Abstract
Emerging evidence shows that compared to pre-pandemic norms pregnant women report significant increases in clinical levels of depressive and anxiety symptoms during COVID-19. This pre-registered study examined cognitive and social vulnerability factors for poor mental health in pregnancy during COVID-19. Understanding vulnerability profiles is key to identifying women at risk for deteriorating peripartum mental health. N = 742 pregnant women and N = 742 age and country-matched controls from the COVID-19 Risks Across the Lifespan Study were included. Using a case-match control design allowed us to explore whether the cognitive vulnerability profiles would differ between pregnant and non-pregnant women. The findings showed that COVID-19-related stress was associated with heightened levels of depression and anxiety during pregnancy. Its impact was greatest in women with cognitive (i.e., higher intolerance of uncertainty and tendency to worry) and social (i.e., higher level of self-reported loneliness) vulnerabilities. Importantly, our data show that the mental health impacts of the pandemic were greater in pregnant women compared to women who were not pregnant, especially those with cognitive and social vulnerabilities. The results highlight the urgent need to prioritize mental health care for pregnant women to mitigate the impact of COVID-19-related stress on women's postpartum mental health and their infants' well-being.
Keywords: Pregnancy, Postpartum depression, COVID-19, Worry, Intolerance of uncertainty, Loneliness
1. Introduction
Pregnancy is a sensitive period and major transition in a woman's life that is associated with increased rates of mental health problems and psychological distress (Canário and Figueiredo, 2017). Antenatal psychological distress in turn is associated with postpartum mental health problems (Fawcett et al., 2019; Howard et al., 2018), obstetric complications (e.g., preterm labour (Snapper et al., 2018)) as well as poor infant outcomes (Netsi et al., 2018). Worryingly, a recent meta-analysis estimated the worldwide prevalence of antenatal depression during COVID-19 at 25.6 % and 30.5 % for anxiety (Tomfohr-Madsen et al., 2021). Rates of clinically elevated symptoms of depression and anxiety reported during the pandemic also exceed pre-pandemic levels (Davenport et al., 2020; Durankuş and Aksu, 2022; Lebel et al., 2020). These rises in poor maternal mental health are likely associated with pandemic related stressors such as worldwide increases in health and economic uncertainty. Understanding individual differences in the impact of COVID-19-related stress on antenatal mental health is essential to provide targeted prevention and intervention for peripartum mental health problems during public health crises and improve infant outcomes.
1.1. Cognitive vulnerability to COVID-19-related stress
COVID-19-related stressors may be exacerbated during pregnancy, especially in pregnant women who are intolerant of uncertainty and those that tend to worry. Worry is a form of repetitive negative thinking, which has been associated with depressive and anxiety symptoms in pregnant women (Moulds et al., 2018; Schmidt et al., 2016). Worrying about perceived COVID-19-related threats for themselves and their unborn baby may lead to poorer mental health outcomes (Preis et al., 2020). Indeed, during previous coronavirus outbreaks such as SARS, pregnant women were identified as amongst the most worried about spreading or contracting the virus (Brooks et al., 2020; Caparros-Gonzalez and Alderdice, 2020). Worry has also been associated with greater distress in pregnant women during COVID-19 (Mertens et al., 2020). In addition to worry, individual differences in intolerance of uncertainty have been associated with mental health problems in pregnant women (Sbrilli et al., 2021). The continuously changing information regarding the effects of the virus on the health of women and their babies (Rasmussen and Jamieson, 2021) may be particularly stressful for these women. COVID-19-related stress then may be associated with poorer mental health in women with heightened worry and intolerance of uncertainty, especially during pregnancy.
1.2. Social vulnerability to COVID-19-related stress
A further source of stress introduced by the pandemic, beyond health and economic uncertainty, are social distancing measures implemented to reduce the spread of COVID-19 (Minihan et al., 2022). These measures have limited access to and social contact with healthcare providers, as well as social support from relatives and friends for all (Holmes et al., 2020) and may have been particularly detrimental to the wellbeing of pregnant women. As humans, social connection helps us cope with stress, build meaningful support networks and promote resilience (Bavel et al., 2020), which pregnant women rely on. In contrast, loneliness (Junttila et al., 2015) and inadequate social support (Hetherington et al., 2018) are associated with increased risk of depression and anxiety in pregnancy. Together the nature of COVID-19 and its public health sequalae may have potentiated the social risk for antenatal mental health problems in pregnant women by increasing loneliness and limiting opportunities for interaction and social support.
In this pre-registered study (https://osf.io/bsng7), we examined whether individual differences in cognitive (worry and intolerance of uncertainty) and social (loneliness, social support, and social interactions) risk explained variance in the association between COVID-19-related stress and mental health in pregnant women. Importantly, and in contrast with most existing research, we explored these questions in a case-control design. To do this we drew data from the COVID-19 Risks Across the Lifespan (CORAL; https://www.thecoralstudy.com/) study. This dataset allowed us to investigate the following hypotheses:
First, we predicted that COVID-19-related stress would be highest in countries with the highest government imposed social distancing measures (H1). Second, we hypothesised that increased COVID-19-related stress would be associated with heightened levels of mental health problems (H2). In line with the reviewed literature, we further predicted that cognitive risk (H3a) and social risk (H3b) would account for variance in the relationship between COVID-19-related stress and mental health in pregnant women. Finally, we predicted that all observed associations would be stronger in pregnant compared to non-pregnant women (H4).
