Abstract
Background
It is imperative to provide care for patients with terminal illnesses such as cancer, though it demands time, financial resources and other unmet needs. Subsequently, caregivers might be exposed to psychological stress and other mental health problems. Previous meta‐analysis finding shows caregivers of cancer patient suffer from depression. During the past 4 years, there has been a considerable increase in the number of newly studies, and we therefore intended to update this finding and provide current global prevalence of depression among caregivers of Cancer patients.
Methods
We searched PubMed, SCOPUS, CINAHIL, Embase, and PsychINFO to identify peer‐reviewed studies which reported the prevalence of depression among caregivers of cancer patients using pre‐defined eligibility criteria. Studies were pooled to estimate the global prevalence of depression using a random‐effect meta‐analysis model. Heterogeneity was assessed using Cochran's Q and I 2 statistics. Funnel plot asymmetry and Egger's regression tests were used to check for publication bias.
Result
Our search identified 4375 studies, of which 35 studies with 11,396 participants were included in the meta‐analysis. In the current review, the pooled prevalence of depression among caregivers of Cancer patients was 42.08% (95% CI: 34.71–49.45). The pooled prevalence of depression was higher in the studies that used cross‐sectional data (42%, 95% CI: 31–52) than longitudinal data (34%, 95% CI: 18–50). We also observed a higher rate of depression among female caregivers when compared to their male counterparts (57.6%) (95% CI: 29.5–81.5).
Conclusion
Globally, around two in five cancer patient caregivers screened positive for depression, which needs due attention. Routine screening of depressive symptoms and providing psychosocial support for caregivers is crucial.
Keywords: cancer, cancer patient, caregivers, depression, family, meta‐analysis, oncology, prevalence, Spouse, systematic review
1. BACKGROUND
Globally, Cancer is the leading cause of mortality, accounting for approximately 10 million deaths in 2020. 1 Caregivers of cancer patients play an essential role in reducing mortality of cancer patients through effective palliative care and supporting clinical management. 2 More than 90% of individuals living with Cancer have a caregiver (a friend or family member) who can provide care throughout their disease and treatment. 3 Caregivers play a leading role in community‐based models of cancer care, 4 and their position can extend for several years. 5
Even though some caregivers recognize their role positively, 6 the health impact of caring is substantial. 7 But some caregivers consider the role as an obligation, perceiving they don't have other options. 2 Despite caregivers' critical but demanding role, they are not getting enough support. 4 , 8 , 9 As a result, caregivers experience unmet needs, 10 leading to psychological distress. 11 Besides, the diagnosis of Cancer itself can also have an adverse impact on the mental health of a family caregiver. 12 Caregivers of terminal cancer patients may suffer an even higher burden as the patient's health condition deteriorates, leading caregivers to be physically and emotionally exhausted. 13 Studies demonstrate that the caregiver's burden might increase because of the unmet need of the patient. 14 The burden caregivers of cancer patients experience is strongly linked with the patient's well‐being. 15 If the unmet needs of caregivers of cancer patients are not addressed, it will affect the psychological well‐being of caregivers 16 and the health outcomes of cancer patients. 17
Epidemiological studies reported a higher rate of depression (12%–59%) 18 and anxiety (30%–50%) 15 , 18 among caregivers of cancer patients. A study conducted on family caregivers of home‐based palliative care patients (n = 300), found that around half of the caregivers (50%) met the criteria for psychological distress. 19 A global level systematic review and meta‐analysis reported a pooled prevalence of 42.3% depression and 46.55% anxiety among caregivers of Cancer patients. 20 Surprisingly, this high burden of mental health problems among caregivers didn't get attention and is subsequently not yet addressed clinically. 21
Caregivers' mental health can be enhanced by providing routine psychosocial support. 22 , 23 , 24 Further, health policymakers should develop evidence‐based interventions capable of improving caregivers' physical and psychological well‐being. 25 , 26 However, updating data on the burden of Caregivers' mental health problems should be prioritised before designing interventional strategies. 26
The availability of updated evidence on the burden of depression can help synthesize updated knowledge on the topic and address the need to develop policies and strengthen programs for caregivers of cancer patients. Despite variations in the magnitude of depression among caregivers across different countries, pooling the available up‐to‐date evidence and reporting the prevalence more precisely might help policymakers prioritize the problem and encourage governments to act accordingly. A systematic review and meta‐analysis on a similar topic by Geng et al. was published in 2018 and summarized 17 studies through March 2018, reporting a 42.3% pooled prevalence of depression. 20 During the past 4 years, there has been a considerable increase in the number of available data, and we therefore intended to update this finding and provide current global prevalence of depression among caregivers of Cancer patients.
2. METHODS
2.1. Search strategy and selection process
A systemic review and meta‐analysis was conducted using studies that examined the prevalence of depression among caregivers of Cancer patients. The strategy for literature search, selection of studies, data extraction, and reporting of results for the current review was designed following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses) guidelines 27 (Supplementary File S1). The protocol for the current review has been registered in PROSPERO (CRD42022297623).
Five electronic databases (PubMed, SCOPUS, CINAHIL, Embase, and PsychINFO) were searched to identify studies that report the prevalence of depression among caregivers of Cancer patients. Searching in PubMed was performed using the following terms: (Prevalence OR Magnitude OR Epidemiology OR Incidence OR Estimates OR Burden) AND (depression OR depressive symptoms OR depressive disorder OR major depressive disorder OR major depression) AND (caregivers of cancer patient OR carers of cancer patients OR family of cancer patient OR friend of Cancer patient OR partner of cancer patient OR Spouse of cancer patient). Database‐specific subject headings associated with the above terms were used to screen studies indexed in SCOPUS, CINAHIL, Embase, and PsychINFO databases. Besides, we observed the reference lists of published studies to identify additional articles.
2.2. Eligibility criteria
In the current review, we have included observational studies reporting the prevalence of depression among caregivers of Cancer patients and published in English language. Eligible studies included for this review had to fulfil the following criteria: first, the type of study has to be observational (cross‐sectional, nested case‐control, or follow‐up studies). Follow‐up studies are longitudinal studies that employed continuous or repeated measures to follow individual Caregivers of cancer patients over time. Second, the study participants should be adults (whose age is greater than or equal to 18 years). Third, the measurement of depression has to be a diagnostic or validated screening tool.
