Abstract
A paradigm shift in public health and medicine has broadened the field from a singular focus on the ill effects of negative states and psychopathology to an expanded view that examines protective psychological assets that may promote improved physical health and longevity. We summarize recent evidence of the link between psychological well-being (including positive affect, optimism, life meaning and purpose, and life satisfaction) and physical health, with particular attention to outcomes of mortality and chronic disease incidence and progression. Within this evolving discipline there remain controversies and lessons to be learned. We discuss measurement-related challenges, concerns about the quality of the evidence, and other shortcomings in the field, along with a brief discussion of hypothesized biobehavioral mechanisms involved. Finally, we suggest next steps to move the field forward.
Keywords: psychological well-being, positive emotion, optimism, physical health, physical illness, health behaviors
Introduction
As early as the 3rd century BC, work by the classic Greek philosophers like Aristotle and Socrates offered thoughtful discourse regarding the link of mental states and physiological processes (Menninger & Menninger, 1936). Since then, the detrimental health effects associated with psychological ill-being (e.g., depression, anxiety) have been well documented (Boehm, Trudel-Fitzgerald, Kivimaki, & Kubzansky, 2015; Cuijpers & Smit, 2002; Suls, 2017). But, a recent paradigm shift in the field of public health and medicine expands focus by identifying and examining protective psychological assets that may preserve or promote greater physical health and longevity. Some have termed this shift a “quiet revolution” broadening from the deleterious effects of negative psychological constructs to a more positive orientation that considers the potential unique beneficial effects of positive psychological constructs (Boehm & Kubzansky, 2012; Labarthe, 2012; Labarthe et al., 2016).
However, as with any emergent field and evolving discipline, there remain inconsistencies, controversies, challenges, and lessons to be learned. The current review summarizes recent prospective evidence of the link between psychological well-being (e.g., positive affect, optimism, life satisfaction, and purpose in life) and physical health, paying particular attention to the question of whether the literature is robust enough to explore differential health effects across individual domains or subtypes of psychological well-being (see Suls (2017), this issue, for examination of differential health effects for aspects of negative affective constructs). In this selective review we focus on evidence published in the last decade (2006 to present), studies presenting objective measure of health, and those that shed light on potential differential effects of different aspects of psychological well-being. In our concluding remarks, we briefly explore evidence for potential biological and behavioral pathways through which positive psychological functioning may influence physical health and end with discussion of measurement challenges, gaps in the field, and suggestions for next important steps.
Definition of Psychological Well-being
The construct of psychological well-being is multifaceted and research in the area of physical health has included a broad array of positively toned subjective states and cognitions. For the purposes of this review, the term psychological well-being will be used throughout and is defined as the subjective experience of positively valenced feelings or cognitive appraisals including lower activation affects such as calm or satisfied, as well as higher activation affects such as excited or thrilled. We include multiple operationalizations of psychological well-being including life purpose, emotional vitality, positive affect, life satisfaction, happiness, and optimism (Boehm & Kubzansky, 2012; Ryff, Singer, & Love, 2004). These indicators of well-being presume heighted experience of positively valenced emotion. More existential indices of well-being (e.g., life meaning), however, can relate to emotions that are neutral or negative in nature but which ultimately promote future emergence of positive feelings and cognitions.
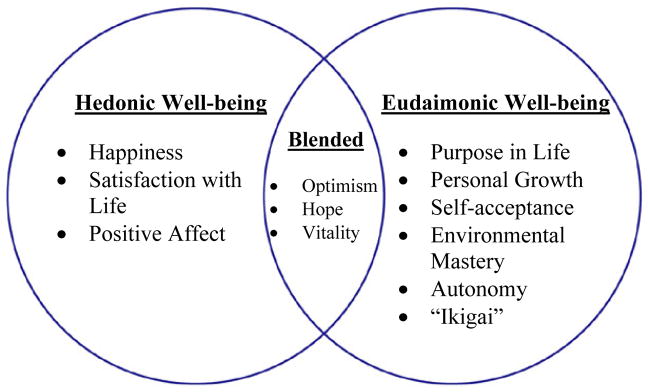
The multi-dimensional construct of well-being can be organized into two domains: hedonic and eudaimonic (Deci & Ryan, 2008; Ryff et al., 2004; Winefield, Gill, Taylor, & Pilkington, 2012). Hedonic well-being includes such attributes as pleasure, happiness, positive affect, and life satisfaction, whereas eudaimonic well-being includes life meaning and purpose, self-actualization, and autonomy (Deci & Ryan, 2008). Although skeptics question the extent of meaningful partitioning across well-being domains (Kashdan, Biswas-Diener, & King, 2008), there is evidence that while hedonic and eudaimonic aspects of well-being are correlated, they diverge and map onto empirically distinct planes, with different predictors and consequences (Keyes, Shmotkin, & Ryff, 2002). Using factor analysis on Cantril’s Self-Anchoring Scale and Ryff’s Scales of Psychological Well-being, Keyes et al. (2002) identified two correlated latent factors reflecting eudaimonic and hedonic aspects. Specifically, the first factor included features of autonomy, purpose in life, personal growth, positive relations, environmental mastery, and self-acceptance, while the second was comprised of positive affect, life satisfaction, and absence of negative affect. As conceptualized by Keyes (2002), eudaimonic indices centering on highly existential domains (e.g., purpose in life) were least correlated to hedonic measures of affect, pleasure, and happiness; correlation coefficients (r’s) across well-being domains ranged from as low as 0.13 to moderate values of 0.62. More recently, additional subtyping has emerged (Boehm & Kubzansky, 2012) for constructs not easily categorized as purely hedonic or eudaimonic but which constitute elements of both, i.e., optimism, hope, and vitality. Figure 1 summarizes the cataloguing of psychological well-being and its associated domains as explored in our current review; we exclude indicators assessing absence of negative affect as this does not guarantee presence of psychological assets.
Figure 1.
Conception and Categorization of Psychological Well-being
Theoretical and empirical evidence provides further justification of the distinction between hedonic and eudemonic indices. Hedonic well-being is said to emerge from procurement of basic biologic requisites and securing of resources to ensure attainment of homeostasis, comfort, and survival (Baumeister, Vohs, Aaker, & Garbinsky, 2013). The origins of eudaimonic well-being are thought to be more complex and are largely dictated by cultural context (Baumeister et al., 2013). Using survey and experimental methodology, Baumeister and colleagues (2013) found that hedonic well-being is linked to acquisition of core desires (both needs and wants) and focuses largely on present moment circumstances. Conversely, eudaimonic well-being involves cognitive appraisals across a larger timeframe, incorporating past, present, and future experiences with emphasis on actualization of the self and exercising of generosity toward others (Vallacher & Wegner, 1987). Differential consequences by well-being subtype are also documented. In experimental trials, more long-term and enduring improvements in mental health are documented for interventions seeking to boost eudaimonic well-being versus those emphasizing pursuit of hedonia (Huta & Ryan, 2010). There is also evidence to suggest that when compared to hedonic indices, eudaimonia is associated with more favorable psychological functioning and overall well-being (Steger, Kashdan, & Oishi, 2008).
Given variant corollaries of hedonic and eudaimonic well-being, the current review queries whether individual indices are differentially linked to physical health. We consider the evidence regarding whether the hedonic/eudaimonic distinction or others (e.g., high activation vs. low activation; cognitive vs. affective constructs) adds significantly to our understanding of the links between psychological well-being and health. Attention to differential conceptions of psychological well-being adds to our understanding of the links with physical health, may further hint to underlying mechanisms, and suggests avenues for interventions that target specific aspects of well-being.
