Abstract
Melioidosis is an infection caused by Burkholderia pseudomallei. It is a non notifiable disease and is not included in Integrated Disease Surveillance Program by National Center of Disease Control. India is predicted to have highest burden of disease with an estimated mortality of 32,000 per year. Melioidosis presents with a wide range of clinical manifestations like pneumonia, liver and splenic abscess, septicemia etc. This wide spectrum of presentation and mimicry with other infections leads to its misdiagnosis or underdiagnosis. The only source of disease burden in India is few case reports and the true burden and distribution of disease still needs to be assessed. We, hereby, report a case series of four cases aged 28 years, 53 years, 33 years and 22 years. All cases had different clinical presentation ranging from abdominal wall abscess to septicemia and neurological manifestations making the diagnosis challenging. Three of the four cases were discharged after complete recovery while one case went leave against medical advice.
To our knowledge this is the first series describing complete recovery of three out of four cases. This case series will help the physicians to raise their index of clinical suspicion of melioidosis in high risk patients presenting with various findings thus improving the chances of correct diagnosis and treatment.
Keywords: Burkholderia pseudomallei, Melioidosis, Mimicry, Underdiagnosis, Case series
Introduction
Melioidosis, also known as Whitmore disease, was first described by Alfred Whitmore and Krishnaswami in Burma in the year 1912 as a “Glanders – like disease”. The infection is caused by Burkholderia pseudomallei which is an aerobic, non- spore forming, nonfermenting, facultative intracellular motile gram-negative bacillus and resides in soil, surface and ground water [1], [2], [3], [4]. Melioidosis occurs predominantly in Southeast Asia, northern Australia, South Asia, and China [2], [5]. Most of the cases in India have been reported from the southern states like Kerala, Karnataka and Tamil Nadu with isolated cases being reported from eastern and northeastern parts of India [6], [7], [8].
Melioidosis has high fatality rate of 19–36 % in endemic areas [9] and the global mortality rates vary between 9 % and 70 % [10]. The infection is seen in both human and animals. It is classified as category B bioterrorism agent and is designated a tier 1 select agent by the U.S. Centers for Disease Control and Prevention (CDC) [1], [11].
Melioidosis has a wide range of clinical presentation, the infection may be acute or chronic, localized or disseminated [1]. The disease mimics other infections like tuberculosis making the clinical diagnosis very challenging. Hence a strong clinical suspicion is required to make the correct diagnosis. The most important risk factors for melioidosis are diabetes, chronic alcohol use, chronic kidney disease, and chronic lung disease [2], [12]. The incidence is more in the rainy season as the predominant mode of transmission is percutaneous inoculation during exposure to wet season soils or contaminated water.
We hereby report four cases of melioidosis who were successfully managed despite the various challenges faced during their management.
Case#1
A 28 year old male with no known co morbidities was admitted to our center with chief complaints of high grade fever and pain in abdomen for 20 days and cough with expectoration for 15 days. He was being treated in a local hospital for the above complaints where diagnosis of type 1 respiratory failure with liver abscess was made. He was, however, later referred to our center when his clinical condition didn’t improve after five days of admission.
On admission, the patient was conscious and oriented with heart rate of 121/min, BP-131/92 mmHg, RR-32/min and SpO2 91% on NRMB with O2 flow of 12 L/min.
His ABG showed pH of 7.47, pCO2 28 mmHg, pO2 71 mmHg and HCO3- 20 mmol/L. His initial laboratory findings are shown in Table 1. Blood sugar was 180 mg/dl and urine R/M showed 2 + ketone bodies, 1 + protein, 2 + glucose and pus cells 31 WBC/HPF.
Table 1.
