Abstract
Background: Breast cancer developed at a young age (≤45 years) is hypothesized to have unique biology; however, findings in this field are controversial. Methods: We compared the whole transcriptomic profile of young vs. old-age breast cancer using DNA microarray. RNA was extracted from 13 fresh estrogen receptor (ER)-positive primary breast cancer tissues of untreated patients (7 = young age ≤45 years and 6 = old age ≥55 years). In silico validation for the differentially expressed genes (DEGs) by young-age patients was conducted using The Cancer Genome Atlas (TCGA) database. Next, we analyzed the protein expression encoded by two of the significantly down-regulated genes by young-age patients, Glycine N-acyltransferase-like 1 (GLYATL-1) and Ran-binding protein 3 like (RANBP3L), using immunohistochemical analysis in an independent cohort of 56 and 74 ER-positive pre-therapeutic primary breast cancer tissues, respectively. Results: 12 genes were significantly differentially expressed by young-age breast cancers (fold change >2 or <2- with FDR p-value < 0.05). TCGA data confirmed the differential expression of six genes. Protein expression analysis of GLYATL-1 and RANBP3L did not show heterogeneous expression between young and old-age breast cancer tissues. Loss of expression of GLYATL-1 was significantly (p-value 0.005) associated with positive lymph node status. Higher expression of RANBP3L was significantly associated with breast cancers with lower histopathological grades (p-value 0.038). Conclusions: At the transcriptomic level, breast cancer developed in young and old age patients seems homogenous. The variation in the transcriptomic profiles can be attributed to the other clinicopathological characteristics rather than the age of the patient.
Keywords: breast cancer, young age, gene expression, estrogen-receptor-positive, transcriptomic profile, GLYATL-1, RANBP3L
1. Introduction
Breast cancer developed at a young age (≤45 years) has aggressive clinicopathological characteristics and poor clinical outcomes compared to breast cancer developed at old age [1,2,3,4,5,6,7,8]. An earlier gene expression study revealed that breast cancer at a young age (≤45 years) differentially expresses more than 350 gene sets compared to breast cancer in older women (≥65 years) [9]. The research group reanalyzed the exact data and found that breast cancer at a young age has a higher proportion of aggressive intrinsic subtypes rather than a distinct transcriptomic profile, and thereby recommended that treatment options must rely on the tumor grade and molecular subtype and not on the age of the patient [10]. In contrast, a literature-based study reported that 12 genes were expressed in an age-related manner in breast cancer tissue; the upregulated genes were involved in biological processes associated with immature mammary cell populations and growth factor signaling, while the downregulated genes were related to apoptotic pathways, suggesting that young patients may benefit from targeted therapy [11]. Johnson et al. also found that several genes for proliferation, invasion, and metastasis show differential expression between young (<40 years) and old (>40 years) age breast tumors. In addition, the expression of those genes appears to correlate with patient prognosis [12]. Analyzing a large cohort of breast cancer gene expression data, Liao et al. found that the distinct genomic profile of breast cancer at a young age (≤45 years) can only be observed in estrogen-receptor (ER)-positive cancer, whereas in ER-negative tumors, the unique biology vanishes [13]. Using DNA microarray analysis, Malvia and colleagues found that numerous genes implicated in breast cancer invasion and metastasis were significantly upregulated in early-onset breast cancer (≤40 years) compared to late-onset breast cancer (≥55 years) [14]. A recent study analyzed publicly available gene expression data sets of primary breast cancer. The study reported that young-age breast cancers are enriched with cell proliferation gene signatures that have strong prognostic values; these findings were observed mainly in luminal subtypes [15].
With all these controversial findings regarding the biology of breast cancer at a young age, further research in light of previous literature is warranted. The current study focused on ER-positive cancer as those tumors encompass more than 70% of all breast cancers [16]. In addition, previous findings emphasized that the gene expression profile of ER-negative tumors does not show variation among different age groups [13]. Furthermore, epidemiological studies highlighted that among ER-positive breast cancer patients, age remains an independent prognostic factor for clinical outcomes [7,8].
2. Materials and Methods
2.1. Breast Cancer Tissues
We collected 13 fresh ER-positive primary breast cancer tissues from untreated patients (7 = young age ≤45 years and 6 = old age ≥55 years). Breast tissue samples were transferred immediately from the operation theatre to Pathology Laboratory, Hospital Universiti Sains Malaysia (HUSM) for further analysis. Less than approximately 50 mg of tissue was collected from the tumor area by a well-trained pathologist. Tumor tissues were placed immediately in Paxgene Fixative solution (PreAnalytiX, Hombrechtikon, Zürich, Switzerland) and kept overnight at 4 °C. After 24 h, the tissues were transferred to Paxgene stabilizer solution (PreAnalytiX, Hombrechtikon, Zürich, Switzerland) and kept at −80 °C until the RNA extraction procedure. Paxgene fixative can preserve tissue morphology and nucleic acid integrity. Breast cancer tissues were used in agreement with the ethical approval obtained from the Human Research Ethics Committee (HREC), Universiti Sains Malaysia, which complies with the declaration of Helsinki, Study protocol code USM/JEPeM/19090547, approved on the 2 January 2020.
2.2. RNA Extraction
Less than 50 mg of breast cancer tissue was used for RNA extraction. Total RNA was extracted using TRIzol reagent (Sigma-Aldrich, St Louis, MO, USA) and RNeasy Mini Kit (QIAGEN, Hilden, Germany), following manufacturer instructions with minimal modifications. Quality was assessed using Agilent 2100 Bioanalyzer (Thermo Fisher Scientific, Waltham, MA, USA). RNA samples with RNA integrity number (RIN) ≥7 indicated good quality RNA. In our study, 9 out of 13 samples had RIN above 7, and 4 samples had RIN numbers below 7 (sample no. 5 = 6.8, sample no. 17 = 6.4, and sample no. 19 = 6.80), which were also used for transcriptomic profiling. One sample from young age patients was excluded from further analysis as the RIN number was 3.90.
2.3. Transcriptomic Profiling
Gene expression profiling was performed using the Affymetrix Clariom S Human microarray gene chip. The gene chip contains probe sets that interrogate more than 21,000 well-annotated genes. In summary, 125 ng RNA was processed by a Whole Transcript (WT) Plus reagent kit (#902280) from Thermo Fisher Scientific to synthesize the cDNA. Following, cDNA was fragmented and labeled. Labeled cDNA was added to the hybridization mix and incubated in a Clariom S human array for 16 h at 45 °C. Subsequently, the Gene Chip FS450 fluidics station was used to stain and wash the cartridges. Finally, the Gene Chip Scanner 3000 7G was used to scan the cartridges. Raw data were imported to transcriptome analysis console (TAC) software (version 4.0.2.15) for further analyses.
2.4. Differential Gene Expression Analysis
Gene expression analysis was performed using TAC software. The CEL files were normalized and summarized using the robust multi-array analysis (RMA) algorithm [17]. The Limma package was used to identify the differentially expressed genes (DEGs) between young and old-age breast cancers.
2.5. In Silico Validation for the Differentially Expressed Genes by Young Age Breast Cancer Tissues
The expression of the 12 differentially expressed genes by young-age breast cancer was validated using the web-portal UALCAN http://ualcan.path.uab.edu (accessed on 12 December 2022) [18], a database that utilizes The Cancer Genome Atlas (TCGA) gene expression data.
2.6. Analysis of Prognostic Significance of the Differentially Expressed Genes by ER-Positive Young-Age Breast Cancer
A Kaplan-Meier plotter for breast cancer (http://kmplot.com/analysis/, accessed on 12 December 2022) was used to assess the prognostic value of the DEGs by young-age patients. The relapse-free survival curves were presented with hazard ratio and 95% confidence intervals [19].
