Abstract
Emerging studies allude to high stress in autistic adults. Considering the detrimental impact of stress on health outcomes, examining individual resources which may influence the extent to which stress is experienced (e.g., coping and resilience) is vital. Using a person‐focused approach, this study aimed to identify coping‐resilience profiles, and examine their relations to general perceived stress and daily hassles in a sample of autistic adults (N = 86; aged 19–74 years). Cluster analysis identified four coping‐resilience profiles (i.e., high cope/ low resilience, low cope/ high resilience, engage cope/ high resilience, and disengage cope/ low resilience). The high cope/ low resilience and disengage cope/ low resilience groups had significantly higher general perceived stress than the remaining groups. No significant group differences were noted in relation to daily hassles. Jointly addressing coping and resilience may be beneficial on the perceived stress experienced in autistic adults. The use of coping‐resilience profiles may also allow for the personalization of stress management and support options in the autistic adult population.
Keywords: adults, autism spectrum disorders, coping, resilience, stress
Lay summary
High stress is increasingly reported in autistic adults. As stress can impact individual health, examining how autistic individuals cope with stress, and their resilience when faced with stressful events, is important. In this study, we grouped 86 autistic individuals aged 19–74 years based on their coping and resilience patterns. We then compared these groups across their general sense of stress and stress over daily hassles. Four coping‐resilience groups were identified, where those demonstrating a combination of high disengagement coping strategy use and low resilience reported the highest general sense of stress. These results suggest that a joint focus on coping strategies and resilience may be beneficial in understanding the stress experienced in autistic adults. Characterizing individuals based on their coping‐resilience patterns can inform support services, personalize stress management options and identify individuals who may be at risk for experiencing high stress in the autistic adult population.
Stress can be conceptualized as person‐environment transactions where demands placed on the individual are appraised as either taxing or exceeding the resources necessary to cope (Lazarus & Folkman, 1984). Stressors, by definition, demand and/or deplete resources (Halbesleben et al., 2014; Hobfoll, 1989) and it is the relative ratio between perceived demands and personal resources that determines the extent to which an individual experiences stress (Epel et al., 2018). Across a range of clinical and non‐clinical samples alike, high stress has been established as a risk factor for detrimental outcomes in both physical and mental health, well‐being, and quality of life (e.g., Cohen et al., 2007; Edman et al., 2017; Nelas et al., 2016; Ribeiro et al., 2018; Watson et al., 2008). These associations may be particularly relevant to the autistic population considering the high prevalence of co‐occurring physical health issues (Croen et al., 2015; Jones et al., 2016), mental health conditions (Hollocks et al., 2019; Lai et al., 2019), and poor quality of life (Lawson et al., 2020; Mason et al., 2018; van Heijst & Geurts, 2015).
Although there is a substantial degree of research on physiological correlates of stress (e.g., cortisol) in the autistic population (e.g., Corbett et al., 2009; Lydon et al., 2016), less is known about subjective evaluations of stress across contexts in autistic individuals. Indeed, central to experiences of stress are not only encounters with stressors, but also the ways in which they are subsequently perceived or appraised (Lazarus & Folkman, 1984). Stressful encounters and events are typically assessed using measures of life events or daily hassles. While the occurrences of stressful major life events (e.g., divorce, major illness) can undoubtedly invoke stress and require significant adjustments, there is also potential for minor stressors and hassles that characterize daily life to be enduring, reoccurring and to have a cumulative impact over time (Kanner et al., 1981; Lazarus & Folkman, 1984; Wheaton et al., 2013). On the other hand, the subjectivity of stressful experiences, influenced by individual differences in stressor appraisals and coping resources, is captured through measures of perceived stress. Perceived stress measures may be broad, tapping into how unpredictable, uncontrollable and overloaded individuals might generally perceive their lives to be (Cohen et al., 1983) or context‐specific, such as in response to specific events or encounters in various life domains.
Emerging studies in the autistic population have alluded to elevated levels of stress and frequent stressful encounters (e.g., Gillot & Standen, 2007; Kerns et al., 2015). Autistic individuals are suggested to be at increased risk for experiencing more frequent and varied stressful encounters in their daily lives (Twachtman‐Cullen et al., 2006), as well as more frequent occurrences of stressful life events (Bishop‐Fitzpatrick et al., 2017; Moseley et al., 2021) than non‐autistic individuals. Autistic adults also report higher levels of perceived stress compared to non‐autistic adults (e.g., Bishop‐Fitzpatrick et al., 2015, 2017), with higher autistic traits associated with increased levels of perceived stress in autistic adults (Hirvikoski & Blomqvist, 2015). Relatedly and concerningly, autistic adults are also at an increased vulnerability for experiencing adverse life events such as bullying, discrimination, victimization and exploitation (Griffiths et al., 2019; Johnson & Joshi, 2016), all of which are likely to result in more intense and ongoing, chronic levels of stress over time. Indeed, autistic adults have described the accumulation of these negative experiences as traumatic, resulting in poor mental health outcomes (Benevides et al., 2020).
Studies examining associations between various measures of stress and resultant outcomes in the autistic population show findings concordant with those of the wider literature. For example, an increase in parent‐reported frequency of daily hassles in autistic youth was related to an increase in behavioral and emotional problems for these youth (Khor et al., 2014). This is consistent with findings illustrating the cumulative impact of daily stressors and their negative consequences for physical and psychological health in a range of non‐autistic populations (Beasley et al., 2003; Mroczek et al., 2015; Charles et al., 2013; Seiffge‐Krenke, 2000; Sin et al., 2015). Similarly, associations between elevated perceptions of stress and a range of poor outcomes have also been reported in autistic adults, particularly in relation to poorer social functioning, greater social disability, and reduced quality of life (Bishop‐Fitzpatrick et al., 2015, 2017; Hong et al., 2016).
To further understand the experiences of stress in the autistic population, it is also important to consider the influence of psychosocial resources, which reflect intervening factors that can moderate the meaning of, or regulate reactions to stressful encounters (Lazarus & Folkman, 1984). Individual differences in stress experiences in response to otherwise objectively equal stressors can be largely due to differences in the nature and availability of individual and environmental resources (Lazarus & Folkman, 1984). While many environmental circumstances (e.g., socio‐economic status, availability of employment) may be difficult to control (Hobfoll, 2011), there are some individual resources that are malleable. Examples of these resources include coping and resilience, both of which can impact the stress process through their influence on stressor appraisals and coping abilities (Dabrowska & Pisula, 2010; Muller & Spitz, 2003; Smith et al., 2010).
Coping reflects the use of specific cognitive and behavioral strategies in response to stressful encounters (Folkman & Moskowitz, 2004). While many classifications of coping strategies exist (see Skinner et al., 2003), engagement coping often represents active coping strategies that focus on resolving the stressor and/or feelings of stress (e.g., problem solving, positive reappraisals), whereas disengagement coping strategies (e.g., behavioral disengagement such as giving up attempts to cope, being in denial) focus on avoiding these, in autistic and non‐autistic samples (e.g., Compas et al., 2001; Muniandy et al., 2021a). From a dispositional perspective, coping reflects the habitual ways in which individuals use strategies from their coping repertoire to respond to stressful encounters (Carver et al., 1989).
Use of coping strategies can be influenced by personal disposition, coping skills as well as prior coping experience (Endler & Parker, 1994), highlighting that coping is modifiable and responsive to targeted intervention (e.g., Compas et al., 2010). The coping literature in autistic adults is limited to date, however this scarcity is complemented by the emotion regulation literature. Although coping and emotion regulation are related, with some overlap in strategies examined, emotion regulation strategies are used across stressful and non‐stressful contexts as well as in response to positive and negative emotions, whereas coping strategies are only deployed in response to stressors, and typically negative emotions associated with stressful encounters (see review by Compas et al., 2014).
Resilience can be defined as the ability to ‘bounce back’, adaptat, and/or the maintenance of normal functioning despite exposure to stress and adversity (Luthar, 2006; Rutter, 2012; Smith et al., 2010). As a construct, resilience can be operationalized as a trait, process or outcome (Fletcher & Sarkar, 2013). Resilience as a trait encapsulates a continuum of individual attitudes, characteristics and learned skills that denotes general hardiness, resourcefulness and the ability to withstand and flexibly adapt to the changing demands of stressful experiences (Block & Block, 1980; Connor & Davidson, 2003; Skodol, 2010; Smith et al., 2010). These traits are suggested to be both innate and acquired, stable yet malleable (Hu et al., 2015; Joyce et al., 2018). Indeed, resilience traits can be influenced by social factors such as social support (van Kessel, 2013) and are modifiable through targeted interventions (e.g., Steinhardt & Dolbier, 2008). Resilience operationalized as a process captures the interaction of adversity, outcomes, and protective factors, where evidence of adversity and reports of positive outcomes infer the presence of resilience (e.g., Fergus & Zimmerman, 2005). As an outcome, resilience is demonstrated through an immediate outcome measure such as the presence of favorable behavior, maintenance of functioning or the absence of psychopathological symptoms in the context of risk or adversity (e.g., Luthar & Zelazo, 2003). In this study, resilience was approached from a trait perspective, representing a dynamic individual resource that can facilitate the ways in which individuals face, adapt to, and recover from stress.
Both coping and resilience can either ameliorate or aggravate the experiences of stress (Skodol, 2010). Coping strategies characterized as engagement‐oriented have been linked to reduced stress, whereas coping strategies that are disengaging in nature have been associated with increased stress (Brougham et al., 2009; Cherkil et al., 2013; Dabrowska & Pisula, 2010; Muller & Spitz, 2003; O'Brien et al., 2012; Reeve et al., 2013). Similarly, resilient individuals, who are likely to have a more optimistic outlook and a stronger belief in their abilities (Schoon & Bynner, 2003), have reported higher resistance to stress (Ong & Bergeman, 2004), lower perceived and chronic stress, and fewer occurrences of stressful life events (Cowden et al., 2016; García‐León et al., 2019; Rahimi et al., 2014; Wilks, 2008). Although higher engagement coping, lower disengagement coping and higher levels of resilience traits have been separately associated with improved outcomes such as better mental health and well‐being in autistic adults (Hwang et al., 2020; Muniandy et al., 2022), the ways in which coping and resilience may relate to stress in autistic adults have not yet been examined. Given their malleability, coping strategies and resilience may be important resources that can be developed and honed through support and intervention to mitigate some of the stressful encounters faced by autistic individuals.
The inter‐relationship between coping and resilience has been noted in autistic and non‐autistic samples, where higher resilience is associated with increased use of engagement coping strategies, and lower resilience with disengagement coping strategies (Campbell‐Sills et al., 2006; Moore et al., 2017; Muniandy et al., 2021b; Thompson et al., 2018). However, little is known about how coping and resilience in autistic people might co‐occur at an individual level. There is increasing evidence to suggest that an individual's beliefs about a stressful encounter can subsequently influence their ability to cope effectively (Crum et al., 2013). Utilizing a person‐focused approach such as cluster analysis in a given sample may help to identify distinct coping‐resilience profiles, which are characterized by individual patterns of coping strategy use and levels of resilience.
Increasingly used in the wider coping literature, the classification of individuals based on their coping profiles operates under the premise that during a stressful encounter individuals utilize coping strategies in conjunction with one another, rather than in isolation (Eisenbarth, 2012; Garnefski et al., 2001; Sideridis, 2006). Coping profiles are typically determined using cluster analytical procedures on a measure of coping strategy use, allowing the identification and description of subgroups based on their unique combinations of coping strategies (e.g., Doron et al., 2014; Steele et al., 2008; Tolan et al., 2002). These distinct combinations of coping strategies that make up these coping profiles have been found to associate differently with a range of outcome measures including stress, and psychological and physical health outcomes (Doron et al., 2014; Eisenbarth, 2012; Gaylord‐Harden et al., 2008). Coping profiles suggesting ‘risk’ for poor outcomes on health indicators are identified and subsequently can be used to shape intervention designs and efforts. To date, coping profiles have not been examined in the autistic population.