Baseline investigations of all the cases.
| Laboratory parameters | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Hb (gm/dL) | 11.7 | 11.6 | 12.8 (28/9/21) | 14.2 |
| TLC (*109/L) | 10.86 | 9.52 | 4.31 | 11.67 |
| Platelets (*109/L) | 165 | 290 | 109 | 278 |
| Urea (mg/dL) | 39 | 33 | 38 | 14 |
| Creatinine (mg/dL) | 0.7 | 0.4 | 1.2 | 0.8 |
| PT/INR | 11.7/1.15 | 12.8/1.24 | 11.3/1.09 | 13.2/1.16 |
| S. bilirubin (mg/dl) | 1.4 | 0.6 | 0.2 | 0.9 |
| SGOT (U/L) | 42 | 20 | 20 | 24 |
| SGPT (U/L) | 41 | 26 | 12 | 26 |
| Albumin (g/dL) | 2.5 | 2.8 | 3.4 | 4.2 |
| B. Sugar (mg/dL) | 192 | 197 | 312 | 146 |
| Procalcitonin (ng/ml) | 0.88 | 10.6 (day 3) | 3.2 | 0.05 |
| HbA1c | 12 | 10 | 13.3 | 6.0 |
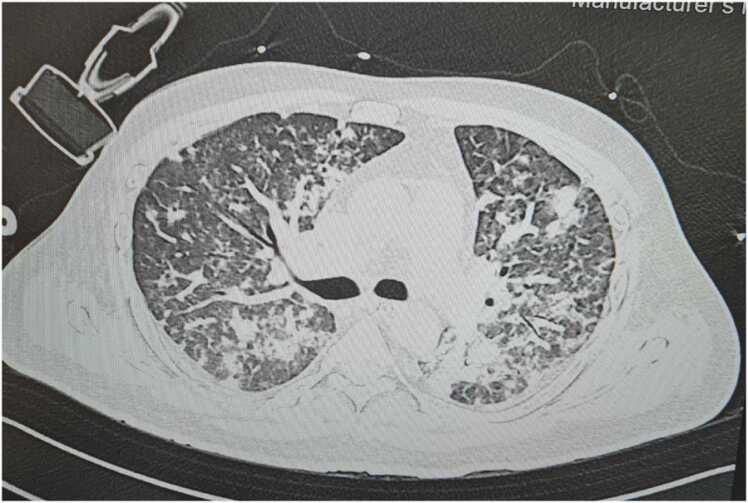
On arrival to ICU he was started he was started on NIV support in view of respiratory distress and low saturation with settings of FiO2 0.8, PEEP 8 cm H2O and PS above PEEP 12 cm H2O. Urgent USG abdomen showed hepatomegaly with right lobe live liver abscess and splenic abscess. Provisional diagnosis of sepsis with MODS (? Melioidosis) with diabetic ketoacidosis was made. Blood, urine, sputum cultures were sent before starting the antibiotics. The patient was started on meropenem, metronidazole, teicoplanin, doxycycline, low molecular weight heparin (LMWH) and i.v. insulin infusion. Further investigations showed areas of consolidation and diffuse ground glass opacities in bilateral lung fields in HRCT chest (Fig. 1). CECT abdomen revealed multiple liver abscess in right lobe of liver, multiple splenic abscesses with hepatosplenomegaly (Fig. 2). Diagnostic tap of liver abscess was sent to confirm the diagnosis and ensure long term compliance of the patient with the oral antibiotics to be given for the eradication regime of Burkholderia pseudomallei.
Fig. 1.
HRCT chest of case 1- Consolidation and ground glass opacities in bilateral lung fields.
Fig. 2.
CECT abdomen of case 1- Multiple liver abscess in right lobe of liver, multiple splenic abscess.
After 24 h, the clinical condition of the patient improved and he was shifted on HFNC with O2 flow 40 L/min, FiO2 0.3 and was maintaining SpO2 95%.
However, on day 3 his TLC count increased to 14.81 * 109/L and procalcitonin decreased to 0.18 ng/ml. His urine and sputum culture showed growth of Candida albicans, blood showed growth of Staphylococcus hominis and liver abscess had Burkholderia pseudomallei. Patient was immediately started on fluconazole in addition to the ongoing treatment. References were sought from the concerned departments (endocrinology, gastromedicine, gastrosurgery, intervention radiology) and their advices were incorporated.
