Abstract
Nutraceuticals have emerged as potential compounds to attenuate the COVID‐19 complications. Precisely, these food additives strengthen the overall COVID treatment and enhance the immunity of a person. Such compounds have been used at a large scale, in almost every household due to their better affordability and easy access. Therefore, current research is focused on developing newer advanced formulations from potential drug candidates including nutraceuticals with desirable properties viz, affordability, ease of availability, ease of administration, stability under room temperature, and potentially longer shelf‐lives. As such, various nutraceutical‐based products such as compounds could be promising agents for effectively managing COVID‐19 symptoms and complications. Most importantly, regular consumption of such nutraceuticals has been shown to boost the immune system and prevent viral infections. Nutraceuticals such as vitamins, amino acids, flavonoids like curcumin, and probiotics have been studied for their role in the prevention of COVID‐19 symptoms such as fever, pain, malaise, and dry cough. In this review, we have critically reviewed the potential of various nutraceutical‐based therapeutics for the management of COVID‐19. We searched the information relevant to our topic from search engines such as PubMed and Scopus using COVID‐19, nutraceuticals, probiotics, and vitamins as a keyword. Any scientific literature published in a language other than English was excluded.
Practical applications
Nutraceuticals possess both nutritional values and medicinal properties. They can aid in the prevention and treatment of diseases, as well as promote physical health and the immune system, normalizing body functions, and improving longevity. Recently, nutraceuticals such as probiotics, vitamins, polyunsaturated fatty acids, trace minerals, and medicinal plants have attracted considerable attention and are widely regarded as potential alternatives to current therapeutic options for the effective management of various diseases, including COVID‐19.
Keywords: COVID‐19, nutraceuticals, probiotics, vitamins
Short abstract
Regular consumption of such nutraceuticals has been shown to boost the immune system and prevent viral infections. Nutraceuticals such as vitamins, amino acids, flavonoids like curcumin, and probiotics have been studied for their beneficial effects in the prevention of COVID‐19 symptoms such as fever, pain, malaise, and dry cough. As such, various nutraceutical‐based products such as compounds could be promising agents for the effective management of COVID‐19 symptoms and complications.
1. INTRODUCTION
The coronavirus pandemic that emerged during the latter part of December 2019 continues to cause a massive health risk to the global population. Citizens from various countries have been provided free COVID‐19 vaccines as it is a highly contagious respiratory disease caused by a novel pathogen belonging to the family Coronaviridae. The causative pathogen was initially named novel coronavirus 2019 (2019‐nCoV) by the WHO, which was then renamed severe acute respiratory syndrome (SARS) coronavirus‐2 (SARS‐CoV)‐2 as genomic studies had by then revealed that it was highly homologous to SARS‐CoV, which was the pathogen responsible for the significant outbreak of the SARS pandemic during the years 2002–2003 (Mehta et al., 2020; Parasher, 2021). Generally, individuals infected with SARS‐CoV‐2 present early symptoms of fever, dry cough, shortness of breath, and tachypnoea. Other reported symptoms include malaise, muscle pain, weakness, respiratory distress, as well as loss of taste and smell. Recovery from mild infection of SARS‐CoV‐2 commonly occurs within seven to ten days upon onset of symptoms, whereas it could take up to three to six weeks in severe and critical illness (Esakandari et al., 2020; Raveendran et al., 2021). Nevertheless, there is a subset of patients who even after recovery continue to experience various symptoms that persist and do not resolve over the course of many months to years. These patients are classified as having long COVID or post‐acute sequelae of COVID‐19 (PASC) (Proal & VanElzakker, 2021). The clinical manifestations and symptoms of PASC are clinically heterogenous which suggests the involvement of multiple organs and systems. Fatigue, headache, myalgia, loss of memory, breathlessness, and cognitive impairment are among the prevalent symptoms of PASC. Hence, both COVID‐19 and PASC represent a major burden to public healthcare systems while contributing to substantial economic and productivity losses, especially in low‐ and middle‐income countries. Given the high infectivity rate of SARS‐CoV‐2, the identification and development of novel agents for the treatment of COVID‐19 is crucial to reducing its impact on global morbidity and mortality.
Nutraceuticals are hybrid products generally containing both nutrients and pharmaceuticals. In addition to their medicinal properties, they possess nutritional values, acting as dietary supplements for maintaining body health, at the same time, providing the body with the necessary nutrition that is required for multiple metabolic processes and the regulation of normal body functions. Typically, the use of nutraceuticals can aid in the prevention and treatment of diseases, as well as promote physical health and the immune system, normalizing body functions, and improving longevity (Chan et al., 2021; Chanda et al., 2019). Nutraceuticals also present several advantages in contrast to synthetic drugs. For instance, the use of nutraceuticals can reduce the high production costs of modern pharmaceuticals. The costs involved in setting up a mass production system for growing plants as well as the maintenance of infrastructure involved in the harvesting of natural products and curation of raw extracts are remarkably lower. Therefore, deploying such a system in low‐ to middle‐income countries in which high infrastructure costs represent a barrier to research and development of novel therapeutics is highly feasible. Moreover, such low production costs can effectively lower the price of therapeutics to be made more affordable, thereby addressing the issue of inequality in access to medicines, especially for patients residing in rural areas in low‐income countries (Sack et al., 2015; Sofowora et al., 2013). Therefore, a gap between different therapies to combat the infections with COVID‐19 could be reduced to a maximum extent by the addition of nutraceuticals to the diet. Also, due to their significant positive outcomes, these compounds improve overall human health and thus, the application of nutraceuticals has emerged as an option to prevent comorbidity. Nutraceuticals are typically derived from natural sources, they could overcome the limitations of poor tolerability and toxicity, as well as the poor safety profile that is often associated with synthetic compounds (Gulati et al., 2016; Imran, Saleem et al., 2020). Studies have also shown that natural products imbue physicochemical characteristics superior to synthetic compounds such as fewer aromatic rings, lower nitrogen content, and increased oxygen content, thereby contributing to their greater ability to actively engage biological targets and produce biological activity (Wright, 2019). Hence, nutraceuticals such as probiotics, vitamins, polyunsaturated fatty acids, trace minerals, and medicinal plants have attracted considerable attention from medical researchers, and they are widely regarded as potential alternatives to current therapeutic options for the effective management of various diseases, including COVID‐19.
2. INTRODUCTION TO NUTRACEUTICALS
Nutraceuticals are well‐known compounds in the form of nutrients and pharmaceuticals that provides benefits in terms of medical and health by preventing and treating any disease. Previously, several publications demonstrated the role of nutraceuticals in the management of COVID‐19. A detailed discussion on the role of nutraceuticals in improving human health and attenuating disease complications has been mentioned in the next sections of the manuscript.
3. NUTRACEUTICALS AND THE MANAGEMENT OF COVID
3.1. Management of acute symptoms
COVID‐19 is associated with a condition “cytokine storm” induced by the virus that results in a massive release of proinflammatory cytokines leading to severe inflammatory symptoms in various organs including the lungs (Ragab et al., 2020). Apart from this, COVID‐19 infection also poses a high risk of patients being malnourished. Therefore, an effective nutritional approach could be one of the promising strategies to alleviate the worsening of various acute symptoms. There are reportedly various nutraceutical therapies implemented in hospital settings to improve patients' health. The body's immune response to rapidly replicate the corona viral proteins leads to symptoms of fever, pain, malaise, dyspnoea, loss of appetite, and dry cough (Donma & Donma, 2020; Parasher, 2021). In some cases, nausea/vomiting and diarrhea could precede fever and respiratory symptoms (Derosa et al., 2021). Several nutraceuticals including probiotics, polyphenols, high molecular weight polysaccharides, lectins, and berberine are being proposed to be protective agents against the symptoms of COVID‐19 in infected patients. Some of these nutraceuticals are reported to be promising prophylactic agents and they could possibly reduce the burden and severity of the COVID‐19 disease (Derosa et al., 2021). Commercially available nutraceutical products such as selenium, zinc, ascorbic acid/vitamin C, and vitamin A have possibly benefited from reducing acute symptoms by boosting the immune response (Jayawardena et al., 2020). There are plenty of herbal plant‐based nutraceutical formulations that could be potentially used to target each of the symptoms of COVID‐19. A recent review has proposed several Traditional Chinese nutraceutical‐based approaches for controlling fever symptoms in COVID‐19 patients by including medicinal plants such as Bupleuri radix, Scutellariae radix, Chuanxiong rhizome, Cinnamomi ramulus, Forsythiae fructus, and Lonicera japonica that possess significant antipyretic activity. Furthermore, single compounds such as Saikosaponin A, Baicalin, Baicalein, Ephedrine, and Geniposide are also well known for their antipyretic activity (Ma et al., 2021). Some of these herbal‐based medicines are combined to formulate a complex prescription (for example, Qingkailing injection and Shuang‐Huang‐Lian Preparation) for the treatment of fever (Gao et al., 2013, 2014). Similarly, for the management of pain, plants such as Nigella sativa could be beneficial as this plant is already well known to possess analgesic and antipyretic properties (Oskouei et al., 2018). α‐Hederin and nigellidine are the active ingredients of Nigella sativa and multiple in silico studies have proven that these compounds could be possible inhibitors of SARS CoV‐2 (Koshak & Koshak, 2020). A clinical trial involving Nigella sativa supplement to investigate its efficacy in mild symptomatic COVID‐19 patients is ongoing (Koshak et al., 2020). A recent systematic review also highlighted those Chinese herbal medicines can be used in the treatment of mild to moderate COVID‐19 and they are very effective in the reduction of symptoms of fever and cough in COVID patients (Du et al., 2021). The illustration (Figure 1) shows the role of Nutraceuticals in the management of COVID‐19.
FIGURE 1.
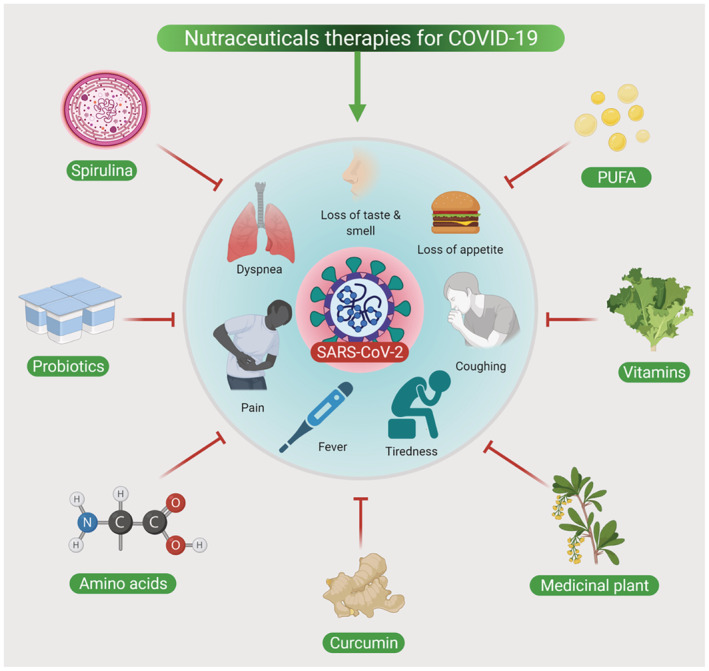
Management of COVID‐19 symptoms by nutraceuticals
Loss of appetite during COVID is due to the leptin hormone and garlic is known to recover the appetite by decreasing the leptin concentrations in the body (Donma & Donma, 2020). A naturopathic treatment strategy consisting of a multi‐nutrient, herbal and probiotic‐based treatment was designed to investigate its efficacy in mild and moderate COVID‐19 patients. The primary aim of this approach was to measure the safety of the treatment while the secondary aim was to observe an alteration in symptoms, progression to disease severity, the incidence of long COVID, and time taken for recovery. Interestingly, this treatment approach appeared to be well‐tolerated without any side effects and there was a resolution of symptoms associated with COVID‐19 infection in all patients suggesting the clinical benefit of this strategy and warrants further clinical trials with COVID‐19 cases (Barber et al., 2021). Nutraceuticals are also proven to be beneficial to non‐intensive care unit (ICU) COVID patients with loss of appetite. A recent study from Italy during the COVD‐19 pandemic investigated a short age‐adjusted nutritional risk screening in 94 non‐ICU patients (68 of these were >70 years of age). These patients received a personalized nutritional plan based on their body conditions and the plan consisted of a high‐protein and high‐calorie pureed diet, oral nutritional supplements, and/or artificial nutrition. The nutritional treatment was well tolerated by the patients. Unfortunately, 19.1% of the patients were dead and they were mostly elderly women with high body mass indices. Seventy‐two patients scored positive on at least one nutritional risk screening item. Notably, the patients whose overall energy and protein needs were not met were elderly and they had high mortality than patients whose energy needs were fulfilled. This clinical experience of a nutritional plan for COVID‐19 highlights the importance of nutraceuticals for patients with COVID‐19 (Formisano et al., 2021). Collectively, this information suggests that nutraceuticals can be a promising approach to the treatment of acute symptoms of COVID.
3.2. Nutraceuticals and immune response—innate, adaptive, and combined
3.2.1. Probiotics
Probiotics are already well established as beneficial nutraceuticals to the host to battle against a range of diseases as they help to modulate local immunity (by maintaining the well‐being of the gut microbiome and boosting the gut health) and systemic immunity (by stimulating specific/non‐specific immune response). Therefore, the use of probiotics is practical to prevent or combat several illnesses including virus infections (Kanauchi et al., 2018). According to the Food and Agriculture Association, probiotic bacteria must have the following features; (a) the ability to survive and grow in the intestine; (b) impart favorable activity in the body; (c) non‐toxic and non‐pathogenic; (d) protect from microorganisms that are known to cause harm through various mechanisms; (e) lack transferable antibiotic resistance (Imran et al., 2022; Lopez‐Santamarina et al., 2021; Morelli & Capurso, 2012). Probiotics can regulate both innate and adaptive immune systems by modulating the functions of key immune cells such as dendritic cells, macrophages, and T and B lymphocytes (Gasmi et al., 2021). Probiotics primarily exert two different immunomodulatory functions: first, their immunostimulatory function which involves interleukin (IL)‐12 production [a cytokine that regulates the T‐cell and natural killer (NK)‐cell responses, stimulates interferon‐γ (IFN‐γ) production, and helps T helper 1 (Th1) differentiation] and second, their immunoregulatory effect that includes IL‐10 stimulation and Treg cell activation by Th2, dendritic cells, B cells, and monocytes for adaptive immunity of the host (Chiba et al., 2010; Trinchieri, 2003). The combination therapy consisting of probiotic strains of Lactobacillus and Bifidobacterium, vitamins, and minerals were found to be beneficial over control therapy (vitamins and minerals) to decrease the duration and the severity of an influenza‐induced common cold. Intriguingly, this therapy demonstrated an increase in the number of key immune cells; T‐helper cells, cytotoxic T cells, and T suppressor cells (de Vrese et al., 2006). During the asymptomatic stage and acute symptoms stage of COVID‐19 infection, boosting immune responses by probiotics to eliminate the virus and halt disease progression to severe stages is extremely beneficial through a network of signals mediated by probiotics of the bacterial origin or their cell wall structure (Sundararaman et al., 2020). Taken together, we can speculate that probiotics are a good option for the therapeutic management of COVID and long‐COVID. However, the current evidence is too premature to make any valid conclusions on the applications of a specific probiotic strain.