2.7. Protein Expression Analysis Using Immunohistochemical (IHC) Staining
IHC staining was performed to measure the change in protein expression associated with the change in mRNA levels. Two significantly differentially expressed genes by young-age breast cancer tissues were selected (GLYATL-1 and RANBP3L) (Fold change = −21.37, −14.28, False Discovery Rate (FDR) p-value 0.033, 0.0247), respectively. Both genes showed loss of expression in young age compared to old age cancers in the current gene expression study. Antibodies against the encoded proteins were applied to the formalin-fixed paraffin-embedded tissue sections of an independent larger breast cancer cohort.
2.7.1. Breast Cancer Tissue Blocks
IHC analysis was carried out at the Pathology laboratory, Universiti Sains Malaysia, Kelantan, Malaysia. Surgical and core biopsy tissue blocks of breast carcinoma patients who were diagnosed histopathologically in the period between January 2013 and June 2022 were retrieved. The inclusion and exclusion criteria for the protein expression study matched those mentioned earlier for gene expression analysis (positive ER status, age at diagnosis ≤45 years or ≤55 years, pre-therapeutic samples). In addition, patients with unavailable tissue blocks or who had tissue blocks but with insufficient material for immunohistochemical analysis were excluded. A total of 74 patients were included. However, later on, 74 samples were successfully stained with RANBP3L and 57 samples were stained for GLYATL-1 due to limited resources. The corresponding demographic and clinicopathological features were recorded, including the patient’s age, tumor size, histopathological grade, histopathological subtype, lymph node positivity, progesterone receptor (PR) status, and HER-2 amplification status by IHC and equivocal cases were confirmed by the dual– scolor hapten brightfield in situ hybridization method (DDISH).
2.7.2. Immunohistochemical Staining
3 µm formalin-fixed paraffin-embedded (FFPE) tissue sections were cut on poly L lysine slides using a microtome (LEICA RM 2245). The sections were dewaxed and hydrated using xylene and gradient ethanol. Then, slides were immersed in a target antigen retrieval solution (pH 6.0, citrate buffer) in a pressure cooker for 30 min to retrieve the masked epitopes. Next, sections were incubated with 3% hydrogen peroxide for 10 min to block the endogenous peroxidase activity. Then, for each patient, one section was incubated with Rabbit polyclonal GLYATL-1 primary antibody (Abcam, UK, cat No: ab187859, 1:100 dilution) and one was incubated with Rabbit polyclonal RANBP3L primary antibody (Abbexa, cat No: abx027590, 1:100 dilution); the incubation period for both antibodies was overnight at 4 °C. The next day, slides were washed twice with Tris Buffered Saline (TBS) and incubated with horse reddish peroxidase (Dako REAL EnVision™+System, cat No: K5007) for 30 min at room temperature. To visualize the antigen-antibody reaction, slides were incubated with 3, 3′-diaminobenzidine tetrahydrochloride chromogen for 5 min. Finally, slides were washed with the TBS and stained with freshly prepared hematoxylin for 5 min. Finally, sections were dehydrated, cleared, and mounted.
As recommended by the manufacturer, kidney tissue sections were used for positive and negative controls for both antibodies. In case of negative control the primary antibody incubation step was omitted.
2.7.3. IHC Scoring
The H-score system was used for both antibodies. This scoring system depends on determining the intensity of the stain (0, no staining; 1, weak staining; 2, mild to moderate staining; 3, strong staining) and the percentage of positive tumor cells. The following equation was used to calculate the score [20].
H-score = (% of cells with weak staining × 1) + (% of cells with moderate staining × 2) + (% of cells with strong staining × 3).
The resulting H-score ranged from 0 to 300. An H-score of more than the median value (200 for both markers) was established as a cut-off value to distinguish high expression from low expression. The positive control section of the GLYATL-1 antibody needed to show cytoplasmic immunoreactivity, whereas nuclear and cytoplasmic immunoreactivity was required for the RANBP3L antibody. All slides were scored by two independent observers who were blinded to the study design and the clinicopathological features of included cases.
2.8. Statistical Analysis
A one-way ANOVA test was used to determine the differentially expressed genes between young and old-age breast cancers. The estimated variance by the ANOVA test for each probeset was corrected using the information from other probesets (eBayes empirical parameter) [21]. Using eBayes is mandatory in studies utilizing a small sample size. The moderated t-statistics test was used to calculate the p-value for each transcript cluster (gene). To control the false discovery rate resulting from multiple testing, Benjamini- Hochberg’s method was applied. Each gene with a fold change >2 or <−2 with an adjusted p-value of less than 0.05 was considered significantly differentially expressed.
For the protein expression, data analysis was performed using SPSS software version 26.0. Descriptive statistics were used to describe the clinicopathological characteristics of the included cases. Variables were presented as frequency (n) and percentage (%). Associations between GLYATL-1 and RANBP3L expression and various clinicopathological characteristics were assessed using Pearson’s chi-square test and Fisher’s exact test. An association with a p-value less than 0.05 was considered significant.
3. Results
3.1. Patients and Clinicopathological Characteristics of Breast Cancer Samples
From July 2020 to May 2021, 19 breast cancer tissue samples from untreated patients were collected at the histopathology laboratory at Hospital Universiti Sains Malaysia (HUSM). Of these 19 samples, 13 patients met the inclusion criteria. Of the 13 cases, 7 were ≤45 years of age and 6 were ≥55 years. All patients were diagnosed histopathologically with invasive breast carcinoma of no specific type except one mucinous-type case. All the tumors were ER-receptor positive by IHC analysis. Later on, one patient from the young age group was excluded due to the poor quality of the extracted RNA (RNA Integrity Number 3.9). Accordingly, a total of 12 patients were successfully enrolled in the gene expression study. The clinicopathological characteristics of the patients included in the gene expression study are summarized in Table 1.
Table 1.
Clinicopathological characteristics of breast cancer cases included in the gene expression study.
| Patients ID | Age/Year | Age Group | Tumor Size/cm | TNM Stage | Bloom Richardson Grading |
Lymph Node Status | Histological Subtype | ER | PR | HER-2 |
|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 58 | Old | 2 to 5 | pT1N1 | Grade 2 | Positive | IDC-NST | Positive | Positive | 3+ |
| 3 | 82 | Old | 2 to 5 | Unknown | Grade 1 | Negative | Mucinous | Positive | Positive | 1+ |
| 5 | 45 | Young | 2 to 5 | pT2N3a | Grade 2 | Positive | IDC-NST | Positive | Positive | 3+ |
| 7 | 39 | Young | >5 cm | pT3N0Mx | Grade 3 | Negative | IDC-NST | Positive | Negative | 3+ |
| 8 | 43 | Young | 2 to 5 | PT2N2a | Grade 2 | Positive | IDC-NST | Positive | Positive | 3+ |
| 9 | 67 | Old | <2 cm | pT1cN3a | Grade 2 | Positive | IDC-NST | Positive | Positive | 1+ |
| 10 | 45 | Young | 2 to 5 | pT2N1 | Grade 3 | Positive | IDC-NST | Positive | Positive | 3+ |
| 12 | 60 | Old | >5 cm | Unknown | Grade 1 | Negative | IDC-NST | Positive | Positive | 1+ |
| 13 | 38 | Young | <2 cm | pT1N2aMx | Grade 2 | Positive | IDC-NST | Positive | Positive | 3+ |
| 17 | 69 | Old | <2 cm | pT2pN0 | Grade 3 | Negative | IDC-NST | Positive | Negative | 3+ |
| 18 | 45 | Young | <2 cm | pT2N2aMx | Grade 2 | Positive | IDC-NST | Positive | Positive | 1+ |
| 19 | 61 | Old | >5 cm | pT3N3a | Grade 3 | Positive | IDC-NST | Positive | Positive | 1+ |
The expression of estrogen receptor (ER), progesterone receptor (PR), and HER-2 was assessed by immunohistochemical staining. Equivocal HER-2 expression was confirmed using the dual-color dual-hapten brightfield in situ hybridization method (DDISH), Invasive ductal carcinoma- no specific type (IDC-NST).
