Abstract
Both animal models and human observational and genetic studies have shown that immune and inflammatory mechanisms play a key role in hypertension and its complications. We review the effects of immunomodulatory interventions on blood pressure, target organ damage, and cardiovascular risk in humans. In experimental and small clinical studies, both non-specific immunomodulatory approaches, such as mycophenolate mofetil and methotrexate, and medications targeting T and B lymphocytes, such as tacrolimus, cyclosporine, everolimus, and rituximab, lower blood pressure and reduce organ damage. Mechanistically targeted immune interventions include isolevuglandin scavengers to prevent neo-antigen formation, co-stimulation blockade (abatacept, belatacept), and anti-cytokine therapies (e.g. secukinumab, tocilizumab, canakinumab, TNF-α inhibitors). In many studies, trial designs have been complicated by a lack of blood pressure-related endpoints, inclusion of largely normotensive study populations, polypharmacy, and established comorbidities. Among a wide range of interventions reviewed, TNF-α inhibitors have provided the most robust evidence of blood pressure lowering. Treatment of periodontitis also appears to deliver non-pharmacological anti-hypertensive effects. Evidence of immunomodulatory drugs influencing hypertension-mediated organ damage are also discussed. The reviewed animal models, observational studies, and trial data in humans, support the therapeutic potential of immune-targeted therapies in blood pressure lowering and in hypertension-mediated organ damage. Targeted studies are now needed to address their effects on blood pressure in hypertensive individuals.
Keywords: Hypertension, Inflammation, Immune system, Immunomodulatory, Blood pressure
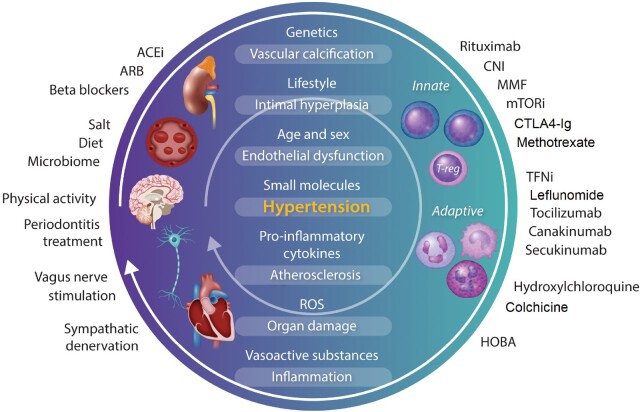
Graphical Abstract
1. Introduction
In atherosclerosis, the role of inflammation is well defined,1–5 and a co-existing chronic inflammatory condition such as rheumatoid arthritis (RA), inflammatory bowel disease, ankylosing spondylitis, or psoriasis is considered an additional risk factor, including in ESC Cardiovascular Disease Prevention guidelines.6–8 Anti-inflammatory therapies are recommended in such patients,6 and targeting inflammation to improve cardiovascular outcomes has been supported by recent clinical trials such as CANTOS, COLCOT, and LoDoCo2.9–12 Hypertension is the most common cardiovascular risk factor worldwide.13 For more than half a century, immune cells have been observed to infiltrate the kidney and vasculature of hypertensive humans and animals with experimental hypertension, and increasing evidence indicates that immune and inflammatory mechanisms promote this disease. It is therefore essential to identify the clinically permissible therapeutic interventions that address inflammatory targets in hypertension, and patient populations that would benefit from such treatment. While basic and translational evidence suggests that interfering in immune-inflammatory processes may aid in control of blood pressure (BP) and prevention of target organ damage,14–17 the clinical evidence for these interventions has not been systematically analysed. Accordingly, we review potential immune therapeutic targets to identify approaches for which well-designed clinical studies may prove fruitful.
2. Immune and inflammatory targets for treatment of hypertension
Inflammation and immune activation were first implicated as being involved in hypertension through the work of Grollman, Okuda, Svendsen,18–21 and Olsen.22,23 In the last decade, new research has begun to reveal the mechanisms that explain this.17 Using animal models of genetic and pharmacological targeting, the regulatory role of T cells,24–34 γδ cells,35 monocytes/macrophages,36–39 dendritic cells (DC),40 B cells,41,42 NK cells,43 as well as other components of a complex immuno-inflammatory network have been assessed.17,44–48 The initiation of inflammation in hypertension appears to be associated with oxidative stress and redox-dependent mechanisms within the vascular and renal tissues.49,50 These lead to generation of neo-antigens,51 damage-associated molecular patterns,52 and neuroimmune mechanisms53,54 that trigger maladaptive immune responses, which compound hypertension and its' associated organ damage. Although antigen(s) responsible for activation of adaptive immunity have not been definitively identified, potential candidates are isolevuglandin (isoLG) adducted proteins. IsoLGs are oxidation products of arachidonic acid that rapidly ligate lysines on self-proteins and accumulate in antigen-presenting cells and are presented within major histocompatibility complexes. These activate a subset of CD4+ and CD8+ T cells. Importantly, the selective isoLG scavenger 2-hydroxybenzylamine can prevent immune activation and lower BP in several animal models of hypertension.51 Data from both animal and human studies also identify HSP70 as a potential auto-antigen.55 Numerous animal studies in a wide range of models, reviewed previously,56–58 highlight that immunomodulating inflammatory activation and effector cytokine release may curb BP increases and lessen development of vascular, cardiac, and renal damage.59–66 Many of these studies have employed germline knockout animals. In addition, small molecule or neutralizing antibodies that target immune mediators have been used to determine the effect of selective blockade on experimental hypertension (Table 1). These have targeted both the innate (e.g. IL-1, TLR4) and adaptive (e.g. IL-17, CD80/86) immune system. Careful analysis of these studies helps identify potential therapeutic targets, but also highlights the impact of treatment protocol and animal model selection for BP and target organ damage outcomes (Table 1 and Figure 1).
Table 1.
Key findings relevant to the relationship between the immune system and hypertension arising from animal models
| Immune target and therapeutic agent | Model | Result relative to non-treated mice | References |
|---|---|---|---|
|
TNF-α
|
SHR rat |
|
Filho et al.67 |
| Etanercept (TNF-inhibitor) | Rat (8% NaCl diet + 14 days ang-II) |
|
Elmarakby et al.68 |
| Etanercept | Mice infused with ang-II for 14 days | ↓ BP | Guzik et al.25 |
| Etanercept | Spontaneously hypertensive dTGR rats |
|
Muller et al.69 |
| Etanercept | Dahl salt-sensitive rat with renal interstitial administration of etanercept |
|
Huang et al.49 |
| Etanercept | High fructose-fed rats |
|
Tran et al.70 |
| Etanercept | Mouse model of SLE |
|
Venegas-Pont et al.71 |
| PEG-sTNFR1 (TNF inhibitor) | Renal mass reduction induced renal failure in rats |
|
Therrien et al.72 |
|
Uni-nephrectomized wild-type mice treated with DOCA-salt up to 28 days |
|
Krishnan et al.73 |
|
SHR rats |
|
Rodríguez-Iturbe et al.44 |
| PDTC | 2K1C rats |
|
Cau et al.74 |
|
Mice treated with ang-II for 21 days |
|
Zhang et al.75 |
| Anakinra | Uni-nephrectomized mice treated with DOCA-salt in drinking water for 21 days |
|
Ling et al.76 |
|
Dahl salt-sensitive rats fed 4% NaCl for up to 11 days |
|
Hashmat et al.77 |
|
Mouse model of SLE |
|
Mathis et al.78 |
|
Mice treated with ang-II for 14 days |
|
Ma et al.79 |
|
Mice treated with ang-II for 7 or 14 days |
|
Caillon et al.35 |
|
Mice treated with ang-II for 14 days |
|
Majeed et al.80 |
| IL-2/Anti-IL-2 Ab complex | Transverse aortic constriction (TAC) in mice |
|
Wang et al.81 |
|
Wild-type mice treated with ang-II for 14 days | ↔ BP | Guzik et al.25 |
| Neutralizing anti-IFN-γ Ab | Mice with T-cell restricted overexpression of mineralocorticoid receptor (TMROV mice) treated with ang-II for 21 days | ↓ BP | Sun et al.82 |
|
Wild-type mice treated with ang-II for 14 days | ↔ BP and cardiac hypertrophy | Markó et al.83 |
| Neutralizing anti-IL-17A Ab | Rats treated with anti-IL-17A Ab for 28 days using the DOCA-salt model |
|
Amador et al.84 |
| Neutralizing anti-IL-17A Ab | Calcineurin-inhibitor treated mice |
|
Chiasson et al.85 |
| Neutralizing anti-IL-17A, IL-17F or Il-17RA | Wild-type mice treated for 28 days with ang-II (14 days with Ab treatment) |
|
Saleh et al.86 |
| IL-17 soluble receptor C | Preeclampsia rat model |
|
Cornelius et al.87 |
|
Wild-type mice treated with ang-II for 14 days | ↔ BP and cardiac hypertrophy | Marko et al.83 |
|
Dahl salt-sensitive rat fed 4% NaCl for 21-28 days |
|
Murphy et al.88 |
|
Wild-type mice treated with ang-II for 28 days | ↓ BP | Chan et al.41 |
|
Wild-type mice were uni-nephrectomized and treated with DOCA-salt for 21 days |
|
Chan et al.89 |
| INCB3344 | Wild-type mice treated with ang-II for 28 days (21 days with CCR2 antagonist) |
|
Moore et al.37 |
|
Wild-type mice infused with ang-II for 14 days. |
|
Mikolajczyk et al.90 |
|
Rats infused with Aldo-salt for 28 days |
|
De Batista et al.91 |
| Neutralizing anti‐TLR4 Ab | Wild-type mice treated with ang-II for 14 days |
|
Hernanz et al.92 |
| Neutralizing anti‐TLR4 Ab | SHR rat |
|
Bomfin et al.93 |
| Neutralizing anti‐TLR4 Ab | Mice treated for 28 days with ang-II (14 days with Ab treatment) |
|
Nunes et al.94 |
| Neutralizing anti‐TLR4 Ab | SHR rat |
|
Echem et al.95 |
|
SHR rat |
|
McCarthy et al.96 |
|
Wild-type mice infused with ang-II for 14 days, or uni-nephrectomized and treated with DOCA-salt for 21 days |
|
Vinh et al.24 |
|
Preeclampsia rat model |
|
Cornelius et al.97 |
|
Wild-type mice were infused with ang-II for 14 |
|
Kirabo et al.51 |
|
Dahl salt-sensitive rats fed a 4% NaCl diet for up to 21 days |
|
Kumar et al.98 |
|
SHR Rat |
|
Rodríguez-Iturbe et al.99 |
| MMF | Uni-nephrectomized rats implanted with DOCA-salt pellets + 0.9% NaCl drinking water for up to 21 days. |
|
Boesen et al.100 |
| MMF | Mouse model of SLE |
|
Taylor and Ryan101 |
|
DOCA-salt in pregnant rats |
|
Tinsley et al.102 |
Ab, antibody; ang-II, angiotensin II; BP, blood pressure; CCR, CC motif chemokine receptor; CD, cluster of differentiation; CNI, calcineurin inhibitor; CTLA4-Ig, cytotoxic T-lymphocyte-associated protein 4 immunoglobulin; DOCA, deoxycorticosterone acetate; dTGR, double transgenic rats; IL, interleukin; IFN-γ, interferon γ; ΙMPDH, Inosine-5′-monophosphate dehydrogenase; mTOR: mammalian target of rapamycin; MTX: methotrexate; NF-κb, nuclear factor kappa b; NLRP3, NOD-like receptor family pyrin domain containing 3; PDTC; pyrrolidine dithiocarbamate; SHR, spontaneously hypertensive rat; SLE, systemic lupus erythematosus; TGF-β, transforming growth factor beta; TLR, Toll-like receptor; TNF, tumour necrosis factor.
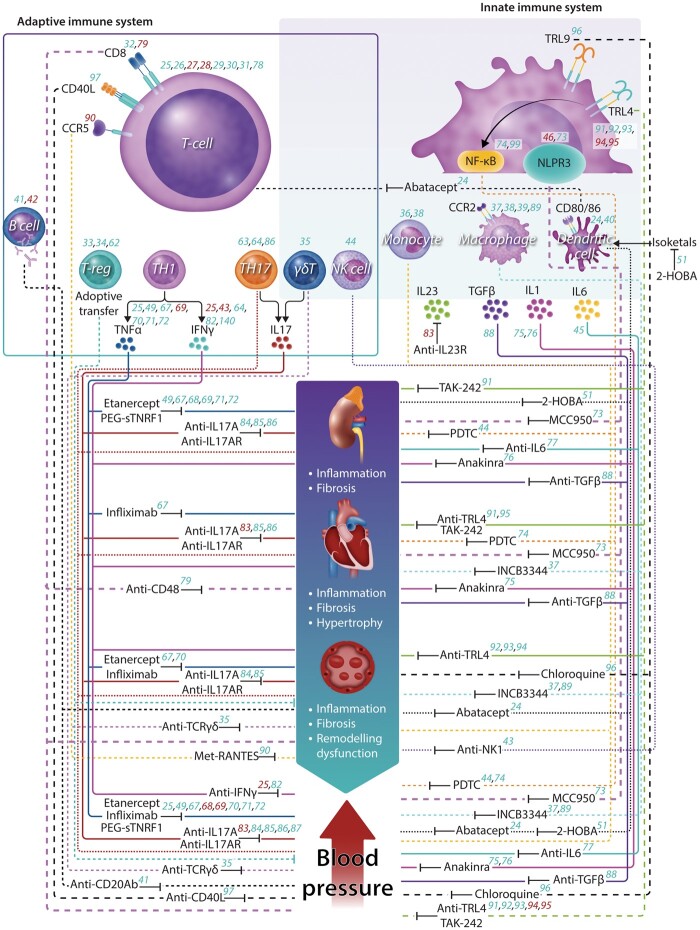
Figure 1.
Role of the immune system in the pathogenesis of experimental hypertension and potential immunomodulators for the treatment of hypertension and cardiovascular organ damage. Animal studies implicate virtually all immune cell subsets (dash lines) and cytokines (solid lines) in the pathogenesis of hypertension and target organ damage. Initially, classical immunosuppressants such as mycophenolate59,60 or rapamycin58 showed improvement in renal damage and blood pressure regulation, by non-specific mechanisms. The introduction of cell/cytokine-specific immunomodulators (small-molecule inhibitors, antibodies, antagonists or scavengers) with beneficial effect in hypertension and hypertension-mediated organ damage, emphasize the potential use of immunomodulators as a pharmacological tool. More details about the inhibitors are presented in Table1. Numbers indicate references represent a positive (green) or negative (red) effect. Legend: CD, cluster of differentiation; CCR, chemokine receptor; Treg, T-regulatory cell; TH, T-helper cell; IL, interleukin; TNF-α, tumour necrosis factor alfa; NF-κB, Nuclear factor kappa B; IFN-γ, interferon γ; NLPR3, NOD-like receptor family, pyrin domain-containing protein 3; TGF-β, transforming growth factor beta; TLR, Toll-like receptor; PEG-sTNFR1, PEGylated soluble tumour necrosis factor receptor 1; TAK-242, inhibitor of TLR4 signalling; 2-HOBA, 2-hydroxybenzylamine; MCC950, small-molecule inhibitor of the NLRP3 pathway; INCB3344, CCR2 antagonist; Met-RANTES, CCR5 antagonist.
3. Clinical evidence
Epidemiological and observational human data supports a relationship between the immune system and hypertension, including the observation that humans with hypertension are at increased risk of COVID-19 infection-related death.103,104 Inflammatory biomarkers105–107 correlate with systolic BP (SBP) in acute stroke, each 10 mmHg BP elevation increasing the odds of an elevated C-reactive protein level by 72%.108 Similarly, observational and clinical trial data demonstrate BP increases with each C-reactive protein quartile.109,110 A nested case–control study of 400 normotensive women indicated that the risk of developing hypertension during follow-up increases with higher quartiles of IL-6 and C-reactive protein.111 In addition to C-reactive protein and IL-6, TNF-α, IL-1β, IL-18, and CCL2 cytokine levels also appear to be increased in hypertension and may confer risk of developing the disease.112–118 These cytokines likely promote cell infiltration, affect renal sodium transport,75 and alter vascular function and structure, ultimately leading to sodium and volume retention, increased systemic vascular resistance, and the phenotype of hypertension.
Circulating leucocytes, which are important cellular components of the immune system, show significant perturbations in hypertension. Data from NHANES III demonstrate higher numbers of circulating leucocytes are associated with hypertension.107 UK Biobank data similarly indicate that quintile distribution of lymphocyte, monocyte, neutrophil, and eosinophil count is positively associated with BP.119 Other studies show that an increased neutrophil to lymphocyte ratio (NLR) predicts development of hypertension.120–122 Intermediate and non-classical monocytes are associated with inflammatory states and endothelial dysfunction and are also increased in hypertensive patients.123–125 A recent study has shown that signals from the activated endothelium in hypertension induces conversion of classical CD14++/CD16low monocytes to CD14++CD16+ intermediate monocytes. This seems to be mediated by STAT3 activation and associated with increases in IL-6, IL-1β, IL-23, CCL4, and TNF-α.123 Monocytes from hypertensive patients also express higher TLR4, and BP control reverses this.126
A causal role of lymphocytes in human hypertension is supported by large-scale Mendelian randomization genetic evidence.119 T lymphocytes of hypertensive individuals are activated, with increased IL-17A and interferon γ (IFN-γ) production and proportionally higher memory T cells (CD45RO+) in adults.127 Youn et al.128 have shown that patients with hypertension have an increased fraction of immunosenescent, proinflammatory, cytotoxic CD8+ T cells. Even among hypertensive adolescents, a subset of pro-inflammatory CD4+ T cells is associated with SBP and arterial stiffness.129 Increased circulating effector memory CD4+/CD8+ T cells and CD8+CD28 null T cells are also present at this early time point in hypertension.129,130
In summary, clinical studies identify greater proportions of activated pro-inflammatory monocytes and lymphocytes in hypertension. This may promote their infiltration into target organs, leading to perturbations in vascular and renal function, and ultimately modulating BP.
