Abstract
The murine macrophage-like cell line J774.A1 ingests and allows intracellular growth of Francisella tularensis. We demonstrate that, after 24 h of infection, a pronounced cytopathogenicity resulted and the J774 cells were undergoing apoptosis. Despite this host cell apoptosis, no decrease in bacterial numbers was observed. When internalization of bacteria was prevented or intracellularly located F. tularensis bacteria were eradicated within 12 h, the progression of host cell cytopathogenicity and apoptosis was prevented.
Macrophages play a central role in host defense against infection by effectuating the killing of microbes and by controlling host inflammatory responses. When fulfilling these functions, macrophages are controlled via processes regulating both cell proliferation and apoptosis. There is growing evidence that microbes may affect the survival of macrophages or other host cells via regulation of apoptosis. The intracellular bacteria Chlamydia trachomatis, Brucella suis, and Rickettsia rickettsii have the capability to inhibit apoptosis (5, 8, 14), thereby preserving the intracellular habitat and enabling their multiplication. By contrast, there are numerous examples of gram-negative bacteria, gram-positive bacteria, and mycobacteria that induce apoptosis (4, 9, 10, 15, 16, 21–24). Apart from the advantage that microbes may gain from controlling host cell apoptosis, it has been suggested that apoptosis may function as a host defense mechanism by depriving microorganisms adapted to the intracellular environment of their preferred habitat (17).
Francisella tularensis is a highly virulent intracellular pathogen capable of infecting many mammalian species and various types of cells. Little is known about how it survives within host cells, since, unlike many other facultative intracellular bacteria, it produces no toxins and harbors no secretion systems. A relatively avirulent Francisella strain, the live vaccine strain (LVS), is fully pathogenic for certain animals and causes a lethal infection in mice that is indistinguishable from human disease (1, 7). We have shown that LVS is very well adapted to the intracellular environment of macrophages, since it shows very few signs of stress during intracellular growth (12). This is remarkable, particularly since F. tularensis is localized in the hostile environment of an endosome (2). Previous studies have shown that F. tularensis exerts a cytopathogenic effect on murine macrophages (2, 3, 12). To understand more about the intracellular life of F. tularensis, we investigated the mechanism of this cytopathogenic effect on the host cell.
Intracellular multiplication of F. tularensis leads to cytopathogenicity of J774 macrophages
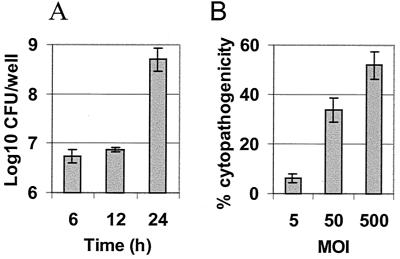
F. tularensis LVS infection of the murine macrophage-like cell line J774.A1 was performed as previously described (12). Marginal bacterial multiplication occurred within the first 12 h of intracellular infection. Rapid multiplication was evident between 12 and 24 h after infection, during which time the bacterial numbers increased by approximately 2 log10 (Fig. 1A). Cytopathogenicity was followed by measuring the release of lactate dehydrogenase (LDH) in the cell culture supernatants. After 24 h, the bacterial infection resulted in cytopathogenicity in a dose (i.e., multiplicity of infection [MOI])-dependent manner (Fig. 1B). The cytopathogenicity was also time-dependent, and when a high MOI of 500 was used, the value was 7.8 ± 1.9% at 6 h, 13.9 ± 5.6% at 12 h, and 51.9 ± 5.5% at 24 h. When cell detachment was monitored by using a previously described protocol (20, 26), the progression of detachment was similar to that of the LDH release. A high percentage (80.7 ± 5.2%) of J774 cells were detached at 24 h at an MOI of 500. When lower MOIs were used and the observation time was extended, the cell detachment reached the same high level at 72 h with an MOI of 50, whereas the cells were unaffected for more than a week at an MOI of 5 (data not shown).
FIG. 1.
