Abstract
Aortic stiffness increases with age and is a robust predictor of cerebrovascular events and cognitive decline including Alzheimer's disease and other forms of dementia. Recent clinical studies have investigated the association between proximal aortic stiffness and pulsatile energy transmission that has deleterious effects on the cerebrovascular network in order to identify potential therapeutic targets. Aging causes disproportionate stiffening of the aorta compared with the carotid arteries, reducing protective impedance mismatches at their interface, increasing the transmission of destructive pulsatile pressure and energy to the cerebral circulation, and leading to cerebral small vessel disease. Thus, aortic stiffening and high-flow pulsatility are associated with alterations in the microvasculature of the brain, vascular endothelial dysfunction, and white matter damage, which contribute to impaired memory function with advancing age. Previous studies have also shown that silent lacunar infarcts and white matter hyperintensities are strongly associated with arterial stiffness. More and more evidence suggests that vascular etiologies, including aortic stiffness, impedance match, and microvascular damage, are associated with cognitive impairment and the pathogenesis of dementia. The measurement of arterial flow and pressure can help understand pulsatile hemodynamics and its impact on vital organs. Interventions that reduce aortic stiffness, such as improvement of the living environment, management of risk factors, and innovation and development of novel drugs, may reduce the risk for dementia.
Keywords: Arterial stiffness, Carotid artery, Cognitive dysfunction, Excessive pulsatile energy, Vascular hemodynamics
Introduction
The number of subjects with dementia is growing as the population ages [1]. Cardiovascular (CV) risk factors, including arterial stiffness, are associated with various types of dementia and represent potentially modifiable intervention targets [1]. Vascular dysfunction has been demonstrated to manifest together with other disease markers, such as accumulation of β-amyloid plaques and tau protein tangles common to Alzheimer's disease [2]. Evidence also showed that pressure and flow pulsatility in the macrocirculation and microcirculation are associated with microvascular damage in the high-flow brain and kidneys [3]. Small vessel disease and white matter damage associated with advanced aortic stiffness contribute to impaired memory with age.
To slow down aging-associated target organ damage and CV complications, early vascular aging (EVA) [4] and supernormal vascular aging (SUPERNOVA) [5] have been proposed to better understand the process of vascular aging and provide the opportunity to discover the determinants of arterial stiffness and corresponding preventive and treatment targets. In this review, we will address the concepts of EVA and SUPERNOVA and the consequence of pulsatile hemodynamics and arterial stiffening on target organ damage.
What Is EVA and SUPERNOVA?
EVA and SUPERNOVA are vascular aging phenotypes [5]. By calculating the so-called delta age, which is the chronological age subtracted by vascular age, we can classify subjects into different phenotypes of vascular aging. The younger vascular age compared to real chronological age is more likely to be SUPERNOVA. On the contrary, the older vascular age (negative delta age) is more likely to be EVA [4]. The top and bottom 10% of delta ages have been used to define EVA and SUPERNOVA, respectively [5].
How to Define Vascular Age?
One could estimate vascular age [6] with these three methods: carotid-femoral pulse wave velocity (cf-PWV) alone, cf-PWV together with age and blood pressure (BP) (age- and BP-stratified cf-PWV), and cf-PWV plus CV risk factors and treatments. The combination of the cf-PWV and CV risk factors may be more suitable for calculating vascular age in populations with various CV risk factor burdens.
In a study published in hypertension, a regression equation was constructed by using cf-PWV and CV risk factors. In the equation, cf-PWV, CV risk factors, and treatments were independent variables, and age was a dependent variable. Delta age is the chronological age subtracted by vascular age, as mentioned earlier. In the validation cohort, EVA had a higher risk of CV events, with a hazard ratio of 2.61 (95% confident interval [CI]: 1.50–4.53) compared with SUPERNOVA 0.61 (95% CI: 0.42–0.87) [7].
Steady and Pulsatile Hemodynamics and Hydraulic Energy
In the past, we only used pressure or flow to evaluate the influence of circulatory arterial waves on vital organs [8]. However, it might be the energy that provides the real and more important effects on systemic circulation. The power is the product of pressure and flow waveform. By integrating the power over time, we can derive the energy. Previous evidence had supported the concept that pulsatile power is a more sensitive and accurate measure for excessive pulsatility transmission to the brain compared to conventional pressure or flow pulsatility indices alone [9].
