Key Points
Question
Is there an association between intimate partner violence, maternal depressive symptoms, harsh child discipline, child stimulation, and children’s socioemotional development in rural Tanzania?
Findings
This cross-sectional study used data from 981 mothers and their children aged 18 to 36 months and noted that physical only and physical and sexual intimate partner violence were associated with lower child socioemotional development scores. An association was also observed between mild to severe maternal depressive symptoms and lower child socioemotional development scores.
Meaning
The findings of this cross-sectional study suggest that children whose mothers experienced intimate partner violence or depressive symptoms appear to have poorer socioemotional development.
Abstract
Importance
Approximately 1 in 4 women experience intimate partner violence (IPV) or nonpartner sexual violence during their lifetime. Mothers exposed to IPV are more likely to experience depressive symptoms and to discipline their children harshly, which may affect their children’s socioemotional development; however, there is limited evidence on these outcomes.
Objective
To examine the association between IPV, maternal depressive symptoms, harsh child discipline, and child stimulation with child socioemotional development.
Design, Setting, and Participants
This study used cross-sectional follow-up data collected from February 19 to October 10, 2014, from a birth cohort of children aged 18 to 36 months who were enrolled in a randomized, double-blind, placebo-controlled trial of neonatal vitamin A supplementation in the Morogoro region of Tanzania. Data analysis occurred between September 10, 2019, and January 20, 2020.
Exposures
Lifetime experience of IPV was assessed using an abbreviated module of the Tanzania Demographic and Health Survey, maternal depressive symptoms were assessed with the Patient Health Questionnaire, and data on harsh child discipline and maternal stimulation of their children were collected using modules of the United Nations Children's Fund Multiple Indicator Cluster Survey.
Main Outcomes and Measures
Child socioemotional development was measured by the Caregiver-Reported Early Childhood Development Instruments.
Results
A total of 981 mother-child dyads were included in the analytic sample; 388 children (39.6%) were between ages 18 and 24 (mean [SD] age, 27.06 [6.08]) months, and 515 (52.5%) were male children. A negative association was observed between maternal report of physical IPV only (mean difference, −0.022; 95% CI, −0.045 to −0.006) and physical and sexual IPV (mean difference, −0.045; 95% CI, −0.077 to −0.013) with child socioemotional scores, but neither was statistically significant after including depressive symptoms in the model, which is consistent with mediation. Furthermore, a negative association was observed between maternal mild to severe depressive symptoms and child socioemotional development, including adjustment for IPV (mean difference, −0.073; 95% CI, −0.103 to −0.043). Harsh disciplinary practices and stimulation were not associated with child socioemotional development after adjusting for IPV, maternal depressive symptoms, and other factors.
Conclusions and Relevance
The findings of this study suggest that maternal depressive symptoms may explain the negative association between IPV and child socioemotional development.
This cross-sectional study examines factors associated with the socioemotional development of children whose mothers experience intimate partner violence.
Introduction
Global estimates indicate that approximately 1 in 4 women have experienced physical and/or sexual intimate partner violence (IPV) or nonpartner sexual violence during their lifetime.1 The prevalence of IPV in low- and middle-income countries is high, with a prevalence of 42% in Western Africa and South Asia and 66% in central sub-Saharan Africa.2 Women who experience IPV report higher rates of several substantial physical and mental health problems, including depression and posttraumatic stress disorder.3 In addition to affecting a woman’s health, IPV may present risks to the safety and well-being of children living in the household, including a higher risk of mortality4 and severe acute malnutrition.5 Furthermore, IPV has been shown to be associated with poorer early child development (ECD) outcomes.6,7 However, the association between sexual and physical IPV with socioemotional development is less clear.
In addition to the direct effects on stress and well-being that IPV may have on children who witness their mothers being abused,8 the association between IPV and ECD may be partially mediated by household and maternal factors, including an increased risk of maternal depression and suboptimal parenting practices. Intimate partner violence may serve as a source of trauma and stress for mothers, compromising their own well-being as well as their ability to respond sensitively and responsively to their children’s needs.9 For example, a study conducted in Tanzania observed that 30.0% of mothers who reported experiencing at least 1 type of IPV during their pregnancy had an increased risk of postpartum depression.10 Childcare practices can also be affected by IPV experience as IPV has been identified as a risk factor for harsh child discipline.11 In Tanzania specifically, a national survey observed that almost three-quarters of children had experienced physical disciplinary practices (eg, being kicked or spanked) and more than one-quarter had experienced emotional violence (eg, being yelled at and humiliated).12 In addition, a recent study reported that the negative association between IPV and overall ECD was mediated by lower levels of maternal and paternal stimulation (the engagement of caregivers in play and learning activities with their young children).6
Independent of IPV, studies have reported that maternal depressive symptoms are associated with lower levels of child socioemotional development13 and increased emotional regulation problems.14 Exposure to maternal depressive symptoms concurrent with IPV has also been noted to be associated with poor language and gross motor development.15 However, despite the volume of literature linking IPV to suboptimal development, there is comparatively limited evidence on the association between IPV, maternal depressive symptoms, and parenting practices with children’s socioemotional development.