3.2. Differentially Expressed Genes
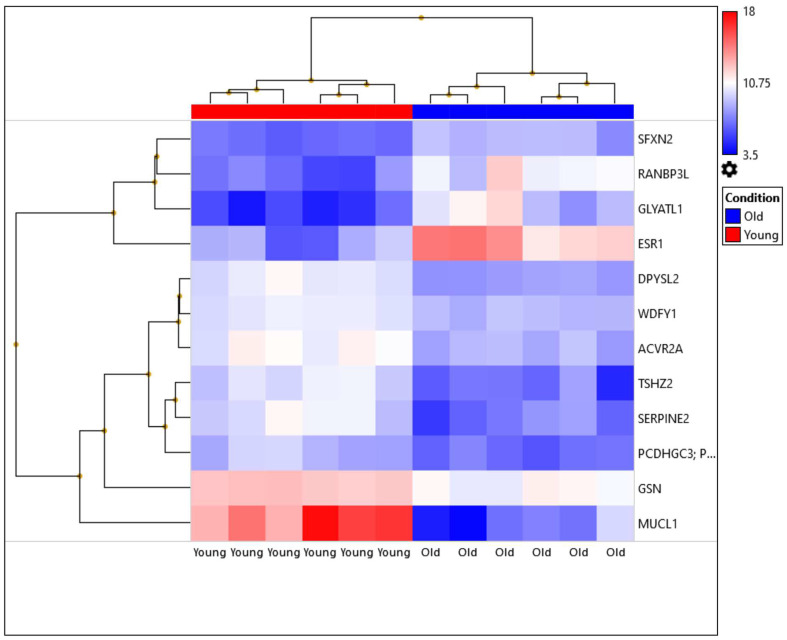
Out of 21,448 tested genes, only 12 genes were significantly differentially expressed in young-age breast cancer (fold change of <2 or >2 and FDR p-value < 0.05). Of these differentially expressed genes, 8 were upregulated (DPYSL2, MUCL1, GSN, ACVR2A, TSHZ2, SERPINE2, WDFY1, and PCDHGB7), while 4 were down-regulated (SFXN2, RANBP3L, ESR1, and GLYATL1). The level of expression of the DEGs (n = 12) is illustrated in Table 2 and Figure 1. A summary regarding the significance of the DEGs in tumorigenesis and cancer progression is presented in Table 3.
Table 2.
List of the significantly differentially expressed genes by young-age breast cancer tissues.
| Young Average (log2) | Old Average (log2) | Fold Change | p-Value | FDR p-Value |
Gene Symbol |
Description |
|---|---|---|---|---|---|---|
| 9.99 | 7.91 | 4.25 | 7.30 × 10−7 | 0.0099 | DPYSL2 | Dihydropyrimidinase-like 2 |
| 15.26 | 6.45 | 448.69 | 9.25 × 10−7 | 0.0099 | MUCL1 | Mucin-like 1 |
| 6.59 | 8.84 | −4.76 | 5.35 × 10−6 | 0.0247 | SFXN2 | Sideroflexin 2 |
| 12.42 | 10.69 | 3.32 | 5.47 × 10−6 | 0.0247 | GSN | Gelsolin |
| 6.61 | 10.44 | −14.28 | 6.71 × 10−6 | 0.0247 | RANBP3L | RAN binding protein 3-like |
| 8.63 | 13.13 | −22.62 | 6.90 × 10−6 | 0.0247 | ESR1 | Estrogen receptor 1 |
| 10.7 | 8.5 | 4.6 | 1.30 × 10−5 | 0.0332 | ACVR2A | Activin A receptor type IIA |
| 5.17 | 9.59 | −21.37 | 1.35 × 10−5 | 0.0332 | GLYATL1 | Glycine-N-acyltransferase-like 1 |
| 9.76 | 6.68 | 8.44 | 1.39 × 10−5 | 0.0332 | TSHZ2 | Teashirt zinc finger homeobox 2 |
| 9.96 | 6.75 | 9.27 | 2.60 × 10−5 | 0.0497 | SERPINE2 | Serpin peptidase inhibitor, clade E |
| 10.1 | 8.77 | 2.52 | 2.63 × 10−5 | 0.0497 | WDFY1 | WD repeat and FYVE domain containing 1 |
| 8.41 | 6.55 | 3.63 | 2.78 × 10−5 | 0.0497 | PCDHGB7 | Protocadherin gamma subfamily B, 7 |
Figure 1.
Heatmap illustrating the expression levels of the differentially expressed genes (DEGs) between the young and old-age breast cancer tissues (n = 12). Hierarchical clustering of the 12 ER-positive breast cancer cases. Six samples of young age patients ≤45 years and six samples of old age patients ≥55 years. The expression levels for each differentially expressed gene are reflected by a color ranging from blue (low) to red (high).
Table 3.
The implication of the differentially expressed genes by young age ER-positive breast cancer in tumorigenesis and cancer progression.
| Gene ID | Expression Status in Young-Age Breast Cancer | Fold Change | FDR p-Value | Significance from Previous Literature | References |
|---|---|---|---|---|---|
| DPYSL2 | Up-regulated | 4.25 | 0.0099 | DYYSL2 is a regulator of cytoskeletal dynamics in growing axons. DPYSL2 knockout in mesenchymal-like cells inhibits cell migration, invasion, stemness features, tumour growth rate, and metastasis. Interaction between DPYSL2 and Janus kinase 1 induces the expression of vimentin which is a marker for epithelial-mesenchymal transition (EMT) and involved in cancer progression. | [22] |
| MUCL1 | Up-regulated | 448.69 | 0.0099 | Higher expression of MUCL1 was observed in HER2-amplified breast tumors. MUCL1 plays an essential role for MUCL1 in the proliferation of breast cancer cells, through the FAK/JNK signaling pathway. | [23] |
| SFXN2 | Down-regulated | −4.76 | 0.0247 | Loss of SFXN2 resulted in the accumulation of mitochondrial iron, and increased mitochondrial iron levels in TNBC generated large amounts of ROS that activated the NF-κB and TGF-β signaling pathways, which eventually promoted cell migration. | [24] |
| GSN | Up-regulated | 3.32 | 0.0247 | Higher expression of gelsolin was reported to be associated with axillary lymph node metastasis. | [25] |
| RANBP3L | Down-regulated | 14.28 | 0.0277 | In murine renal cells, loss of Ranbp3L expression resulted in the loss of epithelial characteristics, enhanced migration behavior and colony-forming capacity, and substantially altered gene expression profiles. | [26,27] |
| ESR1 | Down-regulated | −22.62 | 0.0247 | In estrogen receptor-positive breast cancer, a low level of ESR1 mRNA expression was a determinant of tamoxifen resistance in both adjuvant treatment and prevention settings. | [28] |
| ACVR2A | Up-regulated | 4.65 | 0.0259 | Over-expression of ACVR2A was associated with larger tumors (T3 and T4) in colorectal cancer clinical samples. This indicates an association between ACVR2A expression and the tumor growth process. | [29] |
| GLYATL1 | Down-regulated | −21.37 | 0.0332 | Down-regulated in several cancers and loss of expression was associated with higher tumor grade and poor prognosis in prostate adenocarcinoma and hepatocellular carcinoma patients. | [30,31] |
| TSHZ2 | Up-regulated | 8.44 | 0.0332 | Up-regulation of TSHZ2 was found to repress tumor growth and metastasis and induce mammary gland development in mice. | [32] |
| SERPINE2 | Up-regulated | 9.27 | 0.0497 | SerpinE2 overexpression in breast cancer was shown to promote metastatic spread by modulating the extracellular matrix. | [33] |
| WDFY1 | Up-regulated | 2.52 | 0.0497 | WDFY1 positively regulated Toll-like receptor (TLR) 3 and 4 signalings. TLR signaling regulates breast cancer cell proliferation in TP53 mutated cells. | [34] |
| PCDHGB7 | Up-regulated | 3.63 | 0.0497 | Overexpression of PCDH7 stimulated breast cancer cell proliferation and invasion in vitro and the formation of bone metastasis in vivo. PCDH7 was found to play role in bone metastasis in breast cancer. | [35] |
3.3. In Silico Validation of the Differentially Expressed Genes by Young-Age Breast Cancer
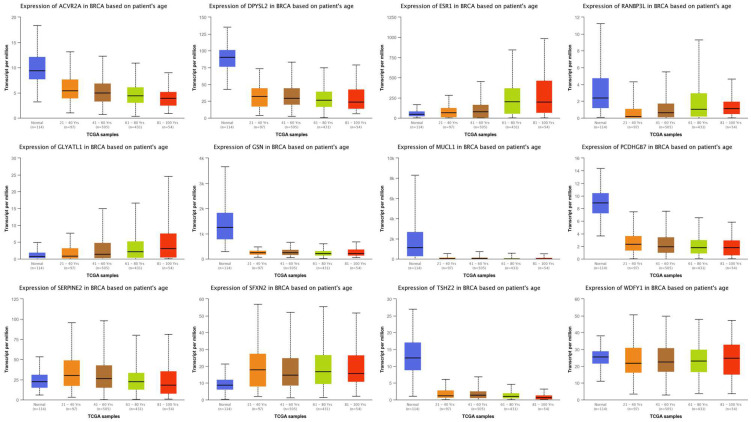
To validate the expression levels of the DEGs in a larger sample size, we used the web portal UALCAN http://ualcan.path.uab.edu [18], a database that utilizes The Cancer Genome Atlas (TCGA) gene expression data. Breast cancer expression data were used and a filter was set to determine the expression of the 12 genes among different age groups in breast cancer. Six genes out of twelve showed consistent expression (RANBP3L, GLYATL1, ESR1, ACVR2A, SERPINE2, and PCDHGB7) (Figure 2).