Different aspects of arterial hemodynamics are observed including steady and pulsatile hemodynamics. For steady flow, we can use mean BP to describe the arterial pressure, which is determined by cardiac output and total peripheral resistance. The arterial pulse is generated by the left ventricle. During the transmission of the arterial pulse in the systolic phase, the large arteries expand to store the pulse energy so that the blood flow can sustain during the diastolic phase. This property of arterial compliance is analogous to that of a Windkessel chamber. The arterial system in human youth is delicately designed for the role of receiving jets of blood from the left ventricle and allocating this as a steady flow through peripheral capillaries. Central to such design is the “accommodation” of the heart to the arterial tree; this minimizes the “tidal wave” effect from aortic pressure fluctuations and confines flow pulsations to the larger arteries [10]. With aging, repetitive pulsations (around 30 million/year) cause exhaustion and fracture of elastin lamellae of central arteries, resulting in stiffening and dilatation, so that reflections return earlier to the heart; as a consequence, aortic systolic pressure rises, diastolic pressure falls, and pulsations of flow extend further into smaller vessels of vasodilated organs, notably the brain [11] and kidney [12]. Stiffening leads to increased left ventricular load with hypertrophy, an increased risk of new-onset atrial fibrillation [13], increased myocardial oxygen demand [14], decreased capacity for myocardial perfusion as pulse pressure widens and diastolic BP decreases [15], and increased stresses on small arterial vessels, particularly of the brain and kidney. Clinical manifestations are a result of left ventricular diastolic dysfunction [16] with dyspnea, predisposition to angina, heart failure [17, 18], and small vessel degeneration in the brain and the kidney with resultant intellectual deterioration and renal failure. While aortic stiffening is the principal cause of CV disease [19] in aged persons who escape atherosclerotic complications, it is not a therapeutic target currently. The principal available treatment target is the smooth muscle in distributing arteries, whose relaxation has caused a substantial reduction in the magnitude of wave reflection. Such relaxation can be achieved through regular exercise and the use of vasodilating drugs for the management of hypertension and cardiac failure.
On the other hand, the arterial pulse wave is reflected at sites such as bifurcations, narrowing of arteries, or change of impedance. Both arterial compliance and wave reflections can influence the shape of the arterial pressure waveforms. BP is the pressure exerted by circulating blood upon the walls of blood vessels and determined by several physical factors, including rate of pumping, blood volume, resistance, arterial stiffness, and arterial wave reflections. The BP is usually measured at a person's upper arm, i.e., the brachial artery pressure. It has been recognized that BP at the brachial artery is different from the pressure at the central aorta, mainly due to the phenomenon of pressure amplification. Although current diagnosis and management of hypertension are based on the measurement of brachial BP, it has been a long debate whether central BP or individual components of BP are clinically more useful than systolic BP [20, 21].
The Relationship between Vascular Aging and Dementia
Dementia and cognitive decline have become major health care concerns, especially in aging populations around the world [22]. There have been many risk factors implicated in the pathophysiology of cognitive decline. Among them, vascular aging and arterial stiffness have been proposed as important factors contributing to dementia [23, 24, 25].
Central hemodynamics plays a key role in understanding brain damage in hypertension because arterial stiffening is a major determinant of elevated central BP and high central pulsatility is a mechanical factor for brain tissue damage [26, 27], cognitive impairment [28], and cerebral small vessel disease, which included recent small subcortical infarcts, white matter hyperintensity, lacunae, microbleeds, and perivascular space [29]. It has been shown that both increased arterial stiffness and central BP are predictive of stroke [30] and the functional outcome in patients after ischemic stroke [31]. Previous studies also showed that the mechanics and remodeling of an extracranial large artery (common carotid artery) are representative of wall damage of an intracranial large artery [32]. However, whether antihypertensive treatment targeted to reduce aortic stiffness and central BP could prevent stroke, white matter lesions, and cognitive decline remains to be determined.
How Does Arterial Stiffness Associate with Microvascular Disease in the Brain?
