Abstract
OBJECTIVE
To investigate the causal role of choline metabolites mediating sodium–glucose cotransporter 2 (SGLT2) inhibition in coronary artery disease (CAD) and type 2 diabetes (T2D) using Mendelian randomization (MR).
RESEARCH DESIGN AND METHODS
A two-sample two-step MR was used to determine 1) causal effects of SGLT2 inhibition on CAD and T2D; 2) causal effects of three choline metabolites, total choline, phosphatidylcholine, and glycine, on CAD and T2D; and 3) mediation effects of these metabolites. Genetic proxies for SGLT2 inhibition were identified as variants in the SLC5A2 gene that were associated with both levels of gene expression and hemoglobin A1c. Summary statistics for metabolites were from UK Biobank, CAD from CARDIoGRAMplusC4D (Coronary ARtery DIsease Genome wide Replication and Meta-analysis [CARDIoGRAM] plus The Coronary Artery Disease [C4D] Genetics) consortium, and T2D from DIAbetes Genetics Replication And Meta-analysis (DIAGRAM) and the FinnGen study.
RESULTS
SGLT2 inhibition (per 1 SD, 6.75 mmol/mol [1.09%] lowering of HbA1c) was associated with lower risk of T2D and CAD (odds ratio [OR] 0.25 [95% CI 0.12, 0.54], and 0.51 [0.28, 0.94], respectively) and positively with total choline (β 0.39 [95% CI 0.06, 0.72]), phosphatidylcholine (0.40 [0.13, 0.67]), and glycine (0.34 [0.05, 0.63]). Total choline (OR 0.78 [95% CI 0.68, 0.89]) and phosphatidylcholine (OR 0.81 [0.72, 0.91]) were associated with T2D but not with CAD, while glycine was associated with CAD (0.94 [0.91, 0.98]) but not with T2D. Mediation analysis showed evidence of indirect effect of SGLT2 inhibition on T2D through total choline (0.91 [0.83, 0.99]) and phosphatidylcholine (0.93 [0.87, 0.99]) with a mediated proportion of 8% and 5% of the total effect, respectively, and on CAD through glycine (0.98 [0.96, 1.00]) with a mediated proportion of 2%. The results were well validated in at least one independent data set.
CONCLUSIONS
Our study identified the causal roles of SGLT2 inhibition in choline metabolites. SGLT2 inhibition may influence T2D and CAD through different choline metabolites.
Introduction
Sodium–glucose cotransporter 2 (SGLT2) inhibitors, including canagliflozin, dapagliflozin, and empagliflozin, are widely approved antihyperglycemic agents to lower blood glucose and cardiovascular risk in patients with diabetes (1). Large clinical trials have provided compelling evidence to support their beneficial effects on major adverse cardiovascular events, hospitalization for heart failure (2–6), and renal outcomes (7,8). SGLT2 inhibitors have been demonstrated to have metabolic effects, though the underlying mechanism is unclear (9–11). In a prospective study, a wide range of metabolites changes was identified in the empagliflozin-treated patients with type 2 diabetes (T2D) and cardiovascular disease (CVD) through use of untargeted metabolomics (10). However, it did not yield definitive mechanisms or inference of causal effect of SGLT2 inhibition on the circulating metabolites because of the observational nature of the study (10). In the male Zucker diabetic fatty rats after treatment with empagliflozin for 6 weeks, the hepatic lipidome was changed toward a protective profile, through an increase of phosphatidylcholines and related metabolites (11).
Choline, an essential nutrient that plays a vital role in human metabolism and health, is involved in the synthesis of phospholipids, betaine, and acetylcholine (12). Elevated levels of choline metabolites generated from the metabolism of dietary choline and phosphatidylcholine (mostly originated from red meat, eggs, and fish) by gut microbiome were found to be associated with increased risk of CVD (13–16) and T2D (17). In a recent case-cohort study investigators reported that plasma concentrations of choline pathway metabolites (choline, phosphocholine, and a-glycerophosphocholine) and a metabolite score combining choline pathway metabolites were associated with risk of major cardiovascular events during ∼5 years of follow-up (18). However, the causal effects of the choline metabolites on T2D and CVD events are unclear, and whether the SGLT2 inhibition acts on the choline metabolism pathway remains unknown.
Mendelian randomization (MR) is an approach that uses genetic variants that are robustly associated with exposure as potentially unconfounded instruments to infer a causal relation between exposure and outcome. New methods such as genetic colocalization and genetic variants that are associated with drug target mRNA expression (expression quantitative trait loci [eQTLs]) can be used to create MR instruments for drug exposure (19). This strategy can be introduced for investigation of the biological mechanisms involved in the effects of SGLT2 inhibition on diabetes and CVD.
Given the underexplored metabolic mechanism of SGLT2 inhibition in protection against CVD and T2D, and the important role of choline metabolism pathway in pathogenies of these cardiometabolic diseases, we hypothesized that the effect of SGLT2 inhibition on cardiovascular events or diabetes might be mediated through the choline metabolic pathway. We performed a two-sample, two-step MR study to investigate the causal role of choline metabolites in linking the effect of SGLT2 inhibition with coronary artery disease (CAD) and T2D (Fig. 1). We identified a causal effect of SGLT2 inhibition on choline metabolites, which would guide the mechanism exploration of SGLT2 inhibition in reducing cardiometabolic disease risk.
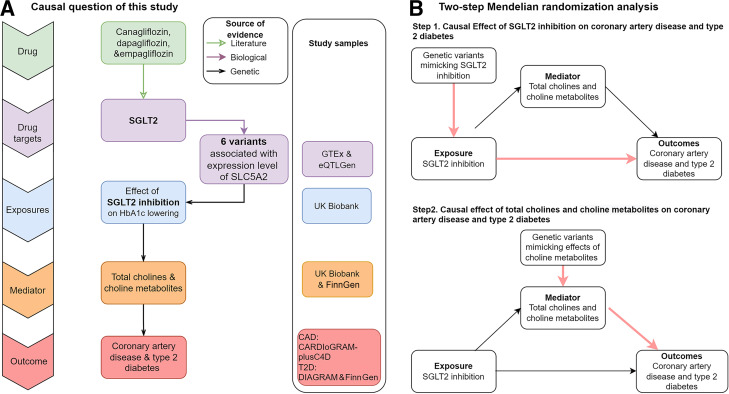
Figure 1.
Study design. A: The study question is whether there is a causal role of choline metabolites (mediators) in mediating the effect of SGLT2 inhibition (exposures) on CAD and T2D (outcomes). The green modules and arrow show the selected drugs and their targets, which come from the literature evidence. The purple modules and arrow show the process of looking up genetic variants associated with the expression level of SLC5A2 gene (using data from GTEx and eQTLGen Consortium), the functional gene of SGLT2 inhibitors, which means a biological link. The blue modules and black arrows indicate the MR estimates of effects of the variants on HbA1c level using data from the UK Biobank. The orange modules indicate the selected metabolites from the UK Biobank, and data are from the population-based GWAS. The red modules represent selected cardiometabolic outcomes, T2D, and CAD. B: Diagram of the two steps of MR models: step 1, to establish the causal effect of SGLT2 inhibition on CAD and T2D, and step 2, to establish the causal effect of the choline metabolites on CAD and T2D.