The patient’s clinical condition continued to improve, oxygen support was continuously decreasing and was finally taken on nasal prongs after 7 days. He was shifted to HDU after 8 days of ICU stay and was further shifted to ward when he was off oxygen support. He was given intravenous (i.v.) meropenem for 4 weeks and was discharged in stable clinical condition after completion of the course of i.v. antibiotics. He was discharged with advice of the eradication regime of Burkholderia pseudomallei of oral co-trimoxazole for 3 months.
Case # 2
A 33 year old, recently diagnosed diabetic male was admitted to our center with chief complaints of abdominal wall abscess located in left hypochondriac region since 1 month, high grade fever for 15 days and bilateral knee pain for 15 days along with loss of appetite and weight loss. He was chronic alcoholic for 18 years. The patient was undergoing treatment for the above complaints in some other hospital but was referred to our center after 12 days when his clinical condition didn’t improve despite the ongoing treatment.
On admission, he was conscious, oriented, with heart rate of 78/min, BP – 130/88 mmHg, RR – 28/min and SpO2 99 % on room air and was therefore admitted to ward. His initial laboratory findings are shown in Table 1.
CECT abdomen was done which revealed multiple ill-defined hypotenuse lesion with peripheral and septal enhancement in right lobe of liver (largest 15 * 12 mm)? Abscess ? granuloma, splenic infarct at inferior pole and bilateral renal stone. Pus from base of ulcer was sent for culture and sensitivity and patient started on meropenem and metronidazole.
However, on day 3 patient’s condition deteriorated. SpO2 dropped to 88 % and the sensorium was altered. He was immediately shifted to intensive care unit and was started on oxygen support via HFNC (FiO2–0.35, O2 flow-40 L/min.). ABG showed hypoxemic respiratory failure with pH of 7.498, pCO2 23.9 mmHg, pO2-58 mmHg HCO3-18.1 mmol/L.
HRCT chest was done which showed multiple tiny conglomerated nodules in B/l upper and middle lobes, B/L lower lobe consolidation, multiple subcentimetric, prevascular, pre and para tracheal and pre-carinal lymph nodes (Fig. 3). Repeat laboratory test was sent along with blood and urine culture and sensitivity. Bilateral knee joints were tense n tender, pus aspiration done and sent for culture and sensitivity.
Fig. 3.
HRCT Chest of case 2- Bilateral lower lobe consolidation.
Provisional diagnosis of melioidosis with MODS was made and patient upgraded to ceftazidime + avibactam, linezolid, doxycycline, trimethoprim and sulfamethoxazole.
Pus c/s from ulcer base, blood c/s and knee aspiration fluid showed growth of Burkholderia pseudomallei.
Patient’s clinical condition was progressively improving, however, on day 8 he developed hypoxemic respiratory failure and was intubated in view of the same. Due to financial concern attendants took the patient leave against medical advice (LAMA) on day 10.
Case # 3
A 53 year male, known case of diabetes mellitus and hypertension, chronic alcoholic and smoker, presented in gastroenterology OPD with chief complaints of on and off low grade fever since 2 months associated with low appetite and weight loss. Before presenting to our center, the patient was undergoing treatment elsewhere for the above complaints where he was diagnosed to have multiple liver abscess. He came to our set up when his clinical condition didn’t improve despite the ongoing treatment.
HRCT Thorax and CECT abdomen was performed which showed right lower lobe consolidation, multiple hypodense lesion in liver and spleen. FNAC from liver lesion showed acute inflammation suggestive of abscess. Patient was started on oral antibiotics on OPD basis, but subsequently patient lost the follow up.
He came back again to our center after 3 months. The patient was undergoing treatment at some other center where he was started on ATT. A repeat USG abdomen performed which showed increased in size and number of abscess both in liver and spleen. Initial lab investigations are shown in Table 1. The case was discussed with the Critical care Medicine (CCM) team on OPD basis, a strong suspicion of melioidosis was made and USG guided pus aspiration was done which was sent for culture sensitivity, tuberculosis and immuno-histochemistry.
