Summary
Background
Tracking progress and providing timely evidence is a fundamental step forward for countries to remain aligned with the targets set by WHO to eliminate cervical cancer as a public health problem (ie, to reduce the incidence of the disease below a threshold of 4 cases per 100 000 women-years). We aimed to assess the extent of global inequalities in cervical cancer incidence and mortality, based on The Global Cancer Observatory (GLOBOCAN) 2020 estimates, including geographical and socioeconomic development, and temporal aspects.
Methods
For this analysis, we used the GLOBOCAN 2020 database to estimate the age-specific and age-standardised incidence and mortality rates of cervical cancer per 100 000 women-years for 185 countries or territories aggregated across the 20 UN-defined world regions, and by four-tier levels of the Human Development Index (HDI). Time trends (1988–2017) in incidence were extracted from the Cancer Incidence in Five Continents (CI5) plus database. Mortality estimates were obtained using the most recent national vital registration data from WHO.
Findings
Globally in 2020, there were an estimated 604 127 cervical cancer cases and 341 831 deaths, with a corresponding age-standardised incidence of 13·3 cases per 100 000 women-years (95% CI 13·3–13·3) and mortality rate of 7·2 deaths per 100 000 women-years (95% CI 7·2–7·3). Cervical cancer incidence ranged from 2·2 (1·9–2·4) in Iraq to 84·6 (74·8–94·3) in Eswatini. Mortality rates ranged from 1·0 (0·8–1·2) in Switzerland to 55·7 (47·7–63·7) in Eswatini. Age-standardised incidence was highest in Malawi (67·9 [95% CI 65·7 –70·1]) and Zambia (65·5 [63·0–67·9]) in Africa, Bolivia (36·6 [35·0–38·2]) and Paraguay (34·1 [32·1–36·1]) in Latin America, Maldives (24·5 [17·0–32·0]) and Indonesia (24·4 [24·2–24·7]) in Asia, and Fiji (29·8 [24·7–35·0]) and Papua New Guinea (29·2 [27·3–31·0]) in Melanesia. A clear socioeconomic gradient exists in cervical cancer, with decreasing rates as HDI increased. Incidence was three times higher in countries with low HDI than countries with very high HDI, whereas mortality rates were six times higher in low HDI countries versus very high HDI countries. In 2020 estimates, a general decline in incidence was observed in most countries of the world with representative trend data, with incidence becoming stable at relatively low levels around 2005 in several high-income countries. By contrast, in the same period incidence increased in some countries in eastern Africa and eastern Europe. We observed different patterns of age-specific incidence between countries with well developed population-based screening and treatment services (eg, Sweden, Australia, and the UK) and countries with insufficient and opportunistic services (eg, Colombia, India, and Uganda).
Interpretation
The burden of cervical cancer remains high in many parts of the world, and in most countries, the incidence and mortality of the disease remain much higher than the threshold set by the WHO initiative on cervical cancer elimination. We identified substantial geographical and socioeconomic inequalities in cervical cancer globally, with a clear gradient of increasing rates for countries with lower levels of human development. Our study provides timely evidence and impetus for future strategies that prioritise and accelerate progress towards the WHO elimination targets and, in so doing, address the marked variations in the global cervical cancer landscape today.
Funding
French Institut National du Cancer, Horizon 2020 Framework Programme for Research and Innovation of the European Commission; and EU4Health Programme.
Research in context.
Evidence before this study
We searched PubMed from database inception to April 14, 2022, without language restrictions, for previously published studies addressing cervical cancer patterns and trends using the following combination of words in titles or abstracts: “cervical cancer”, “incidence”, “mortality”, “trend”, “age-specific rates”. We also reviewed references from retrieved articles to identify additional studies, yielding a total of 264 studies, supplemented with an additional four articles that were addedon the basis of reviewer's suggestions. Published studies have reported that despite cervical cancer incidence falling in many countries and world regions, incidence is increasing in some settings, including some countries in eastern Africa and western Asia. Studies have reported a continuous increase in the number of new cases globally, with the majority of cases and deaths concentrated in low-income and middle-income countries, where progress to reduce the burden has been negligible relative to their high-income counterparts. Following the launch of the WHO Cervical Cancer Elimination Initiative (CCEI), with a goal to reduce incidence to the threshold of 4 cases per 100 000 women-years or fewer in every country of the world, it is important to establish baseline statistics to monitor progress as the CCEI scales up. Baseline assessment includes the monitoring of the geographical, temporal, and socioeconomic evolution of cervical cancer, and how the risk of the disease evolves with age in settings with or without organised population-based screening programmes.
Added value of this study
We have benchmarked countries and regions worldwide with respect to the goal set by the CCEI, and by providing a comprehensive, up-to-date picture of the extent of global inequalities. The GLOBOCAN 2020 estimates indicate that large between-region and within-region variations exist in cervical cancer incidence at the national level, with a 40–50 times difference in incidence (ranging from 2 to 84 cases per 100 000 women) and mortality rates (ranging from 1 to 56 cases per 100 000 women). Incidence for 172 of 185 countries or territories included in this analysis exceeded the threshold set by the CCEI. We confirmed findings of a clear socioeconomic gradient in incidence and mortality, with progressively lower rates observed as national Human Development Index values increase. We demonstrated that the progress in reducing the cervical cancer burden has been heavily imbalanced across countries and world regions in the past two decades, with the positive impact of mass population-based screening programmes exclusively visible in high-income countries. This study provides timely evidence and impetus for national strategies that tackle the increasing burden of cervical cancer now, and in future decades.
Implications of all the available evidence
This study emphasizes the equitable allocation of resources and access to services as key elements in reducing inequalities in cervical cancer outcomes. Within the ultimate aim of the CCEI to reduce cervical cancer incidence below a threshold of 4 cases per 100 000 women-years, the sustainable expansion of population-based cancer registries in every country of the world represents a crucial gold standard in monitoring progress in meeting the 90–70–90 targets as part of national scale-up the elimination strategy.
Introduction
Cervical cancer is a global public health problem, with a particularly high burden in many low-income and middle-income countries (LMICs). The proven effectiveness of intervention measures, such as vaccination against the most oncogenic human papilloma virus (HPV) types1 (the central cause of cervical cancer) and screening, particularly with HPV-based methods, makes cervical cancer a largely preventable disease.2 However, progress in terms of a reduction in cervical cancer incidence and mortality, has thus far been observed predominantly in countries with a high Human Development Index (HDI), where high-quality screening, timely treatment, and follow-up care services are routinely available. In LMICs, where the vast majority of cases and deaths occur, progress in reducing incidence and mortality has been slow, with a number of countries reporting increases in incidence or mortality rates in the past decade.3, 4, 5, 6, 7
In 2020, WHO launched the global Cervical Cancer Elimination Initiative to accelerate the elimination of cervical cancer,8 aiming to reduce incidence below a threshold of 4 cases per 100 000 women-years in every country and thus narrow international disparities associated with this disease. The 90–70–90 target set by the initiative to be achieved by 2030 requires 90% of girls to be vaccinated by age 15 years, 70% of women to be screened with a high-performance test at least two times by age 45 years, and 90% of women identified with cervical precancer or cancer to be treated. The WHO elimination strategy has emphasized the need for continuous and improved surveillance and monitoring for cervical cancer as a fundamental step forward for action that will enable programme managers to identify gaps and take specific actions.8
Cancer incidence and mortality data collated by the International Agency for Research on Cancer (IARC) provides an opportunity to estimate the burden of cervical cancer between countries and world regions across several decades. Thus, in this study, we aimed to assess the global epidemiological landscape of cervical cancer in 2020 across several axes, including geographical and socioeconomic development, and considering the temporal dynamics, using high-quality databases.
