Abstract
Stroke remains the second leading cause of global disability with 87% of stroke-related disability occurring in low- and middle-income countries (LMICs). In LMIC countries, access to acute stroke interventions is often limited, making effective post-stroke rehabilitation potentially the best available intervention to promote post-stroke recovery. Here, we build on our experience as an illustrative example of barriers individuals with stroke face in accessing rehabilitation services and review the literature to summarize challenges to providing effective rehabilitation in LMICs. First, we focus on barriers individuals with stroke face in accessing rehabilitation in LMICs, including health system barriers, such as lack of national guidelines, low prioritization of rehabilitation services, and inadequate numbers of skilled rehabilitation specialists, as well as patient factors, including limited health literacy, financial constraints and transportation limitations. Next, we highlight consequences of this lack of rehabilitation access, including higher mortality, poorer functional outcomes, financial burden, caregiver stress, and loss of gross domestic product at a national level. Finally, we review possible strategies that could improve access and quality of rehabilitation services in LMICs, including creation of inpatient stroke units, increased training opportunities for rehabilitation specialists, task-shifting to available healthcare workers or caregivers, telerehabilitation, and community-based rehabilitation services.
Keywords: Stroke, rehabilitation, low- and middle-income countries, post-stroke rehabilitation, rehabilitation services
INTRODUCTION
Stroke is the second leading cause of disability and mortality worldwide, and 87% of stroke-related disability occurs in low- and middle-income countries (LMICs).1 This burden is further exacerbated by the lack of rehabilitation experts in many regions of the world. On average, LMICs have just 10 total skilled rehabilitation experts for every one million population whereas high-income countries average over 400 occupational therapists, 900 physical therapists, 400 speech therapists and 20 physical medicine and rehabilitation physicians per one million population (Figure 1).2 Overall, a survey by the World Stroke Organization found that specialized stroke rehabilitation services were present in only 18% of responding LMICs as compared to 91% of HICs, thus highlighting the dearth of rehabilitation opportunities available to individuals recovering from stroke in the majority of LMICs.3
Figure 1.
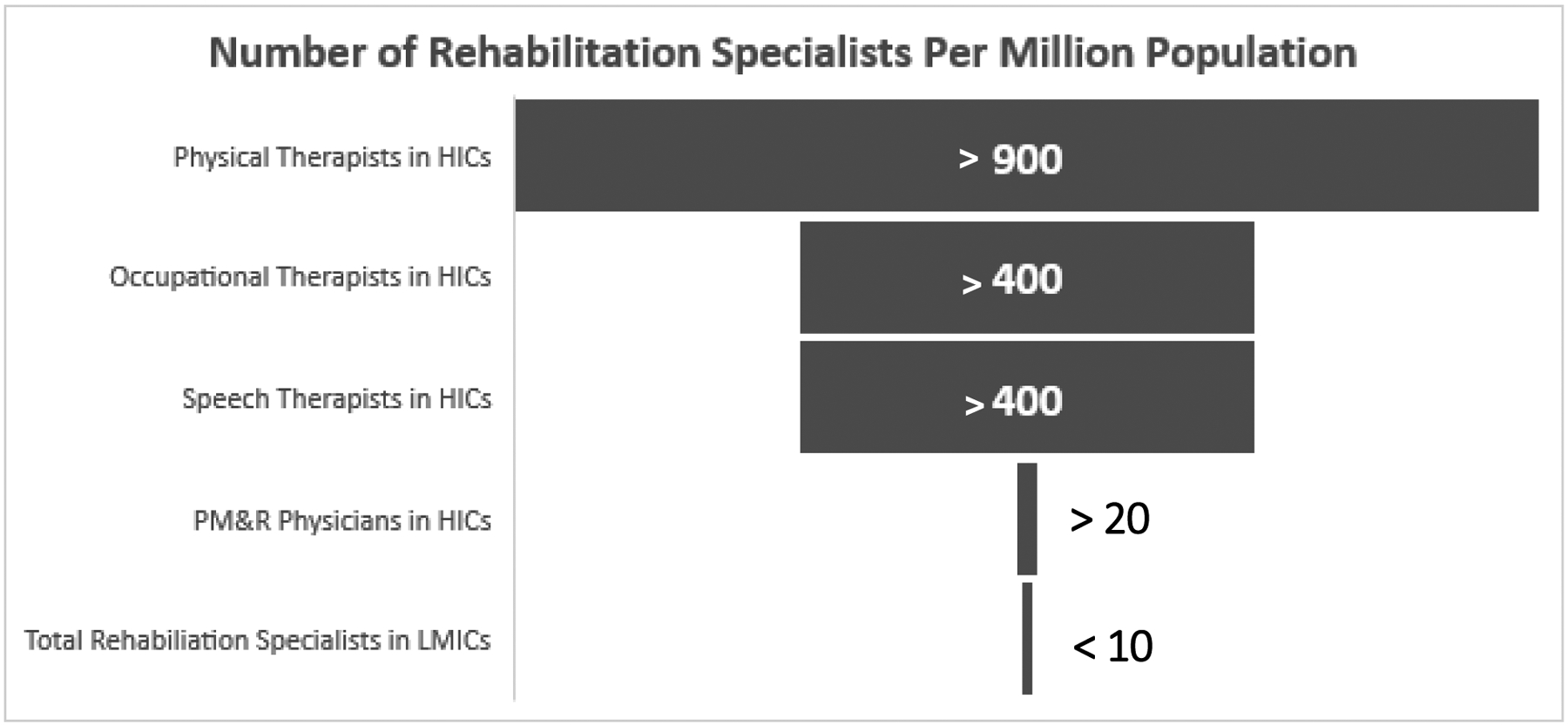
Estimated number of rehabilitation specialists per one million population in high-income countries (HICs) versus low- and middle-income countries (LMICs).2
Abbreviations: PM&R: physical medicine and rehabilitation.
The World Health Organization’s Rehabilitation 2030 Action Plan acknowledges how rehabilitation, the most effective method for improving long-term stroke outcomes after acute interventions, is an integral part of quality healthcare.4 While high-income countries (HICs) have a variety of options and skilled specialists for stroke rehabilitation, LMCIs do not, even though stroke incidence and fatalities are higher in LMICs than HICs. In this review, we discuss the current state of stroke rehabilitation services in LMICs using our experience in Zambia as an illustrative case and highlight barriers to rehabilitation and their consequences as well as opportunities for improving post-stroke rehabilitation (Table 1).
