Abstract
The field of human space travel is in the midst of a dramatic revolution. Upcoming missions are looking to push the boundaries of space travel, with plans to travel for longer distances and durations than ever before. Both the National Aeronautics and Space Administration (NASA) and several commercial space companies (e.g., Blue Origin, SpaceX, Virgin Galactic) have already started the process of preparing for long-distance, long-duration space exploration and currently plan to explore inner solar planets (e.g., Mars) by the 2030s. With the emergence of space tourism, space travel has materialized as a potential new, exciting frontier of business, hospitality, medicine, and technology in the coming years. However, current evidence regarding human health in space is very limited, particularly pertaining to short-term and long-term space travel. This review synthesizes developments across the continuum of space health including prior studies and unpublished data from NASA related to each individual organ system, and medical screening prior to space travel. We categorized the extraterrestrial environment into exogenous (e.g., space radiation and microgravity) and endogenous processes (e.g., alteration of humans’ natural circadian rhythm and mental health due to confinement, isolation, immobilization, and lack of social interaction) and their various effects on human health. The aim of this review is to explore the potential health challenges associated with space travel and how they may be overcome in order to enable new paradigms for space health, as well as the use of emerging Artificial Intelligence based (AI) technology to propel future space health research.
Keywords: human health, space travel, space mission, space exploration, space radiation, microgravity
1. Introduction
Until now space missions have generally been either of short distance (Low Earth Orbit—LEO) or short duration (Apollo Lunar Missions). However, upcoming missions are looking to push the boundaries of space travel, with plans to travel for longer distances and durations than ever before. Both the National Aeronautics and Space Administration (NASA) and several commercial space companies (e.g., Blue Origin, SpaceX) have already started the process of preparing for long distance, long-duration space exploration and currently plan to explore inner solar planets (e.g., Mars) by the 2030s [1].
Within the extraterrestrial environment, a multitude of exogenous and endogenous processes could potentially impact human health in several ways. Examples of exogenous processes include exposure to space radiation and microgravity while in orbit. Space radiation poses a risk to human health via a number of potential mechanisms (e.g., alterations of gut microbiome biosynthesis, accelerated atherosclerosis, bone remodeling, and hematopoietic effects) and prolonged microgravity exposure presents additional potential health risks (e.g., viral reactivation, space motion sickness, muscle/bone atrophy, and orthostatic intolerance) [2,3,4,5,6,7]. Examples of endogenous processes potentially impacted by space travel include alteration of humans’ natural circadian rhythm (e.g., sleep disturbances) and mental health disturbances (e.g., depression, anxiety) due to confinement, isolation, immobilization, and lack of social interaction [8,9,10]. Finally, the risk of unknown exposures, such as yet undiscovered pathogens, remain persistent threats to consider. Thus, prior to the emergence of long distance, long duration space travel it is critical to anticipate the impact of these varied environmental factors and identify potential mitigating strategies. Here, we review the available medical literature on human experiments conducted during space travel and summarize our current knowledge on the effects of living in space for both short and long durations of time. We also discuss the potential countermeasures currently employed during interstellar travel, as well as future directions for medical research in space.
1.1. Medical Screening and Certification Prior to Space Travel
When considering preflight medical screening and certification, the requirements and recommendations vary based on the duration of space travel. Suborbital spaceflight, part of the new era of space travel, has participants launching to the edge of space (defined as the Karman line, 100 Km above mean sea level) for brief 3–5 min microgravity exposures. Orbital spaceflight, defined as microgravity exposure for up to 30 days, involves healthy individuals with preflight medical screening. In addition to a physical examination and metabolic screening, preflight medical screening assessing aerobic capacity (VO2max), and muscle strength and function may be sufficient to ensure proper conditioning prior to mission launch [11,12,13,14]. Age-appropriate health screening tests (e.g., colonoscopy, serum prostate specific antigen in men, and mammography in women) are generally recommended for astronauts in the same fashion as their counterparts on Earth. In individuals with cardiovascular risk factors or with specific medical conditions, additional screening may be required [15]. The goal of these preflight screening measures is to ensure that medical conditions that may result in sudden incapacitation are identified and either disqualified or treated before the mission begins. In addition to the medical screening described above, short-duration space travelers are also required to undergo acceleration training, hypobaric and hypoxia exposure training, and hypercapnia awareness procedures as part of the preflight training phase.
In preparation for long-duration space travel, astronauts generally undergo a general physical examination, as well as imaging and laboratory studies at the time of initial selection. These screening tests would then be repeated annually, as well as upon assignment to an International Space Station (ISS) mission. ISS crew members are medically certified for long-duration spaceflight missions through individual agency medical boards (e.g., NASA Aerospace Medical Board) and international medical review boards (e.g., Multilateral Space Medicine Board) [16,17]. In order for an individual to become certified for long-duration space travel, an individual must be at the lowest possible risk for the occurrence of medical events during the preflight, infight, and postflight periods. Following spaceflight, it is recommended that returning astronauts undergo occupational surveillance for the remainder of their lifetime for the detection of health issues related to space travel (e.g., NASA’s Lifetime Surveillance of Astronaut Health program) [18]. Table 1 summarizes the preflight, inflight, and postflight screening recommendations for each organ system. Further research utilizing data from either long-term space missions or simulated environments is required in order to develop an adequate preflight scoring system capable of predicting inflight and postflight health outcomes in space travelers based on various risk factors.
Table 1.
Summarizes the pre-flight, in-flight and post-flight screening in each system.
| Scheme | Pre-Flight | In-Flight | Post-Flight |
|---|---|---|---|
| Physical Fitness Assessment | Cardiovascular fitness: VO2max measured cycle ergometry Flexibility: Sit & reach; shoulder flexibility Muscular strength and endurance: Maximum push-ups in 2 min; maximum sit-ups in 2 min; maximum pull-ups; handgrip strength with dynamometer |
Cardiovascular fitness: Flight day (FD) +30, +120, return day (R) −30 VO2max
FD+3 through day prior to return. Resistance: 3x/wk (60 min) Aerobic: 3x/wk (30 min) |
Functional fitness assessment: R+7, R+30 Cardiovascular fitness: R+7, R+30 VO2max |
| Cardiovascular | Coronary artery calcium (CAC) score every 5 years Echocardiogram annually VO2max cycle test annually Fasting lipid panel High Sensitivity C-Reactive Peptide (HS-CRP) Carotid Intima-Media Thickness (CIMT) annually Individuals with cardiovascular disease history (e.g., compensated heart failure, asymptomatic CAD, arrhythmias) are not currently eligible for either long- or short-term space travel |
Quarterly VO2max cycle testing Quarterly vascular US Monthly health surveillance exam with blood pressure measurement |
VO2max cycle test at R+7, R+30 Resting 12-lead ECG annually Blood pressure measurement Echocardiogram Fasting lipid panel HS-CRP Hypertension screening using a sphygmomanometer annually and as clinically indicated Cardiovascular health screening annually |
| Pulmonology | Pulmonary function testing annually 6-Minute Walk Test for patients with chronic pulmonary disease |
None | Pulmonary function testing Purified Protein Derivative (PPD) (tuberculin) skin test for tuberculosis screening, unless clinically contraindicated |
| Ophthalmology | SANS-surveillance, to include baseline testing of: Visual acuity OCT US MRI orbits Tonometry Ophthalmologic examination Color vision Phoria testing Ophthalmologic screening for ocular health and visual status (e.g., testing for refractive errors or cataracts) is recommended |
See attached chart for inflight scheduling details | Visual acuity, color vision, and extraocular muscle testing (annually) Tonometry (annually) Dilated fundus exam, retinal photographs, and optical coherence tomography (OCT) |
| Otorhinolaryngology | Screening audiometry Tympanography |
Quarterly On Orbit Hearing Assessment (OOHA) | Hearing questionnaire and pure-tone audiometry testing (annually) |
| Hematology | Complete Blood Count (CBC) with differential Iron studies |
CBC every 60 days | CBC, CMP (annually) |
| Immunology | Administration of vaccines (e.g., Shingrix) for prevention of inflight VZV reactivation Immunoglobulins (annually) TB screening with PPD, Quantiferon Gold |
None | NASA has recommended post-flight quarantine and immune status monitoring (i.e., immune-boosting protocol) to mitigate the risk of infection |
| Gastroenterology | Age appropriate colon cancer screening | None | Lifetime Surveillance of Astronaut Health (LSAH) |
| Musculoskeletal | Annual DXA for osteoporosis screening for postmenopausal females and males >50 years old Cervical and thoracic spine MRI |
None | Post-flight DXA for BMD Spine MRI |
| Dermatology | Annual skin examination | None | Visual exam of the skin with photo documentation of any abnormalities, particularly for melanoma and non-melanoma skin cancers (R+0/1 day and annually) |
| Genitourinary | PSA in males Annual urinalysis, 24-h urine collection |
Quarterly 24-h urine collection | Urinalysis 24-h urine collection |
| Neurology | MRI brain Neurovestibular platform test |
None | Neurovestibular platform test |
| Endocrine | TSH, free T4 Thyroid US |
None | Annual TSH, free T4 |
| Dental | Annual dental examinations Orthopantomogram X-rays |
None | Post-flight dental examination |
| Oncology | Age-appropriate pap smear and mammogram in females Age-appropriate colon cancer screening |
Below we discuss potential Space Hazards for each organ system along with possible countermeasures (Table 2). Table 3 lists prospective opportunities for artificial intelligence (AI) implementation.
Table 2.
Summary of Space Hazards to each organ system and potential countermeasures.
| Tread/Hazards | Health Risks | Current Countermeasure |
|---|---|---|
| Microgravity | ||
| Musculoskeletal | Muscle and bone atrophy [19] | A combination of adequate exercise and antiresorptive medications [20,21] |
| Impaired wound healing [22,23,24] | No specific countermeasures exist | |
| Neurology | Space motion sickness (SMS) [25] | Scopolamine administered orally or via transdermal patch with or without an amphetamine (to counteract drowsiness), or intramuscular Promethazine [26] |
| Alterations of smell and taste [27] | No specific countermeasures exist | |
| Self-reported congestion [27] | Lower body negative pressure may help, but the effects are transient | |
| Internal jugular vein thrombosis [28,29] | No specific countermeasures exist | |
| Post-flight motion sickness [30] | No specific countermeasures exist | |
| Immunology | Reactivation of latent viruses [31,32] | Preflight vaccination [32] Treatment with polyclonal immunoglobulin (IG) and Interleukin-2 (SC) [33] Adequate exercise and nutrition [33] |
| Hypersensitivity [34] | No specific countermeasures exist | |
| Gastroenterology | Gut microbiota dysbiosis [2] | Probiotics, synthetic peptides, synthetic biology [35,36,37,38] |
| Acute appendicitis and cholecystitis | Inflight medical management or minimally invasive procedures (e.g., ultrasound guided percutaneous drainage) of traditionally “surgical” conditions. [39] Alternatively, can consider prophylactic minimally invasive surgery prior to prolonged space flight in at-risk individuals [40] | |
| Cardiovascular | Orthostatic intolerance [41] | Regular exercise training and adequate hydration prior to landing |
| Cardiac myocyte atrophy [42] | Restores back to baseline after returning from spaceflight | |
| Ophthalmology | Spaceflight-Associated Neuro-Ocular Syndrome (SANS) [43] | The lower body negative pressure device has been proposed as a countermeasure but is currently unproven |
| Dermatology | Skin tinning, dry skin, delayed wound healing, or skin infections [44] | No specific countermeasures exist |
| Traumatology | Increased risk of traumatic injury with construction, inadvertent acceleration of large masses when in zero gravity, impaired physiologic responses to hemorrhage and shock in zero gravity, bone demineralization increases risk of traumatic fractures, micrometeorites in EVA activities [45,46,47] | No specific countermeasures exist |
| Radiation | ||
| Most systems | Cancer induction | Shielding, including advanced shielding options. [48,49] Optimize mission according to solar cycle [48,49] Sex- and age-based selection criteria for astronauts [48] |
| Musculoskeletal | Bone cell remodeling [6] | Shielding [7] |
| Hematology | Acute hematopoietic effects [7] | Shielding [7] |
| Space-related hemolytic anemia [50,51] | Screening and monitoring for hemolysis | |
| Neurology | Neuro-degenerative disorders and central nervous system changes [52,53,54,55,56] | Adaptive visuo-motor training, active sensory feedback to guide task performance, galvanic vestibular stimulation (GVS) |
| Gastroenterology | Gut microbiota dysbiosis [2] | Probiotics, synthetic peptides, synthetic biology [35,36,37,38] |
| Cardiovascular | Accelerated atherosclerosis [3,4,57,58,59,60] | Shielding [7] |
| Ophthalmology | Radiation-induced cataract [61,62] | No specific countermeasures exist |
| Pulmonology | Lung adenocarcinomas and squamous cell carcinomas [63] | Shielding [7] |
| Dermatology | Melanoma and non-melanoma skin cancers [44] | Inflight telediagnostic system |
| Others | ||
| Nutrition | Nutritional deficiencies [64] | Telehealth and routine lab work for identification of nutritional deficiencies, and adequate supplementation as needed |
| Mental health | Psychologic distress [10,65] | Stress-relieving breathing exercises and/or mindfulness/positive visualization exercises [66] |
| Depression, confinement, isolation, immobilization lack of social interaction [10,65,67] | Telepsychiatry, telepsychotherapy, space social media using LunaNet [68,69,70]. | |
| Altered circadian rhythms | Circadian de-synchronization and sleep loss [71] | Melatonin supplementation may be useful [72] |
| Dust exposure | Extraterrestrial dust exposure [73] | No specific countermeasures exist |
| Auditory exposures | Noise generated from man-made sources such as mechanical equipment (Noise/sound does not propagate in the vacuum of space and it requires an atmosphere to propagate, e.g., the pressurized spacecraft interior) [74] | Hearing protection in the form of foam ear plugs [74] |
| Unknown infections | Mission-threatening risks from unknown infections or novel bacterial/viral phenotypes [75,76] | PPE and post-exposure quarantine [77] |
Table 3.
Potential AI applications in space health.
| Potential AI Applications |
|---|
| Risk Prediction Models |
| Risk prediction models for development of cancer due to ionizing radiation exposure based on animal models [78,79] |
| Inflight AI assisted multi-omic research using the Edge TPU to generate novel risk prediction scores [80] |
| Risk prediction models for the development of cardiovascular disease based on carotid-femoral pulse wave velocity obtained via Doppler ultrasound or AI-guided analysis of 3D printed tissue models [81] |
| Risk prediction models such as the modified Astro-CHARM model which combines a patient’s CAC score with non-traditional risk factors associated with space travel (e.g., radiation exposure, microgravity exposure, dysbiosis of gut microbiota, etc.) to identify those at risk for accelerated atherosclerosis [82] |
| Predicting antimicrobial resistance of novel bacterial species (e.g., Methylobacterium ajmalii sp. nov., Methylobacterium rhodesianum, etc.) based on whole genome sequencing data [83] |
| AI-based models for the identification of causal relationships between various exposures and subsequent cancer development (e.g., CRISP) [84] |
| Medical Screening Preflight and Inflight Monitoring |
| AI monitoring for gut microbiota dysbiosis using smart toilets during pre-, intra-, and post-flight periods [2,85,86] |
| Screening for latent virus infection or reactivation based on immunological variables, which can then be used as a biomarker for assessment of adaptive immune function [87,88] |
| The Edge TPU and other similar low-power AI ASICs could be used to monitor genomic imprinting (e.g., DNA methylation signatures or epigenetic/transcriptomic-based tests) for inflight lung cancer screening (may be equivalent to low-dose CT chest screening) [63,89,90] |
| AI screening for mental illness through facial recognition and vocal analysis [68,69] |
| A combination of AI and imaging could potentially identity abnormal or misfolded proteins [91,92] |
| Deep learning algorithms for the inflight telediagnosis of various conditions (e.g., skin lesions or SANS) [93,94,95] |
| AI-integrated wearable technology for space suits (e.g., exoskeletons) to monitor biodata (e.g., electrocardiogram, blood pressure, sleep cycle, body temperature, etc.) [96,97] |
| AI monitoring of metabolomics-based biomarkers for assessment of sleep quality and circadian rhythm [98] |
| AI can be used to analyze retinal fundus photography to identify and monitor space anemia [99] |
| Medical Diagnostic Tools |
| The Edge TPU and other similar low-power AI ASICs (i.e., Google Coral Edge TPU, NVIDIA Jetson Nano, Intel Neural Compute Stick 2) could advance image segmentation AI models, allowing for these models to be feasibly deployed in ultrasound point-of-care settings (e.g., detection of DVT, structural heart disease, hemodynamic changes), even procedural guidance [100]. |
| AI-based system designed to guide non-physicians on the proper acquisition of medical diagnostic testing using The Edge TPU and deep reinforcement learning |
| AI-enhanced 3D-imaging technology (e.g., micro-CT scanners) [101] |
| Utilization of the Edge TPU and other similar low-power AI ASICs to provide the necessary processing power for high-performance parallel-processing space research [102] |
| Intervention |
| AI-guided minor surgical procedures [such as incision and drainage (I&D)] using next-generation High Performance Spaceflight Computing (HPSC) [103] |
| AI-assisted, remotely controlled robotic PCI and robotic laparoscopic surgery (e.g., telecholecystectomy and teleappendectomy); made possible by a reduction in communication latency beyond a lag of 200 ms [103,104,105,106,107] |
| Using AI predictions of drug metabolism and effectiveness based on an individual’s multiomic data prior to medication or supplement distribution (e.g., melatonin, immune supplements, probiotics) [108,109] |
| Disease Prevention |
| AI-integrated space suits (e.g., exoskeletons) to maximize EVA time and operating pressure, and minimize space radiation exposure [110,111] |
| 3D printing of personalized devices (e.g., ear plugs to prevent noise source generated from man-made sources), space shields, space suits for use in emergency scenarios [112,113,114] |
| AI-based chatbots or social media could potentially be used to prevent anxiety and depression during long-duration space travel. The Edge TPU could potentially be used in advancing an internet or social media for the moon, known as LunaNet [115]. |
| AI-improved augmented reality/virtual reality to reduce/prevent Spaceflight-Associated Neuro-Ocular Syndrome (SANS), space motion sickness (SMS), and post-flight motion sickness (PFMS) [116,117,118] |
| AI identification of an individual’s radiosensitivity (genotype-phenotype) using multiomics to prevent the negative effects of ionizing radiation [119,120,121] |
| Emerging technology could allow for the transfer of large volumes of data at faster rates in order to facilitate medical research in space [122] |
| AI can be used to create novel metrics (e.g., travelers’ satisfactions, post spaceflight measurements for travelers) and ethics (e.g., health insurance) |
1.2. Effects on the Cardiovascular System
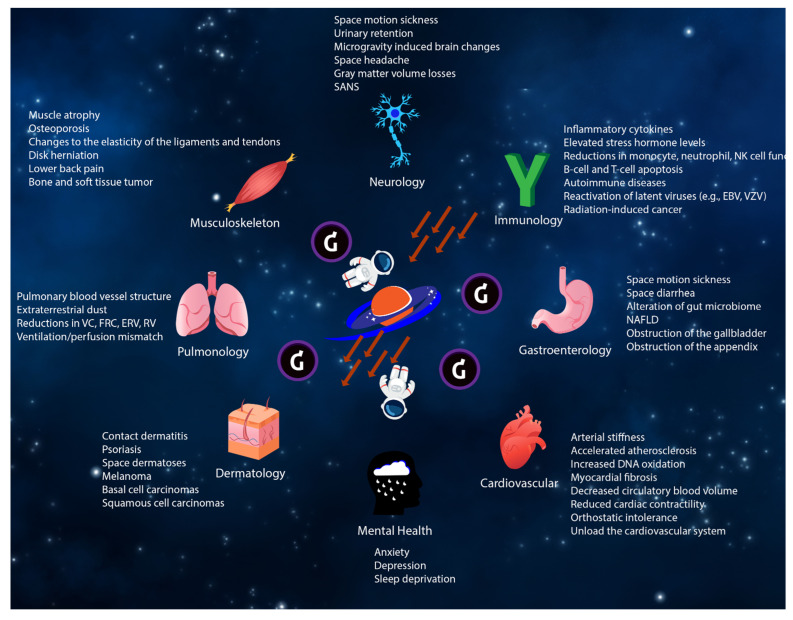
During short-duration spaceflight, microgravity alters cardiovascular physiology by reducing circulatory blood volume, diastolic blood pressure, left ventricular mass, and cardiac contractility [42,123]. Several studies have demonstrated that peak exercise performance is reduced both inflight and immediately after short-duration spaceflight due primarily to a reduction in maximal cardiac output and O2 delivery [124,125]. Prolonged exposure to microgravity does cause unloading of the cardiovascular system (e.g., removal of expected loading effects from Earth’s gravity when upright during the day), resulting in cardiac atrophy. These changes may be an example of adaptive physiologic changes (“physiologic atrophy”) that returns to baseline after returning from spaceflight. This process may be similar to the adaptive physiologic changes to the cardiovascular system seen during athletic training (“physiologic hypertrophy”). Thus far, there is no evidence that the observed short-term cardiac atrophy could permanently impair systolic function. However, this physiologic adaptation to microgravity in space could lead to orthostatic hypotension/intolerance upon returning to Earth’s gravity due to changes in the comparative position of peripheral resistance and sympathetic nerve activity [41,126,127]. Figure 1 demonstrates potential effects of the space environment on each organ system.