Research Design and Methods
Study Design
Figure 1A illustrates the diagram of the study design. 1) Selection of genetic variants that were proxies of the effect of SGLT2 inhibition. 2) Selection of three metabolites on the choline metabolism pathways as potential mediators. 3) Selection of two cardiometabolic outcomes: CAD and T2D. 4) Two-step MR analysis estimating the causal effects of SGLT2 inhibition and choline metabolites on the two cardiometabolic diseases, respectively, and estimation of the mediation effect of choline metabolites linking SGLT2 inhibition with the two disease outcomes. And 5) integration of causal evidence with biological pathway information.
Selection and Validation for Genetic Predictors of SGLT2 Inhibition
The selection of genetic variants that were proxies of SGLT2 inhibition involved four steps (Fig. 1A). 1) Select genetic variants associated with mRNA expression level of SLC5A2 gene using data from Genotype-Tissue Expression (GTEx) (20) and eQTLGen Consortium (21) and the potential functional gene of SGLT2 inhibitors (Supplementary Table 1). 2) Estimate the association of each SLC5A2 variant with HbA1c level (an indicator of glucose-lowering effect via SGLT2 inhibition) and select variants that show regional-wide association with HbA1c using data from a subgroup of unrelated individuals of European ancestry without diabetes in the UK Biobank (n = 344,182) (association P value = 1 × 10−4) (Supplementary Table 1) (22). 3) Validate whether SLC5A2 and HbA1c share the same causal variant using the genetic colocalization approach. Colocalization is a bivariable genetic approach with application of a Bayesian model to estimate the posterior probability that the two traits, expression of SLC5A2 and circulating HbA1c level, share the same causal variant in the SLC5A2 region (19). Colocalization probability >70% between SLC5A2 expression and HbA1c was used as evidence of colocalization and noted as “colocalized.” The rest of the gene-disease associations were noted as “not colocalized” (Supplementary Table 1). And 4) after selection and validation, conduct a standard clumping process (using correlation among variants <0.8 as threshold to remove variants with very high correlation). To quantify the statistical power of the genetic variants, we estimated the strength of the genetic predictors of each tested exposure using F statistics. After selection and multiple validation steps, six genetic variants robustly associated with SGLT2 inhibition via HbA1c were selected as genetic predictors for the MR analysis (Supplementary Table 2).
Selection of Choline Metabolites
We systematically searched 249 metabolites from UK Biobank, and 3 choline metabolites were available including total choline, phosphatidylcholine, and glycine (n = 114,999). The full genome-wide association studies (GWAS) summary statistics of the three choline metabolites were made publicly available via the IEU OpenGWAS database with GWAS identifier met-d-Cholines, met-d-Phosphatidylc, and met-d-Gly (22). The genetic variants that showed strong associations with the above three metabolites (P < 5 × 10−8) were selected as candidate genetic predictors of these metabolites. A clumping was further conducted to remove genetic variants with correlation to each other (correlation among variants <0.001). After selection and validation, 64 variants associated with total choline, 61 associated with phosphatidylcholine, and 49 associated with glycine were selected as genetic predictors of the three choline metabolites, respectively (Supplementary Table 3). We searched other key choline metabolites including betaine and acetylcholine. There is only one GWAS of circulating betaine in 3,829 individuals (23), where four genetic variants were reported. No GWAS data for circulating acetylcholine are available to date. On considering the data availability and the statistical power, we therefore did not include betaine or acetylcholine in this study.
Study Outcomes
Due to the outstanding beneficial effects of SGLT2 inhibition on cardiometabolic diseases, we focused our study on the two major outcomes, CAD and T2D. The summary data of the genetic association for T2D were obtained from the DIAbetes Genetics Replication And Meta-analysis (DIAGRAM) consortium (74,124 cases) (24) and the FinnGen study (37,031 cases) as a validation data set. The genetic association for CAD was extracted from a meta-GWAS of CARDIoGRAMplusC4D (Coronary ARtery DIsease Genome wide Replication and Meta-analysis [CARDIoGRAM] plus The Coronary Artery Disease [C4D] Genetics) and UK Biobank with 71,602 CAD cases (25) and an independent data set with 60,801 CAD cases in CARDIoGRAMplusC4D as a validation (26) (Supplementary Table 4).
Statistical Analyses
Heritability and Genetic Correlation Analysis of Choline Metabolites
To estimate the heritability of the three choline metabolites, we used single-trait linkage disequilibrium (LD) score regression (27). LD scores were calculated for all high-quality genetic variants (i.e., INFO score > 0.9 and minor allele frequency > 0.1%) from the metabolites GWASs. We further quantified the overall variant-based heritability with LD score regression using a subset of 1.2 million HapMap genetic variants (with variants in major histocompatibility complex region been removed due to complex correlation structure among genetic variants; Supplementary Table 5).
To further understand the correlation between the choline metabolites, we conducted a pairwise genetic correlation analysis of the three choline metabolites using bivariate LD score regression. The LD score regression method uses summary statistics from the GWAS of total choline, phosphatidylcholine, and glycine; calculates the cross product of test statistics at each variant; and then regresses the cross product on the LD score (which is a measure of how much variation each variant tags). In total, three pairs of genetic correlations were estimated.
MR Analysis of SGLT2 Inhibition and CAD and T2D Risk
First, we estimated the effect of SGLT2 inhibition on CAD and T2D risk (Fig. 1B). A generalized inverse variance–weighted (IVW) approach was applied to boost the power of this analysis, where the method includes consideration of the correlation between the six genetic predictors of SGLT2 inhibition (therefore we were able to use a relaxed clumping threshold of 0.8). Specifically, we got an LD matrix of correlation values for each pair of variants present in the 1000 Genomes data set. Then, we used IVW and MR-Egger method to estimate the MR effect considering the LD matrix of six variants. This method used partially correlated variants based on principal components analysis of a weighted version of the genetic correlation matrix, which would improve numerical efficiency and stability, since the extra variants explained additional variation in the exposure (28).
Mediation MR Analysis Linking SGLT2 Inhibition With CAD and T2D via Choline Metabolites
We assessed the causal effect of metabolites on CAD and T2D (Fig. 1B). The 64 variants associated with total choline, 61 with phosphatidylcholine, and 49 with glycine were used as genetic predictors for the three exposures, and CAD and T2D were selected as the outcomes.
We estimated the effect of SGLT2 on three choline metabolites. The six genetic variants mimicking SGLT2 inhibition were used as the exposure, and the three choline metabolites were used as outcomes.
We performed multivariable MR as another method to determine the mediation effect of the metabolites on SGLT2 inhibition and T2D and CAD (29,30). We used IVW as our main approach to estimate the effect of SGLT2 inhibition on the metabolites (β1) and multivariable MR to estimate the effect of each metabolite on risk of T2D and CAD adjusting for the genetic effect of SGLT2 inhibition (β2). To calculate the indirect mediation effect of SGLT2 inhibition on diseases outcomes, we used the product of coefficients method as our main method, i.e., the casual effect of SGLT2 inhibition on outcomes via metabolites (β1 × β2). The direct effect was the estimate of SGLT2 inhibition on outcomes with adjustment for each mediator individually (β3) and total effect was the sum of direct and indirect effect (β3 + β1 × β2). Thus, the proportion of the total effect mediated by each metabolite separately was estimated by dividing the indirect effect by the total effect [β1 × β2/(β3 + β1 × β2)].
