Abstract
Background
Identifying proximal risk factors for suicidal ideation that are modifiable and relevant for adolescents and young adults is critical for suicide prevention. This study used an intensive monitoring approach to examine whether objectively‐ and subjectively‐ measured sleep characteristics predict next‐day suicidal ideation occurrence and intensity through affective reactivity to interpersonal events in young people at high risk for suicide.
Methods
Participants included 59 (13–23 years; 76% White; 75% female) adolescents and young adults undergoing intensive outpatient program treatment for depression and suicidality. Participants completed daily ratings of suicidal ideation, sleep quality, and affective reactivity to positive and negative interpersonal events for up to 3 months (M = 56 days, SD = 24.13). Actigraphy captured behavioral sleep duration and timing. Multilevel modeling was used to evaluate within‐person fluctuations in sleep and affective reactivity as predictors of suicidal ideation, and multilevel mediation tested the indirect effects of sleep on suicidal ideation via affective reactivity to interpersonal events.
Results
Results indicate significant indirect effects of objectively measured sleep duration and subjective sleep quality on next‐day suicidal ideation via affective reactivity to negative and positive interpersonal events, respectively. Shorter‐than‐usual sleep predicted the presence and intensity of next‐day suicidal ideation via heightened affective reactivity to negative interpersonal events. Worse sleep quality than usual predicted next‐day suicidal ideation via reduced affective reactivity to positive interpersonal events.
Conclusions
Affectivity reactivity is a proximal mechanism through which sleep indices may influence risk for suicidal thinking on a daily basis. Findings highlight the utility of targeting sleep and emotion regulation in suicide prevention among adolescents and young adults at high‐risk for suicide.
Keywords: Adolescence, suicide, interpersonal, affective reactivity, sleep, intensive monitoring, actigraphy
Introduction
Suicide is a major public health problem and the second leading cause of death among adolescents and young adults (CDC, 2020). Despite advancements in understanding risk factors for suicidal ideation (SI) and behavior, our ability to predict suicide using established risk factors remains only slightly better than chance (Franklin et al., 2017). Limited progress may be due, in part, to the predominant focus of prior research on distal or static risk factors. Yet, research indicates that SI fluctuates across days within individuals (Kleiman et al., 2017), with 86.5% of proximal suicide planning steps taking place within 1 week of making a suicide attempt and 66.6% occurring within 12 hr of suicidal behavior (Millner et al., 2018). Despite the importance of predicting suicidal behavior, there is clinical utility in identifying factors that predict the occurrence of SI among individuals who are at high‐risk for suicide (Jobes & Joiner, 2019; Kleiman, 2020). Identifying risk factors that are proximal, dynamic, and also modifiable (or amenable to intervention) for near‐term SI is critical to better understand when individuals are most at risk (Glenn & Nock, 2014), which may inform suicide prevention programs to prevent suicidal behavior and ultimately death by suicide.
Sleep and circadian processes constitute such factors as time‐varying, proximal, and modifiable risk factors for SI that also are particularly relevant to the developmental transition of adolescence and young adulthood (Goldstein & Franzen, 2022). Indeed, research has linked disruptions in sleep with prospective SI among adolescents and young adults (Harris, Huang, Linthicum, Bryen, & Ribeiro, 2020; Liu, Steele, et al., 2020). Given that both sleep disruption and SI fluctuate across days (Kleiman et al., 2017; Littlewood et al., 2019), intensive monitoring designs are particularly well‐suited to examine whether changes in sleep within person proximally influence subsequent SI on a daily basis. Recent research using intensive monitoring designs finds that sleep disturbance predicts next‐day active SI (Brüdern et al., 2022; Littlewood et al., 2019), including self‐reported sleep problems among adolescents following discharge from a psychiatric hospital (Glenn et al., 2022). Despite these advancements, our understanding of the potential mechanisms through which sleep and SI are linked in adolescents and young adults remains limited.
