Abstract
The ongoing COVID-19 pandemic is not only an immediate hazard but also a long-term risk to the development of depressive symptoms. However, it remains unclear how people's depressive symptoms change with the process of COVID-19. Further, there is also a paucity of research on the underlying antecedents and outcomes of depressive symptoms during this global health crisis. In this study, a longitudinal study was conducted in China and the data of 559 participants were collected from the outbreak period to the normalization period of the pandemic through self-report questionnaires. Depressive symptoms were longitudinally analyzed using Patient Health Questionnaire-9. Core variables involving society, family, individual cognition, and behaviors were studied as determinants or consequences. Latent growth curve model analyses indicated that college students had mild depressive symptoms at the initial stage of COVID-19 with a subsequent decreasing linear slope. Depressive symptoms were significantly predicted by college students’ risk perception of COVID-19, social support, family functioning, and smartphone addiction tendency. Further, their depressive symptoms predicted the changes in smartphone addiction tendency and levels of hope. In conclusion, current findings can provide implications for future prevention and intervention of mental disorders to assist college students through such challenging times.
Keywords: COVID-19, Depressive symptoms, College students, Latent growth curve model
1. Introduction
As a significant global public health emergency in the 21st century, the coronavirus disease 2019 (COVID-19) pandemic not only poses a tremendous threat to individuals’ lives but also has an unprecedented impact on their mental health (Xiong et al., 2020). The highly contagious and life-threatening nature of COVID-19 has led to increased psychological distress (Vindegaard and Benros, 2020). The torrent of news and information regarding COVID-19 further results in the emergence of an infodemic (World Health Organization, 2021) and causes chronic pandemic-related distress in the general population (Banerjee and Meena, 2021). In addition, the economic regression, unemployment, and disruptions to normal routines resulting from the pandemic have become new stressors that pose challenges to individuals’ mental health (Talevi et al., 2020; Torales et al., 2020). For example, the extant literature has found steep increases in the prevalence of anxiety, depression, and stress following the outbreak of COVID-19 (Planchuelo-Gómez et al., 2020; Wang et al., 2020a). The prevalence of depressive symptoms has become a global concern, ranging from 14.6% to 48.3% in different countries (e.g., China, Spain, Italy, and the USA) (Xiong et al., 2020). Unfortunately, although research has already highlighted the changes in depressive experiences that occurred during the pandemic, the conclusions of those studies may have been limited due to their cross-sectional nature (e.g., Wang et al. 2020a) or short research periods (e.g., Magson et al. 2020). Moreover, the core determinants and consequences of depressive symptoms in this crisis require further exploration. Considering the acute and persistent effects of COVID-19, the present study aimed to shed light on these questions by investigating the trajectories of depressive symptoms from the outbreak of the pandemic to the normalization period. More importantly, we examined key antecedents of the pandemic and related outcomes to explore the development and influence of depressive symptoms during the COVID-19 pandemic.
1.1. The longitudinal development of depressive symptoms
Depression is one of the most commonly reported mental disorders during the pandemic. During the initial stage of COVID-19, Wang et al. (2020a) conducted a survey featuring more than 1000 participants in China and found that 16.5% of the participants reported moderate-to-severe depressive symptoms. On the one hand, pandemic-related stressors could exacerbate the risk of depression. The unknown infection mechanism, limited social interactions, and excessive media information were found to promote a global atmosphere of depression (Ettman et al., 2020; Ho et al., 2020; Pierce et al., 2020). On the other hand, pandemic prevention measures may unexpectedly lead to some mental problems. For instance, home quarantine is beneficial with regard to stopping the spread of COVID-19 but may result in higher rates of depression (Planchuelo-Gómez et al., 2020). Furthermore, a series of public health policies and measures have made some progress in the fight against COVID-19, and China has entered a period of basic containment (Liu et al., 2020). After new arrangements allowing for a full resumption of work, people's lives are gradually returning to normalcy, and their depressive symptoms may decrease alongside the positive trend in pandemic containment. Compared to studies that featured less than three months of follow-up, a cohort study that featured more than three months of follow-up reported a lower prevalence of depression (Bourmistrova et al., 2022). Based on the research literature we reviewed, we hypothesized that people would be likely to exhibit more depressive symptoms during the outbreak of COVID-19 and that their depressive symptoms would display a decreasing trend over time.
1.2. Antecedents of depressive symptoms
According to the Process-Person-Context-Time model (PPCT) based on ecological systems theory (Bronfenbrenner and Morris, 2006), four components (i.e., proximal processes, person characteristics, context, and time) contribute greatly to individuals’ development. In this study, we aimed to explore the mechanisms underlying the development of college students’ depressive symptoms (process) during the pandemic (time) by identifying the potential antecedents, ranging from the macroscopic to the microcosmic. We examined the role of pandemic situation (i.e., risk perception), a societal factor (i.e., social support; context—mesosystem), a family factor (i.e., family functioning; context—microsystem), and an individual behavior factor (i.e., smartphone addiction tendency; person characteristic).
1.2.1. Risk perception
Focusing on people's perceived risk is an important way to understand their psychological and behavioral responses during a crisis (Qin et al., 2018). Risk perception is defined as individuals’ subjective evaluations and judgments regarding the real risks associated with a situation (Slovic, 1987; Xie and Xu, 1996). High perceived risk has been found to result in social unrest, pressure on health care (Peres et al., 2020), sleep disturbances, anxiety and stress (Casagrande et al., 2020). During this pandemic, risk perception was also considered to be a key antecedent of depressive symptoms (Ding et al., 2020), with evidence suggesting that perception of COVID-19 risk was related to increased death distress and reduced happiness (Yıldırım and Güler, 2021). In addition, higher risk perception may cause people to experience more fear of infection, which can lead to increased negative emotions (Zhao et al., 2021; Zheng et al., 2019) and exacerbate depressive symptoms (Ding et al., 2020).
Previous studies have shown that risk perception is greatly influenced by trust in information, familiarity with epidemic situations, and interpersonal distance from people located at the epicenter (Chen et al., 2021). In addition, popular opinions, recovery rates, and government preventive measures can also change people's risk perception. A longitudinal study conducted during the period during which severe acute respiratory syndrome (SARS) was prevalent demonstrated that residents dealt with information regarding SARS in a more rational manner and reported a lower risk perception of SARS after the epidemic situation was under control (Shi and Hu, 2004). Therefore, we considered the risk perception of COVID-19 to be a time-varying variable and expected it to positively predict depressive symptoms.
1.2.2. Social support
Support from others is an important aspect of people's ability to overcome difficulties. Generally, social support is defined as referring to both the mental and the material support that people obtain from their social networks (Cobb, 1976). Empirical studies have revealed a positive association between social support and individuals’ psychological well-being (Peirce et al., 2000; Uchino, 2006, 2009). According to the buffering effect model, social support buffers the pathogenic influences of stressful events on individuals by enhancing people's perceived coping ability and reducing their harmful psychological responses (Cohen and Willis, 1985). In nonpandemic situations, social support is purported to alleviate people's mental distress after suffering natural disasters (Xu et al., 2013). Evidence has been found suggesting that people with less social support are more likely to experience depressive symptoms (Alsubaie et al., 2019; Guntzviller et al., 2020). During the COVID-19 pandemic, negative associations between social support and depression have also been documented (Li et al., 2020). A study of Chinese adolescents indicated that adolescents with less social support faced greater risks of depression in China during the outbreak of COVID-19 (Qi et al., 2020). Given that social support is an indicator of one's support system and resources, which remain relatively stable, we treated social support as a time-invariant predictor and hypothesized that the level of social support would negatively predict depressive symptoms.