Table 1.
Overview of barriers and consequences of limited access to stroke rehabilitation services in low- and middle-income countries as well as potential opportunities to improve access to these services.
| Barriers |
|---|
Health Systems Factors
|
Individual Factors
|
| Consequences |
Individual Consequences
|
Caregiver Consequences
|
Population-Level/National Consequences
|
| Opportunities |
|
STROKE REHABILITATION FROM THE ZAMBIAN PERSPECTIVE
Patients with stroke in Zambia face a multitude of challenges on the road to recovery, beginning with limited access to rehabilitation services during their acute hospitalization for stroke. While most hospitals are staffed with physical therapists, their numbers are small and patient volume is high, such that any given patient may only be evaluated once or twice during their hospitalization. We prospectively studied rehabilitation services provided for adults hospitalized with stroke at the University Teaching Hospital, Zambia’s national referral hospital in the capital city of Lusaka over one year. In this cohort of 250 adults with stroke, only 27% (n=67) received any physical therapy evaluation during their hospitalization. Those that did receive rehabilitation services received only a median of 1 (interquartile range 1–2) sessions during their hospitalization (unpublished data). Of note, our hospital has only 33 physical therapists working in both the inpatient and outpatient settings of the children’s hospital, women and newborn hospital, and adult hospital housed on our campus. There are no physical medicine and rehabilitation doctors at our hospital or within Zambia. Furthremore, occupational therapists and speech therapists are nearly absent across Zambia, and none are employed at our hospital so these services are unavailable to patients hospitalized at our facility. Similar findings have been reported from other hospitals in the region, including a study at Kilimanjaro Christian Medical Center Hospital, the largest and highest volume healthcare facility in Tanzania, where only 47% of adults hospitalized with stroke received access to rehabilitation during their hospitalization, and speech therapy was entirely unavailable.5
After discharge, the vast majority of Zambian patients return directly home into the care of a family member who serves as an informal caregiver. Post-discharge inpatient rehabilitation facilities are not available in the public sector, and in-home nursing and rehabilitation services do not exist. Patients and their families often do not have the financial means to purchase ambulatory aids or wheelchairs and, thus, may be reliant on family members to physically carry them between locations. Private vehicles are a luxury meaning that many patients with limited mobility remain reliant on public transportation unequipped for individuals with disability. With the majority of the population living at least several kilometers from the nearest health facility, impaired mobility and the cost of transportation serve as further barriers to accessing post-discharge rehabilitative services.
In our cohort, only 33% of discharged patients with stroke were actively participating in physiotherapy at 90-days post-discharge, of whom 45% attended multiple sessions per week, 37% attended weekly sessions, 3% attended sessions every other week, and 16% attended monthly sessions. Among patients not receiving physiotherapy, barriers to participation identified were varied and multifactorial, including lack of referrals, distance to the nearest health facility with physiotherapy services, limited finances for transportation, and uncontrolled chronic diseases, such as hypertension, that rendered them unable to participate in therapy (unpublished data).
BARRIERS TO STROKE REHABILITATION IN LMICs
In this section, we highlight common barriers that stroke survivors in LMICs encounter when accessing rehabilitation services. As illustrated in Figure 2, these barriers are numerous, multifactorial, and occur at every step in the rehabilitation care pathway.
Figure 2.
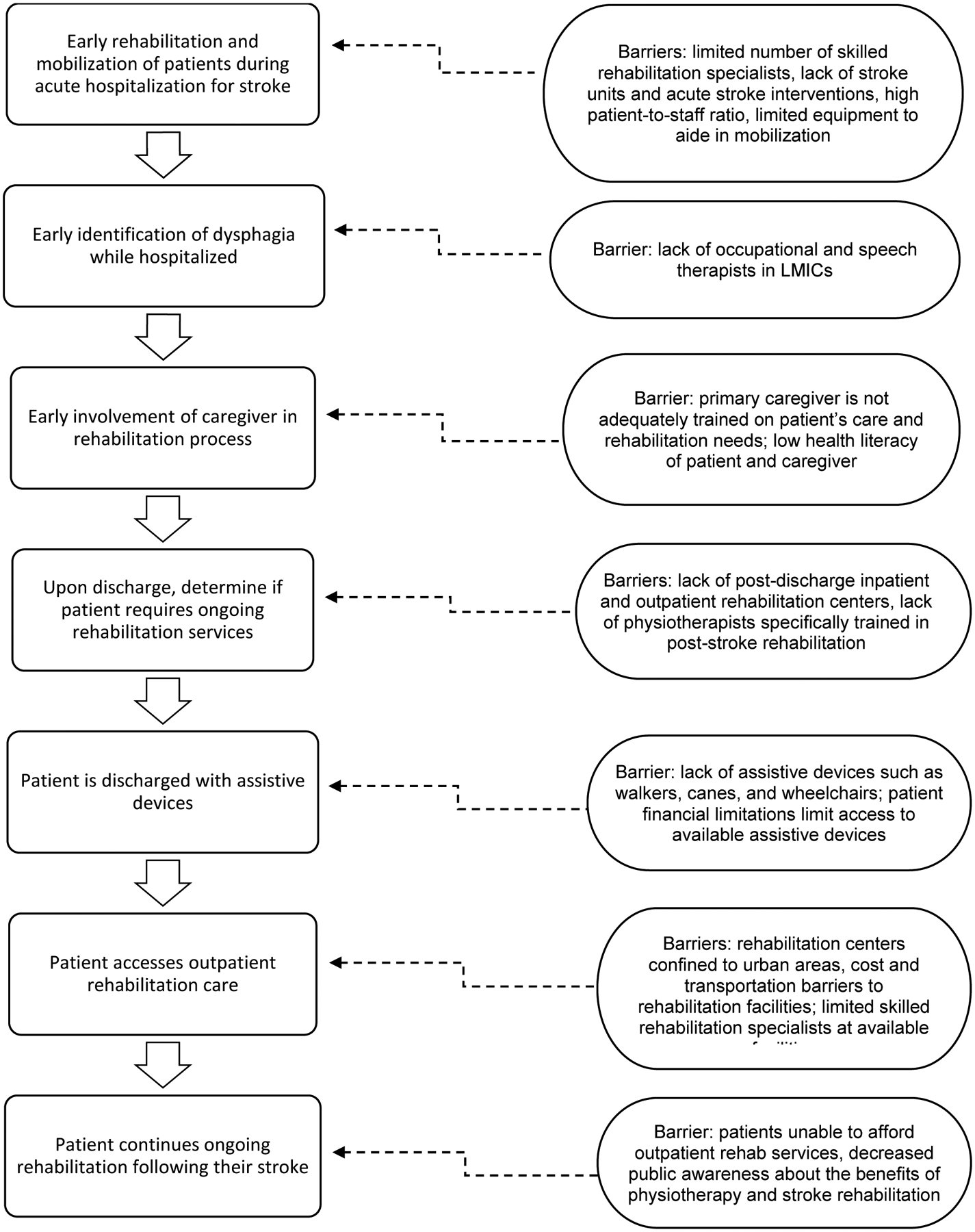
Pathway to stroke rehabilitation services and associated barriers. The left half of the figure demonstrates a typical patient pathway to accessing stroke rehabilitation services while the right half of the figure lists common barriers encountered at each step of the pathway.