2. Method
2.1. Study design
The study was approved by the University of New South Wales' Human Research Ethics Committee (HC200287). Data was drawn from the CORAL study, a three-wave longitudinal study investigating the impact of the COVID-19 pandemic on the wellbeing of young people, pregnant women, adults, and older adults. The larger CORAL study comprised of 3208 eligible participants from Australia, the UK, and USA. Participants completed an online survey thrice at three-monthly intervals between May 2020 and April 2021. The present study analyses included data from time 1 collected between May 5th 2020 and September 30th 2020.
2.2. Participants
Participants were eligible for the larger CORAL study if they were: fluent in English; lived in Australia, the UK or USA; over 11 years of age; had no neurological or developmental condition or history of a traumatic brain injury; responded to no >1 attention check item incorrectly (the survey included a total of 5 attention check items that were designed to ensure that participants were reading questionnaire items attentively); and were capable of providing informed consent (Minihan et al., 2022). For the present study, only eligible female participants at time 1 were included in the analyses based on their pregnancy status in a screening questionnaire within the survey.
Participants were 742 pregnant women (M = 31.63 years, SD = 4.94) and 742 non-pregnant women (M = 30.82 years, SD = 5.56) case-matched controls (Table 1 ; for clinical and psychological characteristics see Table S1). The sample of non-pregnant controls was drawn from a larger sample of 1139 female participants. Participants were matched using the ‘nearest neighbour’ method. A ratio of 1 was selected to perform a one-to-one matching of pregnant women with the closest eligible non-pregnant women control (Ho et al., 2011).
Table 1.
Participant demographics by pregnant status.
| Pregnant |
Non-pregnant |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Total N = 1484 | 742 | 50 | 742 | 50 |
| Country of residence | ||||
| Australia | 212 | 50 | 212 | 50 |
| United Kingdom | 344 | 50 | 344 | 50 |
| United States of America | 186 | 50 | 186 | 50 |
| Education | ||||
| High school | 62 | 4.2 | 78 | 5.3 |
| Professional/vocational training | 109 | 7.3 | 96 | 6.5 |
| University | 527 | 35.5 | 523 | 35.2 |
| Ethnicity | ||||
| Aboriginal or Torres Strait Islander | 4 | 0.3 | 2 | 0.1 |
| African | 4 | 0.3 | 7 | 0.5 |
| Asian | 27 | 1.8 | 42 | 2.8 |
| Hispanic | 18 | 1.2 | 14 | 0.9 |
| Mixed | 15 | 1 | 24 | 1.6 |
| White | 598 | 40.3 | 572 | 35.2 |
| Other | 28 | 1.9 | 28 | 1.9 |
| Prefer not to say | 3 | 0.2 | 8 | 0.5 |
| History of mental health diagnosis | ||||
| Yes | 235 | 15.8 | 289 | 19.5 |
| No | 463 | 31.2 | 408 | 27.5 |
Note. N = total number of participants; % = percentage of total number of participants.
2.3. Procedure
Participants were recruited via social media, paid online advertising, online pregnancy forums, mothers groups' newsletters, mental health organisations, as well as researchers' networks. Participants were emailed a link to complete an online survey at each time point (1, 2, 3), approximately 3 months apart. Data was collected using Qualtrics and written informed consent was obtained by completing an online Consent Form. Participants who completed the survey at time 1 were entered into a draw for the chance to receive an AUD$100 (USD$60/GBP£50) Amazon gift voucher.
2.4. Measures
Only the measures relevant to the present study are described below (for the full list of measures see Minihan et al., 2022).
2.4.1. COVID-19 related stress
The Pandemic Anxiety Scale (PAS), a 9-item questionnaire, was used to measure COVID-19-related stress (McElroy et al., 2020). The items (e.g., “I'm worried that I will catch COVID-19”) were rated on a 5-point Likert scale ranging from 0 (“Strongly disagree”) to 4 (“Strongly agree”), with higher scores indicating greater COVID-19-related stress. In the present study, the PAS demonstrated acceptable internal consistency (ωT = 0.82).
2.4.2. Mental health
2.4.2.1. Depression
Depressive symptoms were measured using the Patient Health Questionnaire (PHQ-8; Kroenke et al., 2001), excluding question nine, which assessed suicidality, as clinical risk could not be managed in the context of an online study. Participants rated the extent to which they experienced depressive symptoms over the previous two weeks (e.g., “little interest or pleasure in doing things”), on a 4-point Likert scale ranging from 0 (“not at all”) to 3 (“nearly every day”). Higher scores indicate greater levels of depressive symptoms. The PHQ-8 has demonstrated similar sensitivity, specificity, and diagnostic accuracy to the PHQ-9 (Kroenke et al., 2001). The internal consistency of the PHQ-8 in the current study was good (ωT = 0.93).
2.4.2.2. Anxiety
Symptoms and severity of anxiety were measured using the Generalized Anxiety Disorder scale (GAD-7; Spitzer et al., 2006). The GAD-7, comprised of 7 items (e.g., “worrying too much about different things”), is rated on a 4-point Likert scale from 0 (“Not at all”) to 3 (“Nearly every day”) with higher scores indicating greater levels of generalized anxiety. The GAD-7 has demonstrated excellent internal consistency in a primary care setting (Spitzer et al., 2006) and was good in the current sample (ωT = 0.96).