4. Genetic and multi-omics evidence
Data from Genome-Wide Association Studies (GWAS) and the transcriptome link hypertension with immune cellular defence and inflammatory responses.130,131 This link is supported by integrative network analysis132 and Mendelian randomization approaches,119 and is important, considering that heritability of BP is between 33% and 57%.133–135
Several GWAS have implicated SH2B3/LNK gene in hypertension and myocardial infarction.130,132,136,137 SH2B3 encodes a docking protein that seems to be a modulator of T cell activation. Variants of this gene are linked to autoimmune diseases such as multiple sclerosis, coeliac disease, and type 1 diabetes.137 Single nucleotide polymorphism (SNP) rs3184504 in SH2B3 is evidential or its' trans-regulatory role in gene expression; regulating 6 out of the 34 BP-related signature genes identified by meta-analysis of GWAS reporting gene expression profiles from 7017 individuals not on anti-hypertensive treatment. All regulated genes are expressed in leucocytes.138 Integrative network analysis of BP GWAS with mRNA expression profiles from 3679 participants not on anti-hypertensive agents confirms molecular interactions between key drivers such as SH2B3 and hypertension-related genes.132 Mechanistically, T cells from LNK knockout mice produce high levels of type I cytokines and these mice exhibit increased sensitivity to angiotensin II (Ang II), leading to hypertension, endothelial and renal dysfunction, increased inflammatory cell infiltrate, and oxidative stress.139,140 Mendelian randomization evidence based on 120 SNPs predictive of leucocyte subpopulations demonstrates a clear, potentially causal, relationship between lymphocyte count and systolic and diastolic BP, while BP itself appears to affect monocyte and neutrophil counts.119 Finally, the recent multi-omic kidney analysis uncovered many immunity-related genes (such as IRF5, IRAK1, BP1, TRAF1) whose expression, splicing, and/or methylation ostensibly demonstrate causal relationships with BP.141
5. Effects of immunomodulatory drugs on BP
Clinically available immunomodulatory drugs employ heterogeneous mechanisms of action, and hence their impact on BP regulatory systems is likely to be diverse. Agents reviewed below are selected to illustrate this breadth.
5.1 Selected anti-cytokine therapies
5.1.1 TNF-α inhibitors
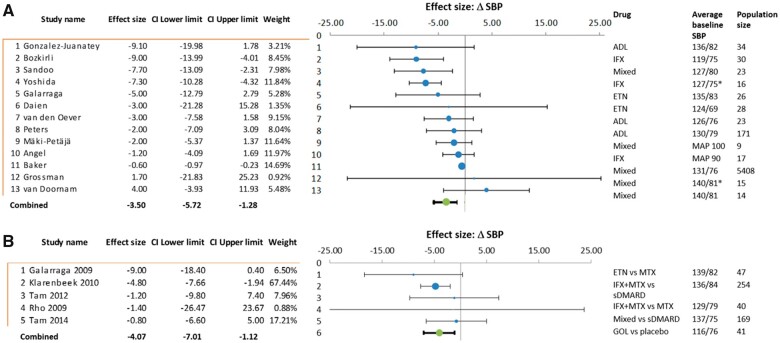
Using a systematized search, we identified 20 studies reporting BP in patients prescribed adalimumab, infliximab, etanercept, golimumab, and six papers with a mix of TNF-α inhibitors used (see Table 2). Study populations included those with RA, ankylosing spondylitis, psoriasis, and combined rheumatological diseases. Follow-up was from 2 weeks to 12 months and cohort sizes varied from 9 to 5408. Only 5 of the 20 studies were randomized and/or placebo controlled.148,149,156,159 Seventeen of these studies contained data adequate for meta-analysis (see Supplementary material online, methods and Figure 2): the combined estimate from 13 studies comparing average BP before and after TNF-α blockade was a 3.5 mmHg reduction in SBP (95% CI: –5.7 to –1.3), P = 0.001. Five randomized trials with placebo or other pharmacotherapy comparators produce a combined estimate of 4.1 mmHg SBP lowering (95% CI: –7.0 to –1.1), P < 0.001. Only two studies used the gold standard of ambulatory BP monitoring (ABPM), Yoshida et al.146 demonstrating a SBP reduction of 7.3 mmHg. In contrast Grossman et al.160 showed that TNF-α blockade caused an increase of 1.7 mmHg. Elevated BP was not an inclusion criterion in any of the studies and hypertension was reported inconsistently. Two of the studies reported only mean arterial pressure,153,162 six studies did not report prevalence or use of anti-hypertensives,144,145,153,156,158,161 and one specified no anti-hypertensive use.143 Hypertension prevalence in the remaining studies ranged between 7% and 53%.142,146–152,157,159,160 In some studies, good BP control was an inclusion criteria.142,147,150,160 Finally, individual level data was not available, thus any effect in hypertensive participants may be masked through reporting of average BP across whole study cohorts, though despite this, combined estimates from observational and randomized trials do suggest a BP-lowering effect of anti-TNF-α agents (Figure 2). Observational data on incident rates of hypertension offer additional insight. In comparison with non-biologic anti-inflammatory medications, 4822 anti-TNF-α initiators demonstrated no difference in crude or adjusted rates of incident hypertension (HR: 0.95, 95% CI: 0.74–1.2),163 results supported by a smaller Korean cohort of 996 patients with RA.164 Paradoxically, previous meta-analysis suggested higher rates of incident hypertension as adverse events in TNF-α inhibitor recipients (OR: 1.89, 95% CI: 1.35–2.65).165 This disparity indicates need for targeted studies in hypertensive populations.
Table 2.
Human studies pertaining to TNF-α inhibitor use and reporting data on BP outcomes
| References | Population F=female | Design/comparator/follow-up | SBP Baseline mmHg | Δ SBP mmHg P value |
Notable and confounding features |
|---|---|---|---|---|---|
| Gonzalez-Juanatey et al.142 |
|
|
136 ± 17.8 | –9.1 (–20, 2) P = 0.1 |
9/34 had controlled HTN. Other DMARDs/anti-hypertensives permitted, but no alterations to concomitant medication during study. |
| Bozkirli et al.143 |
|
|
119 ± 9.9 |
|
|
| Komai et al.144 |
|
Pre-/post-IFX +MTX 6 weeks |
127.9 ± 5.6 |
|
|
| Sandoo et al.145 |
|
|
127 ± 15 |
|
|
| Yoshida et al.146 |
|
|
127.4 ± 21.8 |
|
|
| Galarraga et al.147 |
|
|
|
|
|
| Klarenbeek et al.148 |
|
|
136 ± 20 |
|
|
| Tam et al.149 |
|
|
|
|
|
| Daïen et al.150 |
|
|
124 ± 15 |
|
|
| van den Oever et al.151 |
|
|
126 ± 17 |
|
|
| Peters et al.152 |
|
|
130 ± 30 |
|
|
| Mäki-Petäjä et al.153 |
|
|
|
|
|
| Rho et al.154 |
|
|
133.6 ± 21.2 |
|
53% of whole cohort (90/169) had HTN, not broken down by drug class. |
| Angel et al.155 |
|
|
|
|
|
| Thaci et al.156 |
|
|
126.3 |
|
Rates of baseline HTN/BP medications unknown. Secukinumab and placebo arms, but data only reported for former. |
| Baker et al.157 |
|
|
131 ± 16 |
|
|
| Mäki-Petäjä et al.158 |
|
|
|
|
9/17 treated HTN |
| Tam et al.159 |
|
|
|
|
|
| Grossman et al.160 |
|
|
120.9 ± 11.8 | 1.7 (–22, 25) P = 0.88 |
|
| van Doornum et al.161 |
|
|
140 ± 6 |
|
|
ADL, Adalimumab, ank spod, ankylosing spondylitis; IFX, infliximab; ETN, etanercept; GOL, golimumab; MAP, mean arterial pressure; PsA, psoriatic arthritis; RA, rheumatoid arthritis. Asterix (*) is used to indicate a comment in the final column relating specifically to the asterixed result.
Figure 2.
Meta-analysis and Forest Plot using random effect model, of TNF-α inhibitor studies reporting SBP outcomes, with reference to average baseline SBP, population size, and study weighting. Effect size reports average change in SBP in mmHg; * indicates ambulatory BP monitoring and MAP indicates only mean arterial pressure data available. Panel A includes cohort studies reporting average SBP prior and subsequent to drug initiation; panel B includes randomized trials with comparison to placebo or other pharmacotherapy. Overall change in average SBP accompanied by 95% confidence interval. ADL, adalimumab; ETN, etanercept; GOL, golimumab; IFX, infliximab; Mixed, different TNF-α inhibitors within the study; SBP, systolic blood pressure; sDMARD, conventional synthetic disease modifying anti-rheumatic; TNF-α, tumour necrosis factor alpha.
5.1.2 IL-1β inhibition (CANTOS trial)
In a large RCT of patients with prior myocardial infarction and elevated high-sensitivity C-reactive protein, the IL-1β antagonist canakinumab 150 mg demonstrated benefit vs. placebo for a composite end point of myocardial infarction, stroke, or cardiovascular death. Largest effect size was in the quartile demonstrating greatest high-sensitivity C-reactive protein and IL-6 reductions.10,166 Rates of incident hypertension, however, did not differ by high-sensitivity C-reactive protein tertiles; nor did canakinumab demonstrate a reduction in incident hypertension [HR: 0.96 (0.85–1.08), P > 0.2]. Ostensibly, this suggests that BP may not be the mechanism by which benefit was exerted; however, baseline prevalence of hypertension was 80%, thus only 20% of participants were ‘at risk’ from incident hypertension.167 In the canakinumab arm, only subgroups with baseline BP (SBP ≥130 mm Hg) demonstrated BP lowering, as well as protection from major adverse cardiac events (MACE).167 Fatal infections were increased with canakinumab, highlighting the importance of selecting permissible targets.10
5.1.3 Anti-IL-17
Considering other cytokine inhibitor approaches, we focused on pharmacotherapies with both animal study evidence and use in clinical practice: secukinumab and tocilizumab. We identified the FIXTURE trial of IL-17 antagonist secukinumab (150 and 300 mg groups) in patients with psoriasis. Despite BP being the primary outcome, this trial reported no change at 1 year, though patients were not hypertensive at baseline.156 In contrast, a study of 50 patients with psoriasis commenced on secukinumab demonstrated a 6 mmHg reduction of SBP (130–124 mmHg, P = 0.3).168 This is particularly important as psoriasis, like RA, appears to be associated with increased prevalence of hypertension and cardiovascular disease.165,169,170
5.1.4 Anti-IL-6
Three papers were identified reporting BP data with IL-6 antagonist tocilizumab, two used in combination with methotrexate (MTX).171,172 SBP increase was demonstrated by Elmedany et al.171 (116 ± 16 vs. 129 ± 17 mmHg, P = 0.001), the other two papers reporting no change in BP with IL-6 blockade,172,173 though the average baseline BP values were normal range. Overall, the minimally available evidence (detailed in Supplementary material online, Table) does not support an association with BP lowering.
5.2 Immunosuppressant agents
5.2.1 Mycophenolate mofetil
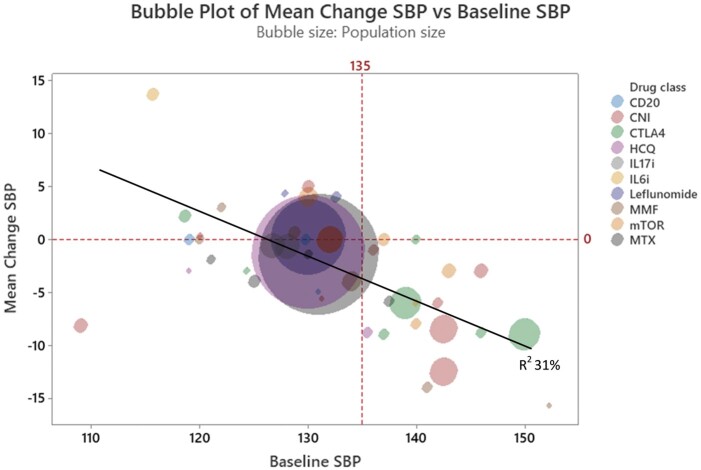
Mycophenolate mofetil (MMF) inhibits nucleotide synthesis and thus prevents lymphocyte proliferation. In an early study, Herrera et al. demonstrated a reduction in average BP from 152/92 to 137/83 mmHg at 12 weeks in eight patients with psoriasis. Notably, BP increased following MMF cessation in this study. The authors also demonstrated a reduction in urinary TNF-α was during MMF therapy.174 Other studies reporting BP data are confounded by the presence of nephropathy, with concomitant anti-hypertensive treatment to achieve target BP under 130/80 mmHg, or organ transplantation in which improvement in volume status could obscure any independent impact of MMF on BP. With these caveats in mind, two trials of MMF in IgA nephropathy report BP reduction of –7 to –14 mmHg.175,176 In two other studies of patients with lower enrolment BP, MMF did not reduce SBP beyond treatment with angiotensin-converting enzyme inhibitors (ACEi) alone, or ACEi plus placebo.177,178 Head-to-head trials in transplantation showed that treatment with tacrolimus/MMF lowered SBP by 4 mmHg (P = 0.08) and diastolic BP by 3 mmHg (P = 0.02) at 6 months compared to transplanted patients receiving tacrolimus/sirolimus. Ninety percent of these subjects had hypertension at baseline.179 In a smaller study, no change in BP occurred in 58 liver transplant patients treated with a tacrolimus/MMF (P = 0.88, baseline average 129/70 mmHg) whilst a group treated with tacrolimus/steroid showed an 8 mmHg rise in SBP.180 Overall, the clinical evidence favours association of MMF with BP reduction in hypertension (see Figure 3); however, no data specifically pertaining to hypertensive patients are available.
Figure 3.
Bubble plot illustrating immunomodulatory agents plotted by baseline SBP (x-axis) and average change in SBP (y-axis), both in mmHg, with bubble area representing cohort size. R2 = 31% fpr average change in SBP by average baseline SBP. CNI, calcineurin inhibitor; CTLA4-Ig, cytotoxic T-lymphocyte-associated protein 4 immunoglobulin; HCQ, hydroxychloroquine; IL, interleukin; MMF, mycophenolate mofetil; mTOR: mammalian target of rapamycin; MTX: methotrexate; SBP, systolic blood pressure; TNF, tumour necrosis factor.
5.2.2 Methotrexate
MTX is a chemotherapy agent and disease-modifying anti-rheumatic drug (DMARD). Five studies involving between 20 and 8065 participants were identified, reporting average baseline SBP between 121 and 137.5 mmHg. Only one of these employed ABPM. Average SBP lowering ranged from 1.4 to 5.9 mmHg, and diastolic blood pressure (DBP) reduction of up to 4.4 mmHg (see Supplementary material online, Table and Figure 3).149,154,157,181,182 Conversely, Makavos et al.168 and CIRT183 RCTs in psoriasis and patients with established cardiovascular risk, respectively, did not demonstrate average BP reduction with MTX. Considering the discrepancy, although 90% of the CIRT cohort had hypertension diagnoses, baseline BP values were not reported, precluding assessment of BP effects in individuals with uncontrolled hypertension.
5.2.3 Hydroxychloroquine
Hydroxychloroquine is an antimalarial agent that is used as a DMARD, and experimentally in IgA nephropathy.154,157,184 This agent has been shown to reduce circulating dendritic cells (DCs) and reduces IFN-α, IL-6, and TNF-α levels.185 Three studies of hydroxychloroquine have demonstrated BP lowering. The largest of these involved 7147 patients with RA and showed that hydroxychloroquine lowered BP by 1.2 mmHg systolic/0.6 mmHg diastolic from a baseline of 130/75 mmHg at 6 months.157 Two smaller studies report SBP lowering of 3–8.8 mmHg (see Supplementary material online, Table).
5.2.4 Leflunomide
Leflunomide is a pyrimidine synthesis inhibitor used in active RA and psoriatic arthritis. In three studies, in which the subjects had an average baseline SBP ranging from 128 to 133 mmHg, a small increase of 1.44–4.3 mmHg systolic and 0.57–4.8 mmHg diastolic in office and ambulatory BP was observed.154,157,186
5.2.5 Calcineurin inhibitors
Calcineurin inhibitors (CNIs) block the earliest steps of T cell activation, but also have substantial off-target effects, including stimulation of endothelin production, increases in sympathetic outflow, renal vasoconstriction, salt retention, and hypertension (Figure 4).187,188 Eight studies with BP data following 12–36 months of CNI treatment are reviewed (see Supplementary material online). In four of these, the baseline BP was in the hypertensive range.189–192 Six reported lowering of BP (range –1 to –13 mmHg),189–194 while two demonstrated a rise in BP of 5–11 mmHg.168,195 Further detail is available in the Supplementary material online and reviewed elsewhere,188 but in summary, limitations of trial design, and CNI off target effects make interpretation of BP effects of CNIs difficult (Figure 4).
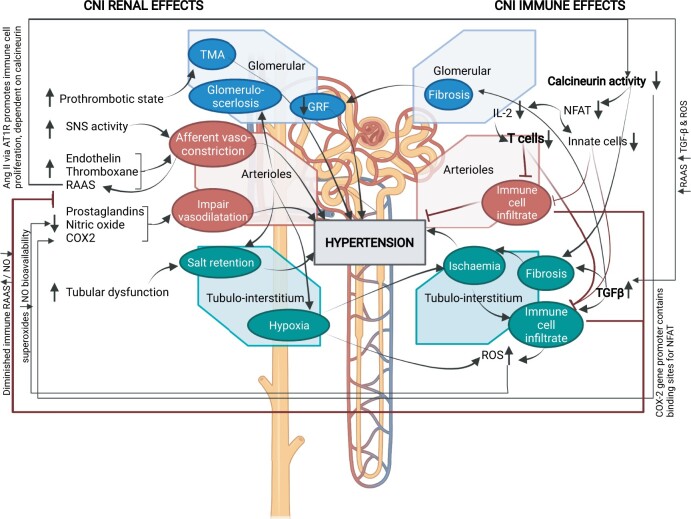
Figure 4.
Renal and immune system effects of calcineurin inhibitors influencing blood pressure. COX2, cyclooxygenase-2; GFR, glomerulofiltration rate; IL-2, interleukin-2; NFAT, nuclear factor of activated T cells; NO, nitric oxide; TMA, thrombotic microangiopathy; RAAS, renin–angiotensin–aldosterone system; ROS, reactive oxygen species; SNS, sympathetic nervous system; TGF-β, transforming growth factor beta. Created in BioRender.
5.2.6 Mammalian target of rapamycin inhibitors
Mammalian target of rapamycin (mTOR) inhibitors such as sirolimus and everolimus regulate cellular metabolism, growth, and proliferation, offering alternative immunosuppression following transplantation. Of six studies we found reporting BP values, the three reporting an average baseline SBP >140 mmHg all suggested a reduction in BP of between 3 and 8 mmHg,189,190,192 though only one achieved statistical significance.189 ABPM was only measured in the SCHEDULE trial of heart transplant patients treated with everolimus. An 8 mmHg fall in SBP (P = 0.05), and no change in DBP occurred from 2 weeks post-transplant to 12 months follow-up. This was dominated by reduction in nocturnal SBP in both the everolimus and cyclosporine arms.189 BP lowering was not observed when the average baseline BP for the study was in the normotensive range.195 mTOR inhibitors in comparison with other agents reported SBP outcomes that were neutral or elevated (0 or +4 mmHg change).179,195,196 These studies are complicated by the concomitant use of multiple other drugs (see Supplementary material online).