Health Systems Factors
Barriers to accessing stroke rehabilitation in many LMICs begin with health systems-related factors. For example, most LMICs lack rehabilitation staff, especially those with specialized training in stroke recovery, and rehabilitation facilities are few, centered in urban areas, under-funded, and largely under-equipped.6, 7
Competing Health System Demands.
In addition to lack of rehabilitation specialists, competing healthcare demands in LMICs also leads to difficulty growing capacity for stroke rehabilitation. A study of healthcare providers’ priorities and their perceptions regarding the feasibility of implementing those priorities demonstrated that healthcare workers from HICs were in a better position to prioritize, facilitate and implement specialized stroke rehabilitation services while healthcare providers from LMICs were more supportive of the intensification of existing rehabilitation services, however vague, due to the expense associated with developing specialized services.8
Non-transferrable clinical practice guidelines.
Challenges with competing demands has been further illustrated in attempts to actualize stroke rehabilitation programs outside of HICs. Less than half of LMICs have guidelines and protocols on standards of care for stroke rehabilitation methods and frequency.3 However, several middle-income countries, including South Africa and the Philippines, have adopted stroke rehabilitation guidelines that were developed in HICs.9 Unfortunately, these proved difficult to implement in practice, primarily due to a lack of resources and especially in rural areas. As such, the approach of blanket implementation of stroke rehabilitation guidelines without adaptation to the local context and available resources is unlikely to be successful. Locally contextualized guidelines are needed for successful implementation of national stroke rehabilitation plans in LMICs.
Lack of facilities/equipment.
Even amongst those individuals with stroke who do access rehabilitation services in LMICs, the therapeutic modalities available to them are often very limited. A wide array of physical rehabilitation options that cater for specific stroke-related deficits exist in many HICs, ranging from motor skill exercises, mobility training, constraint-induced therapy and range of motion therapy to functional electrical stimulation, virtual reality or even robotic technology.10 Modalities also exist for cognitive and emotional rehabilitation. However, only a limited range of therapeutic options exist in most LMIC settings. A 2021 study of rehabilitation services across nine hospitals in one rural South African district found that patients’ needs were not met due to a lack of assistive devices that could be used for mobility training, such as walkers, canes, wheelchairs and ankle braces, resulting in very limited rehabilitation options and compromising patients’ recovery potential.11
Lack of stroke rehabilitation specialists.
Furthermore, rehabilitation therapists available in LMICs are more likely to have a multidisciplinary focus rather than a focus on stroke alone and to be entry-level therapists with limited experience, thus further compromising rehabilitation options available to individuals with stroke.8, 12 Ultimately, lack of specialized personnel and standardized overarching structures for rehabilitation services in combination with limited expertise for stroke rehabilitation and poor processes leads to poor quality services and, ultimately, poor patient outcomes.13
Severely limited resources in rural areas.
Furthermore, when present, stroke rehabilitation centers and services in LMICs are almost entirely limited to urban areas, though the majority of people in LMICs live in rural areas.7 Rural areas are served with primary level health facilities providing basic diagnostic and therapeutic healthcare and often serving large populations spread over long distances. These facilities are usually staffed by health personnel with no specific training in rehabilitation, often requiring patients in need of rehabilitation to be referred to higher level facilities. Rural healthcare facilities in LMICs also tend to be underfunded and are even less likely to have stroke rehabilitation therapists compared to more urban hospitals.14, 15 Finally, the rural communities are less attractive employment sites for physiotherapists and other needed rehabilitation specialists, making it unlikely that the human resource gap in rural areas will be closed in the near term.16
Poor upstream acute stroke care.
It is also important to note that most patients with stroke in LMICs lack access to acute stroke interventions that would result in improved long-term stroke outcomes, including intravenous tissue plasminogen activator and endovascular interventions, that result in improved long-term stroke outcomes.17 Stroke units, defined as standardized systems of primarily nursing-based care for patients with stroke, have resulted in significant improvement in functional outcomes in the settings where they have been implemented as well. These systems are associated with substantial reductions in death (odds ratio [OR] 0.87), death/dependency (OR 0.79), and death/institutionalized care (OR 0.78) independent of acute interventions.18 Unfortunately, stroke centers are also lacking in most LMICs, especially in sub-Saharan Africa.17 As a result, patients surviving their acute stroke hospitalization in LMICs are likely to have more substantial disability and functional impairment than their counterparts from HICs, thus increasing their needs for specialized rehabilitation services.
Patient Factors
In addition to barriers related to health systems factors, personal factors also substantially impact a stroke survivor’s ability to obtain necessary rehabilitation services. In Zambia and other sub-Saharan Africa settings, adult stroke survivors receive few inpatient and outpatient physical therapy sessions not only as a result of inadequate rehabilitation services, but also due to individual challenges such as insufficient finances, long distances to rehabilitation facilities, and lack of transportation.19
Limited Transportation Options.
For persons with stroke and other disabilities, transportation to and from health centers can be challenging. Small mini-buses, trucks, motorcycles and even boats and canoes make up some of the most common modes of transportation in most LMICs. Further, public transportation in most LMICs is poorly organized and does not specifically cater for persons with disability, thus limiting their overall mobility and ability to participate in rehabilitation activities at healthcare facilities.20 As a result, stroke survivors are often carried on the backs of caregivers to access health facilities in rural areas with limited transportation options.16 This is not safe nor sustainable where distances to health centers can be vast.