1.2.3. Family functioning
During the outbreak of the pandemic, many families spent more time at home than normal due to confinement measures. Therefore, the organizational properties of a family group and the interactions among family members may have significantly affected people's mental health. Family functioning refers to the ability of the family to satisfy the basic needs of its members (Ryan and Keitner, 2009) and the effectiveness of family communication, emotional connection, and ability to cope with developmental changes or situational stressors (Olson, 2000; Olson et al., 1983). According to family system theory, family functioning plays a significant role in child development and mental health (Beavers and Hampson, 2000). Good family functioning has been found to be related to fewer negative outcomes, such as suicidal behaviors (King et al., 1993) and depressive symptoms. In contrast, adolescents with less supportive and more conflictual family environments tend to become more depressed (Sheeber et al., 1997). In pandemic situations, the effect of family functioning on individuals’ mental health may be amplified. Studies have indicated that individuals with poor family functioning exhibit higher levels of perceived stress (Wu et al., 2021), anxiety, and depressive symptoms (Li et al., 2020) during COVID-19. In this study, college students’ family functioning was viewed as a time-invariant predictor due to its stability across time (Zhao et al., 2021). We further expected this factor to be negatively associated with depressive symptoms during the COVID-19 pandemic.
1.2.4. Smartphone addiction tendency
With regard to individual behavior, we sought to explore the influence of smartphone use in this context. Due to the demands of entertainment and productivity during the period of home-quarantine, people spent more time using smartphones to connect with the world (Liu, 2020). Increased smartphone use may represent a hidden crisis with regard to the development of smartphone addiction and further lead to physical and psychological problems (Ratan et al., 2021). The present study conceptualizes smartphone addiction, which has been a widely studied behavioral addiction in recent years, in terms of individuals’ inability to control their smartphone use to the extent that they neglect other aspects of their lives and experience psychological and behavioral problems (Lee et al., 2014; Liu et al., 2017). Geng et al. (2021) reported that people with higher smartphone addiction tendency are more likely to postpone their bedtime, which may generate more negative emotions such as depression and anxiety. Moreover, a systematic review suggested a positive association of medium strength between smartphone addiction and depressive symptoms (Elhai et al., 2017). During the COVID-19 pandemic, although the effectiveness of smartphones with regard to satisfying people's needs has generally been recognized, it is noteworthy that excessive smartphone use might result in more depressive symptoms, especially during the outbreak of COVID-19. A survey of home-confined adolescents noted that COVID-19-related exposure severity increased their tendency toward smartphone addiction and further exacerbated their post-traumatic stress disorder (PTSD) symptoms (Hu et al., 2021). Therefore, we considered college students’ smartphone addiction tendency to be an important predictor of their depressive symptoms.
1.3. Outcomes of depressive symptoms
Exploring the outcomes of depressive symptoms can expand our understanding of the long-term effects of depressive symptoms. In this study, we considered both general and problematic outcomes. Specifically, after experiencing a public health emergency, depression may change people's perspectives on the world and the ways in which they approach their future lives. Moreover, as smartphone use becomes part of college students’ daily routine in this digital age, the question of whether depression could affect their subsequent internet-specific behavior or problematic device use requires further examination. Therefore, we included college students’ hope (i.e., general cognitive-emotional outcome) and smartphone addiction tendency (i.e., problematic behavioral outcome) as a complementary set of outcomes that are able to provide a more detailed picture of the potential consequences of depressive symptoms trajectories.
1.3.1. Smartphone addiction tendency
In addition to the potential predictive effect of smartphone addiction, some researchers have argued that there is a reciprocal relationship between smartphone addiction and depressive symptoms (Park et al., 2019; Stanković et al., 2021). Therefore, we also acknowledged the plausible status of smartphone addiction tendency as an outcome of depressive symptoms. The Interaction of Person-Affect-Cognition-Execution (I-PACE) model proposes that people may exhibit maladaptive use of the internet and smartphones in stressful environments (Brand et al., 2016, 2019). Use of smartphones as terminals to access the internet is considered to constitute a coping strategy for negative emotions (Elhai et al., 2020). During the COVID-19 pandemic, Jin et al. (2021) argued that individuals with more depressive symptoms tended to use smartphones to relieve the stress caused by the pandemic, which further increased their risk of becoming addicted to smartphones. Based on previous findings, we hypothesized that college students’ depressive symptoms would be positively associated with their smartphone addiction tendency.
1.3.2. Hope
Hope refers to the perceived capability to explore the potential pathways that can be followed to achieve one's goals (pathway) and to motivate oneself to use those pathways (agency) (Snyder, 1995, 2002). Previous studies have reported that college students’ mental health status could negatively predict their level of hope (Li, 2021). Additionally, research on patients with depression found that such patients exhibit much lower levels of hope (Ren et al., 2018). People with depressive symptoms tend to have more negative self-perceptions (e.g., self-esteem, self-efficacy; Dai and Feng 2008), unclear goals and insufficient motivation, which result in a lower level of hope (Phan, 2013). Similarly, college students who experienced more depression during the COVID-19 pandemic may have felt hopeless about their established goals and future lives. In the present study, we hypothesized that depressive symptoms during the COVID-19 pandemic would negatively predict college students’ levels of hope.
2. Method
2.1. Participants
The dataset used in this study was drawn from a longitudinal study focused on the effects of the COVID-19 pandemic on college students’ mental health and behaviors. Participants were recruited from different universities in China. Based on the development of previous epidemics (e.g., SARS) and the COVID-19 pandemic in China, participants were surveyed four times corresponding to the different periods of the pandemic (i.e., outbreak, basic containment, regular control, and normalization). A sample of 559 college students (29.16% male, M age = 20.42, SD = 1.39) participated in the initial investigation, and there were 557 participants at Time 2 (T2). Subsequently, 474 students and 445 students from the original research group completed the follow-up investigations at Time 3 (T3) and Time 4 (T4), respectively. Chi-square tests and independent sample t-tests indicated no significant differences in terms of gender (χ 2(1)= 0.144, p > 0.05), age (t(557) = −1.25, p > 0.05), depressive symptoms (t(557) = −0.63, p > 0.05), risk perception (t(557) = −1.82, p > 0.05), social support (t(557) = 1.45, p > 0.05), family functioning (t(557) = −1.13, p > 0.05), and smartphone addiction tendency (t(557) = −0.66, p > 0.05), thus suggesting a random pattern of missing data.
2.2. Procedure
This study was approved by the Research Ethics Committee of the author's institution, and we also obtained informed consent from all participants. The initial investigation was conducted in June 2020, and participants were told to recall their psychological and behavioral responses between January and March 2020 (T1; the outbreak period of COVID-19). At the beginning of the questionnaire, we provided some detailed information (e.g., confirmed case data, official news, and government policies) to illustrate the development of COVID-19 in China from January to March 2020 to help participants recall their feelings and behaviors more accurately. One week later, the second wave of data collection (T2; the basic containment period of COVID-19) was performed to measure participants’ psychological status at that time. Furthermore, participants were asked to complete a survey regarding their feelings and behaviors in September 2020 (T3; the regular control period of COVID-19) and December 2020 (T4; the normalization period of COVID-19).
