Abstract
Over 70% of men are overweight, and most desire weight loss; however, men are profoundly underrepresented in weight loss programs. Gamification represents a novel approach to engaging men and may enhance efficacy through two means: (1) game-based elements (e.g., streaks, badges, team-based competition) to motivate weight control behaviors and (2) arcade-style “neurotraining” to enhance neurocognitive capacities to resist the temptation of unhealthy foods and more automatically select healthy foods. This study will use a 2 x 2 factorial design to examine the independent and combinatory efficacy of gamification and inhibitory control training (ICT). Men with overweight/obesity (N = 228) will receive a 12-month mobile weight loss program that incorporates behavioral weight loss strategies (e.g., self-monitoring, goal setting, stimulus control). Men will be randomly assigned to a non-gamified or gamified version, and an active or sham ICT. A game design company will create the program, with input from a male advisory panel. Aims of the project are to test whether a gamified (versus non-gamified) weight loss program and/or ICT (versus sham) promotes greater improvements in weight, diet, and physical activity; whether these treatment factors have combinatory or synergistic effects; to test whether postulated mechanisms of action (increased engagement, for gamification, and inhibitory control, for ICT) mediate treatment effects; and whether baseline gameplay frequency and implicit preferences for ICT-targeted foods moderate effects. It is hoped this study will contribute to improved mHealth programs for men and enhance our understanding of the impact of gamified elements and neurocognitive training on weight control.
Keywords: obesity, weight loss, men, gamification, inhibitory control training
Introduction
Over 70% of US men have overweight/obesity.1 Although 41% of men with overweight/obesity express interest in losing weight,2 men find conventional interventions unappealing,3,4 and few enroll in either face-to-face or mobile programs.5 In attempts to attract men, researchers and commercial entities have utilized modified advertising when discussing weight loss benefits, focusing on improvements in job performance and less on changes in body shape)6,7 and recruitment strategies (e.g., in-stadium advertising).8 In addition, researchers have created male-oriented programs that incorporate effective components of weight loss (e.g., dietary restriction, physical activity, and teaching behavioral tools) in self-help- and internet-based in format while emphasizing autonomy and flexibility—attributes that men prefer.9 For instance, in one weight loss program designed for men, men selected the order of online lessons and calorie reduction strategies.10 However, outcomes of these approaches have not resulted in sufficient increases in male interest and enrollment. Thus, a radically different form of intervention that appeals to men must be identified.11,12
Gamification
A game-based (“gamified”) mHealth program holds promise in attracting men and enhancing efficacy. Video games are highly appealing to men (over 70% of men play regularly),13,14 and men are more motivated by aspects of gamification (e.g., competition) than women.15,16 Gamification techniques (e.g., badges, leaderboards, “streaks,” team-based competition, story elements), have shown promise for improving health behavior outside the context of weight loss.17 For example, “exergame” mHealth interventions have successfully utilized gamification to increase physical activity enjoyment18 and behavior.18–20
To date, most of the very few attempts to gamify weight loss have prioritized increasing physical activity and shown only modest success.21 Gamification may be more effective in programs that primarily emphasize dietary intake, the stronger determinant of weight loss.22,23
Inhibitory Control Training
One promising way to gamify eating behavior is through neurocognitive training games (“neurotraining”), such as inhibitory control training (ICT), which trains basic brain capacity to inhibit responses for high calorie food and/or changes food valuation, such that highly palatable foods seem less appealing (thus facilitating consumption of lower calorie alternatives).24-26 ICTs with specific attributes (e.g., trainings delivered repeatedly) can successfully reduce consumption,27-29 change palatability ratings of targeted foods/beverages,30,31 reduce calorie intake,32 and improve short-term weight loss.32-34 ICT could integrate into a gamified system, as it requires trainees to quickly follow rules on a specialized computer interface, adjusting difficulty levels with performance. The research team’s pilot study demonstrated that a short, daily ICT game produced greater weight loss for individuals with higher-than-average implicit preferences for high-sugar foods, compared to an almost-identical sham training.35 Moreover, adding gamified elements to the ICT produced additional weight loss among men.36
Study Aims
Previous work, including our pilot, demonstrates promise for gamification and neurotraining to facilitate weight loss. However, critical questions remain unanswered, including: whether ICT and gamification have independent and/or synergistic effects, and whether ICT and/or gamification facilitate meaningful weight loss long-term (>1 year). The current project tests hypotheses that (1) a gamified weight loss program and ICT will independently promote greater improvements in weight, diet, and physical activity among men with overweight/obesity, and (2) increased engagement, inhibitory control and valuation of healthy foods, and decreased valuation of unhealthy foods, will mediate these effects. As an exploratory aim, we will examine the interaction of gamification and ICT to determine whether they have combinatory or synergistic effects. Because those with stronger implicit preferences for targeted foods may benefit most from improvements in inhibitory control, we also aim to test whether baseline implicit preferences moderate neurotraining effects. Finally, we will test the hypothesis that men with more baseline video gameplay will benefit the most from gamification.