Studies that reported the pooled prevalence of depression, RCTs (Randomised Controlled Trials) had a poor quality score on the New Castle Ottawa Scale (NOS), duplicate studies, conference proceedings, commentaries, abstracts, reports, short communications and letters to editors were excluded.
2.3. Data extraction and study quality assessment
Data were extracted using a specific form developed by authors. The data extraction form included the following information: Name of the author, year of publication, country, study design, sample size, tools used to assess depression, the number of positive cases for depression, the prevalence of depression, stage of cancer, a primary site of cancer, and the relationship of caregivers with the patient. AB conducted the primary data extraction, and then BD assessed the extracted data independently. Any disagreements and discrepancies were resolved through discussion with the third author GD.
The methodological qualities of each included article were assessed by using a modified version of the Newcastle‐Ottawa Scale. 28 The methodological quality and eligibility of the identified articles were evaluated by two reviewers (AB and GD), and disagreements among reviewers were resolved through discussion with the third Author (BD). Finally, studies with a scale of ≥5 out of 10 were included in the current meta‐analysis.
2.4. Data analysis
The prevalence report extracted from all the included primary studies were meta‐analyzed. We have examined publication bias by visual inspection of a funnel plot and Egger's regression test. 29 , 30 A p‐value <0.05 was used to declare the statistical significance of publication bias. Studies were pooled to estimate pooled prevalence and 95% CI using a random‐effect model. 31 We have assessed heterogeneity using Cochran's Q and I 2 statistics. 32 I 2 statistics is used to quantify the percentage of the total variation in the study estimate due to heterogeneity. Due to the presence of significant heterogeneity, we have conducted a subgroup analysis based on the study design, gender of participants, and the type of tool used to detect depression. All the extracted data were analyzed using STATA 16.
3. RESULTS
3.1. Identification of studies
We retrieved a total of 4375 records via bibliographic databases searching. After removing duplicates, 3056 records were contained for title screening. Then, after removing 2311 records because of the irrelevance of the topic to the review criteria, 745 studies were retrieved for abstract screening. Seven hundred articles were excluded during the abstract screening because of the discrepancy between the study results and our review objective. Subsequently, the remaining 45 full‐text articles were assessed for eligibility. Of these screened full‐text articles (n = 45), 14 new articles, together with four articles identified through reference searching fulfilled the criteria for our meta‐analysis. Then, together with 17 studies from the previous review, 16 a total of 35 articles were included in the current updated systematic review and meta‐analysis (Figure 1).
FIGURE 1.
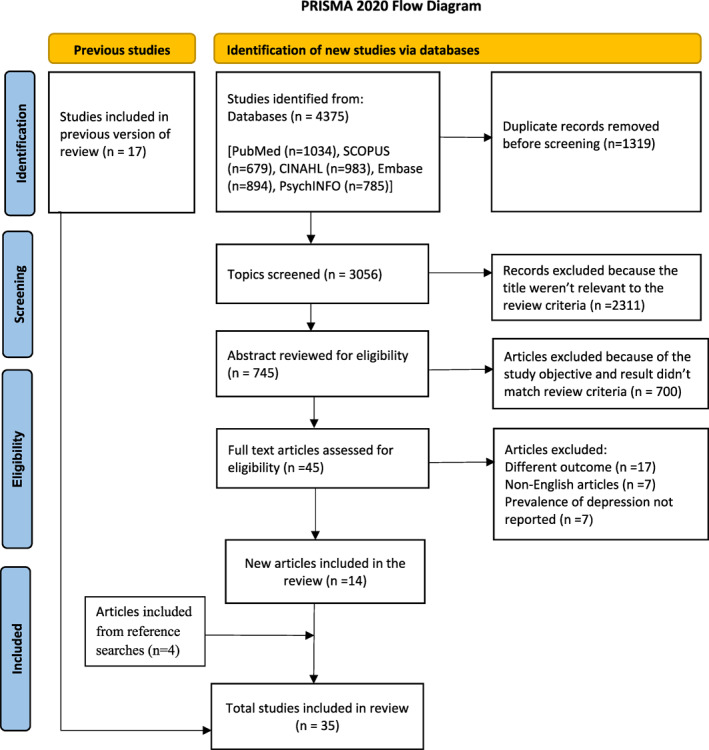
PRISMA flow chart of the study identification process for the systematic reviews and meta‐analysis
3.2. Characteristics of included studies
Table 1 has summarized the key characteristics of the studies included in this systematic review and meta‐analysis. The sample size of study participants who completed a study ranged from 41 33 up to 2743 participants. 34 The studies included in this review were available online between the year 1998 35 and 2018. 36 Seven studies were conducted using a prospective longitudinal study design 37 , 38 , 39 , 40 , 41 , 42 , 43 whereas the remaining twenty eight studies used a cross‐sectional study design to examine depression among caregivers of cancer patients.
TABLE 1.
