Abstract
Background
Irritable bowel syndrome (IBS) is a disorder of brain-gut interactions characterized by abdominal pain and bowel dysfunction. Exercise and mindfulness have been reported to be effective on IBS, but there has been no study of their interaction. In this study, we hypothesized that exercise and mindfulness interactively affect the severity of IBS symptoms.
Methods
Subjects were 703 adolescents with 590 women and 113 men. Their IBS status was evaluated with Rome III Diagnostic Questionnaire and IBS Severity Index (IBS-SI). They also fulfilled past exercise experience, athletic performance and exercise enthusiasm, International Physical Activity Questionnaire (IPAQ), Mindful Attention Awareness Scale (MAAS), Kessler 6 Scale (K6), and Perceived Stress Scale (PSS). Statistical analysis was performed using SPSS v25.
Results
In this population, 184 (158 women and 26 men, 14.1%) subjects had Rome III IBS symptoms. IBS subjects scored significantly less in exercise enthusiasm at high school (p = 0.017) and MAAS (p < 0.001) and significantly more K6 (p < 0.001) and PSS (p < 0.001) than non-IBS. The two-way ANOVA on IBS-SI showed a significant main effect of MAAS (p < 0.001) and interaction between MAAS and IPAQ (p = 0.008).
Conclusion
It is suggested that mindfulness per se decreases IBS severity, but that mindfulness and physical activity interactively affect the severity. Further studies on how to design interventional trials for IBS patients with mindfulness and physical exercise are warranted.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00535-022-01938-9.
Keywords: Brain-gut interactions, Irritable bowel syndrome, Exercise experience, Physical activity, Mindfulness
Introduction
Irritable bowel syndrome (IBS) is a disorder of brain–gut interactions characterized by abdominal pain and bowel dysfunction [1]. It is a functional disorder where the underlying organic disease is not detected on routine clinical examination [1, 2]. Gastrointestinal symptoms in IBS patients are characterized by stress-induced onset and exacerbation [3] with psychiatric comorbidities such as depression and anxiety [4], suggesting that exaggerated brain-gut interactions are the key features of IBS. The brain–gut correlation is brought about by the nervous, endocrine, and immune systems around the hypothalamus-pituitary-adrenal (HPA) axis [5–9]. IBS significantly impairs the quality of life and social functioning [10]. Prevalence of IBS in the general population shows 10–20% with Rome III criteria [11] and 4.1% with more restrictive Rome IV criteria [12].
IBS patients express steeper correlation coefficient between psychosocial stress and gastrointestinal symptoms than healthy controls [13]. IBS patients experience high-stress levels daily, triggering psychological abnormalities such as anxiety, tension, and depression [14]. IBS patients have visceral hypersensitivity and central sensitization, which in turn result in feedback gastrointestinal dysfunction [15].
Recently, exercise therapy has been reported to have health-promoting effects on various diseases [16]. Long-term aerobic exercise increases serotonin activity in the central nervous system (CNS) [17, 18], parasympathetic activity, including in the circulatory system [19, 20], and reduces mild to moderate anxiety and depression [21, 22]. Exercise also affects the HPA axis. Long-term voluntary exercise in mice more adaptively alters the stress response via the HPA axis [23]. It increased circulating cortisol concentrations at moderate to high exercise loads in humans, but decreased them at low exercise loads [24]. Physical activity improves abdominal transit time [25] and gas [26] and produces anti-inflammatory and antioxidant effects in IBS [27]. Exercise therapy under proper guidance also improves IBS symptoms [28, 29] with positive evaluation in the Japanese IBS guidelines [2]. While such effects of physical activity on IBS symptoms have been observed, the actual amount of physical activity in IBS has been reported to be lower than that in healthy subjects [30, 31]. An individual’s motivation and psychological state significantly influence the effectiveness of exercise therapy [32, 33].
Mindfulness has also been focused as a psychological factor in combating IBS. Mindfulness is the intentional, non-judgmental attention to the present moment, accepting the sensations and experiences as they are [34]. Mindfulness-based stress reduction interventions were reported to alleviate IBS symptoms [35]. Within mindfulness, an increased "ability to maintain focus, especially in the present moment, and to act with awareness" significantly improves IBS symptoms [36].
From the above background, it is natural to assume that physical activity and mindfulness may synergistically influence IBS severity. However, there was no study of their interaction. In this study, we hypothesized that exercise and mindfulness interactively affect the severity of IBS symptoms.
Methods
Study participants
This study was conducted among 1,475 adolescents in the departments of nursing, nutrition, rehabilitation, childcare, and business-related departments at Sendai Seiyo Gakuin College in Miyagi, Japan. Data from 703 responders (response rate: 47.7%) were obtained. They consisted of 590 (83.9%) women and 113 (16.1%) men of age 19.3 ± 2.9 years.
Study design
This study was conducted using a cross-sectional, online questionnaire method.
Setting
The researcher explained the study orally to each department and grade level during a non-lecture time and asked them to answer questions on an online questionnaire using Google forms. No rewards were given. The time required to complete the questionnaire ranged from 20 to 30 min. Data were collected from April 13, 2021, to July 3, 2021.
Ethical considerations
This study was conducted with the approval of the Ethics Committee of Tohoku University Graduate School of Medicine (Clinical Trial Registration Number: 2020-1-836) and the Research Ethics Review Committee of Sendai Seiyo Gakuin College (Approval Number: 0222). Participants' responses were voluntary, and their consent was taken by giving them the "I consent to this study" option before answering the questionnaire. Disagreement to consent was confirmed by them not responding to the option.
Questionnaire
Gender and age data were obtained. In addition, the demographic attribute variables regarding IBS symptoms, exercise, mental anguish, stress, and mindfulness were obtained using the following tools.
Rome III Diagnostic Criteria for IBS
The diagnosis of study participants as IBS or non-IBS was determined from their responses to the Rome III Diagnostic Questionnaire for IBS [1, 11]. The diagnosis was based on recurrent abdominal pain or discomfort on at least 3 days per month for the past 3 months (12 weeks) and two or more of the following three criteria: (1) improvement in bowel movements, (2) change in stool frequency with onset, and (3) change in stool morphology with the onset of symptoms that began 6 months earlier and have continued. The IBS diagnostic criteria have been updated from Rome III [11] to Rome IV [37]. The major difference in Rome IV from Rome III is restriction of abdominal pain and frequency (once per week or more) of abdominal pain. The global epidemiological study clarified 2.2% [95% confidence interval: 1.6–2.7] with Rome IV IBS and 9.3% [95% confidence interval: 8.2–10.4] with Rome III IBS in the Japanese general population [12]. It is natural to assume that only 15 subjects with Rome IV IBS would be extracted from the study sample. By contrast, subjects with Rome III IBS would be good sample size enough to test the hypothesis.
Bristol Stool Form Scale
It is a seven-point scale from hardest (Type 1) to softest stool (Type 7) for measuring stool shape, widely used in clinical and research settings [38, 39]. Types 1 and 2 are considered constipation; Types 6 and 7 are diarrhea. Types 3–5 are generally considered normal stools.
IBS Severity Index (IBS-SI)
It measures the severity of IBS, with total scores ranging from 0 to 500. Higher scores indicate severe abdominal symptoms. The items evaluated are the presence of abdominal pain, the severity of abdominal pain, average number of abdominal pain in 10 days, presence of abdominal distension, degree of abdominal distension, satisfaction with bowel movements, and impact of abdominal symptoms on daily life [40, 41].