2.3. Measures
2.3.1. Depressive symptoms (T1-T4)
Participants’ depressive symptoms were evaluated using the Patient Health Questionnaire-9 (PHQ-9), which is a reliable and valid measure of depression severity (Kroenke et al., 2001). Participants were asked to indicate how often they had been bothered by the problems described by the items over the past two weeks. Each item was scored on a scale ranging from 0 (not at all) to 3 (nearly every day), with a higher score indicating a higher level of depressive symptoms. In the present study, Cronbach's alpha coefficients for this scale were 0.92 at T1, 0.88 at T2, 0.90 at T3, and 0.90 at T4.
2.3.2. Risk perception (T1-T4)
We adapted the public risk perception scale (Dai et al., 2020) to measure participants’ risk perception of the COVID-19 pandemic. This 10-item scale originally measured people's risk perception regarding public health emergencies; thus, in this study, we reworded the scale to refer to the COVID-19 pandemic. Participants responded to each item on a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree), and a higher score was indicative of greater risk perception of the COVID-19 pandemic. The Cronbach's alpha coefficients of this scale were 0.81 at T1, 0.75 at T2, 0.84 at T3, and 0.83 at T4.
2.3.3. Social support (T1)
Participants’ self-reports of social support during the outbreak of the COVID-19 pandemic were assessed using the Social Support Rating Scale (Xiao, 1999). This 10-item scale includes three dimensions, including subjective support, objective support, and support-seeking behavior. Some expressions were modified to suit the actual situation of college students (e.g., “colleagues” → “students”). A higher score suggested a higher level of social support. The Cronbach's alpha coefficient of this scale in this study was 0.68 (T1).
2.3.4. Family functioning (T1)
Five items drawn from the short version of the General Functioning subscale of The McMaster Family Assessment Device (FAD) (Boterhoven et al., 2015) were used to measure participants’ family functioning. Participants rated each item on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree), and a higher score indicated a higher level of family functioning. In the present study, Cronbach's alpha coefficient of this scale was 0.93 (T1).
2.3.5. Smartphone addiction tendency (T1, T4)
This scale was adapted from the Smartphone Addiction Scale (Su et al., 2014). Specifically, we used six items to assess participants’ smartphone addiction tendency at T1 and T4. Participants were asked to rate how applicable each item was to them on a 5-point scale ranging from 1 (not at all) to 5 (always true). The smartphone addiction tendency scores were created by summing these items, with a higher score indicating a stronger tendency toward smartphone addiction. The Cronbach's alpha coefficients of this scale in this study were 0.80 (T1) and 0.81 (T4).
2.3.6. Hope (T4)
We used the State Hope Scale (Snyder et al., 1996) to measure participants’ levels of hope. This scale consisted of six items, and participants were asked to rate the extent to which the items described their thinking at the moment they completed the measure on a scale ranging from 1 (definitely false) to 8 (definitely true). A higher score indicates a higher level of hope. In this study, Cronbach's alpha coefficient of this scale was 0.90 (T4).
2.4. Statistical analysis
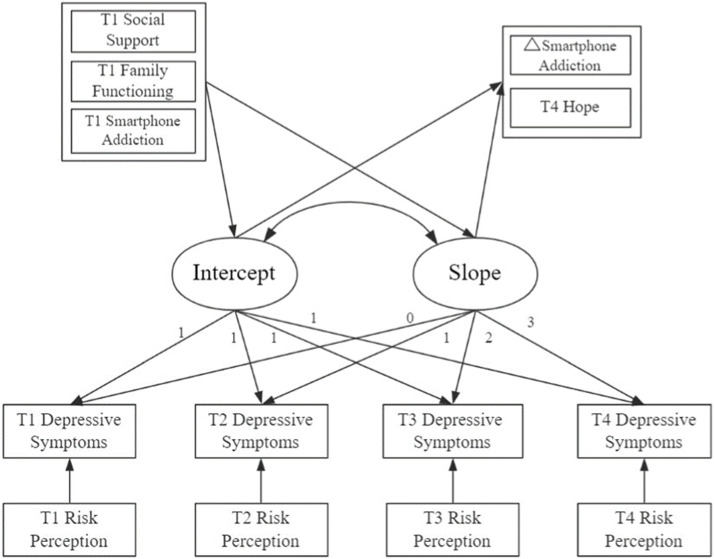
First, we used SPSS 22.0 software to conduct the descriptive analyses and examine the correlations among research variables. Subsequently, we evaluated model adequacy using Mplus 7.4 software and addressed missing data using full information maximum likelihood (FIML). Thereafter, the latent growth curve model (LGCM) was used to represent college students’ developmental trajectories of depressive symptoms. Consistent with a linear LGCM parameterization, an intercept factor, which reflected the average initial level of depressive symptoms, and a slope factor, which reflected the average level of change in depressive symptoms, were estimated. Subsequently, risk perception of the COVID-19 pandemic was considered to be a time-varying predictor of college students’ depressive symptoms within each time wave. Baseline (T1) levels of social support, family functioning, and smartphone addiction tendency were also incorporated into the model as time-invariant predictors and were used to predict the intercept and slope factors of depressive symptoms. Finally, we estimated the outcomes of the intercept and slope factors by incorporating participants’ smartphone addiction tendency and hope at T4. The LGCM model including all predictors and outcomes is presented in Fig. 1 .
Fig. 1.
The LGCM model.
3. Results
3.1. Preliminary analysis
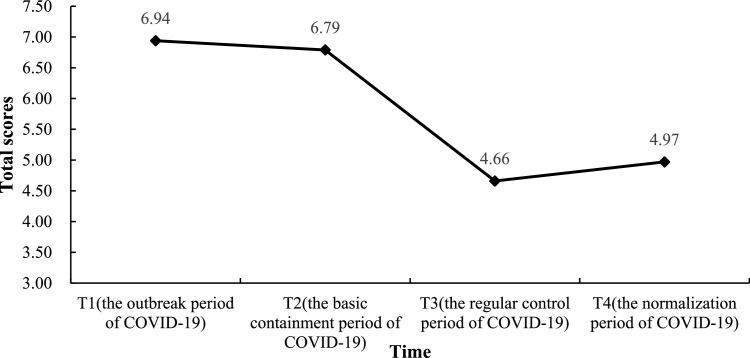
The descriptive statistics and correlations among the study variables are presented in Table 1 . Overall, college students’ depressive symptoms decreased successively from T1 to T3 but increased slightly at T4 (see Fig. 2 ). With regard to previous suggestions concerning the severity of depression symptoms (Kroenke et al., 2001), we found that 30.23% of participants experienced mild depressive symptoms and 28.26% of participants experienced moderate to severe depression at T1. The results of the paired sample t-tests showed that college students’ levels of depressive symptoms at T1 and T2 were significantly higher than those at T3 and T4 (T1-T3, t(473) = 9.06; T1-T4, t(444) = 7.63; T2-T3, t(472) = 9.25; T2-T4, t(443) = 7.30, all p < 0.001). The correlation analysis also validated the hypothesized relationships among the research variables.
