Abstract
The American Diabetes Association (ADA) “Standards of Care in Diabetes” includes the ADA’s current clinical practice recommendations and is intended to provide the components of diabetes care, general treatment goals and guidelines, and tools to evaluate quality of care. Members of the ADA Professional Practice Committee, a multidisciplinary expert committee, are responsible for updating the Standards of Care annually, or more frequently as warranted. For a detailed description of ADA standards, statements, and reports, as well as the evidence-grading system for ADA’s clinical practice recommendations and a full list of Professional Practice Committee members, please refer to Introduction and Methodology. Readers who wish to comment on the Standards of Care are invited to do so at professional.diabetes.org/SOC.
Building positive health behaviors and maintaining psychological well-being are foundational for achieving diabetes treatment goals and maximizing quality of life (1,2). Essential to achieving these goals are diabetes self-management education and support (DSMES), medical nutrition therapy (MNT), routine physical activity, tobacco cessation counseling when needed, health behavior counseling, and psychosocial care. Following an initial comprehensive medical evaluation (see Section 4, “Comprehensive Medical Evaluation and Assessment of Comorbidities”), people with diabetes and health care professionals are encouraged to engage in person-centered collaborative care (3–6), which is guided by shared decision-making in treatment plan selection; facilitation of obtaining medical, behavioral, psychosocial, and technology resources as needed; and shared monitoring of agreed-upon treatment plans and behavioral goals (7,8). Reevaluation during routine care should include assessment of medical, behavioral, and mental health outcomes, especially during times of change in health and well-being.
Diabetes Self-Management Education and Support
Recommendations
5.1 All people with diabetes should participate in diabetes self-management education and support to facilitate the knowledge, decision-making, and skills mastery for diabetes self-care. A
5.2 There are four critical times to evaluate the need for diabetes self-management education and support to promote skills acquisition to aid treatment plan implementation, medical nutrition therapy, and well-being: at diagnosis, annually and/or when not meeting treatment targets, when complicating factors develop (medical, physical, psychosocial), and when transitions in life and care occur. E
5.3 Clinical outcomes, health status, and well-being are key goals of diabetes self-management education and support that should be measured as part of routine care. C
5.4 Diabetes self-management education and support should be person-centered, may be offered in group or individual settings, and should be communicated with the entire diabetes care team. A
5.5 Digital coaching and digital self-management interventions can be effective methods to deliver diabetes self-management education and support. B
5.6 Reimbursement by third-party payers is recommended C because diabetes self-management education and support can improve outcomes and reduce costs. B
5.7 Identify and address barriers to diabetes self-management education and support that exist at the health system, payer, health care professional, and individual levels. E
5.8 Include social determinants of health of the target population in guiding design and delivery of diabetes self-management education and support C with the ultimate goal of health equity across all populations.
5.9 Consider addressing barriers to diabetes self-management education and support access through telehealth delivery of care B and other digital health solutions. C
The overall objectives of diabetes self-management education and support (DSMES) are to support informed decision-making, self-care behaviors, problem-solving, and active collaboration with the health care team to improve clinical outcomes, health status, and well-being in a cost-effective manner (2). DSMES services facilitate the knowledge, decision-making, and skills mastery necessary for optimal diabetes self-care and incorporate the needs, goals, and life experiences of the person with diabetes. Health care professionals are encouraged to consider the burden of treatment (9) and the person’s level of confidence and self-efficacy for management behaviors as well as the level of social and family support when providing DSMES. An individual’s engagement in self-management behaviors and the effects on clinical outcomes, health status, and quality of life, as well as the psychosocial factors impacting the person’s ability to self-manage, should be monitored as part of routine clinical care. A randomized controlled trial (RCT) testing a decision-making education and skill-building program (10) showed that addressing these targets improved health outcomes in a population in need of health care resources. Furthermore, following a DSMES curriculum improves quality of care (11).
Additionally, in response to the growing body of evidence that associates potentially judgmental words with increased feelings of shame and guilt, health care professionals are encouraged to consider the impact that language has on building therapeutic relationships and to choose positive, strength-based words and phrases that put people first (4,12). Please see Section 4, “Comprehensive Medical Evaluation and Assessment of Comorbidities,” for more on use of language.
In accordance with the national standards for DSMES (13), all people with diabetes should participate in DSMES as it helps people with diabetes to identify and implement effective self-management strategies and cope with diabetes (2). Ongoing DSMES helps people with diabetes to maintain effective self-management throughout the life course as they encounter new challenges and as advances in treatment become available (14).
There are four critical time points when the need for DSMES should be evaluated by the health care professional and/or multidisciplinary team, with referrals made as needed (2):
At diagnosis
Annually and/or when not meeting treatment targets
When complicating factors (health conditions, physical limitations, emotional factors, or basic living needs) develop that influence self-management
When transitions in life and care occur
DSMES focuses on empowering individuals with diabetes by providing people with diabetes the tools to make informed self-management decisions (15). DSMES should be person-centered. This is an approach that places the person with diabetes and their family and/or support system at the center of the care model, working in collaboration with health care professionals. Person-centered care is respectful of and responsive to individual preferences, needs, and values. It ensures that the values of the person with diabetes guide all decision-making (16).
Evidence for the Benefits
DSMES is associated with improved diabetes knowledge and self-care behaviors (17), lower A1C (17–21), lower self-reported weight (22), improved quality of life (19,23,24), reduced all-cause mortality risk (25), positive coping behaviors (5,26), and reduced health care costs (27–29). DSMES is associated with an increased use of primary care and preventive services (27,30,31) and less frequent use of acute care and inpatient hospital services (22). People with diabetes who participate in DSMES are more likely to follow best practice treatment recommendations, particularly those with Medicare, and have lower Medicare and insurance claim costs (28,31). Better outcomes were reported for DSMES interventions that were more than 10 h over the course of 6–12 months (20), included ongoing support (14,32), were culturally (33–35) and age appropriate (36,37), were tailored to individual needs and preferences, addressed psychosocial issues, and incorporated behavioral strategies (15,26,38,39). Individual and group approaches are effective (40–42), with a slight benefit realized by those who engage in both (20). Strong evidence now exists on the benefits of virtual, telehealth, or internet-based DSMES services for diabetes prevention and management in a wide variety of populations (43–54).
Technologies such as mobile apps, simulation tools, digital coaching, and digital self-management interventions can also be used to deliver DSMES (55–60). These methods provide comparable or even improved outcomes compared with traditional in-person care (61). Greater A1C reductions are demonstrated with increased patient engagement (62), although data from trials are considerably heterogeneous.
Technology-enabled diabetes self-management solutions improve A1C most effectively when there is two-way communication between the person with diabetes and the health care team, individualized feedback, use of person-generated health data, and education (46). Continuous glucose monitoring, when combined with individualized diabetes education or behavioral interventions, has demonstrated greater improvement on glycemic and psychosocial outcomes compared with continuous glucose monitoring alone (63,64). Incorporating a systematic approach for technology assessment, adoption, and integration into the care plan may help ensure equity in access and standardized application of technology-enabled solutions (8,30,65–67).
Research supports diabetes care and education specialists (DCES), including nurses, registered dietitian nutritionists (RDNs), and pharmacists as providers of DSMES who may also tailor curriculum to the person’s needs (68–70). Many other health disciplines can also become DCES. Members of the DSMES team should have specialized clinical knowledge in diabetes and behavior change principles. In addition, a DCES needs to be knowledgeable about technology-enabled services and may serve as a technology champion within their practice (65). Certification as a DCES (cbdce.org/) and/or board certification in advanced diabetes management (diabeteseducator.org/education/certification/bc_adm) demonstrates an individual’s specialized training in and understanding of diabetes management and support (43), and engagement with qualified professionals has been shown to improve disease-related outcomes. Additionally, there is growing evidence for the role of community health workers (71,72), as well as peer (71–76) and lay leaders (77), in providing ongoing support.
Given individual needs and access to resources, a variety of culturally adapted DSMES programs need to be offered in a variety of settings. The use of technology to facilitate access to DSMES services, support self-management decisions, and decrease therapeutic inertia suggests that these approaches need broader adoption (78). Additionally, it is important to include social determinants of health (SDOH) of the target population in guiding design and delivery of DSMES. The DSMES team should take into account demographic characteristics such as race, ethnic/cultural background, sex/gender, age, geographic location, technology access, education, literacy, and numeracy (43,79).
Despite the benefits of DSMES, reports indicate that only 5–7% of individuals eligible for DSMES through Medicare or a private insurance plan actually receive it (80,81). Barriers to DSMES exist at the health system, payer, health care professional, and individual levels. This low participation may be due to lack of referral or other identified barriers, such as logistical issues (accessibility, timing, costs) and the lack of a perceived benefit (81). Health system, programmatic, and payer barriers include lack of administrative leadership support, limited numbers of DSMES professionals, not having referral to DSMES services effectively embedded in the health system service structure, and limited reimbursement rates (82). Thus, in addition to educating referring health care professionals about the benefits of DSMES and the critical times to refer, efforts need to be made to identify and address all of the various potential barriers (2). Support from institutional leadership is foundational for the success of DSMES services. Expert stakeholders should also support DSMES by providing input and advocacy (43). Alternative and innovative models of DSMES delivery (56) need to be explored and evaluated, including the integration of technology-enabled diabetes and cardiometabolic health services (8,65). Barriers to equitable access to DSMES may be addressed through telehealth delivery of care and other digital health solutions (43).
Reimbursement
Medicare reimburses DSMES when that service meets the national standards (2,43) and is recognized by the American Diabetes Association (ADA) through the Education Recognition Program (professional.diabetes.org/diabetes-education) or Association of Diabetes Care & Education Specialists (diabeteseducator.org/practice/diabetes- education-accreditation-program). DSMES is also covered by most health insurance plans. Ongoing support has been shown to be instrumental for improving outcomes when it is implemented after the completion of education services. DSMES is frequently reimbursed when performed in person. However, although DSMES can also be provided via phone calls and telehealth, these remote versions may not always be reimbursed (13). Medicare reimburses remote physiologic monitoring for glucose and other cardiometabolic data if certain conditions are met (83).
Changes in reimbursement policies that increase DSMES access and utilization will result in a positive impact to beneficiaries’ clinical outcomes, quality of life, health care utilization, and costs (13,84–86). During the time of the coronavirus disease 2019 (COVID-19) pandemic, reimbursement policies were revised (professional.diabetes.org/content-page/dsmes-and-mnt-during-covid-19-national-pandemic), and these changes may provide a new reimbursement paradigm for future provision of DSMES through telehealth channels.
Medical Nutrition Therapy
Please refer to the ADA consensus report “Nutrition Therapy for Adults with Diabetes or Prediabetes: A Consensus Report” for more information on nutrition therapy (70). Despite agreement in nutrition recommendations from large scientific bodies, including the American Heart Association, American College of Lifestyle Medicine, and the U.S. Dietary Guidelines (87–93), confusion and controversy remain. For many individuals with diabetes, the most challenging part of the treatment plan is determining what to eat. There is not a “one-size-fits-all” eating pattern for individuals with diabetes, and meal planning should be individualized. Nutrition therapy plays an integral role in overall diabetes management, and each person with diabetes should be actively engaged in education, self-management, and treatment planning with the health care team, including the collaborative development of an individualized eating plan (70,94). All health care professionals should refer people with diabetes for individualized MNT provided by an RDN who is knowledgeable and skilled in providing diabetes-specific MNT (21,95,96) at diagnosis and as needed throughout the life span, similar to DSMES. MNT delivered by an RDN is associated with A1C absolute decreases of 1.0–1.9% for people with type 1 diabetes (97) and 0.3–2.0% for people with type 2 diabetes (97). See Table 5.1 for specific nutrition recommendations. Because of the progressive nature of type 2 diabetes, behavior modification alone may not be adequate to maintain euglycemia over time. However, after medication is initiated, nutrition therapy continues to be an important component, and RDNs providing MNT in diabetes care should assess and monitor medication changes in relation to the nutrition care plan (70,94).
Table 5.1.
Medical nutrition therapy recommendations
| Recommendations | |
|---|---|
| Effectiveness of nutrition therapy | 5.10 An individualized medical nutrition therapy program as needed to achieve treatment goals, provided by a registered dietitian nutritionist, preferably one who has comprehensive knowledge and experience in diabetes care, is recommended for all people with type 1 or type 2 diabetes, prediabetes, and gestational diabetes mellitus. A |
| 5.11 Because diabetes medical nutrition therapy can result in cost savings B and improved cardiometabolic outcomes A, medical nutrition therapy should be adequately reimbursed by insurance and other payers. E | |
| Energy balance | 5.12 For all people with overweight or obesity, behavioral modification to achieve and maintain a minimum weight loss of 5% is recommended. A |
| Eating patterns and macronutrient distribution | 5.13 There is no ideal macronutrient pattern for people with diabetes; meal plans should be individualized while keeping nutrient quality, total calorie, and metabolic goals in mind. E |
| 5.14 A variety of eating patterns can be considered for the management of type 2 diabetes and to prevent diabetes in individuals with prediabetes. B | |
| 5.15 Reducing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia and may be applied to a variety of eating patterns that meet individual needs and preferences. B | |
| Carbohydrates | 5.16 Carbohydrate intake should emphasize nutrient-dense carbohydrate sources that are high in fiber (at least 14 g fiber per 1,000 kcal) and minimally processed. Eating plans should emphasize nonstarchy vegetables, fruits, legumes, and whole grains, as well as dairy products, with minimal added sugars. B |
| 5.17 People with diabetes and those at risk are advised to replace sugar-sweetened beverages (including fruit juices) with water or low calorie, no calorie beverages as much as possible to manage glycemia and reduce risk for cardiometabolic disease B and minimize consumption of foods with added sugar that have the capacity to displace healthier, more nutrient-dense food choices. A | |
| 5.18 When using a flexible insulin therapy program, education on the glycemic impact of carbohydrate A, fat, and protein B should be tailored to an individual’s needs and preferences and used to optimize mealtime insulin dosing. | |
| 5.19 When using fixed insulin doses, individuals should be provided with education about consistent patterns of carbohydrate intake with respect to time and amount while considering the insulin action time, as it can result in improved glycemia and reduce the risk for hypoglycemia. B | |
| Protein | 5.20 In individuals with type 2 diabetes, ingested protein appears to increase insulin response without increasing plasma glucose concentrations. Therefore, carbohydrate sources high in protein should be avoided when trying to treat or prevent hypoglycemia. B |
| Dietary fat | 5.21 An eating plan emphasizing elements of a Mediterranean eating pattern rich in monounsaturated and polyunsaturated fats may be considered to improve glucose metabolism and lower cardiovascular disease risk. B |
| 5.22 Eating foods rich in long-chain n-3 fatty acids, such as fatty fish (EPA and DHA) and nuts and seeds (ALA), is recommended to prevent or treat cardiovascular disease. B | |
| Micronutrients and herbal supplements | 5.23 There is no clear evidence that dietary supplementation with vitamins, minerals (such as chromium and vitamin D), herbs, or spices (such as cinnamon or aloe vera) can improve outcomes in people with diabetes who do not have underlying deficiencies, and they are not generally recommended for glycemic control. C There may be evidence of harm for certain individuals with β carotene supplementation. B |
| Alcohol | 5.24 Adults with diabetes who drink alcohol should do so in moderation (no more than one drink per day for adult women and no more than two drinks per day for adult men). C |
| 5.25 Educating people with diabetes about the signs, symptoms, and self-management of delayed hypoglycemia after drinking alcohol, especially when using insulin or insulin secretagogues, is recommended. The importance of glucose monitoring after drinking alcoholic beverages to reduce hypoglycemia risk should be emphasized. B | |
| Sodium | 5.26 Sodium consumption should be limited to <2,300 mg/day. B |
| Nonnutritive sweeteners | 5.27 The use of nonnutritive sweeteners as a replacement for sugar-sweetened products may reduce overall calorie and carbohydrate intake as long as there is not a compensatory increase in energy intake from other sources. There is evidence that low- and no-calorie sweetened beverages are a viable alternative to water. B |
Goals of Nutrition Therapy for Adults with Diabetes
- To promote and support healthful eating patterns, emphasizing a variety of nutrient-dense foods in appropriate portion sizes, to improve overall health and:
- achieve and maintain body weight goals
- attain individualized glycemic, blood pressure, and lipid goals
- delay or prevent the complications of diabetes
To address individual nutrition needs based on personal and cultural preferences, health literacy and numeracy, access to healthful foods, willingness and ability to make behavioral changes, and existing barriers to change
To maintain the pleasure of eating by providing nonjudgmental messages about food choices while limiting food choices only when indicated by scientific evidence
To provide an individual with diabetes the practical tools for developing healthy eating patterns rather than focusing on individual macronutrients, micronutrients, or single foods
Weight Management
Management and reduction of weight is important for people with type 1 diabetes, type 2 diabetes, or prediabetes with overweight or obesity. To support weight loss and improve A1C, cardiovascular disease (CVD) risk factors, and well-being in adults with overweight/obesity and prediabetes or diabetes, MNT and DSMES services should include an individualized eating plan in a format that results in an energy deficit in combination with enhanced physical activity (70). Lifestyle intervention programs should be intensive and have frequent follow-up to achieve significant reductions in excess body weight and improve clinical indicators. There is strong and consistent evidence that modest, sustained weight loss can delay the progression from prediabetes to type 2 diabetes (97–99) (see Section 3, “Prevention or Delay of Type 2 Diabetes and Associated Comorbidities”) and is beneficial for the management of type 2 diabetes (see Section 8, “Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes”).
In prediabetes, the weight loss goal is 7–10% for preventing progression to type 2 diabetes (100). In conjunction with support for healthy lifestyle behaviors, medication-assisted weight loss can be considered for people at risk for type 2 diabetes when needed to achieve and sustain 7–10% weight loss (101,102) (see Section 8, “Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes”). People with prediabetes at a healthy weight should also be considered for behavioral interventions to help establish routine aerobic and resistance exercise (100,103,104) as well as to establish healthy eating patterns. Services delivered by practitioners familiar with diabetes and its management, such as an RDN, have been found to be effective (95).
For many individuals with overweight and obesity with type 2 diabetes, 5% weight loss is needed to achieve beneficial outcomes in glycemic control, lipids, and blood pressure (105). It should be noted, however, that the clinical benefits of weight loss are progressive, and more intensive weight loss goals (i.e., 15%) may be appropriate to maximize benefit depending on need, feasibility, and safety (106,107). Long-term durability of weight loss remains a challenge; however, newer medications (beyond metabolic surgery) may have potential for sustainability, impact on cardiovascular outcomes, and weight reduction beyond 10–15% (108–111).
In select individuals with type 2 diabetes, an overall healthy eating plan that results in energy deficit in conjunction with weight loss medications and/or metabolic surgery should be considered to help achieve weight loss and maintenance goals, lower A1C, and reduce CVD risk (101,112,113). Overweight and obesity are also increasingly prevalent in people with type 1 diabetes and present clinical challenges regarding diabetes treatment and CVD risk factors (114,115). Sustaining weight loss can be challenging (105,116) but has long-term benefits; maintaining weight loss for 5 years is associated with sustained improvements in A1C and lipid levels (117). MNT guidance from an RDN with expertise in diabetes and weight management throughout the course of a structured weight loss plan is strongly recommended.
Along with routine medical management visits, people with diabetes and prediabetes should be screened during DSMES and MNT encounters for a history of dieting and past or current disordered eating behaviors. Nutrition therapy should be individualized to help address maladaptive eating behavior (e.g., purging) or compensatory changes in medical treatment plan (e.g., overtreatment of hypoglycemic episodes, reduction in medication dosing to reduce hunger) (70) (see disordered eating behavior, below). Disordered eating, eating disorders, and/or disrupted eating can increase challenges for weight and diabetes management. For example, caloric restriction may be essential for glycemic management and weight maintenance, but rigid meal plans may be contraindicated for individuals who are at increased risk of clinically significant maladaptive eating behaviors (118). If eating disorders are identified during screening with diabetes-specific questionnaires, individuals should be referred to a qualified mental health professional (1).
Studies have demonstrated that a variety of eating plans, varying in macronutrient composition, can be used effectively and safely in the short term (1–2 years) to achieve weight loss in people with diabetes. These plans include structured low-calorie meal plans with meal replacements (106,117,119), a Mediterranean eating pattern (120), and low-carbohydrate meal plans with additional support (121,122). However, no single approach has been proven to be consistently superior (70,123–125), and more data are needed to identify and validate those meal plans that are optimal with respect to long-term outcomes and acceptability. The importance of providing guidance on an individualized meal plan containing nutrient-dense foods, such as vegetables, fruits, legumes, dairy, lean sources of protein (including plant-based sources as well as lean meats, fish, and poultry), nuts, seeds, and whole grains, cannot be overemphasized (124), as well as guidance on achieving the desired energy deficit (126–129). Any approach to meal planning should be individualized, considering the health status, personal preferences, and ability of the person with diabetes to sustain the recommendations in the plan.
Eating Patterns and Meal Planning
Evidence suggests that there is not an ideal percentage of calories from carbohydrate, protein, and fat for people with diabetes. Therefore, macronutrient distribution should be based on an individualized assessment of current eating patterns, preferences, and metabolic goals. Dietary guidance should emphasize the importance of a healthy dietary pattern as a whole rather than focusing on individual nutrients, foods, or food groups, given that individuals rarely eat foods in isolation. Personal preferences (e.g., tradition, culture, religion, health beliefs and goals, economics), as well as metabolic goals, need to be considered when working with individuals to determine the best eating pattern (70,97,130). Members of the health care team should complement MNT by providing evidence-based guidance that helps people with diabetes make healthy food choices that meet their individualized needs and improve overall health. A variety of eating patterns are acceptable for the management of diabetes (70,97,131,132). Health care professionals should focus on the core dimensions common among the patterns: 1) emphasize nonstarchy vegetables, 2) minimize added sugars and refined grains, and 3) choose whole foods over highly processed foods to the extent possible (70). An individualized eating pattern also considers the individual’s health status, food and numeracy skills, resources, food preferences, health goals, and food access. Any member of the health care team can screen for food insecurity using The Hunger Vital Sign. Households are considered at risk if they answer either or both of the following statements as “often true” or “sometimes true” (compared with “never true”) (133):
“Within the past 12 months, we worried whether our food would run out before we got money to buy more.”
“Within the past 12 months, the food we bought just didn’t last, and we didn’t have money to get more.”
Referral to an RDN is essential to assess the overall nutrition status of, and to work collaboratively with, the person with diabetes to create a personalized meal plan that coordinates and aligns with the overall treatment plan, including physical activity and medication use. The Mediterranean (130,134–136), low-carbohydrate (137–139), and vegetarian or plant-based (135,136,140,141) eating patterns are all examples of healthful eating patterns that have shown positive results in research for individuals with type 2 diabetes, but individualized meal planning should focus on personal preferences, needs, and goals. There is currently inadequate research in type 1 diabetes to support one eating pattern over another. Moreover, there is a paucity of evidence and agreement as it relates to nutrition management among children and adolescents with type 1 diabetes. There remains a significant gap in the literature as it relates to the efficacy and long-term management implications of nutrition interventions for young children with type 1 diabetes (142).