3.2.2. Vitamin D
Vitamin D is another well‐known nutraceutical candidate that stimulates innate immunity and modulates acquired immunity in diseases such as tuberculosis and its supplement can help in the prevention of acute respiratory tract infections (Brighenti et al., 2018; Prietl et al., 2013). Epithelial cells of the airway constitutively express the vitamin D receptor that enables the protective function of vitamin D against pathogens. Vitamin D may target cell signaling pathways involved in airway inflammation to show beneficial activity in respiratory diseases such as asthma and lung infection (Agrawal et al., 2013). An in vitro experiment has revealed that vitamin D inhibits the nuclear factor kappa B (NF‐κB) pathway activation through the up‐regulation of NF‐κB inhibitory protein IκB kinase β (IKKβ) (Chen et al., 2013). The inhibition of the NF‐κB pathway by Vitamin D is also confirmed in a mice model of allergic asthma induced by the allergen ovalbumin. Vitamin D also reduces the levels of pro‐inflammatory type 1 cytokines including IL‐12, IL‐16, IL‐8, tumor necrosis factor (TNF)‐α, IFN‐γ and increases type 2 cytokines including IL‐4, IL‐5, IL‐10, and regulatory T cells (Jeffery et al., 2009; Lemire et al., 1995). As mentioned earlier COVID‐19 causes cytokine storm. Vitamin D could be another promising nutraceutical supplement for regulating the worsening of symptoms by inhibiting these pro‐inflammatory cytokines. It has been observed that human bronchial epithelial cells infected by the SARS‐CoV virus generate various NF‐κB‐mediated cytokines, including IL‐6 and IL‐8. Therefore, Vitamin D could be a promising nutraceutical to mitigate airway inflammation (Yoshikawa et al., 2009). Apart from controlling inflammation, Vitamin D also upregulates the levels of antioxidant gene nuclear factor, erythroid 2‐related factor 2 (Nrf2) to prevent mitochondrial stress, lipid peroxidation, protein oxidation, and DNA damage (Wimalawansa, 2019). As deficiency of vitamin D is common, to reduce the risk of infections such as influenza and COVID‐19, it is recommended to take 10,000 IU/day of vitamin D3 for a few weeks to increase the level of 25 dihydroxy vitamin D [25(OH)D] in the body, followed by tapering down the dose to 5000 IU/d until the goal to increase 25(OH)D level to more than 40–60 ng/ml (100–150 nmol/L) is achieved (Grant et al., 2020). This high‐dose vitamin D is reported to be effective, tolerable in high‐risk older patients, and immediately accessible for the treatment of COVID‐19 (Annweiler et al., 2020). A pilot study has shown that a high dose of calcifediol or 25(OH)D administered to COVID‐19 patients remarkably reduced the need for ICU treatment during hospitalization. While 25(OH)D seems to decrease the disease severity, larger cohort studies with groups properly matched will be required to validate the use of 25(OH)D in COVID‐19 (Entrenas Castillo et al., 2020). Nevertheless, the literature acknowledges that specific high‐quality data are needed to demonstrate the efficacy of vitamin D supplementation in the prevention of COVID‐19 (Zemb et al., 2020).
3.2.3. Vitamin C
As there are limited proven drugs for the effective management of COVID‐19, vitamin C can be an adjunctive therapy for the prevention and amelioration of COVID‐19 infection as it possesses antioxidant, anti‐inflammatory, and immunomodulating activity (Holford et al., 2020). Vitamin C has a wide range of functions, and it acts on various cells of the immune system. For example, Vitamin C inhibits various forms of T‐cell apoptosis (Campbell et al., 1999) and drastically decreases the levels of high‐sensitivity C‐reactive protein, IL‐6 (Ellulu et al., 2015). Vitamin C can boost the immune system by supporting the cells of the innate/adaptive immune system. Vitamin C is also known to accumulate in neutrophils and enhance chemotaxis, phagocytosis, and production of ROS to kill the pathogens. Vitamin C supplementation is known to prevent respiratory tract infections although there is conflicting evidence if Vitamin C prevents common cold (Carr & Maggini, 2017). A recent clinical trial has revealed that patients with COVID‐19 have fivefold less vitamin C in their blood compared to healthy volunteers (2.00 mg/L in COVID‐19 patients versus 9.23mg/L in healthy volunteers). Administration of high‐dose intravenous Vitamin C (100 mg/kg/day) to these COVID‐19 patients increased the plasma Vitamin C to 13.46mg/L (slightly higher than healthy volunteers). Ultra‐high‐performance liquid chromatography‐tandem mass spectrometry may assist to quantify Vitamin C levels in COVID‐19 patients and could be helpful to precisely measure the levels of Vitamin C and thereby calculate the dosage of Vitamin C supplementation required to bring its level to baseline (Xing et al., 2021). Another clinical trial found that low dose of Vitamin C (1000 mg once daily for a median duration of 11 days) as an adjunctive therapy in COVID‐19 patients did not benefit with respect to the mortality rate, but it lowered the incidence of thrombosis (Al Sulaiman et al., 2021). The combination therapy of Vitamin C (500mg four times daily) along with vitamin A (25,000 IU daily), B complex (one amp daily), and vitamin D (60,000 IU daily) for 7 days in COVID‐19 patients significantly decreased disease severity and inflammation. Among inflammatory cytokines, TNF‐α, IL‐6, and C‐reactive protein were significantly decreased in COVID‐19 patients through this multivitamin supplementation approach (Beigmohammadi et al., 2021). Other similar trials investigating the efficacy of high‐dose vitamin C for the treatment of severe COVID‐19 are ongoing and the findings will be disseminated soon (Liu et al., 2020).
3.2.4. Zinc (Zn)
Zinc has diverse biological functions in our body and is therefore considered as an essential substance. It is involved in various cellular processes such as growth, DNA synthesis, RNA transcription, as a cofactor, and as a structural element (Read et al., 2019). Zinc possesses immune‐boosting activity and exerts antiviral and antioxidant functions (Read et al., 2019). Due to these properties, it has the potential to be a supportive treatment in COVID‐19 patients (Shakoor et al., 2021). It has been proposed that zinc could enhance the efficacy of other treatment modalities such as hydroxychloroquine which is currently under investigation (Rahman & Idid, 2021). Experimental animal models have shown that Zn deficiency leads to oxidative stress, production of TNF‐α, increased expression of vascular cell adhesion molecule and results in airway remodeling that can be partly reversed by the supplementation of Zinc (Biaggio et al., 2010). Similarly, in vitro studies have shown that Zinc deficiency results in increased IL‐6, IL‐1β production, and increased expression of intercellular adhesion molecule 1 that helps in leukocytes' extravasation (Wong et al., 2015). A recent cross‐sectional study reported that serum samples from 25 out of 34 (73.5%) COVID‐19 non‐survivors and 40.9% (56 out of 137) of survivors had their Zinc levels below the threshold for Zinc deficiency (<638.7 μg/L) (Heller et al., 2021). Therefore, Zinc supplementation may be helpful to prevent “cytokine storm” in COVID‐19. Moreover, Zinc enhances IFN‐α function by an order of magnitude that can be helpful to battle IFN antagonism by SARS‐CoV‐2 proteins (Berg et al., 2001). In COVID‐19 patients, excessive amounts of circulating neutrophils (neutrophilia) is observed (Qin et al., 2020). It is known that Zinc gluconate supplementation can reduce airway neutrophil infiltration (Morgan et al., 2011). The level of Zinc in the body is a critical factor that determines anti‐viral immunity, as Zinc deficient subjects are considered at a risk of acquiring viral infections (for example: hepatitis C and HIV) (Read et al., 2019). Zinc is also known to influence virus entry into the cells, fusion, rapid replication, viral protein translation, and virus budding of respiratory viruses (Lazarczyk & Favre, 2008; Read et al., 2019) An in vitro study has shown that Zn2+ can inhibit coronavirus/SARS‐CoV and arterivirus RNA polymerase activity and can impair the viral replication (te Velthuis et al., 2010). A pilot study (phase IIa trial) investigating the safety and feasibility of high‐dose intravenous zinc (HDIVZn) in COVID‐19 patients admitted to the hospital found that administration of HDIVZn (n = 15) and placebo (n = 18) per day for 1 week to 15 COVID‐19 patients increased the Zinc levels above the deficiency threshold of 10.7 μmol/L (p < .001) on Day 6 in the HDIVZn group but not in the placebo group. HDIVZn administration to COVID‐19 patients was safe, feasible, and was not associated with any adverse event as only 3 patients experienced minimal infusion site irritation (Patel et al., 2021). Thus, Zinc could be considered as a promising supportive therapy against COVID‐19 disease due to its immunomodulatory and antiviral activities (Zhang & Liu, 2020).
3.2.5. Curcumin
Curcumin has diverse beneficial functions in our physiological system such as, antioxidant, anticancer, anti‐inflammatory, and antimicrobial (bacterial, viral, fungal) (Hardwick et al., 2021; Patel et al., 2020). The antiviral activity of curcumin resulting in the inhibition of viral entry to the cell, inhibition of encapsulation of the virus, and viral protease makes it a potential candidate drug for the management of SARS‐CoV‐2 (Zahedipour et al., 2020). A recent randomized control trial evaluated the efficacy of the nano‐micellar form of curcumin formulation to modulate the inflammatory cytokines in COVID‐19 patients. Twenty COVID‐19 patients receiving 160mg of nano‐curcumin daily for 14 days showed a significant decrease (compared to the COVID‐19 patients receiving placebo) in mRNA expression of IL‐6 and IL‐1β in activated peripheral blood mononuclear cells PBMC. Similarly, a significant decrease in IL‐6 and IL‐1β secretions (measured by ELISA) was also observed in the serum of COVID‐19 subjects receiving nano‐curcumin compared to placebo. This suggests the anti‐inflammatory role of curcumin to improve clinical outcomes and overall recovery (Valizadeh et al., 2020). Another randomized control trial found that curcumin nanomicelles administration to COVID‐19 patients decreased the serum level of IFN‐γ and IL‐17 while increasing the levels of IL‐4 and TGF‐β compared to the placebo group. This suggests that nano‐curcumin formulation can be administered to COVID‐19 patients in the inflammatory phase to hasten the recovery (Hassaniazad et al., 2021). As powder curcumin form has very low bioavailability, researchers/pharmaceutical industries are designing various highly bioavailable forms of curcumin to increase cellular uptake and efficacy. CurcuRougeTM is a recently developed curcumin formulation with enhanced bioavailability. A double‐blind randomized control trial found that administration of CurcuRougeTM for 4 weeks significantly decreased the elevated neutrophil/lymphocyte levels in healthy elderly subjects (Kishimoto et al., 2021). As COVID‐19 patients have elevated neutrophil/lymphocyte ratio, CurcuRougeTM could be a better alternative to treat COVID‐19 patients (Zeng et al., 2021). Collectively, these clinical studies found potent immune‐boosting and anti‐inflammatory effects of curcumin. Therefore, curcumin could be a beneficial nutraceutical supplement to combat inflammatory diseases due to “cytokine storm” during a COVID‐19 infection (Table 1).
TABLE 1.
Nutraceuticals targeting immune response—innate, adaptive, and combined
| Nutraceuticals | Study model | Findings | Reference |
|---|---|---|---|
| Probiotics | Probiotics strain of Lactobacillus and Bifidobacterium, vitamins, and minerals | Decrease the duration and the severity of influenza‐induced common cold. This therapy was able to increase the number of key immune cells; T‐helper cells, cytotoxic T cells, and T suppressor cells | (de Vrese et al., 2006) |
| Probiotics strain of Lactobacillus plantarum NCIMB 8826 against RSV, pneumovirus | TLR‐dependent inflammatory response | (Al Kassaa et al., 2014) | |
| Probiotic strain of Lactobacillus rhamnosus M21 against pneumonia and influenza | Increases interferon‐γ and interleukin‐2 | (Song et al., 2016) | |
| Probiotic strain of Lactobacillus casei DN‐114001aganist RTI, rhinopharyngitis, and influenza | Enhanced defensin expression and innate immunity | (Guillemard et al., 2010) | |
| Vitamin | Patients aged ≥ 65 years with COVID‐19 (high‐risk older patients) | High dose of calcifediol or 25(OH)D administered to COVID‐19 patients remarkably reduced the need for ICU treatment during hospitalization | (Annweiler et al., 2020) |
| To evaluate the efficacy and safety of using ascorbic acid in supplemental doses as adjunctive therapy for critically ill (ICU admitted) COVID‐19 patients | Low dose of Vitamin C (1000 mg once daily for a median duration of 11 days) as an adjunctive therapy in COVID‐19 patients did not benefit in mortality rate but it lowered the incidence of thrombosis | (Al Sulaiman et al., 2021) | |
| Multivitamin supplement | The combination therapy of vitamin C (500mg four times daily) along with vitamin A (25,000 IU daily), B complex (one amp daily), and D (60,000 IU daily) for 7 days in COVID‐19 | The combination therapy significantly decreased disease severity and inflammation. Among inflammatory cytokines, TNF‐α, IL‐6, and C‐reactive protein was significantly decreased in COVID‐19 patient by this multivitamin supplementation approach | (Beigmohammadi et al., 2021) |
| Zinc | In vitro study on Vero‐E6 cells infected with SARS‐CoV | Zn2+ inhibits coronavirus/SARS‐CoV and arterivirus RNA polymerase activity and impairs the viral replication | (te Velthuis et al., 2010) |
| A pilot study (phase IIa trial) investigating the safety and feasibility of high‐dose intravenous zinc (HDIVZn) in COVID‐19 patients admitted to hospital |
Administration of HDIVZn and placebo per day for 1 week to 15 COVID‐19 patients increased the level Zn level above the deficiency threshold of 10.7 μmol/L on Day 6 in the HDIVZn group but not in the placebo group. HDIVZn was found to be safe, feasible, and not associated with any adverse events as only 3 patients experienced minimal infusion site irritation |
(Patel et al., 2021) | |
| Curcumin | To identify the effects of nano‐curcumin on the modulation of inflammatory cytokines in COVID‐19 patients | COVID‐19 patients receiving 160mg of nano‐curcumin daily for 14 days showed a significant decrease (compared to the COVID‐19 patients receiving placebo) in mRNA expression of IL‐6 and IL‐1β in activated peripheral blood mononuclear cells PBMC. Similarly, a significant decrease in IL‐6 and IL‐1β secretion (measured by ELISA) was also observed in serum of COVID‐19 receiving nano‐curcumin compared to placebo | (Valizadeh et al., 2020) |
| Berbamine, an alkaloidal moiety presents in the plant Berberis amurensis | In vitro study to investigate if berbamine effectively inhibited the entry of SARS‐CoV‐2‐S or MERS‐CoV‐S into host cells (primary human lung fibroblasts and Vero‐E6 cell line) | Berbamine efficiently protected the cells from different coronaviral (SARS‐CoV‐2 and MERS‐CoV) infections by inhibiting the transient receptor potential cation channel, mucolipin subfamily (a Ca2+ permeable non‐selective cation channels in endosomes and lysosomes) leading to impairment in endolysosomal trafficking of viral receptors ACE2 and DPP4 | (Huang et al., 2021) |
| Resveratrol and its analog pterostilbene | In vitro study on air‐liquid interface cultured human primary bronchial epithelial cells to test the efficacy of resveratrol and pterostilbene to inhibit SARS‐CoV‐2 replication | Resveratrol and its analog pterostilbene inhibited the SARS‐CoV‐2 viral replication in human primary broncho epithelial cells up to 48 hours post‐infection | (Ter Ellen et al., 2021) |
3.3. Management of extra‐pulmonary complications in COVID‐19 by nutraceuticals
3.3.1. Mental health—neurotransmitters, anxiety, depression
COVID‐19 systems are accompanied by short‐ and long‐term neuropsychiatric symptoms and long‐term brain sequelae. In addition, few patients also experienced loss of sense of smell, increased stress levels, cognitive and attention deficits, symptoms of anxiety, depression, seizures, and even suicidal behavior (Cheng et al., 2004; Lee et al., 2007; Meinhardt et al., 2021; Woo et al., 2020). These symptoms present prior, during, and after patients develop respiratory symptoms (Woo et al., 2020) suggesting independent brain damage. To date, few studies have evaluated the possible mental health outcomes of COVID‐19 infection demonstrating that in patients with COVID‐19 during their acute phase had a prevalence of 96.2% of post‐traumatic stress disorder symptoms (Bo et al., 2021), 34.72 and 28.47% of anxiety and depression symptoms respectively. Moreover, few studies have also reported post‐COVID‐19 neuropsychiatric symptoms in 20% to 70% of patients lasting for longer periods even after respiratory symptoms were resolved, suggesting the involvement of the brain (Woo et al., 2020). Taken together, these data indicate that infection with COVID‐19, can yield an adverse impact on the well‐being of mental health both short‐ and long‐term.
3.3.2. COVID‐19‐related inflammation and neurotoxicity
Interestingly, studies have reported that patients with severe COVID‐19 infection experience increased serum levels of pro‐inflammatory cytokines including IL‐1β, IL‐6, IL‐10, and TNF‐α. This increase in cytokines could damage the BBB thus affecting its permeability that enables TNF‐α to directly cross the blood‐brain barrier (BBB) leading to the activation of microglia and astrocytes (Liddelow et al., 2017; Pan & Kastin, 2007). These activated microglia secrete inflammatory mediators, including glutamate, quinolinic acid, complement proteins, ILs, and TNF‐α (Vasek et al., 2016). Importantly, an increase in quinolinic acid results in higher glutamate levels and upregulation of NMDA receptors (glutamate and ion channel protein receptor), conceivably inducing altered memory, neuroplasticity, and hallucinations.