Methods
Study Design
This study will use a 2 x 2 factorial design (see Table 1). Participants (N = 228) will be randomized to a gamified or non-gamified version of a 12-month mobile weight loss program. We will examine outcomes at 1-month, 6-month, and post-treatment (12-months, the primary study endpoint) assessments. The study coordinator will randomize participants following the baseline assessment via computerized block randomization by age and BMI to either non-game or game factor and sham or ICT neurotraining factor. In both conditions, the program will include digital self-monitoring, neurotraining, self-selected dietary targets (to use as neurotraining stimuli), and physical activity and calorie goals. Both programs will also include gold-standard behavioral weight loss strategies from previous successful in-person, remote, and mHealth interventions.5,37,38 Methods of customizing for men, including intervention modules tailored for men, and autonomy with dietary choices will be adapted from prior behavioral weight loss programs for men.8 The game-based version will feature additional gamification features (e.g., teams, badges, leveling, challenges), all within a themed game wrapper (e.g., science fiction; spaceships). To isolate the potential effect of the ICT within the respective programs, participants in both conditions will also be randomly assigned to receive the true ICT or sham training. During the program development phase, we will recruit a separate group of 150 men with overweight or obesity to provide opinions and feedback on gamification features and user testing through surveys and focus groups at each iteration.
Table 1.
The 4 Study Conditions of the 2 x 2 Factorial Design
| Gamification of Behavioral Weight Loss App |
|||
|---|---|---|---|
| Gamified | Non-Gamified | ||
| Inhibitory Control Neuro-training (ICT) | Sham (inert) | Gamified weight loss with gamified, sham ICT | Non-gamified weight loss with non-gamified sham ICT |
| Active | Gamified weight loss with active, gamified ICT | Non-gamified weight loss with non-gamified, active ICT | |
Trial registration and Informed Consent
The study was pre-registered on ClinicalTrials.gov (NCT05408494) and approved by the Drexel Institutional Review Board (2107008697). Before enrollment participants will meet (via video call) with a staff member who will fully explain study procedures, answer any questions, and then review, and obtain electronic signature on the informed consent document.
Interventions
Iterative Development
App Development.
Both the control and the game-based intervention program will be developed by FableVision Studios, in close collaboration with the investigators. FableVision will employ a standard iterative development process which involves many cycles of fast prototyping.
Advisory Panel.
Using ResearchMatch, we will recruit approximately 150 men (ages 18-55) with overweight/obesity to join an advisory panel to inform the development of the gamified weight loss app and ICT. Men will be regularly invited to complete surveys and participate in focus groups to share their opinions throughout app development. The advisory panel will also perform user testing and provide feedback on the app in its early iterations. Men will be compensated $40 an hour. As an example, a selection of men (N = 70) was provided with mockups created by the game design company portraying 15 different gamification themes and were asked to rank these in order of appeal (a space adventure/battle theme emerged as the top choice).
Non-Gamified (Base) App
The app hosts an independent 12-month mobile weight loss program that includes digital self-monitoring, goal setting, feedback on progress, simplified and self-selected dietary targets, and psychoeducation on gold-standard behavioral weight loss strategies. Tracked weight, calorie, and physical activity data will be displayed graphically, with the ability to view data across different time periods and in conjunction with goals (Figure 1a). Participants will set weight loss goals between 0-3 lbs. each week, with zero representing the goal of weight loss maintenance (Figure 1b). Participants will also set (and can revise) a total weight loss goal, with a 10% weight loss goal encouraged as per the behavioral weight loss standard. Weekly informational modules featuring text, tables, figures, and video will be assigned each week (Figure 1c).
Figure 1.

Non-gamified (control) App
To promote autonomy and identify ICT targets,39 participants will select (from a menu of targets within the app) “green” (lower-calorie, healthy foods whose consumption should be increased) and “red” target foods (higher-calorie and/or less healthy foods whose consumption should be decreased). Target foods will be classified as either red or green based on specific definitions that relate to energy density and larger category grouping (e.g., all sweetened beverages are red, and all vegetables are green). Each week, for four weeks, participants will choose 1 new red category (e.g., fast food) and 5 specific red food targets within that category (e.g., burgers, fries, chicken nuggets, chicken sandwiches, fried fish sandwiches), such that they will have identified 4 red categories and 20 specific red target foods to avoid/reduce at the end of the month. Similarly, participants will choose 1 new green category and 3 specific green food targets within that category over four weeks, ending with 4 green categories and 12 specific green target foods whose consumption participants strive to increase. Starting in week 5, participants can choose to swap out red and/or green food categories and foods, or to maintain them, based on their current goals. Foods that participants track in Fitbit will be categorized as red or green and displayed in the program app, sorted by calorie contribution (red foods) and consumption (green foods) in order of to help participants select the best targets for their future eating behavior.