For individuals with type 2 diabetes not meeting glycemic targets or for whom reducing glucose-lowering drugs is a priority, reducing overall carbohydrate intake with a low- or very-low-carbohydrate eating pattern is a viable option (137–139). As research studies on low-carbohydrate eating plans generally indicate challenges with long-term sustainability (143), it is important to reassess and individualize meal plan guidance regularly for those interested in this approach. In response to questions regarding implementation of low-carbohydrate and very-low-carbohydrate eating patterns, the ADA has developed a guide for health care professionals that may assist in the practical implementation of these eating patterns (144). Most individuals with diabetes report a moderate intake of carbohydrates (44–46% of total calories) (97,144). Efforts to modify habitual eating patterns are often unsuccessful in the long term; people generally go back to their usual macronutrient distribution (97). Thus, the recommended approach is to individualize meal plans with a macronutrient distribution that is more consistent with personal preference and usual intake to increase the likelihood for long-term maintenance.
An RCT found that two meal-planning approaches (diabetes plate method and carbohydrate counting) were effective in helping achieve improved A1C (145). The diabetes plate method is a commonly used visual approach for providing basic meal planning guidance. This simple graphic (featuring a 9-inch plate) shows how to portion foods (1/2 of the plate for nonstarchy vegetables, 1/4 of the plate for protein, and 1/4 of the plate for carbohydrates). Carbohydrate counting is a more advanced skill that helps plan for and track how much carbohydrate is consumed at meals and snacks. Meal planning approaches should be customized to the individual, including their numeracy (145) and food literacy level. Food literacy generally describes proficiency in food-related knowledge and skills that ultimately impact health, although specific definitions vary across initiatives (146,147).
There has been an increased interest in time-restricted eating and intermittent fasting as strategies for weight management. Intermittent fasting is an umbrella term which includes three main forms of restricted eating: alternate-day fasting (energy restriction of 500–600 calories on alternate days), the 5:2 diet (energy restriction of 500–600 calories on consecutive or nonconsecutive days) with usual intake the other five, and time-restricted eating (daily calorie restriction based on window of time of 8–15 h). Each produces mild to moderate weight loss (3–8% loss from baseline) over short durations (8–12 weeks) with no significant differences in weight loss when compared with continuous calorie restriction (148–151). A few studies have extended up to 52 weeks and show similar findings (152–155). Time-restricted eating (shortening the eating window) is generally easier to follow compared with alternative-day fasting or the 5:2 plan, largely due to ease, no need to count calories, sustainability, and feasibility. This may have implications as people with diabetes are looking for practical eating management tools.
Carbohydrates
Studies examining the ideal amount of carbohydrate intake for people with diabetes are inconclusive, although monitoring carbohydrate intake and considering the blood glucose response to dietary carbohydrate are key for improving postprandial glucose management (156,157). The literature concerning glycemic index and glycemic load in individuals with diabetes is complex, often with varying definitions of low- and high-glycemic-index foods (158,159). The glycemic index ranks carbohydrate foods on their postprandial glycemic response, and glycemic load takes into account both the glycemic index of foods and the amount of carbohydrate eaten. Studies have found mixed results regarding the effect of glycemic index and glycemic load on fasting glucose levels and A1C, with one systematic review finding no significant impact on A1C (160) while others demonstrated A1C reductions of 0.15% (158) to 0.5% (161,162).
Reducing overall carbohydrate intake for individuals with diabetes has demonstrated evidence for improving glycemia and may be applied in a variety of eating patterns that meet individual needs and preferences (70). For people with type 2 diabetes, low-carbohydrate and very-low-carbohydrate eating patterns in particular have been found to reduce A1C and the need for antihyperglycemic medications (70,130,143,163–165). Systematic reviews and meta-analyses of RCTs found carbohydrate-restricted eating patterns, particularly those considered low carbohydrate (<26% total energy), were effective in reducing A1C in the short term (<6 months), with less difference in eating patterns beyond 1 year (125,126,137,138,164). Questions still remain about the optimal degree of carbohydrate restriction and the long-term effects of those meal patterns on cardiovascular disease. A systematic review and meta-analysis of RCTs investigating the dose-dependent effect of carbohydrate restriction on metabolic control found each 10% decrease in carbohydrate intake had reductions in levels of A1C, fasting plasma glucose, body weight, lipids, and systolic blood pressure at 6 months, but favorable effects diminished and were not maintained at follow-up or at greater than 12 months. This systematic review highlights the metabolic complexity of response to dietary intervention in type 2 diabetes as well as the need to better understand longer-term sustainability and results (166). Part of the challenge in interpreting low-carbohydrate research has been due to the wide range of definitions for a low-carbohydrate eating plan (139,161). Weight reduction was also a goal in many low-carbohydrate studies, which further complicates evaluating the distinct contribution of the eating pattern (47,121,125,167).
The quality of carbohydrate and/or what is absent from the diet may contribute to confounding results. However, when core dimensions of the comparative diets are similar, there is little difference in outcome measures. When Gardner et al. (168) tested a low-carbohydrate ketogenic diet and a low-carbohydrate Mediterranean diet, in a randomized crossover design, metabolic improvements were seen in both diets without significant differences between them. Each of the interventions avoided added sugars and refined grains and included nonstarchy vegetables. Legumes, fruits, and whole intact grains were included in the Mediterranean but not in the ketogenic diet. The improvements (fasting glucose, insulin, HDL cholesterol, and A1C) were likely due to the nutritional quality of both interventions. However, the ketogenic plan led to a greater decrease in triglycerides (168) but also a greater increase in LDL cholesterol.
As studies on low-carbohydrate eating plans generally indicate challenges with long-term sustainability (143), it is important to reassess and individualize meal plan guidance regularly for those interested in this approach. Health care professionals should maintain consistent medical oversight and recognize that insulin and other diabetes medications may need to be adjusted to prevent hypoglycemia, and blood pressure will need to be monitored. In addition, very-low-carbohydrate eating plans are not currently recommended for individuals who are pregnant or lactating, children, people who have renal disease, or people with or at risk for disordered eating, and these plans should be used with caution in those taking sodium–glucose cotransporter 2 inhibitors because of the potential risk of ketoacidosis (169,170).
Regardless of amount of carbohydrate in the meal plan, focus should be placed on high-quality, nutrient-dense carbohydrate sources that are high in fiber and minimally processed. The addition of dietary fiber modulates composition of gut microbiota and increases gut microbial diversity. Although there is still much to be elucidated with the gut microbiome and chronic disease, higher-fiber diets are advantageous (171). Both children and adults with diabetes are encouraged to minimize intake of refined carbohydrates with added sugars, fat, and sodium and instead focus on carbohydrates from vegetables, legumes, fruits, dairy (milk and yogurt), and whole grains. People with diabetes and those at risk for diabetes are encouraged to consume a minimum of 14 g of fiber/1,000 kcal, with at least half of grain consumption being whole, intact grains, according to the Dietary Guidelines for Americans (172). Regular intake of sufficient dietary fiber is associated with lower all-cause mortality in people with diabetes (173,174), and prospective cohort studies have found dietary fiber intake is inversely associated with risk of type 2 diabetes (175–177). The consumption of sugar-sweetened beverages and processed food products with large amounts of refined grains and added sugars is strongly discouraged (172,178,179), as these have the capacity to displace healthier, more nutrient-dense food choices.
Individuals with type 1 or type 2 diabetes taking insulin at mealtime should be offered intensive and ongoing education on the need to couple insulin administration with carbohydrate intake. For people whose meal schedule or carbohydrate consumption is variable, regular education to increase understanding of the relationship between carbohydrate intake and insulin needs is important. In addition, education on using insulin-to-carbohydrate ratios for meal planning can assist individuals with effectively modifying insulin dosing from meal to meal to improve glycemic management (97,156,180–183). Studies have shown that dietary fat and protein can impact early and delayed postprandial glycemia (184–187), and it appears to have a dose-dependent response (188–191). Results from high-fat, high-protein meal studies highlight the need for additional insulin to cover these meals; however, more studies are needed to determine the optimal insulin dose and delivery strategy. The results from these studies also point to individual differences in postprandial glycemic response; therefore, a cautious approach to increasing insulin doses for high-fat and/or high-protein mixed meals is recommended to address delayed hyperglycemia that may occur 3 h or more after eating (70). If using an insulin pump, a split bolus feature (part of the bolus delivered immediately, the remainder over a programmed duration of time) may provide better insulin coverage for high-fat and/or high-protein mixed meals (185,192).
The effectiveness of insulin dosing decisions should be confirmed with a structured approach to blood glucose monitoring or continuous glucose monitoring to evaluate individual responses and guide insulin dose adjustments. Checking glucose 3 h after eating may help to determine if additional insulin adjustments are required (i.e., increasing or stopping bolus) (185,192,193). Refining insulin doses to account for high-fat and/or -protein meals requires determination of anticipated nutrient intake to calculate the mealtime dose. Food literacy, numeracy, interest, and capability should be evaluated (70). For individuals on a fixed daily insulin schedule, meal planning should emphasize a relatively fixed carbohydrate consumption pattern with respect to both time and amount while considering insulin action. Attention to resultant hunger and satiety cues will also help with nutrient modifications throughout the day (70,194).
Protein
There is no evidence that adjusting the daily level of protein intake (typically 1–1.5 g/kg body wt/day or 15–20% total calories) will improve health, and research is inconclusive regarding the ideal amount of dietary protein to optimize either glycemic management or CVD risk (159,195). Therefore, protein intake goals should be individualized based on current eating patterns. Some research has found successful management of type 2 diabetes with meal plans including slightly higher levels of protein (20–30%), which may contribute to increased satiety (196).
Historically, low-protein eating plans were advised for individuals with diabetic kidney disease (DKD) (with albuminuria and/or reduced estimated glomerular filtration rate); however, current evidence does not suggest that people with DKD need to restrict protein to less than the generally recommended protein intake (70). Reducing the amount of dietary protein below the recommended daily allowance of 0.8 g/kg is not recommended because it does not alter glycemic measures, cardiovascular risk measures, or the rate at which glomerular filtration rate declines and may increase risk for malnutrition (197,198).
In individuals with type 2 diabetes, protein intake may enhance or increase the insulin response to dietary carbohydrates (199). Therefore, use of carbohydrate sources high in protein (e.g., nuts) to treat or prevent hypoglycemia should be avoided due to the potential concurrent rise in endogenous insulin. Health care professionals should counsel patients to treat hypoglycemia with pure glucose (i.e., glucose tablets) or carbohydrate-containing foods at the hypoglycemia alert value of <70 mg/dL. See Section 6, “Glycemic Targets,” for more information.
Fats
Evidence suggests that there is not an ideal percentage of calories from fat for people with or at risk for diabetes and that macronutrient distribution should be individualized according to the patient’s eating patterns, preferences, and metabolic goals (70). The type of fats consumed is more important than total amount of fat when looking at metabolic goals and CVD risk, and it is recommended that the percentage of total calories from saturated fats should be limited (120,172,200–202). Multiple RCTs including people with type 2 diabetes have reported that a Mediterranean eating pattern (120,203–208) can improve both glycemic management and blood lipids. The Mediterranean eating pattern is based on the traditional eating habits in the countries bordering the Mediterranean Sea. Although eating styles vary, they share a number of common features, including consumption of fresh fruits and vegetables, whole grains, beans, and nuts/seeds; olive oil as the primary fat source; low to moderate amounts of fish, eggs, and poultry; and limited added sugars, sugary beverages, sodium, highly processed foods, refined carbohydrates, saturated fats, and fatty or processed meats.
Evidence does not conclusively support recommending n-3 (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]) supplements for all people with diabetes for the prevention or treatment of cardiovascular events (70,209,210). In individuals with type 2 diabetes, two systematic reviews with n-3 and n-6 fatty acids concluded that the dietary supplements did not improve glycemic management (159,211). In the ASCEND trial (A Study of Cardiovascular Events iN Diabetes), when compared with placebo, supplementation with n-3 fatty acids at the dose of 1 g/day did not lead to cardiovascular benefit in people with diabetes without evidence of CVD (212). However, results from the Reduction of Cardiovascular Events With Icosapent Ethyl–Intervention Trial (REDUCE-IT) found that supplementation with 4 g/day of pure EPA significantly lowered the risk of adverse cardiovascular events. This trial of 8,179 participants, in which over 50% had diabetes, found a 5% absolute reduction in cardiovascular events for individuals with established atherosclerotic CVD taking a preexisting statin with residual hypertriglyceridemia (135–499 mg/dL) (213). See Section 10, “Cardiovascular Disease and Risk Management,” for more information. People with diabetes should be advised to follow the guidelines for the general population for the recommended intakes of saturated fat, dietary cholesterol, and trans fat (172). Trans fats should be avoided. In addition, as saturated fats are progressively decreased in the diet, they should be replaced with unsaturated fats and not with refined carbohydrates (207).
Sodium
As for the general population, people with diabetes are advised to limit their sodium consumption to <2,300 mg/day (70). Restriction to <1,500 mg, even for those with hypertension, is generally not recommended (214–216). Sodium recommendations should take into account palatability, availability, affordability, and the difficulty of achieving low-sodium recommendations in a nutritionally adequate diet (217).
Micronutrients and Supplements
There continues to be no clear evidence of benefit from herbal or nonherbal (i.e., vitamin or mineral) supplementation for people with diabetes without underlying deficiencies (70). Metformin is associated with vitamin B12 deficiency per a report from the Diabetes Prevention Program Outcomes Study (DPPOS), suggesting that periodic testing of vitamin B12 levels should be considered in people taking metformin, particularly in those with anemia or peripheral neuropathy (218). Routine supplementation with antioxidants, such as vitamins E and C, is not advised due to lack of evidence of efficacy and concern related to long-term safety. Based on the recent U.S. Preventative Services Task Force statement, the harms of β-carotene outweigh the benefits for the prevention of CVD or cancer. β-Carotene was significantly associated with increased lung cancer and cardiovascular mortality risk (219).
In addition, there is insufficient evidence to support the routine use of herbal supplements and micronutrients, such as cinnamon (220), curcumin, vitamin D (221), aloe vera, or chromium, to improve glycemia in people with diabetes (70,222).
Although the Vitamin D and Type 2 Diabetes Study (D2d) prospective RCT showed no significant benefit of vitamin D versus placebo on the progression to type 2 diabetes in individuals at high risk (223), post hoc analyses and meta-analyses suggest a potential benefit in specific populations (223–226). Further research is needed to define individual characteristics and clinical indicators where vitamin D supplementation may be of benefit.
For special populations, including pregnant or lactating individuals, older adults, vegetarians, and people following very-low-calorie or low-carbohydrate diets, a multivitamin may be necessary.
Alcohol
Moderate alcohol intake does not have major detrimental effects on long-term blood glucose management in people with diabetes. Risks associated with alcohol consumption include hypoglycemia and/or delayed hypoglycemia (particularly for those using insulin or insulin secretagogue therapies), weight gain, and hyperglycemia (for those consuming excessive amounts) (70,222). People with diabetes should be educated about these risks and encouraged to monitor glucose frequently after drinking alcohol to minimize such risks. People with diabetes can follow the same guidelines as those without diabetes. For women, no more than one drink per day, and for men, no more than two drinks per day is recommended (one drink is equal to a 12-oz beer, a 5-oz glass of wine, or 1.5 oz of distilled spirits).
Nonnutritive Sweeteners
The U.S. Food and Drug Administration has approved many nonnutritive sweeteners for consumption by the general public, including people with diabetes (70,227). For some people with diabetes who are accustomed to regularly consuming sugar-sweetened products, nonnutritive sweeteners (containing few or no calories) may be an acceptable substitute for nutritive sweeteners (those containing calories, such as sugar, honey, and agave syrup) when consumed in moderation (228,229). Nonnutritive sweeteners do not appear to have a significant effect on glycemic management (97,230,231), and they can reduce overall calorie and carbohydrate intake (97,228) as long as individuals are not compensating with additional calories from other food sources (70,232). There is mixed evidence from systematic reviews and meta-analyses for nonnutritive sweetener use with regard to weight management, with some finding benefit in weight loss (233–235) while other research suggests an association with weight gain (236,237). This may be explained by reverse causality and residual confounding variables (237). The addition of nonnutritive sweeteners to diets poses no benefit for weight loss or reduced weight gain without energy restriction (238). In a recent systematic review and meta-analysis using low-calorie and no-calorie sweetened beverages as an intended substitute for sugar-sweetened beverages, a small improvement in body weight and cardiometabolic risk factors was seen without evidence of harm and had a direction of benefit similar to that seen with water. Health care professionals should continue to recommend water, but people with overweight or obesity and diabetes may also have a variety of no-calorie or low-calorie sweetened products so that they do not feel deprived (239).
Physical Activity
Recommendations
5.28 Children and adolescents with type 1 diabetes C or type 2 diabetes or prediabetes B should engage in 60 min/day or more of moderate- or vigorous-intensity aerobic activity, with vigorous muscle-strengthening and bone-strengthening activities at least 3 days/week.
5.29 Most adults with type 1 diabetes C and type 2 diabetes B should engage in 150 min or more of moderate- to vigorous-intensity aerobic activity per week, spread over at least 3 days/week, with no more than 2 consecutive days without activity. Shorter durations (minimum 75 min/week) of vigorous-intensity or interval training may be sufficient for younger and more physically fit individuals.
5.30 Adults with type 1 diabetes C and type 2 diabetes B should engage in 2–3 sessions/week of resistance exercise on nonconsecutive days.
5.31 All adults, and particularly those with type 2 diabetes, should decrease the amount of time spent in daily sedentary behavior. B Prolonged sitting should be interrupted every 30 min for blood glucose benefits. C
5.32 Flexibility training and balance training are recommended 2–3 times/week for older adults with diabetes. Yoga and tai chi may be included based on individual preferences to increase flexibility, muscular strength, and balance. C
5.33 Evaluate baseline physical activity and sedentary time. Promote increase in nonsedentary activities above baseline for sedentary individuals with type 1 diabetes E and type 2 diabetes. B Examples include walking, yoga, housework, gardening, swimming, and dancing.
Physical activity is a general term that includes all movement that increases energy use and is an important part of the diabetes management plan. Exercise is a more specific form of physical activity that is structured and designed to improve physical fitness. Both physical activity and exercise are important. Exercise has been shown to improve blood glucose levels, reduce cardiovascular risk factors, contribute to weight loss, and improve well-being (240). Physical activity is as important for those with type 1 diabetes as it is for the general population, but its specific role in the prevention of diabetes complications and the management of blood glucose is not as clear as it is for those with type 2 diabetes. Many individuals with type 2 diabetes do not meet the recommended exercise level per week (150 min). Objective measurement by accelerometer in 871 individuals with type 2 diabetes showed that 44.2%, 42.6%, and 65.1% of White, African American, and Hispanic individuals, respectively, met the recommended threshold of exercise (241). An RCT in 1,366 individuals with prediabetes combined a physical activity intervention with text messaging and telephone support, which showed improvement in daily step count at 12 months compared with the control group. Unfortunately, this was not sustained at 48 months (242). Another RCT, including 324 individuals with prediabetes, showed increased physical activity at 8 weeks with supportive text messages, but by 12 weeks there was no difference between groups (243). It is important for diabetes care management teams to understand the difficulty that many people have reaching recommended treatment targets and to identify individualized approaches to improve goal achievement, which may need to change over time.
Moderate to high volumes of aerobic activity are associated with substantially lower cardiovascular and overall mortality risks in both type 1 and type 2 diabetes (244). A prospective observational study of adults with type 1 diabetes suggested that higher amounts of physical activity led to reduced cardiovascular mortality after a mean follow-up time of 11.4 years for people with and without chronic kidney disease (245). Additionally, structured exercise interventions of at least 8 weeks’ duration have been shown to lower A1C by an average of 0.66% in people with type 2 diabetes, even without a significant change in BMI (246). There are also considerable data for the health benefits (e.g., increased cardiovascular fitness, greater muscle strength, improved insulin sensitivity) of regular exercise for those with type 1 diabetes (247). Exercise training in type 1 diabetes may also improve several important markers such as triglyceride level, LDL cholesterol, waist circumference, and body mass (248). In adults with type 2 diabetes, higher levels of exercise intensity are associated with greater improvements in A1C and in cardiorespiratory fitness (249); sustained improvements in cardiorespiratory fitness and weight loss have also been associated with a lower risk of heart failure (250). Other benefits include slowing the decline in mobility among overweight people with diabetes (251). The ADA position statement “Physical Activity/Exercise and Diabetes” reviews the evidence for the benefits of exercise in people with type 1 and type 2 diabetes and offers specific recommendations (252). Increased physical activity (soccer training) has also been shown to be beneficial for improving overall fitness in Latino men with obesity, demonstrating feasible methods to increase physical activity in an often hard-to-engage population (253). Physical activity and exercise should be recommended and prescribed to all individuals who are at risk for or with diabetes as part of management of glycemia and overall health. Specific recommendations and precautions will vary by the type of diabetes, age, activity, and presence of diabetes-related health complications. Recommendations should be tailored to meet the specific needs of each individual (252).
Exercise and Children
All children, including children with diabetes or prediabetes, should be encouraged to engage in regular physical activity. Children should engage in at least 60 min of moderate to vigorous aerobic activity every day, with muscle- and bone-strengthening activities at least 3 days per week (254). In general, youth with type 1 diabetes benefit from being physically active, and an active lifestyle should be recommended to all (255). Youth with type 1 diabetes who engage in more physical activity may have better health outcomes and health-related quality of life (256,257). See Section 14, “Children and Adolescents,” for details.
Frequency and Type of Physical Activity
People with diabetes should perform aerobic and resistance exercise regularly (209). Aerobic activity bouts should ideally last at least 10 min, with the goal of ∼30 min/day or more most days of the week for adults with type 2 diabetes. Daily exercise, or at least not allowing more than 2 days to elapse between exercise sessions, is recommended to decrease insulin resistance, regardless of diabetes type (258,259). A study in adults with type 1 diabetes found a dose-response inverse relationship between self-reported bouts of physical activity per week and A1C, BMI, hypertension, dyslipidemia, and diabetes-related complications such as hypoglycemia, diabetic ketoacidosis, retinopathy, and microalbuminuria (260). Over time, activities should progress in intensity, frequency, and/or duration to at least 150 min/week of moderate-intensity exercise. Adults able to run at 6 miles/h (9.7 km/h) for at least 25 min can benefit sufficiently from shorter-intensity activity (75 min/week) (252). Many adults, including most with type 2 diabetes, may be unable or unwilling to participate in such intense exercise and should engage in moderate exercise for the recommended duration. Adults with diabetes should engage in 2–3 sessions/week of resistance exercise on nonconsecutive days (261). Although heavier resistance training with free weights and weight machines may improve glycemic control and strength (262), resistance training of any intensity is recommended to improve strength, balance, and the ability to engage in activities of daily living throughout the life span. Health care professionals should help people with diabetes set stepwise goals toward meeting the recommended exercise targets. As individuals intensify their exercise program, medical monitoring may be indicated to ensure safety and evaluate the effects on glucose management. (See physical activity and glycemic control, below.)
Evidence supports that all individuals, including those with diabetes, should be encouraged to reduce the amount of time spent being sedentary—waking behaviors with low energy expenditure (e.g., working at a computer, watching television)—by breaking up bouts of sedentary activity (>30 min) by briefly standing, walking, or performing other light physical activities (263,264). Participating in leisure-time activity and avoiding extended sedentary periods may help prevent type 2 diabetes for those at risk (265,266) and may also aid in glycemic management for those with diabetes.
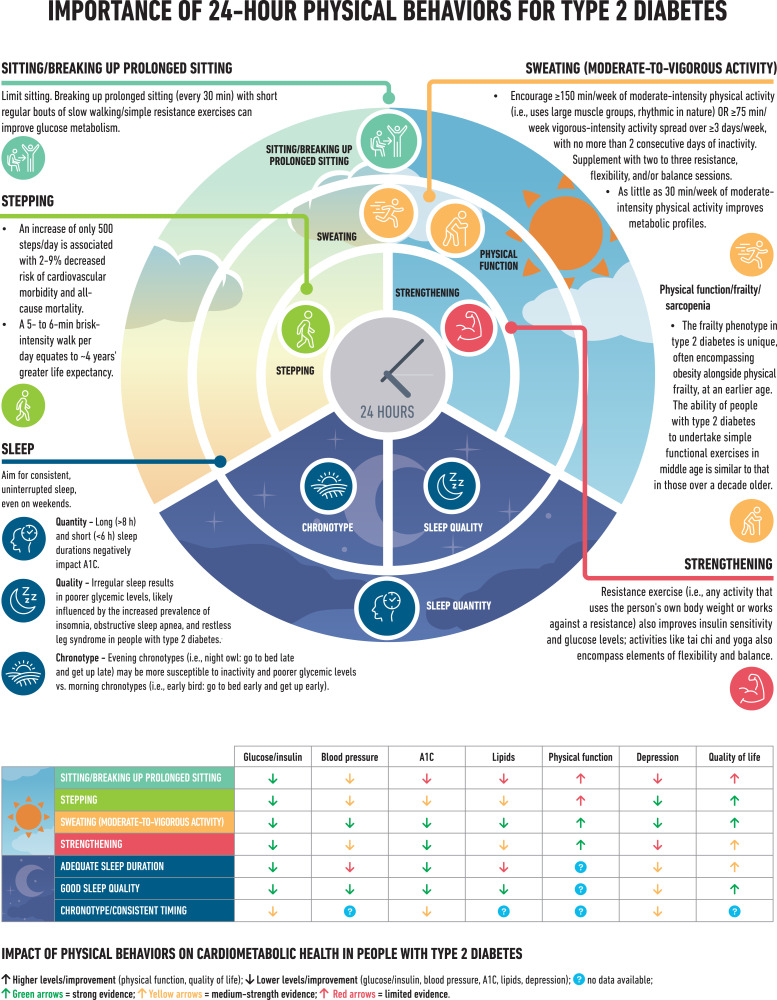
A systematic review and meta-analysis found higher frequency of regular leisure-time physical activity was more effective in reducing A1C levels (267). A wide range of activities, including yoga, tai chi, and other types, can have significant impacts on A1C, flexibility, muscle strength, and balance (240,268–270). Flexibility and balance exercises may be particularly important in older adults with diabetes to maintain range of motion, strength, and balance (252) (Fig. 5.1).
Figure 5.1.
Importance of 24-h physical behaviors for type 2 diabetes. Reprinted from Davies et al. (88).
Physical Activity and Glycemic Management
Clinical trials have provided strong evidence for the A1C-lowering value of resistance training in older adults with type 2 diabetes (252) and for an additive benefit of combined aerobic and resistance exercise in adults with type 2 diabetes (271). If not contraindicated, people with type 2 diabetes should be encouraged to do at least two weekly sessions of resistance exercise (exercise with free weights or weight machines), with each session consisting of at least one set (group of consecutive repetitive exercise motions) of five or more different resistance exercises involving the large muscle groups (272).
For people with type 1 diabetes, although exercise, in general, is associated with improvement in disease status, care needs to be taken in titrating exercise with respect to glycemic management. Each individual with type 1 diabetes has a variable glycemic response to exercise. This variability should be taken into consideration when recommending the type and duration of exercise for a given individual (247).
Individuals of childbearing potential with preexisting diabetes, particularly type 2 diabetes, and those at risk for or presenting with gestational diabetes mellitus should be advised to engage in regular moderate physical activity prior to and during their pregnancies as tolerated (252).
Pre-exercise Evaluation
As discussed more fully in Section 10, “Cardiovascular Disease and Risk Management,” the best protocol for assessing asymptomatic people with diabetes for coronary artery disease remains unclear. The ADA consensus report “Screening for Coronary Artery Disease in Patients With Diabetes” (273) concluded that routine testing is not recommended. However, health care professionals should perform a careful history, assess cardiovascular risk factors, and be aware of the atypical presentation of coronary artery disease, such as recent reported or tested decrease in exercise tolerance in people with diabetes. Certainly, those with high risk should be encouraged to start with short periods of low-intensity exercise and slowly increase the intensity and duration as tolerated. Health care professionals should assess for conditions that might contraindicate certain types of exercise or predispose to injury, such as uncontrolled hypertension, untreated proliferative retinopathy, autonomic neuropathy, peripheral neuropathy, and a history of foot ulcers or Charcot foot. Age and previous physical activity level should be considered when customizing the exercise plan to the individual’s needs. Those with complications may need a more thorough evaluation prior to starting an exercise program (247).
Hypoglycemia
In individuals taking insulin and/or insulin secretagogues, physical activity may cause hypoglycemia if the medication dose or carbohydrate consumption is not adjusted for the exercise bout and postbout impact on glucose. Individuals on these therapies may need to ingest some added carbohydrate if pre-exercise glucose levels are <90 mg/dL (5.0 mmol/L), depending on whether they are able to lower insulin doses during the workout (such as with an insulin pump or reduced pre-exercise insulin dosage), the time of day exercise is done, and the intensity and duration of the activity (247). In some people with diabetes, hypoglycemia after exercise may occur and last for several hours due to increased insulin sensitivity. Hypoglycemia is less common in those who are not treated with insulin or insulin secretagogues, and no routine preventive measures for hypoglycemia are usually advised in these cases. Intense activities may actually raise blood glucose levels instead of lowering them, especially if pre-exercise glucose levels are elevated (247). Because of the variation in glycemic response to exercise bouts, people with diabetes need to be educated to check blood glucose levels before and after periods of exercise and about the potential prolonged effects (depending on intensity and duration).
Exercise in the Presence of Microvascular Complications
See Section 11, “Chronic Kidney Disease and Risk Management,” and Section 12, “Retinopathy, Neuropathy, and Foot Care,” for more information on these long-term complications.
Retinopathy
If proliferative diabetic retinopathy or severe nonproliferative diabetic retinopathy is present, then vigorous-intensity aerobic or resistance exercise may be contraindicated because of the risk of triggering vitreous hemorrhage or retinal detachment (274). Consultation with an ophthalmologist prior to engaging in an intense exercise plan may be appropriate.
Peripheral Neuropathy
Decreased pain sensation and a higher pain threshold in the extremities can result in an increased risk of skin breakdown, infection, and Charcot joint destruction with some forms of exercise. Therefore, a thorough assessment should be done to ensure that neuropathy does not alter kinesthetic or proprioceptive sensation during physical activity, particularly in those with more severe neuropathy. Studies have shown that moderate-intensity walking may not lead to an increased risk of foot ulcers or reulceration in those with peripheral neuropathy who use proper footwear (275). In addition, 150 min/week of moderate exercise was reported to improve outcomes in people with prediabetic neuropathy (276). All individuals with peripheral neuropathy should wear proper footwear and examine their feet daily to detect lesions early. Anyone with a foot injury or open sore should be restricted to non–weight-bearing activities.
Autonomic Neuropathy
Autonomic neuropathy can increase the risk of exercise-induced injury or adverse events through decreased cardiac responsiveness to exercise, postural hypotension, impaired thermoregulation, impaired night vision due to impaired papillary reaction, and greater susceptibility to hypoglycemia (277). Cardiovascular autonomic neuropathy is also an independent risk factor for cardiovascular death and silent myocardial ischemia (278). Therefore, individuals with diabetic autonomic neuropathy should undergo cardiac investigation before beginning physical activity more intense than that to which they are accustomed.
Diabetic Kidney Disease
Physical activity can acutely increase urinary albumin excretion. However, there is no evidence that vigorous-intensity exercise accelerates the rate of progression of DKD, and there appears to be no need for specific exercise restrictions for people with DKD in general (274).
Smoking Cessation: Tobacco and E-Cigarettes
Recommendations
5.34 Advise all individuals not to use cigarettes and other tobacco products or e-cigarettes. A
5.35 After identification of tobacco or e-cigarette use, include smoking cessation counseling and other forms of treatment as a routine component of diabetes care. A
5.36 Address smoking cessation as part of diabetes education programs for those in need. B
Results from epidemiologic, case-control, and cohort studies provide convincing evidence to support the causal link between cigarette smoking and health risks (279). Data show tobacco use is higher among adults with chronic conditions (280) as well as in adolescents and young adults with diabetes (281). People with diabetes who smoke (and people with diabetes exposed to second-hand smoke) have a heightened risk of CVD, premature death, microvascular complications, and worse glycemic outcomes when compared with those who do not smoke (282–284). Smoking may have a role in the development of type 2 diabetes (285–287).
The routine and thorough assessment of tobacco use is essential to prevent smoking or encourage cessation. Numerous large RCTs have demonstrated the efficacy and cost-effectiveness of brief counseling in smoking cessation, including the use of telephone quit lines, in reducing tobacco use. Pharmacologic therapy to assist with smoking cessation in people with diabetes has been shown to be effective (288), and for people who are motivated to quit, the addition of pharmacologic therapy to counseling is more effective than either treatment alone (289). Special considerations should include assessment of level of nicotine dependence, which is associated with difficulty in quitting and relapse (290). Although some people may gain weight in the period shortly after smoking cessation (291), recent research has demonstrated that this weight gain does not diminish the substantial CVD benefit realized from smoking cessation (292). One study in people who smoke who had newly diagnosed type 2 diabetes found that smoking cessation was associated with amelioration of metabolic parameters and reduced blood pressure and albuminuria at 1 year (293).
In recent years, e-cigarettes have gained public awareness and popularity because of perceptions that e-cigarette use is less harmful than regular cigarette smoking (294,295). However, in light of recent Centers for Disease Control and Prevention evidence (296) of deaths related to e-cigarette use, no individuals should be advised to use e-cigarettes, either as a way to stop smoking tobacco or as a recreational drug.
Diabetes education programs offer potential to systematically reach and engage individuals with diabetes in smoking cessation efforts. A cluster randomized trial found statistically significant increases in quit rates and long-term abstinence rates (>6 months) when smoking cessation interventions were offered through diabetes education clinics, regardless of motivation to quit at baseline (297).
Supporting Positive Health Behaviors
Recommendation
5.37 Behavioral strategies should be used to support diabetes self-management and engagement in health behaviors (e.g., taking medications, using diabetes technologies, physical activity, healthy eating) to promote optimal diabetes health outcomes. A
Given associations with glycemic outcomes and risk for future complications (298,299), it is important for diabetes care professionals to support people with diabetes to engage in health-promoting behaviors (preventive, treatment, and maintenance), including blood glucose monitoring, taking insulin and medications, using diabetes technologies, engaging in physical activity, and making nutritional changes. Evidence supports using a variety of behavioral strategies and multicomponent interventions to help people with diabetes and their caregivers or family members develop health behavior routines and overcome barriers to self-management behaviors (300–302). Behavioral strategies with empirical support include motivational interviewing (303–305), patient activation (306), goal setting and action planning (305,307–309), problem-solving (308,310), tracking or self-monitoring health behaviors with or without feedback from a health care professional (305,307–309), and facilitating opportunities for social support (305,308,309). Multicomponent intervention packages have the highest efficacy for behavioral and glycemic outcomes (300,309,311). For youth with diabetes, family-based behavioral intervention packages and multisystem interventions that facilitate health behavior change demonstrate benefit for increasing management behaviors and improving glycemic outcomes (301). Health behavior change strategies may be delivered by mental health professionals, DCES, or other trained health care professionals (307,312–314) or qualified community health workers (307,308). These approaches may be delivered via digital health tools (309,313,315).
Psychosocial Care
Recommendations
5.38 Psychosocial care should be provided to all people with diabetes, with the goal of optimizing health-related quality of life and health outcomes. Such care should be integrated with routine medical care and delivered by trained health care professionals using a collaborative, person-centered, culturally informed approach. A When indicated and available, qualified mental health professionals should provide additional targeted mental health care. B
5.39 Diabetes care teams should implement psychosocial screening protocols that may include but are not limited to attitudes about diabetes, expectations for treatment and outcomes, general and diabetes-related mood, stress and/or quality of life, available resources (financial, social, family, and emotional), and/or psychiatric history. Screening should occur at periodic intervals and when there is a change in disease, treatment, or life circumstances. C
5.40 When indicated, refer to mental health professionals or other trained health care professionals for further assessment and treatment for symptoms of diabetes distress, depression, suicidality, anxiety, treatment-related fear of hypoglycemia, disordered eating, and/or cognitive capacities. Such specialized psychosocial care should use age-appropriate standardized and validated tools and treatment approaches. B
5.41 Consider screening older adults (aged ≥65 years) with diabetes for cognitive impairment, frailty, and depressive symptoms. Monitoring of cognitive capacity, i.e., the ability to actively engage in decision-making regarding treatment plan behaviors, is advised. B
Please refer to the ADA position statement “Psychosocial Care for People With Diabetes” for a list of assessment tools and additional details (1) and the ADA Mental Health Toolkit for assessment questionnaires and surveys (professional.diabetes.org/mental-health-toolkit).
Complex environmental, social, family, behavioral, and emotional factors, known as psychosocial factors, influence living with diabetes, both type 1 and type 2, and achieving optimal health outcomes and psychological well-being. Thus, individuals with diabetes and their families are challenged with complex, multifaceted issues when integrating diabetes care into daily life (183). Clinically significant mental health diagnoses are considerably more prevalent in people with diabetes than in those without (316,317). Emotional well-being is an important part of diabetes care and self-management. Psychological and social problems can impair the individual’s (43,318–322) or family’s (321) ability to carry out diabetes care tasks and, therefore, potentially compromise health status. Therefore, psychological symptoms, both clinical and subclinical, must be addressed. In addition to impacting a person’s ability to carry out self-management and the association of mental health diagnosis with poorer short-term glycemic stability, symptoms of emotional distress are associated with mortality risk (316,323).
There are opportunities for diabetes health care professionals to routinely monitor and screen psychosocial status in a timely and efficient manner for referral to appropriate services (324,325). Various health care professionals working with people with diabetes may contribute to psychosocial care in different ways based on training, experience, need, and availability (313,326,327). Ideally, qualified mental health professionals with specialized training and experience in diabetes should be integrated with or provide collaborative care as part of diabetes care teams (328–331), or referrals for in-depth assessment and treatment for psychosocial concerns should be made to such mental health professionals when indicated (314,332,333). A systematic review and meta-analysis showed that psychosocial interventions modestly but significantly improved A1C (standardized mean difference –0.29%) and mental health outcomes (334). There was a limited association between the effects on A1C and mental health, and no intervention characteristics predicted benefit on both outcomes. However, cost analyses have shown that behavioral health interventions are both effective and cost-efficient approaches to the prevention of diabetes (335).
Screening
Health care teams should develop and implement psychosocial screening protocols to ensure routine monitoring of psychosocial well-being and concerns among people with diabetes, following published guidance and recommendations (336–340). Topics to screen for may include, but are not limited to, attitudes about diabetes, expectations for treatment and outcomes (especially related to starting a new treatment or technology), general and diabetes-related mood, stress, and/or quality of life (e.g., diabetes distress, depressive symptoms, anxiety symptoms, and/or fear of hypoglycemia), available resources (financial, social, family, and emotional), and/or psychiatric history. A list of age-appropriate screening and evaluation measures is provided in the ADA position statement “Psychosocial Care for People with Diabetes” (1). Key opportunities for psychosocial screening occur at diabetes diagnosis, during regularly scheduled management visits, during hospitalizations, with new onset of complications, during significant transitions in care such as from pediatric to adult care teams (341), at the time of medical treatment changes, or when problems with achieving A1C goals, quality of life, or self-management are identified. People with diabetes are likely to exhibit psychological vulnerability at diagnosis, when their medical status changes (e.g., end of the honeymoon period), when the need for intensified treatment is evident, and when complications are discovered. Significant changes in life circumstances and SDOH are known to considerably affect a person’s ability to self-manage their condition. Thus, screening for SDOH (e.g., loss of employment, birth of a child, or other family-based stresses) should also be incorporated into routine care (342). In circumstances where individuals other than the person with diabetes are significantly involved in diabetes management (e.g., caregivers or family members), these issues should be monitored and treated by appropriate professionals (341,343,344).
Standardized, validated, age-appropriate tools for psychosocial monitoring and screening can also be used (1). Health care professionals may also use informal verbal inquires, for example, by asking whether there have been persistent changes in mood during the past 2 weeks or since the individual’s last appointment and whether the person can identify a triggering event or change in circumstances. Diabetes care professionals should also ask whether there are new or different barriers to treatment and self-management, such as feeling overwhelmed or stressed by having diabetes (see diabetes distress, below), changes in finances, or competing medical demands (e.g., the diagnosis of a comorbid condition).
Psychological Assessment and Treatment
When psychosocial concerns are identified, referral to a qualified behavioral and/or mental health professional, ideally one specializing in diabetes, should be made for comprehensive evaluation, diagnosis, and treatment (313,314,332,333). Indications for referral may include positive screening for overall stress related to work-life balance, diabetes distress, diabetes management difficulties, depression, anxiety, disordered eating, and cognitive dysfunction (see Table 5.2 for a complete list). It is preferable to incorporate psychosocial assessment and treatment into routine care rather than waiting for a specific problem or deterioration in metabolic or psychological status to occur (38,321). Health care professionals should identify behavioral and mental health professionals, knowledgeable about diabetes treatment and the psychosocial aspects of diabetes, to whom they can refer patients. The ADA provides a list of mental health professionals who have specialized expertise or who have received education about psychosocial and behavioral issues related to diabetes in the ADA Mental Health Professional Directory Listing (professional.diabetes.org/mhp_listing). Ideally, mental health professionals should be embedded in diabetes care settings. In recognition of limited behavioral health resources and to optimize availability, other health care professionals who have been trained in behavioral and mental health interventions may also provide this specialized psychosocial care (326,329,345,346). Although some health care professionals may not feel qualified to treat psychological problems (347), optimizing the relationship between a person with diabetes and health care professional may increase the likelihood of the individual accepting referral for other services. Collaborative care interventions and a team approach have demonstrated efficacy in diabetes self-management, outcomes of depression, and psychosocial functioning (5,6).
Table 5.2.
Situations that warrant referral of a person with diabetes to a qualified behavioral or mental health professional for evaluation and treatment
| • A positive screen on a validated screening tool for depressive symptoms, diabetes distress, anxiety, fear of hypoglycemia, or cognitive impairment |
| • The presence of symptoms or suspicions of disordered eating behavior, an eating disorder, or disrupted patterns of eating |
| • Intentional omission of insulin or oral medication to cause weight loss is identified |
| • A serious mental illness is suspected |
| • In youth and families with behavioral self-care difficulties, repeated hospitalizations for diabetic ketoacidosis, failure to achieve expected developmental milestones, or significant distress |
| • Declining or impaired ability to perform diabetes self-care behaviors |
| • Before undergoing bariatric or metabolic surgery and after surgery, if assessment reveals an ongoing need for adjustment support |
Evidence supports interventions for people with diabetes and psychosocial concerns, including issues that affect mental and behavioral health. Successful therapeutic approaches include cognitive behavioral (330,332,348,349) and mindfulness-based therapies (346,350,351). See the sections below for details about interventions for specific psychological concerns. Behavioral interventions may also be indicated in a preventive manner even in the absence of positive psychosocial screeners, such as resilience-promoting interventions to prevent diabetes distress in adolescence (352,353) and behavioral family interventions to promote collaborative family diabetes management in early adolescence (354,355) or to support adjustment to a new treatment plan or technology (64). Psychosocial interventions can be delivered via digital health platforms (356). Group-based or shared diabetes appointments that address both medical and psychosocial issues relevant to living with diabetes are a promising model to consider (327,357).
Although efficacy has been demonstrated with psychosocial interventions, there has been varying success regarding sustained increases in engagement in health behaviors and improved glycemic outcomes associated with behavioral and mental health issues. Thus, health care professionals should systematically monitor these outcomes following implementation of current evidence-based psychosocial treatments to determine ongoing needs.
Diabetes Distress
Recommendation
5.42 Routinely monitor people with diabetes, caregivers, and family members for diabetes distress, particularly when treatment targets are not met and/or at the onset of diabetes complications. Refer to a qualified mental health professional or other trained health care professional for further assessment and treatment if indicated. B
Diabetes distress is very common (321,358–360). While it shares some features with depression, diabetes distress is distinct and has unique relationships with glycemic and other outcomes (359,361). Diabetes distress refers to significant negative psychological reactions related to emotional burdens and worries specific to an individual’s experience in having to manage a severe, complicated, and demanding chronic condition such as diabetes (358,359,362). The constant behavioral demands of diabetes self-management (medication dosing, frequency, and titration; monitoring of glucose, food intake, eating patterns, and physical activity) and the potential or actuality of disease progression are directly associated with reports of diabetes distress (358). The prevalence of diabetes distress is reported to be 18–45%, with an incidence of 38–48% over 18 months in people with type 2 diabetes (362). In the second Diabetes Attitudes, Wishes, and Needs (DAWN2) study, significant diabetes distress was reported by 45% of the participants, but only 24% reported that their health care teams asked them how diabetes affected their lives (321). Similar rates have been identified among adolescents with type 1 diabetes (360) and in parents of youth with type 1 diabetes. High levels of diabetes distress significantly impact medication-taking behaviors and are linked to higher A1C, lower self-efficacy, and less optimal eating and exercise behaviors (5,358,362). Diabetes distress is also associated with symptoms of anxiety, depression, and reduced health-related quality of life (363).
Diabetes distress should be routinely monitored (364) using diabetes-specific validated measures (1). If diabetes distress is identified, it should be acknowledged and addressed. If indicated, the person should be referred for follow-up care (333). This may include specific diabetes education to address areas of diabetes self-care causing distress and impacting clinical management and/or behavioral intervention from a qualified mental health professional, ideally with expertise in diabetes, or from another trained health care professional. Several educational and behavioral intervention strategies have demonstrated benefits for diabetes distress and, to a lesser degree, glycemic outcomes, including education, psychological therapies such as cognitive behavioral therapy and mindfulness-based therapies, and health behavior change approaches such as motivational interviewing (348,349,365,366). Data support diabetes distress interventions delivered using technology (356). DSMES has been shown to reduce diabetes distress (5) and may also benefit A1C when combined with peer support (367). It may be helpful to provide counseling regarding expected diabetes-related versus generalized psychological distress, both at diagnosis and when disease state or treatment changes occur (368). A multisite RCT with adults with type 1 diabetes and elevated diabetes distress and A1C demonstrated large improvements in diabetes distress and small reductions in A1C through two 3-month intervention approaches: a diabetes education intervention with goal setting and a psychological intervention that included emotion regulation skills, motivational interviewing, and goal setting (369). Among adults with type 2 diabetes in the Veterans Affairs system, an RCT demonstrated benefits of integrating a single session of mindfulness intervention into DSMES, followed by a booster session and mobile app-based home practice over 24 weeks, with the strongest effects on diabetes distress (370). An RCT of cognitive behavioral therapy demonstrated positive benefits for diabetes distress, A1C, and depressive symptoms for up to 1 year among adults with type 2 diabetes and elevated symptoms of distress or depression (371). An RCT among people with type 1 and type 2 diabetes found mindful self-compassion training increased self-compassion, reduced depression and diabetes distress, and improved A1C (372). An RCT of a resilience-focused cognitive behavioral and social problem-solving intervention compared with diabetes education (353) in teens with type 1 diabetes showed that diabetes distress and depressive symptoms were significantly reduced for up to 3 years post-intervention, though neither A1C nor self-management behaviors improved over time. These recent studies support that a combination of educational, behavioral, and psychological intervention approaches is needed to address distress, depression, and A1C.
As with treatment of other diabetes-associated behavioral and psychosocial factors affecting disease outcomes, there is little outcome data on long-term systematic treatment of diabetes distress integrated into routine care. As the diabetes disease course and its management are fluid, it can be expected that related distress may fluctuate and may need different methods of remediation at different points in the life course and as disease progression occurs.
Anxiety
Recommendations
5.43 Consider screening people with diabetes for anxiety symptoms or diabetes-related worries. Health care professionals can discuss diabetes-related worries and may refer to a qualified mental health professional for further assessment and treatment if anxiety symptoms indicate interference with diabetes self-management behaviors or quality of life. B
5.44 Refer people with hypoglycemia unawareness, which can co-occur with fear of hypoglycemia, to a trained professional to receive evidence-based intervention to help re-establish awareness of symptoms of hypoglycemia and reduce fear of hypoglycemia. A
Anxiety symptoms and diagnosable disorders (e.g., generalized anxiety disorder, body dysmorphic disorder, obsessive compulsive disorder, specific phobias, and posttraumatic stress disorder) are common in people with diabetes (373). The Behavioral Risk Factor Surveillance System estimated the lifetime prevalence of generalized anxiety disorder to be 19.5% in people with either type 1 or type 2 diabetes (374). A common diabetes-specific concern is fears related to hypoglycemia (375,376), which may explain avoidance of behaviors associated with lowering glucose, such as increasing insulin doses or frequency of monitoring. Other common sources of diabetes-related anxiety include not meeting blood glucose targets (373), insulin injections or infusion (377), and onset of complications (1). People with diabetes who exhibit excessive diabetes self-management behaviors well beyond what is prescribed or needed to achieve glycemic targets may be experiencing symptoms of obsessive-compulsive disorder (378). General anxiety is a predictor of injection-related anxiety and is associated with fear of hypoglycemia (376,379).
Psychological and behavioral care can be helpful to address symptoms of anxiety in people with diabetes. Among adults with type 2 diabetes and elevated depressive symptoms, an RCT of collaborative care demonstrated benefits on anxiety symptoms for up to 1 year (380). Fear of hypoglycemia and hypoglycemia unawareness often co-occur, so interventions aimed at treating one often benefit both (381). If fear of hypoglycemia is identified and a person does not have symptoms of hypoglycemia, a structured program of blood glucose awareness training delivered in routine clinical practice can improve A1C, reduce the rate of severe hypoglycemia, and restore hypoglycemia awareness (382,383). If not available within the practice setting, a structured program targeting both fear of hypoglycemia and unawareness should be sought out and implemented by a qualified behavioral practitioner (381,383–385). An RCT comparing blood glucose awareness training with a cognitively focused psychoeducation program in adults with type 1 diabetes and impaired awareness of hypoglycemia that has been treatment resistant suggested that both approaches were beneficial for reducing hypoglycemia (386). Thus, specialized behavioral intervention from a trained health care professional is needed to treat hypoglycemia-related anxiety and unawareness.
Depression
Recommendations
5.45 Consider at least annual screening of depressive symptoms in all people with diabetes, especially those with a self-reported history of depression. Use age-appropriate, validated depression screening measures, recognizing that further evaluation will be necessary for individuals who have a positive screen. B
5.46 Beginning at diagnosis of complications or when there are significant changes in medical status, consider assessment for depression. B
5.47 Refer to qualified mental health professionals or other trained health care professionals with experience using evidence-based treatment approaches for depression in conjunction with collaborative care with the diabetes treatment team. A
History of depression, current depression, and antidepressant medication use are risk factors for the development of type 2 diabetes, especially if the individual has other risk factors such as obesity and family history of type 2 diabetes (387–389). Elevated depressive symptoms and depressive disorders affect one in four people with type 1 or type 2 diabetes (320). Thus, routine screening for depressive symptoms is indicated in this high-risk population, including people with type 1 or type 2 diabetes, gestational diabetes mellitus, and postpartum diabetes. Regardless of diabetes type, women have significantly higher rates of depression than men (390).
Routine monitoring with age-appropriate validated measures (1) can help to identify if referral is warranted (333,339). Multisite studies have demonstrated feasibility of implementing depressive symptom screening protocols in diabetes clinics and published practical guides for implementation (336–339,391). Adults with a history of depressive symptoms need ongoing monitoring of depression recurrence within the context of routine care (387). Integrating mental and physical health care can improve outcomes. When a person with diabetes is receiving psychological therapy, the mental/behavioral health professional should be incorporated into or collaborate with the diabetes treatment team (392). As with DSMES, person-centered collaborative care approaches have been shown to improve both depression and medical outcomes (392). Depressive symptoms may also be a manifestation of reduced quality of life secondary to disease burden (also see diabetes distress, above) and resultant changes in resource allocation impacting the person and their family. When depressive symptoms are identified, it is important to query origins, both diabetes-specific and due to other life circumstances (363,393).
Trials have shown consistent evidence of improvements in depressive symptoms and variable benefits for A1C when depression is simultaneously treated (331,392,394), whether through pharmacological treatment, group therapy, psychotherapy, or collaborative care (328,348,349,395,396). Psychological interventions targeting depressive symptoms have shown efficacy when delivered via digital technologies (397). Physical activity interventions also demonstrate benefits for depressive symptoms and A1C (398). It is important to note that medical treatment plan should also be monitored in response to reduction in depressive symptoms. People may agree to or adopt previously refused treatment strategies (improving ability to follow recommended treatment behaviors), which may include increased physical activity and intensification of treatment plan behaviors and monitoring, resulting in changed glucose profiles.
Disordered Eating Behavior
Recommendations
5.48 Consider screening for disordered or disrupted eating using validated screening measures when hyperglycemia and weight loss are unexplained based on self-reported behaviors related to medication dosing, meal plan, and physical activity. In addition, a review of the medical treatment plan is recommended to identify potential treatment-related effects on hunger/caloric intake. B
5.49 Consider reevaluating the treatment plan of people with diabetes who present with symptoms of disordered eating behavior, an eating disorder, or disrupted patterns of eating, in consultation with a qualified professional as available. Key qualifications include familiarity with the diabetes disease physiology, treatments for diabetes and disordered eating behaviors, and weight-related and psychological risk factors for disordered eating behaviors. B
Estimated prevalence of disordered eating behavior and diagnosable eating disorders in people with diabetes varies (399–401). For people with type 1 diabetes, insulin omission causing glycosuria in order to lose weight is the most commonly reported disordered eating behavior (402,403); in people with type 2 diabetes, bingeing (excessive food intake with an accompanying sense of loss of control) is most commonly reported. For people with type 2 diabetes treated with insulin, intentional omission is also frequently reported (404). People with diabetes and diagnosable eating disorders have high rates of comorbid psychiatric disorders (405). People with type 1 diabetes and eating disorders have high rates of diabetes distress and fear of hypoglycemia (406).
Diabetes care professionals should monitor for disordered eating behaviors using validated measures (407). When evaluating symptoms of disordered or disrupted eating (when the individual exhibits eating behaviors that appear maladaptive but are not volitional, such as bingeing caused by loss of satiety cues), etiology and motivation for the behavior should be evaluated (401,408). Mixed intervention results point to the need for treatment of eating disorders and disordered eating behavior in the context of the disease and its treatment. Given the complexities of treating disordered eating behaviors and disrupted eating patterns in people with diabetes, it is recommended that multidisciplinary care teams include or collaborate with a health professional trained to identify and treat eating behaviors with expertise in disordered eating and diabetes (409). Key qualifications for such professionals include familiarity with the diabetes disease physiology, weight-related and psychological risk factors for disordered eating behaviors, and treatments for diabetes and disordered eating behaviors. More rigorous methods to identify underlying mechanisms of action that drive change in eating and treatment behaviors, as well as associated mental distress, are needed (410). Health care teams may consider the appropriateness of technology use among people with diabetes and disordered eating behaviors, although more research on the risks and benefits is needed (411). Caution should be taken in labeling individuals with diabetes as having a diagnosable psychiatric disorder, i.e., an eating disorder, when disordered or disrupted eating patterns are found to be associated with the disease and its treatment. In other words, patterns of maladaptive food intake that appear to have a psychological origin may be driven by physiologic disruption in hunger and satiety cues, metabolic perturbations, and/or secondary distress because of the individual’s inability to control their hunger and satiety (401,408).
The use of incretin therapies may have potential implications and relevance for the treatment of disrupted or disordered eating (see Section 8, “Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes”). These medications promote substantial weight loss and maintenance of lost weight beyond conventional nutrition therapies (412), which may improve quality of life. Incretin therapies work in the appetite and reward circuitries to modulate food intake and energy balance, reducing uncontrollable hunger, overeating, and bulimic symptoms (413), although mechanisms are not completely understood. Health care professionals may see expanded use of these medications as data become available (401). This therapy has the potential to improve psychosocial outcomes and control overeating behaviors in people with diabetes, which may ultimately benefit engagement with medical nutrition therapy recommendations (414). More research is needed about adjunctive use of incretins and other medications affecting physiologically based eating behavior in people with diabetes.
Serious Mental Illness
Recommendations
5.50 Provide an increased level of support for people with diabetes and serious mental illness through enhanced monitoring of and assistance with diabetes self-management behaviors. B
5.51 In people who are prescribed atypical antipsychotic medications, screen for prediabetes and diabetes 4 months after medication initiation and sooner if clinically indicated, at least annually. B
5.52 If a second-generation antipsychotic medication is prescribed for adolescents or adults with diabetes, changes in weight, glycemia, and cholesterol levels should be carefully monitored, and the treatment plan should be reassessed accordingly. C
Studies of individuals with serious mental illness, particularly schizophrenia and other thought disorders, show significantly increased rates of type 2 diabetes (415). People with schizophrenia should be monitored for type 2 diabetes because of the known comorbidity. Disordered thinking and judgment can be expected to make it difficult to engage in behavior that reduces risk factors for type 2 diabetes, such as restrained eating for weight management. Further, people with serious mental health disorders and diabetes frequently experience moderate psychological distress, suggesting pervasive intrusion of mental health issues into daily functioning (416).
Coordinated management of diabetes or prediabetes and serious mental illness is recommended to achieve diabetes treatment targets. The diabetes care team, in collaboration with other care professionals, should work to provide an enhanced level of care and self-management support for people with diabetes and serious mental illness based on individual capacity and needs. Such care may include remote monitoring, facilitating health care aides, and providing diabetes training for family members, community support personnel, and other caregivers. Qualitative research suggests that educational and behavioral intervention may provide benefit via group support, accountability, and assistance with applying diabetes knowledge (417). In addition, those taking second-generation (atypical) antipsychotics, such as olanzapine, require greater monitoring because of an increase in risk of type 2 diabetes associated with this medication (418–420). Because of this increased risk, people should be screened for prediabetes or diabetes 4 months after medication initiation and at least annually thereafter. Serious mental illness is often associated with the inability to evaluate and utilize information to make judgments about treatment options. When a person has an established diagnosis of a mental illness that impacts judgment, activities of daily living, and ability to establish a collaborative relationship with care professionals, it is wise to include a nonmedical caretaker in decision-making regarding the medical treatment plan. This person can help improve the patient’s ability to follow the agreed-upon treatment plan through both monitoring and caretaking functions (421).
Cognitive Capacity/Impairment
Recommendations
5.53 Cognitive capacity should be monitored throughout the life span for all individuals with diabetes, particularly in those who have documented cognitive disabilities, those who experience severe hypoglycemia, very young children, and older adults. B
5.54 If cognitive capacity changes or appears to be suboptimal for patient decision-making and/or behavioral self-management, referral for a formal assessment should be considered. E
Cognitive capacity is generally defined as attention, memory, logic and reasoning, and auditory and visual processing, all of which are involved in diabetes self-management behavior (422). Having diabetes over decades—type 1 and type 2—has been shown to be associated with cognitive decline (423–425). Declines have been shown to impact executive function and information processing speed; they are not consistent between people, and evidence is lacking regarding a known course of decline (426). Diagnosis of dementia is also more prevalent among people with diabetes, both type 1 and type 2 (427). Thus, monitoring of cognitive capacity of individuals is recommended, particularly regarding their ability to self-monitor and make judgments about their symptoms, physical status, and needed alterations to their self-management behaviors, all of which are mediated by executive function (427). As with other disorders affecting mental capacity (e.g., major psychiatric disorders), the key issue is whether the person can collaborate with the care team to achieve optimal metabolic outcomes and prevent complications, both short and long term (416). When this ability is shown to be altered, declining, or absent, a lay care professional should be introduced into the care team who serves in the capacities of day-to-day monitoring as well as a liaison with the rest of the care team (1). Cognitive capacity also contributes to ability to benefit from diabetes education and may indicate the need for alternative teaching approaches as well as remote monitoring. Youth will need second-party monitoring (e.g., parents and adult caregivers) until they are developmentally able to evaluate necessary information for self-management decisions and to inform resultant behavior changes.
Episodes of severe hypoglycemia are independently associated with decline, as well as the more immediate symptoms of mental confusion (428). Early-onset type 1 diabetes has been shown to be associated with potential deficits in intellectual abilities, especially in the context of repeated episodes of severe hypoglycemia (429). (See Section 14, “Children and Adolescents,” for information on early-onset diabetes and cognitive abilities and the effects of severe hypoglycemia on children’s cognitive and academic performance.) Thus, for myriad reasons, cognitive capacity should be assessed during routine care to ascertain the person’s ability to maintain and adjust self-management behaviors, such as dosing of medications, remediation approaches to glycemic excursions, etc., and to determine whether to enlist a caregiver in monitoring and decision-making regarding management behaviors. If cognitive capacity to carry out self-maintenance behaviors is questioned, an age-appropriate test of cognitive capacity is recommended (1). Cognitive capacity should be evaluated in the context of the person’s age, for example, in very young children who are not expected to manage their disease independently and in older adults who may need active monitoring of treatment plan behaviors.
Sleep Health
Recommendation
5.55 Consider screening for sleep health in people with diabetes, including symptoms of sleep disorders, disruptions to sleep due to diabetes symptoms or management needs, and worries about sleep. Refer to sleep medicine and/or a qualified behavioral health professional as indicated. B
The associations between sleep problems and diabetes are complex: sleep disorders are a risk factor for developing type 2 diabetes (430,431) and possibly gestational diabetes mellitus (432,433). Moreover, sleep disturbances are associated with less engagement in diabetes self-management and may interfere with the achievement of glycemic targets among people with type 1 and type 2 diabetes (434–439). Disrupted sleep and sleep disorders, including obstructive sleep apnea (440), insomnia, and sleep disturbances (435), are common among people with diabetes. In type 1 diabetes, estimates of poor sleep range from 30% to 50% (441), and estimates of moderate to severe obstructive sleep apnea are >50% (436). In type 2 diabetes, 24–86% of people are estimated to have obstructive sleep apnea (442), 39% to have insomnia, and 8–45% to have restless leg syndrome (439). Risk of hypoglycemia poses specific challenges for sleep in people with type 1 diabetes and may require targeted assessment and treatment approaches (443). People with diabetes and their family members also describe diabetes management needs interfering with sleep and experiencing worries about poor sleep; technology has been described as both a help and challenge in relation to sleep (444). Cognitive behavioral therapy shows benefits for sleep in people with diabetes (348), including cognitive behavioral therapy for insomnia, which demonstrates improvements in sleep outcomes and possible small improvements in A1C and fasting glucose (445). There is also evidence that sleep extension and pharmacological treatments for sleep can improve sleep outcomes and possibly insulin resistance (443,445). Thus, referral to sleep specialists to address the medical and behavioral aspects of sleep is recommended, ideally in collaboration with the diabetes care professional (Fig. 5.1).
Footnotes
Disclosure information for each author is available at https://doi.org/10.2337/dc23-SDIS.
Suggested citation: ElSayed NA, Aleppo G, Aroda VR, et al., American Diabetes Association. 5. Facilitating positive health behaviors and well-being to improve health outcomes: Standards of Care in Diabetes—2023. Diabetes Care 2023;46(Suppl. 1):S68–S96
References
- 1. Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care 2016;39:2126–2140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Powers MA, Bardsley JK, Cypress M, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care 2020;43:1636–1649 [DOI] [PubMed] [Google Scholar]
- 3. Rutten GEHM, Alzaid A. Person-centred type 2 diabetes care: time for a paradigm shift. Lancet Diabetes Endocrinol 2018;6:264–266 [DOI] [PubMed] [Google Scholar]
- 4. Dickinson JK, Guzman SJ, Maryniuk MD, et al. The use of language in diabetes care and education. Diabetes Care 2017;40:1790–1799 [DOI] [PubMed] [Google Scholar]
- 5. Fisher L, Hessler D, Glasgow RE, et al. REDEEM: a pragmatic trial to reduce diabetes distress. Diabetes Care 2013;36:2551–2558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huang Y, Wei X, Wu T, Chen R, Guo A. Collaborative care for patients with depression and diabetes mellitus: a systematic review and meta-analysis. BMC Psychiatry 2013;13:260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hill-Briggs F. Problem solving in diabetes self-management: a model of chronic illness self-management behavior. Ann Behav Med 2003;25:182–193 [DOI] [PubMed] [Google Scholar]
- 8. Greenwood DA, Howell F, Scher L, et al. A framework for optimizing technology-enabled diabetes and cardiometabolic care and education: the role of the diabetes care and education specialist. Diabetes Educ 2020;46:315–322 [DOI] [PubMed] [Google Scholar]
- 9. Tran VT, Barnes C, Montori VM, Falissard B, Ravaud P. Taxonomy of the burden of treatment: a multi-country web-based qualitative study of patients with chronic conditions. BMC Med 2015;13:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fitzpatrick SL, Golden SH, Stewart K, et al. Effect of DECIDE (Decision-making Education for Choices In Diabetes Everyday) program delivery modalities on clinical and behavioral outcomes in urban African Americans with type 2 diabetes: a randomized trial. Diabetes Care 2016;39:2149–2157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brunisholz KD, Briot P, Hamilton S, et al. Diabetes self-management education improves quality of care and clinical outcomes determined by a diabetes bundle measure. J Multidiscip Healthc 2014;7:533–542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dickinson JK, Maryniuk MD. Building therapeutic relationships: choosing words that put people first. Clin Diabetes 2017;35:51–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Davis J, Fischl AH, Beck J, et al. 2022 National standards for diabetes self-management education and support. Sci Diabetes Self Manag Care 2022;48:44–59 [DOI] [PubMed] [Google Scholar]
- 14. Tang TS, Funnell MM, Brown MB, Kurlander JE. Self-management support in “real-world” settings: an empowerment-based intervention. Patient Educ Couns 2010;79:178–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Marrero DG, Ard J, Delamater AM, et al. Twenty-first century behavioral medicine: a context for empowering clinicians and patients with diabetes: a consensus report. Diabetes Care 2013;36:463–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rutten GEHM, Van Vugt H, de Koning E. Person-centered diabetes care and patient activation in people with type 2 diabetes. BMJ Open Diabetes Res Care 2020;8:e001926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159–1171 [DOI] [PubMed] [Google Scholar]
- 18. Frosch DL, Uy V, Ochoa S, Mangione CM. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Arch Intern Med 2011;171:2011–2017 [DOI] [PubMed] [Google Scholar]
- 19. Cooke D, Bond R, Lawton J, et al.; U.K. NIHR DAFNE Study Group . Structured type 1 diabetes education delivered within routine care: impact on glycemic control and diabetes-specific quality of life. Diabetes Care 2013;36:270–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Patient Educ Couns 2016;99:926–943 [DOI] [PubMed] [Google Scholar]
- 21. Marincic PZ, Salazar MV, Hardin A, et al. Diabetes self-management education and medical nutrition therapy: a multisite study documenting the efficacy of registered dietitian nutritionist interventions in the management of glycemic control and diabetic dyslipidemia through retrospective chart review. J Acad Nutr Diet 2019;119:449–463 [DOI] [PubMed] [Google Scholar]
- 22. Steinsbekk A, Rygg LØ, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res 2012;12:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cochran J, Conn VS. Meta-analysis of quality of life outcomes following diabetes self-management training. Diabetes Educ 2008;34:815–823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Davidson P, LaManna J, Davis J, et al. The effects of diabetes self-management education on quality of life for persons with type 1 diabetes: a systematic review of randomized controlled trials. Sci Diabetes Self Manag Care 2022;48:111–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. He X, Li J, Wang B, et al. Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Endocrine 2017;55:712–731 [DOI] [PubMed] [Google Scholar]
- 26. Thorpe CT, Fahey LE, Johnson H, Deshpande M, Thorpe JM, Fisher EB. Facilitating healthy coping in patients with diabetes: a systematic review. Diabetes Educ 2013;39:33–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Robbins JM, Thatcher GE, Webb DA, Valdmanis VG. Nutritionist visits, diabetes classes, and hospitalization rates and charges: the Urban Diabetes Study. Diabetes Care 2008;31:655–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Duncan I, Ahmed T, Li QE, et al. Assessing the value of the diabetes educator. Diabetes Educ 2011;37:638–657 [DOI] [PubMed] [Google Scholar]
- 29. Strawbridge LM, Lloyd JT, Meadow A, Riley GF, Howell BL. One-year outcomes of diabetes self-management training among medicare beneficiaries newly diagnosed with diabetes. Med Care 2017;55:391–397 [DOI] [PubMed] [Google Scholar]
- 30. Johnson TM, Murray MR, Huang Y. Associations between self-management education and comprehensive diabetes clinical care. Diabetes Spectr 2010;23:41–46 [Google Scholar]
- 31. Duncan I, Birkmeyer C, Coughlin S, Li QE, Sherr D, Boren S. Assessing the value of diabetes education. Diabetes Educ 2009;35:752–760 [DOI] [PubMed] [Google Scholar]
- 32. Piatt GA, Anderson RM, Brooks MM, et al. 3-year follow-up of clinical and behavioral improvements following a multifaceted diabetes care intervention: results of a randomized controlled trial. Diabetes Educ 2010;36:301–309 [DOI] [PubMed] [Google Scholar]
- 33. Dallosso H, Mandalia P, Gray LJ, et al. The effectiveness of a structured group education programme for people with established type 2 diabetes in a multi-ethnic population in primary care: a cluster randomised trial. Nutr Metab Cardiovasc Dis 2022;32:1549–1559 [DOI] [PubMed] [Google Scholar]
- 34. Glazier RH, Bajcar J, Kennie NR, Willson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care 2006;29:1675–1688 [DOI] [PubMed] [Google Scholar]
- 35. Hawthorne K, Robles Y, Cannings-John R, Edwards AGK. Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database Syst Rev 1996;3:CD006424. [DOI] [PubMed] [Google Scholar]
- 36. Chodosh J, Morton SC, Mojica W, et al. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med 2005;143:427–438 [DOI] [PubMed] [Google Scholar]
- 37. Sarkisian CA, Brown AF, Norris KC, Wintz RL, Mangione CM. A systematic review of diabetes self-care interventions for older, African American, or Latino adults. Diabetes Educ 2003;29:467–479 [DOI] [PubMed] [Google Scholar]
- 38. Peyrot M, Rubin RR. Behavioral and psychosocial interventions in diabetes: a conceptual review. Diabetes Care 2007;30:2433–2440 [DOI] [PubMed] [Google Scholar]
- 39. Naik AD, Palmer N, Petersen NJ, et al. Comparative effectiveness of goal setting in diabetes mellitus group clinics: randomized clinical trial. Arch Intern Med 2011;171:453–459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mannucci E, Giaccari A, Gallo M, et al. Self-management in patients with type 2 diabetes: group-based versus individual education. A systematic review with meta-analysis of randomized trails. Nutr Metab Cardiovasc Dis 2021 [DOI] [PubMed] [Google Scholar]
- 41. Duke SAS, Colagiuri S, Colagiuri R. Individual patient education for people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2009;2009:CD005268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Odgers-Jewell K, Ball LE, Kelly JT, Isenring EA, Reidlinger DP, Thomas R. Effectiveness of group-based self-management education for individuals with type 2 diabetes: a systematic review with meta-analyses and meta-regression. Diabet Med 2017;34:1027–1039 [DOI] [PubMed] [Google Scholar]
- 43. Davis J, Fischl AH, Beck J, et al. 2022 National standards for diabetes self-management education and support. Diabetes Care 2022;45:484–494 [DOI] [PubMed] [Google Scholar]
- 44. Pereira K, Phillips B, Johnson C, Vorderstrasse A. Internet delivered diabetes self-management education: a review. Diabetes Technol Ther 2015;17:55–63 [DOI] [PubMed] [Google Scholar]
- 45. Sepah SC, Jiang L, Peters AL. Long-term outcomes of a web-based diabetes prevention program: 2-year results of a single-arm longitudinal study. J Med Internet Res 2015;17:e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Greenwood DA, Gee PM, Fatkin KJ, Peeples M. A systematic review of reviews evaluating technology-enabled diabetes self-management education and support. J Diabetes Sci Technol 2017;11:1015–1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Athinarayanan SJ, Adams RN, Hallberg SJ, et al. Long-term effects of a novel continuous remote care intervention including nutritional ketosis for the management of type 2 diabetes: a 2-year non-randomized clinical trial. Front Endocrinol (Lausanne) 2019;10:348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kumar S, Moseson H, Uppal J, Juusola JL. A diabetes mobile app with in-app coaching from a certified diabetes educator reduces A1C for individuals with type 2 diabetes. Diabetes Educ 2018;44:226–236 [DOI] [PubMed] [Google Scholar]
- 49. Hallberg SJ, McKenzie AL, Williams PT, et al. Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: an open-label, non-randomized, controlled study. Diabetes Ther 2018;9:583–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Xu T, Pujara S, Sutton S, Rhee M. Telemedicine in the management of type 1 diabetes. Prev Chronic Dis 2018;5:E13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Dening J, Islam SMS, George E, Maddison R. Web-based interventions for dietary behavior in adults with type 2 diabetes: systematic review of randomized controlled trials. J Med Internet Res 2020;22:e16437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Anderson A, O’Connell SS, Thomas C, Chimmanamada R. Telehealth interventions to improve diabetes management among Black and Hispanic patients: a systematic review and meta-analysis. J Racial Ethn Health Disparities 2022;9:2375–2386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sherifali D, Brozic A, Agema P, et al. Effect of diabetes health coaching on glycemic control and quality of life in adults living with type 2 diabetes: a community-based, randomized, controlled trial. Can J Diabetes 2021;45:594–600 [DOI] [PubMed] [Google Scholar]
- 54. von Storch K, Graaf E, Wunderlich M, Rietz C, Polidori MC, Woopen C. Telemedicine-assisted self-management program for type 2 diabetes patients. Diabetes Technol Ther 2019;21:514–521 [DOI] [PubMed] [Google Scholar]
- 55. Omar MA, Hasan S, Palaian S, Mahameed S. The impact of a self-management educational program coordinated through WhatsApp on diabetes control. Pharm Pract (Granada) 2020;18:1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Liang K, Xie Q, Nie J, Deng J. Study on the effect of education for insulin injection in diabetic patients with new simulation tools. Medicine (Baltimore) 2021;100:e25424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sahin C, Courtney KL, Naylor PJ, E Rhodes R. Tailored mobile text messaging interventions targeting type 2 diabetes self-management: a systematic review and a meta-analysis. Digit Health 2019;5:2055207619845279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Leong CM, Lee TI, Chien YM, Kuo LN, Kuo YF, Chen HY. Social media-delivered patient education to enhance self-management and attitudes of patients with type 2 diabetes during the COVID-19 pandemic: randomized controlled trial. J Med Internet Res 2022;24:e31449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Xia SF, Maitiniyazi G, Chen Y, et al. Web-based TangPlan and WeChat combination to support self-management for patients with type 2 diabetes: randomized controlled trial. JMIR Mhealth Uhealth 2022;10:e30571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Jiang Y, Ramachandran HJ, Teo JYC, et al. Effectiveness of a nurse-led smartphone-based self-management programme for people with poorly controlled type 2 diabetes: a randomized controlled trial. J Adv Nurs 2022;78:1154–1165 [DOI] [PubMed] [Google Scholar]
- 61. Gershkowitz BD, Hillert CJ, Crotty BH. Digital coaching strategies to facilitate behavioral change in type 2 diabetes: a systematic review. J Clin Endocrinol Metab 2021;106:e1513–e1520 [DOI] [PubMed] [Google Scholar]
- 62. Lee MK, Lee DY, Ahn HY, Park CY. A novel user utility score for diabetes management using tailored mobile coaching: secondary analysis of a randomized controlled trial. JMIR Mhealth Uhealth 2021;9:e17573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Yoo JH, Kim G, Lee HJ, Sim KH, Jin SM, Kim JH. Effect of structured individualized education on continuous glucose monitoring use in poorly controlled patients with type 1 diabetes: a randomized controlled trial. Diabetes Res Clin Pract 2022;184:109209. [DOI] [PubMed] [Google Scholar]
- 64. Strategies to Enhance New CGM Use in Early Childhood (SENCE) Study Group . A randomized clinical trial assessing continuous glucose monitoring (CGM) use with standardized education with or without a family behavioral intervention compared with fingerstick blood glucose monitoring in very young children with type 1 diabetes. Diabetes Care 2021;44:464–472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Isaacs D, Cox C, Schwab K, et al. Technology integration: the role of the diabetes care and education specialist in practice. Diabetes Educ 2020;46:323–334 [DOI] [PubMed] [Google Scholar]
- 66. Scalzo P. From the Association of Diabetes Care & Education Specialists: the role of the diabetes care and education specialist as a champion of technology integration. Sci Diabetes Self Manag Care 2021;47:120–123 [DOI] [PubMed] [Google Scholar]
- 67. Greenwood DA, Litchman ML, Isaacs D, et al. A new taxonomy for technology-enabled diabetes self-management interventions: results of an umbrella review. J Diabetes Sci Technol 2021;16:812–824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. van Eikenhorst L, Taxis K, van Dijk L, de Gier H. Pharmacist-led self-management interventions to improve diabetes outcomes. A systematic literature review and meta-analysis. Front Pharmacol 2017;8:891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Tshiananga JKT, Kocher S, Weber C, Erny-Albrecht K, Berndt K, Neeser K. The effect of nurse-led diabetes self-management education on glycosylated hemoglobin and cardiovascular risk factors: a meta-analysis. Diabetes Educ 2012;38:108–123 [DOI] [PubMed] [Google Scholar]
- 70. Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care 2019;42:731–754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Shah M, Kaselitz E, Heisler M. The role of community health workers in diabetes: update on current literature. Curr Diab Rep 2013;13:163–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Spencer MS, Kieffer EC, Sinco B, et al. Outcomes at 18 months from a community health worker and peer leader diabetes self-management program for Latino adults. Diabetes Care 2018;41:1414–1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med 2010;153:507–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Long JA, Jahnle EC, Richardson DM, Loewenstein G, Volpp KG. Peer mentoring and financial incentives to improve glucose control in African American veterans: a randomized trial. Ann Intern Med 2012;156:416–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Fisher EB, Boothroyd RI, Elstad EA, et al. Peer support of complex health behaviors in prevention and disease management with special reference to diabetes: systematic reviews. Clin Diabetes Endocrinol 2017;3:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Litchman ML, Oser TK, Hodgson L, et al. In-person and technology-mediated peer support in diabetes care: a systematic review of reviews and gap analysis. Diabetes Educ 2020;46:230–241 [DOI] [PubMed] [Google Scholar]
- 77. Foster G, Taylor SJC, Eldridge SE, Ramsay J, Griffiths CJ. Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev 2007:CD005108. [DOI] [PubMed] [Google Scholar]
- 78. Powell RE, Zaccardi F, Beebe C, et al. Strategies for overcoming therapeutic inertia in type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab 2021;23:2137–2154 [DOI] [PubMed] [Google Scholar]
- 79. Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care 2020. dci200053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Strawbridge LM, Lloyd JT, Meadow A, Riley GF, Howell BL. Use of Medicare’s diabetes self-management training benefit. Health Educ Behav 2015;42:530–538 [DOI] [PubMed] [Google Scholar]
- 81. Horigan G, Davies M, Findlay-White F, Chaney D, Coates V. Reasons why patients referred to diabetes education programmes choose not to attend: a systematic review. Diabet Med 2016 [DOI] [PubMed] [Google Scholar]
- 82. Carey ME, Agarwal S, Horne R, Davies M, Slevin M, Coates V. Exploring organizational support for the provision of structured self-management education for people with type 2 diabetes: findings from a qualitative study. Diabet Med 2019;36:761–770 [DOI] [PubMed] [Google Scholar]
- 83. Department of Health and Human Services . Telehealth.HHS.gov. Telehealth and remote patient monitoring. Accessed 6 October 2022. Available from: https://telehealth.hhs.gov/providers/preparing-patients-for-telehealth/telehealth-and-remote-patient-monitoring/
- 84. Center For Health Law and Policy Innovation . Reconsidering cost-sharing for diabetes self-management education: recommendations for policy reform. Accessed 19 October 2022. Available from https://chlpi.org/wp-content/uploads/2015/07/6.11.15-Reconsidering-Cost-Sharing-for-DSME-cover.jpg
- 85. Turner RM, Ma Q, Lorig K, Greenberg J, DeVries AR. Evaluation of a diabetes self-management program: claims analysis on comorbid illnesses, health care utilization, and cost. J Med Internet Res 2018. 20:e207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Centers for Medicare & Medicaid Services . COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing. 19 October 2022. Available from https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf
- 87. Holt RIG, DeVries JH, Hess-Fischl A, et al. The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2021;44:2589–2625 [DOI] [PubMed] [Google Scholar]
- 88. Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2022;45:2753–2786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. English LK, Ard JD, Bailey RL, et al. Evaluation of dietary patterns and all-cause mortality: a systematic review. JAMA Netw Open 2021;4:e2122277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Dietary Guidelines for America Committee . Scientific report of the 2020 Dietary Guidelines Advisory Committee: advisory report to the Secretary of Agriculture and the Secretary of Health and Human Services. Washington, DC, Agricultural Research Service, 2020. Available from 10.52570/DGAC2020 [DOI]
- 91. Lichtenstein AH, Appel LJ, Vadiveloo M, et al. 2021 Dietary guidance to improve cardiovascular health: a scientific statement from the American Heart Association. Circulation 2021;144:e472–e487 [DOI] [PubMed] [Google Scholar]
- 92. Rosenfeld RM, Kelly JH, Agarwal M, et al. Dietary interventions to treat type 2 diabetes in adults with a goal of remission: an expert consensus statement from the American College of Lifestyle Medicine. Am J Lifestyle Med 2022;16:342–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Joseph JJ, Deedwania P, Acharya T, et al.; American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Clinical Cardiology; and Council on Hypertension . Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement from the American Heart Association. Circulation 2022;145:e722–e759 [DOI] [PubMed] [Google Scholar]
- 94. Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018;41:2669–2701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Briggs Early K, Stanley K. Position of the Academy of Nutrition and Dietetics: the role of medical nutrition therapy and registered dietitian nutritionists in the prevention and treatment of prediabetes and type 2 diabetes. J Acad Nutr Diet 2018;118:343–353 [DOI] [PubMed] [Google Scholar]
- 96. Dobrow L, Estrada I, Burkholder-Cooley N, Miklavcic J. Potential effectiveness of registered dietitian nutritionists in healthy behavior interventions for managing type 2 diabetes in older adults: a systematic review. Front Nutr 2022;8:737410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Franz MJ, MacLeod J, Evert A, et al. Academy of Nutrition and Dietetics Nutrition practice guideline for type 1 and type 2 diabetes in adults: systematic review of evidence for medical nutrition therapy effectiveness and recommendations for integration into the nutrition care process. J Acad Nutr Diet 2017;117:1659–1679 [DOI] [PubMed] [Google Scholar]
- 98. Mudaliar U, Zabetian A, Goodman M, et al. Cardiometabolic risk factor changes observed in diabetes prevention programs in US settings: a systematic review and meta-analysis. PLoS Med 2016;13:e1002095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Balk EM, Earley A, Raman G, Avendano EA, Pittas AG, Remington PL. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the community preventive services task force combined diet and physical activity promotion programs to prevent diabetes. Ann Intern Med 2015;163:437–451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Hamman RF, Wing RR, Edelstein SL, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care 2006;29:2102–2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Garvey WT, Ryan DH, Bohannon NJV, et al. Weight-loss therapy in type 2 diabetes: effects of phentermine and topiramate extended release. Diabetes Care 2014;37:3309–3316 [DOI] [PubMed] [Google Scholar]
- 102. Kahan S, Fujioka K. Obesity pharmacotherapy in patients with type 2 diabetes. Diabetes Spectr 2017;30:250–257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care 2007;30:744–752 [DOI] [PubMed] [Google Scholar]
- 104. Duncan GE, Perri MG, Theriaque DW, Hutson AD, Eckel RH, Stacpoole PW. Exercise training, without weight loss, increases insulin sensitivity and postheparin plasma lipase activity in previously sedentary adults. Diabetes Care 2003;26:557–562 [DOI] [PubMed] [Google Scholar]
- 105. Franz MJ, Boucher JL, Rutten-Ramos S, VanWormer JJ. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. J Acad Nutr Diet 2015;115:1447–1463 [DOI] [PubMed] [Google Scholar]
- 106. Lean ME, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 2018;391:541–551 [DOI] [PubMed] [Google Scholar]
- 107. Wing RR, Lang W, Wadden TA, et al.; Look AHEAD Research Group . Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011;34:1481–1486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Look AHEAD Research Group . Does lifestyle intervention improve health of adults with overweight/obesity and type 2 diabetes? Findings from the Look AHEAD randomized trial. Obesity (Silver Spring) 2021;29:1246–1258 [DOI] [PubMed] [Google Scholar]
- 109. Garvey WT. Long-term health benefits of intensive lifestyle intervention in the Look AHEAD study. Obesity (Silver Spring) 2021;29:1242–1243 [DOI] [PubMed] [Google Scholar]
- 110. Davies M, Færch L, Jeppesen OK, et al.; STEP 2 Study Group . Semaglutide 2.4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet 2021;397:971–984 [DOI] [PubMed] [Google Scholar]
- 111. Jastreboff AM, Aronne LJ, Ahmad NN, et al.; SURMOUNT-1 Investigators . Tirzepatide once weekly for the treatment of obesity. N Engl J Med 2022;387:205–216 [DOI] [PubMed] [Google Scholar]
- 112. Sjöström L, Peltonen M, Jacobson P, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA 2014;311:2297–2304 [DOI] [PubMed] [Google Scholar]
- 113. Cefalu WT, Leiter LA, de Bruin TWA, Gause-Nilsson I, Sugg J, Parikh SJ. Dapagliflozin’s effects on glycemia and cardiovascular risk factors in high-risk patients with type 2 diabetes: a 24-week, multicenter, randomized, double-blind, placebo-controlled study with a 28-week extension. Diabetes Care 2015;38:1218–1227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Prinz N, Schwandt A, Becker M, et al. Trajectories of body mass index from childhood to young adulthood among patients with type 1 diabetes—a longitudinal group-based modeling approach based on the DPV Registry. J Pediatr 2018;201:78–85.e4 [DOI] [PubMed] [Google Scholar]
- 115. Lipman TH, Levitt Katz LE, Ratcliffe SJ, et al. Increasing incidence of type 1 diabetes in youth: twenty years of the Philadelphia Pediatric Diabetes Registry. Diabetes Care 2013;36:1597–1603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med 2011;365:1597–1604 [DOI] [PubMed] [Google Scholar]
- 117. Hamdy O, Mottalib A, Morsi A, et al. Long-term effect of intensive lifestyle intervention on cardiovascular risk factors in patients with diabetes in real-world clinical practice: a 5-year longitudinal study. BMJ Open Diabetes Res Care 2017;5:e000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Nip ASY, Reboussin BA, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . Disordered eating behaviors in youth and young adults with type 1 or type 2 diabetes receiving insulin therapy: the SEARCH for Diabetes in Youth Study. Diabetes Care 2019;42:859–866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Mottalib A, Salsberg V, Mohd-Yusof BN, et al. Effects of nutrition therapy on HbA1c and cardiovascular disease risk factors in overweight and obese patients with type 2 diabetes. Nutr J 2018;17:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. PREDIMED Study Investigators . Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med 2018;378:e34. [DOI] [PubMed] [Google Scholar]
- 121. Saslow LR, Daubenmier JJ, Moskowitz JT, et al. Twelve-month outcomes of a randomized trial of a moderate-carbohydrate versus very low-carbohydrate diet in overweight adults with type 2 diabetes mellitus or prediabetes. Nutr Diabetes 2017;7:304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Yancy WS, Crowley MJ, Dar MS, et al. Comparison of group medical visits combined with intensive weight management vs group medical visits alone for glycemia in patients with type 2 diabetes: a noninferiority randomized clinical trial. JAMA Intern Med 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Emadian A, Andrews RC, England CY, Wallace V, Thompson JL. The effect of macronutrients on glycaemic control: a systematic review of dietary randomised controlled trials in overweight and obese adults with type 2 diabetes in which there was no difference in weight loss between treatment groups. Br J Nutr 2015;114:1656–1666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Gardner CD, Trepanowski JF, Del Gobbo LC, Hauser ME, Rigdon J, Ioannidis JPA, et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial. JAMA 2018;319:667–679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Korsmo-Haugen HK, Brurberg KG, Mann J, Aas AM. Carbohydrate quantity in the dietary management of type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab 2019;21:15–27 [DOI] [PubMed] [Google Scholar]
- 126. Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med 2009;360:859–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. de Souza RJ, Bray GA, Carey VJ, et al. Effects of 4 weight-loss diets differing in fat, protein, and carbohydrate on fat mass, lean mass, visceral adipose tissue, and hepatic fat: results from the POUNDS LOST trial. Am J Clin Nutr 2012;95:614–625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Johnston BC, Kanters S, Bandayrel K, et al. Comparison of weight loss among named diet programs in overweight and obese adults: a meta-analysis. JAMA 2014;312:923–933 [DOI] [PubMed] [Google Scholar]
- 129. Fox CS, Golden SH, Anderson C, et al.; American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Clinical Cardiology, Council on Cardiovascular and Stroke Nursing, Council on Cardiovascular Surgery and Anesthesia, Council on Quality of Care and Outcomes Research; American Diabetes Association . Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care 2015;38:1777–1803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Schwingshackl L, Chaimani A, Hoffmann G, Schwedhelm C, Boeing H. A network meta-analysis on the comparative efficacy of different dietary approaches on glycaemic control in patients with type 2 diabetes mellitus. Eur J Epidemiol 2018;33:157–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Schwingshackl L, Schwedhelm C, Hoffmann G, et al. Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr 2017;105:1462–1473 [DOI] [PubMed] [Google Scholar]
- 132. Benson G, Hayes J. An update on the Mediterranean, vegetarian, and DASH eating patterns in people with type 2 diabetes. Diabetes Spectr 2020;33:125–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010;126:e26–e32 [DOI] [PubMed] [Google Scholar]
- 134. Esposito K, Maiorino MI, Ciotola M, et al. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med 2009;151:306–314 [DOI] [PubMed] [Google Scholar]
- 135. de Carvalho GB, Dias-Vasconcelos NL, Santos RKF, Brandão-Lima PN, da Silva DG, Pires LV. Effect of different dietary patterns on glycemic control in individuals with type 2 diabetes mellitus: a systematic review. Crit Rev Food Sci Nutr 2020;60:1999–2010 [DOI] [PubMed] [Google Scholar]
- 136. Papamichou D, Panagiotakos DB, Itsiopoulos C. Dietary patterns and management of type 2 diabetes: a systematic review of randomised clinical trials. Nutr Metab Cardiovasc Dis 2019;29:531–543 [DOI] [PubMed] [Google Scholar]
- 137. Sainsbury E, Kizirian NV, Partridge SR, Gill T, Colagiuri S, Gibson AA. Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract 2018;139:239–252 [DOI] [PubMed] [Google Scholar]
- 138. van Zuuren EJ, Fedorowicz Z, Kuijpers T, Pijl H. Effects of low-carbohydrate- compared with low-fat-diet interventions on metabolic control in people with type 2 diabetes: a systematic review including GRADE assessments. Am J Clin Nutr 2018;108:300–331 [DOI] [PubMed] [Google Scholar]
- 139. Snorgaard O, Poulsen GM, Andersen HK, Astrup A. Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res Care 2017;5:e000354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Rinaldi S, Campbell EE, Fournier J, O’Connor C, Madill J. A comprehensive review of the literature supporting recommendations from the Canadian Diabetes Association for the use of a plant-based diet for management of type 2 diabetes. Can J Diabetes 2016;40:471–477 [DOI] [PubMed] [Google Scholar]
- 141. Pawlak R. Vegetarian diets in the prevention and management of diabetes and its complications. Diabetes Spectr 2017;30:82–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Handu D, Piotrowski M. Nutrition interventions in pediatric patients with type 1 diabetes: an evidence analysis center scoping review. J Acad Nutr Diet 2021;122:424–431 [DOI] [PubMed] [Google Scholar]
- 143. Kirkpatrick CF, Bolick JP, Kris-Etherton PM, et al. Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: a scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J Clin Lipidol 2019;13:689–711.e1 [DOI] [PubMed] [Google Scholar]
- 144. Siverhus K. Low carbohydrate and very low carbohydrate eating patterns in adults with diabetes: a guide for health care providers. Arlington, VA, American Diabetes Association. Accessed 9 September 2022. Available from https://shopdiabetes.org/products/low-carbohydrate-and-very-low-carbohydrate-eating-patterns-in-adults-with-diabetes-a-guide-for-health-care-providers
- 145. Bowen ME, Cavanaugh KL, Wolff K, et al. The diabetes nutrition education study randomized controlled trial: a comparative effectiveness study of approaches to nutrition in diabetes self-management education. Patient Educ Couns 2016;99:1368–1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Truman E, Lane D, Elliott C. Defining food literacy: a scoping review. Appetite 2017;116:365–371 [DOI] [PubMed] [Google Scholar]
- 147. Food Literacy Center . What is food literacy? Accessed 31 August 2021. Available from https://www.foodliteracycenter.org/about
- 148. Jamshed H, Steger FL, Bryan DR, et al. Effectiveness of early time-restricted eating for weight loss, fat loss, and cardiometabolic health in adults with obesity: a randomized clinical trial. JAMA Intern Med 2022;182:953–962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Lowe DA, Wu N, Rohdin-Bibby L, et al. Effects of time-restricted eating on weight loss and other metabolic parameters in women and men with overweight and obesity: the TREAT randomized clinical trial. JAMA Intern Med 2020;180:1491–1499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Gabel K, Hoddy KK, Haggerty N, et al. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: a pilot study. Nutr Healthy Aging 2018;4:345–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Chow LS, Manoogian ENC, Alvear A, et al. Time-restricted eating effects on body composition and metabolic measures in humans who are overweight: a feasibility study. Obesity (Silver Spring) 2020;28:860–869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Liu D, Huang Y, Huang C, et al. Calorie restriction with or without time-restricted eating in weight loss. N Engl J Med 2022;386:1495–1504 [DOI] [PubMed] [Google Scholar]
- 153. Trepanowski JF, Kroeger CM, Barnosky A, et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern Med 2017;177:930–938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Carter S, Clifton PM, Keogh JB. Effect of intermittent compared with continuous energy restricted diet on glycemic control in patients with type 2 diabetes: a randomized noninferiority trial. JAMA Netw Open 2018;1:e180756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Overland J, Toth K, Gibson AA, et al. The safety and efficacy of weight loss via intermittent fasting or standard daily energy restriction in adults with type 1 diabetes and overweight or obesity: A pilot study. Obes Med 2018;12:13–17 [Google Scholar]
- 156. DAFNE Study Group . Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ 2002;325:746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Delahanty LM, Nathan DM, Lachin JM, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes . Association of diet with glycated hemoglobin during intensive treatment of type 1 diabetes in the Diabetes Control and Complications Trial. Am J Clin Nutr 2009;89:518–524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Zafar MI, Mills KE, Zheng J, Regmi A, Hu SQ, Gou L, et al. Low-glycemic index diets as an intervention for diabetes: a systematic review and meta-analysis. Am J Clin Nutr 2019;110:891–902 [DOI] [PubMed] [Google Scholar]
- 159. Wheeler ML, Dunbar SA, Jaacks LM, et al. Macronutrients, food groups, and eating patterns in the management of diabetes: a systematic review of the literature, 2010. Diabetes Care 2012;35:434–445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Vega-López S, Venn BJ, Slavin JL. Relevance of the glycemic index and glycemic load for body weight, diabetes, and cardiovascular disease. Nutrients 2018;10:E1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Thomas D, Elliott EJ. Low glycaemic index, or low glycaemic load, diets for diabetes mellitus. Cochrane Database Syst Rev 2009;2009:CD006296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Chiavaroli L, Lee D, Ahmed A, Cheung A, Khan TA, Blanco S, et al. Effect of low glycaemic index or load dietary patterns on glycaemic control and cardiometabolic risk factors in diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ 2021;374:n1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Meng Y, Bai H, Wang S, Li Z, Wang Q, Chen L. Efficacy of low carbohydrate diet for type 2 diabetes mellitus management: A systematic review and meta-analysis of randomized controlled trials. Diabetes Res Clin Pract 2017;131:124–131 [DOI] [PubMed] [Google Scholar]
- 164. Goldenberg JZ, Day A, Brinkworth GD, et al. Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta-analysis of published and unpublished randomized trial data. BMJ 2021;372:m4743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Lennerz BS, Koutnik AP, Azova S, Wolfsdorf JI, Ludwig DS. Carbohydrate restriction for diabetes: rediscovering centuries-old wisdom. J Clin Invest 2021;131:142246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Jayedi A, Zeraattalab-Motlagh S, Jabbarzadeh B, et al. Dose-dependent effect of carbohydrate restriction for type 2 diabetes management: a systematic review and dose-response meta-analysis of randomized controlled trials. Am J Clin Nutr 2022;116:40–56 [DOI] [PubMed] [Google Scholar]
- 167. Tay J, Luscombe-Marsh ND, Thompson CH, et al. Comparison of low- and high-carbohydrate diets for type 2 diabetes management: a randomized trial. Am J Clin Nutr 2015;102:780–790 [DOI] [PubMed] [Google Scholar]
- 168. Gardner CD, Landry MJ, Perelman D, et al. Effect of a ketogenic diet versus mediterranean diet on HbA1c in individuals with prediabetes and type 2 diabetes mellitus: the interventional keto-med randomized crossover trial. Am J Clin Nutr 2022;116:640–652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. U.S. Food and Drug Administration . FDA revises labels of SGLT2 inhibitors for diabetes to include warnings about too much acid in the blood and serious urinary tract infections. Silver Spring, MD, U.S. Food and Drug Administration. Accessed 30 August 2022. Available from https://www.fda.gov/drugs/drug-safety-and-availability/fda-revises-labels-sglt2-inhibitors-diabetes-include-warnings-about-too-much-acid-blood-and-serious
- 170. Blau JE, Tella SH, Taylor SI, Rother KI. Ketoacidosis associated with SGLT2 inhibitor treatment: analysis of FAERS data. Diabetes Metab Res Rev 2017;33: 10.1002/dmrr.2924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Cronin P, Joyce SA, O’Toole PW, O’Connor EM. Dietary fibre modulates the gut microbiota. Nutrients 2021;13:1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. U.S. Department of Agriculture and U.S. Department of Health and Human Services . Dietary guidelines for Americans 2020–2025. 9th Edition, December 2020. Accessed 19 October 2022. Available from https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
- 173. He M, van Dam RM, Rimm E, Hu FB, Qi L. Whole-grain, cereal fiber, bran, and germ intake and the risks of all-cause and cardiovascular disease-specific mortality among women with type 2 diabetes mellitus. Circulation 2010;121:2162–2168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Burger KNJ, Beulens JWJ, van der Schouw YT, et al. Dietary fiber, carbohydrate quality and quantity, and mortality risk of individuals with diabetes mellitus. PLoS One 2012;7:e43127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Partula V, Deschasaux M, Druesne-Pecollo N, Latino-Martel P, Desmetz E, Chazelas E, et al. Associations between consumption of dietary fibers and the risk of cardiovascular diseases, cancers, type 2 diabetes, and mortality in the prospective NutriNet-Santé cohort. Am J Clin Nutr 2020;112:195–207 [DOI] [PubMed] [Google Scholar]
- 176. Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet 2019;393:434–445 [DOI] [PubMed] [Google Scholar]
- 177. Hu Y, Ding M, Sampson L, et al. Intake of whole grain foods and risk of type 2 diabetes: results from three prospective cohort studies. BMJ 2020;370:m2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Nansel TR, Lipsky LM, Liu A. Greater diet quality is associated with more optimal glycemic control in a longitudinal study of youth with type 1 diabetes. Am J Clin Nutr 2016;104:81–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Katz ML, Mehta S, Nansel T, Quinn H, Lipsky LM, Laffel LMB. Associations of nutrient intake with glycemic control in youth with type 1 diabetes: differences by insulin regimen. Diabetes Technol Ther 2014;16:512–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Rossi MCE, Nicolucci A, Di Bartolo P, et al. Diabetes Interactive Diary: a new telemedicine system enabling flexible diet and insulin therapy while improving quality of life: an open-label, international, multicenter, randomized study. Diabetes Care 2010;33:109–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Laurenzi A, Bolla AM, Panigoni G, et al. Effects of carbohydrate counting on glucose control and quality of life over 24 weeks in adult patients with type 1 diabetes on continuous subcutaneous insulin infusion: a randomized, prospective clinical trial (GIOCAR). Diabetes Care 2011;34:823–827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Sämann A, Mühlhauser I, Bender R, Kloos Ch, Müller UA. Glycaemic control and severe hypoglycaemia following training in flexible, intensive insulin therapy to enable dietary freedom in people with type 1 diabetes: a prospective implementation study. Diabetologia 2005;48:1965–1970 [DOI] [PubMed] [Google Scholar]
- 183. Bell KJ, Barclay AW, Petocz P, Colagiuri S, Brand-Miller JC. Efficacy of carbohydrate counting in type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2014;2:133–140 [DOI] [PubMed] [Google Scholar]
- 184. Bell KJ, Smart CE, Steil GM, Brand-Miller JC, King B, Wolpert HA. Impact of fat, protein, and glycemic index on postprandial glucose control in type 1 diabetes: implications for intensive diabetes management in the continuous glucose monitoring era. Diabetes Care 2015;38:1008–1015 [DOI] [PubMed] [Google Scholar]
- 185. Bell KJ, Toschi E, Steil GM, Wolpert HA. Optimized mealtime insulin dosing for fat and protein in type 1 diabetes: application of a model-based approach to derive insulin doses for open-loop diabetes management. Diabetes Care 2016;39:1631–1634 [DOI] [PubMed] [Google Scholar]
- 186. Smart CEM, Evans M, O’Connell SM, et al. Both dietary protein and fat increase postprandial glucose excursions in children with type 1 diabetes, and the effect is additive. Diabetes Care 2013;36:3897–3902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Smith TA, Smart CE, Howley PP, Lopez PE, King BR. For a high fat, high protein breakfast, preprandial administration of 125% of the insulin dose improves postprandial glycaemic excursions in people with type 1 diabetes using multiple daily injections: a cross-over trial. Diabet Med 2021;38:e14512. [DOI] [PubMed] [Google Scholar]
- 188. Paterson MA, Smart CEM, Lopez PE, et al. Increasing the protein quantity in a meal results in dose-dependent effects on postprandial glucose levels in individuals with type 1 diabetes mellitus. Diabet Med 2017;34:851–854 [DOI] [PubMed] [Google Scholar]
- 189. O’Connell SM, O’Toole N, Cronin C, et al. Is the glycaemic response from fat in meals dose dependent in children and adolescents with T1DM on intensive insulin therapy? ESPE Abstracts 89 FC3.4, 2018. Accessed 19 October 2022. Available from https://abstracts.eurospe.org/hrp/0089/hrp0089fc3.4
- 190. Bell KJ, Fio CZ, Twigg S, et al. Amount and type of dietary fat, postprandial glycemia, and insulin requirements in type 1 diabetes: a randomized within-subject trial. Diabetes Care 2020;43:59–66 [DOI] [PubMed] [Google Scholar]
- 191. Furthner D, Lukas A, Schneider AM, et al. The role of protein and fat intake on insulin therapy in glycaemic control of paediatric type 1 diabetes: a systematic review and research gaps. Nutrients 2021;13:3558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Metwally M, Cheung TO, Smith R, Bell KJ. Insulin pump dosing strategies for meals varying in fat, protein or glycaemic index or grazing-style meals in type 1 diabetes: a systematic review. Diabetes Res Clin Pract 2021;172:108516. [DOI] [PubMed] [Google Scholar]
- 193. Campbell MD, Walker M, King D, et al. Carbohydrate counting at meal time followed by a small secondary postprandial bolus injection at 3 hours prevents late hyperglycemia, without hypoglycemia, after a high-carbohydrate, high-fat meal in type 1 diabetes. Diabetes Care 2016;39:e141–e142 [DOI] [PubMed] [Google Scholar]
- 194. Angelopoulos T, Kokkinos A, Liaskos C, et al. The effect of slow spaced eating on hunger and satiety in overweight and obese patients with type 2 diabetes mellitus. BMJ Open Diabetes Res Care 2014;2:e000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Tuttle KR, Bakris GL, Bilous RW, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Diabetes Care 2014;37:2864–2883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet 2014;383:1999–2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Pan Y, Guo LL, Jin HM. Low-protein diet for diabetic nephropathy: a meta-analysis of randomized controlled trials. Am J Clin Nutr 2008;88:660–666 [DOI] [PubMed] [Google Scholar]
- 198. Robertson L, Waugh N, Robertson A. Protein restriction for diabetic renal disease. Cochrane Database Syst Rev 2007;4:CD002181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Layman DK, Clifton P, Gannon MC, Krauss RM, Nuttall FQ. Protein in optimal health: heart disease and type 2 diabetes. Am J Clin Nutr 2008;87:1571S–1575S [DOI] [PubMed] [Google Scholar]
- 200. Ros E. Dietary cis-monounsaturated fatty acids and metabolic control in type 2 diabetes. Am J Clin Nutr 2003;78(Suppl.):617S–625S [DOI] [PubMed] [Google Scholar]
- 201. Forouhi NG, Imamura F, Sharp SJ, et al. Association of plasma phospholipid n-3 and n-6 polyunsaturated fatty acids with type 2 diabetes: the EPIC-InterAct case-cohort study. PLoS Med 2016;13:e1002094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Wang DD, Li Y, Chiuve SE, et al. Association of specific dietary fats with total and cause-specific mortality. JAMA Intern Med 2016;176:1134–1145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Brehm BJ, Lattin BL, Summer SS, et al. One-year comparison of a high-monounsaturated fat diet with a high-carbohydrate diet in type 2 diabetes. Diabetes Care 2009;32:215–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Shai I, Schwarzfuchs D, Henkin Y, et al.; Dietary Intervention Randomized Controlled Trial (DIRECT) Group . Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med 2008;359:229–241 [DOI] [PubMed] [Google Scholar]
- 205. Brunerova L, Smejkalova V, Potockova J, Andel M. A comparison of the influence of a high-fat diet enriched in monounsaturated fatty acids and conventional diet on weight loss and metabolic parameters in obese non-diabetic and type 2 diabetic patients. Diabet Med 2007;24:533–540 [DOI] [PubMed] [Google Scholar]
- 206. Bloomfield HE, Koeller E, Greer N, MacDonald R, Kane R, Wilt TJ. Effects on health outcomes of a Mediterranean diet with no restriction on fat intake: a systematic review and meta-analysis. Ann Intern Med 2016;165:491–500 [DOI] [PubMed] [Google Scholar]
- 207. Sacks FM, Lichtenstein AH, Wu JHY, et al.; American Heart Association . Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation 2017;136:e1–e23 [DOI] [PubMed] [Google Scholar]
- 208. Jacobson TA, Maki KC, Orringer CE, et al.; NLA Expert Panel . National lipid association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipid 2015;9:S1–S122.e1 [DOI] [PubMed] [Google Scholar]
- 209. Holman RR, Paul S, Farmer A, Tucker L, Stratton IM; Atorvastatin in Factorial with Omega-3 EE90 Risk Reduction in Diabetes Study Group . Atorvastatin in Factorial with Omega-3 EE90 Risk Reduction in Diabetes (AFORRD): a randomised controlled trial. Diabetologia 2009;52:50–59 [DOI] [PubMed] [Google Scholar]
- 210. Bosch J, Gerstein HC, Dagenais GR, et al.; ORIGIN Trial Investigators . n-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. N Engl J Med 2012;367:309–318 [DOI] [PubMed] [Google Scholar]
- 211. Brown TJ, Brainard J, Song F, Wang X, Abdelhamid A, Hooper L, et al. Omega-3, omega-6, and total dietary polyunsaturated fat for prevention and treatment of type 2 diabetes mellitus: systematic review and meta-analysis of randomised controlled trials. BMJ 2019;366:l4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. ASCEND Study Collaborative Group, Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, et al. Effects of n-3 fatty acid supplements in diabetes mellitus. N Engl J Med 2018;379:1540–1550 [DOI] [PubMed] [Google Scholar]
- 213. Bhatt DL, Steg PG, Miller M, et al.; REDUCE-IT Investigators . Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med 2019;380:11–22 [DOI] [PubMed] [Google Scholar]
- 214. Thomas MC, Moran J, Forsblom C, et al.; FinnDiane Study Group . The association between dietary sodium intake, ESRD, and all-cause mortality in patients with type 1 diabetes. Diabetes Care 2011;34:861–866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Ekinci EI, Clarke S, Thomas MC, et al. Dietary salt intake and mortality in patients with type 2 diabetes. Diabetes Care 2011;34:703–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Lennon SL, DellaValle DM, Rodder SG, et al. 2015 Evidence analysis library evidence-based nutrition practice guideline for the management of hypertension in adults. J Acad Nutr Diet 2017;117:1445–1458.e17 [DOI] [PubMed] [Google Scholar]
- 217. Maillot M, Drewnowski A. A conflict between nutritionally adequate diets and meeting the 2010 dietary guidelines for sodium. Am J Prev Med 2012;42:174–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Aroda VR, Edelstein SL, Goldberg RB, et al.; Diabetes Prevention Program Research Group . Long-term metformin use and vitamin B12 deficiency in the Diabetes Prevention Program Outcomes Study. J Clin Endocrinol Metab 2016;101:1754–1761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Mangione CM, Barry MJ, Nicholson WK, et al.; US Preventive Services Task Force . Vitamin, mineral, and multivitamin supplementation to prevent cardiovascular disease and cancer: US Preventive Services Task Force recommendation statement. JAMA 2022;327:2326–2333 [DOI] [PubMed] [Google Scholar]
- 220. Allen RW, Schwartzman E, Baker WL, Coleman CI, Phung OJ. Cinnamon use in type 2 diabetes: an updated systematic review and meta-analysis. Ann Fam Med 2013;11:452–459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Mitri J, Pittas AG. Vitamin D and diabetes. Endocrinol Metab Clin North Am 2014;43:205–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation 2016;133:187–225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Pittas AG, Dawson-Hughes B, Sheehan P, et al.; D2d Research Group . Vitamin D supplementation and prevention of type 2 diabetes. N Engl J Med 2019;381:520–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Dawson-Hughes B, Staten MA, Knowler WC, et al.; D2d Research Group . Intratrial exposure to vitamin D and new-onset diabetes among adults with prediabetes: a secondary analysis from the Vitamin D and Type 2 Diabetes (D2d) study. Diabetes Care 2020;43:2916–2922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Zhang Y, Tan H, Tang J, et al. Effects of vitamin D supplementation on prevention of type 2 diabetes in patients with prediabetes: a systematic review and meta-analysis. Diabetes Care 2020;43:1650–1658 [DOI] [PubMed] [Google Scholar]
- 226. Barbarawi M, Zayed Y, Barbarawi O, et al. Effect of vitamin D supplementation on the incidence of diabetes mellitus. J Clin Endocrinol Metab 2020;105:dgaa335. [DOI] [PubMed] [Google Scholar]
- 227. National Agricultural Library, U.S. Department of Agriculture . Nutritive and nonnutritive sweetener resources. Accessed 19 October 2022. Available from https://www.nal.usda.gov/human-nutrition-and-food-safety/food-composition/sweeteners
- 228. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;140:e596–e646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Johnson RK, Lichtenstein AH, Anderson CAM, et al.; American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Quality of Care and Outcomes Research; Stroke Council . Low-calorie sweetened beverages and cardiometabolic health: a science advisory from the American Heart Association. Circulation 2018;138:e126–e140 [DOI] [PubMed] [Google Scholar]
- 230. Grotz VL, Pi-Sunyer X, Porte D Jr, Roberts A, Richard Trout J. A 12-week randomized clinical trial investigating the potential for sucralose to affect glucose homeostasis. Regul Toxicol Pharmacol 2017;88:22–33 [DOI] [PubMed] [Google Scholar]
- 231. Lohner S, Kuellenberg de Gaudry D, Toews I, Ferenci T, Meerpohl JJ. Non-nutritive sweeteners for diabetes mellitus. Cochrane Database Syst Rev 2020;5:CD012885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Sylvetsky AC, Chandran A, Talegawkar SA, Welsh JA, Drews K, El Ghormli L. Consumption of beverages containing low-calorie sweeteners, diet, and cardiometabolic health in youth with type 2 diabetes. J Acad Nutr Diet 2020;120:1348–1358.e6 [DOI] [PubMed] [Google Scholar]
- 233. Miller PE, Perez V. Low-calorie sweeteners and body weight and composition: a meta-analysis of randomized controlled trials and prospective cohort studies. Am J Clin Nutr 2014;100:765–777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Rogers PJ, Hogenkamp PS, de Graaf C, et al. Does low-energy sweetener consumption affect energy intake and body weight? A systematic review, including meta-analyses, of the evidence from human and animal studies. Int J Obes 2016;40:381–394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Laviada-Molina H, Molina-Segui F, Pérez-Gaxiola G, et al. Effects of nonnutritive sweeteners on body weight and BMI in diverse clinical contexts: systematic review and meta-analysis. Obes Rev 2020;21:e13020. [DOI] [PubMed] [Google Scholar]
- 236. Azad MB, Abou-Setta AM, Chauhan BF, et al. Nonnutritive sweeteners and cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. CMAJ 2017;189:E929–E939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Lee JJ, Khan TA, McGlynn N, et al. Relation of change or substitution of low- and no-calorie sweetened beverages with cardiometabolic outcomes: a systematic review and meta-analysis of prospective cohort studies. Diabetes Care 2022;45:1917–1930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238. Mattes RD, Popkin BM. Nonnutritive sweetener consumption in humans: effects on appetite and food intake and their putative mechanisms. Am J Clin Nutr 2009;89:1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. McGlynn ND, Khan TA, Wang L, et al. Association of low- and no-calorie sweetened beverages as a replacement for sugar-sweetened beverages with body weight and cardiometabolic risk: a systematic review and meta-analysis. JAMA Netw Open 2022;5:e222092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. 2018 Physical Activity Guidelines Advisory Committee . 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC, U.S. Department of Health and Human Services, 2018 [Google Scholar]
- 241. Bazargan-Hejazi S, Arroyo JS, Hsia S, Brojeni NR, Pan D. A racial comparison of differences between self-reported and objectively measured physical activity among US adults with diabetes. Ethn Dis 2017;27:403–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242. Khunti K, Griffin S, Brennan A, et al. Behavioural interventions to promote physical activity in a multiethnic population at high risk of diabetes: PROPELS three-arm RCT. Health Technol Assess 2021;25:1–190 [DOI] [PubMed] [Google Scholar]
- 243. Bootwong P, Intarut N. The effects of text messages for promoting physical activities in prediabetes: a randomized controlled trial. Telemed J E Health 2022;28:896–903 [DOI] [PubMed] [Google Scholar]
- 244. Sluik D, Buijsse B, Muckelbauer R, et al. Physical activity and mortality in individuals with diabetes mellitus: a prospective study and meta-analysis. Arch Intern Med 2012;172:1285–1295 [DOI] [PubMed] [Google Scholar]
- 245. Tikkanen-Dolenc H, Wadén J, Forsblom C, et al.; FinnDiane Study Group . Physical activity reduces risk of premature mortality in patients with type 1 diabetes with and without kidney disease. Diabetes Care 2017;40:1727–1732 [DOI] [PubMed] [Google Scholar]
- 246. Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA 2001;286:1218–1227 [DOI] [PubMed] [Google Scholar]
- 247. Peters AL, Laffel L (Eds.). American Diabetes Association/JDRF Type 1 Diabetes Sourcebook. Alexandria, VA, American Diabetes Association, 2013 [Google Scholar]
- 248. Ostman C, Jewiss D, King N, Smart NA. Clinical outcomes to exercise training in type 1 diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract 2018;139:380–391 [DOI] [PubMed] [Google Scholar]
- 249. Boulé NG, Kenny GP, Haddad E, Wells GA, Sigal RJ. Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in type 2 diabetes mellitus. Diabetologia 2003;46:1071–1081 [DOI] [PubMed] [Google Scholar]
- 250. Pandey A, Patel KV, Bahnson JL, et al.; Look AHEAD Research Group . Association of intensive lifestyle intervention, fitness, and body mass index with risk of heart failure in overweight or obese adults with type 2 diabetes mellitus: an analysis from the Look AHEAD Trial. Circulation 2020;141:1295–1306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251. Rejeski WJ, Ip EH, Bertoni AG, et al.; Look AHEAD Research Group . Lifestyle change and mobility in obese adults with type 2 diabetes. N Engl J Med 2012;366:1209–1217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care 2016;39:2065–2079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253. Frediani JK, Bienvenida AF, Li J, Higgins MK, Lobelo F. Physical fitness and activity changes after a 24-week soccer-based adaptation of the U.S diabetes prevention program intervention in Hispanic men. Prog Cardiovasc Dis 2020;63:775–785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 2010;7:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255. Riddell MC, Gallen IW, Smart CE, et al. Exercise management in type 1 diabetes: a consensus statement. Lancet Diabetes Endocrinol 2017;5:377–390 [DOI] [PubMed] [Google Scholar]
- 256. Anderson BJ, Laffel LM, Domenger C, et al. Factors associated with diabetes-specific health-related quality of life in youth with type 1 diabetes: the Global TEENs Study. Diabetes Care 2017;40:1002–1009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257. Adolfsson P, Riddell MC, Taplin CE, et al. ISPAD Clinical Practice Consensus Guidelines 2018: exercise in children and adolescents with diabetes. Pediatr Diabetes 2018;19(Suppl. 27):205–226 [DOI] [PubMed] [Google Scholar]
- 258. Jelleyman C, Yates T, O’Donovan G, et al. The effects of high-intensity interval training on glucose regulation and insulin resistance: a meta-analysis. Obes Rev 2015;16:942–961 [DOI] [PubMed] [Google Scholar]
- 259. Little JP, Gillen JB, Percival ME, et al. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J Appl Physiol 2011;111:1554–1560 [DOI] [PubMed] [Google Scholar]
- 260. Bohn B, Herbst A, Pfeifer M, et al.; DPV Initiative . Impact of physical activity on glycemic control and prevalence of cardiovascular risk factors in adults with type 1 diabetes: a cross-sectional multicenter study of 18,028 patients. Diabetes Care 2015;38:1536–1543 [DOI] [PubMed] [Google Scholar]
- 261. U.S. Department of Health and Human Services . Physical Activity Guidelines for Americans, 2nd ed. Accessed 19 October 2022. Available from https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf
- 262. Willey KA, Singh MAF. Battling insulin resistance in elderly obese people with type 2 diabetes: bring on the heavy weights. Diabetes Care 2003;26:1580–1588 [DOI] [PubMed] [Google Scholar]
- 263. Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc 2009;41:998–1005 [DOI] [PubMed] [Google Scholar]
- 264. Dempsey PC, Larsen RN, Sethi P, et al. Benefits for type 2 diabetes of interrupting prolonged sitting with brief bouts of light walking or simple resistance activities. Diabetes Care 2016;39:964–972 [DOI] [PubMed] [Google Scholar]
- 265. Wang Y, Lee DC, Brellenthin AG, et al. Leisure-time running reduces the risk of incident type 2 diabetes. Am J Med 2019;132:1225–1232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266. Schellenberg ES, Dryden DM, Vandermeer B, Ha C, Korownyk C. Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med 2013;159:543–551 [DOI] [PubMed] [Google Scholar]
- 267. Pai LW, Li TC, Hwu YJ, Chang SC, Chen LL, Chang PY. The effectiveness of regular leisure-time physical activities on long-term glycemic control in people with type 2 diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract 2016;113:77–85 [DOI] [PubMed] [Google Scholar]
- 268. Cui J, Yan JH, Yan LM, Pan L, Le JJ, Guo YZ. Effects of yoga in adults with type 2 diabetes mellitus: a meta-analysis. J Diabetes Investig 2017;8:201–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. Lee MS, Jun JH, Lim HJ, Lim HS. A systematic review and meta-analysis of tai chi for treating type 2 diabetes. Maturitas 2015;80:14–23 [DOI] [PubMed] [Google Scholar]
- 270. Rees JL, Johnson ST, Boulé NG. Aquatic exercise for adults with type 2 diabetes: a meta-analysis. Acta Diabetol 2017;54:895–904 [DOI] [PubMed] [Google Scholar]
- 271. Church TS, Blair SN, Cocreham S, et al. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial. JAMA 2010;304:2253–2262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272. Kanaley JA, Colberg SR, Corcoran MH, et al. Exercise/physical activity in individuals with type 2 diabetes: a consensus statement from the American College of Sports Medicine. Med Sci Sports Exerc 2022;54:353–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Bax JJ, Young LH, Frye RL, Bonow RO, Steinberg HO; ADA . Screening for coronary artery disease in patients with diabetes. Diabetes Care 2007;30:2729–2736 [DOI] [PubMed] [Google Scholar]
- 274. Colberg SR. Exercise and Diabetes: A Clinician’s Guide to Prescribing Physical Activity. 1st ed. Alexandria, VA, American Diabetes Association, 2013 [Google Scholar]
- 275. Lemaster JW, Reiber GE, Smith DG, Heagerty PJ, Wallace C. Daily weight-bearing activity does not increase the risk of diabetic foot ulcers. Med Sci Sports Exerc 2003;35:1093–1099 [DOI] [PubMed] [Google Scholar]
- 276. Smith AG, Russell J, Feldman EL, et al. Lifestyle intervention for pre-diabetic neuropathy. Diabetes Care 2006;29:1294–1299 [DOI] [PubMed] [Google Scholar]
- 277. Spallone V, Ziegler D, Freeman R, et al.; Toronto Consensus Panel on Diabetic Neuropathy . Cardiovascular autonomic neuropathy in diabetes: clinical impact, assessment, diagnosis, and management. Diabetes Metab Res Rev 2011;27:639–653 [DOI] [PubMed] [Google Scholar]
- 278. Pop-Busui R, Evans GW, Gerstein HC, et al.; Action to Control Cardiovascular Risk in Diabetes Study Group . Effects of cardiac autonomic dysfunction on mortality risk in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Diabetes Care 2010;33:1578–1584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279. Suarez L, Barrett-Connor E. Interaction between cigarette smoking and diabetes mellitus in the prediction of death attributed to cardiovascular disease. Am J Epidemiol 1984;120:670–675 [DOI] [PubMed] [Google Scholar]
- 280. Stanton CA, Keith DR, Gaalema DE, et al. Trends in tobacco use among US adults with chronic health conditions: National Survey on Drug Use and Health 2005-2013. Prev Med 2016;92:160–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Bae J. Differences in cigarette use behaviors by age at the time of diagnosis with diabetes from young adulthood to adulthood: results from the National Longitudinal Study of Adolescent Health. J Prev Med Public Health 2013;46:249–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282. Śliwińska-Mossoń M, Milnerowicz H. The impact of smoking on the development of diabetes and its complications. Diab Vasc Dis Res 2017;14:265–276 [DOI] [PubMed] [Google Scholar]
- 283. Kar D, Gillies C, Zaccardi F, Webb D, Seidu S, Tesfaye S, et al. Relationship of cardiometabolic parameters in non-smokers, current smokers, and quitters in diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol 2016;15:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284. Pan A, Wang Y, Talaei M, Hu FB. Relation of smoking with total mortality and cardiovascular events among patients with diabetes mellitus: a meta-analysis and systematic review. Circulation 2015;132:1795–1804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285. Jankowich M, Choudhary G, Taveira TH, Wu WC. Age-, race-, and gender-specific prevalence of diabetes among smokers. Diabetes Res Clin Pract 2011;93:e101–e105 [DOI] [PubMed] [Google Scholar]
- 286. Akter S, Goto A, Mizoue T. Smoking and the risk of type 2 diabetes in Japan: a systematic review and meta-analysis. J Epidemiol 2017;27:553–561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287. Liu X, Bragg F, Yang L, et al.; China Kadoorie Biobank Collaborative Group . Smoking and smoking cessation in relation to risk of diabetes in Chinese men and women: a 9-year prospective study of 0·5 million people. Lancet Public Health 2018;3:e167–e176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288. Tonstad S, Lawrence D. Varenicline in smokers with diabetes: a pooled analysis of 15 randomized, placebo-controlled studies of varenicline. J Diabetes Investig 2017;8:93–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289. West R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol Health 2017;32:1018–1036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290. Ranney L, Melvin C, Lux L, McClain E, Lohr KN. Systematic review: smoking cessation intervention strategies for adults and adults in special populations. Ann Intern Med 2006;145:845–856 [DOI] [PubMed] [Google Scholar]
- 291. Tian J, Venn A, Otahal P, Gall S. The association between quitting smoking and weight gain: a systematic review and meta-analysis of prospective cohort studies. Obes Rev 2015;16:883–901 [DOI] [PubMed] [Google Scholar]
- 292. Clair C, Rigotti NA, Porneala B, et al. Association of smoking cessation and weight change with cardiovascular disease among adults with and without diabetes. JAMA 2013;309:1014–1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293. Voulgari C, Katsilambros N, Tentolouris N. Smoking cessation predicts amelioration of microalbuminuria in newly diagnosed type 2 diabetes mellitus: a 1-year prospective study. Metabolism 2011;60:1456–1464 [DOI] [PubMed] [Google Scholar]
- 294. Huerta TR, Walker DM, Mullen D, Johnson TJ, Ford EW. Trends in E-cigarette awareness and perceived harmfulness in the U.S. Am J Prev Med 2017;52:339–346 [DOI] [PubMed] [Google Scholar]
- 295. Pericot-Valverde I, Gaalema DE, Priest JS, Higgins ST. E-cigarette awareness, perceived harmfulness, and ever use among U.S. adults. Prev Med 2017;104:92–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Centers for Disease Control and Prevention . Smoking & tobacco use: outbreak of lung injury associated with e-cigarette use, or vaping, products. Accessed 19 October 2022. Available from https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html
- 297. Reid RD, Malcolm J, Wooding E, et al. Prospective, cluster-randomized trial to implement the Ottawa model for smoking cessation in diabetes education programs in Ontario, Canada. Diabetes Care 2018;41:406–412 [DOI] [PubMed] [Google Scholar]
- 298. Hood KK, Peterson CM, Rohan JM, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics 2009;124:e1171–e1179 [DOI] [PubMed] [Google Scholar]
- 299. Asche C, LaFleur J, Conner C. A review of diabetes treatment adherence and the association with clinical and economic outcomes. Clin Ther 2011;33:74–109 [DOI] [PubMed] [Google Scholar]
- 300. Hood KK, Rohan JM, Peterson CM, Drotar D. Interventions with adherence-promoting components in pediatric type 1 diabetes: meta-analysis of their impact on glycemic control. Diabetes Care 2010;33:1658–1664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301. Hilliard ME, Powell PW, Anderson BJ. Evidence-based behavioral interventions to promote diabetes management in children, adolescents, and families. Am Psychol 2016;71:590–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302. Hood KK, Hilliard M, Piatt G, Ievers-Landis CE. Effective strategies for encouraging behavior change in people with diabetes. Diabetes Manag (Lond) 2015;5:499–510 [PMC free article] [PubMed] [Google Scholar]
- 303. Berhe KK, Gebru HB, Kahsay HB. Effect of motivational interviewing intervention on HgbA1C and depression in people with type 2 diabetes mellitus (systematic review and meta-analysis). PLoS One 2020;15:e0240839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304. Powell PW, Hilliard ME, Anderson BJ. Motivational interviewing to promote adherence behaviors in pediatric type 1 diabetes. Curr Diab Rep 2014;14:531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305. Liang W, Lo SHS, Tola YO, Chow KM. The effectiveness of self-management programmes for people with type 2 diabetes receiving insulin injection: a systematic review and meta-analysis. Int J Clin Pract 2021;75:e14636. [DOI] [PubMed] [Google Scholar]
- 306. Almutairi N, Hosseinzadeh H, Gopaldasani V. The effectiveness of patient activation intervention on type 2 diabetes mellitus glycemic control and self-management behaviors: a systematic review of RCTs. Prim Care Diabetes 2020;14:12–20 [DOI] [PubMed] [Google Scholar]
- 307. Rosales CB, Denman CA, Bell ML, et al. Meta Salud Diabetes for cardiovascular disease prevention in Mexico: a cluster-randomized behavioural clinical trial. Int J Epidemiol 2021;50:1272–1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308. Gray KE, Hoerster KD, Taylor L, Krieger J, Nelson KM. Improvements in physical activity and some dietary behaviors in a community health worker-led diabetes self-management intervention for adults with low incomes: results from a randomized controlled trial. Transl Behav Med 2021;11:2144–2154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309. Van Rhoon L, Byrne M, Morrissey E, Murphy J, McSharry J. A systematic review of the behaviour change techniques and digital features in technology-driven type 2 diabetes prevention interventions. Digit Health 2020;6:2055207620914427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310. Fitzpatrick SL, Schumann KP, Hill-Briggs F. Problem solving interventions for diabetes self-management and control: a systematic review of the literature. Diabetes Res Clin Pract 2013;100:145–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311. Avery L, Flynn D, van Wersch A, Sniehotta FF, Trenell MI. Changing physical activity behavior in type 2 diabetes: a systematic review and meta-analysis of behavioral interventions. Diabetes Care 2012;35:2681–2689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312. Nicolucci A, Haxhi J, D’Errico V, et al.; Italian Diabetes and Exercise Study 2 (IDES_2) Investigators . Effect of a behavioural intervention for adoption and maintenance of a physically active lifestyle on psychological well-being and quality of life in patients with type 2 diabetes: the IDES_2 randomized clinical trial. Sports Med 2022;52:643–654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313. Crowley MJ, Tarkington PE, Bosworth HB, et al. Effect of a comprehensive telehealth intervention vs telemonitoring and care coordination in patients with persistently poor type 2 diabetes control: a randomized clinical trial. JAMA Intern Med 2022;182:943–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314. Kichler JC, Harris MA, Weissberg-Benchell J. Contemporary roles of the pediatric psychologist in diabetes care. Curr Diabetes Rev 2015;11:210–221 [DOI] [PubMed] [Google Scholar]
- 315. Harris MA, Freeman KA, Duke DC. Seeing is believing: using skype to improve diabetes outcomes in youth. Diabetes Care 2015;38:1427–1434 [DOI] [PubMed] [Google Scholar]
- 316. Naicker K, Johnson JA, Skogen JC, et al. Type 2 diabetes and comorbid symptoms of depression and anxiety: longitudinal associations with mortality risk. Diabetes Care 2017;40:352–358 [DOI] [PubMed] [Google Scholar]
- 317. de Groot M, Golden SH, Wagner J. Psychological conditions in adults with diabetes. Am Psychol 2016;71:552–562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318. Anderson RJ, Grigsby AB, Freedland KE, et al. Anxiety and poor glycemic control: a meta-analytic review of the literature. Int J Psychiatry Med 2002;32:235–247 [DOI] [PubMed] [Google Scholar]
- 319. Delahanty LM, Grant RW, Wittenberg E, et al. Association of diabetes-related emotional distress with diabetes treatment in primary care patients with type 2 diabetes. Diabet Med 2007;24:48–54 [DOI] [PubMed] [Google Scholar]
- 320. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 2001;24:1069–1078 [DOI] [PubMed] [Google Scholar]
- 321. Nicolucci A, Kovacs Burns K, Holt RIG, et al.; DAWN2 Study Group . Diabetes Attitudes, Wishes and Needs second study (DAWN2): cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet Med 2013;30:767–777 [DOI] [PubMed] [Google Scholar]
- 322. Ducat L, Philipson LH, Anderson BJ. The mental health comorbidities of diabetes. JAMA 2014;312:691–692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323. Guerrero Fernández de Alba I, Gimeno-Miguel A, Poblador-Plou B, et al. Association between mental health comorbidity and health outcomes in type 2 diabetes mellitus patients. Sci Rep 2020;10:19583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324. Gonzalvo JD, Hamm J, Eaves S, et al. A practical approach to mental health for the diabetes educator. AADE Pract 2019;7:29–44 [Google Scholar]
- 325. Robinson DJ, Coons M, Haensel H, Vallis M; Diabetes Canada Clinical Practice Guidelines Expert Committee . Diabetes and mental health. Can J Diabetes 2018;42(Suppl. 1):S130–S141 [DOI] [PubMed] [Google Scholar]
- 326. Cho MK, Kim MY. Self-management nursing intervention for controlling glucose among diabetes: a systematic review and meta-analysis. Int J Environ Res Public Health 2021;18:12750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327. Majidi S, Reid MW, Fogel J, et al. Psychosocial outcomes in young adolescents with type 1 diabetes participating in shared medical appointments. Pediatr Diabetes 2021;22:787–795 [DOI] [PubMed] [Google Scholar]
- 328. Diaz Bustamante L, Ghattas KN, Ilyas S, Al-Refai R, Maharjan R, Khan S. Does treatment for depression with collaborative care improve the glycemic levels in diabetic patients with depression? A systematic review. Cureus 2020;12:e10551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329. Phillips S, Culpepper J, Welch M, et al. A multidisciplinary diabetes clinic improves clinical and behavioral outcomes in a primary care setting. J Am Board Fam Med 2021;34:579–589 [DOI] [PubMed] [Google Scholar]
- 330. Xu C, Dong Z, Zhang P, et al. Effect of group cognitive behavioural therapy on psychological stress and blood glucose in people with type 2 diabetes mellitus: a community-based cluster randomized controlled trial in China. Diabet Med 2021;38:e14491. [DOI] [PubMed] [Google Scholar]
- 331. Ali MK, Chwastiak L, Poongothai S, et al.; INDEPENDENT Study Group . Effect of a collaborative care model on depressive symptoms and glycated hemoglobin, blood pressure, and serum cholesterol among patients with depression and diabetes in India: the INDEPENDENT randomized clinical trial. JAMA 2020;324:651–662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332. Rechenberg K, Koerner R. Cognitive behavioral therapy in adolescents with type 1 diabetes: an integrative review. J Pediatr Nurs 2021;60:190–197 [DOI] [PubMed] [Google Scholar]
- 333. McMorrow R, Hunter B, Hendrieckx C, et al. Effect of routinely assessing and addressing depression and diabetes distress on clinical outcomes among adults with type 2 diabetes: a systematic review. BMJ Open 2022;12:e054650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334. Harkness E, Macdonald W, Valderas J, Coventry P, Gask L, Bower P. Identifying psychosocial interventions that improve both physical and mental health in patients with diabetes: a systematic review and meta-analysis. Diabetes Care 2010;33:926–930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335. Radcliff TA, Côté MJ, Whittington MD, et al. Cost-effectiveness of three doses of a behavioral intervention to prevent or delay type 2 diabetes in rural areas. J Acad Nutr Diet 2020;120:1163–1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336. T1D Exchange . Depression screening change package. Accessed 10 September 2022. Available from https://t1dexchange.org/depression-screening-change-package/
- 337. Mulvaney SA, Mara CA, Kichler JC, et al. A retrospective multisite examination of depression screening practices, scores, and correlates in pediatric diabetes care. Transl Behav Med 2021;11:122–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338. Monaghan M, Mara CA, Kichler JC, et al. Multisite examination of depression screening scores and correlates among adolescents and young adults with type 2 diabetes. Can J Diabetes 2021;45:411–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339. Watson SE, Spurling SE, Fieldhouse AM, Montgomery VL, Wintergerst KA. Depression and anxiety screening in adolescents with diabetes. Clin Pediatr (Phila) 2020;59:445–449 [DOI] [PubMed] [Google Scholar]
- 340. Brodar KE, Davis EM, Lynn C, et al. Comprehensive psychosocial screening in a pediatric diabetes clinic. Pediatr Diabetes 2021;22:656–666 [DOI] [PubMed] [Google Scholar]
- 341. Weissberg-Benchell J, Shapiro JB. A review of interventions aimed at facilitating successful transition planning and transfer to adult care among youth with chronic illness. Pediatr Ann 2017;46:e182–e187 [DOI] [PubMed] [Google Scholar]
- 342. O’Gurek DT, Henke C. A practical approach to screening for social determinants of health. Fam Pract Manag 2018;25:7–12 [PubMed] [Google Scholar]
- 343. Zhang H, Zhang Q, Luo D, et al. The effect of family-based intervention for adults with diabetes on HbA1c and other health-related outcomes: systematic review and meta-analysis. J Clin Nurs 2022;31:1488–1501 [DOI] [PubMed] [Google Scholar]
- 344. McBroom LA, Enriquez M. Review of family-centered interventions to enhance the health outcomes of children with type 1 diabetes. Diabetes Educ 2009;35:428–438 [DOI] [PubMed] [Google Scholar]
- 345. Oyedeji AD, Ullah I, Weich S, Bentall R, Booth A. Effectiveness of non-specialist delivered psychological interventions on glycemic control and mental health problems in individuals with type 2 diabetes: a systematic review and meta-analysis. Int J Ment Health Syst 2022;16:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346. Chen SM, Lin HS, Atherton JJ, MacIsaac RJ, Wu CJJ. Effect of a mindfulness programme for long-term care residents with type 2 diabetes: a cluster randomised controlled trial measuring outcomes of glycaemic control, relocation stress and depression. Int J Older People Nurs 2020;15:e12312. [DOI] [PubMed] [Google Scholar]
- 347. Beverly EA, Hultgren BA, Brooks KM, Ritholz MD, Abrahamson MJ, Weinger K. Understanding physicians’ challenges when treating type 2 diabetic patients’ social and emotional difficulties: a qualitative study. Diabetes Care 2011;34:1086–1088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348. Li Y, Storch EA, Ferguson S, Li L, Buys N, Sun J. The efficacy of cognitive behavioral therapy-based intervention on patients with diabetes: a meta-analysis. Diabetes Res Clin Pract 2022;189:109965. [DOI] [PubMed] [Google Scholar]
- 349. Vlachou E, Ntikoudi A, Owens DA, Nikolakopoulou M, Chalimourdas T, Cauli O. Effectiveness of cognitive behavioral therapy-based interventions on psychological symptoms in adults with type 2 diabetes mellitus: an update review of randomized controlled trials. J Diabetes Complications 2022;36:108185. [DOI] [PubMed] [Google Scholar]
- 350. Nikkhah Ravari O, Mousavi SZ, Babak A. Evaluation of the effects of 12 weeks mindfulness-based stress reduction on glycemic control and mental health indices in women with diabetes mellitus type 2. Adv Biomed Res 2020;9:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351. Ni YX, Ma L, Li JP. Effects of mindfulness-based intervention on glycemic control and psychological outcomes in people with diabetes: a systematic review and meta-analysis. J Diabetes Investig 2021;12:1092–1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352. Hood KK, Iturralde E, Rausch J, Weissberg-Benchell J. Preventing diabetes distress in adolescents with type 1 diabetes: results 1 year after participation in the STePS Program. Diabetes Care 2018;41:1623–1630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353. Weissberg-Benchell J, Shapiro JB, Bryant FB, Hood KK. Supporting Teen Problem-Solving (STEPS) 3 year outcomes: preventing diabetes-specific emotional distress and depressive symptoms in adolescents with type 1 diabetes. J Consult Clin Psychol 2020;88:1019–1031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354. Laffel LMB, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr 2003;142:409–416 [DOI] [PubMed] [Google Scholar]
- 355. Wysocki T, Harris MA, Buckloh LM, et al. Effects of behavioral family systems therapy for diabetes on adolescents’ family relationships, treatment adherence, and metabolic control. J Pediatr Psychol 2006;31:928–938 [DOI] [PubMed] [Google Scholar]
- 356. Yap JM, Tantono N, Wu VX, Klainin-Yobas P. Effectiveness of technology-based psychosocial interventions on diabetes distress and health-relevant outcomes among type 2 diabetes mellitus: a systematic review and meta-analysis. J Telemed Telecare 26 November 2021 [Epub ahead of print]. DOI: 10.1177/1357633X211058329 [DOI] [PubMed] [Google Scholar]
- 357. Bisno DI, Reid MW, Fogel JL, Pyatak EA, Majidi S, Raymond JK. Virtual Group Appointments Reduce Distress and Improve Care Management in Young Adults with Type 1 Diabetes. J Diabetes Sci Technol 2021;30:19322968211035768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358. Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful? Establishing cut points for the Diabetes Distress Scale. Diabetes Care 2012;35:259–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359. Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care 2010;33:1034–1036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360. Hagger V, Hendrieckx C, Sturt J, Skinner TC, Speight J. Diabetes distress among adolescents with type 1 diabetes: a systematic review. Curr Diab Rep 2016;16:9. [DOI] [PubMed] [Google Scholar]
- 361. Wasserman RM, Eshtehardi SS, Anderson BJ, Weissberg-Benchell JA, Hilliard ME. Profiles of depressive symptoms and diabetes distress in preadolescents with type 1 diabetes. Can J Diabetes 2021;45:436–443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362. Aikens JE. Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care 2012;35:2472–2478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363. Liu X, Haagsma J, Sijbrands E, et al. Anxiety and depression in diabetes care: longitudinal associations with health-related quality of life. Sci Rep 2020;10:8307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364. Snoek FJ, Bremmer MA, Hermanns N. Constructs of depression and distress in diabetes: time for an appraisal. Lancet Diabetes Endocrinol 2015;3:450–460 [DOI] [PubMed] [Google Scholar]
- 365. Sturt J, Dennick K, Hessler D, Hunter BM, Oliver J, Fisher L. Effective interventions for reducing diabetes distress: systematic review and meta-analysis. International Diabetes Nursing. 2015;12:40–55 [Google Scholar]
- 366. Ngan HY, Chong YY, Chien WT. Effects of mindfulness- and acceptance-based interventions on diabetes distress and glycaemic level in people with type 2 diabetes: systematic review and meta-analysis. Diabet Med 2021;38:e14525. [DOI] [PubMed] [Google Scholar]
- 367. Presley C, Agne A, Shelton T, Oster R, Cherrington A. Mobile-enhanced peer support for African Americans with type 2 diabetes: a randomized controlled trial. J Gen Intern Med 2020;35:2889–2896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368. Fisher L, Skaff MM, Mullan JT, et al. Clinical depression versus distress among patients with type 2 diabetes: not just a question of semantics. Diabetes Care 2007;30:542–548 [DOI] [PubMed] [Google Scholar]
- 369. Fisher L, Hessler D, Polonsky WH, et al. T1-REDEEM: a randomized controlled trial to reduce diabetes distress among adults with type 1 diabetes. Diabetes Care 2018;41:1862–1869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370. DiNardo MM, Greco C, Phares AD, et al. Effects of an integrated mindfulness intervention for veterans with diabetes distress: a randomized controlled trial. BMJ Open Diabetes Res Care 2022;10:e002631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371. Lutes LD, Cummings DM, Littlewood K, et al. A tailored cognitive-behavioural intervention produces comparable reductions in regimen-related distress in adults with type 2 diabetes regardless of insulin use: 12-month outcomes from the COMRADE trial. Can J Diabetes 2020;44:530–536 [DOI] [PubMed] [Google Scholar]
- 372. Friis AM, Johnson MH, Cutfield RG, Consedine NS. Kindness matters: a randomized controlled trial of a mindful self-compassion intervention improves depression, distress, and HbA1c among patients with diabetes. Diabetes Care 2016;39:1963–1971 [DOI] [PubMed] [Google Scholar]
- 373. Smith KJ, Béland M, Clyde M, et al. Association of diabetes with anxiety: a systematic review and meta-analysis. J Psychosom Res 2013;74:89–99 [DOI] [PubMed] [Google Scholar]
- 374. Li C, Barker L, Ford ES, Zhang X, Strine TW, Mokdad AH. Diabetes and anxiety in US adults: findings from the 2006 Behavioral Risk Factor Surveillance System. Diabet Med 2008;25:878–881 [DOI] [PubMed] [Google Scholar]
- 375. Cox DJ, Irvine A, Gonder-Frederick L, Nowacek G, Butterfield J. Fear of hypoglycemia: quantification, validation, and utilization. Diabetes Care 1987;10:617–621 [DOI] [PubMed] [Google Scholar]
- 376. Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder-Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: implications for diabetes management and patient education. Patient Educ Couns 2007;68:10–15 [DOI] [PubMed] [Google Scholar]
- 377. Zambanini A, Newson RB, Maisey M, Feher MD. Injection related anxiety in insulin-treated diabetes. Diabetes Res Clin Pract 1999;46:239–246 [DOI] [PubMed] [Google Scholar]
- 378. American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013 [Google Scholar]
- 379. Mitsonis C, Dimopoulos N, Psarra V. P01-138 Clinical implications of anxiety in diabetes: a critical review of the evidence base. Eur Psychiatry 2009;24:S526 [Google Scholar]
- 380. Kemp CG, Johnson LCM, Sagar R, et al. Effect of a collaborative care model on anxiety symptoms among patients with depression and diabetes in India: the INDEPENDENT randomized clinical trial. Gen Hosp Psychiatry 2022;74:39–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381. Yeoh E, Choudhary P, Nwokolo M, Ayis S, Amiel SA. Interventions that restore awareness of hypoglycemia in adults with type 1 diabetes: a systematic review and meta-analysis. Diabetes Care 2015;38:1592–1609 [DOI] [PubMed] [Google Scholar]
- 382. Cox DJ, Gonder-Frederick L, Polonsky W, Schlundt D, Kovatchev B, Clarke W. Blood glucose awareness training (BGAT-2): long-term benefits. Diabetes Care 2001;24:637–642 [DOI] [PubMed] [Google Scholar]
- 383. Gonder-Frederick LA, Schmidt KM, Vajda KA, et al. Psychometric properties of the hypoglycemia fear survey-ii for adults with type 1 diabetes. Diabetes Care 2011;34:801–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384. Cox DJ, Kovatchev B, Koev D, et al. Hypoglycemia anticipation, awareness and treatment training (HAATT) reduces occurrence of severe hypoglycemia among adults with type 1 diabetes mellitus. Int J Behav Med 2004;11:212–218 [DOI] [PubMed] [Google Scholar]
- 385. Lamounier RN, Geloneze B, Leite SO, et al.; HAT Brazil study group . Hypoglycemia incidence and awareness among insulin-treated patients with diabetes: the HAT study in Brazil. Diabetol Metab Syndr 2018;10:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386. Amiel SA, Potts L, Goldsmith K, et al. A parallel randomised controlled trial of the Hypoglycaemia Awareness Restoration Programme for adults with type 1 diabetes and problematic hypoglycaemia despite optimised self-care (HARPdoc). Nat Commun 2022;13:2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387. Lustman PJ, Griffith LS, Clouse RE. Depression in adults with diabetes. Results of 5-yr follow-up study. Diabetes Care 1988;11:605–612 [DOI] [PubMed] [Google Scholar]
- 388. de Groot M, Crick KA, Long M, Saha C, Shubrook JH. Lifetime duration of depressive disorders in patients with type 2 diabetes. Diabetes Care 2016;39:2174–2181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389. Rubin RR, Ma Y, Marrero DG, et al.; Diabetes Prevention Program Research Group . Elevated depression symptoms, antidepressant medicine use, and risk of developing diabetes during the diabetes prevention program. Diabetes Care 2008;31:420–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390. Clouse RE, Lustman PJ, Freedland KE, Griffith LS, McGill JB, Carney RM. Depression and coronary heart disease in women with diabetes. Psychosom Med 2003;65:376–383 [DOI] [PubMed] [Google Scholar]
- 391. Vassilopoulos A, Nicholl M, Wolf RM, Slifer KJ, Cirincione L. Discrepancies in assessing symptoms of depression in adolescents with diabetes using the patient health questionnaire and semi-structured interviews. Diabetes Spectr 2020;33:339–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392. Katon WJ, Von Korff M, Lin EHB, et al. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry 2004;61:1042–1049 [DOI] [PubMed] [Google Scholar]
- 393. Cannon A, Handelsman Y, Heile M, Shannon M. Burden of illness in type 2 diabetes mellitus. J Manag Care Spec Pharm 2018;24(Suppl.):S5–S13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394. Atlantis E, Fahey P, Foster J. Collaborative care for comorbid depression and diabetes: a systematic review and meta-analysis. BMJ Open 2014;4:e004706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395. van der Feltz-Cornelis C, Allen SF, Holt RIG, Roberts R, Nouwen A, Sartorius N. Treatment for comorbid depressive disorder or subthreshold depression in diabetes mellitus: systematic review and meta-analysis. Brain Behav 2021;11:e01981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396. Lu X, Yang D, Liang J, et al. Effectiveness of intervention program on the change of glycaemic control in diabetes with depression patients: a meta-analysis of randomized controlled studies. Prim Care Diabetes 2021;15:428–434 [DOI] [PubMed] [Google Scholar]
- 397. Varela-Moreno E, Carreira Soler M, Guzmán-Parra J, Jódar-Sánchez F, Mayoral-Cleries F, Anarte-Ortíz MT. Effectiveness of eHealth-based psychological interventions for depression treatment in patients with type 1 or type 2 diabetes mellitus: a systematic review. Front Psychol 2022;12:746217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398. Mohammad Rahimi GR, Aminzadeh R, Azimkhani A, Saatchian V. The effect of exercise interventions to improve psychosocial aspects and glycemic control in type 2 diabetic patients: a systematic review and meta-analysis of randomized controlled trials. Biol Res Nurs 2022;24:10–23 [DOI] [PubMed] [Google Scholar]
- 399. Pinhas-Hamiel O, Hamiel U, Levy-Shraga Y. Eating disorders in adolescents with type 1 diabetes: challenges in diagnosis and treatment. World J Diabetes 2015;6:517–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400. Papelbaum M, Appolinário JC, Moreira R de O, Ellinger VCM, Kupfer R, Coutinho WF. Prevalence of eating disorders and psychiatric comorbidity in a clinical sample of type 2 diabetes mellitus patients. Rev Bras Psiquiatr 2005;27:135–138 [DOI] [PubMed] [Google Scholar]
- 401. Young-Hyman DL, Davis CL. Disordered eating behavior in individuals with diabetes: importance of context, evaluation, and classification. Diabetes Care 2010;33:683–689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402. Pinhas-Hamiel O, Hamiel U, Greenfield Y, et al. Detecting intentional insulin omission for weight loss in girls with type 1 diabetes mellitus. Int J Eat Disord 2013;46:819–825 [DOI] [PubMed] [Google Scholar]
- 403. Goebel-Fabbri AE, Fikkan J, Franko DL, Pearson K, Anderson BJ, Weinger K. Insulin restriction and associated morbidity and mortality in women with type 1 diabetes. Diabetes Care 2008;31:415–419 [DOI] [PubMed] [Google Scholar]
- 404. Weinger K, Beverly EA. Barriers to achieving glycemic targets: who omits insulin and why? Diabetes Care 2010;33:450–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405. Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry 2007;61:348–358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406. Martyn-Nemeth P, Quinn L, Hacker E, Park H, Kujath AS. Diabetes distress may adversely affect the eating styles of women with type 1 diabetes. Acta Diabetol 2014;51:683–686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407. Pursey KM, Hart M, Jenkins L, McEvoy M, Smart CE. Screening and identification of disordered eating in people with type 1 diabetes: a systematic review. J Diabetes Complications 2020;34:107522. [DOI] [PubMed] [Google Scholar]
- 408. Peterson CM, Fischer S, Young-Hyman D. Topical review: a comprehensive risk model for disordered eating in youth with type 1 diabetes. J Pediatr Psychol 2015;40:385–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409. Zaremba N, Watson A, Kan C, et al. Multidisciplinary healthcare teams’ challenges and strategies in supporting people with type 1 diabetes to recover from disordered eating. Diabet Med 2020;37:1992–2000 [DOI] [PubMed] [Google Scholar]
- 410. Banting R, Randle-Phillips C. A systematic review of psychological interventions for comorbid type 1 diabetes mellitus and eating disorders. Diabetes Manag (Lond) 2018;8:1–18 [Google Scholar]
- 411. Priesterroth L, Grammes J, Clauter M, Kubiak T. Diabetes technologies in people with type 1 diabetes mellitus and disordered eating: A systematic review on continuous subcutaneous insulin infusion, continuous glucose monitoring and automated insulin delivery. Diabet Med 2021;38:e14581. [DOI] [PubMed] [Google Scholar]
- 412. Hansson L, Zanchetti A, Carruthers SG, et al.; HOT Study Group . Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet 1998;351:1755–1762 [DOI] [PubMed] [Google Scholar]
- 413. van Bloemendaal L, IJzerman RG, Ten Kulve JS, et al. GLP-1 receptor activation modulates appetite- and reward-related brain areas in humans. Diabetes 2014;63:4186–4196 [DOI] [PubMed] [Google Scholar]
- 414. Devarajooh C, Chinna K. Depression, distress and self-efficacy: the impact on diabetes self-care practices. PLoS One 2017;12:e0175096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415. Suvisaari J, Perälä J, Saarni SI, et al. Type 2 diabetes among persons with schizophrenia and other psychotic disorders in a general population survey. Eur Arch Psychiatry Clin Neurosci 2008;258:129–136 [DOI] [PubMed] [Google Scholar]
- 416. Mulligan K, McBain H, Lamontagne-Godwin F, et al. Barriers to effective diabetes management–a survey of people with severe mental illness. BMC Psychiatry 2018;18:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417. Schnitzer K, Cather C, Zvonar V, et al. Patient experience and predictors of improvement in a group behavioral and educational intervention for individuals with diabetes and serious mental illness: mixed methods case study. J Particip Med 2021;13:e21934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418. Koro CE, Fedder DO, L’Italien GJ, et al. Assessment of independent effect of olanzapine and risperidone on risk of diabetes among patients with schizophrenia: population based nested case-control study. BMJ 2002;325:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419. American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity . Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care 2004;27:596–601 [DOI] [PubMed] [Google Scholar]
- 420. Holt RIG. Association between antipsychotic medication use and diabetes. Curr Diab Rep 2019;19:96–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421. Kruse J, Schmitz N; German National Health Interview and Examination Survey . On the association between diabetes and mental disorders in a community sample: results from the German National Health Interview and Examination Survey. Diabetes Care 2003;26:1841–1846 [DOI] [PubMed] [Google Scholar]
- 422. Biessels GJ, Whitmer RA. Cognitive dysfunction in diabetes: how to implement emerging guidelines. Diabetologia 2020;63:3–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423. Brands AMA, Biessels GJ, de Haan EHF, Kappelle LJ, Kessels RPC. The effects of type 1 diabetes on cognitive performance: a meta-analysis. Diabetes Care 2005;28:726–735 [DOI] [PubMed] [Google Scholar]
- 424. Carmichael OT, Neiberg RH, Dutton GR, et al. Long-term change in physiological markers and cognitive performance in type 2 diabetes: the Look AHEAD Study. J Clin Endocrinol Metab 2020;105:dgaa591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425. Avila JC, Mejia-Arangom S, Jupiter D, Downer B, Wong R. The effect of diabetes on the cognitive trajectory of older adults in Mexico and the United States. J Gerontol B Psychol Sci Soc Sci 2021;76:e153–e164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426. Munshi MN. Cognitive dysfunction in older adults with diabetes: what a clinician needs to know. Diabetes Care 2017;40:461–467 [DOI] [PubMed] [Google Scholar]
- 427. Biessels GJ, Despa F. Cognitive decline and dementia in diabetes mellitus: mechanisms and clinical implications. Nat Rev Endocrinol 2018;14:591–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428. Feinkohl I, Aung PP, Keller M, et al.; Edinburgh Type 2 Diabetes Study (ET2DS) Investigators . Severe hypoglycemia and cognitive decline in older people with type 2 diabetes: the Edinburgh type 2 diabetes study. Diabetes Care 2014;37:507–515 [DOI] [PubMed] [Google Scholar]
- 429. Strudwick SK, Carne C, Gardiner J, Foster JK, Davis EA, Jones TW. Cognitive functioning in children with early onset type 1 diabetes and severe hypoglycemia. J Pediatr 2005;147:680–685 [DOI] [PubMed] [Google Scholar]
- 430. Anothaisintawee T, Reutrakul S, Van Cauter E, Thakkinstian A. Sleep disturbances compared to traditional risk factors for diabetes development: Systematic review and meta-analysis. Sleep Med Rev 2016;30:11–24 [DOI] [PubMed] [Google Scholar]
- 431. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 2010;33:414–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432. Zhu B, Shi C, Park CG, Reutrakul S. Sleep quality and gestational diabetes in pregnant women: a systematic review and meta-analysis. Sleep Med 2020;67:47–55 [DOI] [PubMed] [Google Scholar]
- 433. Zhang X, Zhang R, Cheng L, et al. The effect of sleep impairment on gestational diabetes mellitus: a systematic review and meta-analysis of cohort studies. Sleep Med 2020;74:267–277 [DOI] [PubMed] [Google Scholar]
- 434. Lee SWH, Ng KY, Chin WK. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: a systematic review and meta-analysis. Sleep Med Rev 2017;31:91–101 [DOI] [PubMed] [Google Scholar]
- 435. Barone MTU, Menna-Barreto L. Diabetes and sleep: a complex cause-and-effect relationship. Diabetes Res Clin Pract 2011;91:129–137 [DOI] [PubMed] [Google Scholar]
- 436. Reutrakul S, Thakkinstian A, Anothaisintawee T, et al. Sleep characteristics in type 1 diabetes and associations with glycemic control: systematic review and meta-analysis. Sleep Med 2016;23:26–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437. Ji X, Wang Y, Saylor J. Sleep and type 1 diabetes mellitus management among children, adolescents, and emerging young adults: a systematic review. J Pediatr Nurs 2021;61:245–253 [DOI] [PubMed] [Google Scholar]
- 438. Perez KM, Hamburger ER, Lyttle M, et al. Sleep in type 1 diabetes: implications for glycemic control and diabetes management. Curr Diab Rep 2018;18:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439. Schipper SBJ, Van Veen MM, Elders PJM, et al. Sleep disorders in people with type 2 diabetes and associated health outcomes: a review of the literature. Diabetologia 2021;64:2367–2377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440. Reutrakul S, Mokhlesi B. Obstructive sleep apnea and diabetes: a state of the art review. Chest 2017;152:1070–1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441. Denic-Roberts H, Costacou T, Orchard TJ. Subjective sleep disturbances and glycemic control in adults with long-standing type 1 diabetes: The Pittsburgh’s Epidemiology of Diabetes Complications study. Diabetes Res Clin Pract 2016;119:1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442. Ogilvie RP, Patel SR. The epidemiology of sleep and diabetes. Curr Diab Rep 2018;18:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443. Tan X, van Egmond L, Chapman CD, Cedernaes J, Benedict C. Aiding sleep in type 2 diabetes: therapeutic considerations. Lancet Diabetes Endocrinol 2018;6:60–68 [DOI] [PubMed] [Google Scholar]
- 444. Carreon SA, Cao VT, Anderson BJ, Thompson DI, Marrero DG, Hilliard ME. ‘I don’t sleep through the night’: qualitative study of sleep in type 1 diabetes. Diabet Med 2022;39:e14763. [DOI] [PubMed] [Google Scholar]
- 445. Kothari V, Cardona Z, Chirakalwasan N, Anothaisintawee T, Reutrakul S. Sleep interventions and glucose metabolism: systematic review and meta-analysis. Sleep Med 2021;78:24–35 [DOI] [PubMed] [Google Scholar]