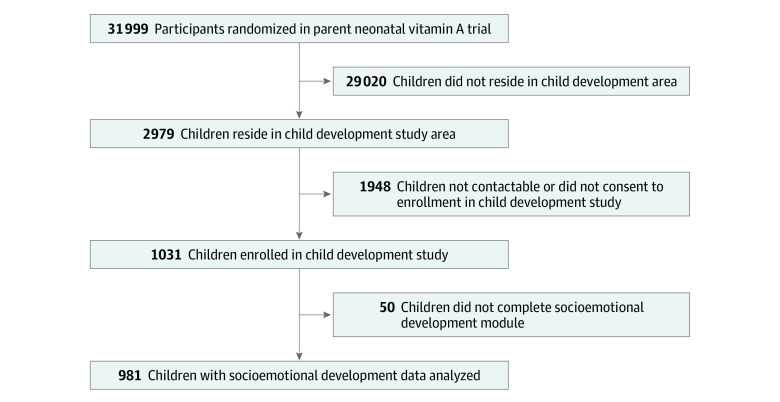
Given these evidence gaps, this study examined the association between IPV, maternal depressive symptoms, harsh child discipline, stimulation, and children’s socioemotional development in rural Tanzania. The hypothesis was that children’s early socioemotional development is associated with maternal experience of IPV, maternal depressive symptoms, and parenting practices (harsh disciplinary practices and early stimulation). The conceptual model we examined is shown in Figure 1.
Figure 1. Conceptual Model.
Methods
Study Design
This analysis used data from a cross-sectional study of child development conducted among a birth cohort of children who were enrolled in a randomized, double-blind, placebo-controlled trial of neonatal vitamin A supplementation (NVAS), conducted in the Morogoro region of Tanzania.16,17 This secondary analysis report is aligned with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. The parent NVAS trial recruited and followed up infants to age 1 year from August 26, 2010, to March 3, 2014. A child development follow-up study was subsequently conducted when the children were aged 18 to 36 months from February 19 to October 10, 2014. The data analysis for the present study occurred between September 10, 2019, and January 20, 2020. Written informed consent was obtained from all participants in this study. All study protocols were approved by institutional review boards at the Harvard T. H. Chan School of Public Health, the National Institute of Medical Research of Tanzania, and the Ifakara Health Institute. Participants were reimbursed for transport expenses based on distance from their home to the study clinic.
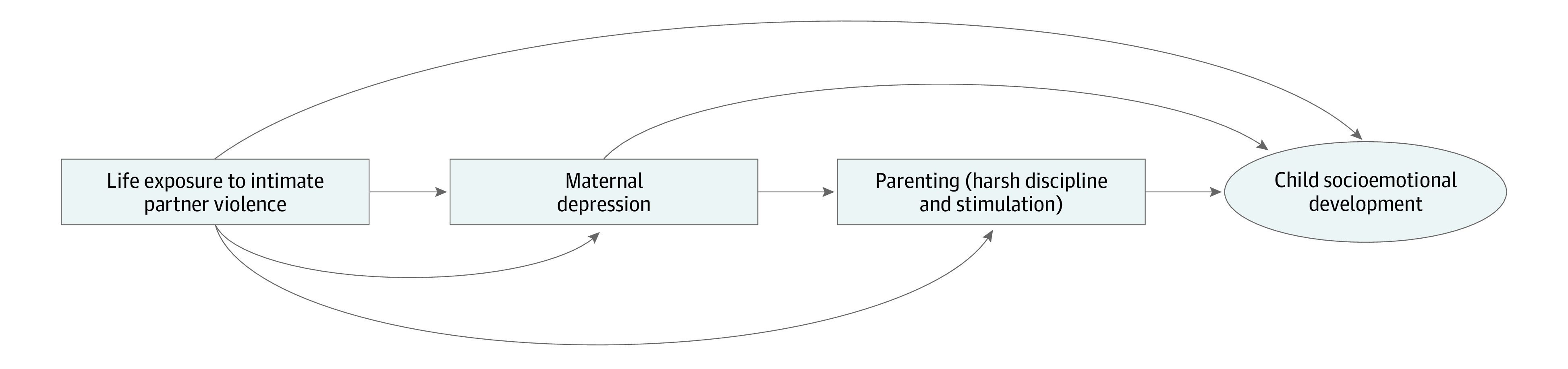
Study Participants
For the NVAS trial, a total of 31 999 randomly selected children living in Morogoro region were enrolled and followed up until age 1 year. For the child development follow-up study, sampling was restricted to a subset of children from the original trial living within the Ifakara Demographic Surveillance Site. The full cohort was not followed up due to logistic and financial reasons. Children were selected for participation in the child development study based on the following inclusion criteria: (1) age 18 to 36 months at the time of assessment, (2) lived in Ifakara town or surrounding villages, and (3) caregiver consented to participate.16 No data on race and ethnicity were recorded. The mother-child pairs included in the sample for this study were selected by a computer-generated random number drawn from the primary NVAS trial sample and received both a home visit and an invitation to an additional clinic visit, which occurred 1 to 6 days after the home visit for data collection activities. The analytic sample comprised 981 mothers who completed the IPV questionnaire, maternal depressive symptoms assessment, and childcare questionnaire.
