Abstract
Background:
Increases in fatal synthetic opioid overdoses over the past 8 years have left states scrambling for effective means to curtail these deaths. Many states have implemented policies and increased service capacity to address this rise. To better understand the effectiveness of policy level interventions we estimated the impact of the presence of naloxone access laws (NALs) on synthetic opioid fatalities at the state level.
Methods:
A multivariable longitudinal linear mixed model with a random intercept was used to determine the relationship between the presence of NALs and synthetic opioid overdose death rates, while controlling for, Good Samaritan laws, opioid prescription rate, and capacity for medication for opioid use disorder (MOUD), utilizing a quadratic time trajectory. Data for the study was collected from the National Vital Statistics System using multiple cause-of-death mortality files linked to drug overdose deaths.
Results:
The presence of an NAL had a significant (univariate P-value = .013; multivariable p-value = .010) negative relationship to fentanyl overdose death rates. Other significant controlling variables were quadratic time (univariate and multivariable P-value < .001), MOUD (univariate P-value < .001; multivariable P-value = .009), and Good Samaritan Law (univariate P-value = .033; multivariable P-value = .018).
Conclusion:
Naloxone standing orders are strongly related to fatal synthetic opioid overdose reduction. The effect of NALs, MOUD treatment capacity, and Good Samaritan laws all significantly influenced the synthetic opioid overdose death rate. The use of naloxone should be a central part of any state strategy to reduce overdose death rate.
Keywords: drug policy, opioids, synthetic opioids, naloxone, naloxone access laws, medication for opioid use disorder
Introduction
Overdose rates involving fentanyl rose from 1.0 per 100 000 in 2013 to 11.4 per 100 000 in 2019, a more than ten-fold increase.1 Fentanyl is a synthetic opioid that is both illicitly and legally produced and is between 50 and 100 times stronger than morphine.2 Fentanyl has been linked to the recent increase in drug overdose deaths.2-12 Analyses of state fatal opioid overdose rates have implicated illicitly manufactured fentanyl (IMF) (which includes multiple analogs) as a driver of increased overdose death rates overall.2,5,10-12 Fentanyl, whether illicitly or legally produced, is captured in the category of synthetic opioids (excluding methadone) in the CDC analyses of opioid overdose rates. While nationally fatal opioid overdose rates went down 2%, and prescription opioids and heroin death rates went down, 13.5% and 4.1% respectively from 2017 to 2018, fatal synthetic opioid overdose rose 10%.13 This is likely driven by increases in IMF.10-14 In 2019, the number of drug overdose deaths reached 70 630 in the United States.15 When adjusting for age, the opioid overdose death rate per 100 000 increased from 20.7 in 2018 to 21.6 in 2019.16
As opioid overdose deaths have risen, attention has focused on systemic means to reduce this tragic trend. Medication for opioid use disorder (MOUD) is the use of medications to treat opioid use disorder.17 MOUD includes full and partial agonist treatments (methadone and buprenorphine) as well as the opioid antagonist treatment (naltrexone) and are typically provided in combination with behavioral counseling. Methadone and buprenorphine have been shown to increase treatment retention, reduce illicit opioid use, and subsequently reduce fatal opioid overdose.18 Another pharmacological intervention for opioid overdose fatality reduction is naloxone. Naloxone is a pure competitive opioid antagonist that has a stronger affinity to the mu-opioid receptor than opioids, including fentanyl. When naloxone is injected or sprayed into the nose of a person experiencing respiratory depression due to opioid overdose, the active opioids attached to the mu-opioid receptor are supplanted by naloxone, effectively stopping the respiratory depression and averting subsequent death, and importantly when used on a person that has not taken opioids there is no identified adverse effect.19 This intervention has demonstrated an association with decreased fatal opioid overdose in at least 2 studies and is a key intervention for overdose prevention.20,21
Naloxone has been used for over 50 years to reverse opioid overdose. However, due to the rise in opioid overdose in the past 20 years, the use of naloxone has changed. It is now available without a prescription in 43 states, and its availability has extended to non-medically trained workers, such as community health workers and police, as well as by laypeople including opioid users.22 In fact, in 2013 a total of 140 048 doses of naloxone were distributed to laypeople by 50 harm reduction agencies located nationwide that are regularly tracked by the national Harm Reduction Coalition. The Department of Health and Human Services (DHHS) declared expanded use and distribution of naloxone as one of 3 priority areas to reduce opioid overdose, and as such, assessing the impact of this potentially lifesaving intervention is critical.23 This expansion of distribution is in large part due to states adopting naloxone access laws (NALs) for all people to access naloxone without a prescription. These laws involve documents signed by a medical professional (ie, physician, nurse practitioner, or pharmacist) that allow all citizens of the state to access naloxone without a prescription. While the U.S. Surgeon General and the DHHS indicate that all community members that encounter people at risk for overdose should have access to and knowledge of how to administer naloxone, states can institute naloxone distribution policies in different ways, and these differences could affect the outcomes of the policy. For instance, some state policies indicate laypeople are immune from criminal liability when administering naloxone, while others do not, and the lack of immunity might well be seen as a disincentive to administer naloxone.
It is particularly important to assess the impact of macro-level variables, such as the impact of NALs, Good Samaritan Laws, and availability of MOUD on fatal synthetic opioid overdose as at this point fentanyl involved overdose deaths are rising. Identifying the impact of each intervention on fatal overdose due to use of different categories of opioids (ie, heroin, semi-synthetic, and synthetic) is also key to developing successful overdose prevention strategies. In this study we utilized publicly available data to assess the impact of NALs, Good Samaritan Laws, availability of MOUD, and opioid prescription rates on fatal synthetic opioid overdose. After extensive review of similar studies, the impact of the variables in this study have been examined but never in combination,24-33 nor with a focus on the category of overdose fatality (synthetic opioid overdose) that is growing most rapidly in the US today. We utilized data from 14 years of overdose records for each state to assess the relationships of these interventions to the rate of overdose.
Materials and Methods
A multivariable longitudinal linear mixed model with a random intercept was used to determine the relationship between the presence of NALs and synthetic opioid overdose death rates, while controlling for, Good Samaritan laws, opioid prescription rate, and capacity for medication for opioid use disorder (MOUD), utilizing a quadratic time trajectory. All overdose death data was collected through the Kaiser Family Foundation. This data was retrieved from the National Vital Statistics System using multiple cause-of-death mortality files to identify drug overdose deaths. Drug overdose deaths were classified using the International Classification of Disease, Tenth Revision (ICD-10), based on the ICD-10 underlying cause-of-death codes X40–44 (unintentional), X60–64 (suicide), X85 (homicide), or Y10–Y14 (undetermined intent). Among the deaths with drug overdose as the underlying cause, we selected the ICD-10 cause-of-death code T40.3 or synthetic opioids, other than methadone. Deaths from IMF cannot be distinguished from pharmaceutical fentanyl in the data source, and as such, deaths from both legally prescribed and illegally produced fentanyl are included in these data.