Validation and Sensitivity Analysis
We obtained independent data sets for independent validation. The data source was listed in Supplementary Table 4. To control for heterogeneity, we applied the Mendelian Randomization Pleiotropy RESidual Sum and Outlier (MR-PRESSO) method. To test the underlying MR assumptions, e.g., assessing influence of directional pleiotropy, we applied the generalized MR-Egger regression method. The pleiotropy test using MR-Egger intercept term and heterogeneity test (Cochran Q statistic for IVW and the global test for MR-PRESSO) across predictors were both applied to quantify the level of pleiotropy of the MR analysis. The Bonferroni-correlated threshold of 0.025 (0.05/2) was used as the threshold to control for multiple testing.
Due to the strong genetic correlation between total choline and phosphatidylcholine, we applied the PhenoSpD approach (31) to estimate the complete and independent tests that had been conducted for the two-step MR analysis and used it as the multiple testing correction threshold.
All MR analyses were conducted with the MendelianRandomization R package (32) and TwoSampleMR R package (github.com/MRCIEU/TwoSampleMR). We plotted results as forest plots using code derived from the ggplot2 package in R.
Integration of Genetic and Biological Pathway Evidence
We further integrated the genetic evidence generated in this study with protein-protein interaction (PPI) information from the STRING database for better understanding of the causal mechanisms linking SGLT2 inhibition with the two cardiometabolic diseases (33). To build up a comprehensive PPI network, we selected proteins/genes from three resources: 1) the drug target SGLT2-related gene SLC5A2, 2) 82 genes/proteins near the 174 genetic variants associated with the three choline metabolites (Supplementary Table 3), and 3) five enzymes in choline-glycine and four enzymes in choline-phosphatidylcholine biosynthesis pathway. The PPI network was built with stringApp in Cytoscape with following parameters: data source = protein query, species = Homo sapiens, network type = full STRING network, confidence score ≥0.4, layout = yFiles Organic layout.
Data and Resource Availability
The GWAS summary statistics used in this article were accessed from the IEU OpenGWAS project (https://gwas.mrcieu.ac.uk/), the GTEx Portal (https://www.gtexportal.org/), the eQTLGen Consortium (https://eqtlgen.org/), the DIAGRAM consortium (https://diagram-consortium.org/), and the CARDIoGRAMplusC4D consortium (http://www.cardiogramplusc4d.org/) and the FinnGen study (https://finngen.gitbook.io/documentation/data-download).
Results
Heritability and Genetic Correlation of Choline Metabolites
GWAS results of the choline metabolites were available in up to 114,999 European participants in UK Biobank. There was little evidence of inflation of the association results, as the LD score regression intercept terms were 1.039, 1.037, and 1.029 for choline, phosphatidylcholine, and glycine, respectively (an intercept term close to 1 means little influence of population structure). Single-trait LD score regression results showed that common variants included in the GWAS explained 13.6%, 14.5%, and 14.1% of the heritability of choline, phosphatidylcholine, and glycine, respectively (Supplementary Table 5). Genetic correlation analysis among the three choline metabolites revealed a very high genetic correlation between choline and phosphatidylcholine (genetic correlation = 0.992, P = 0) but relatively low genetic correlations between choline/phosphatidylcholine and glycine (genetic correlation between choline and glycine 0.027, P = 0.583, and genetic correlation between phosphatidylcholine and glycine 0.022, P = 0.637) (Supplementary Fig. 1 and Supplementary Table 5).
MR Analyses
Strength of the Genetic Predictors for SGLT2 Inhibition and Choline Metabolites
The predictors of SGLT2 inhibition showed strong strength (F statistic = 24.1, which is over the common threshold of 10) (Supplementary Table 2). The predictors for the three choline metabolites were all very strong (F statistics for glycine = 437.0, phosphatidylcholine = 126.7, and total choline = 110.3) (Supplementary Table 3). Due to good strength, all of these genetic predictors were kept for the MR analysis.
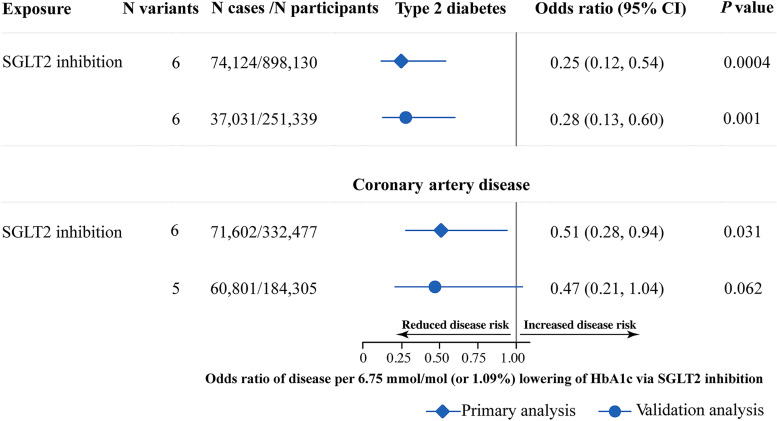
Effect of SGLT2 Inhibition on CAD and T2D Risk
SGLT2 inhibition was associated with reduced risk of T2D (odds ratio [OR] 0.25 [95% CI 0.12, 0.54], P = 4.0 × 10−4) and reduced risk of CAD (0.51 [0.28, 0.94], P = 0.030) for per 1-SD unit (6.75 mmol/mol or 1.09%) lowering of HbA1c via SGLT2 inhibition (Table 1 and Fig. 2). The heterogeneity test using Cochran Q test for IVW showed that the Q statistics and P values were not significant (P = 0.63 and 0.66, respectively), which implied no evidence of heterogeneity for the effect of SGLT2 inhibition on CAD and T2D. The pleiotropy test using the MR-Egger intercept term showed that P values of intercept were 0.39 to 0.50, respectively, which means directional pleiotropy is not an issue for these results (Table 1).
Table 1.
