Abstract
Background:
Although residing in lower surrounding greenness and transient exposure to air pollution are independently associated with higher risk of adverse health outcomes, little is known about their interactions.
Objectives:
To estimate whether residential neighborhood greenness modifies the short-term association between air pollution and respiratory mortality among the Chinese Elderly Health Service Cohort in Hong Kong.
Methods:
We estimated residential surrounding greenness by measuring satellite-derived normalized difference vegetation index (NDVI) from Landsat within catchments of residential addresses of participants who died of respiratory diseases between 1998 and 2011. We first dichotomized NDVI into low and high greenness and used a time-stratified case-crossover approach to estimate the percent excess risk of respiratory mortality associated with fine particulate matter (PM2.5), respirable particulate matter (PM10), nitrogen dioxide (NO2), and ozone (O3). We further classified NDVI into greenness quartiles and introduced an interaction term between air pollution and the assigned median values of the NDVI quartiles into the models to assess the trend of greenness modification on the air pollution and respiratory mortality associations.
Results:
Among 3,159 respiratory deaths during the follow-up, 2,058 were pneumonia and 947 were chronic obstructive pulmonary disease. Elders living in the low greenness areas were associated with a higher risk of pneumonia mortality associated with NO2 (p=0.049) and O3 (p=0.025). The mortality risk of pneumonia showed a decreasing trend for NO2 (p for trend=0.041), O3 (p for trend=0.006), and PM2.5 (p for trend=0.034) with greenness quartiles increasing from Quartile 1 (lowest) to Quartile 4 (highest).
Conclusions:
Our findings suggest that elders living in higher greenness areas are less susceptible to pneumonia mortality associated with air pollution, which provides evidence for optimizing allocation, siting, and quality of urban green space to minimize detrimental health effects of air pollution.
Keywords: Air pollution, Greenness, Respiratory disease, Case-Crossover study
Graphical Abstract
1. Introduction
Respiratory disease is a leading cause of disability, morbidity, and mortality, which imposes an immense health burden worldwide (Dicker et al. 2018). More than 1 billion people suffer from either acute or chronic respiratory conditions, and 4 million people die prematurely from the chronic respiratory diseases each year (WHO 2014). Respiratory diseases make up five of the 30 most common causes of death and account for more than 10% of all disability-adjusted life-years (DALYs) (Dicker et al. 2018; Kyu et al. 2018).
Air pollution is an important contributor to respiratory diseases (Li et al. 2016; Pirozzi et al. 2018; Tian and Sun 2017). Although continuous efforts have been made to improve air quality, yet ~90% of the world’s population lives in areas with air quality levels exceeding the World Health Organization (WHO) limits (WHO 2018). Thus, it is of significant public health interest to identify potential modifying factors that could be targeted at for interventions and thereby alleviate the health burden of respiratory diseases associated with air pollution.
Numerous studies have explored how nature, specifically green vegetation, is beneficial to an array of health outcomes (Banay et al. 2017; Fong et al. 2018; James et al. 2015; Sarkar et al. 2019; Twohig-Bennett and Jones 2018; WHO 2017). Greenness may reduce health risks by reducing personal exposure to air pollution (Dadvand et al. 2012; Givoni 1991) and/or providing opportunities to do physical activity, which might make individuals less susceptible to air pollution (James et al. 2015; Van den Berg et al. 2010). Very few studies have investigated the modification effect of greenness on the adverse health effects of air pollution (Table S1), and findings have been mixed (de Keijzer et al. 2017b; Dimitrova and Dzhambov 2016; Dimitrova and Dzhambov 2017; Heo and Bell 2019; Kioumourtzoglou et al. 2016; Vivanco-Hidalgo et al. 2018; Yitshak-Sade et al. 2019). A study conducted in 364 US counties found that risks of cardiovascular hospitalizations associated with particulate matter were reduced in higher greenness areas (Heo and Bell 2019). A small-area study in Spain found that the effect modification of the association between air pollution and all-natural mortality by neighborhood greenness varied by urban and rural areas (de Keijzer et al. 2017b). On the other hand, higher mortality risks of air pollution were found in greater neighborhood greenness in an analysis of over 35 million Medicare enrollees from 207 US cities (Kioumourtzoglou et al. 2016), or no evidence of greenness effect modification was reported in a study in Spain (Vivanco-Hidalgo et al. 2018).
In this study, we aimed to examine the effect modification of greenness on the association between air pollution and respiratory mortality. We hypothesize that higher level of greenness alleviates the respiratory mortality risk associated with air pollution. To test this hypothesis, we conducted a case-crossover study in Hong Kong, leveraging a large prospective elderly cohort, where greenness at the residential address of each deceased participant was quantified by Normalized Difference Vegetation Index (NDVI) measured from satellite imagery.