5.2.7 Cytotoxic T-lymphocyte-associated protein 4-Ig
Abatacept is composed of the Fc region of the immunoglobulin IgG1 fused to the extracellular domain of cytotoxic T-lymphocyte-associated protein 4 (CTLA-4). This agent targets T cell co-stimulation and is commonly used in transplant and rheumatologic diseases. In five studies of RA patients reporting BP outcomes with abatacept, specific values were not available for two and none of the others reported a statistically significant effect on BP.171,173,197–199 Seven studies reporting BP outcomes using Belatacept, an alternative CTLA-Ig, were identified. All of these were in transplant recipients and were compared to patients receiving CNIs. Two of these studies involved cross over from CNI to Belatacept and showed a SBP reduction of 5.4 and 8.8 mmHg (P = 0.38 and 0.03, respectively).200,201 A case–control study reported a 9 mmHg lower SBP in subjects treated with this agent (P = 0.68).202 Three RCTs showed a reduction in SBP between –2.4 and –9 mmHg,203–205 but only one of these reached statistical significance204 (see Supplementary material online, Table). One RCT reported no difference in mean SBP.206 In only two studies did the subjects have an average baseline SBP in the hypertensive range,199,201 and no studies employed ABPM. The apparent BP benefit with belatacept but not abatacept likely reflects population differences (transplant vs. RA, respectively), potential physiological changes post-transplantation, and the cross-over effect from CNI, which as noted above, has off-target effects that can raise BP.
5.2.8 Rituximab
Rituximab is a monoclonal antibody against CD20, resulting in B cell apoptosis and depletion. It is used in lymphoid and blood malignancies and diverse autoimmune diseases. Trials reporting BP that are not confounded by polypharmacy were sparse. We identified four such studies, and none involved patient groups with uncontrolled hypertension—the average participant baseline SBP being 131/83 mmHg or lower.173,207–209 An early reduction in BP is common, but data reporting longer-term trends were discordant. No BP effect was seen in RA173,207,208; but a BP reduction was observed in membranous nephropathy at 4 weeks, though not sustained to 20 weeks.209
5.3 Determinants of the BP effects of immunosuppressants
In summary, trials in rheumatic, autoimmune, and transplant patients indicate a possible BP-lowering effect of selected anti-inflammatory therapies targeting diverse pathways previously identified by pre-clinical studies. The evidence appears to be most consistent in relation to anti-TNF-α agents, while other therapies such as hydroxychloroquine, MMF, and mTORs all suggest BP-lowering effect (Figures 3 and 5). Data are however conflicting, and hypertension was rarely a pre-specified outcome measure. Trials often involved normotensive populations in which BP lowering is difficult to observe. A combined analysis of studies discussed in this paper shows that cohorts with higher average baseline SBP appear to achieve greater BP-lowering effect (Figure 3), an association also reported for anti-hypertensive drugs.210–212
Figure 5.
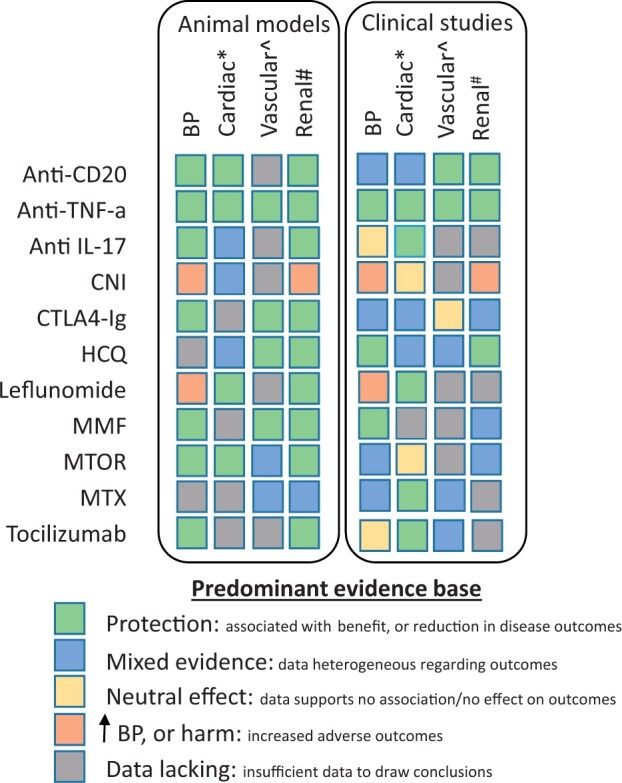
Immunomodulatory drugs and the level of animal and clinical evidence available regarding blood pressure and organ system outcomes. Summarized according to the aggregated weight of the available evidence. BP, blood pressure; CD, cluster of differentiation; CNI, calcineurin inhibitor; CTLA4-Ig, cytotoxic T-lymphocyte-associated protein 4 immunoglobulin; HCQ, hydroxychloroquine; IL, interleukin; MMF, mycophenolate mofetil; mTOR: mammalian target of rapamycin; MTX: methotrexate; TNF, tumour necrosis factor. *Cardiovascular outcomes. ^Includes arterial stiffness, endothelial function, and cerebrovascular outcomes. #Includes chronic kidney disease, end-stage kidney disease, fibrosis, and inflammation.
5.4 Non-pharmacological interventions
Several non-pharmacological treatment approaches have shown beneficial effects in reducing inflammation and therefore improving patient outcomes in the context of hypertension.
5.4.1 Periodontitis targeting and BP
Animal studies suggest that periodontal Porphyromonas gingivalis infection increases IFN-γ and TNF-α production through modulation of Th1 responses, leading to BP elevation, endothelial dysfunction, and vascular inflammation.213 This link is supported by Mendelian randomization,214 observational data, and meta-analysis.215–218 Data from well-controlled trials demonstrate that intense treatment of periodontitis can improve endothelial function,219 lower inflammatory markers, and BP as measured by ABPM, with a reduction in SBP of 5 mmHg (P < 0.01).220 A meta-analysis of eight studies involving intensive periodontal treatment showed an average decrease of SBP of −4.3 mm Hg (95% CI: –9.1 to –0.5) and DBP –3.16 mm Hg (95% CI: –6.5 to –0.2), though none of these achieved statistical significance. As in the case of pharmacological interventions, BP reductions were not observed in normotensive individuals.221
5.4.2 Energy metabolism, microbiome, and salt
Physical activity has an established role in BP regulation, with 3 months of exercise lowering SBP by approximately 5 mmHg and DBP by 3 mmHg.222 Physical activity also has demonstrable immune effects.223 Exercise can both increase circulating numbers of T cells224 and improve response to influenza vaccination.225
For dietary interventions, most research has focused on CVD risk reduction, though BP lowering has also been demonstrated in both normotensive and hypertensive cohorts,226,227 at least in part immune-mediated via effects of diet on the microbiome.228 Metagenome-wide association evidence of gut dysbiosis in hypertension includes restricted sample diversity, higher lipopolysaccharide synthesis, membrane transport, and steroid degradation; suggesting low-grade inflammatory stimuli may be the mechanism.229 Evidence is accumulating that plant-based dietary protein may promote bacterial species associated with anti-inflammatory effects, while meat consumption is linked to CVD and inflammatory bowel disease.230
Dietary salt is another dominant driver of hypertension, primarily through activation of renin–angiotensin–aldosterone system231; at higher concentration, salt also favours pro-inflammatory monocyte232 and T cell phenotypes with increased tissue infiltration233 and microvascular dysfunction.234 Highly controlled experimental reduction in salt intake lowers pro-inflammatory IL-6 and IL-23, and increases IL-10 levels,235 though this effect was not detected in a larger observational study.236
5.4.3 Neuronal manipulations
The central nervous system regulates vascular and kidney function through sympathetic innervation but is also a potent modulator of immune responses. Animal and human studies demonstrate the role of neuroimmune axis in the pathogenesis of hypertension,237,238 with murine renal denervation (RDN) inducing a reduction in BP,239–242 and reduction in renal inflammation, T cell activation, and pro-inflammatory cytokine production.240,243 However, SIMPLICITY, SPYRAL, and RADIANCE human clinical trials demonstrate inconsistent results, mostly favouring sustained BP reduction.244,245 Some but not all246 of these were sham-controlled RDN designs.247–249 The effect of RDN on immune activation in humans is less clear. One trial demonstrated reductions in TNF-α and IL-1β, and up-regulation of IL-10 one day after RDN; however, this did not persist to day 3,250 and was not corroborated elsewhere.251,252
An alternative approach to sympathetic denervation is augmentation of parasympathetic activity through vagus nerve stimulation (VNS). This approach has proven effective in hypertensive rodent models.253–255 VNS limits hypertension-induced endothelial dysfunction256 and reduces levels of systemic cytokines and mRNA expression in target organs,257 with both afferent and efferent VNS protecting mice from kidney injury.258 Anti-inflammatory effects of VNS are abolished in immune-deficient and β2 adrenergic receptor-deficient mice.259 When stimulated by Ang II or bioelectronic signals, a splenic neuroimmune cascade is triggered via α-adrenergic receptors. In response, CD8+ effector T cells with a role in hypertension25 egress from the spleen.260 VNS has not yet been tested in human hypertension, but has been used in epilepsy and in RA, demonstrating lowering of circulating TNF-α, IL-1-β, and IL-6 levels and improvement in disease activity.261
5.5 Hypertension-mediated organ damage
Hypertension-mediated organ damage (HMOD) correlates with BP values in hypertension262,263; however, genetics, lifestyle, and co-morbid conditions may also contribute to end-organ damage independently of BP levels. Similarly, the target organ benefit of immunomodulation might be partially independent of BP effects. The strength of evidence regarding the effects of immunomodulatory therapy on HMOD in experimental and clinical settings is summarized in Figure 5. Registry data of active RA, with 30% hypertension prevalence, suggested no difference in myocardial infarction rates in response to TNF-α inhibitors vs. DMARDs. However, 60% fewer events did occur in the TNF-α inhibitor responder subgroup vs. non-responders.264 The observational QUEST-RA study included subjects with hypertension prevalence of 32% and was adjusted for traditional risk factors. This study reported a reduction in cardiovascular risk in response to numerous immunomodulatory drugs, including biologic agents (HR: 0.42; 95% CI: 0.21–0.81), MTX (HR: 0.85; 95% CI: 0.81–0.89), sulfasalazine (HR: 0.92; 95% CI: 0.87–0.98), and leflunomide (HR: 0.59; 95% CI: 0.43–0.79); P < 0.05.265 Baseline BP values were not reported in either paper. Nurmohamed et al. reviewed 90 studies reporting cardiovascular risk outcomes in rheumatological conditions treated with abatacept, TNF-α inhibitors, rituximab, secukinumab, tocilizumab, and tofacitinib. They report a neutral effect on BP, on surrogate markers of cardiovascular risk, and on MACE, though authors emphasise the variation in quantity and quality of evidence.266
Observational data based on 13 000 matched pairs from Medicare and MarketScan patients with RA and newly treated with abatacept or a TNF-α inhibitor found benefit of abatacept in MACE restricted to the subgroup with diabetes [HR: 0.74 (95% CI: 0.57–0.96)].267 Potential confounding arose from higher rates of hypertension in the diabetic subgroups, again supporting potential benefit of TNF-α inhibitors in hypertension.167 Finally, a meta-analysis of 14 studies in patients with RA, adjusted for hypertension, concluded that DMARDs were associated with an increased risk of MACE relative to TNF-α inhibitor therapy [OR: 1.58 (95% CI: 1.16–2.15); I2 = 16%], effect maintained in presence or absence of MTX.268
Colchicine is hypothesized to inhibit microtubular polymerization, assembly of the NLRP3 inflammasome, and IL-1β and IL-18 production. In acute coronary syndrome, colchicine abrogates local increases in IL-1β, IL-18, and IL-6 levels,269 and its addition to aspirin and statin reduces high-sensitivity C-reactive protein.270 Colchicine 0.5 mg daily has been demonstrated to reduce MACE by 67% compared to placebo in LoDoCo RCT of 532 patients with stable coronary artery disease,271 though the similarly sized COPS trial found no benefit in cardiovascular outcomes.272 The larger COLCOT trial of 4745 participants recruited within 30 days of acute coronary syndrome reported composite cardiovascular end-point occurrences in 5.5% of the colchicine group vs. 7.1% of the placebo group (HR: 0.77; 95% CI: 0.61–0.96; P = 0.02).9 Half of these patients had hypertension. Similarly, LoDoCo2 randomized 5522 chronic coronary disease patients to low-dose colchicine, with composite end-point events in 6.8% of the colchicine group vs. 9.6% of placebo group (HR: 0.69; 95% CI: 0.57–0.83; P < 0.001).11
Overall, we would conclude that there is evidence of improvement in MACE for TNF-α inhibitors, MTX, tocilizumab, secukinumab, leflunomide and colchicine, though heterogeneity of study designs and outcomes limits the strength of this statement, and we have not explored the relationship between reduction in inflammation and MACE suggested by CANTOS and TNF-α inhibitor responders in the registry data above. HMOD outcomes beyond MACE are surmised in Figure 5 for common immunomodulatory drugs.
6. Conclusions
While experimental, genetic, and clinical evidence supports the role of inflammation and immune system involvement in hypertension and associated vascular, renal, and cardiac pathology, immunomodulatory approaches are not currently considered therapeutic options in BP lowering and cardiovascular disease reduction. Indeed, clinical evidence reviewed in this paper shown a highly heterogeneous effect of immune targeting on BP and cardiovascular events across a wide range of patients mainly with various underlying immune-mediated diseases. Going forward, there are several important considerations. As is the case with traditional anti-hypertensive medications, the BP-lowering effects of anti-inflammatory agents appear to be limited to those with uncontrolled hypertension. This is not surprising as numerous compensatory mechanisms make lowering beyond normal BP difficult. It is also important to consider that the effects may be limited to patients with active pro-hypertensive inflammatory mechanisms. The lesson from CIRT, TNF-α inhibitor responders vs. non-responders, CANTOS, and the body of the evidence presented is that there must be active inflammation. Hence, cardiovascular risk reduction with immune modulation is mediated not through BP alone, but via broader mechanisms of oxidative stress, endothelial function, vascular remodelling, and endocrine regulation, that are the ‘common denominators’ of a dysfunctional relationship. Secondly, we must target the optimal checkpoint in the inflammation–hypertension relationship to optimize benefit without adverse effect, and so far, this has remained elusive at a population level. Finally, it is important to consider that virtually all of the preclinical studies investigating the anti-hypertensive effect of immune interventions on hypertension have involved treatment of animals at the onset on hypertension, often concomitantly with the onset of the disease. In contrast, these agents are usually given to humans with long-standing hypertension. It is possible, and even likely that once hypertension has been established, there are chronic changes in renal and vascular function and structure that render such treatment less effective. In this regard, treatment of younger individuals with early onset hypertension might yield different results than those observed in the studies summarized here.
Supplementary material
Supplementary material is available at Cardiovascular Research online.
Conflict of interest: none to declare.
Funding
This work was supported by the European Research Council (Project Identifier: 726318); the British Heart Foundation grants PG/19/84/34771, PG/21/10541, and RE/13/5/30177; the Marie Sklodowska Curie CIG Award 3631773; the Wellcome Trust grant 204820/Z/16/Z; and the University of Glasgow, Scottish Funding Council and the Global Challenges Research Fund.
Data availability
Data derived from sources in the public domain. Reference details are provided in full.
Supplementary Material
Acknowledgements
Statistical assistance was provided by Dr John McClure, University of Glasgow. Software used in the generating of this manuscript includes BioRender.com (figures), Minitab-19 Statistical Software, and Meta-essentials (meta-analysis).273
Contributor Information
Eleanor C Murray, Institute of Cardiovascular and Medical Sciences, College of Medical, Veterinary and Life Sciences, University of Glasgow, G12 8TA Glasgow, UK.
Ryszard Nosalski, Institute of Cardiovascular and Medical Sciences, College of Medical, Veterinary and Life Sciences, University of Glasgow, G12 8TA Glasgow, UK; Department of Internal Medicine, Collegium Medicum, Jagiellonian University, 31-008 Kraków, Poland.
Neil MacRitchie, Centre for Immunobiology, Institute of Infection, Immunity and Inflammation, College of Medical, Veterinary and Life Sciences, University of Glasgow, G12 8TA Glasgow, UK.
Maciej Tomaszewski, Division of Cardiovascular Sciences, Faculty of Medicine, Biology and Health, University of Manchester, M13 9PL Manchester, UK; Manchester Heart Centre and Manchester Academic Health Science Centre, Manchester University NHS Foundation Trust, M13 9WL Manchester, UK.
Pasquale Maffia, Institute of Cardiovascular and Medical Sciences, College of Medical, Veterinary and Life Sciences, University of Glasgow, G12 8TA Glasgow, UK; Centre for Immunobiology, Institute of Infection, Immunity and Inflammation, College of Medical, Veterinary and Life Sciences, University of Glasgow, G12 8TA Glasgow, UK; Department of Pharmacy, University of Naples Federico II, 80131 Naples, Italy.
David G Harrison, Division of Clinical Pharmacology, Department of Medicine, Vanderbildt University Medical Centre, Nashville, 37232 TN, USA.
Tomasz J Guzik, Institute of Cardiovascular and Medical Sciences, College of Medical, Veterinary and Life Sciences, University of Glasgow, G12 8TA Glasgow, UK; Department of Internal Medicine, Collegium Medicum, Jagiellonian University, 31-008 Kraków, Poland.
This article is part of the Spotlight Issue on Cardiovascular Immunology.
Tomasz Guzik and Pasquale Maffia have positions within CVR; the manuscript was handled by a consulting editor.