Intracellular replication of F. tularensis in J774 cells results in a dose-dependent cytopathogenicity in J774 cells. (A) Replication of F. tularensis in J774 cells. F. tularensis infections were performed at an MOI of 500 in triplicate wells, each containing 2 × 105 J774 cells. The number of F. tularensis bacteria in the monolayers was determined by lysis of cells with phosphate-buffered saline–buffered 0.1% sodium deoxycholate solution for 2 min and plating of 10-fold dilutions on agar plates. The number of F. tularensis bacteria recovered at the start of the experiment was 6 × 106 CFU. Data are means ± standard deviations of three wells from one representative experiment of three. (B) Cytopathogenicity of J774 cells was assayed by release of LDH at 24 h and expressed as cytopathogenicity relative to that observed after lysis of the cells. Twenty thousand J774 cells were seeded per well 18 h before use and were infected at the indicated MOI. Supernatants of the infected macrophages were sampled at the indicated time points and assayed for the presence of released LDH (18) using the Cytotox 96 Kit (Promega, Madison, Wis.) according to the manufacturer's instructions. The F. tularensis strain does not have endogenous LDH activity when grown aerobically. Data are means ± standard deviations of four wells from one representative experiment of three.
F. tularensis bacteria kill J774 cells through apoptosis.
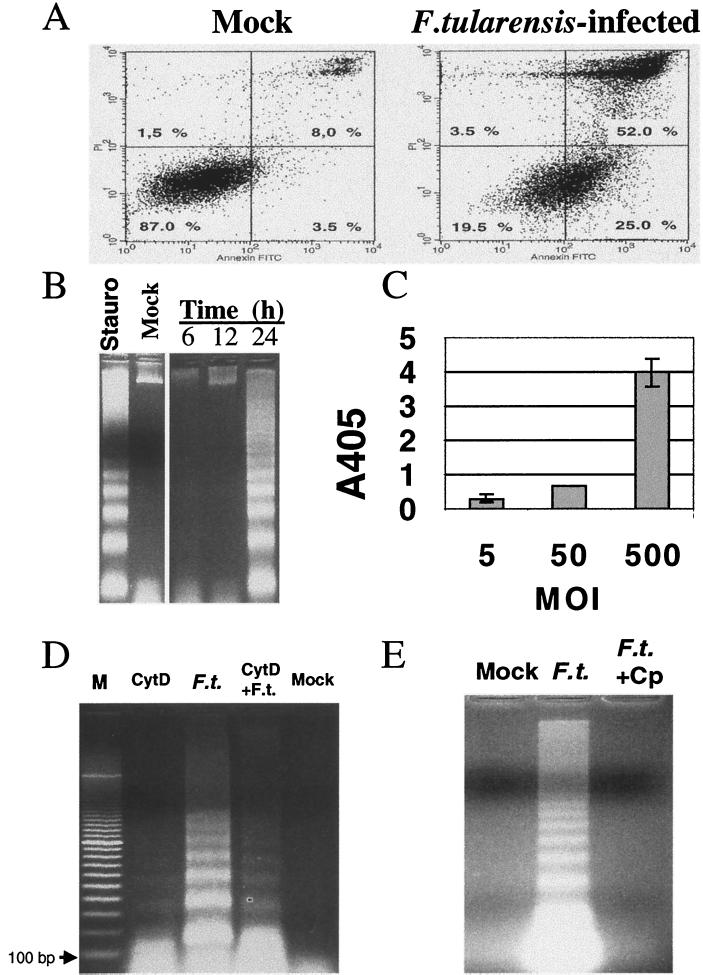
To determine if there is a role of apoptosis in infection-induced cytopathogenicity, we monitored the presence of surface-exposed phosphatidylserine, the appearance of terminal deoxynucleotidyltransferase-mediated dUTP-biotin nick end labeling (TUNEL)-positive infected cells, the presence of the DNA ladder, and the release of nucleosomes, all of which are characteristic of apoptosis. Surface exposure of phosphatidylserine was examined by labeling with fluorescein isothiocyanate-conjugated annexin V and was analyzed by flow cytometry. To monitor the integrity of the plasma membrane, the cells were simultaneously stained with propidium iodide (PI). At 12 h, infected and noninfected cells showed low levels (<6%) of annexin V and PI staining (not shown). Eighteen hours after infection, 25.0% of the cells showed annexin V staining, 52.0% of the cells showed staining with both annexin V and PI, and 3.5% of the cells were stained with PI only (Fig. 2A). Among noninfected cells, 3.5% were stained with annexin V, 8.0% of the cells showed staining with both annexin V and PI, and 1.5% showed staining with PI (Fig. 2A). These results indicate that after infection, a significant increase occurred from 12 to 18 h in the relative numbers of apoptotic cells (annexin positive) but not of necrotic cells (PI positive only). Cells stained with both PI and annexin V presumably had died from apoptosis.