State law data were obtained from the Prescription Drug Abuse Policy System, a National Institute on Drug Abuse funded system maintained by the Center of Public Health Law Research at Temple University that was created to track key state laws related to prescription drug use. Laws codifying NALs differ greatly by jurisdiction, we created a binary variable indicating the presence or absence of an NAL in each state. Specific details of the law were not identified for this variable. NALs have been shown to increase the amount of naloxone in a community,32 thus the presence of such laws should decrease the number of synthetic opioid overdoses. The specific implementation of good Samaritan laws also varies by state, we created a binary variable of whether a state had any version of this law in a specific year. Good Samaritan laws are designed to incentivize calling medical professionals during an overdose by offering partial or full immunity from drug possession charges. Previous studies have indicated the efficacy of Good Samaritan laws are mixed,34-36 with some studies finding no effect, and at least one finding people with knowledge of these laws were more likely to call 911 in the case of an overdose.37-40 States may find a reduction in overdoses due to an increase in the number of paramedics being requested. The number of MOUD facilities were collected from amfAR’s, End the HIV Epidemic Plan website. This is a measure of the number of facilities in a state that offer either methadone, buprenorphine, naltrexone, or any combination of the 3 types of MOUD. In our study we operationalized this variable as the rate of facilities per 100 000 offering any of the aforementioned. Individuals engaging in care to reduce illicit opioid use, in theory, should result in an opioid overdose decrease. Finally, we use opioid prescriptions as a proxy for supply of semisynthetic opioids. When prescriptions are reduced rapidly, many individuals will seek illicit ways of acquiring opioids increasing the potential for overdose due to lack of knowledge of the composition of the drug.41,42
Analysis
Thirteen states were excluded from analysis due to counts of missing data which exceeded the statistical norm and prohibited the appropriate application of multiple imputations. A total of 518 observations from 37 states over 14 years (2006-2019) were included. Univariate analysis was applied first to provide a description of overdose rates across states by time. Subsequently, we used univariate analysis to identify relationships between the central outcome variable (NAL) as well as all the co-variates and synthetic opioid overdose. These univariate relationships were used to assist in designing a multivariable longitudinal mixed effect model with a quadratic time trajectory. After observing the time-dependent pattern of the synthetic opioid overdose death rate by examining its’ scatterplots, we observed that a quadratic time pattern would be more appropriate to best fit the data. Univariate and multivariable longitudinal mixed models were used to examine the effect of NALs on the synthetic opioid overdose death rate. To capture variation across states we used the random intercept model, while controlling for rate of facilities, offering any form of MOUD, Good Samaritan law status, opioid prescription rate, and quadratic time. Interactions between variables were tested and model fit was examined. All variable rates used in this study are per 100 000.
Results
Univariate Analysis
Table 1 indicates the rate of synthetic overdose in each state as well as the mean number of MOUD provider facilities, and opioid prescription rate per 100 000. The mean synthetic opioid death rate for all states across all years in the analysis is 3.79 deaths per 100 000 with a standard deviation of 6.08. With respect to synthetic opioid overdose death, West Virginia had the highest mean (mean = 12.40) and median (median = 5.42) rate among all 37 states from 2006 to 2019. Texas had the lowest mean synthetic opioid overdose death rate (mean = 0.72). California and Louisiana tied for the lowest median synthetic opioid overdose death rate (median = 0.52). Regarding opioid prescription rates, Alabama had the highest mean opioid prescription rate (mean = 123.14) and West Virginia had the highest median opioid prescription rate (median = 129.45). The state of New York had both the lowest mean (mean = 44.83) and median (median = 45.60) opioid prescription rates.
Table 1.
Descriptive Statistics for Continuous Variables.
| Territory | Variable name | Mean (±SD) | 95% CI | Median | Min | Max |
|---|---|---|---|---|---|---|
| US | Synthetic death rate | 3.79 (±6.08) | (3.26, 4.31) | 1.25 | 0.23 | 34.03 |
| MOUD | 1.03 (±0.75) | (0.96, 1.09) | 0.84 | 0 | 4.43 | |
| Opioid prescription rate | 80.24 (±24.61) | (78.11, 82.36) | 77.20 | 30.90 | 146.90 | |
