Abstract
Background
Up to 3% of all Emergency Department (ED) visits are due to skin and soft tissue infections such as non-purulent cellulitis. The current treatment failure rate is approximately 20%. Evidence is lacking regarding the optimal outpatient management of cellulitis.
Objectives
To evaluate the feasibility of a randomized trial comparing high-dose (1000 mg) to standard-dose (500 mg) cephalexin to treat ED patients with cellulitis.
Methods
A parallel arm double-blind randomized controlled pilot trial conducted at two EDs in Canada. Eligible participants were adults (age ≥ 18 years) presenting to the ED with non-purulent cellulitis and determined by the treating emergency physician to be eligible for outpatient management with oral antibiotics. Participants were randomized to high-dose or standard-dose cephalexin four times daily for 7 days. The primary feasibility outcome was participant recruitment rate (target ≥ 35%). The preliminary primary effectiveness outcome was oral antibiotic treatment failure.
Results
Of 134 eligible participants approached for trial participation, 69 (51.5%, 95% CI 43.1 to 59.8%) were recruited and randomized. After excluding three randomized participants due to an alternate diagnosis, 33 participants were included in each arm. Nineteen eligible cases (14.2%) were missed. Loss to follow-up was 6.1%. Treatment failure occurred in four patients (12.9%) in the standard-dose arm versus one patient (3.2%) in the high-dose arm. A greater proportion had minor adverse events in the high-dose arm. No patients had an unplanned hospitalization within 14 days.
Conclusion
This pilot randomized controlled trial comparing high-dose to standard-dose cephalexin for ED patients with cellulitis demonstrated a high participant recruitment rate and that a full-scale trial is feasible. High-dose cephalexin had fewer treatment failures but with a higher proportion of minor adverse effects. The findings of this pilot will be used to inform the design of a future large trial.
Trial registration
This trial was registered at ClinicalTrials.gov (NCT04471246).
Supplementary Information
The online version contains supplementary material available at 10.1007/s43678-022-00433-7.
Keywords: Cellulitis, Oral antibiotics, Treatment failure, Cephalexin
Résumé
Contexte
Jusqu'à 3% de toutes les visites aux urgences sont dues à des infections de la peau et des tissus mous, comme la cellulite non purulente. Le taux actuel d’échec du traitement est d’environ 20%. Il manque des données probantes sur la gestion optimale de la cellulite en consultation externe.
Objectifs
Évaluer la faisabilité d'un essai randomisé comparant la céfalexine à dose élevée (1000 mg) à la céfalexine à dose normale (500 mg) pour traiter les patients des urgences atteints de cellulite.
Méthodes
Un essai pilote contrôlé randomisé en double aveugle à bras parallèles mené dans deux services d'urgence au Canada. Les participants éligibles étaient des adultes (âge ≥ 18 ans) se présentant aux urgences avec une cellulite non purulente et déterminés par l'urgentiste traitant comme pouvant bénéficier d'une prise en charge ambulatoire par antibiotiques oraux. Les participants ont été randomisés entre la céfalexine à dose élevée et la céfalexine à dose normale, quatre fois par jour pendant 7 jours. Le résultat primaire de faisabilité était le taux de recrutement des participants (objectif ≥ 35%). Le résultat primaire préliminaire d'efficacité était l'échec du traitement antibiotique oral.
Résultats
Sur les 134 participants éligibles sollicités pour participer à l'essai, 69 (51,5%, IC à 95% 43,1% à 59,8%) ont été recrutés et randomisés. Après avoir exclu trois participants randomisés en raison d'un autre diagnostic, 33 participants au total ont été inclus dans chaque bras. Au total, 19 cas éligibles (14,2%) ont été manqués. Le taux de perte au suivi était de 6,1%. L'échec du traitement est survenu chez quatre patients (12,9%) dans le groupe à dose standard contre un patient (3,2%) dans le groupe à dose élevée. Une plus grande proportion de patients ont eu des effets indésirables mineurs dans le groupe à forte dose. Aucun patient n'a été hospitalisé de façon imprévue dans les 14 jours.
Conclusion
Cet essai pilote randomisé et contrôlé comparant la céphalexine à dose élevée à la céfalexine à dose normale pour les patients des urgences atteints de cellulite a démontré un taux élevé de recrutement de participants et la faisabilité d'un essai à grande échelle. La céfalexine à forte dose a entraîné moins d'échecs thérapeutiques, mais avec une proportion plus élevée d'effets indésirables mineurs. Les résultats de ce projet pilote serviront de base à la conception d'un futur essai à grande échelle.