Gamified App
For the gamification conditions, the app will include not only the base features described above, but also gamification elements to incentivize desired behaviors and outcomes, e.g., self-monitoring (of weight, calories, and physical activity), weight loss, ICT/sham completion, physical activity, and reductions or increases in consumption of targeted red- and green-zone foods (Figure 2a). Table 2 delineates components included in the non-gamified and gamified apps. Behaviors and outcomes are operationalized both in terms of increasing levels (e.g., 4% to 5% weight loss, Figure 2b) and streaks (e.g., meeting 10 moderate-to-vigorous physical activity goals in a row, weighing 14 days in a row). Gamified incentives include badges rewarding important program benchmarks (e.g., 10% weight loss), team campaigns challenging users to complete a challenge within a 2-week period (e.g., accumulate a total of 300 minutes of moderate to vigorous physical activity), and in-game currency or “gems” earned by completing program tasks (e.g., weighing in, completing team campaigns). Points can be spent on ship upgrades and customizations, and power ups used within the ICT minigames.
Figure 2.

Gamified app mockup
Table 2.
Composition of intervention conditions
| Both Base and Gamified App | Gamified App Only |
|---|---|
| Interactive, educative text and video modules based on gold standard behavioral weight loss interventions Simplified dietary targets, allowing for autonomy Graded and increasing moderate-vigorous physical activity goals Calorie and weight-loss goal Simplified, in-app dietary tracking Tracking of physical activity in-app Neurotraining (inhibitory control training)—sham or active (i.e., tailored to self-selected dietary targets) |
Gamification strategies to enhance behavior change • Tracking and rewarding behavioral “streaks” (e.g., viewing modules, tracking weight, tracking physical activity) • Tracking and rewarding major milestones through badges (e.g., weight loss benchmarks, meeting physical activity goals, reducing consumption of targeted food) • Cooperati on with team members for team points • Levelling system rewarding progress in major milestones (i.e., Physical activity, weight loss, Inhibitory Control Training game) Neurotraining video game • Inhibitory Control Training (active or sham) will be built into an engaging video game with story, graphics, sound effects, music, feedback, scoring |
Participants will also be able to compete and cooperate with one another in pre-assigned teams, accumulating points for all app activities. Participants can view their team’s progress in real time on a universal leaderboard (Figure 2a). In addition, teams will participate in monthly “campaigns,” i.e., larger challenges based on specific metrics (e.g., number of meals or snacks tracked). The campaign’s goal will be scaled based on the number of participants per team (e.g., walking the equivalent of 5 miles per team member, such that a team of 5 would have a goal of 25 miles, and a team of 10 would have a goal of 50 miles). All teams who meet the goal will earn points; more points are awarded to the team who ranks first. Participant accomplishments for their team are rewarded through in-game currency and upgrades, and significant accomplishments will be broadcast so that they can be recognized by other team members through “high fives” and other simple social interactions. The ICT will also be gamified in this condition; see description below.
Inhibitory Control Training
Participants will be assigned to receive either an active or inert (sham) ICT. Training (ICT and sham) length and schedule will be the same (7 minutes or approximately 220 trials; daily for 4 weeks, then weekly for 11 months) across conditions. In order to determine the specific methodology of our ICT (i.e., timing of Go/No Go signals and adaptation as participants improve), we ran an ICT evaluation mini-study to compare three versions of ICT, as well as a sham, that have been utilized by our group and others. In brief, we randomized 181 men with overweight to one of three ICT variations or a sham. Results (in terms of preferring healthy compared to unhealthy foods) indicated that the three active ICT versions were comparable and superior to sham, but that a delay between the stimulus and Go/No Go signal produced the best results.
Thus, in the active ICT conditions, a 50 millisecond pause will separate the presentation of the stimuli and the Go or No Go signal. The stimuli will be made up of each participant’s personalized red and green targets, and those targets will be both direct food matches and randomly selected foods from these target categories (to promote greater generalization to more foods). Participants must tap or refrain from tapping according to the signal, and difficulty is adaptive, such that the time given to respond starts at 800 milliseconds, but, every 24 trials, will increase or decrease by 50 milliseconds depending on accuracy (i.e., latency will decrease if accuracy is high and increase if accuracy is low).
As per our pilot study36, sham ICT conditions are designed to be an attention control without training inhibition. In this condition, 50% of the stimuli will be personalized red/green food targets (as per above) and 50% will be non-food items. Participants will have a limited time (adapted as above) to tap on the on the left or right side of the screen to specify if the stimulus is a food or non-food.
Gamified vs. Non-Gamified ICT.
In the non-gamified conditions, ICT training will take place on a blank screen, with no audio or other gamified features (Figure 3a). In the gamified condition, the ICT training will occur within the context of a narrative goal (e.g., delivering goods to planets or fighting aliens and enemy ships; Figure 3b), with occasional side tasks (e.g., wiping asteroid debris from windshield). Participant responses to stimuli will be used to determine their progress toward that goal (e.g., faster and more accurate responses mean that their ship will fly faster). Players can use “power-ups” to improve their ships’ abilities and can receive these power-ups as a reward for satisfactory performance during the trials.
Figure 3.
