Abstract
Dentin hypersensitivity (DH) is a very common dental problem that can have a negative impact on the quality of life and can lead to invasive dental procedures. Prevention of DH and control of symptoms are highly desirable. Hydroxyapatite (HAP) has been shown in vitro to block dentinal tubules and in vivo to be a safe and effective additive in oral care products that reduce DH clinically. This study’s aim was to conduct a systematic review and meta-analysis of the current evidence that HAP-containing oral care products reduce DH. Databases were searched, and only clinical trials in humans were included; studies conducted in vitro or on animals were not included. Publications in a foreign language were translated and included. We found 44 published clinical trials appropriate for systematic analysis. More than half of the trials had high-quality GRADE scores. HAP significantly reduced dentin hypersensitivity compared to placebo (39.5%; CI 95% [48.93; 30.06]), compared to fluoride (23%; CI 95% [34.18; 11.82]), and with a non-significant tendency compared to other desensitizing agents (10.2%; CI 95% [21.76; −19.26]). In conclusion, the meta-analysis showed that HAP added to oral care products is a more effective agent than fluoride in controlling dentin hypersensitivity and may be superior to other desensitizers.
Keywords: hydroxyapatite, dentin hypersensitivity, remineralization, dentin tubule, quality of life, pain, systematic review, meta-analysis
1. Introduction
While enamel is acellular and comprised of nearly entirely inorganic mineral apatite, making it relatively inert, healthy teeth can respond to stimuli applied to the tooth such as thermal stimuli (ice and heat) and tactile because the underlying connective tissue, the dentin, is connected to the pulp complex, a highly innervated live tissue with nerve fibers capable of detecting stimuli and transmitting signals to the brain. Teeth become ‘extra’ sensitive for many reasons. For example, hairline cracks, poorly bonded restorations, or advanced carious lesions can cause pathological pain that brings patients into the dental office for treatment. Another very common problem of dental pain is called dentin hypersensitivity (DH), usually the result of exposure to the surface of dentin, generally at the cement-enamel junction. Gingival recession and loss of cementum from excessive tooth brushing or demineralization by highly acidic dietary (or external) acidic challenges can cause the entrances of dentin tubules to be exposed to the oral environment. Once this happens, even the mildest cold or airflow stimuli or focused tactile stimuli can result in sharp, severe pain. DH is, therefore, a “short, sharp pain arising from exposed dentin in response to stimuli, typically thermal, evaporative, tactile, osmotic, or chemical and which cannot be ascribed to any other form of dental defect or disease” [1,2,3]. It is this form of dentin pain that is the focus of this systematic review.
The current accepted theory of the induction of pain from DH is the “hydrodynamic theory” [4,5]. When the extracellular fluid in dentin tubules moves, the dentinal tubule processes of the odontoblasts can detect this movement. Through their close contact with the afferent pain nerve fibers in the tubules, the odontoblasts transmit the pain sensation. The movement of fluid can be created through desiccation, thermal changes (cold hot), physical force (fingernail or dental explorer), or osmotic pressures (dissolution of sugars).
DH is very common in the adult population. A recent systematic review showed that patients of all ages with permanent teeth have reported DH, with a prevalence of about one-third of the population at any given time across all studies [6].
The primary strategy for treating DH and maintaining reduced hypersensitivity is to physically cover the exposed dentin and prevent the movement of fluid in or out of the dentin tubules. Conservative procedures should be considered prior to using irreversible ones, such as dental fillings, or periodontal surgery [2]. Chemically occluding the entrances to the dental tubules, either with in-office procedures or with therapies administered at home, is a more conservative and effective approach. There are several agents that have been investigated in the past to conservatively treat DH [7,8]. There have been 8 systematic reviews of therapeutic treatment of dentin hypersensitivity published in the recent past that included studies on hydroxyapatite (HAP) as an active desensitization agent [8,9,10,11,12,13,14,15] (Supplementary Materials: Table S1). They included studies on HAP that ranged in number from just one to as many as 20 studies. All of them concluded that HAP was an effective dentin desensitizer. Two systematic reviews concluded that HAP was superior to other methods of controlling dentin hypersensitivity [11,13]. Those treatments that achieve dentin tubule occlusion with physical deposits for extended periods of time are considered better treatments than those that only achieve that on a short-term basis. Ingredients that encourage and speed up the natural remineralization process are also well suited for lowering DH symptoms. Biomimetic HAP seems to be one of those agents that fulfills both roles, since it is very similar to the HAP crystals between and intertwined within the collagen fiber bundles of dentin [16].
Since the most recent meta-analysis on the science of HAP reducing DH is 3 years old and we wanted to include foreign language studies, we conducted an updated systematic review and meta-analysis on all the RCTs where HAP was shown in clinical trials to reduce DH.
2. Materials and Methods
We used the PICO framework to guide the focus of this literature review. P: Patients—patients of all ages with healthy, non-carious dentitions with some level of dentin hypersensitivity. Patients undergoing periodontal or vital bleaching were not excluded. I: Intervention—the introduction of one of the following oral care products containing biomimetic HAP as an active ingredient; toothpaste, mouthwash, professional product or gel, either in-office professionally administered or self-administered at home. C: Comparison—no intervention (comparison to baseline), placebo controls (HAP-free oral care products), and positive controls (containing other desensitizing agents) were all considered. O: Outcome—a reduction in dentin hypersensitivity, which included reduction from tactile, cold air, ice water, heat, and electrical stimuli as measured by electric pulp testing, visual analogue scales, ordinal scale scores, or subject questionnaire self-assessments.
The following primary databases were searched: PubMed (Ovid Medline), EMBASE, Scopus, Cochrane Library, and Web of Science. Google Scholar was also searched. Two authors had a previous list of published papers. These provided 3 additional publications found outside of the search. The PRISMA guidelines for literature searches [17] were followed (see Supplementary Materials for the completed PRISMA-S checklist). We did not limit our search to English language publications. We found studies in the Korean, Italian, German, and Russian languages. These were translated using Google Translate. We searched the literature up to and including 1 May 2022. No studies on animals, in vitro or in situ human studies were included, even though mechanistic occlusion of exposed dentin tubules is the proposed mechanism of HAP desensitization. We also crosschecked the references that were reported in our previous comprehensive search [18]. For this updated meta-analysis on the efficacy of HAP in reducing DH, we were interested only in human clinical trials providing clinical evidence of efficacy in patients who could report changes in dentin hypersensitivity.
A qualitative analysis (synthesis) was completed for the studies that met the inclusion criteria. We rated the quality of the evidence using the guidelines in dentistry and GRADE graphics described by Richards et al. [19]. A Cochrane Risk of Bias (RoB) analysis using the methods of Sterne et al. [20] was conducted, and a table was generated.
For the meta-analysis, studies that met the inclusion criteria where at least two groups were compared were used. Where baseline data and data from the final examination were available, we calculated the mean reduction of DH (Schiff-Score, Wong–Baker, or VAS-Scale) for each group and then the difference between the groups. Those data were also calculated as the mean relative difference between the groups (in %), which were then used for the meta-analysis. Three different forest-plots were generated: HAP compared to placebo (1), HAP compared to fluoride (2), and HAP compared to other known actives for reducing DH (3). As (3) comprises many different active ingredients, weighting of the sample sizes was not performed for all analyses (1–3) to reduce the possible risk of bias. The calculation and meta-analysis were performed using the open-source software R, version 4.2.1 (R-project.org). We also used the packages dplyr and forestplot [21].
3. Results
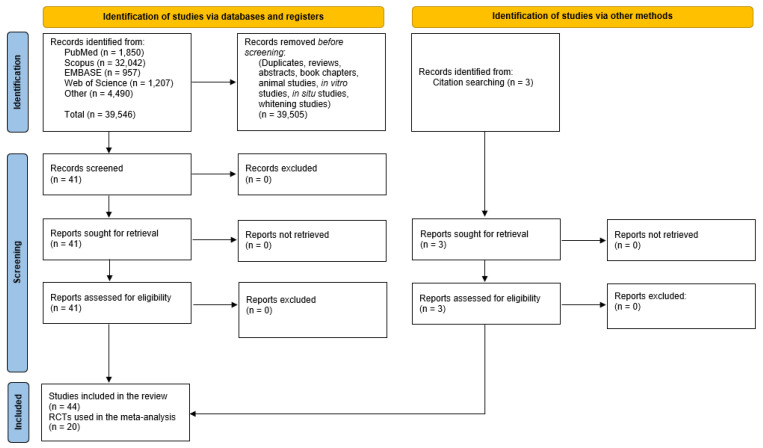
Despite limiting our search to human dentin sensitivity and HAP, nearly 40,000 titles had to be screened in order to avoid missing any published studies. After duplicates and irrelevant papers, reviews, abstracts, book chapters, experiments conducted on animals, in vitro and in situ were all rejected (for not meeting our inclusion criteria), we found 44 relevant clinical trials where HAP was investigated clinically for the reduction of DH. Figure 1 summarizes the results of the search using the strategies outlined in the methods.
Figure 1.
Flow diagram summary of the systematic review search strategy and results.
A complete list of search words is provided in the Supplementary Materials (Table S2), along with the results of the number of citations found. The details of the 44 publications that met the inclusion criteria for the qualitative and quantitative synthesis are shown in Table 1. All retrieved studies were read in detail and assessed for quality. The GRADE assignments are shown in the table.
Table 1.
Summary of all clinical trials of hydroxyapatite (HAP) treatment of dentin sensitivity with GRADE assignments.
| Study Author (Country) | Subjects | HAP Product |
Controls | Study Design and Length | Experi-mental Conditions | Blinding and Random-ization |
p-Value (</=) |
Exam-iner Cali-bration | Study Conclusion |
Comments | Quality of Evidence | GRADE Graphic |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Al Asmari & Khan, 2019 (Saudi Arabia) [22] |
72 adults 20–70 years |
Biorepair (20% Zn-carbonate hydroxy-apatite) (Zn-CHA) |
none | Clinical trial 8 weeks of 2 times/day brushing with the toothpaste Baseline + 2 follow up exams |
-air blast then Schiff sensitivity scale | Not Report-ed (NR) |
0.001 | Kappa = 0.83 | “The use of the desensitizing toothpaste containing Zn-CHA in patients with DH provides significant rapid relief from DH.” | -a before and after trial design with no control -no blinding or randomiza-tion |
LOW |

|
| Alencar et al., 2020 (Brazil) [23] |
32 adult subjects | 1. nHAP tooth-paste (simul- ated light) 2. nHAP tooth-paste after laser light treatment |
3. laser light + HAP-free toothpaste 4. simulated laser light + nHAP-free toothpaste |
1-month clinical trial baseline, 1, 2 applications, then 1 month measure-ment -toothpastes used at home between treatments |
Tactile and air blast VAS scale |
Double blinded and random-ized | 0.05 | NR | “Intragroup analysis showed that only the GnHAP (simul -ated light and nHAP toothpaste) group showed a regression of DH at 1 month for the two applied stimuli.” |
Small RCT with significant reduction in the nHAP toothpaste group | MODER-ATE |

|
| Alharith et al., 2021 (Saudi Arabia) [24] |
63 adults 18–60 years (mean age 39 years) |
1. Nano-XIM (15% HAP) | 2. Fluorophat Pro (5% NaF) 3. Glycerin water placebo |
1 week RCT |
-explorer tactile stimulus or -cold air blast -then Schiff sensitivity scale |
Double blinded | 0.001 | Kappa = 0.76, 0.79 | “Within the limitations of the study, n-HA paste was the most effective desensitizing paste compared to fluoride and placebo pastes.” | -a well conducted RCT to test relief of dentin sensitivity after 1 week use of the test paste | HIGH |

|
| Alsen et al., 2022 (Brazil) [25] |
30 adult subjects 20 to 50 years |
1. Nano-P containing nHAP (+9000 ppm fluoride, 5% KO3) | 2. Flor-opal (0.5% fluoride, 3% KNO3) 3. H2O |
1-month RCT single in office application before vital bleaching |
Air stimulation followed by Numerical Rating Scale (=VAS) scores |
Blinding not possible for the exam-iner -patient partially blinded |
0.05 | NR | “Nanohydroxyapatite was more effective than fluoride, the commonly used material in this field, in reducing DH instantly after its application, though both materials had similar effects two- weeks and one-month post application.” | -in office one-time application -low subject numbers |
LOW |