It has also been suggested that EVA could increase carotid pressure and flow pulsatility due to decreased wave reflection at the aorta-carotid interface, which then causes microvascular damage and impairs vasomotor reactivity and further microvascular and tissue damage [33]. Pulse wave encephalopathy refers to brain tissue damage in response to an increased central artery. An increased aortic and carotid artery stiffness leads to higher arterial pulsatility and higher transmission of pulsatile energy into cerebral arterioles. Aortic stiffness is also associated with an increased risk of ischemic stroke through atherosclerosis [34], the risk for plaque rupture [35], reversal diastolic flow [36], increased myogenic tone, and limited autoregulation of cerebral blood flow [37]. A strong body of evidence supports the association between vascular dementia and Alzheimer's disease with hemodynamic abnormalities [1, 38]. It has been shown that people developing high BP in the middle of life have a much greater likelihood of developing vascular dementia [39] and cognitive impairment [40] in later life. In our previous study [41], we have shown that higher BP and lower carotid flow velocity were associated with lower brain volume and a higher risk of the cerebral small vessel. Furthermore, in prospective design study [8], we have clearly revealed that the carotid flow pulsatility index, combined with central systolic BP, was positively associated with stroke incidence. In each stratum of central SBP, high carotid flow pulsatility was associated with a higher incidence of stroke. Moreover, cf-PWV, the biomarker of vascular stiffness, instead of augmentation index or pulse pressure, was consistently associated with an earlier microstructural injury before white matter hyperintensities and regional earlier brain atrophy in younger individuals, suggesting that the initial and continuous brain damage related to arterial stiffness begins in or precede midlife [42].
Impedance Mismatch
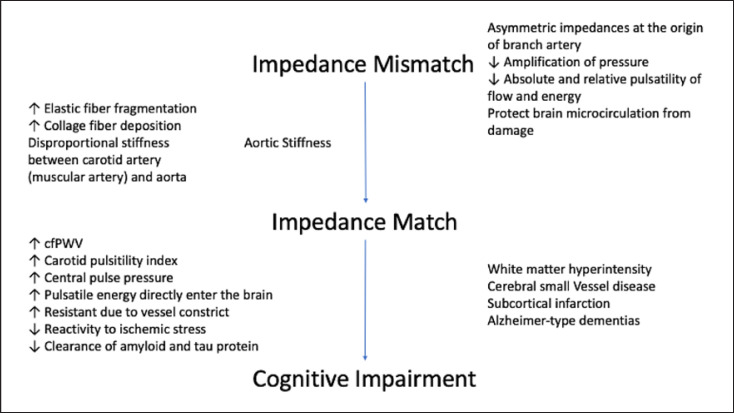
The concept of impedance mismatch has been proposed to illustrate the mechanistic linkage between vascular aging and target organ damage [43, 44, 45]. Younger, healthy subjects generally have a highly compliant aorta and relatively stiff muscular arteries, which act like a gate and create a discontinuity of impedance to pulsatile flow at the transition between the aorta and first-generation branch arteries. This impedance mismatch reflects a portion of the pulsatile energy saved in the forward-traveling wave, restricting its transmission into the peripheral vasculature. Beyond midlife, the impedance of the aorta increases disproportionately to that of the muscular arteries, leading to impedance matching and a reduction in wave reflection through irreversible fragmentation of elastic fibers, contributing to deposition and progressive engagement of much stiffer collagen fibers within the wall, ultimately to the progressive stiffening of the proximal aorta. The proximal aorta is susceptible to earlier deterioration than peripheral arteries since the proximal thoracic aorta bears the force of the pulsatile strain directly from cardiac ejection and stiffening of the wall of the aorta. The vascular aging process results in higher central pulse pressure, characteristic impedance, cf-PWV, altered timing of the reflected wave, and reduced proximal wave reflection [46]. Such change diminishes a protective mechanism that normally buffers the peripheral microcirculation from excessive pulsatility. The loss of the natural barrier enables the pulse waves can easily enter our brain and cause damage [44]. Moreover, in response to excessive pressure and flow pulsatility, the microvessels constrict to protect the microcirculation but also result in increased microvascular resistance, reduced blood flow [47, 48], and reduced microvascular reactivity in response to ischemic stress [49] and labile BP caused by stiff arteries [50]. Thus, the cumulative sequelae of elevated aortic stiffness and impedance matching, especially for the brain, characterized by high-flow, low microvascular impedance, and vulnerability to pressure and flow pulsatility [33], manifests as white matter hyperintensities, tissue atrophy, and cognitive impairment and dementia [51]. We summarized the process from impedance mismatch to cognitive impairment, mediated by aging and aortic stiffness in Figure 1.
