Abstract
Background:
Transportation noise may induce cardiovascular disease, but the public health implications are unclear.
Objectives:
The study aimed to assess exposure–response relationships for different transportation noise sources and ischemic heart disease (IHD), including subtypes.
Methods:
Pooled analyses were performed of nine cohorts from Denmark and Sweden, together including 132,801 subjects. Time-weighted long-term exposure to road, railway, and aircraft noise, as well as air pollution, was estimated based on residential histories. Hazard ratios (HRs) were calculated using Cox proportional hazards models following adjustment for lifestyle and socioeconomic risk factors.
Results:
A total of 22,459 incident cases of IHD were identified during follow-up from national patient and mortality registers, including 7,682 cases of myocardial infarction. The adjusted HR for IHD was 1.03 [95% confidence interval (CI) 1.00, 1.05] per 10 dB for both road and railway noise exposure during 5 y prior to the event. Higher risks were indicated for IHD excluding angina pectoris cases, with HRs of 1.06 (95% CI: 1.03, 1.08) and 1.05 (95% CI: 1.01, 1.08) per 10 dB for road and railway noise, respectively. Corresponding HRs for myocardial infarction were 1.02 (95% CI: 0.99, 1.05) and 1.04 (95% CI: 0.99, 1.08). Increased risks were observed for aircraft noise but without clear exposure–response relations. A threshold at around 55 dB was suggested in the exposure–response relation for road traffic noise and IHD.
Discussion:
Exposure to road, railway, and aircraft noise in the prior 5 y was associated with an increased risk of IHD, particularly after exclusion of angina pectoris cases, which are less well identified in the registries. https://doi.org/10.1289/EHP10745
Introduction
Exposure to traffic noise is increasing because of ongoing urbanization, densification of urban settlements, and growth of the transport sector. In 2017, Europeans were estimated to be exposed to road traffic noise levels of at least 55 dB , which is the health-based indicator level used for noise mapping by the European Environment Agency.1 The World Health Organization (WHO) has estimated that more than 1 million healthy years of life are lost annually due to traffic-related noise in Western Europe, primarily caused by sleep disturbance and annoyance, but cardiovascular disease also contributes.2 The burden of disease from transportation noise was ranked the second highest in Europe, after air pollution, among environmental causes, and in 2018 the WHO proposed stricter environmental noise guidelines for the European Region.
A systematic review on environmental noise exposure and cardiovascular diseases for the WHO guidelines concluded that the evidence linking exposure to road traffic noise and incidence of ischemic heart disease (IHD) was of high quality.3 Longitudinal epidemiological studies on traffic noise and incidence of IHD also including data on lifestyle factors provide the most compelling information, and such studies published after those included in the WHO review provide a mixed picture,4–11 however, mostly reporting that transportation noise exposure was associated with IHD and/or myocardial infarction. Most of the evidence relates to road traffic noise, and only few of the studies assessed exposure to railway and/or aircraft noise.5,7,9 Moreover, it is not clear whether risks associated with noise exposure differ between major subtypes of IHD, primarily myocardial infarction and angina pectoris, or between nonfatal and fatal IHD. Detailed evaluations of the shape of the exposure–response relationships were generally not performed; however, two recent studies indicated that there may be thresholds in the association between road traffic noise and incidence of IHD8 or myocardial infarction,11 which would be crucial for health impact assessments.
Assessment of interactions between traffic noise exposure and other risk factors for IHD may be important in prioritization of preventive action, e.g., for identification of vulnerable groups, as well as for the understanding of etiological mechanisms. For example, long-term exposure to air pollution such as fine particulate matter ( ) increases the risk of cardiovascular disease, including IHD.12 A growing number of studies on cardiovascular disease have estimated exposure to both road traffic noise and air pollution,4,6–11,13–17 but the evidence on interactions is not consistent. Other risk factors of interest include smoking, physical activity, body mass index (BMI), and socioeconomic status. However, no clear picture on interactions with traffic noise in relation to IHD has emerged, partly because of lack of data.18
The aim of this study was to assess exposure–response relations for long-term exposure to noise from road traffic, railways and aircraft, and incidence of IHD based on combined analyses of nine Scandinavian cohorts. In particular, we studied associations for common subtypes of IHD and whether the noise-related risks were modified by other risk factors, including air pollution. This constitutes a major extension of earlier publications based on the cohorts, including longer follow-up and substantially increased number of cases, which together with pooled analyses, enables detailed evaluation of the shape of exposure–response functions and interactions and for subtypes of IHD.
Methods
Study Population
The study is based on the “Nordic studies on occupational and traffic noise in relation to disease” (NordSOUND) project (www.nordsound.dk), and uses pooled data from nine Scandinavian cohorts.17 Two cohorts were included from Denmark: the nationwide Danish Nurse Cohort (DNC) and the Diet, Cancer and Health cohort (DCH) from Copenhagen/Aarhus. The seven Swedish cohorts originated from Malmö, with the Malmö Diet and Cancer Study (MDC); Gothenburg, including the Swedish Primary Prevention Cohort (PPS) and the GOT-MONICA cohort; and Stockholm County: the Swedish National Study of Aging and Care in Kungsholmen (SNAC-K), the Stockholm Screening Across the Lifespan Twin Study (SALT), the Stockholm 60 Years Old study (Sixty), and the Stockholm Diabetes Prevention Program (SDPP). The four cohorts from Stockholm used identical methodology for environmental exposure assessment and harmonized covariate information.19 The nine study cohorts are described in detail in Table S1, including key references. All cohorts had registry-based residential address history for participants, with estimated transportation noise exposure for each address. If needed, delayed entry was used for the study participants, implying that follow-up started when transportation noise data for all relevant sources were available during the 5 preceding years. This is referred to as the study baseline.
The study was conducted in accordance with the Helsinki Declaration and approved by relevant ethics review boards for the included cohorts. Informed consent was obtained from all cohort participants.
Outcome Assessment
Data on individual IHD events were obtained via linkage to national patient and mortality registers. Each event was defined based on the International Classification of Diseases (ICD) versions 9 or 10 as hospitalization or death with principal diagnosis of IHD (ICD9: 410–414; ICD10: I20–I25), and the two subgroups IHD excluding angina pectoris (ICD9: 410, 411, 412, 414; ICD10: I21–I25) and myocardial infarction (ICD9: 410; ICD10: I21–I23). The selection of the subgroup IHD excluding angina pectoris was made to achieve a better comparability between the Danish and Swedish data because angina pectoris constituted a considerably larger part of IHD in the Danish cohorts (cf. Table 1). Myocardial infarction was included because it was the outcome analyzed in several earlier studies on traffic noise and this diagnosis generally has a high quality. Supplementary analyses were also performed focusing on the subgroups angina pectoris (ICD9: 413; ICD10: I20) and IHD excluding angina pectoris and myocardial infarction (ICD9: 411, 412, 414; ICD10: I25). Subjects with an IHD diagnosis before the study baseline were excluded from the analyses because they generally receive medical treatment and may change their lifestyle, which could affect the susceptibility to noise. All first events (hospitalization or death) of IHD during follow-up were classified as incident. IHD cases were coded as fatal if they originated from a mortality registry or if deaths from any cause occurred within 28 d after hospitalization for IHD.
Table 1.
Administrative and baseline characteristics of nine included cohorts from Scandinavia () at study baseline.