2. Methods
2.1. Study population
The study population is the participants of the Chinese Elderly Health Service Cohort, which is a prospective cohort initiated by the Hong Kong Department of Health. From 1998 to 2001, 66,820 elders aged 65 years or above in Hong Kong, about 9% of Hong Kong older adults were enrolled into the cohort and were followed up until December 31st, 2011. Demographics and lifestyle information were collected by registered doctors and nurses through face-to-face interviews using a standardized and structured questionnaire (Lam et al. 2007; Schooling et al. 2014). Detailed information on cohort profile and data collection have been described elsewhere (Schooling et al. 2014; Sun et al. 2019a). To ascertain death, we linked the cohort with the death registration database from Department of Health by the unique Hong Kong identity card number and coded deaths according to the International Classification of Diseases, Tenth Revision (ICD-10): total respiratory diseases (J00-J47, J80-J99), pneumonia (J12-J18), and chronic obstructive pulmonary diseases (COPD, J40-J44, J47). Most deaths in Hong Kong occur in hospital and cause of deaths are accurately ascertained (Hospital Authority 2014). For participants whose cause of death cannot be ascertained, telephone interviews have been conducted to obtain this information (Schooling et al. 2014).
2.2. Residential greenness assessment
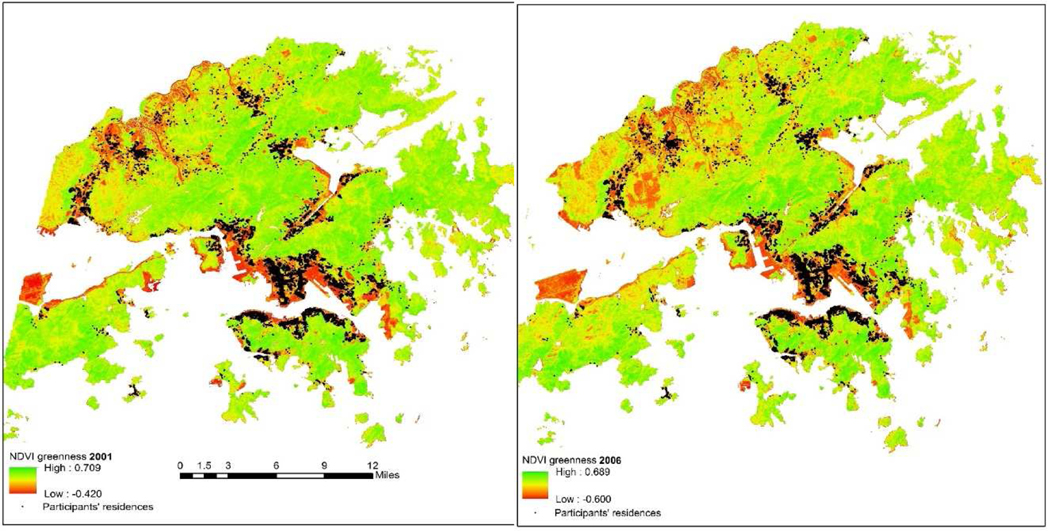
We quantified vegetation greenness by measuring the Normalized Difference Vegetation Index (NDVI), a satellite-image-based vegetation index measured from the differential absorbance and reflectance wavelengths by chlorophyll in green vegetation. NDVI has been widely used as an indicator of green intensity and is measured as the ratio of the difference between the spectral reflectance measurements in the near-infrared region and red (visible) regions of the electromagnetic spectrum and the sum of these two measures. It ranges from −1 to 1, with higher values indicating higher levels of vegetative density (Earth Observatory 2000; Tucker 1979). We obtained NDVI at two time points of 2001 and 2006 from the 30m resolution Landsat 5, Thematic Mapper satellite data (Fig. 1). Image chunks of the area covering Hong Kong were mosaicked, and mean NDVI within a buffer of 250 m (NDVI250m) and 500 m (NDVI500m) radius around each study participant’ geocoded residential address was measured. The 250 m radius is a measure of greenness immediately surrounding the residence (James et al. 2016), and the 500 m radius is a measure of greenness within a walking distance neighborhood of their homes, which was supported by a prior pilot study of this cohort (Cerin et al. 2013).
Fig. 1.
Normalized Difference Vegetation Index (NDVI) greenness of Hong Kong measured from 30m resolution Landsat TM data in 2001 and 2006 and geocoded residential locations of Elderly Health Service Cohort participants (n=66,820).
As the overall temporal vegetation coverage in Hong Kong was generally stable between 2000 and 2011 and the spatial changes were also limited (Hu and Xia 2019), we used the mean of NDVI at the year of 2001 and 2006 as the greenness exposure. We first dichotomized participants into those living in areas with low and high residential greenness based on the NDVI median of the participants who died of respiratory diseases (cases). To investigate whether there was a trend in the air pollution and respiratory mortality association by greenness, we further categorized NDVI into greenness quartiles.
2.3. Air pollution assessment
Hourly concentrations of fine particulate matter (PM2.5), respirable particulate matter (PM10), nitrogen dioxide (NO2), and ozone (O3) between 1998 and 2011 were obtained from ten general air monitoring stations that met the quality assurance and quality control procedure of Hong Kong Government (Sun et al. 2019b). We created a territory-wide daily time-series of air pollutants by averaging daily air pollutants that have ≥75% of the 1 hour values on that particular day across the ten air monitoring stations (Wong et al. 2008). We would exclude the entire station if >25% of the daily values for a particular pollutant were missing for the whole study period.