MR estimates of the effect of SGLT2 inhibition and choline metabolites on T2D and CAD
| Exposure/mediator | Outcome | Method | OR (95% CI) | P | Q statistic* | P h | Egger intercept | P intercept |
|---|---|---|---|---|---|---|---|---|
| SGLT2 inhibition | T2D | IVW | 0.25 (0.12, 0.54) | 0.0004 | 3.250 | 0.661 | ||
| MR-Egger | 0.62 (0.04, 9.63) | 0.732 | 2.530 | 0.639 | 0.012 | 0.500 | ||
| MR-PRESSO | 0.22 (0.12, 0.39) | 0.003 | 4.959 | 0.698 | ||||
| CAD | IVW | 0.51 (0.28, 0.94) | 0.031 | 3.487 | 0.625 | |||
| MR-Egger | 0.19 (0.02, 2.18) | 0.181 | 2.049 | 0.727 | −0.014 | 0.391 | ||
| MR-PRESSO | 0.51 (0.38, 0.68) | 0.006 | 1.904 | 0.923 | ||||
| Total choline | T2D | IVW | 0.78 (0.68, 0.89) | 0.0006 | 259.773 | 9.41 × 10−30 | ||
| MR-Egger | 0.91 (0.70, 1.18) | 0.498 | 249.715 | 2.44 × 10−28 | −0.010 | 0.162 | ||
| Weighted median | 0.88 (0.79, 0.98) | 0.021 | ||||||
| Simple mode | 0.81 (0.65, 1.01) | 0.066 | ||||||
| Weighted mode | 0.91 (0.83, 1.00) | 0.058 | ||||||
| MR-PRESSO | 0.82 (0.74, 0.90) | 0.0003 | 286.130 | <0.0001 | ||||
| CAD | IVW | 1.12 (0.95, 1.31) | 0.212 | 642.922 | 1.40 × 10−99 | |||
| MR-Egger | 0.95 (0.70, 1.30) | 0.769 | 628.440 | 3.10 × 10−97 | 0.010 | 0.257 | ||
| Weighted median | 1.12 (1.02, 1.23) | 0.018 | ||||||
| Simple mode | 1.10 (0.90, 1.35) | 0.365 | ||||||
| Weighted mode | 1.08 (0.98, 1.19) | 0.114 | ||||||
| MR-PRESSO | 1.10 (1.01, 1.20) | 0.311 | 661.626 | <0.0001 | ||||
| Phosphatidylcholine | T2D | IVW | 0.81 (0.72, 0.91) | 0.0009 | 233.996 | 1.37 × 10−24 | ||
| MR-Egger | 0.90 (0.73, 1.12) | 0.357 | 227.538 | 8.07 × 10−24 | −0.008 | 0.230 | ||
| Weighted median | 0.89 (0.81, 0.99) | 0.026 | ||||||
| Simple mode | 0.88 (0.72, 1.06) | 0.177 | ||||||
| Weighted mode | 0.91 (0.83, 0.99) | 0.028 | ||||||
| MR-PRESSO | 0.84 (0.77, 0.93) | 0.001 | 246.155 | <0.0001 | ||||
| CAD | IVW | 1.08 (0.94, 1.24) | 0.270 | 491.466 | 6.84 × 10−71 | |||
| MR-Egger | 0.98 (0.77, 1.25) | 0.870 | 483.221 | 8.98 × 10−70 | 0.007 | 0.337 | ||
| Weighted median | 1.10 (1.01, 1.20) | 0.036 | ||||||
| Simple mode | 1.11 (0.91, 1.36) | 0.317 | ||||||
| Weighted mode | 1.09 (1.00, 1.19) | 0.049 | ||||||
| MR-PRESSO | 1.10 (1.02, 1.18) | 0.020 | 506.247 | <0.0001 | ||||
| Glycine | T2D | IVW | 0.93 (0.86, 1.01) | 0.137 | 245.898 | 1.23 × 10−30 | ||
| MR-Egger | 1.00 (0.91, 1.10) | 0.988 | 211.364 | 8.42 × 10−25 | −0.013 | 0.013 | ||
| Weighted median | 0.96 (0.93, 1.00) | 0.067 | ||||||
| Simple mode | 0.80 (0.63, 1.02) | 0.073 | ||||||
| Weighted mode | 0.96 (0.92, 1.00) | 0.072 | ||||||
| MR-PRESSO | 0.85 (0.75, 0.97) | 0.023 | 348.477 | <0.0001 | ||||
| CAD | IVW | 0.94 (0.91, 0.98) | 0.008 | 100.528 | 1.05 × 10−6 | |||
| MR-Egger | 0.97 (0.93, 1.03) | 0.326 | 85.529 | 5.65 × 10−5 | −0.007 | 0.011 | ||
| Weighted median | 0.96 (0.93, 0.99) | 0.013 | ||||||
| Simple mode | 0.90 (0.79, 1.03) | 0.151 | ||||||
| Weighted mode | 0.95 (0.92, 0.99) | 0.008 | ||||||
| MR-PRESSO | 0.88 (0.81, 0.96) | 0.006 | 226.771 | 0.015 |
OR, 95% CI, and P values were for the respective MR analysis. Ph, P value for heterogeneity; Pintercept, P value for intercept of MR-Egger regression.
Heterogeneity test in the IVW methods was through use of Cochran Q statistic and for the MR-PRESSO method the global test.
Figure 2.
Causal effect of SGLT2 inhibition on T2D and CAD. The OR and 95% CI indicate the effect estimates of decrease in T2D and CAD per SD unit (6.75 mmol/mol or 1.09%) lowering of HbA1c via SGLT2 inhibition with use of the IVW method. The T2D data were from the DIAGRAM consortium in the primary analysis (the diamonds) and FinnGen study in the validation analysis (dots). The CAD data were from a meta-GWAS of CARDIoGRAMplusC4D and UK Biobank in the primary analysis (diamonds) and CARDIoGRAMplusC4D only in the validation analysis (dots).
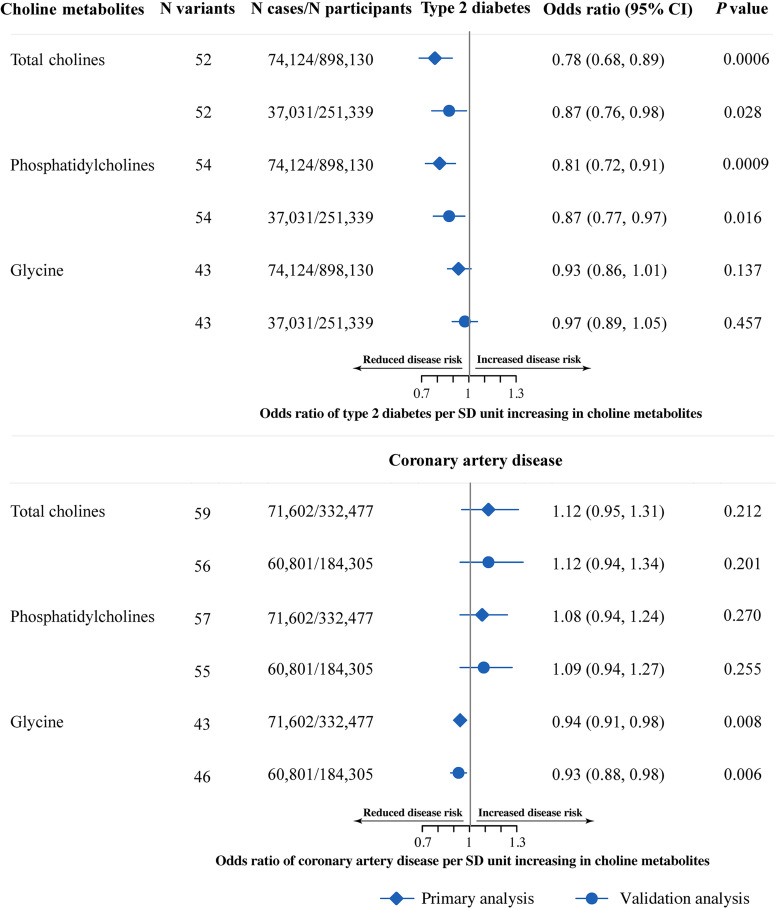
Mediation MR of SGLT2 Inhibition, Choline Metabolites, and CAD and T2D Risk
We estimated the effect of total choline and two choline metabolites on risk for the two cardiometabolic diseases, CAD and T2D (six independent tests due to correlation among the metabolites, Bonferroni-corrected threshold = 8.33 × 10−3). For total choline and phosphatidylcholine, we observed negative associations with T2D (OR for total choline 0.78 [95% CI 0.68, 0.89], P = 6.0 × 10−4; OR for phosphatidylcholine 0.81 [0.72, 0.91], P = 9.0 × 10−4) but little evidence to support association with CAD (Table 1 and Fig. 3). For glycine, we observed a negative association with CAD (0.94 [0.91, 0.98], P = 8.0 × 10−3). Glycine showed similar effect with T2D (0.93 [0.86, 1.01], P = 0.137), but due to heterogeneity across genetic predictors (P value of Cochran Q = 1.23 × 10−30), the CI was wide and across OR of 1 (Table 1).