Methods
Study design and data sources
We extracted the number of cases of and deaths from cancer of the cervix (International Classification of Diseases tenth revision code C539) for 185 countries or territories in 2020 from the Global Cancer Observatory (GLOBOCAN) database, as collated by IARC. The GLOBOCAN estimates are derived from the best available recorded data from national (or subnational) cancer registries and national vital registry systems in countries of the world. The data sources and hierarchy of methods used to compile the cancer estimates have been described previously,10 and data sources per country are available online.
Briefly, the incidence estimates for 2020 for 185 countries or territories were derived from national or subnational population-based cancer registry data including submissions to the eleventh volume of Cancer Incidence in Five Continents (CI5; 2008–2012),11 and from members of the African Cancer Registry Network in sub-Saharan Africa. The methods used to estimate the global incidence and mortality rates in 2020 have been published previously10 and uncertainty intervals for the estimates are available online.
Time trends of cervical cancer incidence for the period 1988–2017 (availability of data within this period varied by country; appendix p 7), recorded by one or more subnational or national population-based cancer registries included in the CI5 plus database, were retrieved from the Global Cancer Observatory website. For Uganda, the USA, the UK (England and Wales), Australia, Denmark, Iceland, Norway, Sweden, and Ukraine, cancer data were available up to year 2017. We obtained mortality estimates using the most recent national vital registration data from WHO.12 We extracted corresponding population data from the UN website.13
Statistical analysis
We calculated the estimated number of cervical cancer cases and deaths in each country by applying the estimated age-specific rates for 2020 to the corresponding population strata. Data were aggregated by 5-year age group (0–4, 5–9, ..., 80–84 years), with the exception of the oldest age group, which was an open category comprising women aged 85 years or older.
We calculated the age-standardised incidence or mortality rate per 100 000 women-years based on the 1966 Segi-Doll World standard population.14, 15 The estimated annual percentage change (EAPC) in incidence for the previous 10 years available for each country was used to describe the magnitude of the changes in trend; the average annual rate of change in the age-standardised rates during the relevant time period was obtained by fitting a regression line to the natural logarithm of the age-standardised rates with calendar year as a regressor variable and was expressed as a percentage.16 The results were presented by country and aggregated for 20 subregions (as defined by UN) and six world regions (as defined by WHO). Additionally, countries were categorised into four tiers of the HDI, a composite index based on life expectancy, education, and per-capita income indicators for 2018 as developed by the UN Development Programme.17
Age-specific incidence during the most recent 10-year period was assessed in two groups of countries selected according to whether they had established screening programmes (Sweden, the UK, Australia, and the USA) or sporadic or no existing programmes for cervical cancer (Colombia, India, and Uganda). All analysis were done using R statistical software (version 4.2.0).
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
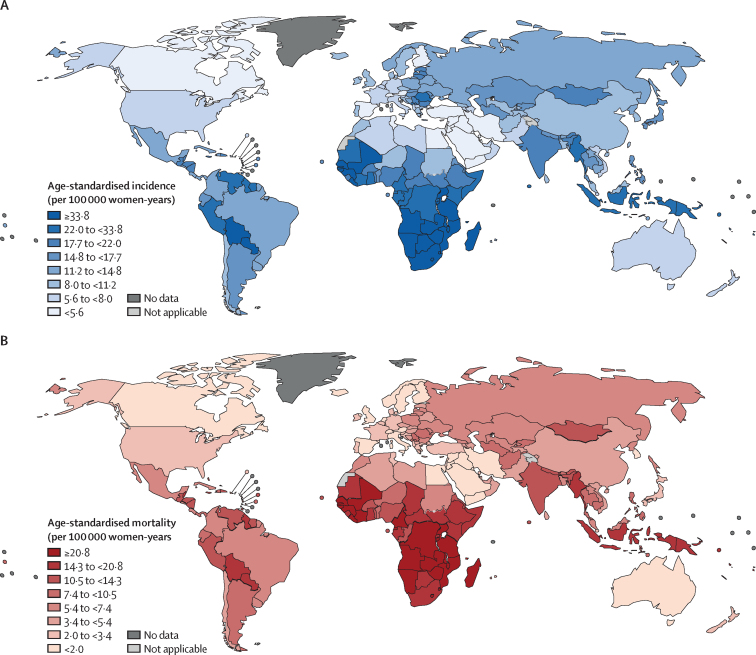
Globally, an estimated 604 127 new cases of cervical cancer and 341 831 deaths occurred in 2020 (table). Incidence varied by at least 10 times between regions, with the highest age-standardised incidence rates observed in eastern Africa (40 cases per 100 000 women-years [95% CI 39·7–40·4]), followed by southern Africa (36·4 [35·8–37·1]), Middle Africa (31·6 [31·1–32·1]), and Melanesia (28·3 [26·7–29·9]). Cervical cancer incidence was high in Malawi (67·9 [65·7–70·1]) and Zambia (65·5 [63·0–67·9]) in Africa, Bolivia (36·6 [35·0–38·2]) and Paraguay (34·1 [32·1–36·1]) in Latin America, Maldives (24·5 [17·0–32·0]) and Indonesia (24·4 [24·2– 24·7]) in Asia, and in Fiji (29·8 [24·7–35·0]) and Papua New Guinea (29·2 [27·3–31·0]) in Melanesia (figure 1A; appendix pp 9–16). Mortality rates ranged from 1·0 (0·8–1·2) in Switzerland to 55·7 (47·7–63·7) in Eswatini (figure 1B; appendix pp 4–5). The estimated number of cervical cancer cases and deaths, globally and by country, are shown in the appendix (pp 1–5).
Table.