2.4.3. Cognitive risk
2.4.3.1. Worry
The Penn State Worry Questionnaire for Children (PSWQ-C; Chorpita et al., 1997) is a 14 item self-report measure used to assess the tendency to worry. The child version was administered due to the wide age range of participants completing this measure within the larger CORAL study. The items (e.g., “My worries really bother me”) are rated on a 4-point Likert scale from 0 (“Never true”) to 3 (“Always true”), with higher scores reflecting more frequent and uncontrollable worries. The PSWQ-C has excellent internal consistency, good convergent and discriminant validity, and test-retest reliability in clinical and non-clinical samples (Chorpita et al., 1997; Pestle et al., 2008). In the current study, the PSWQ-C demonstrated good internal consistency (ωT = 0.96).
2.4.3.2. Intolerance of uncertainty
Participants' intolerance of uncertainty was assessed with the Intolerance of Uncertainty Scale – short version (IUS-12; Carleton et al., 2007). Participants responded to 12 items (e.g., “I must get away from all situations where I don't know what will happen”) on a 5-point Likert scale from 1 (“Not at all”) to 5 (“Very much”). The IUS-12 has shown excellent internal consistency in previous samples (Carleton et al., 2007). The current study showed good internal consistency (ωT = 0.93).
2.4.4. Social risk
2.4.4.1. Loneliness
The UCLA Loneliness Scale (Russell, 1996) was administered to measure subjective feelings of loneliness as well as feelings of social isolation. The 20-item questionnaire (e.g., “I feel completely alone”) is rated on a 4-point Likert scale ranging from 0 (“I often feel this way”) to 4 (“I never feel this way”). The UCLA Loneliness Scale has shown excellent internal consistency in a young adult sample (Russell, 1996), and the present study (ωT = 0.97).
2.4.4.2. Interactions
Changes in peer interactions were measured with a bespoke 6-item questionnaire. Participants rated the extent to which their face-to-face interactions with friends and use of a number of online platforms (e.g., social media, text messaging, video calling) have changed since the COVID-19 pandemic. Ratings were provided on a sliding scale ranging from “Much decreased” to “No change” to “Much increased”. The interaction items showed good internal consistency (ωT = 0.96).
2.4.4.3. Social support
Participants rated the extent to which their social support from family and friends has changed since the COVID-19 pandemic on a bespoke 2-item questionnaire. Ratings were provided on a sliding scale from “Much decreased” to “No change” to “Much increased”. Internal reliability for social support was not calculated due to this variable being assessed by only two items.
2.4.5. Government response
Participants' country of residence (Australia, the UK, or the USA) was used as a proxy for the stringency index. Participants were currently residing in the UK (46.4 %), Australia (28.6 %), or USA (25.1 %). That is, countries with varying levels of social distancing measures operationalized as the stringency index (Oxford Coronavirus Government Response Tracker project; Hale et al., 2021). The stringency index measures the magnitude of government response to COVID-19 and constitutes a composite measure of 9 indices (i.e., school closures, workplace closures, cancellation of public events, restrictions on gatherings, closure of public transport, stay at home requirements, restrictions on internal movements, international travel controls, and the presence of public information campaigns). The average stringency index for countries in the present study during the study period was; UK = 73.3, USA = 68.5, and Australia = 63.9 (on a scale of 0–100, with 100 reflecting the greatest stringency), which was rank ordered from 3 (highest stringency) to 1 (lowest stringency).
2.4.6. COVID-19 risk
Binary response items were used to assess whether: participants or anyone in their home had been quarantined due to having COVID-19; participants had been hospitalized due to COVID-19; or participants knew anyone personally who had been diagnosed with, hospitalized due to or passed away from COVID-19. These items were combined into a COVID-risk variable, in order to control for the potential impact of COVID-19-related risk on mental health.
2.4.7. Social distancing adherence
Participants responded to an item indicating how well they were following the social distancing guidelines in place in their community. This item was included as a covariate in subsequent analyses, as social distancing adherence significantly differed between countries (F(2, 1357) = 29.21, p < .001). The UK demonstrated the highest adherence to social distancing guidelines (M = 4.34, SD = 0.71), followed by Australia (M = 4.05, SD = 0.8), then the USA with the lowest adherence (M = 3.99, SD = 0.88).
2.5. Data analysis
The present study was pre-registered (https://osf.io/bsng7). All analyses were conducted in R Studio (version 4.1.0) using the lavaan (Rosseel, 2012) and matchit (Ho et al., 2011) packages, with robust full information maximum likelihood estimation used to account for missing data. Latent factor scores for Mental Health (PHQ-8 and GAD-7), Cognitive Risk (IUS-12 and PSWQ-C) and Social Risk (loneliness, interactions, and social support) were created using structural equation modelling. Model fit was assessed using standard criteria (Schermelleh-Engel et al., 2003), with good fit indicated by Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) values of ≥0.90, and Root Mean Square Error of Approximation (RMSEA) and Standardized Root Mean Square Residual (SRMR) values of ≤0.08.
2.5.1. Mental health factor score
For the mental health factor score, the bifactor structure where the PHQ-8 and GAD-7 items loaded onto individual factors, with the latent variables then loading onto an overall general mental health factor showed a significantly better fit (CFI = 0.92, TLI = 0.91, RMSEA = 0.10, SRMR = 0.05) compared to a single factor model (χ2 diff = 239.49, df diff = 1; p < .001). The bifactor model was therefore retained for analyses.