Inscription à l'essai
Cet essai a été enregistré sur ClinicalTrials.gov (NCT04471246).
Mots clés: cellulite, antibiotiques oraux, échec du traitement, céfalexine
Introduction
Non-purulent cellulitis is a painful bacterial skin and soft tissue infection affecting the subcutaneous tissue [1]. Up to 3% of all emergency department (ED) visits are for skin and soft tissue infections [2, 3]. Most ED patients with cellulitis may be treated with oral antibiotics and discharged home. Oral antibiotic therapy holds several advantages over the intravenous route, including lower risk of complications, decreased cost, and increased patient convenience and comfort [4, 5]. However, overuse of intravenous antibiotics is common [6, 7]. There has been limited evidence-based guidance for clinicians with respect to cellulitis treatment.
Owing to a lack of high-quality evidence, published empiric treatment guidelines are largely based on expert opinion [8–11]. In addition, the current oral antibiotic treatment failure rate of 20% is unacceptably high [12–14]. Cephalexin is the most commonly prescribed antibiotic for cellulitis treatment in Canadian EDs [15]. High-dose cephalexin (1000 mg four times daily) achieves a higher peak serum concentration than standard-dose cephalexin (500 mg four times daily), and reaches serum concentrations that are comparable to intravenous cephalosporins [16, 17]. When compared to standard-dose oral cephalexin, high-dose cephalexin may reduce treatment failure, which would decrease the need for intravenous antibiotics and subsequent hospitalization.
We conducted a double-blind pilot randomized controlled trial comparing high-dose to standard-dose cephalexin for ED patients with cellulitis. The overall goals were to (1) establish feasibility and refine study procedures before embarking on a larger, fully powered multicenter trial; and (2) describe clinical outcomes of interest in the intervention and control arms. The specific objectives were to (1) measure feasibility outcomes (e.g., recruitment rate, success of blinding, and adherence); and (2) measure patient outcomes, including oral antibiotic treatment failure and frequency of adverse events.
Methods
Study design and setting
We conducted a parallel arm double-blind randomized controlled pilot trial at the Civic and General campus EDs of The Ottawa Hospital. The study was conducted between August 16, 2021 and February 23, 2022. The study was approved by the Ottawa Health Science Network Research Ethics Board and the trial was registered on ClinicalTrials.gov (NCT04471246).
Participants
Eligible participants were adults (age ≥ 18 years) presenting to the ED with non-purulent cellulitis and determined by the treating emergency physician to be eligible for outpatient management with oral antibiotics. Reasons for exclusion were as follows: (i) patient already taking oral antibiotics; (ii) abscess requiring incision and drainage; (iii) known prior cellulitis secondary to methicillin-resistant Staphylococcus aureus; (iv) cellulitis secondary to a human or animal bite wound; (iv) surgical site infection; (v) malignancy being treated with chemotherapy; (vi) febrile neutropenia (temperature ≥ 38.0 °C plus absolute neutrophil count < 500 cells/μL); (vii) transplant recipient; (viii) renal impairment with creatinine clearance < 30 mL/min; (ix) pregnant or breastfeeding; (x) allergy to cephalosporins or known anaphylaxis to penicillin; and (xi) inability or refusal to provide consent.
Interventions
Experimental group
Participants randomized to the experimental group received a 7-day prescription of cephalexin 1000 mg four times daily.
Control group
Participants randomized to the control group received a 7-day course of cephalexin 500 mg four times daily plus oral placebo. Cephalexin and placebo tablets were encased in identical capsules and prepared independently by The Ottawa Hospital Pharmacy. The patients, treating physician and research team were blinded. Blinding was important in order to eliminate bias for reporting patient-important outcomes such as degree of pain and adverse events.
Procedures
Eligible participants were approached by the research team (available 7 days a week from 0800 to 2000) for trial participation using integrated verbal consent. Enrolled participants were randomized (1:1) to high-dose versus standard-dose arms. The randomization sequence was computer generated using a permuted block design with block lengths of 4. Allocation was stratified by infection site (lower limb vs. other).
At the index ED visit, a research assistant collected baseline clinical data including triage vital signs, comorbidities, infection location, area of erythema and degree of pain using an 11-point numeric rating scale (NRS) from 0 to 10. All participants were provided with disposable tape measures and temperature strips to record area of erythema and temperature at follow-up visits, respectively. The research assistant asked each participant to download a free mobile application (Preventicus Heartbeats; https://www.preventicus.com/en/) to allow participants to measure their heart rate at follow-up visits.