Large variability exists in the ways in which resilience profiles are derived in the literature, which is not unexpected given the heterogeneity in the operationalizations of resilience as a construct. Resilience profiles have been determined through cluster analytical procedures on single resilience measures (e.g., Kumar et al., 2010; Prince‐Embury & Steer, 2010), a combination of characteristics typically associated with resilience (e.g., hardiness, self‐efficacy, coping, and social support; Wilson et al., 2016), or a combination of risk (e.g., stressful life events, low income) and positive adjustment (e.g., competence, absence of psychopathology) measures. In this latter approach, individuals who demonstrate high risk and good adaptation or adjustment are typically grouped into the ‘resilient’ profile (e.g., Gerber et al., 2013). As far as we know, the specific combination of coping profiles and resilience profiles (i.e., coping‐resilience profiles) has not been examined in autistic or non‐autistic samples thus far. This is surprising given the increasing evidence surrounding the associations between these two constructs at the variable level.
Considering the high stress and poor health‐related outcomes reported for autistic adults, the examination of coping‐resilience profiles can help further our understanding of the ways in which coping and resilience might co‐occur within autistic individuals. Determining how these profiles may differentially relate to experiences of stress may also be especially useful in the tailoring of support options based on an individual's unique disposition to, and risk of stress.
CURRENT STUDY
The main aim of the current study was to identify coping‐resilience profiles in a sample of autistic adults using a person‐focused approach, and to examine their relationships with experiences of stress (i.e., general perceived stress and daily hassles stress). Although there were no specific hypotheses regarding the profiles that would be derived due to the novelty of coping‐resilience profiles in the general population and the scarcity of coping and resilience literature in autism research to date, it was expected that individuals characterized by high resilience, high engagement coping and low disengagement coping would report lower levels of general perceived stress and daily hassles stress. In contrast, individuals with low resilience, low engagement coping and high disengagement coping were expected to report higher stress.
METHODS
The current study was conducted during the ongoing coronavirus pandemic (COVID‐19; June to November 2020). Although examining stress, coping and resilience specifically in response to COVID‐19 was not the aim of the study, additional information on COVID‐19 associated fear and stress was captured and is included at different points in this manuscript where relevant, to provide further context to the overall stress experienced by our sample during this period.
Participants
The participants consisted of 86 autistic adults (29 males, 57 females, M age = 40.76, SD age = 13.47, range: 19–74 years). They all resided in Australia and self‐reported a formal diagnosis of ASD, including their specific diagnosis, year of diagnosis, and details of their diagnosing professional. The inclusion criteria were autistic adults aged 18 years and above, with a formal diagnosis of autism, who were based in Australia, and were proficient in English.
To ensure that participants understood the study requirements and were able to provide informed consent, only individuals who self‐reported not having a co‐occurring diagnosis of intellectual disability on the study eligibility page, were included in the study. The Autism‐Spectrum Quotient Short (AQ‐Short) was also used as an inclusion criterion, where only participants who met criteria for ASD on the AQ‐Short (>65; Hoekstra et al., 2011) were included in the sample for analysis. Participant demographic information is presented in Table 1.
TABLE 1.
Demographic information
| M (SD; range) N or frequency | ||
|---|---|---|
| N | 86 | |
| Age | 40.76 years (13.47; 19–74 years) | |
| Sex designated at birth | Male | 29 (33.7%) |
| Female | 57 (66.3%) | |
| Gender identity | Male | 28 (32.6%) |
| Female | 47 (54.7%) | |
| Genderqueer or non‐conforming | 8 (9.3%) | |
| Different identity | 1 (1.2%) | |
| Missing | 2 (2.3%) | |
| Self‐reported diagnoses | Autism spectrum disorder | 56 (65.1%) |
| Autistic disorder | 0 | |
| Asperger's syndrome | 28 (32.6%) | |
| High functioning autism | 1 (1.2%) | |
| Pervasive developmental disorder–not otherwise specified | 1 (1.2%) | |
| Age of diagnoses (years) | 1–10 | 11 (12.8%) |
| 11–20 | 11 (12.8% | |
| 21–30 | 13 (15.1%) | |
| 31–40 | 19 (22.1%) | |
| 41–50 | 23 (26.7%) | |
| 51–60 | 3 (3.5%) | |
| 61–70 | 5 (5.8%) | |
| Missing | 1 (1.2%) | |
| Australian state of residence | Victoria | 47 (54.7%) |
| New South Wales | 17 (19.8%) | |
| Western Australia | 4 (4.7%) | |
| South Australia | 6 (7.0%) | |
| Queensland | 9 (10.5%) | |
| Tasmania | 1 (1.2%) | |
| Australian Capital Territory | 2 (2.3%) | |
| COVID‐19 | ||
| Diagnosed with COVID‐19 | Self | 1 (1.2%) |
| Close family or friends | 1 (1.2%) | |
| Extended family or friends | 5 (5.8%) | |
| Had COVID‐19 symptoms | Self | 15 (17.4%) |
| Close family or friends | 10 (11.6%) | |
| Extended family or friends | 8 (9.3%) | |
| Since the COVID‐19 pandemic, experienced changes and disruptions in | Employment | 47 (54.7%) |
| Education | 19 (22.1%) | |
| Living situation | 38 (44.2%) | |
| Social relationships | 48 (55.8%) | |
Procedures
Following institutional ethics approval from La Trobe University Human Ethics Committee (HEC19443), recruitment for the study targeted formally diagnosed autistic adults through a range of channels, including Australian and state‐based autism organizations (e.g., Autism CRC, Autism Queensland), autism‐specific service providers, and participant databases from various autism research organizations. Upon expression of interest, the study information statement and an online link to REDCap (Research Electronic Data Capture; Harris et al., 2009) were provided to potential participants. The online link included an eligibility page, where once the criteria were met and informed consent indicated, participants were automatically directed to the start of the survey. The online survey included questions on basic demographics and a range of questionnaires encompassing experiences of stress, coping and resilience, psychological well‐being and quality of life. Upon study completion, all participants were offered the option of receiving a $10 e‐voucher. Participants who agreed to this were re‐directed to a new page, where an e‐mail address of choice could be provided.
MEASURES
Autism traits
The Autism Quotient‐Short (AQ‐Short; Hoekstra et al., 2011) is a 28‐item abbreviated version of the 50‐item AQ screening questionnaire (Baron‐Cohen et al., 2001) widely used to measure autistic traits. Using a 4‐point Likert, scale ranging from definitely agree (1) to definitely disagree (4), higher scores are indicative of increased autism traits. A total score can be generated using the sum of the individual items, where a total cut‐off score greater than 65 has high sensitivity (0.97) and specificity (0.82) with a clinical diagnosis of ASD (Hoekstra et al., 2011). A high Cronbach alpha value (0.81) was found in the current study.
COVID‐19 fear
Fear of COVID‐19 was assessed using the Fear of Coronavirus Questionnaire (FCQ; Mertens et al., 2020), which contained eight statements to assess components of fear (e.g., worry, attentional biases, avoidant behavior) in relation to COVID‐19. The items tap into aspects of fear such as threat of infection in themselves (e.g., ‘For my personal health, I find the virus to be much more dangerous than the seasonal flu’) and in others (e.g., I am worried that friends or family will be infected), precautionary and safety behaviors to prevent infection (e.g., I take more precautions compared to most people to not become infected), as well as attentional biases (e.g., I am constantly following all news updates regarding the virus). Rated on a 5‐point Likert scale, ranging from (1) Strongly disagree to (5) Strongly agree, a higher total score indicates a higher fear of COVID‐19. A total score is derived using the sum of the eight item scores. To date, good internal consistency has been reported in other studies (α = 0.77 and 0.80; Mertens et al., 2020; Vos et al., 2021), including the present sample (α = 0.79).
COVID‐19 stress
Considering the uneven spread of COVID‐19 exposures and infections across Australia due to variable and changing state and territory border closures and lockdowns during the time of study, it was deemed unsuitable to measure stress directly related to contracting COVID‐19. Rather, the authors developed questions to measure perceived stress in major life domains as a result of COVID‐19 and its associated movement restrictions. Stress associated with COVID‐19 disruptions and changes in major life domains (i.e., employment, education, living situation and social relationships) was assessed with a yes/no item “Since the COVID‐19 pandemic, have you experienced changes in your________?”. Respondents who indicated a change in any of the domains were then asked to specify details of the change and the extent of stress experienced because of this change on a 5‐point Likert scale from (1) Not stressful at all, to (5) Extremely stressful. Participants who indicated no change in any domain were assigned a score of 0 in this domain. A total COVID‐19 stress score was derived using the sum of stress over the four domains, where scores ranged from 0 to 20. The internal consistency for the total COVID‐19 stress score in the current sample was 0.86.
Coping strategies
The Brief COPE (Carver, 1997) is a 28‐item abbreviated version of the original COPE inventory (Carver et al., 1989) where use of coping strategies is measured using a 4‐point scale ranging from (1) I have not been doing this at all to (4) I have been doing this a lot. A 6‐factor structure for the Brief COPE has been reported for autistic adults by Muniandy, Richdale, Trollor, and Lawson (2021a), with good internal consistencies across all six coping subscales (Engagement coping: 0.86, Support‐seeking coping: 0.88, Disengagement coping: 0.76, Substance‐use coping: 0.95, Humor coping: 0.82 and Religious coping: 0.78). In the present study, the 8‐item engagement coping (e.g., “I've been trying to come up with a strategy about what to do”) and 5‐item disengagement coping (e.g. “I've been refusing to believe that it has happened”) subscales (Supplementary Table A1) were examined given their strong associations with stress in the wider non‐autistic coping literature (e.g., Arsenio & Loria, 2014; Coiro et al., 2017; Yang et al., 2008). The total score for each subscale is obtained by summing the constituent items, where higher scores reflect more frequent use of the respective coping strategy. Both the engagement coping and disengagement coping subscales had good internal consistencies, with alpha values of 0.77 and 0.76 respectively in the current sample.
Resilience
The Connor‐Davidson Resilience Scale‐10 (CD‐RISC‐10; Campbell‐Sills & Stein, 2007) is the 10‐item abridged version of the CD‐RISC (Connor & Davidson, 2003), designed to assess various aspects of resilience such as hardiness (e.g., ‘I am able to adapt to changes when they occur or ‘I tend to bounce back after illness, injury or other hardships') and persistence (e.g., ‘I believe I can achieve my goals, even if there are obstacles'). Items are rated on a 5‐point scale ranging from (0) not true at all to (4) true nearly all the time. A total resilience score is obtained using the sum of items, where a higher score reflects higher levels of resilience. The CD‐RISC‐10 has good construct validity (Campbell‐Sills & Stein, 2007) and high internal consistency is reported in the general population (α = 0.85 in Campbell‐Sills & Stein, 2007; α = 0.88 in Scali et al., 2012). It has also been validated for use in an autistic adult sample, with high internal consistency (α = 0.92; Hwang et al., 2020). High internal consistency was found for the current sample (Cronbach's alpha = 0.88).
General perceived stress
The Perceived Stress Scale (PSS‐10; Cohen & Williamson, 1988) is a shortened version of the original PSS (Cohen et al., 1983), used to evaluate the degree to which individuals appraise their lives as generally stressful. Respondents rate the frequency of certain feelings and thoughts over the last month on a 5‐point scale ranging from never (1) to very often (5). Cut‐off total scores are commonly used in the literature to suggest low (0–13), moderate (14–26) and high (27–40) levels of stress. Good to excellent internal reliability has been reported for the PSS‐10 in adults from the general (α = 0.91; Mitchell et al., 2008; Wu & Amtmann, 2013) and the autistic population (α = 0.87, Bishop‐Fitzpatrick et al., 2018; α = 0.76, Hong et al., 2016), as was the case in the present study (0.90).
Daily hassles stress
The Daily Stress Inventory (DSI; Brantley et al., 1987) is a 58‐item self‐report measure that allows respondents to indicate the occurrence of daily events often viewed as stressful or unpleasant, and has been used extensively across clinical (e.g., Felsten, 2004; Houle et al., 2012) and non‐clinical populations (e.g., Bell & D'zurilla, 2009; Winzeler et al., 2014). Upon indicating the occurrence of an event, individuals rate their perceived stressfulness on a Likert‐type scale ranging from Occurred but was not stressful (1) to Caused me to panic (7). Three scores are derived from the DSI: (1) Frequency: the number of stressful events experienced; (2) Sum: total stress across events; and (3) Average stress: the average stress experienced over an event, calculated by dividing the sum of stress by the frequency of events (Brantley et al., 1987). Cronbach alpha for the frequency of events and the sum of stress in the present study were 0.91 and 0.92, respectively.