Study Data Collection
Trained field staff visited the home to administer a questionnaire to collect mothers’ demographic, socioeconomic, and environmental information, as well as their reports on parenting practices (disciplinary practices and stimulation) and child development using the Caregiver-Reported Early Childhood Development Instruments (CREDI),16,18,19 as explained with more details in the Measures section. Data collectors were 8 male, secondary school–educated field workers with previous experience in research with families and children in the area. The coordinators were provided with a 2-day training session on the CREDI and other study assessments. They supported the data collectors in the field once every 2 weeks to ensure continued adherence to study protocols. The data collectors observed the caregivers’ understanding of the CREDI items and recorded any questions or concerns stated by the caregivers during the interview.
Measures
Children’s Socioemotional Development
Children’s socioemotional development was the primary outcome of interest and was measured using the CREDI.16 The CREDI is a caregiver-reported, low-cost, and culturally neutral measure of ECD in children younger than 3 years. The CREDI was validated for the Tanzania population with good acceptability and adequate reliability. Cronbach α coefficients calculated suggested acceptable internal consistency and interitem reliability, with an internal consistency for the socioemotional subscale of α = 0.68.16 The initial validation effort in Tanzania suggested that the CREDI tool may provide a valid method for capturing young children’s development across socioemotional domains and an acceptable tool for use in low-resourced settings.16 The socioemotional scale comprises 20 items on emotional and behavioral self-regulation, emotional knowledge, and social competence. For example, the field team asked the mother 2 questions: “Does the child involve others in play (ie, play interactive games with other children)?” “Does the child smile when others smile at him/her?” The CREDI is scored continuously using age-standardized scoring procedures that are based on children’s raw percentage yes (pass) responses within each age group. The CREDI average scores range from 0 to 1, with lower scores indicating lower development.
Intimate Partner Violence
Lifetime exposure to IPV was assessed using an abbreviated IPV module of the Tanzania Demographic and Health Survey.20 Four categories were considered: none when the mother did not experience any type of IPV, IPV physical (only) if the mother answered yes when asked about whether her partner had ever physically hurt her, IPV sexual (only) if the mother answered yes when asked whether her partner had ever forced her to have sexual intercourse or perform other sexual acts with him, and IPV physical and sexual when the mother answered yes for both questions.
Maternal Depressive Symptoms
The Patient Health Questionnaire-9 (PHQ-9) is a scale of maternal depressive symptoms in diverse contexts that scores 9 symptoms of depression.21 The scale has an estimated 90% to 94% sensitivity and a specificity of 75% to 99% for major depressive disorder (assessed with the Mini International Neuropsychiatric Interview) in various groups.22,23 The PHQ-9 has been used as a reliable assessment in primary care settings in sub-Saharan Africa.7,24 The PHQ-9 scores for depressive symptoms are calculated by taking a sum of all 9 items, which are rated on a 0 to 3 response scale (not at all = 0, several days = 1, more than half the days = 2, and nearly every day = 3). Maternal depressive symptoms were then categorized into the following groups: none to minimal (0-4), mild (5-9), moderate (10-14), moderate to severe (15-19), and severe (20-27).21 We merged into 2 categories none to minimal (0-4) and moderate to severe (10-27) due to the low number of participants who scored moderate to severe depressive symptoms (10 participants scored >9 points).
Harsh Child Discipline
Questions on disciplinary practices were taken from the early childhood development module of the United Nations Children's Fund Multiple Indicator Cluster Surveys (MICS), which have been used widely in Tanzania. The questions used in the MICS were drawn from a modified version of the Parent-Child Conflict Tactics Scale25 and asked the mother, “In the past 3 days, has an adult done any of the following with the child: yelled at or scolded him/her? Spanked or hit him/her?” These items were scored considering 0 when the mother’s answer was no and 1 when the answer was yes.
Maternal Stimulation
Maternal stimulation was defined by the mother’s report of whether the child’s mother engaged in 6 play and learning activities with the child in the past 3 days: reading books or looking at pictures; telling stories; taking the child outside of the home compound; playing with the child; naming, counting, or drawing things with the child; and talking with the child while working or doing homework. These series of questions, also drawn from the MICS, are widely used, reliable, and valid measures of parental stimulation with predictive validity for ECD outcomes.26,27,28 We created a total stimulation score by summing the number of activities that the mother did with the child (range, 0-6), with higher values indicating greater maternal stimulation and lower values indicating low stimulation. After that, we created categories for low (0-2 items), moderate (3-4 items), and high (5-6 items) stimulation.29
Statistical Analysis
The cross-sectional associations between experience of IPV, maternal depression, harsh discipline, child stimulation, and early childhood CREDI socioemotional scores were examined. Normality of the socioemotional development variable was assessed with the Shapiro-Wilk test and indicated that the outcome of interest was normally distributed (P > .05).
We constructed univariable linear regression models to assess these associations. We then constructed 3 multivariable linear regression models based on our conceptualization of the associations between the exposures of interest and the children’s socioemotional development (Figure 1). All multivariable models also included adjustment for maternal age (15-24, 25-34, and 35-44 years), maternal educational attainment (primary, secondary, and college), maternal occupation (income-generating activity and no income-generating activity), paternal presence in the home, household wealth quintile, child age and child sex, and the randomized vitamin A or placebo regimen in the parent NVAS trial.