Throughout the manuscript we use the term psychological ill-being when referring to negative psychological states or traits (e.g., depression, anxiety, negative affect). As researchers seek to establish unique and independent contributions of psychological well-being on physical health, indicators of psychological ill-being are frequently controlled in the analyses and included as a covariate to counter the contention that effects of psychological well-being are simply the absence of distress or psychological ill-being. It is imperative to establish that health benefits are not merely conferred by absence of psychological distress and that well-being is not simply the flipside of negative affect or ill-being. This notion has not been without contention. Near the end of the 20th century, Russell and Carroll (1999) stipulated that mixed emotions could not simultaneously be experienced, thus refuting the individual ability to feel both positive and negative emotion at a single point in time. In their bipolar model, positive and negative emotions rest on opposite poles of a vector, making them mutually exclusive sensations. As stated by Russell and Carroll (1999), “Bipolarity says that when you are happy, you are not sad and that when you are sad, you are not happy.” Since then, evidence refuting this claim has emerged. Larsen and colleagues (2014), provide evidence that co-occurence of opposite-valenced emotions is not only conceivable but indeed commonplace. In this evaluative space model (Cacioppo & Berntson, 1994), positive and negative emotions are independent psychological states (Larsen & McGraw, 2014; Larsen, McGraw, & Cacioppo, 2001). Applied studies of people experiencing major life stressors such as caregiving demonstrate that it is common for positive and negative affect to co-occur; to experience positive affect despite high levels of stress and distress (Folkman, 1997). More recently, from a neuroscience perspective, positive and negative emotions are said to process from different brain regions allowing for their simultaneous activation, i.e., the mesolimbic dopaminergic pathway vs. the amygdala, respectively (Hoebel, Rada, Mark, & Pothos, 1999; Larsen et al., 2001).
We first discuss the relationship of psychological well-being and incidence of chronic illness in initially healthy samples and its progression in those with existing illness. We then summarize recent findings of the association of well-being and mortality highlighting advances in understanding of this link. In order to guide our reader, we include Figure 1 listing the well-being indicators discussed in our current review, along with information on their classification by well-being subtype (e.g., hedonic vs. eudaimonic). Table 1 summarizes the literature included in the current selective review. A more in-depth summary of each study included in our review is found in Table 2 of supplementary materials. As part of our final remarks we discuss the hypothesized biobehavioral pathways through which psychological well-being confers good health and suggest areas of research focus needed to move the field forward.
Table 1.
Summary of protective influence and/or null association of psychological well-being and physical health
| Hedonic | Eudaimonic | Optimism and other measures of well-being | Blended Construct | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Satisfaction with Life | Positive affect | Purpose in Life | Life Meaning | Life Engagement | “Ikigai” | Optimism | Vitality | ||
| 1. Incidence of Chronic Illness | |||||||||
| CVD-related Event | |||||||||
| Heart Disease | ο | + ο ο ο | + | ++ | + | ο | |||
| Stroke | + | + | + | ο | |||||
| Venous Thromboembolism | + | ||||||||
| CVD Risk Factor | |||||||||
| Hypertension | ο | + | |||||||
| Diabetes | ++ | ο | + | + | |||||
| Cancer | + | + | ο | ||||||
| Lung Disease | + | ||||||||
| Arthritis | + | ||||||||
| 2. Chronic Disease Progression | |||||||||
| Cardiac Patients | |||||||||
| Subsequent Event(s)/Symptoms | ++ | ||||||||
| Re-hospitalization | + | + | + | ||||||
| HIV | |||||||||
| Slower progression/decreased viral load | + | + | |||||||
| 3. Mortality | |||||||||
| Cardiac-related | + | ||||||||
| All-cause | + | ++++ο | ++ | + | + | ++ | |||
+ = significant protective effect; ο = null findings.
Psychological Well-being and Disease Onset in Initially Healthy Samples
In early work in this area (Cohen, Doyle, Turner, Alper, & Skoner, 2003) laboratory trials where healthy volunteers were injected with the rhinovirus fueled curiosity in the scientific community regarding the influence of psychological well-being on emergence of illness. The studies exposed healthy volunteers to a cold virus, then assessed who became infected and developed cold symptoms. Positive affect was measured with nine items tapping vigor (lively, full-of-pep, energetic), well-being (happy, pleased, cheerful), and calmness (at ease, calm, relaxed). After controlling for sex, race, education, body mass index (BMI), month of exposure, virus type, immune factors, and negative affect (depression, anxiety and hostility), positive affect was related to lower likelihood of developing a cold up to five days after exposure. In follow-up analyses looking at the individual positive affect scales, only vigor and well-being, but not calm, were protective against development of a cold. Cohen’s discovery begs the question of whether activated domains of positive emotion (e.g., enthusiasm) are more salient to disease incidence than those tapping low arousal emotions of calmness and relaxation and highlights the importance of examining the possibility of differential health effects for different aspects of well-being.
Expanding on Cohen’s investigation of protective health effects of psychological well-being with respect to onset of acute illness, in the next section, we explore the relationship of psychological well-being and incidence of chronic illness, with particular attention to cardiovascular disease (CVD) events (coronary heart disease and stroke), development of CVD risk factors (hypertension, hypercholesterolemia, and diabetes), and cancer. We organize findings by stratifying across well-being domains where possible, i.e., hedonic vs. eudaimonic vs. conception blending both elements (see Figure 1). We make special note of covariates included when modeling the relationship of well-being and physical health, as this is vital given controversy that one is merely capturing the absence of psychological distress and that important confounders are being overlooked.
A large prospective study using data of the European Prospective Investigation into Cancer and Nutrition (EPIC)-Germany Study investigated the association of hedonic well-being and an array of disease outcomes within a single cohort. After 8 years of follow-up, life satisfaction was associated with reduced risk for chronic illness incidence in their cohort of ~28,704 women (Feller, Teucher, Kaaks, Boeing, & Vigl, 2013). Women reporting low levels of life satisfaction had a 45% increased risk of cancer, 69% for stroke incidence, and 27% for diabetes mellitus; covariates considered included lifestyle factors, demographic characteristics, and traditional CVD risk factors. In one of the few studies to use a non-self-report measure of positive affect to document possible cardioprotective effects, research staff coded the frequency of displayed positive emotion as expressed verbally, behaviorally (e.g., smiling), and via vocal cues (e.g., cheerfulness). In this sample of 1,739 Nova Scotians, each unit increase in staff-coded positive affect was associated with 22% reduced odds of a cardiac event within 10 years, controlling for socio-demographic factors, major cardiovascular disease risk factors (e.g., smoking status), and psychological distress (Davidson, Mostofsky, & Whang, 2010). In the above studies, health effects of psychological well-being remained significant after controlling for factors hypothesized to comprise the mechanistic pathway, e.g., such as behavioral and traditional biologic risk factors. Not all studies link hedonic well-being to better heart health, however. In the Rotterdam cohort study (N = 6,349), for example, self-reported positive affect (i.e., positive affect items from the Center for Epidemiologic Studies Depression Scale (CES-D) and Hospital Anxiety and Depression Scale (HADS)) was not predictive of incident cardiovascular disease (stoke, heart failure, CHD) over an 11.9-year follow-up period (Freak-Poli et al., 2015). One possible explanation for the divergent findings of the link between positive affect and health is the use of non-ideal measures of psychological well-being. This can occur when validated measures of psychological ill-being (e.g., intended to assess depression, anxiety, or stress) are used to derive positively valenced constructs by pooling positively worded items, instead of reverse coding them to comprise ill-being (Freak-Poli et al., 2015). However, null findings are also reported using data of the Whitehall II cohort study (Nabi, Kivimaki, De Vogli, Marmot, & Singh-Manoux, 2008) which employed a scale specifically designed to capture positive affect (i.e., Bradburn Affect Balance Scale). This begs the question of whether measurement error is a potential culprit for discrepant findings or whether divergent scales tap into different dimension of related emotions.
Although scarce and with limited available evidence, there is some support for associations of eudaimonic well-being and chronic disease incidence. In a meta-analysis investigating the influence of life purpose on CVD events, a protective effect was evident with significantly lower risk for myocardial infarction, sudden cardiac death, and stroke (RR = 0.83, 95% CI = 0.75–0.92) when pooling across 10 studies (Cohen, Bavishi, & Rozanski, 2016). Pertinent covariates and potential confounders were frequently included across the individually pooled studies including demographic characteristics, health behavior adherence, self-rated health, and extant medical comorbidities. Wakai and colleagues (Wakai et al., 2007) studied the well-being indictor of “ikigai” (defined as, “presence of something that makes one’s life worth living”) and its prospective role in the incidence of breast cancer in 34,497 Japanese women. In the U.S., ikigai is often categorized as a eudaimonic index. Women with greater levels of ikigai had lower odds of developing breast cancer (RR = 0.66, 95% CI = 0.47–0.94) over a 7.5-year period, independent of sociodemographic characteristics, lifestyle factors, and individual/familial medical history.