Moreover, increased inflammation activates key enzymes such as indoleamine dioxygenase, that ultimately, metabolizes tryptophan to kynurenine instead of serotonin (Roman & Irwin, 2020). Indeed, neurotransmitter release was affected in interferon (IFN)‐α treated patients as they presented with depression and fatigue severity. Since inflammation leads to reduced neurotransmission, cognitive and psychomotor activity, depression, and suicidal behavior, in patients, studies have shown that they poorly respond to traditional anti‐depressants (Roman & Irwin, 2020). Studies have found that individuals with major depressive disorder have elevated levels of IL‐1 and IL‐6 in blood and cerebrospinal fluid (CSF) and C‐reactive protein in serum. This suggests that elevated levels of ILs have a significant correlation with brain glutamate levels in patients (Boldrini et al., 2019; Mahajan et al., 2018). Thus, neuroinflammation may contribute to reduced activity of neurotransmitters and increased excitotoxicity (Roman & Irwin, 2020).
3.3.3. Management of mental health by nutraceuticals
3.3.3.1. Omega 3 denosyl‐Methionine
Epidemiological studies have reported that the prevalence of decline in anxiety and depression is associated with a high intake of ω‐3 polyunsaturated fatty acids (ω‐3 PUFAs). The major source of this substance is fish. Interestingly, countries with higher fish consumption support the finding that fish oil may be a key source to prevent mental health disorders such as anxiety and depression as they are less common in those countries.
Importantly, studies have shown that G‐proteins within the lipid rafts are the main sites of action where PUFAs at the cell membrane interact with. Given that it interacts with the PUFAs present at the cell membrane, every change in protein location at this site will be able to translate alterations in the signaling of neurotransmitters (Burhani & Rasenick, 2017). In addition, these proteins are also key targets for anti‐depressant agents. This suggests that the lipid rafts may play an important role in the treatment efficacy and therapeutic outcomes (Burhani & Rasenick, 2017; Djuricic & Calder, 2021; Torres et al., 2020). A meta‐analysis and meta‐regression study observed that higher dose supplementation of ω‐3 PUFAs particularly, eicosapentaenoic acid (EPA) in patients with mental health disorders had a significant clinical benefit (Liao et al., 2019; Mocking et al., 2016). Thus, the findings from various studies indicate that ω‐3 PUFAs with EPA may have pleiotropic effects including anti‐inflammatory action and neuroprotective effect (i.e., the modification of signaling membrane proteins and the endocannabinoid effect); all of which contribute to anti‐depressant action. Although these pleiotropic effects have been appreciated by various authors, the elucidation of these mechanisms will prove beneficial.
3.3.3.2. Vitamin D
The main source of fat‐soluble Vitamin D specifically Vitamin D3 (also known as 1, 25‐dihydroxycholecalciferol or calcitriol), i.e., 7‐dehydrocholesterol is the sunlight. It is produced in the skin upon exposure to sunlight (Mostafa & Hegazy, 2015). Vitamin D3 is more efficient and is mainly found in fish oil, cod fish liver, or milk. Interestingly, clinical studies have demonstrated that vitamin D deficiency in patients with depression has an association with the symptoms and this is because vitamin D can influence the levels of serotonin and melatonin thereby, affecting mood, and sleep patterns (Gao et al., 2018; Huiberts & Smolders, 2021). Notably, studies have demonstrated the inverse relationship between vitamin D and melatonin thus indicating that both may share common mechanisms that could be relevant for brain disorders (Gao et al., 2018; Huiberts & Smolders, 2021).
Moreover, vitamin D mediates the synthesis of brain serotonin from amino acids such as tryptophan which ultimately, activates the transcription of the serotonin‐synthesizing gene tryptophan hydroxylase 2 (TPH2) in the brain. Thus, vitamin D in combination with tryptophan supplementation may prove to be a practical therapy for depression. Importantly, studies have shown that imbalance in vitamin D, EPA, or DHA levels can disturb serotonin activation and function significantly (Patrick & Ames, 2014, 2015). Nevertheless, optimal concentrations of vitamin D can enhance the synthesis of serotonin that mimics Monoamine oxidase (MAO) inhibitors thus, increasing serotonin in the central nervous system (CNS) (Sabir et al., 2018). These findings suggest that vitamin D is crucial for brain function. However, further elucidation is required in deriving the optimal time of administration, and its dosage based on inter‐individual requirements (Patrick & Ames, 2015; Sabir et al., 2018).
3.3.3.3. Methylfolate
Studies have shown that patients with depression have reduced levels of folate in their serum and diet (Bender et al., 2017). Interestingly, genetic polymorphism in the Methylenetetrahydrofolate reductase (MTHFR) gene, the MTHFR C677T variant is associated with an increased risk of depression and other psychiatric disorders (Wan et al., 2018). Thus, supplementation with folate and its different forms such as 5‐MTHF has proven to be effective in the treatment of patients with depression (Fava & Mischoulon, 2009). Current studies support the possible use of 5‐MTHF in the clinical management of mental disorders, prominently as adjunctive therapy in combination with anti‐depressants (Fava & Mischoulon, 2009).
3.3.3.4. Creatine and amino acids
Creatine is an organic compound naturally synthesized in our cells, also found exogenously in different food products, such as fish and meat. Creatine is a well‐known supplement among athletes, as this component exerts a plethora of ergogenic benefits. However, recent studies have elucidated the central role of creatinine which is an organic compound naturally synthesized in human cells, and also found exogenously in various foods such as fish and meat. Studies have also reported the role of this substance in health and disease conditions as it has an array of targets both at the cellular and molecular levels (Kreider & Stout, 2021). The key effects of creatine include its role in the regulation of metabolic activities by decreasing the production of reactive oxygen species (ROS) and also as a potential anti‐inflammatory agent by diminishing homocysteine levels (Clarke et al., 2020). The synthesis of creatine occurs in the liver, kidney, and pancreas from amino acids such as glycine, methionine, and arginine. Indeed, studies have shown that creatine is a central molecule that is involved in the metabolism of amino acids, notably in the met cycle, where its synthesis account for 40% (Brosnan et al., 2011). In particular, with the brain, creatine supplementation is associated with significant benefits in regulating cognitive function, especially post‐deficiency that is induced by acute stressors such as exercise, stress, sleep deprivation, or under chronic pathological conditions (Balestrino & Adriano, 2019). Studies have also shown that patients with depression have demonstrated a reduced intake of dietary creatine thus affecting their creatine levels overall (Bakian et al., 2020) and abnormal metabolism of creatine in the brain (Pazini et al., 2019). Thus, supplementation of creatine may be a potential therapeutic approach for depression. Studies have also shown that amino acids such as phenylalanine and tyrosine both are key regulators in the synthesis of neurotransmitters, dopamine, and norepinephrine (Lakhan & Vieira, 2008), thus, affecting the neuroinflammatory response in the brain of patients suffering from depression (Miller & Raison, 2016; Strasser et al., 2017). Indeed, studies have shown that patients with low levels of dopamine may benefit from the supplementation of tyrosine (Mouret et al., 1988). Notably, clinical studies have shown that higher consumption of dietary tryptophan reduces symptoms related to depression due to its direct effects on the synthesis of serotonin synthesis (Kikuchi et al., 2021; Lindseth et al., 2015; Turner et al., 2006). Thus, tryptophan may be a potential therapy for depression.
3.3.3.5. Plant‐derived bioactive compounds
Growing evidence suggests that bioactive compounds such as polyphenols that are synthesized by plants act as strong antioxidants in the management of various diseases (Gonzalez, 2020; Singla et al., 2019). Polyphenols are classified into two subtypes, that is, flavonoids and non‐flavonoids. Quercetin is a key flavonoid that possesses antidepressant properties including (Panche et al., 2016) an improved functioning of the monoaminergic system, GABAergic transmission, brain‐derived neurotrophic factor (BNDF), and amelioration of the neuroinflammatory response in the brain (Hritcu et al., 2017). Notably, curcumin—a non‐flavonoid compound present in Curcuma longa has a beneficial effect in the treatment of depression. Apart from the anti‐oxidant and anti‐inflammatory properties, Curcumin also has shown its role in the improvement of BDNF activity, serotoninergic, and dopamine transmission (Trebaticka & Durackova, 2015). Indeed, studies have shown that Curcumin may be a potential therapy in the clinical management of anxiety and depression (Fusar‐Poli et al., 2020).
3.3.4. COVID‐19 and depression/peripheral neuropathy symptoms/cognitive impairment
Globally, several cohort studies conducted in hospitals have reported an association between neuro‐behavioral implications with COVID‐19. Anosmia, ageusia, anxiety, stress, and depression are some of the neurological manifestations reported in patients suffering from COVID‐19. Some of the symptoms have a direct relation to a viral infection, and some of them are results of changes in lifestyle as well as due to certain required restrictions during lockdown that have caused quarantine blues. Quarantine blues further lead to anxiety, which is further associated with disturbance in sleep pattern, duration, and depression. Moreover, SARS‐CoV‐2 is associated with inflammatory responses causing the excessive generation and release of cytokines. This has led to the development of other comorbidities. Neuronal implications and their involvement in COVID‐19 mainly correspond to three situations, that is, (1) neurological manifestations of viral infection, (2) infection in patients with neurological co‐morbidity, and (3) post‐infective neurological complications (Sharma et al., 2021). All these factors have created a major impact on mental health apart from the pulmonary system and have triggered neuro‐immunological reactions. It is well established that anxiety‐induced inflammatory responses are not only limited to cellular immunity but also associated with humoral immunity. As a consequence, it is suggested evidently that individuals suffering from chronic anxiety are more susceptible to infections and inflammatory responses (Rammal et al., 2010). Although there is no standard line of treatment available for COVID‐19 worldwide, physicians recommend nutraceuticals in order to boost immunity and for controlling neuro‐behavioral implications (Sharma et al., 2021). Nutraceuticals have dual applications including preventive and therapeutic. During previous similar COVID‐19 outbreaks like SARS‐CoV and MERS‐CoV, few nutraceuticals were studied and observed to have a significant influence on the prevention of the occurrence of the disease (Savant et al., 2021). Since ancient times, due to their anti‐viral property and potential benefits on the nervous system, nutraceuticals are widely used for prophylaxis and as an adjunct therapy to deal with various viral infections and associated neurological manifestations (Subedi et al., 2021). It is evident that the functional network and activity of the brain are related to mood, depression, and anxiety which are mediated by neuronal signaling. The neuronal signaling is further associated with the release of neurotransmitters at synapses. Several nutraceuticals and dietary supplements have proven to be a rich source of various amino acids (tyrosine and tryptophan) which are precursors of several neurotransmitters like dopamine, norepinephrine, and serotonin. Studies and clinical trials have shown that supplementation of these agents could improve cognitive performance during stressful conditions. Several water‐soluble vitamins (e.g., vitamin C), fat‐soluble vitamins (vitamin D), minerals (zinc, magnesium, manganese, and selenium) along with plants (Bacopa monnieri, Withania somnifera, and Curcuma longa) that contain several bioactive substances such as alkaloids, and flavonoids are proven to be beneficial. These bioactive compounds are also observed to have potential neuroprotective benefits (Ghosh, 2021). Plant‐based nutraceuticals like apigenin and luteolin, which belong to the class of flavonoids, are suggested to activate the nitric oxide signaling pathway and regulate cyclic guanosine monophosphate levels (Roberts et al., 2013). Consequently, it causes vascular relaxation resulting in lowering the elevated blood pressure and heart rate during sleep. These are the important processes of non‐rapid eye movement (REM) sleep, thus these flavonoids and related biomolecules influence sleep patterns and anxiety processes (Nami et al., 2020). Certain plant‐based bioactive compounds like valerenic acid, mahanimbine, and coumarins have sedative, anxiolytic, and antidepressant activities (Batra et al., 2018; Jung et al., 2015; Sharma et al., 2017). Studies have shown that valerenic acid has benzodiazepine‐like tranquilizing activity which acts by increasing the levels of gamma‐aminobutyric acid (GABA). Therefore, valerenic acid produces a calming effect along with the anxiolytic activity.
Among the vitamins, vitamin D is widely studied to explain its role in brain health. Studies have explained that vitamin D reduces the increased levels of calcium in neurons which is one of the important factors of depression. Also, it is suggested by several researchers that vitamin D regulates the survival of hippocampal neurons through the release of nerve growth factors. Vitamin D insufficiency is also correlated with cognitive impairment, psychosis, and an alteration in the level of neurotransmitters (Berridge, 2017; Gezen‐Ak et al., 2014). Minerals, namely zinc have been demonstrated to have antidepressant activity. Zinc is a trace mineral required for the normal function of the brain which also includes the uptake of neurotransmitters like serotonin and acts as a cofactor to various enzymatic reactions including neurotransmitter activity in the central nervous system (Levenson, 2006). Several studies including clinical trials have reported that zinc has a protective effect against brain damage as well as improves behavioral and cognitive activities (da Silva et al., 2021; Partyka et al., 2011). Zinc levels can be applied as a biomarker to determine depression or anxiety, as reduced levels of zinc have been observed in depressed patients. Possible hypotheses suggested in several studies for this correlation are (1) anxiety‐induced activation of immunity and elevated inflammatory responses lead to utilization of zinc that consequently causes a reduction in the level of zinc. (2) Increased production of cortisol in depressed patients promotes the synthesis of metallothionein (a zinc‐binding protein) causing the reduction in zinc levels (Levenson, 2006).
Turmeric extracts
Studies have shown that turmeric greatly improve musculoskeletal pain with less side effects as well as adverse effects compared to NSAIDs such as Ibuprofen (Chandran & Goel, 2012; Daily et al., 2016; Kuptniratsaikul et al., 2009, 2014). Furthermore, propriety formulations containing turmeric extracts have been developed across the globe by drug manufacturers that have proven to impart a promising effect on improving musculoskeletal health. In addition, several studies have demonstrated that curcumin (BCM‐95®) itself or in combination with NSAIDs such as diclofenac sodium showed greater disease activity scores, improved inflammatory biomarker levels such as C‐reactive protein (CRP) and erythrocyte sedimentation rate (ESR), compared to diclofenac sodium alone (Chandran & Goel, 2012; Shep et al., 2019). Notably, studies have also shown that herbal formulations containing substances like curcumin, gingerols, and piperine, can aid in reducing prostaglandin E2 levels in patients that have musculoskeletal pain to the same extent as NSAIDs (Heidari‐Beni et al., 2020). There is growing evidence of turmeric extracts showing anti‐inflammatory properties such as, decreased production of pro‐inflammatory cytokines such as TNF‐α, IL‐1β, IL‐8, IL‐6, and structural degradation proteases such as matrix metalloproteinases (MMPs), collagenase, and anti‐oxidant properties (Bengmark, 2006; Heidari‐Beni et al., 2020; Khanna et al., 2007; Kim et al., 2012; Oyagbemi et al., 2009; Saja et al., 2007; Yang et al., 2013). Turmeric extracts are well documented to inhibit the NFκB pathway and other proinflammatory signaling pathways including cyclooxygenase (COX)‐2, AP‐1, Egr‐1, STAT (signal transducers and activators of transcription), and mitogen‐activated protein (MAP) kinases (Goel et al., 2001, 2008; Reuter et al., 2011). These data undoubtedly point toward the definite effectiveness of turmeric extracts as a promising therapy in musculoskeletal pain, if administered at an early stage.
Terrestrial botanicals
Interestingly, terrestrial botanicals such as avocado or soybean extracts are being appreciated in literature to have shown positive therapeutic benefits in relieving musculoskeletal pain (Appelboom et al., 2001; Gluszko & Stasiek, 2016). Specifically, avocado or soybean extracts have shown to inhibit the production of cytokines such as IL‐1, IL‐6, IL‐8, and PGE‐2. Moreover, they also promote the expression of TGF‐β and activation of collagen synthesis thereby reducing the production of stromelysin (Boumediene et al., 1999; Henrotin et al., 2003). These data suggest that avocado/soybean can impact both inflammatory and structural proteins that shape the physiology of the musculoskeletal system. Similar effects have been found with the species belonging to the Ginger root family as they aid in blocking the development of inflammatory mediators such as thromboxane, leukotrienes, and prostaglandins and inhibit COX and lipoxygenase which are key factors in arachidonic acid metabolism (Lantz et al., 2007; Niempoog et al., 2012; Nurtjahja‐Tjendraputra et al., 2003; Paramdeep, 2013).