Figure 2.
Validation of the differentially expressed genes by young-age breast cancer tissues using RNA-seq data from TCGA database. ACVR2A, SERPINE2, and PCDHGB7 show upregulation in young-age breast cancer patients compared to old age patients. RANBP3L, GLYATL-1, and ESR1 show down-regulation in young age patients compared to old age patients. p-values for each comparison are presented in Supplementary Table S1.
3.4. Prognostic Significance of the Differentially Expressed Genes by Young Age ER-Positive Breast Cancer
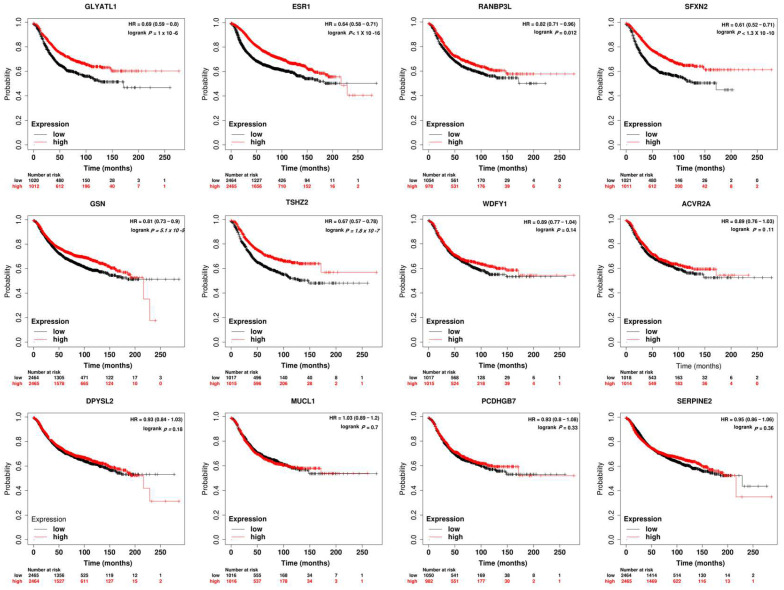
Survival analysis showed that the loss of expression of RANBP3L, GLYATL1, ESR1, and SFXN2 was significantly related to shorter relapse-free survival (RFS). High expressions of GSN and TSHZ2 were significantly related to longer RFS (Figure 3).
Figure 3.
Prognostic Significance of the differentially expressed genes by ER-positive young-age breast cancer. Lower expression of RANBP3L, GLYATL1, ESR1, and SFXN2 were significantly related to shorter relapse-free survival (RFS). However, high expressions of GSN and TSHZ2 were significantly related to longer RFS.
3.5. Evaluation of GLYALT-1 and RANBP3L Protein Expression Using Immunohistochemical Analysis
The clinicopathological characteristics of breast cancer patients included in the immunohistochemical analysis of GLYALT-1 and RANBP3L (n = 56 and 73 patients, respectively) included age, tumor size, histopathological grade, histopathological subtype, lymph node positivity, progesterone receptor status and HER-2 expression status. These characteristics are summarized in Table 4 and Table 5.
Table 4.
Clinicopathological characteristics of 56 breast carcinoma cases stained with GLYATL-1.
| Demographic and Clinicopathological Characteristics | Frequency (Percentage) |
|---|---|
| Age | |
| Old (≥55 years) | 25 (44.6) |
| Young (≤45 years) | 31 (55.4) |
| Tumor size | |
| <2 cm | 9 (16.1) |
| >5 cm | 8 (14.3) |
| 2–5 cm | 30 (53.6) |
| Unknown | 9 (16.1) |
| Histopathological grade (Modified Bloom Richardson Grading system) | |
| Grade 1 | 12 (21.4) |
| Grade 2 | 25 (44.6) |
| Grade 3 | 13 (23.2) |
| Unknown | 6 (10.7) |
| Histopathological subtype | |
| Invasive carcinoma, No Special Type (NST) | 48 (85.7) |
| Other subtypes | 7 (12.5) |
| Unknown | 1 (1.8) |
| Lymph node positivity | |
| Negative | 18 (32.1) |
| Positive | 29 (51.8) |
| Unknown | 9 (16.1) |
| Progesterone receptor status | |
| Negative | 9 (16.1) |
| Positive | 47 (83.9) |
| HER-2 expression | |
| Negative | 35 (62.5) |
| Positive | 14 (25.0) |
| Unknown | 7 (12.5) |
| GLYATL-1 expression | |
| High | 23 (41.1) |
| Low | 33 (58.9) |
Table 5.
Clinicopathological characteristics of 74 breast carcinoma cases stained with RANBP3L.
| Demographic and Clinicopathological Characteristics | Frequency (Percentage) |
|---|---|
| Age | |
| Old (≥55 years) | 41 (55.4) |
| Young (≤45 years) | 33 (44.6) |
| Tumor size | |
| <2 cm | 11 (14.9) |
| >5 cm | 13 (17.6) |
| 2–5 cm | 38 (51.4) |
| Unknown | 12 (16.2) |
| Histopathological grade (Modified Bloom Richardson Grading system) | |
| Grade 1 | 24 (32.4) |
| Grade 2 | 31 (41.9) |
| Grade 3 | 14 (18.9) |
| Unknown | 5 (6.8) |
| Histopathological subtype | |
| Invasive carcinoma, No Special Type (NST) | 62 (83.8) |
| Other subtypes | 12 (16.2) |
| Lymph node positivity | |
| Negative | 27 (36.5) |
| Positive | 31 (41.9) |
| Unknown | 16 (21.6) |
| Progesterone receptor status | |
| Negative | 12 (16.2) |
| Positive | 60 (81.1) |
| Unknown | 2 (2.7) |
| HER-2 expression | |
| Negative | 49 (66.2) |
| Positive | 16 (21.6) |
| Unknown | 9 (12.2) |
| RANBP3L expression | |
| High | 47 (63.5) |
| Low | 27 (36.5) |
3.5.1. GLYATL-1 Expression in Breast Carcinoma Tissues
An immunohistochemical stain of GLYATL-1 was performed for 56 breast carcinoma tissue sections. The expression of GLYATL-1 was localized to the cytoplasm. Higher expression of GLYATL-1 was observed in 41.1% of the sample (23/56), whereas 58% (33/56) of cases exhibited a low level of expression. Normal breast ducts showed a higher expression of GLYATL-1 compared to breast carcinoma in situ and invasive breast carcinoma tissues (Figure 4).