FIG. 2.
F. tularensis infection results in DNA fragmentation, release of nucleosomes, and annexin V staining of J774 cells and requires intracellular multiplication of bacteria. (A) Annexin V and PI staining of infected J774 cells. Cells were infected at an MOI of 500 and at 18 h of infection were stained with Annexin-V-Fluos (Boehringer, Mannheim, Germany) according to the manufacturer's instructions. Stained cells were analyzed by flow cytometry and data were analyzed by use of CellQuest (Becton-Dickinson, Sunnyvale, Calif.). Data as percentages from one of two similar experiments are shown. The y axis represents PI staining (10,000 cells) and the x axis represents annexin V staining. (B) Fragmentation of DNA from J774 cells was monitored in relation to the duration of the F. tularensis infection. J774 cells (5 × 106 per dish) were infected at an MOI of 500, and at the indicated time points eukaryotic DNA was prepared following a previously described protocol (19). Lane “Stauro” represents DNA from apoptotic J774 cells after staurosporine treatment (4 μM for 6 h) and serves here as a positive control, and lane “Mock” is DNA preparations from noninfected cells at 24 h. (C) Determination of release of nucleosome fragments from J774 cells after F. tularensis infection. The release of cytoplasmic DNA fragments was monitored using the cell death detection enzyme-linked immunosorbent assay (Boehringer) according to the instructions of the manufacturer and as described previously (19). The substrate reaction time was 10 min. Representative results from one of two experiments are shown. Error bars represent standard deviations of triplicate samples. The standard deviation at an MOI of 50 was 0.0. (D) Fragmentation of DNA from J774 cells after F. tularensis infection in the presence (CytD + F.t.) or absence (F.t.) of cytochalasin D (CytD). Cells were treated for 30 min prior to infection with 1 μg of cytochalasin D ml−1 (Sigma) and during the 2 h of incubation with F. tularensis. Cells were infected and the eukaryotic DNA was prepared and analyzed as described for panel B. The “Mock” lane represents preparations from noninfected cells. DNA was prepared at 24 h. A 100-bp DNA molecular size marker (Bio-Rad) was included as a standard (lane M, arrow points to the position of 100 bp). (E) Fragmentation of DNA from J774 cells after F. tularensis infection in the presence (F.t. + Cp) or absence (F.t.) of ciprofloxacin. Cells were infected and the eukaryotic DNA was prepared and analyzed as for panel B. Ciprofloxacin was used at a concentration of 20 μg ml−1 and was added at 2 h after the addition of F. tularensis. DNA was prepared after 24 h of infection.
With the same kinetics as the progression of cytopathogenicity, F. tularensis infection caused distinct DNA fragmentation as revealed by gel electrophoresis in a time- (Fig. 2B) and dose-dependent manner (not shown). A similar DNA ladder resulted from treatment with staurosporine, a known inducer of apoptosis (Fig. 2B). The enzyme-linked immunosorbent assay results of the release of cytoplasmic DNA fragments depicted in Fig. 2C show that, at 24 h, a strong signal was detected in the cells infected at an MOI of 500, indicating the occurrence of apoptosis at this time point. We also quantitated by fluorescence-activated cell sorter analysis the percentage of J774 cells that were TUNEL positive. The percentage of TUNEL-positive cells remained at background levels at 6 and 12 h regardless of the MOI and at 24 h when infection had been performed at an MOI of 5 (data not shown). At 24 h, the percentage of TUNEL-positive cells was 10% at an MOI of 50 and 60% at an MOI of 500, while only 1.0% of the noninfected cells were positively stained.
Entry of viable F. tularensis bacteria into host cells is required to trigger cytopathogenicity and apoptosis.