Characteristics of the studies included in this systematic review and meta‐analysis
| First author, year | Country | Sample size | Study design | The primary site of cancer | Stage of cancer | Relationship to the patient | The tool used to assess depression/Cut‐off score | Prevalence of depression (case/total sample) (%) | NOS score |
|---|---|---|---|---|---|---|---|---|---|
| Given, 2005 56 | USA | 152 | Longitudinal | Breast, colon, lung and prostate cancer | I‐IV | Spouse, Daughter/Son or others | CESD‐20 (≥16 out of 60) | 47/152 = 31% | 8 |
| Young, 2008 57 | South Korea | 310 | CS | Stomach, liver, lung, colorectal, uterus, breast | I‐IV | Spouse, family member, or friend | BDI (>13 out of 63) | 207/310 = 66.7% | 8 |
| Tang, 2007 58 | Taiwan | 170 | CS | Any type | IV | Spouse or other family member | CESD‐20 (≥16 out of 60) | 75.90% | 8 |
| Grov, 2005 47 | Norway | 96 | CS | GI, Prostate, breast and others | IV | Spouse or other family member | HADS‐D (>8 out of 21) | 23/96 = 24% | 8 |
| Lauren, 2005 38 | USA | 200 | Longitudinal | Any type | IV | Spouse, child, sibling, friend, parent, other family member | DSM IV | 9/200 = 4.5% | 8 |
| Mohammed 2012 48 | Iran | 63 | CS | Breast cancer | I‐IV | Family member or friends | BDI (>10 out of 63) | 38/63 = 60.3% | 6 |
| Jill, 2002 59 | Canada | 44 | CS | Colorectal, pancreatic, leukemia, stomach, lung carcinoma & others | III and IV | Spouse, daughter or son | Short | 23/44 = 53% | 5 |
| Chris, 1999 39 | Netherlands | 148 | Longitudinal | Colorectal carcinoma | I‐IV | Spouse | Form of the profile of mood states | 71/148 = 48% | 7 |
| Serge, 2006 40 | Canada | 212 | Longitudinal | GI, lung and others | I‐IV | Spouse/other family member/friend | CES‐D 20 (≥16 out of 60) | 41/212 = 19.2% | 8 |
| Patricia, 2000 44 | USA | 51 | CS | Lung, colorectal, or other sites | III and IV | Spouse, adult child and other family member | IDPESQ | 27/51 = 52.9% | 5 |
| Mariah, 2006 60 | South Korea | 103 | CS | Gastric cancer | III and IV | Family member | CES‐D 20 (≥16 out of 60) | 56/103 = 55% | 6 |
| Price, 2010 41 | Australia | 373 | Longitudinal | Ovarian cancer | I‐IV | Spouse or other family member | CES‐D 20 (≥16 out of 60) | 22/373 = 5.9% | 8 |
| Victoria, 1998 35 | USA | 164 | CS | Any type | I‐IV | Adult daughter | CES‐D 20 (≥16 out of 60) | 49/164 = 30% | 8 |
| Jacquelyn, 2000 45 | USA | 117 | CS | Any type | IV | Family member | CES‐D 20 (≥16 out of 60) | 58/117 = 50% | 7 |
| Paula, 2005 46 | USA | 104 | CS | Brain tumor | I‐IV | Spouse, other family member | CES‐D 20 (≥16 out of 60) | 38/104 = 36.9% | 6 |
| Irma, 2007 33 | USA | 41 | CS | Brain and neck | I‐IV | Spouse, other family member | CES‐D 20 (≥16 out of 60) | 8/41 = 20% | 5 |
| Zümrüt, 2012 61 | Turkey | 60 | CS | Any type | I‐IV | Family member | HADS‐D (>8 out of 21) | 34/60 = 57% | 5 |
| Badger, 2007 42 | USA | 96 | Longitudinal | Breast cancer | I‐IV | Partner | CESD‐20 (>16 out of 60) | 71/96 = 74% | 8 |
| Heckel, 2015 10 | Australia | 150 | CS | Any type | IV | Spouse/partner | CESD‐20 (≥16 out of 60) | 54/150 = 36% | 9 |
| Kim, 2007 62 | USA | 98 | CS | Colorectal | I‐IV | Family or close friend | CES‐D 20 (≥16 out of 60) | 29/98 = 29.6% | 8 |
| Tang, 2013 43 | Taiwan | 193 | Longitudinal | Any type | IV | Family caregiver | CES‐D 20 (≥16 out of 60) | 106/193 = 55% | 8 |
| Yang, 2012 63 | China | 312 | CS | Any type | IV | Spousal/family caregiver | CES‐D 20 (≥16 out of 60) | 198/312 = 63.5% | 8 |
| Jaafar, 2014 49 | Malaysia | 130 | CS | Breast cancer | I‐IV | Any family member | DASS‐21 (NA) | 64/130 = 49.2% | 9 |
| Gotze, 2014 50 | Germany | 106 | CS | Any type | I‐IV | Family caregiver | HADS‐D (≥10) | 30/106 = 28% | 9 |
| Leroy, 2015 51 | France | 60 | CS | Any type | I‐IV | Family caregiver | HADS‐D (≥10) | 27/60 = 45% | 7 |
| Park, 2013 64 | South Korea | 897 | CS | Any type | I‐IV | Family caregiver | HADS‐D (≥8) | 737/897 = 82.2% | 9 |
| Yu, 2017 65 | China | 309 | CS | Leukemia | I‐IV | Family caregiver | HADS‐D (≥8) | 65/309 = 21% | 8 |
| Nielsen, 2017a 34 | Denmark | 2743 | CS | Any type | IV | Family caregiver | BDI‐II (21 item) (NA) | 473/2743 = 17.2% | 8 |
| Nielsen, 2017b 66 | Denmark | 1989 | CS | Any type | IV | Family caregiver | BDI‐II (21 item) (NA) | 312/1989 = 15.6% | 8 |
| Rhee, 2008 57 | South Korea | 310 | CS | Any type | I‐IV | Family caregiver | BDI (>13) | 207/310 = 67% | 7 |
| Trevino, 2018 36 | USA | 540 | CS | Any type | I‐IV | Family caregiver | HADS‐D (≥10) | 22/518 = 4.2% | 8 |
| Mhaidat, 2011 52 | Jordan | 302 | CS | Any type | I‐IV | Family caregiver | HADS‐D (≥8) | 247/302 = 82% | 7 |
| Catende, 2017 53 | Uganda | 119 | CS | Any type | I‐IV | Family caregiver | HDS‐D (≥11) | 31/119 = 26% | 8 |
| Sahadevan, 2019 54 | India | 384 | CS | Breast cancer | I‐IV | Family caregiver | HAM‐D (≥8) | 202/384 = 53% | 8 |
| Lutfi M, 2019 55 | Iraq | 250 | CS | Leukemia | I‐IV | Family caregiver | BDI‐II (≥17) | 180/250 = 72% | 7 |
Abbreviations: CS, Cross‐sectional, NA, Data not available.
Of the thirty five studies included, ten studies were from USA, 33 , 35 , 37 , 38 , 44 , 45 , 46 four studies from South Korea, and two studies each from Canada, Australia, Denmark, China, Taiwan and Turkey. Also, one study from each of the following countries namely, Norway, 47 Iran, 48 The Netherlands, 39 Malaysia, 49 Germany, 50 France, 51 Jordan, 52 Uganda, 53 India 54 and Iraq. 55
Regarding the tool used to screen/diagnose depression, nineteen studies have used the Center for Epidemiological Studies‐Depression (CES‐D‐20), eight studies used Hospital Anxiety and Depression scale (HADS‐D), four studies used the Beck Depression Inventory (BDI), one study each used ‘Indice de détresse psychologique de Santé Québec (IDPESQ)’, fourth version of the Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV), Depression Anxiety Stress scale and Hamilton rating scale for depression (HAM‐D).