Table 1.
Means, standard deviations, and correlations among study variables.
| Variables | M ± SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 SS | 37.44 ± 6.27 | — | ||||||||||||
| 2. T1 FF | 19.82 ± 3.94 | 0.42⁎⁎⁎ | — | |||||||||||
| 3. T1 SA | 19.80 ± 4.61 | −0.06 | −0.01 | — | ||||||||||
| 4. T1 DS | 6.94 ± 5.99 | −0.15⁎⁎⁎ | −0.22⁎⁎⁎ | 0.41⁎⁎⁎ | — | |||||||||
| 5. T1 RP | 35.75 ± 6.11 | 0.05 | 0.07 | 0.22⁎⁎⁎ | 0.26⁎⁎⁎ | — | ||||||||
| 6. T2 DS | 6.79 ± 5.49 | −0.23⁎⁎⁎ | −0.27⁎⁎⁎ | 0.34⁎⁎⁎ | 0.59⁎⁎⁎ | 0.17⁎⁎⁎ | — | |||||||
| 7. T2 RP | 32.27 ± 5.58 | −0.01 | −0.01 | 0.20⁎⁎⁎ | 0.17⁎⁎⁎ | 0.54⁎⁎⁎ | 0.21⁎⁎⁎ | — | ||||||
| 8. T3 DS | 4.66 ± 4.84 | −0.16⁎⁎ | −0.20⁎⁎⁎ | 0.24⁎⁎⁎ | 0.47⁎⁎⁎ | 0.04 | 0.51⁎⁎⁎ | 0.12⁎⁎ | — | |||||
| 9. T3 RP | 30.33 ± 6.94 | 0.06 | 0.03 | 0.08 | 0.12⁎⁎ | 0.34⁎⁎⁎ | 0.13⁎⁎ | 0.50⁎⁎⁎ | 0.14⁎⁎ | — | ||||
| 10. T4 DS | 4.97 ± 5.08 | −0.14⁎⁎ | −0.18⁎⁎⁎ | 0.21⁎⁎⁎ | 0.47⁎⁎⁎ | 0.12* | 0.45⁎⁎⁎ | 0.12* | 0.58⁎⁎⁎ | 0.15⁎⁎ | — | |||
| 11. T4 RP | 30.31 ± 6.71 | 0.07 | 0.09* | 0.07 | 0.04 | 0.26⁎⁎⁎ | 0.07 | 0.40⁎⁎⁎ | 0.08 | 0.60⁎⁎⁎ | 0.12* | — | ||
| 12. T4 SA | 19.11 ± 4.56 | −0.03 | −0.06 | 0.47⁎⁎⁎ | 0.24⁎⁎⁎ | 0.12* | 0.26⁎⁎⁎ | 0.15⁎⁎ | 0.25⁎⁎⁎ | 0.12* | 0.31⁎⁎⁎ | 0.14⁎⁎ | — | |
| 13. T4 H | 32.36 ± 7.18 | 0.20⁎⁎⁎ | 0.20⁎⁎⁎ | −0.17⁎⁎⁎ | −0.21⁎⁎⁎ | −0.03 | −0.28⁎⁎⁎ | −0.06 | −0.40⁎⁎⁎ | −0.02 | −0.43⁎⁎⁎ | 0.03 | −0.27⁎⁎⁎ | — |
Note: N = 559. SS = social support; FF = family functioning; SA= smartphone addiction tendency; DS = depressive symptoms; RP = risk perception of COVID-19; H = hope. *p < 0.05. ⁎⁎p < 0.01. ⁎⁎⁎p < 0.001.
Fig. 2.
The changes in depressive symptoms from T1 to T4.
3.2. Latent growth curve model
The results indicated that the unconditional LGCM exhibited an adequate level of fit, χ 2/df = 10.377, RMSEA = 0.130 (90% CI = [0.099, 0.163]), CFI = 0.924, TLI = 0.909, SRMR = 0.054. The parameter estimates of this model are reported in Table 2 . The intercept factor was significantly higher than 0, and depressive symptoms at T1 exhibited significant interindividual variability. In addition, these results showed a statistically significant decreasing linear slope, thus also indicating significant interindividual variability. The correlation between these two growth factors was −0.608 (p < 0.001), suggesting that participants with higher initial depressive symptoms tended to exhibit steeper declines.
Table 2.
Parameter estimates from the unconditional LGCM.
| Depressive symptoms | ||
|---|---|---|
| Intercept factor | Linear slope factor | |
| Growth parameters | ||
| M | 7.049(0.238) ⁎⁎⁎ | −0.822(0.089) ⁎⁎⁎ |
| Variance | 22.008(2.061) ⁎⁎⁎ | 1.467(0.317) ⁎⁎⁎ |
| Correlations between the intercept and slope factor |
−0.608(0.056) ⁎⁎⁎ | |
Note: Numbers in parentheses are standard errors *p < 0.05. ⁎⁎p < 0.01. ⁎⁎⁎p < 0.001.
The predictors and outcomes were then incorporated into the LGCM, which exhibited a good fit index (χ 2/df = 2.042, RMSEA = 0.050 (90% CI = [0.034, 0.065]), CFI = 0.957, TLI = 0.940, SRMR = 0.031). The results showed that participants’ risk perception of the COVID-19 pandemic positively predicted their depressive symptoms at each time point. Social support and family functioning at T1 negatively predicted the intercept factor of depressive symptoms. In addition, participants’ smartphone addiction at T1 positively predicted the intercept factor and negatively predicted the slope factor. With respect to the outcomes, we found that the slope factor positively predicted changes in smartphone addiction tendency, and both the intercept and the slope factor of depressive symptoms negatively predicted hope levels at T4 (see Table 3 ).
Table 3.
Parameter estimates from the conditional LGCM.
| Predictors | Outcomes | β | S. E. |
|---|---|---|---|
| T1 Social support | Depression intercept | −0.128⁎⁎ | 0.049 |
| Depression slope | 0.040 | 0.057 | |
| T1 Family functioning | Depression intercept | −0.245⁎⁎⁎ | 0.048 |
| Depression slope | 0.023 | 0.066 | |
| T1 Smartphone addiction tendency | Depression intercept | 0.544⁎⁎⁎ | 0.046 |
| Depression slope | −0.737⁎⁎⁎ | 0.058 | |
| T1 Risk perception | T1 Depressive symptom | 0.155⁎⁎⁎ | 0.031 |
| T2 Risk perception | T2 Depressive symptom | 0.148⁎⁎⁎ | 0.023 |
| T3 Risk perception | T3 Depressive symptom | 0.110⁎⁎⁎ | 0.027 |
| T4 Risk perception | T4 Depressive symptom | 0.095⁎⁎ | 0.034 |
| Depression intercept | △Smartphone addiction tendency | 0.249 | 0.165 |
| Depression slope | 0.881⁎⁎⁎ | 0.123 | |
| Depression intercept | T4 Hope | −0.608⁎⁎⁎ | 0.069 |
| Depression slope | −0.276⁎⁎ | 0.090 |
Note: β = standardized regression coefficients, S. E. = standard errors of the coefficient
*p < 0.05. ⁎⁎p < 0.01. ⁎⁎⁎p < 0.001.