|
| Amaechi et al., 2018 (USA) [26] |
52 adult subjects 18 to 80 years |
Apadent Pro (20% HAP) dental cream | 20% silica cream | -ribbon of cream applied in tray for 5 min after brushing each evening before bed 8-week RCT with evaluations at 2, 4, 6, and 8 weeks |
4-point Dental Pain Scale + VAS scale after cold and air stimulation |
Double blinded, random-ized | 0.001 | Kappa Values = 0.80/0.88 (Air VAS), 0.87/0.89 (Air DPS), 0.91/0.94 (Cold VAS), 0.90/0.89 (Cold DPS) |
“Within the limits of this study, it can be concluded that 20% nHAP dental cream is an effective method to promote the relief of DHS symptoms when applied daily.” | -a well conducted RCT | HIGH |

|
| Amaechi et al., 2021 (USA) [27] |
105 adult subjects 18 to 80 years |
1. 10% n-HAP paste 2. 15% n-HAP paste |
3. 10% n-HAP + 5% KNO3 4. CPSC + Na-MFP (1450 ppm fluoride) |
2 times brushing per day 8-week RCT with evaluations at 2, 4, 6, and 8 weeks |
Endo-ice cold test air stimulation |
Double blinded, random-ized | 0.001 | Kappa Values = 0.91/0.94 (Cold VAS) 0.80/0.88 (Air VAS) |
“… it can be concluded that toothpaste containing nano-HAP alone (10 or 15% nano-HAP) or supplemented with KNO3 (10%nano-HAKN) was effective in relieving DHS symptoms when used at least twice daily. The study further demonstrated that the toothpaste containing 15% nano-HAP was more effective in sensitivity reduction than that containing 10% nano-HAP.” | -a well conducted RCT -dose response demon-strated |
HIGH |

|
| Amin et al., 2015 (India) [28] |
30 adult subjects 20 male, 10 female |
Aclaim (15% Hap) | none | 6-month trial -toothpaste used at home -evaluations at baseline, 1, 3, and 6 months |
-air stimulation -ice water then VAS |
NR | 0.0001 | NR | “This study proves the efficacy of nano- hydroxyapatite paste in treating dentinal hyper-sensitivity.” | -a before and after trial design with no control -no blinding or randomization |
LOW |

|
| Anand et al., 2018 (India) [29] |
60 adult subjects mean age 42 42% males |
1% nHAP toothpaste | Pro-Argin sensitivity fluoride toothpaste | 4-week trial -toothpastes used at home -evaluations at baseline, 5 min, 1 week, and 4 weeks |
-tactile test, and air stimulation then VAS for pain -digital electric pulp tester recordings |
Double blinded -random ization by comp-uter and allot-ment carried out by another clinician |
0.000 | NR | “It appears from this study that both nHA based and arginine-based toothpastes are useful in the management of dentin hypersen-sitivity.” | -a well conducted RCT | HIGH |

|
| Barrone & Malpassi, 1991 (Italy) [30] |
40 adult subjects | 15% HAP paste | No control | 6-month trial -toothpastes used at home -evaluations at baseline, 1, 2, 4, 12, and 24 weeks |
Dental pulp test | NR | NR | “The topical application of a 15% gel of supermicron hydroxylapalite dentin according to our clinical experiences leads to an almost complete resolution of the symptoms in a very short time.” | A longitudinal before and after study showing effective reduction in dentin sensitivity (no control) | LOW |

|
|
| Bevilacqua et al., 2016 (Brazil) [31] |
30 adult subjects 18 to 60 years of age |
Desensi-bilize Nano-P (contain-ing 20% nHAP + 9000 ppm fluoride, 5% KO3) | 1.23% fluoride gel Biosilicate |
3-month split mouth design, professional application of either fluoride or biosilcate followed by Nano-P at baseline, week 1, 2 and 3 -final analysis at 3 months |
Air blast stimulus 10-point VAS scale |
Double blinded Randomization method not reported |
0.05 | NR | “It can be concluded that there were no significant differences between treatments evaluated and, at the end of three months, all tested desensitizing agents reduced dentin hypersen-sitivity.” | A 3-month RCT with professional application -HAP was suspected of helping to reduce DS but did not show clearly because of the RCT design |
LOW |

|
| Browning et al., 2011 (USA) [32] |
42 adult subjects | Renamel After-Bleach) nHAP-paste |
Zero nHAP placebo | 2-week trial -desensitizer paste applied twice daily by tray 30 min after at home 7% hydrogen peroxide tray bleaching -Aim fluoride toothpaste without desensitizer was used by all subjects |
-diary-based VAS pain scores recorded by subjects daily for 2 weeks | -double blinded -alloca-tion by random-ization chart |
0.001 | NR | “Within the limits of the study it can be concluded that use of a nano-hydroxyapatite paste following application of a tooth whitening agent was associated with a statistically significant reduction in the duration of tooth sensitivity.” | -no supervised pain stimuli used -diary method of subjective VAS pain score -method-ologically weak design |
LOW |

|
| Choi et al., 2014 (Korea) [33] |
24 adult subjects 21 to 61 years of age -average age 38.1 years |
10% HAP + 19% TCP in commer-cial fluoride tooth-paste | Fluoride toothpaste control | 4-week clinical trial baseline, 1, 2, and 4 weeks |
Cold water test 10 cm VAS scale + 4-point Verbal rating scale |
NR | NR | NR | “The toothpaste made with hydroxyapatite and tricalcium phosphate significantly relieves pain depending on the period of use.” | Statistical reduction in HS when HAP and TCP are added to fluoridated toothpaste-unable to show if it was the HAP or TCP | LOW |

|
| Da Silva et al., 2018 (Brazil) [34] |
60 adult subjects 18 to 26 yrs of age |
1. Nano-P containing 20% nHAP (+9000 ppm fluoride, 5% KO3) | 2. Colgate Sensitive ProArgin 3. Contene Organic without desensitizing additives |
3-month trial 5 min application after bleaching then 3 times/day brushing with the paste |
Sensitivity scores from 0 to 4 -eval-uations before bleaching, 1- and 10-days during bleaching, then at 1, 2, and 3 months |
Randomization by numerical draw | 0.05 | NR | “The subjects treated with n-HAP and arginine presented lower sensitivity when compared to the control group.” | Well done RCT with ordinal scores | HIGH |

|
| de Oliveira et al., 2016 (Brazil) [35] |
8 adult subjects, 138 sensitive teeth age 24–46 years |
1. Nano-P contain-ing 20% nHAP (+9000 ppm fluoride, 5% KO3) |
2. Sensodyne Rapid Relief 3. Colgate Sensitive Pro-Relief 4. Fluoride-free toothpaste (Cocorico) |
10 s (Nano-P) to 60 s applications (digital vs. hand-piece brush) -in-office single application |
VAS score immediately, at 1 day and at 30 days | double blinded sealed random allocation by an independent researcher |
0.001 | Calibrated examiners with an interclass corre-lation of 0.99 | “The only desensitizing toothpaste that provided an immediate relief effect after both stimuli was that composed of calcium phosphate nanoparticles in the form of hydroxy-apatite.” | -in-office one time application low subject numbers but adequate number of teeth compared |
MODER-ATE |

|
| Ding et al., 2020 (China) [36] |
45 adult subjects 18 to 60 years |
20% n-CAP (nanocarbonate apatite) (Denti-guard Sensitive) |
Placebo toothpaste | 6-week RCT -toothpaste applied 2 times/day at home |
Air blast then VAS and Schiff Cold Air sensitivity scores 12 to 24 h after root planning, then at 0, 2, 4, and 6 weeks |
Double blinded Random-ization by com-puter |
0.001 | NR | “The application of n-CAP-based dentifrice after non-surgical periodontal therapy could had some benefit on the reduction of DH after 4-week at- home use compared to the control dentifrice.” | Well done clinical trial showing the test toothpaste was signifi-cantly better than placebo in lowering dentin sensitivity at 6 weeks |
HIGH |

|
| Ehlers et al., 2021 (Germany) [37] |
21 subjects with MIH age 6 to 16 years |
10% HAP (Kinder Karex) | 1400 ppm amine fluoride toothpaste (Elmex Junior) |
2-month (mean = 56 days) trial -toothpaste applied 2 times/day |
Air blast then Schiff Cold Air Sensitivity Score + Tactile stimulus followed by Wong–Baker FACES pain rating scale |
Double blinded SAS comp-uter gener-ated random-ization with age stratifi-cation |
0.013 | NR | “Both toothpastes (hydroxy-apatite versus amine fluoride) were effective in re- lieving hypersen-sitivity and maintaining desensitisation for 8 weeks.” | Well done clinical trial showing HAP works as well as amine fluoride to reduce sensitivity in young patients with MIH | HIGH |

|
| Gopinath et al., 2015 (India) [38] |
36 adult subjects age 18 to 60 years |
n-HAP (Acclaim) | 5% calcium sodium phosphor-silicate (CSP) (Shy-NM with NovaMin) |
4-week clinical trial toothpaste applied 2 times/day at home -baseline and 4th week measure-ments |
tactile, air, then cold water applica-tions (in order, 5 min apart) then 10-point VAS scale scores | Double blinded Randomization allocation not reported |
0.000 to 0.004 | NR | “NovaMin and nano- HAP showed significant reductions in dentine hypersensitivity at the end of 4 weeks.” | A double blinded trial with just one time point measured after toothpaste use | MODER-ATE |

|
| Gümüstas et al., 2021 (Turkey) [39] |
64 subjects 18 to 40 years of age |
30% n-HAP in alcohol (Prof. Oral Care nHAP Desenstizer) | CPP-ACP (Tooth Mousse) 2.09% NaF (Ionite) placebo |
1 week trial after vital bleaching -application was made for 4 min prior to bleaching |
Air blast stimulation Followed by 5-point VAS scale scores |
Triple blinded (patient, operator and evalu-ator all masked to group assign-ment) -third person did random- ization -method not reported |
0.05 | NR | “Remineralization agents used for the treatment of post-operative sensitivity from tooth bleaching reduces the severity of the hyper-sensitivity, but does not prevent it from happening” | An in-office, single application trial with 1 and 7 day follow up | MODER-ATE |

|
| Hütte-mann & Dönges, 1987 (Germany) [40] |
140 adult subjects 20 to 60 years old |
A: 17% HAP (6 µm) H: 17% HAP (2 µm) |
B: 17% salt C: 0.125% benzocaine D: placebo E: 9% HAP. 8% salt, 0.125% benzocaine F: 17% HAP, 6% SrCl2 G: 17% HAP, 5% SrCl2, 1% amine fluoride |
1 to 2-week trial -paste applied at home |
Standard-ized cold test -question-naire results |
NR | NR | NR | “The efficacy of finely granular hydroxyapatite in the treatment of dentine sensitivity was demonstrated, 90% of the subjects indicated improvement after 3 to 5 days, 50% were pain-free within the period of the study.” | Trial comparing multiple pastes -subjective patient reporting of home experience with pastes |
LOW |

|
| Jena & Shash-irekha, 2015 (India) [41] |
45 adult subjects age 18 to 50 years |
15% HAP (nano-XIM) | 5% NovaMin (Vantej) 8% arginine Colgate Sensitive Pro-Relief) |
4-week trial one time application of paste |
-Tactile test 10-point VAS scale -Air blast -Schiff Cold Air Sensi-tivity Score -evalua-tions at 1 and 4 weeks |
Double blinded Random-ization with comp-uter-gener-ated table |
0.05 | NR | “15% n-HA containing toothpaste was found to be most effective followed by 8% arginine and 5% NovaMin group.” | RCT with one time application | HIGH |

|
| Kang et al., 2009 (Korea) [42] |
150 adult subjects mean age of 35 years |
HAP tooth-paste (Diome Plus PRTC, Korea) | Fluoride toothpaste (2080 Korea) Strontium chloride toothpaste (Senso-dyne GSK) |
4-week trial assessments at 1 and 4 weeks -toothpastes used at home |
Ice test stimulus -11-point VAS |
NR | 0.0001 | NR | “Toothpaste containing hydroxyapatite is effective in reducing hyper-sensitivity.” | Clinical trial showing HAP toothpaste reduced DS | LOW |

