Abstract
Background
The pathogenesis of pulmonary arterial hypertension (PAH) and associated biomarkers remain to be studied. Copper metabolism is an emerging metabolic research direction in many diseases, but its role in PAH is still unclear.
Methods
PAH-related datasets were downloaded from the Gene Expression Omnibus database, and 2067 copper metabolism-related genes (CMGs) were obtained from the GeneCards database. Differential expression analysis and the Venn algorithm were used to acquire the differentially expressed CMGs (DE-CMGs). DE-CMGs were then used for the coexpression network construction to screen candidate key genes associated with PAH. Furthermore, the predictive performance of the model was verified by receiver operating characteristic (ROC) analysis, and genes with area under the curve (AUC) values greater than 0.8 were selected as diagnostic genes. Then support vector machine, least absolute shrinkage and selection operator regression, and Venn diagrams were applied to detect biomarkers. Moreover, gene set enrichment analysis was performed to explore the function of the biomarkers, and immune-related analyses were utilized to study the infiltration of immune cells. The drug-gene interaction database was used to predict potential therapeutic drugs for PAH using the biomarkers. Biomarkers expression in clinical samples was verified by real-time quantitative PCR.
Results
Four biomarkers (DDIT3, NFKBIA, OSM, and PTGER4) were screened. The ROC analysis showed that the 4 biomarkers performed well (AUCs > 0.7). The high expression groups for the 4 biomarkers were enriched in protein activity-related pathways including protein export, spliceosome and proteasome. Furthermore, 8 immune cell types were significantly different between the two groups, including naive B cells, memory B cells, and resting memory CD4 T cells. Afterward, a gene-drug network was constructed. This network illustrated that STREPTOZOCIN, IBUPROFEN, and CELECOXIB were shared by the PTGER4 and DDIT3. Finally, the results of RT-qPCR in clinical samples further confirmed the results of the public database for the expression of NFKBIA and OSM.
Conclusion
In conclusion, four biomarkers (DDIT3, NFKBIA, OSM, and PTGER4) with considerable diagnostic values were identified, and a gene-drug network was further constructed. The results of this study may have significant implications for the development of new diagnostic biomarkers and actionable targets to expand treatment options for PAH patients.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12890-023-02326-6.
Keywords: Pulmonary arterial hypertension, Copper metabolism-related genes, Biomarkers
Introduction
Pulmonary hypertension (PH) is defined by a mean pulmonary arterial pressure ≥ 20 mmHg at rest as assessed by right heart catheterization. PH is a devastating vascular disease characterized by remodeling of pulmonary arteries, elevated pulmonary artery pressure, and subsequent development of right heart failure. Pulmonary arterial hypertension (PAH; World Health Organization Group 1) represents a specific subset of this disease that is focused on the lung vasculature, the most common types of PAH are idiopathic PAH and PAH associated with connective tissue disease [1]. Without effective treatment, PAH results in high morbidity and mortality [2], and early and accurate diagnosis of PAH is critical to patient prognosis. The development of comprehensive mechanistic theories for PAH may improve our understanding of the disease and facilitate the development and translation of effective therapies and biomarkers.
The gold standard approach to confirm PAH is right heart catheterization, but this is an invasive test that is not easily accepted by patients, so the development of biomarkers is an ongoing quest to improve outcomes. Researchers determined that none of the blood biomarkers identified in149 articles provide enough accuracy to replace current diagnostic approaches, either due to a lack of data or a lack of specificity [3]. To move closer towards precision medicine for PAH, there is an urgent need to identify novel biomarkers with high value. Increasing evidence has shown that a multiple-biomarker approach could be superior to using a single biomarker.
Recently, the metabolic theory of PAH has emerged, which facilitates the identification of several key metabolic targets that are directly involved in PAH pathogenesis and can form the basis of biomarker and drug discovery programs [4]. Metabolic changes occur in PAH pulmonary arteries, including abnormalities in glycolysis and glucose oxidation, fatty acid oxidation, glutaminolysis, arginine metabolism, one-carbon metabolism, and the tricarboxylic acid cycle; PAH-associated nuclear and mitochondrial mutations can also affect metabolism [5, 6]. Copper metabolism has also become an emerging metabolic research direction. Copper is one of the most abundant basic transition metals in the human body; both excess copper levels and copper deficiency can be harmful, and careful homeostatic control via copper metabolism is important [7]. In addition, recent exciting work has implicated copper-handling and copper-utilizing proteins in controlling the striking metabolic changes that occur in proliferating cells [8], indicating a potential role of copper metabolism in PAH pathogenesis. It was indeed proven that copper could be a biomarker for PAH [9]. Copper also plays a significant role in the control of endothelial cell proliferation in PAH [10], but the mechanisms and genes related to copper metabolism that are involved in PAH development are still not clear. Copper participates in PAH development, but the role of specific genes related to copper metabolism in pathogenesis of PAH remain to be determined, which would help to identify potential treatment targets and biomarkers.
Based on this rationale, in this study, PAH-related datasets were downloaded from the GEO database, and copper metabolism-related genes were obtained from the GeneCards database. Bioinformatics analysis methods such as limma, weighted gene coexpression network analysis (WGCNA), support vector machine (SVM), least absolute shrinkage and selection operator (LASSO) regression, and Venn diagrams were used to identify copper metabolism-related genes with diagnostic value for PAH. This study will increase our knowledge of the basic pathologic mechanisms behind vascular pulmonary disease, contribute to the early diagnosis and differentiation of PAH from other diseases and improve risk assessment before and during treatment using novel copper metabolism-related biomarkers. In the best-case scenario, the findings might even help in individualizing prevention and treatment. We present the following article in accordance with the TRIPOD reporting checklist.
Materials and methods
Data source
The PAH-related GSE33463 and GSE113439 datasets and the corresponding sample grouping information were downloaded from the GEO database (https://www.ncbi.nlm.nih.gov/geo/). Among them, the GSE33463 dataset with 71 samples (PAH: Control = 30: 41) was used as the training set, and the GSE113439 dataset with 17 samples (PAH: Control = 6: 11) was used for the validation of the diagnostic model. In addition, 2067 CMGs were obtained from the GeneCards database (https://www.genecards.org/) with "copper metabolism" as keywords.
Identification of DE-CMGs and functional enrichment analysis
The "limma" package [11] was used to perform differential analysis to obtain DEGs based on 31 PAH samples and 40 control samples from the GSE33463 dataset (|log2(fold change)(FC)|> 0.5 and p value < 0.05). Furthermore, to screen the DE-CMGs, the "ggvenn" package was used to perform Venn analysis on the DEGs and CMGs. Subsequently, Gene Ontology (GO) annotation and Kyoto Encyclopedia of Genes and Genomes (KEGG) functional enrichment of DE-CMGs were analysed by the "clusterProfiler" package [12–15], and visualized by the "ggplot2" package.
Identification of DE-CMG modules significantly associated with PAH using WGCNA
The DE-CMG expression matrices of 71 samples in GSE33463 were used as input data for WGCNA using the "WGCNA" package [16], and PAH and control were used as trait data to construct a coexpression network. First, all samples were clustered, and redundant samples were eliminated. Sample clusters and trait heatmaps were built, and the optimal soft threshold was determined. The modules were divided by the dynamic cutting tree algorithm, and the parameter minModuleSize was set to 10 to obtain the gene module. Correlation analysis was performed to determine the relationship between the modules and PAH and those modules with strong correlations were selected for subsequent analysis.