Measures related to autism traits (AQ‐Short) and COVID‐19 (FCQ and COVID‐19 stress) provided further information about the sample characteristics. To derive coping‐resilience profiles, coping (Brief COPE) and resilience (CD‐RISC‐10) scores were utilized, while the subsequent associations between these profiles and experiences of stress were examined across three measures of stress (PSS, Average Daily Hassles stress and COVID‐19 stress).
Data analysis
Descriptive statistics were used to report levels of stress while associations between key variables in the study were examined using correlation analyses. To empirically derive resilience‐coping profiles based on similar patterns of coping strategy use and resilience in the current sample, cluster analysis was conducted. As the measures of coping and resilience were differently scaled, all scores were standardized to z‐scores prior to cluster analytic procedures (e.g., Macnab et al., 2001; Vesanto, 2001). An intra‐cluster sum of squared distances scree plot was produced using R version 4.1.0, where the apparent plateau or ‘elbow’ in the plot indicated the optimal number of clusters (k; Everitt & Hothorn, 2011). Cluster validity was evaluated using an average Silhouette coefficient threshold of ≥0.5 (Dalmaijer et al., 2022; Kaufman & Rousseeuw, 1990). The value of k was then utilized in the k‐means cluster analysis conducted in SPSS version 27.0.0 with the default 10 iterations, to characterize participants according to their patterns in coping strategy use and resilience. The derived clusters and their compositions were subsequently examined to ensure meaningful interpretation (Rapkin & Luke, 1993).
To explore cluster‐level differences, Pearson's chi‐square for independence tests and one‐way analysis of variance (ANOVA) with post‐hoc tests via Bonferroni were utilized to explore cluster‐level differences in variables of interest. Effect size measure for each ANOVA was determined using Eta squared (ƞ 2), where 0.01 was interpreted as a small, 0.06 as a medium, and 0.14 as a large effect. As several variables violated the assumptions of normality, bootstrapping analysis using 2000 resamples and 95% bias‐corrected and accelerated (BCa) confidence intervals (CI) were applied to the correlation analyses and ANOVAs for more robust statistics (Field, 2013). In these analyses, BCa confidence intervals that do not include zero demonstrate statistically significant estimates (Hayes, 2009). Missing data were pairwise excluded where possible, with the exception of bootstrapped analyses, which require list wise exclusion.
RESULTS
Descriptive and correlation analyses
Descriptive statistics and correlations are provided in Table 2. Relatively high levels of general perceived stress were noted in the sample, with total PSS scores primarily ranging from moderate to high (low, 5.8%; moderate, 48.8%; high, 40.7%). The mean frequency of daily hassle events encountered was 16.62 (possible range: 0–58) and the average daily hassles stress was 4.32 (possible range: 1–7).
TABLE 2.
Study variables (M, SD, range) and Pearson's 2000 bootstrapped re‐samples correlations for full sample (n = 80)
| Variable | Range | M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 19–74 | 40.76 (13.47) | — | |||||||||
| 2. Se a | — | — | −0.217 | — | ||||||||
| 3. Autism traits | 67–112 | 87.96 (9.52) | −0.004 | 0.060 | — | |||||||
| 4. COVID‐19 fear | 15–38 | 26.80 (5.90) | 0.110 | 0.022 | 0.011 | — | ||||||
| 5. COVID‐19 stress | 0–20 | 5.56 (4.62) | −0.212 | 0.114 | −0.052 | 0.153 | — | |||||
| 6. Daily hassles frequency | 2–45 | 16.62 (9.48) | −0.232 * | 0.026 | 0.063 | 0.220 | 0.409 ** | — | ||||
| 7. Daily hassles average stress | 2.5–6.6 | 4.32 (0.91) | −0.095 | 0.267 * | 0.264 * | 0.151 | 0.195 | 0.340 ** | — | |||
| 8. Perceived stress | 6–39 | 24.80 (6.96) | −0.172 | 0.129 | 0.236 * | 0.037 | 0.379 ** | 0.344 ** | 0.639 ** | — | ||
| 9. Engagement coping | 12–29 | 20.80 (4.11) | 0.143 | 0.110 | −0.054 | 0.077 | −0.032 | 0.060 | −0.185 | −0.180 | — | |
| 10. Disengagement coping | 5–19 | 9.60 (3.47) | −0.119 | −0.119 | 0.199 | 0.041 | 0.144 | 0.341 ** | 0.351 ** | 0.561 ** | −0.329 ** | — |
| 11. Resilience | 0–37 | 18.40 (7.48) | 0.019 | −0.020 | −0.315 ** | 0.007 | −0.060 | −0.099 | −0.334 ** | −0.528 ** | 0.385 ** | −0.610 ** |
Note: BCa 95% confidence intervals that do not cross zero are in bold and significance based on p‐values (*) are noted.
p < 0.05.
p < 0.01.
Positive direction indicates female.
General perceived stress was positively correlated with all other stress measures (i.e., daily hassles frequency and stress, and COVID‐19 stress). Higher use of disengagement coping was associated with increased general perceived stress and average daily hassles stress, whereas higher levels of resilience were related to reduced general and daily hassles stress. Coping strategies and resilience were not significantly associated with either COVID‐19 fear or COVID‐19 stress.
Coping‐resilience profiles
Four clusters were identified based on the examination of the intra‐cluster sum of squared distances scree plot indicating a plateau or ‘elbow’, silhouette figures, and interpretability of clusters. The first group (n = 15) was characterized by high use of both coping strategies (i.e., Engagement and Disengagement coping), and low Resilience; hereafter labeled high cope/ low resilience. The second group (n = 27) was labeled low cope/ high resilience, reflecting low use of both coping strategies and high Resilience scores relative to the coping scores reported in this cluster. The third group (n = 20) reported high use of Engagement coping but low use of Disengagement coping, and high Resilience, and was subsequently labeled engage cope/ high resilience. The fourth group (n = 18) was labeled disengage cope/ low resilience, considering the high Disengagement coping, but low use of Engagement coping, and low Resilience scores. The composition of scores for each cluster can be seen in Figure 1 and Table 3. Standardized score composition for each cluster by sex is presented in the Supplemental (Figure A1).
FIGURE 1.
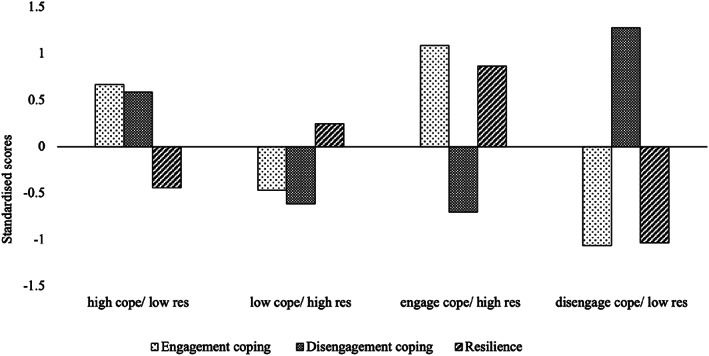
Composition of standardized scores for engagement coping, disengagement coping and resilience across the four groups
TABLE 3.
Descriptive statistics (M, SD) for each coping‐resilience profile
| High cope/low resilience (n = 15) | Low cope/high resilience (n = 27) | Engage cope/high resilience (n = 20) | Disengage cope/low resilience (n = 18) | |
|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | |
| Age | 40.84 (10.41) | 36.63 (11.07) | 47.55 (14.34) | 39.89 (15.90) |
| Female (%) | 8 (53.3) | 20 (74.1) | 15 (75) | 11 (61.1) |
| Autism traits | 89.87 (10.04) | 86.30 (8.99) | 86.60 (9.98) | 90.78 (8.97) |
| COVID‐19 fear | 28.27 (6.33) | 26.41 (6.06) | 26.65 (6.03) | 25.67 (5.90) |
| COVID‐19 stress | 7.00 (5.71) | 4.70 (3.94) | 5.00 (4.23) | 6.00 (5.43) |
| Daily hassles frequency | 19.47 (13.62) | 14.59 (8.03) | 15.50 (7.59) | 18.72 (10.13) |
| Daily hassles average stress | 4.28 (1.14) | 4.22 (0.82) | 4.09 (0.85) | 4.73 (0.93) |
| Perceived stress | 27.00 (6.35) | 22.41 (5.73) | 21.70 (7.55) | 29.22 (5.64) |
| Engagement coping | 23.53 (2.39) | 18.89 (2.19) | 25.25 (2.00) | 16.44 (2.53) |
| Disengagement coping | 11.60 (1.92) | 7.41 (1.78) | 7.10 (1.59) | 14.00 (2.50) |
| Resilience | 15.20 (6.69) | 20.37 (5.06) | 25.00 (5.00) | 10.78 (5.30) |
Profile‐differences across variables
Profile‐differences across key variables are presented in Table 3. There were no between‐group differences in relation to participant sex ratio [x 2 (3) = 2.752, p = 0.431], autistic traits, [F (3, 76) = 1.15, p = 0.333] or COVID‐19 fear [F (3,76) = 0.527, p = 0.665]. While individuals in the low cope/ high resilience group were younger than the engage cope/ high resilience group [F (3, 76) = 2.74, p = 0.049], no other significant age differences between the groups were noted.
In relation to stress, significant profile differences were noted in general perceived stress, with large effect size [F (3, 76) = 6.40, p = 0.001, ƞ 2 = 0.20]. As illustrated in Figure 2, the high cope/ low resilience group had higher general perceived stress compared to the low cope/ high resilience (BCa 95% CI = 0.62, 8.41) and engage cope/ high resilience (BCa 95% CI = 0.89, 9.97) groups. Likewise, the disengage cope/ low resilience group reported higher general perceived stress compared to the low cope/ high resilience (BCa 95% CI = −9.92, −3.59) and engage cope/ high resilience (BCa 95% CI = −11.76, −3.57) groups. No significant profile differences were noted across average daily hassles stress [F (3, 76) = 1.74, p = 0.167] or COVID‐19 stress [F (3, 76) = 0.899, p = 0.446].
FIGURE 2.
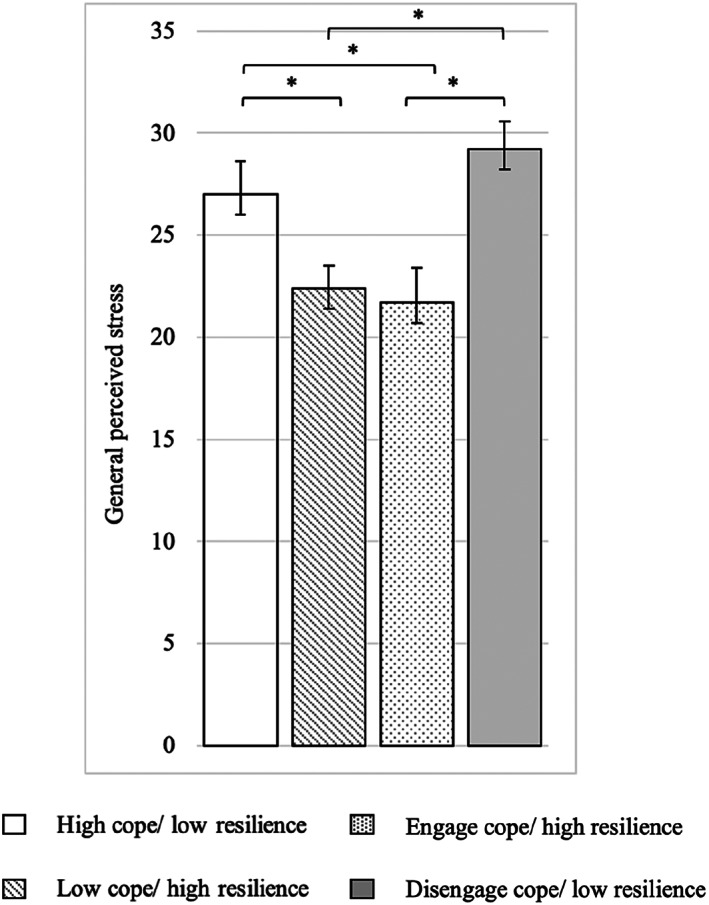
Profile differences in relation to general perceived stress. Bars represent stress scores (+/− SE). Bracketed bars with an asterisk (*) are significantly different.