| Copenhagen or Aarhus, DK | Denmark | Malmö, SE | Gothenburg, SE | Stockholm, SE | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristicsa | DCH | DNC | MDC | PPS | GOT-MONICA | SDPP | SIXTY | SNAC-K | SALT | Total |
| Follow-up period (y) | 1994–2016 | 1993–2016 | 1992–2017 | 1972–2011 | 1985–2011 | 1992–2011 | 1997–2017 | 2001–2016 | 1998–2016 | 1975–2017 |
| Median length of follow-upa (y) | 20.0 (4.0–20.5) | 15.5 (4.2–20.5) | 19.5 (2.7–24.7) | 21.5 (5.3–36.5) | 12.5 (2.5–17.5) | 20.1 (12.0–24.7) | 19.5 (6.0–20.0) | 14.5 (3.0–6.5) | 16.7 (6.7–19.0) | 19.7 (3.7–24.0) |
| Analytical sampleb (n) | 52,948 | 26,126 | 26,573 | 5,234 | 2,310 | 7,534 | 3,770 | 2,252 | 6,054 | 132,801 |
| Person-years (n) | 891,183 | 427,793 | 441,991 | 115,968 | 29,891 | 159,941 | 68,277 | 30,462 | 97,784 | 2,263,290 |
| IHD (n) | 10,086 | 3,271 | 5,024 | 1,849 | 137 | 368 | 584 | 396 | 744 | 22,459 |
| IHD excluding angina pectoris (n) | 5,027 | 1,479 | 3,054 | 1,441 | 83 | 221 | 348 | 273 | 473 | 12,399 |
| Myocardial infarction (n) | 2,606 | 668 | 2,265 | 1,222 | 70 | 170 | 227 | 160 | 294 | 7,682 |
| Fatal IHD (n) | 590 | 286 | 882 | 554 | 22 | 48 | 80 | 118 | 160 | 2,740 |
| Sex [n (%)] | ||||||||||
| Men | 24,699 (46.7) | 0 (0.0) | 10,112 (38.1) | 5,234 (100.0) | 1,089 (47.1) | 2,949 (39.1) | 1,756 (46.6) | 876 (38.9) | 2,675 (44.2) | 49,390 (37.2) |
| Women | 28,249 (53.3) | 26,126 (100.0) | 16,461 (61.9) | 0 (0.0) | 1,221 (52.9) | 4,585 (60.9) | 2,014 (53.4) | 1,376 (61.1) | 3,379 (55.8) | 83,411 (62.8) |
| Age at study baselinea (y) | 56.1 (50.8–64.2) | 51.0 (45.0–71.5) | 57.7 (47.2–71.4) | 55.0 (49.8–59.9) | 50.2 (31.8–67.1) | 47.9 (37.9–53.8) | 60.3 (60.2–60.6) | 72.2 (60.3–90.3) | 56.1 (44.3–78.8) | 55.4 (45.7–69.7) |
| Educational levelc (%) | ||||||||||
| Low | 15,856 (29.9) | 0 (0.0) | 18,000 (67.7) | 3,570 (68.2) | 470 (20.3) | 2,374 (31.5) | 1,480 (39.3) | 510 (22.6) | 1,585 (26.2) | 43,845 (33.0) |
| Medium | 24,552 (46.4) | 26,126 (100.0) | 4,719 (17.8) | 1,071 (20.5) | 1,164 (50.4) | 2,905 (38.6) | 1,226 (32.5) | 898 (39.9) | 2,216 (36.6) | 64,877 (48.9) |
| High | 12,540 (23.7) | 0 (0.0) | 3,854 (14.5) | 593 (11.3) | 676 (29.3) | 2,255 (29.9) | 1,064 (28.2) | 844 (37.5) | 2,253 (37.2) | 24,079 (18.1) |
| Marital statusd (%) | ||||||||||
| Single | 12,343 (23.3) | 7,681 (29.4) | 9,261 (34.9) | 742 (14.2) | 721 (31.2) | 1,246 (16.5) | 976 (25.9) | 1,138 (50.5) | 1,945 (32.1) | 36,053 (27.1) |
| Married | 40,605 (76.7) | 18,445 (70.6) | 17,312 (65.1) | 4,492 (85.8) | 1,589 (68.8) | 6,288 (83.5) | 2,794 (74.1) | 1,114 (49.5) | 4,109 (67.9) | 96,748 (72.9) |
| Area-level incomee (%) | ||||||||||
| 1st quartile | 17,557 (33.2) | 8,593 (32.9) | 6,164 (23.2) | 1,352 (25.8) | 505 (21.9) | 263 (3.5) | 165 (4.4) | 65 (2.9) | 429 (7.1) | 35,093 (26.4) |
| 2nd quartile | 11,904 (22.5) | 6,942 (26.6) | 5,580 (21.0) | 1,168 (22.3) | 351 (15.2) | 421 (5.6) | 324 (8.6) | 0 (0.0) | 623 (10.3) | 27,313 (20.6) |
| 3rd quartile | 8,956 (16.9) | 6,462 (24.7) | 7,068 (26.6) | 1,283 (24.5) | 500 (21.7) | 1,589 (21.1) | 908 (24.1) | 6 (0.3) | 1,107 (18.3) | 27,879 (21.0) |
| 4th quartile | 14,531 (27.4) | 4,129 (15.8) | 7,761 (29.2) | 1,431 (27.4) | 954 (41.2) | 5,261 (69.8) | 2,373 (62.9) | 2,181 (96.8) | 3,895 (64.3) | 42,516 (32.0) |
| Smoking status (%) | ||||||||||
| Current | 19,127 (36.1) | 9,193 (35.2) | 7,571 (28.5) | 2,089 (39.9) | 650 (28.1) | 1,983 (26.3) | 788 (20.9) | 349 (15.5) | 1,237 (20.4) | 42,987 (32.4) |
| Former | 14,723 (27.8) | 7,973 (30.5) | 8,766 (33.0) | 1,741 (33.3) | 543 (23.5) | 2,747 (36.5) | 1,449 (38.4) | 903 (40.1) | 2,157 (35.6) | 41,002 (30.9) |
| Never | 19,098 (36.1) | 8,960 (34.3) | 10,236 (38.5) | 1,404 (26.8) | 1,117 (48.4) | 2,804 (37.2) | 1,533 (40.7) | 1,000 (44.4) | 2,660 (44.0) | 48,812 (36.7) |
| Physical activityf (%) | ||||||||||
| Low | 27,194 (51.4) | 1,771 (6.8) | 13,570 (51.1) | 1,325 (25.3) | 402 (17.4) | 4,955 (65.8) | 2,602 (69.0) | 1,662 (73.8) | 3,280 (54.2) | 56,761 (42.7) |
| Medium | 10,422 (19.7) | 17,350 (66.4) | 5,516 (20.8) | 3,090 (59.0) | 1,452 (62.9) | 1,998 (26.5) | 882 (23.4) | 433 (19.2) | 2,217 (36.6) | 43,360 (32.7) |
| High | 15,332 (28.9) | 7,005 (26.8) | 7,487 (28.1) | 819 (15.7) | 456 (19.7) | 581 (7.7) | 286 (7.6) | 157 (7.0) | 557 (9.2) | 32,680 (24.6) |
| BMIa, | 25.5 (20.4–33.3) | 23.1 (19.2–30.1) | 25.2 (20.2–32.9) | 25.1 (20.7–30.5) | 24.5 (19.7–32.3) | 25.1 (20.4–33.3) | 26.1 (20.9–34.3) | 25.3 (19.9–32.8) | 24.1 (19.6–30.5) | 24.9 (20.0–32.6) |
| Smoking intensitya,g [g/d (among current smokers)] | 15.0 (5.0–32.1) | 15.0 (2.0–26.0) | 14.0 (1.0–30.0) | —g | 15.0 (4.0–25.0) | 15.0 (2.0–25.0) | 13.0 (2.0–25.0) | 10.0 (0.0–30.0) | 11.0 (2.0–25.0) | 15.0 (3.0–30.0) |
| Alcohol intakeh (%) | ||||||||||
| Daily | 10,418 (19.7) | 3,267 (12.8) | 4,338 (16.6) | —h | 23 (1.0) | 301 (4.0) | 210 (5.6) | 244 (10.8) | 549 (9.1) | 19,350 (15.3) |
| Weekly | 31,378 (59.3) | 15,310 (60.1) | 8,971 (34.3) | — | 814 (35.5) | 4,897 (65.2) | 1,508 (40.0) | 1,083 (48.1) | 3,867 (63.9) | 67,828 (53.7) |
| Seldom | 9,641 (18.2) | 2,917 (11.5) | 8,539 (32.7) | — | 1,292 (56.4) | 2,059 (27.4) | 1,689 (44.8) | 768 (34.1) | 1,469 (24.3) | 28,374 (22.4) |
| Never | 1,479 (2.8) | 3,976 (15.6) | 4,307 (16.4) | — | 164 (7.1) | 255 (3.4) | 361 (9.6) | 157 (7.0) | 167 (2.7) | 10,866 (8.6) |
Note: —, no data; BMI, body mass index; DCH, the Danish Diet Cancer and Health cohort; DK, Denmark; DNC, the Danish Nurse Cohort; GOT-MONICA, the Gothenburg cohort of “Multinational Monitoring of Trends and Determinants in Cardiovascular Diseases” (MONICA) project, Sweden; IHD, ischemic heart disease; MDC, the Malmö Diet and Cancer cohort, Sweden; PPS, the Primary Prevention Study cohort, Gothenburg, Sweden; SDPP, the Stockholm Diabetes Preventive Program, Sweden; SE, Sweden; SIXTY, the 60-Years cohort, Stockholm, Sweden; SNAC-K, the Swedish National Study of Aging and Care in Kungsholmen, Stockholm, Sweden.
Median and 5th–95th percentiles, unless otherwise stated.
Exclusion of prevalent IHD cases and subjects with missing information on covariates in Model 2 (age, cohort, sex, calendar year, educational level, marital status, area-income, road traffic noise, or railway noise).
Educational level is defined as “low” for primary school or less, “medium” for up to secondary school or equivalent, and “high” for university degree and more.