Fig. 1.
The conceptual process from impedance mismatch to cognitive impairment and neurological disease, mediated by aging and aortic stiffness.
However, some have contemplated that since the aorta-carotid bifurcation is with a reflection coefficient of 0–15% and relatively well matched, any effect of local wave reflection on transmitted power at the junction is insignificant, with 97% and 100% of incident power conveyed [52]. Moreover, transmitted pulsatile pressure increases with bifurcation reflection coefficients, which should be deleterious in terms of downstream organ function [53]. Others have reported that bifurcations in the arterial system are usually impedance matched in the forward, instead of the backward direction, optimally transmitting forward hydraulic power while causing backward-traveling power to be stuck in daughter arteries by reflection [54, 55]. Subsequently, Haidar et al. had assessed this controversial issue with aortic flow, carotid pressure, flow and hydraulic power, brain magnetic resonance images, and cognitive scores in AGES-Reykjavik study [56] by enrolling 668 subjects without history of stroke, transient ischemic attack, or dementia. Higher carotid flow pulsatility was associated with lower white matter volume and memory scores. Marked asymmetry of characteristic impedances at aorta-branch artery bifurcations reduces amplification of pressure and the absolute and relative pulsatility of transmitted flow and hydraulic power into branch arteries, which protects the downstream local microcirculation from pulsatile damage [57].
Conclusions
The concept of EVA and SUPERNOVA is proposed to better understand the process of vascular aging and develop corresponding preventive and treatment targets. EVA and SUPERNOVA can be defined by calculating vascular age and the corresponding delta age. In EVA subjects, with advanced proximal aortic stiffness and resultant eroded aortic impedance mismatch, the excessive pulsatile energy is transmitted across the aorta-carotid interface into the carotid artery and associates with increased carotid pulsatile energy and reduced cognitive function. The measurement of arterial flow and pressure can help better understand pulsatile hemodynamics and its impact on vital organs.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
Grants from the Ministry of Health and Welfare (MOHW104-TDU-B-211-113-003, MOHW106-TDU-B-211-113001), an intramural grant from National Yang Ming Chiao Tung University (E107F-M01-0501), and the Ministry of Science and Technology (MOST 106-2314-B-075 -051 -MY3, MOST 109-2314-B-010-061 -). The funding sources are not involved in the manuscript preparation.
Author Contributions
Wei-Ting Wang, Wei-Lun Chang, and Hao-Min Cheng contributed to the concept and design of this review and critical revision of the manuscript for important intellectual content and read and approved the final version of the manuscript. Wei-Ting Wang drafted the preliminary manuscript.
Funding Statement
Grants from the Ministry of Health and Welfare (MOHW104-TDU-B-211-113-003, MOHW106-TDU-B-211-113001), an intramural grant from National Yang Ming Chiao Tung University (E107F-M01-0501), and the Ministry of Science and Technology (MOST 106-2314-B-075 -051 -MY3, MOST 109-2314-B-010-061 -). The funding sources are not involved in the manuscript preparation.