The microbiological reports showed the growth of Burkholderia pseudomallei (Fig. 4) and was treated with inj. Ceftazidime for intensive phase. After the intensive phase, patient was started on eradication phase therapy (Tab Co-trimoxazole).
Fig. 4.
Pus culture and sensitivity report of case 3 shows the growth of Burkholderia pseudomallei.
Case # 4
A 22 year old male, known case of hypothyroidism and bipolar disorder, alcoholic and smoker, known case of attention deficit hyperactive disorder, was admitted in our center with chief complaint of right sided weakness for 4 days, 2 episodes of seizure, vomiting and fever for 3 days. Initial labs are mentioned in table1.
On admission patient was afebrile, conscious and oriented with HR 76/min, BP 116/80 mmHg, SpO2 100 % on room air, RBS 146 mg/dl. On examination, the power in right upper limb was 4/5 and right lower limb was 1/5, pain and touch sensation decreased on right side, right side planter was equivocal, findings on the other side were within normal range.
NCCT brain was done which was suggestive of left parietal inflammatory granuloma. MRI brain showed left high frontal and parietal granulomatous etiology (? atypical tuberculosis, ? neurosarcoidosis, ? malignancy). CSF analysis was inconclusive.
The patient’s family didn’t give consent for intracranial biopsy and hence he was empirically started on ATT, meropenem and teicoplanin.
The patient was intubated on day 10 in view of fall in oxygen saturation and worsening sensorium. Repeat MRI brain was done which showed new onset involvement of brainstem and left cerebral hemisphere with increase in mass effect (Fig. 5). The family was recounselled and biopsy was taken after proper consent. Brain abscess and endotracheal tube culture showed the growth of Burkholderia pseudomallei.
Fig. 5.
MRI brain of case 4- Left high frontal and parietal lobe granulomatous etiology.
The patient was then started on ceftazidime and cotrimoxazole. His clinical condition started to improve after 24 h and was extubated after three days. The patient was finally discharged in stable clinical condition after 28 days of hospital admission.
Discussion
Melioidosis presents with wide spectrum of clinical manifestations ranging from isolated cutaneous lesion to systemic manifestations, fulminant sepsis and death. Disseminated infection can present with pneumonia, abscesses in liver, spleen, kidney, prostate, skin and subcutaneous tissue, septic arthritis, osteomyelitis, meningoencephalitis and subdural empyema. Our all the four cases presented with different manifestations of the disease. While case 1 presented with sepsis and multiorgan dysfunction, case 2 presented with abdominal wall abscess, knee joint pain and loss of weight and appetite. Case 3 had vague complains of off and on low grade fever with loss of appetite and weight loss. Case 4 presented with neurological complications. This wide range of presentation is one of the reasons of underdiagnosis/misdiagnosis of melioidosis. Barman et al. [13] reported a case where melioidosis remained undiagnosed for two months. Clinical diagnosis, therefore, is very challenging, particularly when the disease can mimic other infections especially tuberculosis [14], which is highly endemic in resource limited country like India. It also mimics pyogenic abscess and other tropical illness with fatal septicemia and multi-organ dysfunction syndrome. Our case 3 rightly depicts this situation. He was initially treated on the line of pyogenic abscess followed by tuberculosis treatment and had to suffer for quite long duration because of misdiagnosis. Perera et al. [15] reported a case of 62 year old male where the causative agent was initially misidentified as Pseudomonas. However, when the patient’s condition continued to deteriorate, repeat culture showed the growth of Burkholderia pseudomallei. The patient finally succumbed to the disease despite optimal antibiotic coverage.
Our case 1, 2 and 4 were reported during the rainy season in North India. Our all four cases had risk factors for melioidosis. Case 1 was diagnosed diabetes mellitus at our center, case 2 was diabetic and chronic alcoholic, case 3 was also diabetic and alcoholic and case 4 was alcoholic, hypothyroidic and smoker. Vidyalakshmi et al. [16] found 76 % correlation of diabetes with melioidosis. Diabetes mellitus has been found to be a major risk factor and therefore, the increasing cases of diabetes has been postulated as a probable cause for the increasing prevalence of melioidosis [3].