Cervical cancer incidence and mortality in 2020, by world region and HDI level
| Total female population (thousands) |
Incidence |
Mortality |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases, n | Proportion of all cases, % | Global age-standardised rate (per 100 000 women-years; 95% CI) | Deaths, n | Proportion of all deaths, % | Global age-standardised rate (per 100 000 women-years; 95% CI) | ||||
| World | 3 864 825 | 604 127 | 100·0 | 13·3 (13·3–13·3) | 341 831 | 100·0% | 7·2 (7·2–7·3) | ||
| Region | |||||||||
| Eastern Africa | 224 366 | 54 560 | 9·0% | 40·1 (39·7–40·4) | 36 497 | 10·7% | 28·6 (28·3–28·9) | ||
| Middle Africa | 89 973 | 15 646 | 2·6% | 31·6 (31·1–32·1) | 10 572 | 3·1% | 22·7 (22·2–23·1) | ||
| Northern Africa | 122 510 | 6971 | 1·2% | 6·2 (6·1–6·4) | 4033 | 1·2% | 3·7 (3·6–3·8) | ||
| Southern Africa | 34 290 | 12 333 | 2·0% | 36·4 (35·8–37·1) | 6867 | 2·0% | 20·6 (20·1–21·1) | ||
| Western Africa | 199 581 | 27 806 | 4·6% | 23·0 (22·7–23·2) | 18 776 | 5·5% | 16·6 (16·4–16·9) | ||
| Caribbean | 22 038 | 3857 | 0·6% | 13·7 (13·3–14·2) | 2495 | 0·7% | 8·2 (7·9–8·6) | ||
| Central America | 91 619 | 13 848 | 2·3% | 13·8 (13·5–14·0) | 6866 | 2·0% | 6·8 (6·6–7·0) | ||
| South America | 218 677 | 41 734 | 6·9% | 15·4 (15·2–15·5) | 22 221 | 6·5% | 7·8 (7·7–7·9) | ||
| Northern America | 186 289 | 14 971 | 2·5% | 6·2 (6·1–6·2) | 6343 | 1·9% | 2·1 (2·0–2·2) | ||
| Eastern Asia | 822 614 | 129 567 | 21·4% | 10·8 (10·8–10·9) | 66 436 | 19·4% | 5·0 (4·9–5·0) | ||
| Excluding China | 117 143 | 19 826 | 3·3% | 11·9 (11·7–12·1) | 7376 | 2·2% | 3·1 (3·0–3·2) | ||
| China | 705 471 | 109 741 | 18·2% | 10·7 (10·6–10·8) | 59 060 | 17·3% | 5·3 (5·2–5·3) | ||
| Southeastern Asia | 334 688 | 68 623 | 11·4% | 17·8 (17·7–17·9) | 38 530 | 11·3% | 10·0 (9·9–10·1) | ||
| South-central Asia | 977 111 | 148 128 | 24·5% | 15·3 (15·2–15·4) | 91 985 | 26·9% | 9·6 (9·6–9·7) | ||
| Excluding India | 314 207 | 24 221 | 4·0% | 8·4 (8·3–8·6) | 14 637 | 4·3% | 5·3 (5·2–5·3) | ||
| India | 662 903 | 123 907 | 20·5% | 18·0 (17·9–18·1) | 77 348 | 22·6% | 11·3 (11·3–11·4) | ||
| Western Asia | 132 576 | 5402 | 0·9% | 4·1 (4·0–4·3) | 2951 | 0·9% | 2·3 (2·2–2·4) | ||
| Central-eastern Europe | 155 183 | 32 348 | 5·4% | 14·5 (14·3–14·7) | 15 854 | 4·6% | 6·1 (6·0–6·2) | ||
| Northern Europe | 53 774 | 6666 | 1·1% | 10·4 (10·2–10·7) | 2134 | 0·6% | 2·2 (2·1–2·3) | ||
| Southern Europe | 78 450 | 9053 | 1·5% | 7·7 (7·5–7·9) | 3705 | 1·1% | 2·3 (2·2–2·4) | ||
| Western Europe | 99 772 | 10 102 | 1·7% | 7·0 (6·9–7·2) | 4296 | 1·3% | 2·0 (2·0–2·1) | ||
| Australia and New Zealand | 15 253 | 1094 | 0·2% | 5·6 (5·3–6·0) | 409 | 0·1% | 1·6 (1·4–1·7) | ||
| Melanesia | 5452 | 1330 | 0·2% | 28·3 (26·7–29·9) | 818 | 0·2% | 18·6 (17·3–19·9) | ||
| Micronesia and Polynesia | 609 | 88 | 0 | 13·6 (10·8–16·5) | 43 | 0 | 6·6 (4·6–8·6) | ||
| HDI level | |||||||||
| Low | 494 473 | 81 922 | 13·6% | 27·2 (27·0–27·4) | 56 167 | 16·4% | 19·8 (19·7–20·0) | ||
| Medium | 1 136 006 | 182 866 | 30·3% | 16·6 (16·5–16·6) | 113 149 | 33·1% | 10·4 (10·4–10·5) | ||
| High | 1 441 956 | 240 400 | 39·8% | 12·7 (12·6–12·7) | 129 444 | 37·9% | 6·5 (6·5–6·6) | ||
| Very high | 790 732 | 98 675 | 16·3% | 9·1 (9·1–9·2) | 42 920 | 12·6% | 3·1 (3·1–3·2) | ||
HDI=Human Development Index.
Figure 1.
Age-standardised incidence (A) and mortality rates (B) of cervical cancer by country in 2020
Data are from the GLOBOCAN database, collated by the International Agency for Research on Cancer and hosted by the Global Cancer Observatory.
Age-standardised incidence was lowest in western Asia (4·1 cases per 100 000 women-years [95% CI 4·0–4·3]). Incidence was relatively low in Oceania, northern America, and most regions of Europe, with the exception of some countries in central and eastern Europe—eg, Romania (22·6 [21·8–23·5]) and Bulgaria (18·0 [16·8–19·2]; figure 1A; appendix pp 2, 9–12). Mortality rates followed a similar pattern to incidence, with marked variation across regions, with the highest mortality rates observed in eastern Africa (28·6 deaths per 100 000 women-years [95% CI 28·3–28·9]) and the lowest rates observed in western Europe (2·0 [2·0–2·1]; figure 1B; appendix (pp 3, 13–16).
More than 58% of all cases of cervical cancer globally were estimated in Asia followed by Africa (20%), Europe (10%) and Latin America (10%; table 1) and more than half of deaths were estimated in Asia (58%) followed by Africa (22%), and Latin America (9%; table). 39% of all cases occurred in China (18%) and India (21%) and 40% of total deaths from cervical cancer (17% in China; 23% in India).