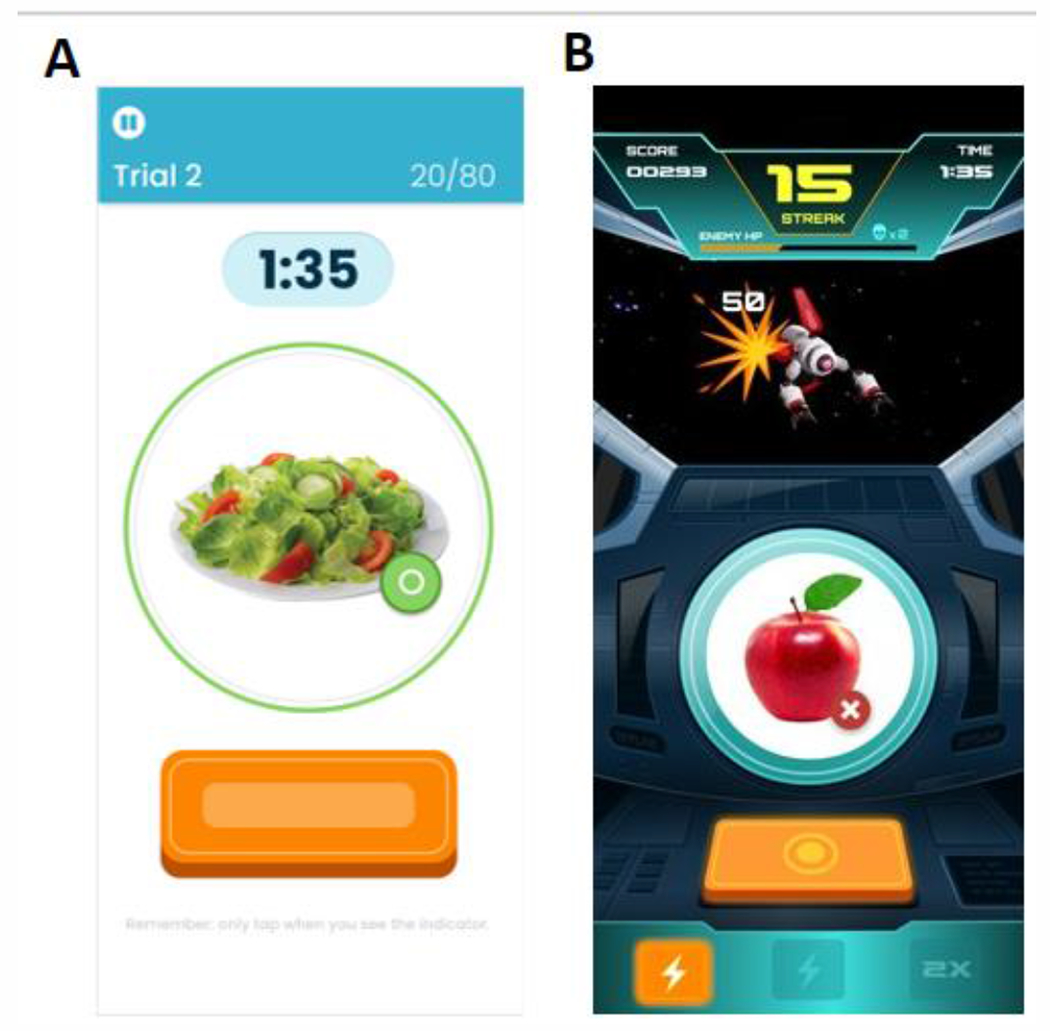
Non-Gamified and Gamified Inhibitory Control Training Mock-Ups
Note. Panel A depicts the non-gamified active inhibitory control training; Panel B depicts the gamified activity inhibitory control training.
Participants
Men with overweight or obesity (N = 228) will be recruited nationally using social media posts and ads, web search, and radio and podcast shows with high male listenership. To ensure sufficient recruitment of racial/ethnic minority participants, advertisements will include culturally diverse images and target outlets with predominantly minority audiences.
Eligibility
Participants will be excluded if they: are unable to provide informed consent, engage in sufficient physical activity to meet the program requirements (defined as the ability to walk at least two city blocks without stopping); have a medical or psychiatric condition that currently affects weight/appetite, may limit participants’ ability to comply with the program, or may make participation unsafe; have recently begun or changed the dose of a weight-affecting medication; have a history of bariatric surgery; weight loss >5% in the past 3 months; or are planning to participate in another weight loss program (self-help or guided) over the next 12 months (exercise programs and/or personal trainers are acceptable). BMI must be between 27 kg/m2 and 50 kg/m2 . Age will be restricted to 18-55 given that older adults may respond differently to neurotraining. A minimum BMI of 27 kg/m2 was chosen because participants with a lower BMI may not be appropriate candidates for a 10% weight loss. A maximum BMI of 50 kg/m2 was chosen because those with a higher BMI frequently need more intensive intervention and exhibit more serious medical comorbidities.
Assessments
Assessments will be conducted remotely and will occur at months 0, 1, 6 and 12 months according to the schedule shown in Table 3. To maximize retention and attendance of assessments, compensation will increase over consecutive assessments ($50 for 0-month, $60 for 1-month, $75 for 6-month, $100 for 12-month).
Table 3.