2.5.2. Cognitive risk factor score
A cognitive factor score was created using items measuring the tendency to worry (PSWQ-C) and intolerance of uncertainty (IUS-12). A measurement model where all items loaded on to the same factor, was compared to a measurement model where the items first loaded onto individual factors, with these two factors then loading onto an overall general cognitive risk factor. The model where the IUS-12 and PSWQ-C items loaded onto individual factors, with factors loading onto an overall general cognitive risk factor (CFI = 0.91, TLI = 0.90, RMSEA = 0.07, SRMR = 0.05) was retained for analysis as this was found to fit significantly better than the model loading all items onto the same factor (χ2 diff = 1097.70, df diff = 1; p < 0).
2.5.3. Social risk factor score
Social risk factors were measured with the UCLA Loneliness Scale and bespoke items assessing face-to-face and online peer interactions, as well as social support from family and friends. Social risk could not be modelled as one latent factor as the model did not converge. Therefore, the loneliness items, interactions items and social support items were modelled as three separate latent variables (Minihan et al., 2022). The measurement models of loneliness (CFI = 0.87, TLI = 0.85, RMSEA = 0.11, SRMR = 0.06) and social support (CFI = 1, TLI = 1, RMSEA = 0, SRMR = 0) demonstrated an adequate fit to the data. However, the latent model for interactions did not demonstrate an adequate model fit (CFI = 0.62, TLI = 0.60, RMSEA = 0.42, SRMR = 2.90). To improve model fit, an exploratory analysis was conducted removing one of the interaction items considered least relevant to the demographic of pregnant women (i.e., playing video games). However, removing this item resulted in poor internal consistency (ωT = 0.20) and the model did not converge. The social interaction factor was therefore excluded from the analyses.
2.5.4. Complete measurement model
A complete measurement model was specified, with the PHQ-8, GAD-7, IUS-12, PSWQ-C, UCLA Loneliness Scale and social support items firstly loading onto separate individual factors. The PHQ-8 and GAD-7 factors then loaded onto a general mental health factor and the IUS-12 and PSWQ-C factors loaded onto a general cognitive factor. The loneliness and social support items remained as two individual factors. The complete measurement model showed an acceptable fit to the data (CFI = 0.84, TLI = 0.84, RMSEA = 0.06, SRMR = 0.24). Predicted values for each latent factor were extracted from this model and used in all subsequent analyses to address the hypotheses.
2.5.5. Hypothesis testing
As per our pre-registration, demographics (age, ethnicity and education as a proxy for socioeconomic status) were included as covariates. The analysis also included COVID-19-related risk as a covariate as countries with greater restrictions arguably had worse outbreaks and thus greater COVID-19 related risk. Additionally, self-reported adherence to social distancing restrictions was included as a covariate as it was shown to significantly vary across countries.
The first hypothesis (H1: the effect of country of residence on COVID-19-related stress) and the second hypothesis (H2: the relationship between COVID-19 related stress and mental health) were examined using general linear models. To investigate the third hypothesis, whether the association between COVID-19-related stress and mental health would vary as a function of cognitive (H3a) and social (H3b) risk factors, separate path analyses were conducted using structural equation models. As per our pre-registration, mediation was employed to avoid artificially partitioning our social and cognitive risk factors into high versus low (or other subdivision). However, it should be noted that statistical mediation does imply neither causal nor temporal mediation in a cross-sectional dataset. Finally, pregnancy status was included in analyses 2 and 3 to test the fourth hypothesis that the associations between COVID-19-related stress and mental health would be stronger in pregnant compared to non-pregnant women.
3. Results
3.1. The effect of social distancing on COVID-19-related stress in pregnancy
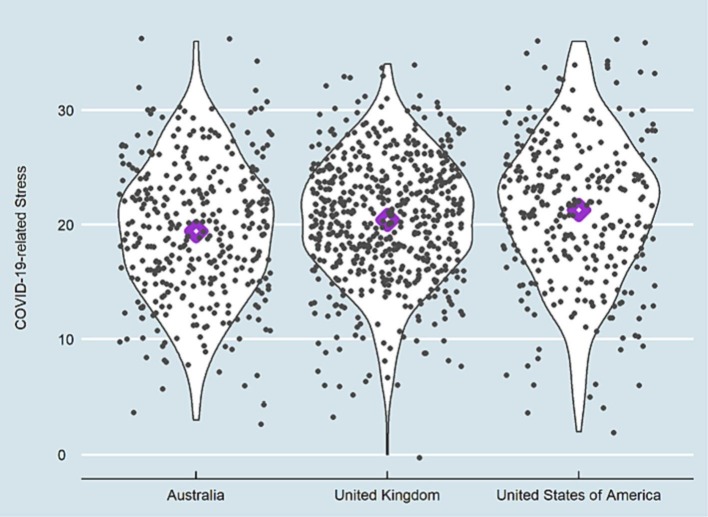
In line with our first hypothesis, there was a significant effect of social distancing measures on COVID-19-related stress, demonstrated by a significant main effect of country as a proxy for government restrictions (F = 5.11, p = .006, R 2 = 0.08) with pregnant women residing in countries with higher government-imposed social distancing measures (UK and US) reporting higher levels of COVID-19-related stress (Fig. 1 ; full model Table S2).