|
| Kim et al., 2008 (Korea) [43] |
100 adult subjects age 22 to 69 years mean age 47.2 years |
10% HAP (Diomi-plus PRTC, Korea) |
Strontium chloride toothpaste (Senso-dyne, GSK) | 4-week trial assessments at 1 and 4 weeks -toothpastes used at home |
cold test stimulus 11-point VAS |
NR | 0.0001 | NR | “The toothpaste containing apatite showed statistically significant similar results to the toothpaste containing strontium chloride, which is known to have a significant effect on hypersensiti-vity through several previous studies.” | Clinical trial showing HAP toothpaste reduced DS as well as strontium chloride toothpaste | LOW |

|
| Kim et al., 2009 (Korea) [44] |
55 adult subjects mean age of 43.5 years |
10% HAP (Diomi-plus PRTC, Korea) |
Strontium chloride toothpaste (Sensodyne GSK) | 8-week trial -baseline, 2-, 4- and 8-week assessments -toothpastes used at home |
Cold water and air blast stimulus 10 cm VAS scale + Verbal rating score |
Double blinded (method not re-ported) Random-ized (method not re-ported) |
0.05 | NR | “The toothpaste containing hydroxyapatite showed no statistical difference in reducing hyper-sensitivity from the toothpaste containing strontium chloride, which was previously known to be effective for dental hyper-sensitivity, and showed significant clinical improvement during the 8-week period of use” | RCT showing HAP toothpaste reduced DS as well as strontium chloride toothpaste |
MODER-ATE |

|
| Kondyurova et al., 2019 (Russia) [45] |
60 adult subjects age 18 to 65 (mean = 39.5) |
0.5% nHAP (SPLAT Sensitive Ultra) | 0.1% nHAP (Splat Profess-ional Sensitive White) | 4-week trial -exam-inations at baseline, 2 and 4 weeks |
air blast (using Schiff sensitivity score) after tactile then chemical stimuli, both scored with a 4-point scale | Tooth-pastes handed out in original package labels Com-puter-gener-ated random-ization |
0.05 | NR | “In conclusion, the results of this study support the short term efficacy of a x% nHAP occlusion technology-based toothpaste for the relief of dentin hyper-sensitivity.” | Not blinded -significant reduction of dentin sensitivity for both concen-trations of HAP |
LOW |

|
| Lee et al., 2015 (Korea) [46] |
82 adult subjects 20 to 65 years of age mean age 37.2 years |
1. 20% n-CAP (Carbon-ated HAP), 8% silica (Denti-guard Sensitive) | 2. 10% CaCO3, 10% SrCl2 (Senso-dyne, GSK) 3. Laser treatment |
4-week trial -profession-al laser treatment at baseline, week 1 and week 2 -test toothpastes used at home 2 times/day -then standard fluoride toothpaste used for the remaining 2 weeks |
Tactile and air blast sensitivity 10 cm VAS scale + 4 point Schiff scores |
Single blinded Random-ization claimed but not reported |
0.05 | Two exam-iners were cali-brated Kappa not reported |
“The use of both the desensitizing dentifrices containing 20% n-CAP as self-care and the Er,Cr:YSGG laser as professional treatment were effective in reducing dentin hyper-sensitivity.” | A single blinded RCT showing carbonated HAP in silica reduced DS as well as laser and strontium chloride toothpaste | MODER-ATE |

|
| Loguercio et al., 2015 (Brazil) [47] |
40 adult subjects 22 to 24 years of age |
Nano-P (20% nHAP + 9000 ppm fluoride + 5% KO3) | Placebo paste | 2-day trial -paste was applied in office before vital bleaching |
Tooth sensitivity was recorded using a numeric rating scale (0–4) during bleaching and up to 48 h after each session. | Double blinded -the pack-aging was the same, but the placebo had a different consist-ency Comp-uter-gener-ated random-ization tables |
0.53 | 85% kappa agree-ment for patient allo-cation |
“The use of a nano-calcium phosphate paste containing potassium nitrate, fluoride, and calcium phosphate prior to in-office bleaching did not reduce bleaching-induced tooth sensitivity measured during and up to 48 h after each session.” | Short trial -no significant de-sensitizing -placebo was missing fluoride and KNO3 so no conclusion could have been reached about HAP |
LOW |

|
| Low et al., 2015 (USA) [48] |
60 adult patients 18 to 75 years of age 47 females, 13 males |
AO Pro Tooth-paste sensitive (KNO3, MFP, nHAP, phloretin, ferulic acid, syli-marin) |
No control |
2-week trial -assessment at baseline and then at home after 2 weeks using the toothpaste |
Question-naire -five questions, rated on a 10-point scale, asking (i) degree of pain, (ii) duration of pain, (iii) intensity of pain, (iv) tolerability of pain, and (v) description of pain. | NR | 0.001 | NR | “The outstanding results of speed and effectiveness of the commercially available toothpaste suggest the contributing activity of the newer nano-hydroxyapatite and of the polyphenol antioxidants.’ | Not able to determine which ingredient worked -results qualitative -no control |
VERY LOW |

|
| Maharani et al., 2012 (Indon-esia) [49] |
20 adult subjects | A: commer-cial HAP tooth-paste with potas-sium and zinc C: citrates, MFP and phos-phate | B: placebo (no active ingre-dients) | 8-hr trial measuring DS at baseline, 30 sec after application of the paste and after 8 hr | Electric pulp tester followed by a 10-point VAS | Double blinded | 0.05 | Kappa = 0.87 (intra-exam-iner) |
“It may be concluded that treatment with (hydroxy-apatite toothpaste) effectively reduced dentin hyper-sensitivity. The effect was instant and long lasting.” | Short duration, low number of subjects clinical trial -cannot determine which ingredient was effective |
VERY LOW |

|
| Makeeva et al., 2016 (Russia) [50] |
30 adult subjects one group younger than the other 17 to 44 years of age |
Medical HAP (Apadent Total Care) |
No control |
3-month clinical trial -toothpaste used at home |
Air blast sensitivity test 4 point Schiff score |
NR | NR | NR | “Long-term use of Apadent Total Care toothpaste effectively reduces tooth sensitivity in patients of different age groups.” | Simple trial –before and after design with no control | LOW |

|
| Makeeva et al., 2018 (Russia) [51] |
40 young adult subjects 20–25 years of age |
6% Nano-HAP (Innova paste) + 1% Nano-HAP liquid (Liquid Enamel) |
No paste, liquid control | 14-day trial assessment at 3, 7, and 14 days |
Air blast sensitivity test 4 point Schiff score |
NR | NR | NR | “Nano-HAP 6% paste and 1% suspensions can be used as an alternative replacement therapy in the treatment of enamel hyperesthesia.” | Simple trial –before and after design with no control | LOW |

|
| Orsini et al., 2010 (Italy) [52] |
75 adult subjects -between 18 and 75 years |
30% Zn Carbon-ate Hydroxy-apatite tooth-paste (BioRe-pairPlus) |
Sensodyne Pronamel | 8-week trial -subjects brushed teeth 2 times per day for at least 1 min for the entire trial |
Tactile, air and cold tests 3-point sensitivity scale plus 10-point subjective pain scale |
Double blinded Comp-uter-gener-ated random-ization |
0.001 to 0.009 | NR | “This trial represents the first clinical demonstration that nanostructured CHA microparticles may significantly reduce painful stimuli and could therefore be used as active ingre- dients for desensitizing dentifrices.” | Well done clinical trial with significant reduction in dentin sensitivity | HIGH |

|
| Orsini et al., 2013 (Italy) [53] |
90 adult subjects 18 to 75 years of age 29 males, 69 females |
30% Zn Carbon-ate Hydroxy-apatite tooth-paste (BioRe-pairPlus) |
8% Arginine carbonate 1450 ppm F MFP (Colgate Sensitive) 8% Sr Acetate, 1044 F NaF (Senso-dyne Rapid Relief) |
3-day trial subjects brushed teeth 2 times/day for the 3-day trial |
Tactile, air and cold tests 3-point sensitivity scale plus 10-point subjective pain scale |
Double blinded Com-puter-gener-ated random- ization |
0.003 | One exam-iner, no Kappa statistics reported | “The three tested dentifrices significantly reduced DH after 3-day treatment, supporting their use in clinical practice.” | A short well done clinical trial |
HIGH |

|
| Park et al., 2005 (Korea) [54] |
44 adult subjects 26 to 71 years of age |
Tooth-paste with microcrystalline HAP | No control | 8-week clinical trial -assess-ments at 2, 4, and 8 weeks |
-cold, air, tactile stimula-tions 10 cm VAS scale + 4-point verbal rating scale |
NR | 0.05 | NR | “The toothpaste containing micro-crystalline hydroxyapatite has a relieving effect on various stimuli that cause hyper-sensitivity symptoms such as cold stimulation, compressed air stimulation, and tactile stimulation during the period of use for 8 weeks” | Simple trial –before and after design with no control | LOW |

|
| Pinojj et al., 2014 (India) [55] |
80 teeth per group Subjects were 18 to 50 years of age |
nHAP tooth-paste (SHY NM) | Calcium Phospho-silicate (SHY) CPP-ACP paste |
3-month trial -baseline, 2, 4 weeks, 2, 3-month exam-inations after using toothpastes 2 times/day at home |
Air and cold-water stimulus 10-point VAS scale + Schiff base 3-point scores |
Triple blinded Random-ization method not reported |
0.000 | NR | “The nanoparticle hydroxyapatite group was found to be significantly better in reducing the visual analog scale score as well as Schiff test score and at any time point for both measures of sensitivity.” | A clinical trial showing superiority of nHAP toothpaste in lowering dentin sensitivity. | MODER-ATE |

|
| Polyakova et al., 2022 (Russia) [56] |
30 adult subjects 35–45 years of age |
20% n-HAP paste | nZnMg-HAP positive control n-FAP positive control |
1 month trial evaluated at baseline, 2 and 4 weeks |
Air blast stimulus 4-point Schiff sensitivity score |
Double blinded Ran- Domized (details not pro-vided) |
0.00083 | NR | “The nZnMgHAP-containing toothpaste provided a significant reduction in airblast sensitivity after 2 weeks of daily use in adult patients with cervical non-carious defects. This effect was significantly greater compared to pure nHAP and nFAP.” | The 20% n-HAP paste significantly reduced DH at 4 weeks compared to baseline. Mg and Zn seemed to improve the desensitisation effect |
HIGH |

|
| Porciani et al., 2014 (Italy) [57] |
100 adult subjects 18 to 65 years of age |
12 mg CaHAP + 97 mg diCaPhos-phate Dihy-drate (DPD) per 1.4 gm chewing gum stick | Placebo control | 2-week trial -two chewing sticks 3 times/day for 2 weeks -exam-ination at baseline, 1 and 2 weeks |
Air blast, tactile, cold-water test 3-score sensitivity test + 10-point subjective score |
Double blinded Random-ization method not reported |
0.001 to 0.05 | NR | “The group using the chewing gum containing calcium hydroxyapatite had a statistically significant reduction in all clinical test indexes for dentin hyper-sensitivity after one and two weeks, and a statistically significant reduction compared to the control gum group.” | A 2 week chewing gum blinded trial showed either CaHAP or DPD or both effectively lowered dentin sensitivity | LOW |

|
| Reddy et al., 2014 (India) [58] |
30 adult subjects | Acclaim (15% HAP) | Colgate Pro-Argin | 3-day clinical trial -toothpaste used at home |
Air blast and cold-water stimu-lation 10-point verbal rating scale |
Blinding not reported Random-ization details not pro-vided |
0.001 | NR | “’Both the experimental dentifrices Pro-Argin and Acclaim were found to provide rapid relief in patients.” | Short trial, lower quality with significant results for both toothpastes in lowering dentin sensitivity | LOW |