References
- 1. Libby P. The changing landscape of atherosclerosis. Nature 2021;592:524–533. [DOI] [PubMed] [Google Scholar]
- 2. Liberale L, Montecucco F, Tardif JC, Libby P, Camici GG. Inflamm-ageing: the role of inflammation in age-dependent cardiovascular disease. Eur Heart J 2020;41:2974–2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nus M, Mallat Z, Sage A. Beating (T-lymphocyte driven) atherosclerosis with B- and T-lymphocyte attenuator. Cardiovasc Res 2020;116:251–252. [DOI] [PubMed] [Google Scholar]
- 4. van Kuijk K, Kuppe C, Betsholtz C, Vanlandewijck M, Kramann R, Sluimer JC. Heterogeneity and plasticity in healthy and atherosclerotic vasculature explored by single-cell sequencing. Cardiovasc Res 2019;115:1705–1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Douna H, Amersfoort J, Schaftenaar FH, Kröner MJ, Kiss MG, Slütter B, Depuydt MAC, Bernabé Kleijn MNA, Wezel A, Smeets HJ, Yagita H, Binder CJ, Bot I, van Puijvelde GHM, Kuiper J, Foks AC. B- and T-lymphocyte attenuator stimulation protects against atherosclerosis by regulating follicular B cells. Cardiovasc Res 2020;116:295–305. [DOI] [PubMed] [Google Scholar]
- 6. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, Benetos A, Biffi A, Boavida J-M, Capodanno D, Cosyns B, Crawford C, Davos CH, Desormais I, Di Angelantonio E, Franco OH, Halvorsen S, Hobbs FDR, Hollander M, Jankowska EA, Michal M, Sacco S, Sattar N, Tokgozoglu L, Tonstad S, Tsioufis KP, van Dis I, van Gelder IC, Wanner C, Williams B. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021;42:3227–3337. [DOI] [PubMed] [Google Scholar]
- 7. Steffens S, van LS, Sluijter JPG, Tocchetti CG, Thum T, Madonna R. Stimulating pro-reparative immune responses to prevent adverse cardiac remodelling: consensus document from the joint 2019 meeting of the ESC Working Groups of cellular biology of the heart and myocardial function. Cardiovasc Res 2020;116:1850–1862. [DOI] [PubMed] [Google Scholar]
- 8. Elnabawi YA, Dey AK, Goyal A, Groenendyk JW, Chung JH, Belur AD, Rodante J, Harrington CL, Teague HL, Baumer Y, Keel A, Playford MP, Sandfort V, Chen MY, Lockshin B, Gelfand JM, Bluemke DA, Mehta NN. Coronary artery plaque characteristics and treatment with biologic therapy in severe psoriasis: results from a prospective observational study. Cardiovasc Res 2019;115:721–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tardif J-CC, Kouz S, Waters DD, Bertrand OF, Diaz R, Maggioni AP, Pinto FJ, Ibrahim R, Gamra H, Kiwan GS, Berry C, López-Sendón J, Ostadal P, Koenig W, Angoulvant D, Grégoire JC, Lavoie M-AA, Dubé M-PP, Rhainds D, Provencher M, Blondeau L, Orfanos A, L’Allier PL, Guertin M-CC, Roubille F. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med 2019;381:2497–2499. [DOI] [PubMed] [Google Scholar]
- 10. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ, Krum H, Varigos J. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 2017;377:1119–1131. [DOI] [PubMed] [Google Scholar]
- 11. Nidorf SM, Fiolet ATL, Mosterd A, Eikelboom JW, Schut A, Opstal TSJ, The SHK, Xu X-F, Ireland MA, Lenderink T, Latchem D, Hoogslag P, Jerzewski A, Nierop P, Whelan A, Hendriks R, Swart H, Schaap J, Kuijper AFM, van Hessen MWJ, Saklani P, Tan I, Thompson AG, Morton A, Judkins C, Bax WA, Dirksen M, Alings M, Hankey GJ, Budgeon CA, Tijssen JGP, Cornel JH, Thompson PL; LoDoCo2 Trial Investigators. Colchicine in patients with chronic coronary disease. N Engl J Med 2020;383:1838–1847. [DOI] [PubMed] [Google Scholar]
- 12. Weber BN, Blankstein R. Something old, something new: a paradigm for considering immune therapies for cardiovascular disease. Cardiovasc Res 2020;116:e51–e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1923–1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Markó L, Park J-K, Henke N, Rong S, Balogh A, Klamer S, Bartolomaeus H, Wilck N, Ruland J, Forslund SK, Luft FC, Dechend R, Müller DN. B-cell lymphoma/leukaemia 10 and angiotensin II-induced kidney injury. Cardiovasc Res 2020;116:1059–1070. [DOI] [PubMed] [Google Scholar]
- 15. Grabie N, Lichtman AH, Padera R. T cell checkpoint regulators in the heart. Cardiovasc Res 2019;115:869–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Peet C, Ivetic A, Bromage DI, Shah AM. Cardiac monocytes and macrophages after myocardial infarction. Cardiovasc Res 2020;116:1101–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Drummond GR, Vinh A, Guzik TJ, Sobey CG. Immune mechanisms of hypertension. Nat Rev Immunol 2019;19:517–532. [DOI] [PubMed] [Google Scholar]
- 18. Okuda T, Grollman A. Passive transfer of autoimmune induced hypertension in the rat by lymph node cells. Tex Rep Biol Med 1967;25:257–264. [PubMed] [Google Scholar]
- 19. Svendsen U. The role of thymus for the development and prognosis of hypertension and hypertensive vascular disease in mice following renal infarction. Acta Pathol Microbiol Scand A 1976;84:235–243. [DOI] [PubMed] [Google Scholar]
- 20. Svendsen UG. Influence of neonatal thymectomy on blood pressure and hypertensive vascular diseases in rats with renal hypertension. Acta Pathol Microbiol Scand A 1975;83:199–205. [DOI] [PubMed] [Google Scholar]
- 21. Svendsen UG. Thymus dependency of periarteritis nodosa in DOCA and salt treated mice. Acta Pathol Microbiol Scand A 1974;82:30–34. [DOI] [PubMed] [Google Scholar]
- 22. Olsen F. Transfer of arterial hypertension by splenic cells from DOCA-salt hypertensive and renal hypertensive rats to normotensive recipients. Acta Pathol Microbiol Scand C 1980;88:1–6. [DOI] [PubMed] [Google Scholar]
- 23. Olsen F. Evidence for an immunological factor in the hypertensive vascular disease. Acta Pathol Microbiol Scand A 1971;79:22–26. [DOI] [PubMed] [Google Scholar]
- 24. Vinh A, Chen W, Blinder Y, Weiss D, Taylor WR, Goronzy JJ, Weyand CM, Harrison DG, Guzik TJ. Inhibition and genetic ablation of the B7/CD28 T-cell costimulation axis prevents experimental hypertension. Circulation 2010;122:2529–2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Guzik TJ, Hoch NE, Brown KA, McCann LA, Rahman A, Dikalov S, Goronzy J, Weyand C, Harrison DG. Role of the T cell in the genesis of angiotensin II–induced hypertension and vascular dysfunction. J Exp Med 2007;204:2449–2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pollow DP, Uhrlaub J, Romero-Aleshire M, Sandberg K, Nikolich-Zugich J, Brooks HL, Hay M. Sex differences in T-lymphocyte tissue infiltration and development of angiotensin II hypertension. Hypertension 2014;64:834–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Seniuk A, Thiele JL, Stubbe A, Oser P, Rosendahl A, Bode M, Meyer-Schwesinger C, Wenzel UO, Ehmke H. B6.Rag1 Knockout mice generated at the Jackson Laboratory in 2009 show a robust wild-type hypertensive phenotype in response to Ang II (angiotensin II). Hypertension 2020;75:1110–1116. [DOI] [PubMed] [Google Scholar]
- 28. Ji H, Pai AV, West CA, Wu X, Speth RC, Sandberg K. Loss of resistance to angiotensin II-induced hypertension in the Jackson Laboratory recombination-activating gene null mouse on the C57BL/6J background. Hypertension 2017;69:1121–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mattson DL, Lund H, Guo C, Rudemiller N, Geurts AM, Jacob H. Genetic mutation of recombination activating gene 1 in Dahl salt-sensitive rats attenuates hypertension and renal damage. Am J Physiol Regul Integr Comp Physiol 2013;304:R407–R414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Crowley SD, Song Y-S, Lin EE, Griffiths R, Kim H-S, Ruiz P. Lymphocyte responses exacerbate angiotensin II-dependent hypertension. Am J Physiol Regul Integr Comp Physiol 2010;298:1089–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wu J, Thabet SR, Kirabo A, Trott DW, Saleh MA, Xiao L, Madhur MS, Chen W, Harrison DG. Inflammation and mechanical stretch promote aortic stiffening in hypertension through activation of p38 mitogen-activated protein kinase. Circ Res 2014;114:616–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Trott DW, Thabet SR, Kirabo A, Saleh MA, Itani H, Norlander AE, Wu J, Goldstein A, Arendshorst WJ, Madhur MS, Chen W, Li C-I, Shyr Y, Harrison DG. Oligoclonal CD8+ T cells play a critical role in the development of hypertension. Hypertension 2014;64:1108–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kvakan H, Kleinewietfeld M, Qadri F, Park J-K, Fischer R, Schwarz I, Rahn H-P, Plehm R, Wellner M, Elitok S, Gratze P, Dechend R, Luft FC, Muller DN. Regulatory T cells ameliorate angiotensin II-induced cardiac damage. Circulation 2009;119:2904–2912. [DOI] [PubMed] [Google Scholar]
- 34. Barhoumi T, Kasal DA, Li MW, Shbat L, Laurant P, Neves MF, Paradis P, Schiffrin EL. T regulatory lymphocytes prevent angiotensin II-induced hypertension and vascular injury. Hypertension 2011;57:469–476. [DOI] [PubMed] [Google Scholar]
- 35. Caillon A, Mian MOR, Fraulob-Aquino JC, Huo K-G, Barhoumi T, Ouerd S, Sinnaeve PR, Paradis P, Schiffrin EL. γδ T cells mediate angiotensin II-induced hypertension and vascular injury. Circulation 2017;135:2155–2162. [DOI] [PubMed] [Google Scholar]
- 36. Wenzel P, Knorr M, Kossmann S, Stratmann J, Hausding M, Schuhmacher S, Karbach SH, Schwenk M, Yogev N, Schulz E, Oelze M, Grabbe S, Jonuleit H, Becker C, Daiber A, Waisman A, Münzel T. Lysozyme M-positive monocytes mediate angiotensin ii-induced arterial hypertension and vascular dysfunction. Circulation 2011;124:1370–1381. [DOI] [PubMed] [Google Scholar]
- 37. Moore JP, Vinh A, Tuck KL, Sakkal S, Krishnan SM, Chan CT, Lieu M, Samuel CS, Diep H, Kemp-Harper BK, Tare M, Ricardo SD, Guzik TJ, Sobey CG, Drummond GR. M2 macrophage accumulation in the aortic wall during angiotensin II infusion in mice is associated with fibrosis, elastin loss and elevated blood pressure. Am J Physiol Heart Circ Physiol 2015;309:H906–H917. [DOI] [PubMed] [Google Scholar]
- 38. De Ciuceis C, Amiri F, Brassard P, Endemann DH, Touyz RM, Schiffrin EL. Reduced vascular remodeling, endothelial dysfunction, and oxidative stress in resistance arteries of angiotensin II-infused macrophage colony-stimulating factor-deficient mice: evidence for a role in inflammation in angiotensin-induced vascular injury. Arterioscler Thromb Vasc Biol 2005;25:2106–2113. [DOI] [PubMed] [Google Scholar]
- 39. Huang L, Wang A, Hao Y, Li W, Liu C, Yang Z, Zheng F, Zhou M-S. Macrophage depletion lowered blood pressure and attenuated hypertensive renal injury and fibrosis. Front Physiol 2018;9:e473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hevia D, Araos P, Prado C, Luppichini Rojas FE, Alzamora M, Cifuentes-Araneda R, Gonzalez F, Amador AA, Pacheco CA, Michea R. L. Myeloid CD11c+ antigen-presenting cells ablation prevents hypertension in response to angiotensin II plus high-salt diet. Hypertension 2018;71:709–718. [DOI] [PubMed] [Google Scholar]
- 41. Chan CT, Sobey CG, Lieu M, Ferens D, Kett MM, Diep H, Kim HA, Krishnan SM, Lewis CV, Salimova E, Tipping P, Vinh A, Samuel CS, Peter K, Guzik TJ, Kyaw TS, Toh BH, Bobik A, Drummond GR. Obligatory role for B cells in the development of angiotensin II-dependent hypertension. Hypertension 2015;66:1023–1033. [DOI] [PubMed] [Google Scholar]
- 42. Chen Y, Dale BL, Alexander MR, Xiao L, Ao M, Pandey AK, Smart CD, Davis GK, Madhur MS. Class switching and high-affinity immunoglobulin G production by B cells is dispensable for the development of hypertension in mice. Cardiovasc Res 2021;117:1217–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kossmann S, Schwenk M, Hausding M, Karbach SH, Schmidgen MI, Brandt M, Knorr M, Hu H, Kröller-Schön S, Schönfelder T, Grabbe S, Oelze M, Daiber A, Münzel T, Becker C, Wenzel P. Angiotensin ii-induced vascular dysfunction depends on interferon-γ- driven immune cell recruitment and mutual activation of monocytes and NK-cells. Arterioscler Thromb Vasc Biol 2013;33:1313–1319. [DOI] [PubMed] [Google Scholar]
- 44. Rodríguez-Iturbe B, Ferrebuz A, Vanegas V, Quiroz Y, Mezzano S, Vaziri ND. Early and sustained inhibition of nuclear factor-kappaB prevents hypertension in spontaneously hypertensive rats. J Pharmacol Exp Ther 2005;315:e51–e57. [DOI] [PubMed] [Google Scholar]
- 45. Brands MW, Banes-Berceli AKL, Inscho EW, Al-Azawi H, Allen AJ, Labazi H. Interleukin 6 knockout prevents angiotensin II hypertension: role of renal vasoconstriction and janus kinase 2/signal transducer and activator of transcription 3 activation. Hypertension 2010;56:879–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wen Y, Liu Y, Tang T, Lv L, Liu H, Ma K, Liu B. NLRP3 inflammasome activation is involved in Ang II-induced kidney damage via mitochondrial dysfunction. Oncotarget 2016;7:54290–54302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Huang B, Cheng Y, Usa K, Liu Y, Baker MA, Mattson DL, He Y, Wang N, Liang M. Renal tumor necrosis factor α contributes to hypertension in Dahl salt-sensitive rats. Sci Rep 2016;6:21960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. McShane L, Tabas I, Lemke G, Kurowska-Stolarska M, Maffia P. TAM receptors in cardiovascular disease. Cardiovasc Res 2019;115:1286–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Nosalski R, Mikolajczyk T, Siedlinski M, Saju B, Koziol J, Maffia P, Guzik TJ. Nox1/4 inhibition exacerbates age dependent perivascular inflammation and fibrosis in a model of spontaneous hypertension. Pharmacol Res 2020;161:105235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. MacRitchie N, Grassia G, Noonan J, Cole JE, Hughes CE, Schroeder J, Benson RA, Cochain C, Zernecke A, Guzik TJ, Garside P, Monaco C, Maffia P. The aorta can act as a site of naïve CD4+ T-cell priming. Cardiovasc Res 2020;116:306–316. [DOI] [PubMed] [Google Scholar]
- 51. Kirabo A, Fontana V, de Faria APC, Loperena R, Galindo CL, Wu J, Bikineyeva AT, Dikalov S, Xiao L, Chen W, Saleh MA, Trott DW, Itani HA, Vinh A, Amarnath V, Amarnath K, Guzik TJ, Bernstein KE, Shen XZ, Shyr Y, Chen S-C, Mernaugh RL, Laffer CL, Elijovich F, Davies SS, Moreno H, Madhur MS, Roberts J, Harrison DG. DC isoketal-modified proteins activate T cells and promote hypertension. J Clin Invest 2014;124:4642–4656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Krishnan SM, Dowling JK, Ling YH, Diep H, Chan CT, Ferens D, Kett MM, Pinar A, Samuel CS, Vinh A, Arumugam TV, Hewitson TD, Kemp-Harper BK, Robertson AAB, Cooper MA, Latz E, Mansell A, Sobey CG, Drummond GR. Inflammasome activity is essential for one kidney/deoxycorticosterone acetate/salt-induced hypertension in mice. Br J Pharmacol 2016;173:752–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Carnevale D, Perrotta M, Pallante F, Fardella V, Iacobucci R, Fardella S, Carnevale L, Carnevale R, De LM, Cifelli G, Lembo G. A cholinergic-sympathetic pathway primes immunity in hypertension and mediates brain-to-spleen communication. Nat Commun 2016;7:13035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Carnevale D, Pallante F, Fardella V, Fardella S, Iacobucci R, Federici M, Cifelli G, De Lucia M, Lembo G. The angiogenic factor PIGF mediates a neuroimmune interaction in the spleen to allow the onset of hypertension. Immunity 2014;41:737–752. [DOI] [PubMed] [Google Scholar]
- 55. Rodriguez-Iturbe B, Lanaspa MA, Johnson RJ. The role of autoimmune reactivity induced by heat shock protein 70 in the pathogenesis of essential hypertension. Br J Pharmacol 2019;176:1829–1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Idris-Khodja N, Mian MOR, Paradis P, Schiffrin EL. Dual opposing roles of adaptive immunity in hypertension. Eur Heart J 2014;35:1238–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Madhur MS, Kirabo A, Guzik TJ, Harrison DG. From rags to riches: moving beyond Rag1 in studies of hypertension. Hypertension 2020;75:930–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Xiao L, Harrison DG. Inflammation in hypertension. Can J Cardiol 2020;36:635–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Nosalski R, Siedlinski M, Denby L, McGinnigle E, Nowak M, Cat AND, Medina-Ruiz L, Cantini M, Skiba D, Wilk G, Osmenda G, Rodor J, Salmeron-Sanchez M, Graham G, Maffia P, Graham D, Baker AH, Guzik TJ. T-cell-derived miRNA-214 mediates perivascular fibrosis in hypertension. Circ Res 2020;126:988–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hoyer FF, Nahrendorf M. Interferon-γ regulates cardiac myeloid cells in myocardial infarction. Cardiovasc Res 2019;115:1815–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Abdellatif M, Zirlik A. Immunometabolism: a key target to improve microcirculation in ageing. Cardiovasc Res 2020;116:e48–e50. [DOI] [PubMed] [Google Scholar]