3.3.5. Insomnia/sleep disorders
Treatment options for sleep disorders are mainly associated only with the management of dependence symptoms. This has led to a search for better therapeutic options such as nutraceuticals. Interestingly, various studies have implicated positive effects from nutraceuticals such as caffeine, chamomile, kava kava, cherries, and its extract, valerian, and Lemon balm in the treatment of sleep disorders as most of them are not associated with dependence or withdrawal symptoms (Andrews et al., 2007; Beaumont et al., 2004; Donath et al., 2000; Esteban et al., 2004; Hadley & Petry, 2003; Nicholson et al., 2004; Rowe et al., 2011; Rycroft, 2003).
3.3.6. Cardiovascular disorders (CVD)
Phytosterols
Phytosterols are found in a range of plant products including fruits, vegetables, cereals, seeds, and nuts. They have a molecular skeleton similar to cholesterol thus, possessing their biological activity in treating CVD (Moreau et al., 2002).
Polyphenols
Polyphenols are phytochemicals such as flavonoids, phenolic acids, stilbenes, and lignans that are structurally diverse with widespread distribution in foods of plant origin (Pandey & Rizvi, 2009). Polyphenols extracted from grapes and its derivatives, tea, and cocoa are implicated in the prevention of CVD. Grapes contain phenolic compounds including anthocyanins, flavonols, stilbenes, and phenolic acids, where resveratrol (3,5,4′‐trihydroxy‐trans‐stilbene) is the most extensively studied bioactive compound (Burns et al., 2002; Spacil et al., 2008). Cocoa and its derivatives such as Theobroma cacao are widely used polyphenols in CVD (Andres‐Lacueva et al., 2008). In addition, other derivatives also include anthocyanins, catechins, flavonol glycosides, and procyanidins (Hammerstone et al., 1999; Lee et al., 2003). Polyphenols found in tea include catechins, theaflavins, tannins, and flavonoids. As per the literature, the minimally fermented green tea contains more catechins such as epigallocatechin gallate, epicatechin‐3‐gallate, epigallocatechin, and epicatechin (Khan & Mukhtar, 2007) compared to black tea that is rich in flavins and thearubigins (Balentine et al., 1997).
3.3.7. Musculoskeletal disorders and the influence of nutraceuticals
Prevalence of muscle fatigue, muscle weakness, back pain, myalgia, and arthralgia are the common manifestations observed in COVID‐19. Some of the reports have also mentioned about the association of Guillain‐Barré syndrome with COVID‐19 (Caress et al., 2020). Moreover, prolonged administration of corticosteroids has also impacted bone mineral density resulting in osteoporosis and osteonecrosis (Vaishya et al., 2021). One of the possible reasons for such manifestation is the activation of aggressive inflammatory responses influenced by the viral infection. Thus, identifying the musculoskeletal manifestations associated with COVID‐19 and an early diagnosis would be beneficial to manage the condition at its earliest and this also may ensure immediate recovery. Potassium, phosphorous, zinc, calcium, vitamin D, vitamin C, vitamin B1, B2, B3, B5, and B12, vitamin K2, leucine, omega‐3 fatty acids, phosphatidic acid, folic acid, and creatine are some of the examples of nutraceuticals and dietary supplements that are reported to improve the musculoskeletal health and cognitive functions (Boros, 2013; Deane et al., 2017; Iolascon et al., 2017). All these nutraceuticals and dietary supplements are responsible to prevent osteoarthritis and autoimmune disorders and promote bone formation, regulation of proteins in bone tissue, modulating muscle contraction, collagen synthesis, initiating cell division, and osteoblast activity (Boros, 2013). Apart from all these evidence published in literature regarding the influence of nutraceuticals in managing musculoskeletal manifestations, it is necessary to have accurate information and education regarding the use of appropriate nutraceuticals. Because these are not evaluated for their safety and specific effectiveness by regulatory agencies and a proper regimen and dose intake are of utmost importance to manage musculoskeletal manifestations in an efficient way.
3.3.8. Dermatological infections associated with COVID‐19
Many studies have reported where COVID‐19 infection has caused various dermatological symptoms such as rashes, itching, urticaria and other dermatitis‐related infections that affect the body, hands, and faces (Darlenski & Tsankov, 2020). In one of the studies, Yan and co‐workers reported the problems related to the skin caused by the SARS‐CoV‐2 virus. Health care personnel who have been assigned for controlling and reducing the SARS‐CoV‐2 virus infection, have the greatest risk of developing skin issues and mucous membrane damage, which may result in acute or chronic dermatitis infections, secondary infection, and aggravation of pre‐existing skin illnesses. Latex gloves are mostly employed in workplaces to prevent the spread of the SARS‐CoV‐2 virus, which causes skin softness, maceration, whitening, and wrinkles (Yan et al., 2020). During the COVID‐19 pandemic, it has been observed that lifestyle modifications such as wearing masks and hand gloves have caused several skin allergies (Yan et al., 2020). Gheisari et al., have investigated the dermatological infections caused using N95 masks. According to this study, 35.5% of medical personnel used N95 masks on a daily basis, resulting in acne, facial dermatitis, and pigmentation of the chin, cheeks, and nasal bridge. Additionally, it was found that dermatitis with pruritic lesions mostly resulted in irritation and allergic contact dermatitis that generally developed as a result of the adhesives or other components of the breathing mask, such as rubber straps and metal clips (Gheisari et al., 2020). In another study, Donovan et al., 2007 reported that N95 masks caused reactions during the time of the SARS epidemic in Toronto (Donovan et al., 2007). Urticarial facial eruptions were reported in 3 patients, dermatitis in 5 patients, and acute respiratory symptoms without skin lesions in 2 patients were observed (Sharma & Malviya, 2020).
Many other related symptoms were also observed among COVID‐19 patients during the time of the COVID‐19 pandemic such as patchy rash, blisters that look like chickenpox, a lace‐like pattern on the skin, large patch with several smaller ones, itchy bumps, round, pinpoint spots on the skin, flat spots, and raised bumps that join together (Genovese et al., 2021). Among these infections, urticaria along with angioedema i caused by several bacteria and viruses, such as herpes virus, cytomegalo virus, epstein‐Barr virus, and mycoplasma (Kanani et al., 2011). In one of the studies, Galván Casas et al., 2020 reported that urticarial rash occurred in 19% of their cohort under observation. These rashes appeared simultaneously with systemic symptoms and lasted approximately 1 week. It was observed that these were associated with medium and high severity of COVID‐19. In urticarial rash, inflammatory responses were elevated which enhanced the immune hypersensitivity response, cytokine release syndrome, SARS‐Cov2‐RNA, deposition of microthrombi as well as vasculitis along with superficial perivascular dermatitis of microthrombi (Galván Casas et al., 2020).
Nutraceuticals and dermatological infection associated with COVID‐19
Several nutraceuticals have been reported that may be beneficial in reducing the symptoms of dermatological infections. Among them, some of the nutraceuticals also reduce symptoms of COVID‐19 and COVID‐19‐induced dermatological symptoms. Some of the important nutraceuticals are probiotics, prebiotics (Olaimat et al., 2020), resveratrol (Liao et al., 2021), hesperidin, quercetin (Saeedi‐Boroujeni & Mahmoudian‐Sani, 2021), lactoferrin (Chang et al., 2020), vitamin A, C, D, K (Goddek, 2020; Slominski et al., 2020), Zinc (Mossink, 2020), and omega‐C fatty acid (Gutiérrez et al., 2019; Hathaway et al., 2020). The nutraceuticals discussed above are reported to attenuate the progression of inflammation, mitochondrial dysfunction, endoplasmic reticulum stress, oxidative stress, and apoptosis pathways associated with urticaria, psoriasis, rash, and other dermatological infections induced by COVID‐19. Furthermore, they also helped in the reduction of skin infections (Lordan et al., 2021; Nwanodi, 2018).
Resveratrol
Resveratrol promotes the nuclear factor erythroid 2–related factor 2/antioxidant responsive element (Nrf2/ARE) pathway, which mediates anti‐inflammatory, anti‐oxidative, and anti‐apoptotic effects. The cis‐acting component ARE is responsible for the transcriptional activation of protective genes against SARS‐CoV‐2 infection. Nrf2 attaches to ARE and triggers the Nrf2/ARE pathway, which protects cells against oxidative stress. Resveratrol facilitates the expression of HO‐1 via activating the Nrf2/ARE pathway, thereby attenuating the effects of NF‐κB on antioxidants and its activation of inflammatory flares. Moreover, activation of the Nrf2/ARE pathway increases the expression of SIRT1/AMPK, which results in decreased inflammation. These inflammatory mediators and oxidants are activated by SARS‐CoV‐2 viruses and cause various dermatological infections. Resveratrol protects the cells from apoptosis and reduces dermatological symptoms by attenuating these inflammatory mediators thereby producing antioxidative effects (Imran, Iqbal et al., 2020; Liao et al., 2021).
Vitamin D
Vitamin D and its activated hydroxyl form possess anti‐inflammatory properties (Jan et al., 2019). They induce antioxidative responses and stimulate the innate defense against infectious pathogens. Calcitriol and the non‐calcemic hydroxy derivatives produced by CYP11A1 have been reported to demonstrate these features. They suppress the production of pro‐inflammatory cytokines, downregulate NF‐κB, exhibit antagonism on ROR, and protect against oxidative stress via NRF‐2 activation. As a result, direct distribution of vitamin D hydroxy derivatives should be considered for the treatment of COVID‐19 or acute respiratory distress syndromes of various aetiologies. Additionally, COVID‐19 patients should receive a high dose of vitamin D because patients who are most susceptible to this illness are usually vitamin D deficient. It has been predicted that different modes of administration (oral and parenteral) of vitamin D or vitamin D derivatives would have varying effects on the clinical and therapeutic outcomes (Slominski et al., 2020).
Omega‐3 fatty acid
Omega‐3 fatty acids are a group of polyunsaturated fatty acids that stimulate immune cell activation, especially in T‐cells, B‐cells, dendritic cells, macrophages, neutrophils, basophils, natural killer cells, mast cells, and eosinophils. Omega‐3 fatty acids are critical components of the host cellular membrane. They regulate membrane fluidity and the intricate lipid raft assembly process (Hathaway et al., 2020). Omega‐3 fatty acids provide an anti‐inflammatory impact by activating the TLR4 and G‐protein coupled receptor‐120 pathways, therefore reduce the level of NF‐κB expression (Gutiérrez et al., 2019; Hathaway et al., 2020).
Probiotics
The administration of probiotics in COVID‐19 patients has shown to increase their immunity and general health. Probiotics such as Lactobacillus casei also interact with TLRs on epithelial cells, increase the generation of cytokines that are critical for enhancing epithelial cell productivity and preventing apoptosis. Hence, they promote their survival and proliferation during the restoration process (Baud et al., 2020).
4. CONCLUSION AND FUTURE PERSPECTIVES
Based on the current evidence from the literature, it could be concluded that there are several promising therapeutic benefits of effectively using nutraceutical‐based products in the management of viral infections such as COVID‐19. Moreover, they are affordable, possess a long shelf‐life, easy to handle and store, easy to be administered compared to other complex injectable dosage forms such as vaccines, and intravenous injections containing allopathic medicines. In order to recommend the use of these compounds as an antiviral therapy, more detailed studies are required. Existing evidence is not translatable to humans because of several important limitations. Most of the tests are performed on in vitro or cell‐free/cell‐based models, which do not necessarily produce a human response. Inadequate pharmacokinetic and toxicological studies along with not standardized or inadequately titrated extracts may also contribute to this problem. Due to differences in bioavailability and bioactivity between individuals and their different biologic responses, estimating their bioavailability and bioactivity can also be challenging. Thus, advanced in vitro and animal studies are still needed to determine the mechanisms of action, pharmacokinetics, and safety profile of the isolated bioactive compounds and plant complexes before conducting human clinical trials. Over the past two years, drug manufacturers around the world have come up with newer and more effective nutraceutical‐based formulations for infectious diseases, like COVID‐19 in particular. Patanjali, a nutraceutical‐based drug company in India has designed a commercial oral tablet dosage form named “Coronil Kit®” which contains various therapeutic nutraceuticals. The formulation has been claimed to boost the immune system to fight against various common viral infections. However, more in‐depth research studies are necessary to validate their therapeutic potential before they can be translated for clinical usage. These compounds can be preliminarily assessed using observational studies focusing on outcomes such as hospitalizations and mortality rates. Ultimately, support from the national health systems would be crucial to ensuring adequate provision of these nutraceuticals.
AUTHOR CONTRIBUTIONS
Keshav Raj Paudel: Writing—original draft; Writing—review & editing. Vyoma Patel: Writing—original draft; Writing—review & editing. Sukriti Vishwas: Writing—original draft; Writing—review & editing. Saurabh Gupta: Writing—review & editing. Sumit Sharma: Writing—review & editing; Writing—original draft. Yinghan Chan: Writing—original draft. Niraj Kumar Jha: Writing—original draft. Jesus Shrestha: Writing—review & editing; Writing—original draft. Mohammad Imran: Writing—review & editing. Nisha Panth: Writing—review & editing. Shakti Dhar Shukla: Writing—review & editing. Saurav Kumar Jha: Writing—review & editing. Hari Prasad Devkota: Supervision. Majid Ebrahimi Warkiani: Supervision. Sachin Kumar Singh: Writing—review & editing; Supervision. Md Khadem Ali: Writing—review & editing. Gaurav Gupta: Writing—review & editing; Supervision. Dinesh Kumar Chellappan: Supervision; Writing—review & editing. Philip M. Hansbro: Supervision; Writing—review & editing. Kamal Dua: Writing ‐ review & editing; Supervision.
FUNDING INFORMATION
The author(s) report no funding associated with this work featured in this article.
CONFLICT OF INTEREST
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
ACKNOWLEDGMENT
Open access publishing facilitated by University of Technology Sydney, as part of the Wiley ‐ University of Technology Sydney agreement via the Council of Australian University Librarians.
Paudel, K. R. , Patel, V. , Vishwas, S. , Gupta, S. , Sharma, S. , Chan, Y. , Jha, N. K. , Shrestha, J. , Imran, M. , Panth, N. , Shukla, S. D. , Jha, S. K. , Devkota, H. P. , Warkiani, M. E. , Singh, S. K. , Ali, M. K. , Gupta, G. , Chellappan, D. K. , Hansbro, P. M. , & Dua, K. (2022). Nutraceuticals and COVID‐19: A mechanistic approach toward attenuating the disease complications. Journal of Food Biochemistry, 46, e14445. 10.1111/jfbc.14445
Contributor Information
Philip M. Hansbro, Email: philip.hansbro@uts.edu.au.