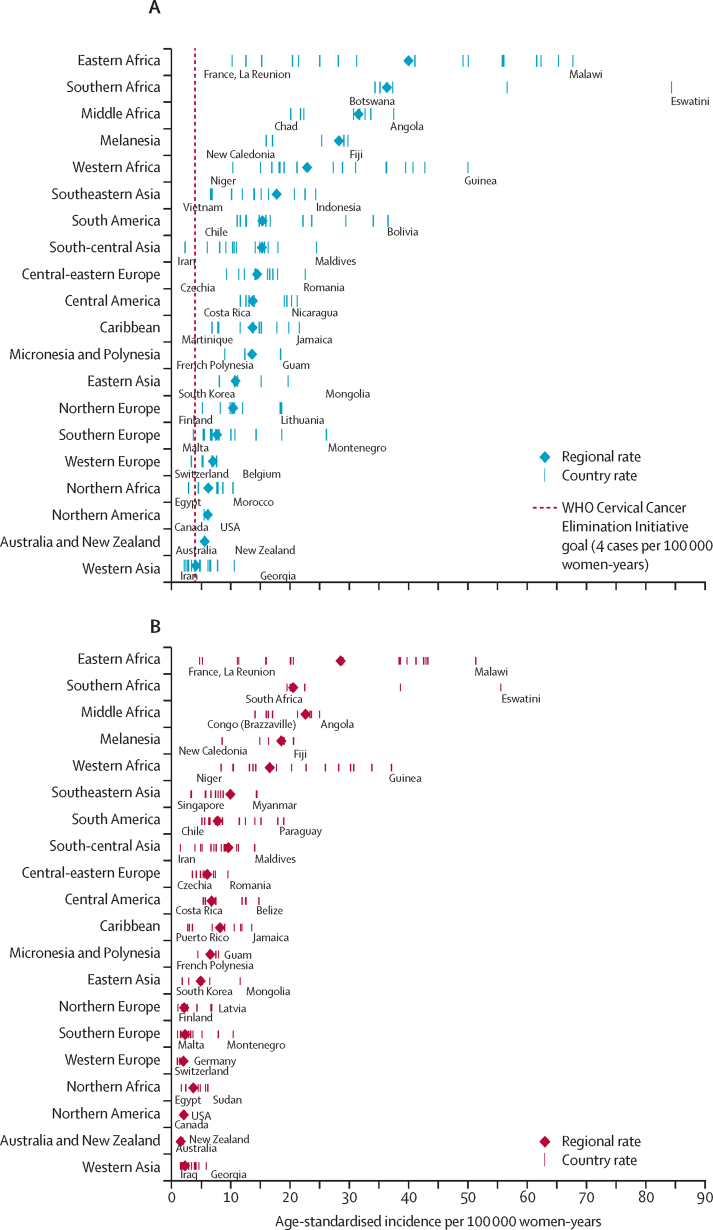
In 173 of 185 countries or territories, the age-standardised incidence of cervical cancer in 2020 was higher than the threshold set by WHO's Cervical Cancer Elimination Initiative (figure 2A). Incidence was markedly above the WHO threshold in populous countries such as China (10·7 cases per 100 000 women-years [95% CI 10·6–10·8]), India (18·0 [17·9–18·1]), Indonesia (24·4 [24·2–24·7]), Russia (14·1 [13·9–14·4]), and Brazil (12·7 [12·5–12·9]; figure 1A; appendix pp 2, 9–12). Large between-country variability was observed, even within regions. The regions with the largest variability in age-standardised incidence were eastern Africa (10·3 [7·8–12·8] in France, La Reunion compared with 67·9 [65·7–70·1] in Malawi), western Africa (10·4 [9·5–11·2] in Niger compared with 50·1 [47·9–52·4]) in Guinea) and South America (11·1 [10·6–11·7] in Chile compared with 36·6 [35·0–38·2] in Bolivia). Regions with relatively low between-country variability, and with incidence closer to the WHO threshold for most countries, were western Europe (3·4 [2·9–3·9] in Switzerland compared with 7·7 [7·0–7·3] in Belgium), northern Africa (2·9 [2·8–3·1] in Egypt compared with 10·4 [10·0–10·9] in Morocco), and western Asia (2·2 [1·9–2·4] in Iraq compared with 10·6 [9·4–11·8] in Georgia). Mortality followed a similar pattern, with the largest variation observed in eastern Africa, followed by western Africa, southern Africa, and southern America (figure 2B).
Figure 2.
Age-standardised incidence (A) and mortality rates (B) of cervical cancer by country within world region in 2020
Regions are displayed in same order for incidence and mortality and countries with the highest and lowest age-standardised rates are labelled in each region.
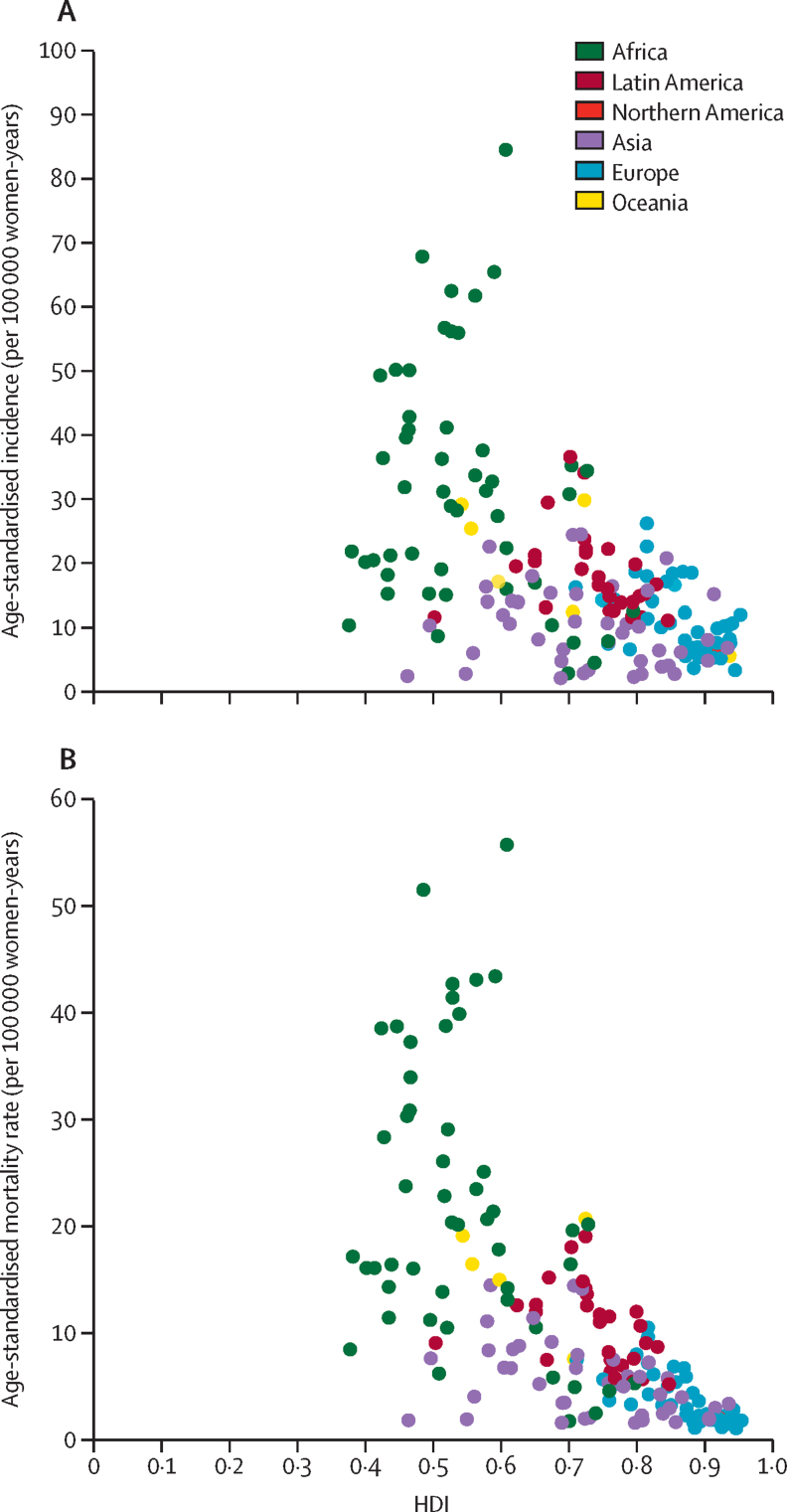
A clear and strong socioeconomic gradient was observed between cervical cancer incidence and mortality rates and the mean national HDI values, with progressively lower rates observed as HDI increased. Incidence was three times higher in low-HDI countries than very high-HDI countries (27·2 cases per 100 000 women-years [95% CI 27·0–27·4] in countries with low HDI vs 9·1 [9·1–9·2] in countries with very high HDI; table; figure 3; appendix p 1). The socioeconomic gradient was stronger for cervical cancer mortality; mortality rates were six times higher in countries with a low HDI than countries with very high HDI (19·8 deaths per 100 000 women-years [19·7–20·0] vs 3·1 [3·1–3·2]).