References
- 1.Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2011 Sep;42((9)):2672–713. doi: 10.1161/STR.0b013e3182299496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iadecola C. The pathobiology of vascular dementia. Neuron. 2013 Nov 20;80((4)):844–66. doi: 10.1016/j.neuron.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Climie RED, Picone DS, Blackwood S, Keel SE, Qasem A, Rattigan S, et al. Pulsatile interaction between the macro-vasculature and micro-vasculature: proof-of-concept among patients with type 2 diabetes. Eur J Appl Physiol. 2018 Nov;118((11)):2455–63. doi: 10.1007/s00421-018-3972-2. [DOI] [PubMed] [Google Scholar]
- 4.Nilsson PM, Boutouyrie P, Laurent S. Vascular aging: a tale of EVA and ADAM in cardiovascular risk assessment and prevention. Hypertension. 2009 Jun;54((1)):3–10. doi: 10.1161/HYPERTENSIONAHA.109.129114. [DOI] [PubMed] [Google Scholar]
- 5.Laurent S, Boutouyrie P, Cunha PG, Lacolley P, Nilsson PM. Concept of extremes in vascular aging. Hypertension. 2019 Aug;74((2)):218–28. doi: 10.1161/HYPERTENSIONAHA.119.12655. [DOI] [PubMed] [Google Scholar]
- 6.Redheuil A, Kachenoura N, Bollache E, Yu WC, Opdahl A, Decesare A, et al. Left ventricular and proximal aorta coupling in magnetic resonance imaging: aging together? Am J Physiol Heart Circ Physiol. 2019 Aug 1;317((2)):H300–07. doi: 10.1152/ajpheart.00694.2018. [DOI] [PubMed] [Google Scholar]
- 7.Bruno RM, Nilsson PM, Engstrom G, Wadstrom BN, Empana JP, Boutouyrie P, et al. Early and supernormal vascular aging: clinical characteristics and association with incident cardiovascular events. Hypertension. 2020 Nov;76((5)):1616–24. doi: 10.1161/HYPERTENSIONAHA.120.14971. [DOI] [PubMed] [Google Scholar]
- 8.Chuang SY, Cheng HM, Bai CH, Yeh WT, Chen JR, Pan WH. Blood pressure, carotid flow pulsatility, and the risk of stroke: a community-based study. Stroke. 2016 Sep;47((9)):2262–8. doi: 10.1161/STROKEAHA.116.013207. [DOI] [PubMed] [Google Scholar]
- 9.Aghilinejad A, Amlani F, King KS, Pahlevan NM. Dynamic effects of aortic arch stiffening on pulsatile energy transmission to cerebral vasculature as A determinant of brain-heart coupling. Sci Rep. 2020 May 29;10((1)):8784. doi: 10.1038/s41598-020-65616-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Rourke MF, Hashimoto J. Mechanical factors in arterial aging: a clinical perspective. J Am Coll Cardiol. 2007 Jul 3;50((1)):1–13. doi: 10.1016/j.jacc.2006.12.050. [DOI] [PubMed] [Google Scholar]
- 11.Henskens LH, Kroon AA, van Oostenbrugge RJ, Gronenschild EH, Fuss-Lejeune MM, Hofman PA, et al. Increased aortic pulse wave velocity is associated with silent cerebral small-vessel disease in hypertensive patients. Hypertension. 2008 Dec;52((6)):1120–6. doi: 10.1161/HYPERTENSIONAHA.108.119024. [DOI] [PubMed] [Google Scholar]
- 12.Foudi N, Palayer M, Briet M, Garnier AS. Arterial remodelling in chronic kidney disease: impact of uraemic toxins and new pharmacological approaches. J Clin Med. 2021 Aug 25;10((17)):3803. doi: 10.3390/jcm10173803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mitchell GF, Vasan RS, Keyes MJ, Parise H, Wang TJ, Larson MG, et al. Pulse pressure and risk of new-onset atrial fibrillation. JAMA. 2007 Feb 21;297((7)):709–15. doi: 10.1001/jama.297.7.709. [DOI] [PubMed] [Google Scholar]
- 14.Kelly RP, Tunin R, Kass DA. Effect of reduced aortic compliance on cardiac efficiency and contractile function of in situ canine left ventricle. Circ Res. 1992 Sep;71((3)):490–502. doi: 10.1161/01.res.71.3.490. [DOI] [PubMed] [Google Scholar]
- 15.Kass DA, Saeki A, Tunin RS, Recchia FA. Adverse influence of systemic vascular stiffening on cardiac dysfunction and adaptation to acute coronary occlusion. Circulation. 1996 Apr 15;93((8)):1533–41. doi: 10.1161/01.cir.93.8.1533. [DOI] [PubMed] [Google Scholar]