Affective reactivity to interpersonal events may constitute one such mechanism. Social relationships and socio‐emotional responses have long been implicated in research and theories of suicide (Connor & Nock, 2014) and are highly salient among young people (King & Merchant, 2008; Stewart et al., 2019). Individuals who are at heightened risk for suicide (based on having recent SI and/or a lifetime history of suicide attempts) are more likely to have interpersonal stressors (Stewart et al., 2019) and heightened affective reactivity to negative interpersonal events (Herres, Ewing, & Kobak, 2016). Recent studies also highlight the role of interpersonal factors, such as social connectedness, burdensomeness, and higher levels of daily negative life events on daily SI (Czyz, Horwitz, Arango, & King, 2019; Glenn, Kleiman, Kandlur, Esposito, & Liu, 2021), further highlighting the potential importance of affective responses to interpersonal events as proximal predictors of daily SI. Research also demonstrates a robust association between anhedonia (including social anhedonia) and current SI (Ducasse et al., 2018). These findings suggest that reduced ability to enjoy positive interactions, in addition to heightened reactivity to negative interactions, may be important in understanding risk for SI. Consequently, adolescents and young adults at high risk for suicide may have both more intense emotional distress following negative interpersonal events and be less responsive to positive interpersonal events that might otherwise buffer or protect them from near‐term SI.
Sleep disruptions have been linked with greater affective dysregulation, including more negative emotions or distress and blunted positive affect (Palmer & Alfano, 2017). Experimentally, sleep restriction in middle school‐aged youth led to increased physiological reactivity to negative affective stimuli, higher negative and lower positive mood self‐reports, and increased negative interpersonal behaviors during discussion of a conflict (McMakin et al., 2016). Shorter sleep duration, later sleep timing (both measured with actigraphy), and poorer self‐reported sleep quality were associated with blunting of ventral striatal activity to monetary reward in youth ages 11–13 (Holm et al., 2009). These studies support the role of affective reactivity as a potential mechanism through which sleep processes might proximally influence SI. In adults, experimental and observational studies have demonstrated the effects of sleep duration and disturbances on increases in negative affect, including neurobiological stress reactivity (Konjarski, Murray, Lee, & Jackson, 2018). Further, a recent study of adults found that nights of shorter‐than‐usual sleep duration predicted greater decreases in positive affect in response to daily stressors and smaller increases in positive affect in response to daily positive events, compared to usual sleep duration (Sin, Wen, Klaiber, Buxton, & Almeida, 2020). Due to heightened sensitivity to social events among adolescents and young adults (Schriber & Guyer, 2016), these individuals may be even more reactive to negative and less reactive to positive interpersonal events that occur following a night of shorter, later, or poorer sleep. Thus, proximal SI may be more likely to occur following a night of poor sleep because of increased negative emotions and reduced positive emotions following interpersonal events (Littlewood et al., 2019).
The goal of the present study was to examine affective reactivity to interpersonal events as a potential mechanism through which disrupted sleep might be associated with SI among adolescents and young adults at high risk for suicide. Given the importance of examining proximal predictors for SI at the individual level, the current study used an intensive longitudinal design to evaluate within‐person associations of daily sleep on next‐day affective reactivity and suicidal ideation among adolescents and young adults at high risk for suicidal behavior. Intensive monitoring designs provide the unique opportunity to disentangle near‐term predictors of SI within individuals (Brüdern et al., 2022; Glenn, Kleiman, Kearns, et al., 2021; Kleiman et al., 2017; Littlewood et al., 2019), allowing for each person to be their own control over time and taking into account all stable person‐level factors (Russell & Gajos, 2020). In recent years, intensive monitoring designs have been demonstrated to be acceptable and feasible, and to better capture the occurrence of SI among clinical samples of adolescents than end‐of‐study assessments (Czyz, King, & Nahum‐Shani, 2018). Thus, using intensive monitoring for longer periods of time may identify proximal predictors and actionable mechanisms linking sleep and SI at the daily level. In this study, it was hypothesized that shorter, later, and poorer sleep compared to an individual's usual amount (or average) would predict heightened negative and blunted positive next‐day affective reactivity to interpersonal events, which would, in turn, predict the occurrence and intensity of same‐day SI. Ultimately, results of this study will contribute to identifying a proximal and modifiable pathway through which adolescents and young adults are at heightened risk for daily SI, which is critical to inform intervention and prevention programs targeting high‐risk young people.