Figure 4.
GLYATL-1 expression in normal breast duct, breast carcinoma in situ, and invasive breast carcinoma tissues. GLYATL-1 expression in (A,B) normal breast duct tissues. (C,D) Breast carcinoma in situ. (E,F) Invasive breast carcinoma tissues. (A,C,E) ×20 μm. (B,D,F) ×40 μm.
3.5.2. Association between GLYATL-1 Expression with the Age and Other Clinicopathological Parameters of Patients with Breast Carcinoma
Lower expression of GLYATL-1 was strongly associated with positive lymph node status (p < 0.005 obtained by Fisher’s exact test). However, no significant association was found between GLYATL-1 expression and the other clinicopathological features including: age, tumor size, histopathological grade, histopathological subtype, PR and HER-2 status (see Table 6).
Table 6.
Association between GLYATL-1 expression and the clinicopathological features of breast cancer patients.
| Parameters | N | GLYATL-1 Expression | p-Value | |
|---|---|---|---|---|
| High | Low | |||
| Total, n (%) | 56 | 23 (41.1) | 33 (58.9) | |
| Age (years) | 0.551 | |||
| ≥55 | 25 (44.6) | 10 (43.5) | 15 (45.5) | |
| ≤ 45 | 31 (55.4) | 13 (56.5) | 18 (54.5) | |
| Tumor size | 0.507 | |||
| <2 cm | 9 (16.1) | 2 (8.7) | 7 (21.2) | |
| >5 cm | 8 (14.3) | 4 (17.4) | 4 (12.1) | |
| 2–5 cm | 30 (53.6) | 12 (52.2) | 18 (54.5) | |
| Unknown | 9 (16.1) | 5 (21.7) | 4 (12.1) | |
| Histopathological grade | 0.574 | |||
| Grade 1 | 12 (21.4) | 5 (21.7) | 7 (21.2) | |
| Grade 2 | 25 (44.6) | 10 (43.5) | 15 (45.5) | |
| Grade 3 | 13 (23.2) | 4 (17.4) | 9 (27.3) | |
| Unknown | 6 (10.7) | 4 (17.4) | 2 (6.1) | |
| Histopathological Subtype | 0.11 | |||
| Invasive carcinoma, No Special Type (NST) | 48 (15.2) | 18 (78.3) | 30 (90.9) | |
| Other subtypes | 7 (67.5) | 5 (21.7) | 2 (6.1) | |
| Unknown | 1 (1.8) | 0 (0.0) | 1 (3.0) | |
| Lymph node status | 0.005 | |||
| Negative | 18 (32.1) | 12 (52.2) | 6 (18.2) | |
| Positive | 29 (51.8) | 6 (26.1) | 23 (69.7) | |
| Unknown | 9 (16.1) | 5 (21.7) | 4 (12.1) | |
| PR status | 0.449 | |||
| Negative | 9 (16.1) | 3 (13.0) | 6 (18.2) | |
| Positive | 47 (83.9) | 20 (87.0) | 27 (81.8) | |
| HER-2 | 0.786 | |||
| Negative | 35 (62.5) | 13 (56.5) | 22 (66.7) | |
| Positive | 14 (25.0) | 7 (30.4) | 7 (21.2) | |
| Unknown | 7 (12.5) | 3 (13.0) | 4 (12.1) | |
3.5.3. Expression of RANBP3L in Breast Cancer Tissues
The expression level of RANBP3L was examined in 74 breast carcinoma tissue sections. The signal we obtained was nuclear and cytoplasmic (Figure 5). A high level of RANBP3L expression was observed in 64% of the cases (47/74), whereas 36% of cases (27/74) exhibited a low level of expression. A strong nuclear signal was observed in normal breast ducts, whereas moderate nuclear and cytoplasmic signals were observed in ductal carcinoma in situ cases. The signal faded with a higher histopathological grade (Figure 5).
Figure 5.
RANBP3L expression in normal breast duct, ductal carcinoma in situ, and invasive breast carcinoma tissues. RANBP3L expression in (A,B) normal breast duct tissues, (C,D) ductal carcinoma in situ tissues, and (E,F) invasive breast carcinoma tissues; (A,E,F), ×50 μm, (B), ×20 μm, (C,D), ×100 μm.
3.5.4. Association between RANBP3L Expression and Age and Other Clinicopathological Parameters of Patients with Breast Carcinoma
Higher expression of RANBP3L was significantly associated with a lower histopathological grade (Grade 1) (p < 0.038 obtained by Fisher’s exact test); however, no significant association was found between RANBP3L expression and the other clinicopathological features such as: age, tumor size, histopathological subtype, PR and HER-2 status (see Table 7).
Table 7.
Association of RANBP3L expression with the clinicopathological features of breast cancer patients.
| Parameters | N | RANBP3L Expression | p-Value | |
|---|---|---|---|---|
| High | Low | |||
| Total, n (%) | 74 | 47 (63.5) | 27 (36.5) | |
| Age (years) | 0.108 | |||
| ≥55 | 41 (55.4) | 23 (48.9) | 18 (66.7) | |
| ≤45 | 33 (44.6) | 24 (51.1) | 9 (33.3) | |
| Tumor size | 0.088 | |||
| <2 cm | 11 (14.9) | 5 (10.6) | 6 (22.2) | |
| >5 cm | 13 (17.6) | 7 (14.9) | 6 (22.2) | |
| 2–5 cm | 38 (51.4) | 24 (51.1) | 14 (51.9) | |
| Unknown | 12 (16.2) | 11 (23.4) | 1 (3.7) | |
| Histopathological grade | 0.038 | |||
| Grade I | 24 (32.4) | 20 (42.6) | 4(18.4) | |
| Grade II | 31 (41.9) | 19 (40.4) | 12 (44.4) | |
| Grade III | 14 (18.9) | 6 (12.8) | 8 (29.6) | |
| Unknown | 5 (6.8) | 2 (4.3) | 3 (11.1) | |
| Histopathological Subtype | 0.54 | |||
| Invasive carcinoma, No Special Type (NST) | 62 (83.8) | 39 (83.0) | 23 (85.2) | |
| Other subtypes | 12 (16.2) | 8 (17.0) | 4 (14.8) | |
| Lymph node status | 0.202 | |||
| Negative | 27 (36.5) | 19 (40.4) | 8 (29.6) | |
| Positive | 31 (41.9) | 16 (34.0) | 15 (55.6) | |
| Unknown | 16 (21.6) | 12 (25.5) | 4 (14.8) | |
| PR status | 0.108 | |||
| Negative | 12 (16.2) | 9 (19.1) | 3 (11.1) | |
| Positive | 60 (81.1) | 38 (80.9) | 22 (81.5) | |
| Unknown | 2 (2.7) | 0 (0.0) | 2 (7.4) | |
| HER-2 | 0.584 | |||
| Negative | 49 (66.2) | 29 (61.7) | 20 (74.1) | |
| Positive | 16 (21.6) | 11 (23.4) | 5 (18.5) | |
| Unknown | 9 (12.2) | 7 (14.9) | 2 (7.4) | |
4. Discussion
Management of breast cancer developed at a young age is considered a clinical dilemma as breast cancer at a young age has poor clinicopathological characteristics at the time of presentation compared to breast cancer that arises in old age [36,37]; in addition, locoregional recurrence is a more frequent event in young age patients [38]. Furthermore, young age has been proposed as an independent factor for shorter breast cancer-specific and overall survival [39,40].
In the current study, we compared the transcriptomic profile of young (≤45 years) versus old age (≥55 years) ER-positive breast cancers of untreated patients. The differential gene expression analysis revealed that 12 genes were differentially expressed by young-age breast cancer tissues (fold change >2 or <−2 with FDR p-value < 0.05). Of the 12 genes, 8 were upregulated and 4 were downregulated.