Fig. 1.
The graph shows COVID-19-related stress as measured on the 9-item Pandemic Anxiety Scale range: 1–36 (McElroy et al., 2020); across countries with low (Australia) to high (UK) stringency index.
3.2. COVID-19-related stress and mental health in pregnancy
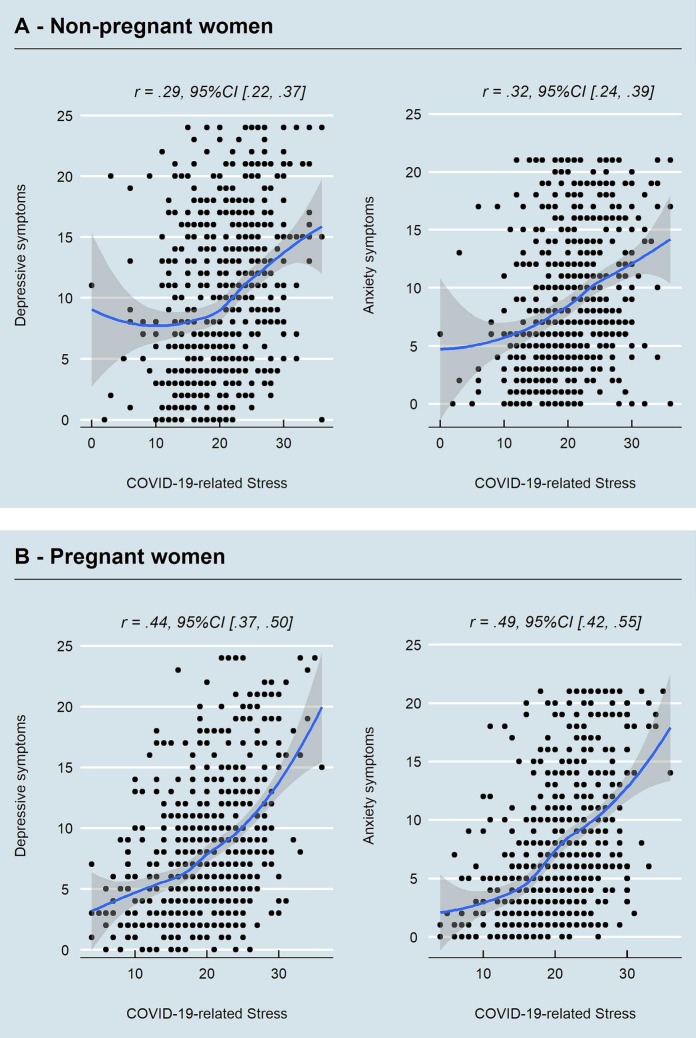
COVID-19-related stress was positively associated (F = 237.05, p < .001, R 2 = 0.34) with mental health problems in pregnant women. The total model accounted for 34 % of the variance in mental health (Table S3). The same pattern of results (Fig. 2B) was observed when running the models for observed symptoms of depression (F = 160.73, p < .001, R 2 = 0.28) and anxiety (F = 206.33, p < .001, R 2 = 0.32) separately.
Fig. 2.
Association between COVID-19-related stress and mental health in pregnant women who are pregnant and women who are not.
Note. Symptoms of depression (Kroenke et al., 2001) and generalized anxiety disorder (Spitzer et al., 2006); COVID-19-related stress = total score on the Pandemic Anxiety Scale (McElroy et al., 2020).
We next examined, whether the association between COVID-19-related stress and mental health could be accounted for by interindividual variance in cognitive and social vulnerability. Path analyses showed that cognitive vulnerability and loneliness, but not social support, showed a significant indirect effect on the association between COVID-19-related stress and mental health (Table 2 ).
Table 2.
Path analyses investigating variance in the association between COVID-19-related stress and mental health accounted for by cognitive risk, loneliness and social support.
| Mental health problems |
||||||
|---|---|---|---|---|---|---|
| β | CI95% |
z | p | R2 | ||
| LL | UL | |||||
| Mental health problems | ||||||
| ~COVID-19-related stress | 0.01 | 0.01 | 0.02 | 3.69 | <.001 | |
| ~Cognitive vulnerability | 0.62 | 0.57 | 0.67 | 23.66 | <.001 | |
| ~Loneliness | 0.39 | 0.33 | 0.45 | 13.31 | <.001 | |
| ~Social support | 0.04 | −0.01 | 0.08 | 1.71 | .09 | |
| Intercepts and model effect sizes | ||||||
| Mental health problems | −0.25 | −0.38 | −0.12 | −2.46 | <.001 | 0.84 |
| Cognitive vulnerability | −1.57 | −1.81 | −1.32 | −12.59 | <.001 | 0.20 |
| Loneliness | −1.39 | −1.63 | −1.14 | −11.20 | <.001 | 0.16 |
| Social support | 0.43 | 0.17 | 0.70 | 3.18 | .001 | 0.02 |
| Indirect effects | ||||||
| Cognitive vulnerability | 0.05 | 0.04 | 0.06 | 10.13 | <.001 | |
| Loneliness | 0.03 | 0.02 | 0.03 | 8.56 | <.001 | |
| Social support | 0.00 | −0.00 | 0.00 | −1.62 | .11 | |
| Sum indirect effects | 0.07 | 0.06 | 0.09 | 13.74 | <.001 | |
| Total effect | 0.09 | 0.08 | 0.10 | 14.87 | <.001 | |
Note. Mental health problems = latent factor computed from observed symptoms of depression (Kroenke et al., 2001) and generalized anxiety disorder (Spitzer et al., 2006); COVID-19 stress = total score on the Pandemic Anxiety Scale (McElroy et al., 2020); Loneliness = total score on the UCLA Loneliness Scale (Russell, 1996); Social support = measured with two bespoke items assessing social support from family and friends.