Marital status “single” category includes widowed or never married; “married” also includes those living with a partner.
Registry-based data from small socioeconomically homogeneous areas with inhabitants, categorized in country-specific quartiles.
Physical activity during leisure-time is defined as “low” in those active once a month or per week; “medium” in those active about once a week or ; “high” in those active 3 times a week or more or h/wk.
No data on smoking intensity were available in the PPS cohort. In other cohorts such information was missing for up to 0.7%.
No data on alcohol intake were available in the PPS cohort. In other cohorts such information was missing for up to 2.5%.
Noise Exposure Assessment
Noise levels for each address during the study period were calculated as the equivalent continuous A-weighted sound pressure level () at the most exposed façade for day (07:00–19:00 h), evening (19:00–22:00 h), and night (22:00–07:00 h), and expressed as , following penalties of 5 dB and 10 dB for noise occurring during the evening and night, respectively. For the Gothenburg cohorts, road and railway noise were estimated yearly, whereas for the Danish and Stockholm cohorts every fifth year, and for the Malmö cohort every 10th year. Noise levels for the years between those with estimates were calculated based on linear interpolation or other approximation methods (see Table S2).
All cohorts modeled road traffic and railway noise using the Nordic Prediction Method or an update of this method, Nord2000.20 For road traffic noise the input variables included geocodes, screening by terrain (except MDC) and buildings, and information on annual average daily traffic, distribution of light/heavy traffic, travel speed, and road type for all major road links. Furthermore, all cohorts but the Stockholm cohorts also included traffic information from minor roads ( vehicles per day), and the cohorts from Denmark and Gothenburg additionally included information on noise barriers. Ground absorption was considered in all estimations. Table S2 provides further details on the exposure assessment for road traffic noise.
Railway noise was calculated for all addresses within a buffer around all railway tracks, and the methods used for the different cohorts are described in Table S2. Input variables included geocodes, screening by terrain (except MDC) and buildings, and average number of trains per period (day/evening/night), train types, and travel speed. In addition, cities with trams (Gothenburg and Stockholm) and/or metro (Stockholm and Copenhagen) included these in the calculations. Cohorts from Denmark and Gothenburg also used information on noise barriers. Ground absorption was considered in all estimations.
Aircraft noise was estimated in the Danish and Stockholm cohorts using noise maps obtained from local authorities and Swedavia, respectively (Table S2). For Malmö and Gothenburg, aircraft noise was not estimated due to very low numbers of exposed. In Denmark, modeled noise exposure from airports and airfields was obtained in 5 dB categories using the Danish Airport Noise Simulation Model and the Integrated Noise Model. For Stockholm, noise was estimated in 1 dB categories using the Integrated Noise Model 7.0.
Covariates
Selection of covariates was done a priori, based on existing literature and availability of harmonizable variables across cohorts. Cohort participants filled in questionnaires at recruitment with dietary and lifestyle variables, including smoking status (current, former, never), smoking intensity (among current smokers, grams per day; not available for the PPS cohort), alcohol consumption (daily, weekly, seldom, never; not available for the PPS cohort) and leisure-time physical activity (“low” as once a month or per week, “medium” as about once a week or approximately 1 h per week, “high” as 3 times a week or more or h per week), as well as weight and height. Information on educational level (“low” as primary school or less, “medium” as up to secondary school or equivalent, or “high” as university degree and more) and marital status (“single” as widowed or never married, or “married,” which also included those living with partner) was obtained from national registers or questionnaires, and area-level (small socioeconomically homogeneous areas with inhabitants) mean income from registries, categorized in country-specific quartiles. Harmonization of covariate information between cohorts was usually achieved by relying on broad categories, such as current, former, and never for smoking. In other instances, the information was not comparable, e.g., with regard to area-level income, where country-specific distributions were used. Air pollution levels were estimated at all residential addresses during the study period using high-resolution dispersion models (see Table S3 for details). Air pollution exposure was represented by PM with a diameter (), which is influenced by both long-range transport and local emissions and by nitrogen dioxide (), primarily reflecting local emissions, such as from road traffic.21
Statistical Methods
Data from the nine cohorts were harmonized, checked and analyzed according to a common protocol. In pooled analyses we used Cox proportional hazards models, with age as underlying timescale, to calculate IHD hazard ratios (HRs) per 10 dB higher levels of road and railway noise separately for IHD, IHD excluding angina pectoris, and myocardial infarction. Aircraft noise was estimated in 5-dB intervals in the Danish cohorts and analyzed only as a categorical variable. All road, railway, and aircraft noise values below 40 dB were set to 40 dB, due to imprecision of low-level noise estimates. Each cohort member was followed from the study baseline until the IHD outcome of interest or any other incident IHD outcome, death, emigration, loss to follow-up, or end of follow-up for the different cohorts (31 December 2011–31 December 2017; see Table S1), whichever occurred first. Exposure to noise was modeled as time-weighted means (energy-weighted) over 1- and 5-y periods preceding the IHD event, taking all addresses during these periods into account. The time periods for the estimation of air pollution exposure corresponded to those for transportation noise.
The proportional hazards assumption was tested by a correlation test between scaled Schoenfeld residuals and the rank order of event time. Deviation from the assumption was detected for sex, marital status, educational level, smoking, and physical activity, which were therefore included as strata (Table S4). All models were stratified by cohort, thereby allowing different baseline hazards across cohorts.
The association between transportation noise and IHD or IHD subtypes was analyzed in four predefined models with increasing adjustment: Model 1, adjusted for age (by design), cohort, sex, and calendar year (5 y categories); Model 2 with additional adjustment for educational status (low, medium, high), marital status (married/cohabiting, single); area-level income (percentage in national quartiles), and other transportation noise sources (binary indicator for each noise source with a cutoff at 45 dB ). In Model 3 we further included lifestyle factors: smoking status (never, former, current) and physical activity (low, medium, high), and in Model 4, we added time-weighted exposure to to Model 2. A priori, Model 2 was selected as the main model, and subjects lacking information on any of the covariates in this model were excluded in all analyses. Lifestyle factors such as smoking and physical activity were not included in the main model because they may be modified by transportation noise exposure and thus included in some causal pathways.22 Air pollution was not included in the main model, which was used in complete case analyses, primarily because we lacked information on and/or for a sizable fraction of the study subjects in two cohorts.
Exposure–response relationships for IHD and subtypes in relation to road traffic and railway noise exposure were explored using cubic splines with four degrees of freedom. The overall assumption of linearity was evaluated by comparing models with linear terms of noise exposure and with smoothed splines using a chi-square test and the Akaike information criterion (AIC) to assess the best fit. In case of departure from linearity, we evaluated the location of potential thresholds in the exposure–response function by comparing models with binary exposure indicators at different levels as an interaction term with exposure.
Effect modification of the association between road traffic noise and IHD was investigated in relation to the risk factors included in the adjustment models, i.e., age, sex, marital status, BMI, physical activity, smoking status, educational level, calendar year, , and , by incorporating an interaction term between the potential effect modifier and the 5 y mean noise exposure. The Wald test was used to calculate p-values of interaction. Sensitivity analyses comprised additional adjustment for BMI, alcohol consumption, and smoking intensity, inclusion of instead of , fatal IHD as outcome, and exclusion of each of the three larger cohorts separately. Spearman’s rank correlation coefficients were used to evaluate relations between individual exposure to road, railway, and aircraft noise as well as to and during 5 y preceding the study baseline.
Analyses were performed in SAS (version 9.4; SAS Institute Inc.), Stata 14.2 (Stata Corp) and R (version 3.5.1; R Development Core Team).
Results
Overall, 149,894 persons were included in the original cohorts, but following exclusion of 5,186 with IHD before the study baseline, 981 with missing administrative or transportation noise exposure data, and 10,926 with missing covariate data included in the main model (Model 2) or Model 3, 132,801 persons remained for the pooled analysis, who were followed for 19.7 y on average (Table 1; Figure S1). A total of 22,459 incident cases of IHD were diagnosed during follow-up, including 7,682 cases of myocardial infarction. Angina pectoris accounted for more than 50% of the IHD cases in the Danish cohorts (DCH and DNS), whereas it was 40% or less in the Swedish cohorts. On the other hand, the fraction of fatal IHD cases was lower in the Danish cohorts. One of the cohorts was restricted to women (DNC) and another to men (PPS), whereas the other cohorts included both sexes. The median age at study baseline varied from 47.9 to 72.2 y, and the distribution of some risk factors also differed between the cohorts, such as for smoking, physical activity, educational level, and area-level income.