Method
Participants and recruitment
Adolescents and young adults at high risk for suicidal behavior were recruited from two Intensive Outpatient Programs (IOP) for depression and suicidality—one for secondary students and one for college students. These IOPs serve as a hospital diversion and/or as a step‐down from inpatient care. Treatment consists of three‐hour sessions three times per week of skills groups, individual psychotherapy, and medication management. Potentially eligible study participants were identified and referred by clinic staff during the first month of IOP treatment. Participants were informed that participation in the study was voluntary and separate from clinical services rendered. In total, 203 individuals were approached about the study, 64 participants consented/assented for the study (5 of whom were withdrawn prior to completing the baseline assessment, one due to requiring a higher level of care, 2 because they were no longer receiving care within the clinic, and 2 changed their mind), and 59 participants contributed data. Reasons cited for declining participation included time commitment and/or a desire to focus only on treatment.
Participants (and parents for youth under the age of 18) provided informed consent and assent to participate. The only inclusion criteria for this study were being enrolled in the clinic IOP, willingness to participate, having a parent willing to consent (for youth under the age of 18), and access to a cellphone or computer at home. Participants received monetary compensation of up to $278 for completing all parts of the study, including baseline, monthly study visits, and each day that the daily assessments were completed and each day the actigraph was worn during the intensive monitoring study portion. Participants also received a bonus each month based on adherence for completing at least 25 days/month of the intensive monitoring portion. The University Institutional Review Board approved study procedures.
Procedure
At a baseline assessment and at monthly follow‐up visits, participants completed clinical interviews and self‐report questionnaires. The clinical interview included the clinician‐administered Adolescent Longitudinal Follow‐Up Evaluation (ALIFE) Psychiatric Severity Rating (PSR) scales (Keller et al., 1987), which yielded week‐by week ratings of DSM diagnoses prior to study enrollment. Study assessors utilized diagnoses listed in the electronic medical record from the participants' clinical intake assessment at the affiliated clinic to inform the PSR interview. At the baseline assessment, participants were provided with an actigraph and instructions for completing daily surveys and wearing actigraphic devices. For up to 3 months, participants were asked to continuously wear their actigraph and complete twice‐daily ratings throughout their study participation using a secure web‐based platform. Participants received a link via SMS text messaging (or email for participants without access to a cellphone), which directly launched a secure web‐based platform to complete assessments without requiring a login. Daily assessment links were sent 30 min after habitual waketimes (subjective sleep diary assessment) and 45 min before habitual bedtimes (daily suicidal thoughts, depression severity, and reactivity to positive and negative interpersonal events), although participants could click on a prior link if they woke up or went to bed earlier than these habitual times. Daily assessments and other research procedures were halted if participants were no longer enrolled in either IOP or outpatient treatment within the clinic. Given the naturalistic nature and design of the study, the length of study participation differed based on each participants' treatment course and plan.
If participants endorsed any level of suicidal ideation on the daily assessments, an automated message was immediately triggered that prompted the participant to contact the provided emergency phone numbers if they felt they could not remain safe. If suicidal ideation with intent and/or recent suicidal behavior was endorsed, email alerts were sent to the study team and also conveyed to the participant's treatment team. Study investigators and/or clinic staff conducted a suicide risk assessment within 24 hr to ensure participant safety. Our approach to participant safety was largely consistent with expert consensus statements on ethical and safety practices for conducting digital monitoring studies with individuals at risk of suicide (Nock et al., 2021). More details on the suicide safety protocol during the intensive monitoring study are available in the Supporting Information (Appendix S1).
Measures
Behavioral sleep assessment
Daily behavioral sleep data were collected using actigraphy—the gold standard objective ambulatory monitoring method (Meltzer, Montgomery‐Downs, Insana, & Walsh, 2012). Participants wore a GT9x Link actigraph (ActiGraph Corp, Pensacola, FL), a wristwatch‐sized device that records the number of movements using average activity in 60‐s epochs. Participants were instructed to wear actigraphs continuously (except when swimming or engaging in other high‐intensity sports), and devices were charged every 1–2 weeks at in‐person clinical visits. The Cole‐Kripke algorithm, implemented in ActiLife software (ActiGraph Corp, Pensacola, FL), was used to compute sleep epochs (Cole, Kripke, Gruen, Mullaney, & Gillin, 1992). The algorithm has been validated against polysomnography and other actigraph devices in both adolescents and adults (Meltzer, Walsh, Traylor, & Westin, 2012; Quante et al., 2018). Sleep period detection options in ActiLife included a bedtime definition of 10 min and wake time definition of 20 min. Primary sleep variables derived from actigraphy included sleep duration (i.e. total time sleep during nocturnal sleep) and sleep timing (e.g. timing of sleep onset).
Subjective daily sleep assessment
Each morning, participants completed a sleep diary (Pittsburgh Sleep Diary; Monk et al., 1994), reporting the time they went to bed (“lights out”), the time they woke up, and sleep quality (Visual Analogue Scale [VAS] from 0 “very bad” to 100 “very good”). In the current study, sleep quality was used as the primary subjective sleep variable of interest.
Daily suicidal ideation and depression severity
Each night, participants indicated whether they had suicidal thoughts (passive death wish, ideation, plan, or intent) derived from the Columbia‐Suicide Severity Rating Scale (C‐SSRS; Posner et al., 2011). Here, we focus on reports of Suicidal Ideation (“I thought about killing myself”: No/Yes) and intensity of suicidal thoughts (“How intense were your thoughts of killing yourself”?). Participants responded to these questions on a VAS scale of 0 (“Not at all intense”) to 100 (“Very intense”), which has been validated in prior research for suicidal thoughts (Bryan, 2019). Participants also reported daily depressed mood: “The worst my depression was today”, using a VAS from 0 (“I didn't feel depressed at all”) to 100 (“Horrible, the worst it gets”), which was included as a covariate in the current study. VAS scales are commonly used in research with intensive monitoring designs to assess mood (Hall, Scherner, Kreidel, & Rubel, 2021).
Daily interpersonal events
Participants responded to whether they experienced any negative or positive events that day involving other people (No/Yes). For negative events, participants then responded to “How stressful/upsetting was your most negative event (conflict/excluded/insulted) today?” on a scale of 0 “Not at all upsetting” to 100 “Extremely upsetting”. For positive events, participants reported “How enjoyable/pleasant was your most positive event (had fun/was complimented) today?”, with scores ranging from 0 “Not at all enjoyable” to 100 “Extremely enjoyable”. Participants selected who was involved in the events (e.g. family, peers, and/or other adults). To confirm only interpersonal events were included, events were removed if participants endorsed that an event had occurred, but did not specify that it involved anyone (N = 17 [0.008%] observations removed). Of note, participants were trained by research assistants on the daily survey protocol, provided with examples of daily interpersonal events, and instructed how to use the subjective ratings scales.
More details about the selection and construction of the daily surveys are included in the Supporting Information (Appendix S2), along with the limitations and future directions for ensuring item validity.
Analytic plan
Descriptive tests were conducted to examine within‐person correlations for primary study variables. Variability in study outcomes was calculated using intraclass coefficients (ICCs) to estimate variance at the between‐ and within‐person levels. Multilevel modeling was conducted in R (R Core Team, 2021) using lme4 (Aguiar & Sala, 1998) for linear models. Continuous predictors were person‐centered to compute within‐person daily fluctuations in sleep compared to an individual's mean across the study period. Between‐person sleep characteristics (i.e. averages across the study) were included as covariates in the models. Random intercepts were included to allow for individual variations in outcomes. Between‐person study covariates included age and gender. Within‐person (level 1) covariates included time (study day) and prior‐day depression (lagged daily depressed mood rating), which provides a more conservative test of the effects of sleep and affective reactivity on next‐day SI beyond the effect of daily depression. To determine directionality of associations, supplemental multilevel models were conducted examining reverse associations of within‐person fluctuations in positive and negative affective ratings predicting that night's sleep.
The glmer package in R was used to test the multilevel logistic models with a random intercept to examine whether affective reactivity to positive and negative events predicted same‐day SI. Within‐person affective responses to positive and negative events (i.e. individual fluctuations compared to a person's own mean) were entered in models as predictors of daily SI. Multilevel linear modeling analyses examined whether affective responses to interpersonal events predicted daily SI intensity on the days when SI was endorsed. Between‐person means of affective responses across the study period also were included in these models.
Indirect effects of within‐person fluctuations of sleep on SI (occurrence and intensity) via affective reactivity to interpersonal events were estimated using multilevel mediation models within a 1‐1‐1‐ multilevel modeling framework (Preacher, Zyphur, & Zhang, 2010) conducted in Mplus (Muthén & Muthén, 1998‐2017). Given the focus on indirect effects, evidence of a direct effect between sleep and SI (c′) is not necessary to conduct a test of the indirect effects (a′*b′)(Hayes & Preacher, 2010), which is distinct from a causal steps approach to mediation. Direct effects of within‐person sleep fluctuations on next‐day SI occurrence and intensity were evaluated in these models to estimate main effects (c′). Analyses focused on evaluating indirect effects only when there were significant relationships identified in prior analyses of within‐person sleep and affective reactivity (a′), and affective reactivity and SI (b′). Affective reactivity to interpersonal events (positive or negative) were included as (Level 1) mediating variables, person‐centered sleep measures as (Level 1) predictor variables, and SI occurrence and intensity as (Level 1) dependent variables. Models were separately conducted for each indirect effect. All models included a random intercept. Dependent and mediating variables were regressed on the predictor variables and all covariates, and the dependent variable was regressed on the mediating variable. Between‐person sleep and affective reactivity (level 2) were also included in the model to covary for between‐person effects. Monte Carlo integration and 95% confidence intervals were used to determine significance of indirect effects. Using PASS software (Ahn, Heo, & Zhang, 2015; Olivier, May, & Bell, 2017; PASS, 2020), power curve analyses for multilevel modeling studies indicate adequate power (.80) to detect medium effects for within‐person analyses for both logistic and linear multilevel models. 1 There also was 80% power to detect significant mediation effects, as long as the two paths of the indirect pathway are of at least medium size.
Results
Preliminary analyses
A total of 59 individuals between the ages of 13–23 (75% female sex at birth; Mean age = 16.59, SD = 2.74) participated in the study. Table 1 includes demographic information, including psychiatric comorbidity, and within‐person means for primary study variables. Across all participants, there was a total of 3,475 days during which data could be collected (M = 56.31; SD = 24.13; range = 11–90). However, as is common in intensive monitoring designs, there was some missing data due to equipment failures and study protocol non‐adherence. For actigraphy, there were equipment or data issues on 432 days (12.43%). Of possible days for actigraphy data collection (3,043 days total across participants), adherence was 92% on average across all participants (20–100%; M = 46.58 days, SD = 23.29, 7–90 days). For daily surveys, there were issues with data collection (web‐based platform) on 176 days (5%). Of possible days for survey completion (3,299 days across all participants), participants completed 82% of morning surveys (16–100%; M = 45.02 days, SD = 25.01, range = 10–88 days); and 83% of evening surveys (30–100%; M = 45.00 days, SD = 25.29, range = 11–90 days).
Table 1.
Demographics and primary study variable descriptives
| Variables | Sample |
|---|---|
| Gender, n (%) | |
| Female | 44 (74.58%) |
| Male | 15 (25.42%) |
| Race, n (%) | |
| White | 45 (76.27%) |
| Black or African American | 4 (6.78%) |
| Asian | 6 (10.17%) |
| Other (or not specified) | 4 (6.78%) |
| Ethnicity, n (%) | |
| Hispanic or Latino | 2 (3%) |
| Age, mean (SD) | 16.59 (2.74) |
| Clinical/Psychiatric Presentation | |
| Depressive episode, n (%) | 59 (100%) |
| Any anxiety disorder | 41 (69.49%) |
| Post‐traumatic stress disorder | 7 (11.86%) |
| History of hypo/mania | 7 (11.86%) |
| Lifetime suicide attempt | 26 (44.07%) |
| Any psychiatric medication | 53 (89.83%) |
| Depression medication, n (%) | 39 (66.10%) |
| Study variables, mean (SD) | |
| Negative affective reactivity | 53.97 (14.03) |
| Positive affective reactivity | 65.08 (11.76) |
| Sleep duration | 6.91 (0.90) |
| Sleep timing (onset), hours from midnight (24) | 25.07 (1.67) |
| Sleep quality | 52.59 (12.87) |
| Suicidal ideation (percent, range) | 21.78% (0–43) |
| Suicidal ideation intensity | 49.25 (14.06) |
All study variables (affective reactivity, sleep, and suicidal ideation) are averages of within‐person means. Suicidal ideation days and intensity are reported for those who endorsed any suicidal ideation during the study (N = 44). Psychiatric ratings are based on the clinician‐administered Psychiatric Severity Rating (PSR; Keller et al., 1987) scale at the baseline assessment (all ratings at or above 4 out of 6 on the PSR). Anxiety disorder includes any of the following current disorders: panic disorder, agoraphobia, specific phobia, separation anxiety disorder, social anxiety disorder, or generalized anxiety disorder; History of hypo/mania disorder includes both hypomanic and manic episodes (indicating bipolar I or II disorder). In the sample, 3 (5.08%) participants had Attention‐Deficit Hyperactive Disorder, 3 (5.08%) participants had Obsessive–Compulsive Disorder, and 1 participant had cannabis abuse disorder. There were no participants with eating disorders, conduct disorder, oppositional defiant disorder, or other substance use disorders. Please note that a full diagnostic history was not obtained in the current study. Medical records from the participants' clinical intake assessment at the affiliated clinic informed the PSR interview. Since not all disorder modules were administered by study clinicians, participants' full clinical history may not be fully captured. Depression medication included selective serotonin reuptake inhibitors (SSRI), selective norepinephrine reuptake inhibitors (SNRI), and Bupropion. Sleep timing 24 represents 12 AM.
In total, 44% of the sample reported a past suicide attempt. Across all participants, 74.58% of participants reported SI on at least one day over the study period. There were 481 days on which individuals endorsed SI, and a total of 466 days in which participants reported SI intensity (M = 49.25 out of 100; SD = 14.06, range 2–100). On average, participants reported SI on 21.78% of days that they participated in the study (range = 0–43% of days per person), which was 18% of all study days across all participants. In terms of safety alerts resulting from reports of intent or attempt, there were 47 suicide alerts from 23 distinct participants, which included 11 participants generating one alert, six generating two alerts, four generating three alerts, and two generating five or more alerts.
Self‐reported sleep quality was correlated with actigraphy‐derived sleep duration (r = .24, p < .001) and sleep onset timing (r = −.11, p < .001), and sleep duration was correlated with sleep timing (r = .41, p < .001). Individuals who reported more affective reactivity to negative interpersonal events reported less affective reactivity to positive interpersonal events (r = −.17, p < .001). ICC analyses indicated that there was considerable variability within‐person for sleep domains (58–77%), affective ratings for interpersonal events (74–76%), and SI occurrence (75%) and intensity (80%).
Sleep and affective reactivity to negative and positive interpersonal events
Individual fluctuations in sleep duration predicted next‐day affective reactivity to negative interpersonal events (Table 2; Figure 1A), such that getting shorter sleep compared to an individual's usual amount (i.e. lower levels relative to their own mean) predicted higher levels of next‐day affective reactivity. Individual fluctuations in sleep timing or sleep quality did not predict next‐day affective reactivity (Table 2). Within‐person fluctuations in sleep timing and sleep quality predicted affective reactivity to positive interpersonal events (Table 3); both later‐than‐usual sleep timing and poorer‐than‐usual sleep quality, but not shorter‐than‐usual sleep duration, predicted lower levels of next‐day affective responsiveness to positive interpersonal events (Figure 1B,C).
Table 2.
Sleep domains predicting next‐day negative affective reactivity to negative interpersonal events
| Predictors | Outcome: Negative affective reactivity | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1: Sleep duration | Model 2: Sleep timing | Model 3: Sleep quality | |||||||
| Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | |
| (Intercept) | 53.63 | .83 | <.001 | 53.48 | 3.09 | <.001 | 51.67 | 2.92 | <.001 |
| Age | −2.73 | .55 | <.001 | −2.84 | .58 | <.001 | −2.31 | .51 | <.001 |
| Gender | 1.39 | 3.34 | .68 | 1.64 | 3.35 | .63 | 3.42 | 3.14 | .28 |
| Prior‐day depression | .12 | .03 | <.001 | .12 | .03 | <.001 | .14 | .03 | <.001 |
| Study Day | .03 | .03 | .27 | .03 | .03 | .27 | .02 | .03 | .39 |
| Sleep domain | |||||||||
| Between‐person average | .11 | 1.55 | .94 | .51 | 1.00 | .63 | .30 | .10 | <.004 |
| Within‐person fluctuations | −1.19 | .37 | .001 | −.30 | .38 | .43 | −.06 | .03 | .06 |
| Random effects | |||||||||
| Residual (σ2) | 514.00 | 517.28 | 515.17 | ||||||
| Intercept (τ00) | 78.11 | 78.32 | 65.18 | ||||||
Continuous between‐person (level 2) predictors were centered. Age and gender are between‐person (level 2) covariates. Prior‐depression reflects depressed mood the prior day (lagged). Both prior‐day depression and study day are within‐person (level 1) covariates. Within‐person fluctuations reflect person‐centered fluctuations from individual means. Unstandardized regression estimates are included.
The bold values indicate statistically significance (p <.05).
Figure 1.
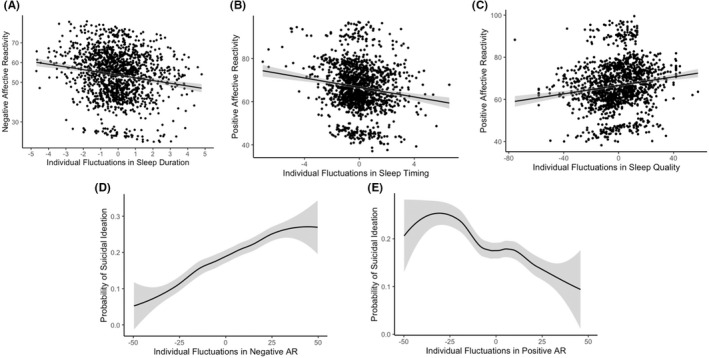
Direct effects of sleep, affective reactivity to negative and positive events, and probability of suicidal ideation. (A) Shorter sleep compared to an individual's usual amount predicted higher levels of next‐day affective reactivity to negative interpersonal events. (B) Later‐than‐usual sleep timing predicted lower levels of next‐day affective reactivity to positive interpersonal events. (C) Poorer‐than‐usual sleep quality predicted lower levels of next‐day affective reactivity to positive interpersonal events. (D) Higher levels of affective reactivity to negative interpersonal events relative to an individual's mean significantly predicted days on which they reported having suicidal ideation. (E) Lower levels of affective reactivity to positive interpersonal events relative to an individual's mean significantly predicted days on which they reported having suicidal ideation
Table 3.
Sleep domains predicting next‐day positive affective reactivity to positive interpersonal events
| Predictors | Outcome: Positive affective reactivity | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1: Sleep Duration | Model 2: Sleep Timing | Model 3: Sleep Quality | |||||||
| Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | |
| (Intercept) | 64.57 | 3.13 | <.001 | 64.53 | 13.13 | <.001 | 62.31 | 2.94 | <.001 |
| Age | −.92 | .56 | .11 | −1.02 | .60 | .09 | −.22 | .52 | .67 |
| Gender | 1.57 | 3.46 | .65 | 1.64 | 3.46 | .64 | 3.91 | 3.24 | ,23 |
| Prior‐day depression | −.08 | .02 | <.001 | −.08 | .02 | <.001 | −.08 | .02 | <.001 |
| Study Day | .03 | .02 | .16 | .03 | .02 | .12 | .03 | .02 | .11 |
| Sleep domain | |||||||||
| Between‐person average | −1.96 | 1.64 | .24 | .82 | 1.02 | .42 | .50 | .11 | <.001 |
| Within‐person fluctuations | .13 | .28 | .65 | −.69 | .29 | .02 | .09 | .03 | <.001 |
| Random effects | |||||||||
| Residual (σ2) | 334.34 | 333.32 | 328.82 | ||||||
| Intercept (τ00) | 107.50 | 107.20 | 88.97 | ||||||
Continuous between‐person (level 2) predictors were centered. Age and gender are between‐person (level 2) covariates. Prior‐day depression reflects depressed mood the prior day (lagged). Both prior‐day depression and study day are within‐person (level 1) covariates. Within‐person fluctuations reflect person‐centered fluctuations from individual means. Unstandardized regression estimates are included.