3.3. Cognitive and social vulnerability to COVID-19-related stress in pregnant women compared to women who are not
The impact of COVID-19-related stress on the mental health of pregnant women (Fig. 2B) was significantly greater compared to non-pregnant women (Fig. 2A), as evidenced by a significant pregnancy status by COVID-19-related stress interaction (F = 121.21, p < .001, R 2 = 0.14) in a general linear model. The model showed that the interacting effects of pregnancy and COVID-19-related stress accounted for 14 % of the variance in mental health problems. Investigating the effect across disorders showed the model to account for 15 % of variance in depression symptoms and 18 % of variance in anxiety symptoms (Table S4).
Pregnancy status moderated the indirect effects of the cognitive and social factors as evidenced by significant differences between conditional indirect effects of COVID-19-related stress via cognitive vulnerability, loneliness and social support (for the latent mental health variable: Wald test χ2 = 292.43, df = 10, p < .001; as well as for depression: Wald test χ2 = 344.81, df = 10, p < .001; and anxiety: Wald test χ2 = 437.99, df = 10, p < .001). The results showed that these vulnerability factors influenced the mental health of pregnant women more compared to non-pregnant women (Table S5).
4. Discussion
The present findings show that pregnant women living in countries with higher levels of government-mandated COVID-19 restrictions experienced higher levels of COVID-19-related stress. This was not due to exposure to worse COVID-19-related outbreaks in the US and UK compared to Australia as evidenced by non-significant effects of COVID-19-related risk. COVID-19-related stress in turn was associated with higher levels of depressive and anxiety symptoms in pregnant women. This is consistent with emerging studies from the COVID-19 pandemic, showing heightened depressive and anxiety symptoms in pregnant women during the COVID-19 pandemic (Tomfohr-Madsen et al., 2021) as well as research from past pandemics (Schwartz and Graham, 2020). Importantly, this case-control study showed that the impact of COVID-19-related stress on mental health was greater in pregnant women compared to women who were not pregnant.
Together, these results highlight the importance of considering the multifaceted impact public health measures have. While the measures were arguably critical in curbing the spread of COVID-19, thereby reducing morbidity and mortality rates, the unintended adverse impact on antenatal mental health may be long-lasting and potentially intergenerational (Poon et al., 2020). The impact may be protracted as peripartum stress and poor maternal peripartum mental health have been related to adverse outcomes for infants, such as reduced mother and child bonding (Hare et al., 2021), cognitive and developmental delays (Netsi et al., 2018; Bauer et al., 2016), as well as greater levels of emotional and behavioural problems that can persist into childhood and adolescence (Netsi et al., 2018; Rees et al., 2019; Szekely et al., 2021).
The adverse impact of COVID-19-related stress on the mental health of pregnant women in the current sample was partially accounted for by greater cognitive vulnerability and increased loneliness. The impact of cognitive vulnerability, which was a latent factor encapsulating a tendency to worry and intolerance of uncertainty, is in line with evidence from previous pandemics that shows the negative impact of pandemic-related concerns in pregnant women (Preis et al., 2020). The association between COVID-19-related stress and greater adherence to strict social distancing measures imposed during the pandemic may also have increased perceived loneliness and social isolation (Palgi et al., 2020),with loneliness being reliably associated with poorer mental health during pregnancy (Perzow et al., 2021).
These cognitive and social vulnerability factors had a greater effect on the association between COVID-19-related stress and mental health in pregnant women compared to women who were currently not pregnant. The findings illustrate the value of using a case-control approach. A possible account for the greater impact of COVID-19-related stress on the mental health of pregnant women compared to those who are not, may be due to heightened uncertainty. Pregnancy is a period in a women's life that is marred by uncertainty. This includes obstetric and foetal health-related uncertainties (Richardson et al., 2017; Lilley et al., 2009), economic uncertainties due to impact of motherhood on employment (Kreyenfeld, 2010), as well as general uncertainty about being a good parent (Donegan et al., 2022). During the pandemic these common uncertainties played out in the context of heightened global health, economic and social uncertainty, which the present study's findings suggest amplified their effect in pregnant women.
A limitation of the present study is that it only analysed data from the first wave of data collection. Exploring these associations longitudinally and in datasets that have pre-pandemic comparison samples will help establish causal associations, which cannot be inferred from the current analyses. Future research should extend the investigation of these effects onto infant well-being as well as to the study of maternal mental health in low- and middle-income countries to increase the generalizability of the findings beyond the global North.
In sum, the present study highlights the relative mental health vulnerability of pregnant women during the pandemic compared to women who are not. COVID-19-related stress had a more detrimental impact on mental health in pregnant women compared to those who are not pregnant. Given the lasting impact of peripartum mental health on both the mother and child, this study highlights the need to urgently address maternal mental health during the pandemic. The study identified worry, intolerance of uncertainty and loneliness as potential targets for intervention, as they accounted for significant variance in the association between COVID-19-related stress and antenatal mental health.