|
| Seong et al., 2021 (England) [59] |
82 adult subjects age 18 to 65 years |
KNO3/Al/HAP/ MFP (Sunstar) |
5% KNO3/NaF (Senso-dyne) | 2-week clinical trial baseline, 1- and 2-week exam-inations toothpaste used 2 times/day at home |
Tactile then cold test 3-point VAS scale + quality of life question-naire |
Exam-iner blinding Ran-dom- ization method not reported |
0.001 | NR | “This study demonstrated the efficacy of an aluminium lactate/ potassium nitrate/ hydroxyl-apatite toothpaste compared to a potassium nitrate control toothpaste for the prevention of dentine hyper-sensitivity both immediately and over a 2-week period.” |
Single blinded RCT -HAP may have reduced DS, but positive control selection meant other ingredients (Al, MFP) could have helped |
LOW |

|
| Shetty et al., 2010 (India) [60] |
486 teeth in 45 adult subjects -aged 28 to 42 years |
A: HAP in dry sol powder B: HAP liquid |
C: placebo D: no treatment |
8-week trial In-office application -baseline, + 1-, 2-, 4- and 8-week exam-inations |
Tactile, cold water, air blast stimuli -Linear VAS scores, and verbal rated scores of 0 to 3 |
Single blinded -method of random- ization not reported |
0.001 | NR | “HAP shows definite potential as an effective desensitizing agent providing quick relief from symptoms.” | Single blinded, but well controlled clearly showing in office treatment with HAP reduces DS for 4 weeks but not 8 weeks. | LOW |

|
| Vano et al., 2014 (Italy) [61] |
105 adult subjects mean age 43 years |
Group 1: 15% nHAP (Prev-Dent) |
Group 2: Positive fluoride paste control (1500 ppm F as MFP- Colgate Cavity protection) Group 3: Prev-Dent Placebo |
4-week RCT -baseline + 2- and 4-week exam-inations -toothpaste used 2 times/day at home |
Tactile and air blast stimuli -VAS scale and examiner-based Schiff assessment |
Double blinded Random number gener-ator used for random-ization |
0.001 | Kappa statistics was con-ducted on inter-examiner perfor-mance on 10% of subjects but results not reported | “The findings of the present study encourage the application of nano-hydroxyapatite in fluoride-free toothpaste as an effective desensitizing agent providing quick relief from symptoms after 2 and 4 weeks.” | Well done HAP RCT showing HAP toothpaste desensitized dentin better than regular fluoride toothpaste and the placebo | HIGH |

|
| Vano et al., 2015 (Italy) [62] |
60 subjects 27 to 29 years of age |
6% hydrogen peroxide with 2% nHAP (Prev-Dent) | 6% hydrogen peroxide control group | A 2-week dentin sensitivity trial within a 9 mo. vital bleaching trial -the active ingredient was compared to the control at 1, 7, and 14 days |
Tactile and air blast stimuli -VAS scale and examiner-based Schiff assessment |
Random card gener-ated allo-cation -blinded to the exam-iner |
0.05 | Kappa Score of 0.89 on duplicate exam-inations of 10% of the subjects | “6% HP with 2% n-HA resulted in significant lower tooth sensitivity at 24 h post-treatment.” | Single blinded RCT with significant reduction of DS during vital bleaching | MODER-ATE |

|
| Vano et al., 2018 (Italy) [63] |
105 adult subjects average age of 39 yrs |
2% nHAP tooth-paste (Cavex Bite and White ExSense) | Colgate Cavity Gel protection Placebo |
4-week clinical trial -gel applied 10 min daily examination at baseline, 2 and 4 weeks |
-cold air and tactile sensitivity 100 mm VAS scale and Schiff base 4-point scores |
Double blinded Com-puter-gener-ated random-ization table |
0.05 | Kappa statistics was con-ducted on inter-examiner perfor-mance on 10% of subjects but results not reported | “The application of nano-hydroxyapatite in gel toothpaste fluoride free is an effective desensitizing agent providing relief from symptoms after 2 and 4 weeks”. | Double blinded RCT showing significant reduction of DS by 2% nHAP gel | HIGH |

|
| VJ Nar-mantha & Thakur, 2014 (India) [64] |
45 adult patients | 1% nHAP (Acclaim) |
5% KNO3
(Senso-dent-K) Propolis toothpaste |
Air blast sensitivity | 100 mm VAS scale | NR | 0.03 | NR | “It can be concluded that nanohydroxy-apatite and propolis are a potential treatment modality for dentin hyper-sensitivity.” | Small, not randomised and not blinded study | LOW |

|
| Wang et al., 2016 (Brazil) [65] |
28 adult subjects, 137 teeth -between 18 and 60 years old |
Destab-ilize Nano-P (20% nHAP, KNO3, 9000 fluoride NaF) Home-care Nano-P (10% HAP, KNO3, 900 ppm F NaF) |
Pro-Relief Pro-Argin (8% arginine) Duraphat varnish (26,300 ppm fluoride) |
3-month clinical trial -varnish and professional paste applied profess-ionally at each appoint-ment but home care pastes applied at home -assessment at 1 and 3 months |
Air blast stimulus 10-point VAS scale |
Double blinded Randomization by MS Excel program |
0.94 (no diff-erence bet-ween groups) |
Cali- brated exam-iners |
“Nano-hydroxy-apatite formulations (with or without home-care product association) were as effective as the other treatments in reducing dentin hyper-sensitivity over three months.” |
Mixed RCT with profess-ional + home care (patients likely not blinded to professional treatment) |
MODER-ATE |

|
3.1. Testing Dentin Hypersensitivity (DH)
A variety of tests to illicit DH were used. The most common was an air blast using compressed air from a standard dental chair air–water syringe. Ice, or ice water, was also used as a cold stimulus, and tactile stimuli were used by applying a dental explorer. Most researchers have standardized their stimuli (same distance, isolation of neighboring teeth). Some studies evaluated DH at baseline, and many evaluated only one time point after the start of the clinical trials. Others tested DH at several time points at 2, 3, or even 4 weeks apart after measuring the baseline DH.
3.2. Dentin Hypersensitivity (DH) Scoring Results
Nearly all the studies involved using a patient response scoring system that involved a 4-point scale of increasing sensitivity severity (Schiff score [66]), a 10-point visual analogue scale (VAS), or one that required the subject to place a mark on a distance scale (e.g., 10 cm). One study [49] used an electric pulp tester, which eliminated the subjective aspects of dentin sensitivity reporting. Another study [37], which involved younger patients, used the Wong–Baker FACES pain rating scale [67]. The sensitivity tests were reproducible, accurate, and produced, in nearly all the clinical trials, changes in dentin hypersensitivity that showed statistically significant improvements in comfort in the subjects examined.
3.3. Qualitative Synthesis
3.3.1. GRADE Assignments
Of the 44 clinical trials found, half were double-blinded and randomized clinical trials (RCTs). The quality of those RCTs was rated as moderate to high. Some studies reported as RCTs were downgraded because they failed to provide the methods used for randomization. Some claimed they were blinded studies but did not provide the details of how the examiners or patients were blinded. These also received a lower GRADE score. Of the 44 trials, 11 were conducted to investigate the HAP application in an office setting with one or two applications. The others involved sending the subjects home with products to use. The length of the studies varied from a few days to 3 months. One study was conducted for 6 months. Three-month observation periods were used most often to evaluate the long-term efficacy of the test products.
From Table 1, it can be seen that all the studies except for one showed a statistically significant clinical benefit of HAP in reducing DH. In those studies where HAP was applied professionally, immediate relief of DH was achieved. HAP helped in the reduction of post-bleaching sensitivity in DH. At home application of HAP was in the form of gels in custom trays, but mostly it was in the form of toothpaste used twice a day. One study found that adding HAP to chewing gum worked to reduce DH. Compared to the placebo, HAP reduced DH from 6% to 80%. HAP was as good as or better than fluoride controls in reducing DH and as good or better than other desensitizing agents in reducing DH. This was confirmed in the meta-analyses of those studies that could be included in the meta-analyses (see Section 3.4 below).
3.3.2. Risk of Bias
The Risk of Bias (RoB) assignments of 44 clinical trials included in the qualitative synthesis are shown in Table 2. Of those, 23 had low risk of bias, 15 had high risk of bias, and the remainder fell in between those ratings.
Table 2.
Risk of Bias (RoB) assignments of the hydroxyapatite (HAP) and dentin hypersensitivity clinical trials.
| Study | Tested Products |
Application Protocol |
Trial Length (Weeks) |
Random Sequence Genera- tion a (Selection Bias) |
Allocation Conceal- ment b (Selection Bias) |
Blinding of Participants and Personnel b (Performance Bias) | Blinding of Outcome Data c (Attrition Bias) | Incomplete Outcome Data d (Attrition Bias) | Selective Reporting e (Reporting Bias) | Overall BIAS |
|---|---|---|---|---|---|---|---|---|---|---|
| Al Asmari & Khan, 2019 [22] |
Zn-carbonate HAP before and after trial -no placebo |
At home toothpaste | 8 | NA | NA |

|

|

|

|

|
| Alencar et al., 2020 [23] |
Nano-P HAP paste vs. placebo after laser | Profess- ional + at home toothpaste |
4 |

|

|

|

|

|

|

|
| Alharith et al., 2021 [24] |
NanoXIM (15% HAP), Fluorophat Pro (5% NaF), placebo | Profess- ional (one time) |
1 |

|

|

|

|

|

|

|
| Alsen et al., 2022 [25] |
Nano-P, Fluor-Opal, dH20 (placebo) | Profess- ional (one time) |
4 |

|

|

|

|

|

|

|
| Amaechi et al., 2018 [26] |
one 5 min application each day in custom tray 20% nHAP cream vs. 20% Silica |
At home (custom tray) |
8 |

|

|

|

|

|

|

|
| Amaechi et al., 2021 [27] |
10%nHAP (+/− KNO3), 15% nHAP, CSPS | At home (tooth paste) |
8 |

|

|

|

|

|

|

|
| Amin et al., 2015 [28] |
before and after Acclaim (1% HAP), no placebo or pos. control |
At home (tooth paste) |
24 | NA | NA |

|

|

|

|

|
| Anand at al, 2018 [29] |
Aclaim (1% HAP) vs. Colgate Sensitive Pro-Relief (8% Arginine) | At home (tooth paste) |
4 |

|

|

|

|

|

|

|
| Barone & Malpassi, 1991 [30] |
before and after trial 15% HAP gel applied 10 sec. 3x/day |
At home gel applica- tion 2 weeks |
24 | NA | NA |

|

|

|

|

|
| Bevilacqua et al., 2016 [31] |
1.23% APF gel + nano-P vs. APF-gel + Biosilicate | Profess- ional one time for 1 min |
12 |

|

|

|

|

|

|

|
| Browning et al., 2011 [32] |
nHAP (Renamel AfterBleach) placebo control |
At home (custom tray after bleaching) |
4 |

|

|

|

|

|

|

|
| Choi et al., 2014 [33] |
10% HAP (+ F, TCP) vs. control (not specified) | At home toothpaste | 4 |

|

|

|

|

|

|

|
| Da Silva et al., 2018 [34] |
20% HAP paste (Nano P) vs. placebo or Colgate Sensitive ProArgin (8% arginine) | At home toothpaste (after bleaching) | 12 |

|

|

|

|

|

|

|
| De Oliveira et al., 2016 [35] |
20% HAP (Nano P) vs. Sesnodyne, Sensitive Pro-Relief, placebo | Profess- ional (one time) |
4 |

|

|

|

|

|

|

|
| Ding et al., 2020 [36] |
20% HAP paste vs. placebo | At home toothpaste | 6 |

|

|

|

|

|

|

|
| Ehrlers et al., 2021 [37] |
Kinder Karex (10% HAP) toothpaste vs. Elmex (amine fluoride, 1400 ppm fluoride) | At home toothpaste | 8 |

|

|

|

|

|

|

|
| Gopinath et al., 2015 [38] |
Aclaim (1% HAP) vs. 5% CSPS paste | At home toothpaste | 4 |

|

|

|

|

|

|

|
| Gümüştaş & Dikmen, 2021 [39] |
Oral Care Nano HAP (30% Hap) vs. placebo, Tooth Mousse, 2.09% NaF (Ionite) | Profess- ional one time before bleaching |
1 |