The median road traffic noise exposure at baseline ranged from 40.2 to 58.3 dB in the different cohorts, with upper 95th percentiles from 54.2 to 72.4 dB (Table 2). The distribution of road traffic noise exposure in the cohorts is further illustrated in Figure S2, showing that some cohorts contributed only marginally to exposures above 60 dB , such as most cohorts from Stockholm. Overall, railway and aircraft noise exposure tended to be lower than road traffic noise exposure, with fewer exposed to 40 dB and higher (Table 2). The levels showed a downward gradient from south to north with highest estimated concentrations in the Danish cohorts (the order of the cohorts in Table 2 generally is from south to north). levels tended to be higher in the cohorts based in urban areas (DCH, MDC, PPS, GOT-MONICA, and SNAC-K, Table S1). In general, there were low to moderate correlations between the different exposures; however, for road traffic noise exposure and , the correlation coefficient was 0.62 (Table S5).
Table 2.
Exposure to traffic noise and air pollution during 5 y prior to study baseline in nine cohorts from Scandinavia.
| Characteristicsa | Copenhagen or Aarhus, DK | Denmark | Malmö, SE | Gothenburg, SE | Stockholm, SE | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| DCH | DNC | MDC | PPS | GOT-MONICA | SDPP | SIXTY | SNAC-K | SALT | Total | |
| NordSOUND baseline | 1993–1997 | 1993, 1999 | 1991–1996 | 1975 | 1985, 1990, 1995 | 1992–1998 | 1997–1999 | 2001–2004 | 1998–2002 | 1975–2002 |
| Road traffic noise [5 y at 40 dB and above (%)] | 52,517 (99.2) | 24,902 (95.3) | 25,719 (96.8) | 5,145 (98.3) | 2,184 (94.6) | 3,845 (51.0) | 2,842 (75.4) | 2,182 (96.9) | 4,595 (75.9) | 123,931 (93.3) |
| Road traffic noisea [5 y (dB )] | 56.6 (45.0–69.4) | 53.6 (40.2–66.9) | 54.6 (42.4–67.5) | 57.5 (45.4–72.4) | 56.1 (40.0–69.2) | 40.2 (40.0–54.2) | 46.6 (40.0–62.7) | 58.3 (44.8–68.2) | 47.3 (40.0–63.3) | 54.5 (40.0–68.1) |
| Railway noise at 40 dB and above (%) | 13,638 (25.8) | 5,008 (19.2) | 7,438 (28.0) | 788 (15.1) | 460 (19.9) | 1,093 (14.5) | 1,196 (31.7) | 1,170 (52.0) | 2,063 (34.1) | 32,854 (24.7) |
| Railway noisea,b [5 y (dB )] | 52.3 (42.1–66.6) | 52.9 (41.8–65.9) | 46.8 (40.6–67.7) | 44.8 (40.4–58.8) | 44.6 (40.3–57.7) | 50.5 (42.2–67.3) | 48.9 (40.8–63.6) | 49.1 (41.6–59.5) | 49.2 (40.7–64.1) | 50.5 (41.0–66.0) |
| Aircraft noise at baselinec [5 y (%)] | ||||||||||
| dB | 52,215 (98.6) | 25,816 (98.8) | —c | — | — | 5,638 (74.8) | 3,146 (83.5) | 364 (16.1) | 5,037 (83.2) | 126,333 (95.1) |
| 40.1–50 dB | 351 (0.7) | 102 (0.4) | — | — | — | 720 (9.6) | 510 (13.5) | 1,472 (65.4) | 820 (13.5) | 3,975 (3.0) |
| dB | 382 (0.7) | 208 (0.8) | — | — | — | 1,176 (15.6) | 114 (3.0) | 416 (18.6) | 197 (3.3) | 2,493 (1.9) |
| a,d,e [5 y ()] | 19.2 (18.5–24.0) | 20.7d (15.3–26.2) | 11.0 (9.7–12.4) | 9.7e (6.4–12.2) | 9.9 (8.0–11.9) | 7.6 (6.7–8.4) | 8.0 (6.8–9.5) | 8.3 (7.7–10.3) | 7.7 (6.4–9.3) | 18.7 (7.4–24.1) |
| a,d,e [5 y ()] | 27.5 (19.6–46.5) | 10.8d (5.6–28.0) | 24.2 (13.7–34.9) | 30.7e (22.9–43.5) | 27.5 (18.4–42.4) | 8.6 (4.9–13.9) | 13.0 (5.3–26.2) | 20.5 (15.0–32.2) | 13.1 (5.5–25.6) | 23.9 (7.0–40.7) |
Note: —, no data; dB, decibel; DK, Denmark; DCH, the Danish Diet Cancer and Health cohort; DNC, the Danish Nurse Cohort; GOT-MONICA, the Gothenburg cohort of “Multinational Monitoring of Trends and Determinants in Cardiovascular Diseases” (MONICA) project, Sweden; , day-evening-night noise level based on energy equivalent noise level over a whole day with a penalty of 10 dB for nighttime noise (23.00–7.00) and a penalty of 5 dB for evening noise (i.e., 19.00–23.00); MDC, the Malmö Diet and Cancer cohort, Sweden; , particulate matter with an aerodynamic diameter of (fine particulate matter); PPS, the Primary Prevention Study cohort, Gothenburg, Sweden; , nitrogen dioxide; SDPP, the Stockholm Diabetes Preventive Program, Sweden; SE, Sweden; SIXTY, the 60-Years Cohort, Stockholm, Sweden; SNAC-K, the Swedish National Study of Aging and Care in Kungsholmen, Stockholm, Sweden.
Median and 5th–95th percentiles, unless otherwise stated.
Calculated among those with railway noise exposure at 40 dB and above.
Only among cohorts with aircraft noise exposure (thus excluding MDC, PPS, and GOT-MONICA).
Data on exposure to and missing for 9.2% in DNC.
Data on exposure to and missing for 99.1% and 2.7%, respectively, in the PPS cohort. The high fraction of missing values for is explained by recruitment in 1970–1973 and start of modeling in 1990 (see Tables S1 and S3).
Table 3 shows HRs for IHD and subtypes in relation to estimated exposure 5 y prior to the event to noise from road traffic and railways, analyzed as continuous variables. Based on the main Model 2, a HR of 1.03 (95% CI: 1.00, 1.05) per 10 dB was observed for both road traffic and railway noise exposure. For IHD excluding angina pectoris, the corresponding HRs were 1.06 (95% CI: 1.03, 1.08) and 1.05 (95% CI: 1.01, 1.08), respectively. Excess risks persisted after further adjustment for lifestyle factors (Model 3) or (Model 4), however, with some suggestion of positive confounding. Results for myocardial infarction generally pointed in the same direction but with weaker associations. Supplementary analyses focusing on angina pectoris showed HRs per 10 dB based on Model 2 of 0.99 (95% CI: 0.96, 1.02) for road traffic noise and 1.01 (95% CI: 0.97, 1.04) for railway noise. Corresponding results for the category IHD excluding angina pectoris and myocardial infarction, primarily comprising “chronic IHD” (ICD9: 414 and ICD10: I25), were 1.12 (95% CI: 1.08, 1.17) and 1.05 (95% CI: 1.02, 1.07) for road and railway noise, respectively. For aircraft noise, increased HRs were noted for the IHD subgroups in Table 3 among those exposed at 40 dB and above but without clear exposure–response relations. Results were quite similar for the different transportation noise sources and IHD groups when a 1-y exposure window was used instead of 5 y prior to the event (Table S6). Cohort-specific data focusing on IHD excluding angina pectoris suggested weaker associations for road traffic noise in the Stockholm cohorts, but a less coherent picture occurred for railway noise (Figure S3). Corresponding data for aircraft noise suggested some heterogeneity in exposure category specific risk estimates between cohorts, with the clearest exposure–response trend in the SDPP cohort (Figure S4).
Table 3.