Figure 3.
Age-standardised incidence (A) and mortality rates (B) of cervical cancer, by HDI in 2020
Data are from the GLOBOCAN database, collated by the International Agency for Research on Cancer and hosted by the Global Cancer Observatory. Each dot represents a country. HDI=Human Development Index.
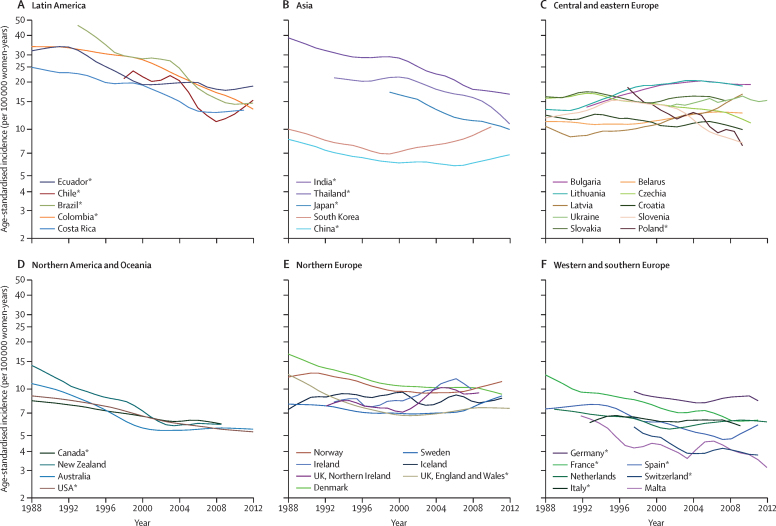
The availability of trend data by country is provided in the appendix (p 7). Between 1988 and 2017, major declines in incidence were observed in some Latin American countries, including Brazil, Colombia, and Costa Rica (figure 4). A similar pattern was observed in Asia in India, Thailand, and South Korea, while incidence in Japan and China remained stable with a slight increase between 2007 and 2017. In Europe, incidence increased in Latvia, Lithuania, and Bulgaria, whereas incidence decreased in Poland, Slovenia, and Czechia. In Oceania (Australia and New Zealand), and northern America (Canada and the USA), age-standardised incidence declined continuously from 1988 until around 2005, with incidence remaining stable (approximately 6 cases per 100 000 women-years) thereafter. A similar pattern was observed in western Europe, with the exception of Italy and the Netherlands, where incidence increased after 2003 in the Netherlands, and after 2009 in Italy.
Figure 4.
Age-standardised incidence of cervical cancer by world region, by age (1988–2017)
Data are from the GLOBOCAN database, collated by the International Agency for Research on Cancer and hosted by the Global Cancer Observatory. Only countries with population-based incidence data available in the Cancer Incidence in Five Continents plus database were included. Lines were smoothed by the LOESS regression algorithm (bandwidth 0·3) and the rates are shown in semi-log scale. *Subnational data.
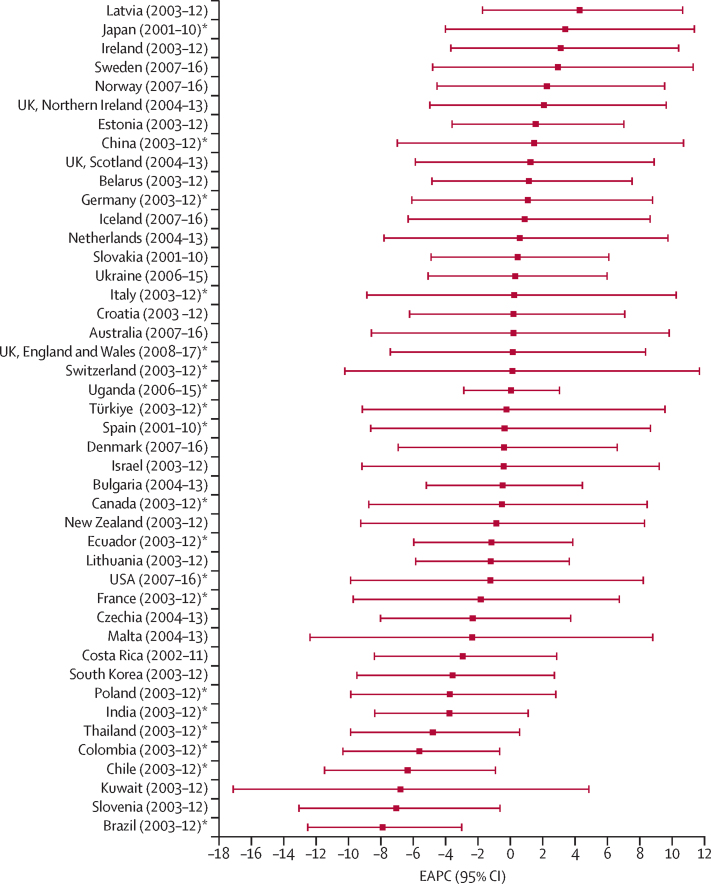
Countries with the largest declines in incidence (EAPC >4% per year) were Brazil (–7·9% [95% CI –12·5 to –3], Slovenia (–7·1% [13·1 to –0·6]), Kuwait (–6·8% [–17·1 to 4·8]), and Chile (–6·3% [–11·5 to –0·9]), whereas the highest increases in incidence were observed in Latvia (4·3% [–1·7 to 10·6]), Japan (3·4% [–4·0 to 11·4]), Ireland (3·1% [–3·7% to 10·4]), Sweden (2·9% [–4·8 to 11·3%]), Norway (2·3% [–4·5 to 9·5]), Northern Ireland (2·1% [–5·0 to 9·6]), Estonia (1·6% [–3·6 to 7·0]), and China (1·5% [–7·0 to 10·7; figure 5; appendix p 8).