|

|

|

|

|

|

|
| Hüttemann & Dönges, 1987 [40] |
9 to 17% HAP (+/- benzocaine, SrCl2, Amine fluoride) |
At home toothpaste | 1+ |

|

|

|

|

|

|

|
| Jena & Shashire-kha, 2015 [41] |
15% HAP vs. 5% Novamin, 8% arginine toothpaste | Profess- ional one time |
4 |

|

|

|

|

|

|

|
| Kang et al., 2009 [42] |
HAP vs. SrCl2, fluoride toothpaste (compositions unknown) |
At home toothpaste | 4 |

|

|

|

|

|

|

|
| Kim et al., 2008 [43] |
Diomiplus PRTC (fluoride toothpaste with 10% HAP) vs. Sensodyne | At home toothpaste | 4 |

|

|

|

|

|

|

|
| Kim et al., 2009 [44] |
Diomiplus PRTC (fluoride toothpaste with 10% HAP) vs. Sensodyne | At home toothpaste | 8 |

|

|

|

|

|

|

|
| Kondyurova et al., 2019 [45] |
SPLAT 0.5% HAP vs. SPLAT (0.1% HAP) | At home toothpaste | 4 |

|

|

|

|

|

|

|
| Lee et al., 2015 [46] |
Dentiguard Sensitive (20% carbonate HAP, 8% silica) vs. SrCl2, Laser | -Laser in office (twice) -at home toothpaste |
4 |

|

|

|

|

|

|

|
| Loguercio et al., 2015 [47] |
Nano P vs. placebo | Profess- ional one time 10 min |
2 |

|

|

|

|

|

|

|
| Low et al., 2015 [48] |
HAP toothpaste with MFP, KO3 -no placebo control |
At home toothpaste | 2 |

|

|

|

|

|

|

|
| Maharani, 2012 [49] |
HAP toothpaste with zinc, TSP, MFP vs. placebo | Profess- ional one time |
8 h |

|

|

|

|

|

|

|
| Makeeva et al., 2016 [50] |
Apadent Total Care (7.0% HAP) | At home toothpaste | 12 |

|

|

|

|

|

|

|
| Makeeva et al., 2018 [51] |
6% HAP paste + 1% INNOVA vs. no treatment control | At home toothpaste and rinse | 2 |

|

|

|

|

|

|

|
| Orsini et al., 2010 [52] |
Biorepair (Zn-carbonated HAP) vs. ProNamel | At home toothpaste | 8 |

|

|

|

|

|

|

|
| Orsini et al., 2013 [53] |
Zn-carbonate 30% HAP vs. 8% arginine +1450 ppm F, 8% SrAcetate + 1040 ppm fluoride toothpastes | At home toothpaste | 3 days |

|

|

|

|

|

|

|
| Park et al., 2005 [54] |
HAP toothpaste (content not provided), no control | At Home toothpaste | 8 |

|

|

|

|

|

|

|
| Pinojj et al., 2014 [55] |
Aclaim (1.0 % HAP) vs. CSPS, CPP-ACP | At Home toothpaste | 12 |

|

|

|

|

|

|

|
| Polyakova et al., 2022 [56] |
20% HAP paste vs. ZnMgHAP and F-HAP pastes | At home toothpaste | 4 |

|

|

|

|

|

|

|
| Porciani et al., 2016 [57] |
HAP + dicalcium phosphate dihydrate chewing gum vs. palcebo | At home chewing gum 3 times/day | 2 |

|

|

|

|

|

|

|
| Reddy et al., 2014 [58] |
Aclaim (1% HAP) vs. Coglate ProArgin | At home toothpaste | 3 |

|

|

|

|

|

|

|
| Seong et al., 2021 [59] |
HAP (+KNO3, Al-lactate) vs. Sensodyne | At home toothpaste | 2 |

|

|

|

|

|

|

|
| Shetty et al., 2010 [60] |
High % HAP slurry vs. placebo | Professional one time |
8 |

|

|

|

|

|

|

|
| Vano et al., 2014 [61] |
15% HAP paste vs. fluoride paste vs. placebo | At home toothpaste | 4 |

|

|

|

|

|

|

|
| Vano et al., 2015 [62] |
2% HAP in 6% carbamide peroxide bleach vs. CP bleach without HAP | At home gel applica- tion 2 weeks |
2 |

|

|

|

|

|

|

|
| Vano et al., 2018 [63] |
Cavex (2% HAP paste) vs. Colgate Cavity Gel (1500 ppm fluoride in MFP) paste vs. glycerin placebo | At home gel applica- tion one time/day 10 min |
4 |

|

|

|

|

|

|

|
| VJ Narmatha & Thakur, 2014 [64] |
Aclaim (1% HAP) vs. Sensodent-K (5%KNO3) vs. 10% propolis | At home toothpaste | 4 |

|

|

|

|

|

|

|
| Wang et al., 2016 [65] |
Desensibilize Nano-P (20% HAP, 9000 ppm F, KNO3) vs. ProArgin, Prorelief, 5% NaF varnish | Professional application one time/week, 3 weeks |
12 |