Figure 3.
Causal effect of choline metabolites on T2D and CAD. The OR and 95% CI indicate the effect estimates of decrease in T2D and CAD risk per SD unit of each choline metabolite with use of the IVW method. The T2D data were from the DIAGRAM consortium in the primary analysis (diamonds) and FinnGen study in the validation analysis (dots). The CAD data were from a meta-GWAS of CARDIoGRAMplusC4D and UK Biobank in the primary analysis (diamonds), and CARDIoGRAMplusC4D only in the validation analysis (dots).
We estimated the effect of SGLT2 inhibition on the three choline metabolites (two independent tests due to correlation among metabolites, Bonferroni-corrected threshold = 0.025) (Table 2). SGLT2 inhibition was associated with total choline (β = 0.39 [95% CI 0.06, 0.72], P = 0.020), phosphatidylcholine (0.40 [0.13, 0.67], P = 0.006), and glycine (0.34 [0.05, 0.63], P = 0.023), which implies that SGLT2 inhibition may have a general effect on choline metabolism. The Q statistics and P values were not significant (P values between 0.24 and 0.54), which implied no evidence of heterogeneity for the effect of SGLT2 on choline metabolites. The pleiotropy test using the MR-Egger intercept term showed that P values of the intercepts were between 0.13 and 0.38, which means litter directional pleiotropy (Table 2).
Table 2.
MR estimates of the effect of SGLT2 inhibition on choline metabolites
| Exposure | Mediator | Method | β (95% CI) | P | Q statistic* | P h | Egger intercept | P intercept |
|---|---|---|---|---|---|---|---|---|
| SGLT2 inhibition | Total choline | IVW | 0.39 (0.06, 0.72) | 0.020 | 6.782 | 0.237 | ||
| MR Egger | −0.23 (−1.08, 0.62) | 0.599 | 4.349 | 0.361 | 0.009 | 0.127 | ||
| MR PRESSO | 0.35 (0.09, 0.62) | 0.048 | 8.539 | 0.389 | ||||
| SGLT2 inhibition | Phosphatidylcholine | IVW | 0.40 (0.13, 0.67) | 0.006 | 4.324 | 0.504 | ||
| MR Egger | 0.02 (−0.88, 0.91) | 0.975 | 3.402 | 0.493 | 0.005 | 0.376 | ||
| MR PRESSO | 0.37 (0.16, 0.58) | 0.018 | 5.293 | 0.691 | ||||
| SGLT2 inhibition | Glycine | IVW | 0.34 (0.05, 0.63) | 0.023 | 5.207 | 0.391 | ||
| MR Egger | −0.11 (−0.95, 0.73) | 0.800 | 3.958 | 0.412 | 0.006 | 0.266 | ||
| MR-PRESSO | 0.40 (0.22, 0.59) | 0.007 | 3.859 | 0.784 |
β, 95% CI, and P values were for the respective MR analysis. Ph, P value for heterogeneity; Pintercept, P value for intercept of MR-Egger regression.
Heterogeneity test in the IVW methods was through use of Cochran Q statistic and for the MR-PRESSO method the global test.
We observed an indirect effect of SGLT2 inhibition on T2D through total choline (OR 0.91 [95% CI 0.83, 0.99]), with a mediated proportion of 8% of the total effect, and through phosphatidylcholine (0.93 [0.86, 0.98]) with a mediated proportion of 5%. The indirect effect of SGLT2 inhibition on CAD through glycine had an OR of 0.98 (0.96, 1.00), with a mediated proportion of 2%. Glycine did not have significant mediation effect in causal relation of SGLT2 inhibition on T2D (1.00 [0.98, 1.02]); total choline and phosphatidylcholine did not have significant mediation effect in causal relation of SGLT2 inhibition on CAD (1.04 [0.97, 1.13], and 1.04 [0.98, 1.10], respectively).
Validation and Sensitivity Analysis
All of the results were well replicated in the independent data sets or populations (Figs. 2 and 3 and Supplementary Tables 6 and 7). The MR-PRESSO analysis reported a narrower 95% CI of the effects after exclusion of the outlier single nucleotide polymorphisms (SNPs) (for example, IVW estimate for effect of SGLT2 inhibition on total choline 0.39 [95% CI 0.06, 0.72] and MR-PRESSO 0.35 [0.09, 0.62]) (Table 1 and Supplementary Table 7). The distortion test comparing the causal estimates before and after outlier removal suggested no statistical difference between the two (distortion test P = 0.651). The MR sensitivity analyses including MR-Egger, weighted median, and mode estimator showed similar effect estimates (Tables 1 and 2 and Supplementary Tables 6 and 7).
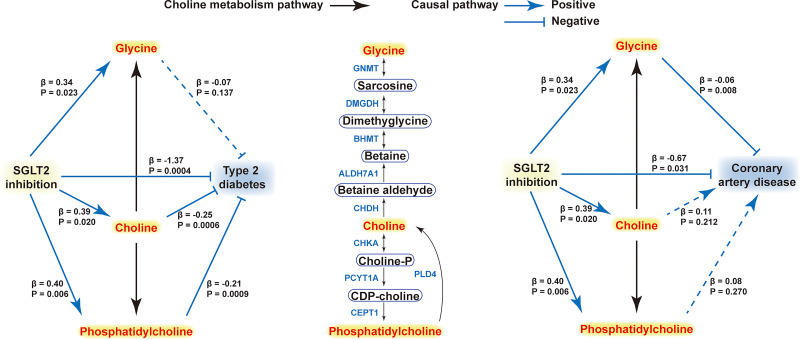
Integration of Choline Metabolism Pathway Information With Genetic Evidence
The PPI network suggested that SGLT2 (tagged by SLC5A2 protein) showed interaction with lipid metabolism–related proteins (such as LCAT) and glycine-related proteins (such as PPARG) via two distinguished pathways (Fig. 4). SGLT2 interacted with glycine metabolism–related proteins through the PPARG protein, while with choline metabolism it could be influenced by proteins involved in the lipid metabolism pathway via key proteins such as LCAT.
Figure 4.