Questions about exercise at each time
To determine the exercise experience of the study participants, the number of months and days of exercise per week was determined for each of the following periods based on the Japanese educational curriculum: pre-school (age 5 and under), elementary school (age 6–12), junior high school (age 13–15), high school (age 16–18), and the present (age 18 and onward). The number of exercise days for each time was calculated as follows: 1 month was converted into 4 weeks, and the number of exercise months × 4 × the number of exercise days per week. The number of exercise days in each period was summed to calculate total exercise days (TED) [42]. Exercise did not include physical education lectures or athletic events at educational facilities. However, club activities outside of lectures and the local community were included.
A athletic performance at each period, responses were evaluated on participation in competitions with regard to a particular athletic activity. The responses were obtained on a six-point scale: "no experience," "no participation or no affiliation," "municipal competition," "prefectural competition," "regional competition," and "national/international competition." The score for "no athletic experience" was zero, and the "national/international competition" was five, with higher scores corresponding to participation in higher-level competitions.
Additionally, respondents were asked to indicate their level of enthusiasm for exercise at each time period on a six-point Likert scale: "no experience," "not at all enthusiastic," "not very enthusiastic," "undecided," "fairly enthusiastic," and "very enthusiastic." A score of zero was given for "no experience" and five for "very enthusiastic." The score was higher according to the response with a higher level of enthusiasm.
International Physical Activity Questionnaire (IPAQ)
It calculates the study participants' daily physical activities [43, 44]. The weekly frequency and average daily minutes were multiplied by the "calorie expenditure (8.0 kcal) of vigorous physical activity," which was defined as "any activity that is physically demanding and causes considerable breathing disturbance." and "calorie expenditure (4.0 kcal) of moderate exercise," defined as "an activity that is somewhat physically demanding and leaves you slightly out of breath." The usual speed of walking was identified as "fast with disrupted breathing (5.0 kcal)," "slightly breathless (3.3 kcal)," or "leisurely (2.5 kcal)," and each speed was multiplied by the weekly frequency and the average daily minutes. The values calculated for vigorous exercise, moderate exercise, and walking speed were added together and divided by seven to obtain the daily physical activity.
Kessler 6 Scale
It measures the nonspecific psychological distress [45, 46]. It is a six-item, five-point scale which assesses depression and anxiety symptoms during the past month. The score ranges from 0 to 24. Higher scores indicate high psychological distress.
Perceived Stress Scale
It measures the perceived degree of stress state. It consists of 14 items and is rated on a five-point scale [47, 48]. It is expressed on a scale of 0–56 points. The ratings were reversed for reversed items. A high score indicated a high stress level.
Mindful Attention Awareness Scale
It measures mindfulness tendency and consists of 15 items, rated on a six-point scale [49]. Scores range from 15 to 90. The validated Japanese version of the MAAS by Fujino et al. [50] was used in this study. Considering the differences between the Japanese version and the original version, we asked respondents to respond based on the Japanese version's six-point scale (1: "almost always," 2: "very often," 3: "somewhat often," 4: "not very often," 5: "seldom," 6: "almost never”). All the questions on the MAAS are described in terms that negate mindfulness, such as "I could be experiencing some emotion and not be conscious of it until sometime later." The more "almost never" a subject responds to that question, the more mindful the subject is. Thus, high scores indicate high mindfulness tendencies.
Statistical analysis
Descriptive statistics were first performed on the overall data and the IBS and non-IBS groups, describing the sample size, number, and proportion of gender in each group, and the number and proportion of subtypes in the IBS group. For gender, χ2 tests were performed to check for significant differences.
For each variable, the means and standard deviations for the overall data and the IBS and non-IBS groups are shown, and the variables for the IBS and non-IBS groups are compared using a Student’s t test. Spearman's rank correlation was performed for the overall data and the IBS and non-IBS groups, respectively, to evaluate the relationship of each variable.
To examine the effects of the presence or absence of IBS symptoms and past exercise experience on the variables, the following groups were studied: IBS group with TED greater than or equal to standard deviation (SD) (IBS × TED + SD), IBS group with TED less than or equal to SD (IBS × TED − SD), non-IBS group with TED greater than or equal to SD (non-IBS × TED + SD), and IBS group with TED less than or equal to SD (non-IBS × TED − SD). The group was divided into four groups. Normality was checked for IBS-SI, IPAQ, K6, PSS, and MAAS in each group. For factors for which normality was confirmed, multiple comparisons were performed using the Sidak method after a one-factor analysis of variance. For factors for which normality was not found, multiple comparisons between groups were made using the Dunn–Bonferroni method after the Kruskal–Wallis test.
Furthermore, we tested how mindfulness tendency and physical activity level affect IBS-SI. In a two-way ANOVA, MAAS and IPAQ were divided into low, middle, and high as independent variables, and IBS-SI as the dependent variable. Main effects and interactions were confirmed, followed by multiple comparisons using the Sidak method. This was done for the overall data, the IBS group, and the non-IBS group, respectively.
The normality of each variable in each group was checked using the Shapiro–Wilk test. Statistical analyses were performed using IBM SPSS Statistics 25 (IBM Corp., Armonk, NY, USA). The significant level was defined as p < 0.05.
Results
Participant characteristics
Of the 703 participants in this study, 184 (158 women and 26 men, 14.1%) had symptoms of IBS according to the Rome III diagnostic criteria for IBS. There was no significant difference in the gender ratio between the IBS and non-IBS groups (χ2 (2) = 0.698, p = 0.404). The subtypes of IBS in the IBS group were IBS-C in 28 patients (15.2%), IBS-D in 68 patients (37.0%), IBS-M in 80 patients (43.5%), and IBS-U in 8 patients (4.4%) (Table 1).
Table 1.
Participant characteristics
| N | OVERALL | IBS | Non-IBS | χ2 test p value | |||||
|---|---|---|---|---|---|---|---|---|---|
| 703 | 184 | 519 | |||||||
| n | % | n | % | n | % | ||||
| Men | 113 | 16.1 | 26 | 14.1 | 87 | 16.8 | 0.404 | ||
| Women | 590 | 83.9 | 158 | 85.9 | 432 | 83.2 | |||
| IBS subtypes | |||||||||
| IBS-C | 28 | 15.2 | |||||||
| IBS-D | 68 | 37.0 | |||||||
| IBS-M | 80 | 43.5 | |||||||
| IBS-U | 8 | 4.4 | |||||||
The characteristics of the participants of this study. It contains the overall number and percentages of men and women who participated in the study, and the same distribution across the IBS and Non-IBS groups. The results of the χ2 test for gender ratios in each group and the number and proportion of IBS subtypes in the IBS group are shown
Comparison between groups
Mean values and standard deviations are shown for age, IBS-SI, K6, PSS, MAAS, number of exercise days per period, TED, exercise performance, exercise enthusiasm, and IPAQ for the overall data and the IBS and non-IBS groups. The results of comparisons between IBS and non-IBS groups by Student's t test are shown. In addition, Shapiro-Wilk test results for each factor in the overall data are shown (Table 2). The results of the Shapiro-Wilk test showed normality only for MAAS and IBS-SI. No normality was found for the other factors. There were significant difference in IBS-SI (t (701) = 15.57, p < 0.001), K6 (t(268.61) = 8.74, p < 0.001), PSS (t(701) = 5.979, p < 0.001), MAAS (t(340.33) = 5.82, p < 0.001) and exercise enthusiasm of high school students (t(335.99) = 2.39, p = 0.017) between the IBS and non-IBS groups. The IBS group had higher IBS-SI, K6, and PSS, and lower MAAS and high school students' exercise enthusiasm than the non-IBS group. There were no differences in TED or the number of exercise days at each period.