A considerable number of studies focus on the health effects of well-being constructs that blend hedonic and eudaimonic elements. In a recent piece by Okely and Gale (2016), they used data of the English Longitudinal Study of Ageing (ELSA) to examine the prospective relationship of psychological well-being and incidence of stroke, myocardial infarction, diabetes, arthritis, chronic lung disease, and cancer. Their sample included 8,182 older adults over the age of 50. Operationalization of well-being consisted of a blended derived score that included hedonic (pleasure) and eudaimonic (control, autonomy, self-realization) domains. After controlling for socio-demographic characteristics, depressive symptoms, BMI, and health behavior adherence, each SD increase in psychological well-being was associated with reduced incidence of arthritis (HR = 0.89, 95% CI = 0.83–0.96), diabetes (HR = 0.82, 95% CI = 0.71–0.95), and lung disease (HR = 0.80, 95% CI = 0.66–0.97). Effect modification was evident across age categories (<65 vs. ≥65), explicitly for diabetes and lung disease, where associations remained significant only for those <65 years of age. In this ELSA cohort, psychological well-being was unrelated to risk for stroke, myocardial infarction, and cancer when controlling for traditional risk factors.
The Whitehall II cohort study of British civil servants captured two measures of psychological well-being classified as containing both hedonic and eudaimonic elements--optimism (expectation that positive things will occur in the future) and emotional vitality (“a sense of positive energy, the ability to effectively regulate emotions and behaviors, and positive well-being”)--between 1991 and 1994 and tracked incidence of coronary heart disease (CHD) after 5 years of follow-up. In this sample of 7,792, there was an 11% reduction in CHD risk with each SD increase in emotional vitality and a 13% decrease in CHD associated with higher levels of baseline optimism (Boehm, Peterson, Kivimaki, & Kubzansky, 2011). Effects of each well-being construct (optimism vs. emotional vitality) were independently assessed, however; analyses did not include both within a single model. Associations were slightly attenuated but remained statistically significant when controlling for health behavior adherence and psychological ill-being (i.e., Short-Form General Health Survey). Similar results were seen in older adults (≥50 years) of the Health and Retirement Study (Kim, Smith, & Kubzansky, 2014). Each standard deviation increase in optimism as measured at baseline resulted in a 26% reduction in the risk for heart failure after four years of follow-up. Cardio-protective effects of optimism remained after adjustment for a wide range of competing risk factors such as health behavior adherence and medical comorbidities (e.g., hypertension, diabetes). In fact, investigators noted a dose-response relationship whereby a monotonic decrease in heart failure risk was observed with each stepwise increase in optimism (Kim et al., 2014).
More recently, protective effects of emotional vitality against stroke risk were documented using data of the National Health and Nutrition Examination Survey Epidemiologic Follow-Up Study--a representative sample of US adults (Lambiase, Kubzansky, & Thurston, 2015). In models controlling for traditional CVD risk factors and depressive symptoms, each SD increase in emotional vitality resulted in 11% reduction in stroke risk (mean follow-up of 16.3 years). Finally, in 25,964 adults from Norway, a blended construct of well-being capturing levels of happiness and optimism was associated with a 40% risk reduction for incident venous thromboembolism (Enga, Braekkan, Hansen-Krone, & Hansen, 2012) controlling for socio-demographic factors, behavioral and biologic risk factors, and medical comorbidities.
Psychological well-being is not only implicated in the incidence of CVD events but also to the upstream development of CVD risk factors. In a prospective study that used data of the Whitehall II cohort of British civil servants, more favorable baseline levels of emotional vitality (but not optimism) were associated with lower odds for developing hypertension after 3 years of follow-up (Trudel-Fitzgerald, Boehm, Kivimaki, & Kubzansky, 2014). Effects of emotional vitality remained significant after adjustment for socio-demographic factors, current health status, health behavior adherence, and ill-being. Psychological well-being is also associated with lower risk for development of diabetes (Boehm, Trudel-Fitzgerald, Kivimaki, & Kubzansky, 2015). Researchers observed lower odds for diabetes onset among individuals with greater life satisfaction and emotional vitality, but not in those with greater levels of optimism; note, well-being indicators were not pitted against each other in regression models negating ability to infer individual effects for each attribute controlling for rival indicators (see Suls (2017), this issue). The measure of emotional vitality was constructed borrowing items from various sources including the Short Form-36--e.g., “how often have you felt full of life, had a lot of energy, and had been a happy person.” Future evidence will afford a definitive answer, but we surmise that items tapping emotional vitality may prove to be non-ideal indicators of psychological well-being as probed symptoms are often a consequence of compromised physical health.
Evidence presented thus far raises two important questions: First, is the association between well-being and illness onset dependent on disease type suggesting a shared etiological mechanism that must be implicated in order for well-being to exert its unique influence? Second, and as we contend is still largely unclear based on the current literature, do well-being subtypes differentially influence disease onset? In studies reported thus far, a majority of available evidence points to a salubrious effect of well-being for cardiometabolic health, e.g., diabetes, hypertension, stroke, and CHD, and cancer incidence. Lung disease and arthritis have been less studied. Well-being constructs that repeatedly offset disease onset were positive affect (particularly high activation subtypes), emotional vitality and life satisfaction, with less consistent results seen for optimism and constructs that blend across domains. Despite lack of agreement when conceptualizing and operationally defining psychological well-being, these observational findings have reached critical mass and have stimulated development and implementation of trials to examine whether augmentation of psychological well-being leads to physiologic benefits and increased health (Huffman et al., 2011; Huffman et al., 2015).
Psychological Well-being and Disease Progression
There is evidence that psychological well-being is related to improved prognosis and slower disease progression in people with a chronic condition. In a meta-analysis of 11 total studies, DuBois et al. (2015) found multiple positive psychological constructs (e.g., positive affect, optimism) to confer a protective effect on rates of rehospitalization and mortality among cardiac patients. Each 1-SD increase in psychological well-being was associated with an 11% reduced risk for either re-hospitalization or mortality. Negating simultaneous inclusion across regression models, this meta-analysis examined individual effects of each well-being indicator without pitting constructs against each other. Similarly, Ronaldson et al. (2014) found greater levels of optimism, as measured pre-operatively, to be inversely associated with self-reported pain intensity and adverse physical symptoms (e.g., bruising, numbness, swelling) in patients who underwent coronary artery bypass graft (CABG) surgery. In this prospective study, optimism (i.e., Life Orientation Test-Revised (LOT-R)) was measured four weeks prior to surgery while pain and cardiac-related outcomes were measured 6–8 weeks post-surgery (Ronaldson et al., 2014). Potential confounds considered in this study were factors such as comorbid chronic illness and psychological distress. In patients with stable CHD who were part of the Heart and Soul Study, with a mean follow-up of 7 years, Hoen et al. (2013) examined the prospective association of positive affect and risk for a recurrent CVD event and all-cause mortality adjusting for depression (but not negative affect), disease severity, health behaviors, and biomarkers. The hedonic indicator of positive affect (PANAS) was not significantly associated with incidence of a CVD event. However, each SD increase in positive affect reduced risk of all-cause mortality by 16%. Conversely, in a sample of CHD patients ending cardiac rehabilitation, those with greater comparative optimism at termination of therapy were less likely to experience an adverse outcome within 12 months (Hevey, McGee, & Horgan, 2014). Investigators measured comparative optimism by asking patients to rate their expectancy for positive health outcomes compared to a targeted reference group of individuals with a prior cardiac event.
