Abstract
Tooth number abnormality is one of the most common dental developmental diseases, which includes both tooth agenesis and supernumerary teeth. Tooth development is regulated by numerous developmental signals, such as the well-known Wnt, BMP, FGF, Shh and Eda pathways, which mediate the ongoing complex interactions between epithelium and mesenchyme. Abnormal expression of these crutial signalling during this process may eventually lead to the development of anomalies in tooth number; however, the underlying mechanisms remain elusive. In this review, we summarized the major process of tooth development, the latest progress of mechanism studies and newly reported clinical investigations of tooth number abnormality. In addition, potential treatment approaches for tooth number abnormality based on developmental biology are also discussed. This review not only provides a reference for the diagnosis and treatment of tooth number abnormality in clinical practice but also facilitates the translation of basic research to the clinical application.
Subject terms: Disease genetics, Tissue engineering, Stem cells, Experimental organisms, Mesenchymal stem cells
Introduction
Dental anomalies are characterised by abnormalities in the number, size, structure or shape of the teeth. Tooth number abnormality is a common human dental anomaly, including supernumerary teeth and tooth agenesis. Supernumerary teeth are defined as teeth that develop in addition to the regular number of teeth, including odontoma.1 Their prevalence varies from region to region and is between 0.2% and 5.3%.2 The maxillary anterior region is the most common site where a supernumerary tooth occurs. Tooth agenesis is the congenital absence of a tooth owing to the developmental arrest of the corresponding tooth germ,3 and its prevalence ranges from 1.6% to 6.9%.4 Congenital absence of mandibular incisors is the most common deciduous tooth agenesis. Tooth agenesis in the permanent dentition is common in the lateral incisors and second premolars. These two diseases cannot be treated with clinical intervention because their aetiology remains unclear.
The mouse is one of the most conventional animals used for exploring the intricate aetiology of tooth number abnormality, considering that the basic process of tooth development is similar among all jawed vertebrates. In the past decades, various mouse models have been used to study the causes of tooth number abnormality. The aetiologies of both supernumerary teeth and tooth agenesis are associated with mechanisms that govern tooth development, which have been extensively investigated from morphological, molecular and cellular perspectives. Development of tooth germ requires signalling centres and a series of events.5–11 Any minor change in signalling pathway molecules during the early stage of tooth development may lead to variations in tooth number. To understand the detailed underlying mechanisms, we summarised the developmental process and mouse models related to tooth number abnormality.
Considerable progress has been achieved in clinical studies on tooth number abnormality. Some clinical studies suggest that tooth number abnormality can contribute to the diagnosis of some important systemic diseases (such as related syndromes and tumours).12–14 Compared with the extended diagnostic significance, new advances in treatment are more noteworthy. Supernumerary teeth can provide postpartum stem cells,15 which can be used to relieve the symptoms of hepatic fibrosis and systemic lupus erythematosus.16,17 As a developmental biology-based treatment approach, genetic intervention has been used to treat tooth agenesis and supernumerary teeth in mouse models.18–20 Tissue engineering for whole-tooth regeneration is a promising therapeutic strategy for tooth agenesis and has been extensively investigated in mice, pigs and other animal models.21,22
In this review, we first summarised the basic research findings on tooth development, which can help to understand the mechanisms underlying tooth number abnormality. Subsequently, we summarised key clinical studies of tooth number abnormality, introduced the biological mechanisms study models of tooth number abnormality, and prospected novel treatment strategies.
Process of tooth development
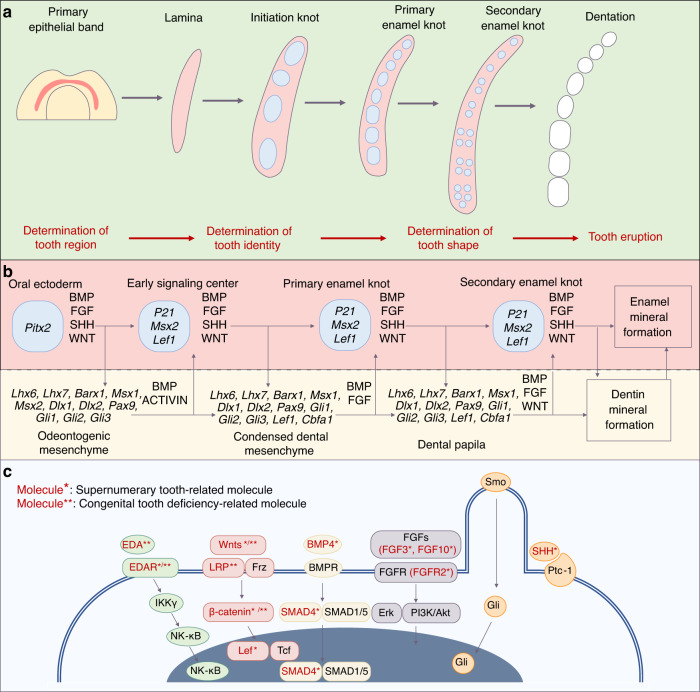
Mammalian odontogenic processes are similar, and the signals involved are conserved.23 Tooth development in both humans and mice is regulated by several signalling centres involving multiple transcription factors and signalling pathways24 (Fig. 1). The primary epithelial band, which is characteristic of the initiation of tooth development, develops to dentition through many processes. Before tooth eruption, these processes are involved in determination of its region, identity and shape25 (Fig. 1).
Fig. 1.
Tooth development process and summary of key odontogenic signal pathways. a The development process from primary epithelial band to dentation. b Molecules and signal pathways involved in tooth development. c Five key odontogenic signal pathways and related molecules involved in tooth number abnormality
Tooth region determination
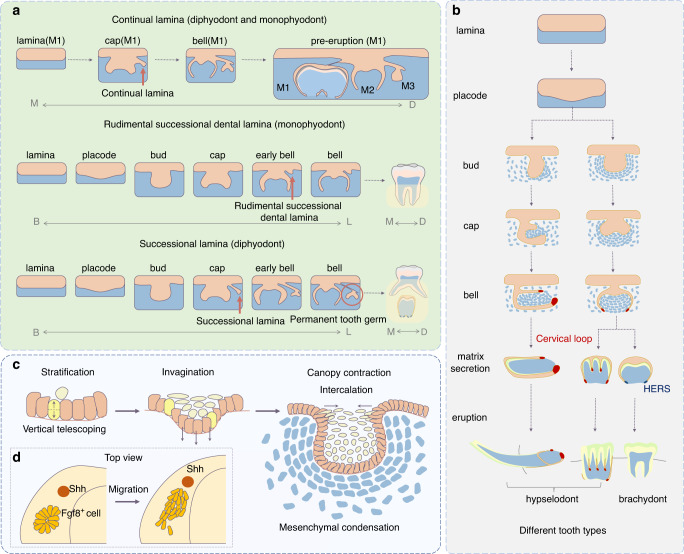
The human tooth germ originates from ectoderm based on the interaction between the original oral epithelium and ectomesenchyme derived from the neural crest. At approximately 4 weeks of gestation, the epithelium begins assuming odontogenic (tooth-forming) capacity and proliferates to form a continuous U-shaped band called the primary epithelial band. The formation of this band signifies the initiation of tooth development. As the embryo develops, the band extends into the underlying mesenchyme and gradually forms two branches: the dental and vestibular laminae. The dental lamina is the source of subsequent activity and differentiation relative to tooth development, whose expansion may lead to the development of supernumerary teeth.26 It can be classified as continual and successional laminae. The continual lamina horizontally forms from the posterior extension of the dental lamina,27 whereas the successional lamina vertically forms from the lingual side of the dental lamina. The successional lamina eventually forms a second dentition (permanent dentition) by disconnecting from the oral epithelium through apoptosis and epithelial-to-mesenchymal transition28 (Fig. 4a). A few monophyodonts, such as mice, possess the rudimental successional dental lamina, which is similar to the human successional lamina but disappears after birth owing to cell proliferation cessation29 and connective tissue and capillary invasion in the dental stalk30 (Fig. 2a).
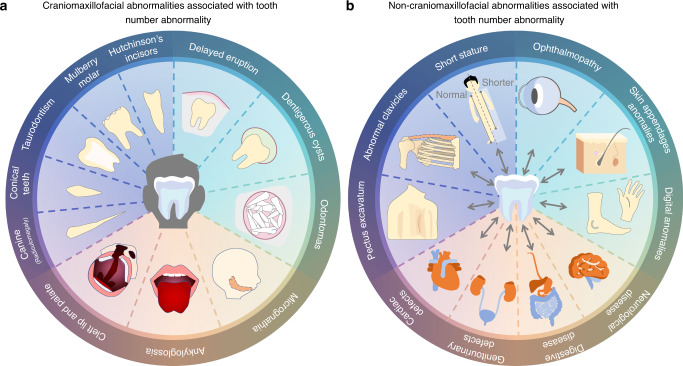
Fig. 4.
Human diseases connected with tooth number abnormalities. a Craniomaxillofacial abnormalities associated with tooth number abnormality. b Non-craniomaxillofacial abnormalities associated with tooth number abnormality
Fig. 2.
Schematic of tooth development process. a The continual lamina is present in diphyodonts and monophyodonts. The rudimental successional dental lamina cannot develop into a tooth under normal conditions, whereas the successional lamina forms the second dentition in diphyodonts. The dotted arrow indicates that a few parts of the tooth developmental process are omitted. B: buccal; L: lingual; M: mesial; D: distal; M1: first molar; M2: second molar; M3: third molar. b Different tooth types are classified according to the clinical crown-to-root ratio and the self-renewal ability after eruption. c Cell behaviour during early tooth development. Yellow cells form the suprabasal cells (light yellow) via asymmetric division; orange cells undergo vertical expansion. Grey–blue mesenchymal cells condense around the epithelium. d Top view of the migration of Fgf8+ epithelium in the lower jaw
The formation of lamina from the primary epithelial band is a complex process, which is accompanied by the expression of many odontogenic transcription factors. Pitx20, Foxi3, Dlx2, Lef1 and p63 are specifically expressed in the dental lamina.10,11 Early tooth development relies on the proper expression of these factors. Pitx2 is among the earliest markers of tooth development, such as Lef1, and interacts with β-catenin.31 Pitx2, Lef1 and Sox2 can participate in the transcriptional mechanism to regulate the steady state of dental epithelial stem cells (EpSCs)32 and formation of dental signalling centres.33 Sox2 can inhibit the transcriptional activity of Pitx2 to repress the activation of Lef1 promoter by Pitx2–Lef1.33,34 Pitx2 deficiency, in turn, delays the invagination of both dental epithelium and vestibular lamina, with reduced Shh expression.33 p63 is crucial for the formation of the dental lamina. A gene regulatory network dominated by p63, which can regulate the adhesion, polarity and migration of odontogenic cells, may exist during the determination period of the dental-forming region.35 Deficiencies of these transcription factors (Pitx2, Lef1 and P63) inhibit early tooth development, consequently leading to missing teeth.33,36–40
The developmental stage subsequent to the laminal stage is the placode stage (Fig. 2b). The formation of all epidermal appendages, including teeth, begins with the placode stage, and the formation of placodes signifies initiation of the formation of individual tooth.10 Cellular behaviours during early tooth development include cell migration, intercalation and condensation.6–9 Abnormalities in these behaviours can affect the number of teeth. From the top view, a cluster of Fgf8+ dental epithelial cells appear to be arranged in a rosette formation. As the embryo develops, these cells migrate to the mesial Shh signalling centre (possibly the initiation knot [IK]) and form a placode.7 From the sectional view, complex cellular behaviour is observed. Epithelial monolayer columnar cells migrate upward relative to their adjacent central cells, with their apex protruding toward the centre. This process is known as vertical telescoping.8 Simultaneously, the FGF signalling-dependent division of perpendicular cells produces suprabasal cells to stratify the epithelium. Subsequently, Shh signalling triggers the rearrangement of cells in the tissue, driving an epithelial invagination9 (Fig. 2c). However, epithelial evagination owing to the perturbation of Wnt signalling results in the formation of supernumerary teeth.41
Tooth identity determination
The bud stage subsequent to the placode stage is important for the determination of tooth identity. As the placode develops, suprabasal cells located at the canopy horizontally intercalate and centripetally migrate, pushing the epithelium to embed in the mesenchyme while narrowing the tooth germ neck. This process, known as canopy contraction, contributes to the gradual transformation of the epithelium into a bud shape.42 Subsequently, mesenchymal cells respond to FGF8 and SEMA3F secreted by the epithelium to condensate around the bud-shaped epithelium with increasing collagen VI expression. This process induces the mesenchyme to express odontogenic transcription factors (Pax9 and Msx1) by inhibiting the mechanical signalling molecule Rho A43–45 (Fig. 2c). During this process, the odontogenesis potential and tooth identity information are transferred from the epithelium to mesenchyme, with mesenchymal condensation and expression of specific odontogenic molecules.46–50
Recently, it was found that a few epithelial cells condensate to form a signalling centre known as IK, which sends signals to neighbouring cells, thereby inducing proliferation to complete the placode-to-bud transition.51 IK is silenced via apoptosis at the bud stage.5,52 IK with specific Eda and NFkB signalling was originally observed in the incisors, and its size affects the incisor germ size.53 The molar IK has high expression of Wnt and Shh, and interference of IK formation via physical ablation or Wnt signal confusion can prevent the development of the tooth germ.5
Tooth shape determination
After the determination of tooth identity, different types of tooth germ begin to show morphological differences. Different types of teeth form their unique shapes during this process, which is difficult to achieve in tissue-engineered tooth regeneration. Compared with the previous two stages, the possibility of developing tooth number abnormalities is reduced; however, tooth agenesis may occur owing to the arrest of tooth germ development in the cap or bell stage.32,54
The process of tooth shape determination includes the bud, cap and bell stages (Fig. 2b). The morphological features of teeth are predominantly controlled by signal centres known as enamel knots (EKs) during tooth shape determination. Single-cusp teeth (e.g., incisors) only possess primary EKs (pEKs), whereas poly-cusp teeth (e.g., molars) possess two signal centres, namely, pEKs and secondary EKs (sEKs). In the late bud stage of the molars, a group of apoptotic cells is concentrated at the tip of the tooth bud, with the expression of p21.55 P21+ cells, which are insensitive to proliferative signals, congregate in the basal layer of the epithelial centre, forming a pEK.56 Various signals regulate pEK formation during the late bud stage. Sufu inhibition in the mesenchyme or Gpr177 deletion in the epithelium can lead to the failed formation of a functional pEK, which further results in developmental retardation or arrest of the tooth germ.54,57 Subsequently, the molar tooth germ forms a new signal centre (sEK) during the cap-to-bell transition. The molar anterior buccal sEK, the first sEK, is derived from the pEK.58 and consists of non-proliferating cells consistent with the pEK, whereas the second sEK established through de novo signalling contains dividing cells.59 All sEKs are located in the inner enamel epithelial region where the tooth cusps initiate.60
Clinical studies of tooth number abnormalities
Tooth number abnormalities are common dental disease in humans. They can occur alone or accompanied by other diseases. For non-syndromic tooth number abnormalities, the general treatment could achieve satisfactory results. Whereas syndromic tooth number abnormalities require specific treatment strategies tailored to an individual’s complications or related symptoms.