|

|

|

|

|

|

|
a Randomization: Was the allocation sequence random? Was the allocation sequence concealed until the participants were assigned to the intervention. Did the baseline difference suggest a problem with the randomization process? b Deviations from intended interventions: Were participants aware of the assigned intervention? Were people delivering interventions aware of the participants’ assigned intervention? If yes, were there deviations from the intended intervention that arose because of trial context? If yes, were these deviations likely to have affected the outcome? If yes, were these deviations balanced between the groups? If yes, was an appropriate analysis used to estimate the effect of assignment to intervention? If no, was there potential for substantial impact on the result? c Missing outcome data: Were data for this outcome for all or nearly all participants randomized? If no, is there evidence that the result was not biased by missing outcome data? If no, could missingness of outcome data depend on its true value? d Measurement of the outcome: Was the method of measuring the outcome appropriate? Could measurement of the outcome have differed between intervention groups? If no, were outcome assessors aware of the intervention received by the study participants? If yes, could assessment of the outcome have been influenced by the knowledge of if the intervention received? If yes, is it likely that this occurred? e Selection of the reported result: Were the data that produced the results analyzed in accordance to the prespecified analysis plan that was finalized before unblinded outcome data were available for analysis? Is the numerical result being assessed likely to have been selected, on the basis of the results, from (a) multiple eligible outcome measurements? (b) multiple eligible analyses of the data?
3.4. Quantitative Synthesis—Meta-Analysis
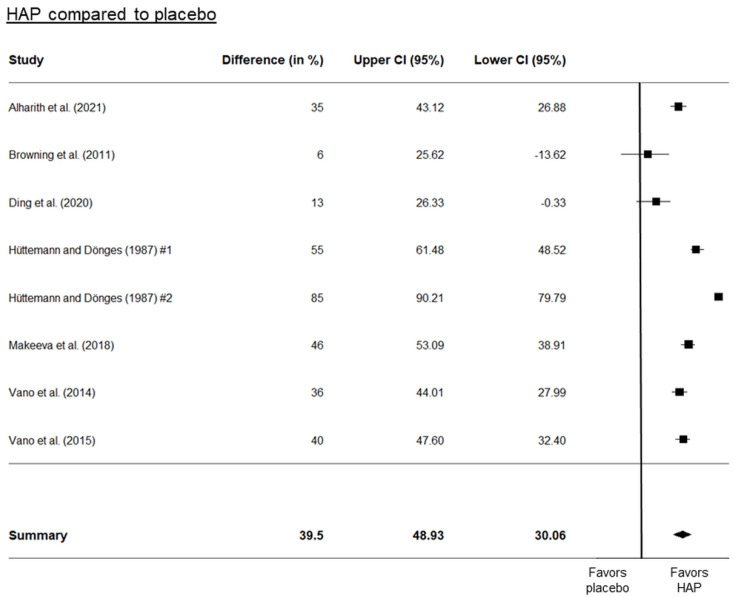
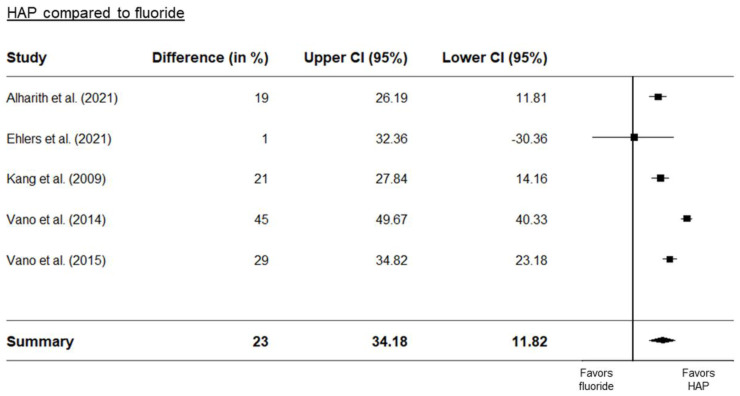
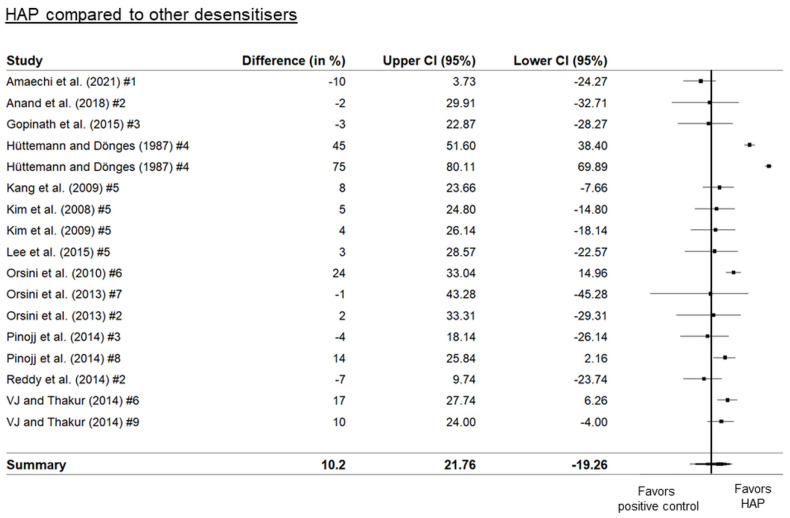
Three separate forest plots were generated from the meta-analysis. These included a comparison between HAP and placebo (Figure 2), between HAP and fluoride (Figure 3), and between HAP and other desensitizers (Figure 4). The results showed that HAP worked as well or better than fluoride or other desensitizing agents in reducing DH. The degree of mean relative reduction ranged from 10.2% (CI 95% [21.76; −19.26]) reduction in the HAP-group compared to positive controls, mean relative reduction of 23% (CI 95% [34.18; 11.82]) in the HAP-group compared to fluoride, and mean relative reduction of 39.5% (CI 95% [48.93; 30.06]) in the HAP-group compared to placebo. Figure 2, Figure 3 and Figure 4 show the forest plots of the main outcome comparisons.
Figure 2.
Forest plot of HAP compared to placebo. Hüttemann and Dönges [40] tested the different particle sizes of HAP. #1 indicates a particle diameter of 6 µm, and #2 indicates a particle diameter of 2 µm. Details of the studies in this figure are in Table 1. Other references: Alharith [24], Browning [32], Ding [36], Makeeva [51], Vano [61,62].
Figure 3.
Forest plot of HAP compared to fluoride. Details of the studies in this figure can be found in Table 1. References: Alharith [24], Ehlers [37], Kang [42]. Vano [61,62].
Figure 4.
Forest plot of HAP compared to other desensitizing agents. Numbers indicate different types of agents: #1: 20% silica, #2: arginine, #3: Bioglass (calcium sodium phosphosilicate), #4: 0.125% benzocaine, #5: SrCl2 combined with CaCO3, #6: KNO3, #7: strontium acetate, #8: casein-phosphoprotein amorphous calcium phosphate (CPP-ACP), #9: propolis. Details of the studies in this figure and the ingredient comparisons are provided in Table 1. References: Amaechi [27], Anand [29], Gopinath [38], Hüttemann [40], Kim [43,44], Lee [46], Orsini [52,53], Pinojj [55], Reddy [58], VJ and Thakur [64].
4. Discussion
Two of the most common clinical problems of dentition for which patients seek professional help are dental decay and hypersensitive teeth. While the former can lead to tooth loss and the latter is more of an annoyance, making consuming foods and beverages of different temperatures and sweetness very uncomfortable, both conditions can benefit from the attention of a preventive dentistry professional before the problem becomes too difficult to manage. In our last systematic review, we focused on the anti-caries efficacy of HAP in toothpaste to reduce dental caries in children [18]. Here, we have turned our attention to the ability of HAP toothpaste to manage dentin hypersensitivity in adults, a very common condition. The prevalence of DH varies greatly, but based on a meta-analysis [6], at least every third adult, on average, suffers, or has suffered from the condition.
HAP has been used for decades in toothpaste in Japan, where it was first developed, and in other countries (e.g., Germany), but it is a relatively new product in North America. Despite its widespread use in other dental applications, such as coating dental implants, bone repair, and periodontal surgery (see review by Chen et al. [68]), it has only recently become an accepted ingredient in oral care products in North America. Supplementary Material Table S3 lists those products for use in Canada approved by Health Canada for sensitive teeth. Most products for use in the USA can be purchased through online importers, such as Amazon.com.
4.1. How HAP Reduces Dentin Hypersensitivity (DH)
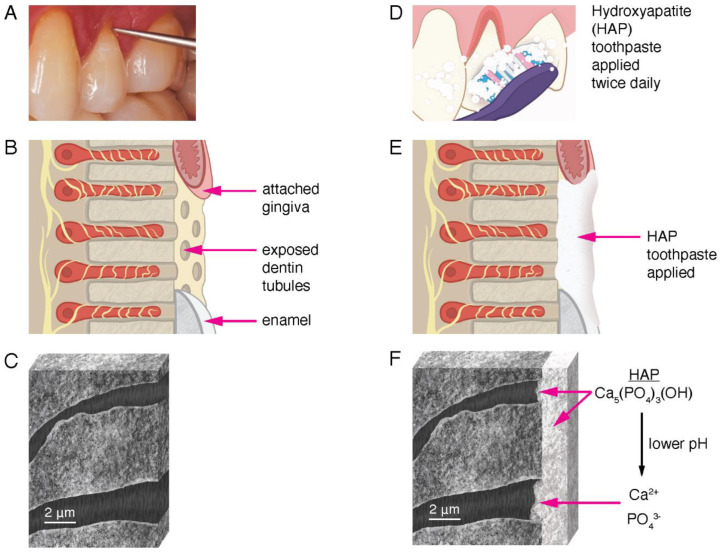
Many in vitro experiments have shown that HAP in toothpaste and other oral care products adhere to the exposed dentin surface, coat the surfaces with microscopic particles of HAP, and occlude open dentin tubules, thereby reducing fluid flow and blocking pain signals from the odontoblast processes to the brain [69]. In addition, studies have shown that a lower plaque pH (or lower pH from dietary exposure) encourages dissociation of the HAP particles into calcium and phosphate ions [66,70,71]. Existing HAP crystals grow in the presence of excess calcium and phosphate ions. These are provided by the dissociation of HAP particles supplied by the oral care products exposed to a lower pH. The calcium and phosphate ions diffuse further into the dentin tubules. The pH is higher in the tubules the further from the surface the ions diffuse, and eventually salivary buffers neutralize the weak acids. This encourages the mineral phase to remineralize, grow, and occlude the tubules further than the physical obstructions provided by the HAP particles, which are still intact. When added to oral care products that are used regularly at home simply by brushing teeth twice a day, HAP-particles can serve to block dentin tubules and contribute to their remineralization (Figure 5).
Figure 5.
Illustration of the mechanism of HAP reduction of dentin sensitivity. (A): Clinical photograph of gingival recession on tooth 24, showing exposed dentin at the cervical margin indicated by the tip of the explorer. Tactile sensitivity occurs when the explorer makes contact with the exposed dentin. (B): Drawing of the area in (A) showing exposed dentin tubules. The attached gingiva, exposed dentin tubules, and enamel are labeled (not to scale). The yellow structures are nerve endings extending into the dentin tubules in close proximity to the odontoblast processes. The movement of liquid through the tubule elicits dentin hypersensitivity. (C): Drawing of an actual SEM image at high magnification of a section of exposed and demineralized human dentin showing two open dentin tubules. (D): Drawing of toothbrush application of hydroxyapatite toothpaste to the area in (A). (E): Drawing of the same area in (B) showing a layer of HAP toothpaste after one application. (F): After multiple uses, the entire dentin surface (in the before illustration in (C)) is covered with a layer of HAP. The dentin tubules are also occluded with HAP minerals. Both intact HAP molecules and ions from the dissociation of HAP contribute to the remineralization of the dentin surface, reducing dentin sensitivity. The HAP layer is stable with continued use of HAP toothpaste, producing a long-term reduction in dentin hypersensitivity.
The oral care products used in the studies listed in Table 1 varied in their synthetic HAP particle sizes. HAP is synthesized in various processes, which leads to a variety of particle dimensions. Most particles are micrometer in size, and can sometimes be measured in nanometer widths, as shown in many SEM studies in vitro. With dentin tubule width in the µm range (Figure 5), the small dimensions of the nano- and micro-HAP particles explain how they can accumulate in the dentin tubules and eventually occlude them, reducing dentin hypersensitivity. Specific crystal morphology and size have not been studied in detail to determine what the optimum dimensions for biomimetic HAP should be for dentin tubule occlusion and dentin adherence.
4.2. Strength of Evidence and Results of the Meta-Analysis
Our meta-analysis clearly demonstrates that there are many well-conducted clinical studies that show a significant lowering of DH in patients who report (or test positive for) hypersensitive teeth due mainly to exposed root surfaces after gingival recession. Overall, a significant reduction of 39.5% (CI 95% [48.93; 30.06]) can be expected when HAP toothpaste is used exclusively for a few weeks, compared to the placebo. Evidence from well-conducted clinical trials that HAP is an effective dentin desensitizer comes from many studies already published and reviewed (see Supplementary Material Table S1, which contains recent systematic reviews). We have updated the literature in the present systematic review and meta-analysis, having found 44 clinical trials on HAP in oral care products to desensitize sensitive teeth. Our meta-analysis of 22 RCTs is the most up-to-date quantitative synthesis of the evidence, indicating that HAP is an effective dentin desensitizer.
Enax et al. [72] reviewed the safety of calcium phosphates, including biomimetic HAP, and it was concluded that HAP can be safely swallowed when used in oral care products. However, most subjects expectorate and rinse after using their toothpaste. Toothpastes are not the only method of applying HAP to sensitive teeth. At home custom tray application can be a method of application. Leaving the HAP in contact with exposed dentin for longer periods of time may increase its efficacy, but more RCTs are required to determine if this is truly the case. The use of HAP products in patients after vital bleaching or periodontal therapy, whitening teeth with carbamide peroxides either professionally, or with home use products, can increase dentin hypersensitivity [73]. Even though the hypersensitivity is transient and thought to be the result of inflammation of the pulp, designers of in-office vital bleaching gels are testing whether the addition of HAP to their products can reduce after-treatment DH [74]. Those patients who have already experienced exposed dentin before bleaching could benefit from using HAP gels and toothpastes.
There were 11 clinical trials in which the test HAP-containing product was applied professionally by the clinician. In some of those studies, the product applied (a toothpaste) was also used at home. Apart from one study [20], the trials involving professional application were not included in the meta-analysis because the data from these studies were not comparable. However, all studies where HAP was professionally applied showed a benefit of using HAP-products as professional (in-office) treatment with respect to reducing DH [23,24,25,31,35,39,47,49,60]. Patients with exposed dentin may have very uncomfortable hypersensitivity after vigorous periodontal therapy (root planing) or after periodontal surgery [75]. The studies we found showed that patients can be helped after their periodontal surgery to manage dentin hypersensitivity when their root surfaces have been exposed.
4.3. Enhancing HAP Efficiency