DISCUSSION
The primary aim of this study was to characterize the individual patterns of coping strategy use and resilience in a sample of autistic adults and subsequently examine its relationship with levels of general perceived stress and daily hassles stress. We also examined whether COVID‐19 fear or COVID‐19 related stress impacted our findings. Based on the distribution of resilience, engagement coping and disengagement coping scores, four profiles were derived: high cope/ low resilience, low cope/ high resilience, engage cope/ high resilience, and disengage cope/ low resilience. Both the high cope/ low resilience and disengage cope/ low resilience groups reported significantly higher general perceived stress compared to the low cope/ high resilience and engage cope/ high resilience groups. However, no significant profile differences were found in relation to average daily hassles stress, COVID‐19 related stress, or COVID‐19 fear.
Relatively high levels of general perceived stress were noted in the current sample, with almost half the autistic adults (48.8%) reporting moderate stress, and more than a third (40%), high stress, corroborating findings of previous research surrounding high perceived stress in autistic adults (e.g., Bishop‐Fitzpatrick et al., 2018; Bishop‐Fitzpatrick et al., 2017; Hirvikoski & Blomqvist, 2015). The significant positive associations between general perceived stress and the other context‐specific stress measures (i.e., daily hassles and COVID‐19 stress) also suggests the influence of stress over specific contexts in an individual's overall sense of life stressfulness, and vice‐versa. Thus, the measure of general perceived stress seems to have captured aspects of context‐specific stress related to daily life and COVID‐19 pandemic disruptions in our sample of autistic adults during this time.
Daily hassles stress in the current sample (mean stress: 4.32) appeared relatively higher than population norms to date (i.e., score range of 2.22–2.59; Bell & D'zurilla, 2009; Brantley et al., 1987; Houle et al., 2012; Winzeler et al., 2014), although the frequency with which these hassles occurred (mean frequency: 16.62), while at the high end, was within the range of those reported for other adult samples (i.e., range: 9–17; Brantley et al., 1987; Orsega‐Smith et al., 2004; Winzeler et al., 2014). As far as we know, this is the first study that captured a snapshot of both the frequency and stress of daily hassles in a sample of autistic adults; previous research has only explored daily hassles in autistic youth (Khor et al., 2014). These findings suggest that although autistic adults may not necessarily face an increased number of hassles and irritants in their everyday life, these encounters, as well as life in general, are perceived as more stressful. Future studies may benefit from measuring daily hassles in autistic adults over an extended period (e.g., using a weekly/ monthly hassles log or momentary time sampling) to examine potential changes in, or accumulation of hassles over time.
The four distinct profiles (i.e., high cope/ low resilience, low cope/ high resilience, engage cope/ high resilience, and disengage cope/ low resilience) identified through patterns of coping and resilience closely align with coping profiles identified in numerous non‐clinical samples to date (e.g., Doron et al., 2014; Gadreau & Blondin, 2004; Seiffge‐Krenke & Klessinger, 2000; Smith & Wallston, 1996). Indeed, although labeled differently, four coping profiles, characterized by both low and high use of all coping strategies, and the relative emphasis/de‐emphasis of some strategies over others, have been commonly reported. This suggests that relying solely on the dominance of, or preference for some coping strategies over others does not adequately account for the ways in which individuals cope.There are individuals who use various strategies within their repertoire to similar degrees (i.e., both sparingly or frequently), as noted in our low and high cope groups. These findings mirror those reported in the autism emotion regulation literature where individuals are said to employ a repertoire of dispositional emotion regulation strategies that vary in nature and approaches, and that considering a combination of strategies is important in determining their joint impact on outcome measures (Cai et al., 2018). Our results not only complement the growing use of person‐centered approaches in the coping literature (e.g., Freire et al., 2020; Hasselle et al., 2019), but our inclusion of resilience provides an additional dimension, indicating that while individuals may use a combination of coping strategies, these combinations may also co‐occur differently with resilience, supporting the supposition that coping and resilience are inter‐related and multidimensional in nature.
As hypothesized, the engage cope/high resilience group reported significantly less general perceived stress compared to the disengage cope/low resilience group. To remind the reader, engage cope reflects high use of engagement coping and low use of disengagement coping, whereas disengage cope refers to high use of disengagement coping and low use of engagement coping. While coping styles characterized by active, approach‐oriented coping (i.e., high engagement, low disengagement coping) and high resilience are personal resources that have been separately associated with lower stress (e.g., Dabrowska & Pisula, 2010; Ong & Bergeman, 2004), it is plausible that the combination of both, as endorsed by some individuals, is beneficial in a cumulative manner in relation to individuals' stress experiences. This is congruent with the Conservation of Resources theory (Hobfoll 2002; Hobfoll et al., 2018), which postulates that individuals with high personal resources (e.g., high resilience) may further acquire, develop and preserve new resources (e.g., engagement coping strategy repertoire) making them less vulnerable to stress, whereas those with low resources (e.g., low resilience) may be on a downward spiral of losing resources (e.g., disengaging as a means of coping), making these individuals even more vulnerable to stress. In the context of stress in autistic adults, focusing on and developing engagement coping, reducing disengagement coping and improving resilience in conjunction with each other may be especially beneficial in creating an ‘upward spiral’ of resource gain (Hobfoll, 2002, 2011).
Differences in average daily hassles stress and COVID‐19 stress between the engage cope/high resilience group and the disengage cope/low resilience group did not reach statistical significance. The lack of profile differences in these latter measures of stress may be related to them being context specific. Indeed, as coping‐resilience profiles in the present study were derived using coping and resilience scores measured using a dispositional approach, it is possible that potential discrepancies in context‐specific stress, if any, would be best‐captured using coping and resilience measures that are also situation‐specific. It may be worthwhile for future studies to examine situational coping‐resilience profiles in response to specific stressful encounters to continue unpacking the relationships between coping, resilience, and stress in the autistic population. Further, although unexamined in and beyond the aims of the current study, there are constructs such as perceived control (Dijkstra & Homan, 2016; Ong & Bergeman, 2004) and self‐efficacy (Benight & Cieslak, 2011; Hamill, 2003) which may impact both coping and resilience. Exploring these constructs in the context of stressful encounters may further elucidate the mechanisms that underlie the associations between coping and resilience, and subsequent levels of perceived stress in the autistic population.
Of particular interest was the low cope/ high resilience group, which formed about a third (33.8%) of the sample and the relatively low levels of stress reported across the three stress measures. This ‘low coper’ profile, reflecting a low use of both coping strategies, is not uncommon in the literature and has been similarly noted in other samples to be associated with relatively good outcomes such as reduced stress, pain, depressive and emotional symptoms, and higher personal adjustment (Aldridge & Roesch, 2008; Doron et al., 2014; Smith & Wallston, 1996; Steele et al., 2008). It is possible that the low use of engagement coping in the low cope/ high resilience group may have been buffered by both a similarly low use of disengagement coping and high resilience, with resulting lower stress. Nevertheless, the cross‐sectional data in our study limits our ability to establish the direction of these relationships and it is just as possible that individuals who perceive less stress in their lives simply have less to cope with, and thus utilize all coping strategies to a lesser extent. Longitudinal data in future studies would be especially important in determining the directions of these relationships. Similarly, we note that the low cope/ high resilience group was younger in age compared to the engage cope/ high resilience group. While this might indicate the broadening of coping strategy repertoire with age, future longitudinal research may be better able to ascertain the stability of coping‐resilience profiles over time, and whether individual profile membership may change with age.
A key practical implication from this study is the need for personalization of stress support and intervention options. Although not all autistic adults experience high stress, the use of coping‐resilience profiles could help identify those at highest risk of experiencing stress (i.e., disengage cope/ low resilience or high cope/ low resilience groups), especially during times when stress may be expected (e.g., transitional periods, occurrence of significant life changes). Based on coping‐resilience profiles, individual‐specific aspects of coping and resilience can be determined and addressed according to individual need. For example, autistic individuals characterized by the high cope/ low resilience profile may be more susceptible to high perceived stress and may therefore benefit from interventions focusing on reducing disengagement coping tendencies and increasing resilience (thus shifting them towards a lower stress risk profile). On the other hand, individuals presenting with an engage cope/ high resilience profile may not be at risk for high perceived stress and may not require coping strategy or resilience‐related support at the time of assessment.
Beyond this, these profiles can also be useful in providing an initial snapshot of an individual's current repertoire of coping strategies and levels of resilience, subsequently informing more in‐depth discussions with them surrounding self‐beliefs, experiences of recovery after challenging events, effectiveness of and motivations behind preferred coping strategies, as well as potential barriers which may impede the use of certain coping strategies. It is possible for example, that disengagement coping strategies, which are frequently endorsed in the autistic population (e.g., Muniandy et al., 2022), may be helpful for autistic adults in a way that was not captured in the present study. Indeed, disengaging from stressful encounters, at least briefly, may be beneficial in allowing individuals to avoid further input, stimulation or sensory overload (Crane et al., 2009; Halim et al., 2018).
Interventions in autistic adults have largely focused on reducing symptoms of co‐occurring mental health conditions (Benevides et al., 2020). Although some of these may already incorporate elements of coping and resilience among their areas of focus (McGillivray & Evert, 2014; Oswald et al., 2018), interventions with an explicit focus on stress reduction and management in autistic adults are relatively limited. Further, while there are promising programs referred to as resilience interventions with autistic youth (e.g., Resourceful Adolescent Program–Autism Spectrum Disorder, RAP‐ASD; Shochet et al., 2022 or Resilience Builder Therapy Program, RBP; Habayeb et al., 2017), these interventions do not incorporate resilience as a primary target or outcome measure. As far as we know, stress interventions are yet to be designed and conducted in autistic adults, which specifically target and measure coping strategy use and resilience.
Our consideration of resilience in addition to coping in autistic adults supports the increasing focus on stress reappraisal and mindset interventions in the wider stress‐management literature (e.g., Hagger et al., 2020; Jamieson et al., 2018), which aims for stressors to be re‐interpreted as challenging, enhancing and to be approached (rather than threatening, deleterious and to be avoided), not unlike the characteristics reflected in resilience. For example, interventions which focus on identifying and altering maladaptive thinking or disempowering interpretations of situations (e.g., catastrophising or overgeneralizing) can help reduce the likelihood of individuals succumbing to their stressful encounters or feeling defeated, thus enhancing their resilience levels. A joint focus on coping strategies would allow individuals to build on their coping strategy repertoire, limit the use of unhelpful coping strategies (e.g., alcohol use), and improve self‐efficacy surrounding their coping abilities. Indeed, there is evidence surrounding the effectiveness of interventions targeting both resilience and coping in improving overall well‐being across non‐autistic samples (Burton et al., 2010; Steinhardt & Dolbier, 2008). In particular, the use of Cognitive Behavioral Therapy (CBT) and mindfulness‐based approaches has been noted to be effective in the promotion of resilience and resilience‐related factors (such as coping) in the general population (Joyce et al., 2018).
When considering the autistic adult population, stress interventions focusing on coping and resilience, through the incorporation of mindfulness‐based approaches (e.g., acceptance, being calm and present) and CBT‐based approaches (e.g., cognitive appraisals and flexibility, problem solving skills) can be beneficial in fostering adjustments to stressful encounters (Helmreich et al., 2017), and may result in reduced perceived stress and other negative stress‐related outcomes. Such interventions would be best designed in collaboration with the autistic community, where suitable adaptations (e.g., communication methods, use of language; Spain & Happé, 2019; Spek et al., 2013), as well as potential autism‐unique considerations for promoting coping and resilience may be identified. For example, given that a sense of social inclusion and belonging has been highlighted by autistic adults as important in their development of resilience and coping (Ghanouni & Quirke, 2022), fostering positive relationships and building support systems for autistic adults may be an important area of focus. It would also be useful for these interventions to utilize coping and resilience measures using psychometric tools that have been validated for use in this population, such as the Brief COPE and CD‐RISC‐10.