Funding statement
This work was funded by the UNSW COVID-19 Rapid Response initiative. SM is funded by a UNSW Scientia PhD scholarship, CDL is funded by the National Institute of Mental Health (R01MH126979, R01MH124866, R01MH111600, R21MH122808), ALvH is funded by the Leiden University Social Safety and Resilience Programme, JHP is funded by the National Institute of Mental Health (R01/R56 MH107418). EF's work on the development of the MFQ was funded by the Economic and Social Research Council (ES/R004285/1). SS is funded by a Wellcome Trust fellowship (209127/A/17/Z), National Health and Medical Research Council (APP1184136) and Jacobs Foundation (Young Scholar Award). This research was funded in part by the Wellcome Trust [grant number 209127/A/17/Z]. For the purpose of open access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission. The funding sources did not have any involvement in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
CRediT authorship contribution statement
SS designed the study, AS and SM collected the data. AS and SS analysed the data and wrote the manuscript. All authors commented on the manuscript.
Conflict of interest
The authors declare no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2023.01.053.
Appendix A. Supplementary data
Supplementary tables
References
- Bauer A., Knapp M., Parsonage M. Lifetime costs of perinatal anxiety and depression. J. Affect. Disord. 2016;192:83–90. doi: 10.1016/j.jad.2015.12.005. [DOI] [PubMed] [Google Scholar]
- Bavel J.J.V., et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Weston D., Greenberg N. Psychological impact of infectious disease outbreaks on pregnant women: rapid evidence review. Public Health. 2020;189:26–36. doi: 10.1016/j.puhe.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canário C., Figueiredo B. Anxiety and depressive symptoms in women and men from early pregnancy to 30 months postpartum. J. Reprod. Infant Psychol. 2017;35:431–449. doi: 10.1080/02646838.2017.1368464. [DOI] [PubMed] [Google Scholar]
- Caparros-Gonzalez R.A., Alderdice F. The COVID-19 pandemic and perinatal mental health. J. Reprod. Infant Psychol. 2020;38:223–225. doi: 10.1080/02646838.2020.1786910. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Norton M.A.P.J., Asmundson G.J.G. Fearing the unknown: a short version of the intolerance of uncertainty scale. J. Anxiety Disord. 2007;21:105–117. doi: 10.1016/j.janxdis.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Chorpita B.F., Tracey S.A., Brown T.A., Collica T.J., Barlow D.H. Assessment of worry in children and adolescents: an adaptation of the Penn State worry questionnaire. Behav. Res. Ther. 1997;35:569–581. doi: 10.1016/s0005-7967(96)00116-7. [DOI] [PubMed] [Google Scholar]
- Davenport M.H., Meyer S., Meah V.L., Strynadka M.C., Khurana R. Moms are not OK: COVID-19 and maternal mental health. Front. Glob. Womens Health. 2020;1 doi: 10.3389/fgwh.2020.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donegan E., Frey B.N., McCabe R.E., Streiner D.L., Green S.M. Intolerance of uncertainty and perfectionistic beliefs about parenting as cognitive mechanisms of symptom change during cognitive behavior therapy for perinatal anxiety. Behav. Ther. 2022;53:738–750. doi: 10.1016/j.beth.2022.02.005. [DOI] [PubMed] [Google Scholar]
- Durankuş F., Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J. Matern. Fetal Neonatal Med. 2022;35:205–211. doi: 10.1080/14767058.2020.1763946. [DOI] [PubMed] [Google Scholar]
- Fawcett E.J., Fairbrother N., Cox M.L., White I.R., Fawcett J.M. The prevalence of anxiety disorders during pregnancy and the postpartum period: a multivariate Bayesian meta-analysis. J. Clin. Psychiatry. 2019;80:1181. doi: 10.4088/JCP.18r12527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T., et al. A global panel database of pandemic policies (Oxford COVID-19 government response Tracker) Nat. Hum. Behav. 2021;5:529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- Hare M.M., Kroll-Desrosiers A., Deligiannidis K.M. Peripartum depression: does risk versus diagnostic status impact mother–infant bonding and perceived social support? Depress. Anxiety. 2021;38:390–399. doi: 10.1002/da.23121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetherington E., McDonald S., Williamson T., Patten S.B., Tough S.C. Social support and maternal mental health at 4 months and 1 year postpartum: analysis from the all our families cohort. J. Epidemiol. Community Health. 2018;72:933–939. doi: 10.1136/jech-2017-210274. [DOI] [PubMed] [Google Scholar]
- Ho D.E., Imai K., King G., Stuart E.A. MatchIt : nonparametric preprocessing for parametric causal inference. J. Stat. Softw. 2011;42 [Google Scholar]
- Holmes E.A., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard L.M., et al. Accuracy of the whooley questions and the Edinburgh postnatal depression scale in identifying depression and other mental disorders in early pregnancy. Br. J. Psychiatry. 2018;212:50–56. doi: 10.1192/bjp.2017.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junttila N., et al. Intercorrelations and developmental pathways of mothers’ and fathers’ loneliness during pregnancy, infancy and toddlerhood–STEPS study. Scand. J. Psychol. 2015;56:482–488. doi: 10.1111/sjop.12241. [DOI] [PubMed] [Google Scholar]