In the first multivariable model, which was the primary analysis, we estimated the association between lifetime experience of IPV as the variable and early child socioemotional development as the outcome. We then constructed secondary models to examine depressive symptoms and harsh punishment as potential mediators for the association of IPV with socioemotional development. In the second model, we examined the association between current maternal depressive symptoms and early child socioemotional development and included adjustment for IPV. In the third model, we examined the association between maternal report of current harsh disciplinary practices and child stimulation with socioemotional development as the outcome, including adjustment for IPV. In the final model, we adjusted for both maternal depressive symptoms and harsh discipline in addition to IPV. We used Q-Q plots to assess the normality of residuals and all models appeared to meet the homoscedasticity and normality assumptions of linear regression. All hypothesis tests were 2-sided and P values <.05 were considered statistically significant. Missing data were included in the multiple models by creating missing value categories. All analyses were conducted using Stata, version 15 (StataCorp LLC).
Results
A total of 981 mother-child dyads were included in the analytic sample (Figure 2). Overall, 388 of the children (39.6%) were between ages 18 and 24 months (mean [SD] age, 27.06 [6.08] months), 515 were male children (52.5%), and 466 were female children (47.5%). Household, maternal, and child characteristics are presented in Table 1. In this sample, 257 mothers (26.2%) reported experiencing physical and/or sexual IPV and 83 mothers (8.5%) were experiencing mild to severe depressive symptoms. The majority of mothers (876 [89.3%]) reported yelling at their children, 609 (62.1%) mothers spanked or hit their children, and 930 (94.8%) reported using a moderate or low number of stimulation activities. The mean (SD) child CREDI socioemotional development score was 0.73 (0.12).
Figure 2. Flow Diagram of Participant Recruitment.
Table 1. Household, Maternal, and Child Characteristics of the Study Population.
| Characteristic | No. (%) |
|---|---|
| Household | |
| Head of the familya | |
| No. | 960 |
| Mother | 52 (5.4) |
| Father | 757 (78.9) |
| Grandparents | 131 (13.6) |
| Other | 20 (2.1) |
| Father stays in the homea | |
| No. | 960 |
| No | 148 (15.4) |
| Yes | 810 (84.4) |
| Not applicable | 2 (0.2) |
| Source of household watera | |
| No. | 960 |
| Pipe water | 223 (23.2) |
| Public tap | 266 (27.7) |
| Open well | 402 (41.9) |
| Closed well | 47 (4.9) |
| Surface water | 13 (1.3) |
| Tube well, borehole, or hand pump | 9 (1.0) |
| Latrinea | |
| No. | 960 |
| Flush toilet | 238 (24.8) |
| Pit latrine | 714 (74.4) |
| Other | 8 (0.8) |
| No. of rooms in the housea | |
| No. | 960 |
| ≤2 | 280 (29.2) |
| 3 | 287 (29.9) |
| ≥4 | 393 (40.9) |
| No. of people that regularly eat in the householda | |
| No. | 977 |
| ≤3 | 243 (24.9) |
| 4-5 | 408 (41.8) |
| ≥6 | 326 (33.4) |
| Mother | |
| Age, ya | |
| No. | 958 |
| 15-24 | 415 (43.3) |
| 25-34 | 439 (45.7) |
| 35-44 | 104 (10.9) |
| No. of childrena | |
| No. | 981 |
| 1 | 264 (26.9) |
| 2 | 247 (25.2) |
| 3 | 204 (20.8) |
| ≥4 | 266 (27.1) |
| Level of educationa | |
| No. | 957 |
| None/some primary | 50 (5.2) |
| Completed primary | 841 (87.9) |
| Secondary or advanced | 66 (6.9) |
| Lifetime exposure to IPV | |
| No. | 981 |
| None | 724 (73.8) |
| Physical violence | 144 (14.7) |
| Sexual violence | 50 (5.1) |
| Physical and sexual violence | 63 (6.4) |
| Depressive symptoms | |
| No. | 981 |
| None or minimal symptoms (PHQ-9 <5) | 898 (91.5) |
| Mild-to-severe symptoms (PHQ-9 ≥5) | 83 (8.5) |
| Mother yells at the child | |
| No. | 981 |
| No | 105 (10.7) |
| Yes | 876 (89.3) |
| Mother spanks/hits the child | |
| No. | 981 |
| No | 372 (37.9) |
| Yes | 609 (62.1) |
| Child stimulation | |
| No. | 981 |
| High | 51 (5.2) |
| Moderate | 529 (53.9) |
| Low | 401 (40.9) |
| Child | |
| No. | 981 |
| CREDI socioemotional development score, mean (SD) | 0.73 (0.12) |
| Age, moa | |
| No. | 980 |
| 18-23 | 388 (39.6) |
| 24-30 | 249 (25.4) |
| 30-36 | 343 (35.0) |
| Sex | |
| No. | 981 |
| Male | 515 (52.5) |
| Female | 466 (47.5) |
Abbreviations: CREDI, Caregiver-Reported Early Childhood Development Instruments; IPV, intimate partner violence; PHQ-9, Patient Health Questionnaire.
Missing information.
In the unadjusted analysis, experience of physical IPV only, both physical and sexual IPV, and increased maternal depressive symptoms were significantly associated with lower socioemotional development scores for children (Table 2). Multivariable models are presented in Table 3. In multivariable model 1, physical IPV alone was significantly negatively associated CREDI child socioemotional development scores (mean difference, −0.022; 95% CI, −0.045 to −0.006), and both physical and sexual IPV was also significantly negatively associated CREDI child socioemotional development scores (mean difference −0.045; 95% CI, −0.077 to −0.013). Subsequent models were exploratory and examined the potential factors that mediated the association between IPV and child development outcomes. In model 2, exposure to maternal depressive symptoms was negatively associated with child socioemotional development after adjustment for IPV (mean difference, −0.071; 95% CI, −0.102 to −0.041). In model 3, no associations were observed with exposure to harsh punishment after adjustment for IPV and maternal depressive symptoms. In the final model, maternal depressive symptoms, but not IPV exposure, was negatively associated with early child socioemotional development (mean difference, −0.073; 95% CI, −0.103 to −0.043).