The daily mean concentrations of air pollution were 37.3μg/m for PM2.5, 52.3μg/m3 for PM10, 57.7μg/m3 for NO2, and 35.2μg/m3 for O3 (Table 1). We found the Pearson correlation between air pollutants were generally high (r>0.5), except for the correlation between O3 and NO2 (r=0.27). Daily ambient temperature (°C) and relative humidity (%) were obtained from the Hong Kong Observatory.
Table 1.
Air pollution concentration on the day of respiratory mortality and Pearson correlation coefficients between air pollutants.
| Air pollutants (μg/m3) | Mean ± SD | Pearson correlation |
|||
|---|---|---|---|---|---|
| PM2.5 | PM10 | NO2 | O3 | ||
| PM2.5 | 37.3 ± 21.2 | 1.00 | 0.91 | 0.76 | 0.46 |
| PM10 | 52.3 ± 28.2 | 1.00 | 0.68 | 0.51 | |
| NO2 | 57.7 ± 20.1 | 1.00 | 0.27 | ||
| O3 | 35.2 ± 20.2 | 1.00 | |||
Abbreviations: SD=standard deviation; PM2.5= particulate matter with aerodynamic diameter ≤ 2.5μm; PM10= particulate matter with aerodynamic diameter ≤ 10μm; NO2=nitrogen dioxide; O3=ozone.
2.4. Statistical analysis
We used a time-stratified case-crossover approach to estimate the short-term association between air pollutants and respiratory deaths. The case-crossover approach is a case-only design in which case serves as his/her own control (Maclure 1991). To control for long-term trend and seasonality, we selected control periods as the same year, month, and day of the week as the case (the event days) (Carracedo-Martínez et al. 2010). We adjusted for variables that fluctuate on a daily basis including ambient temperature at the same day and moving average of the prior 1 to 3 days (lag1–3) with natural cubic splines (NS) with three degrees of freedom (df) each simultaneously in the model (Orazzo et al. 2009; Sun et al. 2020), relative humidity (NS with 3df), influenza epidemics, and public holidays.
As the incubation period of infectious diseases may be 1 to 4 days (Lessler et al. 2009), we estimated the effects of air pollution at the 4-day moving average (lag0–3). We calculated odds ratios (OR) per 10μg/m3 increase in each air pollutant from the conditional logistic regression and expressed results as percent excess risk (ER%; ER%=[OR-1]×100%).
To estimate the differences between risk estimates of air pollution in the low and high greenness, we introduced an interaction term in the models, which was the product of air pollutants and the residential greenness (low and high). p-value of the interaction term <0.05 indicates a statistically significant difference between the risk estimates of air pollution in the low and high greenness areas.
To assess the trend of greenness modification, we further classified NDVI into greenness quartiles: Quartile 1 (lowest), Quartile 2, Quartile 3, and Quartile 4 (highest). We estimated the additional percent excess risk associated with air pollutants in greenness Quartile 2, Quartile 3, and Quartile 4 relative to Quartile 1 by adding an interaction term of the air pollution and greenness quartiles into the models with Quartile 1 as the reference group (Fig. S1) (Sun et al. 2020; Sun et al. 2019b). We tested for a trend in relation to the additional percent excess risks by assigning median values of the NDVI quartiles as a continuous variable in the models (Bhaskaran et al. 2011).
To exclude the possibility of area-level confounding, we conducted a nested case-control study after adjusted for individual- (e.g., age, sex) and area- (e.g., long-term PM2.5 air pollution exposure) level confounders, in addition to the variables that fluctuate on a daily basis (i.e., day of the week, ambient temperature, relative humidity, and influenza epidemics) (Sun et al. 2019b; Sun et al. 2016) (Supplementary Material). We conducted all analyses in R software version 3.5.1 with the “Survival” package version 2.42–6 for the conditional logistic regression.
3. Results
Table 2 shows the baseline characteristics of respiratory cases by residential greenness. We identified 3,159 respiratory deaths (cases), of which 2,058 were pneumonia and 947 were COPD. About half (52.5%) of the respiratory cases were males, and less than one-third were married, overweight or obese, ever-drinker, ever-smokers, or had received secondary or post-secondary education. The characteristics of participants lived in the low and high greenness areas were generally similar.
Table 2.
Descriptive characteristic for participants by residential greenness in the Chinese Elderly Health Service Cohorta.