4. Discussion
Exploring the development of college students’ depressive symptoms during the COVID-19 pandemic helps us understand how these symptoms emerge and fluctuate over time. The present study thus investigated the developmental trajectories of depressive symptoms with regard to COVID-19 from its outbreak to the normalization period as well as the potential antecedents and outcomes of such symptoms.
4.1. Developmental trajectories of depressive symptoms
Our findings revealed that Chinese college students initially experienced mild depressive symptoms, which were followed by an overall decreasing trend in subsequent periods. More specifically, we found that their depressive symptoms decreased from T1 to T3 and slightly increased at T4 (compared to T3). These findings were consistent with both theoretical results and the actual situation. During the outbreak of COVID-19, unique pandemic-related stress drastically altered people's mental status (Ellis et al., 2020) and greatly elevated depression levels (Bourmistrova et al., 2022; Schafer et al., 2022). During the basic containment period, the pandemic situation in China was under control, thus, Chinese college students might have exhibited more confidence in the diagnosis and treatment of COVID-19 during this time (Wang et al., 2020b), which helped reduce their depressive symptoms. Thereafter, comprehensive recovery in work and life further changed college students’ lives in terms of increased gratitude and health concerns, resulting in a steady decline in depressive symptoms during the regular control period of COVID-19. During the normalization period, the risks of a second wave and a new peak of infections may have had a rebound effect with regard to depressive symptoms. Some schools were quarantined, and such school closures caused students to experience more depressive symptoms (Grey et al., 2020). College students may also have faced substantially more academic pressure at the end of this term, which caused them to experience more negative emotions. Besides, we found a significant negative relationship between the intercept and the slope of depressive symptoms. This relationship was probably due to the fact that college students who experienced more depressive symptoms during the initial period were more affected by the pandemic, which may reflect their higher environmental sensitivity or limited external support. As the pandemic situation gradually improved, information regarding preventative measures may have reassured individuals with higher levels of depression (Tran et al., 2020). College students were also able to return to normal life with additional support and care, thus leading to a faster decline in depressive symptoms. Furthermore, interindividual variability was observed in relation to the intercept and slope factor of depressive symptoms, which suggested that not all college students experienced a similarly decreasing trajectory. Some individual characteristics were identified as being associated with depressive symptoms during the COVID-19 pandemic, such as gender (Mazza et al., 2020) and initial mental status (Dai et al., 2022). These findings reinforce the need to better understand factors involved in the prediction and outcomes of depressive symptoms trajectories.
4.2. The antecedents and outcomes of depressive symptoms
First, the present study revealed that college students’ risk perception of the COVID-19 pandemic positively predicted their depressive symptoms, and these associations were found to generalize over the whole time period referenced by this study. Our results were convergent with the conclusions of previous research, which has found that higher risk perception causes a higher likelihood of depressive symptoms (Ding et al., 2020). It has been found that information regarding infection and personal interest had a negative impact on people's risk perception of SARS, which might elicit a higher sense of panic and lead to more depressive symptoms (Shi et al., 2003). Additionally, people with limited knowledge of COVID-19 tend to exhibit increased risk perception and thus experience more fear of infection and negative emotions (Zhao et al., 2021).
Second, this study expanded previous studies by showing that the levels of social support during the outbreak of COVID-19 negatively predicted initial depressive symptoms, although no additional relations were observed between social support and the slope of the developmental trajectory. These findings highlight the protective effect of social support in cases of stressful events. During the initial stage of the pandemic, college students with higher social support received more material aid and psychological care, which in turn decreased their depressive symptoms (Li et al., 2020). In addition, our findings provided more empirical evidence to support the buffering effect model of social support. When individuals face stressful events, social support can buffer the potential negative impacts by reducing their unrealistic evaluations and negative emotions (Ding et al., 2005); however, its subsequent role in predicting fluctuations in depressive symptoms appears to be minor. However, due to the limitations entailed by our consideration of social support as a time-invariant predictor, future research should examine these associations using more dynamic measures of social support.
Third, we found that family functioning during the outbreak of COVID-19 negatively predicted the initial level of depressive symptoms rather than its trend. On the one hand, our results, in line with those reported by previous studies, showed that family functioning can protect against depressive symptoms. It was noted that positive relationships and interactions among family members are conducive to reducing college students’ perceived stress and depressive symptoms (Li et al., 2020; Wu et al., 2021), especially during home quarantine. In addition, college students with good family functioning may experience effective emotional regulation and family coping strategies, which are associated with fewer depressive symptoms (Cao et al., 2013; Freed et al., 2016). On the other hand, family functioning was not identified as a predictor of the developmental trajectory of depressive symptoms. This result may be explained by reference to environmental changes. When college students return to campus, they may have fewer connections with their families and spend more time with their classmates or friends. Consequently, the role and importance of family functioning are less evident in this context. Moreover, some families suffered both financial and psychological hardships following this pandemic, which may have had a negative impact on family functioning (Ferrara et al., 2021), thus mitigating its ability to serve as a dynamic predictor of the subsequent development of college students’ depressive symptoms. Previous studies have verified the protective role of family functioning, while the current findings provide further empirical evidence regarding the changing relationship between family functioning and depressive symptoms throughout the development of pandemic situations.
Fourth, the present study revealed that college students with a higher smartphone addiction tendency initially exhibited more depressive symptoms but also that their depressive symptoms declined more quickly. These results suggest that initial levels of smartphone addiction tendency might play two opposing roles in relation to depressive symptoms. During the outbreak of the COVID-19 pandemic, people's problematic smartphone use was found to result in more PTSD symptoms (Hu et al., 2021). The increased amount of time spent on smartphones replaced interpersonal interactions offline, thus leading to a higher risk of anxiety and depression (Zhang et al., 2019). Second, initial levels of smartphone addiction tendency may also predict decreases over time in depressive symptoms because smartphone addicts may receive additional help and pleasure from the internet that allows them to relieve their depression and satisfy their psychological needs. Moreover, the present research documented the reciprocal effect of depressive symptoms on smartphone addiction tendency. Specifically, the slope of the depressive symptoms trajectories positively predicted the changes in smartphone addiction tendency, showing that a slower decrease in depressive symptoms was related to a lower decline in smartphone addiction tendency. As suggested by the I-PACE model (Brand et al., 2016, 2019), college students with a slower decrease in depressive symptoms habitually depend on problematic smartphone use to release their negative emotions and seek pleasure, thereby resulting in a long-lasting risk of smartphone addiction (Jin et al., 2021). Thus, depression may be a salient risk factor with regard to smartphone addiction. Future cross-lagged studies can improve our understanding of the complex interaction between smartphone addiction and depressive symptoms during the COVID-19 pandemic.
Additionally, we explored the potential influence of depressive symptoms on people's hope. Our results showed that both the initial level and the slope of depressive symptoms were negatively associated with college students’ state hope during the COVID-19 normalization period. Hope theory (Synder, 2002) has highlighted the key role of a goal in promoting pathway and agency thinking. College students with more depressive symptoms during the outbreak period tended to have more negative perceptions of themselves (Dai and Feng, 2008) and to engage in less goal setting, which subsequently resulted in a lower level of hope. Previous studies have also demonstrated that patients with depression exhibit much lower levels of hope and emotional self-efficacy (Ren et al., 2018). Moreover, college students with a slower decrease rate of depressive symptoms might immerse themselves in negative emotions for a long time, which is detrimental to the development of hope.