To our knowledge, this is the first case series of four cases where three out of four cases had 100 % recovery and one case went leave against medical advice with improving clinical and laboratory parameters. Previously, a case series of two cases was reported by Alhatmi et al. [17] where one patient survived while the other one couldn’t be saved despite maximum ICU support and antibiotic treatment. Similarly, Deshmukh et al. [18] reported as case of 43 year male where the patient succumbed to melioidosis as he could not be started on appropriate antibiotics due to delay in diagnosis. A similar case was reported by Miralles et al. [19] where a 10 year old male child could not come out of septicemia due to delayed diagnosis.
Therefore, with such high mortality and variable antibiotic sensitivity pattern, a strong clinical suspicion is required to help in making a diagnosis especially due to its non specific presentation and mimicry with other diseases. This is particularly important in patients with predisposing risk factors like diabetes mellitus, chronic alcohol use, chronic kidney disease, chronic lung disease, immunosuppressed and history of travel to endemic regions. Any young patient with or without risk factors if present with multi-system disease or abscess should be evaluated for possibilities of melioidosis and microbiological confirmation of the diagnosis is necessary even if patient responds to the initial antimicrobial therapy, as this is the only way to provide them such a long course of antibiotics with potential side effects.
Conclusion
The case series emphasizes on the need to create awareness among the physician with high index of suspicion for the clinical diagnosis. To control this emerging disease, we need to improve the awareness among clinicians through training programs, workshop and conferences along-with establishing good microbiological testing laboratories with the hope of early detection, timely management and improved outcome.
CRediT authorship contribution statement
Dilip Kumar Dubey: Conceptualization, Investigation, Supervision, Writing – review & editing. Noor Bano: Conceptualization, Writing – original draft. Madhulika Dubey: Conceptualization, Writing – original draft, Writing – review & editing. Pushpender Sangwan: Investigation, Writing – original draft. Sandeep Kumar Mitra: Supervision, Writing – review & editing. Vidushi Kulshrestha: Writing – original draft. Bhawna Jain: Investigation. Imran Mehdi: Writing – original draft, Writing – review & editing.
Sources of funding
None.
Ethical approval
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Declaration of Interest
None.
Footnotes
Institution where the study was performed: Institute of Critical Care and Pulmonary medicine, Medanta Hospital, Lucknow, Uttar Pradesh, India.
Contributor Information
Dilip Kumar Dubey, Email: drdilipdubey2d@gmail.com.
Noor Bano, Email: drnoorbano7@gmail.com.
Madhulika Dubey, Email: madhulika16sep@gmail.com.
Pushpender Sangwan, Email: drsangwan25@gmail.com.
Sandeep Kumar Mitra, Email: sandeepmitra.mitra59@gmail.com.
Vidushi Kulshrestha, Email: wittyvidushi@gmail.com.
Bhawna Jain, Email: bhawna.jain@medanta.org.
Imran Mehdi, Email: drimranmehdi@gmail.com.