3.3. The quality of studies included in the review
The methodological quality of studies included in this review was assessed by the modified version of the Newcastle‐Ottawa Scale. 28 Of the total thirty‐five studies checked for methodological quality, twenty‐two (64.5%), nine (19.4%), and four studies (12.9%) were of high (NOS score ≥8), moderate (NOS score 6–7) and low methodologic quality, respectively (Table 1).
3.4. Meta‐analysis
Globally, the pooled prevalence of depression among caregivers of Cancer patients was 42.08% (95% CI: 34.71–49.45) and the observed heterogeneity was substantial (I 2 = 99.09%, Q = 5463.56, p < 0.001) (Figure 2).
FIGURE 2.
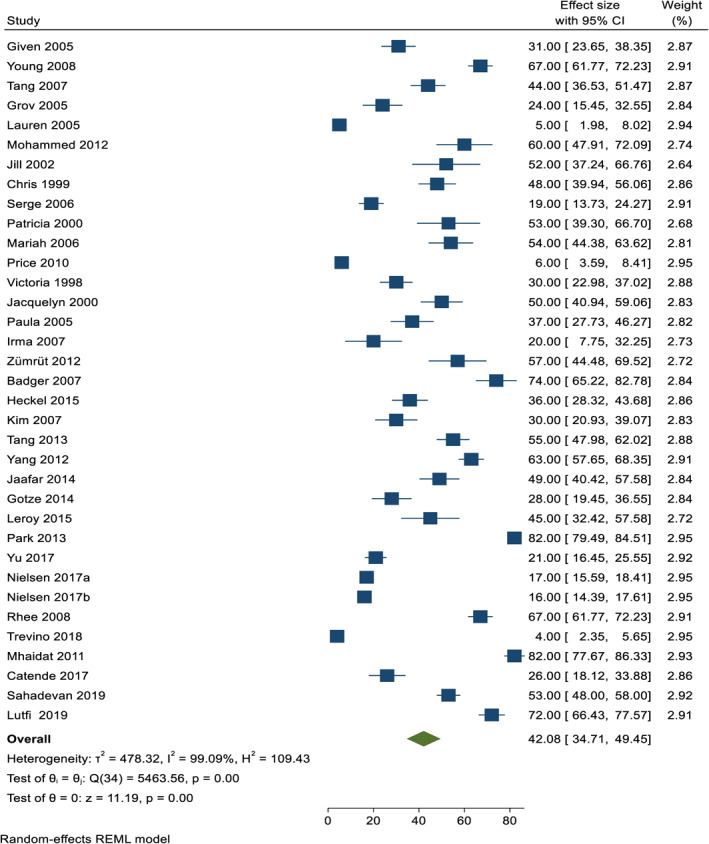
Fore plot showing the pooled prevalence of depression among caregivers of cancer patients
3.5. Subgroup analysis and publication bias
Table 2 has presented the findings of subgroup analysis. The prevalence of depression that was noted in this review was diverse by the methodological designs the studies followed, the tools the studies used to measure depression, the stages of cancer, and the gender of participants.
TABLE 2.
Subgroup analysis for the prevalence of depression among caregivers of cancer patients
| Subgroups | No. of studies | Prevalence (%) | 95% CI | Heterogeneity within the study (I 2 statistics (%)) |
|---|---|---|---|---|
| Types of tools used to assess depression | ||||
| BDI | 4 | 65.3 | 58.5–72.0 | 63.7 |
| CES‐D | 19 | 42.5 | 31.9–53.09 | 97.8 |
| HADS‐D | 8 | 34.4 | 21.0–47.8 | 99.5 |
| IDPESQ | 1 | 19 | 13.7–24.3 | 0.00 |
| DSM‐IV | 1 | 5 | 1.98–8.02 | 0.00 |
| DASS‐21 | 1 | 82 | 79.4–84.5 | 0.00 |
| HAM‐D | 1 | 53% | 48.0–47.9 | 0.00 |
| Study design used | ||||
| Cross‐sectional | 28 | 42.2 | 33.8–54.6 | 99.4 |
| Longitudinal | 7 | 33.6 | 17.7–49.6 | 98.7 |
| Gender of study participants | ||||
| Male | 4 | 34.4 | 12.4–66.1 | 97.4 |
| Female | 4 | 57.6 | 29.5–81.5 | 90.03 |
| Stage of cancer | ||||
| Terminal stage (stage 3 and 4) | 12 | 38.64 | 27.67–49.62 | 98.97 |
| Others | 23 | 43.82 | 34.10–53.54 | 98.93 |
The pooled prevalence of depression among caregivers of cancer patients differed when the methodological designs of the studies varied. For example, the pooled prevalence of depression in the studies that used a cross‐sectional study design (42.2%) was higher than those studies that have followed a longitudinal study design (33.6%).
Further, the higher prevalence of depression was observed in the studies that used DASS‐21 (82%), followed by BDI (65.3%), and HAM‐D (53%), whereas the lowest pooled prevalence was observed in the study that used DSM‐IV (5%). We further employed a subgroup analysis limiting the analysis to the studies that have reported prevalence for male and female caregivers of cancer patients. A higher prevalence of depression found among female caregivers (57.6%) than males (34.4%). Finally, a subgroup analysis was conducted based on the stages of cancer (terminally ill patient vs. stages one and two). A slightly higher prevalence of depression was observed among caregivers of stage one and stage 2 cancer patients (43.8%, 95% CI: 34.10–53.54) compared to caregivers of terminally ill cancer patients (38.64%, 95% CI: 27.67–49.62).
For the overall meta‐analysis of the prevalence of depression among caregivers of Cancer patients, both the visual inspection of the funnel plot (Figure 3), and Egger's regression, showed no evidence of publication bias (B = 3.05, SE = 2.086, p = 0.144).
FIGURE 3.