- 62. Matrougui K, Abd Elmageed Z, Zakaria AE, Kassan M, Choi S, Nair D, Gonzalez-Villalobos RA, Chentoufi AA, Kadowitz P, Belmadani S, Partyka M. Natural regulatory T cells control coronary arteriolar endothelial dysfunction in hypertensive mice. Am J Pathol 2011;178:434–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Madhur MS, Lob HE, McCann LA, Iwakura Y, Blinder Y, Guzik TJ, Harrison DG. Interleukin 17 promotes angiotensin II-induced hypertension and vascular dysfunction. Hypertension 2010;55:500–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kamat N. V, Thabet SR, Xiao L, Saleh MA, Kirabo A, Madhur MS, Delpire E, Harrison DG, McDonough AA. Renal transporter activation during angiotensin-II hypertension is blunted in interferon-γ-/- and interleukin-17A-/- mice. Hypertension 2015;65:569–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Zhang J, Patel MB, Griffiths R, Mao A, Song Y, Karlovich NS, Sparks MA, Jin H, Wu M, Lin EE, Crowley SD. Tumor necrosis factor-α produced in the kidney contributes to angiotensin II-dependent hypertension. Hypertension 2014;64:1275–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Yvan-Charvet L, Bonacina F, Guinamard RR, Norata GD. Immunometabolic function of cholesterol in cardiovascular disease and beyond. Cardiovasc Res 2019;115:1393–1407. [DOI] [PubMed] [Google Scholar]
- 67. Filho AG, Kinote A, Pereira DJ, Rennó A, Dos Santos RC, Ferreira-Melo SE, Velloso LA, Bordin S, Anhê GF, Junior HM. Infliximab prevents increased systolic blood pressure and upregulates the AKT/eNOS pathway in the aorta of spontaneously hypertensive rats. Eur J Pharmacol 2013;700:201–209. [DOI] [PubMed] [Google Scholar]
- 68. Elmarakby AA, Quigley JE, Pollock DM, Imig JD. Tumor necrosis factor alpha blockade increases renal Cyp2c23 expression and slows the progression of renal damage in salt-sensitive hypertension. Hypertension 2006;47:557–562. [DOI] [PubMed] [Google Scholar]
- 69. Muller DN, Shagdarsuren E, Park J-K, Dechend R, Mervaala E, Hampich F, Fiebeler A, Ju X, Finckenberg P, Theuer J, Viedt C, Kreuzer J, Heidecke H, Haller H, Zenke M, Luft FC. Immunosuppressive treatment protects against angiotensin II-induced renal damage. Am J Pathol 2002;161:1679–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Tran LT, MacLeod KM, McNeill JH. Chronic etanercept treatment prevents the development of hypertension in fructose-fed rats. Mol Cell Biochem 2009;330:219–228. [DOI] [PubMed] [Google Scholar]
- 71. Venegas-Pont M, Manigrasso MB, Grifoni SC, LaMarca BB, Maric C, Racusen LC, Glover PH, Jones AV, Drummond HA, Ryan MJ. Tumor necrosis factor-alpha antagonist etanercept decreases blood pressure and protects the kidney in a mouse model of systemic lupus erythematosus. Hypertension 2010;56:643–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Therrien FJ, Agharazii M, Lebel M, Larivière R. Neutralization of tumor necrosis factor-alpha reduces renal fibrosis and hypertension in rats with renal failure. Am J Nephrol 2012;36:151–161. [DOI] [PubMed] [Google Scholar]
- 73. Krishnan SM, Ling YH, Huuskes BM, Ferens DM, Saini N, Chan CT, Diep H, Kett MM, Samuel CS, Kemp-Harper BK, Robertson AAB, Cooper MA, Peter K, Latz E, Mansell AS, Sobey CG, Drummond GR, Vinh A. Pharmacological inhibition of the NLRP3 inflammasome reduces blood pressure, renal damage, and dysfunction in salt-sensitive hypertension. Cardiovasc Res 2018;61:776–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Cau SBA, Guimaraes DA, Rizzi E, Ceron CS, Gerlach RF, Tanus-Santos JE. The nuclear factor kappaB inhibitor pyrrolidine dithiocarbamate prevents cardiac remodelling and matrix metalloproteinase-2 up-regulation in renovascular hypertension. Basic Clin Pharmacol Toxicol 2015;117:234–241. [DOI] [PubMed] [Google Scholar]
- 75. Zhang J, Rudemiller NP, Patel MB, Karlovich NS, Wu M, McDonough AA, Griffiths R, Sparks MA, Jeffs AD, Crowley SD. Interleukin-1 receptor activation potentiates salt reabsorption in angiotensin II-induced hypertension via the NKCC2 Co-transporter in the nephron. Cell Metab 2016;23:360–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ling YH, Krishnan SM, Chan CT, Diep H, Ferens D, Chin-Dusting J, Kemp-Harper BK, Samuel CS, Hewitson TD, Latz E, Mansell A, Sobey CG, Drummond GR. Anakinra reduces blood pressure and renal fibrosis in one kidney/DOCA/salt-induced hypertension. Pharmacol Res 2017;116:77–86. [DOI] [PubMed] [Google Scholar]
- 77. Hashmat S, Rudemiller N, Lund H, Abais-Battad JM, Van Why S, Mattson DL. Interleukin-6 inhibition attenuates hypertension and associated renal damage in Dahl salt-sensitive rats. Am J Physiol Renal Physiol 2016;311:F555–F561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Mathis KW, Taylor EB, Ryan MJ. Anti-CD3 antibody therapy attenuates the progression of hypertension in female mice with systemic lupus erythematosus. Pharmacol Res 2017;120:252–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ma F, Feng J, Zhang C, Li Y, Qi G, Li H, Wu Y, Fu Y, Zhao Y, Chen H, Du J, Tang H. The requirement of CD8+ T cells to initiate and augment acute cardiac inflammatory response to high blood pressure. J Immunol 2014;192:3365–3373. [DOI] [PubMed] [Google Scholar]
- 80. Majeed B, Tawinwung S, Eberson LS, Secomb TW, Larmonier N, Larson DF. Interleukin-2/anti-interleukin-2 immune complex expands regulatory T cells and reduces angiotensin II-induced aortic stiffening. Int J Hypertens 2014;2014:126365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Wang H, Hou L, Kwak D, Fassett J, Xu X, Chen A, Chen W, Blazar BR, Xu Y, Hall JL, Ge J-B, Bache RJ, Chen Y. Increasing regulatory T cells with interleukin-2 and interleukin-2 antibody complexes attenuates lung inflammation and heart failure progression. Hypertension 2016;68:114–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Sun X-NN, Li C, Liu YY, Du L-J, Zeng M-RR, Zheng X-JJ, Zhang W-CC, Liu YY, Zhu M, Kong D, Zhou L, Lu L, Shen Z-XX, Yi Y, Du L-J, Qin M, Liu X, Hua Z, Sun S, Yin H, Zhou B, Yu Y, Zhang Z, Duan S-ZZ. T-cell mineralocorticoid receptor controls blood pressure by regulating interferon-gamma. Circ Res 2017;120:1584–1597. [DOI] [PubMed] [Google Scholar]
- 83. Markó L, Kvakan H, Park JK, Qadri F, Spallek B, Binger KJ, Bowman EP, Kleinewietfeld M, Fokuhl V, Dechend R, Müller DN. Interferon-γ signaling inhibition ameliorates angiotensin ii-induced cardiac damage. Hypertension 2012;60:1430–1436. [DOI] [PubMed] [Google Scholar]
- 84. Amador CA, Barrientos V, Peña J, Herrada AA, González M, Valdés S, Carrasco L, Alzamora R, Figueroa F, Kalergis AM, Michea L. Spironolactone decreases DOCA-salt-induced organ damage by blocking the activation of T helper 17 and the downregulation of regulatory T lymphocytes. Hypertension 2014;63:797–803. [DOI] [PubMed] [Google Scholar]
- 85. Chiasson VL, Pakanati AR, Hernandez M, Young KJ, Bounds KR, Mitchell BM. Regulatory T-cell augmentation or interleukin-17 inhibition prevents calcineurin inhibitor-induced hypertension in mice. Hypertension 2017;70:183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Saleh MA, Norlander AE, Madhur MS. Inhibition of interleukin 17-A but not interleukin-17F signaling lowers blood pressure and reduces end-organ inflammation in angiotensin II-induced hypertension. JACC Basic Transl Sci 2016;1:606–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Cornelius DC, Hogg JP, Scott J, Wallace K, Herse F, Moseley J, Wallukat G, Dechend R, LaMarca B. Administration of interleukin-17 soluble receptor C suppresses TH17 cells, oxidative stress, and hypertension in response to placental ischemia during pregnancy. Hypertension 2013;62:1068–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Murphy SR, Dahly-Vernon AJ, Dunn KMJ, Chen CCA, Ledbetter SR, Williams JM, Roman RJ. Renoprotective effects of anti-TGF-β antibody and antihypertensive therapies in Dahl S rats. Am J Physiol Regul Integr Comp Physiol 2012;303:R57–R69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Chan CT, Moore JP, Budzyn K, Guida E, Diep H, Vinh A, Jones ES, Widdop RE, Armitage JA, Sakkal S, Ricardo SD, Sobey CG, Drummond GR. Reversal of vascular macrophage accumulation and hypertension by a CCR2 antagonist in deoxycorticosterone/salt-treated mice. Hypertension 2012;60:1207–1212. [DOI] [PubMed] [Google Scholar]
- 90. Mikolajczyk TP, Nosalski R, Szczepaniak P, Budzyn K, Osmenda G, Skiba D, Sagan A, Wu J, Vinh A, Marvar PJ, Guzik B, Podolec J, Drummond G, Lob HE, Harrison DG, Guzik TJ. Role of chemokine RANTES in the regulation of perivascular inflammation, T-cell accumulation, and vascular dysfunction in hypertension. FASEB J 2016;30:1987–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. De Batista PR, Palacios R, Martín A, Hernanz R, Médici CT, Silva MASC, Rossi EM, Aguado A, Vassallo DV, Salaices M, Alonso MJ. Toll-like receptor 4 upregulation by angiotensin II contributes to hypertension and vascular dysfunction through reactive oxygen species production. PLoS One 2014;9:e104020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Hernanz R, Martínez-Revelles S, Palacios R, Martín A, Cachofeiro V, Aguado A, García-Redondo L, Barrús MT, De Batista PR, Briones AM, Salaices M, Alonso MJ. Toll-like receptor 4 contributes to vascular remodelling and endothelial dysfunction in angiotensin II-induced hypertension. Br J Pharmacol 2015;172:3159–3176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Bomfim GF, Echem C, Martins CB, Costa TJ, Sartoretto SM, Dos Santos RA, Oliveira MA, Akamine EH, Fortes ZB, Tostes RC, Webb RC, Carvalho MHC. Toll-like receptor 4 inhibition reduces vascular inflammation in spontaneously hypertensive rats. Life Sci 2015;122:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Nunes KP, Bomfim GF, Toque HA, Szasz T, Clinton Webb R. Toll-like receptor 4 (TLR4) impairs nitric oxide contributing to Angiotensin II-induced cavernosal dysfunction. Life Sci 2017;191:219–226. [DOI] [PubMed] [Google Scholar]
- 95. Echem C, Bomfim GF, Ceravolo GS, Oliveira MA, Santos-Eichler RA, Bechara LR, Veras MM, Saldiva PHN, Ferreira JC, Akamine EH, Fortes ZB, Dantas AP, de Carvalho MHC. Anti-toll like receptor 4 (TLR4) therapy diminishes cardiac remodeling regardless of changes in blood pressure in spontaneously hypertensive rats (SHR). Int J Cardiol 2015;187:243–245. [DOI] [PubMed] [Google Scholar]
- 96. McCarthy CG, Wenceslau CF, Goulopoulou S, Baban B, Matsumoto T, Webb RC. Chloroquine suppresses the development of hypertension in spontaneously hypertensive rats. Am J Hypertens 2017;30:173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Cornelius DC, Castillo J, Porter J, Amaral LM, Campbell N, Paige A, Thomas AJ, Harmon A, Cunningham MW, Wallace K, Herse F, Wallukat G, Dechend R, LaMarca B. Blockade of CD40 ligand for intercellular communication reduces hypertension, placental oxidative stress, and AT1-AA in response to adoptive transfer of CD4+ T lymphocytes from RUPP rats. Am J Physiol Regul Integr Comp Physiol 2015;309:R1243–R1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Kumar V, Wollner C, Kurth T, Bukowy JD, Cowley AW. Inhibition of mammalian target of rapamycin complex 1 attenuates salt-induced hypertension and kidney injury in Dahl salt-sensitive rats. Hypertension 2017;70:813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Rodríguez-Iturbe B, Quiroz Y, Nava M, Bonet L, Chávez M, Herrera-Acosta J, Johnson RJ, Pons HA. Reduction of renal immune cell infiltration results in blood pressure control in genetically hypertensive rats. Am Jf Physiol Renal Physiol 2002;282:F191–F201. [DOI] [PubMed] [Google Scholar]
- 100. Boesen EI, Williams DL, Pollock JS, Pollock DM. Immunosuppression with mycophenolate mofetil attenuates the development of hypertension and albuminuria in deoxycorticosterone acetate-salt hypertensive rats. Clin Exp Pharmacology Physiol 2010;37:1016–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Taylor EB, Ryan MJ. Immunosuppression with mycophenolate mofetil attenuates hypertension in an experimental model of autoimmune disease. J Am Heart Assoc 2017;6:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Tinsley JH, Chiasson VL, South S, Mahajan A, Mitchell BM. Immunosuppression improves blood pressure and endothelial function in a rat model of pregnancy-induced hypertension. Am J Hypertens 2009;22:1107–1114. [DOI] [PubMed] [Google Scholar]
- 103. Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, Madhur MS, Tomaszewski M, Maffia P, D’Acquisto F, Nicklin SA, Marian AJ, Nosalski R, Murray EC, Guzik B, Berry C, Touyz RM, Kreutz R, Wang DW, Bhella D, Sagliocco O, Crea F, Thomson EC, McInnes IB. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res 2020;116:1666–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Bienvenu LA, Noonan J, Wang X, Peter K. Higher mortality of COVID-19 in males: sex differences in immune response and cardiovascular comorbidities. Cardiovas Res 2020;116:2197–2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Bautista LE, Vera LM, Arenas IA, Gamarra G. Independent association between inflammatory markers (C-reactive protein, interleukin-6, and TNF-α) and essential hypertension. Jf Hum Hypertens 2005;19:149–154. [DOI] [PubMed] [Google Scholar]
- 106. Puszkarska A, Niklas A, Głuszek J, Lipski D, Niklas K. The concentration of tumor necrosis factor in the blood serum and in the urine and selected early organ damages in patients with primary systemic arterial hypertension. Medicine (Baltimore) 2019;98:e15773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Chan SP, Kim HY, Park HJ, Jang SW, Ihm SH, Lee JM, Yoo KD, Jeon DS, Baek SH, Youn HJ, Seung KB, Kim JH, Choi KB. Association between the JNC 7 classification of the stages of systolic hypertension and inflammatory cardiovascular risk factors. Korean Circ J 2007;37:623–662. [Google Scholar]
- 108. Di Napoli M, Papa F. Association between blood pressure and C-reactive protein levels in acute ischemic stroke. Hypertension 2003;42:1117–1123. [DOI] [PubMed] [Google Scholar]
- 109. Ridker PM, MacFadyen JG, Everett BM, Libby P, Thuren T, Glynn RJ, Ridker PM, MacFadyen JG, Everett BM, Libby P, Thuren T, Glynn RJ, Kastelein J, Koenig W, Genest J, Lorenzatti A, Varigos J, Siostrzonek P, Sinnaeve P, Fonseca F, Nicolau J, Gotcheva N, Yong H, Urina-Triana M, Milicic D, Cifkova R, Vettus R, Anker SD, Manolis AJ, Wyss F, Forster T, Sigurdsson A, Pais P, Fucili A, Ogawa H, Shimokawa H, Veze I, Petrauskiene B, Salvador L, Cornel JH, Klemsdal TO, Medina F, Budaj A, Vida-Simiti L, Kobalava Z, Otasevic P, Pella D, Lainscak M, Seung K-B, Commerford P, Dellborg M, Donath M, Hwang J-J, Kultursay H, Flather M, Ballantyne C, Bilazarian S, Chang W, East C, Forgosh L, Harris B, Ligueros M. Relationship of C-reactive protein reduction to cardiovascular event reduction following treatment with canakinumab: a secondary analysis from the CANTOS randomised controlled trial. Lancet 2018;391:319–328. [DOI] [PubMed] [Google Scholar]
- 110. Stuveling EM, Hillege HL, Bakker SJL, Gans ROB, De Jong PE, De Zeeuw D. C-reactive protein is associated with renal function abnormalities in a non-diabetic population. Kidney Int 2003;63:654–661. [DOI] [PubMed] [Google Scholar]
- 111. Sesso HD, Wang L, Buring JE, Ridker PM, Gaziano JM. Comparison of interleukin-6 and C-reactive protein for the risk of developing hypertension in women. Hypertension 2007;49:304–310. [DOI] [PubMed] [Google Scholar]
- 112. Schnabel R, Larson MG, Dupuis J, Lunetta KL, Lipinska I, Meigs JB, Yin X, Rong J, Vita JA, Newton-Cheh C, Levy D, Keaney JF, Vasan RS, Mitchell GF, Benjamin EJ. Relations of inflammatory biomarkers and common genetic variants with arterial stiffness and wave reflection. Hypertension 2008;51:1651–1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Swerdlow DI, Holmes MV, Kuchenbaecker KB, Engmann JEL, Shah T, Sofat R, Guo Y, Chung C, Peasey A, Pfister R, Mooijaart SP, Ireland HA, Leusink M, Langenberg C, Li K, Palmen J, Howard P, Cooper JA, Drenos F, Hardy J, Nalls MA, Li YR, Lowe G, Stewart M, Bielinski SJ, Peto J, Timpson NJ, Gallacher J, Dunlop M, Houlston R. The interleukin-6 receptor as a target for prevention of coronary heart disease: a Mendelian randomisation analysis. Lancet 2012;379:1214–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Cai T, Zhang Y, Ho YL, Link N, Sun J, Huang J, Cai TA, Damrauer S, Ahuja Y, Honerlaw J, Costa L, Schubert P, Hong C, Gagnon D, Sun Y, Sun YV, Gaziano JM, Wilson P, Cho K, Tsao P, O’Donnell CJ, Liao KP, Gaziano MJ, Ramoni R, Breeling J, Chang KM, Huang G, Muralidhar S, Tsao PS, Moser J; VA Million Veteran Program. Association of interleukin 6 receptor variant with cardiovascular disease effects of interleukin 6 receptor blocking therapy: a phenome - Wide association study. JAMA Cardiol 2018;3:849–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Dalekos GN, Elisaf M, Bairaktari E, Tsolas O, Siamopoulos KC. Increased serum levels of interleukin-1β in the systemic circulation of patients with essential hypertension: additional risk factor for atherogenesis in hypertensive patients? J Lab Clin Med 1997;129:300–308. [DOI] [PubMed] [Google Scholar]