| Alabama | Synthetic death rate | 1.51 (±1.47) | (0.66, 2.36) | 0.68 | 0.33 | 4.34 |
| MOUD | 0.71 (±0.26) | (0.56, 0.86) | 0.62 | 0.39 | 1.13 | |
| Opioid prescription rate | 123.14 (±16.78) | (113.46, 132.83) | 125.55 | 85.80 | 143.80 | |
| Arizona | Synthetic death rate | 2.28 (±3.09) | (0.49, 4.06) | 0.88 | 0.55 | 10.94 |
| MOUD | 1.24 (±0.60) | (0.89, 1.59) | 1.16 | 0.44 | 2.38 | |
| Opioid prescription rate | 74.36 (±13.63) | (66.48, 82.23) | 78.75 | 44.10 | 88.60 | |
| Arkansas | Synthetic death rate | 1.66 (±0.89) | (1.14, 2.17) | 1.37 | 0.68 | 3.81 |
| MOUD | 0.40 (±0.25) | (0.25, 0.54) | 0.37 | 0.07 | 0.93 | |
| Opioid prescription rate | 110.63 (±12.27) | (103.54, 117.72) | 114.90 | 80.90 | 123.20 | |
| California | Synthetic death rate | 0.96 (±1.07) | (0.34, 1.57) | 0.52 | 0.38 | 4.24 |
| MOUD | 0.78 (±0.23) | (0.64, 0.91) | 0.82 | 0.31 | 1.10 | |
| Opioid prescription rate | 49.20 (±8.42) | (44.34, 54.06) | 53.15 | 30.90 | 56.40 | |
| Colorado | Synthetic death rate | 1.52 (±0.95) | (0.97, 2.08) | 1.29 | 0.57 | 4.43 |
| MOUD | 1.05 (±0.70) | (0.64, 1.45) | 0.92 | 0.17 | 2.11 | |
| Opioid prescription rate | 63.38 (±10.58) | (57.27, 69.48) | 66.80 | 40.00 | 73.50 | |
| Connecticut | Synthetic death rate | 6.75 (±9.36) | (1.35, 12.16) | 1.05 | 0.31 | 26.65 |
| MOUD | 1.97 (±0.94) | (1.42, 2.51) | 1.63 | 1.00 | 3.78 | |
| Opioid prescription rate | 61.41 (±10.18) | (55.53, 67.29) | 66.70 | 40.50 | 69.30 | |
| Florida | Synthetic death rate | 3.71 (±4.44) | (1.15, 6.27) | 0.97 | 0.71 | 13.21 |
| MOUD | 0.67 (±0.40) | (0.44, 0.90) | 0.57 | 0.19 | 1.42 | |
| Opioid prescription rate | 72.76 (±12.74) | (65.41, 80.12) | 74.70 | 45.40 | 87.60 | |
| Georgia | Synthetic death rate | 1.76 (±1.31) | (1.00, 2.51) | 0.97 | 0.60 | 4.02 |
| MOUD | 0.73 (±0.27) | (0.57, 0.89) | 0.73 | 0.26 | 1.18 | |
| Opioid prescription rate | 80.36 (±9.95) | (74.61, 86.10) | 83.15 | 57.90 | 90.20 | |
| Illinois | Synthetic death rate | 3.85 (±4.71) | (1.31, 6.58) | 0.94 | 0.65 | 13.46 |
| MOUD | 1.00 (±0.40) | (0.77, 1.23) | 0.95 | 0.36 | 1.69 | |
| Opioid prescription rate | 57.94 (±6.99) | (53.90, 61.97) | 59.70 | 43.10 | 66.10 | |
| Indiana | Synthetic death rate | 3.38 (±4.45) | (0.81, 5.95) | 0.92 | 0.52 | 13.35 |
| MOUD | 0.89 (±0.61) | (0.53, 1.24) | 0.73 | 0.17 | 2.15 | |
| Opioid prescription rate | 93.22 (±16.16) | (83.89, 102.55) | 98.20 | 60.40 | 110.50 | |
| Iowa | Synthetic death rate | 1.45 (±0.87) | (0.95, 1.95) | 1.16 | 0.54 | 3.23 |
| MOUD | 0.50 (±0.44) | (0.25, 0.76) | 0.28 | 0.10 | 1.39 | |
| Opioid prescription rate | 61.60 (±8.76) | (56.54, 66.66) | 61.35 | 43.00 | 74.10 | |
| Kansas | Synthetic death rate | 1.17 (±0.53) | (0.86, 1.48) | 1.17 | 0.63 | 2.57 |
| MOUD | 0.87 (±0.49) | (0.58, 1.16) | 0.88 | 0.14 | 1.68 | |
| Opioid prescription rate | 79.91 (±8.59) | (74.95, 84.87) | 81.65 | 63.70 | 90.30 | |
| Kentucky | Synthetic death rate | 6.10 (±6.79) | (2.17, 10.02) | 1.73 | 0.87 | 18.47 |
| MOUD | 1.11 (±0.92) | (0.58, 1.64) | 0.70 | 0.14 | 3.00 | |
| Opioid prescription rate | 113.43 (±22.49) | (100.44, 126.41) | 117.15 | 72.30 | 137.00 | |
| Louisiana | Synthetic death rate | 1.54 (±2.04) | (0.36, 2.72) | 0.52 | 0.23 | 6.97 |
| MOUD | 0.57 (±0.35) | (0.36, 0.77) | 0.42 | 0.16 | 1.29 | |
| Opioid prescription rate | 100.35 (±13.19) | (95.74, 110.96) | 109.65 | 74.60 | 113.70 | |
| Maryland | Synthetic death rate | 8.76 (±12.02) | (1.83, 15.70) | 1.26 | 0.62 | 31.71 |
| MOUD | 2.32 (±0.81) | (1.86, 2.79) | 2.35 | 0.76 | 3.57 | |
| Opioid prescription rate | 62.13 (±9.67) | (56.55, 67.71) | 64.40 | 42.30 | 72.90 | |
| Massachusetts | Synthetic death rate | 9.25 (±10.96) | (2.92, 15.58) | 1.42 | 0.83 | 27.00 |
| MOUD | 1.92 (±0.82) | (1.44, 2.39) | 1.78 | 0.70 | 3.33 | |
| Opioid prescription rate | 57.59 (±12.84) | (50.17, 65.00) | 64.35 | 35.30 | 69.20 | |
| Michigan | Synthetic death rate | 4.79 (±5.78) | (1.45, 8.13) | 1.37 | 0.71 | 15.32 |
| MOUD | 0.96 (±0.33) | (0.78, 1.15) | 1.03 | 0.29 | 1.41 | |
| Opioid prescription rate | 86.52 (±13.37) | (78.80, 94.24) | 90.20 | 58.00 | 100.70 | |
| Minnesota | Synthetic death rate | 1.50 (±1.53) | (0.61, 2.38) | 0.74 | 0.48 | 5.48 |
| MOUD | 1.03 (±0.53) | (0.72, 1.34) | 0.99 | 0.17 | 1.75 | |
| Opioid prescription rate | 51.52 (±9.36) | (46.12, 56.93) | 55.10 | 32.10 | 60.90 | |
| Mississippi | Synthetic death rate | 1.40 (±1.17) | (0.72, 2.07) | 0.94 | 0.38 | 4.74 |
| MOUD | 0.38 (±0.26) | (0.23, 0.53) | 0.34 | 0.00 | 0.87 | |
| Opioid prescription rate | 106.41 (±16.58) | (96.84, 115.99) | 112.05 | 67.00 | 121.80 | |
| Missouri | Synthetic death rate | 4.40 (±4.97) | (1.53, 7.27) | 1.70 | 0.93 | 14.44 |
| MOUD | 1.02 (±0.73) | (0.60, 1.44) | 0.85 | 0.15 | 2.01 | |
| Opioid prescription rate | 82.92 (±11.20) | (76.46, 89.39) | 85.65 | 58.30 | 95.40 | |