Kamal Dua, Email: kamalpharmacist02@gmail.com.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- Agrawal, T. , Gupta, G. K. , & Agrawal, D. K. (2013, June). Vitamin D supplementation reduces airway hyperresponsiveness and allergic airway inflammation in a murine model. Clinical and Experimental Allergy, 43(6), 672–683. 10.1111/cea.12102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Kassaa, I. , Hober, D. , Hamze, M. , Chihib, N. E. , & Drider, D. (2014, December). Antiviral potential of lactic acid bacteria and their bacteriocins. Probiotics and Antimicrobial Proteins, 6(3‐4), 177–185. 10.1007/s12602-014-9162-6 [DOI] [PubMed] [Google Scholar]
- Al Sulaiman, K. , Aljuhani, O. , Saleh, K. B. , Badreldin, H. A. , Al Harthi, A. , Alenazi, M. , Alharbi, A. , Algarni, R. , Al Harbi, S. , Alhammad, A. M. , Vishwakarma, R. , & Aldekhyl, S. (2021, September 3). Ascorbic acid as an adjunctive therapy in critically ill patients with COVID‐19: A propensity score matched study. Scientific Reports, 11(1), 17648. 10.1038/s41598-021-96703-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andres‐Lacueva, C. , Monagas, M. , Khan, N. , Izquierdo‐Pulido, M. , Urpi‐Sarda, M. , Permanyer, J. , & Lamuela‐Raventos, R. M. (2008, May 14). Flavanol and flavonol contents of cocoa powder products: Influence of the manufacturing process. Journal of Agricultural and Food Chemistry, 56(9), 3111–3117. 10.1021/jf0728754 [DOI] [PubMed] [Google Scholar]
- Andrews, K. W. , Schweitzer, A. , Zhao, C. , Holden, J. M. , Roseland, J. M. , Brandt, M. , Dwyer, J. T. , Picciano, M. F. , Saldanha, L. G. , Fisher, K. D. , Yetley, E. , Betz, J. M. , & Douglass, L. (2007, September). The caffeine contents of dietary supplements commonly purchased in the US: Analysis of 53 products with caffeine‐containing ingredients. Analytical and Bioanalytical Chemistry, 389(1), 231–239. 10.1007/s00216-007-1437-2 [DOI] [PubMed] [Google Scholar]
- Annweiler, C. , Beaudenon, M. , Gautier, J. , Simon, R. , Dubee, V. , Gonsard, J. , Parot‐Schinkel, E. , & Group, C.‐T. (2020, December 28). Covid‐19 and high‐dose VITamin D supplementation TRIAL in high‐risk older patients (COVIT‐TRIAL): Study protocol for a randomized controlled trial. Trials, 21(1), 1031. 10.1186/s13063-020-04928-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appelboom, T. , Schuermans, J. , Verbruggen, G. , Henrotin, Y. , & Reginster, J. Y. (2001). Symptoms modifying effect of avocado/soybean unsaponifiables (ASU) in knee osteoarthritis. A double blind, prospective, placebo‐controlled study. Scandinavian Journal of Rheumatology, 30(4), 242–247. 10.1080/030097401316909602 [DOI] [PubMed] [Google Scholar]
- Bakian, A. V. , Huber, R. S. , Scholl, L. , Renshaw, P. F. , & Kondo, D. (2020, February 3). Dietary creatine intake and depression risk among U.S. adults. Translational Psychiatry, 10(1), 52. 10.1038/s41398-020-0741-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balentine, D. A. , Wiseman, S. A. , & Bouwens, L. C. (1997, December). The chemistry of tea flavonoids. Critical Reviews in Food Science and Nutrition, 37(8), 693–704. 10.1080/10408399709527797 [DOI] [PubMed] [Google Scholar]
- Balestrino, M. , & Adriano, E. (2019, November). Beyond sports: Efficacy and safety of creatine supplementation in pathological or paraphysiological conditions of brain and muscle. Medicinal Research Reviews, 39(6), 2427–2459. 10.1002/med.21590 [DOI] [PubMed] [Google Scholar]
- Barber, M. S. , Barrett, R. , Bradley, R. D. , & Walker, E. (2021, December). A naturopathic treatment approach for mild and moderate COVID‐19: A retrospective chart review. Complementary Therapies in Medicine, 63, 102788. 10.1016/j.ctim.2021.102788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batra, S. , Kumar, A. , & Sharma, A. (2018). Isolation, characterization and antianxiety activity of pentacosan‐13‐ol from Ferula sumbul Hook. roots. Journal of Biologically Active Products from Nature, 8(3), 171–179. [Google Scholar]
- Baud, D. , Dimopoulou Agri, V. , Gibson, G. R. , Reid, G. , & Giannoni, E. (2020). Using probiotics to flatten the curve of coronavirus disease COVID‐2019 pandemic. Frontiers in Public Health, 8, 186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaumont, M. , Batejat, D. , Pierard, C. , Van Beers, P. , Denis, J. B. , Coste, O. , Doireau, P. , Chauffard, F. , French, J. , & Lagarde, D. (2004, January). Caffeine or melatonin effects on sleep and sleepiness after rapid eastward transmeridian travel. Journal of Applied Physiology (1985), 96(1), 50–58. 10.1152/japplphysiol.00940.2002 [DOI] [PubMed] [Google Scholar]
- Beigmohammadi, M. T. , Bitarafan, S. , Hoseindokht, A. , Abdollahi, A. , Amoozadeh, L. , & Soltani, D. (2021, November 14). The effect of supplementation with vitamins A, B, C, D, and E on disease severity and inflammatory responses in patients with COVID‐19: A randomized clinical trial. Trials, 22(1), 802. 10.1186/s13063-021-05795-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender, A. , Hagan, K. E. , & Kingston, N. (2017, December). The association of folate and depression: A meta‐analysis. Journal of Psychiatric Research, 95, 9–18. 10.1016/j.jpsychires.2017.07.019 [DOI] [PubMed] [Google Scholar]
- Bengmark, S. (2006, January–February). Curcumin, an atoxic antioxidant and natural NFkappaB, cyclooxygenase‐2, lipooxygenase, and inducible nitric oxide synthase inhibitor: A shield against acute and chronic diseases. JPEN Journal of Parenteral and Enteral Nutrition, 30(1), 45–51. 10.1177/014860710603000145 [DOI] [PubMed] [Google Scholar]
- Berg, K. , Bolt, G. , Andersen, H. , & Owen, T. C. (2001, July). Zinc potentiates the antiviral action of human IFN‐alpha tenfold. Journal of Interferon & Cytokine Research, 21(7), 471–474. 10.1089/10799900152434330 [DOI] [PubMed] [Google Scholar]
- Berridge, M. J. (2017). Vitamin D and depression: Cellular and regulatory mechanisms. Pharmacological Reviews, 69(2), 80–92. [DOI] [PubMed] [Google Scholar]
- Biaggio, V. S. , Perez Chaca, M. V. , Valdez, S. R. , Gomez, N. N. , & Gimenez, M. S. (2010, February). Alteration in the expression of inflammatory parameters as a result of oxidative stress produced by moderate zinc deficiency in rat lung. Experimental Lung Research, 36(1), 31–44. 10.3109/01902140903061787 [DOI] [PubMed] [Google Scholar]
- Bo, H. X. , Li, W. , Yang, Y. , Wang, Y. , Zhang, Q. , Cheung, T. , Wu, X. , & Xiang, Y. T. (2021, April). Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID‐19 in China. Psychological Medicine, 51(6), 1052–1053. 10.1017/S0033291720000999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boldrini, M. , Galfalvy, H. , Dwork, A. J. , Rosoklija, G. B. , Trencevska‐Ivanovska, I. , Pavlovski, G. , Hen, R. , Arango, V. , & Mann, J. J. (2019, May 15). Resilience is associated with larger dentate gyrus, while suicide decedents with major depressive disorder have fewer granule neurons. Biological Psychiatry, 85(10), 850–862. 10.1016/j.biopsych.2018.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boros, S. (2013). The role of nutrition in the treatment of chronic musculoskeletal diseases. Nutrition Journal, 12, 146.24215592 [Google Scholar]
- Boumediene, K. , Felisaz, N. , Bogdanowicz, P. , Galera, P. , Guillou, G. B. , & Pujol, J. P. (1999, January). Avocado/soya unsaponifiables enhance the expression of transforming growth factor beta1 and beta2 in cultured articular chondrocytes. Arthritis and Rheumatism, 42(1), 148–156. [DOI] [PubMed] [Google Scholar]
- Brighenti, S. , Bergman, P. , & Martineau, A. R. (2018, May 27). Vitamin D and tuberculosis: Where next? Journal of Internal Medicine, 284, 145–162. 10.1111/joim.12777 [DOI] [PubMed] [Google Scholar]
- Brosnan, J. T. , da Silva, R. P. , & Brosnan, M. E. (2011, May). The metabolic burden of creatine synthesis. Amino Acids, 40(5), 1325–1331. 10.1007/s00726-011-0853-y [DOI] [PubMed] [Google Scholar]
- Burhani, M. D. , & Rasenick, M. M. (2017). Fish oil and depression: The skinny on fats. Journal of Integrative Neuroscience, 16(s1), S115–S124. 10.3233/JIN-170072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns, J. , Mullen, W. , Landrault, N. , Teissedre, P. L. , Lean, M. E. , & Crozier, A. (2002, July 3). Variations in the profile and content of anthocyanins in wines made from cabernet sauvignon and hybrid grapes. Journal of Agricultural and Food Chemistry, 50(14), 4096–4102. 10.1021/jf011233s [DOI] [PubMed] [Google Scholar]
- Campbell, J. D. , Cole, M. , Bunditrutavorn, B. , & Vella, A. T. (1999, May 25). Ascorbic acid is a potent inhibitor of various forms of T cell apoptosis. Cellular Immunology, 194(1), 1–5. 10.1006/cimm.1999.1485 [DOI] [PubMed] [Google Scholar]
- Caress, J. B. , Castoro, R. J. , Simmons, Z. , Scelsa, S. N. , Lewis, R. A. , Ahlawat, A. , & Narayanaswami, P. (2020). COVID‐19–associated Guillain‐Barré syndrome: The early pandemic experience. Muscle & Nerve, 62(4), 485–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr, A. C. , & Maggini, S. (2017, November 3). Vitamin C and Immune Function. Nutrients, 9(11), 1–25. 10.3390/nu9111211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, Y. , Raju Allam, V. S. R. , Paudel, K. R. , Singh, S. K. , Gulati, M. , Dhanasekaran, M. , Gupta, P. K. , Jha, N. K. , Devkota, H. P. , Gupta, G. , Hansbro, P. M. , Oliver, B. G. G. , Chellappan, D. K. , & Dua, K. (2021, October 6). Nutraceuticals: Unlocking newer paradigms in the mitigation of inflammatory lung diseases. Critical Reviews in Food Science and Nutrition, 1–31. 10.1080/10408398.2021.1986467 [DOI] [PubMed] [Google Scholar]
- Chanda, S. , Tiwari, R. K. , Kumar, A. , & Singh, K. (2019). Nutraceuticals inspiring the current therapy for lifestyle diseases. Advances in Pharmacological Sciences, 2019, 6908716. 10.1155/2019/6908716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandran, B. , & Goel, A. (2012, November). A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytotherapy Research, 26(11), 1719–1725. 10.1002/ptr.4639 [DOI] [PubMed] [Google Scholar]
- Chang, R. , Ng, T. B. , & Sun, W.‐Z. (2020). Lactoferrin as potential preventative and adjunct treatment for COVID‐19. International Journal of Antimicrobial Agents, 56(3), 106118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y. , Zhang, J. , Ge, X. , Du, J. , Deb, D. K. , & Li, Y. C. (2013, July 5). Vitamin D receptor inhibits nuclear factor kappaB activation by interacting with IkappaB kinase beta protein. The Journal of Biological Chemistry, 288(27), 19450–19458. doi: 10.1074/jbc.M113.467670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, S. K. , Tsang, J. S. , Ku, K. H. , Wong, C. W. , & Ng, Y. K. (2004, April). Psychiatric complications in patients with severe acute respiratory syndrome (SARS) during the acute treatment phase: A series of 10 cases. The British Journal of Psychiatry, 184, 359–360. 10.1192/bjp.184.4.359 [DOI] [PubMed] [Google Scholar]
- Chiba, Y. , Shida, K. , Nagata, S. , Wada, M. , Bian, L. , Wang, C. , Shimizu, T. , Yamashiro, Y. , Kiyoshima‐Shibata, J. , Nanno, M. , & Nomoto, K. (2010, July). Well‐controlled proinflammatory cytokine responses of Peyer's patch cells to probiotic Lactobacillus casei. Immunology, 130(3), 352–362. 10.1111/j.1365-2567.2009.03204.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, H. , Kim, D. H. , Meza, C. A. , Ormsbee, M. J. , & Hickner, R. C. (2020, September 16). The evolving applications of creatine supplementation: Could creatine improve vascular health? Nutrients, 12(9), 1–23. 10.3390/nu12092834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva, L. E. M. , de Santana, M. L. P. , Costa, P. R. , Pereira, E. M. , Nepomuceno, C. M. M. , Queiroz, V. A. , de Oliveira, L. P. M. , Machado, M. E. P. C. , & de Sena, E. P. (2021). Zinc supplementation combined with antidepressant drugs for treatment of patients with depression: A systematic review and meta‐analysis. Nutrition Reviews, 79(1), 1–12. [DOI] [PubMed] [Google Scholar]
- Daily, J. W. , Yang, M. , & Park, S. (2016, August). Efficacy of turmeric extracts and curcumin for alleviating the symptoms of joint arthritis: A systematic review and meta‐analysis of randomized clinical trials. Journal of Medicinal Food, 19(8), 717–729. 10.1089/jmf.2016.3705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darlenski, R. , & Tsankov, N. (2020). COVID‐19 pandemic and the skin: What should dermatologists know? Clinics in Dermatology, 38(6), 785–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vrese, M. , Winkler, P. , Rautenberg, P. , Harder, T. , Noah, C. , Laue, C. , Ott, S. , Hampe, J. , Schreiber, S. , Heller, K. , & Schrezenmeir, J. (2006, November 10). Probiotic bacteria reduced duration and severity but not the incidence of common cold episodes in a double blind, randomized, controlled trial. Vaccine, 24(44‐46), 6670–6674. 10.1016/j.vaccine.2006.05.048 [DOI] [PubMed] [Google Scholar]
- Deane, C. S. , Wilkinson, D. J. , Phillips, B. E. , Smith, K. , Etheridge, T. , & Atherton, P. J. (2017). “Nutraceuticals” in relation to human skeletal muscle and exercise. American Journal of Physiology Endocrinology and Metabolism, 312(4), E282–E299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derosa, G. , Maffioli, P. , D'Angelo, A. , & Di Pierro, F. (2021). Nutraceutical approach to preventing coronavirus disease 2019 and related complications. Frontiers in Immunology, 12, 582556. 10.3389/fimmu.2021.582556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djuricic, I. , & Calder, P. C. (2021, July 15). Beneficial outcomes of omega‐6 and omega‐3 polyunsaturated fatty acids on human health: An update for 2021. Nutrients, 13(7), 1–23. 10.3390/nu13072421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donath, F. , Quispe, S. , Diefenbach, K. , Maurer, A. , Fietze, I. , & Roots, I. (2000, March). Critical evaluation of the effect of valerian extract on sleep structure and sleep quality. Pharmacopsychiatry, 33(2), 47–53. 10.1055/s-2000-7972 [DOI] [PubMed] [Google Scholar]
- Donma, M. M. , & Donma, O. (2020, November). The effects of allium sativum on immunity within the scope of COVID‐19 infection. Medical Hypotheses, 144, 109934. 10.1016/j.mehy.2020.109934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan, J. , Kudla, I. , Holness, L. D. , Skotnicki‐Grant, S. , & Nethercott, J. R. (2007). Skin reactions following use of N95 facial masks. Dermatitis, 18(2), 104. [Google Scholar]
- Du, X. , Shi, L. , Cao, W. , Zuo, B. , & Zhou, A. (2021). Add‐on effect of Chinese herbal medicine in the treatment of mild to moderate COVID‐19: A systematic review and meta‐analysis. PLoS One, 16(8), e0256429. 10.1371/journal.pone.0256429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellulu, M. S. , Rahmat, A. , Patimah, I. , Khaza'ai, H. , & Abed, Y. (2015). Effect of vitamin C on inflammation and metabolic markers in hypertensive and/or diabetic obese adults: A randomized controlled trial. Drug Design, Development and Therapy, 9, 3405–3412. 10.2147/DDDT.S83144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entrenas Castillo, M. , Entrenas Costa, L. M. , Vaquero Barrios, J. M. , Alcala Diaz, J. F. , Lopez Miranda, J. , Bouillon, R. , & Quesada Gomez, J. M. (2020, October). Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID‐19: A pilot randomized clinical study. The Journal of Steroid Biochemistry and Molecular Biology, 203, 105751. 10.1016/j.jsbmb.2020.105751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esakandari, H. , Nabi‐Afjadi, M. , Fakkari‐Afjadi, J. , Farahmandian, N. , Miresmaeili, S. M. , & Bahreini, E. (2020). A comprehensive review of COVID‐19 characteristics. Biological Procedures Online, 22, 19. 10.1186/s12575-020-00128-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteban, S. , Nicolaus, C. , Garmundi, A. , Rial, R. V. , Rodriguez, A. B. , Ortega, E. , & Ibars, C. B. (2004, December). Effect of orally administered L‐tryptophan on serotonin, melatonin, and the innate immune response in the rat. Molecular and Cellular Biochemistry, 267(1‐2), 39–46. 10.1023/b:mcbi.0000049363.97713.74 [DOI] [PubMed] [Google Scholar]