| Population characteristics | Total | Low greenness | High greenness |
|---|---|---|---|
| Participants, n | 3,159 | 1,579 | 1,580 |
| Age, years, mean (SD) | 84.3 (6.6) | 84.4 (6.6) | 84.3 (6.5) |
| Sex, n (%) | |||
| Male | 1,658 (52.5) | 846 (53.6) | 812 (51.4) |
| Female | 1,501 (47.5) | 733 (46.4) | 768 (48.6) |
| Marital status, n (%) | |||
| Married | 753 (23.8) | 371 (23.5) | 382 (24.2) |
| Unmarried | 2,406 (76.2) | 1,208 (76.5) | 1,198 (75.8) |
| BMI quartile, n (%) | |||
| Underweight [<19.0 kg/m2] | 684 (21.7) | 349 (22.1) | 335 (21.2) |
| Normal [19.0–25.0 kg/m2] | 1,663 (52.6) | 846 (53.6) | 817 (51.7) |
| Overweight [25.0–30.0 kg/m2] | 719 (22.8) | 336 (21.3) | 383 (24.2) |
| Obese [≥30.0 kg/m2] | 93 (2.9) | 48 (3.0) | 45 (2.8) |
| Exercise | |||
| Days per week, mean (SD) | 5.4 (2.8) | 5.4 (2.8) | 5.4 (2.8) |
| Education, n (%) | |||
| Uneducated | 1,392 (44.1) | 623 (39.5) | 769 (48.7) |
| Primary | 1,238 (39.2) | 628 (39.8) | 610 (38.6) |
| Secondary | 426 (13.5) | 255 (16.1) | 171 (10.8) |
| Post-secondary | 103 (3.3) | 73 (4.6) | 30 (1.9) |
| Alcohol consumption, n (%) | |||
| Never drink | 2,088 (66.1) | 1,064 (67.4) | 1,024 (64.8) |
| Former drink | 566 (17.9) | 256 (16.2) | 310 (19.6) |
| Social/seasonal drinker | 370 (11.7) | 193 (12.2) | 177 (11.2) |
| Regular drinker | 135 (4.3) | 66 (4.2) | 69 (4.4) |
| Smoking status, n (%) | |||
| Never | 2,022 (64.0) | 1,033 (65.4) | 989 (62.6) |
| Quit | 889 (28.1) | 432 (27.4) | 457 (28.9) |
| Current | 248 (7.9) | 114 (7.2) | 134 (8.5) |
Abbreviations: BMI=body mass index; SD=standard deviation.
Low and high greenness were defined by the median (0.065) of normalized difference vegetation index within 250m.
The risks of total and pneumonia mortality associated with air pollution were stronger in the low residential greenness areas than that in the high greenness areas (Table 3 & Table S2). For example, when using NDVI250m to define residential greenness, the ER% per 10μg/m3 increase in NO2 at 4-day moving average for total respiratory was 3.39% (95% CI: −1.26%, 8.05%) in the low greenness areas and −1.21% (95% CI: −5.92%, 3.51%) in the high greenness areas, and for pneumonia was 4.58% (95% CI: −1.23%, 10.41%) in the low greenness areas and −3.22% (95% CI: −9.15%, 2.75%) in the high residential greenness areas, respectively. The difference between the ERs% of pneumonia in the low and high residential greenness was statistically significant for NO2 (p=0.049) and O3 (p=0.025), and was marginally significant (p=0.075) for PM2.5.
Table 3.
Percent excess risk and 95% confidence interval of respiratory mortality per 10μg/m3 increase in air pollutants at 4-day moving average in the low and high residential greenness areas measured by normalized difference vegetation index with 250ma.
| Mortality | Air pollutant | Low greennessa | High greennessa | p-Value |
|---|---|---|---|---|
| Total respiratory | PM2.5 | 1.61 (−2.77, 6.01) | −1.49 (−5.92, 2.95) | 0.311 |
| PM10 | 0.79 (−2.31, 3.90) | −0.66 (−3.80, 2.49) | 0.505 | |
| NO2 | 3.39 (−1.26, 8.05) | −1.21 (−5.92, 3.51) | 0.146 | |
| O3 | 2.08 (−2.33, 6.50) | −2.10 (−6.58, 2.39) | 0.167 | |
| Pneumonia | PM2.5 | 3.25 (−2.25, 8.79) | −3.57 (−9.06, 1.95) | 0.075 |
| PM10 | 1.62 (−2.16, 5.42) | −1.87 (−5.66, 1.94) | 0.186 | |
| NO2 | 4.58 (−1.23, 10.41) | −3.22 (−9.15, 2.75) | 0.049 | |
| O3 | 3.12 (−2.31, 8.59) | −5.20 (−10.68, 0.31) | 0.025 | |
| COPD | PM2.5 | 0.11 (−7.76, 8.05) | 6.03 (−2.18, 14.30) | 0.292 |
| PM10 | 0.81 (−4.85, 6.51) | 4.47 (−1.92, 10.90) | 0.382 | |
| NO2 | 1.39 (−7.04, 9.88) | 7.99 (−0.33, 16.38) | 0.248 | |
| O3 | 0.52 (−7.56, 8.67) | 6.16 (−2.24, 14.62) | 0.315 |
Abbreviations: PM2.5=particulate matter ≤2.5μm in aerodynamic diameter; PM10=particulate matter ≤10μm in aerodynamic diameter; NO2=nitrogen dioxide; O3=ozone; COPD=chronic obstructive pulmonary disease.
Low and high greenness were defined by the median (0.065) of normalized difference vegetation index within 250m.