- 116. Rabkin SW. The role of interleukin 18 in the pathogenesis of hypertension-induced vascular disease. Nat Clin Pract Cardiovasc Med 2009;6:192–199. [DOI] [PubMed] [Google Scholar]
- 117. Madej A, Okopień B, Kowalski J, Haberka M, Herman ZS. Plasma concentrations of adhesion molecules and chemokines in patients with essential hypertension. Pharmacol Rep 2005;57:878–881. [PubMed] [Google Scholar]
- 118. Carranza-Leon DA, Oeser A, Wu Q, Stein CM, Ormseth MJ, Chung CP. Ambulatory blood pressure in patients with systemic lupus erythematosus: association with markers of immune activation. Lupus 2020;29:1683–1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Siedlinski M, Jozefczuk E, Xu X, Teumer A, Evangelou E, Schnabel RB, Welsh P, Maffia P, Erdmann J, Tomaszewski M, Caulfield MJ, Sattar N, Holmes MV, Guzik TJ. White blood cells and blood pressure: a Mendelian randomization study. Circulation 2020;141:1307–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Tatsukawa Y, Hsu WL, Yamada M, Cologne JB, Suzuki G, Yamamoto H, Yamane K, Akahoshi M, Fujiwara S, Kohno N. White blood cell count, especially neutrophil count, as a predictor of hypertension in a Japanese population. Hypertens Res 2008;31:1391–1397. [DOI] [PubMed] [Google Scholar]
- 121. Liu X, Zhang Q, Wu H, Du H, Liu L, Shi H, Wang C, Xia Y, Guo X, Li C, Bao X, Su Q, Sun S, Wang X, Zhou M, Jia Q, Zhao H, Song K, Niu K. Blood neutrophil to lymphocyte ratio as a predictor of hypertension. Am J Hypertens 2015;28:1339–1346. [DOI] [PubMed] [Google Scholar]
- 122. Belen E, Sungur A, Sungur MA, Erdoğan G. Increased neutrophil to lymphocyte ratio in patients with resistant hypertension. J Clin Hypertens 2015;17:532–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Loperena R, Van Beusecum JP, Itani HA, Engel N, Laroumanie F, Xiao L, Elijovich F, Laffer CL, Gnecco JS, Noonan J, Maffia P, Jasiewicz-Honkisz B, Czesnikiewicz-Guzik M, Mikolajczyk T, Sliwa T, Dikalov S, Weyand CM, Guzik TJ, Harrison DG. Hypertension and increased endothelial mechanical stretch promote monocyte differentiation and activation: roles of STAT3, interleukin 6 and hydrogen peroxide. Cardiovasc Res 2018;114:1547–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Urbanski K, Ludew D, Filip G, Filip M, Sagan A, Szczepaniak P, Grudzien G, Sadowski J, Jasiewicz-Honkisz B, Sliwa T, Kapelak B, McGinnigle E, Mikolajczyk T, Guzik TJ. CD14+CD16++ “nonclassical” monocytes are associated with endothelial dysfunction in patients with coronary artery disease. Thromb Haemost 2017;117:971–980. [DOI] [PubMed] [Google Scholar]
- 125. Mikołajczyk TP, Osmenda G, Batko B, Wilk G, Krezelok M, Skiba D, Sliwa T, Pryjma JR, Guzik TJ. Heterogeneity of peripheral blood monocytes, endothelial dysfunction and subclinical atherosclerosis in patients with systemic lupus erythematosus. Lupus 2016;25:18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Marketou ME, Kontaraki JE, Zacharis EA, Kochiadakis GE, Giaouzaki A, Chlouverakis G, Vardas PE. TLR2 and TLR4 gene expression in peripheral monocytes in nondiabetic hypertensive patients: the effect of intensive blood pressure-lowering. J Clin Hypertens (Greenwich) 2012;14:330–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Itani HA, McMaster WG, Saleh MA, Nazarewicz RR, Mikolajczyk TP, Kaszuba AM, Konior A, Prejbisz A, Januszewicz A, Norlander AE, Chen W, Bonami RH, Marshall AF, Poffenberger G, Weyand CM, Madhur MS, Moore DJ, Harrison DG, Guzik TJ. Activation of human T cells in hypertension: studies of humanized mice and hypertensive humans. Hypertension 2016;68:123–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Youn JC, Yu HT, Lim BJ, Koh MJ, Lee J, Chang DY, Choi YS, Lee SH, Kang SM, Jang Y, Yoo OJ, Shin EC, Park S. Immunosenescent CD8+T clls and C-X-C cemokine receptor type 3 chemokines are increased in human hypertension. Hypertension 2013;62:126–133. [DOI] [PubMed] [Google Scholar]
- 129. Gackowska L, Michałkiewicz J, Niemirska A, Helmin-Basa A, Kłosowski M, Kubiszewska I, Obrycki Ł, Szalecki M, Wierzbicka A, Kułaga Z, Wiese M, Litwin M. Loss of CD31 receptor in CD4+ and CD8+ T-cell subsets in children with primary hypertension is associated with hypertension severity and hypertensive target organ damage. J Hypertens 2018;36:2148–2156. [DOI] [PubMed] [Google Scholar]
- 130. , Litwin M, Kułaga Z. Obesity, metabolic syndrome, and primary hypertension. Pediatr Nephrol 2021;36:825–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Levy D, Ehret GB, Rice K, Verwoert GC, Launer LJ, Dehghan A, Glazer NL, Morrison AC, Johnson AD, Aspelund T, Aulchenko Y, Lumley T, Köttgen A, Vasan RS, Rivadeneira F, Eiriksdottir G, Guo X, Arking DE, Mitchell GF, Mattace-Raso FUS, Smith AV, Taylor K, Scharpf RB, Hwang S-J, Sijbrands EJG, Bis J, Harris TB, Ganesh SK, O'Donnell CJ, Hofman A, Rotter JI, Coresh J, Benjamin EJ, Uitterlinden AG, Heiss G, Fox CS, Witteman JCM, Boerwinkle E, Wang TJ, Gudnason V, Larson MG, Chakravarti A, Psaty BM, van Duijn CM. Genome-wide association study of blood pressure and hypertension. Nat Genet 2009;41:677–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Huan T, Meng Q, Saleh MA, Norlander AE, Joehanes R, Zhu J, Chen BH, Zhang B, Johnson AD, Ying S, Courchesne P, Raghavachari N, Wang R, Liu P, O’Donnell CJ, Vasan R, Munson PJ, Madhur MS, Harrison DG, Yang X, Levy D; International Consortium for Blood Pressure GWAS (ICBP). Integrative network analysis reveals molecular mechanisms of blood pressure regulation. Mol Syst Biol 2015;11:799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Jermendy G, Horváth T, Littvay L, Steinbach R, Jermendy ÁL, Tárnoki ÁD, Tárnoki DL, Métneki J, Osztovits J. Effect of genetic and environmental influences on cardiometabolic risk factors: a twin study. Cardiovas Diabetol 2011;10:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Levy D, DeStefano AL, Larson MG, O'Donnell CJ, Lifton RP, Gavras H, Cupples LA, Myers RH. Evidence for a gene influencing blood pressure on chromosome 17: genome scan linkage results for longitudinal blood pressure phenotypes in subjects from the Framingham Heart Study. Hypertension 2000;36:477–483. [DOI] [PubMed] [Google Scholar]
- 135. Mitchell GF, DeStefano AL, Larson MG, Benjamin EJ, Chen MH, Vasan RS, Vita JA, Levy D. Heritability and a genome-wide linkage scan for arterial stiffness, wave reflection, and mean arterial pressure: the Framingham heart study. Circulation 2005;112:194–199. [DOI] [PubMed] [Google Scholar]
- 136. Rudemiller NP, Lund H, Priestley JRC, Endres BT, Prokop JW, Jacob HJ, Geurts AM, Cohen EP, Mattson DL. Mutation of SH2B3 (LNK), a genome-wide association study candidate for hypertension, attenuates Dahl salt-sensitive hypertension via inflammatory modulation. Hypertension 2015;65:1111–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Devallière J, Charreau B. The adaptor Lnk (SH2B3): an emerging regulator in vascular cells and a link between immune and inflammatory signaling. Biochem Pharmacol 2011;82:1391–1402. [DOI] [PubMed] [Google Scholar]
- 138. Huan T, Esko T, Peters MJ, Pilling LC, Schramm K, Schurmann C, Chen BH, Liu C, Joehanes R, Johnson AD, Yao C, Ying S-X, Courchesne P, Milani L, Raghavachari N, Wang R, Liu P, Reinmaa E, Dehghan A, Hofman A, Uitterlinden AG, Hernandez DG, Bandinelli S, Singleton A, Melzer D, Metspalu A, Carstensen M, Grallert H, Herder C, Meitinger T, Peters A, Roden M, Waldenberger M, Dörr M, Felix SB, Zeller T, Vasan R, O’Donnell CJ, Munson PJ, Yang X, Prokisch H, Völker U, van Meurs JBJ, Ferrucci L, Levy D; International Consortium for Blood Pressure GWAS (ICBP). A meta-analysis of gene expression signatures of blood pressure and hypertension. PLOS Genet 2015;11:e1005035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. McMaster W, Saleh M, Kirabo A, Itani H, Harrison D, Madhur M. Deficiency of LNK/SH2B3 promotes hypertension, endothelial dysfunction, and aortic dissection. Angiogenesis 2014;17:935–984. [Google Scholar]
- 140. Saleh MA, McMaster WG, Wu J, Norlander AE, Funt SA, Thabet SR, Kirabo A, Xiao L, Chen W, Itani HA, Michell D, Huan T, Zhang Y, Takaki S, Titze J, Levy D, Harrison DG, Madhur MS. Lymphocyte adaptor protein LNK deficiency exacerbates hypertension and end-organ inflammation. J Clin Invest 2015;125:1189–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Eales JM, Jiang X, Xu X, Saluja S, Akbarov A, Cano-Gamez E, McNulty MT, Finan C, Guo H, Wystrychowski W, Szulinska M, Thomas HB, Pramanik S, Chopade S, Prestes PR, Wise I, Evangelou E, Salehi M, Shakanti Y, Ekholm M, Denniff M, Nazgiewicz A, Eichinger F, Godfrey B, Antczak A, Glyda M, Król R, Eyre S, Brown J, Berzuini C, Bowes J, Caulfield M, Zukowska-Szczechowska E, Zywiec J, Bogdanski P, Kretzler M, Woolf AS, Talavera D, Keavney B, Maffia P, Guzik TJ, O'Keefe RT, Trynka G, Samani NJ, Hingorani A, Sampson MG, Morris AP, Charchar FJ, Tomaszewski M. Uncovering genetic mechanisms of hypertension through multi-omic analysis of the kidney. Nat Genet 2021;53:630–637. [DOI] [PubMed] [Google Scholar]
- 142. Gonzalez-Juanatey C, Vazquez-Rodriguez TR, Miranda-Filloy JA, Gomez-Acebo I, Testa A, Garcia-Porrua C, Sanchez-Andrade A, Llorca J, Gonzlez-Gay MA, González-Gay MA, Gonzlez-Gay MA. Anti-TNF-alpha-adalimumab therapy is associated with persistent improvement of endothelial function without progression of carotid intima-media wall thickness in patients with rheumatoid arthritis refractory to conventional therapy. Mediators Inflamm 2012;2012:674265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Bozkirli EDE, Bozkirli E, Yucel AE. Effects of infliximab treatment in terms of cardiovascular risk and insulin resistance in ankylosing spondylitis patients. Mod Rheumatol 2014;24:335–339. [DOI] [PubMed] [Google Scholar]
- 144. Komai N, Morita Y, Sakuta T, Kuwabara A, Kashihara N. Anti-tumor necrosis factor therapy increases serum adiponectin levels with the improvement of endothelial dysfunction in patients with rheumatoid arthritis. Mod Rheumatol 2007;17:385–390. [DOI] [PubMed] [Google Scholar]
- 145. Sandoo A, Panoulas VF, Toms TE, Smith JP, Stavropoulos-Kalinoglou A, Metsios GS, Gasparyan AY, Carroll D, Veldhuijzen Van Zanten JJCS, Kitas GD. Anti-TNFα therapy may lead to blood pressure reductions through improved endothelium-dependent microvascular function in patients with rheumatoid arthritis. J Hum Hypertens 2011;25:699–702. [DOI] [PubMed] [Google Scholar]
- 146. Yoshida S, Takeuchi T, Kotani T, Yamamoto N, Hata K, Nagai K, Shoda T, Takai S, Makino S, Hanafusa T. Infliximab, a TNF-α inhibitor, reduces 24-h ambulatory blood pressure in rheumatoid arthritis patients. J Hum Hypertens 2014;28:165–169. [DOI] [PubMed] [Google Scholar]
- 147. Galarraga B, Khan F, Kumar P, Pullar T, Belch JJF. Etanercept improves inflammation-associated arterial stiffness in rheumatoid arthritis. Rheumatology (Oxford) 2009;48:1418–1423. [DOI] [PubMed] [Google Scholar]
- 148. Klarenbeek NB, Van Der Kooij SM, Huizinga TJW, Goekoop-Ruiterman YPM, Hulsmans HMJ, Van Krugten MV, Speyer I, De Vries-Bouwstra JK, Kerstens PJSM, Huizinga TWJ, Dijkmans BAC, Allaart CF. Blood pressure changes in patients with recent-onset rheumatoid arthritis treated with four different treatment strategies: a post hoc analysis from the BeSt trial. Ann Rheum Dis 2010;69:1342–1335. [DOI] [PubMed] [Google Scholar]
- 149. Tam LS, Shang Q, Li EK, Wang S, Li RJ, Lee KL, Leung YY, Ying KY, Yim CW, Kun EW, Leung MH, Li M, Li TK, Zhu TY, Chui RK, Tseung L, Yu SL, Kuan WP, Yu CM. Infliximab is associated with improvement in arterial stiffness in patients with early rheumatoid arthritis – a randomized trial. J Rheumatol 2012;39:2267–2275. [DOI] [PubMed] [Google Scholar]
- 150. Daïen CI, Fesler P, Du Cailar G, Daïen V, Mura T, Dupuy AM, Cristol JP, Ribstein J, Combe B, Morel J. Etanercept normalises left ventricular mass in patients with rheumatoid arthritis. Ann Rheum Dis 2013;72:881–887. [DOI] [PubMed] [Google Scholar]
- 151. van den Oever IAM, Baniaamam M, Simsek S, Raterman HG, van Denderen JC, van Eijk IC, Peters MJL, van der Horst-Bruinsma IE, Smulders YM, Nurmohamed MT. The effect of anti-TNF treatment on body composition and insulin resistance in patients with rheumatoid arthritis. Rheumatol Int 2021;41:319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Peters MJL, Welsh P, McInnes IB, Wolbink G, Dijkmans BAC, Sattar N, Nurmohamed MT. Tumour necrosis factor α blockade reduces circulating N-terminal pro-brain natriuretic peptide levels in patients with active rheumatoid arthritis: results from a prospective cohort study. Ann Rheum Dis 2010;69:1281–1285. [DOI] [PubMed] [Google Scholar]
- 153. Mäki-Petäjä KM, Hall FC, Booth AD, Wallace SML, Yasmin, Bearcroft PWP, Harish S, Furlong A, McEniery CM, Brown J, Wilkinson IB. Rheumatoid arthritis is associated with increased aortic pulse-wave velocity, which is reduced by anti-tumor necrosis factor-α therapy. Circulation 2006;114:1185–1192. [DOI] [PubMed] [Google Scholar]
- 154. Rho YH, Oeser A, Chung CP, Milne GL, Stein CM. Drugs used in the treatment of rheumatoid arthritis: relationship between current use and cardiovascular risk factors. Arch Drug Inf 2009;2:34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Angel K, Provan SA, Hammer HB, Mowinckel P, Kvien TK, Atar D. Changes in arterial stiffness during continued infliximab treatment in patients with inflammatory arthropathies. Fundam Clin Pharmacol 2011;25:511–517. [DOI] [PubMed] [Google Scholar]
- 156. Thaci D, Girolomoni G, Philipp S, Qureshi A, You R, Fox T. Secukinumab treatment does not induce blood pressure change in subjects with moderate to severe plaque psoriasis: results from the FIXTURE study. J Am Acad Dermatol 2016;74:AB273. [Google Scholar]
- 157. Baker JF, Sauer B, Teng CC, George M, Cannon GW, Ibrahim S, Cannella A, England BR, Michaud K, Caplan L, Davis LA, O’Dell J, Mikuls TR. Initiation of disease-modifying therapies in rheumatoid arthritis is associated with changes in blood pressure. J Clin Rheumatol 2018;24:203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Mäki-Petäjä KM, Elkhawad M, Cheriyan J, Joshi FR, Östör AJK, Hall FC, Rudd JHF, Wilkinson IB. Anti-tumor necrosis factor-α therapy reduces aortic inflammation and stiffness in patients with rheumatoid arthritis. Circulation 2012;126:2473–2480. [DOI] [PubMed] [Google Scholar]
- 159. Tam L-SS, Shang Q, Kun EW, Lee K-LL, Yip M-LL, Li M, Li TK, Zhu TY, Pui MO, Li EK, Yu C-MM. The effects of golimumab on subclinical atherosclerosis and arterial stiffness in ankylosing spondylitis-a randomized, placebo-controlled pilot trial. Rheumatology (Oxford) 2014;53:1065–1074. [DOI] [PubMed] [Google Scholar]
- 160. Grossman C, Bornstein G, Leibowitz A, Ben-Zvi I, Grossman E. Effect of tumor necrosis factor-α inhibitors on ambulatory 24-h blood pressure. Blood Pressure 2017;26:24–29. [DOI] [PubMed] [Google Scholar]
- 161. Van Doornum S, McColl G, Wicks IP. Tumour necrosis factor antagonists improve disease activity but not arterial stiffness in rheumatoid arthritis. Rheumatology (Oxford) 2005;44:1428–1432. [DOI] [PubMed] [Google Scholar]
- 162. Angel K, Provan SA, Gulseth HL, Mowinckel P, Kvien TK, Atar D. Tumor necrosis factor-α antagonists improve aortic stiffness in patients with inflammatory arthropathies: a controlled study. Hypertension 2010;55:333–338. [DOI] [PubMed] [Google Scholar]
- 163. Desai RJ, Solomon DH, Schneeweiss S, Danaei G, Liao KP, Kim SC. Tumor necrosis factor-α inhibitor use and the risk of incident hypertension in patients with rheumatoid arthritis. Epidemiology 2016;27:414–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Kim SK, Kwak SG, Choe JY. Association between biologic disease modifying anti-rheumatic drugs and incident hypertension in patients with rheumatoid arthritis: results from prospective nationwide KOBIO Registry. Medicine (Baltimore) 2020;99:e19415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zhao Q, Hong D, Zhang Y, Sang Y, Yang Z, Zhang X. Association between anti-TNF therapy for rheumatoid arthritis and hypertension: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 2015;94:e731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Everett BM, Cornel JH, Lainscak M, Anker SD, Abbate A, Thuren T, Libby P, Glynn RJ, Ridker PM. Anti-inflammatory therapy with canakinumab for the prevention of hospitalization for heart failure. Circulation 2019;139:1289–1299. [DOI] [PubMed] [Google Scholar]