Considerations, limitations and future directions
The COVID‐19 pandemic continues to be an evolving phenomenon. While there is emerging evidence to suggest its deleterious effects on stress and well‐being in autistic individuals (e.g., Ameis et al., 2020; Corbett et al., 2021), the impact of the pandemic will inevitably vary between individuals (Hedley et al., 2021). This is not unlike other contexts in stress research, where despite the use of specific measures of stress and stressor encounters, there remains individual differences in other sources of stress that may be unexamined and unaccounted for. The present study was uniquely placed in the presence of the COVID‐19 pandemic, a large‐scaled, universal stressor faced by all study participants. Further, our incorporation of general and dispositional measures was useful in limiting the impact of contextual factors and individual differences across the examination of stress, coping, and resilience.
While the present study addresses several current gaps in the autism literature, it also includes some limitations. First, due to the relatively modest sample size, replication using a larger sample to evaluate the robustness of the four coping‐resilience profiles is recommended. Although there are no clear rules‐of‐thumb regarding minimum sample sizes in cluster analytical procedures (see Sarstedt & Mooi, 2014 or Dalmaiher et al., 2022), a larger sample of autistic adults could improve generalizability of our results. Larger sample sizes may be more sensitive to stress differences in relation to daily hassles, or may be able to detect statistically significant stress differences between the two higher perceived stress groups (i.e., disengage cope/ low resilience and high cope/ low resilience), and the two lower perceived stress groups (engage cope/ high resilience and low cope/ high resilience). Such studies may also allow for more reliable comparisons of coping‐resilience profiles across other demographic measures such as adult life stages (e.g., young adults vs older adults), as well as other measures more commonly used to characterize the autistic population (e.g., IQ, adaptive functioning, quality of life).
Next, while the present study measured coping by examining the use of engagement and disengagement coping strategies given their associations with stress in the literature, future studies should consider exploring other coping strategies as they may interact differently with resilience. For example, the use of proactive coping, which involves the anticipation of potential stressors and the incorporation of future‐oriented strategies to prevent these from occurring (Greenglas & Fiksenbaum, 2009) may be similarly reflected in more resilient individuals.
Third, our sample included an overrepresentation of female participants (66%), as is similarly reported in online survey studies in autistic and non‐autistic samples (e.g., Kapp et al., 2013; Nicolaidis et al., 2013). While the lack of sex differences between the profiles suggests that group‐differences were not influenced by sex, it may prove useful for future studies with larger samples to characterize coping‐resilience profiles separately in males and females to confirm whether or not sex‐differences in patterns of coping strategy use and levels of resilience d exist. Relatedly, it would be important for future research to examine stress and stress‐related constructs such as coping and resilience within the context of gender diversity. From an intersectionality perspective, it is possible that gender diverse autistic individuals have unique experiences of stress, or reflect different patterns of coping strategies, compared to cisgendered autistic individuals. Additionally, although the constructs of coping, resilience, and perceived stress are commonly examined together in the broader stress literature, it is possible that there are conceptual overlaps between these constructs, which could artificially inflate the relationships between coping‐resilience profile membership and levels of perceived stress. Item‐level comparisons across the measures used here did not identify items identical enough to warrant item deletions, however, future research to determine the distinctiveness of these stress‐related constructs and the extent of any potential overlap, both at the conceptual‐ and item‐levels in the autism population may be warranted.
Finally, the cross‐sectional nature of the data limits our ability to draw causal conclusions. Although we can conclude that individual levels of resilience and coping patterns may confer risk in response to levels of stress experienced, it is equally possible that experiences of stress can influence the resilience and coping strategies used. Indeed, experiences of extreme or chronic stress are likely to impact individual abilities and resources, subsequently influencing the individual's capacities to both withstand and to cope with demands (e.g., Cicchetti & Rogosch, 2009; Schetter & Dolbier, 2011). Although extreme levels of stress were not indicated in any of our stress measures, future work with a longitudinal design would allow for a deeper understanding of the associations between resilience and coping patterns, and stress in autistic adults.
CONCLUSION
In conclusion, the present study offers significant insight into coping and resilience patterns in relation to stress in autistic adults, an otherwise limited area of research in this population. Our findings suggest distinct patterns of coping strategies and resilience on an individual level across four distinct profiles, where autistic adults characterized by the disengage cope/ low resilience and high cope/ low resilience profiles are likely to be at highest risk for elevated stress and may benefit most from stress‐related intervention. Jointly addressing coping and resilience may positively impact the degree of stress experienced by autistic adults, and in turn, has potential to cascade positively into other areas of life such as physical and psychological health, well‐being and quality of life.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ETHICS STATEMENT
Ethics approval was provided by La Trobe University Human Ethics Committee (HEC19443).
Supporting information
Figure A1 Composition of standardized scores for engagement coping, disengagement coping and resilience across the four groups based on sex (a) males; (b) females
Table A1 Coping items in Engagement Coping and Disengagement Coping categories as identified in Muniandy, Richdale, Trollor, and Lawson (2021a).
ACKNOWLEDGMENTS
We gratefully acknowledge the cooperation and participation of all autistic participants involved in this study. All authors acknowledge the financial support of the Cooperative Research Centre for Living with Autism (Autism CRC), established and supported under the Australian Government's Cooperative Research Centers program. Melanie Muniandy is supported by an Autism CRC PhD scholarship while the position held by Lauren P. Lawson was funded by the Autism CRC at the time this research was conducted. Open access publishing facilitated by La Trobe University, as part of the Wiley ‐ La Trobe University agreement via the Council of Australian University Librarians.
Muniandy, M. , Richdale, A. L. , & Lawson, L. P. (2022). Coping‐resilience profiles and experiences of stress in autistic adults. Autism Research, 15(11), 2149–2166. 10.1002/aur.2817
Funding information Cooperative Research Centre for Living with Autism; La Trobe University
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Aldridge, A. A. , & Roesch, S. C. (2008). Developing coping typologies of minority adolescents: A latent profile analysis. Journal of Adolescence, 31(4), 499–517. 10.1016/j.adolescence.2007.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameis, S. H. , Lai, M. C. , Mulsant, B. H. , & Szatmari, P. (2020). Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID‐19 pandemic and beyond. Molecular Autism, 11(1), 1–9. 10.1186/s13229-020-00365-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arsenio, W. F. , & Loria, S. (2014). Coping with negative emotions: Connections with adolescents' academic performance and stress. The Journal of Genetic Psychology, 175(1), 76–90. 10.1080/00221325.2013.806293 [DOI] [PubMed] [Google Scholar]
- Baron‐Cohen, S. , Wheelwright, S. , Skinner, R. , Martin, J. , & Clubley, E. (2001). The autism‐spectrum quotient (AQ): Evidence from Asperger syndrome/high‐functioning autism, males and females, scientists and mathematicians. Journal of Autism and Developmental Disorders, 31(1), 5–17. 10.1023/A:1005653411471 [DOI] [PubMed] [Google Scholar]
- Beasley, M. , Thompson, T. , & Davidson, J. (2003). Resilience in response to life stress: The effects of coping style and cognitive hardiness. Personality and Individual Differences, 34(1), 77–95. 10.1016/S0191-8869(02)00027-2 [DOI] [Google Scholar]
- Bell, A. C. , & D'Zurilla, T. J. (2009). The influence of social problem‐solving ability on the relationship between daily stress and adjustment. Cognitive Therapy and Research, 33(5), 439–448. 10.1007/s10608-009-9256-8 [DOI] [Google Scholar]
- Benevides, T. W. , Shore, S. M. , Palmer, K. , Duncan, P. , Plank, A. , Andresen, M. L. , … Morgan, L. (2020). Listening to the autistic voice: Mental health priorities to guide research and practice in autism from a stakeholder‐driven project. Autism, 24(4), 822–833. 10.1177/1362361320908410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benight, C. C. , & Cieslak, R. (2011). Cognitive factors and resilience: How self‐efficacy contributes to coping with adversities. In S. Southwick, B. Litz, D. Charney, & M. Friedman (Eds.), Resilience and mental health: Challenges across the lifespan (p. 45‐55). Cambridge: Cambridge University Press. [Google Scholar]
- Bishop‐Fitzpatrick, L. , Mazefsky, C. A. , & Eack, S. M. (2018). The combined impact of social support and perceived stress on quality of life in adults with autism spectrum disorder and without intellectual disability. Autism, 22(6), 703–711. 10.1177/1362361317703090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop‐Fitzpatrick, L. , Mazefsky, C. A. , Minshew, N. J. , & Eack, S. M. (2015). The relationship between stress and social functioning in adults with autism spectrum disorder and without intellectual disability. Autism Research, 8(2), 164–173. 10.1002/aur.1433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop‐Fitzpatrick, L. , Minshew, N. J. , Mazefsky, C. A. , & Eack, S. M. (2017). Perception of life as stressful, not biological response to stress is associated with greater social disability in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(1), 1–16. 10.1007/s10803-016-2910-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block, J. H. , & Block, J. (1980). The role of ego‐control and ego‐resiliency in the organization of behavior. In Collins W. A. (Ed.), Development of cognition, affect, and social relations. The Minnesota symposia on child psychology (Vol. 13, pp. 39–101). Lawrence Erlbaum. [Google Scholar]
- Brantley, P. J. , Waggoner, C. D. , Jones, G. N. , & Rappaport, N. B. (1987). A daily stress inventory: Development, reliability, and validity. Journal of Behavioral Medicine, 10(1), 61–73. 10.1007/BF00845128 [DOI] [PubMed] [Google Scholar]
- Brougham, R. R. , Zail, C. M. , Mendoza, C. M. , & Miller, J. R. (2009). Stress, sex differences, and coping strategies among college students. Current Psychology, 28(2), 85–97. 10.1007/s12144-009-9047-0 [DOI] [Google Scholar]
- Burton, N. W. , Pakenham, K. I. , & Brown, W. J. (2010). Feasibility and effectiveness of psychosocial resilience training: A pilot study of the READY program. Psychology, Health & Medicine, 15(3), 266–277. 10.1080/13548501003758710 [DOI] [PubMed] [Google Scholar]