Even in more urban areas, poor access to assistive devices such as wheelchairs, crutches, and walking frames is limited for many patients due to financial constraints resulting in patients or their families having to improvise mobility assistance. For example, many patients resort to using sticks in the absence of canes which lack anti-slip properties and put them at significant risk of falls. Poor urban planning in many LMICs also means there is little consideration of the mobility needs for patients with disability. Lack of dedicated walkways, handrails, designated toilets and parking for persons with disabilities, and lack of access ramps all limit overall mobility of people with disability. Specifically, these factors limit access to physiotherapy and rehabilitation services for the people most in need of those services even when rehabilitation services are available.
Financial Constraints.
In addition to costs associated with transportation to rehabilitation facilities and assistive devices, individuals must also pay for rehabilitation sessions themselves. These costs are borne by the patient and their caregivers, as public options for medical aid and medical insurance are limited in most LMICs. The prolonged nature of rehabilitation makes the cumulative costs high, considering that many families in LMICs are living in extreme poverty (defined as living on less than $1.90 US dollar per day). Furthermore, many people in LMICs are day laborers, dependent on working each day in order to earn a daily wage. If a caregiver is required to attend rehabilitation sessions with the patient, this further results in loss of the caregiver’s daily wages as well.
Role of traditional medicine.
The use of herbal mediccations and traditional systems of care is common in LMICs. For example, 43% of stroke survivors in a Ghanaian study were found to have used herbal medicines after their stroke, often preferring these treatments due to beliefs that they will cure stroke, lead to faster recovery, and be more effective compared to conventional allopathic therapies.21 As such, accessing traditional systems of care may lead to reduced engagement in rehabilitation services.
Health literacy levels.
Low levels of health literacy and general education among many people in LMIC makes understanding stroke and the role of physiotherapy and rehabilitation difficult.22 Furthermore, many cultural groups in LMICs lack chronic disease models23 leading to the expectation amongst patients and their caregivers that stroke recovery is quick and complete. A failure to achieve that recovery then leads to a withdrawal from ongoing physiotherapy as there is no perceived short-term benefit while its associated costs continue to be high.
Lack of formal caregivers.
Because rehabilitation and skilled nursing facilities providing formal post-stroke care are limited in most LMICs, stroke survivors, especially in sub-Saharan Africa, are often informally cared for at home by family members, including parents, spouses, and children.6 These informal caregivers usually lack previous medical training in stroke care and rehabilitation and further lack health systems support such as visiting nurses or formal in-home medical aides. The sudden nature of stroke also means that caregivers have to learn an immense amount of very complicated information about the disease and its long-term effects over a short period of time. Unlike other medical conditions that allow a gradual transition to home-based care needs, the abrupt nature of stroke and a lack of post-discharge inpatient rehabilitation services means families and caregivers have a limited time to prepare to independently meet the complex care needs of stroke survivors in the home. Caregivers are thus scarcely educated or trained to assist stroke survivors’ in activities of daily living, turning or feeding mechanisms to prevent complications such as decubitus ulcers and aspiration pneumonia, or safe handling of assistive devices, if available.24, 25
IMPACT OF LIMITED ACCESS TO REHABILITATION SERVICES IN LMICs
Consequences to Individuals with Stroke
Poor stroke outcomes, exacerbated by the lack of rehabilitation services, result in a variety of challenges for many stroke survivors in LMICs, both physical and psychological. In the short-term, recovery of optimal motor function and independence in activities of daily living is best achieved in the days and weeks immediately following a stroke, with recovery in the majority of individuals that survive stroke reported to occur within the first 30 days to 12 weeks.10 A study in Nigeria showed a shorter length of acute stroke hospitalization in patients with higher rate of in-patient physiotherapy utilization.26 Rehabilitative measures such as early mobilization have also been shown to reduce the occurrence of immobility-associated in-hospital complications, including, deep vein thrombosis, aspiration pneumonia, contractures, and decubitus ulcer formation.10, 26 Thus, lack of access to in-hospital physiotherapy likely results in longer hospitalization, higher rates of in-hospital mortality, and poorer overall recovery among stroke survivors.
Long-term, motor deficits affect stroke survivors’ ability to function independently and lead to increased dependence on others, reduceds quality of life and limited options for gainful employment, which in turn might limit their access to rehabilitation services.27 Targeted interventions such as gait and balance training that utilize assistive devices have shown positive effects even more than one year after stroke onset.28 However, retaining stroke survivors in long-term rehabilitation programs in most LMIC settings is difficult and financially unfeasible.
Approximately one-third of stroke survivors will also experience language impairment as a consequence of their stroke, which poses a unique challenge in adaptation and adjustment that may impact a stroke survivors’ social participation.29 Speech and language therapy has been shown to significantly improve functional communication of patients with language impairment from stroke.30 However, speech and language therapy services are scarcely available in many LMICs and, when present, are primarily found in private facilities which cater for fewer patients than public facilities.31 As a result, stroke survivors with speech impairment in LMICs largely rely on informal caregivers, who frequently lack training in language disability, for communication assistance or recovery programs,31, 32 thus perpetuating long-term dependency.
Consequences to Caregivers
Assuming the caregiver role in settings of limited rehabilitation facilities places a significant burden on caregivers’ livelihoods. Female daughters were most likely to be caregivers in many sub-Saharan African settings, including South Africa and Nigeria.25, 33, 34 As shown in Uganda, female caregivers often already have a regimented and full schedule of completing the daily household work which is then further compounded with the additional responsibilities of washing, toileting, feeding, and exercising the stroke survivor under their care.35 For caregivers who function as the primary wage-earners for families, taking on the role reduces hours at work and places a significant financial burden on the family.34 Ultimately, caring for stroke survivors can result in a decrease in the family’s ability to afford essentials, including food and utilities, let alone participate in costly rehabilitation services.