- 16.Russo C, Jin Z, Palmieri V, Homma S, Rundek T, Elkind MSV, et al. Arterial stiffness and wave reflection: sex differences and relationship with left ventricular diastolic function. Hypertension. 2012 Aug;60((2)):362–8. doi: 10.1161/HYPERTENSIONAHA.112.191148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kawaguchi M, Hay I, Fetics B, Kass DA. Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitations. Circulation. 2003 Feb 11;107((5)):714–20. doi: 10.1161/01.cir.0000048123.22359.a0. [DOI] [PubMed] [Google Scholar]
- 18.Weber T, Wassertheurer S, O'Rourke MF, Haiden A, Zweiker R, Rammer M, et al. Pulsatile hemodynamics in patients with exertional dyspnea: potentially of value in the diagnostic evaluation of suspected heart failure with preserved ejection fraction. J Am Coll Cardiol. 2013 May 7;61((18)):1874–83. doi: 10.1016/j.jacc.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 19.van Popele NM, Grobbee DE, Bots ML, Asmar R, Topouchian J, Reneman RS, et al. Association between arterial stiffness and atherosclerosis: the Rotterdam Study. Stroke. 2001 Feb;32((2)):454–60. doi: 10.1161/01.str.32.2.454. [DOI] [PubMed] [Google Scholar]
- 20.Huang QF, Aparicio LS, Thijs L, Wei FF, Melgarejo JD, Cheng YB, et al. Cardiovascular end points and mortality are not closer associated with central than peripheral pulsatile blood pressure components. Hypertension. 2020 Aug;76((2)):350–8. doi: 10.1161/HYPERTENSIONAHA.120.14787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cheng YB, Thijs L, Aparicio LS, Huang QF, Wei FF, Yu YL, et al. Risk stratification by cross-classification of central and brachial systolic blood pressure. Hypertension. 2022 Mar 4;79((5)):1101–11. doi: 10.1161/HYPERTENSIONAHA.121.18773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.GBD 2019 Dementia Forecasting Collaborators Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2022 Feb;7((2)):e105–e125. doi: 10.1016/S2468-2667(21)00249-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saji N, Toba K, Sakurai T. Cerebral small vessel disease and arterial stiffness: tsunami effect in the brain? Pulse. 2016 Apr;3((3–4)):182–9. doi: 10.1159/000443614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hughes TM, Wagenknecht LE, Craft S, Mintz A, Heiss G, Palta P, et al. Arterial stiffness and dementia pathology: atherosclerosis risk in communities (ARIC)-PET study. Neurology. 2018 Apr 3;90((14)):e1248–56. doi: 10.1212/WNL.0000000000005259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cooper LL, O'Donnell A, Beiser AS, Thibault EG, Sanchez JS, Benjamin EJ, et al. Association of aortic stiffness and pressure pulsatility with global amyloid-beta and regional tau burden among framingham heart study participants without dementia. JAMA Neurol. 2022 Jul 1;79((7)):710–9. doi: 10.1001/jamaneurol.2022.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poels MMF, Zaccai K, Verwoert GC, Vernooij MW, Hofman A, van der Lugt A, et al. Arterial stiffness and cerebral small vessel disease: the Rotterdam Scan Study. Stroke. 2012 Oct;43((10)):2637–42. doi: 10.1161/STROKEAHA.111.642264. [DOI] [PubMed] [Google Scholar]
- 27.Wei J, Palta P, Meyer ML, Kucharska-Newton A, Pence BW, Aiello AE, et al. Aortic stiffness and white matter microstructural integrity assessed by diffusion tensor imaging: the ARIC-NCS. J Am Heart Assoc. 2020 Mar 17;9((6)):e014868. doi: 10.1161/JAHA.119.014868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010 Jun;9((7)):689–701. doi: 10.1016/S1474-4422(10)70104-6. [DOI] [PubMed] [Google Scholar]
- 29.Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013 Aug;12((8)):822–38. doi: 10.1016/S1474-4422(13)70124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saji N, Kimura K, Kawarai T, Shimizu H, Kita Y. Arterial stiffness and progressive neurological deficit in patients with acute deep subcortical infarction. Stroke. 2012 Nov;43((11)):3088–90. doi: 10.1161/STROKEAHA.112.670737. [DOI] [PubMed] [Google Scholar]