Follow-up visits were scheduled on day 3 (mid-therapy) and 7 (end-of-therapy). Trained research assistants conducted follow-up visits virtually using a mobile device (tablet or phone) using Zoom or FaceTime. If patients were unable or declined virtual follow-up, they were given the option of an in-home visit or follow-up in the ED. The following data were collected at the mid-therapy and end-of-therapy visits: temperature, heart rate, degree of pain and area of erythema. Study participants completed a questionnaire on day 7 to assess effectiveness of blinding, medication adherence, adverse events and satisfaction with the integrated consent process (see Appendix). Research assistants contacted all participants via telephone at 14 days to determine if there were any unplanned visits to see a physician or adverse events.
Outcomes
The primary feasibility outcome was participant recruitment rate, defined as the percentage of approached eligible patients successfully recruited over 6 months. The feasibility target was recruitment of ≥ 29% of eligible participants. Secondary feasibility outcomes were: (i) ability to approach eligible participants (goal < 10% missed); (ii) ability to blind patients (assessed using a questionnaire); (iii) adherence to allocated treatment for 7 days; and (iv) loss to follow-up (goal < 10% attrition).
The preliminary primary effectiveness outcome was oral antibiotic treatment failure [18], defined as a change in antibiotic (change in class of oral antibiotic or escalation to intravenous therapy) within 7 days due to worsening infection. Worsening infection was defined as any of the following: (i) new fever (temperature ≥ 38.0 °C) or persistent fever at follow-up; (ii) increasing area of erythema ≥ 20% from baseline; or (iii) increasing pain ≥ 2 points from baseline using the NRS. Patients were assessed for worsening infection criteria at day 3 and 7 follow-up, or if the patient had an unscheduled return ED between day 3 and 7. Secondary effectiveness outcomes were: (i) clinical cure (no erythema, pain and fever) at day 7 and 14; (ii) clinical response (≥ 20% reduction in area of erythema compared to baseline) at day 3; (iii) adverse events at 14 days; and (iv) unplanned return ED visits or hospitalization at 14 days.
Sample size
The sample size for this pilot trial was based on the primary objective of demonstrating feasibility of recruitment. First, we calculated the required sample size for the future large trial. Assuming a treatment failure rate with standard-dose cephalexin of 20% [12–14], a future multicenter trial would require a total of 2552 participants to achieve 90% power to detect a minimum important difference of 5% in treatment failures in the high-dose cephalexin versus standard-dose cephalexin arm.
The sites participating in this trial (Civic and General ED) treat approximately 200 cellulitis patients with oral antibiotics annually [14]. If at least 180 patients can be approached per site per year, a minimum of 29% (52 participants) must be recruited at each site to meet the feasibility target. Based on previous experience with similar trials, we anticipated being able to recruit up to 35% of eligible patients. With 180 patients approached at each site, a 90% two-sided confidence interval around the anticipated recruitment rate would have a total width of 12%, i.e., a lower limit of 29.1% and an upper limit of 41.3%. Since the lower limit excludes the minimum feasibility target of 29%, we can be 90% confident that the future trial is feasible. Thus, our target sample size was 64 patients across both sites over 6 months.
Data management and statistical analysis
All data were entered into a secure web-based electronic data capture system. Baseline demographic and clinical characteristics were described using descriptive statistics. Primary and secondary feasibility and effectiveness outcomes were described using frequency and proportions. As this was a pilot trial, and in accordance with recommendations for pilot studies, no statistical significance testing was carried out to compare outcomes between the groups. Analysis was conducted according to an intention-to-treat protocol.