The limitations in rehabilitation facilities and education in LMICs also render caregivers liable to their own poor health outcomes. A stroke survivor’s physical dependence in combination with the limited training caregivers receive can cause physical injury to their caregivers, including musculoskeletal strain.36 Furthermore, attending to stroke survivors’ continuous needs, including nocturnal bowel and bladder dysfunction, has been correlated with poor sleep and fatigue in caregivers from Nigeria and Malawi.32, 37
In addition to physical strain, the continuous demands exacted on informal caregivers is correlated with poor mental health outcomes. In many LMIC settings, caregivers have a sense of duty and commitment to their ill family members, but witnessing stroke survivors’ suffering as well as post-stroke mood changes, including survivors’ anger and resentment, has been shown to lead to depression and burnout among caregivers.34, 35 In sub-Saharan Africa, depression and burnout may be further exacerbated when caregiving responsibilities fall on one person with limited support from other family members, thus leading primary caregivers to forego attendance at church or recreational time with family and friends, both important community traditions.32 Together, these factors have been shown to negatively impact mental health among caregivers of stroke survivors in sub-Saharan Africa.
Consequences at the National Level
Globally, the rate of moderate or severe functional disability due to stroke in LMICs is 77%, markedly higher than 38% reported from HICs.38 In parallel, the burden of stroke in people younger than 65 years has increased in LMICs over the last few decades.39 With more young people affected in LMICs, this impacts the available workforce and depletes the country economically. While data exploring the economic burden caused by stroke in LMICs is largely lacking, the potential for costs associated with a high stroke burden to negatively impact a country’s economic growth is apparent. For example, India lost $8.7 billion USD in 2005 due to coronary heart disease (CHD), stroke, and diabetes. This number was projected to increase to $54 billion USD by 2015, resulting in a fall in India’s gross domestic product of 1%.40
OPPORTUNITIES FOR IMPROVING STROKE REHABILITATION IN LMICs
Despite the limited availability of rehabilitation services in LMICs, the benefits of rehabilitation after stroke and consequences of limited access to rehabilitation have been well demonstrated as described above. Thus, it is imperative that LMICs discover ways to maximally utilize and expand the reach of available human resources to improve stroke-associated outcomes while also expanding the workforce of rehabilitation specialists in the long-term. Here we review potential opportunities for improving access to stroke rehabilitation in LMICs.
Training more rehabilitation specialists.
Skilled rehabilitation practitioners are lacking in LMICs as are the number of training programs in these disciplines.2, 41 In order to address the long-term shortage of rehabilitation specialists in LMICS, training opportunities must be increased, and this training should ideally extend to the doctoral level. Moreover, rehabilitation has previously received little attention from governments, which has contributed to poor service availability and lack of coordination between services. Organization of services through stroke units and linking them to community health services might create employment opportunities for rehabilitation specialists.2 Thus, there is a need to lobby governments in LMICs to prioritize rehabilitation services in both the inpatient and community settings in order to improve stroke outcomes across the stroke care continuum.
Development of stroke units.
The creation and integration of stroke units in hospitals is an important starting point to address current barriers to stroke rehabilitation in LMICs. Stroke units are proven to reduce stroke-associated morbidity and mortality by providing multidisciplinary care by a team that include physicians, nurses, physical therapists, occupational therapists, speech-language pathologists, and social workers, which allows for systematic integration of early rehabilitation strategies.18
Low-resourced stroke centers have been successfully implemented in several LMICs and shown benefit. For example, the Brazil National Stroke Project was launched in 2008 and supported the construction of acute stroke centers around the country from 2008 to 2012. The number of stroke centers increased from 20 to 37 in the public sector and from 15 to 45 in the private sector.42 Implementation of stroke clinical practice guidelines in one of these stroke centers led to a 53% relative reduction in in-hospital mortality.43 In South Africa, stroke mortality rates decreased from 33% to just 16% after implementation of stroke units.44 Thus, ensuring improved acute stroke care by increasing access to stroke centers and, where possible, acute stroke interventions will likely lead to improved long-term post-stroke rehabilitation outcomes in LMICs as well.
Community-based rehabilitation (CBR).
CBR was originally proposed by the World Health Organization following the Declaration of Alma-Ata in 1978 in an effort to enhance the quality of life for people with disabilities and their families; meet their basic needs; and ensure their inclusion and participation in society by utilizing locally available resources.45 The 2006 United Nations Convention on the Rights of Persons with Disabilities further advocated for comprehensive rehabilitation services focusing on health, employment, education and social services to ensure people with disabilities had the opportunity to attain and maintain maximum independence, full physical, mental, social and vocational ability, and full inclusion and participation in all aspects of life.46 Ideally, CBR programs are cost-effective, comprehensive programs with an equity and participatory focus. However, in practice, they often practice a top-down service delivery approach, are funded in non-sustainable ways primarily by external donors, have scarce resources, and lack community support.47, 48 For example, a CBR program in rural Uganda found that more than half of its participants with physical disabilities had high levels of functional impairment, and this was associated with reduced access to assistive devices and increased use of medical health care.49 Still, when implemented well, these programs can be effective. A CBR program in Afghanistan found participants demonstrated reductions in emotional and social challenges, unemployment and communication difficulties with improvements in overall well-being, even in the midst of ongoing conflict.50
Group Sessions.
Group rehabilitation therapy is defined as sessions involving more than two participants at the same time with tasks assigned according to each individual’s level of ability and an emphasis on improving functional activities and increasing patient motivation, activity and social participation. For example, circuit class therapy, a supervised group class in which individuals rotate through various stations, each of which is focused on a different task, has been shown to be safe and improve walking ability, walking speed and balance.51
Task-shifting and caregiver-led rehabilitation.