| Nevada | Synthetic death rate | 1.59 (±0.82) | (1.12, 2.07) | 1.29 | 0.88 | 3.70 |
| MOUD | 0.60 (±0.18) | (0.50, 0.70) | 0.64 | 0.34 | 0.86 | |
| Opioid prescription rate | 85.06 (±15.68) | (76.00, 94.11) | 90.15 | 49.40 | 100.30 | |
| New Hampshire | Synthetic death rate | 11.02 (±11.99) | (4.10, 17.95) | 2.16 | 1.06 | 28.46 |
| MOUD | 1.37 (±0.92) | (0.83, 1.90) | 1.02 | 0.38 | 3.02 | |
| Opioid prescription rate | 71.45 (±15.10) | (62.73, 80.17) | 79.05 | 38.10 | 83.70 | |
| New Mexico | Synthetic death rate | 2.42 (±1.88) | (1.34, 3.51) | 1.50 | 0.95 | 7.11 |
| MOUD | 1.22 (±0.71) | (0.81, 1.63) | 1.25 | 0.20 | 2.29 | |
| Opioid prescription rate | 67.49 (±11.36) | (60.93, 74.04) | 70.60 | 43.40 | 81.90 | |
| New York | Synthetic death rate | 3.87 (±4.61) | (1.21, 6.53) | 0.99 | 0.59 | 12.02 |
| MOUD | 2.18 (±0.71) | (1.76, 2.59) | 2.12 | 0.94 | 3.32 | |
| Opioid prescription rate | 44.83 (±5.76) | (41.50, 48.16) | 45.60 | 34.00 | 51.80 | |
| North Carolina | Synthetic death rate | 4.32 (±4.65) | (1.63, 7.00) | 1.78 | 1.18 | 13.00 |
| MOUD | 1.01 (±0.57) | (0.68, 1.34) | 0.91 | 0.21 | 2.01 | |
| Opioid prescription rate | 84.82 (±12.73) | (77.47, 92.17) | 88.50 | 56.70 | 98.60 | |
| Ohio | Synthetic death rate | 8.97 (±11.12) | (2.55, 15.39) | 1.48 | 0.79 | 30.22 |
| MOUD | 0.87 (±0.63) | (0.51, 1.24) | 0.65 | 0.10 | 2.05 | |
| Opioid prescription rate | 84.89 (±17.51) | (74.77, 95.00) | 91.10 | 50.80 | 102.40 | |
| Oklahoma | Synthetic death rate | 2.35 (±0.71) | (1.94, 2.75) | 2.24 | 1.25 | 4.30 |
| MOUD | 0.60 (±0.30) | (0.43, 0.78) | 0.59 | 0.17 | 1.12 | |
| Opioid prescription rate | 106.35 (±17.78) | (96.08, 116.62) | 111.10 | 66.00 | 127.40 | |
| Oregon | Synthetic death rate | 1.06 (±0.64) | (0.70, 1.43) | 0.79 | 0.48 | 2.31 |
| MOUD | 0.96 (±0.40) | (0.73, 1.19) | 0.89 | 0.30 | 1.65 | |
| Opioid prescription rate | 86.02 (±17.24) | (76.07, 95.98) | 93.05 | 49.10 | 101.20 | |
| Pennsylvania | Synthetic death rate | 5.49 (±7.51) | (1.15, 9.83) | 0.86 | 0.66 | 20.79 |
| MOUD | 1.23 (±0.69) | (0.83, 1.63) | 1.01 | 0.34 | 2.46 | |
| Opioid prescription rate | 71.82 (±11.91) | (64.95, 78.70) | 76.00 | 47.00 | 83.30 | |
| South Carolina | Synthetic death rate | 3.40 (±3.64) | (1.30, 5.50) | 1.24 | 0.79 | 11.03 |
| MOUD | 0.55 (±0.17) | (0.45, 0.65) | 0.58 | 0.21 | 0.79 | |
| Opioid prescription rate | 90.69 (±12.71) | (83.35, 98.02) | 94.60 | 60.40 | 104.00 | |
| Tennessee | Synthetic death rate | 4.26 (±4.99) | (1.38, 7.14) | 1.55 | 1.00 | 16.87 |
| MOUD | 0.68 (±0.42) | (0.44, 0.92) | 0.56 | 0.10 | 1.46 | |
| Opioid prescription rate | 118.71 (±21.40) | (106.35, 131.06) | 125.95 | 74.60 | 140.00 | |
| Texas | Synthetic death rate | 0.72 (±0.35) | (0.51, 0.92) | 0.60 | 0.35 | 1.46 |
| MOUD | 0.47 (±0.11) | (0.40, 0.54) | 0.48 | 0.27 | 0.69 | |
| Opioid prescription rate | 63.96 (±10.42) | (57.94, 69.97) | 68.50 | 42.10 | 73.40 | |
| Utah | Synthetic death rate | 2.07 (±0.57) | (1.74, 2.40) | 2.07 | 0.98 | 2.97 |
| MOUD | 1.71 (±1.36) | (0.92, 2.50) | 1.08 | 0.20 | 4.43 | |
| Opioid Prescription Rate | 77.81 (±12.64) | (70.51, 85.11) | 83.30 | 51.40 | 91.30 | |
| Virginia | Synthetic Death Rate | 3.78 (±4.06) | (1.44, 6.13) | 1.32 | 0.82 | 11.63 |
| MOUD | 0.74 (±0.37) | (0.53, 0.96) | 0.72 | 0.21 | 1.39 | |
| Opioid prescription rate | 66.89 (±12.22) | (59.84, 73.95) | 71.55 | 40.70 | 79.60 | |
| Washington | Synthetic death rate | 1.36 (±1.07) | (0.74, 1.98) | 0.89 | 0.57 | 4.43 |
| MOUD | 0.93 (±0.46) | (0.66, 1.19) | 0.88 | 0.25 | 1.80 | |
| Opioid prescription rate | 72.60 (±14.17) | (64.42, 80.78) | 76.95 | 42.70 | 86.60 | |
| West Virginia | Synthetic death rate | 12.40 (±11.98) | (5.49, 19.32) | 5.42 | 2.27 | 34.03 |
| MOUD | 1.67 (±0.83) | (1.19, 2.15) | 1.57 | 0.38 | 2.85 | Opioid prescription rate |
| 117.90 (±29.47) | (100.89, 134.91) | 129.45 | 59.40 | 146.90 | Wisconsin | Synthetic death rate |
| 3.25 (±3.54) | (1.20, 5.29) | 1.38 | 0.94 | 11.34 | MOUD | |
| 1.12 (±0.51) | (0.83, 1.42) | 1.04 | 0.20 | 1.84 | Opioid prescription rate | |
| 65.66 (±11.05) | (59.28, 72.04) | 69.90 | 42.50 | 76.80 |
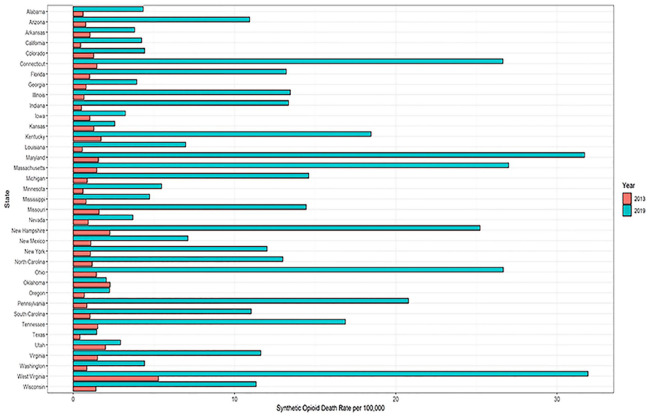
Maryland had the highest mean (mean = 2.32) and median (median = 2.35) MOUD availability rate. Mississippi had the lowest mean availability rate (mean = 0.38) and Iowa had the lowest median availability rate (median = 0.28). The overdose death rates involving synthetic opioids were more than 11 times higher in 2019 when compared with 2013.39 This precipitous rise began in most states in 2013. Figure 1 illustrates the growth of synthetic opioid overdose in all 37 states from 2013 to 2019. In 2019 West Virginia had the highest synthetic opioid overdose death rate followed closely by Maryland, while Texas had the lowest rate.
Figure 1.
Opioid overdose death rates for 37 states in year 2013 and year 2019.