- 31.Gasecki D, Rojek A, Kwarciany M, Kubach M, Boutouyrie P, Nyka W, et al. Aortic stiffness predicts functional outcome in patients after ischemic stroke. Stroke. 2012 Feb;43((2)):543–4. doi: 10.1161/STROKEAHA.111.633487. [DOI] [PubMed] [Google Scholar]
- 32.Laurent S, Boutouyrie P. The structural factor of hypertension: large and small artery alterations. Circ Res. 2015 Mar 13;116((6)):1007–21. doi: 10.1161/CIRCRESAHA.116.303596. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell GF. Effects of central arterial aging on the structure and function of the peripheral vasculature: implications for end-organ damage. J Appl Physiol. 2008 Nov;105((5)):1652–60. doi: 10.1152/japplphysiol.90549.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilkinson IB, McEniery CM, Cockcroft JR. Arteriosclerosis and atherosclerosis: guilty by association. Hypertension. 2009 Dec;54((6)):1213–5. doi: 10.1161/HYPERTENSIONAHA.109.142612. [DOI] [PubMed] [Google Scholar]
- 35.Lovett JK, Howard SC, Rothwell PM. Pulse pressure is independently associated with carotid plaque ulceration. J Hypertens. 2003 Sep;21((9)):1669–76. doi: 10.1097/00004872-200309000-00016. [DOI] [PubMed] [Google Scholar]
- 36.Hashimoto J, Ito S. Aortic stiffness determines diastolic blood flow reversal in the descending thoracic aorta: potential implication for retrograde embolic stroke in hypertension. Hypertension. 2013 Sep;62((3)):542–9. doi: 10.1161/HYPERTENSIONAHA.113.01318. [DOI] [PubMed] [Google Scholar]
- 37.Fernando MS, Simpson JE, Matthews F, Brayne C, Lewis CE, Barber R, et al. White matter lesions in an unselected cohort of the elderly: molecular pathology suggests origin from chronic hypoperfusion injury. Stroke. 2006 Jun;37((6)):1391–8. doi: 10.1161/01.STR.0000221308.94473.14. [DOI] [PubMed] [Google Scholar]
- 38.Ninomiya T, Ohara T, Hirakawa Y, Yoshida D, Doi Y, Hata J, et al. Midlife and late-life blood pressure and dementia in Japanese elderly: the Hisayama study. Hypertension. 2011 Jun;58((1)):22–8. doi: 10.1161/HYPERTENSIONAHA.110.163055. [DOI] [PubMed] [Google Scholar]
- 39.Shokouhi M, Qiu D, Samman Tahhan A, Quyyumi AA, Hajjar I. Differential associations of diastolic and systolic pressures with cerebral measures in older individuals with mild cognitive impairment. Am J Hypertens. 2018 Nov 13;31((12)):1268–77. doi: 10.1093/ajh/hpy104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vasan RS, Pan S, Xanthakis V, Beiser A, Larson MG, Seshadri S, et al. Arterial stiffness and long-term risk of health outcomes: the framingham heart study. Hypertension. 2022 May;79((5)):1045–56. doi: 10.1161/HYPERTENSIONAHA.121.18776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chuang SY, Wang PN, Chen LK, Chou KH, Chung CP, Chen CH, et al. Associations of blood pressure and carotid flow velocity with brain volume and cerebral small vessel disease in a community-based population. Transl Stroke Res. 2021 Apr;12((2)):248–58. doi: 10.1007/s12975-020-00836-7. [DOI] [PubMed] [Google Scholar]
- 42.Maillard P, Mitchell GF, Himali JJ, Beiser A, Tsao CW, Pase MP, et al. Effects of arterial stiffness on brain integrity in young adults from the framingham heart study. Stroke. 2016 Apr;47((4)):1030–6. doi: 10.1161/STROKEAHA.116.012949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cooper LL, Mitchell GF. Aortic stiffness, cerebrovascular dysfunction, and memory. Pulse. 2016 Sep;4((2–3)):69–77. doi: 10.1159/000448176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mitchell GF, van Buchem MA, Sigurdsson S, Gotal JD, Jonsdottir MK, Kjartansson O, et al. Arterial stiffness, pressure and flow pulsatility and brain structure and function: the Age, Gene/Environment Susceptibility–Reykjavik study. Brain. 2011 Nov;134((11)):3398–407. doi: 10.1093/brain/awr253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Roos A, van der Grond J, Mitchell G, Westenberg J. Magnetic resonance imaging of cardiovascular function and the brain: is dementia a cardiovascular-driven disease? Circulation. 