Table 2.
Values and normality of each variable in overall and IBS and non-IBS groups, and comparison of the IBS and non-IBS groups
| Overall | IBS | Non-IBS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | n | Mean | SD | t test p value | Shapiro–Wilk | |
| Age | 703 | 19.27 | 2.86 | 184 | 19.67 | 3.54 | 519 | 19.12 | 2.56 | 0.053 | < 0.05 |
| IBS-SIa | 703 | 123.42 | 92.66 | 184 | 202.26 | 79.30 | 519 | 95.47 | 80.16 | < 0.001 | 0.783 |
| K6b | 703 | 4.84 | 4.68 | 184 | 7.55 | 5.17 | 519 | 3.87 | 4.09 | < 0.001 | < 0.05 |
| PSSc | 703 | 28.68 | 7.00 | 184 | 31.27 | 7.04 | 519 | 27.76 | 6.75 | < 0.001 | < 0.05 |
| MAASd | 703 | 61.74 | 12.20 | 184 | 57.47 | 11.39 | 519 | 63.26 | 12.13 | < 0.001 | 0.092 |
| Pre-school exercise days | 703 | 28.09 | 95.25 | 184 | 29.52 | 86.52 | 519 | 27.58 | 98.24 | 0.812 | < 0.05 |
| Pre-school athletic results | 703 | 0.24 | 0.60 | 184 | 0.24 | 0.57 | 519 | 0.24 | 0.61 | 0.914 | < 0.05 |
| Pre-school exercise enthusiasm | 703 | 0.63 | 1.41 | 184 | 0.65 | 1.45 | 519 | 0.63 | 1.39 | 0.89 | < 0.05 |
| Elementary school exercise days | 703 | 297.51 | 399.25 | 184 | 288.59 | 400.24 | 519 | 300.67 | 399.24 | 0.725 | < 0.05 |
| Elementary school athletic results | 703 | 1.32 | 1.31 | 184 | 1.33 | 1.37 | 519 | 1.32 | 1.29 | 0.928 | < 0.05 |
| Elementary school exercise enthusiasm | 703 | 2.48 | 2.05 | 184 | 2.41 | 2.04 | 519 | 2.50 | 2.05 | 0.624 | < 0.05 |
| Middle school exercise days | 703 | 524.62 | 342.24 | 184 | 520.70 | 346.83 | 519 | 526.01 | 340.93 | 0.856 | < 0.05 |
| Middle school athletics results | 703 | 2.07 | 1.34 | 184 | 2.03 | 1.40 | 519 | 2.09 | 1.32 | 0.626 | < 0.05 |
| Middle school exercise enthusiasm | 703 | 3.30 | 1.94 | 184 | 3.11 | 1.94 | 519 | 3.37 | 1.94 | 0.122 | < 0.05 |
| High school exercise days | 703 | 336.86 | 361.47 | 184 | 308.26 | 357.55 | 519 | 347.00 | 362.66 | 0.212 | < 0.05 |
| High school athletics results | 703 | 1.58 | 1.63 | 184 | 1.43 | 1.67 | 519 | 1.64 | 1.62 | 0.133 | < 0.05 |
| High school exercise enthusiasm | 703 | 2.32 | 2.23 | 184 | 1.99 | 2.15 | 519 | 2.44 | 2.26 | 0.017 | < 0.05 |
| Current exercise days | 703 | 10.40 | 55.07 | 184 | 14.39 | 73.01 | 519 | 8.99 | 47.11 | 0.35 | < 0.05 |
| Current exercise athletics results | 703 | 0.12 | 0.45 | 184 | 0.10 | 0.35 | 519 | 0.13 | 0.47 | 0.473 | < 0.05 |
| Current exercise enthusiasm | 703 | 0.33 | 1.09 | 184 | 0.29 | 0.96 | 519 | 0.34 | 1.14 | 0.559 | < 0.05 |
| TEDe | 703 | 1197.43 | 870.82 | 184 | 1161.46 | 885.05 | 519 | 1210.19 | 866.22 | 0.515 | < 0.05 |
| IPAQf | 703 | 272.29 | 335.20 | 184 | 291.04 | 365.77 | 519 | 265.64 | 323.78 | 0.378 | < 0.05 |
The values of each variable for the overall, IBS, and non-IBS groups in this study, as well as the Shapilo–Wilk test normality for the overall and Student’s t test results for the IBS and non-IBS groups
aIBS-SI = IBS Severity Index, IBS-SSS
bK6 = Kessler 6 Scale
cPSS = Perceived Stress Scale
dMAAS = Mindful Attention Awareness Scale
eTED = total exercise day
fIPAQ = International Physical Activity Questionnaire
Correlation
Table 3 shows the variables that were significantly different in IBS-SI and psychological variables in Spearman's rank correlations for the overall data and the IBS and non-IBS groups. Table 3 shows the variables that were significantly different in IBS-SI and psychological variables in Spearman's rank correlations for the overall data and the IBS and non-IBS groups. For the overall data, IBS-SI showed a significant positive correlation with K6 (ρ = 0.421, p < 0.01) and PSS (ρ = 0.317, p < 0.01), while MAAS (ρ = − 0.364, p < 0.01) showed a significant negative correlation. For the IBS group, variables that showed significant positive correlations with IBS-SI were K6 (ρ = 0.241, p < 0.01) and PSS (ρ = 0.238, p < 0.01), while MAAS (ρ = − 0.222, p < 0.01) showed a significant negative correlation. For the non-IBS group, variables that showed significant positive correlations with IBS-SI were K6 (ρ = 0.317, p < 0.01) and PSS (ρ = 0.241, p < 0.01), while MAAS (ρ = − 0.318, p < 0.01) showed a significant negative correlation.
Table 3.
Correlations between IBS severity and psychological variables
| IBS-SIa | K6b | PSSc | MAASd | ||
|---|---|---|---|---|---|
|
Overall ( n = 703) |
IBS-SIa | 1 | 0.421** | 0.317** | -0.364** |
| K6b | 1 | 0.634** | -0.521** | ||
| PSSc | 1 | -0.428** | |||
| MAASd | 1 | ||||
|
IBS ( n = 184) |
IBS-SIa | 1 | 0.241** | 0.238** | -0.222** |
| K6b | 1 | 0.631** | -0.470** | ||
| PSSc | 1 | -0.379** | |||
| MAASd | 1 | ||||
|
Non-IBS ( n = 719) |
IBS-SIa | 1 | 0.317** | 0.241** | -0.318** |
| K6b | 1 | 0.599** | -0.499** | ||
| PSSc | 1 | -0.399** | |||
| MAASd | 1 |
The correlations between IBS severity and psychological variables for the overall, IBS, and non-IBS groups
aIBS-SI = IBS Severity Index, IBS-SSS
bK6 = Kessler 6 Scale
cPSS = Perceived Stress Scale
dMAAS = Mindful Attention Awareness Scale
** = p < 0.01
Table 4 shows the variables that showed significant differences in Spearman's rank correlations between exercise-related variables and IBS-SI and psychological variables. Exercise-related variables for pre-school, elementary school, and junior high school students were not significantly different from IBS-SI or psychological variables. No variable in the IBS group showed a significant correlation with IBS-SI. However, there was a significant positive correlation (ρ = 0.208, p < 0.01) between IPAQ and K6 and a significant negative correlation (ρ = − 0.193, p < 0.01) with MAAS. In the non-IBS group, no psychological variables correlated with IPAQ.