- Cai, R. Y. , Richdale, A. L. , Dissanayake, C. , & Uljarević, M. (2018). Brief report: Inter‐relationship between emotion regulation, intolerance of uncertainty, anxiety, and depression in youth with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(1), 316–325. 10.1007/s10803-017-3318-7 [DOI] [PubMed] [Google Scholar]
- Campbell‐Sills, L. , Cohan, S. L. , & Stein, M. B. (2006). Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behaviour Research and Therapy, 44(4), 585–599. 10.1016/j.brat.2005.05.001 [DOI] [PubMed] [Google Scholar]
- Campbell‐Sills, L. , & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor‐Davidson resilience scale (CD‐RISC): Validation of a 10‐item measure of resilience. Journal of Trauma and Stress, 20(6), 1019–1028. 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Carver, C. S. (1997). You want to measure coping but your protocol's too long: Consider the brief cope. International Journal of Behavioral Medicine, 4(1), 92–100. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Carver, C. S. , Scheier, M. F. , & Weintraub, J. K. (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56(2), 267–283. 10.1037/0022-3514.56.2.267 [DOI] [PubMed] [Google Scholar]
- Charles, S. T. , Piazza, J. R. , Mogle, J. , Sliwinski, M. J. , & Almeida, D. M. (2013). The wear and tear of daily stressors on mental health. Psychological Science, 24(5), 733–741. 10.1177/0956797612462222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherkil, S. , Gardens, S. J. , & Soman, D. K. (2013). Coping styles and its association with sources of stress in undergraduate medical students. Indian Journal of Psychological Medicine, 35(4), 389–393. 10.4103/0253-7176.122235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti, D. , & Rogosch, F. A. (2009). Adaptive coping under conditions of extreme stress: Multilevel influences on the determinants of resilience in maltreated children. New Directions for Child and Adolescent Development, 2009(124), 47–59. 10.1002/cd.242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. , Janicki‐Deverts, D. , & Miller, G. E. (2007). Psychological stress and disease. JAMA, 298(14), 1685–1687. 10.1001/jama.298.14.1685 [DOI] [PubMed] [Google Scholar]
- Cohen, S. , Kamarck, T. , & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 385–396, 385. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cohen, S. , & Williamson, G. (1988). Perceived stress in a probability sample of the United States. In Spacapan S. & Oskamp S. (Eds.), The social psychology of health (pp. 31–68). Sage. [Google Scholar]
- Coiro, M. J. , Bettis, A. H. , & Compas, B. E. (2017). College students coping with interpersonal stress: Examining a control‐based model of coping. Journal of American College Health, 65(3), 177–186. 10.1080/07448481.2016.1266641 [DOI] [PubMed] [Google Scholar]
- Compas, B. E. , Champion, J. E. , Forehand, R. , Cole, D. A. , Reeslund, K. L. , Fear, J. , … Roberts, L. (2010). Coping and parenting: Mediators of 12‐month outcomes of a family group cognitive–behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology, 78(5), 623–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas, B. E. , Connor‐Smith, J. K. , Saltzman, H. , Thomsen, A. H. , & Wadsworth, M. E. (2001). Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin, 127(1), 87–127. 10.1037/0033-2909.127.1.87 [DOI] [PubMed] [Google Scholar]
- Compas, B. E. , Jaser, S. S. , Dunbar, J. P. , Watson, K. H. , Bettis, A. H. , Gruhn, M. A. , & Williams, E. K. (2014). Coping and emotion regulation from childhood to early adulthood: Points of convergence and divergence. Australian Journal of Psychology, 66(2), 71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor, K. M. , & Davidson, J. R. (2003). Development of a new resilience scale: The Connor‐Davidson resilience scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Corbett, B. A. , Muscatello, R. A. , Klemencic, M. E. , & Schwartzman, J. M. (2021). The impact of COVID‐19 on stress, anxiety, and coping in youth with and without autism and their parents. Autism Research, 14(7), 1496–1511. 10.1002/aur.2521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett, B. A. , Schupp, C. W. , Levine, S. , & Mendoza, S. (2009). Comparing cortisol, stress, and sensory sensitivity in children with autism. Autism Research, 2(1), 39–49. 10.1002/aur.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowden, R. G. , Meyer‐Weitz, A. , & Oppong Asante, K. (2016). Mental toughness in competitive tennis: Relationships with resilience and stress. Frontiers in Psychology, 7, 320. 10.3389/fpsyg.2016.00320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane, L. , Goddard, L. , & Pring, L. (2009). Sensory processing in adults with autism spectrum disorders. Autism, 13(3), 215–228. 10.1177/1362361309103794 [DOI] [PubMed] [Google Scholar]
- Croen, L. A. , Zerbo, O. , Qian, Y. , Massolo, M. L. , Rich, S. , Sidney, S. , & Kripke, C. (2015). The health status of adults on the autism spectrum. Autism, 19(7), 814–823. 10.1177/1362361315577517 [DOI] [PubMed] [Google Scholar]
- Crum, A. J. , Salovey, P. , & Achor, S. (2013). Rethinking stress: The role of mindsets in determining the stress response. Journal of Personality and Social Psychology, 104(4), 716–733. 10.1037/a0031201 [DOI] [PubMed] [Google Scholar]
- Dabrowska, A. , & Pisula, E. (2010). Parenting stress and coping styles in mothers and fathers of pre‐school children with autism and down syndrome. Journal of Intellectual Disability Research, 54(3), 266–280. 10.1111/j.1365-2788.2010.01258.x [DOI] [PubMed] [Google Scholar]
- Dalmaijer, E. S. , Nord, C. L. , & Astle, D. E. (2022). Statistical power for cluster analysis. BMC Bioinformatics, 23(1), 1–28. 10.1186/s12859-022-04675-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dijkstra, M. T. , & Homan, A. C. (2016). Engaging in rather than disengaging from stress: Effective coping and perceived control. Frontiers in Psychology, 7, 1415. 10.3389/fpsyg.2016.01415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doron, J. , Trouillet, R. , Maneveau, A. , Neveu, D. , & Ninot, G. (2014). Coping profiles, perceived stress, and health‐related behaviors: A cluster analysis approach. Health Promotion International, 30(1), 88–100. 10.1093/heapro/dau090 [DOI] [PubMed] [Google Scholar]
- Edman, J. S. , Greeson, J. M. , Roberts, R. S. , Kaufman, A. B. , Abrams, D. I. , Dolor, R. J. , & Wolever, R. Q. (2017). Perceived stress in patients with common gastrointestinal disorders: Associations with quality of life, symptoms and disease management. Explore, 13(2), 124–128. 10.1016/j.explore.2016.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenbarth, C. (2012). Coping profiles and psychological distress: A cluster analysis. North American Journal of Psychology, 14(3), 485‐496. [Google Scholar]
- Endler, N. S. , & Parker, J. D. (1994). Assessment of multidimensional coping: Task, emotion, and avoidance strategies. Psychological Assessment, 6(1), 50–60. 10.1037/1040-3590.6.1.50 [DOI] [Google Scholar]
- Epel, E. S. , Crosswell, A. D. , Mayer, S. E. , Prather, A. A. , Slavich, G. M. , Puterman, E. , & Mendes, W. B. (2018). More than a feeling: A unified view of stress measurement for population science. Frontiers in Neuroendocrinology, 49, 146–169. 10.1016/j.yfrne.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everitt, B. , & Hothorn, T. (2011). An introduction to applied multivariate analysis with R. Springer Science & Business Media. [Google Scholar]
- Felsten, G. (2004). Stress reactivity and vulnerability to depressed mood in college students. Personality and Individual Differences, 36(4), 789–800. [Google Scholar]
- Fergus, S. , & Zimmerman, M. A. (2005). Adolescent resilience: A framework for understanding healthy development in the face of risk. Annual Review of Public Health, 26, 399–419. 10.1146/annurev.publhealth.26.021304.144357 [DOI] [PubMed] [Google Scholar]
- Field, A. (2013). Discovering statistics using IBM SPSS statistics (4th ed.). SAGE. [Google Scholar]
- Fletcher, D. , & Sarkar, M. (2013). Psychological resilience: A review and critique of definitions, concepts, and theory. European psychologist, 18(1), 12–23. 10/1027/1016‐9040/a000124. [Google Scholar]
- Folkman, S. , & Moskowitz, J. T. (2004). Coping: Pitfalls and promise. Annual Review of Psychology, 55, 745–774. 10.1146/annurev.psych.55.090902.141456 [DOI] [PubMed] [Google Scholar]
- Freire, C. , Ferradás, M. D. M. , Regueiro, B. , Rodríguez, S. , Valle, A. , & Núñez, J. C. (2020). Coping strategies and self‐efficacy in university students: A person‐centered approach. Frontiers in Psychology, 11, 841. 10.3389/fpsyg.2020.00841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García‐León, M. Á. , Pérez‐Mármol, J. M. , Gonzalez‐Pérez, R. , del Carmen García‐Ríos, M. , & Peralta‐Ramírez, M. I. (2019). Relationship between resilience and stress: Perceived stress, stressful life events, HPA axis response during a stressful task and hair cortisol. Physiology & Behavior, 202, 87–93. 10.1016/j.physbeh.2019.02.001 [DOI] [PubMed] [Google Scholar]
- Garnefski, N. , Kraaij, V. , & Spinhoven, P. (2001). Negative life events, cognitive emotion regulation and emotional problems. Personality and Individual Differences, 30(8), 1311–1327. 10.1016/S0191-8869(00)00113-6 [DOI] [Google Scholar]
- Gaudreau, P. , & Blondin, J. P. (2004). Different athletes cope differently during a sport competition: A cluster analysis of coping. Personality and Individual Differences, 36(8), 1865–1877. 10.1016/j.paid.2003.08.017 [DOI] [Google Scholar]
- Gaylord‐Harden, N. K. , Gipson, P. , Mance, G. , & Grant, K. E. (2008). Coping patterns of African American adolescents: A confirmatory factor analysis and cluster analysis of the Children's coping strategies checklist. Psychological Assessment, 20(1), 10–22. 10.1037/1040-3590.20.1.10 [DOI] [PubMed] [Google Scholar]
- Gerber, M. , Brand, S. , Feldmeth, A. K. , Lang, C. , Elliot, C. , Holsboer‐Trachsler, E. , & Pühse, U. (2013). Adolescents with high mental toughness adapt better to perceived stress: A longitudinal study with Swiss vocational students. Personality and Individual Differences, 54(7), 808–814. 10.1016/j.paid.2012.12.003 [DOI] [Google Scholar]
- Ghanouni, P. , & Quirke, S. (2022). Resilience and coping strategies in adults with autism Spectrum disorder. Journal of Autism and Developmental Disorders, 1–12. 10.1007/s10803-022-05436-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillott, A. , & Standen, P. J. (2007). Levels of anxiety and sources of stress in adults with autism. Journal of Intellectual Disabilities, 11(4), 359–370. 10.1177/1744629507083585 [DOI] [PubMed] [Google Scholar]
- Greenglass, E. R. , & Fiksenbaum, L. (2009). Proactive coping, positive affect, and well‐being: Testing for mediation using path analysis. European Psychologist, 14(1), 29–39. 10.1027/1016-9040.14.1.29 [DOI] [Google Scholar]
- Griffiths, S. , Allison, C. , Kenny, R. , Holt, R. , Smith, P. , & Baron‐Cohen, S. (2019). The vulnerability experiences quotient (VEQ): A study of vulnerability, mental health, and life satisfaction in autistic adults. Autism Research, 12(10), 1516–1528. 10.1002/aur.2162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habayeb, S. , Rich, B. , & Alvord, M. K. (2017). Targeting heterogeneity and comorbidity in children with autism spectrum disorder through the resilience builder group therapy program. Child & Youth Care Forum (Vol. 46, No. 4, pp. 539‐557). Springer US, 46(4), 539–557. 10.1007/s10566-017-9394-1 [DOI] [Google Scholar]
- Hagger, M. S. , Keech, J. J. , & Hamilton, K. (2020). Managing stress during the coronavirus disease 2019 pandemic and beyond: Reappraisal and mindset approaches. Stress and Health, 36, 396–401. 10.1002/smi.2969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbesleben, J. R. B. , Neveu, J. P. , Paustian‐Underdahl, S. C. , & Westman, M. (2014). Getting to the “COR”: Understanding the role of resources in conservation of resources theory. Journal of Management, 40(5), 1334–1364. 10.1177/0149206314527130 [DOI] [Google Scholar]