Task-shifting is defined as delegating a function normally performed by a qualified professional to someone with a lower level of education or to a person trained specifically to carry out that given task. This usually involves, for example, delegating tasks that would normally be performed by a medical doctor to specifically trained nurses or community healthcare workers. Task-shifting mechanisms have been successful in management of HIV and maternal and child health related problems and screening for non-communicable diseases and cardiovascular disease risk factors (Joshi et al, 2014).52 A study in Nigeria on training of non-neurologist health workers (predominantly nurses and community health workers) for stroke care demonstrated that a one-day training workshop on stroke diagnosis and care significantly improved levels of stroke care knowledge. However, whether these knowledge gains translated to change in behavior and improvement in practice was not evaluated.53
However, results from the few randomized controlled trials of caregiver-led post-stroke rehabilitation interventions that have been completed have been promising. A Cochrane review found low to moderate evidence that caregiver-led exercises were valuable in augmenting stroke rehabilitation without increasing caregiver burden. However, the review was limited by small participant numbers and heterogeneity of studies.54 For example, the ATTEND trial, a family-led rehabilitation randomized controlled trial in India, compared outcomes among 1200 stroke survivors provided rehabilitation by trained and supported family members versus usual care (no formal rehabilitation program).55 Because no difference in dependency, death, or level of disability was found between the two groups, the investigators recommended training healthcare assistants or utilizing CBR and group approaches. Another randomized trial in rural China employed a nurse-led, caregiver-delivered model of stroke rehabilitation compared to usual care (limited access to rehabilitation services and support).56 While participant satisfaction was high, it, too, failed to show a significant difference in outcomes with the authors recommendeding incorporation of community health workers and the use of mobile technologies to further augment potential benefits of such programs. However, similar studies performed in HICs found patients and caregivers had improved quality of life and a reduced sense of psychological burden even though there was no difference in patients’ functional outcomes (Table 2).57, 58 As such, further work is needed to understand how to achieve demonstrable improvements in rehabilitation outcomes when these programs are instituted in LMIC settings without sacrificing participant satisfaction and safety as well as the low associated caregiver burden is essential if these programs are to result in improved access to quality stroke rehabilitation in LMICs.
Table 2.
Randomized controlled trials of caregiver-led rehabilitation programs.
| Study | Participants | Intervention | Outcome | Results/ Conclusions |
|---|---|---|---|---|
| Lindley et al, ATTEND collaboration group55 Year: 2017 Location: India Study Type: Multicenter randomized controlled trial Sample size: 1250 |
Patients >18 with stroke in past 1 month | Informal/ family caregivers received additional structured rehab training for up to 2 months | Death or dependency at 6 months, defined by scores 3–6 on the mRS |
|
| Zhou et al56 Year: 2019 Location: rural China Study Type: Multicenter randomized controlled trial Sample size: 244 |
Patients 18–79yrs with residual disability (Barthel Index score ≤80/100) after a recent stroke | Nurse-led informal care-giver training in-hospital, videos, daily reminders, guide. | Barthel Index at 6 months |
|
| Forster et al57 Year: 2013 Location: United Kingdom Study type: Multicenter randomized controlled trial Sample size: 928 |
Stroke rehabilitation units randomized to intervention or standard of care | London stroke carer training course (LSCTC) administered to caregivers while patient in hospital, One follow-up session. | Functional independence, measured at 6 months. Primary caregiver outcome was caregiver burden. |
|
| Kalra et al58 Year: 2004 Location: United Kingdom Study Type: Single center randomized controlled trial Sample size: 300 |
Inpatients with recent stroke | Caregiver training sessions in multiple competencies, 3 to 5 sessions lasting ~30–45 minutes | Death/ institutionalisation, mRS, EuroQol visual analogue scale, others. Primary caregiver outcomes: caregiver burden, depression and anxiety |
|
Stroke Telerehabilitation.
Home-based telerehabilitation is defined as the use of mobile telecommunication devices by health personnel to provide remote evaluation, support, and guidance to persons with disability, either in their homes or at a distant health facility.59 An intensive telerehabilitation program in China found it was non-inferior to standard in-person rehabilitation in several domains.60 A recent Cochrane review comparing the effectiveness of telerehabilitation to in-person rehabilitation found no difference between the two despite wide heterogeneity among studies.61 Though many studies report cost-savings benefits of telerehabilitation, studies specifically measuring cost-effectiveness of these interventions are lacking.
Given the scarcity of health personnel in LMIC settings, telerehabilitation programs may expand the reach of limited health personnel. Though few, studies in LMICs have demonstrated the acceptability and feasibility of telemedicine programs among patients treated for various medical conditions, including neurological conditions.62 A cross-sectional survey among West African stroke survivors reported that the majority would be willing to consider telerehabilitation services. Less than 30% of the cohort were currently receiving physiotherapy services, citing financial constraints due to cost of physiotherapy services and transportation and premature discharge from physiotherapy as barriers to access. Though majority of participants were urban dwellers, only 35% owned a smartphone, although 80% had a family member who owned one.63 A single-arm pilot program using a mobile phone application-assisted stroke rehabilitation program in Ghana over a 12-week period noted improvement in some stroke disability scores and was acceptable among users.64 Another single-center study in Uganda also assessed the feasibility of using a mobile phone application with individualized support versus standard of care. Though the study was not powered to determine the efficacy of the intervention, it was found to be feasible and acceptable with good satisfaction reported by both providers and participants.65 Challenges faced by telerehabilitation programs such as these in LMICs include mobile phone network instability, computer illiteracy, lack of access to video capable devices, electricity outages, shared phones among multiple family members, and cost considerations for airtime and reimbursement of health care providers. However, considering the potential time and cost-saving benefits and potential to expand the reach of limited human resources, deliberate systemic and institutional changes to support such programs may prove beneficial in the long-term.
CONCLUSION
The current availability and quality of stroke rehabilitation services is highly proportional to a country’s economic resources. As a result, despite experiencing a higher burden of stroke and stroke-related morbidity and mortality, residents of LMICs face multiple health systems and personal barriers to accessing quality stroke rehabilitation that could improve stroke survival and functional outcomes. Measures can be put in place to close the gap between services available in HICs and those available in LMICs, including expanding training opportunities for skilled rehabilitation specialists, implementing cost-effective and low-resourced systems of acute stroke care, developing CBR and group rehabilitation sessions, utilizing telerehabilitation programs, and task-shifting rehabilitation programs to lower level healthcare workers and/or informal family caregivers. However, all of these strategies will require governments in LMICs to prioritize stroke rehabilitation services as a crucial component of achieving the World Health Organization’s Rehabilitation 2030 Action Plan. Prioritizing stroke rehabilitation in LMICs has the potential to lead to better stroke survival and stroke outcomes and, ultimately, to less stroke-related disability at the individual and population level and improved national economic productivity.
Funding:
This work was supported in part by the National Institutes of Health (grant numbers R21 NS118543-01, 1K01TW011771-01A1, D43TW009340).
Footnotes
Disclosures: The authors have no conflicts of interest to disclose.