RANBP3L and GLYATL-1 showed extreme loss of expression in young age patients; this finding is consistent with Liao and colleagues’ findings. They found that ER-positive breast cancer in pre-menopausal women (≤45 years) has a lower level of RANBP3L and GLYATL-1 compared to post-menopausal women (≥55 years). It is noteworthy that Liao et al.’s study included more than 2500 breast cancer cases [13]. The protein encoded by RANBP3L is a nuclear exporter of bone morphogenetic protein-specific smads and plays a critical role in mesenchymal stem cell differentiation [41]. Loss of RANBP3L expression was found to be associated with loss of epithelial differentiation and induced cell migration behavior in renal cancer cells [26]. However, loss of GLYATL-1 expression was significantly associated with higher Gleason scores in prostatic adenocarcinoma [31], with shorter overall survival in hepatocellular carcinoma patients [30].
Estrogen receptor 1 ESR1 also showed down-regulation in young age patients compared to old age patients; this is in line with a previous large-scale genomic analysis that revealed that breast cancer developed in young age patients has a lower level of ESR1 mRNA compared to breast cancer in old age patients [9]. Loss of ESR1 expression is characteristic of acquiring resistance to chemotherapy in ER-positive breast cancer [42]. In a previous study, poor clinical outcomes were observed in young age patients who both received and did not receive tamoxifen therapy. This is a clear indication of endocrine therapy resistance in this group of patients [7].
Another noteworthy significantly down-regulated gene by young age patients in the present study was sideroflexin 2 (SFXN2); the encoded protein by SFXN2 is implicated in mitochondrial iron metabolism [43]. Loss of this protein may result in abnormal iron metabolism which, in turn, may result in tumor initiation, progression, and metastasis [24].
Survival analyses in the present study revealed that loss of RANBP3L, GLYATL-1, ESR1, and SFXN2 was significantly related to lower RFS in breast cancer (p-value < 0.012, 1.1 × 10−6, 1 × 10−16, and 1.3 × 10−10, respectively).
One of the genes that showed significant overexpression by the young age group was mucin-like 1 (MUCL1) (FC = 448.69, FDR-p-value < 0.009). Previous studies found that MUCL1 is expressed by the majority of breast cancer cell lines (>90%) as it is recognized that mucins in general form the ductal surfaces of several organs, including the breast [44]. Overexpression of MUCL1 mRNA was strongly correlated with higher tumor grade, lymph node positivity, and high recurrence and death rates in breast cancer patients [23].
We also validated the expression of the 12 DEGs between young and old-age breast cancer tissues using the TCGA database. The results show that six genes have concordance expression to that obtained in our gene expression experiment. The TCGA data showed that young-age breast cancer patients have a lower level of expression of RANBP3L, GLYATL-1, and ESR1, whereas ACVR2A, SERPINE2, and PCDHGB7 have higher expression in young-age breast cancer patients compared to old age patients.
There is growing evidence showing that genes that show significant differential expression tend to correlate with the expression of their encoded protein [45,46]. Thus, we selected RANBP3L and GLYATL-1 to compare the expression of their encoded proteins in breast carcinoma tissue samples and determine the relationship between the expression of the proteins and the age of breast cancer patients. The expression of both markers has not been comprehensively investigated previously regarding breast cancer. For GLYATL-1, only one published report described the protein expression in clinical breast cancer samples [47]. For RANBP3L, to our knowledge, this is the first study to examine the mRNA and protein expression of RANBP3L in breast cancer clinical samples.
Protein expression analysis results revealed a strong association between the loss of GLYATL-1 expression and breast tumors with positive lymph node status (p-value 0.005). On the other hand, a significant association was found between the high expression of RANBP3L and breast tumors with a low histopathological grade (Modified Bloom Richardson Grade I). However, no significant association was found between the expression of both proteins and the age of breast cancer patients.
These findings indicate that the difference in the transcriptomic profiles we determined in the current study originate from the poor clinicopathological characteristics of breast cancer at a young age, such as positive lymph node status and a higher histopathological tumor grade, rather than the age of the patient. To verify this, we reanalyzed the gene expression data after matching the lymph node status/histopathological grade. The differentially expressed gene list (n = 12) diminished to zero, indicating that the genes that showed differential expression between the two groups were associated with the lymph node positivity status and tumor histopathological grade rather than the age of the patients.
Our findings strongly support an earlier report published by the American Journal of Clinical Oncology verifying that age alone does not add a layer of complexity to the transcriptomic profile of breast cancer but that molecular subtype and tumor grade are the main factors that alter the transcriptomic profile of breast cancer. This study emphasized that treatment options must be selected based on tumor molecular subtype and grade and not patient age [10]. Moreover, an earlier gene expression study involving 99 breast cancer tissue samples concluded that breast cancer gene expression patterns show a strong association with ER status; (this was standardized in the current study), and moderate association with tumor grade; however, no association was found with patient age (<50 years vs. ≥50 years) [48].
Our study limitation is the small sample size used in the gene expression study as a result of using strict inclusion and exclusion criteria; only patients with ER-positive tumors were included as ER-negative tumors do not show differences in the transcriptomic profiles or clinical outcomes among different age groups [8,13]. Additionally, patients who received neoadjuvant therapy were also excluded since it is well-established that neoadjuvant therapy alters the transcriptomic profile of breast cancer [49]. Finally, patients aged between 45–55 years were excluded as they were considered of intermediate age, not belonging to young or old age groups.
Although our study findings do not support the historical hypothesis that breast cancer developed at a young age has unique biology, our findings alter the direction of future research toward other factors that may play a significant role in the poor clinical outcomes of early-onset breast cancer.
5. Conclusions
Our findings indicate that the difference in the transcriptomic profiles between young and old age estrogen-receptor-positive breast cancer is due to the aggressive clinicopathological feature of breast cancer developed in young age patients rather than the age of the patients.
Acknowledgments
The authors wish to express their thanks to the Ministry of Higher Education Malaysia (MOHE) for funding the current study through the fundamental research grant scheme (FRGS), number FRGS/1/2019/SKK08/USM/02/15.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biomedicines11010200/s1, Table S1: Statistical significance of the TCGA data comparison.
Author Contributions
Conceptualization, A.S., W.F.W.A.R., S.N.M.N. and S.S.; methodology, A.S. and W.F.W.A.R.; formal analysis, A.S., R.R. and K.I.M.; investigation, A.S.; writing—original draft preparation, A.S.; Writing-review and editing, W.F.W.A.R., S.N.M.N., M.M.Y. and T.A.D.A.-A.T.D.; supervision, W.F.W.A.R.; patient recruitment, M.M.Y.; funding acquisition, W.F.W.A.R. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Human Research Ethics Committee (HREC), Universiti Sains Malaysia (study protocol code USM/JEPeM/19090547, approved on 2 January 2020).