Table 2. Unadjusted Association of IPV, Maternal Depressive Symptoms, Harsh Child Discipline, and Child Stimulation With Child CREDI Socioemotional Development Scores.
| Variable | Mean difference in CREDI score (95% CI) | P value |
|---|---|---|
| IPV | ||
| None | [Reference] | NA |
| Physical | −0.022 (−0.044 to −0.000) | .04 |
| Sexual | −0.011 (−0.046 to 0.023) | .53 |
| Both physical and sexual | −0.050 (−0.081 to −0.019) | .002 |
| Maternal depressive symptoms | ||
| Minimal or none | [Reference] | NA |
| Mild to high | −0.079 (−0.106 to −0.052) | <.001 |
| Mother yells at the child | ||
| No | [Reference] | NA |
| Yes | 0.020 (−0.004 to 0.045) | .10 |
| Mother spanks/hits the child | ||
| No | [Reference] | NA |
| Yes | 0.015 (−0.000 to 0.030) | .06 |
| Child stimulation | ||
| Low | [Reference] | NA |
| Moderate | 0.006 (−0.009 to 0.022) | .40 |
| High | 0.011 (−0.024 to 0.046) | .54 |
Abbreviations: CREDI, Caregiver-Reported Early Childhood Development Instruments; IPV, intimate partner violence; NA, not applicable.
Table 3. Multivariable Analysis of Exposure to IPV, Maternal Depressive Symptoms, Harsh Child Discipline, and Child Stimulation and Child CREDI Socioemotional Development Scores.
| Variable | Mean difference (CI) | ||
|---|---|---|---|
| Model 1: IPVa | Model 2: Maternal depressiona | Model 3: Harsh punishment and stimulationa | |
| IPV | |||
| None | [Reference] | [Reference] | [Reference] |
| Physical | −0.022 (−0.045 to −0.006)b | −0.015 (−0.037 to 0.006) | −0.014 (−0.036 to 0.008) |
| Sexual | −0.012 (−0.048 to 0.023) | −0.002 (−0.037 to 0.032) | −0.000 (−0.036 to 0.034) |
| Both physical and sexual | −0.045 (−0.077 to −0.013)c | −0.025 (−0.058 to 0.007) | −0.021 (−0.054 to 0.012) |
| Maternal depressive symptoms | |||
| Minimal or none | NA | [Reference] | [Reference] |
| Mild to high | NA | −0.071 (−0.102 to −0.041)c | −0.073 (−0.103 to −0.043)c |
| Mother yells at child | |||
| No | NA | NA | [Reference] |
| Yes | NA | NA | 0.012 (−0.014 to 0.039) |
| Mother spanks/hits child | |||
| No | NA | NA | [Reference] |
| Yes | NA | NA | 0.12 (−0.004 to 0.030) |
| Child stimulation | |||
| High | NA | NA | [Reference] |
| Moderate | NA | NA | 0.007 (−0.008 to 0.023) |
| Low | NA | NA | 0.007 (−0.028 to 0.043) |
| No. | 981 | 981 | 981 |
Abbreviations: CREDI, Caregiver-Reported Early Childhood Development Instruments; IPV, intimate partner violence; NA, not applicable.
Adjusted for child sex, maternal age, maternal educational level, father staying at home, wealth index, and randomized vitamin A or placebo regimen.
P < .05.
P < .001.
Discussion
This study found that 1 in 4 mothers reported experiencing physical and/or sexual IPV and approximately 1 in 12 reported mild to severe depressive symptoms in rural Tanzania. There was a high prevalence of harsh disciplinary practices of yelling and spanking or hitting, and most mothers reported performing a moderate to low number of stimulation activities. Maternal reports of physical only and physical and sexual IPV were associated with lower child socioemotional scores and was no longer significant after including depressive symptoms in the model, which is consistent with mediation. Furthermore, maternal mild to severe depressive symptoms were associated with lower child socioemotional development scores, including adjustment for IPV. Use of harsh disciplinary practices or level of stimulation were not associated with child socioemotional development after adjusting for IPV, maternal depressive symptoms, and other factors.
We found that maternal report of physical only and physical and sexual IPV associated with lower child socioemotional scores is consistent with the literature. Children may not directly experience the violence, but they may still be affected by the abuse through the state of maternal mental health.30 A study in the US observed that children whose mothers were exposed to IPV had delay in at least 1 developmental milestone, increasing almost twice the chance of delay in personal-social development.15 Children exposed to IPV are also at increased risk for adverse mental and behavioral health sequelae, as well as effects on the brain and stress regulation systems.31 The stress regulation systems and children’s own mental health could be additional pathways for explaining the association between IPV and children’s socioemotional development that were not explored in this study.