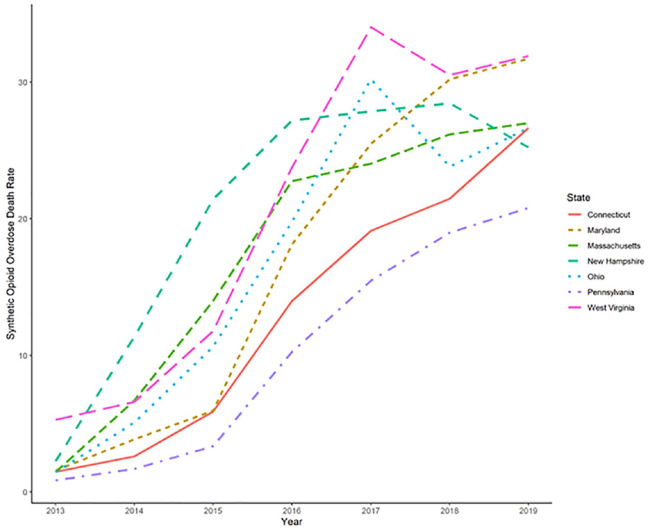
An examination of 37 states from 2006 to 2019 revealed that the North East region of the US had the highest rates of synthetic opioid overdose death. Figure 2 illustrates the 7 states with the highest rates of fatal overdose involving synthetic opioids from 2013 to 2019. This chart demonstrates a sharp increase in synthetic opioid overdose death rates per 100 000 which took place around 2013 because of a sharp increase in the availability of synthetic opioids.
Figure 2.
Seven states with the highest synthetic opioid overdose death rates.
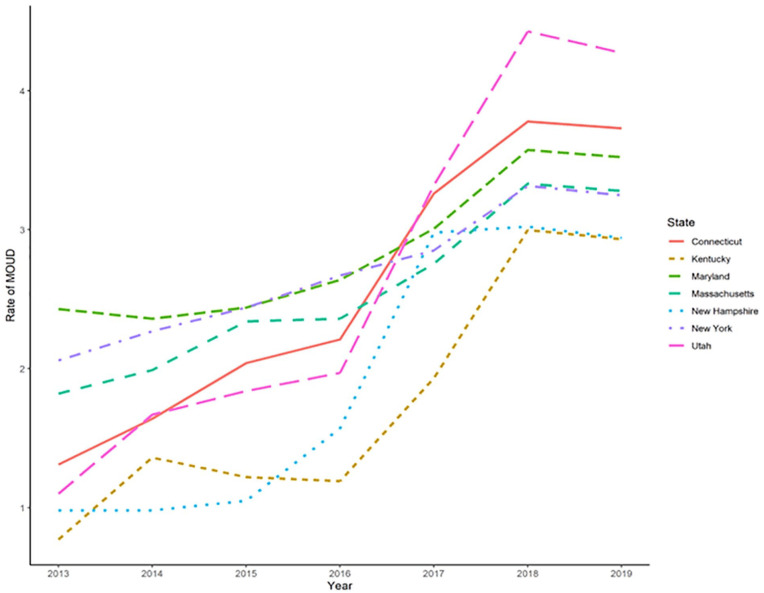
In 2017 Ohio and West Virginia reached their highest rates of synthetic opioid overdose death rates; but from 2017 to 2018 Ohio had the sharpest decrease in synthetic overdose death rate followed by West Virginia. In 2018, both Ohio and West Virginia started again to have an upward trend in their synthetic opioid overdose death rate. As shown in Figure 3, over the period 2013 to 2019, all 7 states with the highest overdose rates had reached their maximum rates in the year 2018. The state of Utah had the highest rate of MOUD followed by Connecticut, Maryland, Massachusetts, New York, New Hampshire, and Kentucky. From 2018 to 2019, all 7 states showed a slight reduction in their MOUD rates.
Figure 3.
Rate for the availability of MOUD for 7 states with the highest rate of MOUD in 2019.
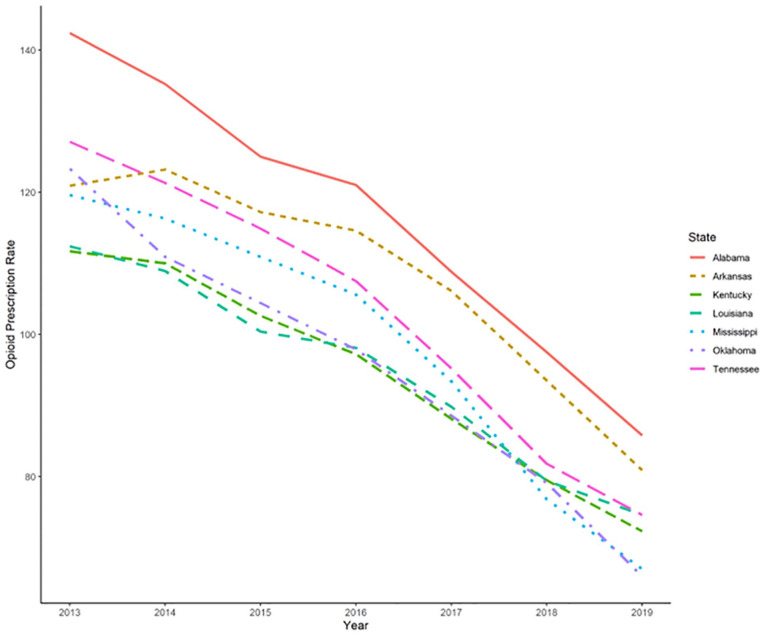
Figure 4 shows the 7 highest opioid prescribing states. These states are all located, or border with, the southeastern region of the United States. Among these states in 2019, Alabama had the highest rate of opioid prescriptions throughout the 2013 to 2019 period, followed by Arkansas, Tennessee, Louisiana, Kentucky, Mississippi, and Oklahoma.
Figure 4.
Opioid prescription rate for the 7 states with the highest rate in 2019.
The presence of an NAL had a significant (univariate P-value = .013) effect on synthetic opioid overdose death rates. Other significant controlling variables were quadratic time (univariate P-values < .001), MOUD (univariate P-value < .001), and Good Samaritan law (univariate P-value = .033). The opioid prescription rate was not a significant factor in predicting synthetic opioid overdose death rate (univariate P-value = .056).
Multivariable Analysis
NALs (multivariable P-value = .010), are a key intervention to address synthetic opioid overdose fatality. As such we focused on NALs. Figure 5 indicates the number of years a naloxone standing order has been present in each of the 37 states in our analysis. While some states (New York, New Mexico, and Connecticut) were early adopters, many states began instituting standing orders in 2013.
Figure 5.