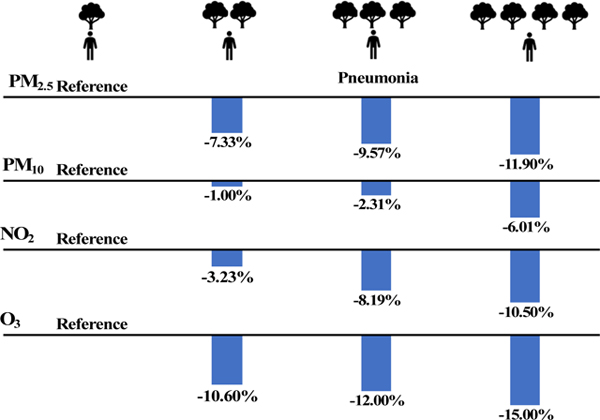
After categorized NDVI into greenness quartiles, we found higher greenness quartiles were generally associated with lower air pollution risk estimates (Table 4 & Table S3). For example, when compared to greenness Quartile 1 (lowest) defined by NDVI250m, the additional percent excess risk of pneumonia per 10 μg/m3 in air pollutants in greenness Quartile 2, Quartile 3, and Quartile 4 was −3.23% (95% CI: −13.90%, 7.54%), −8.19% (95% CI: −19.00%, 2.74%), and −10.50% (95% CI: −21.30%, 0.36%) for NO2, and −10.60% (95% CI: −20.70%, −0.46%), −12.00% (95% CI: −22.00%, −1.88%), and −15.00% (95% CI: −25.10%, −4.72%) for O3, respectively. We observed a decreasing trend in risk estimates of pneumonia for PM2.5 (p for trend=0.034), NO2 (p for trend=0.041), and O3 (p for trend=0.006) with greenness quartiles increasing from Quartile 1 (lowest) to Quartile 4 (highest). However, we found no obvious trend for total respiratory and COPD. Our findings were not materially different when using NDVI500m to define residential greenness or using the nested case-control study to rule out the possibility of area-level confounders (Table S2 to Table S4).
Table 4.
Additional percent excess risk in respiratory mortality associated with 10μg/m3 increase in air pollutants at the 4-day moving average by greenness quartiles within 250m.
| Mortality | Air pollutant | Quartile 1 (lowest) | Quartile 2 | Quartile 3 | Quartile 4 (highest) | p for trend |
|---|---|---|---|---|---|---|
| Total respiratory | PM2.5 | Reference | −6.52 (−14.90, 1.91) | −7.86 (−16.30, 0.67) | −5.13 (−13.70, 3.49) | 0.281 |
| PM10 | Reference | −1.81 (−7.74, 4.16) | −2.49 (−8.42, 3.48) | −2.24 (−8.32, 3.88) | 0.471 | |
| NO2 | Reference | −3.88 (−12.50, 4.80) | −9.12 (−17.80, −0.32) | −4.06 (−12.70, 4.61) | 0.287 | |
| O3 | Reference | −9.79 (−18.00, −1.54) | −9.49 (−17.70, −1.18) | −8.48 (−16.70, −0.20) | 0.070 | |
| Pneumonia | PM2.5 | Reference | −7.33 (−17.80, 3.25) | −9.57 (−20.20, 1.13) | −11.90 (−22.60, −1.10) | 0.034 |
| PM10 | Reference | −1.00 (−8.25, 6.30) | −2.31 (−9.45, 4.88) | −6.01 (−13.60, 1.58) | 0.105 | |
| NO2 | Reference | −3.23 (−13.90, 7.54) | −8.19 (−19.00, 2.74) | −10.50 (−21.30, 0.36) | 0.041 | |
| O3 | Reference | −10.60 (−20.70, −0.46) | −12.00 (−22.00, −1.88) | −15.00 (−25.10, −4.72) | 0.006 | |
| COPD | PM2.5 | Reference | −6.74 (−21.80, 8.58) | −4.69 (−19.90, 10.80) | 10.30 (−5.40, 26.30) | 0.175 |
| PM10 | Reference | −3.06 (−13.90, 7.89) | −3.09 (−14.60, 8.58) | 7.02 (−4.36, 18.50) | 0.237 | |
| NO2 | Reference | −6.39 (−22.20, 9.63) | −6.43 (−22.30, 9.74) | 12.00 (−3.47, 27.70) | 0.098 | |
| O3 | Reference | −7.90 (−22.90, 7.34) | −1.99 (−17.70, 14.00) | 4.66 (−10.40, 19.90) | 0.385 |
Abbreviations: PM2.5=particulate matter ≤2.5μm in aerodynamic diameter; PM10=particulate matter ≤10μm in aerodynamic diameter; NO2=nitrogen dioxide; O3=ozone; COPD=chronic obstructive pulmonary disease.
4. Discussion
Among respiratory deaths in this large prospective cohort of elders in Hong Kong, we found that higher level of residential greenness alleviated the short-term association between air pollution and respiratory mortality. The reduced risks in relation to residential greenness were more pronounced for the mortality risk of pneumonia associated with PM2.5, NO2, and O3.