Figure 1.
Potential effects of the space environment on each organ system.
Another potential effect of microgravity exposure is that an alteration of hydrostatic forces in the vertical gravitational (Gz) axis could lead to the formation of internal jugular vein thromboses [28,29]. Anticoagulation would not be an ideal choice for prevention as astronauts have an increased risk of suffering traumatic injury during spaceflight, thus potentially inflating the risk of developing an intracerebral hemorrhage or subdural hematoma. In addition, if a traumatic accident were to occur during spaceflight, the previously discussed cardiovascular adaptations could impair the body’s ability to tolerate blood loss and shock [45,46,47].
During long-duration spaceflight, one recent study demonstrated that astronauts did not experience orthostatic hypotension/intolerance during routine activities or after landing following 6 months in space [128]. It is worth noting that all of these astronauts performed aggressive exercise countermeasures while in flight [128]. Another study of healthy astronauts after 6 months of space travel showed that the space environment caused transient changes in left atrial structure/electrophysiology, increasing the risk of developing atrial fibrillation (AF) [129]. However, there was no definitive evidence of increased incidence of supraventricular arrhythmias and no identified episodes of AF [129]. Evaluation with echocardiography or cardiac MRI may be considered following long-duration spaceflight in certain cases.
Prior human studies with supplemental data obtained from animal studies, have shown that healthy individuals with prolonged exposure to ionizing radiation may be at increased risk for the development of accelerated atherosclerosis secondary to radiation-induced endothelial damage and a subsequent pro-inflammatory response [3,4,57,58,59,60,123]. One study utilizing human 3D micro-vessel models showed that ionizing radiation inhibits angiogenesis via mechanisms dependent on the linear energy transfer (LET) of charged particles [130], which could eventually lead to cardiac dysfunction [131,132]. In fact, specific characteristics of the radiation encountered in space may be an important factor to understanding its effects. For example, studies of pediatric patients undergoing radiotherapy have shown an increase in cardiac-related morbidity/mortality due to radiation exposure, but not until radiation doses exceeded 10 Gy [133]. At lower dose levels the risk is less clear: while a study of atomic bomb survivors with more than 50 years of followup demonstrated elevated cardiovascular risks at doses < 2 Gy [134]. A recent randomized clinical trial with a 20-year follow-up showed no increase in cardiac mortality in irradiated breast cancer patients with a median dose of 3.0 Gy (1.1–8.1 Gy) [135]. The uncertainty in cardiovascular effects of ionizing radiation, are accentuated in a space environment as the type and quality of radiation likely play an important role as well.
Further research is required to understand the radiation dosage, duration, and quality necessary for cardiovascular effects to manifest, as well as develop preventive strategies for AF and internal jugular vein thrombosis during space travel.
1.3. Effects on the Gastrointestinal System
During short-duration spaceflight, the presence of gastrointestinal symptoms (e.g., diarrhea, vomiting, and inflammation of the gastrointestinal tract) are common due to microgravity exposure [35,136,137]. Still unknown however is whether acute, surgical conditions such as cholecystitis and appendicitis occur more frequently due to microgravity-induced stone formation or alterations in human physiology/anatomy, and immunosuppression [40]. Controlling for traditional risk factors associated with the development of these conditions (e.g., adequate hydration, maintenance of a normal BMI, dietary fat avoidance, etc.) may help mitigate the risk.
During long-duration spaceflight, it is possible that prolonged radiation exposure could lead to radiation-induced gastrointestinal cancer. Gamma radiation exposure is a known risk factor for colorectal cancer via an absence of DNA methylation [138]. NASA has recently developed a space radiation simulator, named the “GCR Simulator”, which allows for the more accurate radiobiologic research into the development and mitigation of radiation-induced malignancies [139]. Preflight colorectal cancer screening via colonoscopy or inflight screening via gut microbiome monitoring may be beneficial, but further research is required to demonstrate their clinical utility. Several studies, including the NASA Twins study have shown that microgravity could lead to alterations in an individual’s gut microbial community (i.e., gut dysbiosis) [2,140,141,142]. While changes to an individual’s gut microbiome can cause inflammation of the gastrointestinal tract [143,144], it remains unclear whether the specific alterations observed during spaceflight pose a risk to astronaut health. In fact, increased gut colonization by certain bacterial species is even associated with a beneficial effect on the gastrointestinal tract [2,140]. (Table S1) Certain limitations of these studies, such as variations in genomic profile, diet, and a lack of adjusted confounders (e.g., the microbial content of samples) should be considered. Another potential consequence of prolonged microgravity exposure is the possibility of increased fatty-acid processing [145], leading to the development of non-alcoholic fatty liver disease (NAFLD) and hepatic fibrosis [146,147].
Further research is required to better understand gut microbial dynamics during space travel, as well as spaceflight-associated risk factors for the development of NAFLD, cholecystitis, and appendicitis.
1.4. Effects on the Immune System
During spaceflight, exposure to microgravity could potentially induce modifications in the cellular function of the human immune system. For example, it has been hypothesized that microgravity exposure could lead to an increase in the production of inflammatory cytokines [148] and stress hormones [149,150], alterations in the function of certain cell lines (NK cells [151,152], B cells [153], monocytes [154], neutrophils [154], T cells [5,155]), and impairments of leukocyte distribution [156] and proliferation [155,157,158]. The resultant immune system dysfunction could lead to the reactivation of latent viruses such as Epstein-Bar Virus (EBV), Varicella-Zoster Virus (VZV), and Cytomegalovirus (CMV) [31,32]. Persistent low-grade pro-inflammatory responses microgravity could lead to space fever. [159] Studies are currently underway to evaluate countermeasures to improve immune function and reduce reactivation of latent herpesviruses [33,160,161,162]. Microgravity exposure could also lead to the development of autoantibodies, predisposing astronauts to various autoimmune conditions [136,163]. (Table S2) Most importantly, studies have shown that bacteria encountered within the space environment appear to be more resistant to antibiotics and more harmful in general compared to bacteria encountered on Earth [164,165]. This is in addition to the threat of novel bacteria species (e.g., Methylobacterium ajmalii sp. Nov. [76]) that we have not yet discovered.
Upon returning from the space environment astronauts remain in an immunocompromised state, which has been particularly problematic in the era of the COVID-19 pandemic. Recently, NASA has recommended postflight quarantine and immune status monitoring (i.e., immune-boosting protocol) to mitigate the risk of infection [77]. This is similar to the Apollo and NASA Health Stabilization Programs that helped establish the preflight protocol (pre-mission quarantine) currently used for this purpose.
Further research is required to understand the mechanisms of antibiotic resistance and the modifications in inflammatory cytokine dynamics, in order to develop immune boosters and surrogate immune biomarkers.
1.5. Effects on the Hematologic System
During short-duration spaceflight, the plasma volume and total blood volume de-crease within the first hours and remain reduced throughout the inflight period, a finding previously identified as space anemia [166]. Space anemia during spaceflight is perhaps due to a normal physiologic adaptation of newly released blood cells and iron metabolism to microgravity [167].
During long-duration spaceflight, microgravity exposure could potentially induce hemoglobin degradation, leading to hemolytic anemia. In a recent study of 14 astronauts who were on 6-month missions onboard the ISS, a 54% increase in hemolysis was ob-served after landing one year later [50]. In another small study, nearly half of astronauts (48%) landing after long duration missions were anemic and hemoglobin levels were characterized as having a dose–response relationship with microgravity exposure [51]. An additional study collected whole blood sample from astronauts during and after up to 6 months of orbital spaceflight [168]. Upon analysis, once the astronauts returned to Earth RBC and hemoglobin levels were significantly elevated. It is worth noting that these studies analyzed blood samples from astronauts collected after spaceflight, which may be influenced by various factors (e.g., the stress of landing and re-adaptation to conditions on Earth). In addition, these studies may be confounded by other extraterrestrial environmental factors such as fluid shifts, dehydration, and alteration of the circadian cycle.
Further research is urgently needed to understand plasma volume physiology dur-ing spaceflight and delineate the etiology and degree of hemolysis with longer space exposure, such as 1-year ISS or Mars exploration missions.
1.6. Oncologic Effects
Even during short-duration spaceflight, the stochastic nature of cancer development makes it possible that space radiation exposure could cause cancer via epigenomic modifications [63]. Currently, our epidemiological understanding of radiation-induced cancer risk is based primarily on atomic bomb survivors and accidental radiation exposures, which both show a clear association between radiation exposure and cancer risk [169,170]. However, these studies are hard to generalize to spaceflight as the patient populations vary significantly (generally healthy astronauts vs. atomic bomb survivors [NCRP 126]) [171]. Moreover, the radiation encountered in space is notably different than that associated with atomic bomb exposure. Most terrestrial exposures are based on low LET radiation (e.g., atomic bomb survivors received <1% dose from high LET neutrons) [172], whereas space radiation is comprised of higher LET ions (solar energetic particles and galactic cosmic rays) [173,174].
During long-duration spaceflight, our current understanding of cancer risk is also largely unknown. Our current epidemiologic understanding of long-duration radiation exposure and cancer risk is primarily based on the study of chronic occupational exposures and medically exposed individuals, supplemented with data obtained from animal studies, which are again based overwhelmingly on low LET radiation [169,170,175,176]. In animal studies, exposure to ionizing radiation (up to 13.5 months) has been associated with an increased risk of developing a variety of cancers [162,177,178,179,180]. Ionizing radiation exposure may cause DNA methylation patterns similar to the specific patterns observed in human adenocarcinomas and squamous cell carcinomas [63]; however, this response is not yet certain [181,182].
For the purposes of risk prediction, the elevated biological potency of heavy ions is modeled through concepts such as the radiation weighting factor, with NASA recently releasing unique quality factors (QNASA) focused on high density tracks [183]. Although these predictive models can only estimate the impact of radiation exposure, extrapolation of current terrestrial-based data suggest that this risk could be at least substantial for astronauts. NASA, for example, has updated crew permissible career exposure limits to 0.6Sv, independent of age and sex. This degree of exposure results in a 2–3% mean increased risk of death from radiation carcinogenesis (NCRP 2021) [184]. This limit would be reached between 200 and 400 days of space travel (depending on degree of radiation shielding) [48].
Further research is urgently needed to understand the true risk of space radiation exposure. This is especially important for individuals with certain genotype-phenotype profiles (e.g., BRCA1 or DNA methylation signatures) who may be more sensitive to the effects of radiation exposure. Most importantly, the utilization of genotype-phenotype profiles of astronauts or space travelers is valuable not just for pre-flight screening, but also during in-flight travel, especially for long-duration flights to deeper space. An individual’s genetic makeup will in-variably change during spaceflight due to the shifting epigenetic microenvironment. Future crewed-missions to deep space will have to adapt to these anticipated changes, be-come aware of impending red-flag situations, and determine whether any meaningful shift or change to ones’ genetic makeup is possible. For example, personalized radiation shields could potentially be tailored to an individuals’ genotype-phenotype profile, individualized pulmonary capillary wedge pressure under microgravity may be different due to transient changes in left atrial structure, or preflight analysis of the globin gene for the prediction of space anemia [50,129,185]. This research should be designed to identify the radiation type, dose, quality, frequency, and duration of exposure required for cancer development.
1.7. Effects on the Neurologic System
During the initial days of spaceflight, space motion sickness (SMS) is the most commonly encountered neurologic condition. Microgravity exposure during spaceflight commonly leads to alterations in spatial orientation and gaze stabilization (e.g., shape recognition [186], depth perception and distance [187,188]). Postflight, impairments in object localization during pitch and roll head movements [189,190] and fine motor control (e.g., force modulation [191], keyed pegboard completion time [192], and bimanual coordination [193]) are common. Anecdotally, astronauts also reported alterations in smell and taste sensations during their missions [27,194,195]. The observed impairment in olfactory function is perhaps due to elevated intracranial pressure (ICP) with increased cerebrospinal fluid outflow along the cribriform plate pathways [196]. However, to date, there have been no studies directly measuring ICP during spaceflight.
Upon returning from spaceflight, studies have observed that astronauts experience decrements in postural and locomotor control that can increase fall risk [197]. These decrements have been observed in both standard sensorimotor testing and functional tasks. While recovery of sensorimotor function occurs rapidly following short-duration spaceflight (within the first several days after return) [192,198], recovery after long-duration spaceflight often takes several weeks. Similar to SMS, post-flight motion sickness (PFMS) is very common and occurs soon after g-transition [30]. Deficits in dexterity, dual-tasking, and vehicle operation [199] are also commonly observed immediately after spaceflight. Therefore, short-duration astronauts are recommended to not drive automobiles for several days, and only after a sensorimotor evaluation (similar to a field sobriety test).
Similarly to the effects seen following short-duration spaceflight, those returning from long-duration spaceflight can also experience deficits in dexterity, dual-tasking, and vehicle operation. Long-duration astronauts are recommended to not drive automobiles for several weeks, and also require a sensorimotor evaluation. While central nervous system (CNS) changes [53] associated with long-duration spaceflight are commonly observed, the resulting effects of these changes both during and immediately after spaceflight remain unclear [199]. Observed CNS changes include structural and functional alterations (e.g., upward shift of the brain within the skull [54], disrupted white matter structural connectivity [55], increased fluid volumes [56], and increased cerebral vasoconstriction [200]), as well as modifications to adaptive plasticity [53]. Adaptive reorganization is primarily observed in the sensory systems. For example, changes in functional connectivity during plantar stimulation have been observed within sensorimotor, visual, somatosensory, and vestibular networks after spaceflight [201]. In addition, functional responses to vestibular stimulation were altered after spaceflight―reducing the typical deactivation of somatosensory and visual cortices [202]. These studies provide evidence for sensory reweighting among visual, vestibular, and somatosensory inputs.
Further research is required to fully understand the observed CNS changes. In addition, integrated countermeasures are needed for the acute effects of g-transitions on sensorimotor and vestibular function.
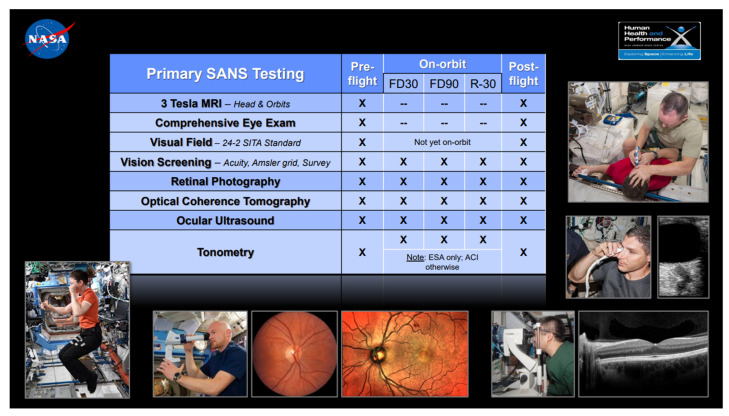
1.7.1. Effects on the Neuro-Ocular System
Prolonged exposure to ionizing radiation is well known to produce secondary cataracts [61,62]. Most importantly, Spaceflight Associated Neuro-Ocular Syndrome (SANS) is a unique constellation of clinical and imaging findings which occur to astronauts both during and after spaceflight, and is characterized by: hyperopic refractive changes (axial hyperopia), optic disc edema, posterior globe flattening, choroidal folds, and cotton wool spots [43]. Ophthalmologic screening for SANS, including both clinical and imaging assessments is recommended. (Figure 2) Although the precise etiology and mechanism for SANS remain ill-defined, some proposed risk factors for the development of SANS include microgravity related cephalad fluid shifts [203], rigorous resistive exercise [204], increased body weight [205], and disturbances to one carbon metabolic pathways [206]. Many scientists believe that the cephalad fluid shift secondary to microgravity exposure is the major pathophysiological driver of SANS [203]. Although inflight lumbar puncture has not been attempted, several mildly elevated ICPs have been recorded in astronauts with SANS manifestations upon returning to Earth [43]. Moreover, changes to the pressure gradient between the intraocular pressure (IOP) and ICP (the translaminar gradient) have been proposed as a pathogenic mechanism for SANS [207]. The translaminar gradient may explain the structural changes seen in the posterior globe such as globe flattening and choroidal folds [207]. Alternatively, the microgravity induced cephalad fluid shift may impair venous or cerebrospinal drainage from the cranial cavity and/or the eye/orbit (e.g., choroid or optic nerve sheath). Impairment of the glymphatic system has also been proposed as a contributing mechanism to SANS, but this remains unproven [208,209]. Although permanent visual loss has not been observed in astronauts with SANS, some structural changes (e.g., posterior globe flattening) may persist and have been documented to remain for up to 7 years of long-term follow-up [210]. Further research is required to better understand the mechanism of SANS, and to develop effective countermeasures prior to longer duration space missions.