Results
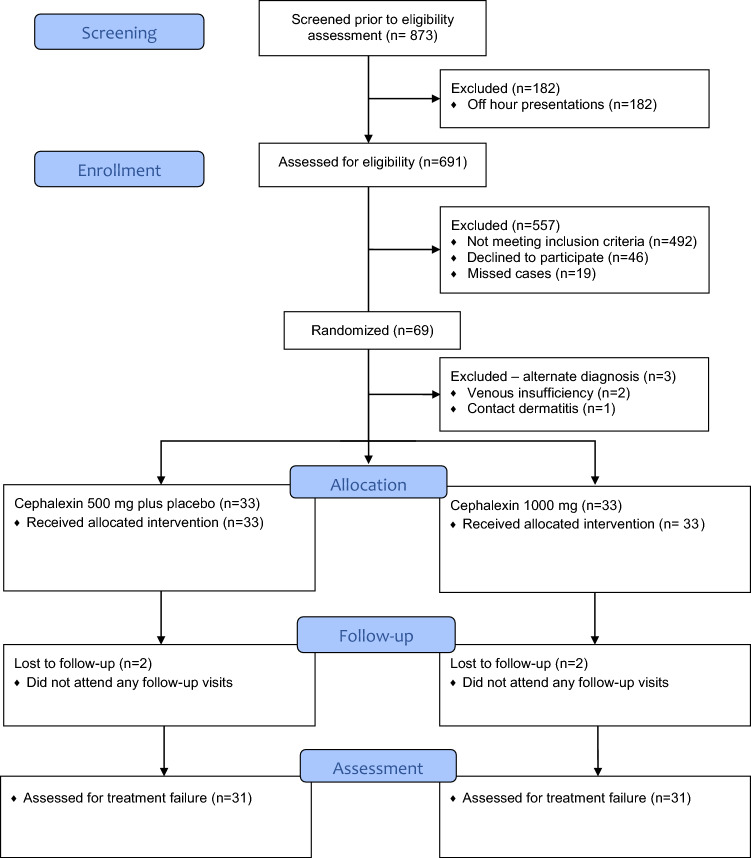
Sixty-nine participants were enrolled into the trial. Three participants were excluded after randomization due to an alternate diagnosis identified at an unscheduled return ED visit within 3 days (2 patients with venous insufficiency, 1 patient with contact dermatitis) and 33 participants were allocated into each study arm (Fig. 1). The baseline demographics are shown in Table 1. There was a higher prevalence in the high-dose cephalexin group versus the standard-dose cephalexin group of obesity (54.5% vs. 36.4%) and diabetes mellitus (24.2% vs. 6.1%). Infection characteristics such as location, baseline pain score and vital signs were similar between the groups.
Fig. 1.
CONSORT flow diagram
Table 1.
Baseline characteristics of N = 66 emergency department patients with cellulitis
| Baseline characteristic | Cephalexin 500 mg plus placebo | Cephalexin 1000 mg |
|---|---|---|
| N = 33 (50.0%) | N = 33 (50.0%) | |
| Hospital site, n (%) | ||
| TOH Civic campus | 12 (36.4%) | 15 (45.5%) |
| TOH General campus | 21 (63.6%) | 18 (54.5%) |
| Age (years), median (IQR) | 57 (40–69) | 56 (34–71) |
| Female sex, n (%) | 13 (39.4%) | 13 (39.4%) |
| Body Mass Index (kg/m2), median (IQR) | 27.9 (23.4–31.6) | 30.4 (24.4–36.8) |
| Comorbidities, n (%) | ||
| Obesity | 12 (36.4%) | 18 (54.5%) |
| Diabetes mellitus | 2 (6.1%) | 8 (24.2%) |
| Prior cellulitis in the past 12 months | 4 (12.1%) | 2 (6.1%) |
| Chronic kidney disease | 1 (3.0%) | 3 (9.1%) |
| Congestive heart failure | 1 (3.0%) | 3 (9.1%) |
| Coronary artery disease | 0 (0.0%) | 2 (6.1%) |
| Injection drug use | 1 (3.0%) | 1 (3.0%) |
| Chronic venous insufficiency | 1 (3.0%) | 0 (0.0%) |
| HIV | 1 (3.0%) | 0 (0.0%) |
| Peripheral vascular disease | 0 (0.0%) | 1 (3.0%) |
| Corticosteroids | 0 (0.0%) | 0 (0.0%) |
| Lymphedema/venous stasis | 0 (0.0%) | 0 (0.0%) |
| History of MRSA infection or colonization | 0 (0.0%) | 0 (0.0%) |
| Infection characteristics, n (%) | ||
| Location | ||
| Lower limb | 20 (60.6%) | 19 (57.6%) |
| Upper limb | 7 (21.2%) | 7 (21.2%) |
| Face | 4 (12.1%) | 3 (9.1%) |
| Torso | 2 (6.1%) | 2 (6.1%) |
| Groin | 0 (0.0%) | 2 (6.1%) |
| Axilla | 0 (0.0%) | 0 (0.0%) |
| Chronic ulcers at site | 3 (9.1%) | 0 (0.0%) |
| Area of erythema (cm2), median (IQR) | 168 (81–512) | 162 (50–240) |
| Baseline pain (NRS 0–10), median (IQR) | 4 (2–7) | 5 (3–8) |
| Triage vital signs, median (IQR) | ||
| Temperature (°C) | 36.7 (36.5–36.9) | 36.6 (36.0–37.0) |
| Heart rate (beats/min) | 83 (70–93) | 90 (77–97) |
| Respiratory rate (breaths/min) | 16 (16–18) | 18 (16–18) |
| Systolic blood pressure (mmHg) | 137.5 (127–153) | 134 (123–147) |
| Diastolic blood pressure (mmHg) | 82 (73–92) | 82 (73–88) |
| Laboratory tests, median (IQR) | ||
| WBC count (× 109/L) | 6.9 (5.2–7.3) | 8.7 (7.8–10.9) |
| Serum creatinine (μmol/L) | 65 (52–97) | 78 (64–108) |
TOH The Ottawa Hospital, IQR interquartile range, HIV human immunodeficiency virus, MRSA methicillin-resistant Staphylococcus aureus, NRS numeric rating scale
The primary feasibility outcome of participant recruitment rate was 51.5% (95% CI 43.1 to 59.8%), which exceeded the minimum target of 35% (Table 2). Nineteen (14.2%) of eligible cases were missed which exceeded our prespecified target of < 10% missed for this secondary feasibility outcome. Only 47.0% of participants were able to correctly guess the treatment allocation. The remainder either guessed incorrectly (27.3%) or were unsure or did not provide an answer (25.7%). Complete loss to follow-up (i.e., did not attend any follow-up visit) was 6.1%, which satisfied our target of < 10% attrition. The majority of participants (75.8%) reported being fully adherent to the treatment regimen.