Few studies have been conducted to examine the interaction between residential greenness and air pollution on health (de Keijzer et al. 2017a; Dimitrova and Dzhambov 2017; Heo and Bell 2019; Kioumourtzoglou et al. 2016; Vivanco-Hidalgo et al. 2018; Yitshak-Sade et al. 2019). Our study is the first to examine the modification effects of residential greenness on the association between transient exposure to air pollution and respiratory mortality. Although no study was directly comparable, our findings were consistent with the United States study conducted by Yitshak-Sade et al. (2019), who found the association between acute air pollution exposure and cardiovascular mortality was alleviated by greater greenness in areas with lower socioeconomic status (Yitshak-Sade et al. 2019). Our findings were also in line with a US study using data of Medicare enrollees from 364 US counties (Heo and Bell 2019). A Canada study examined whether the long-term health effects of air pollution differed by residential greenness (de Keijzer et al. 2017a). Interestingly, this study found that residential greenness modified the adverse effects of air pollutants with stronger long-term effects of PM10, PM2.5, and O3 in rural areas with lower NDVI-measured greenness, but the effects were stronger in urban areas with higher greenness (de Keijzer et al. 2017a). The study also found that the effects of NO2 were consistently stronger in areas with higher greenness in both urban and rural areas (de Keijzer et al. 2017a). On the other hand, higher mortality risks of air pollution were found in greater neighborhood greenness in an analysis of over 35 million Medicare enrollees from 207 US cities (Kioumourtzoglou et al. 2016), or no evidence of greenness effect modification was reported in a study in Spain (Vivanco-Hidalgo et al. 2018). The mixed results in prior studies may be plausibly due to differences in population characteristics, sources of air pollution, greenness quality, as well as differences in perceived and usage of greenness space (Feng and Astell-Burt 2019).
Although the exact biological mechanisms remain largely unclear, several potential pathways have been proposed to explain the observed interactions. Air pollution may lead to impairing epithelial cells, increasing epithelial permeability and reducing mucociliary clearance, which may confer susceptibility to bacterial pathogens (Chauhan and Johnston 2003; Olivieri and Scoditti 2005; Zhou and Kobzik 2007). The observed interaction might also relate to the reduction in personal exposure to air pollution through direct filtering of air pollutants by vegetation or through improving ventilation in greener areas resulting in increased dispersal of air pollutants (Dadvand et al. 2012; James et al. 2016; Shen and Lung 2017). Another possible pathway is that greenness might influence urban microclimate, potentially decreasing the total intake of airborne pollutants (Dadvand et al. 2012; Givoni 1991; Gordon 2003). Greenness is also likely to boost immune functions by promoting physical activity and social engagement, and by improving mental health, rendering people less susceptible to air pollution (James et al. 2015; Van den Berg et al. 2010).
Our study has several potential limitations. First, some degrees of measurement errors may be introduced due to using the territory-wide average air pollution or the residential greenness to represent participants’ exposure. However, our study population is elders and their daily activities mostly occur within a 500 m buffer around the participant’s home (Cerin et al. 2013). Also, the correlation of air pollutants among the ten air monitoring stations in Hong Kong was generally high (Fig. S2 to Fig. S5). Thus, potential exposure misclassification should be negligible. Second, our analysis was conducted among Chinese older adults; whether our findings are generalizable to younger people or Western countries remains unknown. Further studies in diverse geographical contexts and population sub-groups are recommended. Last but not least, we measured greenness using NDVI which only measured the quantity instead of the quality of greenness space. Nevertheless, as far as the authors are aware, our study is the first to examine the interaction between short-term exposure to air pollution and residential greenness leveraging a large prospective cohort. Findings of this study may provide evidence in support of greening policy formulation, urban planning and public health promotion.
5. Conclusions
Among Hong Kong older adults, we found elders living in neighborhoods with greater greenness were associated with lower mortality risks of air pollution on respiratory diseases, which may be useful when arguing for urban greening strategies. These results exemplify the importance of optimizing allocation and designing green spaces as a public health intervention aimed at minimizing/offsetting personal risks posed by exposures to air pollutants in high density urban environments like Hong Kong. From an urban perspective, there is a need for smarter design and configuration of good quality urban greenspaces, given their evidenced potential to reduce pollution loads through multiple mechanisms of adsorption, deposition, dispersion as well as facilitating ventilation corridors for outward pollutant flows. This will also entail a tighter coupling between existing air pollution control, green design, urban transport and public health policies. From a population perspective, with the increasing demographic shifts towards an elderly population, the role of urban green ameliorating and segregating the risks of air pollution in residential neighbourhoods is likely to be more important among the elderly population who are generally prone to co-morbidities and a higher risk of mortality. Future studies from diverse contexts and population sub-groups are required for an integrated green allocation-oriented pollution prevention as a population level intervention.
Supplementary Material
Highlights.
We examined the interaction between greenness and air pollution on respiratory mortality among HK elders.
Elders residing in greater greenness areas are less susceptible to acute air pollution.
Our findings provide evidence for optimizing greenness in a urban environment.
Acknowledgements
We would like to thank the Elderly Health Service, Environmental Protection Department, and Hong Kong Observatory for providing us the data required in this study. CS acknowledges the National Academy of Medicine–Hong Kong University fellowship in Global Health Leadership.
Source of support:
This research was supported by NCI grant R00 CA201542.
Footnotes
Declarations of interest: None.