In people living with HIV, positive affect and related positive constructs are uniquely associated with slower disease progression (Ironson et al., 2005; Ironson & Hayward, 2008). For example, Ickovics et al. (2006) found in a sample of 773 women living with HIV, that positive resources, a scale that combined the hedonic index of positive affect items (e.g., joyful, hopeful, happy), positive expectancies regarding HIV (“if I take care of myself, I will not get sick with HIV”), and eudaimonic meaning-making was associated with significantly slower disease progression and lower risk of mortality controlling for viral load, demographics, and depression. The authors did not report whether the individual types of well-being were differentially predictive of disease progression or mortality on their own. More recently, in a sample that included 995 women of the Women’s Interagency HIV Study, positive affect was significantly associated with viral suppression, such that, in prospective analyses women with high positive affect (when compared to those with low positive affect scores) were twice as likely to have undetectable viral load classifications (OR = 1.92, 95% CI 1.34–2.74), particularly when accompanied by low negative affect profiles (Wilson et al., 2016). The interaction between higher positive affect and lower negative affect predicting suppressed viral load highlights the importance of not only including psychological ill-being in the model as a confounder, but also examining it as an indicator of the broader emotion context within which psychological well-being has the greatest impact.
In summary, psychological well-being appears to be related to lower risk of illness onset and slower disease progression across a number of different samples and types of well-being measures, even when other predictors of health are included in the model (e.g., health behaviors). As before, Table 1 summarizes findings and indicates instances where well-being exerts a health protective effect and when null findings are evident. However, given heterogeneity in conception of psychological well-being and heterogeneity in disease states explored, it is premature to infer differential health effects across well-being subdomains or subtypes. For instance, optimism emerges as a consistent predictor of cardiovascular health, but displays less consistent results for other disease types, e.g., HIV and cancer. Additionally, influences of hedonic domains of well-being are often attenuated when controlling for ill-being in patient populations with pre-existing disease, while investigation of protective effects imparted by eudaimonic subtypes are grossly understudied. Notwithstanding multiple conceptions of well-being and associated attributes, relatively few psychological constructs have received substantial focus when examining influences on morbidity and mortality. Promising well-being targets for therapeutic inventions include boosting of life satisfaction and positive affect, with further work needed for constructs that blend across well-being domains.
Positive Psychological Well-being and Longevity
In the past few decades, a number of studies have examined the link between psychological well-being and longevity with the bulk of published research indicating that constructs such as optimism, positive affect, life satisfaction, and happiness are associated with longer life, independent of the effect of negative constructs (Chida & Steptoe, 2008; Diener & Chan, 2011; Howell, Kern, & Lyubomirsky, 2007; Pressman & Cohen, 2005). As with the literature reviewed above, recent work highlights important nuances to consider in the association between well-being and mortality such as the measurement and operationalization of well-being, the demographic makeup of the samples, and whether control variables entered into the models are better conceptualized as potential mechanisms of the effect of well-being on mortality.
For a number of years, it was innovative to simply look at psychological well-being as a unique predictor of mortality, independent of the effects of ill-being. Recent studies have taken the next step and now include multiple measures of well-being to determine which carry the most predictive weight (see Suls (2017), this issue, for an examination of different aspects of ill-being and cardiovascular disease). For example, in a representative sample of people living in Germany, Wiest and colleagues (2011) demonstrated that both life satisfaction (Pavot & Diener, 1993) and positive affect (the PANAS, (Watson, Clark, & Tellegen, 1988)) independently predict lowered risk of mortality, whereas negative affect was not predictive of mortality in any of the models. This finding indicates that life satisfaction and positive affect may influence longevity through different pathways. There is also support for associations of eudaimonic well-being and longevity. Cohen et al (2016) report a meta-analysis of eudaimonic constructs including purpose in life, life meaning, and life engagement that demonstrates a significant protective effect with respect to mortality. For most of the studies included in the meta-analysis, the effects remain significant even when adjusted for covariates such as age, gender, and negative affect or ill-being (Boyle, Barnes, Buchman, & Bennett, 2009; Gruenewald, Karlamangla, Greendale, Singer, & Seeman, 2007; Hill & Turiano, 2014; Sone et al., 2008). Hill et al. (2014) examined the association of purpose in life with mortality in a sample of 6,163 participants of the MIDUS study, controlling for hedonic well-being (positive affect), negative affect, and positive relations with others. Purpose in life was measured with 3 items from the Ryff Scales of Psychological Well Being (“Some people wander aimlessly through life but I am not one of them;” “I live life one day at a time and don’t really think about the future;” and “I sometimes feel as if I’ve done all there is to do in life.”) and positive and negative affect were measured with 6 affect terms each (“cheerful,” “in good spirits,” “extremely happy,” “calm and peaceful, “satisfied, and “full of life” for positive and “so sad nothing could cheer you up,” “nervous,” “restless or fidgety,” “hopeless,” “that everything was an effort,” and “worthless” for negative affect). When hedonic and eudaimonic constructs were both included as predictors of longevity, eudaimonic constructs remain significant whereas hedonic drop to non-significance (Hill & Turiano, 2014). This finding suggests a need to include both hedonic and eudaimonic constructs in order to best capture the effects of well-being and longevity.
Using a different measurement approach to well-being assessment, Mroczek et al. (2015) examined whether positive emotional reactivity to stress was associated with mortality. The researchers asked 181 men aged 58 to 88 to complete diaries regarding the daily occurrence of stressful events and their end-of-day emotions for 8 days. Positive and negative affect were measured using the PANAS and participants also reported their daily physical symptoms and pain. Investigators examined whether emotional reactivity to stressful events was associated with mortality over the course of 10 years of follow up. Controlling for age, pain, physical symptoms, extraversion, neuroticism, and daily stress frequency, the daily stressor-related decreases in positive affect were associated with a significantly higher risk of mortality over the follow up period. Negative affect reactivity was not predictive of mortality. Thus, those participants who were able to maintain their positive affect in response to a stressful event, lived longer. This study suggests that in addition to paying attention to the particular items used to measure well-being, it is important to consider retrospective time frame (e.g., past day, past week) as well as affective reactivity in response to stress.
Careful consideration of control variables is imperative in examining and interpreting the effects of psychological well-being on mortality. Specifically, researchers need to pay attention to whether a particular variable is better considered a mechanism or mediator of the effect rather than a confounder to be statistically controlled. For example, Nilsson et al. (2011) found that positive (hedonic) well-being (as measured by a subscale of the Psychological General Well-Being questionnaire (Dupuy, 1984) that included items assessing cheerfulness, happiness, and interest) was associated with lower risk of mortality for men, but not women in a sample of 75 year-olds in Sweden. The effect for men fell to marginal significance when the model was adjusted for health behaviors like smoking, health conditions like obesity, and living alone. In the study by Wiest and colleagues (2011), cited above, the significant effect of life satisfaction and positive affect on longevity fell to non-significance when self-rated health and physical activity were included in the model. The findings of Nilsson et al. (2011) and Wiest et al. (2011) suggest that well-being may exert health effects through improved health behaviors and aspects of social support. Similarly, in a study of over 700,000 women, Liu and colleagues (Liu et al., 2016) found that happiness (“How often do you feel happy? Most of the time, usually, sometimes, or rarely/never) was associated with lower risk of all-cause mortality in a model that controlled for age. However, when the model included sociodemographic, health behavior, and health variables, the effect became nonsignificant. A critique of the Liu et al. study (2016) noted that rather than being an indictment of the literature on happiness and health (Diener, Pressman, & Lyubomirsky, 2015), the study demonstrated “Whether a one-item happiness question will predict a shortened life in healthy middle-aged women, if you delete how happiness has affected their health for their first six decades and if you erase the influence of key pathways to health such as social support, smoking and body mass index.” In other words, the statistical controls eliminated many of the likely pathways through which positive affect influenced mortality and thus it wasn’t particularly surprising that positive affect didn’t predict over and above these likely mechanistic pathways.