HRs for IHD, IHD excluding angina pectoris, and myocardial infarction in relation to transportation noise exposure during 5 y prior to the event in pooled data of nine Scandinavian cohorts ().
| Model 1a | Model 2b | Model 3c | Model 4d | |||
|---|---|---|---|---|---|---|
| Exposure/outcome | Cases | Person-years | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Road traffic noise, per 10 dB | ||||||
| IHD | 22,459 | 2,263,290 | 1.04 (1.02, 1.06) | 1.03 (1.00, 1.05) | 1.02 (0.99, 1.04) | 1.02 (1.00, 1.04) |
| IHD excluding angina pectoris | 12,399 | 2,263,290 | 1.09 (1.06, 1.11) | 1.06 (1.03, 1.08) | 1.05 (1.02, 1.07) | 1.04 (1.01, 1.07) |
| Myocardial infarction | 7,682 | 2,263,290 | 1.04 (1.00, 1.07) | 1.02 (0.99, 1.05) | 1.01 (0.97, 1.04) | 1.00 (0.96, 1.04) |
| Railway noise, per 10 dB | ||||||
| IHD | 22,459 | 2,263,290 | 1.05 (1.02, 1.07) | 1.03 (1.00, 1.05) | 1.02 (1.00, 1.05) | 1.03 (1.00, 1.05) |
| IHD excluding angina pectoris | 12,399 | 2,263,290 | 1.07 (1.04, 1.10) | 1.05 (1.01, 1.08) | 1.04 (1.00, 1.07) | 1.05 (1.01, 1.08) |
| Myocardial infarction | 7,682 | 2,263,290 | 1.06 (1.01, 1.10) | 1.04 (0.99, 1.08) | 1.02 (0.98, 1.06) | 1.04 (0.99, 1.08) |
| Aircraft noise ()e | ||||||
| IHD | ||||||
| dB | 14,714 | 1,614,380 | 1 ref | 1 ref | 1 ref | 1 ref |
| 40.1–50 dB | 501 | 60,863 | 1.04 (0.94, 1.16) | 1.06 (0.96, 1.18) | 1.07 (0.96-1.19) | 1.07 (0.96, 1.19) |
| dB | 234 | 32,856 | 0.92 (0.80, 1.05) | 0.95 (0.83, 1.09) | 0.94 (0.82-1.08) | 0.95 (0.83, 1.09) |
| IHD without angina pectoris | ||||||
| dB | 7,344 | 1,614,380 | 1 ref | 1 ref | 1 ref | 1 ref |
| 40.1–50 dB | 326 | 60,863 | 1.14 (1.00, 1.30) | 1.17 (1.02, 1.34) | 1.18 (1.03-1.35) | 1.18 (1.02, 1.35) |
| dB | 151 | 32,856 | 1.03 (0.87, 1.23) | 1.09 (0.91, 1.29) | 1.08 (0.91-1.28) | 1.10 (0.92, 1.31) |
| Myocardial infarction | ||||||
| dB | 3,843 | 1,614,380 | 1 ref | 1 ref | 1 ref | 1 ref |
| 40.1–50 dB | 192 | 60,863 | 1.08 (0.90, 1.28) | 1.11 (0.93, 1.32) | 1.12 (0.94-1.33) | 1.11 (0.93, 1.33) |
| dB | 90 | 32,856 | 1.02 (0.82, 1.28) | 1.06 (0.85, 1.33) | 1.06 (0.84-1.32) | 1.07 (0.86, 1.34) |
Note: The HRs are estimated using Cox proportional hazards models with age as underlying timescale. BMI, body mass index; CI, confidence interval; HR, hazard ratio; IHD, ischemic heart disease; , particulate matter with an aerodynamic diameter of (fine particulate matter); , day-evening-night noise level based on energy equivalent noise level over a whole day with a penalty of 10 dB(A) for nighttime noise (23.00–7.00) and a penalty of 5 dB(A) for evening noise (i.e., 19.00–23.00); ref, reference.
aAdjusted for age (by design), cohort (strata), sex (men/women), and calendar year (in 5 y periods).
bModel 1 plus adjustment for educational level (low/medium/high), marital status (single/married), area-income (quartiles), and other noise sources (yes/no: road, railway, and aircraft noise indicators; for the three cohorts without aircraft noise information, all cohort members were assigned as no exposure).
cModel 2 plus adjustment for smoking status (current/former/never) and physical activity (low/medium/high).
dModel 2 plus adjustment for time-weighted exposure; 20,825 IHD, 11,245 IHD excluding angina pectoris, and 6,846 myocardial infarction cases during 2,120,816 person-years. Because the first year of modeling was 1990 but was 1975 for noise, relevant air pollution data for the model including both noise and were missing at baseline for most of the PPS cohort.
eOnly among cohorts with aircraft noise exposure (thus excluding MDC, PPS, and GOT-MONICA) with remaining 15,499 IHD cases, 7,821 IHD without angina pectoris cases, and 4,125 myocardial infarction cases.
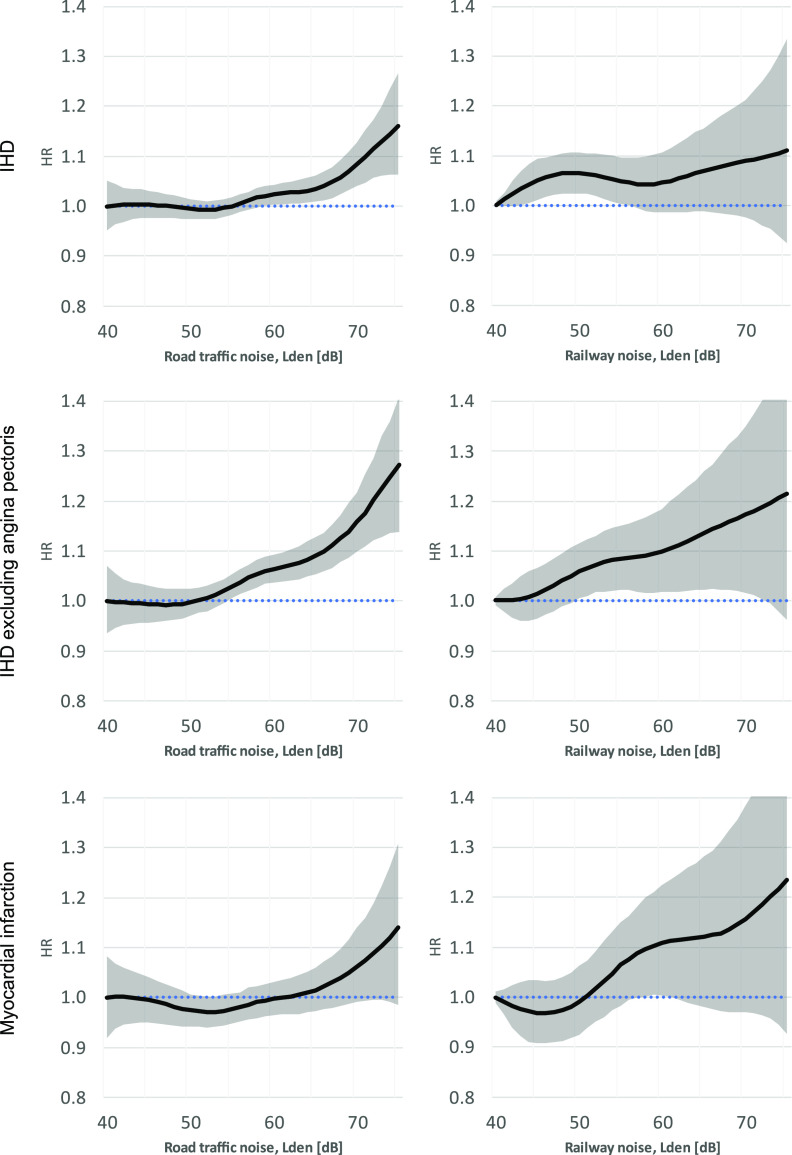
Analyses based on noise as a continuous variable using cubic splines indicated particularly strong exposure–response trends for both road traffic and railway noise in the subgroup IHD excluding angina pectoris (Figure 1). Departure from linearity was indicated for the exposure–response function regarding road traffic noise and IHD by a better fit of the cubic spline than the linear model ( and lower AIC) but not for the two subgroups. A threshold was suggested at 54 dB with a HR and 95% CI based on the main model of 1.05 (95% CI: 1.02, 1.08) per 10 dB for IHD at exposure above this level. Exposure–response relations were more uncertain for railway noise because fewer were exposed, particularly at higher levels. However, no apparent departure from linearity was suggested for any of the three outcome categories.
Figure 1.
HR and 95% CI for IHD, IHD excluding angina pectoris, and myocardial infarction in relation to road traffic and railway noise exposure during 5 y prior to the event in restricted cubic spline analyses of nine cohorts from Denmark and Sweden. All results are adjusted for age (by design), cohort (strata), sex (men/women), calendar year (in 5 y periods), educational level (low/medium/high), marital status (single/married), area-income (quartiles), and other noise sources indicator (yes/no: road, railway, and aircraft noise; for the three cohorts without aircraft noise information, all cohort members were assigned as no exposure). Note: Corresponding numeric data are available in the Supplementary Excel file “Numeric data for Figures EHP10745.” CI, confidence interval; HR, hazard ratio; IHD, ischemic heart disease; , day-evening night noise level based on energy equivalent noise level over a whole day with a penalty of 10 dB(A) for nighttime noise (23.00–7.00) and a penalty of 5 dB(A) for evening noise (i.e., 19.00–23.00).