Integration of causal and choline metabolism evidence. Proteins in the PPI network including 1 drug target (SLC5A2) (red node), 21 glycine-choline pathway-related proteins (5 enzymes in choline-glycine biosynthesis pathway and 16 glycine-associated SNP corresponding proteins) (yellow nodes), and 35 choline-phosphatidylcholine pathway–related proteins (4 enzymes in choline-phosphatidylcholine biosynthesis pathway and 31 choline and phosphatidylcholine-associated SNP corresponding proteins) (blue nodes). Parameters: network type = full STRING network, confidence score ≥0.4. After removal of isolated nodes, the PPI network with 57 nodes (proteins) and 191 edges (interactions) was generated. These proteins/genes were clustered into three groups, proteins related to lipids metabolism, choline metabolism, and glycine metabolism. The PPI network was built with stringApp in Cytoscape with the following parameters: data source = protein query, species = H. sapiens, network type = full STRING network, confidence score ≥0.4, layout = yFiles Organic layout. The edge thickness represents the confidence score of each interaction from evidence channel in STRING. The distance of each edge was automatically generated with Organic layout algorithm, which rearranges the positions of the nodes to reach well-balanced distribution of nodes, few edge crossings, and a minimal sum of distance between nodes and edges. Organic layout is well suited for the visualization of highly connected backbone regions, and different modules of a network can be easily identified with proteins containing more interactions as hub nodes placing in the core of the network and proteins containing less interactions as outliers.
We summarized the causal evidence obtained from MR analysis with the biological evidence obtained from pathway analysis (Fig. 5). We observed two distinguished causal pathways that linked SGLT2 inhibition with CAD and T2D. For the causal pathway linking SGLT2 inhibition with reduced T2D risk, the causal effect was mediated by increasing total choline and phosphatidylcholine but less likely to be mediated by changing glycine levels. For the causal pathway linking SGLT2 inhibition with CAD, the causal effect was mediated by increasing glycine levels rather than choline.
Figure 5.
Summary integrating the causal evidence from MR with the biological evidence from the pathway and PPI analysis. The diagram includes the choline metabolism pathway (middle) and causal pathways of SGLT2 inhibition–metabolites–diseases. In choline metabolism pathway, single-side arrows indicate nonreversible reactions and double-side arrows indicate reversible reactions. In causal pathways, the arrows and T-shaped lines labeled with corresponding enzymes beside signify positive and negative associations, respectively, in which the solid lines indicate significant causality and dotted lines nonsignificant. The β-values are the MR estimates. GNMT, glycine N-methyltransferase; BHMT, betaine-homocysteine S-methyltransferase; CEPT1, choline/ethanolamine phosphotransferase 1; CHDH, choline dehydrogenase; CHKA, choline kinase α; DMGDH, dimethylglycine dehydrogenase; ALDH7A1, aldehyde dehydrogenase 7 family member A1; PCYT1A, phosphate cytidylyltransferase 1A; PLD4, phospholipase D family member 4.
Conclusions
In the present MR study, we identified the causal roles of SGLT2 inhibition on outcomes of cardiometabolic disease, CAD and T2D, and of total choline and two key metabolites on the choline metabolism pathway, phosphatidylcholine and glycine. The mediation MR analysis further suggested that SGLT2 inhibition may influence T2D and CAD via different metabolism pathways. Total choline and phosphatidylcholine were estimated to mediate the effect of SGLT2 inhibition on T2D but showed no association with CAD. In contrast, glycine was estimated to mediate the effect of SGLT2 inhibition on CAD but not T2D. We also demonstrated that total choline and phosphatidylcholine were genetically associated with lower risk of T2D, while glycine was genetically associated with a lower risk of CAD, which would compensate for the present evidence from the observational studies.
Few studies have explored the molecular mechanisms of the effect of SGLT2 inhibition on diabetes and CVD risk prevention. In the previous studies, it was demonstrated that the improvement in cardiovascular outcomes with empagliflozin, one of the SGLT2 inhibitors, is independent of glycemic control (34). In the BI 10773 (Empagliflozin) Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG OUTCOME) trial, the reductions in risks of cardiovascular death were consistent across categories of baseline HbA1c, regardless of the magnitude of reduction in HbA1c or adjustment for HbA1c control at baseline and during the trial (34). This suggests that there may be other metabolic pathways mediating the effects. In a previous prospective study, investigators conducted untargeted metabolomics for 25 empagliflozin-treated patients with T2D and CVD (10). They provided an SGLT2 inhibitor–treated metabolic signature in reporting a wide range of metabolites changes during the treatment. However, due to the limited sample size, the study only provided a systematic snapshot of the effect of empagliflozin on highly relevant metabolic pathways of the whole organism and not elucidation of definitive mechanisms on substrate flux in the myocardium. Again, because of the observational nature of the study, the causal effect of SGLT2 inhibition on the circulating metabolites cannot be inferred. In our present study, we used a set of robust genetic proxies of SGLT2 as the instrument variables (IVs) and the largest metabolites GWAS resource to date as mediators. We showed the causal effects of SGLT2 inhibition on circulating total choline and two of its key metabolites. The results would deepen our understanding of the causal metabolic mechanism of SGLT2 inhibition influencing multiple cardiometabolic diseases.
In our study, genetic SGLT2 inhibition leads to a reduction in risk of T2D and CAD. Whether SGLT2 inhibitors also lead to a reduction in progression to T2D is yet to be confirmed. The very recent study with use of pooled individual patient–level data from the Dapagliflozin And Prevention of Adverse outcomes in Chronic Kidney Disease (DAPA-CKD) and Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure (DAPA-HF) trials (35) showed that treatment with dapagliflozin reduced the incidence of new-onset T2D in participants with chronic kidney disease and heart failure. Our results provide timely and strong evidence of an effect of SGLT2 inhibition on reduced risk of T2D. We show that total choline and phosphatidylcholine were significantly associated with T2D and that SGLT2 inhibition may reduce T2D risk through increasing total choline and phosphatidylcholine levels.
Recent studies suggested that the increased CVD risk is mainly influenced by the gut microbiota–related dietary choline metabolites (14). Additionally, an association between increased whole blood levels of total choline and CVD has also been reported (36). However, our MR results with use of large-scale samples suggested that this observational association may be unlikely to be causal in the general population.
Our findings support that genetically determined glycine level was strongly associated with CAD, which was consistent with findings from an MR study (37) and a recent observational study as well (38). Circulating glycine had negative associations with atherosclerosis through increased expression of APOA1BP in the liver in obese patients (38). In the current study, the genetic evidence did not support a significant causal association of glycine with T2D, which was confirmed by an independent sample set and the previous report (37). However, another MR study showed a significant negative association of glycine with T2D (39). The discrepancy was mainly due to the different study population (DIAGRAM and the FinnGen study in our analysis and DIAGRAM in the study of Wittemans et al. [37] and the GoT2D study in the analysis of Merino et al. [39]), the sample size, and the IVs of glycine they used. Further investigations on this issue are warranted. In the PPI analysis, we found that a group of lipid metabolism–related genes/proteins was involved in the interactions of SLC5A2 and choline metabolism pathways. We highly speculate that the effect of SGLT2 inhibition via glycine on CAD might be partially mediated by lipids metabolism.
Our preliminary data from the bioinformatics analysis showed that several node proteins may be involved in the lipid metabolism pathway via key proteins such as LCAT, which plays a central role in HDL metabolism, and insulin resistance such as PPARG. However, few data have been reported on the potential mechanism of SGLT2 inhibition exerting a beneficial effect on T2D and CAD through the choline metabolism pathways.