Construction and validation of diagnostic models
Based on the modules with strong correlations obtained from WGCNA, genes in the module were identified as DE-CMGs. Additionally, the roc function of the "pROC" package [17] was used to draw ROC curves based on the grouping information of the sample and the expression level of each module DE-CMG to select candidate key genes. The 41 control samples and 30 PHA samples in the GSE33463 dataset were randomly divided into training and testing sets at a ratio of 6:4. In the training set, to examine the impact of different candidate key gene combinations on the diagnostic efficiency, the possible combinations of all candidate key genes were calculated by SVM. The combination with the highest predictive rate for diagnostis (i.e., indicating the genes in the combination are biomarkers) was selected, and a model was built in the training set. The model classification ability was verified using a tenfold cross-validation method, and the sensitivity, specificity, negative predictive value, and positive predictive value of the model for predicting pulmonary hypertension were analysed. LASSO regression was also utilized to screen the candidate biomarkers based on key genes, and tenfold cross-validation was adopted to verify the model. Biomarkers were further detected by intersecting the results of SVM and LASSO regression using a Venn diagram. In addition, the predictive performance of the model was verified by ROC curves and the sensitivity and specificity of the model in the testing set and GSE113439 dataset.
GSEA of biomarkers
To explore the function of the diagnostic genes, the 30 PAH patient samples were divided into high and low expression groups according to the median expression of the diagnostic genes, and GSEA was performed on all genes. The FDR < 25% and NOM.p value < 0.05 were set as significace thresholds.
Immune cell infiltration accessment using the CIBERSORT algorithm
To investigate the immune cells infiltration in the control group and PAH group, the Cell type Identification By Estimating Relative Subsets Of RNA Transcripts (CIBERSORT) algorithm and the LM22 gene set were used to calculate the proportions of 22 immune cell types in 71 samples (Control: PAH = 41:30). The proportion of each immune cell type in each sample was calculated using the CIBERSORT algorithm, and the samples with p > 0.05 were excluded (remaining samples control: PAH = 41: 30), according to the statistical value. According to the scores of each immune cell in the two groups, a score heatmap of 22 immune cell types was drawn. The "ggplot2" package was used to draw boxplots with the Wilcoxon rank sum test method. Then, a correlation heatmap of the biomarkers and 22 immune cell types was plotted, and the two immune cell types that were most positively or negatively correlated with the biomarkers were selected for further analysis of the differences in immune cell expression and their corresponding biomarkers between the control and PAH groups.
Biomarker potential drug prediction using the DGIdb database
The DGIdb (https://dgidb.genome.wustl.edu/) database was used to predict the potential therapeutic drugs for PAH using the biomarkers, and Cytoscape software [18] was used to visualize the prediction results.
Validation of biomarker expression
To further confirm the results of the public database analysis, we collected eight control peripheral blood mononuclear cell (PBMC) samples from healthy subjects and eight PBMC samples from patients with PAH (the basic characteristics of the patients are shown in Additional file 1: Table S1) and isolated RNA for RT-qPCR. Doppler echocardiogram was performed to screen for the presence of PAH. Pulmonary artery systolic pressure (sPAP) was estimated adopting a modified Bernoulli equation [19]: sPAP = 4 x (tricuspid systolic jet)2 + 10 mmHg (estimated right atrial pressure). PAH was defined as an estimated sPAH > 35 mmHg using echocardiograms. Total RNA was separated by TRIzol (Ambion, Austin, USA) based on the manufacturer’s guidance. The inverse transcription of total RNA into cDNA was implemented using the first strand cDNA synthesis kit (Servicebio, Wuhan, China) based on the manufacturer’s instructions. Then, qPCR was carried out utilizing 2 × Universal Blue SYBR Green qPCR Master Mix (Servicebio, Wuhan, China) according to the manufacturer’s instructions. The primer sequences for PCR are listed in Table 1. Expression levels were normalized to the internal reference GAPDH and computed employing the 2−ΔΔCq formula.
Table 1.
The primer sequences for qPCR
| Primer | Sequence |
|---|---|
| DDIT3 For | TCACCACTCTTGACCCTGCTTC |
| DDIT3 Rev | TGACCACTCTGTTTCCGTTTCC |
| NFKBIA For | GAGGAGTACGAGCAGATGGTCAA |
| NFKBIA Rev | CAATTTCTGGCTGGTTGGTGAT |
| OSM For | CACAGACTGGCCGACTTAGAGC |
| OSM Rev | TGAGTGCATGAAGCGATGGTAG |
| PTGER4 For | CAGCAGTACATCTCAGACCCTCC |
| PTGER4 Rev | ACCAGCCTCATCCACCAGTAA |
| GAPDH For | CCCATCACCATCTTCCAGG |
| GAPDH Rev | CATCACGCCACAGTTTCCC |
Statistical analysis
All statistical analyses were performed using R software (version 4.0.3). The differences between the two groups were compared by the Wilcoxon test. P < 0.05 was considered statistically significant.
Results
Identification of DE-CMGs and functional enrichment analysis
A total of 814 DEGs were obtained from the PAH vs. control comparison group, including 258 up-regulated genes and 556 down-regulated genes (Fig. 1A). Moreover, 85 DE-CMGs were identified from the overlap analysis of DEGs and CMGs (Fig. 1B–C). These DE-CMGs were enriched in 445 biological process (BP) terms, 7 cellular component (CC) terms, 22 molecular function (MF) terms, and 55 KEGG signalling pathways. These DE-CMGs were primarily enriched in various inflammatory response, neuron death and apoptotic, ion binding and homeostasis, protein transport and binding GO terms, such as regulation of inflammatory response, regulation of neuron death, neuron apoptotic process, transition metal ion homeostasis and copper ion binding (Fig. 1D). The DE-CMGs were primarily enriched in various immune- and disease-related KEGG pathways, such as Th17 cell differentiation, the IL-17 signaling pathway, coronavirus disease-COVID-19, and Chagas disease (Fig. 1E).
Fig. 1.
Identification of 85 DE-CMGs and their enrichment analysis. A 814 DEGs including 258 up-regulated (red dots) and 556 down-regulated (green dots) genes from the GSE33463 dataset in the volcano map. B Venn diagram to detect 85 DE-CMGs. C Heatmap of the expression of the top 100 DEGs. D The top 27 GO terms included 10 biological process (BP) terms, 7 cellular component (CC) terms, and 10 molecular function (MF) terms of the DE-CMGs. E Top 20 KEGG pathways of the DE-CMGs
Identification of DE-CMG modules significantly associated with PAH using WGCNA
To identify the DE-CMG modules significantly associated with PAH, the WGCNA was performed. Among the 71 samples of the GSE33463 dataset, 8 outlier samples (GSM827709, GSM827715, GSM827721, GSM827734, GSM827730, GSM827723, GSM827718 and GSM827729) were eliminated (Fig. 2A–B). The optimal soft threshold was determined to be 16 (R2 = 0.86) (Fig. 2C), and 4 gene modules were screened (Fig. 2D). Among the 4 gene modules, the turquoise module had a significantly strong correlation with PAH (Fig. 2E).
Fig. 2.