Table 4.
Correlations between IBS severity, psychological variables, and exercise-related variables
| Age | Middle school athletic results | Middle school exercise enthusiasm | High school exercise days | High school athletic results | High school exercise enthusiasm | IPAQe | ||
|---|---|---|---|---|---|---|---|---|
| Overall | n | 703 | 703 | 703 | 703 | 703 | 703 | 703 |
| IBS-SIa | 0.128** | 0.011 | − 0.027 | − 0.063 | − 0.064 | − 0.076* | 0.032 | |
| K6b | 0.098** | − 0.065 | − 0.081* | − 0.084* | − 0.078* | − 0.119** | 0.076* | |
| PSSc | 0.102** | − 0.060 | − 0.076* | − 0.076* | − 0.074* | − 0.113** | − 0.049 | |
| MAASd | − 0.099** | 0.027 | 0.131** | 0.070 | 0.038 | 0.110** | − 0.046 | |
| IBS | n | 184 | 184 | 184 | 184 | 184 | 184 | 184 |
| IBS-SIa | 0.034 | − 0.127 | − 0.057 | − 0.009 | − 0.017 | 0.007 | 0.052 | |
| K6b | 0.077 | − 0.167* | − 0.098 | − 0.072 | − 0.063 | − 0.080 | 0.208** | |
| PSSc | 0.125 | − 0.025 | − 0.001 | − 0.059 | − 0.035 | − 0.048 | − 0.046 | |
| MAASd | − 0.097 | 0.081 | − 0.130 | − 0.005 | − 0.006 | 0.007 | − 0.193** | |
| Non-IBS | n | 519 | 519 | 519 | 519 | 519 | 519 | 519 |
| IBS-SIa | 0.101* | 0.036 | 0.045 | − 0.052 | − 0.044 | − 0.039 | 0.012 | |
| K6b | 0.068 | − 0.003 | − 0.045 | − 0.064 | − 0.051 | − 0.090* | 0.022 | |
| PSSc | 0.068 | − 0.058 | − 0.066 | − 0.063 | − 0.063 | − 0.103* | − 0.063 | |
| MAASd | − 0.078 | 0.079 | 0.117** | 0.080 | 0.032 | 0.115** | 0.005 |
The correlations of exercise-related variables to IBS severity and psychological variables in the overall, IBS, and non-IBS groups
aIBS-SI = IBS Severity Index, IBS-SSS
bK6 = Kessler 6 Scale
cPSS = Perceived Stress Scale
dMAAS = Mindful Attention Awareness Scale
eIPAQ = International Physical Activity Questionnaire. *p < 0.05, **p < 0.01
Multiple comparisons
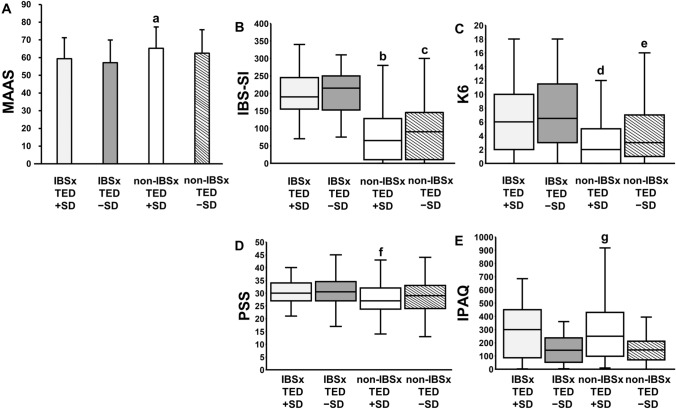
For multiple comparisons in the four groups, IBS × TED + SD, IBS × TED − SD, non-IBS × TED + SD, and non-IBS × TED − SD, the normality of each variable in each group was checked. MAAS showed normality and no normality for IBS-SI, K6, PSS, and IPAQ (Table S1). The results of multiple comparisons by the Sidak method after one-factor analysis of variance by the four groups of MAAS are shown (Fig. 1A). The MAAS showed a significant difference among groups (F (3,256) = 4.496, p = 0.004), and the results of non-IBS × TED + SD were significantly higher than those of IBS × TED − SD (p = 0.005). Multiple comparisons using the Kruskal-Wallis test and the Dunn-Bonferonni method for IBS-SI, K6, PSS, and IPAQ are shown (Fig. 1B–E). IBS-SI showed a significant difference among groups (p < 0.001), and the results of IBS × TED + SD were significantly higher than those of non-IBS × TED + SD (p < 0.001) and non-IBS × TED − SD (p < 0.001), and significantly higher than those of non-IBS × TED + SD (p < 0.001) and non-IBS × TED − SD (p < 0.001). K6 showed a significant difference among groups (p < 0.001), and the results of IBS × TED + SD were significantly higher than those of non-IBS × TED + SD (p = 0.002) and non-IBS × TED − SD (p = 0.044), while those of IBS × TED − SD were significantly higher than those of non-IBS × TED + SD (p < 0.001) and non-IBS × TED − SD (p = 0.004). PSS showed significant differences among groups (p = 0.025), and the results of non-IBS × TED + SD were significantly lower than those of IBS × TED − SD (p = 0.047). IPAQ showed a significant difference among groups (p = 0.002), and the results of non-IBS × TED + SD were significantly higher than those of IBS × TED − SD (p = 0.034) and non-IBS × TED − SD (p = 0.013).
Fig. 1.