Figure 5.
EAPC in age-standardised cervical cancer incidence
Only countries with population-based incidence data available in Cancer Incidence in Five Continents plus database were included. EAPC=estimated annual percentage change. *Subnational data.
We compared age-specific incidence (aged 0–74 years) between countries with high screening coverage (Sweden, the UK, Australia, and the USA; group A) and countries with sporadic or no screening programmes (Colombia, India, and Uganda; group B; appendix p 6). In group A countries, the incidence of cervical cancer increased up to age 35 years and thereafter remained approximately constant at relatively low levels. Conversely, in group B countries, the incidence increased sharply with age, peaking at around age 55–64 years (surpassing 160 cases per 100 000 women-years in Uganda).
Discussion
Our study provides a comprehensive and up-to-date overview of the global, regional, and national patterns of cervical cancer in 2020, highlighting inequalities across geographical, socioeconomic, and temporal axes, and including the progress made at the country-and-region level in the previous three decades. The incidence and mortality rates varied substantially (by 40 to 50 times) across regions and within regions, between countries. Incidence for 172 of 185 countries or territories included in the analysis exceeded the threshold set by the WHO Cervical Cancer Elimination Initiative. The largest within-region variability with particularly high incidence and mortality rates was in sub-Saharan Africa, Latin America, Asia, and Oceania.
Although the incidence of cervical cancer has decreased in many world regions in the previous three decades, notably in Latin America, Asia, western Europe and northern America, the rates and the burden of the disease remain high globally, with 604 127 new cases estimated worldwide in 2020, particularly in many LMICs. Divergence from the decreasing trend, with marked increases in cervical cancer incidence, were observed in some parts of the world, including certain countries in eastern Europe and sub-Saharan Africa. In these populations, trends are likely to continue increasing over the next decades in the absence of a scale-up of preventive interventions, including screening and HPV vaccination, with increase in the absolute number of cases driven also by the growth and ageing of the global population.18 It has been estimated that in resource-poor settings every 100 deaths of mothers due to cervical or breast cancer leads to the premature death of 14 children before they reach the age of 10 years and results in 210 children becoming maternal orphans, thus underscoring the substantial social consequences of these cancers.19, 20
The steep decrease in incidence observed in some countries, such as India, Thailand, Brazil, and Poland, could be attributed to multiple factors, including declines in fertility rates and lower parity, which are declining across successive generations of women (declining cohorts effects),21 or improvement in the coverage of screening programmes and access to treatment services especially in the urban population of the registry catchment areas.22, 23 However, the data reported by the regional registries tend to cover only a fraction of the total population with little or no coverage of rural areas, where women tend to be at higher risk, and hence the trends should be interpreted with some caution if extrapolated to the national level. During the same period, incidence plateaued to relatively low levels in most high-resource countries, while, in contrast, increases were observed in the Baltic countries and eastern European region, including in Estonia, Lithuania, Belarus, and Bulgaria, with the highest annual increase observed in Latvia. Many of these countries do not have effective population-based screening programmes.24, 25 Uganda, which was the only African country with available population-based data, showed the steepest increase in age-specific rates and a continuous increase in incidence between 1996 and 2015, indicating the huge gaps in burden and data availability that exist between countries with different levels of socioeconomic development. The impact of organised population-based screening programmes is evident in our findings for age-specific incidence. The age-specific rates are relatively low in age groups targeted by the screening, and in older age groups, in high-income countries with well organised screening programmes, whereas the risk of cervical cancer continues to increase with age in resource-poor settings without screening programmes. The increase in incidence in young birth cohorts (people born in the mid-1960s or later) from several high-income countries, reinforces the continuous need to encourage screening participation and define optimal screening age, to improve the quality of screening and expand programme coverage, to promote healthy sexual behaviour, and to increase coverage of HPV vaccination among adolescents.23, 26, 27, 28, 29, 30
As the population continue to grow and people live longer than ever before, it is projected that the absolute number of cases and deaths will continue to increase in all WHO regions in the coming decades if effective preventive interventions are not implemented in countries where they are needed. At present, only 20–30% of LMICs have introduced HPV vaccination,8 thus the beneficial impact of vaccination on the incidence of and mortality from cervical cancer, which is already evident in some high-income countries,23, 31 is unlikely to be observed in the next few decades in the majority of these countries.23 The existing discrepancies in cancer screening, diagnosis, and treatment services as reflected in the current allocation of funding for cervical cancer control in LMICs (<10% of WHO's projected need for 2019–2030) poses a huge challenge to achieving the cervical cancer elimination target set by WHO.8, 32 Barriers such as changes in lifestyle and sexual behaviours in young populations, high HIV prevalence in countries in Africa (where the fraction of cervical cancers attributable to HIV is high33) and Latin America should be continuously monitored and addressed in the future.34 Integration of cervical cancer screening with HIV testing services at a single visit to primary health centres could be a cost-effective strategy, and more importantly such integration strategy will benefit women with HIV, who are at high risk of cancer even at a younger age.35
The COVID-19 pandemic has created a new group of susceptible women due to the decrease in screening intensity and detection of cervical precancers,36, 37 but has also boosted the introduction of HPV testing of self-collected specimens, which offers possibilities to increase population coverage.38, 39 Surveillance system and health infrastructures, developed to monitor the COVID-19 pandemic could be customised to improve HPV vaccination, the monitoring of national cervical cancer screening programmes, and to improve health system capacity to deliver more efficient preventive services.40, 41
The COVID-19 pandemic might have had an impact on the incidence and mortality rates of cancers in 2020, which was not taken into account in this study, since GLOBOCAN 2020 estimates are based on incidence and mortality trends from previous years, and therefore these estimates might not reflect exactly the current situation. Future comparisons of the 2020 estimates with the recorded cancer incidence and mortality data in the same year will allow to quantify eventual discrepancies and the impact of COVID-19.
The estimates presented are based on the best available cancer incidence and mortality data within a given country (in terms of completeness, coverage, and accuracy). Caution is warranted in interpreting these findings, especially in countries where estimates are not based on local, population-based information.10 We used long-term time-series data to assess the temporal change in the rates using high-quality cancer registry data compiled in the successive editions of CI5.11 However, we could not quantify the most recent trends in certain countries that have recently introduced routine screening and thus we could not observe the impact of screening in the past decade in those countries. For example, in Slovenia a marked decrease in incidence was observed between 2003 and 2015 after the country moved from an opportunistic to an organised national screening programme.42 Because of the expected changes in cervical cancer prevention and control interventions, future estimates could differ from those presented in this study.