Variables Assessed at each Assessment Point
| Assessment point (month) |
|||||
|---|---|---|---|---|---|
| Variable | Measure | 0 | 1 | 6 | 12 |
| Outcomes | |||||
| Weight | Fitbit Aria Wireless scale | X | X | X | X |
| Physical Activity | Fitbit Inspire Activity Tracker | X | X | X | X |
| Dietary Intake | Fitbit app | X | X | X | X |
| Mediators | |||||
| Food-specific inhibitory control | Go/No Go task | X | X | X | X |
| Valuation of food | Visual analog rating scale | X | X | X | X |
| Engagement | Percent of possible engagements | X | X | X | X |
| Enjoyment | Likert Self-report | X | X | X | X |
| Moderators | |||||
| Baseline gameplay | Gaming Frequency | X | |||
| Implicit preference for high-calorie foods | Implicit Association Test | X | |||
Measures
Outcomes
Weight will be measured using the Fitbit Aria wireless scale, and we will ensure accuracy by providing specific instructions to participants (e.g., ensure the scale is on a flat, hard surface; weigh upon waking, without shoes or heavy clothes) and by using an average of 5 daily weights for each timepoint (disregarding outliers). Such methods have been validated against clinic-measured weights.40 Calorie intake and intake of red and green foods will be measured using the Fitbit app’s built-in dietary tracking system and our customized database. The customized database will have pre-categorized the items men in our previous trials have tracked using the Fitbit app, and we will also complete daily categorization of newly-tracked items throughout the trial. Physical activity will be measured in minutes of moderate-to-vigorous physical activity using the Fitbit Inspire 3, a wrist-worn activity tracker.
Mediators
Food-specific inhibitory control will be measured with a basic, non-gamified Go/No Go task containing 224 trials, similar to the training described above (e.g., short delay between presentation of the stimuli and Go or No Go signal). The stimuli will be a combination of personalized red/green target foods, as described above for the ICT. The Go/No Go will have a starting latency of 800 milliseconds to respond (or withhold a response) to a cue, and this time can increase or decrease by 50ms, every 28 trials, depending on accuracy (i.e., latency will decrease with better performance and increase with poorer performance). Inhibitory control ability will be indexed as the lowest (most difficult) latency level wherein the participant obtained at least 95% accuracy.
Valuation of red and green foods.
Images are presented in the center of the screen one by one, in random order, with the question, “How attractive does this food item look to you?” presented below each image. Images are selected in the same manner as described above for the ICT (i.e., a mix of personalized green/red foods). Participants rate each item by clicking on slider ranging from 0 (not at all attractive) to 100 (extremely attractive). This explicit rating task has proven to be sensitive to training-induced value changes of food items.41
Engagement is operationalized as total time spent on app, as well as the percentage of engagements (out of total possible) across each of these categories: 1) web modules; 2) dietary goal setting; 3) physical activity tracking; 4) dietary tracking; 5) self-weighing; and 6) neurotraining.
Enjoyment will be measured with three Likert scale items assessing the extent to which playing the game was entertaining, enjoyable, and fun.42,43
Moderators
Baseline gameplay is operationalized as the self-reported number of hours per week a participant spends playing games on a smartphone, tablet, game console, and/or computer.
Implicit preferences to highly palatable foods will be measured using the Implicit Association Test. Participants are presented with 3 types of images: good, bad, and food, and sort these images into categories using screen taps. The instructions in each block (of which there are 5) alternate between asking participants to sort, as quickly as possible, food images into the “good” or “bad” categories. A shorter response time to a stimulus indicates a more belief-consistent relationship (e.g., if the participant more quickly sorts a red food image into the “good” category, they have a more positive implicit association with that food)44,45 The food images are selected in the same manner as described above for the Go/No Go task.
Statistical analyses
Baseline variables that differ by condition will be considered for use as covariates in the analyses described below.
Aim 1. We will model the pattern of weight change in participants over time using multilevel models.46 The first level will model an individual participant’s weight loss over time. At the second level, the individual intercept and slope will be entered as outcomes with the intervention factor (e.g., gamification ON vs. OFF) as a predictor. The cross-level interaction between time and intervention factor will be used to determine the effect of the intervention factor on the pattern of change in weight loss. Restricted maximum likelihood will be used to estimate model parameters and to test the significance of random effects. Linear and higher-order time effects will be examined based on model selection criterion such as Akaike Information Criterion and Bayesian Information Criterion.
We will model the change trajectory of diet and physical activity separately using multilevel models similar to what has been described above. The cross-level interaction between time and intervention factor will be used to determine whether improvements in diet and physical activity will be greater when the intervention factor is ON. In addition, statistical contrasts will be performed for each of the intervention factors on primary and secondary outcomes at 12 months.
Aim 2. We will determine whether temporally precedent gains in inhibitory control, valuation and engagement from baseline to later time points (1 and 6 months) mediate differences in weight loss from baseline to 12 months across intervention factors. We will use the mediation model outlined by Preacher and Hayes to estimate the total and specific indirect effects of the potential mediator.47,48 The indirect pathway from gamification to the potential mediator allows us to test whether gamification will produce greater engagement. Similarly, the indirect pathway from neurotraining to the potential mediator allows us to test whether neurotraining will yield improved inhibitory control and/or valuation. The significance of the mediating effect will be based on the bias-corrected bootstrap test.47
Exploratory Aim.