Thus, consistent with several decades of research, recent studies of a number of different psychological well-being constructs including positive affect, life satisfaction, happiness, purpose in life, and optimism indicate that psychological well-being predicts longevity in univariate analyses. In many cases, the effect remains significant when measures of ill-being and physical health are controlled and, although limited, there is some evidence that eudaimonic well-being may be a stronger predictor of longevity when included in the same model as hedonic well-being. However, findings are not entirely consistent and a number of questions remain, particularly regarding best measurement approaches, additional contextual variables to include in the analyses, and whether analyses that control for potential pathways such as health behaviors linking psychological well-being and mortality, should be interpreted as evidence that there is no predictive value in psychological well-being or whether one is simply over adjusting by controlling for a potential mechanism or mediator of the effect of psychological well-being and longevity.
Discussion
In this document we reviewed a body of recent literature demonstrating that psychological well-being is associated with greater health and prolonged life. However, a number of questions remain and we suggest several recommendations to help move the field forward. In our view, key issues in need of attention are conception and measurement of psychological well-being, thoughtful inclusion of plausible mediators and moderators, and implementation of randomized trials testing interventions to increase psychological well-being, to enable stronger causal conclusions regarding the well-being—health link.
Need for Cogent Taxonomy of Well-being
The present review highlights a number of limitations in the literature concerning well-being and physical health. First, there is lack of consistency when defining and sorting across well-being domains. Conception of well-being remains both controversial and unresolved. For instance, optimism is sometimes cataloged as a eudaimonic domain and at others times identified as a blended construct encompassing both hedonic and eudaimonic elements. Second, when operationally defining well-being, some researchers include relatively pure measures that discriminate or separate across domains (i.e., strictly, hedonic or eudaimonic; e.g., (Wilson et al., 2016)) while others create composite scores that blend multiple domains into a single well-being component. The latter may be a consequence of skepticism on meaningful separation across well-being domains given the extent to which they overlap or tap similar psychological processes or may represent a bias whereby researchers include highly recognized or trendy domains. Additionally, it is exceedingly rare for individual well-being types to be considered simultaneously within a single sample, negating the ability to determine whether differential effects are evident for individual attributes of well-being (see Suls (2017), this issue). Third, eudaimonic aspects of well-being are greatly neglected when examining the health protective effects of psychological well-being as very little empirical work includes eudaimonic constructs such as personal growth, self-acceptance, environmental mastery, and autonomy.
As the majority of research on psychological well-being and health emerges from fields of medicine and epidemiology, the measurement focus has mainly been on the physical health outcome rather than the well-being predictors. This has constrained the availability of robust measures of psychological well-being given the overreliance on available constructs in secondary data. As space on questionnaires is often at a premium, large epidemiology studies are restricted by the lack of availability of psychosocial variables--particularly inclusion of instruments assessing psychological well-being--as many were not originally designed to focus on health effects of psychosocial factors. As a consequence, survey data from large cohort studies often include a narrow collection of well-being domains and often only assesses these on one occasion and not across multiple waves. Investigators are then limited to a handful of well-being measures--some with dubious psychometric properties--without the ability to examine individual effects while controlling for other important or competing well-being domains. Thus, we know little about whether discrete domains of well-being differentially relate to health. A variety of well-being constructs emerge as protective factors against disease onset. To date, optimism has received substantial focus and emerges as a salient factor for physical health. However, in our review, additional well-being constructs show a robust health-protective effect including positive affect and life satisfaction. Less work has been done examining eudaimonic components and future studies will want to consider domains such as personal growth and life purpose and meaning. We recommend that researchers more rigorously and systematically evaluate psychological well-being--across distinct domains (e.g., hedonic and eudaimonic) -- in an effort to elucidate their saliency for physiologic functioning and longevity.
Mediators, Moderators, and Confounders
A multi-pronged process is hypothesized to underlie the pathway through which psychological well-being protects against incidence and progression of subclinical and clinical disease, i.e., through promotion of healthy behaviors, augmentation of restorative biological processes, and increased psychosocial and coping resources (Ryff et al., 2004; Nancy L Sin, Moskowitz, & Whooley, 2015). In both healthy populations and those with existing chronic illness, evidence links favorable psychological well-being with enhanced exercise regularity, smoking abstinence (Carvajal, Wiatrek, Evans, Knee, & Nash, 2000), a healthier diet (Kelloniemi, Ek, & Laitinen, 2005; Shepperd, Maroto, & Pbert, 1996), and increased medication regimen adherence. As an example, in an observational study that included two well-being subtypes within a single regression model (e.g., optimism and positive affect), optimism was related to greater treatment adherence in cardiac patients (van Montfort, Denollet, Widdershoven, & Kupper, 2016). Here again we see differential effects across specific well-being indicators. At the physiologic level, biologic dysregulation as measured via cortisol output, heart rate variability, blood pressure, and markers of inflammation (Interleukin 6 and C-reactive protein) is less prevalent among individuals reporting positive psychological well-being (Bacon et al., 2004; Gale, Batty, & Deary, 2008; Rahe, Rubin, Gunderson, & Arthur, 1971; Richman et al., 2005; Roy et al., 2010; Tsenkova, Love, Singer, & Ryff, 2007). Additionally, and although generating some controversy, eudaimonic well-being was associated with decreased expression of genes involved in inflammation and increased expression in genes associated with antiviral response (Brown, MacDonald, Samanta, Friedman, & Coyne, 2014; Cole & Fredrickson, 2014; Fredrickson et al., 2013). The influence of psychological well-being in gene activation and expression and subsequent association with health-related biomarker is an area ripe for future study. Finally, persons with favorable psychological well-being are said to possess more adaptive psychological profiles characterized by healthful coping strategies (e.g., positive reappraisal), increased social connectedness, and reduced cognitive catastrophizing, among others (Folkman & Moskowitz, 2000). These are all likely pathways to be explored in future work.
Our review of the literature reveals that researchers often statically control for a number of constructs, including some of the variables that are hypothesized as potential mediators of the association between psychological well-being and health (e.g., (Liu et al., 2016)). There remains controversy as to whether this constitutes over-adjustment (Diener et al., 2015). We recommend that researchers measure these potential mediators and consider them pathways linking psychological well-being and health. Additional research that carefully delineates timing of the occurrence of various factors along the pathway--psychological well-being leads to better health behaviors (which may also, in turn, improves psychological well-being)--will support our ability to address the question of whether these are variables that should be statistically controlled or instead examined as a critical piece of the puzzle.
A number of factors appear to moderate the association of psychological well-being and health including gender, age, and co-occurring stressful life events. These moderators may explain some of the discrepancies in the literature and future research would benefit from more careful consideration of these potential moderators. For example, using an innovative daily diary approach, Mroczek et al. (2015) were able to identify that it was the positive affect response to daily stressors vs. level of positive or negative affect that was key in predicting longevity. This interesting finding would not have been evident if the moderator of daily stress had not been considered. Culture, too, may be important in terms of the differential conception and value placed on psychological well-being in different cultures. Gratitude--which is often found to boost well-being across the lifespan in English-speaking U.S. samples (e.g., (Watkins, Woodward, Stone, & Kolts, 2003; Wood, Froh, & Geraghty, 2010)--decreased well-being among South Koreans (Layous, Lee, Choi, & Lyubomirsky, 2013). In this case, gratitude was associated with feelings of guilt and the emergent sense of indebtedness appeared detrimental to the well-being of this South Korean sample. Hernandez et al. (2015) recently explored the conception of well-being in US Hispanic/Latino adults and conclude that programs aimed at increasing well-being may need to be adapted before administration in Hispanics/Latinos to include a heightened focus on interpersonal factors with inclusion of religious/spiritual domains. Finally, we can draw on ideas developed by Tsai and colleagues (2006), who have found that people make distinctions between arousal levels of positive affect and that these levels are differentially valued. In the United States and Europe, high-arousal positive affect is often more valued, whereas in Asia, low arousal is often more valued. Future research could examine whether culture alters the impact of high- versus low-arousal positive affect on health.