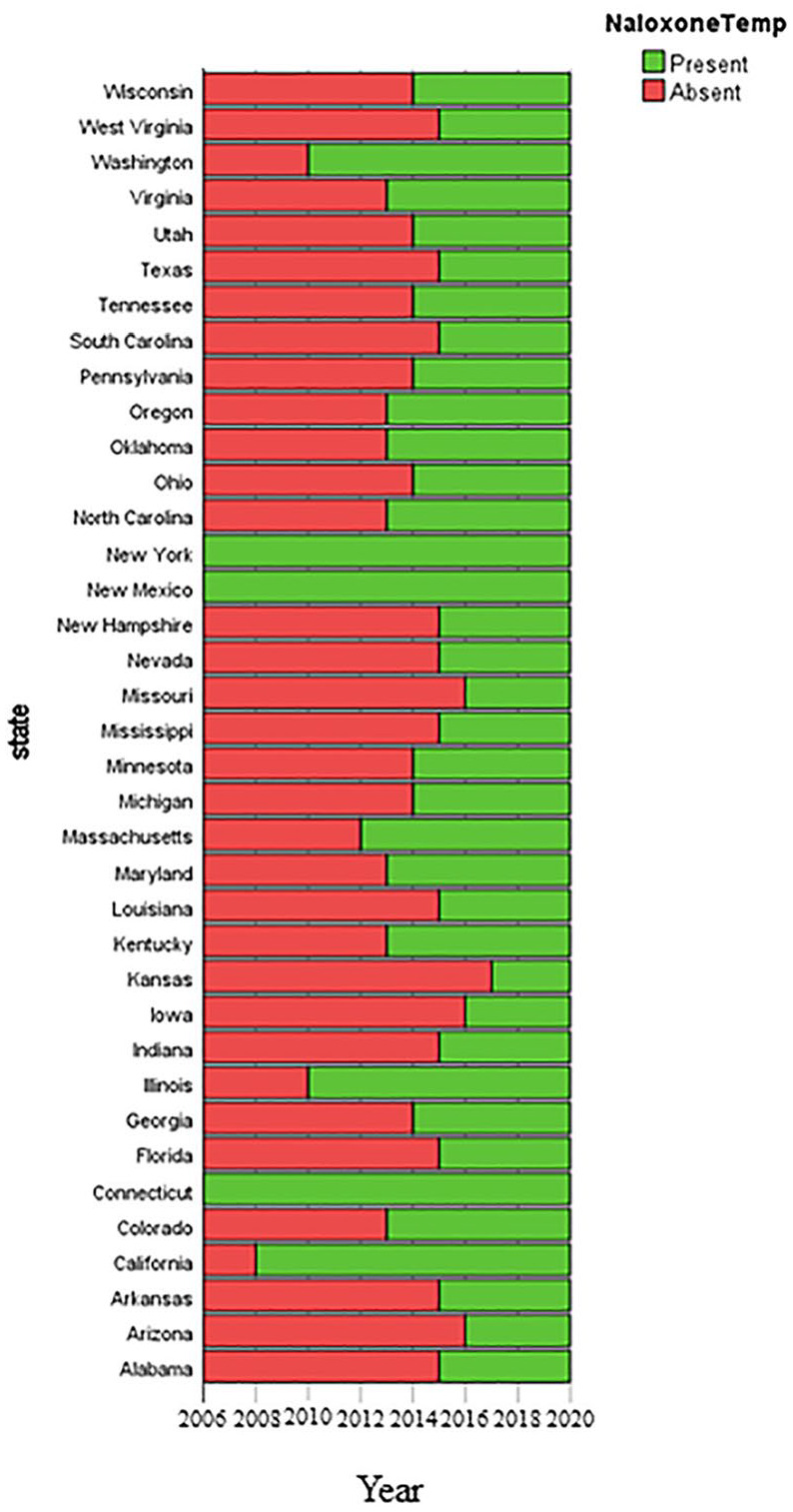
Year since enactment of the Nalaxone law.
The presence of an NAL had a significant (multivariable P-value = .010) effect on synthetic opioid overdose death rates. States who had an NAL had an average 0.313 reduction in deaths per 100 000. Other significant controlling variables were quadratic time (multivariable P-values < .001), MOUD (multivariable P-value = .007), and Good Samaritan law (multivariable P-value = .018). The opioid prescription rate was not a significant factor in predicting synthetic opioid overdose death rate (multivariable P-value = .271). Table 2 gives the results of the multivariable longitudinal mixed effects model.
Table 2.
Multivariable Longitudinal Mixed Effects Model Used to Analyze Opioid Overdose Death Rates.
| Fixed coefficients | ||||||
|---|---|---|---|---|---|---|
| Coefficient | Std. error | t-Value | P-Value | 95% CI | ||
| Lower | Upper | |||||
| Intercept | 1.186 | 0.3064 | 3.871 | <.001 | 0.584 | 1.788 |
| Quadratic time | 0.004 | 0.0011 | 3.559 | <.001 | 0.002 | 0.006 |
| Opioid prescription rate | −0.004 | 0.0033 | −1.101 | .271 | −0.010 | 0.003 |
| MOUD | 0.195 | 0.0719 | 2.718 | .007 | 0.054 | 0.337 |
| Naloxone Law | ||||||
| Present | −0.313 | 0.1217 | −2.573 | .010 | −0.552 | −0.074 |
| Absent | ref | . | . | . | . | . |
| Interaction between Time and Naloxone | ||||||
| Present | 0.008 | 0.0022 | 3.426 | <.001 | 0.003 | 0.012 |
| Absent | ref | . | . | . | . | . |
| Good Samaritan Law | ||||||
| Present | −0.204 | 0.0856 | −2.381 | .018 | −0.372 | −0.036 |
| Absent | ref | . | . | . | . | . |
| Random effect | ||||||
| 95% CI | ||||||
| Random effect covariance | Estimate | Std. error | Z-value | P-value | Lower | Upper |
| Random intercept | 0.546 | 0.151 | 3.608 | <.001 | 0.317 | 0.939 |
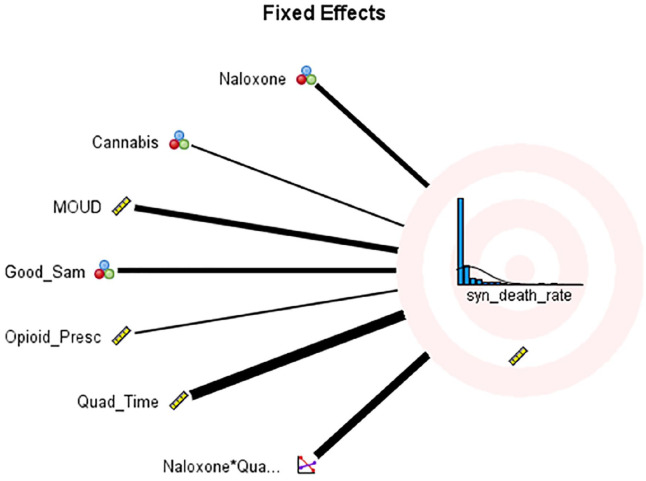
The multivariable longitudinal mixed effect model with random intercept and quadratic time trajectory indicated that there was significant variation across states with respect to opioid overdose death rate (random effect P-value < .001), similar to what was found in a previous study.2 There was a significant interaction between NAL status and quadratic time (P-value < .001 when one uses 5% Type I error probability. The intraclass correlation for our random intercept mixed model was approximately .968. This indicates that approximately 96.8% of the total variation in synthetic opioid overdose death rate is explained by the variation across the 37 states. Figure 6 illustrates a pictorial representation of our fixed variables. The significance of a variable is intensified by the heaviness of the line representing the variable.
Figure 6.
Pictorial significance of fixed effects variables.
Discussion
As the rate of fatal overdose involving synthetic opioid overdose is overtaking all other categories of opioid overdose, it is critical to identify strategies that reduce these fatalities. The results reported here are intended to help assess the impact of several synthetic opioid overdose prevention strategies alone and in combination to guide continued efforts at reduction.