Figure 2.
Ophthalmologic screening for SANS.
1.7.2. Effects on the Neuro-Behavioral System
The combination of mission-associated stressors with the underlying confinement and social isolation of space travel has the potential to lead to cognitive deficits and the development of psychiatric disorders [211]. Examples of previously identified cognitive deficits associated with spaceflight include impaired concentration, short-term memory loss, and an inability to multi-task. These findings are most evident during G-transitions, and are likely due to interactions between vestibular and cognitive function [212,213]. Sopite syndrome, a neurologic component of motion sickness, may account for some cognitive slowing. The term “space fog”, has been used to describe the generalized lack of focus, altered perception of time, and cognitive impairments associated with spaceflight, which can occur throughout the mission. This may be related to chronic sleep deprivation as deficiencies (including decreased sleep duration and quality of sleep) are prevalent despite the frequent use of sleep medications [71]. These results highlight the broad impact of space travel on cognitive and behavioral health, and support the need for integrated countermeasures for long-duration explorative missions.
1.8. Effects on the Musculoskeletal System
During short-duration spaceflight, low back pain and disk herniation are common due to the presence of microgravity. While the pathogenesis of space-related low back pain and disk herniation is complex, the etiology is likely multifactorial in nature (e.g., microgravity induced hydration and swelling of the vertebral disk, muscle atrophy of the neck and lower back) [19,214,215]. Additionally, various joint injuries (e.g., space-suited shoulder injuries) can also occur in space due to the presence of microgravity [16,216,217,218]. Interestingly, one study showed that performing specific exercises could potentially promote automatic and tonic activation of lumbar multifidus and transversus abdominis as well as prevent normal lumbopelvic positioning against gravity following bed rest as a simulation of space flight [219], and the European Space Agency suggested that exercise program could relieve low back pain during spaceflight [220]. Further longitudinal studies are required to develop specialized exercise protocols during space travel.
During long-duration spaceflight, the presence of microgravity could cause an alteration in collagen fiber orientation within tendons, reduce articular cartilage and meniscal glycosaminoglycan content, and impair the wound healing process [22,23,24,221]. These findings seen in animal studies suggest that mechanical loading is required in order for these processes to occur in a physiologic manner. It is theorized that there is a mandatory threshold of skeletal loading necessary to direct balanced bone formation and resorption during healthy bone remodeling [222,223]. Despite the current countermeasure programs, the issue of skeletal integrity is still not solved [224,225,226].
Space radiation could also impact bone remodeling, though the net effect differs based on the amount of radiation involved [6]. In summary, high doses of space radiation lead to bone destruction with increased bone resorption and reduced bone formation, while low doses of space radiation actually have a positive impact with increased mineralization and reduced bone resorption. Most importantly, space radiation, particularly solar particle events in the case of a flare, may induce acute radiation effects, leading to hematopoietic syndrome [7]. This risk is highest for longer duration missions, but can be substantially minimized with current spacecraft shielding options.
Longitudinal studies are required to develop special exercise protocols and further assess the aforementioned risk of space radiation on the development of musculoskeletal malignancies.
1.9. Effects on the Pulmonary System
During short-duration spaceflight, a host of changes to normal, physiologic pulmonary function have been observed [73,227]. Studies during parabolic flight have shown that the diaphragm and abdomen are displaced cranially due to microgravity, which is accompanied by an increase in the diameter of the lower rib cage with outward movement. Due to the observed changes to the shape of the chest wall, diaphragm, and abdomen, alterations to the pressure-volume curve resulted in a net reduction in lung volumes [228]. In five subjects who underwent 25 s of microgravity exposure during parabolic flight, functional residual capacity (FRC) and vital capacity (VC) were found to be reduced [229]. During the Spacelab Life Sciences-1 mission, microgravity exposure resulted in 10%, 15%, 10–20%, and 18% reductions in VC, FRC, expiratory reserve volume (ERV), and residual volume (RV), respectively, compared to values seen in Earth’s gravity [227]. The observed physiologic change in FRC is primarily due to the cranial shift of the diaphragm and abdominal contents described previously, and secondarily to an increase in intra-thoracic blood volume and more uniform alveolar expansion [227].
One surrogate measure for the inhomogeneity of pulmonary perfusion can be assessed through changes in cardiogenic oscillations of CO2 (oscillations in exhaled gas composition due to differential flows from different lung regions with differing gas composition). Following exposure to microgravity, the size of cardiogenic oscillations were significantly reduced to 60% in comparison to the preflight standing values [230,231]. Possible causes of the observed inhomogeneity of ventilation include regional differences in lung compliance, airway resistance, and variations in motion of the chest wall and diaphragm. Access to arterial blood gas analysis would allow for enhanced physiologic evaluations, as well as improved management of clinical emergencies (e.g., pulmonary embolism) occurring during space travel. However, there is currently no suitable method for assessing arterial blood in space. The earlobe arterialized blood technique for collecting blood gas has been proposed, but evidence is limited [232]. Further research is required in this area to establish an effective means for sampling arterial blood during spaceflight.
In comparison to the changes seen during short-duration spaceflight, studies conducted during long-duration spaceflight showed that the heterogeneity of ventilation/perfusion (V/Q) was largely unchanged, with preserved gas exchange, VC, and respiratory muscle strength [73,233,234]. This resulted in overall normal lung function. This is supported by long-duration studies (up to 6 months) in microgravity which demonstrated that the function of the normal human lungs is largely unchanged following the removal of gravity [233,234]. It is worth noting that there were some small changes which were observed (e.g., an increase in ERV in the standing posture) following long-duration spaceflight, which can perhaps be attributed to a reduction in circulating blood volume [233,234]. However, while microgravity can causes temporary changes in lung function, these changes were reversible upon return to Earth’s gravity (even after 6 months of exposure to microgravity). Based on the currently available data, the overall effect of acute and sustained exposure to microgravity does not appear to cause any deleterious effects to gas exchange in the lungs. However, the biggest challenge for long-duration spaceflight is perhaps extraterrestrial dust exposure. Further research is required to identify the long term consequences of extraterrestrial dust exposure and develop potential countermeasures (e.g., specialized face masks) [73].
1.10. Effects on the Dermatologic System
During short-duration space travel, skin conditions such as contact dermatitis, skin sensitivity, biosensor electrolyte paste reactions, and thinning skin are common [44,235]. However, these conditions are generally mild and unlikely to significantly impact astronaut safety or prevent completion of space missions [44].
The greatest dermatologic concern for long-duration space travelers is the theoretical increased risk of developing skin cancer due to space radiation exposure. This hypothesis is supported by one study which found the rate of basal cell carcinoma, melanoma, and squamous cell carcinoma of the skin to be higher among astronauts compared to a matched cohort [236]. While the three-fold increase in prevalence was significant, there were a number of confounders (e.g., the duration of prolonged UV exposure on Earth for training or recreation, prior use of sunscreen protection, genetic predisposition, and variations in immune system function) that must also be taken into account. A potential management strategy for dealing with various skin cancers during space travel involves telediagnostic and telesurgical procedures. Further research is needed to improve the telediagnosis and management of dermatological conditions (e.g., adjustment for a lag in communication time) during spaceflight.
1.11. Diagnostic Imaging Modalities in Space
In addition to routine physical examination, various medical imaging modalities may be required to monitor and diagnose medical conditions during long-duration space travel. To date, ultrasound imaging acquired on space stations has proven to be helpful in diagnosing a wide array of medical conditions, including venous thrombosis, renal and biliary stones, and decompression sickness [29,237,238,239,240,241,242]. Moreover, the Focused Assessment with Sonography for Trauma (FAST), utilized by physicians to rapidly evaluate trauma patients, may be employed during space missions to rule out life-threatening intra-abdominal, intra-thoracic, or intra-ocular pathology [243]. Remote telementored ultrasound (aka tele-ultrasound) has been previously investigated during the NASA Extreme Environment Missions Operations (NEEMO) expeditions [244]. Today, the Butterfly iQ portable ultrasound probe can be linked directly to a smartphone through cloud computing, allowing physicians/specialists to promptly analyze remote ultrasound images [245].
Currently, alternative imaging modalities such as X-ray, CT, PET and MRI scan are unable to be used in space due to substantial limitations (e.g., limited space for large imaging structures, difficulties in interpretation due to microgravity). However, it is possible that the future development of a photocathode-based X-ray source may one day make this a possibility [101,246]. If X-ray imaging was possible, certain caveats would need to be taken into account for accurate interpretation. For example, pleural effusions, air-fluid levels, and pulmonary cephalization commonly seen on terrestrial imaging, would need to be interpreted in an entirely different way due to the effect of microgravity [247]. While this adjustment might be challenging, the altered principles of weightless physiology may provide some advantages as well. For example, one study found that intra-abdominal fluid was better able to be detected in space than in the terrestrial environment due to gravitational alterations in fluid dynamics [248]. Further research is required to identify and optimize inflight imaging modalities for the detection and treatment of various medical conditions.
1.12. Medical and Surgical Procedures in Space
Despite the presence of microgravity, both basic life support and advanced cardiac life support are feasible during space travel with some modifications [249,250]. For example, the recent guidelines for CPR in microgravity recommend specialized techniques for delivering chest compressions [251]. The use of mechanical ventilators, and moderate sedation or general anesthesia in microgravity are also possible but the evidence is extremely limited [252,253]. In addition, there are several procedures such as endotracheal intubation, percutaneous tracheostomy, diagnostic peritoneal lavage, chest tube insertion, and advanced vascular access which have only been studied through artificial stimulation [254,255].
Once traditionally “surgical” conditions are appropriately diagnosed, the next step is to determine whether these conditions should be managed medically, percutaneously, or surgically (laparoscopic vs. open procedures) [47,256]. For example, acute appendicitis or cholecystitis that would historically be managed surgically in terrestrial hospitals, could instead be managed with antibiotics rather than surgery. While the use of antibiotics for these conditions is usually effective on Earth, there remain concerns due to space-induced immune alterations, increased pathogenicity and virulence of microorganisms, and limited resources to “rescue” cases of antibiotic failure [39]. In cases of antibiotic failure, one potential minimally invasive option could be ultrasound-guided percutaneous drainage, which has previously been demonstrated to be possible and effective in microgravity [257]. Another potential approach is to focus on the early diagnosis and minimally invasive treatment of appropriate conditions, rather than treating late stage disease. In addition to expediting the patient’s post-operative recovery, minimally invasive surgery in space has the added benefit of protecting the cabin environment and the remainder of the crew [258,259].
As in all aspects of healthcare delivery in space, the presence of microgravity can complicate even the most basic of procedures. However, based on collective experience to date, if the patient, operators, and all required equipment are restrained, the flow of surgical procedures remains relatively unchanged compared to the traditional, terrestrial experience [260]. A recent animal study confirmed that it was possible to perform minor surgical procedures (e.g., vessel and wound closures) in microgravity [261]. Similar study during parabolic flight has further confirmed that emergent surgery for the purpose of “damage control” in catastrophic scenarios can be conducted in microgravity [262]. As discussed previously, telesurgery may be feasible if the surgery can be performed with an acceptably brief time lag (<200 ms) and if the patient is within a low Earth orbit [263,264]. However, further research and technological advancements are required for this to come to fruition.
1.13. Lifestyle Management in Space
Based on microgravity simulation studies, NASA has proposed several potential biomedical countermeasures in space [33,160,161]. Mandatory exercise protocols in space are crucial and can be used to maintain physical fitness and counteract the effects of microgravity. While these protocols may be beneficial, exercise alone may not be enough to prevent certain effects of microgravity (e.g., an increase in arterial thickness/stiffness) [20,265,266,267]. For example, a recent study found that resistive exercise alone could not suppress the increase in bone resorption that occurs in space [20]. Hence, a combination of resistance training and an antiresorptive medication (e.g., bisphosphonate) appears to be optimal for promotion of bone health [20,21]. Further research is needed to identify the optimal exercise regimen including recommended exercises, duration, and frequency.
In addition to exercise, dietary modification may be another potential area for optimization. The use of a diet based on caloric restriction (CR) in space remains up for debate. Based on data from terrestrial studies, caloric restriction may be useful for improving vascular health; however, this benefit may be offset by the associated muscle atrophy and osteoporosis [268,269]. Given that NASA encourages astronauts to consume adequate energy to maintain body mass, there has been an attempt to mimic the positive effects of CR on vascular health while providing appropriate nutrition. Further research is needed this area to identify the ideal space diet.
Based on current guidelines, only vitamin D supplementation during space travel is recommended. Supplementation of A, B6, B12, C, E, K, Biotin, folic acid are not generally recommended at this time due to insufficient evidence [64] (Table S3). The use of traditional prescription medications may not function as intended on Earth. Therefore, alternative methods such as synthetic biologic agents or probiotics may be considered [35,38]. However, evidence in this area is extremely limited, and it is possible that the synthetic agents or probiotics may themselves be altered due to microgravity and radiation exposure. Further research is needed to investigate the relationship between these supplements and potential health benefits in space.
Currently, most countermeasures are directed towards cardiovascular system and musculoskeletal pathologies but there is little data against issues like immune and sleep deprivation, SANS, skin, etc. Artificial Gravity (AG) has been postulated as adequate multi-system countermeasure especially the chronic exposure in a large radius systems. Previously, the main barrier is the huge increase in costs [270,271,272]. However, there are various studies that show the opposite and also the recent decrease in launch cost makes the budget issue nearly irrelevant especially when a huge effort is paid to counteract the lack of gravity. The use of AG especially long-radius chronic AG is feasible. Further studies are needed to determine the utilization of AG in long-duration space travel.
1.14. Future Directions for Precision Space Health with AI
In this new era of space travel and exploration, ‘future’ tools and novel applications are needed in order to prepare deep space missions, particularly pertaining to strategies for mitigating extraterrestrial environmental factors, including both exogenous and en-dogenous processes. Such ‘future’ tools could help assist and ensure a safe travel to deep space, and more importantly, help bring space travelers and astronauts back to Earth. These tools and methods may initially be ‘remotely’ controlled, or have its data sent back to Earth for analysis. Primarily efforts should be focused on analyzing data in situ, and on site during the mission itself, both for the purpose of efficiency, and for the progressive purpose of slowly weaning off a dependency on Earth.
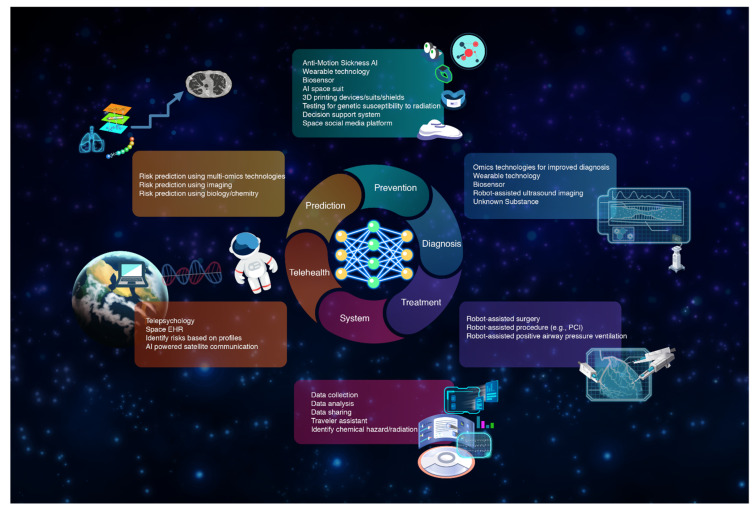
AI is an emerging tool in the big data era and AI is considered a critical aspect of ‘fu-ture’ tools within the healthcare and life science fields. A combination of AI and big data can be used for the purposes of decision making, data analysis and outcome prediction. Just recently, there have been encourage in advancements in AI and space technologies. To date, AI has been employed by astronauts for the purpose of space exploration; however, we may just be scratching the surface of AI’s potential. In the area of medical research, AI technology can be leveraged for the enhancement of telehealth delivery, improvement of predictive accuracy and mitigation of health risks, and performance of diagnostic and interventional tasks [273]. The AI model can then be trained and have its inference leveraged through cloud computing or Edge TPU or NVIDIA Jetson Nano located on space stations. (Table 3 and Table S4) Figure 3 demonstrates potential AI applications in space.
Figure 3.
Potential AI applications in space.
As described previously, the capability to provide telemedicine beyond LEO is primarily limited by the inability to effectively communicate between space and Earth in real-time [274]. However, AI integration may be able to bridge the gap and advance communication capabilities within the space environment [275,276]. One study demonstrated a potential mechanism for AI incorporation in which an AI-generated predictive algorithm displayed the projected motion of surgical tools to adjust for excess communication lag-time [277]. This discovery could potentially enable AI-enhanced robotics to complete repetitive, procedural tasks in space without human inputs (e.g., vascular access) [278]. Today, procedures performed with robotic assistance are not yet fully autonomous (they still require at least one human expert). It is possible with future iterations that an AI integration could be created with the ability to fully replicate the necessary human steps to make terrestrial procedures (e.g., percutaneous coronary intervention, incision and drainage [103], telecholecystectomy [105,106], etc.) feasible in space [275,279]. The seventh NEEMO mission previously demonstrated that robotic surgery controlled by a remote physician is feasible within the environment of a submarine, but it remains to be seen whether this can be expanded to the space environment [280].
On space stations, Edge TPU-accelerated AI inference could be used to generate accurate risk prediction models based on data obtained from simulated environments (e.g., NASA AI Risk Prediction Challenge) [281]. For example, AI could potentially utilize data (e.g., -omics) obtained from research conducted both on Earth and in simulated environments (e.g., NASA GCR Simulator) to predict an astronaut’s risk of developing cancer due to high-LET radiation exposure (cytogenetic damage, mitochondrial dysregulation, epigenetic alterations, etc.) [63,78,79,282,283,284].
Another potential area for AI application is through integration with wearable technology to assist in the monitoring and treatment of a variety of medical conditions. For example, within the field of cardiovascular medicine, wearable sensor technology has the capability to detect numerous biosignals including an individual’s cardiac output, blood pressure, and heart rate [285]. AI-based interpretation of this data can facilitate prompt diagnosis and treatment of congestive heart failure and arrhythmias [285]. In addition, several wearable devices in various stages of development are being created for the detection and treatment of a wide array of medical conditions (obstructive sleep apnea, deep vein thrombosis, SMS, etc.) [285,286,287,288].