Table 2.
Feasibility outcomes
| Feasibility outcome | N (%) |
|---|---|
| Participant recruitment rate | 69/134 (51.5%) |
| Ability to approach eligible patients | 19/134 (14.2% missed) |
| Blinding | |
| Correctly guessed allocation | 31/66 (47.0%) |
| Incorrectly guessed allocation | 18/66 (27.3%) |
| Unsure/missing | 17/66 (25.8%) |
| Full adherence to 7-day treatment course | 50/66 (75.8%) |
| Loss to follow-up* | 4/66 (6.1%) |
*Did not attend any follow-up visit at days 3, 7 and 14
The preliminary effectiveness outcomes are shown in Table 3. For the primary effectiveness outcome, oral antibiotic treatment failure occurred in four patients (12.9%) in the standard-dose arm versus one patient (3.2%) in the high-dose arm. Clinical response was similar at day 3, although a greater proportion of participants had complete clinical cure at day 7 (16.1% vs. 6.5%) and day 14 (45.2% vs. 38.7%) in the high-dose arm versus the standard-dose arm. A greater percentage of participants in the high-dose arm had adverse events (38.7% vs. 25.8%), which were predominantly nausea/vomiting (9.7% vs. 3.2%) or diarrhea (16.1% vs. 6.5%). A similar small number of participants in both groups had an unplanned ED or family doctor visit. No participants had an unplanned hospitalization within 14 days.
Table 3.
Effectiveness outcomes
| Effectiveness outcome, n (% [95% CI]) | Cephalexin 500 mg plus placebo | Cephalexin 1000 mg |
|---|---|---|
| N = 31 (50.0%) | N = 31 (50.0%) | |
| Oral antibiotic treatment failure* | 4 (12.9% [5.1–28.9%]) | 1 (3.2% [0.6–16.2%]) |
| Change in class of oral antibiotic | 3 (9.7% [3.4–24.9%]) | 0 (0.0% [0.0–11.0%] |
| Switch to intravenous antibiotic | 1 (3.2% [0.6–16.2%]) | 1 (3.2% [0.6–16.2%]) |
| Clinical response† (day 3) | 19 (61.3% [43.8–76.3%]) | 18 (58.1% [40.8–73.6%]) |
| Clinical cure¶ | ||
| Day 7 | 2 (6.5% [1.8–20.7%]) | 5 (16.1% [7.1–32.6%]) |
| Day 14 | 12 (38.7% [23.7–56.2%]) | 14 (45.2% [29.2–62.2%]) |
| Adverse events | 8 (25.8% [13.7–43.3%]) | 12 (38.7% [23.7–56.2%]) |
| Nausea or vomiting | 1 (3.2% [0.6–16.2%]) | 3 (9.7% [3.4–24.9%]) |
| Diarrhea | 2 (6.5% [1.8–20.7%]) | 5 (16.1% [7.1–32.6%]) |
| Abdominal pain | 0 (0.0% [0.0–11.0%]) | 1 (3.2% [0.6–16.2%]) |
| Rash | 2 (6.5% [1.8–20.7%]) | 1 (3.2% [0.6–16.2%]) |
| Other | 3 (9.7% [3.4–24.9%]) | 2 (6.5% [1.8–20.7%]) |
| None | 23 (74.2% [56.8–86.3%]) | 19 (61.3% [43.8–76.3%]) |
| Unplanned visit to family doctor within 14 d | 2 (6.5% [1.8–20.7%]) | 2 (6.5% [1.8–20.7%]) |
| Unplanned return ED visit within 14 d | 5 (16.1% [7.1–32.6%]) | 7 (22.6% [11.4–39.8%]) |
| Unplanned hospitalization within 14 d | 0 (0.0% [0.0–11.0%]) | 0 (0.0% [0.0–11.0%]) |
ED emergency department
*Treatment failure: change in antibiotic (class of oral antibiotic or step up to intravenous antibiotic) within 7 days due to worsening infection: (a) new fever or persistent fever; or (b) increasing area of erythema ≥ 20% from baseline; or (c) increasing pain ≥ 2 points from baseline using the numeric rating scale
†Clinical response: ≥ 20% reduction in area of erythema at day 3
¶Clinical cure: no erythema, pain or fever
The majority of participants completed their follow-up assessments virtually at day 3 (90.5%) and day 7 (88.0%). At day 7 follow-up, participants were asked to rate their level of satisfaction with the integrated verbal consent process (very satisfied, satisfied, neutral, unsatisfied, very unsatisfied). There was a high degree of satisfaction with the integrated consent process with 96.5% reporting being either very satisfied or satisfied. No respondents reported dissatisfaction with the consent process. When asked if they would prefer the verbal integrated consent process in a future trial, 74.1% reported they would and 20.7% were unsure. Only 5.2% of respondents indicated they would not prefer this type of consent.