Construction of WGCNA to identify DE-CMG modules in the GSE33463 dataset. A Cluster dendrogram of module eigengenes to detect outlier samples. B Dendrogram of all expressed genes in the PAH and control samples clustered based on a dissimilarity measure (1‐TOM). C Analysis of the scale-free topology fit index and the mean connectivity for various soft-threshold powers (β) for the genes. D Hierarchical clustering tree based on the topological overlap dissimilarity (1-TOM). E Heatmap of the module-trait relationships. The corresponding P values are also annotated
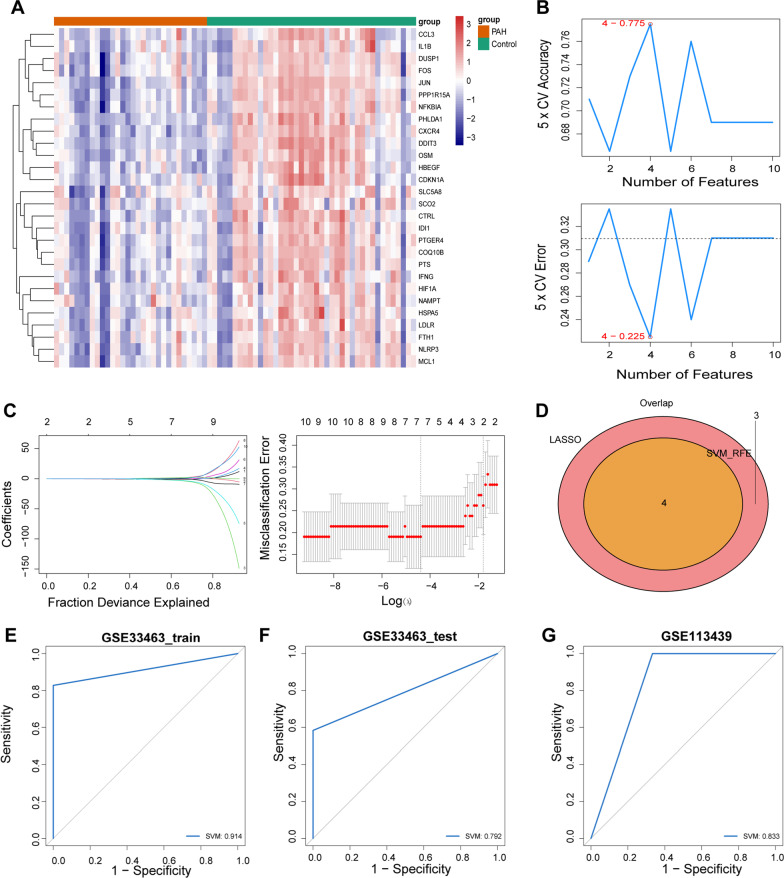
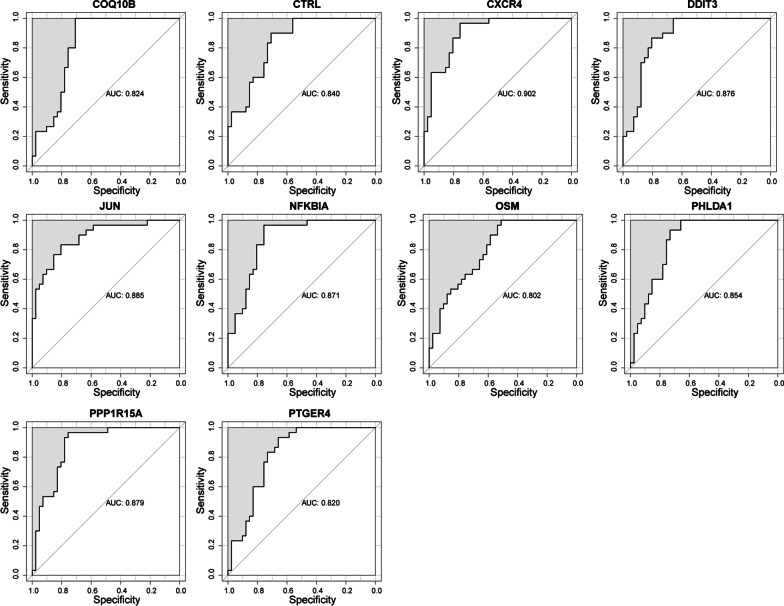
Construction of a diagnostic model based on 4 genes
A total of 28 module DE-CMGs were acquired from the WGCNA, and the expression of these genes was significantly different in the PAH and control groups (Fig. 3A). Furthermore, 10 module DE-CMGs (CXCR4, JUN, DDIT3, PPP1R15A, NFKBIA, PHLDA1, CTRL, OSM, PTGER4, and COQ10B) were screened as candidate key genes according to AUC > 0.8, and the 95% confidence intervals of 28 module DE-CMGs are shown in Additional file 2: Table S2, indicating that these 10 candidate key genes had diagnostic value (Fig. 4). The combination of 4 genes (DDIT3, NFKBIA, OSM, and PTGER4) was filtered by SVM (Fig. 3B). Seven candidate genes (CXCR4, JUN, DDIT3, NFKBIA, OSM, PTGER4, and COQ10B) were filtered using LASSO regression (Fig. 3C). By intersecting the 4 genes filtered by SVM and the 7 genes detected by LASSO regression, 4 biomarkers (DDIT3, NFKBIA, OSM, and PTGER4) for the diagnosis of PAH were identified (Fig. 3D). The combination of the 4 genes distinguished PAH well from the control (Table 2), and the AUC value was greater than 0.7 in the training set, testing set, and GSE113439 dataset respectively, indicating high predictive effectiveness of the model (Fig. 3E–G).
Fig. 3.
Identification and validation of four biomarkers. A Heatmap of the expression of 28 module DE-CMGs in PAH and control samples from the training set. B The accuracy and error of estimate generation for the SVM‐RFE algorithm in the training set. (C) Candidate genes selected by the LASSO regression model. D Four biomarkers detected by Venn diagram. ROC curves of the prognostic values of the four biomarkers in the training (E), testing (F), and GSE113439 (G) sets
Fig. 4.
Ten module DE-CMGs with AUC values > 0.8
Table 2.
Construction and validation of the predictive performance of the four-gene model
| Terms | Training dataset | Testing dataset | GSE113439 dataset | |||
|---|---|---|---|---|---|---|
| Actual disease | Actual normal | Actual disease | Actual normal | Actual disease | Actual normal | |
| Predicted disease | 13 | 5 | 17 | 5 | 4 | 0 |
| Predicted normal | 0 | 24 | 0 | 7 | 2 | 11 |
| Total | 13 | 29 | 17 | 12 | 6 | 11 |
| Correct | 13 | 24 | 17 | 7 | 4 | 11 |
| Senstivity | 100 | 100 | 67 | |||
| (%) | ||||||
| Specificity | 83 | 58 | 100 | |||
| (%) | ||||||
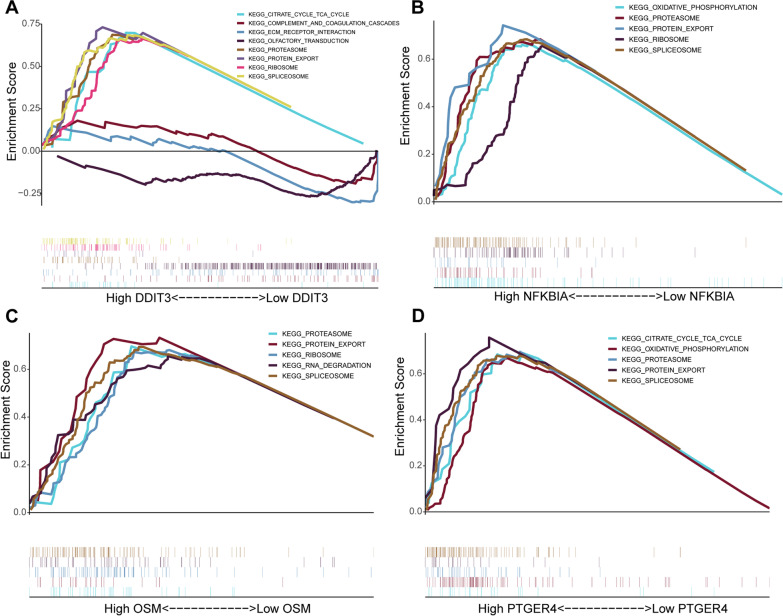
GSEA biomarker enrichment analysis
The top 5 KEGG pathways that were significantly enriched in the high and low expression groups for the 4 biomarkers are shown in Fig. 5. Protein export, spliceosome, citrate cycle TCA cycle, and proteasome were enriched in the high expression groups. In the low DDIT3 expression group, the genes were mainly enriched in the complement and coagulation cascades, ECM receptor interaction, and olfactory transduction pathways.
Fig. 5.
Top 5 KEGG pathways of the four biomarkers. Top 5 KEGG pathways of DDIT3 (A), NFKBIA (B), OSM (C), and PTGER4 (D) by GSEA enrichment
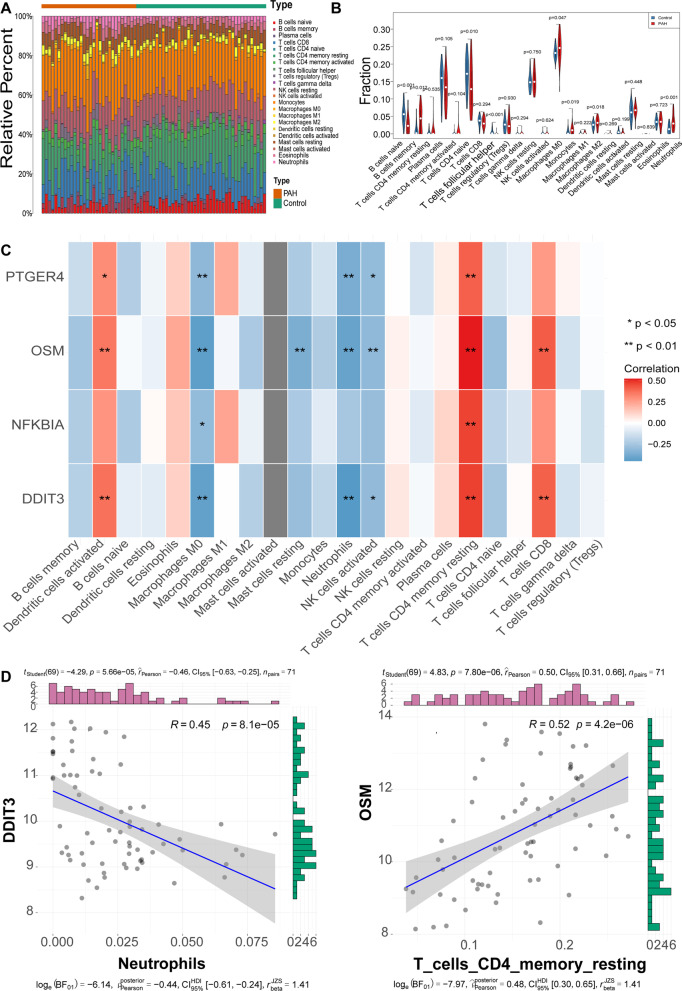
Immune cell infiltration accessment by the CIBERSORT algorithm
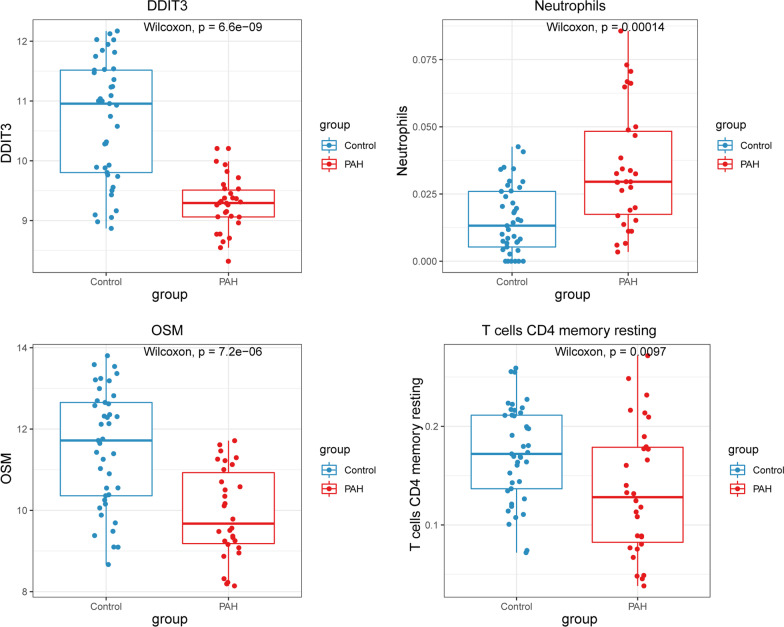
As immunity/inflammation is considered a critical pathogenesis mechanism during PAH development [20, 21]), we investigated the different immune/ inflammatory cells, and employed the CIBERSORT algorithm. Eight immune cell types were significantly different (p < 0.05) between the two groups, including naive B cells, memory B cells, resting memory CD4 T cells, follicular helpe rT cells, monocytes, M0 macrophages, M2 macrophages, and neutrophils (Fig. 6A–B). Among these immune cells, OSM had the most significant positive correlation with resting memory CD4 T cells, and DDIT3 had the most significant negative correlation with neutropils (Fig. 6C–D). Moreover, the expressions levels of OSM and DDIT3, and the abundance of resting memory CD4 T cells and neutropils were significantly different between the PAH and control samples (Fig. 7).
Fig. 6.
Evaluation of immune cell infiltration using the CIBERSORT algorithm. A A stacked bar plot of the proportions of 22 immune cell types in control and PAH samples from the training based on the CIBERSORT algorithm. B Vioplot of 22 immune cell contents in the control and PAH samples from the training set. C Correlations between the 4 biomarkers and 22 immune cell types. D Correlation analysis between the expression level of DDIT3 and abundance of neutrophils (left), and the expression level of OSM and abundance of resting memory CD4 T cells (right) in the training set
Fig. 7.
Wilcoxon’s test. Wilcoxon’s test of the expression of OSM and DDIT3, and the abundance of memory-resting CD4 T cells and neutrophils between the PAH and control samples
Use of biomarkers for potential drug prediction using the DGIdb database
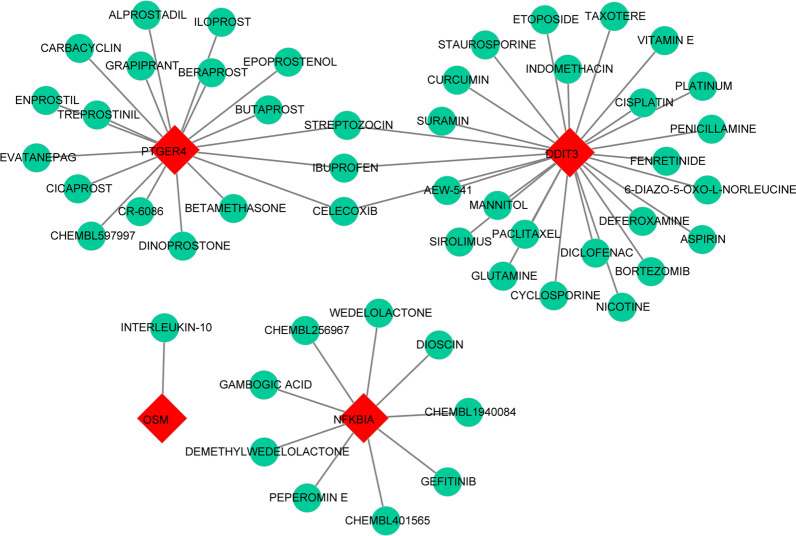
A gene-drug network was constructed and is displayed in Fig. 8. It was found that 27 drugs were predicted by DDIT3, 9 drugs were predicted by NFKBIA, 1 drug was predicted by OSM, and 21 drugs were predicted by PTGER4. Moreover, the network also suggested that STREPTOZOCIN, IBUPROFEN, and CELECOXIB were shared by PTGER4 and DDIT3.
Fig. 8.
Drug–gene interaction diagram. The red square indicates the four biomarkers, and the green circle indicates the drugs
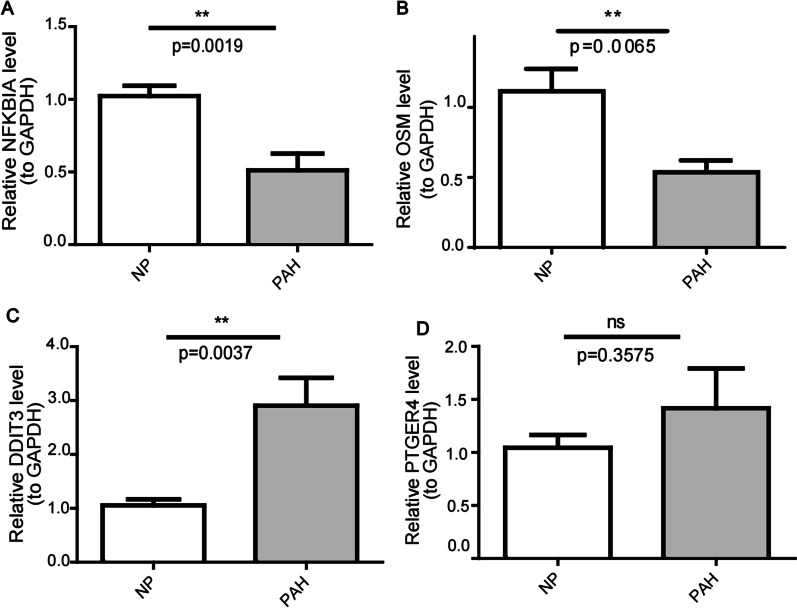
Verification of biomarker expression in clinical samples
As illustrated in Fig. 3A, expression of DDIT3, NFKBIA, OSM, and PTGER4 was reduced in the PAH samples compared with control samples. We then further confirmed the expression in clinical samples (eight control samples and eight PAH samples) by RT-qPCR. In agreement with the results of the public database data analysis, NFKBIA and OSM were markedly down-regulated in clinical PAH samples versus control samples (Fig. 9). However, the trends in DDIT3 and PTGER4 expression were not consistent with the public database results, probably due to sample heterogeneity or limited sample size (Fig. 9).
Fig. 9.
The expression of biomarkers (NFKBIA (A), OSM (B), DDIT3 (C), and PTGER4 (D)) in clinical PBMC samples detected by RT-qPCR. NP indicates normal peopole. **p value < 0.01
Discussion
As early as the 1980s, researchers found that increased serum copper may be a cause or a marker of PAH [22], and intravenous infusion of copper sulfate significantly increased pulmonary vascular resistance. [23], indicating an important role of copper during PAH development. It is critical for organisms to maintain homeostatic concentrations of copper. In recent years, copper metabolism has emerged as an important metabolic research direction for PAH. However, the mechanism underlying the effects of copper and changes in copper metabolism in PAH remain to be studied. To overcome these problems, this study screened differentially expressed copper metabolism-related genes. Four-gene-based models were constructed, and DDIT3, NFKBIA, OSM, and PTGER4 had improved diagnostic value in identifying PAH compared with normal controls, and thus had potential to be biomarkers for PAH. The immune infiltration profiles of PAH and normal controls were significantly different. High proportions of memory B cells, monocytes, M0 macrophages, M2 macrophages, and neutrophils were found in PAH, while high proportions of resting memory CD4 T cells, naïve B cells, and follicular helper T cells were found in normal controls. OSM was most positively correlated with resting memory CD4 T cells, and DDIT3 was most negatively correlated with neutrophils; Drugs were predicted by targeting the 4 biomarkers, and STREPTOZOCIN, IBUPROFEN, and CELECOXIB were shared by PTGER4 and DDIT3.
The copper metabolism-related genes DDIT3, NFKBIA, OSM, and PTGER4 were downregulated in PAH, as identified by WGCNA and SVM. Copper could cause increased expression of DDIT3 [24], DDIT3, as an oncogene [25], has been reported to promote vascular remodeling in MCT-induced PH [26], but its expression and role in PAH have not been studied. In this study, DDIT3 was upregulated in the validated cohort of PAH patients, which is not consistant with our predicted results and requires further studies to understand the possible pathogenic mechanisms as a controversial point. NFKBIA, OSM, and PTGER4, which were predicted to be downregulated in PAH by bioinformatics analysis in the present study have not yet been reported in PAH. The prediction results of NFKBIA and OSM are consistent with the validated results, while the expression of PTGER4 was not significantly changed in the validated cohort of PAH patients. Our study indeed provides new research directions for PAH. Usually, NFKBIA functions as a tumour suppressor and has the potential to be introduced as a novel anti-tumour agent [27, 28], whether it can reverse pulmonary vascular remodeling in PAH is not yet clear. It is known that nuclear factor-κB (NF-κB) plays an important role in PAH [29], which could be regulated by copper [30, 31]. Inhibition of NF-κB, prevents MCT-PH in mice [32]. NFKBIA serves as an inhibitor [33, 34] in regulating NF-κB and is reported to suppress the epithelial-mesenchymal transition (EMT), cell migration, proliferation and invasion [27]. Our results indicated an important role of NFKBIA in PAH development, which provides a new research direction for PAH that needs to be clarified further. OSM, a member of the interleukin 6 cytokine family, can suppress fibroblast activation to prevent cardiac fibrosis by inhibiting the SMAD signaling pathway [35]. OSM treatment preserved cardiac function and inhibited apoptosis and fibrosis after myocardial infarction [36]. In addition, OSM protected against cardiac I/R injury by regulating apoptosis, insulin sensitivity and mitochondrial biogenesis in diabetic mice [37]. Some studies have reported that OSM activates endothelial cells [38] and smooth muscle cells [39], but to date, the role of OSM in PAH and the underlying mechanisms remain to be studied. There is an imbalance between vasodilation and vasoconstriction favouring vasoconstriction with an increase in circulating vasoconstrictors and a decrease in circulating vasodilators (i.e., prostacyclin and prostaglandin) during PAH development. Therefore, prostacyclin and prostaglandin analogs are crucial treatments for PAH [40]. The prostaglandin receptor PTGER4 agonist could attenuate PAH by activating PPARγ [41] and suppressing EndMT [42]. The PAH pharmacotherapies beraprost and iloprost can bind to PTGER4 to mediate vasodilatory functions [43, 44]. A previous study showed that although the prostacyclin receptor was downregulated, PTGER4 had a stable expression [44], which is consistent with our validated results. Studies have also shown increased PTGER4 expression in pulmonary artery aneurysm with dissection in a patient with PAH [45]. However, in this study, we predicted that PTGER4 was downregulated in PAH. Thus, the expression pattern of PTGER4 in different subgroups of PAH need to be researched further.
GSEA enrichment analyses demonstrated key pathways involved in PAH, indicating that the citrate cycle (TCA cycle) participates in PAH development. This finding is consistent with previous studies, and abnormal TCA cycle flux occurrs in PAH [46]. Additional studies should focus on metabolic dysregulation in PAH to offer powerful therapeutic means to prevent or even reverse disease progression at the molecular level.
Immune cells play an indispensable role in the process of pulmonary hypertension vessel remodeling [47]. Therefore, attention should be given to the mechanism of immune cell infiltration in patients with PAH. We found that memory B cells, monocytes, M0 macrophages, M2 macrophages and neutrophils were increased in PAH, while resting CD4 memory T cells, naïve B cells and follicular helper T cells were decreased. A previous study reported that B lymphocytes are involved in vessel biology, vasomotor regulation, angiogenesis and cell proliferation [48]. Macrophages can cause vasoconstriction, increase vascular permeability, and induce proliferation [20]. Different subsets of CD4 + T cells play different roles in PAH, including small pulmonary artery muscularization, initiation and maintenance of inflammation, promotion of vascular remodeling, suppression of vascular inflammation, and limitation of the propagation of vascular injury [49]. Our previous study demonstrated the crucial role of interleukin 17–producing CD4+ effector T cells in hypoxia-induced PH [50], while CD4+ regulatory T cells showed a protective role against PAH [51]. Myeloid cells, specifically nonclassical monocyte lineage cells promote vascular remodeling [52]. It is not yet fully elucidated how these immune cells alterations are involved in PAH, and the molecular mechanisms involved in their activation remain unknown. Our results showed that OSM was most positively correlated with resting memory CD4 T cells, and DDIT3 was most negatively correlated with neutropils, laying the foundation for studying the immune mechanisms of PAH. The possible interaction mechanisms need to be clarified further.
Current PAH treatments generally target vasoconstriction by three different modalities: nitric oxide → soluble guanylate cyclase → cGMP levels, and the endothelin and prostacyclin pathways [53]. The treatment strategy for PAH has thereby changed significantly over the past decade, combination therapy has progressively become the gold standard of care in patients with PAH and is becoming widely used in clinical practice [54]. In this study, we identified 4 hub copper metabolism-related genes and constructed a gene-drug network to obtain agonists and antagonists of these molecules. The results provide a reference for clinicians to decide which drugs should be used in combination with current targeted drugs to improve patient prognosis and which drugs should be used with caution to prevent the clinical deterioration of PAH. The gene-drug network in this study illustrated that STREPTOZOCIN, IBUPROFEN, and CELECOXIB were shared by PTGER4 and DDIT3. Among them, IBUPROFEN and CELECOXIB are non-steroidal anti-inflammatory drugs (NSAIDs) that are commonly used in the clinic, and it has been reported that NSAIDs consumption during pregnancy contributes to an increased risk of persistent pulmonary hypertension of the newborns [55, 56]. Physicians should be alert to the potential dangers of these drugs to PAH patients.
This study uncovers a link between copper metabolism-related genes and pulmonary hypertension, highlighting several potential biomarkers. These biomarkers have the potential to be used as a routine diagnostic strategy and in the evaluation of PAH patients. Copper metabolism has potential as a new diagnostic biomarker as well as a targeted therapy for PAH, while the underlying mechanisms need to be clarified further in future studies.
Conclusions
In summary, this study identified four copper metabolism-related biomarkers (DDIT3, NFKBIA, OSM, and PTGER4) with considerable diagnostic values based on bioinformatics analyses, and further constructed a gene-drug network. The results of this study may have significant implications for the development of new diagnostic biomarkers and actionable targets to expand treatment options for PAH patients.
Supplementary Information
Additional file 1. Supplementary Table 1. Basic characteristics of the CTD-PH patients and the healthy subjects.
Additional file 2. Supplementary Table 2. The ROC values and 95% confidence intervals of 28 module DE-CMGs.
Acknowledgements
We appreciate the GEO database and the GeneCards database for providing their platforms and their contributors for uploading meaningful datasets.
Abbreviations
- PAH
Pulmonary arterial hypertension
- GEO
The Gene Expression Omnibus
- CMGs
Copper metabolism-related genes
- DE-CMGs
Differentially expressed copper metabolism-related genes
- DEGs
Differentially expressed genes
- ROC
Receiver operating characteristic
- AUC
The area under the curve
- SVM
Support vector machine
- LASSO
The least absolute shrinkage and selection operator
- GSEA
Gene set enrichment Analysis
- DGIdb
Drug-Gene Interaction Database
- RT-qPCR
Real-time quantitative PCR
- PH
Pulmonary hypertension
- WGCNA
Weighted gene co-expression network analysis
- CIBERSORT
Cell type identification by estimating relative subsets of RNA transcripts
- PBMC
Peripheral blood mononuclear cell
- GO
Gene Ontology
- BP
Biological process
- CC
Cellular components
- MF
Molecular functions
- KEGG
Kyoto Encyclopedia of Genes and Genomes
- FC
Fold change
- NF-κB
Nuclear factor-κB
- EMT
Epithelial-mesenchymal transition
Author contributions
LW, CX, and JH conceptualized and designed this research; LW, LC, ZW and JH collected and analysed the data; LW wrote the paper. All authors reviewed the manuscript.
Funding
This work was supported by Fundamental Research Funds for the Central Universities (Grant Number xzy012020060), Chinese Postdoctoral Science Foundation (Grant Number 2021M702610), the Natural Science Foundation of Shaanxi Province (Grant Number 2022JQ-940), and National Natural Science Foundation of China (Grant Number 82270055).
Availability of data and materials
The data analysed during this study are available in the GEO database (https://www.ncbi.nlm.nih.gov/geo/; GSE33463 and GSE113439) and the GeneCards database (https://www.genecards.org/).
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Xi’an Jiaotong University (Approval No. 2022‑1026) and was performed in accordance with the Declaration of Helsinki. The study protocol and data collection instruments were submitted and approved by the Data Protection Commission of Xi’an Jiaotong University. All patients provided written informed consent prior to inclusion in the study.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant interests of financial or non-financial interests to declared.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xin Chen, Email: chen_x129@163.com.
Jing Huang, Email: 522181462@qq.com.
References
- 1.Vonk Noordegraaf A, Groeneveldt JA, Bogaard HJ. Pulmonary hypertension. Eur Respir Rev. 2016;25(139):4–11. doi: 10.1183/16000617.0096-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hassoun PM. Pulmonary arterial hypertension. N Engl J Med. 2021;385(25):2361–2376. doi: 10.1056/NEJMra2000348. [DOI] [PubMed] [Google Scholar]
- 3.Smits AJ, Botros L, Mol MAE, Ziesemer KA, Wilkins MR, Vonk Noordegraaf A, Bogaard HJ, Aman J. A systematic review with meta-analysis of biomarkers for detection of pulmonary arterial hypertension. ERJ Open Res. 2022 doi: 10.1183/23120541.00009-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sutendra G, Michelakis ED. The metabolic basis of pulmonary arterial hypertension. Cell Metab. 2014;19(4):558–573. doi: 10.1016/j.cmet.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Xu W, Janocha AJ, Erzurum SC. Metabolism in pulmonary hypertension. Annu Rev Physiol. 2021;83:551–576. doi: 10.1146/annurev-physiol-031620-123956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryan JJ, Archer SL. Emerging concepts in the molecular basis of pulmonary arterial hypertension: part I: metabolic plasticity and mitochondrial dynamics in the pulmonary circulation and right ventricle in pulmonary arterial hypertension. Circulation. 2015;131(19):1691–1702. doi: 10.1161/CIRCULATIONAHA.114.006979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kardos J, Heja L, Simon A, Jablonkai I, Kovacs R, Jemnitz K. Copper signalling: causes and consequences. Cell Commun Signal. 2018;16(1):71. doi: 10.1186/s12964-018-0277-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turski ML, Thiele DJ. New roles for copper metabolism in cell proliferation, signaling, and disease. J Biol Chem. 2009;284(2):717–721. doi: 10.1074/jbc.R800055200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun Q, Hackler J, Hilger J, Gluschke H, Muric A, Simmons S, Schomburg L, Siegert E. Selenium and copper as biomarkers for pulmonary arterial hypertension in systemic sclerosis. Nutrients. 2020;12(6):1894. doi: 10.3390/nu12061894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bogaard HJ, Mizuno S, Guignabert C, Al Hussaini AA, Farkas D, Ruiter G, Kraskauskas D, Fadel E, Allegood JC, Humbert M, et al. Copper dependence of angioproliferation in pulmonary arterial hypertension in rats and humans. Am J Respir Cell Mol Biol. 2012;46(5):582–591. doi: 10.1165/rcmb.2011-0296OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ritchie ME, Phipson B, Wu D, Hu Y, Law CW, Shi W, Smyth GK. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43(7):e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu G, Wang LG, Han Y, He QY. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS. 2012;16(5):284–287. doi: 10.1089/omi.2011.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanehisa M. Toward understanding the origin and evolution of cellular organisms. Protein Sci. 2019;28:1947–1951. doi: 10.1002/pro.3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanehisa M, Furumichi M, Sato Y, Ishiguro-Watanabe M, Tanabe M. KEGG: integrating viruses and cellular organisms. Nucleic Acids Res. 2021;49:D545–D551. doi: 10.1093/nar/gkaa970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinform. 2008;9:559. doi: 10.1186/1471-2105-9-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, Muller M. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 2011;12:77. doi: 10.1186/1471-2105-12-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, Amin N, Schwikowski B, Ideker T. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13(11):2498–2504. doi: 10.1101/gr.1239303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pyxaras SA, Pinamonti B, Barbati G, Santangelo S, Valentincic M, Cettolo F, Secoli G, Magnani S, Merlo M, Lo Giudice F, et al. Echocardiographic evaluation of systolic and mean pulmonary artery pressure in the follow-up of patients with pulmonary hypertension. Eur J Echocardiogr. 2011;12(9):696–701. doi: 10.1093/ejechocard/jer127. [DOI] [PubMed] [Google Scholar]
- 20.Hu Y, Chi L, Kuebler WM, Goldenberg NM. Perivascular inflammation in pulmonary arterial hypertension. Cells. 2020;9(11):2338. doi: 10.3390/cells9112338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liang S, Desai AA, Black SM, Tang H. Cytokines, chemokines, and inflammation in pulmonary arterial hypertension. Adv Exp Med Biol. 2021;1303:275–303. doi: 10.1007/978-3-030-63046-1_15. [DOI] [PubMed] [Google Scholar]
- 22.Ahmed T, Sackner MA. Increased serum copper in primary pulmonary hypertension: a possible pathogenic link? Respiration. 1985;47(4):243–246. doi: 10.1159/000194778. [DOI] [PubMed] [Google Scholar]
- 23.Ahmed T, Januszkiewicz A, Eyre P, Robinson MJ, Sackner MA. Acute pulmonary hemodynamic effects of intravenous copper sulfate: role of alpha-adrenergic system. J Appl Physiol Respir Environ Exerc Physiol. 1981;51(5):1204–1213. doi: 10.1152/jappl.1981.51.5.1204. [DOI] [PubMed] [Google Scholar]
- 24.Song MO, Li J, Freedman JH. Physiological and toxicological transcriptome changes in HepG2 cells exposed to copper. Physiol Genomics. 2009;38(3):386–401. doi: 10.1152/physiolgenomics.00083.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin H, Liu S, Gao W, Liu H. DDIT3 modulates cancer stemness in gastric cancer by directly regulating CEBPbeta. J Pharm Pharmacol. 2020;72(6):807–815. doi: 10.1111/jphp.13243. [DOI] [PubMed] [Google Scholar]
- 26.Jiang H, Ding D, He Y, Li X, Xu Y, Liu X. Xbp1s-Ddit3 promotes MCT-induced pulmonary hypertension. Clin Sci (Lond) 2021;135(21):2467–2481. doi: 10.1042/CS20210612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen M, Liang X, Liang Z, Zhao L. Study on the effect and mechanism of NFKBIA on cervical cancer progress in vitro and in vivo. J Obstet Gynaecol Res. 2021;47(11):3931–3942. doi: 10.1111/jog.14947. [DOI] [PubMed] [Google Scholar]
- 28.Umar M, Upadhyay R, Kumar S, Ghoshal UC, Mittal B. Association of common polymorphisms in TNFA, NFkB1 and NFKBIA with risk and prognosis of esophageal squamous cell carcinoma. PLoS ONE. 2013;8(12):e81999. doi: 10.1371/journal.pone.0081999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Price LC, Caramori G, Perros F, Meng C, Gambaryan N, Dorfmuller P, Montani D, Casolari P, Zhu J, Dimopoulos K, et al. Nuclear factor kappa-B is activated in the pulmonary vessels of patients with end-stage idiopathic pulmonary arterial hypertension. PLoS ONE. 2013;8(10):e75415. doi: 10.1371/journal.pone.0075415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kenneth NS, Hucks GE, Jr, Kocab AJ, McCollom AL, Duckett CS. Copper is a potent inhibitor of both the canonical and non-canonical NFkappaB pathways. Cell Cycle. 2014;13(6):1006–1014. doi: 10.4161/cc.27922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pan Q, Bao LW, Merajver SD. Tetrathiomolybdate inhibits angiogenesis and metastasis through suppression of the NFkappaB signaling cascade. Mol Cancer Res. 2003;1(10):701–706. [PubMed] [Google Scholar]
- 32.Li L, Wei C, Kim IK, Janssen-Heininger Y, Gupta S. Inhibition of nuclear factor-kappaB in the lungs prevents monocrotaline-induced pulmonary hypertension in mice. Hypertension. 2014;63(6):1260–1269. doi: 10.1161/HYPERTENSIONAHA.114.03220. [DOI] [PubMed] [Google Scholar]
- 33.Sogkas G, Adriawan IR, Ringshausen FC, Baumann U, Schroder C, Klemann C, von Hardenberg S, Schmidt G, Bernd A, Jablonka A, et al. A novel NFKBIA variant substituting serine 36 of IkappaBalpha causes immunodeficiency with warts, bronchiectasis and juvenile rheumatoid arthritis in the absence of ectodermal dysplasia. Clin Immunol. 2020;210:108269. doi: 10.1016/j.clim.2019.108269. [DOI] [PubMed] [Google Scholar]
- 34.Li L, Zhang ZT. Genetic association between NFKBIA and NFKB1 gene polymorphisms and the susceptibility to head and neck cancer: a meta-analysis. Dis Markers. 2019;2019:6523837. doi: 10.1155/2019/6523837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abe H, Takeda N, Isagawa T, Semba H, Nishimura S, Morioka MS, Nakagama Y, Sato T, Soma K, Koyama K, et al. Macrophage hypoxia signaling regulates cardiac fibrosis via Oncostatin M. Nat Commun. 2019;10(1):2824. doi: 10.1038/s41467-019-10859-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang X, Zhu D, Wei L, Zhao Z, Qi X, Li Z, Sun D. OSM enhances angiogenesis and improves cardiac function after myocardial infarction. Biomed Res Int. 2015;2015:317905. doi: 10.1155/2015/317905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun D, Li S, Wu H, Zhang M, Zhang X, Wei L, Qin X, Gao E. Oncostatin M (OSM) protects against cardiac ischaemia/reperfusion injury in diabetic mice by regulating apoptosis, mitochondrial biogenesis and insulin sensitivity. J Cell Mol Med. 2015;19(6):1296–1307. doi: 10.1111/jcmm.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marden G, Wan Q, Wilks J, Nevin K, Feeney M, Wisniacki N, Trojanowski M, Bujor A, Stawski L, Trojanowska M. The role of the oncostatin M/OSM receptor beta axis in activating dermal microvascular endothelial cells in systemic sclerosis. Arthritis Res Ther. 2020;22(1):179. doi: 10.1186/s13075-020-02266-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Demyanets S, Kaun C, Rychli K, Pfaffenberger S, Kastl SP, Hohensinner PJ, Rega G, Katsaros KM, Afonyushkin T, Bochkov VN, et al. Oncostatin M-enhanced vascular endothelial growth factor expression in human vascular smooth muscle cells involves PI3K-, p38 MAPK-, Erk1/2- and STAT1/STAT3-dependent pathways and is attenuated by interferon-gamma. Basic Res Cardiol. 2011;106(2):217–231. doi: 10.1007/s00395-010-0141-0. [DOI] [PubMed] [Google Scholar]
- 40.Safdar Z. Treatment of pulmonary arterial hypertension: the role of prostacyclin and prostaglandin analogs. Respir Med. 2011;105(6):818–827. doi: 10.1016/j.rmed.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 41.Li HH, Hsu HH, Chang GJ, Chen IC, Ho WJ, Hsu PC, Chen WJ, Pang JS, Huang CC, Lai YJ. Prostanoid EP4 agonist L-902,688 activates PPARgamma and attenuates pulmonary arterial hypertension. Am J Physiol Lung Cell Mol Physiol. 2018;314(3):L349–L359. doi: 10.1152/ajplung.00245.2017. [DOI] [PubMed] [Google Scholar]
- 42.Lai YJ, Chen IC, Li HH, Huang CC. EP4 agonist L-902,688 suppresses EndMT and attenuates right ventricular cardiac fibrosis in experimental pulmonary arterial hypertension. Int J Mol Sci. 2018;19(3):727. doi: 10.3390/ijms19030727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tian H, Fan F, Geng J, Deng J, Tian H. Beraprost upregulates KV channel expression and function via ep4 receptor in pulmonary artery smooth muscle cells obtained from rats with hypoxia-induced pulmonary hypertension. J Vasc Res. 2019;56(4):204–214. doi: 10.1159/000500424. [DOI] [PubMed] [Google Scholar]
- 44.Lai YJ, Pullamsetti SS, Dony E, Weissmann N, Butrous G, Banat GA, Ghofrani HA, Seeger W, Grimminger F, Schermuly RT. Role of the prostanoid EP4 receptor in iloprost-mediated vasodilatation in pulmonary hypertension. Am J Respir Crit Care Med. 2008;178(2):188–196. doi: 10.1164/rccm.200710-1519OC. [DOI] [PubMed] [Google Scholar]
- 45.Akagi S, Nakamura K, Yokoyama U, Kasahara S, Sarashina T, Ejiri K, Ito H. Enhanced EP4 expression in a pulmonary artery aneurysm with dissection in a patient with pulmonary arterial hypertension. Circ Cardiovasc Imaging. 2017;10(2):e005839. doi: 10.1161/CIRCIMAGING.116.005839. [DOI] [PubMed] [Google Scholar]
- 46.Xu W, Comhair SAA, Chen R, Hu B, Hou Y, Zhou Y, Mavrakis LA, Janocha AJ, Li L, Zhang D, et al. Integrative proteomics and phosphoproteomics in pulmonary arterial hypertension. Sci Rep. 2019;9(1):18623. doi: 10.1038/s41598-019-55053-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rabinovitch M, Guignabert C, Humbert M, Nicolls MR. Inflammation and immunity in the pathogenesis of pulmonary arterial hypertension. Circ Res. 2014;115(1):165–175. doi: 10.1161/CIRCRESAHA.113.301141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Graver JC, Boots AMH, Haacke EA, Diepstra A, Brouwer E, Sandovici M. Massive B-cell infiltration and organization Into artery tertiary lymphoid organs in the aorta of large vessel giant cell arteritis. Front Immunol. 2019;10:83. doi: 10.3389/fimmu.2019.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li C, Liu P, Song R, Zhang Y, Lei S, Wu S. Immune cells and autoantibodies in pulmonary arterial hypertension. Acta Biochim Biophys Sin (Shanghai) 2017;49(12):1047–1057. doi: 10.1093/abbs/gmx095. [DOI] [PubMed] [Google Scholar]
- 50.Wang L, Liu J, Wang W, Qi X, Wang Y, Tian B, Dai H, Wang J, Ning W, Yang T, et al. Targeting IL-17 attenuates hypoxia-induced pulmonary hypertension through downregulation of beta-catenin. Thorax. 2019;74(6):564–578. doi: 10.1136/thoraxjnl-2018-211846. [DOI] [PubMed] [Google Scholar]
- 51.Tian W, Jiang SY, Jiang X, Tamosiuniene R, Kim D, Guan T, Arsalane S, Pasupneti S, Voelkel NF, Tang Q, et al. The role of regulatory T cells in pulmonary arterial hypertension. Front Immunol. 2021;12:684657. doi: 10.3389/fimmu.2021.684657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yu YA, Malakhau Y, Yu CA, Phelan SJ, Cumming RI, Kan MJ, Mao L, Rajagopal S, Piantadosi CA, Gunn MD. Nonclassical monocytes sense hypoxia, regulate pulmonary vascular remodeling, and promote pulmonary hypertension. J Immunol. 2020;204(6):1474–1485. doi: 10.4049/jimmunol.1900239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bisserier M, Pradhan N, Hadri L. Current and emerging therapeutic approaches to pulmonary hypertension. Rev Cardiovasc Med. 2020;21(2):163–179. doi: 10.31083/j.rcm.2020.02.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Burks M, Stickel S, Galie N. Pulmonary arterial hypertension: combination therapy in practice. Am J Cardiovasc Drugs. 2018;18(4):249–257. doi: 10.1007/s40256-018-0272-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Van Marter LJ, Leviton A, Allred EN, Pagano M, Sullivan KF, Cohen A, Epstein MF. Persistent pulmonary hypertension of the newborn and smoking and aspirin and nonsteroidal antiinflammatory drug consumption during pregnancy. Pediatrics. 1996;97(5):658–663. doi: 10.1542/peds.97.5.658. [DOI] [PubMed] [Google Scholar]
- 56.Alano MA, Ngougmna E, Ostrea EM, Jr, Konduri GG. Analysis of nonsteroidal antiinflammatory drugs in meconium and its relation to persistent pulmonary hypertension of the newborn. Pediatrics. 2001;107(3):519–523. doi: 10.1542/peds.107.3.519. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary Table 1. Basic characteristics of the CTD-PH patients and the healthy subjects.
Additional file 2. Supplementary Table 2. The ROC values and 95% confidence intervals of 28 module DE-CMGs.
Data Availability Statement
The data analysed during this study are available in the GEO database (https://www.ncbi.nlm.nih.gov/geo/; GSE33463 and GSE113439) and the GeneCards database (https://www.genecards.org/).