Multiple comparisons among groups of IBS × exercise. Mindful Attention Awareness Scale among four groups of IBS × exercise: IBS with more exercise ≧ SD (IBS × TED + SD), IBS with less exercise < SD (IBS × TED − SD), non-IBS with more exercise ≧ SD (non-IBS × TED + SD), and non-IBS with less exercise < SD (non-IBS × TED − SD). A One-way ANOVA: p = 0.004, post hoc (Sidak) test: a vs. IBS × TED − SD, p = 0.005, height: mean, error bar: standard deviation. IBS severity, depression/anxiety, stress, and physical activity among four groups of IBS x exercise. B IBS-SI: Kruskal-Wallis test, p < 0.001, post hoc (Dunn-Bonferroni multiple comparison) test: b vs. IBS × TED + SD, p < 0.001, and IBS × TED − SD, p < 0.001, c vs. IBS × TED + SD, p < 0.001, and IBS × TED − SD, p < 0.001, C K6: p < 0.001, post hoc: d vs. IBS × TED + SD, p = 0.002, and IBS × TED − SD, p = 0.044, e vs. IBS × TED + SD, p < 0.001, and IBS × TED − SD, p = 0.004, D PSS: p = 0.025, post hoc: f vs. IBS × TED − SD, p = 0.047, E IPAQ: p = 0.002, post hoc: g vs. IBS × TED − SD, p = 0.034, and non-IBS × TED − SD, p = 0.013. height: median, error bar: inter quartile range
Two-way ANOVA
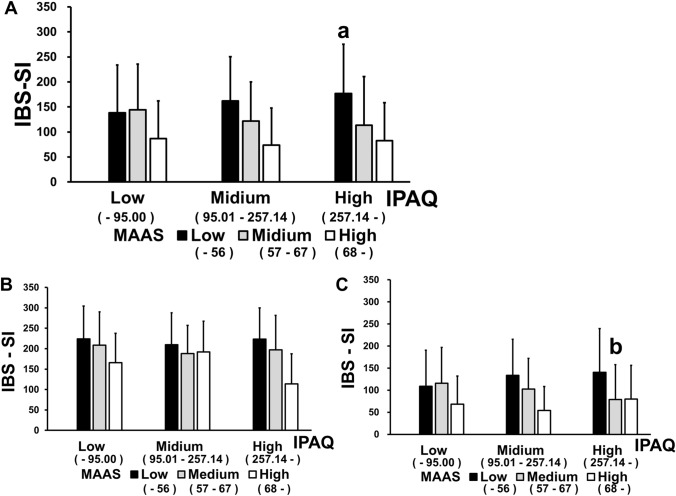
The results of a two-way ANOVA for the overall data with IBS-SI as the dependent variable and MAAS and IPAQ as the independent variables are divided into three parts: low, middle, and high (Fig. 2A, Tables S2.1 and S2.2). The main effect of IPAQ on IBS-SI was not significant (F (2,694) = 0.22, p = 0.803). MAAS had a significant main effect (F (2694) = 45.76, p < 0.001). The interaction between MAAS and IPAQ was significant (F (4,694) = 3.46, p = 0.008). In the low MAAS group, the high IPAQ group showed a significant increase in IBS-SI than the low IPAQ group (p = 0.015). In the IBS group, MAAS had a main effect on IBS-SI (F (2,175) = 6.04, p = 0.003). The main effect of IPAQ on IBS-SI (F (2,175) = 0.871, p = 0.42) and the interaction between MAAS and IPAQ was not significant (F (4,175) = 1.02, p = 0.398) (Fig. 2B, Tables S2.3 and S2.4). In the non-IBS group, the main effect of IPAQ on IBS-SI was not significant (F (2,510) = 0.06, p = 0.94). MAAS had a main effect with IBS-SI (F (2,510) = 26.28, p < 0.001) and an interaction with IPAQ (F (4,510) = 3.84, p = 0.004). In the non-IBS group, IBS-SI decreased significantly as IPAQ increased in the MAAS middle group (p = 0.034) (Fig. 2C, Tables S2.5 and S2.6).
Fig. 2 .
IBS severity depending on mindfulness and exercise. IBS-SI among groups based on MAAS (low, middle, high) × IPAQ (low, middle, high) was analyzed with two-way ANOVA. A All subjects. MAAS group effect, p < 0.001, IPAQ group effect, ns, MAAS × IPAQ interaction, p = 0.008, post hoc (Sidak) test: a vs. low IPAQ x low MAAS group, p = 0.015. B IBS group. MAAS group effect, p < 0.003, IPAQ group effect, ns, MAAS × IPAQ interaction, ns. C Non-IBS group. MAAS group effect, p < 0.001, IPAQ group effect, ns, MAAS × IPAQ interaction, p = 0.004, post hoc (Sidak) test: b vs. low IPAQ × middle MAAS group, p = 0.034
Discussion
This study tested the hypothesis that past exercise experience and current physical activity level influence abdominal symptom severity in relation to psychological factors, particularly mindfulness. The results substantiated the hypothesis that increased physical activity in a state of low mindfulness increased the severity of abdominal symptoms. The results also demonstrated that mindfulness tendency was interactively influenced by the presence or absence of IBS symptoms and the level of the exercise experience.
The IBS group had higher IBS-SI, K6, and PSS and lowered MAAS than the non-IBS group. In previous studies, adolescent students with IBS were more likely to be depressed and anxious [22, 51, 52] and had a stronger reaction to stress [53], identical to the results of the present study. The health status of college students has been reported [54] to relate to perceived stress in college. It has been reported that students involved in medicine and nursing are exposed to various research and work-related stressors and are at high risk of developing burnout and psychotic symptoms [55, 56]. Such characteristics of the study participants may have been reflected in the results.
A comparison of the IBS and non-IBS groups regarding exercise-related variables showed no significant differences in the number of exercise days, exercise performance, or amount of physical activity. A previous study [57] using an Internet-based questionnaire reported a decrease in physical activity in IBS patients. Additionally, a previous study [31] that used pedometers in college students also showed decreased activity. However, in the present study, no group difference in physical activity between the IBS and non-IBS groups occurred. Compared to a study [58] related to physical activity using the IPAQ among Japanese university students in general, the physical activity of the participants in this study was lower in both the IBS and non-IBS groups. This may be related to the differences in the study environment among universities, and the effect of COVID-19 infection prevention measures on physical activity difficulties [59–61]. Due to COVID-19 infection control measures, part-time jobs were prohibited for university students and some departments offered home study through distance lectures. This may have resulted in an overall decrease in physical activity, making it impossible to obtain group differences.
On the other hand, the IBS group showed a positive correlation for IPAQ and K6 and a negative correlation for MAAS. This was not shown for the non-IBS group. In addition, two-way ANOVA showed interaction effects of MAAS and IPAQ on IBS-SI in the non-IBS group, but no effect of physical activity in the IBS group. This indicates that the IBS group is more likely to have negative feelings toward physical activity stimuli. Previous studies reported decreased activity and motivation to exercise in IBS subjects [31, 57]. In this study, the IBS group was less enthusiastic about physical activity in high school than the non-IBS group. The prevalence of IBS is higher during adolescence and young adulthood with decrease in healthy well-being and perceived stress [62]. The association between increased physical activity and decreased mental health found in this study may have influenced the decreased enthusiasm for exercise in high school in the IBS group. Physical activity is more likely to be associated with negative emotion in IBS subjects with less mindfulness.
There was an interaction relationship between the presence of IBS symptoms and past exercise experience on physical activity level, perception of stress state, and mindfulness tendency. In prior studies, IBS patients had abnormal cognitive behavioral aspects associated with reduced activation of inhibitory cortical areas involved in the downward regulation of pain and emotion, selective attention to threat-related stimuli and negative affect [15, 63]. Anxiety and depression worsen along with the long course of IBS and related disorders [64]. Conversely, IBS was found to develop with anxiety or depression after observation for 12 years in a cohort study [64]. One way to control IBS symptoms from stress, anxiety, and depression is through mindfulness-based stress reduction (MBSR) [35, 36]. MBSR encourages curiosity, compassion, and awareness of current experiences (thoughts, feelings, and bodily sensations) without criticism. It is particularly important in MBSR for IBS to promote non-reactivity of digestive-related anxiety [65]. Increased activity in brain regions involved in the cognitive regulation of pain processing (anterior cingulate cortex and anterior insular cortex) has been reported with mindfulness meditation [66]. In other words, abdominal symptoms due to IBS may be an important factor associated with mindfulness tendencies.