Clinical feature and treatment strategies of supernumerary tooth
The occurrence features of supernumerary teeth lacks a uniform description. Study findings vary from region to region, possibly owing to sample differences.61 For instance, the incidence of supernumerary teeth is ~0.05% in Japanese children and ~3.2% in Mexicans.62,63 With respect to sex, several studies have reported that men have a higher risk of developing supernumerary teeth.61,64,65 Additionally, the preferred sites for the occurrence of supernumerary teeth may be sex-related.66 However, a few studies have reported that the incidence of supernumerary teeth does not significantly differ between men and women.67,68
Treatment strategies for supernumerary teeth are improved constantly. The general treatment option for non-syndromic supernumerary teeth is extraction. Additionally, surgical intervention is required in patients with complications or related syndromes.69–71 However, if supernumerary teeth are functionally and aesthetically significant and there is a loss of permanent teeth in the dentition, supernumerary teeth in the dentition can be considered replacement teeth.72
Clinical feature and treatment strategies of tooth agenesis
Tooth agenesis can occur as an isolated disease (non-syndromic tooth agenesis) or can be associated with a syndrome (syndromic tooth agenesis). Several syndromes, including Down syndrome, ectodermal dysplasia and labio-palatal cleft have been associated with severe or moderate tooth agenesis.3 Varied missing teeth sites are found in different syndromes. The common missing tooth site in patients with Down syndrome is the second premolar of the left lower jaw, whereas patients with a cleft lip are more likely to have missing superior incisors.73,74
Tooth agenesis can be definitively diagnosed via imaging; however, the treatment options cannot be generalised because tooth agenesis is often associated with alterations and deformities in the tooth structure, delayed eruption and tooth displacement. For instance, patients with tooth agenesis caused by Wnt10B mutation may also have microdontia and taurodontism.75 In patients with tooth agenesis caused by Pax9 mutations, the middle incisors in the upper jaw are susceptible to microdontia,76 and regional odontodysplasia may also occur.77 In addition, tooth agenesis may affect the oral arch length, jaw position and craniofacial morphological features.78,79 Therefore, imaging is necessary for early diagnosis, prompt intervention80 and multidisciplinary treatment to maintain the aesthetic and functional features of teeth.
Pathogenetic mechanisms of tooth number abnormality
The different occurrence features and related symptoms hint at the complex mechanisms of tooth number abnormality. However, the exact pathogenesis is still unclear. To explore it, many related mouse models have been constructed in laboratories (Table 1, Table 2). Based on the research progress, the appropriate stimulation of signalling pathways are the keys to determining the number of teeth. A few minor disturbances can inhibit development of the tooth germ or lead to the formation of supernumerary teeth.13,27,81
Table 1.
Mouse models of supernumerary tooth
| Pathway | Mouse model | Phenotype | Reference |
|---|---|---|---|
| Wnt | R-spondin2−/− | Mesiodistal supernumerary teeth in the diastema region | 96 |
| K14-Cre8Brn; Apccko/cko | Numerous supernumerary teeth surrounded the principal teeth | 88 | |
| Fgf8CreER; Ctnnb1Δex3fl/+ | Numerous supernumerary teeth surrounded the principal teeth | 41 | |
| K14-Cre Ctnnb1(Ex3) fl/+ | Numerous supernumerary teeth surrounded the principal teeth | 89,90 | |
| Wise−/− | Supernumerary teeth in the incisor, molar, and diastema regions | 93,94 | |
| Lrp4−/− | Supernumerary teeth in the incisor and molar regions | 92 | |
| Wise−/−, Lrp5−/− | Supernumerary teeth in the incisor and diastema regions | 93 | |
| Wise−/−, Lrp5+/− | Supernumerary teeth in the incisor and diastema regions | 93 | |
| Wise−/−, Lrp5+/−, Lrp6+/− | Mesiodistal supernumerary teeth in the diastema regions | 93 | |
| Wnt10a−/− | Mesiodistal supernumerary teeth (M4) in the molar region | 97 | |
| FGF | Spry2−/− | Mesiodistal supernumerary teeth in the diastema region | 112,113 |
| Spry2+/−Spry4−/− | Supernumerary teeth in the incisor region | 184 | |
| Spry4−/− | Mesiodistal supernumerary teeth in the diastema region | 112 | |
| K14-Cre; R26R-fgf8 | Buccolingual supernumerary teeth in the incisor and molar regions | 185 | |
| Shh | Gas1−/− | Mesiodistal supernumerary teeth in the diastema region | 103,186 |
| Wnt1-Cre; Polarisflox/flox | Mesiodistal supernumerary teeth in the diastema region | 186 | |
| PCS1-MRCS1Δ/Δ | Mesiodistal supernumerary teeth in the diastema region | 101 | |
| ΔMRCS1/ΔMRCS1 | Mesiodistal supernumerary teeth in the diastema region | 102 | |
| ΔMRCS1/Shh KO | Mesiodistal supernumerary teeth in the diastema region | 102 | |
| Injection of 5E1 (at E12) * | Mesiodistal supernumerary teeth in the diastema region | 105 | |
| Injection of 5E1 (at E14) * | Buccolingual supernumerary teeth in the incisor and molar regions | 105 | |
| EDA | K14-Eda-A1 | Mesiodistal supernumerary teeth in the diastema region | 187 |
| K14-Eda | Mesiodistal supernumerary teeth in the diastema region | 118,187 | |
| K14-Eda; Fgf20−/− | Mesiodistal supernumerary teeth in the diastema region | 120 | |
| K14-Edar | Mesiodistal supernumerary teeth in the diastema region (sometimes missing third teeth) | 118 | |
| B6CBACa-Aw-J/A-EdaTa/0, | Mesiodistal supernumerary teeth in the diastema region | 188 | |
| Heterozygous Tabby | Mesiodistal supernumerary teeth in the diastema region (sometimes missing third teeth) | 189 | |
| Heterozygous Eda Ta/+ | Mesiodistal supernumerary teeth in the diastema region | 189,190 | |
| Others | Rsk2–/Y | Mesiodistal supernumerary teeth in the diastema region | 191 |
| Tg737orpk mutant | Mesiodistal supernumerary teeth in the diastema region | 186,192 | |
| K14-Cre; Fam20Bflox/flox | Buccolingual supernumerary teeth in the incisor region | 115,116 | |
| Cebpb−/−; Runx2+/− | Buccolingual supernumerary teeth in the incisor region | 193 | |
| Sey/Sey | Supernumerary teeth in the upper incisor region | 194 | |
| Di | Buccolingual supernumerary teeth in the incisor region | 195 | |
| Organ culture of mesenchyme-trimmed germ | Extra incisors develop in wild-type explants when most of the surrounding mesenchyme is removed before culture | 94 | |
| Osr2−/− | Buccolingual supernumerary teeth in the molar region | 108,109 | |
| Epiprofin−/− | Numerous supernumerary teeth in the incisor and molar regions | 196 | |
| Pitx2-Cre; Irf6 F/F | Supernumerary teeth in the incisor and diastema regions | 197 |
*5E1: an IgG1 monoclonal antibody against Shh protein
Table 2.
Mouse models of congenital tooth deficiency
| Pathway | Mouse model | Phenotype | Reference |
|---|---|---|---|
| Wnt | Wnt7b-expressing | Tooth germ development arrested at the bud stage | 99 |
| Fgf8CreER; Ctnnb1f/f | Tooth germ development arrested at the placode–bud transition stage | 41 | |
| Osr2-creKI; Ctnnb1ex3f | Tooth germ development arrests at the cap stage | 133 | |
| Osr2-IresCre; Catnbf/f | Tooth germ development arrested at the bud stage | 150 | |
| Lef1−/− | Tooth germ development arrested at the bud stage | 37–40 | |
| Dkk1-expressing |
Molar tooth germ development arrested at the lamina–early bud stage Incisor tooth germ development arrested at the placode stage |
89 | |
| K14-Dkk1 transgenic mice | Molar tooth germ development arrested at the lamina–early bud stage | 134 | |
| Wnt1-Cre; Rspo3fl/−; Rspo2+/+ | Tooth germ development arrested at the bud stage | 135 | |
| K14-Cre; Apccko/cko | Incisor agenesis | 198 | |
| Shh | Gli2−/−; Gli3+/− | Tooth germ development arrested at the placode stage | 138 |
| Gas1−/−; Shh+/− | Premaxillary incisor agenesis | 104 | |
| K14-Shh | Tooth germ development arrested at the bud stage | 199 | |
| BMP | Wnt1Cre; Bmp4f/f | Tooth germ development arrested at the bud stage | 110,141 |
| Osr2−/−Wnt1Cre; Bmp4f/f | Supernumerary tooth germ development arrested at the placode–bud transition stage | 141 | |
| Bmp4ncko/ncko Inhba−/− | Tooth germ development arrested at the bud stage | 110 | |
| Inhba−/− | Tooth germ development arrest at the bud stage | 110 | |
| K14-Cre43; Bmpr1acl/cl | Tooth germ development arrested at the bud stage | 140 | |
| Wnt1-Cre; Smad4fl/fl | Tooth germ development arrested at the lamina stage | 142 | |
| K14Cre; pMes-Nog | Tooth germ development arrested at the lamina/early–bud stage | 139 | |
| FGF | Fgf3−/−; Fgf10−/− | Tooth germ development arrested prior to bud stage | 154 |
| Fgfr2(IIIb)−/− | Tooth germ development arrest at the bud stage | 152 | |
| K14-Cre; Fgfr2fl/fl | Retarded tooth formation | 153 | |
| Eda | K14–Edar (Intermediate) | Third molar agenesis | 200 |
| Pax9+/−Eda−/− | Incisor and third molar agenesis | 162 | |
| TF | P63−/− | Tooth germ development arrested at the dental lamina stage | 36 |
| Krt14-Cre; Pitx2flox/flox | Tooth germ development arrested at the bud stage | 33 | |
| Msx1−/− | Tooth germ development arrested at the bud stage | 143,144 | |
| Msx1−/− Msx2−/− | Tooth germ development arrested at the dental lamina–early bud stage | 145 | |
| PAX9−/− | Tooth germ development arrested at the bud stage | 159 | |
| Pax9lacZ/lacZ | Tooth germ development arrested at the bud stage | 163 | |
| Pax9neo/lacZ | Tooth germ development arrested at the bell stage | 163 | |
| Pitx2Cre; Sox2F/F | Tooth germ development halted at the late bud-bell stage | 32 | |
| Others | Gpr177 K14cre; Osr2−/− | Supernumerary tooth germ development arrested at the lamina/early bud stage | 54 |
| Gpr177 K14cre | Tooth germ development arrested at the early cap stage | 54 | |
| Wnt1-Cre; Alk5fl/fl | Tooth germ development delayed | 201 | |
| K14Cre; Ctnna1cKO | Tooth germ development arrested at the bud stage | 202 | |
| EL/Sea | Third molar agenesis | 203 | |
| K14-follistatin−/+ | Third molar agenesis | 204 | |
| K5-GR | Second and third molar agenesis | 205 | |
| Pitx2-Cre; Irf6 F/F | Third molar agenesis | 197 |
TF transcription factor
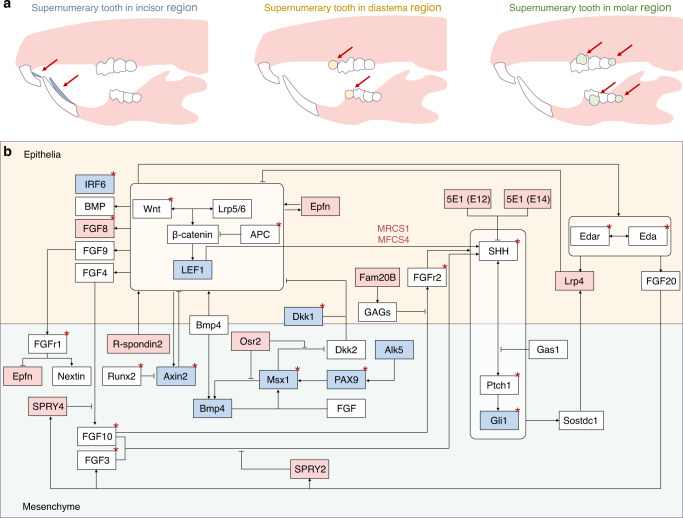
Signalling pathways related to supernumerary tooth
In human, the aetiology of supernumerary teeth is multifactorial and involves both genetic and environmental factors.82 Although the genetic propensity of supernumerary teeth is not consistent with a simple Mendelian pattern, they are more common in the relatives of patients than in the general population.83 To date, multiple genes have been identified in supernumerary teeth cases, such as APC, RUNX2, FAM20A etc..84–86 And related mouse models have been employed to explore the pathogenesis (Table 1).
Wnt signalling pathway
The Wnt signalling pathway genes play important roles in the supernumerary tooth. Among them, APC is one of the most famous pathogenicity genes in human patients.85 Its product inhibits the Wnt signalling pathway by down-regulating β-catenin protein.87 And APC mutation results in the classical Wnt signalling pathway anomaly, thereby forming supernumerary tooth.84
Investigations also support the activation of Wnt signalling and the formation of extra teeth. In the dental epithelium, overactivation of epithelial Wnt/β-catenin signalling owing to stabilisation of β-catenin or ablation of the Wnt inhibitor Apc leads to the occurrence of extra teeth.88 The epithelial overactivation of β-catenin produces a large domed evagination of the epithelium with mesenchymal condensation,41 thus expanding the expression regions of Wnt10b, Lef1, Bmp4, Msx1 and Msx2 and eventually leading to the formation of extra teeth.89 In particular, multiple small teeth surround a larger incisor, and the molar region usually forms dozens of tapered teeth.90 Besides, Wise (SOSTDC1, ectodin and USAG1) serves as an inhibitor of Lrp5- and Lrp6-dependent Wnt signalling and contributes to signal conduction between epithelium and mesenchyme, thus limiting the number of teeth.91,92 Its mutation can lead to supernumerary teeth in mouse93 (Fig. 3). And the extra incisor phenotype of Sostdc1-deficient mice can be replicated by activating Wnt signalling via reducing the mesenchymal tissue around the incisor tooth germ.94
Fig. 3.
Schematic of location and genes regarding tooth number abnormality. a Schematic of supernumerary teeth located in different regions. b Summary of genes related to tooth number abnormality. Red represents genes associated with extra teeth; blue represents genes associated with inhibition of tooth development; Red * represents genes reported in humans
However, function of Wnt signalling is complex during supernumerary tooth formation. On the one hand differences in the location of overactivated Wnt signalling lead to contradictory phenotypes. Overactivation of mesenchymal Wnt/β-catenin signalling in vitro inhibits the formation of M2 and M3.95 On the other hand, downregulation of Wnt signalling may also lead to supernumerary tooth. Mutation in R-spondin2, a Wnt signalling activator, can lead to the formation of an extra tooth in diastema with significant reduction of Wnt signalling activity; however, no significant abnormalities occur in molars or incisors.96 In addition, the role of Wnt signalling in supernumerary tooth is not completely identical in humans or mice. Some mice with Wnt10a mutation (~50%) have the fourth molar, whereas it has not been reported in patients with Wnt10A mutation.97
SHH signalling pathway
Shh signalling pathway is an essential signalling pathway regulated tooth number. Shh, Wnt and their interactions are significant factors regulating the boundaries of the odontogenic region. And Shh signalling pathway is both the downstream signal and negative feedback regulator of Wnt signalling during tooth development98,99 According to a clinical study, Shh can be a molecular biomarker in children with supernumerary teeth due to its higher expression level in patients with supernumerary teeth.100 And modulating SHH signals can lead to the formation of extra teeth in mice. MRCS1 and MFCS4 are enhancers that regulate Shh expression in the mouse tooth epithelium.101 MRCS1 can interact with Lef1/Tcfs and is regulated via Wnt/β-catenin signalling. The loss of these enhancers can result in the formation of an extra tooth in front of M1.102 Gas1, a protein located in the mesenchyme during tooth development, can regulate the number of teeth. It can limit Wnt and FGF signals in the odontogenic epithelium by regulating Shh signal transduction.103,104
Furthermore, a lingual supernumerary tooth model can be constructed by modulating Shh signalling during the special stage of tooth development. 5E1 is a monoclonal antibody against the Shh protein. Injecting 5E1 at E12 results in the formation of a supernumerary tooth in the diastema, whereas injecting it after 2 days (E14) results in the formation of lingual teeth in the incisor and molar regions.105 This phenomenon indicates that odontogenic regulation of Shh signalling is time-specific. Supernumerary teeth located on the lingual side of normal teeth occur more commonly than those on the buccal side, which may be associated with abnormalities in the successional lamina.
BMP signalling pathway
BMP signalling pathway is an essential tooth development-related signalling that also involves the formation of tooth number abnormality. The related genes including BMPR1A, BMPR2, BMP6, BMP2, and SMAD6 have been identified in mesiodens patients. According to gene co-occurrence network analysis BMP, SHH, and WNT signalling pathways together form a genomic alterations network of supernumerary tooth.106
BMP4 is one the most crucial molecules in BMP related genes in mouse tooth germs. It constitutes a signalling axis with Msx1 to regulate tooth development. BMP4 is initially expressed in the epithelium but induces the transcription factors MSX1 and MSX2 in the mesenchyme. Subsequently, the expression of mesenchymal BMP4 increases in an MSX1-dependent manner, and BMP4 returns to the epithelium, inducing the expression of P21.89 The Msx1–Bmp4 axis inhibits Sfrp2 and Dkk2. And Osr2 can inhibit this axis, which is a negative regulator of dental signalling, predominantly in the mesenchyme.107 In Osr2−/− mice, with the increased expression of odontogenesis-related signalling molecules (such as BMP4), extra teeth form at the lingual side of molars, which resemble the second row of teeth in non-mammals.108,109 Moreover, the loss of Osr2 can rescue the arrested molar germ development in Inhb−/− mice.110
FGF signalling pathway
FGF signalling pathway connects with the formation of supernumerary tooth. Controlling some vital FGF-related molecules directly is a typical method to construct a supernumerary tooth model. FGF8 can activate odontogenesis in the diastema region.111 If epithelial FGF8 is ectopically activated directly, genes related to tooth development, such as Pitx2, Sox2, Lef-1, p38 and Erk1/2, are expressed in the incisor lingual epithelium, thereby activating the tooth-forming ability. And loss function of Sprouty (Spry), a negative feedback regulator of FGF also can lead to the formation of supernumerary tooth.112,113
Indirectly interfering with FGF signalling pathways is another pathogenic mechanism of supernumerary tooth. The molecular mechanism of Cleidocranial dysplasia (CCD) related to Runx2 haploinsufficiency involves the activated FGF signalling by freely excessive unbound Twist1.114 Besides, FAM20B is a xylose kinase that is required for glycosaminoglycan (GAG) assembly. Additionally, during the initial stages of tooth development, GAG can limit FGFR2b signalling to regulate the cell fate of the incisor lamina and maintain the balance between the proliferation and differentiation of Sox2+ cells.115 Therefore, after the knockout of Fam20B in the epithelium, supernumerary teeth can appear on the lingual side of the incisor region.116
EDA signalling pathway
Abnormalities Eda signalling pathways also activate the odontogenesis potential. It is identified as morphogenic signalling regulating the formation of tooth including shape, size and number according some developmental researches.117,118 Supernumerary tooth models can be constructed using K14-Eda mice,118,119 and inactivation of Fgf20 increases the probability of developing extra teeth in K14-Eda mice.120 Besides the modulation of EDA signalling pathway on dental formula is also explored through evo-devo approaches.121
Signalling pathways related to tooth agenesis
According to clinical reports, tooth agenesis-related pathogenic genes include Wnt10A, Wnt10B, Msx1, Pax9, TGFA and AXIN2, which are involved in multiple signalling pathways, such as Wnt/β-catenin, TGF-β/BMP and Eda/Edar/NF-κB.122–126 Therefore, even if many factors can prevent or interfere with the development of the tooth germ, such as genetic conditions, trauma, radiation and infectious diseases, studies have mostly focused on abnormalities in Wnt, Shh, Bmp and FGF signalling. To date, increasing mouse models have been constructed to understand the mechanism underlying tooth agenesis (Table 2).
Wnt signalling pathway
The Wnt signalling pathway is a major pathway responsible for human tooth agenesis.127,128 Different combinations of sequence variants in Wnt-related genes (such as WNT10A, WNT10B, LRP6, AXIN2, KREMEN1, etc.) lead to various patterns of missing teeth.129 Wnt10A mutations preferentially affect the permanent dentition instead of the deciduous dentition, indicating that the role of Wnt10A may vary between the development of deciduous and permanent teeth.130 Wnt10B mutations also tend to interfere with the development of permanent teeth, especially the lateral incisors.131
Investigations of mouse models also indicate that the Wnt signalling pathway plays a critical role in the occurrence of tooth agenesis. β-catenin is an important molecule in classical Wnt signalling and binds to TCF/LEF to stimulate the transcription of target genes of Wnt signalling.132 The loss of β-catenin in the epithelium prevents the tooth germ from developing into the bud stage.41 Additionally, after the conditional removal of β-catenin from the mesenchyme, the tooth bud fails to attain the cap stage.133 This phenomenon conforms with the observation that odontogenesis signals are transmitted from the epithelium to mesenchyme. Moreover, tooth development can be blocked by inhibiting Wnt signalling via decreasing the expression of the Wnt activator R-Spondin 3 or increasing the expression of the Wnt inhibitor, Dkkl.89,134,135 The ectopic expression of Wnt7b arrests tooth germ development, which is accompanied by decreased Shh expression.99
In addition, the model of mouse incisor germ demonstrated the importance of the Wnt signalling pathway in tooth agenesis, even if it belongs to hypselodont instead of brachydont (such as teeth of humans and molar of mice). The mouse incisor germ is at risk of developmental arrest owing to abnormality in the Pitx2–Sox2–Lef1 axis (as mentioned in section 1.1). Conditional Sox2 deletion in the dental epithelium arrests the development of incisors, which is related to absorption of the tooth germ caused by decreased stem cell proliferation and differentiation. This phenotype can be rescued via Lef1 overexpression.32
SHH signalling pathway
Shh signalling appears to be specific to maxillary incisor development. The solitary median maxillary central incisor syndrome (SMMCI), a special kind of tooth agenesis in human, is associated with SHH pathway. Its pathogenicity gene includes SHH, SIX3, TGIF1, DISP1, PTCH1, SMO, etc..136,137 Besides, both Gli2−/−; Gli3+/- and Gas1−/−; Shh+/− mice have stunted maxillary incisors. And Gli2−/−; Gli3+/− mice have smaller mandibular incisors and molars compared with wild type whereas Gas1−/−; Shh+/− mice have varying combinations of midline-centred craniofacial deficiencies.104,138
BMP signalling pathway
BMP signalling, downstream of Wnt signalling, also contributes to early tooth development. Overexpression of epithelial Noggin (a BMP antagonist) can arrest tooth germ development,139 and knockout of Bmpr1a in the epithelium exhibits a similar phenotype.140 In addition to abnormalities in epithelial BMP signalling, knockout of some genes in the mesenchyme can prevent tooth germ development by affecting the epithelial–mesenchymal interaction. Knockout of BMP4 in the mesenchyme arrests the development of normal teeth and stagnates the formation of supernumerary teeth before the bud stage,141 and inactivation of mesenchymal Smad4 (TGF-β/BMP signalling) leads to the arrest of tooth germ development.142
Msx1 plays a critical role in the bud-to-cap transition by regulating the expression of Dkk2 and BMP4.89,143 Inactivation of Msx1 terminates tooth germ development at the bud stage,144 whereas deficiency of both Msx1 and Msx2 (Msx1−/−; Msx2−/− double-knockout mice) arrests tooth development earlier at the placode stage.145 The arrested development of the maxillary molar germ in Msx1−/− mice can be rescued by increasing the expression of Bmp4 or suppressing Dkk while inactivating Sfrp2 and Sfrp3.107,146,147
FGF signalling pathway
Failure of FGF signalling is identified as the main pathogenic mechanism in some tooth agenesis patients. Their mutated genes include FGF3, FGF10, FGFR2, and FGFR3.148,149 And according to the study on animal model, FGF signalling is important for the placode-to-bud transition, which is critical for the interaction between the epithelium and mesenchyme.150,151 In Fgfr2-deficient mice, tooth germ development is delayed and fails to progress beyond the bud stage.152,153 Moreover, the formation of both maxillary and mandibular molars is blocked before the bud stage in Fgf3−/−; Fgf10−/− double-mutant mice.154
EDA signalling pathway
Mutations in the EDA signalling pathway (EDA, EDAR, EDARADD etc.) produce an ectodermal dysplasia phenotype that includes missing teeth in human.155 And the related genes may be associated with some specific sites of tooth agenesis. The hypodontia of the lower jaw incisors, second premolars and maxillary lateral incisors is associated with Eda and Edar mutations; and absence of molars, particularly the second molars of the lower jaw, is more likely to be associated with Pax9 mutations.76,156–158 Based on results from mice, Pax9 is involved with EDA signalling pathway during odontogenesis and its’ dosage has a direct impact on tooth development.159–162 Development of the tooth germ stagnates at the bud stage in Pax9lacZ/lacZ mutant mice but progresses to the bell phase in Pax9neo/lacZ mice.163
Besides studies on model animal and human mentioned above, tooth number abnormality of non-model animals or extinct animals provide new perspective to explore the pathogenetic mechanisms. An investigation from Megantereon supports that the occurrence of supernumerary tooth can be considered as evidence of atavism.164 In fact, the changes of tooth cusp in non-model animals or extinct animals gets more attention rather than tooth number abnormality.
Connection between tooth number abnormalities and other human diseases
Numerous cases support a potential connection between tooth number abnormalities and other human diseases. In addition to common Craniomaxillofacial abnormalities, many systemic diseases such as skeletal system diseases, eye diseases, and nervous system diseases can also co-occur with tooth number abnormalities in patients with some syndromes (Fig. 4). To date, a mass of dentition-related syndromes have been identified (Table 3),13,165 and eight of those are more likely to be associated with the supernumerary tooth phenotype (Table 4).166 Therefore, a few syndromes can be diagnosed earlier based on the occurrence of supernumerary teeth. For example, in the case of FAP (OMIM 175100), abnormalities in its pathogenic gene, APC, can affect the activity of Wnt/β-catenin signalling to interfere with tooth development.84,88 Because dental abnormalities are usually detected earlier than gastrointestinal symptoms, supernumerary teeth and odontomas can serve as important diagnostic clues to FAP.14,167,168
Table 3.
Phenotypes of supernumerary teeth-related syndromes
| Syndrome | Oral symptoms | Other symptoms | Reference |
|---|---|---|---|
| Cleidocranial dysplasia |
Delayed eruption of permanent teeth Hypoplastic maxilla Characteristic shapes of the ramus, condyle, and coronoid |
Abnormal clavicles Patent sutures and fontanelles Short stature Pectus excavatum Sinus and middle ear infections |
206–209 |
| Familial adenomatous polyposis |
Unerupted teeth Congenital teeth missing Dentigerous cysts Odontomas |
Adenomas in the rectum and colon Osteomas Congenital hypertrophy of the retinal Pigment epithelium (CHRPE) Desmoid tumours |
84,210 |
| Nance-Horan syndrome |
Notched incised edges (Hutchinson’s incisors) Mulberry molars Talon’s cusp Taurodontism |
Congenital cataract Strabismus |
211–213 |
| Oculofaciocardiodental syndrome |
Radiculomegaly facial anomalies cleft palate |
Microphthalmia Congenital cataracts Cardiac and digital abnormalities neuropathy Muscle hypotonia Pituitary underdevelopment Brain atrophy Lipoma Childhood lymphoma |
214–216 |
| Opitz BBB/G syndrome |
Cleft lip and palate Micrognathia Ankyloglossia High-arched palate |
Hypertelorism Hypospadias Laryngo–tracheo–oesophageal abnormalities Neurological, anal, and cardiac defects Dysphagia Developmental delay |
217–219 |
| Robinow syndrome |
Midline clefting of the lower lip Gum hypertrophy Dental crowding Ankyloglossia or “tongue tie” (bifid tongue) |
Hypertelorism Nasal features (large nasal bridge, short upturned Nose, and anteverted nares) Midface hypoplasia Mesomelic limb shortening Brachydactyly Clinodactyly Micropenis Short stature Umbilical hernia |
220,221 |
|
Rubinstein–Taybi syndrome 1 Rubinstein–Taybi syndrome 2 |
High palate |
Moderate-to-severe intellectual disability Downslanted palpebral fissures Low-hanging columella Grimacing smile Talon cusps Short stature Obesity Eye anomalies |
222,223 |
| Trichorhinophalangeal syndrome type I |
Thin upper lip Small jaw |
Relative macrocephaly Sparse hair Bulbous nasal tip Protruding ears Prominent forehead Short hands and feet Bulbous pear-shaped nose Tented alae Long-extended philtrum Horizontal groove on the chin. |
224,225 |
Table 4.
Syndromes with supernumerary teeth phenotypes
| Syndrome | OMIM | Gene | MOI |
|---|---|---|---|
| Cleidocranial dysplasia# | 119600 | RUNX2 | AD |
| Familial adenomatous polyposis # | 175100 | APC | AD |
| Nance-Horan # | 302350 | NHS | XL |
| Oculofaciocardiodental syndrome # | 300166 | BCL6 | XL* |
| Opitz BBB/G syndrome # | 300000 | MIDLINE 1 | AD |
| Robinow # | 180700 | ROR2 | AD |
|
Rubinstein–Taybi syndrome 1# Rubinstein–Taybi syndrome 2# |
180849 613684 |
CREBBP | AD |
| Trichorhinophalangeal syndrome type I # | 190350 | TRPS1 | AD |
| Amelogenesis Imperfecta | 204690 | FAM20A | AR |
| Bloch-Sulzberger syndrome | 308300 | IKBKG | XL |
| Craniosynostosis | 614188 | IL11RA | AR |
| Crouzon syndrome | 123500 | FGFR2 | AD |
| Ehlers-Danlos Type III | 130020 | COL3A1 | – |
| Ehlers-Danlos Type IV | 225400 | PLOD | AR |
| Ellis–Van Creveld | 225500 | EVC, EVC2 | AR |
| Fabry disease | 301500 | GLA | XL |
| Hallerman-Streiff | 234100 | Unknown | – |
| Noonan syndrome | 163950 | PTPN11 | AD |
| Oral-facial-digital syndrome type I | 311200 | OFD1 | XL |
| Rothmund–Thomson syndrome | 268400 | RECQL4 | AR |
| SOX2 Anophthalmia syndrome | 184429 | SOX2 | AD |
AD Autosomal dominant, AR Autosomal recessive, XL X-linked
*Lethalon males
The potential relationship between tooth agenesis and tumours is noteworthy. Because of the intersection of tumorigenesis- and odontogenesis-associated signalling pathways, tooth agenesis may provide some information regarding cancer susceptibility.12 Wnt signalling-related genes, such as Wnt10A, Wnt10B, AXIN2, MESD, LRP6 and Dkk1, are pathogenic genes related to tooth agenesis.169–171 Patients with AXIN2 mutations are susceptible to colorectal cancer.172 Additionally, patients with hepatocellular carcinoma, prostate cancer, ovarian cancer and lung cancer may have AXIN2 mutations.173 In addition to Wnt signalling, the FGF signalling pathway (FGF3, FGF10 and FGFR2) is associated with cancer susceptibility.174 Moreover, Pax9 is not only a pathogenic gene related to tooth agenesis175 but also a transcription factor that can affect malignant transformation by maintaining the differentiation of squamous cells.176 However, large-scale epidemiological surveys with genetic mapping and follow-up studies on a molecular level are required for determining the correlation between tooth agenesis and cancer.177,178
Furthermore, stem cells from supernumerary tooth provide a new possibility to cure some diseases. Supernumerary tooth was an ideal source of postpartum stem cells15 as the feasibility of deriving stem cells from a supernumerary tooth has been demonstrated.179 Compared with normal dental pulp stem cells (DPSCs), human supernumerary teeth-derived stem cells (SNTSCs) may exhibit a higher proliferation rate and differentiation potential.128 In particular, their osteogenic differentiation can be enhanced by stimulating oncostatin M with the increased expression of BMP2, BMP4, BMP6 and RUNX2, which are genes involved in hard tissue repair.180 Stem cells derived from mesiodens also have a high proliferation rate and an immunophenotype similar to that of DPSCs.181 Owing to their immunomodulatory properties, SNTSCs can ameliorate the symptoms of systemic lupus erythematosus.17 Moreover, the viability and osteogenic differentiation of supernumerary teeth-derived apical papillary stem cells (SCAP-Ss) are better than those of DPSCs. SCAP-Ss are derived easily after birth and have considerable therapeutic efficacy for hepatic fibrosis.16
Genetic intervention strategies for tooth number abnormalities
Tooth development depends on proper odontogenesis signalling. Abnormal signalling seems to be the primary cause of tooth number abnormalities. Therefore, these abnormalities can be treated by intervening with the signalling network, especially in tooth agenesis.18
Tooth agenesis caused by mutations in Msx1 can be rescued via different genetic interventions. As mentioned before, the Bmp4–Msx1 pathway plays an important role during early tooth development, which can regulate the secreted Wnt antagonists, including Dkk2, Sfrp2 and Sostdc1.143 Additionally, Bmp4 promotes the transition of the arrested tooth germ (caused by Msx1 mutations) from the bud stage to the bell stage in vitro.147 Genetic inactivation of Sfrp2 and Sfrp3 in combination with IIIC3a (a Dkk inhibitor) treatment can rescue the arrested Msx1−/− tooth bud in vivo.107 Furthermore, understanding the mechanisms underlying the formation of supernumerary teeth provides novel insights into the treatment of tooth agenesis. Although Msx1 is essential for normal tooth development, it is dispensable for the formation of supernumerary teeth in K14-Cre8Brn; Apccko/cko mice, which suggests that Apc escapes the Msx1–Bmp4 feedback loop to rescue tooth germ arrest and facilitates its development to more advanced stages.88 Sostdc1 (ectodin, Wise and USAG1) is another candidate protein for molecular targeted therapy of tooth agenesis. It was discovered by analysing unknown cDNAs of mice and humans and is located on the human chromosome 7p21.2.182 Sostdc1 has a strong restrictive effect on the spatial localisation of dental signals. Its inactivation leads to the formation of supernumerary teeth, and its excessive activation results in tooth agenesis.91,93 Animal studies have revealed that blocking USAG-1 function via USAG-1 knockout or using anti-USAG-1 antibodies can treat tooth agenesis caused by genetic factors such as Msx1, EDA1 and Runx2.19,20
Lef1 is required for tooth development and is related to tooth agenesis. It mediates the odontogenesis signalling network and is required for the relay of Wnt signalling to a cascade of FGF signalling during tooth morphogenesis.38 The loss of Lef1 causes tooth development arrest at the late bud stage and prevents the expression of multiple signalling molecules.39,183 These effects can be rescued by increasing the expression of FGF4, the downstream target of Lef1 and Wnt signalling.183 In addition, Lef1 regulates the self-renewal ability of EpSCs based on the Pitx2–Sox2–Lef1 interaction.33,34 The development of incisors is arrested in Pitx2Cre; Sox2F/F mice owing to impaired proliferation of EpSCs and defective differentiation of dental epithelial cells. Lef1 overexpression partially rescues tooth development arrest by forming a new EpSC compartment.32
The development of supernumerary tooth germ can be blocked by intervening with genes related to tooth agenesis. The formation of supernumerary incisors in K14Cre; Fam20Bfl/fl mice can be partially prevented by deleting Sox2 from the dental epithelium, whereas it can be completely prevented by increasing the expression of Dkk1.115 The formation of supernumerary teeth relies on the hyperactivation of Wnt signalling. This hypothesis is also supported by the phenotype of Gpr177K14cre/Osr2−/− mice. Proteins coded by Gpr177 regulate Wnt sorting and secretion in mice. The formation of lingual supernumerary teeth in the molar region owing to the deficiency of Osr2 is arrested at the lamina/early bud stage because of epithelial inactivation of Gpr177.54
Conclusion
This review elaborates on the key findings and recent progress of tooth number abnormality based on developmental biology, animal models, clinical diagnosis and treatment. Genes related to the occurrence of anomalies in tooth number have been described in detail, which may also contribute to the development of teeth regeneration in the future. Clinical information regarding the diagnosis and treatment of supernumerary teeth or tooth agenesis may help clinicians to diagnose and manage dentinogenetic abnormalities and other related systemic diseases. In addition, genetic intervention-based treatment approaches for abnormal teeth number have been summarised. Although these ideal treatments have been investigated only in animal studies, these studies provide a rationale for developing treatment strategies for tooth number abnormality in humans.
Acknowledgements
This work was supported by grants from the National Key R&D Program of China (2022YFA1103201), Shanghai Academic Leader of Science and Technology Innovation Action Plan (20XD1424000), Shanghai Experimental Animal Research Project of Science and Technology Innovation Action Plan (201409006400), National Natural Science Foundation of China (82270963, 82061130222) awarded to Y.S., and National Natural Science Foundation Projects of China (92049201) awarded to X.W.
Author contributions
H.Z.: contributed to data acquisition, analysis and interpretation, and drafted manuscript; X.G. contributed to drafted manuscript and critically revised the manuscript; X.X.: contributed to critically revise the manuscript; X.W.: contributed to critically revise the manuscript; Y.S.: contributed to design the study and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Competing interests
The authors declare no competing interests.
Consent for publication
All authors agree to publish.
Footnotes
These authors contributed equally: Han Zhang, Xuyan Gong.
References
- 1.Cammarata-Scalisi F, Avendano A, Callea M. Main genetic entities associated with supernumerary teeth. Arch. Argent. Pediatr. 2018;116:437–444. doi: 10.5546/aap.2018.eng.437. [DOI] [PubMed] [Google Scholar]
- 2.Demiriz L, Durmuslar MC, Misir AF. Prevalence and characteristics of supernumerary teeth: a survey on 7348 people. J. Int Soc. Prev. Community Dent. 2015;5:S39–S43. doi: 10.4103/2231-0762.156151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Santis D, et al. Syndromes associated with dental agenesis. Minerva Stomatol. 2019;68:42–56. doi: 10.23736/S0026-4970.18.04129-8. [DOI] [PubMed] [Google Scholar]
- 4.Al-Ani AH, Antoun JS, Thomson WM, Merriman TR, Farella M. Hypodontia: an update on Its etiology, classification, and clinical management. Biomed. Res. Int. 2017;2017:9378325. doi: 10.1155/2017/9378325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mogollon, I., Moustakas-Verho, J. E., Niittykoski, M. & Ahtiainen, L. The initiation knot is a signaling center required for molar tooth development. Development10.1242/dev.194597 (2021). [DOI] [PMC free article] [PubMed]
- 6.Ahtiainen L, et al. Directional cell migration, but not proliferation, drives hair placode morphogenesis. Dev. Cell. 2014;28:588–602. doi: 10.1016/j.devcel.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Prochazka J, et al. Migration of founder epithelial cells drives proper molar tooth positioning and morphogenesis. Dev. Cell. 2015;35:713–724. doi: 10.1016/j.devcel.2015.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li J, Economou AD, Vacca B, Green JBA. Epithelial invagination by a vertical telescoping cell movement in mammalian salivary glands and teeth. Nat. Commun. 2020;11:2366. doi: 10.1038/s41467-020-16247-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li J, Chatzeli L, Panousopoulou E, Tucker AS, Green JB. Epithelial stratification and placode invagination are separable functions in early morphogenesis of the molar tooth. Development. 2016;143:670–681. doi: 10.1242/dev.130187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balic A. Concise review: cellular and molecular mechanisms regulation of tooth initiation. Stem Cells. 2019;37:26–32. doi: 10.1002/stem.2917. [DOI] [PubMed] [Google Scholar]
- 11.Balic A, Thesleff I. Tissue interactions regulating tooth development and renewal. Curr. Top. Dev. Biol. 2015;115:157–186. doi: 10.1016/bs.ctdb.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 12.Bonczek O, et al. Tooth agenesis: what do we know and is there a connection to cancer? Clin. Genet. 2021;99:493–502. doi: 10.1111/cge.13892. [DOI] [PubMed] [Google Scholar]
- 13.Lu X, et al. The epidemiology of supernumerary teeth and the associated molecular mechanism. Organogenesis. 2017;13:71–82. doi: 10.1080/15476278.2017.1332554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wijn MA, Keller JJ, Giardiello FM, Brand HS. Oral and maxillofacial manifestations of familial adenomatous polyposis. Oral. Dis. 2007;13:360–365. doi: 10.1111/j.1601-0825.2006.01293.x. [DOI] [PubMed] [Google Scholar]
- 15.Mortada I, Mortada R, Al Bazzal M. Dental pulp stem cells and the management of neurological diseases: an update. J. Neurosci. Res. 2018;96:265–272. doi: 10.1002/jnr.24122. [DOI] [PubMed] [Google Scholar]
- 16.Yao J, et al. Human supernumerary teeth-derived apical papillary stem cells possess preferable characteristics and efficacy on hepatic fibrosis in mice. Stem Cells Int. 2020;2020:6489396. doi: 10.1155/2020/6489396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Makino Y, et al. Immune therapeutic potential of stem cells from human supernumerary teeth. J. Dent. Res. 2013;92:609–615. doi: 10.1177/0022034513490732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takahashi K, et al. Development of tooth regenerative medicine strategies by controlling the number of teeth using targeted molecular therapy. Inflamm. Regen. 2020;40:21. doi: 10.1186/s41232-020-00130-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murashima-Suginami A. et al. Anti-USAG-1 therapy for tooth regeneration through enhanced BMP signaling. Sci Adv. 10.1126/sciadv.abf1798 (2021). [DOI] [PMC free article] [PubMed]
- 20.Mishima S, et al. Local application of Usag-1 siRNA can promote tooth regeneration in Runx2-deficient mice. Sci. Rep. 2021;11:13674. doi: 10.1038/s41598-021-93256-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Z, et al. Whole-tooth regeneration by allogeneic cell reassociation in pig jawbone. Tissue Eng. Part A. 2019;25:1202–1212. doi: 10.1089/ten.tea.2018.0243. [DOI] [PubMed] [Google Scholar]
- 22.Nakao K, et al. The development of a bioengineered organ germ method. Nat. Methods. 2007;4:227–230. doi: 10.1038/nmeth1012. [DOI] [PubMed] [Google Scholar]
- 23.Cate, A. J., & Nanci, A. Ten Cate’s Oral Histology: Development, Structure, and Function 9th edn (ed Nanci, A.) Ch. 5 (Elsevier, 2003).
- 24.Lan Y, Jia S, Jiang R. Molecular patterning of the mammalian dentition. Semin Cell Dev. Biol. 2014;25-26:61–70. doi: 10.1016/j.semcdb.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jernvall J, Thesleff I. Reiterative signaling and patterning during mammalian tooth morphogenesis. Mech. Dev. 2000;92:19–29. doi: 10.1016/S0925-4773(99)00322-6. [DOI] [PubMed] [Google Scholar]
- 26.D’Souza RN, Klein OD. Unraveling the molecular mechanisms that lead to supernumerary teeth in mice and men: current concepts and novel approaches. Cells Tissues Organs. 2007;186:60–69. doi: 10.1159/000102681. [DOI] [PubMed] [Google Scholar]
- 27.Juuri E, Balic A. The biology underlying abnormalities of tooth number in humans. J. Dent. Res. 2017;96:1248–1256. doi: 10.1177/0022034517720158. [DOI] [PubMed] [Google Scholar]
- 28.Stembirek J, et al. Early morphogenesis of heterodont dentition in minipigs. Eur. J. Oral. Sci. 2010;118:547–558. doi: 10.1111/j.1600-0722.2010.00772.x. [DOI] [PubMed] [Google Scholar]
- 29.Kim EJ, Jung SY, Wu Z, Zhang S, Jung HS. Sox2 maintains epithelial cell proliferation in the successional dental lamina. Cell Prolif. 2020;53:e12729. doi: 10.1111/cpr.12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dosedelova H, et al. Fate of the molar dental lamina in the monophyodont mouse. PLoS One. 2015;10:e0127543. doi: 10.1371/journal.pone.0127543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amen M, et al. PITX2 and beta-catenin interactions regulate Lef-1 isoform expression. Mol. Cell Biol. 2007;27:7560–7573. doi: 10.1128/MCB.00315-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sun Z, et al. Sox2 and Lef-1 interact with Pitx2 to regulate incisor development and stem cell renewal. Development. 2016;143:4115–4126. doi: 10.1242/dev.138883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu W. et al. Pitx2-Sox2-Lef1 interactions specify progenitor oral/dental epithelial cell signaling centers. Development10.1242/dev.186023 (2020). [DOI] [PMC free article] [PubMed]
- 34.Vadlamudi U, et al. PITX2, beta-catenin and LEF-1 interact to synergistically regulate the LEF-1 promoter. J. Cell Sci. 2005;118:1129–1137. doi: 10.1242/jcs.01706. [DOI] [PubMed] [Google Scholar]
- 35.Rostampour N, Appelt CM, Abid A, Boughner JC. Expression of new genes in vertebrate tooth development and p63 signaling. Dev. Dyn. 2019;248:744–755. doi: 10.1002/dvdy.26. [DOI] [PubMed] [Google Scholar]
- 36.Laurikkala J, et al. p63 regulates multiple signalling pathways required for ectodermal organogenesis and differentiation. Development. 2006;133:1553–1563. doi: 10.1242/dev.02325. [DOI] [PubMed] [Google Scholar]
- 37.Vangenderen C, et al. Development of several organs that require inductive Epithelial–Mesenchymal interactions is impaired in Lef-1-deficient mice. Gene Dev. 1994;8:2691–2703. doi: 10.1101/gad.8.22.2691. [DOI] [PubMed] [Google Scholar]
- 38.Sasaki T, et al. LEF1 is a critical epithelial survival factor during tooth morphogenesis. Dev. Biol. 2005;278:130–143. doi: 10.1016/j.ydbio.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 39.Kratochwil K, Dull M, Farinas I, Galceran T, Grosschedl R. Lef1 expression is activated by BMP-4 and regulates inductive tissue interactions in tooth and hair development. Gene Dev. 1996;10:1382–1394. doi: 10.1101/gad.10.11.1382. [DOI] [PubMed] [Google Scholar]
- 40.Laurikkala J, et al. TNF signaling via the ligand-receptor pair ectodysplasin and edar controls the function of epithelial signaling centers and is regulated by Wnt and activin during tooth organogenesis. Dev. Biol. 2001;229:443–455. doi: 10.1006/dbio.2000.9955. [DOI] [PubMed] [Google Scholar]
- 41.Kim, R. et al. Early perturbation of Wnt signaling reveals patterning and invagination-evagination control points in molar tooth development. Development10.1242/dev.199685 (2021). [DOI] [PMC free article] [PubMed]
- 42.Panousopoulou E, Green JB. Invagination of ectodermal placodes is driven by cell intercalation-mediated contraction of the suprabasal tissue canopy. PLoS Biol. 2016;14:e1002405. doi: 10.1371/journal.pbio.1002405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mammoto T, et al. Mechanochemical control of mesenchymal condensation and embryonic tooth organ formation. Dev. Cell. 2011;21:758–769. doi: 10.1016/j.devcel.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tucker A, Sharpe P. The cutting-edge of mammalian development; how the embryo makes teeth. Nat. Rev. Genet. 2004;5:499–508. doi: 10.1038/nrg1380. [DOI] [PubMed] [Google Scholar]
- 45.Rosowski J, et al. Emulating the early phases of human tooth development in vitro. Sci. Rep. 2019;9:7057. doi: 10.1038/s41598-019-43468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kollar EJ, Baird GR. Tissue interactions in embryonic mouse tooth germs. I. Reorganization of the dental epithelium during tooth-germ reconstruction. J. Embryol. Exp. Morphol. 1970;24:159–171. [PubMed] [Google Scholar]
- 47.Kollar EJ, Baird GR. Tissue interactions in embryonic mouse tooth germs. II. The inductive role of the dental papilla. J. Embryol. Exp. Morphol. 1970;24:173–186. [PubMed] [Google Scholar]
- 48.Thesleff I, Sharpe P. Signalling networks regulating dental development. Mech. Dev. 1997;67:111–123. doi: 10.1016/S0925-4773(97)00115-9. [DOI] [PubMed] [Google Scholar]
- 49.Mina M, Kollar EJ. The induction of odontogenesis in non-dental mesenchyme combined with early murine mandibular arch epithelium. Arch. Oral. Biol. 1987;32:123–127. doi: 10.1016/0003-9969(87)90055-0. [DOI] [PubMed] [Google Scholar]
- 50.Lumsden AG. Spatial organization of the epithelium and the role of neural crest cells in the initiation of the mammalian tooth germ. Development. 1988;103:155–169. doi: 10.1242/dev.103.Supplement.155. [DOI] [PubMed] [Google Scholar]
- 51.Mogollon I, Ahtiainen L. Live tissue imaging sheds light on cell level events during ectodermal organ development. Front. Physiol. 2020;11:818. doi: 10.3389/fphys.2020.00818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abramyan J, Geetha-Loganathan P, Sulcova M, Buchtova M. Role of cell death in cellular processes during odontogenesis. Front Cell Dev. Biol. 2021;9:671475. doi: 10.3389/fcell.2021.671475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ahtiainen L, Uski I, Thesleff I, Mikkola ML. Early epithelial signaling center governs tooth budding morphogenesis. J. Cell Biol. 2016;214:753–767. doi: 10.1083/jcb.201512074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhu XJ, et al. Intra-epithelial requirement of canonical Wnt signaling for tooth morphogenesis. J. Biol. Chem. 2013;288:12080–12089. doi: 10.1074/jbc.M113.462473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Matalova E, Tucker AS, Sharpe PT. Death in the life of a tooth. J. Dent. Res. 2004;83:11–16. doi: 10.1177/154405910408300103. [DOI] [PubMed] [Google Scholar]
- 56.Jernvall J, Aberg T, Kettunen P, Keranen S, Thesleff I. The life history of an embryonic signaling center: BMP-4 induces p21 and is associated with apoptosis in the mouse tooth enamel knot. Development. 1998;125:161–169. doi: 10.1242/dev.125.2.161. [DOI] [PubMed] [Google Scholar]
- 57.Li J, et al. Mesenchymal Sufu regulates development of mandibular molars via Shh signaling. J. Dent. Res. 2019;98:1348–1356. doi: 10.1177/0022034519872679. [DOI] [PubMed] [Google Scholar]
- 58.Du W, Hu JK, Du W, Klein OD. Lineage tracing of epithelial cells in developing teeth reveals two strategies for building signaling centers. J. Biol. Chem. 2017;292:15062–15069. doi: 10.1074/jbc.M117.785923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Obara N, Lesot H. Asymmetrical growth, differential cell proliferation, and dynamic cell rearrangement underlie epithelial morphogenesis in mouse molar development. Cell Tissue Res. 2007;330:461–473. doi: 10.1007/s00441-007-0502-7. [DOI] [PubMed] [Google Scholar]
- 60.Jernvall J, Kettunen P, Karavanova I, Martin LB, Thesleff I. Evidence for the role of the enamel Knot as a control center in mammalian tooth Cusp formation—nondividing cells express growth-stimulating Fgf-4 gene. Int J. Dev. Biol. 1994;38:463–469. [PubMed] [Google Scholar]
- 61.Pippi R. Odontomas and supernumerary teeth: is there a common origin? Int J. Med. Sci. 2014;11:1282–1297. doi: 10.7150/ijms.10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Miyoshi S, et al. An epidemiological study of supernumerary primary teeth in Japanese children: a review of racial differences in the prevalence. Oral. Dis. 2000;6:99–102. doi: 10.1111/j.1601-0825.2000.tb00108.x. [DOI] [PubMed] [Google Scholar]
- 63.Salcido-Garcia JF, Ledesma-Montes C, Hernandez-Flores F, Perez D, Garces-Ortiz M. Frequency of supernumerary teeth in Mexican population. Med. Oral. Patol. Oral. Cir. Bucal. 2004;9:407–409. [PubMed] [Google Scholar]
- 64.Rajab LD, Hamdan MA. Supernumerary teeth: review of the literature and a survey of 152 cases. Int J. Paediatr. Dent. 2002;12:244–254. doi: 10.1046/j.1365-263X.2002.00366.x. [DOI] [PubMed] [Google Scholar]
- 65.Ma X, et al. Epidemiological, clinical, radiographic characterization of non-syndromic supernumerary teeth in Chinese children and adolescents. Oral. Dis. 2021;27:981–992. doi: 10.1111/odi.13628. [DOI] [PubMed] [Google Scholar]
- 66.Kuchler EC, Costa AG, Costa Mde C, Vieira AR, Granjeiro JM. Supernumerary teeth vary depending on gender. Braz. Oral. Res. 2011;25:76–79. doi: 10.1590/S1806-83242011000100013. [DOI] [PubMed] [Google Scholar]
- 67.Alvira-Gonzalez J, Gay-Escoda C. Non-syndromic multiple supernumerary teeth: meta-analysis. J. Oral. Pathol. Med. 2012;41:361–366. doi: 10.1111/j.1600-0714.2011.01111.x. [DOI] [PubMed] [Google Scholar]
- 68.Hajmohammadi E, Najirad S, Mikaeili H, Kamran A. Epidemiology of supernumerary teeth in 5000 radiography films: investigation of patients referring to the clinics of Ardabil in 2015–2020. Int J. Dent. 2021;2021:6669436. doi: 10.1155/2021/6669436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen KC, et al. Unusual supernumerary teeth and treatment outcomes analyzed for developing improved diagnosis and management plans. J. Oral. Maxillofac. Surg. 2019;77:920–931. doi: 10.1016/j.joms.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 70.Mahto RK, et al. Nonsyndromic bilateral posterior maxillary supernumerary teeth: a report of two cases and review. Case Rep. Dent. 2018;2018:5014179. doi: 10.1155/2018/5014179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kreiborg S, Jensen BL. Tooth formation and eruption—lessons learnt from cleidocranial dysplasia. Eur. J. Oral. Sci. 2018;126:72–80. doi: 10.1111/eos.12418. [DOI] [PubMed] [Google Scholar]
- 72.Suljkanovic N, Balic D, Begic N. Supernumerary and supplementary teeth in a non-syndromic patients. Med. Arch. 2021;75:78–81. doi: 10.5455/medarh.2021.75.-78-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Moller LH, Pradel W, Gedrange T, Botzenhart UU. Prevalence of hypodontia and supernumerary teeth in a German cleft lip with/without palate population. BMC Oral. Health. 2021;21:60. doi: 10.1186/s12903-021-01420-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Palaska PK, Antonarakis GS. Prevalence and patterns of permanent tooth agenesis in individuals with Down syndrome: a meta-analysis. Eur. J. Oral. Sci. 2016;124:317–328. doi: 10.1111/eos.12282. [DOI] [PubMed] [Google Scholar]
- 75.Kantaputra PN, et al. WNT10B mutations associated with isolated dental anomalies. Clin. Genet. 2018;93:992–999. doi: 10.1111/cge.13218. [DOI] [PubMed] [Google Scholar]
- 76.Wong SW, et al. Nine novel PAX9 mutations and a distinct tooth agenesis genotype-phenotype. J. Dent. Res. 2018;97:155–162. doi: 10.1177/0022034517729322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Koskinen S, Keski-Filppula R, Alapulli H, Nieminen P, Anttonen V. Familial oligodontia and regional odontodysplasia associated with a PAX9 initiation codon mutation. Clin. Oral. Investig. 2019;23:4107–4111. doi: 10.1007/s00784-019-02849-5. [DOI] [PubMed] [Google Scholar]
- 78.Jurek A., Gozdowski D., Czochrowska E. M., Zadurska M. Effect of tooth agenesis on mandibular morphology and position. Int. J. Environ. Res. Public Health. 10.3390/ijerph182211876 (2021). [DOI] [PMC free article] [PubMed]
- 79.Rodrigues AS, et al. Is dental agenesis associated with craniofacial morphology pattern? A systematic review and meta-analysis. Eur. J. Orthod. 2020;42:534–543. doi: 10.1093/ejo/cjz087. [DOI] [PubMed] [Google Scholar]
- 80.Agarwal P, Vinuth DP, Dube G, Dube P. Nonsyndromic tooth agenesis patterns and associated developmental dental anomalies: a literature review with radiographic illustrations. Minerva Stomatol. 2013;62:31–41. [PubMed] [Google Scholar]
- 81.Thesleff I. The genetic basis of tooth development and dental defects. Am. J. Med. Genet. A. 2006;140:2530–2535. doi: 10.1002/ajmg.a.31360. [DOI] [PubMed] [Google Scholar]
- 82.Palikaraki G., Vardas E., Mitsea A. Two rare cases of non-syndromic paramolars with family occurrence and a review of literature. Dent J (Basel). 10.3390/dj7020038 (2019). [DOI] [PMC free article] [PubMed]
- 83.Garvey MT, Barry HJ, Blake M. Supernumerary teeth-an overview of classification, diagnosis and management. J. Can. Dent. Assoc. 1999;65:612–616. [PubMed] [Google Scholar]
- 84.Yu F, et al. A novel mutation of adenomatous polyposis coli (APC) gene results in the formation of supernumerary teeth. J. Cell Mol. Med. 2018;22:152–162. doi: 10.1111/jcmm.13303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Khan MI, Ahmed N, Neela PK, Unnisa N. The human genetics of dental anomalies. Glob. Med. Genet. 2022;9:76–81. doi: 10.1055/s-0042-1743572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dourado MR, et al. Enamel renal syndrome: a novel homozygous FAM20A founder mutation in 5 new Brazilian families. Eur. J. Med. Genet. 2019;62:103561. doi: 10.1016/j.ejmg.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 87.Neufeld KL, Zhang F, Cullen BR, White RL. APC-mediated downregulation of beta-catenin activity involves nuclear sequestration and nuclear export. EMBO Rep. 2000;1:519–523. doi: 10.1093/embo-reports/kvd117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang XP, et al. Apc inhibition of Wnt signaling regulates supernumerary tooth formation during embryogenesis and throughout adulthood. Development. 2009;136:1939–1949. doi: 10.1242/dev.033803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liu F, et al. Wnt/beta-catenin signaling directs multiple stages of tooth morphogenesis. Dev. Biol. 2008;313:210–224. doi: 10.1016/j.ydbio.2007.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jarvinen E, et al. Continuous tooth generation in mouse is induced by activated epithelial Wnt/beta-catenin signaling. Proc. Natl Acad. Sci. USA. 2006;103:18627–18632. doi: 10.1073/pnas.0607289103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kassai Y, et al. Regulation of mammalian tooth cusp patterning by ectodin. Science. 2005;309:2067–2070. doi: 10.1126/science.1116848. [DOI] [PubMed] [Google Scholar]
- 92.Ohazama A. et al. Lrp4 modulates extracellular integration of cell signaling pathways in development. PLoS One. 3, e4092. (2008). [DOI] [PMC free article] [PubMed]
- 93.Ahn Y, Sanderson BW, Klein OD, Krumlauf R. Inhibition of Wnt signaling by Wise (Sostdc1) and negative feedback from Shh controls tooth number and patterning. Development. 2010;137:3221–3231. doi: 10.1242/dev.054668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Munne PM, Tummers M, Jarvinen E, Thesleff I, Jernvall J. Tinkering with the inductive mesenchyme: Sostdc1 uncovers the role of dental mesenchyme in limiting tooth induction. Development. 2009;136:393–402. doi: 10.1242/dev.025064. [DOI] [PubMed] [Google Scholar]
- 95.Jarvinen E., Shimomura-Kuroki J., Balic A., Jussila M., Thesleff I. Mesenchymal Wnt/beta-catenin signaling limits tooth number. Development10.1242/dev.158048 (2018). [DOI] [PubMed]
- 96.Kawasaki M, et al. R-spondins/Lgrs expression in tooth development. Dev. Dynam. 2014;243:844–851. doi: 10.1002/dvdy.24124. [DOI] [PubMed] [Google Scholar]
- 97.Xu M, et al. WNT10A mutation causes ectodermal dysplasia by impairing progenitor cell proliferation and KLF4-mediated differentiation. Nat. Commun. 2017;8:15397. doi: 10.1038/ncomms15397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hermans, F., Hemeryck, L., Lambrichts, I., Bronckaers, A. & Vankelecom H. Intertwined signaling pathways governing tooth development: a give-and-take between canonical Wnt and Shh. Front. Cell Dev. Biol. 9, 758203 (2021). [DOI] [PMC free article] [PubMed]
- 99.Sarkar L, et al. Wnt/Shh interactions regulate ectodermal boundary formation during mammalian tooth development. Proc. Natl Acad. Sci. USA. 2000;97:4520–4524. doi: 10.1073/pnas.97.9.4520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Talaat DM, Hachim IY, Afifi MM, Talaat IM, ElKateb MA. Assessment of risk factors and molecular biomarkers in children with supernumerary teeth: a single-center study. BMC Oral. Health. 2022;22:117. doi: 10.1186/s12903-022-02151-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Seo H, et al. Upstream enhancer elements of Shh regulate oral and dental patterning. J. Dent. Res. 2018;97:1055–1063. doi: 10.1177/0022034518758642. [DOI] [PubMed] [Google Scholar]
- 102.Sagai T. et al. SHH signaling directed by two oral epithelium-specific enhancers controls tooth and oral development. Sci Rep-UK7,13004 (2017). [DOI] [PMC free article] [PubMed]
- 103.Seppala M, et al. Gas1 regulates patterning of the murine and human dentitions through Sonic Hedgehog. J. Dent. Res. 2022;101:473–482. doi: 10.1177/00220345211049403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Seppala M, et al. Gas1 is a modifier for holoprosencephaly and genetically interacts with sonic hedgehog. J. Clin. Invest. 2007;117:1575–1584. doi: 10.1172/JCI32032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cho SW, et al. Interactions between Shh, Sostdc1 and Wnt signaling and a new feedback loop for spatial patterning of the teeth. Development. 2011;138:1807–1816. doi: 10.1242/dev.056051. [DOI] [PubMed] [Google Scholar]
- 106.Kim YY, et al. Genetic alterations in mesiodens as revealed by targeted next-generation sequencing and gene co-occurrence network analysis. Oral. Dis. 2017;23:966–972. doi: 10.1111/odi.12680. [DOI] [PubMed] [Google Scholar]
- 107.Jia S, et al. Bmp4-Msx1 signaling and Osr2 control tooth organogenesis through antagonistic regulation of secreted Wnt antagonists. Dev. Biol. 2016;420:110–119. doi: 10.1016/j.ydbio.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhang ZY, Lan Y, Chai Y, Jiang RL. Antagonistic actions of Msx1 and Osr2 pattern mammalian teeth into a single row. Science. 2009;323:1232–1234. doi: 10.1126/science.1167418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mikkola ML. Controlling the number of tooth rows. Sci. Signal. 2009;2:pe53. doi: 10.1126/scisignal.285pe53. [DOI] [PubMed] [Google Scholar]