2017 May 30;135((22)):2178–95. doi: 10.1161/CIRCULATIONAHA.116.021978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mitchell GF, Wang N, Palmisano JN, Larson MG, Hamburg NM, Vita JA, et al. Hemodynamic correlates of blood pressure across the adult age spectrum: noninvasive evaluation in the Framingham Heart Study. Circulation. 2010 Oct 5;122((14)):1379–86. doi: 10.1161/CIRCULATIONAHA.109.914507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Williamson GA, Loutzenhiser R, Wang X, Griffin K, Bidani AK. Systolic and mean blood pressures and afferent arteriolar myogenic response dynamics: a modeling approach. Am J Physiol Regul Integr Comp Physiol. 2008 Nov;295((5)):R1502–11. doi: 10.1152/ajpregu.00490.2007. [DOI] [PubMed] [Google Scholar]
- 48.Loutzenhiser R, Bidani A, Chilton L. Renal myogenic response: kinetic attributes and physiological role. Circ Res. 2002 Jun 28;90((12)):1316–24. doi: 10.1161/01.res.0000024262.11534.18. [DOI] [PubMed] [Google Scholar]
- 49.Mitchell GF, Vita JA, Larson MG, Parise H, Keyes MJ, Warner E, et al. Cross-sectional relations of peripheral microvascular function, cardiovascular disease risk factors, and aortic stiffness: the Framingham Heart Study. Circulation. 2005 Dec 13;112((24)):3722–8. doi: 10.1161/CIRCULATIONAHA.105.551168. [DOI] [PubMed] [Google Scholar]
- 50.Schillaci G, Bilo G, Pucci G, Laurent S, Macquin-Mavier I, Boutouyrie P, et al. Relationship between short-term blood pressure variability and large-artery stiffness in human hypertension: findings from 2 large databases. Hypertension. 2012 Aug;60((2)):369–77. doi: 10.1161/HYPERTENSIONAHA.112.197491. [DOI] [PubMed] [Google Scholar]
- 51.Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. Recommendations for improving and standardizing vascular research on arterial stiffness: a scientific statement from the American heart association. Hypertension. 2015 Sep;66((3)):698–722. doi: 10.1161/HYP.0000000000000033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Phan TS, Li JKJ, Segers P, Reddy-Koppula M, Akers SR, Kuna ST, et al. Aging is associated with an earlier arrival of reflected waves without a distal shift in reflection sites. J Am Heart Assoc. 2016 Aug 29;5((9)):e003733. doi: 10.1161/JAHA.116.003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kondiboyina A, Smolich JJ, Cheung MMH, Westerhof BE, Mynard JP. Conduit arterial wave reflection promotes pressure transmission but impedes hydraulic energy transmission to the microvasculature. Am J Physiol Heart Circ Physiol. 2020 Jul 1;319((1)):H66–H75. doi: 10.1152/ajpheart.00733.2019. [DOI] [PubMed] [Google Scholar]
- 54.Baksi AJ, Davies JE, Hadjiloizou N, Baruah R, Unsworth B, Foale RA, et al. Attenuation of reflected waves in man during retrograde propagation from femoral artery to proximal aorta. Int J Cardiol. 2016 Jan 1;202:441–5. doi: 10.1016/j.ijcard.2015.09.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Davies JE, Alastruey J, Francis DP, Hadjiloizou N, Whinnett ZI, Manisty CH, et al. Attenuation of wave reflection by wave entrapment creates a “horizon effect” in the human aorta. Hypertension. 2012 Sep;60((3)):778–85. doi: 10.1161/HYPERTENSIONAHA.111.180604. [DOI] [PubMed] [Google Scholar]
- 56.Harris TB, Launer LJ, Eiriksdottir G, Kjartansson O, Jonsson PV, Sigurdsson G, et al. Age, gene/environment susceptibility-Reykjavik study: multidisciplinary applied phenomics. Am J Epidemiol. 2007 May 1;165((9)):1076–87. doi: 10.1093/aje/kwk115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Haidar MA, van Buchem MA, Sigurdsson S, Gotal JD, Gudnason V, Launer LJ, et al. Wave reflection at the origin of a first-generation branch artery and target organ protection: the AGES-Reykjavik study. Hypertension. 2021 Apr;77((4)):1169–77. doi: 10.1161/HYPERTENSIONAHA.120.16696. [DOI] [PMC free article] [PubMed] [Google Scholar]