- Fava, M. , & Mischoulon, D. (2009). Folate in depression: Efficacy, safety, differences in formulations, and clinical issues. The Journal of Clinical Psychiatry, 70(Suppl 5), 12–17. 10.4088/JCP.8157su1c.03 [DOI] [PubMed] [Google Scholar]
- Formisano, E. , Di Maio, P. , Ivaldi, C. , Sferrazzo, E. , Arieta, L. , Bongiovanni, S. , Panizzi, L. , Valentino, E. , Pasta, A. , Giudice, M. , & Demontis, S. (2021, February). Nutritional therapy for patients with coronavirus disease 2019 (COVID‐19): Practical protocol from a single center highly affected by an outbreak of the novel severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection. Nutrition, 82, 111048. 10.1016/j.nut.2020.111048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar‐Poli, L. , Vozza, L. , Gabbiadini, A. , Vanella, A. , Concas, I. , Tinacci, S. , Petralia, A. , Signorelli, M. S. , & Aguglia, E. (2020). Curcumin for depression: A meta‐analysis. Critical Reviews in Food Science and Nutrition, 60(15), 2643–2653. 10.1080/10408398.2019.1653260 [DOI] [PubMed] [Google Scholar]
- Galván Casas, C. , Catala, A. , Carretero Hernández, G. , Rodríguez‐Jiménez, P. , Fernández‐Nieto, D. , Rodríguez‐Villa Lario, A. , Navarro Fernández, I. , Ruiz‐Villaverde, R. , Falkenhain‐López, D. , & Llamas Velasco, M. (2020). Classification of the cutaneous manifestations of COVID‐19: A rapid prospective nationwide consensus study in Spain with 375 cases. British Journal of Dermatology, 183(1), 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, Q. , Kou, T. , Zhuang, B. , Ren, Y. , Dong, X. , & Wang, Q. (2018, October 1). The association between vitamin d deficiency and sleep disorders: A systematic review and meta‐analysis. Nutrients, 10(10), 1–13. 10.3390/nu10101395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, X. , Guo, M. , Peng, L. , Zhao, B. , Su, J. , Liu, H. , Zhang, L. , Bai, X. , & Qiao, Y. (2013). UPLC Q‐TOF/MS‐based metabolic profiling of urine reveals the novel antipyretic mechanisms of qingkailing injection in a rat model of yeast‐induced pyrexia. Evidence‐based Complementary and Alternative Medicine, 2013, 864747. 10.1155/2013/864747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, Y. , Fang, L. , Cai, R. , Zong, C. , Chen, X. , Lu, J. , & Qi, Y. (2014, March 15). Shuang‐Huang‐Lian exerts anti‐inflammatory and anti‐oxidative activities in lipopolysaccharide‐stimulated murine alveolar macrophages. Phytomedicine, 21(4), 461–469. 10.1016/j.phymed.2013.09.022 [DOI] [PubMed] [Google Scholar]
- Gasmi, A. , Tippairote, T. , Mujawdiya, P. K. , Peana, M. , Menzel, A. , Dadar, M. , Benahmed, A. G. , & Bjorklund, G. (2021, May). The microbiota‐mediated dietary and nutritional interventions for COVID‐19. Clinical Immunology, 226, 108725. 10.1016/j.clim.2021.108725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genovese, G. , Moltrasio, C. , Berti, E. , & Marzano, A. V. (2021). Skin manifestations associated with COVID‐19: Current knowledge and future perspectives. Dermatology, 237(1), 1–12. 10.1159/000512932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gezen‐Ak, D. , Dursun, E. , & Yilmazer, S. (2014). The effect of vitamin D treatment on nerve growth factor (NGF) release from hippocampal neurons. Nöropsikiyatri Arşivi, 51(2), 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gheisari, M. , Araghi, F. , Moravvej, H. , Tabary, M. , & Dadkhahfar, S. (2020). Skin reactions to non‐glove personal protective equipment: An emerging issue in the COVID‐19 pandemic. Journal of the European Academy of Dermatology and Venereology, 34(7), e297–e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh, D. (2021). Role of food or food component in brain health. In Nutraceuticals in brain health and beyond (pp. 3–13). Elsevier. [Google Scholar]
- Gluszko, P. , & Stasiek, M. (2016). Symptom‐modifying effects of oral avocado/soybean unsaponifiables in routine treatment of knee osteoarthritis in Poland. An open, prospective observational study of patients adherent to a 6‐month treatment. Reumatologia, 54(5), 217–226. 10.5114/reum.2016.63661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goddek, S. (2020). Vitamin D3 and K2 and their potential contribution to reducing the COVID‐19 mortality rate. International Journal of Infectious Diseases, 99, 286–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel, A. , Boland, C. R. , & Chauhan, D. P. (2001, October 30). Specific inhibition of cyclooxygenase‐2 (COX‐2) expression by dietary curcumin in HT‐29 human colon cancer cells. Cancer Letters, 172(2), 111–118. 10.1016/s0304-3835(01)00655-3 [DOI] [PubMed] [Google Scholar]
- Goel, A. , Jhurani, S. , & Aggarwal, B. B. (2008, September). Multi‐targeted therapy by curcumin: How spicy is it? Molecular Nutrition & Food Research, 52(9), 1010–1030. 10.1002/mnfr.200700354 [DOI] [PubMed] [Google Scholar]
- Gonzalez, S. (2020, January 29). Dietary bioactive compounds and human health and disease. Nutrients, 12(2), 1–3. 10.3390/nu12020348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant, W. B. , Lahore, H. , McDonnell, S. L. , Baggerly, C. A. , French, C. B. , Aliano, J. L. , & Bhattoa, H. P. (2020, April 2). Evidence that vitamin D supplementation could reduce risk of influenza and COVID‐19 infections and deaths. Nutrients, 12(4), 1–19. 10.3390/nu12040988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillemard, E. , Tondu, F. , Lacoin, F. , & Schrezenmeir, J. (2010, January). Consumption of a fermented dairy product containing the probiotic Lactobacillus casei DN‐114001 reduces the duration of respiratory infections in the elderly in a randomised controlled trial. The British Journal of Nutrition, 103(1), 58–68. 10.1017/S0007114509991395 [DOI] [PubMed] [Google Scholar]
- Gulati, K. , Rai, N. , Chaudhary, S. , & Ray, A. (2016). Nutraceuticals in respiratory disorders. In Nutraceuticals (pp. 75–86). Elsevier. [Google Scholar]
- Gutiérrez, S. , Svahn, S. L. , & Johansson, M. E. (2019). Effects of omega‐3 fatty acids on immune cells. International Journal of Molecular Sciences, 20(20), 5028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley, S. , & Petry, J. J. (2003, April 15). Valerian. American Family Physician, 67(8), 1755–1758 https://www.ncbi.nlm.nih.gov/pubmed/12725454 [PubMed] [Google Scholar]
- Hammerstone, J. F. , Lazarus, S. A. , Mitchell, A. E. , Rucker, R. , & Schmitz, H. H. (1999, February). Identification of procyanidins in cocoa (Theobroma cacao) and chocolate using high‐performance liquid chromatography/mass spectrometry. Journal of Agricultural and Food Chemistry, 47(2), 490–496. 10.1021/jf980760h [DOI] [PubMed] [Google Scholar]
- Hardwick, J. , Taylor, J. , Mehta, M. , Satija, S. , Paudel, K. R. , Hansbro, P. M. , Chellappan, D. K. , Bebawy, M. , & Dua, K. (2021). Targeting cancer using curcumin encapsulated vesicular drug delivery systems. Current Pharmaceutical Design, 27(1), 2–14. 10.2174/1381612826666200728151610 [DOI] [PubMed] [Google Scholar]
- Hassaniazad, M. , Eftekhar, E. , Inchehsablagh, B. R. , Kamali, H. , Tousi, A. , Jaafari, M. R. , Rafat, M. , Fathalipour, M. , Nikoofal‐Sahlabadi, S. , Gouklani, H. , Alizade, H. , & Nikpoor, A. R. (2021, November). A triple‐blind, placebo‐controlled, randomized clinical trial to evaluate the effect of curcumin‐containing nanomicelles on cellular immune responses subtypes and clinical outcome in COVID‐19 patients. Phytotherapy Research, 35(11), 6417–6427. 10.1002/ptr.7294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hathaway, D., III , Pandav, K. , Patel, M. , Riva‐Moscoso, A. , Singh, B. M. , Patel, A. , Min, Z. C. , Singh‐Makkar, S. , Sana, M. K. , & Sanchez‐Dopazo, R. (2020). Omega 3 fatty acids and COVID‐19: A comprehensive review. Infection & Chemotherapy, 52(4), 478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidari‐Beni, M. , Moravejolahkami, A. R. , Gorgian, P. , Askari, G. , Tarrahi, M. J. , & Bahreini‐Esfahani, N. (2020, August). Herbal formulation "turmeric extract, black pepper, and ginger" versus Naproxen for chronic knee osteoarthritis: A randomized, double‐blind, controlled clinical trial. Phytotherapy Research, 34(8), 2067–2073. 10.1002/ptr.6671 [DOI] [PubMed] [Google Scholar]
- Heller, R. A. , Sun, Q. , Hackler, J. , Seelig, J. , Seibert, L. , Cherkezov, A. , Minich, W. B. , Seemann, P. , Diegmann, J. , Pilz, M. , Bachmann, M. , Ranjbar, A. , Moghaddam, A. , & Schomburg, L. (2021, January). Prediction of survival odds in COVID‐19 by zinc, age and selenoprotein P as composite biomarker. Redox Biology, 38, 101764. 10.1016/j.redox.2020.101764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrotin, Y. E. , Sanchez, C. , Deberg, M. A. , Piccardi, N. , Guillou, G. B. , Msika, P. , & Reginster, J. Y. (2003, August). Avocado/soybean unsaponifiables increase aggrecan synthesis and reduce catabolic and proinflammatory mediator production by human osteoarthritic chondrocytes. The Journal of Rheumatology, 30(8), 1825–1834 https://www.ncbi.nlm.nih.gov/pubmed/12913942 [PubMed] [Google Scholar]
- Holford, P. , Carr, A. C. , Jovic, T. H. , Ali, S. R. , Whitaker, I. S. , Marik, P. E. , & Smith, A. D. (2020, December 7). Vitamin C‐an adjunctive therapy for respiratory infection, sepsis and COVID‐19. Nutrients, 12(12), 1–17. 10.3390/nu12123760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hritcu, L. , Ionita, R. , Postu, P. A. , Gupta, G. K. , Turkez, H. , Lima, T. C. , Carvalho, C. U. S. , & de Sousa, D. P. (2017). Antidepressant flavonoids and their relationship with oxidative stress. Oxidative Medicine and Cellular Longevity, 2017, 5762172. 10.1155/2017/5762172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, L. , Yuen, T. T. , Ye, Z. , Liu, S. , Zhang, G. , Chu, H. , & Yue, J. (2021, April 24). Berbamine inhibits SARS‐CoV‐2 infection by compromising TRPMLs‐mediated endolysosomal trafficking of ACE2. Signal Transduction and Targeted Therapy, 6(1), 168. 10.1038/s41392-021-00584-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huiberts, L. M. , & Smolders, K. (2021, February). Effects of vitamin D on mood and sleep in the healthy population: Interpretations from the serotonergic pathway. Sleep Medicine Reviews, 55, 101379. 10.1016/j.smrv.2020.101379 [DOI] [PubMed] [Google Scholar]
- Imran, M. , Iqubal, M. K. , Imtiyaz, K. , Saleem, S. , Mittal, S. , Rizvi, M. M. A. , Ali, J. , & Baboota, S. (2020, September 25). Topical nanostructured lipid carrier gel of quercetin and resveratrol: Formulation, optimization, in vitro and ex vivo study for the treatment of skin cancer. International Journal of Pharmaceutics, 587, 119705. 10.1016/j.ijpharm.2020.119705 [DOI] [PubMed] [Google Scholar]
- Imran, M. , Jha, S. K. , Hasan, N. , Insaf, A. , Shrestha, J. , Shrestha, J. , Devkota, H. P. , Khan, S. , Panth, N. , Warkiani, M. E. , Dua, K. , Hansbro, P. M. , Paudel, K. R. , & Mohammed, Y. (2022, March 8). Overcoming multidrug resistance of antibiotics via nanodelivery systems. Pharmaceutics, 14(3), 1–25. 10.3390/pharmaceutics14030586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imran, M. , Saleem, S. , Chaudhuri, A. , Ali, J. , & Baboota, S. (2020, December 1). Docetaxel: An update on its molecular mechanisms, therapeutic trajectory and nanotechnology in the treatment of breast, lung and prostate cancer. Journal of Drug Delivery Science and Technology, 60, 101959. 10.1016/j.jddst.2020.101959 [DOI] [Google Scholar]
- Iolascon, G. , Gimigliano, R. , Bianco, M. , De Sire, A. , Moretti, A. , Giusti, A. , Malavolta, N. , Migliaccio, S. , Migliore, A. , & Napoli, N. (2017). Are dietary supplements and nutraceuticals effective for musculoskeletal health and cognitive function? A scoping review. The Journal of Nutrition, Health & Aging, 21(5), 527–538. [DOI] [PubMed] [Google Scholar]
- Jan, Y. , Malik, M. , Yaseen, M. , Ahmad, S. , Imran, M. , Rasool, S. , & Haq, A. (2019, October). Vitamin D fortification of foods in India: Present and past scenario. The Journal of Steroid Biochemistry and Molecular Biology, 193, 105417. 10.1016/j.jsbmb.2019.105417 [DOI] [PubMed] [Google Scholar]
- Jayawardena, R. , Sooriyaarachchi, P. , Chourdakis, M. , Jeewandara, C. , & Ranasinghe, P. (2020, July–August). Enhancing immunity in viral infections, with special emphasis on COVID‐19: A review. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 14(4), 367–382. 10.1016/j.dsx.2020.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery, L. E. , Burke, F. , Mura, M. , Zheng, Y. , Qureshi, O. S. , Hewison, M. , Walker, L. S. , Lammas, D. A. , Raza, K. , & Sansom, D. M. (2009, November 1). 1,25‐Dihydroxyvitamin D3 and IL‐2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA‐4 and FoxP3. Journal of Immunology, 183(9), 5458–5467. 10.4049/jimmunol.0803217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung, H. Y. , Yoo, D. Y. , Nam, S. M. , Kim, J. W. , Choi, J. H. , Yoo, M. , Lee, S. , Yoon, Y. S. , & Hwang, I. K. (2015). Valerenic acid protects against physical and psychological stress by reducing the turnover of serotonin and norepinephrine in mouse hippocampus‐amygdala region. Journal of Medicinal Food, 18(12), 1333–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanani, A. , Schellenberg, R. , & Warrington, R. (2011). Urticaria and angioedema. Allergy, Asthma & Clinical Immunology, 7(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanauchi, O. , Andoh, A. , AbuBakar, S. , & Yamamoto, N. (2018). Probiotics and paraprobiotics in viral infection: Clinical application and effects on the innate and acquired immune systems. Current Pharmaceutical Design, 24(6), 710–717. 10.2174/1381612824666180116163411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan, N. , & Mukhtar, H. (2007, July 26). Tea polyphenols for health promotion. Life Sciences, 81(7), 519–533. 10.1016/j.lfs.2007.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna, D. , Sethi, G. , Ahn, K. S. , Pandey, M. K. , Kunnumakkara, A. B. , Sung, B. , Aggarwal, A. , & Aggarwal, B. B. (2007, June). Natural products as a gold mine for arthritis treatment. Current Opinion in Pharmacology, 7(3), 344–351. 10.1016/j.coph.2007.03.002 [DOI] [PubMed] [Google Scholar]
- Kikuchi, A. M. , Tanabe, A. , & Iwahori, Y. (2021). A systematic review of the effect of L‐tryptophan supplementation on mood and emotional functioning. Journal of Dietary Supplements, 18(3), 316–333. 10.1080/19390211.2020.1746725 [DOI] [PubMed] [Google Scholar]