- Halim, A. T. , Richdale, A. L. , & Uljarević, M. (2018). Exploring the nature of anxiety in young adults on the autism spectrum: A quali‐ tative study. Research in Autism Spectrum Disorders, 55, 25–37. 10.1016/j.rasd.2018.07.006 [DOI] [Google Scholar]
- Hamill, S. K. (2003). Resilience and self‐efficacy: The importance of efficacy beliefs and coping mechanisms in resilient adolescents. Colgate University Journal of the Sciences, 35(1), 115–146. [Google Scholar]
- Harris, P. A. , Taylor, R. , Thielke, R. , Payne, J. , Gonzalez, N. , & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata‐driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasselle, A. J. , Schwartz, L. E. , Berlin, K. S. , & Howell, K. H. (2019). A latent profile analysis of coping responses to individuals' most traumatic event: Associations with adaptive and maladaptive mental health outcomes. Anxiety, Stress, & Coping, 32(6), 626–640. 10.1080/10615806.2019.1638733 [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76(4), 408–420. 10.1080/03637750903310360 [DOI] [Google Scholar]
- Hedley, D. , Hayward, S. M. , Denney, K. , Uljarević, M. , Bury, S. , Sahin, E. , … Stokes, M. A. (2021). The association between COVID‐19, personal wellbeing, depression, and suicide risk factors in Australian autistic adults. Autism Research, 14(12), 2663–2676. 10.1002/aur.2614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmreich, I. , Kunzler, A. , Chmitorz, A. , König, J. , Binder, H. , Wessa, M. , & Lieb, K. (2017). Psychological interventions for resilience enhancement in adults. The Cochrane Database of Systematic Reviews, 2017(2), 1‐43. 10.1002/14651858.CD012527 [DOI] [Google Scholar]
- Hirvikoski, T. , & Blomqvist, M. (2015). High self‐perceived stress and poor coping in intellectually able adults with autism spectrum disorder. Autism, 19(6), 752–757. 10.1177/1362361314543530 [DOI] [PubMed] [Google Scholar]
- Hobfoll, S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44(3), 513–524. 10.1037/0003-066X.44.3.513 [DOI] [PubMed] [Google Scholar]
- Hobfoll, S. E. (2002). Social and psychological resources and adaptation. Review of General Psychology, 6(4), 307–324. 10.1037/1089-2680.6.4.307 [DOI] [Google Scholar]
- Hobfoll, S. E. (2011). Conservation of resources theory: Its implication for stress, health, and resilience. In Folkman S. (Ed.), The Oxford handbook of stress, health, and coping (pp. 127–147). Oxford University Press. [Google Scholar]
- Hobfoll, S. E. , Halbesleben, J. , Neveu, J. P. , & Westman, M. (2018). Conservation of resources in the organizational context: The reality of resources and their consequences. Annual Review of Organizational Psychology and Organizational Behavior, 5, 103–128. 10.1146/annurev-orgpsych-032117-104640 [DOI] [Google Scholar]
- Hoekstra, R. A. , Vinkhuyzen, A. A. E. , Wheelwright, S. , Bartels, M. , Boomsma, D. I. , Baron‐Cohen, S. , Posthuma, D. , & van der Sluis, S. (2011). The construction and validation of an abridged version of the autism‐ Spectrum quotient (AQ‐short). Journal of Autism and Developmental Disorders, 41(5), 589–596. 10.1007/s10803-010-1073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollocks, M. J. , Lerh, J. W. , Magiati, I. , Meiser‐Stedman, R. , & Brugha, T. S. (2019). Anxiety and depression in adults with autism spectrum disorder: A systematic review and meta‐analysis. Psychological Medicine, 49(4), 559–572. 10.1017/S0033291718002283 [DOI] [PubMed] [Google Scholar]
- Hong, J. , Bishop‐Fitzpatrick, L. , Smith, L. E. , Greenberg, J. S. , & Mailick, M. R. (2016). Factors associated with subjective quality of life of adults with autism spectrum disorder: Self‐report versus maternal reports. Journal of Autism and Developmental Disorders, 46(4), 1368–1378. 10.1007/s10803-015-2678-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houle, T. T. , Butschek, R. A. , Turner, D. P. , Smitherman, T. A. , Rains, J. C. , & Penzien, D. B. (2012). Stress and sleep duration predict headache severity in chronic headache sufferers. Pain, 153(12), 2432–2440. 10.1016/j.pain.2012.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, T. , Zhang, D. , & Wang, J. (2015). A meta‐analysis of the trait resilience and mental health. Personality and Individual Differences, 76, 18–27. 10.1016/j.paid.2014.11.039 [DOI] [Google Scholar]
- Hwang, Y. I. , Arnold, S. , Trollor, J. , & Uljarević, M. (2020). Factor structure and psychometric properties of the brief Connor–Davidson Resilience Scale for adults on the autism spectrum. Autism, 24(6), 1572–1577. 10.1177/1362361320908095 [DOI] [PubMed] [Google Scholar]
- Jamieson, J. P. , Crum, A. J. , Goyer, J. P. , Marotta, M. E. , & Akinola, M. (2018). Optimizing stress responses with reappraisal and mindset interventions: An integrated model. Anxiety, Stress, & Coping, 31(3), 245–261. 10.1080/10615806.2018.1442615 [DOI] [PubMed] [Google Scholar]
- Johnson, T. D. , & Joshi, A. (2016). Dark clouds or silver linings? A stigma threat perspective on the implications of an autism diagnosis for workplace well‐being. Journal of Applied Psychology, 101(3), 430–449. 10.1037/apl0000058 [DOI] [PubMed] [Google Scholar]
- Jones, K. B. , Cottle, K. , Bakian, A. , Farley, M. , Bilder, D. , Coon, H. , & McMahon, W. M. (2016). A description of medical conditions in adults with autism spectrum disorder: A follow‐up of the 1980s Utah/UCLA autism epidemiologic study. Autism, 20(5), 551–561. 10.1177/1362361315594798 [DOI] [PubMed] [Google Scholar]
- Joyce, S. , Shand, F. , Tighe, J. , Laurent, S. J. , Bryant, R. A. , & Harvey, S. B. (2018). Road to resilience: A systematic review and meta‐analysis of resilience training programs and interventions. BMJ Open, 8(6), e017858. 10.1136/bmjopen-2017-017858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaluza, G. (2000). Changing unbalanced coping profiles: A prospective controlled intervention trial in worksite health promotion. Psychology and Health, 15, 423–433. [Google Scholar]
- Kanner, A. D. , Coyne, J. C. , Schaefer, C. , & Lazarus, R. S. (1981). Comparison of two modes of stress measurement: Daily hassles and uplifts versus major life events. Journal of Behavioral Medicine, 4(1), 1–39. [DOI] [PubMed] [Google Scholar]
- Kapp, S. K. , Gillespie‐Lynch, K. , Sherman, L. E. , & Hutman, T. (2013). Deficit, difference, or both? Autism and neurodiversity. Developmental Psychology, 49(1), 59–71. 10.1037/a0028353 [DOI] [PubMed] [Google Scholar]
- Kaufman, L. , & Rousseeuw, P. J. (1990). Finding groups in data: An introduction to cluster analysis. John Wiley & Sons. [Google Scholar]
- Kerns, C. M. , Newschaffer, C. J. , & Berkowitz, S. J. (2015). Traumatic childhood events and autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(11), 3475–3486. 10.1007/s10803-015-2392-y [DOI] [PubMed] [Google Scholar]
- Khor, A. S. , Melvin, G. A. , Reid, S. C. , & Gray, K. M. (2014). Coping, daily hassles and behavior and emotional problems in adolescents with high‐functioning autism/Asperger's disorder. Journal of Autism and Developmental Disorders, 44(3), 593–608. 10.1007/s10803-013-1912-x [DOI] [PubMed] [Google Scholar]
- Kumar, G. , Steer, R. A. , & Gulab, N. A. (2010). Types of resiliency in child and adolescent psychiatric inpatients. Journal of Psychoeducational Assessment, 28, 315–325. 10.1177/0734282910366834 [DOI] [Google Scholar]
- Lai, M. C. , Kassee, C. , Besney, R. , Bonato, S. , Hull, L. , Mandy, W. , … Ameis, S. H. (2019). Prevalence of co‐occurring mental health diagnoses in the autism population: A systematic review and meta‐analysis. The Lancet Psychiatry, 6(10), 819–829. 10.1016/S2215-0366(19)30289-5 [DOI] [PubMed] [Google Scholar]
- Lawson, L. P. , Richdale, A. L. , Haschek, A. , Flower, R. L. , Vartuli, J. , Arnold, S. R. , & Trollor, J. N. (2020). Cross‐sectional and longitudinal predictors of quality of life in autistic individuals from adolescence to adulthood: The role of mental health and sleep quality. Autism, 24(4), 954–967. 10.1177/1362361320908107 [DOI] [PubMed] [Google Scholar]
- Lazarus, R. S. , & Folkman, S. (1984). Stress. Appraisal and coping. Springer. [Google Scholar]
- Luthar, S. S. (2006). Resilience in development: A synthesis of research across five decades. In Cicchetti D. & Cohen D. J. (Eds.), Developmental psychopathology: Risk, disorder, and adaptation (pp. 739–795). John Wiley & Sons, Inc. [Google Scholar]
- Luthar, S. S. , & Zelazo, L. B. (2003). Research on resilience: An integrative review. Resilience and vulnerability: Adaptation in the context of childhood adversities, 2, 510–549. [Google Scholar]
- Lydon, S. , Healy, O. , Reed, P. , Mulhern, T. , Hughes, B. M. , & Goodwin, M. S. (2016). A systematic review of physiological reactivity to stimuli in autism. Developmental Neurorehabilitation, 19(6), 335‐355. 10.3109/17518423.2014.971975 [DOI] [PubMed] [Google Scholar]
- Macnab, J. J. , Miller, L. T. , & Polatajko, H. J. (2001). The search for subtypes of DCD: Is cluster analysis the answer? Human Movement Science, 20(1–2), 49–72. 10.1016/S0167-9457(01)00028-8 [DOI] [PubMed] [Google Scholar]
- Mason, D. , McConachie, H. , Garland, D. , Petrou, A. , Rodgers, J. , & Parr, J. R. (2018). Predictors of quality of life for autistic adults. Autism Research, 11(8), 1138–1147. 10.1002/aur.1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGillivray, J. A. , & Evert, H. T. (2014). Group cognitive behavioral therapy program shows potential in reducing symptoms of depression and stress among young people with ASD. Journal of Autism and Developmental Disorders, 44(8), 2041–2051. 10.1007/s10803-014-2087-9 [DOI] [PubMed] [Google Scholar]
- Mertens, G. , Gerritsen, L. , Duijndam, S. , Salemink, E. , & Engelhard, I. M. (2020). Fear of the coronavirus (COVID‐19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders, 74, 102258. 10.1016/j.janxdis.2020.102258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell, A. M. , Crane, P. A. , & Kim, Y. (2008). Perceived stress in survivors of suicide: Psychometric properties of the perceived stress scale. Research in Nursing & Health, 31(6), 576–585. 10.1002/nur.20284 [DOI] [PubMed] [Google Scholar]
- Moore, K. A. , Russell, K. , & Bouchoucha, S. L. (2017). Resilience and coping: Cut from the same cloth? In Moore K. A. & Buchwald P. (Eds.), Stress and anxiety: Coping and resilience (pp. 7–16). Deutsche Nationalbibliothek. [Google Scholar]
- Moseley, R. L. , Turner‐Cobb, J. M. , Spahr, C. M. , Shields, G. S. , & Slavich, G. M. (2021). Lifetime and perceived stress, social support, loneliness, and health in autistic adults. Health Psychology, 40(8), 556–568. 10.1037/hea0001108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek, D. K. , Stawski, R. S. , Turiano, N. A. , Chan, W. , Almeida, D. M. , Neupert, S. D. , & Spiro, A., III . (2015). Emotional reactivity and mortality: Longitudinal findings from the VA normative aging study. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 70(3), 398–406. 10.1093/geronb/gbt107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller, L. , & Spitz, E. (2003). Multidimensional assessment of coping: Validation of the brief COPE among French population. L'Encéphale, 29(6), 507–518. [PubMed] [Google Scholar]
- Muniandy, M. , Richdale, A. L. , Arnold, S. R. C. , Trollor, J. N. , & Lawson, L. P. (2021a). Factor structure and psychometric properties of the brief COPE in autistic older adolescents and adults. Research in Autism Spectrum Disorders, 84, 101764. 10.1016/j.rasd.2021.101764 [DOI] [Google Scholar]