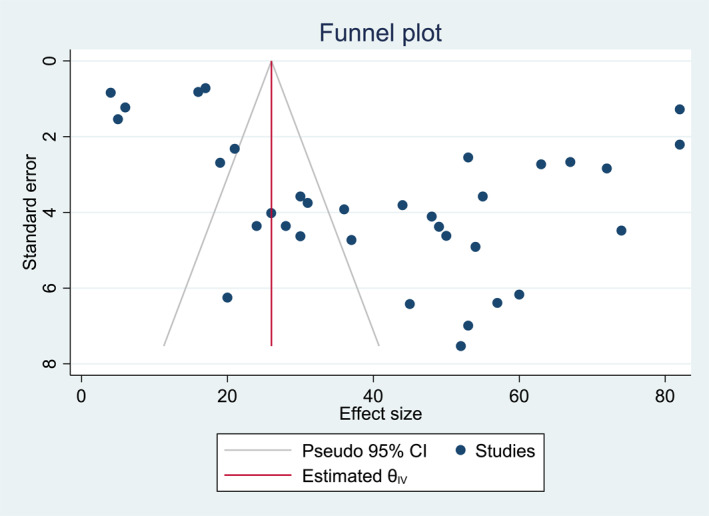
Funnel plot shows no evidence of publication bias among included studies
4. DISCUSSION
Our systematic review and meta‐analysis, estimating the global level pooled prevalence of depression among caregivers of Cancer patients revealed an interesting finding. Thirty five studies, with 11,396 caregivers, conducted across eighteen countries, were included in the current review.
Overall the global prevalence of depression among caregivers of Cancer patients across studies was 42.08% (95% CI: 34.71–49.45). The pooled prevalence in the current review was comparable with a pooled prevalence reported by a previous systematic review and meta‐analysis (42.3%) conducted before 4 years. 20 However, the pooled prevalence of depression in the current study was remarkably higher than the prevalence of depression cases among a general population reported in 2015 (9%). 67 This high prevalence of depression among caregivers of cancer patients might be due to providing care for the patient for long hours per day without getting enough support. 4 , 8 , 9 Besides, those caring for terminal cancer patients may suffer from an even higher burden as the patient's health condition deteriorates, leading caregivers to be physically and emotionally exhausted. 13 Our review also indicated caregivers included in 12 studies (n = 6168) care for terminally ill cancer patients. Furthermore, the unmet need of the patient can also lead caregivers to experience psychological distress. 14
The subgroup analysis conducted using the study design as a moderator demonstrated that the pooled prevalence of depression in the studies that used a cross‐sectional study design (42%) was higher than studies which followed a longitudinal study design (34%). The possible reason for a higher prevalence of depression among cross‐sectional studies might be due to the effect of decreasing participation rates over time on longitudinal studies. 68 Participant non‐response is higher among the most vulnerable members of society, such as those with young age, economically poor and poor health conditions. Therefore the absence of these individuals from longitudinal studies might lower the prevalence of depression, as these individuals are most likely to experience poor mental health. Second, the sample size of the studies which employed a cross‐sectional design had 9627 caregivers of cancer patients compared to that of studies that used a longitudinal study design (n = 1374). Of these twenty eight cross‐sectional studies, ten had only caregivers of terminally ill cancer patients (stage III and IV) (n = 5775) who may suffer a higher burden as the patient's health condition deteriorates. In contrast, of the total seven studies that used a longitudinal design, only two included caregivers of terminally ill cancer patients (n = 393). This finding suggests the need for further studies examining depression among caregivers of cancer patients at different stages of illness with representative sample size and robust study design.
The subgroup analysis conducted using the tool employed to identify depression have showed substantial variation across studies among caregivers of cancer patients. Most importantly, the higher prevalence of depression was observed in the studies that used DASS‐21 (82%), followed by BDI (65.3%), and HAM‐D (53%), whereas the lowest pooled prevalence was observed in the study that used DSM‐IV (5%). This might be due to many studies included in the current meta‐analysis used CES‐D (i.e., 19 out of 35 studies (54.3%)) and BDI (i.e., 4 out of 31 studies (11.4%)) to examine depressive symptoms across studies, which is a highly sensitive screening tool compared to others, 69 suggesting the possibility of overestimation of depression rate. DASS‐21 is also a screening tool for probable depressive symptoms, which is highly sensitive in case detection compared to DSM‐IV, a diagnostic tool. Besides, the observed variation might be due to the difference in the psychometric properties of measures employed across studies.
Our subgroup analysis indicated that the prevalence of depression among female caregivers (57.6%) was higher than that of males (34.4%). The higher prevalence of depression among female caregivers could be because females are highly exposed to sexual violence and have a higher rate of experiencing mental health problems such as depression than males. 70 Also, the diatheses stress model of depression indicated a preponderance of depression among female caregivers, making them more susceptible to depression when facing stressful life events. 71 Furthermore, biological theories suggest that the genetic susceptibility of depression is also higher among females compared to males. 72 , 73 The result suggests more emphasis should be given to female caregivers of cancer patients.
4.1. Clinical implications
Our review had important clinical and research implications. Firstly, our review indicated a higher prevalence of depression among caregivers of cancer patients, which suggests the importance of screening depressive symptoms and implementation of evidence‐based interventions. Secondly, further studies should be conducted to examine the possible reasons for a higher prevalence of depression among caregivers of Cancer patients. Thirdly, our sub‐group analysis shown a difference in the prevalence of depression across male and female caregivers, however further studies are essential to strengthen our findings as we found only eight studies which reported the prevalence of depression for male and females. Finally, future systematic reviews and primary studies examining determinants of depression among caregivers of cancer patients are vital for a better understanding of the epidemiology of depression.
4.2. Study limitations
The following are the limitations of our review, which need to be considered when inferring our findings. First, all the included studies were only from middle and high‐income countries, which lacks representativeness of low‐income countries. Second, we have included only articles published in English, which might introduce selection bias. Third, it is essential to note the difference between depression assessment tools across the studies could also be a potential limitation. Lastly, most studies included in the current review employed a cross‐sectional design, which has the limitation of providing evidence of a temporal relationship between exposure and outcome.
5. CONCLUSION
Our review found that, globally around two in five cancer patient caregivers screened positive for depression, which needs due attention. Early screening of depressive symptoms and targeted psychosocial intervention for caregivers of Cancer patients is highly recommended. Also, expanding on other evidence‐based practices related to addressing depression among caregivers of cancer patients would be beneficial. Further studies should be conducted to examine the possible reasons for a higher prevalence of depression among caregivers of Cancer patients.