As discussed previously, the confinement and social isolation associated with prolonged space travel can have a profound impact on an astronaut’s mental health [8,10,67]. AI-enhanced facial and voice recognition technology can be implemented to detect the early signs of depression or anxiety better than standardized screening questionnaires (e.g., PHQ-9, GAD-7) [68,69]. Therefore, telepsychology or telepsychiatry can be used pre-emptively for the diagnosis of mental illness [68,69,289].
2. Conclusions
Over the next decade, NASA, Russia, Europe, Canada, Japan, China, and a host of commercial space companies will continue to push the boundaries of space travel. Space exploration carries with it a great deal of risk from both known (e.g., ionizing radiation, microgravity) and unknown risk factors. Thus, there is an urgent need for expanded research to determine the true extent of the current limitations of long-term space travel and to develop potential applications and countermeasures for deep space exploration and colonization. Researchers must leverage emerging technology, such as AI, to advance our diagnostic capability and provide high-quality medical care within the space environment.
Acknowledgments
The authors would like to thank Tyson Brunstetter, (NASA Johnson Space Center, Houston, TX) for his suggestions and comments on this article as well as providing the update NASA’s SANS Evidence Report, Ajitkumar P Mulavara, (Neurosciences Laboratory, KBRwyle, Houston, TX), Jonathan Clark, (Neurology & Space Medicine, Center for Space Medicine, Houston, TX), Scott M. Smith, (Nutritional Biochemistry, Biomedical Research and Environmental Sciences Division, Human Health and Performance Directorate, NASA Johnson Space Center, Houston, TX) for his suggestions and providing the update NASA’s Nutrition Report, G. Kim Prisk, (Department of Medicine, Division of Physiology, University of California, San Diego, La Jolla, CA), Lisa C. Simonsen (NASA Langley Research Center, Hampton, VA), Siddharth Rajput, (Royal Australasian College of Surgeons, Australia and Aerospace Medical Association and Space Surgery Association, USA), David S. Martin, MS, (KBR, Houston, TX), David W. Kaczka, (Department of Anesthesia, University of Iowa Carver College of Medicine, Iowa City, Iowa), Benjamin D. Levine (Institute for Exercise and Environmental Medicine, Texas Health Presbyterian Hospital, Dallas, University of Texas Southwestern Medical Center), Afshin Beheshti (NASA Ames Research Center), Christopher Wilson (NASA Goddard Space Flight Center), Michael Lowry (NASA Ames Research Center), Graham Mackintosh (NASA Advanced Supercomputing Division), and staff from NASA Goddard Space Flight Center for their suggestions. In addition, the authors would like to thank the anonymous reviewers for their careful reading of our manuscript, constructive criticism, and insightful comments and suggestions.
Abbreviations
| LEO | Low Earth Orbit |
| NASA | National Aeronautics and Space Administration |
| VO2max | Maximal oxygen consumption |
| AI | Artificial intelligence |
| ISS | International Space Station |
| AF | Atrial fibrillation |
| LET | linear energy transfer |
| MRI | Magnetic resonance imaging |
| Gy | Gray (unit) |
| BMI | Body mass index |
| NAFLD | Non-alcoholic fatty liver disease |
| EBV | Epstein-Bar Virus |
| VZV | Varicella-Zoster Virus |
| CMV | Cytomegalovirus |
| NCRP | National Council on Radiation Protection and Measurements |
| SMS | Space motion sickness |
| ICP | Intracranial pressure |
| PFMS | Post-flight motion sickness |
| CNS | Central nervous system |
| SANS | Spaceflight Associated Neuro-Ocular Syndrome |
| IOP | Intraocular pressure |
| FRC | Functional residual capacity |
| VC | Vital capacity |
| ERV | Expiratory reserve volume |
| RV | Residual volume |
| V/Q | Ventilation/perfusion |
| NEEMO | NASA Extreme Environment Missions Operations |
| FAST | Focused Assessment with Sonography for Trauma |
| PET | Positron emission tomography |
| CPR | Cardiopulmonary Resuscitation |
| CR | Caloric restriction |
| TPU | Tensor Processing Unit |
| PHQ-9 | Patient Health Questionnaire-9 |
| GAD-7 | General Anxiety Disorder-7 |
| GCR | Galactic Cosmic Ray |
| DVT | Deep vein thrombosis |
| ASIC | Application-specific integrated circuit |
| TB | Tuberculosis |
| PSA | Prostate-specific antigen |
| DXA | Dual-energy X-ray absorptiometry |
| T4 | Levothyroxine |
| TSH | Thyroid-stimulating hormone |
| GDR | Galactic cosmic radiation |
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cells12010040/s1, Table S1: title Summary of gut microbial alteration during spaceflight; Table S2: title Summary of immune/cytokine changes during spaceflight; Table S3: title Summary of diet recommendation during spaceflight; Table S4: title Summary of AI technology and potential applications in space.
Conflicts of Interest
Krittanawong discloses the following relationships-Member of the American College of Cardiology Solution Set Oversight Committee, the American Heart Association Committee of the Council on Genomic and Precision Medicine, the American College of Cardiology/American Heart Association (ACC/AHA) Joint Committee on Clinical Data Standards (Joint Committee), and the American College of Cardiology/American Heart Association (ACC/AHA) Task Force on Performance Measures, The Lancet Digital Health (Advisory Board), European Heart Journal Digital Health (Editorial board), Journal of the American Heart Association (Editorial board), JACC: Asia (Section Editor), and The Journal of Scientific Innovation in Medicine (Associate Editor). Other authors have no disclosure.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.The Evolving Landscape of 21st Century American Spaceflight. [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/sites/default/files/files/Emerging_Space_Report.pdf.
- 2.Garrett-Bakelman F.E., Darshi M., Green S.J., Gur R.C., Lin L., Macias B.R., McKenna M.J., Meydan C., Mishra T., Nasrini J., et al. The NASA Twins Study: A multidimensional analysis of a year-long human spaceflight. Science. 2019;364:6436. doi: 10.1126/science.aau8650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Little M.P., Tawn E.J., Tzoulaki I., Wakeford R., Hildebrandt G., Paris F., Tapio S., Elliott P. Review and meta-analysis of epidemiological associations between low/moderate doses of ionizing radiation and circulatory disease risks, and their possible mechanisms. Radiat. Environ. Biophys. 2010;49:139–153. doi: 10.1007/s00411-009-0250-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu T., Parks B.W., Yu S., Srivastava R., Gupta K., Wu X., Khaled S., Chang P.Y., Kabarowski J.H., Kucik D.F. Iron-ion radiation accelerates atherosclerosis in apolipoprotein E-deficient mice. Radiat. Res. 2011;175:766–773. doi: 10.1667/RR2482.1. [DOI] [PubMed] [Google Scholar]
- 5.Crucian B., Stowe R.P., Mehta S., Quiriarte H., Pierson D., Sams C. Alterations in adaptive immunity persist during long-duration spaceflight. NPJ Microgravity. 2015;1:15013. doi: 10.1038/npjmgrav.2015.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donaubauer A.-J., Deloch L., Becker I., Fietkau R., Frey B., Gaipl U.S. The Influence of Radiation on Bone and Bone Cells-Differential Effects on Osteoclasts and Osteoblasts. Int. J. Mol. Sci. 2020;21:6377. doi: 10.3390/ijms21176377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu H., Huff J., Casey R., Kim M., Cucinotta F. Human Health and Performance Risks of Space Exploration Missions. NASA Human Research Program; Houston, TX, USA: 2009. Risk of Acute Radiation Syndromes Due to Solar Particle Events; pp. 171–190. NASA SP-2009-3405. [Google Scholar]
- 8.Kanas N. Psychiatric issues affecting long duration space missions. Aviat. Space Environ. Med. 1998;69:1211–1216. [PubMed] [Google Scholar]
- 9.Arone A., Ivaldi T., Loganovsky T., Palermo S., Parra E., Flamini W., Marazziti D. The Burden of Space Exploration on the Mental Health of Astronauts: A Narrative Review. Clin. Neuropsychiatry. 2021;18:237–246. doi: 10.36131/cnfioritieditore20210502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barratt M.R., Baker E.S., Pool S.L., editors. Principal for Clinical Medicine for Space Flight. 2nd ed. Springer Science and Business Media LLC; Berlin/Heidelberg, Germany: Springer Nature; Cham, Switzerland: 2019. [Google Scholar]
- 11. [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/sites/default/files/atoms/files/nasa-std-3001-vol-1a-chg1.pdf.
- 12. [(accessed on 2 November 2022)]; Available online: https://lsda.jsc.nasa.gov/lsda_data/document/Project/MRID/MR009S.pdf.
- 13.Astronaut Selection and Training. [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/centers/johnson/pdf/606877main_FS-2011-11-057-JSC-astro_trng.pdf.
- 14.Siconolfi S.F., Lemoine S.L. Graded exercise testing for spaceflight. Aviat. Space Environ. Med. 1995;66:435–439. [PubMed] [Google Scholar]
- 15.Hamilton D.R., Murray J.D., Ball C.G. Cardiac health for astronauts: Coronary calcification scores and CRP as criteria for selection and retention. Aviat. Space Environ. Med. 2006;77:377–387. [PubMed] [Google Scholar]
- 16.Scheuring R.A., Mathers C.H., Jones J.A., Wear M.L. Musculoskeletal injuries and minor trauma in space: Incidence and injury mechanisms in U.S. astronauts. Aviat. Space Environ. Med. 2009;80:117–124. doi: 10.3357/ASEM.2270.2009. [DOI] [PubMed] [Google Scholar]
- 17.Gray G.W., Johnston S.L., Saary J., Cook T. Medical Evaluations and Standards. In: Barratt M.R., Baker E.S., Pool S.L., editors. Principles of Clinical Medicine for Space Flight. 2nd ed. Springer Nature; Cham, Switzerland: 2019. [Google Scholar]
- 18.Lifetime Surveillance of Astronaut Health (LSAH) [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/feature/lifetime-surveillanceof-astronaut-health-lsah.
- 19.Chang D.G., Healey R.M., Snyder A.J., Sayson J.V., Macias B.R., Coughlin D.G., Bailey J.F., Parazynski S.E., Lotz J.C., Hargens A.R. Lumbar Spine Paraspinal Muscle and Intervertebral Disc Height Changes in Astronauts After Long-Duration Spaceflight on the International Space Station. Spine. 2016;41:1917–1924. doi: 10.1097/BRS.0000000000001873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sibonga J., Matsumoto T., Jones J., Shapiro J., Lang T., Shackelford L., Smith S.M., Young M., Keyak J., Kohri K., et al. Resistive exercise in astronauts on prolonged spaceflights provides partial protection against spaceflight-induced bone loss. Bone. 2019;128:112037. doi: 10.1016/j.bone.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 21.Leblanc A., Matsumoto T., Jones J., Shapiro J., Lang T., Shackelford L., Smith S.M., Evans H., Spector E., Ploutz-Snyder R., et al. Bisphosphonates as a supplement to exercise to protect bone during long-duration spaceflight. Osteoporos. Int. 2013;24:2105–2114. doi: 10.1007/s00198-012-2243-z. [DOI] [PubMed] [Google Scholar]
- 22.Roffino S., Carnino A., Chopard A., Mutin M., Marini J.F. Structural remodeling of unweighted soleus myotendinous junction in monkey. Comptes Rendus Biol. 2006;329:172–179. doi: 10.1016/j.crvi.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 23.Carnino A., Roffino S., Chopard A., Marini J.F. Effects of a 14-day spaceflight on soleus myotendinous junction ultrastructure in the rhesus monkey. J. Gravit. Physiol. J. Int. Soc. Gravit. Physiol. 2000;7:S65–S68. [PubMed] [Google Scholar]
- 24.Delp M.D. Unraveling the complex web of impaired wound healing with mechanical unloading and physical deconditioning. J. Appl. Physiol. 2008;104:1262–1263. doi: 10.1152/japplphysiol.90393.2008. [DOI] [PubMed] [Google Scholar]
- 25.Clément G., Reschke M.F. Neuroscience in Space. Springer; New York, NY, USA: 2010. [Google Scholar]
- 26.Cheung B., Nakashima A.M., Hofer K.D. Various anti-motion sickness drugs and core body temperature changes. Aviat. Space Environ. Med. 2011;82:409–415. doi: 10.3357/ASEM.2903.2011. [DOI] [PubMed] [Google Scholar]
- 27.Vickers Z.M., Rice B.L., Rose M.S., Lane H.W. Simulated microgravity [bed rest] has little influence on taste, odor or trigeminal sensitivity. J. Sens. Stud. 2001;16:23–32. doi: 10.1111/j.1745-459X.2001.tb00288.x. [DOI] [PubMed] [Google Scholar]
- 28.Auñón-Chancellor S.M., Pattarini J.M., Moll S., Sargsyan A. Venous Thrombosis during Spaceflight. N. Engl. J. Med. 2020;382:89–90. doi: 10.1056/NEJMc1905875. [DOI] [PubMed] [Google Scholar]
- 29.Marshall-Goebel K., Laurie S.S., Alferova I.V., Arbeille P., Auñón-Chancellor S.M., Ebert D.J., Lee S.M.C., Macias B.R., Martin D.S., Pattarini J.M., et al. Assessment of Jugular Venous Blood Flow Stasis and Thrombosis During Spaceflight. JAMA Netw. Open. 2019;2:e1915011. doi: 10.1001/jamanetworkopen.2019.15011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reschke M.F., Good E.F., Clément G.R. Neurovestibular Symptoms in Astronauts Immediately after Space Shuttle and International Space Station Missions. OTO Open. 2017;1:2473974x17738767. doi: 10.1177/2473974X17738767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehta S.K., Laudenslager M.L., Stowe R.P., Crucian B.E., Feiveson A.H., Sams C.F., Pierson D.L. Latent virus reactivation in astronauts on the international space station. NPJ Microgravity. 2017;3:11. doi: 10.1038/s41526-017-0015-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rooney B.V., Crucian B.E., Pierson D.L., Laudenslager M.L., Mehta S.K. Herpes Virus Reactivation in Astronauts During Spaceflight and Its Application on Earth. Front. Microbiol. 2019;10:16. doi: 10.3389/fmicb.2019.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Makedonas G., Mehta S., Choukèr A., Simpson R.J., Marshall G., Orange J.S., Aunon-Chancellor S., Smith S.M., Zwart S.R., Stowe R.P., et al. Specific Immunologic Countermeasure Protocol for Deep-Space Exploration Missions. Front. Immunol. 2019;10:2407. doi: 10.3389/fimmu.2019.02407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cogoli A. The effect of space flight on human cellular immunity. Environ. Med. Annu. Rep. Res. Inst. Environ. Med. Nagoya Univ. 1993;37:107–116. [PubMed] [Google Scholar]
- 35.Turroni S., Magnani M., KC P., Lesnik P., Vidal H., Heer M. Gut Microbiome and Space Travelers’ Health: State of the Art and Possible Pro/Prebiotic Strategies for Long-Term Space Missions. Front. Physiol. 2020;11:553929. doi: 10.3389/fphys.2020.553929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen J., Wang Q., Hao Z., Li Z., Sahu S.K., Liu H., Xiao L. Relationship between the Gut Microbiome and Energy/Nutrient Intake in a Confined Bioregenerative Life Support System. Appl. Environ. Microbiol. 2020;86:e02465-19. doi: 10.1128/AEM.02465-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Y., Zhao W., Shi J., Wang J., Hao J., Pang X., Huang X., Chen X., Li Y., Jin R., et al. Intestinal microbiota contributes to altered glucose metabolism in simulated microgravity mouse model. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2019;33:10140–10151. doi: 10.1096/fj.201900238RR. [DOI] [PubMed] [Google Scholar]
- 38.Menezes A.A., Cumbers J., Hogan J.A., Arkin A.P. Towards synthetic biological approaches to resource utilization on space missions. J. R. Soc. Interface. 2015;12:20140715. doi: 10.1098/rsif.2014.0715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Campbell M.R., Johnston S.L., 3rd, Marshburn T., Kane J., Lugg D. Nonoperative treatment of suspected appendicitis in remote medical care environments: Implications for future spaceflight medical care. J. Am. Coll. Surg. 2004;198:822–830. doi: 10.1016/j.jamcollsurg.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 40.Ball C.G., Kirkpatrick A.W., Williams D.R., Jones J.A., Polk J.D., Vanderploeg J.M., Talamini M.A., Campbell M.R., Broderick T.J. Prophylactic surgery prior to extended-duration space flight: Is the benefit worth the risk? Can. J. Surg. 2012;55:125–131. doi: 10.1503/cjs.024610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buckey J.C., Jr., Lane L.D., Levine B.D., Watenpaugh D.E., Wright S.J., Moore W.E., Gaffney F.A., Blomqvist C.G. Orthostatic intolerance after spaceflight. J. Appl. Physiol. 1996;81:7–18. doi: 10.1152/jappl.1996.81.1.7. [DOI] [PubMed] [Google Scholar]
- 42.Perhonen M.A., Franco F., Lane L.D., Buckey J.C., Blomqvist C.G., Zerwekh J.E., Peshock R.M., Weatherall P.T., Levine B.D. Cardiac atrophy after bed rest and spaceflight. J. Appl. Physiol. 2001;91:645–653. doi: 10.1152/jappl.2001.91.2.645. [DOI] [PubMed] [Google Scholar]
- 43.Mader T.H., Gibson C.R., Pass A.F., Kramer L.A., Lee A.G., Fogarty J., Tarver W.J., Dervay J.P., Hamilton D.R., Sargsyan A., et al. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology. 2011;118:2058–2069. doi: 10.1016/j.ophtha.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 44.Dunn C., Boyd M., Orengo I. Dermatologic manifestations in spaceflight: A review. Dermatol. Online J. 2018;24:11. doi: 10.5070/D32411042001. [DOI] [PubMed] [Google Scholar]
- 45.Kirkpatrick A.W., Campbell M.R., Jones J.A., Broderick T.J., Ball C.G., McBeth P.B., McSwain N.E., Hamilton D.R., Holcomb J.B. Extraterrestrial hemorrhage control: Terrestrial developments in technique, technology, and philosophy with applicability to traumatic hemorrhage control in long-duration spaceflight. J. Am. Coll. Surg. 2005;200:64–76. doi: 10.1016/j.jamcollsurg.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 46.Kirkpatrick A.W., Campbell M.R., Novinkov O.L., Goncharov I.B., Kovachevich I.V. Blunt trauma and operative care in microgravity: A review of microgravity physiology and surgical investigations with implications for critical care and operative treatment in space. J. Am. Coll. Surg. 1997;184:441–453. [PubMed] [Google Scholar]
- 47.Kirkpatrick A.W., Ball C.G., Campbell M., Williams D.R., Parazynski S.E., Mattox K.L., Broderick T.J. Severe traumatic injury during long duration spaceflight: Light years beyond ATLS. J. Trauma Manag. Outcomes. 2009;3:4. doi: 10.1186/1752-2897-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ferrone K.L., Guan F., Ma J., Peterson L.E., Willis C.E., Kry S.F. Reducing space radiation cancer risk with magnetic shielding. Adv. Space Res. 2021;68:153–160. doi: 10.1016/j.asr.2021.03.002. [DOI] [Google Scholar]
- 49.Dobynde M.I., Shprits Y.Y., Drozdov A.Y., Hoffman J., Li J. Beating 1 Sievert: Optimal Radiation Shielding of Astronauts on a Mission to Mars. Space Weather. 2021;19:e2021SW002749. doi: 10.1029/2021SW002749. [DOI] [Google Scholar]
- 50.Trudel G., Shahin N., Ramsay T., Laneuville O., Louati H. Hemolysis contributes to anemia during long-duration space flight. Nat. Med. 2022;28:59–62. doi: 10.1038/s41591-021-01637-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Trudel G., Shafer J., Laneuville O., Ramsay T. Characterizing the effect of exposure to microgravity on anemia: More space is worse. Am. J. Hematol. 2020;95:267–273. doi: 10.1002/ajh.25699. [DOI] [PubMed] [Google Scholar]
- 52.Cherry J.D., Liu B., Frost J.L., Lemere C.A., Williams J.P., Olschowka J.A., O’Banion M.K. Galactic cosmic radiation leads to cognitive impairment and increased aβ plaque accumulation in a mouse model of Alzheimer’s disease. PLoS ONE. 2012;7:e53275. doi: 10.1371/journal.pone.0053275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hupfeld K.E., McGregor H.R., Reuter-Lorenz P.A., Seidler R.D. Microgravity effects on the human brain and behavior: Dysfunction and adaptive plasticity. Neurosci. Biobehav. Rev. 2021;122:176–189. doi: 10.1016/j.neubiorev.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Koppelmans V., Bloomberg J.J., Mulavara A.P., Seidler R.D. Brain structural plasticity with spaceflight. NPJ Microgravity. 2016;2:2. doi: 10.1038/s41526-016-0001-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee J.K., Koppelmans V., Riascos R.F., Hasan K.M., Pasternak O., Mulavara A.P., Bloomberg J.J., Seidler R.D. Spaceflight-Associated Brain White Matter Microstructural Changes and Intracranial Fluid Redistribution. JAMA Neurol. 2019;76:412–419. doi: 10.1001/jamaneurol.2018.4882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kramer L.A., Hasan K.M., Stenger M.B., Sargsyan A., Laurie S.S., Otto C., Ploutz-Snyder R.J., Marshall-Goebel K., Riascos R.F., Macias B.R. Intracranial Effects of Microgravity: A Prospective Longitudinal MRI Study. Radiology. 2020;295:640–648. doi: 10.1148/radiol.2020191413. [DOI] [PubMed] [Google Scholar]
- 57.Baselet B., Rombouts C., Benotmane A.M., Baatout S., Aerts A. Cardiovascular diseases related to ionizing radiation: The risk of low-dose exposure (Review) Int. J. Mol. Med. 2016;38:1623–1641. doi: 10.3892/ijmm.2016.2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hendry J.H., Akahoshi M., Wang L.S., Lipshultz S.E., Stewart F.A., Trott K.R. Radiation-induced cardiovascular injury. Radiat. Environ. Biophys. 2008;47:189–193. doi: 10.1007/s00411-007-0155-7. [DOI] [PubMed] [Google Scholar]
- 59.Soucy K.G., Lim H.K., Kim J.H., Oh Y., Attarzadeh D.O., Sevinc B., Kuo M.M., Shoukas A.A., Vazquez M.E., Berkowitz D.E. HZE ⁵⁶Fe-ion irradiation induces endothelial dysfunction in rat aorta: Role of xanthine oxidase. Radiat. Res. 2011;176:474–485. doi: 10.1667/RR2598.1. [DOI] [PubMed] [Google Scholar]
- 60.Yan X., Sasi S.P., Gee H., Lee J., Yang Y., Mehrzad R., Onufrak J., Song J., Enderling H., Agarwal A., et al. Cardiovascular risks associated with low dose ionizing particle radiation. PLoS ONE. 2014;9:e110269. doi: 10.1371/journal.pone.0110269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lipman R.M., Tripathi B.J., Tripathi R.C. Cataracts induced by microwave and ionizing radiation. Surv. Ophthalmol. 1988;33:200–210. doi: 10.1016/0039-6257(88)90088-4. [DOI] [PubMed] [Google Scholar]
- 62.Ainsbury E.A., Barnard S., Bright S., Dalke C., Jarrin M., Kunze S., Tanner R., Dynlacht J.R., Quinlan R.A., Graw J., et al. Ionizing radiation induced cataracts: Recent biological and mechanistic developments and perspectives for future research. Mutat. Research. Rev. Mutat. Res. 2016;770:238–261. doi: 10.1016/j.mrrev.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 63.Kennedy E.M., Powell D.R., Li Z., Bell J.S.K., Barwick B.G., Feng H., McCrary M.R., Dwivedi B., Kowalski J., Dynan W.S., et al. Galactic Cosmic Radiation Induces Persistent Epigenome Alterations Relevant to Human Lung Cancer. Sci. Rep. 2018;8:6709. doi: 10.1038/s41598-018-24755-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/sites/default/files/human-adaptation-to-spaceflight-the-role-of-nutrition.pdf.