Past exercise experiences may also be an essential factor in facilitating a mindful state of mind. Exercise generally reduces depression [67] and anxiety [68], and relieves stress [69]. Exercise also improves self-monitoring of the whole body and attentional functions to control movement [70, 71]. Mindfulness is facilitated by the input and integrated processing of somatosensory information through exercise habits. These exercise-mediated psychological and neurophysiological effects improve stress response and abdominal symptoms and may provide the basis for increased mindfulness tendencies in the habit of paying attention to one's body. In the present study, IBS symptoms but high exercise experience showed no significant difference from the other group in stress perception and mindfulness tendency, suggesting that abundant exercise experience positively influences psychological tendencies.
A two-way ANOVA of the overall data further illustrates the relationship between physical activity and mindfulness, showing that IBS-SI was exacerbated by exposure to an environment with increased daily physical activity, while MAAS was low. Exercise therapy has been reported to be effective for IBS [2, 28, 29]. However, in the present study, we show that increased physical activity may exacerbate abdominal symptoms in conditions of decreased mindfulness tendency. Mindfulness has been reported to improve physical activity [72, 73], because physical activity creates an opportunity to pay attention to the physical sensations of the whole body, an effect primed by mindfulness [74]. In other words, when mindfulness is high, physical activity is not perceived as stressful and is not associated with abdominal symptoms because people perceive attention to their whole-body sensations as favorable. However, when mindfulness is low, physical activity is perceived as an unpleasant, stressful stimulus, which may exacerbate abdominal symptoms.
The results indicate that mindfulness tendency can be considered an indicator for the effectiveness of the physical activity. When introducing exercise therapy to IBS patients [28, 29], it may be possible to estimate how effective the exercise therapy will be by assessing the mindfulness tendency of the patients. Additionally, combining exercise therapy with psychotherapy, like MBSR [35, 36], may enhance the effectiveness of the exercise therapy further.
In this study, mindfulness tendencies were associated with abdominal symptoms. IBS affects an individual's brain activity through the brain–gut interactions via the autonomic nervous system and the immune system [1]. Therefore, it is crucial to simultaneously assess the visceral status and the individual's mindfulness tendency in a prospective study. In other words, prolonged IBS may reduce MAAS and decrease physical activity. Conversely, exercise habits may counter depression and anxiety and increase mindfulness tendencies. Multidisciplinary collaboration by physical therapists and other professionals to assess the living conditions and amount of physical activity of IBS patients may enhance the effectiveness of treatment.
There are some limitations in this study. Since this is a cross-sectional study, it is difficult to infer a causal relationship for each factor. Additionally, as past exercise experience and the amount of physical activity were confirmed by questionnaire responses, the possibility that cognitive bias or recall bias may have occurred cannot be ruled out. The survey response rate for this study was 47.7%, which is almost half the number of recruits. We consider the response rate to be generally reasonable without honorarium, but it may contain a little selection bias because of the responder’s interest in this study. Data in this study were from college students, limiting the generalizability of results to the general situation [75]. In this study, the present state of consultation to physicians and medication was not analyzed. History of medical visit of college students with IBS is low [76]. The ratio of receiving medical treatment for IBS in this survey is estimated to be lower than the reported value. In the previous epidemiological survey of IBS [12], influence of medical treatment on the surveyed findings was minimal. Even if some IBS subjects were treated by physicians, it unlikely influenced the main results of this study. This study was conducted under COVID-19 pandemic, which limits the activity of many humans [77]. We cannot rule out the influence of the pandemic on this study; however, this is not limited to this study, but also to other human studies. Moreover, the following questions could not be examined using the methods of this study. Does the presence or absence of IBS affect orientation toward exercise? Are abdominal symptoms changed depending on their orientation toward exercise and the amount and duration of physical activity performed? Follow-up studies, such as longitudinal or cohort studies, are needed to address these questions.
Conclusions
It is suggested that mindfulness and physical activity interactively affect the IBS severity. Further studies on how to design interventional trials for IBS patients with mindfulness and physical exercise are warranted.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to express our gratitude to the teachers at Sendai Seiyo Gakuin College, who arranged explanatory opportunities for the study participants during data collection. We also thank all the participants who devoted their time and gave samples for this study.
Abbreviations
- IBS
Irritable bowel syndrome
- HPA
Hypothalamic-pituitary-adrenal
- CNS
Central nervous system
- IBS-SI
IBS Severity Index, (IBS-SSS, IBS-Symptom Severity Scale)
- TED
Total exercise day
- IPAQ
International Physical Activity Questionnaire
- K6
Kessler 6 Scale
- PSS
Perceived Stress Scale
- MAAS
Mindful Attention Awareness Scale
- MBSR
Mindfulness-Based Stress Reduction
Author contributions
Koseki conceptualized the study and all authors contributed to the study design. Data collection was conducted by Koseki and Suzuki. The preparation of the research materials and data analysis were conducted by Koseki, Muratsubaki, Kanazawa, and Fukudo. Results and interpretations of the study data were discussed by all authors. The first draft of the manuscript was written by Koseki, and all authors commented on earlier versions of the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by a JSPS Grant-in-Aid for Scientific Research (JP21K11664). Individual research funds from Sendai Seiyo Gakuin College were also used.
Data Availability
Data are available in Figshare.
Declarations
Conflict of interest
There are no conflicts of interest to be noted in this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Enck P, Aziz Q, Barbara G, et al. Irritable bowel syndrome. Nat Rev Dis Primers. 2016;2:16014. doi: 10.1038/nrdp.2016.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fukudo S, Okumura T, Inamori M, et al. Evidence-based clinical practice guidelines for irritable bowel syndrome 2020. J Gastroenterol. 2021;56:193–217. doi: 10.1007/s00535-020-01746-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mayer EA, Naliboff BD, Chang L, et al. V. Stress and irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2001;280:G519–24. [DOI] [PubMed]
- 4.Fond G, Loundou A, Hamdani N, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): A systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2014;264:651–660. doi: 10.1007/s00406-014-0502-z. [DOI] [PubMed] [Google Scholar]
- 5.Fukudo S. Hypothalamic-pituitary-adrenal axis in gastrointestinal physiology. In: Physiol Gastrointest Tract. 2012;1:791–816.