Informed Consent Statement
Informed consent was obtained from all participants and/or their legal guardian(s) before their inclusion in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
All related data are available within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The current study was funded by the Ministry of Higher Education Malaysia (MOHE), fundamental research grant scheme number FRGS/1/2019/SKK08/USM/02/15, Institutional number 203.PPSP.6171249. The funding body had no role in the study design; the collection, analysis, and interpretation of data; or in writing the manuscript.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Bleyer A., on behalf of the Biology and Clinical Trials Subgroups of the US National Cancer Institute Progress Review Group in Adolescent and Young Adult Oncology. Barr R., Hayes-Lattin B., Thomas D., Ellis C., Anderson B. The distinctive biology of cancer in adolescents and young adults. Nat. Rev. Cancer. 2008;8:288–298. doi: 10.1038/nrc2349. [DOI] [PubMed] [Google Scholar]
- 2.Beadle B.M., Woodward W., Buchholz T.A. The Impact of Age on Outcome in Early-Stage Breast Cancer. Semin. Radiat. Oncol. 2011;21:26–34. doi: 10.1016/j.semradonc.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yıldırım E., Dalgıç T., Berberoğlu U. Prognostic significance of young age in breast cancer. J. Surg. Oncol. 2000;74:267–272. doi: 10.1002/1096-9098(200008)74:4<267::AID-JSO5>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 4.Kataoka A., Iwamoto T., Tokunaga E., Tomotaki A., Kumamaru H., Miyata H., Niikura N., Kawai M., Anan K., Hayashi N., et al. Young adult breast cancer patients have a poor prognosis independent of prognostic clinicopathological factors: A study from the Japanese Breast Cancer Registry. Breast Cancer Res. Treat. 2016;160:163–172. doi: 10.1007/s10549-016-3984-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maggard M.A., O’Connell J.B., Lane K.E., Liu J.H., Etzioni D.A., Ko C.Y. Do young breast cancer patients have worse outcomes? J. Surg. Res. 2003;113:109–113. doi: 10.1016/S0022-4804(03)00179-3. [DOI] [PubMed] [Google Scholar]
- 6.Bertheau P., Steinberg S.M., Cowan K., Merino M.J. Breast cancer in young women: Clinicopathologic correlation. Semin. Diagn. Pathol. 1999;16:248–256. [PubMed] [Google Scholar]
- 7.Ahn S.H., Son B.H., Kim S.W., Kim S.I., Jeong J., Ko S.-S., Han W. Poor Outcome of Hormone Receptor–Positive Breast Cancer at Very Young Age Is Due to Tamoxifen Resistance: Nationwide Survival Data in Korea—A Report From the Korean Breast Cancer Society. J. Clin. Oncol. 2007;25:2360–2368. doi: 10.1200/JCO.2006.10.3754. [DOI] [PubMed] [Google Scholar]
- 8.Partridge A.H., Hughes M.E., Warner E.T., Ottesen R.A., Wong Y.-N., Edge S.B., Theriault R.L., Blayney D.W., Niland J.C., Winer E.P., et al. Subtype-Dependent Relationship Between Young Age at Diagnosis and Breast Cancer Survival. J. Clin. Oncol. 2016;34:3308–3314. doi: 10.1200/JCO.2015.65.8013. [DOI] [PubMed] [Google Scholar]
- 9.Anders C.K., Hsu D.S., Broadwater G., Acharya C.R., Foekens J.A., Zhang Y., Wang Y., Marcom P.K., Marks J.R., Febbo P.G., et al. Young Age at Diagnosis Correlates With Worse Prognosis and Defines a Subset of Breast Cancers With Shared Patterns of Gene Expression. J. Clin. Oncol. 2008;26:3324–3330. doi: 10.1200/JCO.2007.14.2471. [DOI] [PubMed] [Google Scholar]
- 10.Anders C.K., Fan C., Parker J.S., Carey L.A., Blackwell K.L., Klauber-Demore N., Perou C. Breast Carcinomas Arising at a Young Age: Unique Biology or a Surrogate for Aggressive Intrinsic Subtypes? J. Clin. Oncol. 2011;29:e18–e20. doi: 10.1200/JCO.2010.28.9199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azim H.A., Michiels S., Bedard P.L., Singhal S.K., Criscitiello C., Ignatiadis M., Haibe-Kains B., Piccart M.J., Sotiriou C., Loi S. Elucidating Prognosis and Biology of Breast Cancer Arising in Young Women Using Gene Expression Profiling. Clin. Cancer Res. 2012;18:1341–1351. doi: 10.1158/1078-0432.CCR-11-2599. [DOI] [PubMed] [Google Scholar]
- 12.Johnson R.H., Hu P., Fan C., Anders C.K. Gene expression in ‘young adult type’ breast cancer: A retrospective analysis. Oncotarget. 2015;6:13688. doi: 10.18632/oncotarget.4051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liao S., Hartmaier R.J., McGuire K.P., Puhalla S.L., Luthra S., Chandran U.R., Ma T., Bhargava R., Modugno F., Davidson N.E., et al. The molecular landscape of premenopausal breast cancer. Breast Cancer Res. 2015;17:104. doi: 10.1186/s13058-015-0618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malvia S., Bagadi S.A.R., Pradhan D., Chintamani C., Bhatnagar A., Arora D., Sarin R., Saxena S. Study of Gene Expression Profiles of Breast Cancers in Indian Women. Sci. Rep. 2019;9:10018. doi: 10.1038/s41598-019-46261-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ingebriktsen L.M., Finne K., Akslen L.A., Wik E. A novel age-related gene expression signature associates with proliferation and disease progression in breast cancer. Br. J. Cancer. 2022;127:1865–1875. doi: 10.1038/s41416-022-01953-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lumachi F., Brunello A., Maruzzo M., Basso U., Basso S.M.M. Treatment of Estrogen Receptor-Positive Breast Cancer. Curr. Med. Chem. 2013;20:596–604. doi: 10.2174/092986713804999303. [DOI] [PubMed] [Google Scholar]
- 17.Irizarry R.A., Bolstad B.M., Collin F., Cope L.M., Hobbs B., Speed T.P. Summaries of Affymetrix GeneChip probe level data. Nucleic Acids Res. 2003;31:e15. doi: 10.1093/nar/gng015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chandrashekar D.S., Karthikeyan S.K., Korla P.K., Patel H., Shovon A.R., Athar M., Netto G.J., Qin Z.S., Kumar S., Manne U., et al. UALCAN: An update to the integrated cancer data analysis platform. Neoplasia. 2022;25:18–27. doi: 10.1016/j.neo.2022.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Győrffy B. Survival analysis across the entire transcriptome identifies biomarkers with the highest prognostic power in breast cancer. Comput. Struct. Biotechnol. J. 2021;19:4101–4109. doi: 10.1016/j.csbj.2021.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Azim H.A., Peccatori F.A., Brohée S., Branstetter D., Loi S., Viale G., Piccart M., Dougall W.C., Pruneri G., Sotiriou C. RANK-ligand (RANKL) expression in young breast cancer patients and during pregnancy. Breast Cancer Res. 2015;17:24. doi: 10.1186/s13058-015-0538-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de la Nava J.G., van Hijum S., Trelles O. Saturation and quantization reduction in microarray experiments using two scans at different sensitivities. Stat. Appl. Genet. Mol. Biol. 2004;3 doi: 10.2202/1544-6115.1057. [DOI] [PubMed] [Google Scholar]
- 22.Rmaileh A.A., Solaimuthu B., Ben Yosef M., Khatib A. Dihydropyrimidinase-like 2 (DPYSL2) regulates breast cancer migration via a JAK/STAT3/vimentin axis. bioRxiv. 2021;2 doi: 10.1101/2021.03.21.436294. [DOI] [Google Scholar]