There is some evidence that adding other elements to HAP might improve its ability to occlude dentin tubules and provide more stability to deposited crystals. Examples include Zn, Mg, and both [76]. Fluoride is thought to promote the remineralization potential of tubules, and fortifying fluoride toothpastes with HAP to improve the desensitizing potential of fluoride is a strategy that has not been fully tested. Novamin (calcium sodium phosphosilicate) added to fluoride toothpaste seems to be an effective strategy [77], but the evidence suggests that HAP outperforms other methods of desensitization [13].
4.4. Additional Studies
After our search was completed, 4 additional studies appeared in the literature that were not included in this qualitative or quantitative synthesis [78,79,80,81]. These studies were consistent with HAP in reducing dentin hypersensitivity. In all, 48 trials have been published examining the effectiveness of HAP as a dentin-desensitizing additive in oral care products.
4.5. HAP Toothpaste Approved for Use in Canada
Government regulatory agencies have strict regulations for making claims on toothpaste packaging. Without clinical evidence, claims of dentin desensitizing cannot be made. In Canada, a number of toothpastes have received permission from Health Canada to be sold with claims to treat sensitive teeth. See Table S3 in the Supplementary Materials for this list and their characteristics.
5. Conclusions
Based on this systematic review and up-to-date meta-analysis, it can be concluded that hydroxyapatite is a safe biomimetic ingredient in oral care products for the reduction of dentin hypersensitivity, in addition to its already demonstrated anti-caries effects. Dental professionals can consider recommending hydroxyapatite-based oral care products as a primary strategy for the effective management of dentin hypersensitivity, which provides their patients with immediate and long-lasting relief from the dental pain caused by dentin hypersensitivity.
Acknowledgments
The authors wish to thank Kevin Limeback, BSc, BEd, for help with the design and artwork of Figure 5.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biomimetics8010023/s1, Table S1: Previous systematic reviews on DH; Table S2: Search details; Table S3: Health Canada approved HAP toothpastes for DH; PRISMA checklist.
Author Contributions
Conceptualization: H.L., J.E. and F.M.; methodology, H.L., J.E. and F.M.; literature search, qualitative synthesis, H.L.; validation of qualitative synthesis, J.E. and F.M.; meta-analysis data extraction and forest plots, F.M.; illustrations, original draft preparation, H.L.; editing, H.L., J.E. and F.M.; supervision, corresponding author, H.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
J.E. and F.M. are senior scientists and employees of Dr. Kurt Wolff GmbH & Co. KG in Germany.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Holland G.R., Narhi M.N., Addy M., Gangarosa L., Orchardson R. Guidelines for the design and conduct of clinical trials on dentine hypersensitivity. J. Clin. Periodontol. 1997;24:808–813. doi: 10.1111/j.1600-051X.1997.tb01194.x. [DOI] [PubMed] [Google Scholar]
- 2.Canadian Advisory Board on Dentin Hypersensitivity Consensus-based recommendations for the diagnosis and management of dentin hypersensitivity. J. Can. Dent. Assoc. 2003;4:221–226. [PubMed] [Google Scholar]
- 3.Liu X.X., Tenenbaum H.C., Wilder R.S., Quock R., Hewlett E.R., Ren Y.F. Pathogenesis, diagnosis and management of dentin hypersensitivity: An evidence-based overview for dental practitioners. BMC Oral. Health. 2020;20:220. doi: 10.1186/s12903-020-01199-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brannstrom M., Astrom A. The hydrodynamics of dentin and its possible relationship to dentinal pain. Int. Dent. J. 1972;22:219–227. [PubMed] [Google Scholar]
- 5.West N., Seong J., Davies M. Dentine hypersensitivity. Monogr Oral Sci. 2014;25:108–122. doi: 10.1159/000360749. [DOI] [PubMed] [Google Scholar]
- 6.Zeola F.L., Soares P.V., Cunha-Cruz J. Prevalence of dentin hypersensitivity: Systematic review and meta-analysis. J. Dent. 2019;81:1–6. doi: 10.1016/j.jdent.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 7.Clark D., Levin L. Non-surgical management of tooth hypersensitivity. Int. Dent. J. 2016;66:249–256. doi: 10.1111/idj.12247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moraschini V., da Costa L.S., Dos Santos G.O. Effectiveness for dentin hypersensitivity treatment of non-carious cervical lesions: A meta-analysis. Clin. Oral. Investig. 2018;2:617–631. doi: 10.1007/s00784-017-2330-9. [DOI] [PubMed] [Google Scholar]
- 9.Hu M.L., Zheng G., Zhang Y.D., Yan X., Li X.C., Lin H. Effect of desensitizing toothpastes on dentine hypersensitivity: A systematic review and meta-analysis. J. Dent. 2018;75:12–21. doi: 10.1016/j.jdent.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 10.Gul H., Ghaffar M.A., Kaleem M., Khan A.S. Hydroxyapatite, a potent agent to reduce dentin hypersensitivity. J. Pak. Med. Assoc. 2021;71:2604–2610. doi: 10.47391/JPMA.01175. [DOI] [PubMed] [Google Scholar]
- 11.Alencar de Melo C., de Paula B.L.F., Guanipa Ortiz M.I., Baraúna Magno M., Martins Silva C., Cople Maia L. Clinical efficacy of nano-hydroxyapatite in dentin hypersensitivity: A systematic review and meta-analysis. J. Dent. 2019;82:11–21. doi: 10.1016/j.jdent.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Marto C.M., Baptista P.A., Nunes T., Pimenta M., Abrantes A.M., Pires A.S., Laranjo M., Carrilho A., Donato H., Botleho M.F., et al. Evaluation of the efficacy of dentin hypersensitivity treatments-A systematic review and follow-up analysis. J. Oral. Rehabil. 2019;46:952–990. doi: 10.1111/joor.12842. [DOI] [PubMed] [Google Scholar]
- 13.Hu M.L., Zheng G., Lin H., Yang M., Zhang Y.D., Han J.M. Network meta-analysis on the effect of desensitizing toothpastes on dentine hypersensitivity. J. Dent. 2019;88:103170. doi: 10.1016/j.jdent.2019.07.008. [DOI] [PubMed] [Google Scholar]
- 14.Martins C.C., Firmino R.T., Riva J.J., Ge L., Carrasco-Labra A., Brignardello-Petersen R., Colunga-Lozano L.E., Granville-Garcia A.F., Costa F.O., Yepes-Nuñez J.J., et al. Desensitizing Toothpastes for Dentin Hypersensitivity: A Network Meta-analysis. J. Dent. Res. 2020;99:514–522. doi: 10.1177/0022034520903036. [DOI] [PubMed] [Google Scholar]
- 15.Oubenyahya H. Nano hydroxyapatite toothpaste as a treatment for dentine hypersensitivity: A systematic review. Saudi. J. Oral. Sci. 2021;8:122. doi: 10.4103/sjoralsci.sjoralsci_27_21. [DOI] [Google Scholar]
- 16.O’Hagan-Wong K., Enax J., Meyer F., Ganss B. The use of hydroxyapatite toothpaste to prevent dental caries. Odontology. 2022;110:223–230. doi: 10.1007/s10266-021-00675-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rethlefsen M.L., Kirtley S., Waffenschmidt S., Ayala A.P., Moher D., Page M.J., Koffel J.B. PRISMA-S: An extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst. Rev. 2021;10:39. doi: 10.1186/s13643-020-01542-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Limeback H., Enax J., Meyer F. Biomimetic hydroxyapatite and caries prevention: A systematic review and meta-analysis. Can. J. Dent. Hyg. 2021;55:148–159. [PMC free article] [PubMed] [Google Scholar]
- 19.Richards D. Rating the quality of evidence in evidence-based dentistry. Evid. Based Dent. 2019;20:32–33. doi: 10.1038/s41432-019-0008-7. [DOI] [PubMed] [Google Scholar]
- 20.Sterne J.A.C., Savovi J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Cates C.J., Cheng H.Y., Corbett M.S., Eldridge S.M., et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 21.Wickham H., François F., Henry L., Müller K. Dplyr: A Grammar of Data Manipulation. R package version 0.7.6. [(accessed on 15 June 2022)]. Available online: https://CRAN.R-project.org/package=dplyr.
- 22.Al Asmari D., Khan M.K. Evaluate efficacy of desensitizing toothpaste containing zinc-carbonate hydroxyapatite nanocrystals: Non-comparative eight-week clinical study. J. Int. Soc. Prev. Community Dent. 2019;9:566–570. doi: 10.4103/jispcd.JISPCD_261_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alencar C.D., Ortiz M.I., Silva F.A., Alves E.B., Araújo J.L., Silva C.M. Effect of nanohydroxyapatite associated with photobiomodulation in the control of dentin hypersensitivity: A randomized, double-blind, placebo-controlled clinical trial. Am. J. Dent. 2020;33:138–144. [PubMed] [Google Scholar]
- 24.Alharith D.N., Al-Omari M., Almnea R., Basri R., Alshehri A.H., Al-Nufiee A.A. Clinical efficacy of single application of plain nano-hydroxyapatite paste in reducing dentine hypersensitivity–A randomized clinical trial. Saudi. Endod. J. 2021;11:24–30. [Google Scholar]
- 25.Alsen W., Barngkgei I., Dayoub S. Evaluation of desensitizing efficacy of nanohydroxyapatite on the treatment of dentine hypersensitivity following ultrasonic scaling: A randomized controlled trial. Braz. Dent. Sci. 2022;25:e2737. doi: 10.4322/bds.2022.e2737. [DOI] [Google Scholar]
- 26.Amaechi B.T., Lemke K.C., Saha S., Gelfond J. Clinical efficacy in relieving dentin hypersensitivity of nanohydroxyapatite-containing cream: A randomized controlled trial. Open Dent. J. 2018;12:572–585. doi: 10.2174/1874210601812010572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amaechi B.T., Lemke K.C., Saha S., Luong M.N., Gelfond J. Clinical efficacy of nanohydroxyapatite-containing toothpaste at relieving dentin hypersensitivity: An 8 weeks randomized control trial. BDJ Open. 2021;7:23. doi: 10.1038/s41405-021-00080-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amin M., Mehta R., Duseja S., Desai K. Evaluation of the efficacy of comercially available nano hydroxypatite paste (Aclaim) as a desensitizing agent. Adv. Human Biol. 2015;5:34–38. [Google Scholar]
- 29.Anand S., Rejula F., Sam J.V.G., Christaline R., Nair M.G., Dinakaran S. Comparative evaluation of effect of nano-hydroxyapatite and 8% arginine containing toothpastes in managing dentin hypersensitivity: Double blind randomized clinical trial. Acta Medica. 2017;60:114–119. doi: 10.14712/18059694.2018.3. [DOI] [PubMed] [Google Scholar]
- 30.Barone M., Malpassi M. Clinical trial of a 15% supermicronized hydroxyapatite gel for dentin hypersensitivity. G. Ital. Endod. 1991;5:43–47. [PubMed] [Google Scholar]
- 31.Bevilacqua F.M., Catelan A., Araújo G.S.A., Saraceni C.H.C., Sampaio J.E.C. Efficacy of a bioactive material and nanostructured desensitizing (Nano-hydroxyapatite associated with 9000 ppm SF and 5% PN) on dentin hypersensitivity treatment. Rev. Odontol. UNESP. 2016;45:127–131. doi: 10.1590/1807-2577.24115. [DOI] [Google Scholar]
- 32.Browning W.D., Cho S.D., Deschepper E.J. Effect of a nano-hydroxyapatite paste on bleaching-related tooth sensitivity. J. Esthet. Restor. Dent. 2012;24:268–276. doi: 10.1111/j.1708-8240.2011.00437.x. [DOI] [PubMed] [Google Scholar]
- 33.Choi Y.H., Park H.C., Lee S.M., Son H.J., Choi E.B., Ha J.Y., Lee J.Y., Kim K.K. Therapeutic effect of toothpaste containing hydroxyapatite and tribasic calcium phosphate on dentinal hypersensitivity. J. Life Sci. 2014;24:642–647. doi: 10.5352/JLS.2014.24.6.642. [DOI] [Google Scholar]
- 34.da Silva R.C., Alencar C.M., Silva B.H.R., de Paula B.L.F., Barros A.P.O., da Silveira A.D.S., Silva C.M. A clinical, randomised, double-blind study on the use of nano-hydroxyapatite and arginine during at-home tooth bleaching. J. Clin. Diag. Res. 2018;12:ZC01–ZC05. doi: 10.7860/JCDR/2018/37325.12340. [DOI] [Google Scholar]
- 35.Douglas-de-Oliveira D.W., Oliveira E.S., Mota A.F., Pereira V.H., Bastos V.O., Glória J.C., Gonçalves P.F., Flecha O.D. Effectiveness of three desensitizing dentifrices on cervical dentin hypersensitivity: A Pilot Clinical Trial. J. Int. Acad Periodontol. 2016;18:57–65. [PubMed] [Google Scholar]
- 36.Ding P.H., Dai A., Hu H.J., Huang J.P., Liu J.M., Chen L.L. Efficacy of nano-carbonate apatite dentifrice in relief from dentine hypersensitivity following non-surgical periodontal therapy: A randomized controlled trial. BMC Oral. Health. 2020;20:170. doi: 10.1186/s12903-020-01157-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ehlers V., Reuter A.K., Kehl E.B., Enax J., Meyer F., Schlecht J., Schmidtmann I., Deschner J. Efficacy of a toothpaste based on microcrystalline hydroxyapatite on children with hypersensitivity caused by MIH: A randomised controlled trial. Oral. Health Prev. Dent. 2021;19:647–658. doi: 10.3290/j.ohpd.b2403649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gopinath N.M., John J., Nagappan N., Prabhu S., Kumar E.S. Evaluation of dentifrice containing nano-hydroxyapatite for dentinal hypersensitivity: A randomized controlled trial. J. Int. Oral. Health. 2015;7:118–122. [PMC free article] [PubMed] [Google Scholar]