At a minimum, we recommend that all analyses of psychological well-being and health control for psychological ill-being (e.g., depression or negative affect) and baseline physical health. It is important to control for ill-being in order to demonstrate that presence of psychological well-being is not the same as absence of psychological ill-being (Larsen & McGraw, 2014; Larsen et al., 2001). Similarly, it is important to assess objective health outcomes and to do so in the context of prospective and longitudinal designs to elucidate causality and ensure that psychological well-being is not simply a reflection of superior health instead of a predictor of future health and longevity.
Psychological Well-Being Interventions: The Next Big Frontier
A majority of the studies examining the link between psychological well-being and health are observational. Without experimental trials that explicitly manipulate psychological well-being and demonstrate effects on health-relevant outcomes, the causal direction of the link between psychological well-being and health remains open to question. Observational studies do not provide definitive information regarding the direction of causality and the influence of potential unmeasured variables.
Thus, a critical next step for the field is development and testing of interventions that aim to improve psychological well-being to address questions of causality more definitively. Tested in over 4000 subjects across 51 clinical trials, positive psychology-based interventions show effectiveness in amplifying positive affect and psychological well-being and have significantly led to reduced symptoms of depression in heterogeneous samples of mostly healthy adults (Sin & Lyubomirsky, 2009) reduced depression in women with metastatic breast cancer (Cheung et al., 2016) and people with type 2 diabetes (Cohn, Pietrucha, Saslow, Hult, & Moskowitz, 2014). A recently completed study of a positive affect intervention in people newly diagnosed with HIV demonstrated improvements in psychological well-being, decreases in psychological ill being, and improvements in physical health (e.g., suppressed viral load) compared to an attention-matched control condition (Moskowitz et al., 2017). A number of studies to examine the impact of psychological well-being interventions on physical health in other chronic conditions are currently underway (e.g., (Huffman et al., 2011; Huffman et al., 2015; Moskowitz et al., 2017). As intervention research in this area progresses there are multiple questions to consider. For instance, what are the active ingredients across interventions and what well-being constructs exude the most influence on physiologic functioning? What is the most impactful duration or dosage for these positive psychology interventions? How do interventions need to be tailored to best meet the needs of individuals? Where is the most impact seen within the spectrum of disease states, e.g., before disease onset (primary prevention) or as an avenue to enhance rehabilitation after an acute event (tertiary prevention)?
Conclusion
The field of health psychology is noticeably positioned for a shift away from a narrow, ill-being focus toward a broader view that includes psychological well-being as well. This is not to say that psychological ill-being (e.g., depressive symptoms, anxiety) is not important. We do not advocate for a simplistic positive-only approach to improved health. Clearly negative emotions serve important adaptive functions and at sustained or extreme levels--particularly those leading to psychopathology, they need to be addressed directly. Nonetheless, we argue that psychological well-being is a key factor in the effect of psychology on physical health, and it is a worthy focus of future research and intervention.
Supplementary Material
Acknowledgments
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number 1K01HL130712-01A1 (R. Hernandez, PI).
Footnotes
Conflict of Interest. Authors Hernandez, Bassett, Boughton, Schuette, Shiu, and Moskowitz have no conflict of interest.
Supplementary Material. The online data supplements are available at http://emr.sagepub.com/supplemental.
References
- Bacon SL, Watkins LL, Babyak M, Sherwood A, Hayano J, Hinderliter AL, … Blumenthal JA. Effects of daily stress on autonomic cardiac control in patients with coronary artery disease. The American journal of cardiology. 2004;93(10):1292–1294. doi: 10.1016/j.amjcard.2004.02.018. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Vohs KD, Aaker JL, Garbinsky EN. Some key differences between a happy life and a meaningful life. The Journal of Positive Psychology. 2013;8(6):505–516. [Google Scholar]
- Boehm JK, Kubzansky LD. The Heart’s Content: The Association Between Positive Psychological Well-Being and Cardiovascular Health. Psychological bulletin. 2012;138(4):655–691. doi: 10.1037/a0027448. [DOI] [PubMed] [Google Scholar]
- Boehm JK, Peterson C, Kivimaki M, Kubzansky L. A Prospective Study of Positive Psychological Well-Being and Coronary Heart Disease. Health Psychology. 2011;30(3):259–267. doi: 10.1037/a0023124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm JK, Trudel-Fitzgerald C, Kivimaki M, Kubzansky LD. The Prospective Association Between Positive Psychological Well-Being and Diabetes. Health Psychology. 2015 doi: 10.1037/hea0000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle PA, Barnes LL, Buchman AS, Bennett DA. Purpose in life is associated with mortality among community-dwelling older persons. Psychosomatic medicine. 2009;71(5):574. doi: 10.1097/PSY.0b013e3181a5a7c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown NJ, MacDonald DA, Samanta MP, Friedman HL, Coyne JC. A critical reanalysis of the relationship between genomics and well-being. Proceedings of the National Academy of Sciences. 2014;111(35):12705–12709. doi: 10.1073/pnas.1407057111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Berntson GG. Relationship between attitudes and evaluative space: A critical review, with emphasis on the separability of positive and negative substrates. Psychological bulletin. 1994;115(3):401. [Google Scholar]
- Carvajal SC, Wiatrek DE, Evans RI, Knee CR, Nash SG. Psychosocial determinants of the onset and escalation of smoking: cross-sectional and prospective findings in multiethnic middle school samples. Journal of adolescent health. 2000;27(4):255–265. doi: 10.1016/s1054-139x(00)00124-5. [DOI] [PubMed] [Google Scholar]
- Cheung EO, Cohn MA, Dunn LB, Melisko ME, Morgan S, Penedo FJ, … Moskowitz JT. A randomized pilot trial of a positive affect skill intervention (lessons in linking affect and coping) for women with metastatic breast cancer. Psycho-Oncology. 2016 doi: 10.1002/pon.4312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosomatic Medicine. 2008;70(7):741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- Cohen R, Bavishi C, Rozanski A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: A meta-analysis. Psychosomatic medicine. 2016;78(2):122–133. doi: 10.1097/PSY.0000000000000274. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Turner RB, Alper CM, Skoner DP. Emotional style and susceptibility to the common cold. Psychosomatic Medicine. 2003;65:652–657. doi: 10.1097/01.psy.0000077508.57784.da. [DOI] [PubMed] [Google Scholar]
- Cohn MA, Pietrucha ME, Saslow LR, Hult JR, Moskowitz JT. An online positive affect skills intervention reduces depression in adults with type 2 diabetes. Journal of Positive Psychology. 2014;9(6):523–534. doi: 10.1080/17439760.2014.920410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole SW, Fredrickson BL. Errors in the Brown et al. critical reanalysis. Proceedings of the National Academy of Sciences. 2014;111(35):E3581–E3581. doi: 10.1073/pnas.1413316111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. Journal of Affective Disorders. 2002;72(3):227–236. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- Davidson KW, Mostofsky E, Whang W. Don’t worry, be happy: positive affect and reduced 10-year incident coronary heart disease: the Canadian Nova Scotia Health Survey. Eur Heart J. 2010;31(9):1065–1070. doi: 10.1093/eurheartj/ehp603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. Hedonia, eudaimonia, and well-being: An introduction. Journal of Happiness Studies. 2008;9(1):1–11. [Google Scholar]