4.3. Limitations and implications
With respect to limitations, we relied on self-report questionnaires, and the baseline data were collected through participants’ recall. The recall data may be influenced by participants’ current status or may be biased due to intense emotions during a certain month. Besides, as this study was based on the context of the changing pandemic situation in China, the generalizability of our conclusions may be limited when applied in other countries due to varying levels of pandemic severity. Finally, with respect to the selection of the antecedents and outcomes, follow-up studies that include a more comprehensive set of variables (e.g., school-related variables such as academic achievement or adjustment to online learning) may be necessary to complement the current findings.
Despite these limitations, the current findings have great significance. This study provides a more detailed picture of the acute and persistent effects of COVID-19 on college students’ depressive symptoms. Additionally, the present study reveals how depressive symptoms changed as the pandemic progressed, thus helping fill the extant research gaps. In addition, our study complements previous findings and adds another piece to the puzzle by uncovering the core determinants and consequences of depressive symptoms in this context. Furthermore, our findings also provide guidance for the prevention and intervention of college students’ mental disorders during public health emergencies from different perspectives (e.g., individual, family, and society). For example, the current study suggests that educators and mental health workers should pay attention to the development of college students’ psychological status under emergencies. In addition, measures should be taken by college authorities to provide more social support and early psychological interventions, so that college students are more competent for future challenges. Secondly, based on the findings of this study regarding family functioning and depressive symptoms, improving family adaptability, emotional connection, and closeness would be an effective way to reduce college students’ depressive symptoms and other mental health problems. Thirdly, the predictive role of risk perception on depressive symptoms highlights the importance of developing a correct perception of the pandemic. Governments should ensure the proper and timely dissemination of COVID-19 related information to prevent panic from rumors and false information, which could help to relieve the psychological impacts of the COVID-19 pandemic on the general public.
5. Conclusions
This study revealed an initially mild and subsequently decreasing trajectory of depressive symptoms. Social support and family functioning were identified as protective factors for depressive symptoms during the pandemic, while college students’ risk perception and smartphone addiction tendency were significantly related to their depressive symptoms. In turn, depressive symptoms were found to be associated with college students’ behavioral (i.e., smartphone addiction tendency) and cognitive-emotional (i.e., hope) responses. As the pandemic remains ongoing, future studies should explore the effects of COVID-19 on college students’ mental health in the postpandemic era.
Funding
This work was supported by the National Natural Science Foundation of China (32000764) and Fundamental Research Funds for the Central Universities of Central China Normal University (CCNU20TS029). The funders had no roles in study design, collection, analysis, or interpretation of the data, decision to publish, or preparation of the manuscript.
CRediT authorship contribution statement
Jiayin Wu: Conceptualization, Investigation, Formal analysis, Writing – original draft, Writing – review & editing. Qinxue Liu: Conceptualization, Methodology, Supervision, Writing – review & editing, Funding acquisition.
Declaration of Competing Interest
No potential competing interest to report.
References
- Alsubaie M.M., Stain H.J., Webster L.A.D., Wadman R. The role of sources of social support on depression and quality of life for university students. Int. J. Adolesc. Youth. 2019;24(4):484–496. doi: 10.1080/02673843.2019.1568887. [DOI] [Google Scholar]
- Banerjee D., Meena K.S. Covid-19 as an “infodemic” in public health: critical role of the social media. Front. Public Health. 2021;9:231. doi: 10.3389/fpubh.2021.610623. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Beavers R., Hampson R.B. The beavers systems model of family functioning. J. Fam. Ther. 2000;22(2):128–143. doi: 10.1111/1467-6427.00143. [DOI] [Google Scholar]
- Boterhoven d.H.K.L., Hafekost J., Lawrence D., Sawyer M.G., Zubrick S.R. Reliability and validity of a short version of the general functioning subscale of the McMaster family assessment device. Fam. Process. 2015;54(1):116–123. doi: 10.1111/famp.12113. [DOI] [PubMed] [Google Scholar]
- Bourmistrova N.W., Solomon T., Braude P., Strawbridge R., Carter B. Long-term effects of COVID-19 on mental health: a systematic review. J. Affect Disord. 2022;299:118–125. doi: 10.1016/j.jad.2021.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand M., Wegmann E., Stark R., Müller A., Wölfling K., Robbins T.W., Potenza M.N. The interaction of person-affect-cognition-execution (I-PACE) model for addictive behaviors: update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neurosci. Biobehav. Rev. 2019;104:1–10. doi: 10.1016/j.neubiorev.2019.06.032. [DOI] [PubMed] [Google Scholar]
- Brand M., Young K.S., Laier C., Wölfling K., Potenza M.N. Integrating psychological and neurobiological considerations regarding the development and maintenance of specific Internet-use disorders: an Interaction of Person-Affect-Cognition-Execution (I-PACE) model. Neurosci. Biobehav. Rev. 2016;71:252–266. doi: 10.1016/j.neubiorev.2016.08.033. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U., Morris P.A. In: Handbook of Child psychology. Damon W., Lerner R.M., editors. Vol. 1. Wiley; New York: 2006. The bioecological model of human development; pp. 793–828. (Theoretical models of Human Development). [Google Scholar]
- Cao X., Jiang X., Li X., Lo M., Li R., Dou X. Perceived family functioning and depression in bereaved parents in China after the 2008 Sichuan earthquake. Arch. Psychiatr. Nurs. 2013;27(4):204–209. doi: 10.1016/j.apnu.2013.04.001. [DOI] [PubMed] [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Feng J., Chen A., Lee J.E., An L. Risk perception of covid-19: a comparative analysis of China and South Korea. Int. J. Disaster Risk Reduct. 2021;61 doi: 10.1016/j.ijdrr.2021.102373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb S. Presidential address-1976. social support as a moderator of life stress. Psychosom. Med. 1976;38:300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- Cohen S., Willis T.A. Stress, social support and the buffering hypothesis. Psychol. Bull. 1985;98(2):307–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- Dai Q., Feng Z. Research of relationship between depression and self-esteem, self-efficacy. Chin. J. Clin. Psychol. 2008;16(3):283–285. doi: 10.16128/j.cnki.1005-3611.2008.03.033. [DOI] [Google Scholar]