Potential moderators will be added to the models described in aim 1 and allowed to interact with time and intervention factor. The moderator will be considered significant if the interaction term is significant.
Power analysis.
Using the method described by Raudenbush and implemented with Optimal Design, power calculations were made for the multilevel models proposed in the primary aim.49-51 In the pilot DASH project, the effect size of gamification on weight loss was d = 0.59 for men, and the effect size of neurotraining (ICT vs. sham) was d = 0.75 for those with higher implicit preferences for targeted foods. Thus, for our power analysis, we conservatively set an effect size of 0.59. A sample size of 182 is required for 80% power to detect an effect size of 0.59 at α = .05 and four assessment points, assuming the ratio of the variability of level-1 coefficient to the variability of level-1 residual is at least one. If 20% attrition is allowed, the required sample size is 228. This number equals or surpasses the sample size needed for the secondary and tertiary aims.
Attrition.
We will conduct an intention-to-treat analysis to ensure treatment effects are estimated more accurately. Likelihood-based estimation methods and multiple imputation models will be used to handle missing data.52-54 If the missingness mechanism is related to the missing outcome itself, we will use sensitivity analyses to explore how robust our findings are with respect to a range of assumptions regarding missing data.
Discussion
Men in the United States are grossly underrepresented in traditional weight loss programs because they find them unappealing.2,55 A gamified mHealth program offers a radical alternative, given men’s high interest in video gaming15,16, and the ability of gamification features to increase enjoyment, motivation, and engagement. The present study uses a factorial design to examine the independent and combinatory efficacy of gamification and neurotraining on weight, physical activity, and dietary intake, as well as hypothesized mediators (food-specific inhibitory control, valuation engagement, and enjoyment) and moderators (baseline frequency of video gameplay and implicit preferences for ICT-targeted foods).
Several strengths of the study merit highlighting. For instance, the study is currently one of the few attempts to address the underrepresentation of men in BWL programs. Given the modest success of existing attempts to engage men,8,11,12,56,57 the current study takes an innovative and novel approach by using gamification and a professionally designed video game to implicitly train self-regulatory abilities (through an ICT video game), whereas conventional programs train these abilities explicitly, through psychoeducation. The study design is also rigorous in that the controls for gamification and neurotraining are robust (a professionally designed gold-standard behavioral weight loss mobile app, and a sham, respectively). The few previous studies of gamified weight loss21,23,35,58 have relied on rudimentary games created by university teams and/or created simple and narrow gamification targets that were limited to physical activity.18-20 Another strength is the use of an advisory panel of men with overweight/obesity throughout study design to inform development of the gamified weight loss app and ICT. Notable also is the investigation of mechanisms of action which, for instance, should help inform the debate as to whether the ICT, a Go/No Go style of neurotraining, achieves its effects by enhancing inhibitory control and/or by altering valuation of healthy and unhealthy foods.26
There are several challenges inherent in designing an acceptable mobile app for men. For instance, in order to be more acceptable to men, the study incorporates self-selected food category targets, a departure from typical balanced calorie reduction. Designing a gamified app broadly appealing to men also is challenging, given the variability in men’s preferences for themes and gamified features (e.g., preference for cooperation/competition) revealed by the advisory board. In the real world, men can select from any number of types of games and may elect not to use certain game features within these games (e.g., teams, leaderboards). Yet in the current study, all men must be assigned to the same game, and same set of game features. Additionally, there exists a tension between maximizing gamification elements that increase game enjoyment (e.g., an animation of a laser shooting an enemy ship) and maximizing participants’ focus on and depth of processing of the training stimuli/task, especially given that distracting gamification elements could detract from the efficacy of ICT.36
Conclusion
In sum, men are severely underrepresented in behavioral weight loss programs, and standard approaches to engaging men have been only modestly successful. This study will use a factorial design to evaluate whether gamification of a behavioral weight loss program and/or neurotraining enhance the appeal and efficacy of an mHealth weight loss program designed for men with overweight/obesity. If the proposed intervention strategies are found to be effective, future research should continue to investigate gamification and neurotraining approaches for obesity, especially over longer durations, given the challenge of weight maintenance. Future work would also benefit from examining the optimal dose and frequency of neurotraining and disentangling active from inert gamification elements.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health E-Stats. 2020; [Google Scholar]