- Diener E, Chan MY. Happy people live longer: Subjective well-being contributes to health and longevity. Applied Psychology: Health and Well-Being. 2011;3(1):1–43. doi: 10.1111/j.1758-0854.2010.01045.x. [DOI] [Google Scholar]
- Diener E, Pressman SD, Lyubomirsky S. Can 1 million women be wrong about happiness and health. Los Angeles Times. 2015:A21. [Google Scholar]
- DuBois CM, Lopez OV, Beale EE, Healy BC, Boehm JK, Huffman JC. Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: A systematic review. Int J Cardiol. 2015;195:265–280. doi: 10.1016/j.ijcard.2015.05.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupuy HJ. The psychological general well-being (PGWB) index. Assessment of quality of life in clinical trials of cardiovascular therapies. 1984:170–183. [Google Scholar]
- Enga KF, Braekkan SK, Hansen-Krone IJ, Hansen JB. Emotional states and future risk of venous thromboembolism: the Tromso Study. Thromb Haemost. 2012;107(3):485–493. doi: 10.1160/th11-09-0667. [DOI] [PubMed] [Google Scholar]
- Feller S, Teucher B, Kaaks R, Boeing H, Vigl M. Life satisfaction and risk of chronic diseases in the European prospective investigation into cancer and nutrition (EPIC)-Germany study. PLoS One. 2013;8(8):e73462. doi: 10.1371/journal.pone.0073462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S. Positive psychological states and coping with severe stress. Social science & medicine. 1997;45(8):1207–1221. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- Folkman S, Moskowitz JT. Positive affect and the other side of coping. American psychologist. 2000;55(6):647. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- Freak-Poli R, Mirza SS, Franco OH, Ikram MA, Hofman A, Tiemeier H. Positive affect is not associated with incidence of cardiovascular disease: a population-based study of older persons. Prev Med. 2015;74:14–20. doi: 10.1016/j.ypmed.2015.01.032. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, Grewen KM, Coffey KA, Algoe SB, Firestine AM, Arevalo JM, … Cole SW. A functional genomic perspective on human well-being. Proceedings of the National Academy of Sciences. 2013;110(33):13684–13689. doi: 10.1073/pnas.1305419110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale CR, Batty GD, Deary IJ. Locus of control at age 10 years and health outcomes and behaviors at age 30 years: the 1970 British Cohort Study. Psychosomatic medicine. 2008;70(4):397–403. doi: 10.1097/PSY.0b013e31816a719e. [DOI] [PubMed] [Google Scholar]
- Gruenewald TL, Karlamangla AS, Greendale GA, Singer BH, Seeman TE. Feelings of usefulness to others, disability, and mortality in older adults: The MacArthur study of successful aging. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62(1):P28–P37. doi: 10.1093/geronb/62.1.p28. [DOI] [PubMed] [Google Scholar]
- Hernandez R, Kershaw KN, Siddique J, Boehm JK, Kubzansky LD, Diez-Roux A, … Lloyd-Jones DM. Optimism and Cardiovascular Health: Multi-Ethnic Study of Atherosclerosis (MESA) Health Behav Policy Rev. 2015;2(1):62–73. doi: 10.14485/hbpr.2.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hevey D, McGee HM, Horgan JH. Comparative optimism among patients with coronary heart disease (CHD) is associated with fewer adverse clinical events 12 months later. J Behav Med. 2014;37(2):300–307. doi: 10.1007/s10865-012-9487-0. [DOI] [PubMed] [Google Scholar]
- Hill PL, Turiano NA. Purpose in life as a predictor of mortality across adulthood. Psychological science. 2014;25(7):1482–1486. doi: 10.1177/0956797614531799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoebel BG, Rada PV, Mark GP, Pothos EN. Neural systems for reinforcement and inhibition of behavior: Relevance to eating, addiction, and depression 1999 [Google Scholar]
- Hoen PW, Denollet J, de Jonge P, Whooley MA. Positive affect and survival in patients with stable coronary heart disease: findings from the Heart and Soul Study. J Clin Psychiatry. 2013;74(7):716–722. doi: 10.4088/JCP.12m08022. [DOI] [PubMed] [Google Scholar]
- Howell RT, Kern ML, Lyubomirsky S. Health benefits: Meta-analytically determining the impact of well-being on objective health outcomes. Health Psychology Review. 2007;1(1):83–136. [Google Scholar]
- Huffman JC, Mastromauro CA, Boehm JK, Seabrook R, Fricchione GL, Denninger JW, Lyubomirsky S. Development of a positive psychology intervention for patients with acute cardiovascular disease. Heart Int. 2011;6(2):e14. doi: 10.4081/hi.2011.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, Millstein RA, Mastromauro CA, Moore SV, Celano CM, Bedoya CA, … Januzzi JL. A positive psychology intervention for patients with an acute coronary syndrome: Treatment development and proof-of-concept trial. Journal of Happiness Studies. 2015 doi: 10.1007/s10902-015-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huta V, Ryan RM. Pursuing pleasure or virtue: The differential and overlapping well-being benefits of hedonic and eudaimonic motives. Journal of Happiness Studies. 2010;11(6):735–762. [Google Scholar]
- Ickovics JR, Milan S, Boland R, Schoenbaum E, Schuman P, Vlahov D, Group HERS. Psychological resources protect health: 5-year survival and immune function among HIV-infected women from four US cities. Aids. 2006;20(14):1851–1860. doi: 10.1097/01.aids.0000244204.95758.15. [DOI] [PubMed] [Google Scholar]
- Ironson G, Balbin E, Stuetzle R, Fletcher MA, O’Cleirigh C, Laurenceau J, … Solomon G. Dispositional optimism and the mechanisms by which it predicts slower disease progression in HIV: proactive behavior, avoidant coping, and depression. International Journal of Behavioral Medicine. 2005;12(2):86–97. doi: 10.1207/s15327558ijbm1202_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ironson G, Hayward HS. Do positive psychosocial factors predict disease progression in HIV-1? A review of the evidence. Psychosomatic medicine. 2008;70(5):546. doi: 10.1097/PSY.0b013e318177216c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, Biswas-Diener R, King LA. Reconsidering happiness: The costs of distinguishing between hedonics and eudaimonia. The Journal of Positive Psychology. 2008;3(4):219–233. [Google Scholar]
- Kelloniemi H, Ek E, Laitinen J. Optimism, dietary habits, body mass index and smoking among young Finnish adults. Appetite. 2005;45(2):169–176. doi: 10.1016/j.appet.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Keyes CL, Shmotkin D, Ryff CD. Optimizing well-being: the empirical encounter of two traditions. Journal of personality and social psychology. 2002;82(6):1007. [PubMed] [Google Scholar]
- Kim ES, Smith J, Kubzansky LD. Prospective study of the association between dispositional optimism and incident heart failure. Circ Heart Fail. 2014;7(3):394–400. doi: 10.1161/circheartfailure.113.000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labarthe DR. From Cardiovascular Disease to Cardiovascular Health A Quiet Revolution? Circulation-Cardiovascular Quality and Outcomes. 2012;5(6):E86–E92. doi: 10.1161/Circoutcomes.111.964726. [DOI] [PubMed] [Google Scholar]
- Labarthe DR, Kubzansky LD, Boehm JK, Lloyd-Jones DM, Berry JD, Seligman ME. Positive Cardiovascular Health: A Timely Convergence. Journal of the American College of Cardiology. 2016;68(8):860–867. doi: 10.1016/j.jacc.2016.03.608. [DOI] [PubMed] [Google Scholar]
- Lambiase MJ, Kubzansky LD, Thurston RC. Positive psychological health and stroke risk: The benefits of emotional vitality. 2015 doi: 10.1037/hea0000228. [DOI] [PubMed] [Google Scholar]
- Larsen JT, McGraw AP. The case for mixed emotions. Social and Personality Psychology Compass. 2014;8(6):263–274. [Google Scholar]
- Larsen JT, McGraw AP, Cacioppo JT. Can people feel happy and sad at the same time? Journal of personality and social psychology. 2001;81(4):684. [PubMed] [Google Scholar]
- Layous K, Lee H, Choi I, Lyubomirsky S. Culture Matters When Designing a Successful Happiness-Increasing Activity: A Comparison of the United States and South Korea. Journal of Cross-Cultural Psychology. 2013;44(8):1294–1303. doi: 10.1177/0022022113487591. [DOI] [Google Scholar]