- 65.Nicogossian A.E., Williams R.S., Huntoon C.L., Doarn C.R., Polk J.D., Schneider V.S. Space Physiology and Medicine: From Evidence to Practice. Springer; Cham, Switzerland: 2016. [Google Scholar]
- 66.Kiecolt-Glaser J.K., Christian L., Preston H., Houts C.R., Malarkey W.B., Emery C.F., Glaser R. Stress, inflammation, and yoga practice. Psychosom. Med. 2010;72:113–121. doi: 10.1097/PSY.0b013e3181cb9377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. [(accessed on 2 November 2022)]. Available online: https://www.psychologytoday.com/us/blog/home-in-the-cosmos/201902/astronauts-open-about-depression-and-isolation-in-space.
- 68.Gavrilescu M., Vizireanu N. Predicting Depression, Anxiety, and Stress Levels from Videos Using the Facial Action Coding System. Sensors. 2019;19:3693. doi: 10.3390/s19173693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. [(accessed on 2 November 2022)]. Available online: https://www.forbes.com/sites/ganeskesari/2021/05/24/ai-can-now-detect-depression-from-just-your-voice/?sh=19ba3e364c8d.
- 70. [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/feature/goddard/2021/lunanet-empowering-artemis-with-communications-and-navigation-interoperability.
- 71.Barger L.K., Flynn-Evans E.E., Kubey A., Walsh L., Ronda J.M., Wang W., Wright K.P., Jr., Czeisler C.A. Prevalence of sleep deficiency and use of hypnotic drugs in astronauts before, during, and after spaceflight: An observational study. Lancet Neurol. 2014;13:904–912. doi: 10.1016/S1474-4422(14)70122-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dijk D.J., Neri D.F., Wyatt J.K., Ronda J.M., Riel E., Ritz-De Cecco A., Hughes R.J., Elliott A.R., Prisk G.K., West J.B., et al. Sleep, performance, circadian rhythms, and light-dark cycles during two space shuttle flights. Am. J. Physiology. Regul. Integr. Comp. Physiol. 2001;281:R1647–R1664. doi: 10.1152/ajpregu.2001.281.5.R1647. [DOI] [PubMed] [Google Scholar]
- 73.Prisk G.K. Pulmonary challenges of prolonged journeys to space: Taking your lungs to the moon. Med. J. Aust. 2019;211:271–276. doi: 10.5694/mja2.50312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Roller C.A., Clark J.B. Short-duration space flight and hearing loss. Otolaryngol.–Head Neck Surg. 2003;129:98–106. doi: 10.1016/S0194-5998(03)00523-0. [DOI] [PubMed] [Google Scholar]
- 75.Taylor P.W. Impact of space flight on bacterial virulence and antibiotic susceptibility. Infect. Drug Resist. 2015;8:249–262. doi: 10.2147/IDR.S67275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bijlani S., Singh N.K., Eedara V.V.R., Podile A.R., Mason C.E., Wang C.C.C., Venkateswaran K. Methylobacterium ajmalii sp. nov., Isolated From the International Space Station. Front. Microbiol. 2021;12:534. doi: 10.3389/fmicb.2021.639396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Makedonas G., Mehta S.K., Scheuring R.A., Haddon R., Crucian B.E. SARS-CoV-2 Pandemic Impacts on NASA Ground Operations to Protect ISS Astronauts. J. Allergy Clin. Immunol. Pract. 2020;8:3247–3250. doi: 10.1016/j.jaip.2020.08.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.George K., Rhone J., Beitman A., Cucinotta F.A. Cytogenetic damage in the blood lymphocytes of astronauts: Effects of repeat long-duration space missions. Mutat. Res./Genet. Toxicol. Environ. Mutagen. 2013;756:165–169. doi: 10.1016/j.mrgentox.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 79.Rothfuss A., Steger-Hartmann T., Heinrich N., Wichard J. Computational prediction of the chromosome-damaging potential of chemicals. Chem. Res. Toxicol. 2006;19:1313–1319. doi: 10.1021/tx060136w. [DOI] [PubMed] [Google Scholar]
- 80.Biswas N., Chakrabarti S. Artificial Intelligence (AI)-Based Systems Biology Approaches in Multi-Omics Data Analysis of Cancer. Front. Oncol. 2020;10:588221. doi: 10.3389/fonc.2020.588221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhong Q., Hu M.J., Cui Y.J., Liang L., Zhou M.M., Yang Y.W., Huang F. Carotid-Femoral Pulse Wave Velocity in the Prediction of Cardiovascular Events and Mortality: An Updated Systematic Review and Meta-Analysis. Angiology. 2018;69:617–629. doi: 10.1177/0003319717742544. [DOI] [PubMed] [Google Scholar]
- 82.Khera A., Budoff M.J., O’Donnell C.J., Ayers C.A., Locke J., de Lemos J.A., Massaro J.M., McClelland R.L., Taylor A., Levine B.D. Astronaut Cardiovascular Health and Risk Modification (Astro-CHARM) Coronary Calcium Atherosclerotic Cardiovascular Disease Risk Calculator. Circulation. 2018;138:1819–1827. doi: 10.1161/CIRCULATIONAHA.118.033505. [DOI] [PubMed] [Google Scholar]
- 83.Liu Z., Deng D., Lu H., Sun J., Lv L., Li S., Peng G., Ma X., Li J., Li Z., et al. Evaluation of Machine Learning Models for Predicting Antimicrobial Resistance of Actinobacillus pleuropneumoniae From Whole Genome Sequences. Front. Microbiol. 2020;11:48. doi: 10.3389/fmicb.2020.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Budd S., Blaas A., Hoarfrost A., Khezeli K., Silva K.D., Soboczenski F., Mackintosh G., Chia N., Kalantari J. Prototyping CRISP: A Causal Relation and Inference Search Platform applied to Colorectal Cancer Data; Proceedings of the 2021 IEEE 3rd Global Conference on Life Sciences and Technologies (LifeTech); Nara, Japan. 9–11 March 2021; pp. 517–521. [Google Scholar]
- 85.Aryal S., Alimadadi A., Manandhar I., Joe B., Cheng X. Machine Learning Strategy for Gut Microbiome-Based Diagnostic Screening of Cardiovascular Disease. Hypertension. 2020;76:1555–1562. doi: 10.1161/HYPERTENSIONAHA.120.15885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cammarota G., Ianiro G., Ahern A., Carbone C., Temko A., Claesson M.J., Gasbarrini A., Tortora G. Gut microbiome, big data and machine learning to promote precision medicine for cancer. Nat. Rev. Gastroenterol. Hepatol. 2020;17:635–648. doi: 10.1038/s41575-020-0327-3. [DOI] [PubMed] [Google Scholar]
- 87.Estévez O., Anibarro L., Garet E., Pallares Á., Barcia L., Calviño L., Maueia C., Mussá T., Fdez-Riverola F., Glez-Peña D., et al. An RNA-seq Based Machine Learning Approach Identifies Latent Tuberculosis Patients With an Active Tuberculosis Profile. Front. Immunol. 2020;11:1470. doi: 10.3389/fimmu.2020.01470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Andriasyan V., Yakimovich A., Petkidis A., Georgi F., Witte R., Puntener D., Greber U.F. Microscopy deep learning predicts virus infections and reveals mechanics of lytic-infected cells. iScience. 2021;24:102543. doi: 10.1016/j.isci.2021.102543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang X., Hu Y., Aouizerat B.E., Peng G., Marconi V.C., Corley M.J., Hulgan T., Bryant K.J., Zhao H., Krystal J.H., et al. Machine learning selected smoking-associated DNA methylation signatures that predict HIV prognosis and mortality. Clin. Epigenet. 2018;10:155. doi: 10.1186/s13148-018-0591-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kist A. Deep Learning on Edge TPUs. arXiv. 20212108.13732 [Google Scholar]
- 91.Bizzi A., Pascuzzo R., Blevins J., Moscatelli M.E.M., Grisoli M., Lodi R., Doniselli F.M., Castelli G., Cohen M.L., Stamm A., et al. Subtype Diagnosis of Sporadic Creutzfeldt-Jakob Disease with Diffusion Magnetic Resonance Imaging. Ann. Neurol. 2021;89:560–572. doi: 10.1002/ana.25983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tang Z., Chuang K.V., DeCarli C., Jin L.-W., Beckett L., Keiser M.J., Dugger B.N. Interpretable classification of Alzheimer’s disease pathologies with a convolutional neural network pipeline. Nat. Commun. 2019;10:2173. doi: 10.1038/s41467-019-10212-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Esteva A., Kuprel B., Novoa R.A., Ko J., Swetter S.M., Blau H.M., Thrun S. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115–118. doi: 10.1038/nature21056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhu C.Y., Wang Y.K., Chen H.P., Gao K.L., Shu C., Wang J.C., Yan L.F., Yang Y.G., Xie F.Y., Liu J. A Deep Learning Based Framework for Diagnosing Multiple Skin Diseases in a Clinical Environment. Front. Med. 2021;8:626369. doi: 10.3389/fmed.2021.626369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gulshan V., Peng L., Coram M., Stumpe M.C., Wu D., Narayanaswamy A., Venugopalan S., Widner K., Madams T., Cuadros J., et al. Development and Validation of a Deep Learning Algorithm for Detection of Diabetic Retinopathy in Retinal Fundus Photographs. Jama. 2016;316:2402–2410. doi: 10.1001/jama.2016.17216. [DOI] [PubMed] [Google Scholar]
- 96.Toscano W. Wearable Biosensor Monitor to Support Autonomous Crew Health and Readinessto Perform. [(accessed on 2 November 2022)];2017 Available online: https://ntrs.nasa.gov/citations/20190001996.
- 97.Castaldo R., Chappell M.J., Byrne H., Innominato P.F., Hughes S., Pescapè A., Pecchia L. Detection of melatonin-onset in real settings via wearable sensors and artificial intelligence. A pilot study. Biomed. Signal Process. Control. 2021;65:102386. doi: 10.1016/j.bspc.2020.102386. [DOI] [Google Scholar]
- 98.Cogswell D., Bisesi P., Markwald R.R., Cruickshank-Quinn C., Quinn K., McHill A., Melanson E.L., Reisdorph N., Wright K.P., Jr., Depner C.M. Identification of a Preliminary Plasma Metabolome-based Biomarker for Circadian Phase in Humans. J. Biol. Rhythm. 2021;36:369–383. doi: 10.1177/07487304211025402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Waisberg E., Ong J., Zaman N., Kamran S.A., Lee A.G., Tavakkoli A. A non-invasive approach to monitor anemia during long-duration spaceflight with retinal fundus images and deep learning. Life Sci. Space Res. 2022;33:69–71. doi: 10.1016/j.lssr.2022.04.004. [DOI] [PubMed] [Google Scholar]
- 100.Kist A.M., Döllinger M. Efficient Biomedical Image Segmentation on EdgeTPUs at Point of Care. IEEE Access. 2020;8:139356–139366. doi: 10.1109/ACCESS.2020.3012722. [DOI] [Google Scholar]
- 101.Hlushchuk R., Zubler C., Barré S., Correa Shokiche C., Schaad L., Röthlisberger R., Wnuk M., Daniel C., Khoma O., Tschanz S.A., et al. Cutting-edge microangio-CT: New dimensions in vascular imaging and kidney morphometry. Am. J. Physiol. Ren. Physiol. 2018;314:F493–F499. doi: 10.1152/ajprenal.00099.2017. [DOI] [PubMed] [Google Scholar]
- 102.Goodwill J. NASA SpaceCube Edge TPU SmallSat Card for Autonomous Operations and Onboard Science-Data Analysis; Proceedings of the Small Satellite Conference; Logan, UT, USA. 7–12 August 2021. [Google Scholar]
- 103.Broderick T.J., Privitera M.B., Parazynski S.E., Cuttino M. Simulated hand-assisted laparoscopic surgery (HALS) in microgravity. J. Laparoendosc. Adv. Surg. Tech. Part A. 2005;15:145–148. doi: 10.1089/lap.2005.15.145. [DOI] [PubMed] [Google Scholar]
- 104.Tabaza L., Virk H.u.H., Janzer S., George J.C. Robotic-assisted percutaneous coronary intervention in a COVID-19 patient. Catheter. Cardiovasc. Interv. 2021;97:E343–E345. doi: 10.1002/ccd.28982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kane W.J., Charles E.J., Mehaffey J.H., Hawkins R.B., Meneses K.B., Tache-Leon C.A., Yang Z. Robotic compared with laparoscopic cholecystectomy: A propensity matched analysis. Surgery. 2020;167:432–435. doi: 10.1016/j.surg.2019.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Garrow C.R., Kowalewski K.F., Li L., Wagner M., Schmidt M.W., Engelhardt S., Hashimoto D.A., Kenngott H.G., Bodenstedt S., Speidel S., et al. Machine Learning for Surgical Phase Recognition: A Systematic Review. Ann. Surg. 2021;273:684–693. doi: 10.1097/SLA.0000000000004425. [DOI] [PubMed] [Google Scholar]
- 107.Fourati F., Alouini M.-S. Artificial Intelligence for Satellite Communication: A Review. arXiv. 2012 doi: 10.23919/ICN.2021.0015.2101.10899 [DOI] [Google Scholar]
- 108.Chowell D., Yoo S.-K., Valero C., Pastore A., Krishna C., Lee M., Hoen D., Shi H., Kelly D.W., Patel N., et al. Improved prediction of immune checkpoint blockade efficacy across multiple cancer types. Nat. Biotechnol. 2021 doi: 10.1038/s41587-021-01070-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Westfall S., Carracci F., Estill M., Zhao D., Wu Q.-l., Shen L., Simon J., Pasinetti G.M. Optimization of probiotic therapeutics using machine learning in an artificial human gastrointestinal tract. Sci. Rep. 2021;11:1067. doi: 10.1038/s41598-020-79947-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. [(accessed on 2 November 2022)]; Available online: https://oig.nasa.gov/docs/IG-21-025.pdf.