We also found that there was no association of maternal report of IPV with socioemotional development after adjustment for depressive symptoms. As a result, this suggests that maternal depression may mediate the association between IPV and socioemotional development that is consistent with our model presented in Figure 1. Beyond physical manifestations, IPV also affects the mental health of those who experience it. A study in Kenya found that caregivers reporting psychological and physical violence were more likely to be at risk for depression.32 A systematic review noted that children exposed to IPV had a high prevalence of depressive symptoms, insecurity, and posttraumatic stress disorder, followed by adjustment/behavior problems and aggression, and declining academic performance.33 Considering the potential mediation observed in this study, unexplored mother interpersonal and/or contextual factors within maternal depression and IPV should be explored in determining child socioemotional development.
We also found that maternal mild to severe depressive symptoms were associated with lower child socioemotional development scores adjusted for maternal IPV. These findings are consistent with a study conducted in Pakistan reporting that maternal depressive symptoms during the first years of the child’s life were associated with lower child socioemotional development scores.13 A systematic review examined the association between maternal depression among Latina mothers and found that children whose mothers were experiencing depression had significantly poorer sociodevelopmental outcomes than children whose mothers were not depressed.34 Also, a study with children aged 11 years conducted in Brazil found peer relationship problems and lower levels of prosocial behavior when mothers had persistent depressive symptoms, compared with children whose mothers had low levels of depressive symptoms.35 Maternal depressive symptoms can reduce a mother’s emotional readiness to interact with and respond appropriately to their child’s development.36 Also, maternal depression may interfere with mothers’ abilities to be nurturing and has a negative influence on parenting practices.37 Overall, our findings add to the literature that depressive symptoms are associated with low child socioemotional development scores.
In the study context of rural Tanzania, the majority of mothers had low to moderate engagement of play and learning activities with their young child; however, we did not find an association between stimulation and socioemotional development. Prior research shows a generally positive association between higher levels of early stimulation and improved child development.38,39,40,41 A longitudinal study in the UK, with 30 years of follow-up, found positive associations between child stimulation, mental health, and individual resilience.42 In particular, socioemotional development is related to the interaction between humans, which may have a devastating impact due to lack of stimulation and when mothers are unwilling to provide warm interactions, especially during the depressive periods.43
Finally, an association between harsh discipline and socioemotional development was not found, although most children in the sample received harsh discipline. Prior research has found that when maternal depressive symptoms and IPV coexist, there is an increasing chance of harsh child discipline.44 In Nicaragua, a study reported that maternal experience of IPV was associated with a 17% increase in the risk of harsh child discipline.45 As a result, even though we did not identify an association between harsh discipline and child socioemotional development in this analysis, after adjusting for IPV and maternal depressive symptoms, there is a growing amount of literature on how harsh discipline can affect child development.46,47
Limitations
This study has limitations. First, this study is from the Morogoro region in Tanzania, which may not be generalizable to the broader Tanzanian context or other settings. Second, the PHQ-9 measures depressive symptoms and is not a diagnostic measure for maternal depression. Third, we did not measure psychological and other forms of IPV (eg, verbal, financial, and legal), which probably would change the prevalence of IPV experienced. Fourth, the indicator for child stimulation measured the quantity of stimulating activities the caregiver engaged in with their child but does not capture the quality of that engagement. Also, no information was collected regarding father (or other caregiver stimulation) for which emerging evidence suggests implications for child socioemotional development.6 Fifth, we used only 2 questions to measure harsh discipline. Sixth, we did not account for multiple comparisons for secondary analyses and, as a result, there is a risk of type I errors or falsely finding a significant difference.
Conclusions
The high burden of IPV and depression indicates the need for interventions for mothers, children, and families in rural Tanzania and similar settings to reduce and ameliorate IPV and poor maternal mental health. In addition, growing up in an abusive and toxic environment can greatly affect the psychosocial development of children and subsequently affect their life outcomes. Improving access to screening for IPV, maternal depressive symptoms, and protective childcare may be warranted. Clear protocols to help health clinicians, social workers, and protective sectors (eg, police officers) in how to identify all forms of IPV and make appropriate referrals to protect the caregiver and child are warranted. Globally, protection policies for mothers and children are needed to address the prevention of violence and to provide safety and support for those who have experienced violence.