- Dai X., Shao Y., Ren L., Tao W., Wang Y. Risk factors of COVID-19 in subjects with and without mental disorders. J. Affect Disord. 2022;297:102–111. doi: 10.1016/j.jad.2021.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Y.J., Hao Y.H., Wu Q.H., Xu W., Wang X.Y., Wang X.F., Chen C.Y., Cao R.X. Establishment and evaluation on reliability and validity of public risk perception scale for public health emergencies. Chin. J. Public Health. 2020;36(2):227–231. doi: 10.11847/zgggws1119744. [DOI] [Google Scholar]
- Ding Y., Xiao L., Guo W., Huang M. Working model of social support in relationship of life events and mental health. Chin. J. Health Psychol. 2005;13(3):161–164. CNKI:SUN:JKXL.0.2005-03-000. [Google Scholar]
- Ding Y., Xu J., Huang S., Li P., Lu C., Xie S. Risk perception and depression in public health crises: evidence from the covid-19 crisis in China. Int. J. Environ. Res. Public Health. 2020;17(16):5728. doi: 10.3390/ijerph17165728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai J.D., Dvorak R.D., Levine J.C., Hall B.J. Problematic smartphone use: a conceptual overview and systematic review of relations with anxiety and depression psychopathology. J. Affect Disord. 2017;207:251–259. doi: 10.1016/j.jad.2016.08.030. [DOI] [PubMed] [Google Scholar]
- Elhai J.D., Yang H., Fang J., Bai X., Hall B.J. Depression and anxiety symptoms are related to problematic smartphone use severity in Chinese young adults: fear of missing out as a mediator. Addict. Behav. 2020;101 doi: 10.1016/j.addbeh.2019.04.020. [DOI] [PubMed] [Google Scholar]
- Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can. J. Behav. Sci. 2020;52(3):177–187. doi: 10.1037/cbs0000215. [DOI] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Galea S. Prevalence of depression symptoms in us adults before and during the COVID-19 pandemic. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrara P., Franceschini G., Corsello G., Mestrovic J., Giardino I., Vural M., Pop T.L., Namazova-Baranova L., Somekh E., Indrio F., Pettoello-Mantovani M. Effects of coronavirus disease 2019 (COVID-19) on family functioning. J. Pediatr. 2021;237:322–323. doi: 10.1016/j.jpeds.2021.06.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freed R.D., Rubenstein L.M., Daryanani I., Olino T.M., Alloy L.B. The relationship between family functioning and adolescent depressive symptoms: the role of emotional clarity. J. Youth Adolesc. 2016;45(3):505–519. doi: 10.1007/s10964-016-0429-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geng Y., Gu J., Wang J., Zhang R. Smartphone addiction and depression, anxiety: the role of bedtime procrastination and self-control. J. Affect. Disord. 2021;293:415–421. doi: 10.1016/j.jad.2021.06.062. [DOI] [PubMed] [Google Scholar]
- Grey I., Arora T., Thomas J., Saneh A., Tohme P., Abi-Habib R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guntzviller L.M., Williamson L.D., Ratcliff C.L. Stress, social support, and mental health among young adult Hispanics. Fam. Community Health. 2020;43(1):82–91. doi: 10.1097/FCH.0000000000000224. [DOI] [PubMed] [Google Scholar]
- Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singap. 2020;49(1):155–160. doi: 10.47102/annals-acadmedsg.202043. [DOI] [PubMed] [Google Scholar]
- Hu T., Wang Y., Lin L., Tang W. The mediating role of daytime sleepiness between problematic smartphone use and post-traumatic symptoms in COVID-19 home-refined adolescents. Child Youth Serv. Rev. 2021;126 doi: 10.1016/j.childyouth.2021.106012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin L., Hao Z., Huang J., Akram H.R., Saeed M.F., Ma H. Depression and anxiety symptoms are associated with problematic smartphone use under the COVID-19 epidemic: the mediation models. Child Youth Serv. Rev. 2021;121 doi: 10.1016/j.childyouth.2020.105875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King C.A., Segal H.G., Naylor M., Evans T. Family functioning and suicidal behavior in adolescent inpatients with mood disorders. J. Am. Acad. Child Adolesc. Psychiatry. 1993;32(6):1198–1206. doi: 10.1097/00004583-199311000-00013. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H., Ahn H., Choi S., Choi W. The sams: smartphone addiction management system and verification. J. Med. Syst. 2014;38(1):1–10. doi: 10.1007/s10916-013-0001-1. [DOI] [PubMed] [Google Scholar]
- Li C., He A., Wang B. Depression, anxiety, stress and its relationship to personalities and family functioning in family isolation persons during outbreak of COVID-19. J. North China Univ. Sci. Technol. (Health Sci. Ed.) 2020;22(3):207–213. CNKI:SUN:MTYX.0.2020-03-010. [Google Scholar]
- Li D.J., Ko N.Y., Chen Y.L., Wang P.W., Lu W.H. COVID-19 related factors associated with sleep disturbance and suicidal thoughts among the Taiwanese public: a Facebook survey. Int J Environ Res Public Health. 2020;17(12):4479. doi: 10.3390/ijerph17124479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y. The correlation between the mental health, coping style of college students: the intermediary role of hope perception. Chin. J. Clin. Psychology. 2021;29(6):1297–1300. doi: 10.16128/j.cnki.1005-3611.2021.06.036. [DOI] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q., Yang Y., Lin Y., Yu S., Zhou Z., K. Smartphone addiction: concepts, measurements, and factors. Chin. J. Clin. Psychol. 2017;25:82–87. doi: 10.16128/j.cnki.1005-3611.2017.01.019. [DOI] [Google Scholar]
- Liu, S. (2020). Time spent on mobile internet in China before and after COVID-19. Retrieved July 23, 2020, from https://www.statista.com/statistics/1105335/china-time-spent-on-mobile-internet-covid-19/.
- Magson N.R., Freeman J., Rapee R.M., Richardson C.E., Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc. 2020;50(1):44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020;17:3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson D.H. Empirical approaches to family assessment. J. Fam. Ther. 2000;22:121–127. [Google Scholar]
- Olson D.H., Russell C.S., Sprenkle D.H. Circumplex model of marital and family systems: Ⅵ. Theoretical update. Fam. Process. 1983;22(1):69–83. doi: 10.1111/j.1545-5300.1983.00069.x. [DOI] [PubMed] [Google Scholar]
- Park S.Y., Yang S., Shin C.S., Jang H., Park S.Y. Long-term symptoms of mobile phone use on mobile phone addiction and depression among Korean adolescents. Int. J. Environ. Res. Public Health. 2019;16:3584. doi: 10.3390/ijerph16193584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peres D., Monteiro J., Almeida M.A., Ladeira R. Risk perception of COVID-19 among the Portuguese healthcare professionals and general population. J. Hosp. Infect. 2020;105(3):434–437. doi: 10.1016/j.jhin.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phan H.P. Examination of self-efficacy and hope: a developmental approach using latent growth modeling. J.. Educ. Res. 2013;106(2):93–104. doi: 10.1080/00220671.2012.667008. [DOI] [Google Scholar]