AUTHOR CONTRIBUTIONS
The author Asres Bedaso performed the search, quality appraisal, data extraction, analyses, and writing the draft of the initial manuscript. Bereket Duko and Getiye Dejenu participated in quality appraisal, and data extraction. Getiye Dejenu contributed to the consensus. All authors participated in revising the draft manuscript, and approved the final manuscript.
CONFLICT OF INTEREST
The authors declare that there is no competing interest.
Supporting information
Supporting Information S1
ACKNOWLEDGEMENTS
The authors declare that no funding is received for this research work.
Open access publishing facilitated by University of Technology Sydney, as part of the Wiley ‐ University of Technology Sydney agreement via the Council of Australian University Librarians.
Bedaso A, Dejenu G, Duko B. Depression among caregivers of cancer patients: updated systematic review and meta‐analysis. Psychooncology. 2022;31(11):1809‐1820. 10.1002/pon.6045
DATA AVAILABILITY STATEMENT
All data generated or analysed during this study are included in this article.
REFERENCES
- 1. GBD Results Tool . Institute for Health Metrics, University of Washington. 2020. [Google Scholar]
- 2. Aranda S, Peerson A. Caregiving in advanced cancer: lay decision making. J Palliat Care. 2001;17(4):270‐276. 10.1177/082585970101700409 [DOI] [PubMed] [Google Scholar]
- 3. Ugalde A, Krishnasamy M, Schofield P. Development of an instrument to measure self‐efficacy in caregivers of people with advanced cancer. Psycho Oncol. 2013;22(6):1428‐1434. 10.1002/pon.3160 [DOI] [PubMed] [Google Scholar]
- 4. Olson RE. Is cancer care dependent on informal carers? Aust Health Rev. 2012;36(3):254‐257. 10.1071/ah11086 [DOI] [PubMed] [Google Scholar]
- 5. Kim Y, Schulz R. Family caregivers' strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. J Aging Health. 2008;20(5):483‐503. 10.1177/0898264308317533 [DOI] [PubMed] [Google Scholar]
- 6. Hudson P. Positive aspects and challenges associated with caring for a dying relative at home. Int J Palliat Nurs. 2004;10(2):58‐65. 10.12968/ijpn.2004.10.2.12454 [DOI] [PubMed] [Google Scholar]
- 7. Yang X, Hao Y, George SM, Wang L. Factors associated with health‐related quality of life among Chinese caregivers of the older adults living in the community: a cross‐sectional study. Health Qual Life Outcome. 2012;10(1):1‐12. 10.1186/1477-7525-10-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ugalde A, Krishnasamy M, Schofield P. Role recognition and changes to self‐identity in family caregivers of people with advanced cancer: a qualitative study. Support Care Cancer. 2012;20(6):1175‐1181. 10.1007/s00520-011-1194-9 [DOI] [PubMed] [Google Scholar]
- 9. Wolff JL, Dy SM, Frick KD, Kasper JD. End‐of‐life care: findings from a national survey of informal caregivers. Arch Intern Med. 2007;167(1):40‐46. 10.1001/archinte.167.1.40 [DOI] [PubMed] [Google Scholar]
- 10. Heckel L, Fennell K, Reynolds J, et al. Unmet needs and depression among carers of people newly diagnosed with cancer. Eur J Cancer. 2015;51(14):2049‐2057. 10.1016/j.ejca.2015.06.129 [DOI] [PubMed] [Google Scholar]
- 11. Chambers SK, Girgis A, Occhipinti S, et al. Psychological distress and unmet supportive care needs in cancer patients and carers who contact cancer helplines. Eur J Cancer Care. 2012;21(2):213‐223. 10.1111/j.1365-2354.2011.01288.x [DOI] [PubMed] [Google Scholar]
- 12. Mitschke DB. Cancer in the family: review of the psychosocial perspectives of patients and family members. J Fam Soc Work. 2013;11(2):166‐184. 10.1080/10522150802175159 [DOI] [Google Scholar]
- 13. Chang Y‐J, Kwon YC, Lee WJ, et al. Burdens, needs and satisfaction of terminal cancer patients and their caregivers. Asian Pac J Cancer Prev APJCP. 2013;14(1):209‐215. 10.7314/apjcp.2013.14.1.209 [DOI] [PubMed] [Google Scholar]
- 14. Chen S‐C, Tsai M‐C, Liu C‐L, Yu W‐P, Liao C‐T, Chang JT‐C. Support needs of patients with oral cancer and burden to their family caregivers. Cancer Nurs. 2013;32(6):473‐481. 10.1097/ncc.0b013e3181b14e94 [DOI] [PubMed] [Google Scholar]
- 15. Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ (Can Med Assoc J). 2014;170(12):1795‐1801. 10.1503/cmaj.1031205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lund L, Ross L, Petersen MA, Groenvold M. Cancer caregiving tasks and consequences and their associations with caregiver status and the caregiver’s relationship to the patient: a survey. BMC Cancer. 2014;14(1):1‐13. 10.1186/1471-2407-14-541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lambert SD, Harrison JD, Smith E, et al. The unmet needs of partners and caregivers of adults diagnosed with cancer: a systematic review. BMJ Support Palliat Care. 2018;2(3):224‐230. 10.1136/bmjspcare-2012-000226 [DOI] [PubMed] [Google Scholar]
- 18. Hudson PL, Thomas K, Trauer T, Remedios C, Clarke D. Psychological and social profile of family caregivers on commencement of palliative care. J Pain Symptom Manag. 2011;41(3):522‐534. 10.1016/j.jpainsymman.2010.05.006 [DOI] [PubMed] [Google Scholar]
- 19. Hudson P, Trauer T, Kelly B, et al. Reducing the psychological distress of family caregivers of home‐based palliative care patients: short‐term effects from a randomised controlled trial. Psycho Oncol. 2013;22(9):1987‐1993. 10.1002/pon.3242 [DOI] [PubMed] [Google Scholar]
- 20. Geng H‐M, Chuang D‐M, Yang F, et al. Prevalence and determinants of depression in caregivers of cancer patients: a systematic review and meta‐analysis. Medicine. 2018;97(39):e11863. 10.1097/md.0000000000011863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Molassiotis A, Wang M. Understanding and supporting informal cancer caregivers. Curr Treat Options Oncol. 2022;23(4):494‐513. 10.1007/s11864-022-00955-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Applebaum AJ, Breitbart W. Care for the cancer caregiver: a systematic review. Palliat Support Care. 2013;11(3):231‐252. 10.1017/s1478951512000594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Northouse L, Williams A‐l, Given B, McCorkle R. Psychosocial care for family caregivers of patients with cancer. J Clin Oncol. 2012;30(11):1227‐1234. 10.1200/jco.2011.39.5798 [DOI] [PubMed] [Google Scholar]