Discussion
Feasibility and considerations for a future full-scale trial
This study was able to demonstrate that it was feasible to recruit ED patients with non-purulent cellulitis who require outpatient oral antibiotic treatment. The minimum primary feasibility outcome target of at least 35% recruitment was exceeded. Less than half of trial participants were able to correctly guess their treatment allocation, which suggests that blinding was adequate. Total loss to follow-up was less than our prespecified target of < 10% attrition.
However, we did not meet the secondary feasibility outcome of < 10% missed eligible patients approached to participate in this trial. The ED is a fast-paced environment and cellulitis is a diagnosis that is typically made clinically without the need for investigations. Given this, some patients may have been rapidly diagnosed and treated prior to our research team having an opportunity to approach the treating clinician and patient. It is also possible that some clinicians may have not recalled that the trial was underway. In a future trial, we will aim to increase the number of educational sessions for clinicians. Furthermore, we will implement a prompt on the electronic health record for patients with chief complaints related to cellulitis. These steps should improve clinician awareness about the trial and help reduce the number of missed eligible cases.
We were able to successfully implement a verbal integrated consent process and a majority of participants were satisfied with this approach. In our initial planning phase, we intended for in-person home visits or ED visits to complete follow-up visits. With the onset of the COVID-19 pandemic, this was a suboptimal choice as increased in-person contact may increase risk of infection to both patients and the research team. We adapted by instead planning for virtual follow-up visits. Those unable to participate were still given the option of an in-person visit. Almost all participants followed up in a virtual format, which increases patient convenience and maximizes safety with respect to acquired respiratory infections.
Strengths and limitations
This is the first trial to compare two dosing strategies of oral cephalexin to treat cellulitis. We were able to demonstrate that a full-scale trial is feasible. Given challenges with the ongoing COVID-19 pandemic, virtual follow-up strategies were successfully implemented.
There are important limitations that warrant mention. First, there was a small proportion of participants who reported clinical cure (i.e., complete resolution of symptoms) at the end-of-therapy visit. We have recently published a systematic review that demonstrates that symptoms such as pain and erythema can persist beyond 14 days [19]. Second, given the final patient follow-up occurred at 14 days, we were unable to assess for infection recurrence beyond this timeframe. The follow-up time should have been longer. We will mitigate this in a future trial by including a 30-day telephone follow-up to determine rates of clinical cure and infection recurrence. Third, the secondary feasibility target of < 10% missed eligible patients was not met. We will implement strategies (e.g., increased educational sessions, prompts on the electronic health record) to improve study awareness for the future planned trial.