- 6.Fukudo S. IBS: Autonomic dysregulation in IBS. Nat Rev Gastroenterol Hepatol. 2013;10:569–571. doi: 10.1038/nrgastro.2013.166. [DOI] [PubMed] [Google Scholar]
- 7.Kano M, Muratsubaki T, Van Oudenhove L, et al. Altered brain and gut responses to corticotropin-releasing hormone (CRH) in patients with irritable bowel syndrome Sci. Rep. 2017;7:12425. doi: 10.1038/s41598-017-09635-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tanaka Y, Kanazawa M, Kano M, et al. Relationship between sympathoadrenal and pituitary-adrenal response during colorectal distention in the presence of corticotropin-releasing hormone in patients with irritable bowel syndrome and healthy controls. PLoS ONE. 2018;13:e0199698. doi: 10.1371/journal.pone.0199698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yagihashi M, Kano M, Muratsubaki T, et al. Concordant pattern of the HPA axis response to visceral stimulation and CRH administration. Neurosci Res. 2021;168:32–40. doi: 10.1016/j.neures.2021.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Kanazawa M, Endo Y, Whitehead WE, et al. Patients and nonconsulters with irritable bowel syndrome reporting a parental history of bowel problems have more impaired psychological distress. Dig Dis Sci. 2004;49:1046–1053. doi: 10.1023/B:DDAS.0000034570.52305.10. [DOI] [PubMed] [Google Scholar]
- 11.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 12.Sperber AD, Bangdiwala SI, Drossman DA, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome Foundation global study. Gastroenterology. 2021;160:99–114. doi: 10.1053/j.gastro.2020.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Whitehead WE, Crowell MD, Robinson JC, et al. Effects of stressful life events on bowel symptoms: Subjects with irritable bowel syndrome compared with subjects without bowel dysfunction. Gut. 1992;33:825–830. doi: 10.1136/gut.33.6.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okami Y, Kato T, Nin G, et al. Lifestyle and psychological factors related to irritable bowel syndrome in nursing and medical school students. J Gastroenterol. 2011;46:1403–1410. doi: 10.1007/s00535-011-0454-2. [DOI] [PubMed] [Google Scholar]
- 15.Mayer EA, Labus JS, Tillisch K, et al. Towards a systems view of IBS. Nat Rev Gastroenterol Hepatol. 2015;12:592–605. doi: 10.1038/nrgastro.2015.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kesaniemi YK, Danforth E, Jr, Jensen MD, et al. Dose–response issues concerning physical activity and health: an evidence-based symposium. Med Sci Sports Exerc. 2001;33(Suppl):S351–S358. doi: 10.1097/00005768-200106001-00003. [DOI] [PubMed] [Google Scholar]
- 17.Nishii A, Amemiya S, Kubota N, et al. Adaptive changes in the sensitivity of the dorsal raphe and hypothalamic paraventricular nuclei to acute exercise, and hippocampal neurogenesis may contribute to the antidepressant effect of regular treadmill running in rats. Front Behav Neurosci. 2017;11:235. doi: 10.3389/fnbeh.2017.00235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Melancon MO, Lorrain D, Dionne IJ. Exercise increases tryptophan availability to the brain in older men age 57–70 years. Med Sci Sports Exerc. 2012;44:881–887. doi: 10.1249/MSS.0b013e31823ede8e. [DOI] [PubMed] [Google Scholar]
- 19.Jandackova VK, Scholes S, Britton A, et al. Healthy lifestyle and cardiac vagal modulation over 10 years: Whitehall II cohort study. J Am Heart Assoc. 2019;8:e012420. doi: 10.1161/JAHA.119.012420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gourine AV, Ackland GL. Cardiac vagus and exercise. Physiology (Bethesda) 2019;34:71–80. doi: 10.1152/physiol.00041.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fox KR. The influence of physical activity on mental well-being. Public Health Nutr. 1999;2:411–418. doi: 10.1017/S1368980099000567. [DOI] [PubMed] [Google Scholar]
- 22.Josefsson T, Lindwall M, Archer T. Physical exercise intervention in depressive disorders: Meta-analysis and systematic review. Scand J Med Sci Sports. 2014;24:259–272. doi: 10.1111/sms.12050. [DOI] [PubMed] [Google Scholar]
- 23.Droste SK, Gesing A, Ulbricht S, et al. Effects of long-term voluntary exercise on the mouse hypothalamic-pituitary-adrenocortical axis. Endocrinology. 2003;144:3012–3023. doi: 10.1210/en.2003-0097. [DOI] [PubMed] [Google Scholar]
- 24.Hill EE, Zack E, Battaglini C, et al. Exercise and circulating cortisol levels: The intensity threshold effect. J Endocrinol Invest. 2008;31:587–591. doi: 10.1007/BF03345606. [DOI] [PubMed] [Google Scholar]
- 25.Song BK, Cho KO, Jo Y, et al. Colon transit time according to physical activity level in adults. J Neurogastroenterol Motil. 2012;18:64–69. doi: 10.5056/jnm.2012.18.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dainese R, Serra J, Azpiroz F, et al. Effects of physical activity on intestinal gas transit and evacuation in healthy subjects. Am J Med. 2004;116:536–539. doi: 10.1016/j.amjmed.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 27.Hajizadeh Maleki B, Tartibian B, Mooren FC, et al. Low-to-moderate intensity aerobic exercise training modulates irritable bowel syndrome through antioxidative and inflammatory mechanisms in women: Results of a randomized controlled trial. Cytokine. 2018;102:18–25. doi: 10.1016/j.cyto.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 28.Johannesson E, Ringström G, Abrahamsson H, et al. Intervention to increase physical activity in irritable bowel syndrome shows long-term positive effects. World J Gastroenterol. 2015;21:600–608. doi: 10.3748/wjg.v21.i2.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou C, Zhao E, Li Y, et al. Exercise therapy of patients with irritable bowel syndrome: a systematic review of randomized controlled trials. Neurogastroenterol Motil. 2019;31:e13461. doi: 10.1111/nmo.13461. [DOI] [PubMed] [Google Scholar]
- 30.Guo YB, Zhuang KM, Kuang L, et al. Association between diet and lifestyle habits and irritable bowel syndrome: a case-control study. Gut Liver. 2015;9:649–656. doi: 10.5009/gnl13437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hamaguchi T, Tayama J, Suzuki M, et al. Correction: The effects of locomotor activity on gastrointestinal symptoms of irritable bowel syndrome among younger people: an observational study. PLoS ONE. 2020;15:e0244465. doi: 10.1371/journal.pone.0244465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 33.Knapen J, Vancampfort D, Moriën Y, Marchal Y. Exercise therapy improves both mental and physical health in patients with major depression. Disabil Rehabil. 2015;37:1490–1495. doi: 10.3109/09638288.2014.972579. [DOI] [PubMed] [Google Scholar]
- 34.Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. 2004;11:230–241. doi: 10.1093/clipsy.bph077. [DOI] [Google Scholar]
- 35.Gaylord SA, Palsson OS, Garland EL, et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: Results of a randomized controlled trial. Am J Gastroenterol. 2011;106:1678–1688. doi: 10.1038/ajg.2011.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naliboff BD, Smith SR, Serpa JG, et al. Mindfulness-based stress reduction improves irritable bowel syndrome (IBS) symptoms via specific aspects of mindfulness. Neurogastroenterol Motil. 2020;32:e13828. doi: 10.1111/nmo.13828. [DOI] [PubMed] [Google Scholar]
- 37.Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150:1393–1407. doi: 10.1053/j.gastro.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 38.O’Donnell LJ, Virjee J, Heaton KW. Detection of pseudodiarrhoea by simple clinical assessment of intestinal transit rate. BMJ. 1990;300:439–440. doi: 10.1136/bmj.300.6722.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blake MR, Raker JM, Whelan K. Validity and reliability of the Bristol Stool Form Scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44:693–703. doi: 10.1111/apt.13746. [DOI] [PubMed] [Google Scholar]