- 24. Fekete C, Tough H, Siegrist J, Brinkhof MW. Health impact of objective burden, subjective burden and positive aspects of caregiving: an observational study among caregivers in Switzerland. BMJ Open. 2017;7(12):e017369. 10.1136/bmjopen-2017-017369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Adler N, Page A, Institute of Medicine (US). Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting . Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. National Academies Press; 2008. [PubMed] [Google Scholar]
- 26. Schulz R, Eden J, National Academies of Sciences E, Medicine . Family Caregiving Roles and Impacts. Families Caring for an Aging America. National Academies Press (US); 2016. [PubMed] [Google Scholar]
- 27. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015 statement. Syst Rev. 2015;4(1):1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stang A. Critical evaluation of the Newcastle‐Ottawa scale for the assessment of the quality of non randomized studies in meta‐analyses. Eur J Epidemiol. 2010;25(9):603‐605. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 29. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ Clin Res. Ed. 1997;315(7109):629‐634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ioannidis JP. Interpretation of tests of heterogeneity and bias in meta‐analysis. J Eval Clin Pract. 2008;14(5):951‐957. 10.1111/j.1365-2753.2008.00986.x [DOI] [PubMed] [Google Scholar]
- 31. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed‐effect and random‐effects models for meta‐analysis. Res Synth Methods. 2010;1(2):97‐111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 32. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med. 2002;21(11):1539‐1558. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 33. Verdonck‐de Leeuw IM, Eerenstein SE, Van der Linden MH, Kuik DJ, de Bree R, Leemans CR. Distress in spouses and patients after treatment for head and neck cancer. Laryngoscope. 2007;117(2):238‐241. 10.1097/01.mlg.0000250169.10241.58 [DOI] [PubMed] [Google Scholar]
- 34. Nielsen MK, Neergaard MA, Jensen AB, Vedsted P, Bro F, Guldin MB. Preloss grief in family caregivers during end‐of‐life cancer care: a nationwide population‐based cohort study. Psycho Oncol. 2017;26(12):2048‐2056. 10.1002/pon.4416 [DOI] [PubMed] [Google Scholar]
- 35. Raveis VH, Karus DG, Siegel K. Correlates of depressive symptomatology among adult daughter caregivers of a parent with cancer. Cancer. 1998;83(8):1652‐1663. [DOI] [PubMed] [Google Scholar]
- 36. Trevino KM, Prigerson HG, Maciejewski PK. Advanced cancer caregiving as a risk for major depressive episodes and generalized anxiety disorder. Psycho Oncol. 2018;27(1):243‐249. 10.1002/pon.4441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Given B, Wyatt G, Given C, et al. Burden and depression among caregivers of patients with cancer at the end of life. Oncol Nurs Forum. 2004;31(6):1105‐1117. 10.1188/04.onf.1105-1117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vanderwerker LC, Laff RE, Kadan‐Lottick NS, McColl S, Prigerson HG. Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. J Clin Oncol. 2005;23(28):6899‐6907. 10.1200/jco.2005.01.370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nijboer C, Triemstra M, Tempelaar R, Sanderman R, van den Bos GA. Determinants of caregiving experiences and mental health of partners of cancer patients. Cancer. 1999;86(4):577‐588. [DOI] [PubMed] [Google Scholar]
- 40. Dumont S, Turgeon J, Allard P, Gagnon P, Charbonneau C, Vézina L. Caring for a loved one with advanced cancer: determinants of psychological distress in family caregivers. J Palliat Med. 2006;9(4):912‐921. 10.1089/jpm.2006.9.912 [DOI] [PubMed] [Google Scholar]
- 41. Price MA, Butow PN, Costa DS, et al. Prevalence and predictors of anxiety and depression in women with invasive ovarian cancer and their caregivers. Med J Aust. 2010;193(S5):S52‐S57. 10.5694/j.1326-5377.2010.tb03929.x [DOI] [PubMed] [Google Scholar]
- 42. Badger T, Segrin C, Dorros SM, Meek P, Lopez AM. Depression and anxiety in women with breast cancer and their partners. Nurs Res. 2007;56(1):44‐53. 10.1097/00006199-200701000-00006 [DOI] [PubMed] [Google Scholar]
- 43. Tang ST, Chang WC, Chen JS, et al. Course and predictors of depressive symptoms among family caregivers of terminally ill cancer patients until their death. Psycho Oncol. 2013;22(6):1312‐1318. 10.1002/pon.3141 [DOI] [PubMed] [Google Scholar]
- 44. Carter PA, Chang BL. Sleep and depression in cancer caregivers. Cancer Nurs 2000;23(6):410‐415. 10.1097/00002820-200012000-00002 [DOI] [PubMed] [Google Scholar]
- 45. Flaskerud JH, Carter PA, Lee P. Distressing emotions in female caregivers of people with AIDS, age‐related dementias, and advanced‐stage cancers. Psychiatr Care. 2000;36(4):121‐130. 10.1111/j.1744-6163.2000.tb00600.x [DOI] [PubMed] [Google Scholar]
- 46. Sherwood PR, Given BA, Given CW, et al. Predictors of distress in caregivers of persons with a primary malignant brain tumor. Res Nurs Health. 2006;29(2):105‐120. 10.1002/nur.20116 [DOI] [PubMed] [Google Scholar]
- 47. Grov EK, Dahl AA, Moum T, Fosså SD. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Ann Oncol. 2005;16(7):1185‐1191. 10.1093/annonc/mdi210 [DOI] [PubMed] [Google Scholar]