- Kim, K. H. , Lee, E. N. , Park, J. K. , Lee, J. R. , Kim, J. H. , Choi, H. J. , Kim, B. S. , Lee, H. W. , Lee, K. S. , & Yoon, S. (2012, July). Curcumin attenuates TNF‐alpha‐induced expression of intercellular adhesion molecule‐1, vascular cell adhesion molecule‐1 and proinflammatory cytokines in human endometriotic stromal cells. Phytotherapy Research, 26(7), 1037–1047. 10.1002/ptr.3694 [DOI] [PubMed] [Google Scholar]
- Kishimoto, A. , Imaizumi, A. , Wada, H. , Yamakage, H. , Satoh‐Asahara, N. , Hashimoto, T. , & Hasegawa, K. (2021). Newly developed highly bioavailable curcumin formulation, curcuRouge(TM), reduces neutrophil/lymphocyte ratio in the elderly: A double‐blind, placebo‐controlled clinical trial. Journal of Nutritional Science and Vitaminology (Tokyo), 67(4), 249–252. 10.3177/jnsv.67.249 [DOI] [PubMed] [Google Scholar]
- Koshak, A. E. , Koshak, E. A. , Mobeireek, A. F. , Badawi, M. A. , Wali, S. O. , Malibary, H. M. , Atwah, A. F. , Alhamdan, M. M. , Almalki, R. A. , & Madani, T. A. (2020, August 8). Nigella sativa supplementation to treat symptomatic mild COVID‐19: A structured summary of a protocol for a randomised, controlled, clinical trial. Trials, 21(1), 703. 10.1186/s13063-020-04647-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koshak, D. A. E. , & Koshak, P. E. A. (2020). Nigella sativa L as a potential phytotherapy for coronavirus disease 2019: A mini review of in silico studies. Current Therapeutic Research, Clinical and Experimental, 93, 100602. 10.1016/j.curtheres.2020.100602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreider, R. B. , & Stout, J. R. (2021, January 29). Creatine in health and disease. Nutrients, 13(2), 1–27. 10.3390/nu13020447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuptniratsaikul, V. , Dajpratham, P. , Taechaarpornkul, W. , Buntragulpoontawee, M. , Lukkanapichonchut, P. , Chootip, C. , Saengsuwan, J. , Tantayakom, K. , & Laongpech, S. (2014). Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: A multicenter study. Clinical Interventions in Aging, 9, 451–458. 10.2147/CIA.S58535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuptniratsaikul, V. , Thanakhumtorn, S. , Chinswangwatanakul, P. , Wattanamongkonsil, L. , & Thamlikitkul, V. (2009, August). Efficacy and safety of Curcuma domestica extracts in patients with knee osteoarthritis. Journal of Alternative and Complementary Medicine, 15(8), 891–897. 10.1089/acm.2008.0186 [DOI] [PubMed] [Google Scholar]
- Lakhan, S. E. , & Vieira, K. F. (2008, January 21). Nutritional therapies for mental disorders. Nutrition Journal, 7, 2. 10.1186/1475-2891-7-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantz, R. C. , Chen, G. J. , Sarihan, M. , Solyom, A. M. , Jolad, S. D. , & Timmermann, B. N. (2007, February). The effect of extracts from ginger rhizome on inflammatory mediator production. Phytomedicine, 14(2‐3), 123–128. 10.1016/j.phymed.2006.03.003 [DOI] [PubMed] [Google Scholar]
- Lazarczyk, M. , & Favre, M. (2008, December). Role of Zn2+ ions in host‐virus interactions. Journal of Virology, 82(23), 11486–11494. 10.1128/JVI.01314-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, A. M. , Wong, J. G. , McAlonan, G. M. , Cheung, V. , Cheung, C. , Sham, P. C. , Chu, C. M. , Wong, P. C. , Tsang, K. W. , & Chua, S. E. (2007, April). Stress and psychological distress among SARS survivors 1 year after the outbreak. Canadian Journal of Psychiatry, 52(4), 233–240. 10.1177/070674370705200405 [DOI] [PubMed] [Google Scholar]
- Lee, K. W. , Kim, Y. J. , Lee, H. J. , & Lee, C. Y. (2003, December 3). Cocoa has more phenolic phytochemicals and a higher antioxidant capacity than teas and red wine. Journal of Agricultural and Food Chemistry, 51(25), 7292–7295. 10.1021/jf0344385 [DOI] [PubMed] [Google Scholar]
- Lemire, J. M. , Archer, D. C. , Beck, L. , & Spiegelberg, H. L. (1995, June). Immunosuppressive actions of 1,25‐dihydroxyvitamin D3: Preferential inhibition of Th1 functions. The Journal of Nutrition, 125(6 Suppl), 1704S–1708S. 10.1093/jn/125.suppl_6.1704S [DOI] [PubMed] [Google Scholar]
- Levenson, C. W. (2006). Zinc: The new antidepressant? Nutrition Reviews, 64(1), 39–42. [DOI] [PubMed] [Google Scholar]
- Liao, M.‐T. , Wu, C.‐C. , Wu, S.‐F. V. , Lee, M.‐C. , Hu, W.‐C. , Tsai, K.‐W. , Yang, C.‐H. , Lu, C.‐L. , Chiu, S.‐K. , & Lu, K.‐C. (2021). Resveratrol as an adjunctive therapy for excessive oxidative stress in aging covid‐19 patients. Antioxidants, 10(9), 1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao, Y. , Xie, B. , Zhang, H. , He, Q. , Guo, L. , Subramanieapillai, M. , Fan, B. , Lu, C. , & McIntyre, R. S. (2019, August 5). Efficacy of omega‐3 PUFAs in depression: A meta‐analysis. Translational Psychiatry, 9(1), 190. 10.1038/s41398-019-0515-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddelow, S. A. , Guttenplan, K. A. , Clarke, L. E. , Bennett, F. C. , Bohlen, C. J. , Schirmer, L. , Bennett, M. L. , Munch, A. E. , Chung, W. S. , Peterson, T. C. , Wilton, D. K. , Frouin, A. , Napier, B. A. , Panicker, N. , Kumar, M. , Buckwalter, M. S. , Rowitch, D. H. , Dawson, V. L. , Dawson, T. M. , … Barres, B. A. (2017, January 26). Neurotoxic reactive astrocytes are induced by activated microglia. Nature, 541(7638), 481–487. 10.1038/nature21029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindseth, G. , Helland, B. , & Caspers, J. (2015, April). The effects of dietary tryptophan on affective disorders. Archives of Psychiatric Nursing, 29(2), 102–107. 10.1016/j.apnu.2014.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, F. , Zhu, Y. , Zhang, J. , Li, Y. , & Peng, Z. (2020, July 8). Intravenous high‐dose vitamin C for the treatment of severe COVID‐19: Study protocol for a multicentre randomised controlled trial. BMJ Open, 10(7), e039519. 10.1136/bmjopen-2020-039519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez‐Santamarina, A. , Lamas, A. , Del Carmen Mondragon, A. , Cardelle‐Cobas, A. , Regal, P. , Rodriguez‐Avila, J. A. , Miranda, J. M. , Franco, C. M. , & Cepeda, A. (2021, January 9). Probiotic effects against virus infections: New weapons for an old war. Foods, 10(1), 1–20. 10.3390/foods10010130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lordan, R. , Rando, H. M. , & Greene, C. S. (2021). Dietary supplements and nutraceuticals under investigation for COVID‐19 prevention and treatment. mSystems, 6(3), e00122‐00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, L. L. , Liu, H. M. , Luo, C. H. , He, Y. N. , Wang, F. , Huang, H. Z. , Han, L. , Yang, M. , Xu, R. C. , & Zhang, D. K. (2021). Fever and antipyretic supported by traditional Chinese medicine: A multi‐pathway regulation. Frontiers in Pharmacology, 12, 583279. 10.3389/fphar.2021.583279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahajan, G. J. , Vallender, E. J. , Garrett, M. R. , Challagundla, L. , Overholser, J. C. , Jurjus, G. , Dieter, L. , Syed, M. , Romero, D. G. , Benghuzzi, H. , & Stockmeier, C. A. (2018, March 2). Altered neuro‐inflammatory gene expression in hippocampus in major depressive disorder. Progress in Neuro‐Psychopharmacology & Biological Psychiatry, 82, 177–186. 10.1016/j.pnpbp.2017.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta, O. P. , Bhandari, P. , Raut, A. , Kacimi, S. E. O. , & Huy, N. T. (2020). Coronavirus disease (COVID‐19): Comprehensive review of clinical presentation. Frontiers in Public Health, 8, 582932. 10.3389/fpubh.2020.582932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinhardt, J. , Radke, J. , Dittmayer, C. , Franz, J. , Thomas, C. , Mothes, R. , Laue, M. , Schneider, J. , Brunink, S. , Greuel, S. , Lehmann, M. , Hassan, O. , Aschman, T. , Schumann, E. , Chua, R. L. , Conrad, C. , Eils, R. , Stenzel, W. , Windgassen, M. , … Heppner, F. L. (2021, February). Olfactory transmucosal SARS‐CoV‐2 invasion as a port of central nervous system entry in individuals with COVID‐19. Nature Neuroscience, 24(2), 168–175. 10.1038/s41593-020-00758-5 [DOI] [PubMed] [Google Scholar]
- Miller, A. H. , & Raison, C. L. (2016, January). The role of inflammation in depression: From evolutionary imperative to modern treatment target. Nature Reviews. Immunology, 16(1), 22–34. 10.1038/nri.2015.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mocking, R. J. , Harmsen, I. , Assies, J. , Koeter, M. W. , Ruhe, H. G. , & Schene, A. H. (2016, March 15). Meta‐analysis and meta‐regression of omega‐3 polyunsaturated fatty acid supplementation for major depressive disorder. Translational Psychiatry, 6, e756. 10.1038/tp.2016.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreau, R. A. , Whitaker, B. D. , & Hicks, K. B. (2002, November). Phytosterols, phytostanols, and their conjugates in foods: Structural diversity, quantitative analysis, and health‐promoting uses. Progress in Lipid Research, 41(6), 457–500. 10.1016/s0163-7827(02)00006-1 [DOI] [PubMed] [Google Scholar]
- Morelli, L. , & Capurso, L. J. J. (2012). FAO/WHO guidelines on probiotics: 10 years later. Journal of Clinical Gastroenterology, 46, S1–S2. [DOI] [PubMed] [Google Scholar]
- Morgan, C. I. , Ledford, J. R. , Zhou, P. , & Page, K. (2011, December 7). Zinc supplementation alters airway inflammation and airway hyperresponsiveness to a common allergen. Journal of Inflammation, 8, 36. 10.1186/1476-9255-8-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossink, J. (2020). Zinc as nutritional intervention and prevention measure for COVID–19 disease. BMJ Nutrition, Prevention & Health, 3(1), 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mostafa, W. Z. , & Hegazy, R. A. (2015, November). Vitamin D and the skin: Focus on a complex relationship: A review. Journal of Advanced Research, 6(6), 793–804. 10.1016/j.jare.2014.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouret, J. , Lemoine, P. , Minuit, M. P. , & Robelin, N. (1988). L‐tyrosine cures, immediate and long term, dopamine‐dependent depressions. Clinical and polygraphic studies. Comptes Rendus de l'Académie des Sciences. Série III, 306(3), 93–98 https://www.ncbi.nlm.nih.gov/pubmed/3126995 [PubMed] [Google Scholar]
- Nami, M. , Mehrabi, S. , Kamali, A.‐M. , Kazemiha, M. , Carvalho, J. , Derman, S. , Lakey‐Betia, J. , Vasquez, V. , & Kosagisharaf, R. (2020). A new hypothesis on anxiety, sleep insufficiency, and viral infections; reciprocal links to consider in today's “world vs. COVID‐19” endeavors. Frontiers in Psychiatry, 11, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson, A. N. , Turner, C. , Stone, B. M. , & Robson, P. J. (2004, June). Effect of Delta‐9‐tetrahydrocannabinol and cannabidiol on nocturnal sleep and early‐morning behavior in young adults. Journal of Clinical Psychopharmacology, 24(3), 305–313. 10.1097/01.jcp.0000125688.05091.8f [DOI] [PubMed] [Google Scholar]
- Niempoog, S. , Pawa, K. K. , & Amatyakul, C. (2012, January). The efficacy of powdered ginger in osteoarthritis of the knee. Journal of the Medical Association of Thailand, 95 Suppl 1, S59–S64 https://www.ncbi.nlm.nih.gov/pubmed/23964445 [PubMed] [Google Scholar]
- Nurtjahja‐Tjendraputra, E. , Ammit, A. J. , Roufogalis, B. D. , Tran, V. H. , & Duke, C. C. (2003). Effective anti‐platelet and COX‐1 enzyme inhibitors from pungent constituents of ginger. Thrombosis Research, 111(4‐5), 259–265. 10.1016/j.thromres.2003.09.009 [DOI] [PubMed] [Google Scholar]
- Nwanodi, O. (2018). Skin protective nutraceuticals: The current evidence in brief. Healthcare, 6(2), 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olaimat, A. N. , Aolymat, I. , Al‐Holy, M. , Ayyash, M. , Ghoush, M. A. , Al‐Nabulsi, A. A. , Osaili, T. , Apostolopoulos, V. , Liu, S.‐Q. , & Shah, N. P. (2020). The potential application of probiotics and prebiotics for the prevention and treatment of COVID‐19. NPJ Science of Food, 4(1), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oskouei, Z. , Akaberi, M. , & Hosseinzadeh, H. (2018, December). A glance at black cumin (Nigella sativa) and its active constituent, thymoquinone, in ischemia: A review. Iranian Journal of Basic Medical Sciences, 21(12), 1200–1209. 10.22038/ijbms.2018.31703.7630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyagbemi, A. A. , Saba, A. B. , & Ibraheem, A. O. (2009). Curcumin: From food spice to cancer prevention. Asian Pacific Journal of Cancer Prevention, 10(6), 963–967 https://www.ncbi.nlm.nih.gov/pubmed/20192567 [PubMed] [Google Scholar]
- Pan, W. , & Kastin, A. J. (2007, December). Tumor necrosis factor and stroke: Role of the blood‐brain barrier. Progress in Neurobiology, 83(6), 363–374. 10.1016/j.pneurobio.2007.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panche, A. N. , Diwan, A. D. , & Chandra, S. R. (2016). Flavonoids: An overview. Journal of Nutritional Science, 5, e47. 10.1017/jns.2016.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey, K. B. , & Rizvi, S. I. (2009, November–December). Plant polyphenols as dietary antioxidants in human health and disease. Oxidative Medicine and Cellular Longevity, 2(5), 270–278. 10.4161/oxim.2.5.9498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paramdeep, G. (2013, April–June). Efficacy and tolerability of ginger (Zingiber officinale) in patients of osteoarthritis of knee. Indian Journal of Physiology and Pharmacology, 57(2), 177–183 https://www.ncbi.nlm.nih.gov/pubmed/24617168 [PubMed] [Google Scholar]
- Parasher, A. (2021, May). COVID‐19: Current understanding of its pathophysiology, clinical presentation and treatment. Postgraduate Medical Journal, 97(1147), 312–320. 10.1136/postgradmedj-2020-138577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partyka, A. , Jastrzębska‐Więsek, M. , Szewczyk, B. , Stachowicz, K. , Sławińska, A. , Poleszak, E. , Doboszewska, U. , Pilc, A. , & Nowak, G. (2011). Anxiolytic‐like activity of zinc in rodent tests. Pharmacological Reports, 63(4), 1050–1055. [DOI] [PubMed] [Google Scholar]
- Patel, O. , Chinni, V. , El‐Khoury, J. , Perera, M. , Neto, A. S. , McDonald, C. , See, E. , Jones, D. , Bolton, D. , Bellomo, R. , Trubiano, J. , & Ischia, J. (2021, May). A pilot double‐blind safety and feasibility randomized controlled trial of high‐dose intravenous zinc in hospitalized COVID‐19 patients. Journal of Medical Virology, 93(5), 3261–3267. 10.1002/jmv.26895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel, S. S. , Acharya, A. , Ray, R. S. , Agrawal, R. , Raghuwanshi, R. , & Jain, P. (2020). Cellular and molecular mechanisms of curcumin in prevention and treatment of disease. Critical Reviews in Food Science and Nutrition, 60(6), 887–939. 10.1080/10408398.2018.1552244 [DOI] [PubMed] [Google Scholar]
- Patrick, R. P. , & Ames, B. N. (2014, June). Vitamin D hormone regulates serotonin synthesis. Part 1: Relevance for autism. The FASEB Journal, 28(6), 2398–2413. 10.1096/fj.13-246546 [DOI] [PubMed] [Google Scholar]
- Patrick, R. P. , & Ames, B. N. (2015, June). Vitamin D and the omega‐3 fatty acids control serotonin synthesis and action, part 2: Relevance for ADHD, bipolar disorder, schizophrenia, and impulsive behavior. The FASEB Journal, 29(6), 2207–2222. 10.1096/fj.14-268342 [DOI] [PubMed] [Google Scholar]
- Pazini, F. L. , Cunha, M. P. , & Rodrigues, A. L. S. (2019, March 8). The possible beneficial effects of creatine for the management of depression. Progress in Neuro‐Psychopharmacology & Biological Psychiatry, 89, 193–206. 10.1016/j.pnpbp.2018.08.029 [DOI] [PubMed] [Google Scholar]