- 40.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: A simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11:395–402. doi: 10.1046/j.1365-2036.1997.142318000.x. [DOI] [PubMed] [Google Scholar]
- 41.Shinozaki M, Kanazawa M, Sagami Y, et al. Validation of the Japanese version of the Rome II modular questionnaire and irritable bowel syndrome severity index. J Gastroenterol. 2006;41:491–494. doi: 10.1007/s00535-006-1799-9. [DOI] [PubMed] [Google Scholar]
- 42.Ayabe M, Kumahara H, Yamaguchi-Watanabe A, et al. Appendicular muscle mass and exercise/sports participation history in young Japanese women. Ann Hum Biol. 2019;46:335–339. doi: 10.1080/03014460.2019.1641221. [DOI] [PubMed] [Google Scholar]
- 43.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 44.Murase N, Katsumura T, Ueda C, et al. Validity and reliability of Japanese version of International Physical Activity Questionnaire. J Health Welf Stat. 2002;49:1–9. [Google Scholar]
- 45.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- 46.Furukawa TA, Kawakami N, Saitoh M, et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int J Methods Psychiatr Res. 2008;17:152–158. doi: 10.1002/mpr.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 48.Sumi K. Reliability and validity of the Japanese version of the Perceived Stress Scale. Jpn J Health Psychol. 2006;19:44–53. doi: 10.11560/jahp.19.2_44. [DOI] [Google Scholar]
- 49.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 50.Fujino M, Kajimura S, Nomura M. Development and validation of the Japanese version of the mindful attention awareness scale using item response theory analysis. Jpn J Pers. 2015;24:61–76. [Google Scholar]
- 51.Tayama J, Nakaya N, Hamaguchi T, et al. Effects of personality traits on the manifestations of irritable bowel syndrome. Biopsychosoc Med. 2012;6:20. doi: 10.1186/1751-0759-6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sugaya N, Nomura S. Relationship between cognitive appraisals of symptoms and negative mood for subtypes of irritable bowel syndrome. Biopsychosoc Med. 2008;2:9. doi: 10.1186/1751-0759-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Addante R, Naliboff B, Shih W, et al. Predictors of health-related quality of life in irritable bowel syndrome patients compared with healthy individuals. J Clin Gastroenterol. 2019;53:e142–e149. doi: 10.1097/MCG.0000000000000978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.El Ansari W, Oskrochi R, Haghgoo G. Are students’ symptoms and health complaints associated with perceived stress at university? Perspectives from the United Kingdom and Egypt. Int J Environ Res Public Health. 2014;11:9981–10002. doi: 10.3390/ijerph111009981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Labrague LJ, McEnroe-Petitte DM, Gloe D, et al. A literature review on stress and coping strategies in nursing students. J Ment Health. 2017;26:471–480. doi: 10.1080/09638237.2016.1244721. [DOI] [PubMed] [Google Scholar]
- 56.Kunzler AM, Helmreich I, König J, et al. Psychological interventions to foster resilience in healthcare students. Cochrane Database Syst Rev. 2020;7:CD013684. [DOI] [PMC free article] [PubMed]
- 57.Miwa H. Life style in persons with functional gastrointestinal disorders Large scale internet survey of lifestyle in japan. Neurogastroenterol Motil. 2012;24(464–71):e217. doi: 10.1111/j.1365-2982.2011.01872.x. [DOI] [PubMed] [Google Scholar]
- 58.Okazaki K, Okano S, Haga S, et al. One-year outcome of an interactive internet-based physical activity intervention among university students. Int J Med Inform. 2014;83:354–360. doi: 10.1016/j.ijmedinf.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 59.Romero-Blanco C, Rodríguez-Almagro J, Onieva-Zafra MD, et al. Physical activity and sedentary lifestyle in university students: changes during confinement due to the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:6567. doi: 10.3390/ijerph17186567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Castañeda-Babarro A, Arbillaga-Etxarri A, Gutiérrez-Santamaría B, et al. Physical activity change during COVID-19 confinement. Int J Environ Res Public Health. 2020;17:6878. doi: 10.3390/ijerph17186878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Luciano F, Cenacchi V, Vegro V, et al. COVID-19 lockdown: Physical activity, sedentary behaviour and sleep in Italian medicine students. Eur J Sport Sci. 2021;21:1459–1468. doi: 10.1080/17461391.2020.1842910. [DOI] [PubMed] [Google Scholar]
- 62.Endo Y, Shoji T, Fukudo S, et al. The features of adolescent irritable bowel syndrome in Japan. J Gastroenterol Hepatol. 2011;26(Suppl3):106–109. doi: 10.1111/j.1440-1746.2011.06637.x. [DOI] [PubMed] [Google Scholar]
- 63.Aizawa E, Sato Y, Kochiyama T, et al. Altered cognitive function of prefrontal cortex during error feedback in patients with irritable bowel syndrome, based on FMRI and dynamic causal modeling. Gastroenterology. 2012;143:1188–1198. doi: 10.1053/j.gastro.2012.07.104. [DOI] [PubMed] [Google Scholar]
- 64.Koloski NA, Jones M, Kalantar J, et al. The brain–gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut. 2012;61:1284–1290. doi: 10.1136/gutjnl-2011-300474. [DOI] [PubMed] [Google Scholar]
- 65.Garland EL, Gaylord SA, Palsson O, et al. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. J Behav Med. 2012;35:591–602. doi: 10.1007/s10865-011-9391-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zeidan F, Martucci KT, Kraft RA, et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci. 2011;31:5540–5548. doi: 10.1523/JNEUROSCI.5791-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Babyak M, Blumenthal JA, Herman S, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62:633–638. doi: 10.1097/00006842-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 68.Stubbs B, Vancampfort D, Rosenbaum S, et al. An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: a meta-analysis. Psychiatry Res. 2017;249:102–108. doi: 10.1016/j.psychres.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 69.Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44:81–121. doi: 10.1007/s40279-013-0090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Diamond A, Lee K. Interventions shown to aid executive function development in children 4–12 years old. Science. 2011;333:959–964. doi: 10.1126/science.1204529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dishman RK, Berthoud HR, Booth FW, et al. Neurobiology of exercise. Obesity (Silver Spring) 2006;14:345–356. doi: 10.1038/oby.2006.46. [DOI] [PubMed] [Google Scholar]
- 72.Don BP, Van Cappellen P, Fredrickson BL. Understanding engagement in and affective experiences during physical activity: the role of meditation interventions. Psychosom Med. 2021;83:592–601. doi: 10.1097/PSY.0000000000000909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gilbert D, Waltz J. Mindfulness and health. Behav Mindfulness. 2010;1:227–234. doi: 10.1007/s12671-010-0032-3. [DOI] [Google Scholar]
- 74.Salmoirago-Blotcher E, Druker S, Frisard C, et al. Integrating mindfulness training in school health education to promote healthy behaviors in adolescents: feasibility and preliminary effects on exercise and dietary habits. Prev Med Rep. 2018;9:92–95. doi: 10.1016/j.pmedr.2018.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sears DO. College sophomores in the laboratory: influences of a narrow data base on social psychology’s view of human nature. J Pers Soc Psychol. 1986;51:515–530. doi: 10.1037/0022-3514.51.3.515. [DOI] [Google Scholar]
- 76.Drossman DA, Sandler RS, McKee DC, et al. Bowel patterns among subjects not seeking health care. Use of a questionnaire to identify a population with bowel dysfunction. Gastroenterology. 1982;83:529–534. [PubMed]
- 77.Otani K, Watanabe T, Higashimori A, et al. A questionnaire-based survey on the impact of the COVID-19 pandemic on gastrointestinal endoscopy in Asia. Digestion. 2022;103:7–21. doi: 10.1159/000520287. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available in Figshare.