- 48. Heidari Gorji MA, Bouzar Z, Haghshenas M, Kasaeeyan AA, Sadeghi MR, Ardebil MD. Quality of life and depression in caregivers of patients with breast cancer. BMC Res Notes. 2012;5(1):310. 10.1186/1756-0500-5-310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Jaafar NRN, Din SHS, Saini SM, et al. Clinical depression while caring for loved ones with breast cancer. Compr Psychiatr. 2014;55:S52‐S9. 10.1016/j.comppsych.2013.03.003 [DOI] [PubMed] [Google Scholar]
- 50. Götze H, Brähler E, Gansera L, Polze N, Köhler N. Psychological distress and quality of life of palliative cancer patients and their caring relatives during home care. Support Care Cancer. 2014;22(10):2775‐2782. 10.1007/s00520-014-2257-5 [DOI] [PubMed] [Google Scholar]
- 51. Leroy T, Fournier E, Penel N, Christophe V. Crossed views of burden and emotional distress of cancer patients and family caregivers during palliative care. Psycho Oncol. 2016;25(11):1278‐1285. 10.1002/pon.4056 [DOI] [PubMed] [Google Scholar]
- 52. Mhaidat NM, Ai‐Sweedan SA, Alzoubi KH, et al. Prevalence of depression among relatives of cancer patients in Jordan: a cross‐sectional survey. Palliat Support Care. 2011;9(1):25‐29. 10.1017/s1478951510000519 [DOI] [PubMed] [Google Scholar]
- 53. Katende G, Nakimera L. Prevalence and correlates of anxiety and depression among family carers of cancer patients in a cancer care and treatment facility in Uganda: a cross‐sectional study. Afr Health Sci. 2017;17(3):868‐876. 10.4314/ahs.v17i3.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Sahadevan S, Namboodiri V. Depression in caregivers of patients with breast cancer: a cross‐sectional study from a cancer research center in South India. Indian J Psychiatr. 2019;61(3):277‐282. 10.4103/psychiatry.indianjpsychiatry_46_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lutfi NM, Al Lami F. Prevalence and determinants of depression among caregivers of children with leukaemia in Iraq. East Mediterr Health J. 2019;25(6):385‐393. 10.26719/emhj.19.005 [DOI] [PubMed] [Google Scholar]
- 56. Given B, Wyatt G, Given C, et al. eds. Burden and depression among caregivers of patients with cancer at the end‐of‐life NIH Public Access. Oncology Nursing Forum; 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rhee YS, Yun YH, Park S, et al. Depression in family caregivers of cancer patients: the feeling of burden as a predictor of depression. J Clin Oncol. 2008;26(36):5890‐5895. 10.1200/jco.2007.15.3957 [DOI] [PubMed] [Google Scholar]
- 58. Tang ST, Li CY, Liao YC. Factors associated with depressive distress among Taiwanese family caregivers of cancer patients at the end of life. Palliat Med. 2007;21(3):249‐257. 10.1177/0269216307077334 [DOI] [PubMed] [Google Scholar]
- 59. Cameron JI, Franche RL, Cheung AM, Stewart DE. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. 2002;94(2):521‐527. 10.1002/cncr.10212 [DOI] [PubMed] [Google Scholar]
- 60. Cho MH, Dodd MJ, Lee KA, Padilla G, Slaughter R. Self‐reported sleep quality in family caregivers of gastric cancer patients who are receiving chemotherapy in Korea. J Cancer Educ. 2006;21(1 Suppl):S37‐S41. 10.1207/s15430154jce2101s_8 [DOI] [PubMed] [Google Scholar]
- 61. Şahin ZA, Tan M. Loneliness, depression, and social support of patients with cancer and their caregivers. Clin J Oncol Nurs. 2012;16(2):145‐149. 10.1188/12.cjon.145-149 [DOI] [PubMed] [Google Scholar]
- 62. Kim Y, Kashy DA, Evans TV. Age and attachment style impact stress and depressive symptoms among caregivers: a prospective investigation. J Cancer Survivorship Res Pract. 2007;1(1):35‐43. 10.1007/s11764-007-0011-4 [DOI] [PubMed] [Google Scholar]
- 63. Yang X, Wang L, He J, et al. Factors related to depressive symptoms among Chinese caregivers of cancer patients. Psycho Oncol. 2012;21(10):1063‐1070. 10.1002/pon.1999 [DOI] [PubMed] [Google Scholar]
- 64. Park B, Kim SY, Shin J‐Y, et al. Suicidal ideation and suicide attempts in anxious or depressed family caregivers of patients with cancer: a nationwide survey in Korea. PLoS One. 2013;8(4):e60230. 10.1371/journal.pone.0060230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Yu H, Li L, Liu C, et al. Factors associated with the quality of life of family caregivers for leukemia patients in China. Health Qual Life Outcome. 2017;15(1):1‐11. 10.1186/s12955-017-0628-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Nielsen MK, Neergaard MA, Jensen AB, Vedsted P, Bro F, Guldin M.‐B. Predictors of complicated grief and depression in bereaved caregivers: a nationwide prospective cohort study. J Pain Symptom Manag. 2017;53(3):540‐550. 10.1016/j.jpainsymman.2016.09.013 [DOI] [PubMed] [Google Scholar]
- 67. Organization WH . Depression and Other Common Mental Disorders: Global Health Estimates. World Health Organization; 2017. [Google Scholar]
- 68. Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17(9):643‐653. 10.1016/j.annepidem.2007.03.013 [DOI] [PubMed] [Google Scholar]
- 69. Behera P, Pilania M, Yadav V, et al. A Systematic Review Protocol for Estimation of the Prevalence of Depression Using Diagnostic Instruments in the Elderly Population in India, 2000‐2019. medRxiv; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci JPN. 2015;40(4):219‐221. 10.1503/jpn.150205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Girgus JS, Yang K, Ferri CV. The gender difference in depression: are elderly women at greater risk for depression than elderly men? Geriatrics. 2017;2(4):35. 10.3390/geriatrics2040035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Christiansen DM, Berke ET. Gender and sex‐based contributors to sex differences in PTSD. Curr Psychiatr Rep. 2020;22(4):19. 10.1007/s11920-020-1140-y [DOI] [PubMed] [Google Scholar]
- 73. Hyde JS, Mezulis AH. Gender differences in depression: biological, affective, cognitive, and sociocultural factors. Harv Rev Psychiatr. 2020;28(1):4‐13. 10.1097/hrp.0000000000000230 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Data Availability Statement
All data generated or analysed during this study are included in this article.