REFERENCES
- 1.DALYs GBD, Collaborators H. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1603–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Rehabilitation 2030: The Need to Scale Up Rehabilitation. Geneva, Switzerland: World Health Organization, 2017. [Google Scholar]
- 3.Owolabi MO, Thrift AG, Martins S, et al. The state of stroke services across the globe: Report of World Stroke Organization-World Health Organization surveys. Int J Stroke 2021;16:889–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gimigliano F, Negrini S. The World Health Organization “Rehabilitation 2030: a call for action”. Eur J Phys Rehabil Med 2017;53:155–168. [DOI] [PubMed] [Google Scholar]
- 5.Mkoba EM, Sundelin G, Sahlen KG, Sorlin A. The characteristics of stroke and its rehabilitation in Northern Tanzania. Glob Health Action 2021;14:1927507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akinyemi RO, Ovbiagele B, Adeniji OA, et al. Stroke in Africa: profile, progress, prospects and priorities. Nat Rev Neurol 2021;17:634–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prvu Bettger J, Liu C, Gandhi DBC, Sylaja PN, Jayaram N, Pandian JD. Emerging Areas of Stroke Rehabilitation Research in Low- and Middle-Income Countries: A Scoping Review. Stroke 2019;50:3307–3313. [DOI] [PubMed] [Google Scholar]
- 8.Gururaj S, Bird ML, Borschmann K, et al. Evidence-based stroke rehabilitation: do priorities for practice change and feasibility of implementation vary across high income, upper and lower-middle income countries? Disabil Rehabil 2021:1–8. [DOI] [PubMed] [Google Scholar]
- 9.Lynch EA, Connell LA, Carvalho LB, Bird ML. Do clinical guidelines guide clinical practice in stroke rehabilitation? An international survey of health professionals. Disabil Rehabil 2021:1–8. [DOI] [PubMed] [Google Scholar]
- 10.Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet 2011;377:1693–1702. [DOI] [PubMed] [Google Scholar]
- 11.Magaqa Q, Ariana P, Polack S. Examining the Availability and Accessibility of Rehabilitation Services in a Rural District of South Africa: A Mixed-Methods Study. Int J Environ Res Public Health 2021;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Confederation for Physical Therapy. Surveys reveal global state of physical therapy profession. London, United Kingdom: World Physiotherapy, 2019. [Google Scholar]
- 13.Chimatiro GL, Rhoda AJ. Scoping review of acute stroke care management and rehabilitation in low and middle-income countries. BMC Health Serv Res 2019;19:789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strasser R, Kam SM, Regalado SM. Rural Health Care Access and Policy in Developing Countries. Annu Rev Public Health 2016;37:395–412. [DOI] [PubMed] [Google Scholar]
- 15.Johnston K, Guingona M, Elsanousi S, et al. Training a Fit-For-Purpose Rural Health Workforce for Low- and Middle-Income Countries (LMICs): How Do Drivers and Enablers of Rural Practice Intention Differ Between Learners From LMICs and High Income Countries? Front Public Health 2020;8:582464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Igwesi-Chidobe C. Obstacles to obtaining optimal physiotherapy services in a rural community in southeastern Nigeria. Rehabil Res Pract 2012;2012:909675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baatiema L, Chan CKY, Sav A, Somerset S. Interventions for acute stroke management in Africa: a systematic review of the evidence. Syst Rev 2017;6:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stroke Unit Trialists C. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2013:CD000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tawa N, Rhoda A, Brink Y, et al. Stroke rehabilitation services in Africa - Challenges and opportunities: A scoping review of the literature. In: Louw Q, ed. Collaborative capacity development to complement stroke rehabilitation in Africa. Cape Town (ZA)2020. [PubMed] [Google Scholar]
- 20.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013;38:976–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sarfo FS, Ovbiagele B. Quantitative and qualitative analyses of herbal medication use among Ghanaian stroke survivors. J Neurol Sci 2021;427:117540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meherali S, Punjani NS, Mevawala A. Health Literacy Interventions to Improve Health Outcomes in Low- and Middle-Income Countries. Health Lit Res Pract 2020;4:e251–e266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shaw SJ, Huebner C, Armin J, Orzech K, Vivian J. The role of culture in health literacy and chronic disease screening and management. J Immigr Minor Health 2009;11:460–467. [DOI] [PubMed] [Google Scholar]
- 24.Khondowe O, Rhoda A, Mpofu R. Perceived needs of caregivers of stroke patients’ receiving out-patient physiotherapy treatment in Lusaka, Zambia. South African J Physiotherapy 2012;68:1–5. [Google Scholar]
- 25.Hassan S, Visagie S, Mji G. Strain Experienced by Caregivers of Stroke Survivors in the Western Cape. South African J Physiotherapy 2011;67:4–8. [Google Scholar]
- 26.Olaleye OA, Lawal ZI. Utilization of physiotherapy in the continuum of stroke care at a tertiary hospital in Ibadan, Nigeria. Afr Health Sci 2017;17:79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Legg LA, Drummond AE, Langhorne P. Occupational therapy for patients with problems in activities of daily living after stroke. Cochrane Database Syst Rev 2006:CD003585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Norrving B, Barrick J, Davalos A, et al. Action Plan for Stroke in Europe 2018–2030. Eur Stroke J 2018;3:309–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wray F, Clarke D. Longer-term needs of stroke survivors with communication difficulties living in the community: a systematic review and thematic synthesis of qualitative studies. BMJ Open 2017;7:e017944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brady MC, Kelly H, Godwin J, Enderby P, Campbell P. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev 2016:CD000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wylie K, McAllister L, Davidson B, Marshall J. Communication rehabilitation in sub-Saharan Africa: The role of speech and language therapists. Afr J Disabil 2018;7:338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kalavina R, Chisati E, Mlenzana N, Wazakili M. The challenges and experiences of stroke patients and their spouses in Blantyre, Malawi. Malawi Med J 2019;31:112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Imarhiagbe FA, Asemota AU, Oripelaye BA, et al. Burden of informal caregivers of stroke survivors: Validation of the Zarit burden interview in an African population. Ann Afr Med 2017;16:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Masuku KP, Mophosho M, Tshabalala M. ‘I felt pain. Deep pain…’: Experiences of primary caregivers of stroke survivors with aphasia in a South African township. Afr J Disabil 2018;7:368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eriksson GM, Kamwesiga JT, Guidetti S. The everyday life situation of caregivers to family members who have had a stroke and received the rehabilitation intervention F@ce in Uganda. Arch Public Health 2021;79:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Badaru UM, Ogwumike OO, Adeniyi AF, Nelson EE. Determinants of caregiving burden and quality of life of informal caregivers of African stroke survivors: literature review. Int J Disability Hum Develop 2017;16:249–258. [Google Scholar]