- Peirce R.S., Frone M.R., Russell M., Cooper M.L., Mudar P. A longitudinal model of social contact, social support, depression, and alcohol use. Health Psychol. 2000;19(1):28–38. doi: 10.1037/0278-6133.19.1.28. [DOI] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Abel K.M. Mental health before and during the covid-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10) doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planchuelo-Gómez Á., Odriozola-González P., Irurtia M.J., de Luis-García R. Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. J. Affect. Disord. 2020;277:842–849. doi: 10.1016/j.jad.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi M., Zhou S.J., Guo Z.C., Zhang L.G., Min H.J., Li X.M., Chen J.X. The effect of social support on mental health in Chinese adolescents during the outbreak of COVID-19. J. Adolesc. Health. 2020;67:514–518. doi: 10.1016/j.jadohealth.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin N., Yan E.C., Lai D.W. Perceived victimization risk, avoidance behavior, and health of community-dwelling older adults in urban China. Aging Ment. Health. 2018;24(1):171–177. doi: 10.1080/13607863.2018.1523879. [DOI] [PubMed] [Google Scholar]
- Ratan Z.A., Zaman S.B., Islam S., Hosseinzadeh H. Smartphone overuse: a hidden crisis in COVID-19. Health Policy Technol. 2021;10:21–22. doi: 10.1016/j.hlpt.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Q., Li Z., Wu H., Lyu Q., Wan Y. Study on the relationship among hope, emotional self-efficacy and psychological distress in the depressed patients. J. Nurs. Admin. 2018;18(4):258–262. doi: 10.3969/j.issn.1671-315x.2018.04.007. [DOI] [Google Scholar]
- Ryan C.E., Keitner G.I. In: Assessment in Rehabilitation and Health. Mpofu E., Oakland T., editors. Person Education Inc; Upper Saddle River, NJ: 2009. Family functioning assessment in rehabilitation and health; pp. 486–502. [Google Scholar]
- Schafer K., M., Lieberman A., Sever A.C., Joiner T. Prevalence rates of anxiety, depressive, and eating pathology symptoms between the pre- and peri-COVID-19 eras: a meta-analysis. J. Affect. Disord. 2022;298:364–372. doi: 10.1016/j.jad.2021.10.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber L., Hops H., Alpert A., Davis B., Andrews J. Family support and conflict: prospective relations to adolescent depression. J. Abnorm. Child Psychol. 1997;25(4):333–344. doi: 10.1023/A:1025768504415. [DOI] [PubMed] [Google Scholar]
- Shi K., Fan H., Jia J., Li W., Song Z., Gao J., Chen X., Lu J., Hu W. The risk perceptions of SARS and socio-psychological behaviors of urban people in China. Acta Psychol. Sin. 2003;35(4):546–554. [Google Scholar]
- Shi K., Hu W.P. Comparative study on risk perception and coping behavior of Beijing residents during SARS period. Chin. J. Clin. Psychol. 2004;12(3):293–295. doi: 10.3969/j.issn.1005-3611.2004.03.027. [DOI] [Google Scholar]
- Slovic P. Perception of risk. Science. 1987;236(4799):280–285. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- Snyder C.R. Conceptualizing, measuring, and nurturing hope. J. Couns. Dev. 1995;73(3):355–360. doi: 10.1002/j.1556-6676.1995.tb01764.x. [DOI] [Google Scholar]
- Snyder C.R. Hope theory: rainbows in the mind. Psychol. Inq. 2002;13:249–275. doi: 10.1207/S15327965PLI1304_01. [DOI] [Google Scholar]
- Snyder C.R., Sympson S.C., Ybasco F.C., Borders T.F., Babyak M.A., Higgins R.L. Development and validation of the state hope scale. J. Pers. Social Psychol. 1996;70(2):321. doi: 10.1037/0022-3514.70.2.321. [DOI] [PubMed] [Google Scholar]
- Stanković M., Nešić M., Čičević S., Shi Z. Association of smartphone use with depression, anxiety, stress, sleep quality, and internet addiction. Empirical evidence from a smartphone application. Pers. Individ. Dif. 2021;168 doi: 10.1016/j.paid.2020.110342. [DOI] [Google Scholar]
- Su S., Pan T.T., Liu Q.X., Chen X.W., Wang Y.J., Li M.Y. Development of the smartphone addiction scale for college students. Chin. Mental Health J. 2014;28(5):392–397. doi: 10.3969/j.issn.1000-6729.2014.05.013. [DOI] [Google Scholar]
- Talevi D., Pacitti F., Socci V., Renzi G., Alessandrini M.C., Trebbi E., Rossi R. The COVID-19 outbreak: impact on mental health and intervention strategies. J. Psychopathol. 2020;26(2):162–168. doi: 10.36148/2284-0249-393. [DOI] [Google Scholar]
- Torales J., O'Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Social Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Tran B.X., Dang A.K., Thai P.K., Le H.T., Le X.T.T., Do T.T.T., Nguyen T.H., Pham H.Q., Phan H.T., Vu G.T., Phung D.T., Nghiem S.H., Nguyen T.H., Tran T.D., Do K.N., Truong D., V., Vu G.V., Latkin C.A., Ho R.C., Ho C.S. Coverage of health information by different sources in communities: implication for COVID-19 epidemic response. Int. J. Environ. Res. Public Health. 2020;17(10):3577. doi: 10.3390/ijerph17103577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino B.N. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J. Behav. Med. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Uchino B.N. Understanding the links between social support and physical health: a life-span perspective with emphasis on the separability of perceived and received support. Perspect. Psychol. Sci. 2009;4:236–255. doi: 10.1111/j.1745-6924.2009.01122.x. [DOI] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. Covid-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2021. Infodemic.https://www.who.int/westernpacific/health-topics/infodemic [Google Scholar]
- Wu Z., Zou Z., Wang F., Xiang Z., Zhu M., Long Y., Tao H., Palaniyappan L., Liu Z. Family functioning as a moderator in the relation between perceived stress and psychotic-like experiences among adolescents during COVID-19. Compr. Psychiatry. 2021;111 doi: 10.1016/j.comppsych.2021.152274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao S.Y. In: Manual of the mental health assessment scale. Ma H., editor. Chinese Mental Health Journal; Beijing: 1999. Social support rating scale; pp. 127–131. [Google Scholar]
- Xie X.F., Xu L.C. Public bias in risk cognition. J. Dev. Psychol. 1996;14(2):23–26. CNKI:SUN:XLXD.0.1996-02-005. [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L., Mcintyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Mo L., Wu Z. A cross-sectional study on risk factors of depression severity among survivors of the 2008 Sichuan earthquake. Community Ment. Health J. 2013;49(6):847–856. doi: 10.1007/s10597-012-9578-y. [DOI] [PubMed] [Google Scholar]
- Yıldırım M., Gülerc A. Positivity explains how COVID-19 perceived risk increases death distress and reduces happiness. Pers. Individ. Dif. 2021;168 doi: 10.1016/j.paid.2020.110347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang B., Xiong S., Xu Y., Chen Y., Xiao C., Mo Y. A meta-analysis of the relationship between mobile phone use and anxiety/depression. Chin. J. Clin. Psychol. 2019;27(6):1144–1150. doi: 10.16128/j.cnki.1005-3611.2019.06.014. [DOI] [Google Scholar]
- Zhao X., Shi W., Li X., Li W., Li C. Autistic traits and negative emotions in the general population during COVID-19: mediating roles of the behavioural immune system and covid-19 risk perception. Psychiatry Res. 2021;300(2) doi: 10.1016/j.psychres.2021.113918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Zhang X., Guo J. A longitudinal study on the effect of family function on the psychological adaptation of the children relocated for poverty alleviation. China J. Health Psychol. 2021 http://kns.cnki.net/kcms/detail/11.5257.R.20210920.0025.008.html [Google Scholar]
- Zheng C., Zhang J., Guo Y., Zhang Y. Disruption and reestablishment of place attachment after large-scale disasters: the role of perceived risk, emotions, and coping. Int. J. Disaster Risk Reduct. 2019;40 doi: 10.1016/j.ijdrr.2019.101273. [DOI] [Google Scholar]