Conflict of Interest: The authors declare they have no actual or potential conflict of interest
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Banay RF; Bezold CP; James P; Hart JE; Laden F. Residential greenness: current perspectives on its impact on maternal health and pregnancy outcomes. Int J Women’s Health 2017;9:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhaskaran K; Hajat S; Armstrong B; Haines A; Herrett E; Wilkinson P; Smeeth L. The effects of hourly differences in air pollution on the risk of myocardial infarction: case crossover analysis of the MINAP database. BMJ 2011;343:d5531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carracedo-Martínez E; Taracido M; Tobias A; Saez M; Figueiras A. Case-crossover analysis of air pollution health effects: a systematic review of methodology and application. Environ Health Perspect 2010;118:1173–1182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerin E; Lee K.-y.; Barnett A; Sit CH; Cheung M.-c.; Chan W.-m.; Johnston JM Walking for transportation in Hong Kong Chinese urban elders: a cross-sectional study on what destinations matter and when. Int J Behav Nutr Phys Act 2013;10:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan AJ; Johnston SL Air pollution and infection in respiratory illness. Br Med Bull 2003;68:95–112 [DOI] [PubMed] [Google Scholar]
- Dadvand P; de Nazelle A; Triguero-Mas M; Schembari A; Cirach M; Amoly E; Figueras F; Basagaña X; Ostro B; Nieuwenhuijsen M. Surrounding greenness and exposure to air pollution during pregnancy: an analysis of personal monitoring data. Environ Health Perspect 2012;120:1286–1290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Keijzer C; Agis D; Ambrós A; Arévalo G; Baldasano JM; Bande S; Barrera-Gómez J; Benach J; Cirach M; Dadvand P. The association of air pollution and greenness with mortality and life expectancy in Spain: A small-area study. Environ Int 2017a;99:170–176 [DOI] [PubMed] [Google Scholar]
- de Keijzer C; Agis D; Ambros A; Arevalo G; Baldasano JM; Bande S; Barrera-Gomez J; Benach J; Cirach M; Dadvand P; Ghigo S; Martinez-Solanas E; Nieuwenhuijsen M; Cadum E; Basagana X; group M-HS The association of air pollution and greenness with mortality and life expectancy in Spain: A small-area study. Environ Int 2017b;99:170–176 [DOI] [PubMed] [Google Scholar]
- Dicker D; Nguyen G; Abate D; Abate KH; Abay SM; Abbafati C; Abbasi N; Abbastabar H; Abd-Allah F; Abdela J. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1684–1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitrova D; Dzhambov A. Is there an association between urban greenness and air pollution annoyance? Scr Sci Salut Publicae 2016;2 [Google Scholar]
- Dimitrova DD; Dzhambov AM. Perceived access to recreational/green areas as an effect modifier of the relationship between health and neighbourhood noise/air quality: Results from the 3rd European Quality of Life Survey (EQLS, 2011–2012). Urban Forestry & Urban Greening 2017;23:54–60 [Google Scholar]
- Earth Observatory. Measuring vegetation (NDVI&EVI): Normalized Difference Vegetation Index (NDVI). 2000 [Google Scholar]
- Feng X; Astell-Burt T. Can green space quantity and quality help prevent postpartum weight gain? A longitudinal study. J Epidemiol Community Health 2019;73:295–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong KC; Hart JE; James P. A review of epidemiologic studies on greenness and health: Updated literature through 2017. Curr Environ Health Rep 2018;5:77–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Givoni B. Impact of planted areas on urban environmental quality: a review. Atmospheric Environment Part B Urban Atmosphere 1991;25:289–299 [Google Scholar]
- Gordon CJ Role of environmental stress in the physiological response to chemical toxicants. Environ Res 2003;92:1–7 [DOI] [PubMed] [Google Scholar]
- Heo S; Bell ML The influence of green space on the short-term effects of particulate matter on hospitalization in the U.S. for 2000–2013. Environ Res 2019;174:61–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hospital Authority Hospital Authority Statistical Report: 2012–2013. 2014. http://www3.ha.org.hk/data/HAStatistics/DownloadReport/6.2014
- Hu M; Xia B. A significant increase in the normalized difference vegetation index during the rapid economic development in the Pearl River Delta of China. Land Degrad Dev 2019;30:359–370 [Google Scholar]
- James P; Banay RF; Hart JE; Laden F. A review of the health benefits of greenness. Curr Epidemiol Rep 2015;2:131–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James P; Hart JE; Banay RF; Laden F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect 2016;124:1344–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kioumourtzoglou MA; Schwartz J; James P; Dominici F; Zanobetti A. PM2.5 and Mortality in 207 US Cities: Modification by Temperature and City Characteristics. Epidemiology 2016;27:221–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyu HH; Abate D; Abate KH; Abay SM; Abbafati C; Abbasi N; Abbastabar H; Abd-Allah F; Abdela J; Abdelalim A. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1859–1922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam TH; Li ZB; Ho SY; Chan WM; Ho KS; Tham MK; Cowling BJ; Schooling CM; Leung GM Smoking, quitting and mortality in an elderly cohort of 56 000 Hong Kong Chinese. Tob Control 2007;16:182–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessler J; Reich NG; Brookmeyer R; Perl TM; Nelson KE; Cummings DA Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis 2009;9:291–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J; Sun S; Tang R; Qiu H; Huang Q; Mason TG; Tian L. Major air pollutants and risk of COPD exacerbations: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2016;11:3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 1991;133:144–153 [DOI] [PubMed] [Google Scholar]