- Muniandy, M. , Richdale, A. L. , Arnold, S. R. , Trollor, J. N. , & Lawson, L. P. (2021b). Inter‐relationships between trait resilience, coping strategies, and mental health outcomes in autistic adults. Autism Research, 14(10), 2156–2168. 10.1002/aur.2564 [DOI] [PubMed] [Google Scholar]
- Muniandy, M. , Richdale, A. L. , Arnold, S. R. , Trollor, J. N. , & Lawson, L. P. (2022). Associations between coping strategies and mental health outcomes in autistic adults. Autism Research., 15, 929–944. 10.1002/aur.2694 [DOI] [PubMed] [Google Scholar]
- Nelas, P. , Duarte, J. , Dias, A. , Chaves, C. , Coutinho, E. , & Amaral, O. (2016). Vulnerability to stress and quality of life of women with urinary incontinence. Procedia‐Social and Behavioral Sciences, 217, 1118–1123. 10.1016/j.sbspro.2016.02.125 [DOI] [Google Scholar]
- Nicolaidis, C. , Raymaker, D. , McDonald, K. , Dern, S. , Boisclair, W. C. , Ashkenazy, E. , & Baggs, A. (2013). Comparison of healthcare experiences in autistic and non‐autistic adults: A cross‐sectional online survey facilitated by an academic‐community partnership. Journal of General Internal Medicine, 28(6), 761–769. 10.1007/s11606-012-2262-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien, L. , Mathieson, K. , Leafman, J. , & Rice‐Spearman, L. (2012). Level of stress and common coping strategies among physician assistant students. The Journal of Physician Assistant Education, 23(4), 25–29. 10.1097/01367895-201223040-00006 [DOI] [PubMed] [Google Scholar]
- Ong, A. D. , & Bergeman, C. S. (2004). Resilience and adaptation to stress in later life: Empirical perspectives and conceptual implications. Ageing International, 29(3), 219–246. 10.1007/s12126-996-1000-z [DOI] [Google Scholar]
- Orsega‐Smith, E. , Mowen, A. J. , Payne, L. L. , & Godbey, G. (2004). The interaction of stress and park use on psycho‐physiological health in older adults. Journal of Leisure Research, 36(2), 232–256. 10.1080/00222216.2004.11950021 [DOI] [Google Scholar]
- Oswald, T. M. , Winder‐Patel, B. , Ruder, S. , Xing, G. , Stahmer, A. , & Solomon, M. (2018). A pilot randomized controlled trial of the ACCESS program: A group intervention to improve social, adaptive functioning, stress coping, and self‐determination outcomes in young adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(5), 1742–1760. 10.1007/s10803-017-3421-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince‐Embury, S. , & Steer, R. A. (2010). Profiles of personal resiliency for normative and clinical samples of youth assessed by the resiliency scales for children and adolescentsTM. Journal of Psychoeducational Assessment, 28(4), 303–314. 10.1177/0734282910366833 [DOI] [Google Scholar]
- Rahimi, B. , Baetz, M. , Bowen, R. , & Balbuena, L. (2014). Resilience, stress, and coping among Canadian medical students. Canadian medical education journal, 5(1), e5–e12. [PMC free article] [PubMed] [Google Scholar]
- Rapkin, B. D. , & Luke, D. A. (1993). Cluster analysis in community research: Epistemology and practice. American Journal of Community Psychology, 21(2), 247–277. 10.1007/BF00941623 [DOI] [Google Scholar]
- Reeve, K. L. , Shumaker, C. J. , Yearwood, E. L. , Crowell, N. A. , & Riley, J. B. (2013). Perceived stress and social support in undergraduate nursing students' educational experiences. Nurse Education Today, 33(4), 419–424. 10.1016/j.nedt.2012.11.009 [DOI] [PubMed] [Google Scholar]
- Ribeiro, Í. J. , Pereira, R. , Freire, I. V. , de Oliveira, B. G. , Casotti, C. A. , & Boery, E. N. (2018). Stress and quality of life among university students: A systematic literature review. Health Professions Education, 4(2), 70–77. 10.1016/j.hpe.2017.03.002 [DOI] [Google Scholar]
- Rutter, M. (2012). Resilience as a dynamic concept. Development and Psychopathology, 24(2), 335–344. 10.1017/S0954579412000028 [DOI] [PubMed] [Google Scholar]
- Sarstedt, M. , & Mooi, E. (2014). A concise guide to market research. The process, data, and methods using IBM SPSS statistics. Springer. [Google Scholar]
- Scali, J. , Gandubert, C. , Ritchie, K. , Soulier, M. , & Ancelin, M. (2012). Measuring resilience in adult women using the 10‐items Connor‐Davidson resilience scale (CD‐RISC). Role of trauma exposure and anxiety disorders. PLoS One, 7(6), e39879. 10.1371/journal.pone.0039879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schetter, C. D. , & Dolbier, C. (2011). Resilience in the context of chronic stress and health in adults. Social and Personality Psychology Compass, 5(9), 634–652. 10.1111/j.1751-9004.2011.00379.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoon, I. , & Bynner, J. (2003). Risk and resilience in the life course: Implications for interventions and social policies. Journal of Youth Studies, 6(1), 21–31. 10.1080/1367626032000068145 [DOI] [Google Scholar]
- Seiffge‐Krenke, I. (2000). Causal links between stressful events, coping style, and adolescent symptomatology. Journal of Adolescence, 23(6), 675–691. 10.1006/jado.2000.0352 [DOI] [PubMed] [Google Scholar]
- Seiffge‐Krenke, I. , & Klessinger, N. (2000). Long‐term effects of avoidant coping on adolescents' depressive symptoms. Journal of Youth and Adolescence, 29(6), 617–630. 10.1023/A:1026440304695 [DOI] [Google Scholar]
- Shochet, I. M. , Saggers, B. R. , Carrington, S. B. , Orr, J. A. , Wurfl, A. M. , Kelly, R. L. , & Duncan, B. M. (2022). A school‐based approach to building resilience and mental health among adolescents on the autism spectrum: A longitudinal mixed methods study. School Mental Health, 1–23, 753–775. 10.1007/s12310-022-09501-w [DOI] [Google Scholar]
- Sideridis, G. D. (2006). Coping is not an ‘either or’: The interaction of coping strategies in regulating affect, arousal, and performance. Stress and Health: Journal of the International Society for the Investigation of Stress, 22(5), 315–327. 10.1002/smi.1114 [DOI] [Google Scholar]
- Sin, N. L. , Graham‐Engeland, J. E. , Ong, A. D. , & Almeida, D. M. (2015). Affective reactivity to daily stressors is associated with elevated inflammation. Health Psychology, 34(12), 1154–1165. 10.1037/hea0000240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner, E. A. , Edge, K. , Altman, J. , & Sherwood, H. (2003). Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychological Bulletin, 129(2), 216–269. 10.1037/0033-2909.129.2.216 [DOI] [PubMed] [Google Scholar]
- Skodol, A. E. (2010). The resilient personality. In Reich J. W., Zautra A. J., & Hall J. S. (Eds.), Handbook of adult resilience (pp. 112–125). Guilford Press. [Google Scholar]
- Smith, B. W. , Tooley, E. M. , Christopher, P. J. , & Kay, V. S. (2010). Resilience as the ability to bounce back from stress: A neglected personal resource? The Journal of Positive Psychology, 5(3), 166–176. 10.1080/17439760.2010.482186 [DOI] [Google Scholar]
- Smith, C. A. , & Wallston, K. A. (1996). An analysis of coping profiles and adjustment in persons with rheumatoid arthritis. Anxiety, Stress, and Coping, 9(2), 107–122. 10.1080/10615809608249395 [DOI] [Google Scholar]
- Spain, D. , & Happé, F. (2019). How to optimize cognitive behavior therapy (CBT) for people with autism spectrum disorders (ASD): A Delphi study. Journal of Rational‐Emotive & Cognitive‐Behavior Therapy, 38(2), 184–208. 10.1007/s10942-019-00335-1 [DOI] [Google Scholar]
- Spek, A. A. , van Ham, N. C. , & Nyklíček, I. (2013). Mindfulness‐based therapy in adults with an autism spectrum disorder: A randomized controlled trial. Research in Developmental Disabilities, 34(1), 246–253. 10.1016/j.ridd.2012.08.009 [DOI] [PubMed] [Google Scholar]
- Steele, R. G. , Cushing, C. C. , Bender, J. A. , & Richards, M. M. (2008). Profiles and correlates of children's self‐reported coping strategies using a cluster analytic approach. Journal of Child and Family Studies, 17(1), 140–153. 10.1007/s10826-007-9153-2 [DOI] [Google Scholar]
- Steinhardt, M. , & Dolbier, C. (2008). Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. Journal of American College Health, 56(4), 445–453. 10.3200/JACH.56.44.445-454 [DOI] [PubMed] [Google Scholar]
- Thompson, N. J. , Fiorillo, D. , Rothbaum, B. O. , Ressler, K. J. , & Michopoulos, V. (2018). Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. Journal of Affective Disorders, 225, 153–159. 10.1016/j.jad.2017.08.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolan, P. H. , Gorman–Smith, D. , Henry, D. , Chung, K. S. , & Hunt, M. (2002). The relation of patterns of coping of inner–city youth to psychopathology symptoms. Journal of Research on Adolescence, 12(4), 423–449. 10.1111/1532-7795.00040 [DOI] [Google Scholar]
- Twachtman‐Cullen, D. , Baron, G. , Groden, J. , Groden, G. , & Lipsitt, L. (2006). Communication and stress in students with autism spectrum disorders. Stress and coping in autism, 302, 323. [Google Scholar]
- Van Heijst, B. F. , & Geurts, H. M. (2015). Quality of life in autism across the lifespan: A meta‐analysis. Autism, 19(2), 158–167. 10.1177/1362361313517053 [DOI] [PubMed] [Google Scholar]
- Van Kessel, G. (2013). The ability of older people to overcome adversity: A review of the resilience concept. Geriatric Nursing, 34(2), 122–127. 10.1016/j.gerinurse.2012.12.011 [DOI] [PubMed] [Google Scholar]
- Vesanto, J. (2001, April). Importance of individual variables in the k‐means algorithm. In Pacific‐Asia conference on knowledge discovery and data mining (pp. 513–518). Springer. 10.1007/3-540-45357-1_54 [DOI] [Google Scholar]
- Vos, L. M. , Habibović, M. , Nyklíček, I. , Smeets, T. , & Mertens, G. (2021). Optimism, mindfulness, and resilience as potential protective factors for the mental health consequences of fear of the coronavirus. Psychiatry Research, 300, 113927. 10.1016/j.psychres.2021.113927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson, J. M. , Logan, H. L. , & Tomar, S. L. (2008). The influence of active coping and perceived stress on health disparities in a multi‐ethnic low‐income sample. BMC Public Health, 8(1), 1–9. 10.1186/1471-2458-8-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton, B. , Young, M. , Montazer, S. , & Stuart‐Lahman, K. (2013). Social stress in the twenty‐first century. In Handbook of the sociology of mental health (pp. 299–323). Springer. 10.1007/978-94-007-4276-5_15 [DOI] [Google Scholar]
- Wilks, S. E. (2008). Resilience amid academic stress: The moderating impact of social support among social work students. Advances in Social Work, 9(2), 106–125. 10.18060/51 [DOI] [Google Scholar]
- Wilson, P. A. , Meyer, I. H. , Antebi‐Gruszka, N. , Boone, M. R. , Cook, S. H. , & Cherenack, E. M. (2016). Profiles of resilience and psychosocial outcomes among young black gay and bisexual men. American Journal of Community Psychology, 57(1–2), 144–157. 10.1002/ajcp.12018 [DOI] [PubMed] [Google Scholar]
- Winzeler, K. , Voellmin, A. , Schäfer, V. , Meyer, A. H. , Cajochen, C. , Wilhelm, F. H. , & Bader, K. (2014). Daily stress, presleep arousal, and sleep in healthy young women: A daily life computerized sleep diary and actigraphy study. Sleep Medicine, 15(3), 359–366. 10.1016/j.sleep.2013.09.027 [DOI] [PubMed] [Google Scholar]
- Wu, S. M. , & Amtmann, D. (2013). Psychometric evaluation of the perceived stress scale in multiple sclerosis. International Scholarly Research Notices, 2013, 1–9. 10.1155/2013/608356 [DOI] [Google Scholar]
- Yang, H. C. , Brothers, B. M. , & Andersen, B. L. (2008). Stress and quality of life in breast cancer recurrence: Moderation or mediation of coping? Annals of Behavioral Medicine, 35(2), 188–197. 10.1007/s12160-008-9016-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure A1 Composition of standardized scores for engagement coping, disengagement coping and resilience across the four groups based on sex (a) males; (b) females
Table A1 Coping items in Engagement Coping and Disengagement Coping categories as identified in Muniandy, Richdale, Trollor, and Lawson (2021a).
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