- 111.Matar M., Gokoglu S.A., Prelich M.T., Gallo C.A., Iqbal A.K., Britten R.A., Prabhu R.K., Myers J.G., Jr. Machine Learning Models to Predict Cognitive Impairment of Rodents Subjected to Space Radiation. Front. Syst. Neurosci. 2021;15:713131. doi: 10.3389/fnsys.2021.713131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhu Z., Ng D.W.H., Park H.S., McAlpine M.C. 3D-printed multifunctional materials enabled by artificial-intelligence-assisted fabrication technologies. Nat. Rev. Mater. 2021;6:27–47. doi: 10.1038/s41578-020-00235-2. [DOI] [Google Scholar]
- 113. [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/sites/default/files/files/3D_Printing-v3.pdf.
- 114.Galib S.M., Bhowmik P.K., Avachat A.V., Lee H.K. A comparative study of machine learning methods for automated identification of radioisotopes using NaI gamma-ray spectra. Nucl. Eng. Technol. 2021;53:4072–4079. doi: 10.1016/j.net.2021.06.020. [DOI] [Google Scholar]
- 115.Israel D.J., Mauldin K.D., Roberts C.J., Mitchell J.W., Pulkkinen A.A., Cooper L.V.D., Johnson M.A., Christe S.D., Gramling C.J. LunaNet: A Flexible and Extensible Lunar Exploration Communications and Navigation Infrastructure; Proceedings of the 2020 IEEE Aerospace Conference; Big Sky, MT, USA. 7–14 March 2020; pp. 1–14. [Google Scholar]
- 116.Recenti M., Ricciardi C., Aubonnet R., Picone I., Jacob D., Svansson H.Á.R., Agnarsdóttir S., Karlsson G.H., Baeringsdóttir V., Petersen H., et al. Toward Predicting Motion Sickness Using Virtual Reality and a Moving Platform Assessing Brain, Muscles, and Heart Signals. Front. Bioeng. Biotechnol. 2021;9:635661. doi: 10.3389/fbioe.2021.635661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.O’Connell M. Preventing and treating motion sickness using virtual reality; Proceedings of the 43rd COSPAR Scientific Assembly; Sydney, Australia. 28 January–4 February 2021; p. 2071. [Google Scholar]
- 118. [(accessed on 2 November 2022)]; Available online: https://ntrs.nasa.gov/citations/20130012776.
- 119.Lewis J.E., Kemp M.L. Integration of machine learning and genome-scale metabolic modeling identifies multi-omics biomarkers for radiation resistance. Nat. Commun. 2021;12:2700. doi: 10.1038/s41467-021-22989-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kim E., Chung Y. Feasibility study of deep learning based radiosensitivity prediction model of National Cancer Institute-60 cell lines using gene expression. Nucl. Eng. Technol. 2021;56:103156. doi: 10.1016/j.net.2021.10.020. [DOI] [Google Scholar]
- 121.Belli M., Tabocchini M.A. Ionizing Radiation-Induced Epigenetic Modifications and Their Relevance to Radiation Protection. Int. J. Mol. Sci. 2020;21:5993. doi: 10.3390/ijms21175993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. [(accessed on 2 November 2022)]. Available online: https://www.4bridgeworks.com/interview-using-ai-to-revolutionise-data-acceleration/
- 123.Patel S. The effects of microgravity and space radiation on cardiovascular health: From low-Earth orbit and beyond. IJC Heart Vasc. 2020;30:100595. doi: 10.1016/j.ijcha.2020.100595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Levine B.D., Lane L.D., Watenpaugh D.E., Gaffney F.A., Buckey J.C., Blomqvist C.G. Maximal exercise performance after adaptation to microgravity. J. Appl. Physiol. 1996;81:686–694. doi: 10.1152/jappl.1996.81.2.686. [DOI] [PubMed] [Google Scholar]
- 125.Watenpaugh D.E., Hargens A.R. Comprehensive Physiology. Wiley-Blackwell; Hoboken, NJ, USA: 2011. The Cardiovascular System in Microgravity; pp. 631–674. [Google Scholar]
- 126.Norsk P. Blood pressure regulation IV: Adaptive responses to weightlessness. Eur. J. Appl. Physiol. 2014;114:481–497. doi: 10.1007/s00421-013-2797-2. [DOI] [PubMed] [Google Scholar]
- 127.Ertl A.C., Diedrich A., Biaggioni I., Levine B.D., Robertson R.M., Cox J.F., Zuckerman J.H., Pawelczyk J.A., Ray C.A., Buckey J.C., Jr., et al. Human muscle sympathetic nerve activity and plasma noradrenaline kinetics in space. J. Physiol. 2002;538:321–329. doi: 10.1113/jphysiol.2001.012576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Fu Q., Shibata S., Hastings J.L., Platts S.H., Hamilton D.M., Bungo M.W., Stenger M.B., Ribeiro C., Adams-Huet B., Levine B.D. Impact of Prolonged Spaceflight on Orthostatic Tolerance During Ambulation and Blood Pressure Profiles in Astronauts. Circulation. 2019;140:729–738. doi: 10.1161/CIRCULATIONAHA.119.041050. [DOI] [PubMed] [Google Scholar]
- 129.Khine H.W., Steding-Ehrenborg K., Hastings J.L., Kowal J., Daniels J.D., Page R.L., Goldberger J.J., Ng J., Adams-Huet B., Bungo M.W., et al. Effects of Prolonged Spaceflight on Atrial Size, Atrial Electrophysiology, and Risk of Atrial Fibrillation. Circ. Arrhythmia Electrophysiol. 2018;11:e005959. doi: 10.1161/CIRCEP.117.005959. [DOI] [PubMed] [Google Scholar]
- 130.Wuu Y.R., Hu B., Okunola H., Paul A.M., Blaber E.A., Cheng-Campbell M., Beheshti A., Grabham P. LET-Dependent Low Dose and Synergistic Inhibition of Human Angiogenesis by Charged Particles: Validation of miRNAs that Drive Inhibition. iScience. 2020;23:101771. doi: 10.1016/j.isci.2020.101771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Vernice N.A., Meydan C., Afshinnekoo E., Mason C.E. Long-term spaceflight and the cardiovascular system. Precis. Clin. Med. 2020;3:284–291. doi: 10.1093/pcmedi/pbaa022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Abdel-Qadir H., Ethier J.L., Lee D.S., Thavendiranathan P., Amir E. Cardiovascular toxicity of angiogenesis inhibitors in treatment of malignancy: A systematic review and meta-analysis. Cancer Treat. Rev. 2017;53:120–127. doi: 10.1016/j.ctrv.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 133.Shrestha S., Bates J.E., Liu Q., Smith S.A., Oeffinger K.C., Chow E.J., Gupta A.C., Owens C.A., Constine L.S., Hoppe B.S., et al. Radiation therapy related cardiac disease risk in childhood cancer survivors: Updated dosimetry analysis from the Childhood Cancer Survivor Study. Radiother. Oncol. 2021;163:199–208. doi: 10.1016/j.radonc.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Shimizu Y., Kodama K., Nishi N., Kasagi F., Suyama A., Soda M., Grant E.J., Sugiyama H., Sakata R., Moriwaki H., et al. Radiation exposure and circulatory disease risk: Hiroshima and Nagasaki atomic bomb survivor data, 1950-2003. BMJ. 2010;340:b5349. doi: 10.1136/bmj.b5349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Killander F., Wieslander E., Karlsson P., Holmberg E., Lundstedt D., Holmberg L., Werner L., Koul S., Haghanegi M., Kjellen E., et al. No Increased Cardiac Mortality or Morbidity of Radiation Therapy in Breast Cancer Patients After Breast-Conserving Surgery: 20-Year Follow-up of the Randomized SweBCGRT Trial. Int. J. Radiat. Oncol. Biol. Phys. 2020;107:701–709. doi: 10.1016/j.ijrobp.2020.04.003. [DOI] [PubMed] [Google Scholar]
- 136.Crucian B., Babiak-Vazquez A., Johnston S., Pierson D.L., Ott C.M., Sams C. Incidence of clinical symptoms during long-duration orbital spaceflight. Int. J. Gen. Med. 2016;9:383–391. doi: 10.2147/IJGM.S114188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Thornton W.E., Linder B.J., Moore T.P., Pool S.L. Gastrointestinal motility in space motion sickness. Aviat. Space Environ. Med. 1987;58:A16–A21. [PubMed] [Google Scholar]
- 138.Bae J.H., Kim J.G., Heo K., Yang K., Kim T.O., Yi J.M. Identification of radiation-induced aberrant hypomethylation in colon cancer. BMC Genom. 2015;16:56. doi: 10.1186/s12864-015-1229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Simonsen L.C., Slaba T.C., Guida P., Rusek A. NASA’s first ground-based Galactic Cosmic Ray Simulator: Enabling a new era in space radiobiology research. PLoS Biol. 2020;18:e3000669. doi: 10.1371/journal.pbio.3000669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Voorhies A.A., Mark Ott C., Mehta S., Pierson D.L., Crucian B.E., Feiveson A., Oubre C.M., Torralba M., Moncera K., Zhang Y., et al. Study of the impact of long-duration space missions at the International Space Station on the astronaut microbiome. Sci. Rep. 2019;9:9911. doi: 10.1038/s41598-019-46303-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Shao D., Yao L., Riaz M.S., Zhu J., Shi J., Jin M., Huang Q., Yang H. Simulated microgravity affects some biological characteristics of Lactobacillus acidophilus. Appl. Microbiol. Biotechnol. 2017;101:3439–3449. doi: 10.1007/s00253-016-8059-6. [DOI] [PubMed] [Google Scholar]
- 142.Benoit M.R., Li W., Stodieck L.S., Lam K.S., Winther C.L., Roane T.M., Klaus D.M. Microbial antibiotic production aboard the International Space Station. Appl. Microbiol. Biotechnol. 2006;70:403–411. doi: 10.1007/s00253-005-0098-3. [DOI] [PubMed] [Google Scholar]
- 143.Jiang P., Green S.J., Chlipala G.E., Turek F.W., Vitaterna M.H. Reproducible changes in the gut microbiome suggest a shift in microbial and host metabolism during spaceflight. Microbiome. 2019;7:113. doi: 10.1186/s40168-019-0724-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kirkpatrick A.W., Hamilton D.R., McKee J.L., MacDonald B., Pelosi P., Ball C.G., Roberts D., McBeth P.B., Cocolini F., Ansaloni L., et al. Do we have the guts to go? The abdominal compartment, intra-abdominal hypertension, the human microbiome and exploration class space missions. Can. J. Surg. 2020;63:E581–E593. doi: 10.1503/cjs019219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Schmidt M.A., Meydan C., Schmidt C.M., Afshinnekoo E., Mason C.E. The NASA Twins Study: The Effect of One Year in Space on Long-Chain Fatty Acid Desaturases and Elongases. Lifestyle Genom. 2020;13:107–121. doi: 10.1159/000506769. [DOI] [PubMed] [Google Scholar]
- 146.Beheshti A., Chakravarty K., Fogle H., Fazelinia H., Silveira W.A.D., Boyko V., Polo S.L., Saravia-Butler A.M., Hardiman G., Taylor D., et al. Multi-omics analysis of multiple missions to space reveal a theme of lipid dysregulation in mouse liver. Sci. Rep. 2019;9:19195. doi: 10.1038/s41598-019-55869-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Jonscher K.R., Alfonso-Garcia A., Suhalim J.L., Orlicky D.J., Potma E.O., Ferguson V.L., Bouxsein M.L., Bateman T.A., Stodieck L.S., Levi M., et al. Spaceflight Activates Lipotoxic Pathways in Mouse Liver. PLoS ONE. 2016;11:e0152877. doi: 10.1371/journal.pone.0152877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Krieger S.S., Zwart S.R., Mehta S., Wu H., Simpson R.J., Smith S.M., Crucian B. Alterations in Saliva and Plasma Cytokine Concentrations During Long-Duration Spaceflight. Front. Immunol. 2021;12:725748. doi: 10.3389/fimmu.2021.725748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Crucian B.E., Zwart S.R., Mehta S., Uchakin P., Quiriarte H.D., Pierson D., Sams C.F., Smith S.M. Plasma cytokine concentrations indicate that in vivo hormonal regulation of immunity is altered during long-duration spaceflight. J. Interferon Cytokine Res. 2014;34:778–786. doi: 10.1089/jir.2013.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Stowe R.P., Sams C.F., Pierson D.L. Effects of mission duration on neuroimmune responses in astronauts. Aviat. Space Environ. Med. 2003;74:1281–1284. [PubMed] [Google Scholar]
- 151.Buravkova L.B., Rykova M.P., Grigorieva V., Antropova E.N. Cell interactions in microgravity: Cytotoxic effects of natural killer cells in vitro. J. Gravit. Physiol. A J. Int. Soc. Gravit. Physiol. 2004;11:P177–P180. [PubMed] [Google Scholar]
- 152.Bigley A.B., Agha N.H., Baker F.L., Spielmann G., Kunz H.E., Mylabathula P.L., Rooney B.V., Laughlin M.S., Mehta S.K., Pierson D.L., et al. NK cell function is impaired during long-duration spaceflight. J. Appl. Physiol. 2019;126:842–853. doi: 10.1152/japplphysiol.00761.2018. [DOI] [PubMed] [Google Scholar]
- 153.Spielmann G., Agha N., Kunz H., Simpson R.J., Crucian B., Mehta S., Laughlin M., Campbell J. B cell homeostasis is maintained during long-duration spaceflight. J. Appl. Physiol. 2019;126:469–476. doi: 10.1152/japplphysiol.00789.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kaur I., Simons E.R., Castro V.A., Ott C.M., Pierson D.L. Changes in monocyte functions of astronauts. Brain Behav. Immun. 2005;19:547–554. doi: 10.1016/j.bbi.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 155.Schwarzenberg M., Pippia P., Meloni M.A., Cossu G., Cogoli-Greuter M., Cogoli A. Signal transduction in T lymphocytes—A comparison of the data from space, the free fall machine and the random positioning machine. Adv. Space Res. 1999;24:793–800. doi: 10.1016/S0273-1177(99)00075-7. [DOI] [PubMed] [Google Scholar]
- 156.Stowe R.P., Sams C.F., Mehta S.K., Kaur I., Jones M.L., Feeback D.L., Pierson D.L. Leukocyte subsets and neutrophil function after short-term spaceflight. J. Leukoc. Biol. 1999;65:179–186. doi: 10.1002/jlb.65.2.179. [DOI] [PubMed] [Google Scholar]
- 157.Grove D.S., Pishak S.A., Mastro A.M. The effect of a 10-day space flight on the function, phenotype, and adhesion molecule expression of splenocytes and lymph node lymphocytes. Exp. Cell Res. 1995;219:102–109. doi: 10.1006/excr.1995.1210. [DOI] [PubMed] [Google Scholar]
- 158.Nash P.V., Konstantinova I.V., Fuchs B.B., Rakhmilevich A.L., Lesnyak A.T., Mastro A.M. Effect of spaceflight on lymphocyte proliferation and interleukin-2 production. J. Appl. Physiol. 1992;73:186S–190S. doi: 10.1152/jappl.1992.73.2.S186. [DOI] [PubMed] [Google Scholar]
- 159.Stahn A.C., Werner A., Opatz O., Maggioni M.A., Steinach M., von Ahlefeld V.W., Moore A., Crucian B.E., Smith S.M., Zwart S.R., et al. Increased core body temperature in astronauts during long-duration space missions. Sci. Rep. 2017;7:16180. doi: 10.1038/s41598-017-15560-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Crucian B.E., Choukèr A., Simpson R.J., Mehta S., Marshall G., Smith S.M., Zwart S.R., Heer M., Ponomarev S., Whitmire A., et al. Immune System Dysregulation During Spaceflight: Potential Countermeasures for Deep Space Exploration Missions. Front. Immunol. 2018;9:1437. doi: 10.3389/fimmu.2018.01437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Crucian B.E., Makedonas G., Sams C.F., Pierson D.L., Simpson R., Stowe R.P., Smith S.M., Zwart S.R., Krieger S.S., Rooney B., et al. Countermeasures-based Improvements in Stress, Immune System Dysregulation and Latent Herpesvirus Reactivation onboard the International Space Station—Relevance for Deep Space Missions and Terrestrial Medicine. Neurosci. Biobehav. Rev. 2020;115:68–76. doi: 10.1016/j.neubiorev.2020.05.007. [DOI] [PubMed] [Google Scholar]
- 162.Rodman C., Almeida-Porada G., George S.K., Moon J., Soker S., Pardee T., Beaty M., Guida P., Sajuthi S.P., Langefeld C.D., et al. In vitro and in vivo assessment of direct effects of simulated solar and galactic cosmic radiation on human hematopoietic stem/progenitor cells. Leukemia. 2017;31:1398–1407. doi: 10.1038/leu.2016.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Crucian B., Johnston S., Mehta S., Stowe R., Uchakin P., Quiriarte H., Pierson D., Laudenslager M.L., Sams C. A case of persistent skin rash and rhinitis with immune system dysregulation onboard the International Space Station. J. Allergy Clin. Immunol. Pract. 2016;4:759–762.e758. doi: 10.1016/j.jaip.2015.12.021. [DOI] [PubMed] [Google Scholar]
- 164.Nickerson C.A., Ott C.M., Wilson J.W., Ramamurthy R., Pierson D.L. Microbial responses to microgravity and other low-shear environments. Microbiol. Mol. Biol. Rev. 2004;68:345–361. doi: 10.1128/MMBR.68.2.345-361.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Nickerson C.A., Ott C.M., Mister S.J., Morrow B.J., Burns-Keliher L., Pierson D.L. Microgravity as a novel environmental signal affecting Salmonella enterica serovar Typhimurium virulence. Infect. Immun. 2000;68:3147–3152. doi: 10.1128/IAI.68.6.3147-3152.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Alfrey C.P., Udden M.M., Huntoon C.L., Driscoll T. Destruction of newly released red blood cells in space flight. Med. Sci. Sport. Exerc. 1996;28:S42–S44. doi: 10.1097/00005768-199610000-00032. [DOI] [PubMed] [Google Scholar]
- 167.Smith S.M. Red blood cell and iron metabolism during space flight. Nutrition. 2002;18:864–866. doi: 10.1016/S0899-9007(02)00912-7. [DOI] [PubMed] [Google Scholar]
- 168.Kunz H., Quiriarte H., Simpson R.J., Ploutz-Snyder R., McMonigal K., Sams C., Crucian B. Alterations in hematologic indices during long-duration spaceflight. BMC Hematol. 2017;17:12. doi: 10.1186/s12878-017-0083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Preston D.L., Ron E., Tokuoka S., Funamoto S., Nishi N., Soda M., Mabuchi K., Kodama K. Solid cancer incidence in atomic bomb survivors: 1958-1998. Radiat. Res. 2007;168:1–64. doi: 10.1667/RR0763.1. [DOI] [PubMed] [Google Scholar]
- 170.Cardis E., Krewski D., Boniol M., Drozdovitch V., Darby S.C., Gilbert E.S., Akiba S., Benichou J., Ferlay J., Gandini S., et al. Estimates of the cancer burden in Europe from radioactive fallout from the Chernobyl accident. Int. J. Cancer. 2006;119:1224–1235. doi: 10.1002/ijc.22037. [DOI] [PubMed] [Google Scholar]
- 171.National Council on Radiation Protection and Measurements . Uncertainties in Fatal Cancer Risk Estimates Used in Radiation Protection. National Council on Radiation Protection and Measurements; Bethesda, MD, USA: 1997. NCRP Report 126. [Google Scholar]
- 172.Cullings H.M., Pierce D.A., Kellerer A.M. Accounting for neutron exposure in the Japanese atomic bomb survivors. Radiat. Res. 2014;182:587–598. doi: 10.1667/RR13663.1. [DOI] [PubMed] [Google Scholar]
- 173.O’Neill P.M., Golge S., Slaba T.C. NASA Galactic Cosmic Radiation Environment Model: Badhwar-O’Neill (2014); Proceedings of the International Cosmic Ray Conference (ICRC); Moscow, Russia. 25–29 August 2016. [Google Scholar]
- 174.Cucinotta F.A., Kim M.-H.Y., Chappell L.J., Huff J.L. How Safe Is Safe Enough? Radiation Risk for a Human Mission to Mars. PLoS ONE. 2013;8:e74988. doi: 10.1371/journal.pone.0074988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Tubiana M. Prevention of cancer and the dose-effect relationship: The carcinogenic effects of ionizing radiations. Cancer Radiother. J. Soc. Fr. Radiother. Oncol. 2009;13:238–258. doi: 10.1016/j.canrad.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 176.Council N.R. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. The National Academies Press; Washington, DC, USA: 2006. p. 422. [PubMed] [Google Scholar]
- 177.Heuskin A.C., Osseiran A.I., Tang J., Costes S.V. Simulating Space Radiation-Induced Breast Tumor Incidence Using Automata. Radiat. Res. 2016;186:27–38. doi: 10.1667/RR14338.1. [DOI] [PubMed] [Google Scholar]
- 178.Suman S., Kumar S., Fornace A.J., Datta K. Space radiation exposure persistently increased leptin and IGF1 in serum and activated leptin-IGF1 signaling axis in mouse intestine. Sci. Rep. 2016;6:31853. doi: 10.1038/srep31853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Peng Y., Brown N., Finnon R., Warner C.L., Liu X., Genik P.C., Callan M.A., Ray F.A., Borak T.B., Badie C., et al. Radiation leukemogenesis in mice: Loss of PU.1 on chromosome 2 in CBA and C57BL/6 mice after irradiation with 1 GeV/nucleon 56Fe ions, X rays or gamma rays. Part I. Experimental observations. Radiat. Res. 2009;171:474–483. doi: 10.1667/RR1547.1. [DOI] [PubMed] [Google Scholar]
- 180.Watanabe H., Ogiu T., Nishizaki M., Fujimoto N., Kido S., Ishimura Y., Shiraki K., Kuramoto K., Hirata S., Shoji S., et al. Induction of ovarian tumors by heavy ion irradiation in B6C3F1 mice. Oncol. Rep. 1998;5:1377–1380. doi: 10.3892/or.5.6.1377. [DOI] [PubMed] [Google Scholar]
- 181.Bielefeldt-Ohmann H., Genik P.C., Fallgren C.M., Ullrich R.L., Weil M.M. Animal studies of charged particle-induced carcinogenesis. Health Phys. 2012;103:568–576. doi: 10.1097/HP.0b013e318265a257. [DOI] [PubMed] [Google Scholar]
- 182.Lahtz C., Bates S.E., Jiang Y., Li A.X., Wu X., Hahn M.A., Pfeifer G.P. Gamma irradiation does not induce detectable changes in DNA methylation directly following exposure of human cells. PLoS ONE. 2012;7:e44858. doi: 10.1371/journal.pone.0044858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Borak T.B., Heilbronn L.H., Townsend L.W., McBeth R.A., de Wet W. Quality factors for space radiation: A new approach. Life Sci. Space Res. 2014;1:96–102. doi: 10.1016/j.lssr.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 184. [(accessed on 2 November 2022)]. Available online: https://www.nationalacademies.org/news/2021/06/nasa-should-update-astronaut-radiation-exposure-limits-improve-communication-of-cancer-risks#:~:text=WASHINGTON%20%E2%80%94%20To%20protect%20astronauts%20from,Sciences%2C%20Engineering%2C%20and%20Medicine.