In summary, the burden of cervical cancer remains high in many parts of the world, with rates of the disease that in most countries are much higher than the threshold agreed by the WHO Cervical Cancer Elimination Initiative. We identified substantial geographical and socioeconomic inequalities in cervical cancer globally, with a clear gradient of increasing rates in countries with lower levels of human development. Organised screening programmes combined with access to affordable and appropriate treatment services and improved coverage of HPV vaccination will be key to reducing cervical cancer incidence and mortality in the coming decades.23, 41, 43, 44 The valuable new tools for cervical cancer prevention and control developed in the previous 20 years that are feasible to implement in resource-poor settings should be applied judiciously, simultaneously incentivising the social and organisational innovations that are context specific.45, 46
It is important to continue monitoring cervical cancer worldwide, particularly among the most disadvantaged countries and groups of the population,47 using population-based cancer registries and other relevant data.48 Socioeconomic factors are a crucial factor explaining inequalities in cancer between and within countries.49 Our critical appraisal of the data will provide timely evidence and impetus for future strategies aimed to prioritise national efforts and accelerate progress towards the WHO elimination targets and, in so doing, address the marked variations in the global cervical cancer incidence landscape.
Data sharing
The data used in this study are retrievable from the publicly available platform, the Global Cancer Observatory (GLOBOCAN).
Declaration of interests
We declare no competing interests. Where authors are identified as personnel of the International Agency for Research on Cancer/WHO, the authors alone are responsible for the views expressed in this article, and they do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer/WHO. Where authors are identified as personnel of US National Cancer Institute, the opinions expressed are their own and this material should not be interpreted as representing the official viewpoint of the US Department of Health and Human Services, the National Institutes of Health, or the National Cancer Institute.
Acknowledgments
Acknowledgments
We thank the cancer registries worldwide who compiled and submitted their data for the GLOBOCAN project. DS was supported by the French Institut National du Cancer (grant number 2018-116). MA was supported by the Horizon 2020 Framework Programme for Research and Innovation of the European Commission, through the RISCC Network (grant number 847845) and by the EU4Health Programme of DG Santé through the CanScreen-ECIS project (grant number 101056947).
Editorial note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Contributors
DS, SV, and FB conceptualised and designed the study. JV and DS accessed the data and did the formal analysis. DS and SV wrote the report. DS, SV, and FB contributed to data interpretation. All authors critically reviewed the manuscript for important intellectual content and drafting of the manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Supplementary Material
References
- 1.Arbyn M, Xu L. Efficacy and safety of prophylactic HPV vaccines. A Cochrane review of randomized trials. Expert Rev Vaccines. 2018;17:1085–1091. doi: 10.1080/14760584.2018.1548282. [DOI] [PubMed] [Google Scholar]
- 2.Bouvard V, Wentzensen N, Mackie A, et al. The IARC perspective on cervical cancer screening. N Engl J Med. 2021;385:1908–1918. doi: 10.1056/NEJMsr2030640. [DOI] [PubMed] [Google Scholar]
- 3.Ginsburg O, Bray F, Coleman MP, et al. The global burden of women's cancers: a grand challenge in global health. Lancet. 2017;389:847–860. doi: 10.1016/S0140-6736(16)31392-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8:e191–e203. doi: 10.1016/S2214-109X(19)30482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang M, Du J, Lu H, Xiang F, Mei H, Xiao H. Global trends and age-specific incidence and mortality of cervical cancer from 1990 to 2019: an international comparative study based on the Global Burden of Disease. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2021-055470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang X, Zeng Q, Cai W, Ruan W. Trends of cervical cancer at global, regional, and national level: data from the Global Burden of Disease study 2019. BMC Public Health. 2021;21:894. doi: 10.1186/s12889-021-10907-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He WQ, Li C. Recent global burden of cervical cancer incidence and mortality, predictors, and temporal trends. Gynecol Oncol. 2021;163:583–592. doi: 10.1016/j.ygyno.2021.10.075. [DOI] [PubMed] [Google Scholar]
- 8.WHO . World Health Organization; Geneva: 2020. Global strategy to accelerate the elimination of cervical cancer as a public health problem. [Google Scholar]
- 9.WHO . World Health Organization; Geneva: 2016. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. [Google Scholar]
- 10.Ferlay J, Colombet M, Soerjomataram I, et al. Cancer statistics for the year 2020: An overview. Int J Cancer. 2021;149:778–789. doi: 10.1002/ijc.33588. [DOI] [PubMed] [Google Scholar]
- 11.Bray F, Colombet M, Mery L, et al. volume XI. International Agency for Research on Cancer; Lyon: 2021. Cancer incidence in five continents. [Google Scholar]
- 12.WHO . World Health Organization; Geneva: 2020. WHO mortality database.https://www.who.int/data/data-collection-tools/who-mortality-database [Google Scholar]
- 13.UN. Department of Economic and Social Affairs. Population Division World population prospects. 2022. https://population.un.org/wpp/
- 14.Segi M, Kurihara M. Department of Public Health, Tohokur University of Medicine; Sendai: 1960. Cancer mortality for selected sites in 24 countries (1950–1957) [Google Scholar]
- 15.Doll R, Payne P, Waterhouse J. Springer; Geneva: 1966. Cancer incidence in five continents: a technical report. Union Internatinoale Contre le Cancer. [Google Scholar]
- 16.Estève J, Benhamou E, Raymond L. Statistical methods in cancer research. Volume IV. Descriptive epidemiology. IARC Sci Publ. 1994;128:1–302. [PubMed] [Google Scholar]
- 17.United Nations Development Programme Statistical update 2018. Human development indices and indicators. https://hdr.undp.org/en/content/human-development-indices-indicators-2018-statistical-update
- 18.Arbyn M, Castellsagué X, de Sanjosé S, et al. Worldwide burden of cervical cancer in 2008. Ann Oncol. 2011;22:2675–2686. doi: 10.1093/annonc/mdr015. [DOI] [PubMed] [Google Scholar]
- 19.Galukande M, Schüz J, Anderson BO, et al. Maternally orphaned children and intergenerational concerns associated with breast cancer deaths among women in Sub-Saharan Africa. JAMA Oncol. 2021;7:285–289. doi: 10.1001/jamaoncol.2020.6583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mailhot Vega RB, Balogun OD, Ishaq OF, Bray F, Ginsburg O, Formenti SC. Estimating child mortality associated with maternal mortality from breast and cervical cancer. Cancer. 2019;125:109–117. doi: 10.1002/cncr.31780. [DOI] [PubMed] [Google Scholar]