- Liu B, Floud S, Pirie K, Green J, Peto R, Beral V Million Women Study C. Does happiness itself directly affect mortality? The prospective UK Million Women Study. Lancet. 2016;387(10021):874–881. doi: 10.1016/s0140-6736(15)01087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Xiao Q, Cai Y, Li S. The quality of life and mortality risk of elderly people in rural China: the role of family support. Asia Pac J Public Health. 2015;27(2):NP2232–2245. doi: 10.1177/1010539512472362. [DOI] [PubMed] [Google Scholar]
- Menninger KA, Menninger WC. Psychoanalytic observations in cardiac disorders. American Heart Journal. 1936;11(1):10–21. [Google Scholar]
- Moskowitz JT, Carrico AW, Duncan LG, Cohn MA, Cheung EO, Batchelder A, … Folkman S. Randomized controlled trial of a positive affect intervention for people newly diagnosed with HIV. Journal of Consulting and Clinical Psychology. 2017 doi: 10.1037/ccp0000188. In-Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek DK, Stawski RS, Turiano NA, Chan W, Almeida DM, Neupert SD, Spiro A., 3rd Emotional Reactivity and Mortality: Longitudinal Findings From the VA Normative Aging Study. J Gerontol B Psychol Sci Soc Sci. 2015;70(3):398–406. doi: 10.1093/geronb/gbt107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabi H, Kivimaki M, De Vogli R, Marmot MG, Singh-Manoux A. Positive and negative affect and risk of coronary heart disease: Whitehall II prospective cohort study. BMJ. 2008;337:a118. doi: 10.1136/bmj.a118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson G, Ohrvik J, Lonnberg I, Hedberg P. Low Psychological General Well-Being (PGWB) is associated with deteriorated 10-year survival in men but not in women among the elderly. Archives of Gerontology and Geriatrics. 2011;52(2):167–171. doi: 10.1016/j.archger.2010.03.010. [DOI] [PubMed] [Google Scholar]
- Okely JA, Gale CR. Well-being and chronic disease incidence: The English longitudinal study of ageing. Psychosomatic medicine. 2016;78(3):335. doi: 10.1097/PSY.0000000000000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavot W, Diener E. Review of the satisfaction with life scale. Psychological assessment. 1993;5(2):164. [Google Scholar]
- Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Rahe RH, Rubin RT, Gunderson E, Arthur RJ. Psychologic Correlates of Serum Cholesterol in Man: A Longitudinal Study. Psychosomatic medicine. 1971;33(5):399–410. doi: 10.1097/00006842-197109000-00002. [DOI] [PubMed] [Google Scholar]
- Richman LS, Kubzansky L, Maselko J, Kawachi I, Choo P, Bauer M. Positive emotion and health: going beyond the negative. Health Psychology. 2005;24(4):422. doi: 10.1037/0278-6133.24.4.422. [DOI] [PubMed] [Google Scholar]
- Ronaldson A, Poole L, Kidd T, Leigh E, Jahangiri M, Steptoe A. Optimism measured pre-operatively is associated with reduced pain intensity and physical symptom reporting after coronary artery bypass graft surgery. J Psychosom Res. 2014;77(4):278–282. doi: 10.1016/j.jpsychores.2014.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy B, Diez-Roux AV, Seeman T, Ranjit N, Shea S, Cushman M. The association of optimism and pessimism with inflammation and hemostasis in the Multi-Ethnic Study of Atherosclerosis (MESA) Psychosomatic medicine. 2010;72(2):134. doi: 10.1097/PSY.0b013e3181cb981b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell JA, Carroll JM. On the bipolarity of positive and negative affect. Psychological bulletin. 1999;125(1):3. doi: 10.1037/0033-2909.125.1.3. [DOI] [PubMed] [Google Scholar]
- Ryff CD, Singer BH, Love GD. Positive health: Connecting well-being with biology. Philosophical Transactions-Royal Society of London Series B Biological Sciences. 2004:1383–1394. doi: 10.1098/rstb.2004.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepperd JA, Maroto JJ, Pbert LA. Dispositional optimism as a predictor of health changes among cardiac patients. Journal of research in personality. 1996;30(4):517–534. [Google Scholar]
- Sin NL, Lyubomirsky S. Enhancing Well-Being and Alleviating Depressive Symptoms With Positive Psychology Interventions: A Practice-Friendly Meta-Analysis. Journal of Clinical Psychology. 2009;65(5):467–487. doi: 10.1002/Jclp.20593. [DOI] [PubMed] [Google Scholar]
- Sin NL, Moskowitz JT, Whooley MA. Positive affect and health behaviors across 5 years in patients with coronary heart disease: the heart and soul study. Psychosomatic medicine. 2015;77(9):1058–1066. doi: 10.1097/PSY.0000000000000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sone T, Nakaya N, Ohmori K, Shimazu T, Higashiguchi M, Kakizaki M, … Tsuji I. Sense of life worth living (ikigai) and mortality in Japan: Ohsaki Study. Psychosomatic medicine. 2008;70(6):709–715. doi: 10.1097/PSY.0b013e31817e7e64. [DOI] [PubMed] [Google Scholar]
- Steger MF, Kashdan TB, Oishi S. Being good by doing good: Daily eudaimonic activity and well-being. Journal of Research in Personality. 2008;42(1):22–42. [Google Scholar]
- Suls J. Toxic Affect - Are Anger, Anxiety, and Depression Independent Risk Factors for Cardiovascular Disease? Emotion Review 2017 [Google Scholar]
- Trudel-Fitzgerald C, Boehm JK, Kivimaki M, Kubzansky LD. Taking the tension out of hypertension: a prospective study of psychological well being and hypertension. J Hypertens. 2014;32(6):1222–1228. doi: 10.1097/hjh.0000000000000175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai JL, Knutson B, Fung HH. Cultural variation in affect valuation. Journal of Personality and Social Psychology. 2006;90(2):288. doi: 10.1037/0022-3514.90.2.288. [DOI] [PubMed] [Google Scholar]
- Tsenkova VK, Love GD, Singer BH, Ryff CD. Socioeconomic status and psychological well-being predict cross-time change in glycosylated hemoglobin in older women without diabetes. Psychosomatic medicine. 2007;69(8):777–784. doi: 10.1097/PSY.0b013e318157466f. [DOI] [PubMed] [Google Scholar]
- Vallacher RR, Wegner DM. What do people think they’re doing? Action identification and human behavior. Psychological review. 1987;94(1):3. [Google Scholar]
- van Montfort E, Denollet J, Widdershoven J, Kupper N. Interrelation and independence of positive and negative psychological constructs in predicting general treatment adherence in coronary artery patients—Results from the THORESCI study. Journal of psychosomatic research. 2016;88:1–7. doi: 10.1016/j.jpsychores.2016.06.009. [DOI] [PubMed] [Google Scholar]
- Wakai K, Kojima M, Nishio K, Suzuki S, Niwa Y, Lin Y, … Yamamoto A. Psychological attitudes and risk of breast cancer in Japan: a prospective study. Cancer Causes & Control. 2007;18(3):259–267. doi: 10.1007/s10552-006-0111-x. [DOI] [PubMed] [Google Scholar]
- Watkins PC, Woodward K, Stone T, Kolts RL. Gratitude and happiness: Development of a measure of gratitude, and relationships with subjective well-being. Social Behavior and Personality: an international journal. 2003;31(5):431–451. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of personality and social psychology. 1988;54(6):1063. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wiest M, Schuz B, Webster N, Wurm S. Subjective Well-Being and Mortality Revisited: Differential Effects of Cognitive and Emotional Facets of Well-Being on Mortality. Health Psychology. 2011;30(6):728–735. doi: 10.1037/a0023839. [DOI] [PubMed] [Google Scholar]
- Wilson TE, Weedon J, Cohen MH, Golub ET, Milam J, Young MA, … Fredrickson BL. Positive Affect and Its Association With Viral Control Among Women With HIV Infection. Health psychology: official journal of the Division of Health Psychology, American Psychological Association. 2016 doi: 10.1037/hea0000382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winefield HR, Gill TK, Taylor AW, Pilkington RM. Psychological well-being and psychological distress: is it necessary to measure both? Psychology of Well-Being. 2012;2(1):1–14. [Google Scholar]
- Wood AM, Froh JJ, Geraghty AW. Gratitude and well-being: A review and theoretical integration. Clinical psychology review. 2010;30(7):890–905. doi: 10.1016/j.cpr.2010.03.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.