The central finding was that the presence of a NAL, MOUD, Good Samaritan law, and the interaction between NAL with quadratic time trajectory are strongly associated with fatal overdose reduction. The presence of an NAL and MOUD had the strongest relationships to synthetic opioid overdose rates. More studies examining the relationship between naloxone distribution rates and synthetic opioid overdose death rates are needed as well as examining the relationship of rates of MOUD prescribing and synthetic overdose.
The presence of an NAL and MOUD rate had the strongest relationships to fentanyl overdose rates. We examined the binary presence or absence of NALs; however, many nuances are present in the policies from state to state that could impact the effectiveness of the policies. It is likely that within each law, certain facets adopted within the policy may have an impact on the outcomes. Abouk et al26 found that indeed the type of naloxone access law passed did have a relationship to fatal overdose reduction, however, they looked at opioid overdose generally as opposed to focusing on synthetic opioid overdose rates as we have done in this study. Examining the type of NAL and synthetic opioid fatality rates is an important next step in forming an overdose prevention strategy in the current synthetic opioid dominated drug market.
In a rigorous study using matched states the authors found that not only are the specific elements of a naloxone access law associated with differences in fatal overdose rates, but also the region of the country was associated with these differences.43 It is unclear why these laws have had a differential impact across regions. However, the authors posit that the slow infiltration of fentanyl into the Western region’s opioid market may be responsible. Our study looks specifically at the synthetic opioid drug category (excluding methadone), which includes fentanyl, and reductions in fatality associated with these drugs were correlated with NALs. More studies, such as our own, examining the impact of naloxone on synthetic opioids or fentanyl specifically are needed to address the changing drug market.
Another study found reductions in all opioid overdose rates was associated with a combination of Good Samaritan and NALs.44 The authors noted that Good Samaritan laws that provided more broad legal protections were more likely to result in reduced fatal overdoses, and that these are even more effective in combination with NALs. Another study conducted on Midwestern states indicated Good Samaritan laws had no impact on fatal overdose rates. Findings regarding these laws are mixed, and additional research examining specific states, and specific elements of Good Samaritan laws (ie, the degree of protection from prosecution for people using drugs) are needed to maximize the impact of these laws on fatal overdose rates.45
A positive relationship between rates of MOUD prescribing and fatal overdose was also found. A large meta-analysis examining all-cause mortality post medication for opioid use disorder treatment found that retention in either methadone or buprenorphine treatment was associated with lower all-cause mortality.46-48 Other studies have found that overdose rates increase among patients in the induction phase of methadone maintenance treatment, as well as during the period immediately after discontinuation of both methadone and buprenorphine.49 Further study of the impact of MOUD availability taking into account the increased risk of overdose during induction and post attrition, alongside the decreased all-cause mortality that has been associated with MOUD is also needed. Particularly, studies examining the impact of clinic policies that could lead to attrition are needed to ensure the potential benefit of MOUD is maximized while controlling the increased risk of overdose post treatment.
Limitations
Our findings provide a nationwide look at the impact of policies and service availability on fatal synthetic opioid overdose rates. The limitation of this approach is that more direct relationships are not able to be assessed with this level of measurement. For example, while we found the presence of a naloxone standing order prescription was related to lower synthetic opioid fatalities, examining naloxone distribution levels and types of naloxone access programs would provide benchmarks for distribution levels and model programing associated with fatality reduction. Similarly, MOUD treatment capacity has a relationship to lower fatality rates, however, capacity may not be utilized and retention in care may be poor, however, given the current measure of capacity these factors cannot be evaluated. Although the random-intercept model captures the variation across states, our national level analysis cannot consider county-level differences within states, nor did we examine regional differences and these have been shown to be important factors in overdose reduction strategies.18,43 In addition, the state-level capacity measurement employed here cannot account for the initiation nor retention of patients in MOUD treatment, both of which are key to reducing fatal overdose. A statistical limitation was the lack of data availability for all 50 states. We expect that having data on all 50 states, rather than only 37, would have improved the accuracy of the results. Finally, while we assume that the majority of fatal synthetic opioid overdoses are caused by IMF, the current data does not allow us to differentiate between IMF and legally produced fentanyl.
In conclusion, naloxone standing orders, MOUD, and Good Samaritan laws are strongly related to fatal synthetic opioid overdose reduction. Further, additional studies of naloxone distribution levels and access plans outlined in policies are needed that focus on synthetic opioids and/or fentanyl related fatal overdoses. Studies examining the actual numbers of people treated and retained with MOUD, and strategies to increase both can be helpful to refine state approaches to synthetic opioid overdose prevention.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project is supported by the National Institutes of Health- National Institute on Minority Health and Health Disparities for funding this project under the Research Centers in Minority Institutions (RCMI) Grant MD007586.
ORCID iD: Aramandla Ramesh  https://orcid.org/0000-0003-0688-9368
https://orcid.org/0000-0003-0688-9368
References
- 1. Hedegaard H. Drug Overdose Deaths in the United States, 1999-2019. National Center for Health Statistics; 2020: 8. [Google Scholar]
- 2. Lyle Cooper R, Thompson J, Edgerton R, et al. Modeling dynamics of fatal opioid overdose by state and across time. Prev Med Rep. 2020;20:101184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Warner M, Trinidad JP, Bastian BA, Minino AM, Hedegaard H. Drugs most frequently involved in drug overdose deaths: United States, 2010-2014. Natl Vital Stat Rep. 2016;65:1-15. [PubMed] [Google Scholar]
- 4. Hedegaard H, Bastian BA, Trinidad JP, Spencer M, Warner M. Drugs most frequently involved in drug overdose deaths: United States, 2011-2016. Natl Vital Stat Rep. 2018;67:1-14. [PubMed] [Google Scholar]
- 5. Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths—27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65:837-843. [DOI] [PubMed] [Google Scholar]
- 6. Frank RG, Pollack HA. Addressing the fentanyl threat to public health. N Engl J Med. 2017;376:605-607. [DOI] [PubMed] [Google Scholar]
- 7. HAN Archive—00413. Health Alert Network (HAN). 2018. Accessed April 1, 2022. https://emergency.cdc.gov/han/HAN00413.asp
- 8. Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010-2016. J Am Med Assoc. 2018;319:1819-1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65:1445-1452. doi: 10.15585/mmwr.mm655051e1 [DOI] [PubMed] [Google Scholar]