- 167. Rothman AMK, MacFadyen J, Thuren T, Webb A, Harrison DG, Guzik TJ, Libby P, Glynn RJ, Ridker PM. Effects of interleukin-1β inhibition on blood pressure, incident hypertension, and residual inflammatory risk: a secondary analysis of CANTOS. Hypertension 2020;75:477–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Makavos G, Ikonomidis I, Andreadou I, Varoudi M, Kapniari I, Loukeri E, Theodoropoulos K, Pavlidis G, Triantafyllidi H, Thymis J, Parissis J, Tsoumani M, Rafouli-Stergiou P, Katsimbri P, Papadavid E. Effects of interleukin 17A inhibition on myocardial deformation and vascular function in psoriasis. Can J Cardiol 2020;36:100–111. [DOI] [PubMed] [Google Scholar]
- 169. Takeshita J, Wang S, Shin DB, Mehta NN, Kimmel SE, Margolis DJ, Troxel AB, Gelfand JM. Effect of psoriasis severity on hypertension control a population-based study in the United Kingdom. JAMA Dermatol 2015;151:161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Ogdie A, Yu Y, Haynes K, Love TJ, Maliha S, Jiang Y, Troxel AB, Hennessy S, Kimmel SE, Margolis DJ, Choi H, Mehta NN, Gelfand JM. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis 2015;74:326–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Elmedany SH, Mohamed AE, Galil SMA. Efficacy and safety profile of intravenous tocilizumab versus intravenous abatacept in treating female Saudi Arabian patients with active moderate-to-severe rheumatoid arthritis. Clin Rheumatol 2019;38:2109–2117. [DOI] [PubMed] [Google Scholar]
- 172. McInnes IB, Thompson L, Giles JT, Bathon JM, Salmon JE, Beaulieu AD, Codding CE, Carlson TH, Delles C, Lee JS, Sattar N. Effect of interleukin-6 receptor blockade on surrogates of vascular risk in rheumatoid arthritis: MEASURE, a randomised, placebo-controlled study. Ann Rheum Dis 2015;74:694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Provan SA, Berg IJ, Hammer HB, Mathiessen A, Kvien TK, Semb AG. The impact of newer biological disease modifying anti-rheumatic drugs on cardiovascular risk factors: a 12-month longitudinal study in rheumatoid arthritis patients treated with rituximab, abatacept and tociliziumab. PLoS One 2015;10:e0130709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Herrera J, Ferrebuz A, MacGregor EG, Rodriguez-Iturbe B. Mycophenolate mofetil treatment improves hypertension in patients with psoriasis and rheumatoid arthritis. J Am Soc Nephrol 2006;17:S218–S225. [DOI] [PubMed] [Google Scholar]
- 175. Frisch G, Lin J, Rosenstock J, Markowitz G, Agati VD’, Radhakrishnan J, Preddie D, Crew J, Valeri A, Appel G. Mycophenolate mofetil (MMF) vs placebo in patients with moderately advanced IgA nephropathy: a double-blind randomized controlled trial. Nephrol Dial Transplant 2005;20:2139–2145. [DOI] [PubMed] [Google Scholar]
- 176. Liu X, Dewei D, Sun S, Xu G, Liu H, He L, Zhang P. Treatment of severe IgA nephropathy: mycophenolate mofetil/prednisone compared to cyclophosphamide/prednisone. Int J Clin Pharmacol Ther 2014;52:95–102. [DOI] [PubMed] [Google Scholar]
- 177. Tang SCW, Tang AWC, Wong SSH, Leung JCK, Ho YW, Lai KN. Long-term study of mycophenolate mofetil treatment in IgA nephropathy. Kidney Int 2010;77:543–549. [DOI] [PubMed] [Google Scholar]
- 178. Maes BD, Oyen R, Claes K, Evenepoel P, Kuypers D, Vanwalleghem J, Damme B, Van C, Vanrenterghem YF, Vanrenterghem YFC. Mycophenolate mofetil in IgA nephropathy: results of a 3-year prospective placebo-controlled randomized study. Kidney Int 2004;65:1842–1849. [DOI] [PubMed] [Google Scholar]
- 179. Gonwa T, Mendez R, Yang HC, Weinstein S, Jensik S, Steinberg S. Randomized trial of tacrolimus in combination with sirolimus or mycophenolate mofetil in kidney transplantation: results at 6 months. Transplantation 2003;1213–1220. [DOI] [PubMed] [Google Scholar]
- 180. Cuervas-Mons V, Herrero JI, Gomez MA, González-Pinto I, Serrano T, de la Mata M, Fabregat J, Gastaca M, Bilbao I, Varo E, Sánchez-Antolín G, Rodrigo J, Espinosa MD. Impact of tacrolimus and mycophenolate mofetil regimen vs. a conventional therapy with steroids on cardiovascular risk in liver transplant patients. Clin Transplant 2015;29:667–677. [DOI] [PubMed] [Google Scholar]
- 181. Mangoni AA, Baghdadi LR, Shanahan EM, Wiese MD, Tommasi S, Elliot D, Woodman RJ. Methotrexate, blood pressure and markers of arterial function in patients with rheumatoid arthritis: a repeated cross-sectional study. Ther Adv Musculoskelet Dis 2017;9:213–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Gyldenløve M, Jensen P, Løvendorf MB, Zachariae C, Hansen PR, Skov L. Short-term treatment with methotrexate does not affect microvascular endothelial function in patients with psoriasis. J Eur Acad Dermatol Venereol 2015;29:591–594. [DOI] [PubMed] [Google Scholar]
- 183. Ridker PM, Everett BM, Pradhan A, MacFadyen JG, Solomon DH, Zaharris E, Mam V, Hasan A, Rosenberg Y, Iturriaga E, Gupta M, Tsigoulis M, Verma S, Clearfield M, Libby P, Goldhaber SZ, Seagle R, Ofori C, Saklayen M, Butman S, Singh N, Le May M, Bertrand O, Johnston J, Paynter NP, Glynn RJ; CIRT Investigators. Low-dose methotrexate for the prevention of atherosclerotic events. N Engl J Med 2019;380:752–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Gao R, Wu W, Wen Y, Li X. Hydroxychloroquine alleviates persistent proteinuria in IgA nephropathy. Int Urol Nephrol 2017;49:1233–1241. [DOI] [PubMed] [Google Scholar]
- 185. Sacre K, Criswell LA, McCune JM. Hydroxychloroquine is associated with impaired interferon-alpha and tumor necrosis factor-alpha production by plasmacytoid dendritic cells in systemic lupus erythematosus. Arthritis Res Ther 2012;14:R155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Rozman B, Praprotnik S, Logar D, Tomšič M, Hojnik M, Kos-Golja M, Accetto R, Dolenc P. Leflunomide and hypertension. Ann Rheum Dis 2002;61:567–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Hoorn EJ, Walsh SB, McCormick JA, Fürstenberg A, Yang CL, Roeschel T, Paliege A, Howie AJ, Conley J, Bachmann S, Unwin RJ, Ellison DH. The calcineurin inhibitor tacrolimus activates the renal sodium chloride cotransporter to cause hypertension. Nat Med 2011;17:1304–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Hošková L, Málek I, Kopkan L, Kautzner J. Pathophysiological mechanisms of calcineurin inhibitor-induced nephrotoxicity and arterial hypertension. Physiol Res 2017;66:167–180. [DOI] [PubMed] [Google Scholar]
- 189. Andreassen AK, Broch K, Eiskjær H, Karason K, Gude E, Mølbak D, Stueflotten W, Gullestad L; SCHEDULE (SCandinavian HEart transplant everolimus De-novo stUdy with earLy calcineurin inhibitors avoidancE) Investigators. Blood pressure in de novo heart transplant recipients treated with everolimus compared with a cyclosporine-based regimen. Transplantation 2019;103:781–788. [DOI] [PubMed] [Google Scholar]
- 190. Murbraech K, Massey R, Undset LH, Midtvedt K, Holdaas H, Aakhus S. Cardiac response to early conversion from calcineurin inhibitor to everolimus in renal transplant recipients - a three-yr serial echocardiographic substudy of the randomized controlled CENTRAL trial. Clin Transplant 2015;29:678–684. [DOI] [PubMed] [Google Scholar]
- 191. Claes K, Meier-Kriesche HU, Schold JD, Vanrenterghem Y, Halloran PF, Ekberg H. Effect of different immunosuppressive regimens on the evolution of distinct metabolic parameters: evidence from the Symphony study. Nephrol Dial Transplant 2012;27:850–857. [DOI] [PubMed] [Google Scholar]
- 192. van Dijk M, van Roon AM, Said MY, Bemelman FJ, Homan van der Heide JJ, de Fijter HW, de Vries APJ, Bakker SJL, Sanders JSF. Long-term cardiovascular outcome of renal transplant recipients after early conversion to everolimus compared to calcineurin inhibition: results from the randomized controlled MECANO trial. Transpl Int 2018;31:1380–1390. [DOI] [PubMed] [Google Scholar]
- 193. Chamienia A, Biedunkiewicz B, Król E, Dębska-Ślizień A, Rutkowski B. One-year observation of kidney allograft recipients converted from cyclosporine microemulsion to tacrolimus. Transplant Proc 2006;38:81–85. [DOI] [PubMed] [Google Scholar]
- 194. Rostaing L, Sánchez-Fructuoso A, Franco A, Glyda M, Kuypers DR, Jaray J. Conversion to tacrolimus once-daily from ciclosporin in stable kidney transplant recipients: a multicenter study. Transpl Int 2012;25:391–400. [DOI] [PubMed] [Google Scholar]
- 195. Larson TS, Dean PG, Stegall MD, Griffin MD, Textor SC, Schwab TR, Gloor JM, Cosio FG, Lund WJ, Kremers WK, Nyberg SL, Ishitani MB, Prieto M, Velosa JA. Complete avoidance of calcineurin inhibitors in renal transplantation: a randomized trial comparing sirolimus and tacrolimus. Am J Transplant 2006;6:514–522. [DOI] [PubMed] [Google Scholar]
- 196. de Fijter JW, Holdaas H, Øyen O, Sanders JS, Sundar S, Bemelman FJ, Sommerer C, Pascual J, Avihingsanon Y, Pongskul C, Oppenheimer F, Toselli L, Russ G, Wang Z, Lopez P, Kochuparampil J, Cruzado JM, van der Giet M, Gaite LE, Lopez VF, Maldonado R, Massari P, Novoa P, Palti G, Chadban S, Kanellis J, Masterson R, Oberbauer R, Saemann M, Kuypers D; the ELEVATE Study Group. Early conversion from calcineurin inhibitor- to everolimus-based therapy following kidney transplantation: results of the randomized ELEVATE trial. Am J Transplant 2017;17:1853–1867. [DOI] [PubMed] [Google Scholar]
- 197. Ursini F, Russo E, Hribal ML, Mauro D, Savarino F, Bruno C, Tripolino C, Rubino M, Naty S, Grembiale RD. Abatacept improves whole-body insulin sensitivity in rheumatoid arthritis: an observational study. Medicine (Baltimore ) 2015;94:e888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Kume K, Yamada S, Kanazawa T, Hatta K, Amano K. Abatacept does not improve subclinical atherosclerosis despite good response in rheumatoid arthritis: a cohort study. Arthritis Rheumatology 2015:1–4046. [Google Scholar]
- 199. Mathieu S, Couderc M, Glace B, Pereira B, Tournadre A, Dubost JJ, Soubrier M. Effects of 6 months of abatacept treatment on aortic stiffness in patients with rheumatoid arthritis. Biologics 2013;7:259–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Iasella CJ, Winstead RJ, Moore CA, Johnson BA, Feinberg AT, Morrell MR, Hayanga JWA, Lendermon EA, Zeevi A, McDyer JF, Ensor CR. Maintenance belatacept-based immunosuppression in lung transplantation recipients who failed calcineurin inhibitors. Transplantation 2018;102:171–177. [DOI] [PubMed] [Google Scholar]
- 201. Malvezzi P, Fischman C, Rigault G, Jacob MC, Raskovalova T, Jouve T, Janbon B, Rostaing L, Cravedi P. Switching renal transplant recipients to belatacept therapy: results of a real-life gradual conversion protocol. Transpl Immunol 2019;56:101207–101177. [DOI] [PubMed] [Google Scholar]
- 202. Seibert FS, Steltzer J, Melilli E, Grannas G, Pagonas N, Bauer F, Zidek W, Grinyó J, Westhoff TH. Differential impact of belatacept and cyclosporine A on central aortic blood pressure and arterial stiffness after renal transplantation. Clin Transplant 2014;28:1004–1009. [DOI] [PubMed] [Google Scholar]
- 203. Rostaing L, Massari P, Garcia VD, Mancilla-Urrea E, Nainan G, Rial MDC, Steinberg S, Vincenti F, Shi R, Di Russo G, Thomas D, Grinyó J. Switching from calcineurin inhibitor-based regimens to a belatacept-based regimen in renal transplant recipients: a randomized phase II study. Clin J Am Soc Nephrol 2011;6:430–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Durrbach A, Pestana JM, Pearson T, Vincenti F, Garcia VD, Campistol J, Del Carmen Rial M, Florman S, Block A, Di Russo G, Xing J, Garg P, Grinyó J. A phase III study of belatacept versus cyclosporine in kidney transplants from extended criteria donors (BENEFIT-EXT Study). Am J Transplant 2010;10:547–557. [DOI] [PubMed] [Google Scholar]
- 205. Vincenti F, Charpentier B, Vanrenterghem Y, Rostaing L, Bresnahan B, Darji P, Massari P, Mondragon-Ramirez GA, Agarwal M, Di Russo G, Lin C-S, Garg P, Larsen CP. A phase III study of belatacept-based immunosuppression regimens versus cyclosporine in renal transplant recipients (BENEFIT study). Am J Transplant 2010;10:535–546. [DOI] [PubMed] [Google Scholar]
- 206. Ferguson R, Grinyó J, Vincenti F, Kaufman DB, Woodle ES, Marder BA, Citterio F, Marks WH, Agarwal M, Wu D, Dong Y, Garg P. Immunosuppression with belatacept-based, corticosteroid-avoiding regimens in de novo kidney transplant recipients. Am J Transplant 2011;11:66–76. [DOI] [PubMed] [Google Scholar]
- 207. Novikova DS, Popkova TV, Lukina GV, Luchikhina EL, Karateev DE, Volkov AV, Novikov AA, Aleksandrova EN, Nasonov EL. The effects of rituximab on lipids, arterial stiffness, and carotid intima-media thickness in rheumatoid arthritis. J Korean Med Sci 2016;31:202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Mathieu S, Pereira B, Dubost JJ, Lusson JR, Soubrier M. No significant change in arterial stiffness in RA after 6 months and 1 year of rituximab treatment. Rheumatology (Oxford) 2012;51:1107–1111. [DOI] [PubMed] [Google Scholar]
- 209. Remuzzi G, Chiurchiu C, Abbate M, Brusegan V, Bontempelli M, Ruggenenti P. Rituximab for idiopathic membranous nephropathy. Lancet 2002;360:923–924. [DOI] [PubMed] [Google Scholar]
- 210. Runlin G, Junren Z, Guozhang L, Weizhong Z, Tingjie Z, Ningling S, Landen H. Efficacy and safety of nifedipine GITS in Asians with hypertension: results of a post-marketing surveillance study in China. Clin Drug Investig 2007;27:565–572. [DOI] [PubMed] [Google Scholar]
- 211. Hu H, Zhang J, Wang Y, Tian Z, Liu D, Zhang G, Gu G, Zheng H, Xie R, Cui W. Impact of baseline blood pressure on the magnitude of blood pressure lowering by nifedipine gastrointestinal therapeutic system: refreshing the Wilder’s principle. Drug Des Devel Ther 2017;11:3179–3186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Ueng KC, Ningling S, El Maksod A, Hung KY, Yuehui Y. Efficacy and tolerability of long-acting nifedipine GITSOROS monotherapy or combination therapy in hypertensive patients: results of a 12-week international, prospective, multicentre, observational study. Clinical Drug Investig 2011;31:631–642. [DOI] [PubMed] [Google Scholar]
- 213. Czesnikiewicz-Guzik M, Nosalski R, Mikolajczyk TP, Vidler F, Dohnal T, Dembowska E, Graham D, Harrison DG, Guzik TJ. Th1-type immune responses to Porphyromonas gingivalis antigens exacerbate angiotensin II-dependent hypertension and vascular dysfunction. Br J Pharmacol 2019;176:1922–1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Czesnikiewicz-Guzik M, Osmenda G, Siedlinski M, Nosalski R, Pelka P, Nowakowski D, Wilk G, Mikolajczyk TP, Schramm-Luc A, Furtak A, Matusik P, Koziol J, Drozdz M, Munoz-Aguilera E, Tomaszewski M, Evangelou E, Caulfield M, Grodzicki T, D'Aiuto F, Guzik TJ. Causal association between periodontitis and hypertension: evidence from Mendelian randomization and a randomized controlled trial of non-surgical periodontal therapy. Eur Heart J 2019;40:3459–3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Martin-Cabezas R, Seelam N, Petit C, Agossa K, Gaertner S, Tenenbaum H, Davideau JL, Huck O. Association between periodontitis and arterial hypertension: a systematic review and meta-analysis. Am Heart J 2016;180:98–112. [DOI] [PubMed] [Google Scholar]
- 216. Muñoz Aguilera E, Suvan J, Buti J, Czesnikiewicz-Guzik M, Barbosa Ribeiro A, Orlandi M, Guzik TJ, Hingorani AD, Nart J, D’Aiuto F. Periodontitis is associated with hypertension: a systematic review and meta-analysis. Cardiovasc Res 2020;116:28–39. [DOI] [PubMed] [Google Scholar]
- 217. Pietropaoli D, Del Pinto R, Ferri C, Wright JT, Giannoni M, Ortu E, Monaco A. Poor oral health and blood pressure control among US hypertensive adults. Hypertension 2018;72:1365–1373. [DOI] [PubMed] [Google Scholar]
- 218. Ahn YB, Shin MS, Byun JS, Kim HD. The association of hypertension with periodontitis is highlighted in female adults: results from the Fourth Korea National Health and Nutrition Examination Survey. J Clin Periodontol 2015;42:998–1005. [DOI] [PubMed] [Google Scholar]
- 219. Tonetti MS, D'Aiuto F, Nibali L, Donald A, Storry C, Parkar M, Suvan J, Hingorani AD, Vallance P, Deanfield J. Treatment of periodontitis and endothelial function. N Engl J Med 2007;356:911–920. [DOI] [PubMed] [Google Scholar]
- 220.Vidal F, Cordovil I, Figueredo CMS, Fischer RG. Non-surgical periodontal treatment reduces cardiovascular risk in refractory hypertensive patients: a pilot study. J Clin Periodontol 2013;40:681–687. [DOI] [PubMed] [Google Scholar]
- 221. Sharma S, Sridhar S, Mcintosh A, Messow C-M, Aguilera EM, del Pinto R, Pietropaoli D, Górska R, Siedlinski M, Maffia P, Tomaszewski M, Guzik TJ, D’aiuto F, Czesnikiewicz-Guzik M. Periodontal therapy and treatment of hypertension – alternative to the pharmacological approach. A systematic review and meta-analysis. Pharmacol Res 2021;166:e105511. [DOI] [PubMed] [Google Scholar]