This study has several strengths. First, this is the very first study mimicking SGLT2 inhibition using genetics. SGLT2 inhibition is a monotherapy that mainly targets the SLC5A2 gene. This fits well with the MR design of estimating the effect of a single drug target. However, there is a limited number of genetic variants associated with the expression level of SLC5A2, which makes it difficult to obtain enough power for the MR analysis (40). We successfully applied a recent instrument selection pipeline, which identified six genetic variants that are robustly associated with both expression levels of SLC5A2 and HbA1c level. Using these variants as instruments, we obtained good instrument strength to conduct the MR analysis of SGLT2 inhibition (F statistic = 24.1). The causal effects of SGLT2 inhibition with use of the selected IVs on the two outcomes were well validated in independent populations. Second, the sample size of choline metabolites was >110,000 participants, while the T2D and CAD data were derived from one of the largest genetic studies to date, which guaranteed the statistical power to the findings and conclusions of the study. Third, the findings were novel. The metabolic pathway of choline metabolites in mediating the effect of SGLT2 inhibition on T2D and CAD risk may help with understanding of the drug effect and mechanisms when further extensively used in clinical practice.
Study Limitations
Several limitations should be acknowledged. First, limited metabolites were considered. Specific to our hypothesis, only total choline and two choline metabolites were included in this study, which did not cover the whole choline metabolism pathway. This is mainly due to the lack of powerful GWAS data. For example, we used the untargeted nuclear magnetic resonance metabolomics profiling that initially quantified 249 metabolites in the UK Biobank. Therefore, only some low-density choline metabolites were measured. Although we searched other GWAS resources in literature and further included betaine in our study, we still missed some key choline metabolites, such as trimethylamine N-oxide and acetylcholine. The results of our study raise the importance of choline in cardiometabolic health and may encourage more genetic epidemiological studies to investigate the choline metabolism pathway as a whole. However, we still got a substantially large sample size of targeted metabolites measured, which provided sufficient power to reach the conclusion. Second, although our results suggested that SGLT2 may influence T2D via choline and CAD via glycine, we noticed that the center MR estimates of glycine on CAD and T2D were similar. The effect of glycine on T2D showed a wide CI across β of zero due to the heterogeneity across single variant effects. The causal role of glycine for T2D requires further investigation once more heterogeneity robust MR methods have been developed. Third, given that the major and most consistent outcome for SGLT2 inhibitors is reduction of hospitalization for heart failure, further well-designed MR study and investigations on mechanism(s) linking beneficial effects of SGLT2 inhibitors are warranted. Fourth, in our study, there are partially overlapped samples of studies that contributed to both GWAS studies for the exposure and outcome (i.e., the GWAS for metabolites were performed in ∼25% of the UK Biobank, in which the IVs of the exposure SGLT2 inhibition were also from the same cohort). The sample overlap between the exposure and outcome participants, in the case of weak instruments, could bias two-sample MR estimates toward the confounded association between the exposure and the outcome (41). Nevertheless, in the current study, the genetic instruments strongly associated with exposure, as suggested by large F statistics. We also tested the type I errors and replicated the results in independent populations. It showed that it is unlikely that our results were biased by weak instruments. Finally, for the external validity of the MR results, caution should be exercised to generalize the finding to other ethnic groups, given that the study populations were predominantly of European ancestry.
Conclusion
In conclusion, we identified causal roles of SGLT2 inhibition of three metabolites in the choline metabolism pathway. The SGLT2 inhibition may influence T2D and CAD risk via choline and glycine metabolism separately, which implies new mechanisms of this classic metabolism pathway. The findings provide novel insights into the mechanisms of SGLT2 inhibition in reducing cardiometabolic disease risk and evidence to support future clinical trials of choline metabolites and cardiometabolic health.
Article Information
Acknowledgments. This research was conducted with use of the UK Biobank resource (https://www.ukbiobank.ac.uk) (UK Biobank received ethics approval from the Research Ethics Committee [reference no. 11/NW/0382]). Data on outcomes were contributed by the IEU OpenGWAS database investigators and were downloaded from https://gwas.mrcieu.ac.uk/. The authors thank the individual patients who provided the sample that made data available; without them the study would not have been possible. In this study we also used GWAS summary data from the GTEx Portal, the eQTLGen consortium, and the IEU OpenGWAS project, the DIAGRAM consortium, the CARDIoGRAMplusC4D consortium, and the FinnGen study. The authors thank all of the investigators who provided these data to support this study.
Funding. This work was funded by the National Natural Science Foundation of China (81941017, 81930021, 81970728, 81970706, 82022011, 82270859, 91857205, and 82088102), the Shanghai Municipal Education Commission–Gaofeng Clinical Medicine Grant Support (20152508 Round 2), and the Shanghai Shenkang Hospital Development Center (SHDC12019101, SHDC2020CR1001A, and SHDC2020CR3064B). M.X., T.W., J.L., M.L., Y.X., G.N., Y.B., and W.W. are members of the Innovative Research Team of High-level Local Universities in Shanghai. J.Z. is supported by the Academy of Medical Sciences Springboard Award, the Wellcome Trust, the Government Department of Business, Energy and Industrial Strategy (BEIS), the British Heart Foundation, and Diabetes UK (SBF006\1117). J.Z. is funded by the Vice-Chancellor Fellowship from the University of Bristol. J.Z. is supported by Shanghai Thousand Talents Program.
Duality of Interest. J.Z. has received research funding from various pharmaceutical companies to support the application of MR to drug target prioritization. No other potential conflicts of interest relevant to this article were reported.
This study was not supported or funded by any of the pharmaceutical companies from which J.Z. received research funding.
Author Contributions. M.X., J.Z., G.N., Y.B., and W.W. conceived and designed the study. M.X., J.Z., T.H., and H.L. analyzed data. T.W., S.W., J.L. Z.Z., M.L., and Y.X. collected data. All authors were involving in writing and revising the manuscript and had final approval of the submitted and published versions. W.W. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.20440365.
References
- 1. Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ. Sodium glucose cotransporter 2 inhibitors in the treatment of diabetes mellitus: cardiovascular and kidney effects, potential mechanisms, and clinical applications. Circulation 2016;134:752–772 [DOI] [PubMed] [Google Scholar]
- 2. Zinman B, Wanner C, Lachin JM, et al.; EMPA-REG OUTCOME Investigators . Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117–2128 [DOI] [PubMed] [Google Scholar]
- 3. Neal B, Perkovic V, Mahaffey KW, et al.; CANVAS Program Collaborative Group . Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 2017;377:644–657 [DOI] [PubMed] [Google Scholar]
- 4. Wiviott SD, Raz I, Bonaca MP, et al.; DECLARE–TIMI 58 Investigators . Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2019;380:347–357 [DOI] [PubMed] [Google Scholar]
- 5. Cannon CP, Pratley R, Dagogo-Jack S, et al.; VERTIS CV Investigators . Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med 2020;383:1425–1435 [DOI] [PubMed] [Google Scholar]
- 6. McMurray JJV, Solomon SD, Inzucchi SE, et al.; DAPA-HF Trial Committees and Investigators . Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 2019;381:1995–2008 [DOI] [PubMed] [Google Scholar]
- 7. Wanner C, Inzucchi SE, Lachin JM, et al.; EMPA-REG OUTCOME Investigators . Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 2016;375:323–334 [DOI] [PubMed] [Google Scholar]
- 8. Perkovic V, Jardine MJ, Neal B, et al.; CREDENCE Trial Investigators . Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med 2019;380:2295–2306 [DOI] [PubMed] [Google Scholar]
- 9. Cowie MR, Fisher M. SGLT2 inhibitors: mechanisms of cardiovascular benefit beyond glycaemic control. Nat Rev Cardiol 2020;17:761–772 [DOI] [PubMed] [Google Scholar]
- 10. Kappel BA, Lehrke M, Schütt K, et al. Effect of empagliflozin on the metabolic signature of patients with type 2 diabetes mellitus and cardiovascular disease. Circulation 2017;136:969–972 [DOI] [PubMed] [Google Scholar]
- 11. Aragón-Herrera A, Otero-Santiago M, Anido-Varela L, et al. The treatment with the SGLT2 inhibitor empagliflozin modifies the hepatic metabolome of male Zucker diabetic fatty rats towards a protective profile. Front Pharmacol 2022;13:827033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Leermakers ET, Moreira EM, Kiefte-de Jong JC, et al. Effects of choline on health across the life course: a systematic review. Nutr Rev 2015;73:500–522 [DOI] [PubMed] [Google Scholar]
- 13. Wang Z, Klipfell E, Bennett BJ, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 2011;472:57–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tang WHW, Wang Z, Levison BS, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 2013;368:1575–1584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hartiala J, Bennett BJ, Tang WH, et al.; CARDIoGRAM Consortium . Comparative genome-wide association studies in mice and humans for trimethylamine N-oxide, a proatherogenic metabolite of choline and L-carnitine. Arterioscler Thromb Vasc Biol 2014;34:1307–1313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Roe AJ, Zhang S, Bhadelia RA, et al. Choline and its metabolites are differently associated with cardiometabolic risk factors, history of cardiovascular disease, and MRI-documented cerebrovascular disease in older adults. Am J Clin Nutr 2017;105:1283–1290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Palau-Rodriguez M, Tulipani S, Isabel Queipo-Ortuño M, Urpi-Sarda M, Tinahones FJ, Andres-Lacueva C. Metabolomic insights into the intricate gut microbial-host interaction in the development of obesity and type 2 diabetes. Front Microbiol 2015;6:1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guasch-Ferré M, Hu FB, Ruiz-Canela M, et al. Plasma metabolites from choline pathway and risk of cardiovascular disease in the PREDIMED (Prevention With Mediterranean Diet) Study. J Am Heart Assoc 2017;6:e006524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Walker VM, Kehoe PG, Martin RM, Davies NM. Repurposing antihypertensive drugs for the prevention of Alzheimer’s disease: a Mendelian randomization study. Int J Epidemiol 2020;49:1132–1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. GTEx Consortium . The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science 2020;369:1318–1330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Võsa U, Claringbould A, Westra HJ, et al.; BIOS Consortium; i2QTL Consortium . Large-scale cis- and trans-eQTL analyses identify thousands of genetic loci and polygenic scores that regulate blood gene expression. Nat Genet 2021;53:1300–1310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Elsworth B, Lyon M, Alexander T, et al. The MRC IEU OpenGWAS data infrastructure. 10 August 2020 [preprint]. bioRxiv:2020.08.10.244293 [Google Scholar]
- 23. Hartiala JA, Tang WH, Wang Z, et al. Genome-wide association study and targeted metabolomics identifies sex-specific association of CPS1 with coronary artery disease. Nat Commun 2016;7:10558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mahajan A, Taliun D, Thurner M, et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat Genet 2018;50:1505–1513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nelson CP, Goel A, Butterworth AS, et al.; EPIC-CVD Consortium; CARDIoGRAMplusC4D; UK Biobank CardioMetabolic Consortium CHD working group . Association analyses based on false discovery rate implicate new loci for coronary artery disease. Nat Genet 2017;49:1385–1391 [DOI] [PubMed] [Google Scholar]
- 26. Nikpay M, Goel A, Won HH, et al. A comprehensive 1,000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat Genet 2015;47:1121–1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bulik-Sullivan BK, Loh PR, Finucane HK, et al.; Schizophrenia Working Group of the Psychiatric Genomics Consortium . LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet 2015;47:291–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Burgess S, Zuber V, Valdes-Marquez E, Sun BB, Hopewell JC. Mendelian randomization with fine-mapped genetic data: Choosing from large numbers of correlated instrumental variables. Genet Epidemiol 2017;41:714–725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carter AR, Sanderson E, Hammerton G, et al. Mendelian randomisation for mediation analysis: current methods and challenges for implementation. Eur J Epidemiol 2021;36:465–478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Xu L, Borges MC, Hemani G, Lawlor DA. The role of glycaemic and lipid risk factors in mediating the effect of BMI on coronary heart disease: a two-step, two-sample Mendelian randomisation study. Diabetologia 2017;60:2210–2220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zheng J, Richardson TG, Millard LAC, et al. PhenoSpD: an integrated toolkit for phenotypic correlation estimation and multiple testing correction using GWAS summary statistics. Gigascience 2018;7:giy090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hemani G, Zheng J, Elsworth B, et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife 2018;7:e34408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Szklarczyk D, Franceschini A, Wyder S, et al. STRING v10: protein-protein interaction networks, integrated over the tree of life. Nucleic Acids Res 2015;43:D447–D452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Inzucchi SE, Kosiborod M, Fitchett D, et al. Improvement in cardiovascular outcomes with empagliflozin is independent of glycemic control. Circulation 2018;138:1904–1907 [DOI] [PubMed] [Google Scholar]
- 35. Rossing P, Inzucchi SE, Vart P, et al.; DAPA-CKD and DAPA-HF Trial Committees and Investigators . Dapagliflozin and new-onset type 2 diabetes in patients with chronic kidney disease or heart failure: pooled analysis of the DAPA-CKD and DAPA-HF trials. Lancet Diabetes Endocrinol 2022;10:24–34 [DOI] [PubMed] [Google Scholar]
- 36. Danne O, Lueders C, Storm C, Frei U, Möckel M. Whole blood choline and plasma choline in acute coronary syndromes: prognostic and pathophysiological implications. Clin Chim Acta 2007;383:103–109 [DOI] [PubMed] [Google Scholar]
- 37. Wittemans LBL, Lotta LA, Oliver-Williams C, et al. Assessing the causal association of glycine with risk of cardio-metabolic diseases. Nat Commun 2019;10:1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mayneris-Perxachs J, Puig J, Burcelin R, et al. The APOA1bp-SREBF-NOTCH axis is associated with reduced atherosclerosis risk in morbidly obese patients. Clin Nutr 2020;39:3408–3418 [DOI] [PubMed] [Google Scholar]
- 39. Merino J, Leong A, Liu CT, et al. Metabolomics insights into early type 2 diabetes pathogenesis and detection in individuals with normal fasting glucose. Diabetologia 2018;61:1315–1324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Klen J, Dolžan V. Treatment response to SGLT2 inhibitors: from clinical characteristics to genetic variations. Int J Mol Sci 2021;22:9800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Burgess S, Davies NM, Thompson SG. Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol 2016;40:597–608 [DOI] [PMC free article] [PubMed] [Google Scholar]