- 185.Hsu J., Gore-Panter S., Tchou G., Castel L., Lovano B., Moravec C.S., Pettersson G.B., Roselli E.E., Gillinov A.M., McCurry K.R., et al. Genetic Control of Left Atrial Gene Expression Yields Insights into the Genetic Susceptibility for Atrial Fibrillation. Circ. Genom. Precis. Med. 2018;11:e002107. doi: 10.1161/CIRCGEN.118.002107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Harris L.R., Jenkin M., Jenkin H., Zacher J.E., Dyde R.T. The effect of long-term exposure to microgravity on the perception of upright. NPJ Microgravity. 2017;3:3. doi: 10.1038/s41526-016-0005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Clément G., Skinner A., Lathan C. Distance and Size Perception in Astronauts during Long-Duration Spaceflight. Life. 2013;3:524–537. doi: 10.3390/life3040524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Young L.R., Oman C.M., Watt D.G., Money K.E., Lichtenberg B.K. Spatial orientation in weightlessness and readaptation to earth’s gravity. Science. 1984;225:205–208. doi: 10.1126/science.6610215. [DOI] [PubMed] [Google Scholar]
- 189.Benson A.J., Kass J.R., Vogel H. European vestibular experiments on the Spacelab-1 mission: 4. Thresholds of perception of whole-body linear oscillation. Exp. Brain Res. 1986;64:264–271. doi: 10.1007/BF00237742. [DOI] [PubMed] [Google Scholar]
- 190.DiZio P., Lackner J.R. The effects of gravitoinertial force level and head movements on post-rotational nystagmus and illusory after-rotation. Exp. Brain Res. 1988;70:485–495. doi: 10.1007/BF00247597. [DOI] [PubMed] [Google Scholar]
- 191.Rafiq A., Hummel R., Lavrentyev V., Derry W., Williams D., Merrell R.C. Microgravity effects on fine motor skills: Tying surgical knots during parabolic flight. Aviat. Space Environ. Med. 2006;77:852–856. [PubMed] [Google Scholar]
- 192.Mulavara A.P., Peters B.T., Miller C.A., Kofman I.S., Reschke M.F., Taylor L.C., Lawrence E.L., Wood S.J., Laurie S.S., Lee S.M.C., et al. Physiological and Functional Alterations after Spaceflight and Bed Rest. Med. Sci. Sport. Exerc. 2018;50:1961–1980. doi: 10.1249/MSS.0000000000001615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Tays G.D., Hupfeld K.E., McGregor H.R., Salazar A.P., De Dios Y.E., Beltran N.E., Reuter-Lorenz P.A., Kofman I.S., Wood S.J., Bloomberg J.J., et al. The Effects of Long Duration Spaceflight on Sensorimotor Control and Cognition. Front. Neural Circuits. 2021;15:723504. doi: 10.3389/fncir.2021.723504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Taylor A.J., Beauchamp J.D., Briand L., Heer M., Hummel T., Margot C., McGrane S., Pieters S., Pittia P., Spence C. Factors affecting flavor perception in space: Does the spacecraft environment influence food intake by astronauts? Compr. Rev. Food Sci. Food Saf. 2020;19:3439–3475. doi: 10.1111/1541-4337.12633. [DOI] [PubMed] [Google Scholar]
- 195.Olabi A.A., Lawless H.T., Hunter J.B., Levitsky D.A., Halpern B.P. The effect of microgravity and space flight on the chemical senses. J. Food Sci. 2002;67:468–478. doi: 10.1111/j.1365-2621.2002.tb10622.x. [DOI] [PubMed] [Google Scholar]
- 196.Bershad E.M., Urfy M.Z., Calvillo E., Tang R., Cajavilca C., Lee A.G., Venkatasubba Rao C.P., Suarez J.I., Chen D. Marked olfactory impairment in idiopathic intracranial hypertension. J. Neurol. Neurosurg. Psychiatry. 2014;85:959–964. doi: 10.1136/jnnp-2013-307232. [DOI] [PubMed] [Google Scholar]
- 197.Wood S.J., Paloski W.H., Clark J.B. Assessing Sensorimotor Function Following ISS with Computerized Dynamic Posturography. Aerosp. Med. Hum. Perform. 2015;86:A45–A53. doi: 10.3357/AMHP.EC07.2015. [DOI] [PubMed] [Google Scholar]
- 198.Miller C.A., Kofman I.S., Brady R.R., May-Phillips T.R., Batson C.D., Lawrence E.L., Taylor L.C., Peters B.T., Mulavara A.P., Feiveson A.H., et al. Functional Task and Balance Performance in Bed Rest Subjects and Astronauts. Aerosp. Med. Hum. Perform. 2018;89:805–815. doi: 10.3357/AMHP.5039.2018. [DOI] [PubMed] [Google Scholar]
- 199.Moore S.T., Dilda V., Morris T.R., Yungher D.A., MacDougall H.G., Wood S.J. Long-duration spaceflight adversely affects post-landing operator proficiency. Sci. Rep. 2019;9:2677. doi: 10.1038/s41598-019-39058-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Gazenko O.G., Genin A.M., Egorov A.D. Major Medical Results Of The Salyut-6—Soyuz 185-Day Space Flight. In: Napolitano L.G., editor. Space Mankind’s Fourth Environment. Elsevier; Pergamon, Turkey: 1982. pp. 275–293. [Google Scholar]
- 201.Pechenkova E., Nosikova I., Rumshiskaya A., Litvinova L., Rukavishnikov I., Mershina E., Sinitsyn V., Van Ombergen A., Jeurissen B., Jillings S., et al. Alterations of Functional Brain Connectivity After Long-Duration Spaceflight as Revealed by fMRI. Front. Physiol. 2019;10:761. doi: 10.3389/fphys.2019.00761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Hupfeld K.E., McGregor H.R., Koppelmans V., Beltran N.E., Kofman I.S., De Dios Y.E., Riascos R.F., Reuter-Lorenz P.A., Wood S.J., Bloomberg J.J., et al. Brain and Behavioral Evidence for Reweighting of Vestibular Inputs with Long-Duration Spaceflight. Cereb. Cortex. 2021;32:bhab239. doi: 10.1093/cercor/bhab239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Mader T.H., Gibson C.R., Miller N.R., Subramanian P.S., Patel N.B., Lee A.G. An overview of spaceflight-associated neuro-ocular syndrome (SANS) Neurol. India. 2019;67:S206–S211. doi: 10.4103/0028-3886.259126. [DOI] [PubMed] [Google Scholar]
- 204.Lee A.G., Mader T.H., Gibson C.R., Tarver W., Rabiei P., Riascos R.F., Galdamez L.A., Brunstetter T. Spaceflight associated neuro-ocular syndrome (SANS) and the neuro-ophthalmologic effects of microgravity: A review and an update. NPJ Microgravity. 2020;6:7. doi: 10.1038/s41526-020-0097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Wåhlin A., Holmlund P., Fellows A.M., Malm J., Buckey J.C., Eklund A. Optic Nerve Length before and after Spaceflight. Ophthalmology. 2021;128:309–316. doi: 10.1016/j.ophtha.2020.07.007. [DOI] [PubMed] [Google Scholar]
- 206.Zwart S.R., Gibson C.R., Mader T.H., Ericson K., Ploutz-Snyder R., Heer M., Smith S.M. Vision changes after spaceflight are related to alterations in folate- and vitamin B-12-dependent one-carbon metabolism. J. Nutr. 2012;142:427–431. doi: 10.3945/jn.111.154245. [DOI] [PubMed] [Google Scholar]
- 207.Liu K.C., Fleischman D., Lee A.G., Killer H.E., Chen J.J., Bhatti M.T. Current concepts of cerebrospinal fluid dynamics and the translaminar cribrosa pressure gradient: A paradigm of optic disk disease. Surv. Ophthalmol. 2020;65:48–66. doi: 10.1016/j.survophthal.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 208.Wostyn P., De Winne F., Stern C., Mader T.H., Gibson C.R., De Deyn P.P. Potential Involvement of the Ocular Glymphatic System in Optic Disc Edema in Astronauts. Aerosp. Med. Hum. Perform. 2020;91:975–977. doi: 10.3357/AMHP.5670.2020. [DOI] [PubMed] [Google Scholar]
- 209.Wostyn P., Gibson C.R., Mader T.H. The odyssey of the ocular and cerebrospinal fluids during a mission to Mars: The “ocular glymphatic system” under pressure. Eye. 2021;36:686–691. doi: 10.1038/s41433-021-01721-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Mader T.H., Gibson C.R., Barratt M.R., Miller N.R., Subramanian P.S., Killer H.E., Tarver W.J., Sargsyan A.E., Garcia K., Hart S.F., et al. Persistent Globe Flattening in Astronauts following Long-Duration Spaceflight. Neuro-Ophthalmol. (Aeolus Press) 2021;45:29–35. doi: 10.1080/01658107.2020.1791189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Billica R. Presentation to the Institute of Medicine Committee on Creating a Vision for Space Medicine During Travel Beyond Earth Orbit. National Academy Press; Washington, DC, USA: 2000. Inflight medical events for U.S. astronauts during space shuttle programs STS-1 through STS-89, April 1981–January 1998. NASA Johnson Space Center, Houston, 22 February. As cited in: IOM, 2001. Safe passage: Astronaut care for exploration missions. [Google Scholar]
- 212.Kanas N., Manzey D. Space Psychology and Psychiatry. Volume 16 Springer; Dordrecht, The Netherlands: 2003. [Google Scholar]
- 213.Hanes D.A., McCollum G. Cognitive-vestibular interactions: A review of patient difficulties and possible mechanisms. J. Vestib. Res. Equilib. Orientat. 2006;16:75–91. doi: 10.3233/VES-2006-16301. [DOI] [PubMed] [Google Scholar]
- 214.Belavy D.L., Adams M., Brisby H., Cagnie B., Danneels L., Fairbank J., Hargens A.R., Judex S., Scheuring R.A., Sovelius R., et al. Disc herniations in astronauts: What causes them, and what does it tell us about herniation on earth? Eur. Spine J. 2016;25:144–154. doi: 10.1007/s00586-015-3917-y. [DOI] [PubMed] [Google Scholar]
- 215.Bailey J.F., Miller S.L., Khieu K., O’Neill C.W., Healey R.M., Coughlin D.G., Sayson J.V., Chang D.G., Hargens A.R., Lotz J.C. From the international space station to the clinic: How prolonged unloading may disrupt lumbar spine stability. Spine J. 2018;18:7–14. doi: 10.1016/j.spinee.2017.08.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Fincke E.M., Padalka G., Lee D., van Holsbeeck M., Sargsyan A.E., Hamilton D.R., Martin D., Melton S.L., McFarlin K., Dulchavsky S.A. Evaluation of shoulder integrity in space: First report of musculoskeletal US on the International Space Station. Radiology. 2005;234:319–322. doi: 10.1148/radiol.2342041680. [DOI] [PubMed] [Google Scholar]
- 217.Anderson A.P., Newman D.J., Welsch R.E. Statistical Evaluation of Causal Factors Associated with Astronaut Shoulder Injury in Space Suits. Aerosp. Med. Hum. Perform. 2015;86:606–613. doi: 10.3357/AMHP.4220.2015. [DOI] [PubMed] [Google Scholar]
- 218.Fitzgerald J. Cartilage breakdown in microgravity-a problem for long-term spaceflight? NPJ Regen. Med. 2017;2:1–2. doi: 10.1038/s41536-017-0016-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Winnard A., Debuse D., Caplan N. Countermeasure Development for Lumbopelvic Deconditioning in Space. IntechOpen; London, UK: 2018. pp. 121–138. [Google Scholar]
- 220.Snijders C.J.D.L., Hides J.A., Pool-Goudzwaard A.L., Richardson C.A. Study of Low Back Pain in Crew Members During Space Flight (Muscle) University of Rotterdam; Rotterdam, The Netherlands: 2016. [(accessed on 2 November 2022)]. Available online: https://www.nasa.gov/mission_pages/station/research/experiments/176.html. [Google Scholar]
- 221.Kwok A.T., Mohamed N.S., Plate J.F., Yammani R.R., Rosas S., Bateman T.A., Livingston E., Moore J.E., Kerr B.A., Lee J., et al. Spaceflight and hind limb unloading induces an arthritic phenotype in knee articular cartilage and menisci of rodents. Sci. Rep. 2021;11:10469. doi: 10.1038/s41598-021-90010-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Frost H.M. Mechanical determinants of bone modeling. Metab. Bone Dis. Relat. Res. 1982;4:217–229. doi: 10.1016/0221-8747(82)90031-5. [DOI] [PubMed] [Google Scholar]
- 223.Frost H.M. Bone “mass” and the “mechanostat”: A proposal. Anat. Rec. 1987;219:1–9. doi: 10.1002/ar.1092190104. [DOI] [PubMed] [Google Scholar]
- 224.Vico L., van Rietbergen B., Vilayphiou N., Linossier M.-T., Locrelle H., Normand M., Zouch M., Gerbaix M., Bonnet N., Novikov V., et al. Cortical and Trabecular Bone Microstructure Did Not Recover at Weight-Bearing Skeletal Sites and Progressively Deteriorated at Non-Weight-Bearing Sites During the Year Following International Space Station Missions. J. Bone Miner. Res. 2017;32:2010–2021. doi: 10.1002/jbmr.3188. [DOI] [PubMed] [Google Scholar]
- 225.Vico L., Collet P., Guignandon A., Lafage-Proust M.H., Thomas T., Rehaillia M., Alexandre C. Effects of long-term microgravity exposure on cancellous and cortical weight-bearing bones of cosmonauts. Lancet. 2000;355:1607–1611. doi: 10.1016/S0140-6736(00)02217-0. [DOI] [PubMed] [Google Scholar]
- 226.Lang T., Van Loon J.J.W.A., Bloomfield S., Vico L., Chopard A., Rittweger J., Kyparos A., Blottner D., Vuori I., Gerzer R., et al. Towards human exploration of space: The THESEUS review series on muscle and bone research priorities. NPJ Microgravity. 2017;3:8. doi: 10.1038/s41526-017-0013-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Elliott A.R., Prisk G.K., Guy H.J., West J.B. Lung volumes during sustained microgravity on Spacelab SLS-1. J. Appl. Physiol. 1994;77:2005–2014. doi: 10.1152/jappl.1994.77.4.2005. [DOI] [PubMed] [Google Scholar]
- 228.Agostoni E., Hyatt R.E. Comprehensive Physiology. Wiley-Blackwell; Hoboken, NJ, USA: 2011. Static Behavior of the Respiratory System; pp. 113–130. [Google Scholar]
- 229.Paiva M., Verbanck S., Estenne M. Chest wall mechanics in microgravity: Results from parabolic flights. Life Sci. Res. Space. 1994;366:307. [Google Scholar]
- 230.Prisk G.K., Guy H.J., Elliott A.R., West J.B. Inhomogeneity of pulmonary perfusion during sustained microgravity on SLS-1. J. Appl. Physiol. 1994;76:1730–1738. doi: 10.1152/jappl.1994.76.4.1730. [DOI] [PubMed] [Google Scholar]
- 231.Guy H.J., Prisk G.K., Elliott A.R., Deutschman R.A., 3rd, West J.B. Inhomogeneity of pulmonary ventilation during sustained microgravity as determined by single-breath washouts. J. Appl. Physiol. 1994;76:1719–1729. doi: 10.1152/jappl.1994.76.4.1719. [DOI] [PubMed] [Google Scholar]
- 232.Russomano T., Evetts S.N., Castro J., Dos Santos M.A., Gavillon J., Azevedo D.F., Whittle J., Coats E., Ernsting J. A device for sampling arterialized earlobe blood in austere environments. Aviat. Space Environ. Med. 2006;77:453–455. [PubMed] [Google Scholar]
- 233.Prisk G.K., Fine J.M., Cooper T.K., West J.B. Vital capacity, respiratory muscle strength, and pulmonary gas exchange during long-duration exposure to microgravity. J. Appl. Physiol. 2006;101:439–447. doi: 10.1152/japplphysiol.01419.2005. [DOI] [PubMed] [Google Scholar]
- 234.Prisk G.K., Fine J.M., Cooper T.K., West J.B. Lung function is unchanged in the 1 G environment following 6-months exposure to microgravity. Eur. J. Appl. Physiol. 2008;103:617–623. doi: 10.1007/s00421-008-0754-2. [DOI] [PubMed] [Google Scholar]
- 235.Tronnier H., Wiebusch M., Heinrich U. Change in skin physiological parameters in space--report on and results of the first study on man. Ski. Pharmacol. Physiol. 2008;21:283–292. doi: 10.1159/000148045. [DOI] [PubMed] [Google Scholar]