- Kreyenfeld M. Uncertainties in female employment careers and the postponement of parenthood in Germany. Eur. Sociol. Rev. 2010;26:351–366. [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity meausre. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel C., MacKinnon A., Bagshawe M., Tomfohr-Madsen L., Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect. Disord. 2020;277:5–13. doi: 10.1016/j.jad.2020.07.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilley S.A., Andrade J., Turpin G., Sabin-Farrell R., Holmes E.A. Visuospatial working memory interference with recollections of trauma. Br. J. Clin. Psychol. 2009;48:309–321. doi: 10.1348/014466508X398943. [DOI] [PubMed] [Google Scholar]
- McElroy E., et al. Demographic and health factors associated with pandemic anxiety in the context of COVID-19. Br. J. Health Psychol. 2020;25:934–944. doi: 10.1111/bjhp.12470. [DOI] [PubMed] [Google Scholar]
- Mertens G., Gerritsen L., Duijndam S., Salemink E., Engelhard I.M. Fear of the coronavirus (COVID-19): predictors in an online study conducted in march 2020. J. Anxiety Disord. 2020;74 doi: 10.1016/j.janxdis.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minihan S., et al. Social determinants of mental health during a year of the COVID-19 pandemic. Dev. Psychopathol. 2022;1–13 doi: 10.1017/S0954579422000396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulds M.L., Black M.J., Newby J.M., Hirsch C.R. Repetitive negative thinking and its role in perinatal mental health. Psychopathology. 2018;51:161–166. doi: 10.1159/000488114. [DOI] [PubMed] [Google Scholar]
- Netsi E., et al. Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry. 2018;75:247–253. doi: 10.1001/jamapsychiatry.2017.4363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palgi Y., et al. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020;275:109–111. doi: 10.1016/j.jad.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perzow S.E.D., et al. Mental health of pregnant and postpartum women in response to the COVID-19 pandemic. J. Affect. Disord. Rep. 2021;4 doi: 10.1016/j.jadr.2021.100123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pestle S.L., Chorpita B.F., Schiffman J. Psychometric properties of the Penn State worry questionnaire for children in a large clinical sample. J. Clin. Child Adolesc. Psychol. 2008;37:465–471. doi: 10.1080/15374410801955896. [DOI] [PubMed] [Google Scholar]
- Poon L.C., et al. Global interim guidance on coronavirus disease 2019 (COVID-19) during pregnancy and puerperium from FIGO and allied partners: information for healthcare professionals. Int. J. Gynecol. Obstet. 2020;149:273–286. doi: 10.1002/ijgo.13156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis H., Mahaffey B., Heiselman C., Lobel M. Pandemic-related pregnancy stress and anxiety among women pregnant during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. Mfm. 2020;2 doi: 10.1016/j.ajogmf.2020.100155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen S.A., Jamieson D.J. Pregnancy, postpartum care, and COVID-19 vaccination in 2021. JAMA. 2021;325:1099–1100. doi: 10.1001/jama.2021.1683. [DOI] [PubMed] [Google Scholar]
- Rees S., Channon S., Waters C.S. The impact of maternal prenatal and postnatal anxiety on children’s emotional problems: a systematic review. Eur. Child Adolesc. Psychiatry. 2019;28:257–280. doi: 10.1007/s00787-018-1173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson A., Raine-Fenning N., Deb S., Campbell B., Vedhara K. Anxiety associated with diagnostic uncertainty in early pregnancy. Ultrasound Obstet. Gynecol. 2017;50:247–254. doi: 10.1002/uog.17214. [DOI] [PubMed] [Google Scholar]
- Rosseel Y. Lavaan: an R package for structural equation modeling. J. Stat. Softw. 2012;48:1–36. [Google Scholar]
- Russell D.W. UCLA loneliness scale (Version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Sbrilli M.D., Haigler K., Laurent H.K. The indirect effect of parental intolerance of uncertainty on perinatal mental health via mindfulness during COVID-19. Mindfulness. 2021;12:1999–2008. doi: 10.1007/s12671-021-01657-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schermelleh-Engel K., Moosbrugger H., Müller H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness-offit measures. Methods Psychol. Res. 2003:23–74. [Google Scholar]
- Schmidt D., Seehagen S., Vocks S., Schneider S., Teismann T. Predictive importance of antenatal depressive rumination and worrying for maternal–foetal attachment and maternal well-being. Cogn. Ther. Res. 2016;40:565–576. [Google Scholar]
- Schwartz D.A., Graham A.L. Potential maternal and infant outcomes from (Wuhan) coronavirus 2019-nCoV infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020;12 doi: 10.3390/v12020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snapper L.A., Hart K.L., Venkatesh K.K., Kaimal A.J., Perlis R.H. Cohort study of the relationship between individual psychotherapy and pregnancy outcomes. J. Affect. Disord. 2018;239:253–257. doi: 10.1016/j.jad.2018.05.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Szekely E., et al. Maternal prenatal mood, pregnancy-specific worries, and early child psychopathology: findings from the DREAM BIG consortium. J. Am. Acad. Child Adolesc. Psychiatry. 2021;60:186–197. doi: 10.1016/j.jaac.2020.02.017. [DOI] [PubMed] [Google Scholar]
- Tomfohr-Madsen L.M., Racine N., Giesbrecht G.F., Lebel C., Madigan S. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2021;300 doi: 10.1016/j.psychres.2021.113912. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables