first published study to directly compare kinesio-taping, MLD and LLLT.
The strengths of our study are the similarities of age, education level, diagnosis and treatment characteristics of the breast cancer, dominant extremity involvement, compression garment compliance, baseline lymphedematous extremity volumes and stage of lymphedema in all patients.
Limitations include the relatively low number of patients, and short follow-up of this study. Further limitations are the heterogeneity of some group characteristics including rates of obesity and housewife occupations, more chronic cases and less care-giver support in the MLD group.
Lymphedema is a chronic, progressive and disabling disease that needs self-management, including skin care, self-MLD massage, compressive garments, and exercises. Since MLD is time-consuming and tiresome, alternative treatments, such as kinesio-taping and LLLT should be considered. This study has demonstrated a similar effectiveness in treatment of early stage lymphedema.
Footnotes
Ethics Committee Approval: Ethical approval was obtained to conduct this study from the Institutional Review Board for Human Subjects (approval number: E-18-2025, date: 26.06.2018).
Informed Consent: Informed consent was obtained.
Peer-review: Externally peer-reviewed.
Authorship Contributions
Surgical and Medical Practices: S.S.Y., F.F.A.; Concept: S.S.Y., F.F.A.; Design: S.S.Y., F.F.A.; Data Collection and/or Processing: S.S.Y., F.F.A.; Analysis and/or Interpretation: S.S.Y., F.F.A.; Literature Search: S.S.Y., F.F.A.; Writing: S.S.Y., F.F.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 2.Executive Committee. The Diagnosis and Treatment of Peripheral Lymphedema: 2016 Consensus Document of the International Society of Lymphology. Lymphology. 2016;49:170–184. [PubMed] [Google Scholar]
- 3. [Internet] https://www.cancer.gov/aboutcancer/treatment/sideeffects/lymphedema/lymphedema-hp-pdq#link/_8_toc.
- 4.Soran A, D’Angelo G, Begovic M, Ardic F, Harlak A, Samuel Wieand H, et al. Breast cancer-related lymphedema--what are the significant predictors and how they affect the severity of lymphedema? Breast J. 2006;12:536–543. doi: 10.1111/j.1524-4741.2006.00342.x. [DOI] [PubMed] [Google Scholar]
- 5.Sayegh HE, Asdourian MS, Swaroop MN, Brunelle CL, Skolny MN, Salama L, et al. Diagnostic Methods, Risk Factors, Prevention, and Management of Breast Cancer-Related Lymphedema: Past, Present, and Future Directions. Curr Breast Cancer Rep. 2017;9:111–121. doi: 10.1007/s12609-017-0237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deliağaoğlu SÜ. Lenfödem Patofizyolojisi. In: Dalyan M, Borman P, Ayhan FF, editor. Lenfödem. 2017;. p.:29–46. [Google Scholar]
- 7.Tambour M, Holt M, Speyer A, Christensen R, Gram B. Manual lymphatic drainage adds no further volume reduction to Complete Decongestive Therapy on breast cancer-related lymphoedema: a multicentre, randomised, single-blind trial. Br J Cancer. 2018;119:1215–1222. doi: 10.1038/s41416-018-0306-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson B, Gaitatzis K, Janse de Jonge X, Blackwell R, Koelmeyer LA. Manual lymphatic drainage treatment for lymphedema: a systematic review of the literature. J Cancer Surviv. 2021;15:244–258. doi: 10.1007/s11764-020-00928-1. [DOI] [PubMed] [Google Scholar]
- 9.Kilmartin L, Denham T, Fu MR, Yu G, Kuo TT, Axelrod D, Guth AA. Complementary low-level laser therapy for breast cancer-related lymphedema: A pilot, double-blind, randomized, placebo-controlled study. Lasers Med Sci. 2020;35:95–105. doi: 10.1007/s10103-019-02798-1. [DOI] [PubMed] [Google Scholar]
- 10.Ridner SH, Poage-Hooper E, Kanar C, Doersam JK, Bond SM, Dietrich MS. A pilot randomized trial evaluating low-level laser therapy as an alternative treatment to manual lymphatic drainage for breast cancer-related lymphedema. Oncol Nurs Forum. 2013;40:383–393. doi: 10.1188/13.ONF.383-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Y, Ge Y, Xing W, Liu J, Wu J, Lin H, et al. The effectiveness and safety of low-level laser therapy on breast cancer–related lymphedema: An overview and update of systematic reviews. Lasers Med Sci. 2022;37:1389–1413. doi: 10.1007/s10103-021-03446-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torres-Lacomba M, Navarro-Brazález B, Prieto-Gómez V, Ferrandez JC, Bouchet JY, Romay-Barrero H. Effectiveness of four types of bandages and kinesio-tape for treating breast-cancer-related lymphoedema: a randomized, single-blind, clinical trial. Clin Rehabil. 2020;34:1230–1241. doi: 10.1177/0269215520935943. [DOI] [PubMed] [Google Scholar]
- 13.Malicka I, Rosseger A, Hanuszkiewicz J, Wozniewski M. Kinesiology Taping reduces lymphedema of the upper extremity in women after breast cancer treatment: a pilot study. Prz Menopauzalny. 2014;13:221–226. doi: 10.5114/pm.2014.44997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smykla A, Walewicz K, Trybulski R, Halski T, Kucharzewski M, Kucio C, et al. Effect of Kinesiology Taping on breast cancer-related lymphedema: a randomized single-blind controlled pilot study. Biomed Res Int. 2013;2013:767106. doi: 10.1155/2013/767106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanal-Toprak C, Ozsoy-Unubolo T, Bahar-Ozdemir Y, Akyuz G. The efficacy of intermittent pneumatic compression as a substitute for manual lymphatic drainage in complete decongestive therapy in the treatment of breast cancer related lymphedema. Lymphology. 2019;52:82–91. [PubMed] [Google Scholar]
- 16.Belmonte R, Tejero M, Ferrer M, Muniesa JM, Duarte E, Cunillera O, Escalada F. Efficacy of low-frequency low-intensity electrotherapy in the treatment of breast cancer-related lymphoedema: a cross-over randomized trial. Clin Rehabil. 2012;26:607–618. doi: 10.1177/0269215511427414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee KW, Kim SB, Lee JH, Kim YS. Effects of Extracorporeal Shockwave Therapy on Improvements in Lymphedema, Quality of Life, and Fibrous Tissue in Breast Cancer-Related Lymphedema. Ann Rehabil Med. 2020;44:386–392. doi: 10.5535/arm.19213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zuther JE, Norton S. Complex deconjestive therapy. Lymphedema Management, The comprehensive guide for practitioners. 3rd ed. Thieme Verlag KG, Germany, Sttuttgard. 2013;. p.:243–280. [Google Scholar]
- 19.Bosman J. Lymphtaping for lymphoedema: an overview of the treatment and its uses. Br J Community Nurs. 2014;Suppl: S12, S14, S16-S18. doi: 10.12968/bjcn.2014.19.sup4.s12. [DOI] [PubMed] [Google Scholar]
- 20.Kase K, Stockheimer KR. Kinesio taping for the superficial lymphatic pathways. Kinesio Taping for Lymphedema and Chronic Swelling. Kinesio USA, LLC. 2006;. p.:135–161. [Google Scholar]
- 21.Hassan MA, Ismail SM. Kinesio Tape Versus Compression Garment on Post Mastectomy Lymphedema. Med J Cairo Univ. 2015;83:187–192. [Google Scholar]
- 22.Kozanoglu E, Basaran S, Paydas S, Sarpel T. Efficacy of pneumatic compression and low-level laser therapy in the treatment of postmastectomy lymphoedema: a randomized controlled trial. Clin Rehabil. 2009;23:117–124. doi: 10.1177/0269215508096173. [DOI] [PubMed] [Google Scholar]
- 23.Baxter GD, Liu L, Petrich S, Gisselman AS, Chapple C, Anders JJ, et al. Low level laser therapy (Photobiomodulation therapy) for breast cancer-related lymphedema: a systematic review. BMC Cancer. 2017;17:833. doi: 10.1186/s12885-017-3852-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ayhan FF, Aykut M, Genç H, Mansız Kaplan B, Soran A. Is Complex Decongestive Physical Therapy Safe for Median Nerve at the Level of Carpal Tunnel in Breast Cancer Related Lymphedema? Lymphat Res Biol. 2019;17:78–86. doi: 10.1089/lrb.2018.0011. [DOI] [PubMed] [Google Scholar]