Clinical implications: preliminary effectiveness
A greater proportion of patients in the standard-dose arm had a treatment failure. This is despite more patients with obesity and diabetes mellitus in the high-dose arm. In a future full-scale trial, we will stratify the randomization according to body mass index in addition to infection site. A greater proportion of patients in the high-dose arm reported adverse events that were predominantly gastrointestinal symptoms. However, no patients stopped their antibiotic due to adverse events. Importantly, the results concerning preliminary effectiveness should not be used to influence clinical practice: a robust, well-powered future trial is required to address the question of effectiveness.
Pharmacokinetic and pharmacodynamic considerations in relation to any potential benefit of high-dose cephalosporins are important to consider. Cephalosporins are hydrophilic antibiotics that depend on time above the minimum inhibitory concentration levels for their efficacy in treating infections. Cephalexin is rapidly cleared by the kidneys which could lead to accelerated clearance of the drug in obese patients [20, 21]. In addition, cephalosporins are known to exhibit significant inoculum effect by which the minimum inhibitory concentrations for some organisms that are common causes of skin and soft tissue infections (like Staphylococcus aureus) are transiently increased, and therefore, their antibacterial activity is attenuated when the burden of bacteria is high (as may happen in a yet untreated episode of cellulitis) [22, 23]. These are situations in which higher doses of cephalexin could be more effective than lower (i.e., standard) doses. For the full-scale trial, we plan to conduct a subgroup analysis of patients with obesity.
Research implications
The planned full-scale future trial will utilize a verbal integrated consent model and virtual patient follow-ups. Our team will offer alternative methods of patient follow-up to avoid selection bias toward those that possess mobile technologies. We intend to implement a number of strategies to try and increase the proportion of eligible patients that will be approached to participate in the trial. In the full-scale trial, randomization will be stratified by cellulitis location and body mass index. A longer follow-up duration will be incorporated so as not to miss potentially important patient outcomes.
Conclusions
This pilot randomized controlled trial comparing high-dose to standard-dose cephalexin for ED patients with cellulitis demonstrated a high participant recruitment rate and that a full-scale trial is feasible. High-dose cephalexin had fewer treatment failures but with a higher proportion of minor adverse effects. The findings of this trial will be used to optimize the design of a future definitive trial.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to sincerely thank the Network of Canadian Emergency Researchers (NCER) for peer-review and full endorsement of the trial protocol.
Author contributions
KY, DE, JJP, MT, VCM, KNS and IGS were involved in developing the study design. KY and GSG were involved in developing and overseeing study procedures and patient follow-up. MT and MJN oversaw data analysis. All the authors revised and approved the manuscript as a whole.
Funding
Funding was provided by Canadian Association of Emergency Physicians (CAEP) Emergency Medicine Advancement Fund (EMAF) Grant, The Ottawa Hospital Academic Medical Organization (TOHAMO) Innovation Grant.
Declarations
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Stevens DL, Eron LL. Cellulitis and soft-tissue infections. Review. Ann Intern Med. 2009;150(1):ITC11. doi: 10.7326/0003-4819-150-1-200901060-01001. [DOI] [PubMed] [Google Scholar]
- 2.Stenstrom R, Grafstein E, Romney M, et al. Prevalence of and risk factors for methicillin-resistant Staphylococcus aureus skin and soft tissue infection in a Canadian emergency department [Erratum appears in CJEM. 2009 Nov;11(6):570] CJEM Can. 2009;11(5):430–438. doi: 10.1017/S1481803500011623. [DOI] [PubMed] [Google Scholar]