- 21.Vaccarella S, Lortet-Tieulent J, Plummer M, Franceschi S, Bray F. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. Eur J Cancer. 2013;49:3262–3273. doi: 10.1016/j.ejca.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 22.Vaccarella S, Laversanne M, Ferlay J, Bray F. Cervical cancer in Africa, Latin America and the Caribbean and Asia: regional inequalities and changing trends. Int J Cancer. 2017;141:1997–2001. doi: 10.1002/ijc.30901. [DOI] [PubMed] [Google Scholar]
- 23.Simms KT, Steinberg J, Caruana M, et al. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020-99: a modelling study. Lancet Oncol. 2019;20:394–407. doi: 10.1016/S1470-2045(18)30836-2. [DOI] [PubMed] [Google Scholar]
- 24.Poljak M, Rogovskaya SI, Kesić V, et al. Recommendations for cervical cancer prevention in central and eastern Europe and central Asia. Vaccine. 2013;31(suppl 7):H80–H82. doi: 10.1016/j.vaccine.2013.04.038. [DOI] [PubMed] [Google Scholar]
- 25.Arbyn M, Antoine J, Mägi M, et al. Trends in cervical cancer incidence and mortality in the Baltic countries, Bulgaria and Romania. Int J Cancer. 2011;128:1899–1907. doi: 10.1002/ijc.25525. [DOI] [PubMed] [Google Scholar]
- 26.Bray F, Loos AH, McCarron P, et al. Trends in cervical squamous cell carcinoma incidence in 13 European countries: changing risk and the effects of screening. Cancer Epidemiol Biomarkers Prev. 2005;14:677–686. doi: 10.1158/1055-9965.EPI-04-0569. [DOI] [PubMed] [Google Scholar]
- 27.Bray F, Lortet-Tieulent J, Znaor A, Brotons M, Poljak M, Arbyn M. Patterns and trends in human papillomavirus-related diseases in central and eastern Europe and central Asia. Vaccine. 2013;31(suppl 7):H32–H45. doi: 10.1016/j.vaccine.2013.02.071. [DOI] [PubMed] [Google Scholar]
- 28.Vaccarella S, Franceschi S, Engholm G, Lönnberg S, Khan S, Bray F. 50 years of screening in the Nordic countries: quantifying the effects on cervical cancer incidence. Br J Cancer. 2014;111:965–969. doi: 10.1038/bjc.2014.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Martel C, Georges D, Bray F, Ferlay J, Clifford GM. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Glob Health. 2020;8:e180–e190. doi: 10.1016/S2214-109X(19)30488-7. [DOI] [PubMed] [Google Scholar]
- 30.Gallagher KE, LaMontagne DS, Watson-Jones D. Status of HPV vaccine introduction and barriers to country uptake. Vaccine. 2018;36:4761–4767. doi: 10.1016/j.vaccine.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Falcaro M, Castañon A, Ndlela B, et al. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet. 2021;398:2084–2092. doi: 10.1016/S0140-6736(21)02178-4. [DOI] [PubMed] [Google Scholar]
- 32.Together for Health Investing in global cervical cancer prevention: resources for low-income and lower middle-income countries in 2020. https://togetherforhealth.org/wp-content/uploads/CxCa_Investments_2020_web.pdf
- 33.Stelzle D, Tanaka LF, Lee KK, et al. Estimates of the global burden of cervical cancer associated with HIV. Lancet Glob Health. 2021;9:e161–e169. doi: 10.1016/S2214-109X(20)30459-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pan American Health Organization Cervical cancer in women with HIV in Latin America and the Carribbean: update and steps towards elimination. 2021. https://iris.paho.org/handle/10665.2/55706
- 35.Jhpiego Eliminating cervical cancer in Namibia. https://www.jhpiego.org/story/eliminating-cervical-cancer-in-namibia/
- 36.Bonadio RC, Messias AP, Moreira OA, et al. Impact of the COVID-19 pandemic on breast and cervical cancer stage at diagnosis in Brazil. Ecancermedicalscience. 2021;15 doi: 10.3332/ecancer.2021.1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ivanuš U, Jerman T, Gašper Oblak U, et al. The impact of the COVID-19 pandemic on organised cervical cancer screening: the first results of the Slovenian cervical screening programme and registry. Lancet Reg Health Eur. 2021;5 doi: 10.1016/j.lanepe.2021.100101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arbyn M, Smith SB, Temin S, Sultana F, Castle P. Detecting cervical precancer and reaching underscreened women by using HPV testing on self samples: updated meta-analyses. BMJ. 2018;363 doi: 10.1136/bmj.k4823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arbyn M, Bruni L, Kelly D, et al. Tackling cervical cancer in Europe amidst the COVID-19 pandemic. Lancet Public Health. 2020;5:e425. doi: 10.1016/S2468-2667(20)30122-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Basu P, Lucas E, Zhang L, Muwonge R, Murillo R, Nessa A. Leveraging vertical COVID-19 investments to improve monitoring of cancer screening programme–a case study from Bangladesh. Prev Med. 2021;151 doi: 10.1016/j.ypmed.2021.106624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ginsburg O, Basu P, Kapambwe S, Canfell K. Eliminating cervical cancer in the COVID-19 era. Nat Cancer. 2021;2:133–134. doi: 10.1038/s43018-021-00178-9. [DOI] [PubMed] [Google Scholar]
- 42.Maver PJ, Seme K, Korać T, et al. Cervical cancer screening practices in central and eastern Europe in 2012. Acta Dermatovenerol Alp Panonica Adriat. 2013;22:7–19. [PubMed] [Google Scholar]
- 43.Bhatla N, Meena J, Kumari S, Banerjee D, Singh P, Natarajan J. Cervical cancer prevention efforts in India. Indian J Gynecol Oncol. 2021;19:41. doi: 10.1007/s40944-021-00526-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Canfell K, Kim JJ, Brisson M, et al. Mortality impact of achieving WHO cervical cancer elimination targets: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet. 2020;395:591–603. doi: 10.1016/S0140-6736(20)30157-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tsu VD. Cervical cancer elimination: are targets useful? Lancet. 2020;395:539–540. doi: 10.1016/S0140-6736(20)30219-1. [DOI] [PubMed] [Google Scholar]
- 46.The Lancet Cancer care: widening the scope of innovation. Lancet. 2022;399 doi: 10.1016/S0140-6736(22)01134-5. [DOI] [PubMed] [Google Scholar]
- 47.Vaccarella S, Lortet-Tieulent J, Saracci R, Conway DI, Straif K, Wild CP. International Agency for Research on Cancer; Lyon: 2019. Reducing social inequalities in cancer; Lyon Evidence and priorities for research. [PubMed] [Google Scholar]
- 48.Piñeros M, Saraiya M, Baussano I, Bonjour M, Chao A, Bray F. The role and utility of population-based cancer registries in cervical cancer surveillance and control. Prev Med. 2021;144 doi: 10.1016/j.ypmed.2020.106237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vaccarella S, Georges D, Bray F, et al. Socioeconomic inequalities in cancer mortality between and within countries in Europe: a population-based study. Lancet Reg Health Eur. 2022 doi: 10.1016/jlanepe.2022.100551. published online Nov 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study are retrievable from the publicly available platform, the Global Cancer Observatory (GLOBOCAN).