Analyses of interactions focused on exposure to road traffic and railway noise in relation to HR of IHD excluding angina pectoris (Figure 2). For road traffic noise the strongest interaction was observed in relation to BMI, where those below had a higher HR than those with BMI above this level (p-value for interaction ). A BMI of is commonly used to define overweight and is close to the overall median in our study population (cf. Table 1). There was also an interaction with BMI for railway noise. No consistent interactions were noted between other covariates and road traffic or railway noise. In particular, those with exposure above or equal to the median had a higher HR for IHD excluding angina pectoris related to road traffic noise exposure, whereas those with exposure below this level had a higher HR associated with exposure to railway noise. Interactions for all IHD largely confirmed the results for IHD excluding angina pectoris (Figure S5).
Figure 2.
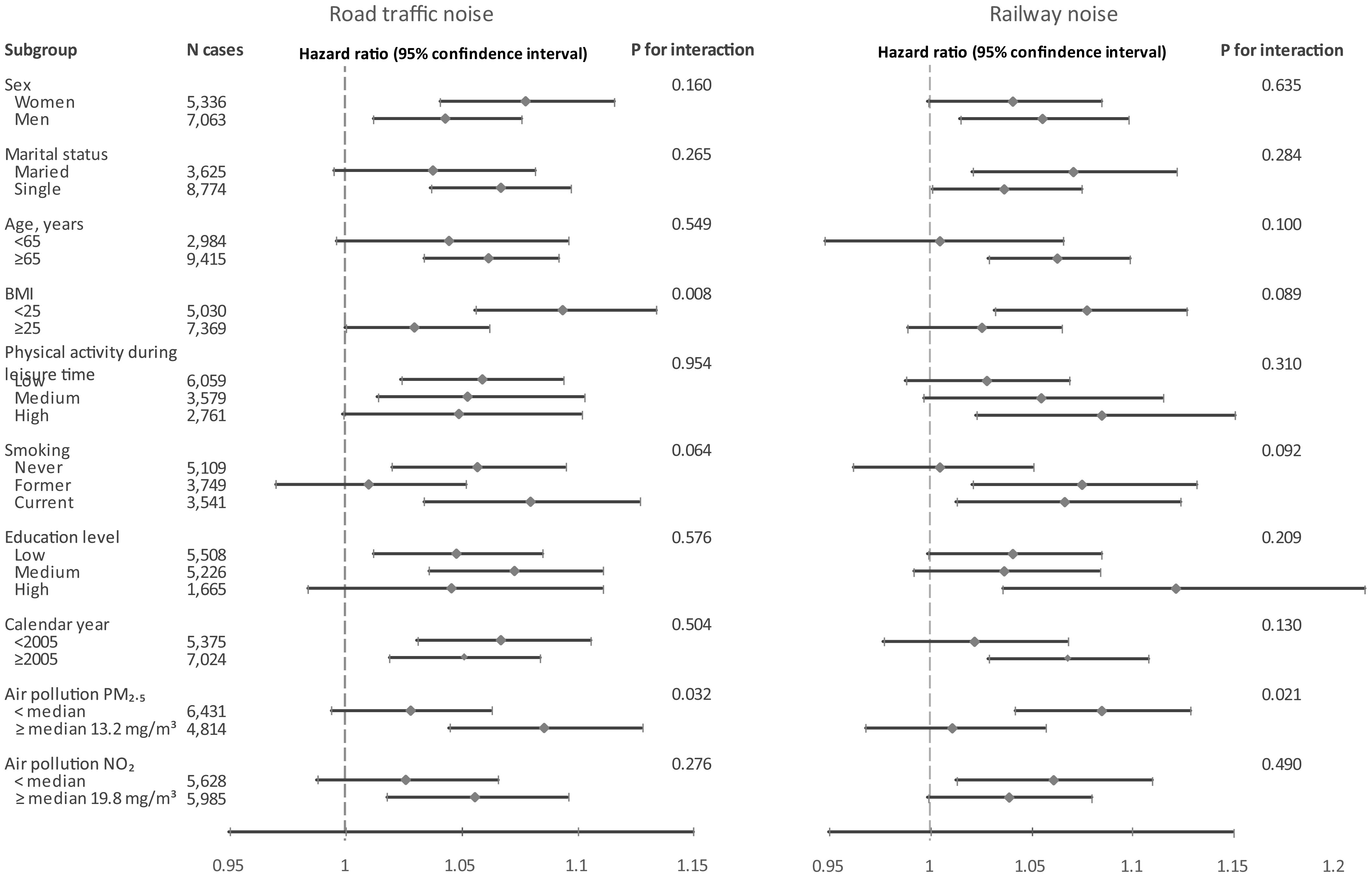
HR and 95% CI for ischemic heart disease excluding angina pectoris in relation to exposure to noise from road traffic (left) and railways (right) per 10 dB during 5 y prior to the event according to covariates and air pollution exposure. p-Values are Wald terms. Results are presented according to strata of potential effect modifiers based on separate models with interaction terms between transportation noise and each potential modifier, adjusted for age (by design), cohort (strata), sex (men/women), calendar year (in 5 y periods), educational level (low/medium/high), marital status (single/married), area-income (quartiles), and other noise sources indicator (yes/no: road, railway, and aircraft noise; for the three cohorts without aircraft noise information, all cohort members were assigned as no exposure). Note: Corresponding numeric data is available in the Supplementary Excel file “Numeric data for Figures EHP10745.” BMI, body mass index; CI, confidence interval; HR, hazard ratio; IHD, ischemic heart disease; , day-evening-night noise level based on energy equivalent noise level over a whole day with a penalty of 10 dB(A) for nighttime noise (23.00–7.00) and a penalty of 5 dB(A) for evening noise (i.e. 19.00–23.00); , nitrogen dioxide; , particulate matter with an aerodynamic diameter of (fine particulate matter).
Sensitivity analyses focusing on IHD excluding angina pectoris are presented in Figure S6. Further adjustment for covariates had limited effects on HRs for road traffic and railway noise, with the exception that adjustment for instead of tended to weaken the association for road traffic noise. Exposure to both road traffic and railway noise was related to an increased risk of fatal IHD excluding angina pectoris. We also calculated HRs for fatal IHD, which were 1.06 (95% CI: 1.01, 1.12) and 1.08 (95% CI: 1.02, 1.15) per 10 dB for road traffic and railway noise, respectively, as well as for fatal myocardial infarction with corresponding risk estimates of 1.02 (95% CI: 0.95, 1.09) and 1.08 (95% CI: 0.99, 1.17). In analyses sequentially leaving out one of the three larger cohorts, exclusion of the Danish DCH cohort tended to reduce the HR for road traffic noise, and exclusion of the Swedish MDC cohort had the same effect for railway noise (Figure S6). The influence was only marginal following exclusions of other cohorts.
Discussion
In this large study based on Danish and Swedish cohorts we observed increased risks of IHD associated with long-term exposure to road traffic and railway noise. Higher risks were indicated following exclusion of angina pectoris cases. Associations were also observed for aircraft noise but without clear exposure–response relations. Particularly strong associations appeared for both road traffic and railway noise among those with BMI below .
We found a HR for IHD of 1.03 (95% CI: 1.00, 1.05) per 10 dB of exposure to road traffic noise. A recent meta-analysis calculated an overall relative risk for IHD of 1.02 (95% CI: 1.00, 1.04) per 10 dB ,23 which is consistent with our estimate. The meta-analysis was based on 16 studies, including six of the cohorts in our study, but mostly with shorter follow-up and a mixture of outcomes (IHD/myocardial infarction). Our results suggest that exposure to road traffic noise below around 55 dB is not associated with an increased risk of IHD. This finding is somewhat different from results regarding stroke in the same study population, where no such “threshold” was observed.17 Our risk estimate of 1.05 (95% CI: 1.02, 1.08) for IHD per 10 dB at exposures above 54 dB appears comparable to the estimate of 1.08 (95% CI: 1.02, 1.15) based on a meta-analysis in the systematic review for the WHO Environmental Noise Guidelines, where the weighted lower exposure level across studies was 53 dB .3 One cohort (DCH) was included in both our analysis and the WHO meta-analysis; however, it contributed only 1,600 cases of myocardial infarction to the meta-analysis based on a shorter follow-up.24 Furthermore, two recent studies suggested thresholds in the exposure–response relation for road traffic noise and incidence of IHD8 or myocardial infarction.11 A threshold in the exposure–response relation could contribute to explaining the absence of association between road traffic noise and IHD in the cohorts from Stockholm in our study, where three out of four had comparatively low exposures, with few exposed over 60 dB . Assessment of exposure–response relationships is crucial for health impact assessments. In particular, the shape of the exposure–response function at low exposure levels is influential, where most of the population is exposed. There is a need for further studies assessing exposure–response relations at low but common levels of traffic noise exposure.
We observed an increased risk of IHD related to exposure to railway noise, particularly following exclusion of angina pectoris cases. Besides two studies on cohorts included in our analysis,7,9 only a pair of longitudinal studies strictly based on registry data analyzed risks of myocardial infarction25 or mortality of IHD and myocardial infarction6 in relation to railway noise exposure. The risk estimates in these studies were 1.023 (95% CI: 1.005, 1.042), 1.012 (95% CI: 1.005, 1.020) and 1.020 (95% CI: 1.007, 1.033), respectively, per 10 dB of exposure to railway noise. These estimates appear lower than the corresponding estimates in our study of 1.04 (95% CI: 0.99, 1.05) for incidence of myocardial infarction and 1.08 (95% CI: 1.02, 1.15) for fatal IHD and 1.08 (95% CI: 0.99, 1.17) for fatal myocardial infarction; however, the wide confidence intervals complicate a detailed quantitative comparison. Railway noise is a relatively rare exposure, which means that population-based epidemiological studies must be quite large to achieve a reasonable study power. Alternatively, studies may be conducted in areas where railway noise exposure is more common. For example, the cohort with the fewest participants in our study (SNAC-K), which had a considerably higher fraction of people exposed to railway noise than any of the other cohorts, showed an increased risk of IHD excluding angina pectoris related to railway noise exposure (Figure S3).
Our results indicated an association between aircraft noise and IHD, particularly when angina pectoris cases were excluded, but without an exposure–response relation. The clearest exposure–response trend was suggested in the SDPP cohort, with many subjects living near the major international airport in Stockholm, which also has nighttime traffic (Figure S4).26 There are few other studies on aircraft noise and IHD or myocardial infarction,6,23 including some of ecological design or strictly based on registry data. Although some of the studies showed increased risks related to aircraft noise exposure, no consistent picture emerged. A recent study suggests that short-term aircraft noise exposure may be of importance for the cardiovascular risks.27 Population studies on aircraft noise exposure are complicated by the fact that houses are more often noise insulated in the most heavily exposed areas near the airports. Such insulation may have affected the exposure–response relation in our study, but we lacked information on noise insulation of individual dwellings.
Knowing whether subtypes of IHD are differentially related to transportation noise exposure is important for the risk assessment and understanding of etiological mechanisms. We found consistent associations between road traffic noise exposure and IHD for different adjustment models in the pooled analyses, particularly when those with the diagnosis based on angina pectoris were excluded. It is compelling that the stronger association for IHD without angina pectoris was confirmed also for railway and aircraft noise, although exposure to the three noise sources showed low correlation. Furthermore, the risks of fatal IHD, which is generally not based on angina pectoris, appeared higher than those for incident IHD, where angina pectoris is more prominent. Angina pectoris constituted a larger part of IHD in the Danish studies, partly because outpatient data were included already from 1995 in the Danish National Patient Register but only from 2001 in the Swedish National Patient Register. We found no association between road or railway noise exposure and angina pectoris, which is less well captured in the national registries than other IHD diagnoses,28 but a particularly strong association between road traffic noise and chronic IHD. Traffic noise exposure has been linked to several cardiovascular outcomes, such as IHD/myocardial infarction, stroke, heart failure, and atrial fibrillation,18 but we are not aware of earlier studies on risks for angina pectoris or chronic IHD.
We observed an interaction in relation to IHD risk between road traffic noise and BMI, with a stronger association among study participants having a BMI below , which was similar for railway noise. No comparable interaction between road traffic noise exposure and BMI in relation to stroke was noted in the same study base.17 Several cohort studies have found an association between traffic noise exposure and obesity markers.26,29–32 This finding opens the possibility that BMI or other obesity markers may be mediators of the association between traffic noise and IHD; however, our results suggest that there are causal pathways not involving BMI. It is not clear why excess risks related to traffic noise exposure would be higher among those with lower BMI, but it may be speculated that other risk factors could be more influential for subjects with higher BMI. A similar absolute risk increase related to noise exposure in both BMI categories would also tend to generate a lower rate ratio among those with high BMI because of the higher IHD incidence in this group. We are not aware of other studies on noise exposure and IHD assessing interactions with BMI, and our results should be interpreted with caution in view of the exploratory nature of these analyses.
Our results did not point to effect modification by other covariates, which was consistent between road traffic and railway noise exposure. In particular, those with exposure above or equal to the median had a higher risk of IHD and of IHD excluding angina pectoris related to road traffic noise, whereas those with exposure below this level had a higher risk associated with exposure to railway noise. The reasons behind this apparent inconsistency are unclear, but one contributing factor is the low levels in the Stockholm cohorts, where the association between road traffic noise and IHD risk was weak. On the other hand, the association between railway noise and IHD was weak in the Danish cohorts, particularly for IHD excluding angina pectoris, where the levels were higher. Several studies on cardiovascular disease have estimated exposure to both road traffic noise and air pollution;4,6–11,13–17 however, no clear picture of interaction has emerged for IHD or myocardial infarction or for other cardiovascular end points.
Our study has several strengths. It is the largest study to date on transportation noise and IHD containing detailed information on socioeconomic and lifestyle risk factors, enabling a high statistical power and careful confounding control also in subgroup analyses. The study constitutes a major extension of earlier publications based on the cohorts, including longer follow-up and substantially increased number of cases, which together with pooled analyses, enables detailed evaluation of the shape of exposure–response functions and interactions, also for subtypes of IHD. We estimated transportation noise and air pollutant levels at residential addresses over time, using validated methods with very high spatial resolution. The study included the five major metropolitan areas in Denmark and Sweden, as well as less urbanized regions, contributing to a substantial contrast in traffic noise exposure. However, the exposure assessment still has uncertainties because only residential addresses were considered and no information was available on indoor noise levels, which depend on façade sound insulation of the building as well as to what extent windows are open or closed. Furthermore, the results may have been influenced by calendar year because exposure was assessed during a period of more than five decades, with differences between cohorts, and changes in noise exposure patterns occurred during that period. The generalizability of our findings may be affected by different building techniques, regulations for noise insulation, and behavioral characteristics in Scandinavian countries and in other countries.33 The health outcome information was obtained from high quality national patient and mortality registers; however, some diagnoses are less well captured in such registers, including angina pectoris.27 Residual confounding must also be considered in the interpretation, particularly because positive confounding was often indicated when adjusting for covariates, such as air pollution. Including data from several cohorts and countries in the analyses has advantages; however, interpretation of results from combined analyses may be complex if cohorts differ substantially in exposures, background risks of IHD, and distribution of covariates. Our results suggest that differences in risk estimates between cohorts to some extent were related to noise exposure distributions, but specifics in the exposure assessment methodologies may also have contributed.
In conclusion, our results showed that long-term exposure to road traffic noise and railway noise was associated with an increased incidence of IHD, especially for those with a diagnosis not based on angina pectoris. A threshold of around 55 dB was suggested in the exposure–response relation for road traffic noise and IHD. Excess risks related to aircraft noise were also observed but without clear exposure–response relations. Our findings underscore the importance of transportation noise as a public health problem and highlight several aspects that can contribute to the understanding of causal pathways and influence the population attributable risks of IHD related to traffic noise exposure.
Supplementary Material
Acknowledgments
This work was supported by NordForsk [Grant No. 83597]. Funding for the included cohorts is shown in Table S1.
References
- 1.European Environment Agency. Environmental Noise in Europe—2020. EEA Report No 22. 2020. https://anima-project.eu/fileadmin/user_upload/Eulalia_Peris_%E2%80%93ANIMA_Noise_In_Europe_Report.pdf [accessed 5 October 2021].