- 236.Longnecker D.E., Manning F.J., Worth M.H. Jr., editors. Review of NASA’s Longitudinal Study of Astronaut Health. National Academy of Sciences; Washington, DC, USA: 2004. [PubMed] [Google Scholar]
- 237.Garcia K.M., Harrison M.F., Sargsyan A.E., Ebert D., Dulchavsky S.A. Real-time Ultrasound Assessment of Astronaut Spinal Anatomy and Disorders on the International Space Station. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2018;37:987–999. doi: 10.1002/jum.14438. [DOI] [PubMed] [Google Scholar]
- 238.Arbeille P., Chaput D., Zuj K., Depriester A., Maillet A., Belbis O., Benarroche P., Barde S. Remote Echography between a Ground Control Center and the International Space Station Using a Tele-operated Echograph with Motorized Probe. Ultrasound Med. Biol. 2018;44:2406–2412. doi: 10.1016/j.ultrasmedbio.2018.06.012. [DOI] [PubMed] [Google Scholar]
- 239.Scott J.M., Downs M., Martin D.S., Hougland E., Sarmiento L., Arzeno N., Pettit D.R., Ploutz-Snyder R., Cunningham D., Jones L.W., et al. Teleguided self-ultrasound scanning for longitudinal monitoring of muscle mass during spaceflight. iScience. 2021;24:102344. doi: 10.1016/j.isci.2021.102344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Martin D.S., South D.A., Garcia K.M., Arbeille P. Ultrasound in space. Ultrasound Med. Biol. 2003;29:1–12. doi: 10.1016/S0301-5629(02)00692-0. [DOI] [PubMed] [Google Scholar]
- 241.Martin D.S., Caine T.L., Matz T., Lee S.M., Stenger M.B., Sargsyan A.E., Platts S.H. Virtual guidance as a tool to obtain diagnostic ultrasound for spaceflight and remote environments. Aviat. Space Environ. Med. 2012;83:995–1000. doi: 10.3357/ASEM.3279.2012. [DOI] [PubMed] [Google Scholar]
- 242.Jones J.A., Sargsyan A.E., Barr Y.R., Melton S., Hamilton D.R., Dulchavsky S.A., Whitson P.A. Diagnostic ultrasound at MACH 20: Retroperitoneal and pelvic imaging in space. Ultrasound Med. Biol. 2009;35:1059–1067. doi: 10.1016/j.ultrasmedbio.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 243.Law J., Macbeth P.B. Ultrasound: From Earth to space. McGill J. Med. MJM Int. Forum Adv. Med. Sci. By Stud. 2011;13:59. doi: 10.26443/mjm.v13i2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Dietrich D., Dekova R., Davy S., Fahrni G., Geissbühler A. Applications of Space Technologies to Global Health: Scoping Review. J. Med. Internet Res. 2018;20:e230. doi: 10.2196/jmir.9458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. [(accessed on 2 November 2022)]; Available online: https://jscfeatures.jsc.nasa.gov/pages.ashx/1065/New%20Innovative%20Technology%20to%20Keep%20Astronauts%20Healthy.
- 246.Cramer A., Hecla J., Wu D., Lai X., Boers T., Yang K., Moulton T., Kenyon S., Arzoumanian Z., Krull W., et al. Stationary Computed Tomography for Space and other Resource-constrained Environments. Sci. Rep. 2018;8:14195. doi: 10.1038/s41598-018-32505-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Hamilton D.R., Sargsyan A.E., Kirkpatrick A.W., Nicolaou S., Campbell M., Dawson D.L., Melton S.L., Beck G., Guess T., Rasbury J., et al. Sonographic detection of pneumothorax and hemothorax in microgravity. Aviat. Space Environ. Med. 2004;75:272–277. [PubMed] [Google Scholar]
- 248.Kirkpatrick A.W., Hamilton D.R., Nicolaou S., Sargsyan A.E., Campbell M.R., Feiveson A., Dulchavsky S.A., Melton S., Beck G., Dawson D.L. Focused Assessment with Sonography for Trauma in weightlessness: A feasibility study. J. Am. Coll. Surg. 2003;196:833–844. doi: 10.1016/S1072-7515(02)01906-3. [DOI] [PubMed] [Google Scholar]
- 249.Johnston S.L., Campbell M.R., Billica R.D., Gilmore S.M. Cardiopulmonary resuscitation in microgravity: Efficacy in the swine during parabolic flight. Aviat. Space Environ. Med. 2004;75:546–550. [PubMed] [Google Scholar]
- 250.Kansagra A.P., Shute T.S. Space: The Final Frontier for IR. J. Vasc. Interv. Radiol. JVIR. 2015;26:825–828. doi: 10.1016/j.jvir.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 251.Hinkelbein J., Kerkhoff S., Adler C., Ahlbäck A., Braunecker S., Burgard D., Cirillo F., De Robertis E., Glaser E., Haidl T.K., et al. Cardiopulmonary resuscitation (CPR) during spaceflight—A guideline for CPR in microgravity from the German Society of Aerospace Medicine (DGLRM) and the European Society of Aerospace Medicine Space Medicine Group (ESAM-SMG) Scand. J. Trauma Resusc. Emerg. Med. 2020;28:108. doi: 10.1186/s13049-020-00793-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Komorowski M., Fleming S., Kirkpatrick A.W. Fundamentals of Anesthesiology for Spaceflight. J. Cardiothorac. Vasc. Anesth. 2016;30:781–790. doi: 10.1053/j.jvca.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 253.Kaczka D.W., Beck G. Mechanical ventilation in orbit: Emphasis on closed-loop ventilation. Respir. Care Clin. North Am. 2004;10:369–400, vii. doi: 10.1016/j.rcc.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 254.Starck C., Thierry S., Bernard C.I., Morineau T., Jaulin F., Chapelain P., Komorowski M. Tracheal intubation in microgravity: A simulation study comparing direct laryngoscopy and videolaryngoscopy(†) Br. J. Anaesth. 2020;125:e47–e53. doi: 10.1016/j.bja.2019.11.029. [DOI] [PubMed] [Google Scholar]
- 255.Campbell M.R., Billica R.D., Johnston S.L., 3rd, Muller M.S. Performance of advanced trauma life support procedures in microgravity. Aviat. Space Environ. Med. 2002;73:907–912. [PubMed] [Google Scholar]
- 256.Campbell M.R. A review of surgical care in space. J. Am. Coll. Surg. 2002;194:802–812. doi: 10.1016/S1072-7515(02)01145-6. [DOI] [PubMed] [Google Scholar]
- 257.Kirkpatrick A.W., Nicolaou S., Campbell M.R., Sargsyan A.E., Dulchavsky S.A., Melton S., Beck G., Dawson D.L., Billica R.D., Johnston S.L., et al. Percutaneous aspiration of fluid for management of peritonitis in space. Aviat. Space Environ. Med. 2002;73:925–930. [PubMed] [Google Scholar]
- 258.Kirkpatrick A.W., Keaney M., Kmet L., Ball C.G., Campbell M.R., Kindratsky C., Groleau M., Tyssen M., Keyte J., Broderick T.J. Intraperitoneal gas insufflation will be required for laparoscopic visualization in space: A comparison of laparoscopic techniques in weightlessness. J. Am. Coll. Surg. 2009;209:233–241. doi: 10.1016/j.jamcollsurg.2009.03.026. [DOI] [PubMed] [Google Scholar]
- 259.Campbell M.R., Kirkpatrick A.W., Billica R.D., Johnston S.L., Jennings R., Short D., Hamilton D., Dulchavsky S.A. Endoscopic surgery in weightlessness: The investigation of basic principles for surgery in space. Surg. Endosc. 2001;15:1413–1418. doi: 10.1007/s004640080178. [DOI] [PubMed] [Google Scholar]
- 260.Campbell M.R., Williams D.R., Buckey J.C., Jr., Kirkpatrick A.W. Animal surgery during spaceflight on the Neurolab Shuttle mission. Aviat. Space Environ. Med. 2005;76:589–593. [PubMed] [Google Scholar]
- 261.Panesar S.S., Ashkan K. Surgery in space. Br. J. Surg. 2018;105:1234–1243. doi: 10.1002/bjs.10908. [DOI] [PubMed] [Google Scholar]
- 262.Kirkpatrick A.W., Mckee J.L., Tien H.C.-N., Laporta A.J., Lavell K., Leslie T., King D., McBeth P.B., Brien S., Roberts D.J., et al. Damage control surgery in weightlessness: A comparative study of simulated torso hemorrhage control comparing terrestrial and weightless conditions. J. Trauma Acute Care Surg. 2017;82:392–399. doi: 10.1097/TA.0000000000001310. [DOI] [PubMed] [Google Scholar]
- 263.Raison N., Khan M.S., Challacombe B. Telemedicine in Surgery: What are the Opportunities and Hurdles to Realising the Potential? Curr. Urol. Rep. 2015;16:43. doi: 10.1007/s11934-015-0522-x. [DOI] [PubMed] [Google Scholar]
- 264.Korte C., Nair S.S., Nistor V., Low T.P., Doarn C.R., Schaffner G. Determining the threshold of time-delay for teleoperation accuracy and efficiency in relation to telesurgery. Telemed. J. e-Health. 2014;20:1078–1086. doi: 10.1089/tmj.2013.0367. [DOI] [PubMed] [Google Scholar]
- 265.Hughson R.L., Robertson A.D., Arbeille P., Shoemaker J.K., Rush J.W., Fraser K.S., Greaves D.K. Increased postflight carotid artery stiffness and inflight insulin resistance resulting from 6-mo spaceflight in male and female astronauts. Am. J. Physiology. Heart Circ. Physiol. 2016;310:H628–H638. doi: 10.1152/ajpheart.00802.2015. [DOI] [PubMed] [Google Scholar]
- 266.Arbeille P., Provost R., Zuj K. Carotid and Femoral Artery Intima-Media Thickness During 6 Months of Spaceflight. Aerosp. Med. Hum. Perform. 2016;87:449–453. doi: 10.3357/AMHP.4493.2016. [DOI] [PubMed] [Google Scholar]
- 267.Després J.P. Physical Activity, Sedentary Behaviours, and Cardiovascular Health: When Will Cardiorespiratory Fitness Become a Vital Sign? Can. J. Cardiol. 2016;32:505–513. doi: 10.1016/j.cjca.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 268.Wang Y., Boerma M., Zhou D. Ionizing Radiation-Induced Endothelial Cell Senescence and Cardiovascular Diseases. Radiat. Res. 2016;186:153–161. doi: 10.1667/RR14445.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Stein T.P. Weight, muscle and bone loss during space flight: Another perspective. Eur. J. Appl. Physiol. 2013;113:2171–2181. doi: 10.1007/s00421-012-2548-9. [DOI] [PubMed] [Google Scholar]
- 270.Clément G.R., Bukley A.P., Paloski W.H. Artificial gravity as a countermeasure for mitigating physiological deconditioning during long-duration space missions. Front. Syst. Neurosci. 2015;9:92. doi: 10.3389/fnsys.2015.00092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Turner A.E. AIAA SPACE 2014 Conference and Exposition. American Institute of Aeronautics and Astronautics; Reston, VA, USA: 2014. Orbit Dynamics and Habitability Considerations for a Space Hotel with Artificial Gravity. AIAA SPACE Forum. [Google Scholar]
- 272.Mehta S., Crucian B., Pierson D., Sams C., Stowe R. Artificial Gravity And The Immune System Function. In: Clément G., Bukley A., editors. Artificial Gravity. Springer; New York, NY, USA: 2007. pp. 271–286. [Google Scholar]
- 273. [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/feature/goddard/2021/-ai-could-speed-fault-diagnosis-in-spacecraft.
- 274.Doarn C.R., Nicogossian A.E., Merrell R.C. Applications of telemedicine in the United States space program. Telemed. J. 1998;4:19–30. doi: 10.1089/tmj.1.1998.4.19. [DOI] [PubMed] [Google Scholar]
- 275.Chelmins D.T., Briones J., Downey J., Clark G., Gannon A. Cognitive communications for NASA space systems; Proceedings of the International Communications Satellite Systems Conference; Washington, DA, USA. 28–29 September 2021. [Google Scholar]
- 276.Laperre B., Amaya J., Lapenta G. Dynamic Time Warping as a New Evaluation for Dst Forecast With Machine Learning. Front. Astron. Space Sci. 2020;7:1–17. doi: 10.3389/fspas.2020.00039. [DOI] [Google Scholar]
- 277.Rayman R., Croome K., Galbraith N., McClure R., Morady R., Peterson S., Smith S., Subotic V., Van Wynsberghe A., Primak S. Long-distance robotic telesurgery: A feasibility study for care in remote environments. Int. J. Med. Robot. Comput. Assist. Surg. MRCAS. 2006;2:216–224. doi: 10.1002/rcs.99. [DOI] [PubMed] [Google Scholar]
- 278.Chen A.I., Balter M.L., Maguire T.J., Yarmush M.L. Deep learning robotic guidance for autonomous vascular access. Nat. Mach. Intell. 2020;2:104–115. doi: 10.1038/s42256-020-0148-7. [DOI] [Google Scholar]
- 279.Pantalone D., Faini G.S., Cialdai F., Sereni E., Bacci S., Bani D., Bernini M., Pratesi C., Stefàno P., Orzalesi L., et al. Robot-assisted surgery in space: Pros and cons. A review from the surgeon’s point of view. NPJ Microgravity. 2021;7:56. doi: 10.1038/s41526-021-00183-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/mission_pages/NEEMO/index.html.
- 281. [(accessed on 2 November 2022)]; Available online: https://www.nasa.gov/risky-space-business-challenge.
- 282.Isaksson L.J., Pepa M., Zaffaroni M., Marvaso G., Alterio D., Volpe S., Corrao G., Augugliaro M., Starzyńska A., Leonardi M.C., et al. Machine Learning-Based Models for Prediction of Toxicity Outcomes in Radiotherapy. Front. Oncol. 2020;10:790. doi: 10.3389/fonc.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Krittanawong C. Big Data Analytics, the Microbiome, Host-omic and Bug-omic Data and Risk for Cardiovascular Disease. Heart Lung Circ. 2018;27:e26–e27. doi: 10.1016/j.hlc.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 284.da Silveira W.A., Fazelinia H., Rosenthal S.B., Laiakis E.C., Kim M.S., Meydan C., Kidane Y., Rathi K.S., Smith S.M., Stear B., et al. Comprehensive Multi-omics Analysis Reveals Mitochondrial Stress as a Central Biological Hub for Spaceflight Impact. Cell. 2020;183:1185–1201.e1120. doi: 10.1016/j.cell.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Krittanawong C., Rogers A.J., Johnson K.W., Wang Z., Turakhia M.P., Halperin J.L., Narayan S.M. Integration of novel monitoring devices with machine learning technology for scalable cardiovascular management. Nat. Rev. Cardiol. 2021;18:75–91. doi: 10.1038/s41569-020-00445-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Chriskos P., Frantzidis C.A., Gkivogkli P.T., Bamidis P.D., Kourtidou-Papadeli C. Achieving Accurate Automatic Sleep Staging on Manually Pre-processed EEG Data Through Synchronization Feature Extraction and Graph Metrics. Front. Hum. Neurosci. 2018;12:110. doi: 10.3389/fnhum.2018.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287. [(accessed on 2 November 2022)]. Available online: https://www.businesswire.com/news/home/20190416005378/en/Recovery-Force-Receives-Prestigious-1.8M-Grant-National.
- 288.Nie G.Y., Duh H.B.L., Liu Y., Wang Y. Analysis on Mitigation of Visually Induced Motion Sickness by Applying Dynamical Blurring on a User’s Retina. IEEE Trans. Vis. Comput. Graph. 2020;26:2535–2545. doi: 10.1109/TVCG.2019.2893668. [DOI] [PubMed] [Google Scholar]
- 289.Varker T., Brand R.M., Ward J., Terhaag S., Phelps A. Efficacy of synchronous telepsychology interventions for people with anxiety, depression, posttraumatic stress disorder, and adjustment disorder: A rapid evidence assessment. Psychol. Serv. 2019;16:621–635. doi: 10.1037/ser0000239. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.