- 10. O’Donnell JK, Halpin J, Mattson CL, Goldberger BA, Gladden RM. Deaths involving fentanyl, fentanyl analogs, and U-47700—10 states, July-December 2016. MMWR Morb Mortal Wkly Rep. 2017;66:1197-1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Somerville NJ, O’Donnell J, Gladden RM, et al. Characteristics of fentanyl overdose - Massachusetts, 2014-2016. MMWR Morb Mortal Wkly Rep. 2017;66:382-386. doi: 10.15585/mmwr.mm6614a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Suzuki J, El-Haddad S. A review: fentanyl and non-pharmaceutical fentanyls. Drug Alcohol Depend. 2017;171:107-116. [DOI] [PubMed] [Google Scholar]
- 13. Wilson N, Kariisa M, Seth P, Smith H, 4TH, Davis NL. Drug and opioid-involved overdose deaths—United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020;69:290-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths—United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67:1419-1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. National Institute on Drug Abuse. Overdose Death Rates. 2022. Accessed May 5, 2022. https://nida.nih.gov/drug-topics/trends-statistics/overdose-death-rates
- 16. Centers for Disease Control. Drug Overdose Deaths. Drug Overdose. 2022. CDC Injury Center. Accessed April 1, 2022. https://www.cdc.gov/drugoverdose/deaths/index.html [Google Scholar]
- 17. Washington State Health Care Authority. Medications for Opioid Use Disorder (MOUD). 2022. Accessed April 1, 2022. https://www.hca.wa.gov/billers-providers-partners/behavioral-health-recovery/medications-opioid-use-disorder-moud
- 18. Linas BP, Savinkina A, Madushani RWMA, et al. Projected estimates of opioid mortality after community-level interventions. JAMA Netw Open. 2021;4:e2037259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jordan MR, Morrisonponce D. Naloxone. StatPearls. StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 20. Visconti AJ, Santos G-M, Lemos NP, Burke C, Coffin PO. Opioid overdose deaths in the city and county of San Francisco: prevalence, distribution, and disparities. J Urban Health. 2015;92:758-772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: Interrupted time series analysis. BMJ. 2013;346:f174-f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Centers for Disease Control and Prevention (CDC). Community-based opioid overdose prevention programs providing naloxone - United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:101-105. [PMC free article] [PubMed] [Google Scholar]
- 23. U.S. Department of Health & Human Services. U.S. Surgeon General’s Advisory on Naloxone and Opioid Overdose. 2022. Accessed May 5, 2022. https://www.hhs.gov/surgeongeneral/reports-and-publications/addiction-and-substance-misuse/advisory-on-naloxone/index.html
- 24. McClellan C, Lambdin BH, Ali MM, et al. Opioid-overdose laws association with Opioid use and overdose mortality. Addict Behav. 2018;86:90-95. [DOI] [PubMed] [Google Scholar]
- 25. Sohn M, Talbert JC, Huang Z, Lofwall MR, Freeman PR. Association of naloxone coprescription laws with naloxone prescription dispensing in the United States. JAMA Netw Open. 2019;2:e196215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Abouk R, Pacula RL, Powell D. Association between state laws facilitating pharmacy distribution of naloxone and risk of fatal overdose. JAMA Intern Med. 2019;179:805-811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Atkins DN, Durrance CP, Kim Y. Good Samaritan harm reduction policy and drug overdose deaths. Health Serv Res. 2019;54:407-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Erfanian E, Grossman D, Collins AR. The impact of naloxone access laws on opioid overdose deaths in the U.S. Rev Reg Stud. 2019;49: 45-72. [Google Scholar]
- 29. Lambdin BH, Davis CS, Wheeler E, Tueller S, Kral AH. Naloxone laws facilitate the establishment of overdose education and naloxone distribution programs in the United States. Drug Alcohol Depend. 2018;188:370-376. [DOI] [PubMed] [Google Scholar]
- 30. Doleac JL, Mukherjee A. The moral hazard of lifesaving innovations: Naloxone access, Opioid Abuse, and Crime. EconStor. 2018; 77. [Google Scholar]
- 31. Gertner AK, Domino ME, Davis CS. Do naloxone access laws increase outpatient naloxone prescriptions? Evidence from Medicaid. Drug Alcohol Depend. 2018;190:37-41. [DOI] [PubMed] [Google Scholar]
- 32. Xu J, Davis CS, Cruz M, Lurie P. State naloxone access laws are associated with an increase in the number of naloxone prescriptions dispensed in retail pharmacies. Drug Alcohol Depend. 2018;189:37-41. [DOI] [PubMed] [Google Scholar]
- 33. Rees DI, Sabia JJ, Argys L, et al. With a little help from my friends: the effects of naloxone access and Good Samaritan laws on opioid-related deaths. National Bureau of Economic Research working paper 23171. 2017.
- 34. Evans TI, Hadland SE, Clark MA, Green TC, Marshall BD. Factors associated with knowledge of a Good Samaritan law among young adults who use prescription opioids non-medically. Harm Reduct J. 2016;13:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gupta R, Shah ND, Ross JS. The rising price of naloxone—risks to efforts to stem overdose deaths. N Engl J Med. 2016;375:2213-2215. [DOI] [PubMed] [Google Scholar]
- 36. Koester S, Mueller SR, Raville L, Langegger S, Binswanger IA. Why are some people who have received overdose education and naloxone reticent to call emergency medical services in the event of overdose? Int J Drug Policy. 2017;48:115-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bird SM, McAuley A, Perry S, Hunter C. Effectiveness of Scotland’s National naloxone Programme for reducing opioid-related deaths: a before (2006-10) versus after (2011-13) comparison. Addiction. 2016;111:883-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Clark AK, Wilder CM, Winstanley EL. A systematic review of community opioid overdose prevention and naloxone distribution programs. J Addict Med. 2014; 8:153-163. [DOI] [PubMed] [Google Scholar]
- 39. Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversal. Ann Intern Med. 2013;158(1):1-9. [DOI] [PubMed] [Google Scholar]
- 40. Giglio RE, Li G, DiMaggio CJ. Effectiveness of bystander naloxone administration and overdose education programs: a meta-analysis. Inj Epidemiol. 2015;2(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cicero TJ, Ellis MS. Abuse-deterrent formulations, and the prescription opioid abuse epidemic in the United States: lessons learned from oxycontin. JAMA Psychiatr. 2015;72:424-430. [DOI] [PubMed] [Google Scholar]
- 42. Kim B. Must-access prescription drug monitoring programs and the opioid overdose epidemic: the unintended consequences. J Health Econ. 2021;75:102408. [DOI] [PubMed] [Google Scholar]
- 43. Cataife G, Dong J, Davis CS. Regional and temporal effects of naloxone access laws on opioid overdose mortality. Subst Abuse. 2021;42(3):329-338. [DOI] [PubMed] [Google Scholar]
- 44. Hamilton L, Davis CS, Kravitz-Wirtz N, Ponicki W, Cerdá M. Good Samaritan laws and overdose mortality in the United States in the fentanyl era. Int J Drug Policy. 2021;97:103294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Adams N, Gundlach E, Cheng CW. An analysis of state-level policies and opioid overdose deaths. West J Nurs Res. 2020;42:535-542. [DOI] [PubMed] [Google Scholar]
- 46. Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann Intern Med. 2018;169:137-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Strang J, McCambridge J, Best D, et al. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ 2003;326:959-960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ma J, Bao YP, Wang RJ, et al. Effects of medication-assisted treatment on mortality among opioids users: a systematic review and meta-analysis. Mol Psychiatry. 2019;24(12):1868-1883. [DOI] [PubMed] [Google Scholar]