- 2.Attempts to Lose Weight Among Adults in the United States, 2013-2016 (Center for Disease Control and Prevention; ) (2018). [Google Scholar]
- 3.Sabinsky MS, Toft U, Raben A, Holm L. Overweight men’s motivations and perceived barriers towards weight loss. European Journal of Clinical Nutrition. 2007;61:526–531. [DOI] [PubMed] [Google Scholar]
- 4.Archibald D, Douglas F, Hoddinott P, et al. A qualitative evidence synthesis on the management of male obesity. BMJ open. 2015;5(10):e008372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gudzune KA, Doshi RS, Mehta AK, et al. Efficacy of commercial weight-loss programs: an updated systematic review. Annals of internal medicine. 2015;162(7):501–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Contois Emily. “Lose like a man:” Gender & the constraints of self-making in Weight Watchers online. https://emilycontois.com/2017/03/31/lose-like-a-man/
- 7.Craig Jenny. Weight loss for men with Jenny Craig. 2018, November 1st;
- 8.Hunt K, Wyke S, Gray CM, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. The Lancet. 2014;383(9924):1211–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolfe BL, Smith JE. Different strokes for different folks: why overweight men do not seek weight loss treatment. Eating disorders. 2002;10(2):115–124. [DOI] [PubMed] [Google Scholar]
- 10.Crane MM, Lutes LD, Ward DS, Bowling JM, Tate DF. A randomized trial testing the efficacy of a novel approach to weight loss among men with overweight and obesity. Obesity. 2015;23(12):2398–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robertson C, Avenell A, Stewart F, et al. Clinical effectiveness of weight loss and weight maintenance interventions for men: A systematic review of men-only randomized controlled trials (the ROMEO project). American journal of men’s health. 2017;11(4):1096–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young M, Morgan P, Plotnikoff R, Callister R, Collins C. Effectiveness of male-only weight loss and weight loss maintenance interventions: a systematic review with meta-analysis. Obesity Reviews. 2012;13(5):393–408. [DOI] [PubMed] [Google Scholar]
- 13.ESA. Essential Facts about the Computer and Video Game Industry. Entertainment Software Association; 2019. [Google Scholar]
- 14.Terlecki M, Brown J, Harner-Steciw L, et al. Sex differences and similarities in video game experience, preferences, and self-efficacy: Implications for the gaming industry. Current Psychology. 2011;30(1):22–33. [Google Scholar]
- 15.Jent S, Janneck M. Using Gamification to Enhance User Motivation: The Influence of Gender and Age. Springer; 2017:3–10. [Google Scholar]
- 16.Williams D, Consalvo M, Caplan S, Yee N. Looking for gender: Gender roles and behaviors among online gamers. Journal of communication. 2009;59(4):700–725. [Google Scholar]
- 17.Sardi L, Idri A, Fernández-Alemán JL. A systematic review of gamification in e-Health. Journal of biomedical informatics. 2017;71:31–48. [DOI] [PubMed] [Google Scholar]
- 18.Matallaoui A, Koivisto J, Hamari J, Zarnekow R. How effective is “exergamification”? A systematic review on the effectiveness of gamification features in exergames. 2017:
- 19.Ahola R, Pyky R, Jämsä T, et al. Gamified physical activation of young men–a Multidisciplinary Population-Based Randomized Controlled Trial (MOPO study). BMC public health. 2013;13(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hightow-Weidman L, Muessig K, Knudtson K, et al. A gamified smartphone app to support engagement in care and medication adherence for HIV-positive young men who have sex with men (AllyQuest): development and pilot study. JMIR public health and surveillance. 2018;4(2):e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ameryoun A, Sanaeinasab H, Saffari M, Koenig HG. Impact of game-based health promotion programs on body mass index in overweight/obese children and adolescents: a systematic review and meta-analysis of randomized controlled trials. Childhood Obesity. 2018; [DOI] [PubMed] [Google Scholar]
- 22.Cox CE. Role of Physical Activity for Weight Loss and Weight Maintenance. Diabetes Spectr. 2017;30(3):157–160. doi: 10.2337/dsl7-0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee W, Chae YM, Kim S, Ho SH, Choi I. Evaluation of a mobile phone-based diet game for weight control. Journal of telemedicine and telecare. 2010;16(5):270–275. [DOI] [PubMed] [Google Scholar]
- 24.Strack F, Deutsch R. Reflective and impulsive determinants of social behavior. Personality and social psychology review. 2004;8(3):220–247. [DOI] [PubMed] [Google Scholar]
- 25.Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cognitive psychology. 2000;41(1):49–100. [DOI] [PubMed] [Google Scholar]
- 26.Veling H, Becker D, Liu H, Quandt J, Holland RW. How go/no-go training changes behavior: A value-based decision-making perspective. Current Opinion in Behavioral Sciences. 2022/October/01/2022;47:101206. doi: 10.1016/j.cobeha.2022.101206 [DOI] [Google Scholar]
- 27.Houben K Overcoming the urge to splurge: Influencing eating behavior by manipulating inhibitory control. Journal of behavior therapy and experimental psychiatry. 2011;42(3):384–388. [DOI] [PubMed] [Google Scholar]
- 28.Houben K, Jansen A. Chocolate equals stop. Chocolate-specific inhibition training reduces chocolate intake and go associations with chocolate. Appetite. 2015;87:318–323. [DOI] [PubMed] [Google Scholar]
- 29.Houben K, Havermans RC, Nederkoorn C, Jansen A. Beer à No-Go: Learning to stop responding to alcohol cues reduces alcohol intake via reduced affective associations rather than increased response inhibition. Addiction. 2012;107(7):1280–1287. [DOI] [PubMed] [Google Scholar]