Cytochalasin D, the inhibitor of actin polymerization, prevented more than 99.9% of the uptake of F. tularensis. Without cytochalasin D the number of CFU at 6 h was 6.7 ± 0.1 log10, and with cytochalasin D the number of CFU at 6 h was 3.1 ± 0.0 log10. After cytochalasin D treatment, the cytopathogenic effect at 24 h resulting from the F. tularensis infection was greatly diminished, as judged by release of LDH (57.5% versus 5.7%) and cell detachment (82% versus 21%). Only a very weak DNA ladder was observed after cytochalasin D treatment of infected cell cultures (Fig. 2D), indicating that F. tularensis bacteria need to be intracellularly localized to induce DNA fragmentation in the J774 cells. F. tularensis viability was essential for induction of apoptosis, since killed bacteria did not induce cytopathogenicity above background levels or DNA fragmentation (data not shown). In cell cultures to which a supernatant from an overnight F. tularensis culture had been added, no cytopathogenicity or DNA fragmentation occurred. This result lends further support to the notion that the cytopathogenic effect resulting from F. tularensis infection is not due to any substance secreted in the infected cell cultures.
Intracellular survival and proliferation of F. tularensis is essential to induce cytopathogenicity and apoptosis.
The role of intracellular multiplication of F. tularensis for induction of cytopathogenicity and apoptosis was investigated. To kill intracellular F. tularensis, ciprofloxacin (Ciproxin; Bayer AG, Leverkusen, Germany) was added to infected cell cultures at various time points. When treatment was instituted within 12 h, an effective though not eradicating effect was observed (the log10 CFU at 24 h decreased from 8.7 ± 0.2 to 4.7 ± 0.0). In cultures with the addition of ciprofloxacin, the cells showed few morphological changes and much less detachment than did untreated infected cells. Moreover, no fragmentation of the DNA (Fig. 2E) or release of LDH (data not shown) occurred in cell cultures with the addition of ciprofloxacin during the observation period of 24 h. When ciprofloxacin was added after 15 h or at later time points, a prominent cytopathogenic effect similar to that observed in untreated infected cell cultures occurred at 24 h (data not shown).
Although in vitro experiments have clearly shown that intracellular growth of F. tularensis in murine macrophages is associated with cytopathogenicity in murine macrophages (2, 3, 12), the underlying mechanism has remained unclear. According to the present results, apoptosis can be demonstrated in the infected cells. The first signs of apoptosis were observed at 18 h of infection and was the probable reason for loss of membrane integrity seen at 24 h.
The Francisella-mediated apoptosis occurred at a later stage of in vitro infection in macrophages than that previously described for Salmonella, Yersinia, Shigella, or Legionella (11). Possibly, such a difference may relate to the reason the microbe induces apoptosis. Shigella and various species of Salmonella and Yersinia do not utilize phagocytic host cells for intracellular replication and might therefore benefit from preventing phagocytosis and subsequent bacterial killing as rapidly as possible. Legionella, on the other hand, invades and replicates in macrophages and has a lifestyle similar to that of Francisella. In vitro studies suggest, however, that Legionella replicates at a much higher rate than Francisella during the first 12 h (10). Consequently, Francisella should benefit from a longer delay before apoptosis is induced than would be optimal for Legionella. This may be a rational strategy for Francisella, allowing the bacterium to utilize the target cell for vigorous growth and then killing the cell to escape when nutrients become scarce.
The induction of apoptosis required the presence of intracellularly proliferating bacteria, since it was triggered by viable F. tularensis. Killing of intracellular bacteria up to 12 h after infection prevented apoptosis. The ability of the pathogen to replicate in professional phagocytes is well documented (6, 13, 25), and this trait seems to be very fundamental for the successful intracellular lifestyle of F. tularensis, since mutants with impaired intracellular replication showed a decreased virulence in mice (3). On the basis of these findings, we propose that the signaling required to induce apoptosis is triggered by the presence of relatively high numbers of F. tularensis in the logarithmic growth phase inside the host cell.
Acknowledgments
Grant support was obtained from the Defense Advanced Project Agency (DARPA), the Swedish Medical Research Council, Samverkansnämnden Norra Sjukvårdsregionen, Umeå, and the Medical Faculty, Umeå University, Umeå, Sweden.
We are grateful to Nils Wierup and Amin Safari Khaledi for their contributions to the early work of this project. We also thank Bernt Eric Uhlin for support, Thorsten Johansson for help with flow cytometry, and Arne Tärnvik and Paul Haemig for critical reading of the manuscript.
REFERENCES
- 1.Anthony L S, Kongshavn P A. Experimental murine tularemia caused by Francisella tularensis, live vaccine strain: a model of acquired cellular resistance. Microb Pathog. 1987;2:3–14. doi: 10.1016/0882-4010(87)90110-0. [DOI] [PubMed] [Google Scholar]
- 2.Anthony L S D, Burke R D, Nano F E. Growth of Francisella spp. in rodent macrophages. Infect Immun. 1991;59:3291–3296. doi: 10.1128/iai.59.9.3291-3296.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatnagar N, Getachew E, Straley S, Williams J, Meltzer M, Fortier A. Reduced virulence of rifampicin-resistant mutants of Francisella tularensis. J Infect Dis. 1994;170:841–847. doi: 10.1093/infdis/170.4.841. [DOI] [PubMed] [Google Scholar]
- 4.Chen Y, Smith M R, Thirumalai K, Zychlinsky A. A bacterial invasin induces macrophage apoptosis by binding directly to ICE. EMBO J. 1996;15:3853–3860. [PMC free article] [PubMed] [Google Scholar]
- 5.Clifton D R, Goss R A, Sahni S K, van Antwerp D, Baggs R B, Marder V J, Silverman D J, Sporn L A. NF-kappa B-dependent inhibition of apoptosis is essential for host cell survival during Rickettsia rickettsii infection. Proc Natl Acad Sci USA. 1998;95:4646–4651. doi: 10.1073/pnas.95.8.4646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Conlan J W, North R J. Early pathogenesis of infection in the liver with the facultative intracellular bacteria Listeria monocytogenes, Francisella tularensis, and Salmonella typhimurium involves lysis of infected hepatocytes by leukocytes. Infect Immun. 1992;60:5164–5171. doi: 10.1128/iai.60.12.5164-5171.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eigelsbach H T, Down C M. Prophylactic effectiveness of live and killed tularemia vaccines. I. Production of vaccine and evaluation in the white mouse and guinea pig. J Immunol. 1961;87:415–425. [PubMed] [Google Scholar]
- 8.Fan T, Lu H, Hu H, Shi L, McClarty G A, Nance D M, Greenberg A H, Zhong G. Inhibition of apoptosis in Chlamydia-infected cells: blockade of mitochondrial cytochrome c release and caspase activation. J Exp Med. 1998;187:487–496. doi: 10.1084/jem.187.4.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gao L Y, Abu Kwaik Y. Activation of caspase 3 during Legionella pneumophila-induced apoptosis. Infect Immun. 1999;67:4886–4894. doi: 10.1128/iai.67.9.4886-4894.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gao L Y, Abu Kwaik Y. Apoptosis in macrophages and alveolar epithelial cells during early stages of infection by Legionella pneumophila and its role in cytopathogenicity. Infect Immun. 1999;67:862–870. doi: 10.1128/iai.67.2.862-870.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gao L Y, Kwaik Y A. The modulation of host cell apoptosis by intracellular bacterial pathogens. Trends Microbiol. 2000;8:306–313. doi: 10.1016/s0966-842x(00)01784-4. [DOI] [PubMed] [Google Scholar]
- 12.Golovliov I, Ericsson M, Sandström G, Tärnvik A, Sjöstedt A. Identification of proteins of Francisella tularensis induced during growth in macrophages and cloning of the gene encoding a prominently induced 23-kilodalton protein. Infect Immun. 1997;65:2183–2189. doi: 10.1128/iai.65.6.2183-2189.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Golovliov I, Sandström G, Ericsson M, Sjöstedt A, Tärnvik A. Cytokine expression in the liver during the early phase of murine tularemia. Infect Immun. 1995;63:534–538. doi: 10.1128/iai.63.2.534-538.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gross A, Terraza A, Ouahrani-Bettache S, Liautard J P, Dornand J. In vitro Brucella suis infection prevents the programmed cell death of human monocytic cells. Infect Immun. 2000;68:342–351. doi: 10.1128/iai.68.1.342-351.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hersh D, Monack D M, Smith M R, Ghori N, Falkow S, Zychlinsky A. The Salmonella invasin SipB induces macrophage apoptosis by binding to caspase-1. Proc Natl Acad Sci USA. 1999;96:2396–2401. doi: 10.1073/pnas.96.5.2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hilbi H, Moss J E, Hersh D, Chen Y, Arondel J, Banerjee S, Flavell R A, Yuan J, Sansonetti P J, Zychlinsky A. Shigella-induced apoptosis is dependent on caspase-1 which binds to IpaB. J Biol Chem. 1998;273:32895–32900. doi: 10.1074/jbc.273.49.32895. [DOI] [PubMed] [Google Scholar]
- 17.Kaufmann S H. Killing vs suicide in antibacterial defence. Trends Microbiol. 1999;7:59–61. doi: 10.1016/s0966-842x(98)01444-9. [DOI] [PubMed] [Google Scholar]
- 18.Korzeniewski C, Callewaert D M. An enzyme-release assay for natural cytotoxicity. J Immunol Methods. 1983;64:313–320. doi: 10.1016/0022-1759(83)90438-6. [DOI] [PubMed] [Google Scholar]
- 19.Lai X H, Arencibia I, Johansson A, Wai S N, Oscarsson J, Kalfas S, Sundqvist K G, Mizunoe Y, Sjöstedt A, Uhlin B E. Cytocidal and apoptotic effects of the ClyA protein from Escherichia coli on primary and cultured monocytes and macrophages. Infect Immun. 2000;68:4363–4367. doi: 10.1128/iai.68.7.4363-4367.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lai X H, Wang S Y, Uhlin B E. Expression of cytotoxicity by potential pathogens in the standard Escherichia coli collection of reference (ECOR) strains. Microbiology. 1999;145:3295–3303. doi: 10.1099/00221287-145-11-3295. [DOI] [PubMed] [Google Scholar]
- 21.Mills S D, Boland A, Sory M P, van der Smissen P, Kerbourch C, Finlay B B, Cornelis G R. Yersinia enterocolitica induces apoptosis in macrophages by a process requiring functional type III secretion and translocation mechanisms and involving YopP, presumably acting as an effector protein. Proc Natl Acad Sci USA. 1997;94:12638–12643. doi: 10.1073/pnas.94.23.12638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monack D M, Mecsas J, Ghori N, Falkow S. Yersinia signals macrophages to undergo apoptosis and YopJ is necessary for this cell death. Proc Natl Acad Sci USA. 1997;94:10385–10390. doi: 10.1073/pnas.94.19.10385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rojas M, Barrera L F, Puzo G, Garcia L F. Differential induction of apoptosis by virulent Mycobacterium tuberculosis in resistant and susceptible murine macrophages: role of nitric oxide and mycobacterial products. J Immunol. 1997;159:1352–1361. [PubMed] [Google Scholar]
- 24.Ruckdeschel K, Harb S, Roggenkamp A, Hornef M, Zumbihl R, Kohler S, Heesemann J, Rouot B. Yersinia enterocolitica impairs activation of transcription factor NF-kappaB: involvement in the induction of programmed cell death and in the suppression of the macrophage tumor necrosis factor alpha production. J Exp Med. 1998;187:1069–1079. doi: 10.1084/jem.187.7.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stenmark S, Sunnemark D, Bucht A, Sjöstedt A. Rapid local expression of interleukin-12, tumor necrosis factor alpha, and gamma interferon after cutaneous Francisella tularensis infection in tularemia-immune mice. Infect Immun. 1999;67:1789–1797. doi: 10.1128/iai.67.4.1789-1797.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vanmaele R P, Finlayson M C, Armstrong G D. Effect of enteropathogenic Escherichia coli on adherent properties of Chinese hamster ovary cells. Infect Immun. 1995;63:191–198. doi: 10.1128/iai.63.1.191-198.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]