- 110.Kwon HE, Jia S, Lan Y, Liu H, Jiang R. Activin and Bmp4 signaling converge on Wnt activation during odontogenesis. J. Dent. Res. 2017;96:1145–1152. doi: 10.1177/0022034517713710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Li L, et al. Exogenous fibroblast growth factor 8 rescues development of mouse diastemal vestigial tooth ex vivo. Dev. Dyn. 2011;240:1344–1353. doi: 10.1002/dvdy.22596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Klein OD, et al. Sprouty genes control diastema tooth development via bidirectional antagonism of epithelial-mesenchymal FGF signaling. Dev. Cell. 2006;11:181–190. doi: 10.1016/j.devcel.2006.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Peterkova R, et al. Revitalization of a diastemal tooth primordium in Spry2 null mice results from increased proliferation and decreased apoptosis. J. Exp. Zool. Part B. 2009;312b:292–308. doi: 10.1002/jez.b.21266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lu Y, et al. Molecular studies on the roles of Runx2 and Twist1 in regulating FGF signaling. Dev. Dyn. 2012;241:1708–1715. doi: 10.1002/dvdy.23858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wu J. Y. et al. FAM20B-catalyzed glycosaminoglycans control murine tooth number by restricting FGFR2b signaling. BMC Biol. 18, 87 (2020). [DOI] [PMC free article] [PubMed]
- 116.Tian Y, et al. Inactivation of Fam20B in the dental epithelium of mice leads to supernumerary incisors. Eur. J. Oral. Sci. 2015;123:396–402. doi: 10.1111/eos.12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yang R., et al. Ectodysplasin A (EDA) signaling: from skin appendage to multiple diseases. Int. J. Mol. Sci. 10.3390/ijms23168911 (2022). [DOI] [PMC free article] [PubMed]
- 118.Tucker AS, Headon DJ, Courtney JM, Overbeek P, Sharpe PT. The activation level of the TNF family receptor, Edar, determines cusp number and tooth number during tooth development. Dev. Biol. 2004;268:185–194. doi: 10.1016/j.ydbio.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 119.Kangas AT, Evans AR, Thesleff I, Jernvall J. Nonindependence of mammalian dental characters. Nature. 2004;432:211–214. doi: 10.1038/nature02927. [DOI] [PubMed] [Google Scholar]
- 120.Haara O, et al. Ectodysplasin regulates activator-inhibitor balance in murine tooth development through Fgf20 signaling. Development. 2012;139:3189–3199. doi: 10.1242/dev.079558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Salomies L, Eymann J, Ollonen J, Khan I, Di-Poï N. The developmental origins of heterodonty and acrodonty as revealed by reptile dentitions. Sci. Adv. 2021;7:eabj7912. doi: 10.1126/sciadv.abj7912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Yin W, Bian Z. The gene network underlying hypodontia. J. Dent. Res. 2015;94:878–885. doi: 10.1177/0022034515583999. [DOI] [PubMed] [Google Scholar]
- 123.Nieminen P, et al. Identification of a nonsense mutation in the PAX9 gene in molar oligodontia. Eur. J. Hum. Genet. 2001;9:743–746. doi: 10.1038/sj.ejhg.5200715. [DOI] [PubMed] [Google Scholar]
- 124.Vieira AR, Meira R, Modesto A, Murray JC. MSX1, PAX9, and TGFA contribute to tooth agenesis in humans. J. Dent. Res. 2004;83:723–727. doi: 10.1177/154405910408300913. [DOI] [PubMed] [Google Scholar]
- 125.Abdalla EM, Mostowska A, Jagodzinski PP, Dwidar K, Ismail SR. A novel WNT10A mutation causes non-syndromic hypodontia in an Egyptian family. Arch. Oral. Biol. 2014;59:722–728. doi: 10.1016/j.archoralbio.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 126.Zheng J, et al. Novel MSX1 variants identified in families with nonsyndromic oligodontia. Int J. Oral. Sci. 2021;13:2. doi: 10.1038/s41368-020-00106-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yu M, Wong SW, Han D, Cai T. Genetic analysis: Wnt and other pathways in nonsyndromic tooth agenesis. Oral. Dis. 2019;25:646–651. doi: 10.1111/odi.12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lu X, et al. A biological study of supernumerary teeth derived dental pulp stem cells based on RNA-seq analysis. Int. Endod. J. 2019;52:819–828. doi: 10.1111/iej.13060. [DOI] [PubMed] [Google Scholar]
- 129.Chu, K. Y. et al. Synergistic mutations of LRP6 and WNT10A in familial tooth agenesis. J. Pers Med. 10.3390/jpm11111217 (2021). [DOI] [PMC free article] [PubMed]
- 130.Yu M, et al. Distinct impacts of bi-allelic WNT10A mutations on the permanent and primary dentitions in odonto-onycho-dermal dysplasia. Am. J. Med. Genet A. 2019;179:57–64. doi: 10.1002/ajmg.a.60682. [DOI] [PubMed] [Google Scholar]
- 131.Yu P, et al. Mutations in WNT10B are identified in individuals with oligodontia. Am. J. Hum. Genet. 2016;99:195–201. doi: 10.1016/j.ajhg.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Daugherty RL, Gottardi CJ. Phospho-regulation of Beta-catenin adhesion and signaling functions. Physiol. (Bethesda) 2007;22:303–309. doi: 10.1152/physiol.00020.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Chen X, et al. Mesenchymal Wnt/beta-catenin signaling induces Wnt and BMP antagonists in dental epithelium. Organogenesis. 2019;15:55–67. doi: 10.1080/15476278.2019.1633871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Andl T, Reddy ST, Gaddapara T, Millar SE. WNT signals are required for the initiation of hair follicle development. Dev. Cell. 2002;2:643–653. doi: 10.1016/S1534-5807(02)00167-3. [DOI] [PubMed] [Google Scholar]
- 135.Dasgupta K. et al. R-Spondin 3 regulates mammalian dental and craniofacial development. J. Dev. Biol. 10.3390/jdb9030031 (2021). [DOI] [PMC free article] [PubMed]
- 136.Poelmans S, et al. Genotypic and phenotypic variation in six patients with solitary median maxillary central incisor syndrome. Am. J. Med. Genet A. 2015;167A:2451–2458. doi: 10.1002/ajmg.a.37207. [DOI] [PubMed] [Google Scholar]
- 137.Li J, Liu D, Liu Y, Zhang C, Zheng S. Solitary median maxillary central incisor syndrome: an exploration of the pathogenic mechanism. Front. Genet. 2022;13:780930. doi: 10.3389/fgene.2022.780930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hardcastle Z, Mo R, Hui CC, Sharpe PT. The Shh signalling pathway in tooth development: defects in Gli2 and Gli3 mutants. Development. 1998;125:2803–2811. doi: 10.1242/dev.125.15.2803. [DOI] [PubMed] [Google Scholar]
- 139.Wang Y, et al. BMP activity is required for tooth development from the lamina to bud stage. J. Dent. Res. 2012;91:690–695. doi: 10.1177/0022034512448660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Andl T, et al. Epithelial Bmpr1a regulates differentiation and proliferation in postnatal hair follicles and is essential for tooth development. Development. 2004;131:2257–2268. doi: 10.1242/dev.01125. [DOI] [PubMed] [Google Scholar]
- 141.Jia SH, et al. Roles of Bmp4 during tooth morphogenesis and sequential tooth formation. Development. 2013;140:423–432. doi: 10.1242/dev.081927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ko SO, et al. Smad4 is required to regulate the fate of cranial neural crest cells. Dev. Biol. 2007;312:435–447. doi: 10.1016/j.ydbio.2007.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lee, J. M. et al. MSX1 drives tooth morphogenesis through controlling Wnt signaling activity. J. Dental Res.101, 832–839 (2022). [DOI] [PMC free article] [PubMed]
- 144.Satokata I, Maas R. Msx1 deficient mice exhibit cleft-palate and abnormalities of craniofacial and tooth development. Nat. Genet. 1994;6:348–356. doi: 10.1038/ng0494-348. [DOI] [PubMed] [Google Scholar]
- 145.Bei M, Maas R. FGFs and BMP4 induce both Msx1-independent and Msx1-dependent signaling pathways in early tooth development. Development. 1998;125:4325–4333. doi: 10.1242/dev.125.21.4325. [DOI] [PubMed] [Google Scholar]
- 146.Zhao X, et al. Transgenically ectopic expression of Bmp4 to the Msx1 mutant dental mesenchyme restores downstream gene expression but represses Shh and Bmp2 in the enamel knot of wild type tooth germ. Mech. Dev. 2000;99:29–38. doi: 10.1016/S0925-4773(00)00467-6. [DOI] [PubMed] [Google Scholar]
- 147.Bei M, Kratochwil K, Maas RL. BMP4 rescues a non-cell-autonomous function of Msx1 in tooth development. Development. 2000;127:4711–4718. doi: 10.1242/dev.127.21.4711. [DOI] [PubMed] [Google Scholar]
- 148.Ye X, Attaie AB. Genetic basis of nonsyndromic and syndromic tooth agenesis. J. Pediatr. Genet. 2016;5:198–208. doi: 10.1055/s-0036-1592421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rodrigues AS, et al. Association between craniofacial morphological patterns and tooth agenesis-related genes. Prog. Orthod. 2020;21:9. doi: 10.1186/s40510-020-00309-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Chen J, Lan Y, Baek JA, Gao Y, Jiang R. Wnt/beta-catenin signaling plays an essential role in activation of odontogenic mesenchyme during early tooth development. Dev. Biol. 2009;334:174–185. doi: 10.1016/j.ydbio.2009.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Biggs LC, Mikkola ML. Early inductive events in ectodermal appendage morphogenesis. Semin Cell Dev. Biol. 2014;25-26:11–21. doi: 10.1016/j.semcdb.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 152.De Moerlooze L, et al. An important role for the IIIb isoform of fibroblast growth factor receptor 2 (FGFR2) in mesenchymal-epithelial signalling during mouse organogenesis. Development. 2000;127:483–492. doi: 10.1242/dev.127.3.483. [DOI] [PubMed] [Google Scholar]
- 153.Hosokawa R, et al. Epithelial-specific requirement of FGFR2 signaling during tooth and palate development. J. Exp. Zool. B Mol. Dev. Evol. 2009;312B:343–350. doi: 10.1002/jez.b.21274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Wang XP, et al. An integrated gene regulatory network controls stem cell proliferation in teeth. PLoS Biol. 2007;5:e159. doi: 10.1371/journal.pbio.0050159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Parveen, A. et al. Deleterious variants in WNT10A, EDAR, and EDA causing isolated and syndromic tooth agenesis: a structural perspective from molecular dynamics simulations. Int. J. Mol. Sci. 10.3390/ijms20215282 (2019). [DOI] [PMC free article] [PubMed]
- 156.Zhou M, et al. Analyses of oligodontia phenotypes and genetic etiologies. Int J. Oral. Sci. 2021;13:32. doi: 10.1038/s41368-021-00135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Arte S, Parmanen S, Pirinen S, Alaluusua S, Nieminen P. Candidate gene analysis of tooth agenesis identifies novel mutations in six genes and suggests significant role for WNT and EDA signaling and allele combinations. PLoS One. 2013;8:e73705. doi: 10.1371/journal.pone.0073705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Zhang L, et al. Comparative analysis of rare EDAR mutations and tooth agenesis pattern in EDAR- and EDA-associated nonsyndromic oligodontia. Hum. Mutat. 2020;41:1957–1966. doi: 10.1002/humu.24104. [DOI] [PubMed] [Google Scholar]
- 159.Peters H, Neubuser A, Kratochwil K, Balling R. Pax9-deficient mice lack pharyngeal pouch derivatives and teeth and exhibit craniofacial and limb abnormalities. Genes Dev. 1998;12:2735–2747. doi: 10.1101/gad.12.17.2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wang Y, Kong H, Mues G, D’Souza R. Msx1 mutations: how do they cause tooth agenesis? J. Dent. Res. 2011;90:311–316. doi: 10.1177/0022034510387430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ogawa T, et al. Functional consequences of interactions between Pax9 and Msx1 genes in normal and abnormal tooth development. J. Biol. Chem. 2006;281:18363–18369. doi: 10.1074/jbc.M601543200. [DOI] [PubMed] [Google Scholar]
- 162.Jia S, et al. Pax9’s interaction with the ectodysplasin signaling pathway during the patterning of dentition. Front Physiol. 2020;11:581843. doi: 10.3389/fphys.2020.581843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kist R, et al. Reduction of Pax9 gene dosage in an allelic series of mouse mutants causes hypodontia and oligodontia. Hum. Mol. Genet. 2005;14:3605–3617. doi: 10.1093/hmg/ddi388. [DOI] [PubMed] [Google Scholar]
- 164.Iurino DA, Sardella R. CT scanning analysis of Megantereon whitei (Carnivora, Machairodontinae) from Monte Argentario (Early Pleistocene, central Italy): evidence of atavistic teeth. Naturwissenschaften. 2014;101:1099–1106. doi: 10.1007/s00114-014-1249-0. [DOI] [PubMed] [Google Scholar]
- 165.Klein OD, et al. Developmental disorders of the dentition: an update. Am. J. Med. Genet C. Semin Med. Genet. 2013;163C:318–332. doi: 10.1002/ajmg.c.31382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Lubinsky M, Kantaputra PN. Syndromes with supernumerary teeth. Am. J. Med. Genet A. 2016;170:2611–2616. doi: 10.1002/ajmg.a.37763. [DOI] [PubMed] [Google Scholar]
- 167.Madani M, Madani F. Gardner’s syndrome presenting with dental complaints. Arch. Iran. Med. 2007;10:535–539. [PubMed] [Google Scholar]
- 168.Panjwani S, Bagewadi A, Keluskar V, Arora S. Gardner’s syndrome. J. Clin. Imaging Sci. 2011;1:65. doi: 10.4103/2156-7514.92187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Dinckan N, et al. Whole-exome sequencing identifies novel variants for tooth agenesis. J. Dent. Res. 2018;97:49–59. doi: 10.1177/0022034517724149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Moosa S, et al. Autosomal-recessive mutations in MESD cause osteogenesis imperfecta. Am. J. Hum. Genet. 2019;105:836–843. doi: 10.1016/j.ajhg.2019.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Yu M, et al. Lrp6 dynamic expression in tooth development and mutations in oligodontia. J. Dent. Res. 2021;100:415–422. doi: 10.1177/0022034520970459. [DOI] [PubMed] [Google Scholar]
- 172.Lammi L, et al. Mutations in AXIN2 cause familial tooth agenesis and predispose to colorectal cancer. Am. J. Hum. Genet. 2004;74:1043–1050. doi: 10.1086/386293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Hlouskova A, Bielik P, Bonczek O, Balcar VJ, Sery O. Mutations in AXIN2 gene as a risk factor for tooth agenesis and cancer: A review. Neuroendocrinol. Lett. 2017;38:131–137. [PubMed] [Google Scholar]
- 174.Kuchler EC, et al. Tooth agenesis association with self-reported family history of cancer. J. Dent. Res. 2013;92:149–155. doi: 10.1177/0022034512468750. [DOI] [PubMed] [Google Scholar]
- 175.Bonczek O, Balcar VJ, Sery O. PAX9 gene mutations and tooth agenesis: a review. Clin. Genet. 2017;92:467–476. doi: 10.1111/cge.12986. [DOI] [PubMed] [Google Scholar]
- 176.Bhol C. S., Patil S., Sahu B. B., Patra S. K., Bhutia S. K. The clinical significance and correlative signaling pathways of paired box gene 9 in development and carcinogenesis. Bba-Rev Cancer. 1876,188561 (2021). [DOI] [PubMed]
- 177.Longtin R. Chew on this: mutation may be responsible for tooth loss, colon cancer. J. Natl Cancer I. 2004;96:987–989. doi: 10.1093/jnci/96.13.987. [DOI] [PubMed] [Google Scholar]
- 178.Paranjyothi MV, et al. Tooth agenesis: a susceptible indicator for colorectal cancer? J. Cancer Res. Ther. 2018;14:527–531. doi: 10.4103/0973-1482.168997. [DOI] [PubMed] [Google Scholar]
- 179.Huang AH, Chen YK, Lin LM, Shieh TY, Chan AW. Isolation and characterization of dental pulp stem cells from a supernumerary tooth. J. Oral. Pathol. Med. 2008;37:571–574. doi: 10.1111/j.1600-0714.2008.00654.x. [DOI] [PubMed] [Google Scholar]
- 180.Kim YH, et al. Oncostatin M enhances osteogenic differentiation of dental pulp stem cells derived from supernumerary teeth. Biochem Biophys. Res. Commun. 2020;529:169–174. doi: 10.1016/j.bbrc.2020.06.013. [DOI] [PubMed] [Google Scholar]
- 181.Honda M, Sato M, Toriumi T. Characterization of coronal pulp cells and radicular pulp cells in human teeth. J. Endod. 2017;43:S35–S39. doi: 10.1016/j.joen.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 182.Laurikkala J, Kassai Y, Pakkasjarvi L, Thesleff I, Itoh N. Identification of a secreted BMP antagonist, ectodin, integrating BMP, FGF, and SHH signals from the tooth enamel knot. Dev. Biol. 2003;264:91–105. doi: 10.1016/j.ydbio.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 183.Kratochwil K, Galceran J, Tontsch S, Roth W, Grosschedl R. FGF4, a direct target of LEF1 and Wnt signaling, can rescue the arrest of tooth organogenesis in Lef1(-/-) mice. Genes Dev. 2002;16:3173–3185. doi: 10.1101/gad.1035602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Charles C, et al. Regulation of tooth number by fine-tuning levels of receptor-tyrosine kinase signaling. Development. 2011;138:4063–4073. doi: 10.1242/dev.069195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Chen Y, Wang Z, Lin C, Hu X, Zhang Y. Activated epithelial FGF8 signaling induces fused supernumerary incisors. J. Dent. Res. 2022;101:458–464. doi: 10.1177/00220345211046590. [DOI] [PubMed] [Google Scholar]
- 186.Ohazama A, et al. Primary cilia regulate Shh activity in the control of molar tooth number. Development. 2009;136:897–903. doi: 10.1242/dev.027979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Mustonen T, et al. Stimulation of ectodermal organ development by Ectodysplasin-A1. Dev. Biol. 2003;259:123–136. doi: 10.1016/S0012-1606(03)00157-X. [DOI] [PubMed] [Google Scholar]
- 188.Peterkova R, Lesot H, Viriot L, Peterka M. The supernumerary cheek tooth in tabby/EDA mice - a reminiscence of the premolar in mouse ancestors. Arch. Oral. Biol. 2005;50:219–225. doi: 10.1016/j.archoralbio.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 189.Peterkova R, Lesot H, Peterka M. Phylogenetic memory of developing mammalian dentition. J. Exp. Zool. Part B. 2006;306b:234–250. doi: 10.1002/jez.b.21093. [DOI] [PubMed] [Google Scholar]
- 190.Charles C, et al. Distinct impacts of Eda and Edar loss of function on the mouse dentition. PLoS One. 2009;4:e4985. doi: 10.1371/journal.pone.0004985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Laugel-Haushalter V., et al. RSK2 is a modulator of craniofacial development. PLoS One9, 0084343 (2014). [DOI] [PMC free article] [PubMed]
- 192.Zhang QH, et al. Loss of the Tg737 protein results in skeletal patterning defects. Dev. Dynam. 2003;227:78–90. doi: 10.1002/dvdy.10289. [DOI] [PubMed] [Google Scholar]
- 193.Saito K, et al. Loss of stemness, EMT, and supernumerary tooth formation in Cebpb(−/−)Runx2(+/−) murine incisors. Sci. Rep. 2018;8:5169. doi: 10.1038/s41598-018-23515-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Kaufman MH, Chang HH, Shaw JP. Craniofacial abnormalities in homozygous small eye (Sey/Sey) embryos and newborn mice. J. Anat. 1995;186:607–617. [PMC free article] [PubMed] [Google Scholar]
- 195.Danforth CH. The occurrence and genetic behavior of duplicate lower incisors in the mouse. Genetics. 1958;43:139–148. doi: 10.1093/genetics/43.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Nakamura T, et al. Transcription factor epiprofin is essential for tooth morphogenesis by regulating epithelial cell fate and tooth number. J. Biol. Chem. 2008;283:4825–4833. doi: 10.1074/jbc.M708388200. [DOI] [PubMed] [Google Scholar]
- 197.Chu EY, et al. Full spectrum of postnatal tooth phenotypes in a novel Irf6 cleft lip model. J. Dent. Res. 2016;95:1265–1273. doi: 10.1177/0022034516656787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Kuraguchi M, et al. Adenomatous polyposis coli (APC) is required for normal development of skin and thymus. Plos Genet. 2006;2:1362–1374. doi: 10.1371/journal.pgen.0020146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Cobourne MT, et al. Sonic hedgehog signalling inhibits palatogenesis and arrests tooth development in a mouse model of the nevoid basal cell carcinoma syndrome. Dev. Biol. 2009;331:38–49. doi: 10.1016/j.ydbio.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Pispa J, et al. Tooth patterning and enamel formation can be manipulated by misexpression of TNF receptor Edar. Dev. Dyn. 2004;231:432–440. doi: 10.1002/dvdy.20138. [DOI] [PubMed] [Google Scholar]
- 201.Zhao H, Oka K, Bringas P, Kaartinen V, Chai Y. TGF-beta type I receptor Alk5 regulates tooth initiation and mandible patterning in a type II receptor-independent manner. Dev. Biol. 2008;320:19–29. doi: 10.1016/j.ydbio.2008.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Li CY, et al. alphaE-catenin inhibits YAP/TAZ activity to regulate signalling centre formation during tooth development. Nat. Commun. 2016;7:12133. doi: 10.1038/ncomms12133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Shimizu T, Han J, Asada Y, Okamoto H, Maeda T. Localization of am3 using EL congenic mouse strains. J. Dent. Res. 2005;84:315–319. doi: 10.1177/154405910508400404. [DOI] [PubMed] [Google Scholar]
- 204.Wang XP, et al. Modulation of activin/bone morphogenetic protein signaling by follistatin is required for the morphogenesis of mouse molar teeth. Dev. Dynam. 2004;231:98–108. doi: 10.1002/dvdy.20118. [DOI] [PubMed] [Google Scholar]
- 205.Cascallana JL, et al. Ectoderm-targeted overexpression of the glucocorticoid receptor induces hypohidrotic ectodermal dysplasia. Endocrinology. 2005;146:2629–2638. doi: 10.1210/en.2004-1246. [DOI] [PubMed] [Google Scholar]
- 206.Symkhampha K, et al. Radiographic features of cleidocranial dysplasia on panoramic radiographs. Imaging Sci. Dent. 2021;51:271–278. doi: 10.5624/isd.20201007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Mundlos S. Cleidocranial dysplasia: clinical and molecular genetics. J. Med. Genet. 1999;36:177–182. [PMC free article] [PubMed] [Google Scholar]
- 208.Xue R, Zhang G, Chen X, Ye X. Cleidocranial dysplasia causing respiratory distress in neonates: a case report and literature review. Front Genet. 2021;12:696685. doi: 10.3389/fgene.2021.696685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Ryoo HM, Kang HY, Lee SK, Lee KE, Kim JW. RUNX2 mutations in cleidocranial dysplasia patients. Oral. Dis. 2010;16:55–60. doi: 10.1111/j.1601-0825.2009.01623.x. [DOI] [PubMed] [Google Scholar]
- 210.Half E, Bercovich D, Rozen P. Familial adenomatous polyposis. Orphanet J. Rare Dis. 2009;4:22. doi: 10.1186/1750-1172-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Gjorup H, Haubek D, Jacobsen P, Ostergaard JR. Nance-horan syndrome-the oral perspective on a rare disease. Am. J. Med. Genet A. 2017;173:88–98. doi: 10.1002/ajmg.a.37963. [DOI] [PubMed] [Google Scholar]
- 212.De Souza N, Chalakkal P, Martires S, Soares R. Oral manifestations of nance-horan syndrome: a report of a rare case. Contemp. Clin. Dent. 2019;10:174–177. doi: 10.4103/ccd.ccd_490_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Seow WK, Brown JP, Romaniuk K. The Nance-Horan syndrome of dental anomalies, congenital cataracts, microphthalmia, and anteverted pinna: case report. Pediatr. Dent. 1985;7:307–311. [PubMed] [Google Scholar]
- 214.Ng D, et al. Oculofaciocardiodental and Lenz microphthalmia syndromes result from distinct classes of mutations in BCOR. Nat. Genet. 2004;36:411–416. doi: 10.1038/ng1321. [DOI] [PubMed] [Google Scholar]
- 215.Oberoi S, Winder AE, Johnston J, Vargervik K, Slavotinek AM. Case reports of oculofaciocardiodental syndrome with unusual dental findings. Am. J. Med. Genet A. 2005;136:275–277. doi: 10.1002/ajmg.a.30811. [DOI] [PubMed] [Google Scholar]
- 216.Ragge N, et al. Expanding the phenotype of the X-linked BCOR microphthalmia syndromes. Hum. Genet. 2019;138:1051–1069. doi: 10.1007/s00439-018-1896-x. [DOI] [PubMed] [Google Scholar]
- 217.Brooks JK, Leonard CO, Coccaro PJ., Jr Opitz (BBB/G) syndrome: oral manifestations. Am. J. Med. Genet. 1992;43:595–601. doi: 10.1002/ajmg.1320430318. [DOI] [PubMed] [Google Scholar]
- 218.Hu CH, et al. A MID1 gene mutation in a patient with opitz G/BBB syndrome that altered the 3D structure of SPRY domain. Am. J. Med. Genet. Part A. 2012;158a:726–731. doi: 10.1002/ajmg.a.35216. [DOI] [PubMed] [Google Scholar]
- 219.Schweiger S, Schneider R. The MID1/PP2A complex: a key to the pathogenesis of Opitz BBB/G syndrome. Bioessays. 2003;25:356–366. doi: 10.1002/bies.10256. [DOI] [PubMed] [Google Scholar]
- 220.Patton MA, Afzal AR. Robinow syndrome. J. Med. Genet. 2002;39:305–310. doi: 10.1136/jmg.39.5.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Mazzeu JF, et al. Clinical characterization of autosomal dominant and recessive variants of Robinow syndrome. Am. J. Med. Genet A. 2007;143:320–325. doi: 10.1002/ajmg.a.31592. [DOI] [PubMed] [Google Scholar]
- 222.van Genderen MM, Kinds GF, Riemslag FC, Hennekam RC. Ocular features in Rubinstein-Taybi syndrome: investigation of 24 patients and review of the literature. Br. J. Ophthalmol. 2000;84:1177–1184. doi: 10.1136/bjo.84.10.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Stevens C. A. GeneReviews (Springer Nature, 1993).
- 224.Trippella G, et al. An early diagnosis of trichorhinophalangeal syndrome type 1: a case report and a review of literature. Ital. J. Pediatr. 2018;44:138. doi: 10.1186/s13052-018-0580-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Carrington PR, Chen H, Altick JA. Trichorhinophalangeal syndrome, type I. J. Am. Acad. Dermatol. 1994;31:331–336. doi: 10.1016/S0190-9622(94)70166-0. [DOI] [PubMed] [Google Scholar]