- Olivieri D; Scoditti E. Impact of environmental factors on lung defences. Eur Respir Rev 2005;14:51–56 [Google Scholar]
- Orazzo F; Nespoli L; Ito K; Tassinari D; Giardina D; Funis M; Cecchi A; Trapani C; Forgeschi G; Vignini M. Air pollution, aeroallergens, and emergency room visits for acute respiratory diseases and gastroenteric disorders among young children in six Italian cities. Environ Health Perspect 2009;117:1780–1785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirozzi CS; Jones BE; VanDerslice JA; Zhang Y; Paine III R; Dean NC Short-Term Air Pollution and Incident Pneumonia. A Case–Crossover Study. Ann Am Thorac Soc 2018;15:449–459 [DOI] [PubMed] [Google Scholar]
- Sarkar C; Zhang B; Ni M; Kumari S; Bauermeister S; Gallacher J; Webster C. Environmental correlates of chronic obstructive pulmonary disease in 96 779 participants from the UK Biobank: a cross-sectional, observational study. Lancet Planet Health 2019;3:e478–e490 [DOI] [PubMed] [Google Scholar]
- Schooling C; Chan W; Leung S; Lam T; Lee S; Shen C; Leung J; Leung G. Cohort profile: Hong Kong Department of Health elderly health service cohort. Int J Epidemiol 2014;45:64–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Y-S; Lung S-CCJSR Mediation pathways and effects of green structures on respiratory mortality via reducing air pollution. 2017;7:42854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S; Cao W; Chan K-P; Ran J; Ge Y; Zhang Y; Feng Y; Zeng Q; Lee R.S.-y.; Wong C-M Cigarette smoking increases deaths associated with air pollution in Hong Kong. Atmos Environ 2020:117266 [Google Scholar]
- Sun S; Cao W; Qiu H; Ran J; Lin H; Shen C; Siu-Yin Lee R; Tian L. Benefits of physical activity not affected by air pollution: a prospective cohort study. Int J Epidemiol 2019a; [DOI] [PubMed] [Google Scholar]
- Sun S; Tian L; Cao W; Lai P-C; Wong PPY; Lee R.S.-y.; Mason TG; Krämer A; Wong C-M Urban climate modified short-term association of air pollution with pneumonia mortality in Hong Kong. Sci Total Environ 2019b;646:618–624 [DOI] [PubMed] [Google Scholar]
- Su S; Tia L; Qi H; Cha K-P; Tsan H; Tan R; Le R.S.-y.; Thach T-Q; Wong C-M The influence of pre-existing health conditions on short-term mortality risks of temperature: Evidence from a prospective Chinese elderly cohort in Hong Kong. Environ Res 2016;148:7–14 [DOI] [PubMed] [Google Scholar]
- Tian L; Sun S. Comparison of Health Impact of Air Pollution Between China and Other Countries. Ambient Air Pollution and Health Impact in China: Springer; 2017 [DOI] [PubMed] [Google Scholar]
- Tucker CJ Red and photographic infrared linear combinations for monitoring vegetation. Remote Sens Environ 1979;8:127–150 [Google Scholar]
- Twohig-Bennett C; Jones A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ Res 2018;166:628–637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Berg AE; Maas J; Verheij RA; Groenewegen PP Green space as a buffer between stressful life events and health. Soc Sci Med 2010;70:1203–1210 [DOI] [PubMed] [Google Scholar]
- Vivanco-Hidalgo RM; Wellenius GA; Basagana X; Cirach M; Gonzalez AG; Ceballos P; Zabalza A; Jimenez-Conde J; Soriano-Tarraga C; Giralt-Steinhauer E; Alastuey A; Querol X; Sunyer J; Roquer J. Short-term exposure to traffic-related air pollution and ischemic stroke onset in Barcelona, Spain. Environ Res 2018;162:160–165 [DOI] [PubMed] [Google Scholar]
- WHO. Global status report on noncommunicable diseases 2014. World Health Organization; 2014 [Google Scholar]
- WHO. Urban Green Space Interventions and Health—A Review of Impacts and Effectiveness. WHO: Geneva, Switzerland: 2017; [Google Scholar]
- WHO. Ambient air pollution - a major threat to health and climate. 2018
- Wong C-M; Vichit-Vadakan N; Kan H; Qian Z. Public Health and Air Pollution in Asia (PAPA): a multicity study of short-term effects of air pollution on mortality. Environ Health Perspect 2008;116:1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yitshak-Sade M; James P; Kloog I; Hart JE; Schwartz JD; Laden F; Lane KJ; Fabian MP; Fong KC; Zanobetti A. Neighborhood Greenness Attenuates the Adverse Effect of PM2.5 on Cardiovascular Mortality in Neighborhoods of Lower Socioeconomic Status. Int J Environ Res Public Health 2019;16:814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou H; Kobzik L. Effect of concentrated ambient particles on macrophage phagocytosis and killing of Streptococcus pneumoniae. Am J Respir Cell Mol Biol 2007;36:460–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.