Data Sharing Statement
References
- 1.World Health Organization . Violence Against Women Prevalence Estimates, 2018. World Health Organization; 2021. [Google Scholar]
- 2.Devries KM, Mak JY, García-Moreno C, et al. Global health: the global prevalence of intimate partner violence against women. Science. 2013;340(6140):1527-1528. doi: 10.1126/science.1240937 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . Global and Regional Estimates of Violence Against Women. World Health Organization; 2013. [Google Scholar]
- 4.Ahmed S, Koenig MA, Stephenson R. Effects of domestic violence on perinatal and early-childhood mortality: evidence from north India. Am J Public Health. 2006;96(8):1423-1428. doi: 10.2105/AJPH.2005.066316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasselmann MH, Reichenheim ME. Parental violence and the occurrence of severe and acute malnutrition in childhood. Paediatr Perinat Epidemiol. 2006;20(4):299-311. doi: 10.1111/j.1365-3016.2006.00735.x [DOI] [PubMed] [Google Scholar]
- 6.Jeong J, Adhia A, Bhatia A, McCoy DC, Yousafzai AK. Intimate partner violence, maternal and paternal parenting, and early child development. Pediatrics. 2020;145(6):e20192955. doi: 10.1542/peds.2019-2955 [DOI] [PubMed] [Google Scholar]
- 7.Neamah HH, Sudfeld C, McCoy DC, et al. Intimate partner violence, depression, and child growth and development. Pediatrics. 2018;142(1):e20173457. doi: 10.1542/peds.2017-3457 [DOI] [PubMed] [Google Scholar]
- 8.Bowen E. The impact of intimate partner violence on preschool children’s peer problems: an analysis of risk and protective factors. Child Abuse Negl. 2015;50:141-150. doi: 10.1016/j.chiabu.2015.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herbell K, Li Y, Bloom T, Sharps P, Bullock LFC. Keeping it together for the kids: new mothers’ descriptions of the impact of intimate partner violence on parenting. Child Abuse Negl. 2020;99:104268. doi: 10.1016/j.chiabu.2019.104268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rogathi JJ, Manongi R, Mushi D, et al. Postpartum depression among women who have experienced intimate partner violence: a prospective cohort study at Moshi, Tanzania. J Affect Disord. 2017;218:238-245. doi: 10.1016/j.jad.2017.04.063 [DOI] [PubMed] [Google Scholar]
- 11.Afifi TO, Mota N, Sareen J, MacMillan HL. The relationships between harsh physical punishment and child maltreatment in childhood and intimate partner violence in adulthood. BMC Public Health. 2017;17(1):493. doi: 10.1186/s12889-017-4359-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.United Nations Children’s Fund . Violence against children in Tanzania: results from a national survey 2009. August 2011. Accessed November 16, 2021. https://evaw-global-database.unwomen.org/-/media/files/un%20women/vaw/full%20text/africa/tanzania%20violence%20against%20children%20survey%202009.pdf?vs=1424
- 13.De Oliveira CVR, Rasheed M, Yousafzai AK. Chronic maternal depressive symptoms are associated with reduced socio-emotional development in children at 2 years of age: analysis of data from an intervention cohort in rural Pakistan. Front Psychiatry. 2019;10:859. doi: 10.3389/fpsyt.2019.00859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howell KH, Graham-Bermann SA, Czyz E, Lilly M. Assessing resilience in preschool children exposed to intimate partner violence. Violence Vict. 2010;25(2):150-164. doi: 10.1891/0886-6708.25.2.150 [DOI] [PubMed] [Google Scholar]
- 15.Gilbert AL, Bauer NS, Carroll AE, Downs SM. Child exposure to parental violence and psychological distress associated with delayed milestones. Pediatrics. 2013;132(6):e1577-e1583. doi: 10.1542/peds.2013-1020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masanja H, Smith ER, Muhihi A, et al. ; Neovita Tanzania Study Group . Effect of neonatal vitamin A supplementation on mortality in infants in Tanzania (Neovita): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;385(9975):1324-1332. doi: 10.1016/S0140-6736(14)61731-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Australian New Zealand Clinical Trials Registry . Efficacy of newborn vitamin A supplementation in improving child survival in Tanzania: generation of evidence necessary for informing global policy. April 14, 2016. Accessed November 16, 2022. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12610000636055
- 18.McCoy DC, Sudfeld CR, Bellinger DC, et al. Development and validation of an early childhood development scale for use in low-resourced settings. Popul Health Metr. 2017;15(1):3. doi: 10.1186/s12963-017-0122-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Waldman M, McCoy DC, Seiden J, et al. Validation of motor, cognitive, language, and socio-emotional subscales using the caregiver reported early development instruments: an application of multidimensional item factor analysis. Int J Behav Dev. 2021;45(4):368-377. doi: 10.1177/01650254211005560 [DOI] [Google Scholar]
- 20.McCoy DC, Waldman M, Team CF, Fink G. Measuring early childhood development at a global scale: evidence from the Caregiver-Reported Early Development Instruments. Early Child Res Q. 2018;45:58-68. doi: 10.1016/j.ecresq.2018.05.002 [DOI] [Google Scholar]
- 21.Tanzania Bureau of Statistics and Macro International . Tanzania demographic and health survey and malaria indicator survey: 2015-16. Accessed June 17, 2020. https://dhsprogram.com/pubs/pdf/FR321/FR321.pdf
- 22.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adewuya AO, Ola BA, Afolabi OO. Validity of the Patient Health Questionnaire (PHQ-9) as a screening tool for depression amongst Nigerian university students. J Affect Disord. 2006;96(1-2):89-93. doi: 10.1016/j.jad.2006.05.021 [DOI] [PubMed] [Google Scholar]