- 2.World Health Organization. Environmental Noise Guidelines for the European Region. 2018. Copenhagen, Denmark: WHO Regional Office for Europe. https://apps.who.int/iris/bitstream/handle/10665/279952/9789289053563-eng.pdf [accessed 5 October 2021]. [Google Scholar]
- 3.van Kempen E, Casas M, Pershagen G, Foraster M. 2018. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health 15(2):379, PMID: , 10.3390/ijerph15020379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bodin T, Björk J, Mattisson K, Bottai M, Rittner R, Gustavsson P, et al. 2016. Road traffic noise, air pollution and myocardial infarction: a prospective cohort study. Int Arch Occup Environ Health 89(5):793–802, PMID: , 10.1007/s00420-016-1115-9. [DOI] [PubMed] [Google Scholar]
- 5.Dimakopoulou K, Koutentakis K, Papageorgiou I, Kasdagli M-I, Haralabidis AS, Sourtzi P, et al. 2017. Is aircraft noise exposure associated with cardiovascular disease and hypertension? Results from a cohort study in Athens, Greece. Occup Environ Med 74(11):830–837, PMID: , 10.1136/oemed-2016-104180. [DOI] [PubMed] [Google Scholar]
- 6.Héritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, Thiesse L, et al. 2018. Diurnal variability of transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Int J Hyg Environ Health 221(3):556–563, PMID: , 10.1016/j.ijheh.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Pyko A, Andersson N, Eriksson C, de Faire U, Lind T, Mitkovskaya N, et al. 2019. Long-term transportation noise exposure and incidence of ischaemic heart disease and stroke: a cohort study. Occup Environ Med 76(4):201–207, PMID: , 10.1136/oemed-2018-105333. [DOI] [PubMed] [Google Scholar]
- 8.Andersson EM, Ögren M, Molnár P, Segersson D, Rosengren A, Stockfelt L. 2020. Road traffic noise, air pollution and cardiovascular events in a Swedish cohort. Environ Res 185:109446, PMID: , 10.1016/j.envres.2020.109446. [DOI] [PubMed] [Google Scholar]
- 9.Roswall N, Raaschou-Nielsen O, Ketzel M, Gammelmark A, Overvad K, Olsen A, et al. 2017. Long-term residential road traffic noise and NO2 exposure in relation to risk of incident myocardial infarction–A Danish cohort study. Environ Res 156:80–86, PMID: , 10.1016/j.envres.2017.03.019. [DOI] [PubMed] [Google Scholar]
- 10.Thacher JD, Hvidtfeldt UA, Poulsen AH, Raaschou-Nielsen O, Ketzel M, Brandt J, et al. 2020. Long-term residential road traffic noise and mortality in a Danish cohort. Environ Res 187:109633, PMID: , 10.1016/j.envres.2020.109633. [DOI] [PubMed] [Google Scholar]
- 11.Lim Y-H, Jørgensen JT, So R, Cramer J, Amini H, Mehta A, et al. 2021. Long-term exposure to road traffic noise and incident myocardial infarction: a Danish nurse cohort study. Environ Epidemiol 5(3):e148, PMID: , 10.1097/EE9.0000000000000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Münzel T, Sørensen M, Gori T, Schmidt FP, Rao X, Brook J, et al. 2017. Environmental stressors and cardio-metabolic disease: part I-epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. Eur Heart J 38(8):550–556, PMID: , 10.1093/eurheartj/ehw269. [DOI] [PubMed] [Google Scholar]
- 13.Beelen R, Hoek G, Houthuijs D, van den Brandt PA, Goldbohm RA, Fischer P, et al. 2009. The joint association of air pollution and noise from road traffic with cardiovascular mortality in a cohort study. Occup Environ Med 66(4):243–250, PMID: , 10.1136/oem.2008.042358. [DOI] [PubMed] [Google Scholar]
- 14.Selander J, Nilsson ME, Bluhm G, Rosenlund M, Lindqvist M, Nise G, et al. 2009. Long-term exposure to road traffic noise and myocardial infarction. Epidemiology 20(2):272–279, PMID: , 10.1097/EDE.0b013e31819463bd. [DOI] [PubMed] [Google Scholar]
- 15.Sørensen M, Lühdorf P, Ketzel M, Andersen ZJ, Tjønneland A, Overvad K, et al. 2014. Combined effects of road traffic noise and ambient air pollution in relation to risk for stroke? Environ Res 133:49–55, PMID: , 10.1016/j.envres.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Sørensen M, Wendelboe Nielsen O, Sajadieh A, Ketzel M, Tjønneland A, Overvad K, et al. 2017. Long-term exposure to road traffic noise and nitrogen dioxide and risk of heart failure: a cohort study. Environ Health Perspect 125(9):097021, PMID: , 10.1289/EHP1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roswall N, Pyko A, Ögren M, Oudin A, Rosengren A, Lager A, et al. 2021. Long-term exposure to transportation noise and risk of incident stroke: a pooled study of nine Scandinavian cohorts. Environ Health Perspect 129(10):107002, PMID: , 10.1289/EHP8949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Münzel T, Sørensen M, Daiber A. 2021. Transportation noise pollution and cardiovascular disease. Nat Rev Cardiol 18(9):619–636, PMID: , 10.1038/s41569-021-00532-5. [DOI] [PubMed] [Google Scholar]
- 19.Korek MJ, Bellander TD, Lind T, Bottai M, Eneroth KM, Caracciolo B, et al. 2015. Traffic-related air pollution exposure and incidence of stroke in four cohorts from Stockholm. J Expo Sci Environ Epidemiol 25(5):517–523, PMID: , 10.1038/jes.2015.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bendtsen H. 1999. The Nordic prediction method for road traffic noise. Sci Total Environ 235(1–3):331–338, 10.1016/S0048-9697(99)00216-8. [DOI] [Google Scholar]
- 21.de Hoogh K, Chen J, Gulliver J, Hoffmann B, Hertel O, Ketzel M, et al. 2018. Spatial PM2.5, NO2, O3 and BC models for Western Europe – evaluation of spatiotemporal stability. Environ Int 120:81–92, PMID: , 10.1016/j.envint.2018.07.036. [DOI] [PubMed] [Google Scholar]
- 22.Roswall N, Christensen JS, Bidstrup PE, Raaschou-Nielsen O, Jensen SS, Tjønneland A, et al. 2018. Associations between residential traffic noise exposure and smoking habits and alcohol consumption-A population-based study. Environ Pollut 236:983–991, PMID: , 10.1016/j.envpol.2017.10.093. [DOI] [PubMed] [Google Scholar]
- 23.Vienneau D, Eze IC, Probst-Hensch N, Rȍȍsli M. Association between transportation noise and cardio-metabolic diseases: an update of the WHO meta-analysis. Proceedings of the 23rd International Congress on Acoustics. Aachen, Germany. 9–13 September 2019. https://edoc.unibas.ch/70857/1/ICA_2019_manuscript%20Vienneau%20final.pdf [accessed 29 November 2021]. [Google Scholar]
- 24.Sørensen M, Andersen ZJ, Nordsborg RB, Jensen SS, Lillelund KG, Beelen R, et al. 2012. Road traffic noise and incident myocardial infarction: a prospective cohort study. PLoS One 7(6):e39283, PMID: , 10.1371/journal.pone.0039283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seidler A, Wagner M, Schubert M, Dröge P, Pons-Kühnemann J, Swart E, et al. 2016. Myocardial infarction risk due to aircraft, road, and rail traffic noise. Dtsch Arztebl Int 113(24):407–414, PMID: , 10.3238/arztebl.2016.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eriksson C, Hilding A, Pyko A, Bluhm G, Pershagen G, Östenson C-G. 2014. Long-term aircraft noise exposure and body mass index, waist circumference, and type 2 diabetes: a prospective study. Environ Health Perspect 122(7):687–694, PMID: , 10.1289/ehp.1307115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saucy A, Schäffer B, Tangermann L, Vienneau D, Wunderli JM, Röösli M. 2021. Does night-time aircraft noise trigger mortality? A case-crossover study on 24 886 cardiovascular deaths. Eur Heart J 42(8):835–843, PMID: , 10.1093/eurheartj/ehaa957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim J-L, Reuterwall C, et al. 2011. External review and validation of the swedish national inpatient register. BMC Public Health 11(1):450, PMID: , 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Christensen JS, Raaschou-Nielsen O, Tjønneland A, Nordsborg RB, Jensen SS, Sørensen TIA, et al. 2015. Long-term exposure to residential traffic noise and changes in body weight and waist circumference: a cohort study. Environ Res 143(Part A):154–161, PMID: , 10.1016/j.envres.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 30.Pyko A, Eriksson C, Lind T, Mitkovskaya N, Wallas A, Ögren M, et al. 2017. Long-term exposure to transportation noise in relation to development of obesity—a cohort study. Environ Health Perspect 125(11):117005, PMID: , 10.1289/EHP1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Foraster M, Eze IC, Vienneau D, Schaffner E, Jeong A, Héritier H, et al. 2018. Long-term exposure to transportation noise and its association with adiposity markers and development of obesity. Environ Int 121(Part 1):879–889, PMID: , 10.1016/j.envint.2018.09.057. [DOI] [PubMed] [Google Scholar]
- 32.Cai Y, Zijlema WL, Sørgjerd EP, Doiron D, de Hoogh K, Hodgson S, et al. 2020. Impact of road traffic noise on obesity measures: observational study of three European cohorts. Environ Res 191:110013, PMID: , 10.1016/j.envres.2020.110013. [DOI] [PubMed] [Google Scholar]
- 33.Rasmussen B. Building acoustic regulations in Europe–brief history and actual situation. In: Baltic-Nordic Acoustics Meeting 2018. 15–18 April 2018. Rekjavik, Iceland. Nordic Acoustic Association. https://events.artegis.com/urlhost/artegis/customers/1571/.lwtemplates/layout/default/events_public/12612/Papers/Keynote_Rasmussen_BNAM2018.pdf [accessed 5 October 2021].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.