- 39.Gümüştaş B., Dikmen B. Effectiveness of remineralization agents on the prevention of dental bleaching induced sensitivity: A randomized clinical trial. Int. J. Dent. Hyg. 2021;20:1–8. doi: 10.1111/idh.12524. [DOI] [PubMed] [Google Scholar]
- 40.Hüttemann R.W., Dönges H. Investigations for treating hypersensitive necks of teeth with hydroxyapatite. Dtsch Zahnärztl Z. 1987;42:486–488. [PubMed] [Google Scholar]
- 41.Jena A., Shashirekha G. Comparison of efficacy of three different desensitizing agents for in-office relief of dentin hypersensitivity: A 4 weeks clinical study. J. Conserv. Dent. 2015;18:389–393. doi: 10.4103/0972-0707.164052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kang S.J., Kwon Y.H., Park J.B., Herr Y., Chung J.H. The effects of hydroxyapatite toothpaste on tooth hypersensitivity. J. Korean Acad. Periodontol. 2009;39:9–16. doi: 10.5051/jkape.2009.39.1.9. [DOI] [Google Scholar]
- 43.Kim M.S., Chae G.J., Choi S.H., Chai J.K., Kim C.K., Cho K.S. Effect of hydroxyapatite containing dentifrice on teeth hypersensitivity after periodontal therapy. J. Korean Acad. Periodontol. 2008;38:1–6. doi: 10.5051/jkape.2008.38.1.1. [DOI] [Google Scholar]
- 44.Kim S.H., Park J.B., Lee C.W., Koo K.T., Kim T.I., Seol Y.J., Lee Y.M., Ku Y., Chung C.P., Rhyu I.C. The clinical effects of a hydroxyapatite containing toothpaste for dentine hypersensitivity. J. Korean Acad. Periodontol. 2009;39:87–94. doi: 10.5051/jkape.2009.39.1.87. [DOI] [Google Scholar]
- 45.Kondyurova E.V., Lisevtsova J.V., Eliseykina E.V., Vilikotskiy A.E., Zakirova S.A. Clinical evaluation of a dentifrice containing Nhap for the reduction of dentin hypersensitivity. Int. J. Oral. Dent. Health. 2019;5:104. doi: 10.23937/2469-5734/1510104. [DOI] [Google Scholar]
- 46.Lee S.-Y., Jung H.-I., Jung B.-Y., Cho Y.-S., Kwon H.-K., Kim B.-I. Desensitizing efficacy of nano-carbonate apatite dentifrice and Er,Cr:YSGG laser:A randomized clinical trial. Photomed. Laser Surg. 2015;33:9–14. doi: 10.1089/pho.2014.3787. [DOI] [PubMed] [Google Scholar]
- 47.Loguercio A.D., Tay L.Y., Herrera D.R., Bauer J., Reis A. Effectiveness of nano-calcium phosphate paste on sensitivity during and after bleaching: A randomized clinical trial. Braz. Oral. Res. 2015;29:1–7. doi: 10.1590/1807-3107BOR-2015.vol29.0099. [DOI] [PubMed] [Google Scholar]
- 48.Low S.B., Allen E.P., Kontogiorgos E.D. Reduction in dental hypersensitivity with nano-hydroxyapatite, potassium nitrate, sodium monoflurophosphate and antioxidants. Open Dent. J. 2015;9:92–97. doi: 10.2174/1874364101509010092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maharani D.A. Efficacy of a commercially available hydroxyapatite-containing toothpaste in reducing dentin hypersensitivity. Int. J. Clin. Prev. Dent. 2012;8:151–154. [Google Scholar]
- 50.Makeeva I.M., Polyakova M.A., Avdeenko O.E., Paramonov Y.O., Kondrati’ev S.A., Pilyagina A.A. Evaluation of the effectiveness of long-term use of Apadent Total Care toothpaste containing medical nano-hydroxyapatite. Stomatologii. 2016;95:34–36. doi: 10.17116/stomat201695434-36. [DOI] [PubMed] [Google Scholar]
- 51.Makeeva I.M., Polyakova M.A., Doroshina V.Y., Sokhova I.A., Arakelyan M.G., Makeeva M.K. Efficiency of paste and suspension with nano-hydroxyapatite on the sensitivity of teeth with gingival recession. Stomatologiia. 2018;97:23–27. doi: 10.17116/stomat20189704123. [DOI] [PubMed] [Google Scholar]
- 52.Orsini G., Procaccini M., Manzoli L., Giuliodori F., Lorenzini A., Putignano A. A double-blind randomized-controlled trial comparing the desensitizing efficacy of a new dentifrice containing carbonate/hydroxyapatite nanocrystals and a sodium fluoride/potassium nitrate dentifrice. J. Clin. Periodontol. 2010;37:510–517. doi: 10.1111/j.1600-051X.2010.01558.x. [DOI] [PubMed] [Google Scholar]
- 53.Orsini G., Procaccini M., Manzoli L., Sparabombe S., Tiriduzzi P., Bambini F., Putignano A. A 3-day randomized clinical trial to investigate the desensitizing properties of three dentifrices. J. Periodontol. 2013;84:e65–e73. doi: 10.1902/jop.2013.120697. [DOI] [PubMed] [Google Scholar]
- 54.Park J.J., Park J.B., Kwon Y.H., Herr Y., Chung J.H. The effects of microcrystalline hydroxyapatite containing toothpaste in the control of tooth hypersensitivity. J. Korean Acad. Periodontol. 2005;35:577–590. doi: 10.5051/jkape.2005.35.3.577. [DOI] [Google Scholar]
- 55.Pinojj A., Shetty A., Shetty D., Shetty S. A comparison of clinical efficacy of dentifrices containing calcium sodium phosphosilicate, nanoparticle hydroxyapatite and a dentifrice containing casein phosphopeptide amorphous calcium phosphate on dentinal hypersensitivity: A comparative triple blind randomized study. Adv. Hum. Biol. 2014;4:57–64. [Google Scholar]
- 56.Polyakova M., Sokhova I., Doroshina V., Arakelyan M., Novozhilova N., Babina K. The effect of toothpastes containing hydroxyapatite, fluoroapatite, and Zn-Mg-hydroxyapatite nanocrystals on dentin hypersensitivity: A randomized clinical trial. J. Internat Soc. Prev. Commun. Dent. 2022;12:252. doi: 10.4103/jispcd.JISPCD_333_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Porciani P.F., Chazine M., Grandini S. A clinical study of the efficacy of a new chewing gum containing calcium hydroxyapatite in reducing dentin hypersensitivity. J. Clin. Dent. 2014;25:32–36. [PubMed] [Google Scholar]
- 58.Reddy S., Prasad M.G.S., Prasad S., Bhowmik N., Ashwini N., Sravya L., Singh S. The effect of pro-argin technology vs nano technology using commercially available dentifrice: A comparative study. Int. J. Appl. Dent. Sci. 2014;1:26–30. [Google Scholar]
- 59.Seong J., Newcombe R.G., Foskett H.L., Davies M., West N.X. A randomised controlled trial to compare the efficacy of an aluminium lactate/potassium nitrate/hydroxylapatite toothpaste with a control toothpaste for the prevention of dentine hypersensitivity. J. Dent. 2021;108:103619. doi: 10.1016/j.jdent.2021.103619. [DOI] [PubMed] [Google Scholar]
- 60.Shetty S., Kohad R., Yeltiwar R. Hydroxyapatite as an in-office agent for tooth hypersensitivity: A clinical and scanning electron microscopic study. J. Periodontol. 2010;81:1781–1789. doi: 10.1902/jop.2010.100172. [DOI] [PubMed] [Google Scholar]
- 61.Vano M., Derchi G., Barone A., Covani U. Effectiveness of nano-hydroxyapatite toothpaste in reducing dentin hypersensitivity: A double-blind randomized controlled trial. Quintessence Internat. 2014;45:703–710. doi: 10.3290/j.qi.a32240. [DOI] [PubMed] [Google Scholar]
- 62.Vano M., Derchi G., Barone A., Genoves A., Covani U. Tooth bleaching with hydrogen peroxide and nano-hydroxyapatite: A 9-month follow-up randomized clinical trial. Int. J. Dent. Hygiene. 2015;13:301–307. doi: 10.1111/idh.12123. [DOI] [PubMed] [Google Scholar]
- 63.Vano M., Derchi G., Barone A., Pinna R., Usai P., Covani U. Reducing dentine hypersensitivity with nano-hydroxyapatite toothpaste: A double-blind randomized controlled trial. Clin. Oral. Investig. 2018;22:313–320. doi: 10.1007/s00784-017-2113-3. [DOI] [PubMed] [Google Scholar]
- 64.Narmatha V.J., Thakur S. An in-vivo comparative study of the efficacy of Propolis, nano-hydroxyapatite and potassium nitrate-containingdesensitizing agents. RRJDS. 2014;2:113–118. [Google Scholar]
- 65.Wang L., Magalhães A.C., Francisconi-Dos-Rios L.F., Calabria M.P., Araújo D.F., Buzalaf M.A., Lauris J.R., Pereira J.C. Treatment of dentin hypersensitivity using nano-hydroxyapatite pastes: A randomized three-month clinical trial. Oper. Dent. 2016;41:E93–E101. doi: 10.2341/15-145-C. [DOI] [PubMed] [Google Scholar]
- 66.Schiff T., Dotson M., Cohen S., De Vizio W., McCool J., Volpe A. Efficacy of a dentifrice containing potassium nitrate, soluble pyrophosphate, PVM/MA copolymer, and sodium fluoride on dentinal hypersensitivity: A twelve-week clinical study. J. Clin. Dent. 1994;5:87–92. [PubMed] [Google Scholar]
- 67.Chambers C.T., Giesbrecht K., Craig K.D., Bennett S.M., Huntsman E. A comparison of faces scales for the measurement of pediatric pain: Children’s and parents’ ratings. Pain. 1999;83:25–35. doi: 10.1016/S0304-3959(99)00086-X. [DOI] [PubMed] [Google Scholar]
- 68.Chen L., Al-Bayatee S., Khurshid Z., Shavandi A., Brunton P., Ratnayake J. Hydroxyapatite in oral care products-A review. Materials. 2021;14:4865. doi: 10.3390/ma14174865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pashley D.H. Dentin permeability, dentin sensitivity, and treatment through tubule occlusion. J Endod. 1986;12:465–474. doi: 10.1016/S0099-2399(86)80201-1. [DOI] [PubMed] [Google Scholar]
- 70.Cieplik F., Rupp C.M., Hirsch S., Muehler D., Enax J., Meyer F., Hiller K.-A., Buchalla W. Ca2+ release and buffering effects of synthetic hydroxyapatite following bacterial acid challenge. BMC Oral Health. 2020;20:85. doi: 10.1186/s12903-020-01080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Enax J., Fabritius H.-O., Fabritius-Vilpoux K., Amaechi B.T., Meyer F. Modes of action and clinical efficacy of particulate hydroxyapatite in preventive oral health care − state of the art. Open Dent. J. 2019;13:274–287. doi: 10.2174/1874210601913010274. [DOI] [Google Scholar]
- 72.Enax J., Meyer F., Schulze zur Wiesche E., Epple M. On the application of calcium phosphate micro- and nanoparticles as food additive. Nanobiomaterials. 2022;12:4075. doi: 10.3390/nano12224075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Maran B.M., Matos T.P., de Castro A.D.S., Vochikovski L., Amadori A.L., Loguercio A.D., Reis A., Berger S.B. In-office bleaching with low/medium vs. high concentrate hydrogen peroxide: A systematic review and meta-analysis. J. Dent. 2020;103:103499. doi: 10.1016/j.jdent.2020.103499. [DOI] [PubMed] [Google Scholar]
- 74.Orilisi G., Tosco V., Monterubbianesi R., Notarstefano V., Özcan M., Putignano A., Orsini G. ATR-FTIR, EDS and SEM evaluations of enamel structure after treatment with hydrogen peroxide bleaching agents loaded with nano-hydroxyapatite particles. PeerJ. 2021;29:e10606. doi: 10.7717/peerj.10606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Canakçi C.F., Canakçi V. Pain experienced by patients undergoing different periodontal therapies. J. Am. Dent. Assoc. 2007;12:1563–1573. doi: 10.14219/jada.archive.2007.0105. [DOI] [PubMed] [Google Scholar]
- 76.Saad A., Nikaido T., Abdou A., Matin K., Burrow M.F., Tagami J. Inhibitory effect of zinc-containing desensitizer on bacterial biofilm formation and root dentin demineralization. Dent. Mater. J. 2019;38:940–946. doi: 10.4012/dmj.2018-352. [DOI] [PubMed] [Google Scholar]
- 77.Amaechi B.T., Mathews S.M., Ramalingam K., Mensinkai P.K. Evaluation of nanohydroxyapatite-containing toothpaste for occluding dentin tubules. Am. J. Dent. 2015;28:33–39. [PubMed] [Google Scholar]
- 78.Butera A., Gallo S., Pascadopoli M., Montasser M.A., Abd El Latief M.H., Modica G.G., Scribante A. Home oral care with biomimetic hydroxyapatite vs. conventional fluoridated toothpaste for the remineralization and desensitizing of white spot lesions: Randomized clinical trial. Int. J. Environ. Res. Public Health. 2022;19:8676. doi: 10.3390/ijerph19148676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moharam L.M., Khadr S., Abdou A., Nagi S.M. Effect of arginine and nano-hydroxyapatite application on the hypersensitivity and color change of bleached enamel: A randomized controlled clinical trial. J. Clin. Exp. Dent. 2022;14:e499–e505. doi: 10.4317/jced.59423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vlasova N., Samusenkov V., Novikova I., Nikolenko D., Nikolashvili N., Gor I., Danilina A. Clinical efficacy of hydroxyapatite toothpaste containing Polyol Germanium Complex (PGC) with threonine in the treatment of dentine hypersensitivity. Saudi. Dent. J. 2022;34:310–314. doi: 10.1016/j.sdentj.2022.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Butera A., Pascadopoli M., Pellegrini M., Trapani B., Gallo S., Radu M., Scribante A. Biomimetic hydroxyapatite paste for molar-incisor hypomineralization: A randomized clinical trial. Oral. Dis. 2022:1–10. doi: 10.1111/odi.14388. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.