- 25.Brorson H, Höijer P. Standardised measurements used to order compression garments can be used to calculate arm volumes to evaluate lymphoedema treatment. J Plast Surg Hand Surg. 2012;46:410–415. doi: 10.3109/2000656X.2012.714785. [DOI] [PubMed] [Google Scholar]
- 26.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:44. doi: 10.1186/1471-2474-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Düger T, Yakut E, Öksüz Ç, Yörükan S, Bilgütay BS, Ayhan C, et al. Reliability and validity of the Turkish version of the disabilities of the arm, shoulder and hand (DASH) questionnaire. Fizyoterapi Rehabilitasyon. 2006;17:99–107. [Google Scholar]
- 28.Keeley V, Crooks S, Locke J, Veigas D, Riches K, Hilliam R. A quality of life measure for limb lymphedema (LYMQOL) J Lymphoedema. 2010;5:26–37. [Google Scholar]
- 29.Borman P, Yaman A, Denizli M, Karahan S, Özdemir O. The reliability and validity of Lymphedema Quality of Life Questionnaire-Arm in Turkish patients with upper limb lymphedema related with breast cancer. Turk J Phys Med Rehabil. 2018;64:205–212. doi: 10.5606/tftrd.2018.2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freynhagen R, Baron R, Gockel U, Tölle TR. PainDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006;22:1911–1920. doi: 10.1185/030079906X132488. [DOI] [PubMed] [Google Scholar]
- 31.Alkan H, Ardic F, Erdogan C, Sahin F, Sarsan A, Findikoglu G. Turkish version of the painDETECT questionnaire in the assessment of neuropathic pain: a validity and reliability study. Pain Med. 2013;14:1933–1943. doi: 10.1111/pme.12222. [DOI] [PubMed] [Google Scholar]
- 32.Riddle DL, Rothstein JM, Lamb RL. Goniometric reliability in a clinical setting. Shoulder measurements. Phys Ther. 1987;67:668–673. doi: 10.1093/ptj/67.5.668. [DOI] [PubMed] [Google Scholar]
- 33.Desu, M. M. and Raghavarao, D. 1990. Sample Size Methodology. Academic Press. New York. Fleiss, Joseph L. 1986. The Design and Analysis of Clinical Experiments. John Wiley & Sons. New York. Kirk, Roger E. 1982. Experimental Design: Procedures for the Behavioral Sciences. Brooks/Cole. Pacific Grove, California. [Internet]
- 34.Ezzo J, Manheimer E, McNeely ML, Howell DM, Weiss R, Johansson KI, et al. Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database Syst Rev. 2015;CD003475. doi: 10.1002/14651858.CD003475.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Müller M, Klingberg K, Wertli MM, Carreira H. Manual lymphatic drainage and quality of life in patients with lymphoedema and mixed oedema: a systematic review of randomised controlled trials. Qual Life Res. 2018;27:1403–1414. doi: 10.1007/s11136-018-1796-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ayhan FF, Duyur Çakıt B. Lenfödem Tedavisinde Kinezyolojik Bantlama. In: Dalyan M, Borman P, Ayhan FF, editor. Lenfödem. 2017;.p.:171–180. [Google Scholar]
- 37.Kasawara KT, Mapa JMR, Ferreira V, Added MAN, Shiwa SR, Carvas N Jr, et al. Effects of Kinesio Taping on breast cancer-related lymphedema: A meta-analysis in clinical trials. Physiother Theory Pract. 2018;34:337–345. doi: 10.1080/09593985.2017.1419522. [DOI] [PubMed] [Google Scholar]
- 38.Gatt M, Willis S, Leuschner S. A meta-analysis of the effectiveness and safety of kinesiology taping in the management of cancer-related lymphoedema. Eur J Cancer Care (Engl) 2017;26. doi: 10.1111/ecc.12510. [DOI] [PubMed] [Google Scholar]
- 39.Dirican A, Andacoglu O, Johnson R, McGuire K, Mager L, Soran A. The short-term effects of low-level laser therapy in the management of breast-cancer-related lymphedema. Support Care Cancer. 2011;19:685–690. doi: 10.1007/s00520-010-0888-8. [DOI] [PubMed] [Google Scholar]
- 40.Smoot B, Chiavola-Larson L, Lee J, Manibusan H, Allen DD. Effect of low-level laser therapy on pain and swelling in women with breast cancer-related lymphedema: a systematic review and meta-analysis. J Cancer Surviv. 2015;9:287–304. doi: 10.1007/s11764-014-0411-1. [DOI] [PubMed] [Google Scholar]