- 37.Akosile C, Okoye E, Adegoke B, Mbada C, Maruf F, Okeke I. Burden, Health and Quality of Life of Nigerian Stroke Caregivers. . Health Care: Curr Rev 2013;1:1000105. [Google Scholar]
- 38.Langhorne P, O’Donnell MJ, Chin SL, et al. Practice patterns and outcomes after stroke across countries at different economic levels (INTERSTROKE): an international observational study. Lancet 2018;391:2019–2027. [DOI] [PubMed] [Google Scholar]
- 39.Krishnamurthi RV, Moran AE, Feigin VL, et al. Stroke Prevalence, Mortality and Disability-Adjusted Life Years in Adults Aged 20–64 Years in 1990–2013: Data from the Global Burden of Disease 2013 Study. Neuroepidemiology 2015;45:190–202. [DOI] [PubMed] [Google Scholar]
- 40.Katan M, Luft A. Global Burden of Stroke. Semin Neurol 2018;38:208–211. [DOI] [PubMed] [Google Scholar]
- 41.Agho AO, John EB. Occupational therapy and physiotherapy education and workforce in Anglophone sub-Saharan Africa countries. Hum Resour Health 2017;15:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martins SC, Pontes-Neto OM, Alves CV, et al. Past, present, and future of stroke in middle-income countries: the Brazilian experience. Int J Stroke 2013;8 Suppl A100:106–111. [DOI] [PubMed] [Google Scholar]
- 43.Rocha MS, Almeida AC, Abath Neto O, Porto MP, Brucki SM. Impact of stroke unit in a public hospital on length of hospitalization and rate of early mortality of ischemic stroke patients. Arq Neuropsiquiatr 2013;71:774–779. [DOI] [PubMed] [Google Scholar]
- 44.de Villiers L, Kalula SZ, Burch VC. Does multidisciplinary stroke care improve outcome in a secondary-level hospital in South Africa? Int J Stroke 2009;4:89–93. [DOI] [PubMed] [Google Scholar]
- 45.World Health Organization. Declaration of Alma-Ata: International Conference on Primary Health Care, Alma-Ata, USSR, 6–12 September 1978. Geneva, Switzerland: World Health Organization, 1978. [Google Scholar]
- 46.United Nations. Convention on the Rights of Persons with Disabilities. New York, NY: United Nations, 2006. [Google Scholar]
- 47.Turmusani M, Vreede A, Wirz SL. Some ethical issues in community-based rehabilitation initiatives in developing countries. Disabil Rehabil 2002;24:558–564. [DOI] [PubMed] [Google Scholar]
- 48.Mauro V, Biggeri M, Grilli L. Does community-based rehabilitation enhance the multidimensional well-being of deprived persons with disabilities? a multilevel impact evaluation. World Dev 2015;76:190–202. [Google Scholar]
- 49.Hamid LN, Kobusingye O, Baine SO, Mayora C, Bentley JA. Disability Characteristics of Community-Based Rehabilitation Participants in Kayunga District, Uganda. Ann Glob Health 2017;83:478–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Trani JF, Vasquez-Escallon J, Bakhshi P. The impact of a community based rehabilitation program in Afghanistan: a longitudinal analysis using propensity score matching and difference in difference analysis. Confl Health 2021;15:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.English C, Hillier S. Circuit class therapy for improving mobility after stroke: a systematic review. J Rehabil Med 2011;43:565–571. [DOI] [PubMed] [Google Scholar]
- 52.Joshi R, Alim M, Kengne AP, et al. Task shifting for non-communicable disease management in low and middle income countries--a systematic review. PLoS One 2014;9:e103754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Akinyemi RO, Owolabi MO, Adebayo PB, et al. Task-shifting training improves stroke knowledge among Nigerian non-neurologist health workers. J Neurol Sci 2015;359:112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vloothuis JD, Mulder M, Veerbeek JM, et al. Caregiver-mediated exercises for improving outcomes after stroke. Cochrane Database Syst Rev 2016;12:CD011058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Group AC. Family-led rehabilitation after stroke in India (ATTEND): a randomised controlled trial. Lancet 2017;390:588–599. [DOI] [PubMed] [Google Scholar]
- 56.Zhou B, Zhang J, Zhao Y, et al. Caregiver-Delivered Stroke Rehabilitation in Rural China. Stroke 2019;50:1825–1830. [DOI] [PubMed] [Google Scholar]
- 57.Forster A, Dickerson J, Young J, et al. A cluster randomised controlled trial and economic evaluation of a structured training programme for caregivers of inpatients after stroke: the TRACS trial. Health Technol Assess 2013;17:1–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kalra L, Evans A, Perez I, et al. Training carers of stroke patients: randomised controlled trial. BMJ 2004;328:1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sarfo FS, Ulasavets U, Opare-Sem OK, Ovbiagele B. Tele-Rehabilitation after Stroke: An Updated Systematic Review of the Literature. J Stroke Cerebrovasc Dis 2018;27:2306–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen J, Sun D, Zhang S, et al. Effects of home-based telerehabilitation in patients with stroke: A randomized controlled trial. Neurology 2020;95:e2318–e2330. [DOI] [PubMed] [Google Scholar]
- 61.Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C. Telerehabilitation services for stroke. Cochrane Database Syst Rev 2020;1:CD010255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Asukile M, Chishimba L, Chomba M, et al. Implementation of a Teleneurology Clinic in Zambia During the COVID-19 Pandemic. Ann Neurol 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sarfo FS, Adamu S, Awuah D, Sarfo-Kantanka O, Ovbiagele B. Potential role of tele-rehabilitation to address barriers to implementation of physical therapy among West African stroke survivors: A cross-sectional survey. J Neurol Sci 2017;381:203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sarfo FS, Adusei N, Ampofo M, Kpeme FK, Ovbiagele B. Pilot trial of a tele-rehab intervention to improve outcomes after stroke in Ghana: A feasibility and user satisfaction study. J Neurol Sci 2018;387:94–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kamwesiga JT, Eriksson GM, Tham K, et al. A feasibility study of a mobile phone supported family-centred ADL intervention, F@ce, after stroke in Uganda. Global Health 2018;14:82. [DOI] [PMC free article] [PubMed] [Google Scholar]