- 30.Veling H, Aarts H, Papies EK. Using stop signals to inhibit chronic dieters’ responses toward palatable foods. Behaviour research and therapy. 2011;49(11):771–780. [DOI] [PubMed] [Google Scholar]
- 31.Stice E, Yokum S, Veling H, Kemps E, Lawrence NS. Pilot test of a novel food response and attention training treatment for obesity: Brain imaging data suggest actions shape valuation. Behaviour research and therapy. 2017;94:60–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lawrence NS, O’Sullivan J, Parslow D, et al. Training response inhibition to food is associated with weight loss and reduced energy intake. Appetite. 2015;95:17–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Preuss H, Pinnow M, Schnicker K, Legenbauer T. Improving inhibitory control abilities (ImpulsE)—A promising approach to treat impulsive eating? European Eating Disorders Review. 2017;25(6):533–543. [DOI] [PubMed] [Google Scholar]
- 34.Veling H, Lawrence NS, Chen Z, van Koningsbruggen GM, Holland RW. What is trained during food go/no-go training? A review focusing on mechanisms and a research agenda. Current addiction reports. 2017;4(1):35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Forman EM, Manasse SM, Dallal DH, et al. Computerized neurocognitive training for improving dietary health and facilitating weight loss. Journal of behavioral medicine. 2019:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Forman EM, Manasse SM, Dallal DH, et al. Gender differences in the effect of gamification on weight loss during a daily, neurocognitive training program. 2021; [DOI] [PMC free article] [PubMed]
- 37.Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. Jama. 2001;285(9):1172–1177. [DOI] [PubMed] [Google Scholar]
- 38.Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. Jama. 2003;289(14):1833–1836. [DOI] [PubMed] [Google Scholar]
- 39.American Gastroenterological Association medical position statement on Obesity. Gastroenterology. Sep 2002;123(3):879–81. doi: 10.1053/gast.2002.35513 [DOI] [PubMed] [Google Scholar]
- 40.Krukowski RA, Ross KM. Measuring weight with e-scales in clinical and research settings during the COVID-19 pandemic. Obesity. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen Z, Veling H, Dijksterhuis A, Holland RW. How does not responding to appetitive stimuli cause devaluation: Evaluative conditioning or response inhibition? Journal of Experimental Psychology: General. 2016;145(12):1687. [DOI] [PubMed] [Google Scholar]
- 42.Diaz KM, Krupka DJ, Chang MJ, et al. Fitbit®: An accurate and reliable device for wireless physical activity tracking. International journal of cardiology. 2015;185:138–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brooke SM, An H-S, Kang S-K, Noble JM, Berg KE, Lee J-M. Concurrent Validity of Wearable Activity Trackers Under Free-Living Conditions. The Journal of Strength & Conditioning Research. 2017;31(4):1097–1106. [DOI] [PubMed] [Google Scholar]
- 44.Egloff B, Schmukle SC. Predictive validity of an Implicit Association Test for assessing anxiety. Journal of personality and social psychology. 2002;83(6):1441–1455. [PubMed] [Google Scholar]
- 45.Banse R, Seise J, Zerbes N. Implicit attitudes towards homosexuality: Reliability, validity, and controllability of the IAT. Zeitschrift für experimentelle Psychologie. 2001;48(2):145–160. [DOI] [PubMed] [Google Scholar]
- 46.Inc. SI.. SAS/STAT ® 9.1 User’s Guide. 2004.
- 47.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior research methods, instruments, & computers. 2004;36(4):717–731. [DOI] [PubMed] [Google Scholar]
- 48.Hayes AF, Preacher KJ. Statistical mediation analysis with a multicategorical independent variable. British Journal of Mathematical and Statistical Psychology. 2014;67(3):451–470. [DOI] [PubMed] [Google Scholar]
- 49.Raudenbush SW, Liu X. Statistical power and optimal design for multisite randomized trials. Psychological methods. 2000;5(2):199. [DOI] [PubMed] [Google Scholar]
- 50.Raudenbush SW. Statistical analysis and optimal design for cluster randomized trials. Psychological Methods. 1997;2(2):173. [DOI] [PubMed] [Google Scholar]
- 51.Raudenbush SW, Liu X-F. Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychological methods. 2001;6(4):387. [PubMed] [Google Scholar]
- 52.Yuan YC. Multiple imputation for missing data: Concepts and new development (Version 9.0). SAS Institute Inc, Rockville, MD. 2010;49:1–11. [Google Scholar]
- 53.Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological methods. 1997;2(1):64. [Google Scholar]
- 54.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological methods. 2002;7(2):147. [PubMed] [Google Scholar]
- 55.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. Jama. 2014;311(8):806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Crane MM, LaRose JG, Espeland MA, Wing RR, Tate DF. Recruitment of young adults for weight gain prevention: randomized comparison of direct mail strategies. Trials. 2016;17(1):282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Crane MM, Sebur E, Levy R, Jeffery R, Sherwood NE. Using targeting to recruit men and women of color into a behavioral weight loss trial. Trials. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kurtzman GW, Day SC, Small DS, et al. Social incentives and gamification to promote weight loss: the LOSE IT randomized, controlled trial. Journal of general internal medicine. 2018;33(10):1669–1675. [DOI] [PMC free article] [PubMed] [Google Scholar]