- 24.Tsai AC. Reliability and validity of depression assessment among persons with HIV in sub-Saharan Africa: systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2014;66(5):503-511. doi: 10.1097/QAI.0000000000000210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sweetland AC, Belkin GS, Verdeli H. Measuring depression and anxiety in sub-saharan Africa. Depress Anxiety. 2014;31(3):223-232. doi: 10.1002/da.22142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: development and psychometric data for a national sample of American parents. Child Abuse Negl. 1998;22(4):249-270. doi: 10.1016/S0145-2134(97)00174-9 [DOI] [PubMed] [Google Scholar]
- 27.Hamadani JD, Tofail F, Hilaly A, Huda SN, Engle P, Grantham-McGregor SM. Use of family care indicators and their relationship with child development in Bangladesh. J Health Popul Nutr. 2010;28(1):23-33. doi: 10.3329/jhpn.v28i1.4520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jeong J, Obradovic J, Rasheed M, McCoy DC, Fink G, Yousafzai AK. Maternal and paternal stimulation: mediators of parenting intervention effects on preschoolers’ development. J Appl Dev Psychol. 2019;60:105-118. doi: 10.1016/j.appdev.2018.12.001 [DOI] [Google Scholar]
- 29.Sun J, Liu Y, Chen EE, Rao N, Liu H. Factors related to parents’ engagement in cognitive and socio-emotional caregiving in developing countries: results from Multiple Indicator Cluster Survey 3. Early Child Res Q. 2016;36:21-31. doi: 10.1016/j.ecresq.2015.12.003 [DOI] [Google Scholar]
- 30.UNICEF . The Formative Years: UNICEF’s Work on Measuring Early Childhood Development. UNICEF; 2014. [Google Scholar]
- 31.Rosser-Limiñana A, Suriá-Martínez R, Mateo Pérez MÁ. Children exposed to intimate partner violence: association among battered mothers’ parenting competences and children’s behavior. Int J Environ Res Public Health. 2020;17(4):1134. doi: 10.3390/ijerph17041134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mueller I, Tronick E. Early life exposure to violence: developmental consequences on brain and behavior. Front Behav Neurosci. 2019;13:156. doi: 10.3389/fnbeh.2019.00156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mugoya GCT, Mumba MN, Hooper LM, Witte T, Youngblood M. Depression and intimate partner violence among urban Kenyan caregivers of children with disabilities. J Psychiatr Ment Health Nurs. 2020;27(1):41-53. doi: 10.1111/jpm.12550 [DOI] [PubMed] [Google Scholar]
- 34.Lourenco LM, Baptista MN, Senra LX, Almeida AA, Basilio C, De Castro Bhona FM. Consequences of exposure to domestic violence for children: a systematic review of the literature. Paidéia. 2013;23(55):263-271. doi: 10.1590/1982-43272355201314 [DOI] [Google Scholar]
- 35.Harris RA, Santos HP Jr. Maternal depression in Latinas and child socioemotional development: a systematic review. PLoS One. 2020;15(3):e0230256. doi: 10.1371/journal.pone.0230256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maruyama JM, Pastor-Valero M, Santos IS, Munhoz TN, Barros FC, Matijasevich A. Impact of maternal depression trajectories on offspring socioemotional competences at age 11: 2004 Pelotas Birth Cohort. J Affect Disord. 2019;253:8-17. doi: 10.1016/j.jad.2019.03.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cooper PJ, Tomlinson M, Swartz L, et al. Improving quality of mother-infant relationship and infant attachment in socioeconomically deprived community in South Africa: randomised controlled trial. BMJ. 2009;338:b974. doi: 10.1136/bmj.b974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O’Brien Caughy M, Huang KY, Lima J. Patterns of conflict interaction in mother-toddler dyads: differences between depressed and non-depressed mothers. J Child Fam Stud. 2009;18(1):10-20. doi: 10.1007/s10826-008-9201-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Urke HB, Contreras M, Matanda DJ. The influence of maternal and household resources, and parental psychosocial child stimulation on early childhood development: a cross-sectional study of children 36-59 months in Honduras. Int J Environ Res Public Health. 2018;15(5):926. doi: 10.3390/ijerph15050926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pitchik HO, Fawzi WW, McCoy DC, et al. Prenatal nutrition, stimulation, and exposure to punishment are associated with early child motor, cognitive, language, and socioemotional development in Dar es Salaam, Tanzania. Child Care Health Dev. 2018;44(6):841-849. doi: 10.1111/cch.12605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hartinger SM, Lanata CF, Hattendorf J, et al. Impact of a child stimulation intervention on early child development in rural Peru: a cluster randomised trial using a reciprocal control design. J Epidemiol Community Health. 2017;71(3):217-224. doi: 10.1136/jech-2015-206536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jeong J, McCoy DC, Yousafzai AK, Salhi C, Fink G. Paternal stimulation and early child development in low- and middle-income countries. Pediatrics. 2016;138(4):e20161357. doi: 10.1542/peds.2016-1357 [DOI] [PubMed] [Google Scholar]
- 43.Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment: evidence from a community sample. Child Abuse Negl. 2007;31(3):211-229. doi: 10.1016/j.chiabu.2007.02.004 [DOI] [PubMed] [Google Scholar]
- 44.Murray L, Cooper P, Fearon P. Parenting difficulties and postnatal depression: implications for primary healthcare assessment and intervention. Community Pract. 2014;87(11):34-38. [PubMed] [Google Scholar]
- 45.Silverstein M, Augustyn M, Young R, Zuckerman B. The relationship between maternal depression, in-home violence and use of physical punishment: what is the role of child behaviour? Arch Dis Child. 2009;94(2):138-143. doi: 10.1136/adc.2007.128595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salazar M, Dahlblom K, Solórzano L, Herrera A. Exposure to intimate partner violence reduces the protective effect that women’s high education has on children’s corporal punishment: a population-based study. Glob Health Action. 2014;7:24774. doi: 10.3402/gha.v7.24774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cuartas J. Corporal punishment and early childhood development in 49 low- and middle-income countries. Child Abuse Negl. 2021;120:105205. doi: 10.1016/j.chiabu.2021.105205 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement