Abstract
Acute hypoglycemia may mimic acute ischemic stroke, but to our knowledge this has never been reported as transient hemineglect syndrome. We present a 60-year-old male with known diabetes mellitus who was brought to the hospital as a stroke alert. The patient had undetectable glucose levels upon arrival of emergency medical services (EMS), therefore hypertonic glucose was given. On our assessment in the emergency department (ED)he turned his head to the right side, looking to the right to answer questions when addressed on his left side. The extinction and neglect assessment revealed left-sided extinction on double tactile and visual stimulation. CT perfusion of the brain showed a decreased perfusion in the right cortical area. Given the unclear last known normal, urgent brain magnetic resonance imaging (MRI) was performed; stroke was excluded. The patient was admitted to the Intensive Care Unit where glucose was closely monitored. Electroencephalogram showed absence of seizure or postictal activity. The following morning, the patient returned to baseline and was able to recall the event. The episode was attributed to the severe hypoglycemia because of a recent medication change.
Keywords: Hypoglycemia, Stroke mimic, Hemineglect
Highlights
-
•
Hypoglycemia should be included in the differential diagnosis for acute neurological impairment including hemineglect.
-
•
Abnormal brain imaging can be present. It should also be emphasized that focal neurological deficits from hypoglycemia may not have an immediate resolution after correcting the glucose level.
-
•
Different brain regions have different metabolic requirements and the highest demand for glucose occurs in the cerebral cortex and basal ganglia. Focal deficits may result from the asymmetric distribution of glucose transporters. Severe episodes of hypoglycemia are more likely to cause hemiparesis and are more likely to mimic ischemic stroke.
-
•
Spatial neglect does not necessarily limit disability to sensory and motor impairment. It can cause other neurologic components like perceptual, representational, visuospatial, and behavioral deficits.
1. Introduction
The phenomena of hemineglect in which a patient becomes unaware of one side of their personal space has fascinated neurologists over the past century. Joseph Babinski coined the term anosognosia to describe the neglect several of his patients exhibited in which they were unaware of significant hemiplegia following stroke. Perceptual neurologists including Walter Russel Brain, Morris B. Bender, and Macdonald Critchley furthered our understanding of right parietal neural networks as they affected perception and emotional awareness [1]. The right posterior parietal cortex, particularly the inferior parietal lobe (IPL) or temporoparietal junction (TPJ), are the most common locations affected in hemineglect. The right hemisphere is the dominant hemisphere for attention while the left is dominant for language [2]. The late and beloved Oliver Sacks in his widely read book “The Man Who Mistook His Wife for a Hat”, described a case of a woman with prominent left side neglect following a right parietal stroke, who would put makeup only on the right-half of her face, and brush hair only on the right side [3]. Right MCA stroke involving the parietal lobe is the most common cause for this syndrome. Parietal lobe brain tumor will often cause neglect to develop insidiously. Traumatic brain injury, and localized seizure activity, particularly non-convulsive status, can cause hemineglect. Degenerative brain disease such as Alzheimer's disease and frontotemporal dementia, and toxic metabolic disturbances have not been associated with the syndrome of neglect [4].
We describe a 60-year-old man who presented with a sudden right hemispheric syndrome with profound left hemineglect due to hypoglycemia. Hypoglycemia is a prevalent complication of anti-glycemic medications in patients with diabetes, especially following adjustment of medication dosage, change in caloric intake, or significant weight loss [5]. Severe hypoglycemia is known to cause a “stroke mimic” with focal neurological signs such as hemiparesis and aphasia. Our patient had prior hypoglycemic events, but no focal neurologic deficits associated with those events. We did not find any reports of hypoglycemia presenting as a hemineglect syndrome.
The syndrome of hemineglect, or spatial neglect, is a common and disabling condition following brain injury. Patients are spatially unaware and display decreased attention to items on one side of the body or environment. Hemineglect syndrome classically presents as non-dominant (often left-sided) spatial disorientation after a right hemisphere stroke syndrome [2].
Spatial neglect does not necessarily limit disability to sensory and motor impairment. It can cause other neurologic components like perceptual, representational, visuospatial, and behavioral deficits. When asked to describe a scene or place with which they are familiar, a patient will describe only the right side of the scene from memory and neglect describing the left side. Other manifestations include patient's lack of awareness or disregard of neurologic deficits, known as anosognosia, and the presence of emotional dysfunction [6].
2. Case presentation
A 63-year-old caucasian man, right-handed, with type two diabetes mellitus was brought by Emergency Medical Services (EMS) as a stroke alert with altered mental status. The onset of his symptoms was unclear and the last known normal per his wife was 3 am. He was found unresponsive by EMS with abnormal respirations at 9 am. The initial fingerstick glucose level was undetectable. He was given 200 milliliters (ml) of 10% hypertonic glucose solution. The patient became more responsive en-route to the hospital.
The neurology stroke team assessed the patient upon arrival to the emergency department (ED). His fingerstick glucose level was 83 and blood pressure was 132/88 mmHg. The patient preferentially turned his head to the right side, most dramatically while looking to the right to answer questions when addressed on his left side. His speech was well articulated, and he was able to recall his age and the date appropriately and discuss his occupation. He was very restless (hyper-arousable state common in right parietal lob syndromes). Gaze assessment revealed he was unable to cross the midline from right to left. However, he had an intact oculocephalic reflex. Visual field testing revealed left-sided homonymous hemianopia. His sensation was diminished on his left upper and lower extremities, although he actively moved all extremities against gravity (minor left arm drift). On the assessment of the National Institute of Health Stroke Scale (NIHSS), he described only the right side of the cookie theft picture (did not see the children) and was only able to name the objects on the right side of the object naming chart. When asked to read sentences, he skipped the initial words (left side) of the sentences. The extinction and neglect assessment revealed left-sided extinction on double tactile and visual stimulation. His NIHSS was 6.
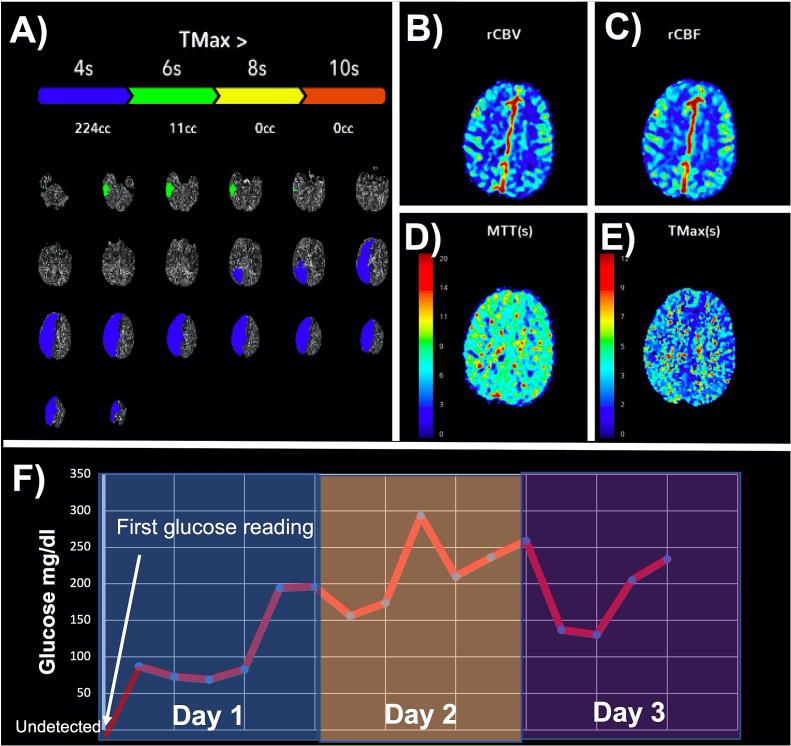
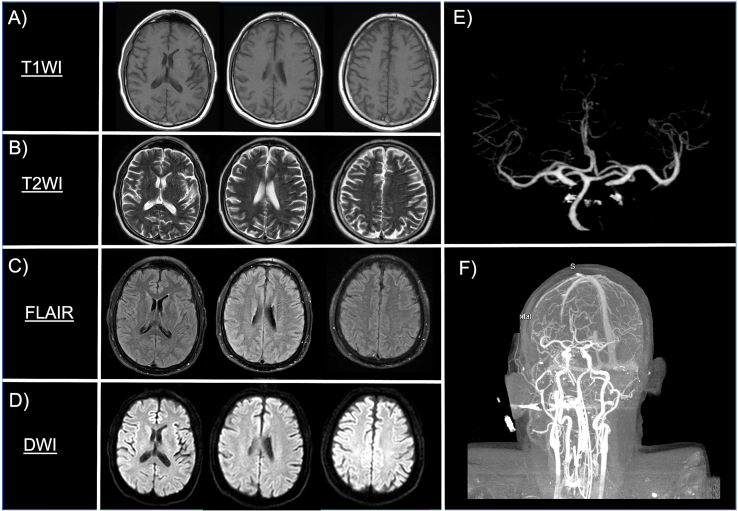
Non-contrast computed tomography (CT) of the brain was normal. Due to restlessness and agitated behavior, he required sedation and intubation to proceed with the acute stroke evaluation. CT perfusion of the brain showed a perfusion decrease in the right cortical area (Fig. 1, Fig. 2). There was no large vessel occlusion on CT angiography of the neck or cerebral circulation. Given the unclear last known normal, urgent brain magnetic resonance imaging (MRI) was performed and was negative for acute stroke. Therefore, TNK was not given. Patient reported that his insulin regimen was recently changed by his primary care physician, and he had fasted the previous night. After the transfer to the Neuro-ICU he was started on an insulin sliding scale. The following day the patient was back at his baseline, without any neurological deficit, and able recall the whole episode.
Fig. 1.
CT perfusion of the brain showed a perfusion decrease in the right cortical area with VIZ artificial intelligence indicating potentially salvageable ischemic brain tissue in the right hemisphere (Green color) (A, B, C, D). Based on the EMS report the glucose level was undetectable when they measured for the first time (White arrow) and patient was given dextrose intravenously. On the arrival to the hospital patient glucose level was 96. (F). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
MRI of the head did not show acute stroke on T1WI, T2WI, FLAIR and DWI sequences (A, B, C, D) and CTA of the head and neck was negative for large vessel occlusion. (E, F).
3. Discussion
Hypoglycemia causes behavioral changes, confusion, loss of consciousness, and seizures. It is well known that hypoglycemia can induce hemiplegia and aphasia. Non-ischemic causes account for around 13% of cases with stroke-like deficits [7]. Hemineglect syndrome may pose as a diagnostic challenge: differentiating a visual field defect from hemineglect is often difficult. Our patient was oriented to person, place, and time, but the repeated turning of his head to the right in search for the examiner when questioned from the left side is suggestive of hemineglect syndrome rather than visual field defect.
During the acute stroke assessment, the NIHSS, which relies predominantly on the subjective impression of performance rather than objective measurement proved useful in identifying his inattention to the left side. Our patient did not have sharp and absolute left-sided hemianopia and was not clearly respecting the midline on visual field testing. These characteristics suggested hemineglect rather than a primary visual field deficit.
Our patient clearly neglected the left side of visual space in all provided images on the NIHSS. Hypoglycemia is a common presenting feature of diabetes in the emergency department. The brain cannot synthesize glucose or store substantial amounts of glycogen in astrocytes; it requires a virtually continuous supply of glucose from the circulation [8]. Different brain regions have different metabolic requirements; the highest demand for glucose occurs in the cerebral cortex and basal ganglia. Focal deficits may result from the asymmetric distribution of glucose transporters. Severe episodes of hypoglycemia are more likely to cause hemiparesis and are more likely to mimic ischemic stroke. We were unable to identify a similar reported case of hypoglycemia induced hemineglect.
Imaging during the onset of stroke can play a major role in diagnosis. Imaging findings in hypoglycemia typically describe bilateral cortical or subcortical changes on CT or MRI. Per Yong and colleagues, 20% mimicked cortical or lacunar stroke by brain imagining. In our patient, CT brain perfusion showed a decreased perfusion at Time-to-Maximum (Tmax) which is a perfusion parameter used both in CT perfusion and MRI perfusion and reflects the time delay between the contrast bolus arriving in the proximal large vessel arterial circulation. Few cases have described hypoglycemia induced focal cerebral hypoperfusion [9]. In our patient's case, the brain MRI was of great utility: it showed there was no acute stroke and indicated that hypoglycemia was the culprit for his symptoms.
Teaching points
-
1.
Hypoglycemia should be included in the differential diagnosis for acute neurological impairment including hemineglect.
-
2.
In hypoglycemia abnormal brain imaging like MRI of CT perfusion can be present. It should also be emphasized that focal neurological deficits from hypoglycemia may not have an immediate resolution after correcting the glucose level.
-
3.
Spatial neglect does not necessarily limit disability to sensory and motor impairment. It can cause other neurologic components like perceptual, representational, visuospatial, and behavioral deficits.
-
4.
Focal deficits may result from the asymmetric distribution of glucose transporters. Severe episodes of hypoglycemia are more likely to cause hemiparesis and are more likely to mimic ischemic stroke
Study funding
The authors report no targeted funding.
Disclosures
The authors report no disclosures relevant to the manuscript.
Instruction to authors
We Confirm that the manuscript complies with all instructions to authors.
Authorship requirements
I confirm that authorship requirements have been met and the final manuscript was approved by all authors.
Previous publications
I confirm that this manuscript has not been published elsewhere and is not under consideration by another journal.
Ethical guidelines
I Confirm adherence to ethical guidelines and indicate ethical approvals (IRB) and use of informed consent.
Contributions
Adrian Rodriguez-Hernandez: Drafting/revision of the manuscript for content, including medical writing for content; Study concept Analysis or interpretation of data.
Denis Babici: Images review. Drafting/revision of the manuscript for content, including medical writing for content.
Maryellen Campbell: Drafting/revision of the manuscript for content, including medical writing for content; Study concept Analysis or interpretation of data.
Octavio Carranza-Reneteria: Drafting/revision of the manuscript for content, including medical writing for content; Study concept Analysis or interpretation of data.
Thomas Hammond: Senior author, Study design and hypothesis development, Drafting/revision of the manuscript for content, including medical writing for content.
Declaration of Competing Interest
Authors confirm no conflict of interests.
Acknowledgements
The authors wish to thank the patient for agreeing with this case report.
Contributor Information
Adrian Rodriguez-Hernandez, Email: adrianrodriguez@health.fau.edu.
Denis Babici, Email: dbabicihealth@health.fau.edu.
Maryellen Campbell, Email: maryellencam2016@health.fau.edu.
Octavio Carranza-Reneteria, Email: ocarranza@health.fau.edu.
Thomas Hammond, Email: Thammond@baptisthealth.net.
References
- 1.Langer K.G. Babinski’s anosognosia for hemiplegia in early twentieth-century French neurology. J Hist Neurosci. 2009;18(4):387–405. doi: 10.1080/09647040802537064. [DOI] [PubMed] [Google Scholar]
- 2.Vallar G., Perani D. The anatomy of unilateral neglect after right-hemisphere stroke lesions. A clinical/CT-scan correlation study in man. Neuropsychologia. 1986;24(5):609–622. doi: 10.1016/0028-3932(86)90001-1. [DOI] [PubMed] [Google Scholar]
- 3.Sacks O. The man who mistook his wife for a hat. Br J Psychiatry. 1995;166(1):130–131. doi: 10.1192/bjp.166.1.130. [DOI] [PubMed] [Google Scholar]
- 4.Li K., Malhotra P.A. Spatial neglect. Pract Neurol. 2015;15(5):333–339. doi: 10.1136/practneurol-2015-001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cryer P.E. The barrier of hypoglycemia in diabetes. Diabetes. 2008;57(12):3169–3176. doi: 10.2337/db08-1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kortte K., Hillis A.E. Recent advances in the understanding of neglect and anosognosia following right hemisphere stroke. Curr Neurol Neurosci Rep. 2009;9(6):459–465. doi: 10.1007/s11910-009-0068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Si Larbi M.T., Al Mangour W., Saba I., Al Naqeb D., Faisal Z.S., Omar S., et al. Ischemic and non-ischemic stroke in young adults - a look at risk factors and outcome in a developing country. Cureus. 2021;13(8) doi: 10.7759/cureus.17079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cryer P.E. Hypoglycemia, functional brain failure, and brain death. J Clin Invest. 2007;117(4):868–870. doi: 10.1172/JCI31669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh R.J., Doshi D., Barber P.A. Hypoglycemia causing focal cerebral Hypoperfusion and acute stroke symptoms. Can J Neurol Sci. 2021;48(4):550–552. doi: 10.1017/cjn.2020.246. [DOI] [PubMed] [Google Scholar]