- 3.Pallin DJ, Egan DJ, Pelletier AJ, Espinola JA, Hooper DC, Camargo CA., Jr Increased US emergency department visits for skin and soft tissue infections, and changes in antibiotic choices, during the emergence of community-associated methicillin-resistant Staphylococcus aureus. Ann Emerg Med. 2008;51(3):291–298. doi: 10.1016/j.annemergmed.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 4.Li HK, Agweyu A, English M, Bejon P. An unsupported preference for intravenous antibiotics. Research Support Non-U.S. Gov't. PLoS Med. 2015;12(5):e1001825. doi: 10.1371/journal.pmed.1001825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cyriac JM, James E. Switch over from intravenous to oral therapy: a concise overview. Review. J Pharmacol Pharmacother. 2014;5(2):83–87. doi: 10.4103/0976-500X.130042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hecker MT, Aron DC, Patel NP, Lehmann MK, Donskey CJ. Unnecessary use of antimicrobials in hospitalized patients: current patterns of misuse with an emphasis on the antianaerobic spectrum of activity. Arch Intern Med. 2003;163(8):972–978. doi: 10.1001/archinte.163.8.972. [DOI] [PubMed] [Google Scholar]
- 7.McCarthy K, Avent M. Oral or intravenous antibiotics? Aust Prescr. 2020;43(2):45–48. doi: 10.18773/austprescr.2020.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Research Support Non-U.S. Gov't. Clin Infect Dis. 2014;59(2):e10–52. doi: 10.1093/cid/ciu444. [DOI] [PubMed] [Google Scholar]
- 9.Clinical Resource Efficiency Support Team . Guidelines on the management of cellulitis in adults. Belfast: CREST; 2005. [Google Scholar]
- 10.British Lymphology Society . Consensus document on the management of cellulitis in lymphoedema. Lichfield: British Lymphology Society; 2016. [Google Scholar]
- 11.Kwak YG, Choi SH, Kim T, et al. Clinical guidelines for the antibiotic treatment for community-acquired skin and soft tissue infection. Infect Chemother. 2017;49(4):301–325. doi: 10.3947/ic.2017.49.4.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murray H, Stiell I, Wells G. Treatment failure in emergency department patients with cellulitis. CJEM. 2005;7(4):228–234. doi: 10.1017/S1481803500014342. [DOI] [PubMed] [Google Scholar]
- 13.Peterson D, McLeod S, Woolfrey K, McRae A. Predictors of failure of empiric outpatient antibiotic therapy in emergency department patients with uncomplicated cellulitis. Acad Emerg Med. 2014;21(5):526–531. doi: 10.1111/acem.12371. [DOI] [PubMed] [Google Scholar]
- 14.Yadav K, Suh KN, Eagles D, et al. Predictors of oral antibiotic treatment failure for non-purulent skin and soft tissue infections in the emergency department. Acad Emerg Med. 2018;26:13492. doi: 10.1111/acem.13492. [DOI] [PubMed] [Google Scholar]
- 15.Yadav K, Gatien M, Corrales-Medina V, Stiell I. Antimicrobial treatment decision for non-purulent skin and soft tissue infections in the emergency department. CJEM. 2017;19(3):175–180. doi: 10.1017/cem.2016.347. [DOI] [PubMed] [Google Scholar]
- 16.Chow M, Quintiliani R, Cunha BA, Thompson M, Finkelstein E, Nightingale CH. Pharmacokinetics of high-dose oral cephalosporins. J Clin Pharmacol. 1979;19(4):185–194. doi: 10.1002/j.1552-4604.1979.tb01650.x. [DOI] [PubMed] [Google Scholar]
- 17.Wise R. The pharmacokinetics of the oral cephalosporins—a review. J Antimicrob Chemother. 1990;26(Suppl E):13–20. doi: 10.1093/jac/26.suppl_E.13. [DOI] [PubMed] [Google Scholar]
- 18.Yadav K, Nath A, Suh KN, Sikora L, Eagles D. Treatment failure definitions for non-purulent skin and soft tissue infections: a systematic review. Infection. 2019 doi: 10.1007/s15010-019-01347-w. [DOI] [PubMed] [Google Scholar]
- 19.Yadav K, Krzyzaniak N, Alexander C, et al. The impact of antibiotics on clinical response over time in uncomplicated cellulitis: a systematic review and meta-analysis. Infection. 2022 doi: 10.1007/s15010-022-01842-7. [DOI] [PubMed] [Google Scholar]
- 20.Griffith RS. The pharmacology of cephalexin. Postgrad Med J. 1983;59(Suppl 5):16–27. [PubMed] [Google Scholar]
- 21.Gerchman F, Tong J, Utzschneider KM, et al. Body mass index is associated with increased creatinine clearance by a mechanism independent of body fat distribution. J Clin Endocrinol Metab. 2009;94(10):3781–3788. doi: 10.1210/jc.2008-2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nannini EC, Stryjewski ME, Singh KV, et al. Determination of an inoculum effect with various cephalosporins among clinical isolates of methicillin-susceptible Staphylococcus aureus. Antimicrob Agents Chemother. 2010;54(5):2206–2208. doi: 10.1128/aac.01325-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lenhard JR, Bulman ZP. Inoculum effect of β-lactam antibiotics. J Antimicrob Chemother. 2019;74(10):2825–2843. doi: 10.1093/jac/dkz226. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.