References
- 1.White N.J. Melioidosis. Lancet. 2003;361:1715–1722. doi: 10.1016/s0140-6736(03)13374-0. [DOI] [PubMed] [Google Scholar]
- 2.Cheng A.C., Currie B.J. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005;18:383–416. doi: 10.1128/CMR.18.2.383-416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wiersinga W.J., Virk H.S., Torres A.G., Currie B.J., Peacock S.J., Dance D.A.B., et al. Melioidosis. Nat Rev Dis Prim. 2018;4:17107. doi: 10.1038/nrdp.2017.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Willcocks S.J., Denman C.C., Atkins H.S., Wren B.W. Intracellular replication of the well-armed pathogen Burkholderia pseudomallei. Curr Opin Microbiol. 2016;29:94–103. doi: 10.1016/j.mib.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Currie B.J., Dance D.A., Cheng A.C. The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg. 2008;102 Suppl. 1:S1. doi: 10.1016/S0035-9203(08)70002-6. [DOI] [PubMed] [Google Scholar]
- 6.Anuradha K., Meena A.K., Lakshmi V. Isolation of Burkholderia pseudomallei from a case of septicaemia: a case report. Indian J Med Microbiol. 2003;21:129–132. [PubMed] [Google Scholar]
- 7.Jesudason M.V., Anbarasu A., John T.J. Septicaemic melioidosis in a tertiary care hospital in south India. Indian J Med Res. 2003;117:119–121. [PubMed] [Google Scholar]
- 8.Viswaroop B.S., Balaji V., Mathai E., Kekre N.S. Melioidosis presenting as genitourinary infection in two men with diabetes. J Post Med. 2007;53:108–110. doi: 10.4103/0022-3859.32210. [DOI] [PubMed] [Google Scholar]
- 9.Churuangsuk C., Chusri S., Hortiwakul T., Charernmak B., Silpapojakul K. Characteristics, clinical outcomes and factors influencing mortality of patients with melioidosis in southern Thailand: a 10-year retrospective study. Asian Pac J Trop Med. 2016;9:256–260. doi: 10.1016/j.apjtm.2016.01.034. [DOI] [PubMed] [Google Scholar]
- 10.Gassiep I., Armstrong M., Norton R. Human melioidosis. Clin Microbiol Rev. 2020;33:e00006–e00019. doi: 10.1128/CMR.00006-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peacock S.J., Schweizer H.P., Dance D.A., Smith T.L., Gee J.E., Wutheikanun V., et al. Management of accidental laboratory exposure to Burkholderia pseudomallei and B. mallei. Emerg Infect Dis. 2008;14(7) doi: 10.3201/eid1407.071501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Currie B.J. Melioidosis: an important cause of pneumonia in residents of and travelers returned from endemic regions. Eur Respir J. 2003;22:542–550. doi: 10.1183/09031936.03.00006203. [DOI] [PubMed] [Google Scholar]
- 13.Barman P., Sidhwa H., Shirkhande P.A. Melioidosis: a case report. J Glob Infect Dis. 2011;3:183–186. doi: 10.4103/0974-777X.81697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vidyalakshmi K., Chakrapani M., Shrikala B., Damodar S., Lipika S., Vishal S. Tuberculosis mimicked by melioidosis. Int J Tuberc Lung Dis. 2008;12:1209–1215. [PubMed] [Google Scholar]
- 15.Perera G.N.D., Dias L.D., Kulatunga A., Corea E., Masakorala A case report of melioidosis. Sri Lankan J Infect Dis. 2012;2(1):47–51. doi: 10.4038/sljid.v2i1.3795. [DOI] [Google Scholar]
- 16.Vidyalakshmi K., Shrikala B., Bharathi B., Suchitra U. Melioidosis: an underdiagnosed entity in western coastal India: a clinico-microbiological analysis. Indian J Med Microbiol. 2007;25:245–248. doi: 10.4103/0255-0857.34767. [DOI] [PubMed] [Google Scholar]
- 17.Alhatmi H., Alharbi A., Bosaeed M., Aldosary O., Aljohani S., Alalwan B., et al. Melioidosis: case reports of confirmed Burkholderia pseudomallei in Saudi Arabia. J Infect Public Health. 2020;13(5):824–826. doi: 10.1016/j.jiph.2020.01.310. [Epub 2020 Mar 7] [DOI] [PubMed] [Google Scholar]
- 18.Deshmukh M., Mundhada S. Chronic suppurative joint effusion due to Burkholderia pseudomallei: a case report. Indian J Pathol Microbiol. 2013;56:460–463. doi: 10.4103/0377-4929.125373. [DOI] [PubMed] [Google Scholar]
- 19.Miralles I.S., Maciel M.C.A., Angelo M.R.F., Gondini M.M., Frota L.H.F., Reis C.M.F., et al. Burkholderia pseudomallei: a case report on a human infection in Ceará, Brazil. Rev Inst Med Trop S Paulo. 2004;46(1):51–54. doi: 10.1590/s0036-46652004000100011. [DOI] [PubMed] [Google Scholar]