- 23.Conley S.J., Bosco E.E., Tice D.A., Hollingsworth R.E., Herbst R., Xiao Z. HER2 drives Mucin-like 1 to control proliferation in breast cancer cells. Oncogene. 2016;35:4225–4234. doi: 10.1038/onc.2015.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen C., Wang S., Liu P. Deferoxamine Enhanced Mitochondrial Iron Accumulation and Promoted Cell Migration in Triple-Negative MDA-MB-231 Breast Cancer Cells Via a ROS-Dependent Mechanism. Int. J. Mol. Sci. 2019;20:4952. doi: 10.3390/ijms20194952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borhan A., Nozarian Z., Abdollahi A., Shahsiah R., Mohammadpour H., Borhan A. Evaluation of the Relationship Between Expression of Villin and Gelsolin Genes and Axillary Lymph Node Metastasis in Patients with Breast Cancer. Iran. J. Pathol. 2021;16:27–32. doi: 10.30699/ijp.2020.121532.2322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chernyakov D., Groß A., Fischer A., Bornkessel N., Schultheiss C., Gerloff D., Edemir B. Loss of RANBP3L leads to transformation of renal epithelial cells towards a renal clear cell carcinoma like phenotype. J. Exp. Clin. Cancer Res. 2021;40:226. doi: 10.1186/s13046-021-01982-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chernyakov D., Bornkessel N., Fischer A., Groß A., Edemir B. RanBP3L is a NFAT5 target gene and its deficiency in principal cells promotes epithelial mesenchymal transition through MAPK signaling. FASEB J. 2020;34:1. doi: 10.1096/fasebj.2020.34.s1.00455. [DOI] [Google Scholar]
- 28.Kim C., Tang G., Pogue-Geile K.L., Costantino J.P., Baehner F.L., Baker J., Cronin M.T., Watson D., Shak S., Bohn O.L., et al. Estrogen Receptor (ESR1) mRNA Expression and Benefit From Tamoxifen in the Treatment and Prevention of Estrogen Receptor–Positive Breast Cancer. J. Clin. Oncol. 2011;29:4160–4167. doi: 10.1200/JCO.2010.32.9615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wodziński D., Wosiak A., Pietrzak J., Świechowski R., Jeleń A., Balcerczak E. Does the expression of the ACVR2A gene affect the development of colorectal cancer? Genet. Mol. Biol. 2019;42:32–39. doi: 10.1590/1678-4685-gmb-2017-0332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guan R., Hong W., Huang J., Peng T., Zhao Z., Lin Y., Yu M., Jian Z. The expression and prognostic value of GLYATL1 and its potential role in hepatocellular carcinoma. J. Gastrointest. Oncol. 2020;11:1305–1321. doi: 10.21037/jgo-20-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eich M.L., Chandrashekar D.S., Rodriguez Peña M.D.C., Robinson A.D., Siddiqui J., Daignault-Newton S., Chakravarthi B.V.S.K., Kunju L.P., Netto G.J., Varambally S. Characterization of glycine-N-acyltransferase like 1 (GLYATL1) in prostate cancer. Prostate. 2019;79:1629–1639. doi: 10.1002/pros.23887. [DOI] [PubMed] [Google Scholar]
- 32.Uribe M.L., Dahlhoff M., Batra R.N., Nataraj N.B., Haga Y., Drago-Garcia D., Marrocco I., Sekar A., Ghosh S., Yarden Y., et al. TSHZ2 is an EGF-regulated tumor suppressor that binds to the cytokinesis regulator PRC1 and inhibits metastasis. Sci. Signal. 2021;14:eabe6156. doi: 10.1126/scisignal.abe6156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smirnova T., Bonapace L., MacDonald G., Kondo S., Wyckoff J., Ebersbach H., Fayard B., Doelemeyer A., Coissieux M.-M., Heideman M.R., et al. Serpin E2 promotes breast cancer metastasis by remodeling the tumor matrix and polarizing tumor associated macrophages. Oncotarget. 2016;7:82289–82304. doi: 10.18632/oncotarget.12927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haricharan S., Brown P. TLR4 has a TP53-dependent dual role in regulating breast cancer cell growth. Proc. Natl. Acad. Sci. USA. 2015;112:E3216–E3225. doi: 10.1073/pnas.1420811112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li A.-M., Tian A.-X., Zhang R.-X., Ge J., Sun X., Cao X.-C. Protocadherin-7 induces bone metastasis of breast cancer. Biochem. Biophys. Res. Commun. 2013;436:486–490. doi: 10.1016/j.bbrc.2013.05.131. [DOI] [PubMed] [Google Scholar]
- 36.Yang Y., Wei W., Jin L., He H., Wei M., Shen S., Pi H., Liu Z., Li H., Liu J. Comparison of the Characteristics and Prognosis Between Very Young Women and Older Women With Breast Cancer: A Multi-Institutional Report From China. Front. Oncol. 2022;12 doi: 10.3389/fonc.2022.783487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Copeland J., Oyedeji A., Powell N., Cherian C.J., Tokumaru Y., Murthy V., Takabe K., Young J. Breast Cancer in Jamaica: Stage, Grade and Molecular Subtype Distributions Across Age Blocks, the Implications for Screening and Treatment. World J. Oncol. 2021;12:93–103. doi: 10.14740/wjon1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bollet M.A., Sigal-Zafrani B., Mazeau V., Savignoni A., de la Rochefordière A., Vincent-Salomon A., Salmon R., Campana F., Kirova Y.M., Dendale R., et al. Age remains the first prognostic factor for loco-regional breast cancer recurrence in young (<40 years) women treated with breast conserving surgery first. Radiother. Oncol. 2007;82:272–280. doi: 10.1016/j.radonc.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 39.Azim H.A., Partridge A.H. Biology of breast cancer in young women. Breast Cancer Res. 2014;16:427. doi: 10.1186/s13058-014-0427-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gabriel C., Domchek S. Breast cancer in young women. Breast Cancer Res. 2010;12:212. doi: 10.1186/bcr2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen F., Lin X., Xu P., Zhang Z., Chen Y., Wang C., Han J., Zhao B., Xiao M., Feng X.-H. Nuclear Export of Smads by RanBP3L Regulates Bone Morphogenetic Protein Signaling and Mesenchymal Stem Cell Differentiation. Mol. Cell. Biol. 2015;35:1700–1711. doi: 10.1128/MCB.00121-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stossi F., Madak-Erdoğan Z., Katzenellenbogen B.S. Macrophage-elicited loss of estrogen receptor-α in breast cancer cells via involvement of MAPK and c-Jun at the ESR1 genomic locus. Oncogene. 2011;31:1825–1834. doi: 10.1038/onc.2011.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen Y., Qian J., Ding P., Wang W., Li X., Tang X., Tang C., Yang Y., Gu C. Elevated SFXN2 limits mitochondrial autophagy and increases iron-mediated energy production to promote multiple myeloma cell proliferation. Cell Death Dis. 2022;13:1–14. doi: 10.1038/s41419-022-05272-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Colpitts T.L., Billing P., Granados E., Hayden M., Hodges S., Roberts L., Russell J., Friedman P., Stroupe S. Identification and Immunohistochemical Characterization of a Mucin-Like Glycoprotein Expressed in Early Stage Breast Carcinoma. Tumor Biol. 2002;23:263–278. doi: 10.1159/000068566. [DOI] [PubMed] [Google Scholar]
- 45.Koussounadis A., Langdon S.P., Um I.H., Harrison D., Smith V.A. Relationship between differentially expressed mRNA and mRNA-protein correlations in a xenograft model system. Sci. Rep. 2015;5:srep10775. doi: 10.1038/srep10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gry M., Rimini R., Strömberg S., Asplund A., Pontén F., Uhlén M., Nilsson P. Correlations between RNA and protein expression profiles in 23 human cell lines. BMC Genom. 2009;10:365. doi: 10.1186/1471-2164-10-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tian X., Wu L., Jiang M., Zhang Z., Wu R., Miao J., Liu C., Gao S. Downregulation of GLYAT Facilitates Tumor Growth and Metastasis and Poor Clinical Outcomes Through the PI3K/AKT/Snail Pathway in Human Breast Cancer. Front. Oncol. 2021;11 doi: 10.3389/fonc.2021.641399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sotiriou C., Neo S.-Y., McShane L.M., Korn E.L., Long P.M., Jazaeri A., Martiat P., Fox S.B., Harris A.L., Liu E.T. Breast cancer classification and prognosis based on gene expression profiles from a population-based study. Proc. Natl. Acad. Sci. USA. 2003;100:10393–10398. doi: 10.1073/pnas.1732912100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Magbanua M.J.M., Wolf D.M., Yau C., Davis S.E., Crothers J., Au A., Haqq C.M., Livasy C., Rugo H.S., Esserman L., et al. Serial expression analysis of breast tumors during neoadjuvant chemotherapy reveals changes in cell cycle and immune pathways associated with recurrence and response. Breast Cancer Res. 2015;17:1–13. doi: 10.1186/s13058-015-0582-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All related data are available within the article.