- Prietl, B. , Treiber, G. , Pieber, T. R. , & Amrein, K. (2013, July 5). Vitamin D and immune function. Nutrients, 5(7), 2502–2521. 10.3390/nu5072502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proal, A. D. , & VanElzakker, M. B. (2021). Long COVID or post‐acute sequelae of COVID‐19 (PASC): An overview of biological factors that may contribute to persistent symptoms. Frontiers in Microbiology, 12, 698169. 10.3389/fmicb.2021.698169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin, C. , Zhou, L. , Hu, Z. , Zhang, S. , Yang, S. , Tao, Y. , Xie, C. , Ma, K. , Shang, K. , Wang, W. , & Tian, D. S. (2020, July 28). Dysregulation of immune response in patients with coronavirus 2019 (COVID‐19) in Wuhan, China. Clinical Infectious Diseases, 71(15), 762–768. 10.1093/cid/ciaa248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ragab, D. , Salah Eldin, H. , Taeimah, M. , Khattab, R. , & Salem, R. J. F. (2020). The COVID‐19 cytokine storm; what we know so far. Frontiers in Immunology, 11, 1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, M. T. , & Idid, S. Z. (2021, February). Can Zn be a critical element in COVID‐19 treatment? Biological Trace Element Research, 199(2), 550–558. 10.1007/s12011-020-02194-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rammal, H. , Bouayed, J. , Falla, J. , Boujedaini, N. , & Soulimani, R. (2010). The impact of high anxiety level on cellular and humoral immunity in mice. Neuroimmunomodulation, 17(1), 1–8. [DOI] [PubMed] [Google Scholar]
- Raveendran, A. V. , Jayadevan, R. , & Sashidharan, S. (2021, May–June). Long COVID: An overview. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 15(3), 869–875. 10.1016/j.dsx.2021.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read, S. A. , Obeid, S. , Ahlenstiel, C. , & Ahlenstiel, G. (2019, July 1). The role of zinc in antiviral immunity. Advances in Nutrition, 10(4), 696–710. 10.1093/advances/nmz013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter, S. , Gupta, S. C. , Park, B. , Goel, A. , & Aggarwal, B. B. (2011, May). Epigenetic changes induced by curcumin and other natural compounds. Genes & Nutrition, 6(2), 93–108. 10.1007/s12263-011-0222-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts, R. , Allen, S. , Chang, A. , Henderson, H. , Hobson, G. , Karania, B. , Morgan, K. , Pek, A. , Raghvani, K. , & Shee, C. (2013). Distinct mechanisms of relaxation to bioactive components from chamomile species in porcine isolated blood vessels. Toxicology and Applied Pharmacology, 272(3), 797–805. [DOI] [PubMed] [Google Scholar]
- Roman, M. , & Irwin, M. R. (2020, January). Novel neuroimmunologic therapeutics in depression: A clinical perspective on what we know so far. Brain, Behavior, and Immunity, 83, 7–21. 10.1016/j.bbi.2019.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe, A. , Narlawar, R. , Groundwater, P. W. , & Ramzan, I. (2011, January). Kavalactone pharmacophores for major cellular drug targets. Mini Reviews in Medicinal Chemistry, 11(1), 79–83. 10.2174/138955711793564088 [DOI] [PubMed] [Google Scholar]
- Rycroft, R. J. (2003, April). Recurrent facial dermatitis from chamomile tea. Contact Dermatitis, 48(4), 229. 10.1034/j.1600-0536.2003.00080.x [DOI] [PubMed] [Google Scholar]
- Sabir, M. S. , Haussler, M. R. , Mallick, S. , Kaneko, I. , Lucas, D. A. , Haussler, C. A. , Whitfield, G. K. , & Jurutka, P. W. (2018). Optimal vitamin D spurs serotonin: 1,25‐dihydroxyvitamin D represses serotonin reuptake transport (SERT) and degradation (MAO‐A) gene expression in cultured rat serotonergic neuronal cell lines. Genes & Nutrition, 13, 19. 10.1186/s12263-018-0605-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sack, M. , Hofbauer, A. , Fischer, R. , & Stoger, E. (2015, April). The increasing value of plant‐made proteins. Current Opinion in Biotechnology, 32, 163–170. 10.1016/j.copbio.2014.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeedi‐Boroujeni, A. , & Mahmoudian‐Sani, M.‐R. (2021). Anti‐inflammatory potential of Quercetin in COVID‐19 treatment. Journal of Inflammation, 18(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saja, K. , Babu, M. S. , Karunagaran, D. , & Sudhakaran, P. R. (2007, December 15). Anti‐inflammatory effect of curcumin involves downregulation of MMP‐9 in blood mononuclear cells. International Immunopharmacology, 7(13), 1659–1667. 10.1016/j.intimp.2007.08.018 [DOI] [PubMed] [Google Scholar]
- Savant, S. , Srinivasan, S. , & Kruthiventi, A. K. (2021). Potential nutraceuticals for COVID‐19. Nutrition and Dietary Supplements, 13, 25. [Google Scholar]
- Shakoor, H. , Feehan, J. , Al Dhaheri, A. S. , Ali, H. I. , Platat, C. , Ismail, L. C. , Apostolopoulos, V. , & Stojanovska, L. (2021, January). Immune‐boosting role of vitamins D, C, E, zinc, selenium and omega‐3 fatty acids: Could they help against COVID‐19? Maturitas, 143, 1–9. 10.1016/j.maturitas.2020.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma, A. , & Malviya, R. (2020). Effects of corona virus on the skin: Symptoms and risks. The Open Dermatology Journal, 14(1), 28–30. [Google Scholar]
- Sharma, P. , Batra, S. , Kumar, A. , & Sharma, A. (2017). In vivo antianxiety and antidepressant activity of Murraya paniculata leaf extracts. Journal of Integrative Medicine, 15(4), 320–325. [DOI] [PubMed] [Google Scholar]
- Sharma, S. , Batra, S. , Gupta, S. , Sharma, K. , Rahman, M. , & Kamal, M. A. (2021). Persons with co‐existing neurological disorders: Risk analysis, considerations and management in COVID‐19 pandemic. CNS & Neurological Disorders‐Drug Targets (Formerly Current Drug Targets‐CNS & Neurological Disorders), 21, 228–234. [DOI] [PubMed] [Google Scholar]
- Shep, D. , Khanwelkar, C. , Gade, P. , & Karad, S. (2019, April 11). Safety and efficacy of curcumin versus diclofenac in knee osteoarthritis: A randomized open‐label parallel‐arm study. Trials, 20(1), 214. 10.1186/s13063-019-3327-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla, R. K. , Dubey, A. K. , Garg, A. , Sharma, R. K. , Fiorino, M. , Ameen, S. M. , Haddad, M. A. , & Al‐Hiary, M. (2019, September 1). Natural polyphenols: Chemical classification, definition of classes, subcategories, and structures. Journal of AOAC International, 102(5), 1397–1400. 10.5740/jaoacint.19-0133 [DOI] [PubMed] [Google Scholar]
- Slominski, R. M. , Stefan, J. , Athar, M. , Holick, M. F. , Jetten, A. M. , Raman, C. , & Slominski, A. T. (2020). COVID‐19 and vitamin D: A lesson from the skin. Experimental Dermatology, 29(9), 885–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofowora, A. , Ogunbodede, E. , & Onayade, A. (2013, August 12). The role and place of medicinal plants in the strategies for disease prevention. African Journal of Traditional, Complementary, and Alternative Medicines, 10(5), 210–229. 10.4314/ajtcam.v10i5.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, J. A. , Kim, H. J. , Hong, S. K. , Lee, D. H. , Lee, S. W. , Song, C. S. , Kim, K. T. , Choi, I. S. , Lee, J. B. , & Park, S. Y. (2016, February). Oral intake of Lactobacillus rhamnosus M21 enhances the survival rate of mice lethally infected with influenza virus. Journal of Microbiology, Immunology, and Infection, 49(1), 16–23. 10.1016/j.jmii.2014.07.011 [DOI] [PubMed] [Google Scholar]
- Spacil, Z. , Novakova, L. , & Solich, P. (2008, June 30). Analysis of phenolic compounds by high performance liquid chromatography and ultra performance liquid chromatography. Talanta, 76(1), 189–199. 10.1016/j.talanta.2008.02.021 [DOI] [PubMed] [Google Scholar]
- Strasser, B. , Sperner‐Unterweger, B. , Fuchs, D. , & Gostner, J. M. (2017). Mechanisms of inflammation‐associated depression: Immune influences on tryptophan and phenylalanine metabolisms. Current Topics in Behavioral Neurosciences, 31, 95–115. 10.1007/7854_2016_23 [DOI] [PubMed] [Google Scholar]
- Subedi, L. , Tchen, S. , Gaire, B. P. , Hu, B. , & Hu, K. (2021). Adjunctive nutraceutical therapies for COVID‐19. International Journal of Molecular Sciences, 22(4), 1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundararaman, A. , Ray, M. , Ravindra, P. V. , & Halami, P. M. (2020, October). Role of probiotics to combat viral infections with emphasis on COVID‐19. Applied Microbiology and Biotechnology, 104(19), 8089–8104. 10.1007/s00253-020-10832-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- te Velthuis, A. J. , van den Worm, S. H. , Sims, A. C. , Baric, R. S. , Snijder, E. J. , & van Hemert, M. J. (2010, November 4). Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS Pathogens, 6(11), e1001176. 10.1371/journal.ppat.1001176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ter Ellen, B. M. , Dinesh Kumar, N. , Bouma, E. M. , Troost, B. , van de Pol, D. P. I. , van der Ende‐Metselaar, H. H. , Apperloo, L. , van Gosliga, D. , van den Berge, M. , Nawijn, M. C. , van der Voort, P. H. J. , Moser, J. , Rodenhuis‐Zybert, I. A. , & Smit, J. M. (2021, July 10). Resveratrol and pterostilbene inhibit SARS‐CoV‐2 replication in air‐liquid interface cultured human primary bronchial epithelial cells. Viruses, 13(7), 1–17. 10.3390/v13071335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres, M. , Rossello, C. A. , Fernandez‐Garcia, P. , Llado, V. , Kakhlon, O. , & Escriba, P. V. (2020, March 27). The implications for cells of the lipid switches driven by protein‐membrane interactions and the development of membrane lipid therapy. International Journal of Molecular Sciences, 21(7), 1–39. 10.3390/ijms21072322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trebaticka, J. , & Durackova, Z. (2015). Psychiatric disorders and polyphenols: Can they be helpful in therapy? Oxidative Medicine and Cellular Longevity, 2015, 248529. 10.1155/2015/248529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinchieri, G. (2003, February). Interleukin‐12 and the regulation of innate resistance and adaptive immunity. Nature Reviews. Immunology, 3(2), 133–146. 10.1038/nri1001 [DOI] [PubMed] [Google Scholar]
- Turner, E. H. , Loftis, J. M. , & Blackwell, A. D. (2006, March). Serotonin a la carte: Supplementation with the serotonin precursor 5‐hydroxytryptophan. Pharmacology & Therapeutics, 109(3), 325–338. 10.1016/j.pharmthera.2005.06.004 [DOI] [PubMed] [Google Scholar]
- Vaishya, R. , Jain, V. K. , & Iyengar, K. P. (2021). Musculoskeletal manifestations of COVID‐19. Journal of Clinical Orthopaedics and Trauma, 17, 280–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valizadeh, H. , Abdolmohammadi‐Vahid, S. , Danshina, S. , Ziya Gencer, M. , Ammari, A. , Sadeghi, A. , Roshangar, L. , Aslani, S. , Esmaeilzadeh, A. , Ghaebi, M. , Valizadeh, S. , & Ahmadi, M. (2020, December). Nano‐curcumin therapy, a promising method in modulating inflammatory cytokines in COVID‐19 patients. International Immunopharmacology, 89(Pt B), 107088. 10.1016/j.intimp.2020.107088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasek, M. J. , Garber, C. , Dorsey, D. , Durrant, D. M. , Bollman, B. , Soung, A. , Yu, J. , Perez‐Torres, C. , Frouin, A. , Wilton, D. K. , Funk, K. , DeMasters, B. K. , Jiang, X. , Bowen, J. R. , Mennerick, S. , Robinson, J. K. , Garbow, J. R. , Tyler, K. L. , Suthar, M. S. , … Klein, R. S. (2016, June 23). A complement‐microglial axis drives synapse loss during virus‐induced memory impairment. Nature, 534(7608), 538–543. 10.1038/nature18283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan, L. , Li, Y. , Zhang, Z. , Sun, Z. , He, Y. , & Li, R. (2018, November 5). Methylenetetrahydrofolate reductase and psychiatric diseases. Translational Psychiatry, 8(1), 242. 10.1038/s41398-018-0276-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wimalawansa, S. J. (2019, May 11). Vitamin D deficiency: Effects on oxidative stress, epigenetics, gene regulation, and aging. Biology (Basel), 8(2), 1–15. 10.3390/biology8020030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, C. P. , Rinaldi, N. A. , & Ho, E. (2015, May). Zinc deficiency enhanced inflammatory response by increasing immune cell activation and inducing IL6 promoter demethylation. Molecular Nutrition & Food Research, 59(5), 991–999. 10.1002/mnfr.201400761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo, M. S. , Malsy, J. , Pottgen, J. , Seddiq Zai, S. , Ufer, F. , Hadjilaou, A. , Schmiedel, S. , Addo, M. M. , Gerloff, C. , Heesen, C. , Schulze Zur Wiesch, J. , & Friese, M. A. (2020). Frequent neurocognitive deficits after recovery from mild COVID‐19. Brain Communications, 2(2), fcaa205. 10.1093/braincomms/fcaa205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, G. D. (2019, January). Unlocking the potential of natural products in drug discovery. Microbial Biotechnology, 12(1), 55–57. 10.1111/1751-7915.13351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing, Y. , Zhao, B. , Yin, L. , Guo, M. , Shi, H. , Zhu, Z. , Zhang, L. , He, J. , Ling, Y. , Gao, M. , Lu, H. , Mao, E. , & Zhang, L. (2021, March 20). Vitamin C supplementation is necessary for patients with coronavirus disease: An ultra‐high‐performance liquid chromatography‐tandem mass spectrometry finding. Journal of Pharmaceutical and Biomedical Analysis, 196, 113927. 10.1016/j.jpba.2021.113927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan, Y. , Chen, H. , Chen, L. , Cheng, B. , Diao, P. , Dong, L. , Gao, X. , Gu, H. , He, L. , & Ji, C. (2020). Consensus of Chinese experts on protection of skin and mucous membrane barrier for health‐care workers fighting against coronavirus disease 2019. Dermatologic Therapy, 33(4), e13310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, Q. , Wu, S. , Mao, X. , Wang, W. , & Tai, H. (2013). Inhibition effect of curcumin on TNF‐alpha and MMP‐13 expression induced by advanced glycation end products in chondrocytes. Pharmacology, 91(1‐2), 77–85. 10.1159/000345345 [DOI] [PubMed] [Google Scholar]
- Yoshikawa, T. , Hill, T. , Li, K. , Peters, C. J. , & Tseng, C. T. (2009, April). Severe acute respiratory syndrome (SARS) coronavirus‐induced lung epithelial cytokines exacerbate SARS pathogenesis by modulating intrinsic functions of monocyte‐derived macrophages and dendritic cells. Journal of Virology, 83(7), 3039–3048. 10.1128/JVI.01792-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahedipour, F. , Hosseini, S. A. , Sathyapalan, T. , Majeed, M. , Jamialahmadi, T. , Al‐Rasadi, K. , Banach, M. , & Sahebkar, A. (2020, November). Potential effects of curcumin in the treatment of COVID‐19 infection. Phytotherapy Research, 34(11), 2911–2920. 10.1002/ptr.6738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemb, P. , Bergman, P. , Camargo, C. A., Jr. , Cavalier, E. , Cormier, C. , Courbebaisse, M. , Hollis, B. , Joulia, F. , Minisola, S. , Pilz, S. , Pludowski, P. , Schmitt, F. , Zdrenghea, M. , & Souberbielle, J. C. (2020, September). Vitamin D deficiency and the COVID‐19 pandemic. Journal of Global Antimicrobial Resistance, 22, 133–134. 10.1016/j.jgar.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng, Z. Y. , Feng, S. D. , Chen, G. P. , & Wu, J. N. (2021, January 18). Predictive value of the neutrophil to lymphocyte ratio for disease deterioration and serious adverse outcomes in patients with COVID‐19: A prospective cohort study. BMC Infectious Diseases, 21(1), 80. 10.1186/s12879-021-05796-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, L. , & Liu, Y. (2020, May). Potential interventions for novel coronavirus in China: A systematic review. Journal of Medical Virology, 92(5), 479–490. 10.1002/jmv.25707 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