- 222. Herrod PJJ, Doleman B, Blackwell JEM, O’Boyle F, Williams JP, Lund JN, Phillips BE. Exercise and other nonpharmacological strategies to reduce blood pressure in older adults: a systematic review and meta-analysis. J Am Soc Hypertens 2018;12:248–267. [DOI] [PubMed] [Google Scholar]
- 223. Valdiglesias V, Sánchez-Flores M, Maseda A, Lorenzo-López L, Marcos-Pérez D, López-Cortón A, Strasser B, Fuchs D, Laffon B, Millán-Calenti JC, Pásaro E. Immune biomarkers in older adults: role of physical activity. J Toxicol Environ Health A 2017;80:605–620. [DOI] [PubMed] [Google Scholar]
- 224. Sagiv M, Ben-Sira D, Goldhammer E. Beta-blockers, exercise, and the immune system in men with coronary artery disease. Med Sci Sports Exerc 2002;34:587–591. [DOI] [PubMed] [Google Scholar]
- 225. Kohut ML, Arntson BA, Lee W, Rozeboom K, Yoon KJ, Cunnick JE, McElhaney J. Moderate exercise improves antibody response to influenza immunization in older adults. Vaccine 2004;22:2298–2306. [DOI] [PubMed] [Google Scholar]
- 226. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N, Simons-Morton D, McCullough M, Swain J, Steele P, Evans MA, Miller ER, Harsha DW. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–1124. [DOI] [PubMed] [Google Scholar]
- 227. Moore TJ, Vollmer WM, Appel LJ, Sacks FM, Svetkey LP, Vogt TM, Conlin PR, Simons-Morton DG, Carter-Edwards L, Harsha DW. Effect of dietary patterns on ambulatory blood pressure: results from the dietary approaches to Stop Hypertension (DASH) Trial. Hypertension 1999;34:472–474. [DOI] [PubMed] [Google Scholar]
- 228. Meli AC. When immune cells are coached by intestinal microbiota. Cardiovasc Res 2020;116:e21–e22. [DOI] [PubMed] [Google Scholar]
- 229. Yan Q, Gu Y, Li X, Yang W, Jia L, Chen C, Han X, Huang Y, Zhao L, Li P, Fang Z, Zhou J, Guan X, Ding Y, Wang S, Khan M, Xin Y, Li S, Ma Y. Alterations of the gut microbiome in hypertension. Front Cell Infect Microbiol 2017;24:381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. De Filippis F, Pellegrini N, Vannini L, Jeffery IB, La Storia A, Laghi L, Serrazanetti DI, Di Cagno R, Ferrocino I, Lazzi C, Turroni S, Cocolin L, Brigidi P, Neviani E, Gobbetti M, O’Toole PW, Ercolini D. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 2016;65:1812–1821. [DOI] [PubMed] [Google Scholar]
- 231. He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev 2013:CD004937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Zhou X, Zhang L, Ji WJ, Yuan F, Guo ZZ, Pang B, Luo T, Liu X, Zhang WC, Jiang TM, Zhang Z, Li YM. Variation in dietary salt intake induces coordinated dynamics of monocyte subsets and monocyte-platelet aggregates in humans: implications in end organ inflammation. PLoS One 2013;8:e60332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. De Miguel C, Das S, Lund H, Mattson DL. T lymphocytes mediate hypertension and kidney damage in Dahl salt-sensitive rats. Am J Physiol Regul Integr Comp Physiol 2010;298:R1136–R1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Marketou ME, Maragkoudakis S, Anastasiou I, Nakou H, Plataki M, Vardas PE, Parthenakis FI. Salt-induced effects on microvascular function: a critical factor in hypertension mediated organ damage. J Clin Hypertens (Greenwich) 2019;21:749–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Yi B, Titze J, Rykova M, Feuerecker M, Vassilieva G, Nichiporuk I, Schelling G, Morukov B, Choukèr A. Effects of dietary salt levels on monocytic cells and immune responses in healthy human subjects: a longitudinal study. Transl Res 2015;166:103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236. Crouch SH, Botha-Le Roux S, Delles C, Graham LA, Schutte AE. Inflammation and salt in young adults: the African-PREDICT study. Eur J Nutr 2021;60:873–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Lob HE, Marvar PJ, Guzik TJ, Sharma S, McCann LA, Weyand C, Gordon FJ, Harrison DG. Induction of hypertension and peripheral inflammation by reduction of extracellular superoxide dismutase in the central nervous system. Hypertension 2010;55:277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238. Marvar PJ, Thabet SR, Guzik TJ, Lob HE, McCann LA, Weyand C, Gordon FJ, Harrison DG. Central and peripheral mechanisms of T-lymphocyte activation and vascular inflammation produced by angiotensin II-induced hypertension. Circ Res 2010;107:263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Ong J, Kinsman BJ, Sved AF, Rush BM, Tan RJ, Carattino MD, Stocker SD. Renal sensory nerves increase sympathetic nerve activity and blood pressure in 2-kidney 1-clip hypertensive mice. J Neurophysiol 2019;122:358–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. Xiao L, Kirabo A, Wu J, Saleh MA, Zhu L, Wang F, Takahashi T, Loperena R, Foss JD, Mernaugh RL, Chen W, Roberts J, Osborn JW, Itani HA, Harrison DG. Renal denervation prevents immune cell activation and renal inflammation in angiotensin II-induced hypertension. Circ Res 2015;117:547–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241. Hart EC, Mcbryde FD, Burchell AE, Ratcliffe LEK, Stewart LQ, Baumbach A, Nightingale A, Paton JFR. Translational examination of changes in baroreflex function after renal denervation in hypertensive rats and humans. Hypertension 2013;62:533–541. [DOI] [PubMed] [Google Scholar]
- 242. Banek CT, Gauthier MM, Baumann DC, Van Helden D, Asirvatham-Jeyaraj N, Panoskaltsis-Mortari A, Fink GD, Osborn JW. Targeted afferent renal denervation reduces arterial pressure but not renal inflammation in established DOCA-salt hypertension in the rat. Am J Physiol Regul Integr Comp Physiol 2018;314:R883–R891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. Banek CT, Gauthier MM, Van Helden DA, Fink GD, Osborn JW. Renal inflammation in DOCA-salt hypertension: role of renal nerves and arterial pressure. Hypertension 2019;73:1079–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Krum H. Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension 2011;57:911–917. [DOI] [PubMed] [Google Scholar]
- 245. Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Böhm M, Mahfoud F, Sievert H, Wunderlich N, Rump LC, Vonend O, Uder M, Lobo M, Caulfield M, Erglis A, Azizi M, Sapoval M, Thambar S, Persu A, Renkin J, Schunkert H, Weil J, Hoppe UC, Walton T, Scheinert D, Binder T, Januszewicz A, Witkowski A, Ruilope LM, Whitbourn R. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 2010;376:1903–1909. [DOI] [PubMed] [Google Scholar]
- 246. Bhatt DL, Kandzari DE, O’Neill WW, D’Agostino R, Flack JM, Katzen BT, Leon MB, Liu M, Mauri L, Negoita M, Cohen SA, Oparil S, Rocha-Singh K, Townsend RR, Bakris GL. A controlled trial of renal denervation for resistant hypertension. N Engl J Med 2014;370:1393–1401. [DOI] [PubMed] [Google Scholar]
- 247. Townsend RR, Mahfoud F, Kandzari DE, Kario K, Pocock S, Weber MA, Ewen S, Tsioufis K, Tousoulis D, Sharp ASP, Watkinson AF, Schmieder RE, Schmid A, Choi JW, East C, Walton A, Hopper I, Cohen DL, Wilensky R, Lee DP, Ma A, Devireddy CM, Lea JP, Lurz PC, Fengler K, Davies J, Chapman N, Cohen SA, DeBruin V, Fahy M, Jones DE, Rothman M, Böhm M, Aoki J, Batson B, Böhm M, Choi JW, Cohen DL, Dangas G, David S, Davies J, Devireddy CM, Kandzari D, Kario K, Lee DP, Lurz PC, Patel M, Patel K, Schmieder RE, Sharp ASP, Singh J, Tsioufis K, Walton A, Weber T, Weil J, Zeller T, Ziada K, Tanabe K, Wilkins R, Mahfoud F, East C, Wilensky R, Contreras J, Steigerwalt S, Chapman N, Lea JP, Reedus D, Hoshide S, Ma A, Fengler K, Svetkey L, Rao A, Schmid A, Watkinson AF, Brown A, Tousoulis D, Hopper I, Suppan M, Agdirlioglu T, Noory E, Chasen C. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet 2017;390:2160–2170. [DOI] [PubMed] [Google Scholar]
- 248. Kandzari DE, Böhm M, Mahfoud F, Townsend RR, Weber MA, Pocock S, Tsioufis K, Tousoulis D, Choi JW, East C, Brar S, Cohen SA, Fahy M, Pilcher G, Kario K, Aoki J, Batson B, Böhm M, Choi JW, Cohen DL, Dangas G, David S, Davies J, Devireddy CM, Kandzari D, Kario K, Lee DP, Lurz PC, Papademetriou V, Patel M, Patel K, Schmieder RE, Sharp ASP, Singh J, Tsioufis K, Walton A, Weber T, Weil J, Zeller T, Ziada K, Tanabe K, Wilkins R, Mahfoud F, East C, Wilensky R, Contreras J, Steigerwalt S, Chapman N, Lea JP, Reedus D, Hoshide S, Ma A, Fengler K, Li P, Svetkey L, Rao A, Schmid A, Watkinson AF, Brown A, Tousoulis D, Hopper I, Suppan M, Agdirlioglu T, Noory E, Chasen C. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial. Lancet 2018;391:2346–2355. [DOI] [PubMed] [Google Scholar]
- 249. Azizi M, Schmieder RE, Mahfoud F, Weber MA, Daemen J, Davies J, Basile J, Kirtane AJ, Wang Y, Lobo MD, Saxena M, Feyz L, Rader F, Lurz P, Sayer J, Sapoval M, Levy T, Sanghvi K, Abraham J, Sharp ASP, Fisher NDL, Bloch MJ, Reeve-Stoffer H, Coleman L, Mullin C, Mauri L; RADIANCE-HTN Investigators. Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO): a multicentre, international, single-blind, randomised, sham-controlled trial. Lancet 2018;391:2335–2345. [DOI] [PubMed] [Google Scholar]
- 250. Hilderman M, Qureshi AR, Abtahi F, Witt N, Jägren C, Olbers J, Delle M, Lindecrantz K, Bruchfeld A. The cholinergic anti-inflammatory pathway in resistant hypertension treated with renal denervation. Mol Med 2019;25:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251. Kampmann U, Mathiassen ON, Christensen KL, Buus NH, Bjerre M, Vase H, Møller N, Kaltoft A, Poulsen PL. Effects of renal denervation on insulin sensitivity and inflammatory markers in nondiabetic patients with treatment-resistant hypertension. J Diabetes Res 2017;2017:6915310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252. Eikelis N, Hering D, Marusic P, Sari C, Walton A, Phillips S, Lambert E, Duval J, Krum H, Lambert G, Esler M, Schlaich M. The effect of renal denervation on endothelial function and inflammatory markers in patients with resistant hypertension. Int J Cardiol 2015;188:96–98. [DOI] [PubMed] [Google Scholar]
- 253. Annoni EM, Van Helden D, Guo Y, Levac B, Libbus I, KenKnight BH, Osborn JW, Tolkacheva EG. Chronic low-level vagus nerve stimulation improves long-term survival in salt-sensitive hypertensive rats. Front Physiol 2019;10:10–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Annoni EM, Xie X, Lee SW, Libbus I, KenKnight BH, Osborn JW, Tolkacheva EG. Intermittent electrical stimulation of the right cervical vagus nerve in salt-sensitive hypertensive rats: effects on blood pressure, arrhythmias, and ventricular electrophysiology. Physiol Rep 2015;3:e12476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255. Plachta DTT, Gierthmuehlen M, Cota O, Espinosa N, Boeser F, Herrera TC, Stieglitz T, Zentner J. Blood pressure control with selective vagal nerve stimulation and minimal side effects. J Neural Eng 2014;11:036011. [DOI] [PubMed] [Google Scholar]
- 256. Chapleau MW, Rotella DL, Reho JJ, Rahmouni K, Stauss HM. Chronic vagal nerve stimulation prevents high-salt diet-induced endothelial dysfunction and aortic stiffening in stroke-prone spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol 2016;311:H276–H285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257. Inoue T, Abe C, Sung SSJ, Moscalu S, Jankowski J, Huang L, Ye H, Rosin DL, Guyenet PG, Okusa MD. Vagus nerve stimulation mediates protection from kidney ischemia-reperfusion injury through α7nAChR+ splenocytes. J Clin Invest 2016;126:1939–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Tanaka S, Abe C, Abbott SBG, Zheng S, Yamaoka Y, Lipsey JE, Skrypnyk NI, Yao J, Inoue T, Nash WT, Stornetta DS, Rosin DL, Stornetta RL, Guyenet PG, Okusa MD. Vagus nerve stimulation activates two distinct neuroimmune circuits converging in the spleen to protect mice from kidney injury. Proc Natl Acad Sci U S A 2021;118:e2021758118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Vida G, Peña G, Kanashiro A, del Thompson‐Bonilla MR, Palange D, Deitch EA, Ulloa L. β2‐Adrenoreceptors of regulatory lymphocytes are essential for vagal neuromodulation of the innate immune system. FASEB J 2011;25:4476–4485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Carnevale L, Pallante F, Perrotta M, Iodice D, Perrotta S, Fardella S, Mastroiacovo F, Carnevale D, Lembo G. Celiac vagus nerve stimulation recapitulates angiotensin II-induced splenic noradrenergic activation, driving egress of CD8 effector cells. Cell Rep 2020;33:108494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Koopman FA, Chavan SS, Miljko S, Grazio S, Sokolovic S, Schuurman PR, Mehta AD, Levine YA, Faltys M, Zitnik R, Tracey KJ, Tak PP. Vagus nerve stimulation inhibits cytokine production and attenuates disease severity in Rheumatoid arthritis. Proc Natl Acad Sci U S A 2016;113:8284–8289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262. Flint AC, Conell C, Ren X, Banki NM, Chan SL, Rao VA, Melles RB, Bhatt DL. Effect of systolic and diastolic blood pressure on cardiovascular outcomes. N Engl J Med 2019;381:243–251. [DOI] [PubMed] [Google Scholar]
- 263. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;14:1903–1913. [DOI] [PubMed] [Google Scholar]
- 264. Dixon WG, Watson KD, Lunt M, Hyrich KL, Silman AJ, Symmons DPM, Maiden N, Price T, Hopkinson N, O’Reilly S, Hordon L, Griffiths I, Porter D, Capell H, Hassell A, Benitha R, Choy E, Walsh D, Emery P, Knight S, Bruce I, Taggart A, Scott D, Thompson P, McCrae F, Goodfellow R, Kitas G, Jubb R, Abernethy R, Sanders P; British Society for Rheumatology Biologics Register. Reduction in the incidence of myocardial infarction in patients with rheumatoid arthritis who respond to anti-tumor necrosis factor α therapy: results from the British Society for Rheumatology Biologics Register. Arthritis Rheum 2007;56:2905–2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265. Naranjo A, Sokka T, Descalzo MA, Calvo-Alén J, Hørslev-Petersen K, Luukkainen RK, Combe B, Burmester GR, Devlin J, Ferraccioli G, Morelli A, Hoekstra M, Majdan M, Sadkiewicz S, Belmonte M, Holmqvist A-C, Choy E, Tunc R, Dimic A, Bergman M, Toloza S, Pincus T; the QUEST-RA Group. Cardiovascular disease in patients with rheumatoid arthritis: results from the QUEST-RA study. Arthritis Res Ther 2008;10:R30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266. Nurmohamed M, Choy E, Lula S, Kola B, DeMasi R, Accossato P. The Impact of Biologics and Tofacitinib on Cardiovascular Risk Factors and Outcomes in Patients with Rheumatic Disease: A Systematic Literature Review. Drug Safety. Berlin, Germany: Springer International Publishing; 2018. p473–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267. Kang EH, Jin Y, Brill G, Lewey J, Patorno E, Desai RJ, Kim SC. Comparative cardiovascular risk of abatacept and tumor necrosis factor inhibitors in patients with rheumatoid arthritis with and without diabetes mellitus: a multidatabase cohort study. J Am Heart Assoc 2018;7:e007393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268. Singh S, Fumery M, Singh AG, Singh N, Prokop LJ, Dulai PS, Sandborn WJ, Curtis JR. Comparative risk of cardiovascular events with biologic and synthetic disease-modifying antirheumatic drugs in patients with rheumatoid arthritis: a systematic review and meta-analysis. Arthritis Care Res 2020;72:561–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. Martínez GJ, Robertson S, Barraclough J, Xia Q, Mallat Z, Bursill C, Celermajer DS, Patel S. Colchicine acutely suppresses local cardiac production of inflammatory cytokines in patients with an acute coronary syndrome. J Am Heart Assoc 2015;4:e002128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270. Nidorf M, Thompson PL. Effect of colchicine (0.5 mg twice daily) on high-sensitivity C-reactive protein independent of aspirin and atorvastatin in patients with stable coronary artery disease. Am J Cardiol 2007;99:805–807. [DOI] [PubMed] [Google Scholar]
- 271. Nidorf S, Eikelboom J, Budgeon C, Thompson P. Low-dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol 2013;61:404–410. [DOI] [PubMed] [Google Scholar]
- 272. Tong DC, Quinn S, Nasis A, Hiew C, Roberts-Thomson P, Adams H, Sriamareswaran R, Htun NM, Wilson W, Stub D, van Gaal W, Howes L, Collins N, Yong A, Bhindi R, Whitbourn R, Lee A, Hengel C, Asrress K, Freeman M, Amerena J, Wilson A, Layland J. Colchicine in patients with acute coronary syndrome. Circulation 2020;142:1890–1900. [DOI] [PubMed] [Google Scholar]
- 273. Suurmond R, van Rhee H, Hak T. Introduction, comparison and validation of Meta-Essentials: a free and simple tool for meta-analysis. Res Synth Methods 2017;8:537–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data derived from sources in the public domain. Reference details are provided in full.