The bold values indicate statistically significance (p <.05).
Testing the reverse associations, within‐person changes in affective reactivity to negative interpersonal events did not predict that night's sleep duration, timing, or quality (Table S1). Only within‐person fluctuations in positive affective reactivity predicted that night's sleep quality, such that higher‐than‐usual positive affective reactivity to interpersonal events predicted better sleep quality that night. There was no effect of positive affective reactivity predicting that night's sleep duration or timing (Table S1).
Affective reactivity to interpersonal events and suicidal ideation
Multilevel logistic models indicated that higher levels of affective reactivity to negative interpersonal events and lower levels of affective reactivity to positive interpersonal events relative to a person's own mean significantly predicted days on which individuals reported having SI (Table 4; Figure 1D,E), covarying for prior‐day depression and between‐person averages. Individual fluctuations in affective reactivity to negative interpersonal events also predicted more intense SI (B = .36; SE = .05; p < .001). Specifically, individuals had more intense suicidal thoughts on days when they had higher affective reactivity to negative interpersonal events compared to their usual amount. Individual fluctuations in affective reactivity to positive interpersonal events did not predict SI intensity (B = −.05; SE = .05; p = .38).
Table 4.
Affective reactivity to interpersonal events predicting same‐day suicidal ideation
| Predictors | Suicidal ideation | Suicidal ideation | ||||
|---|---|---|---|---|---|---|
| Estimate | SE | p | Estimate | SE | p | |
| (Intercept) | −.62 | .63 | <.001 | −1.54 | .65 | .02 |
| Age | −.24 | .15 | .13 | −.37 | .13 | <.01 |
| Gender | −1.28 | .72 | .08 | −.66 | .73 | .36 |
| Prior‐day depression | .01 | <.01 | <.01 | .01 | <.01 | <.01 |
| Study Day | −.02 | <.01 | <.001 | .02 | <.01 | <.001 |
| Negative affective reactivity | ||||||
| Between‐person average | .03 | .03 | .27 | |||
| Within‐person fluctuations | .03 | <.01 | <.001 | |||
| Positive affective reactivity | ||||||
| Between‐person average | −.04 | .03 | .14 | |||
| Within‐person fluctuations | −.02 | <.01 | <.001 | |||
| Random effects | ||||||
| Residual (σ2) | 3.29 | 3.29 | ||||
| Intercept (τ00) | 4.21 | 4.39 | ||||
Continuous between‐person (level 2) predictors were centered. Age and gender are between‐person (level 2) covariates. Prior‐depression reflects depressed mood the prior day (lagged). Both prior‐day depression and study day are within‐person (level 1) covariates. Within‐person fluctuations reflect person‐centered fluctuations from individual means. Unstandardized regression estimates are included.
The bold values indicate statistically significance (p <.05).
Testing the integrated model: Multilevel indirect pathways of sleep, affective reactivity, and suicidal ideation
Multilevel mediational analyses tested the indirect effects for significant within‐person analyses of: (a) within‐person fluctuations in sleep duration to SI occurrence and intensity via affective reactivity to negative interpersonal events, and (b) within‐person fluctuations in sleep timing and sleep quality to SI occurrence via affective reactivity to positive interpersonal events. There were no direct effects of within‐person fluctuations for sleep duration (B = .02, SE = .05, p = .65) or sleep quality (B = −.01, SE < .01, p = .14) on next‐day occurrence of SI. Earlier sleep timing compared to a person's mean predicted a greater likelihood of next‐day ideation (B = −.09, SE = .05, p = .04). Figure 2 presents all significant direct and indirect pathways in the multilevel mediation analyses.
Figure 2.
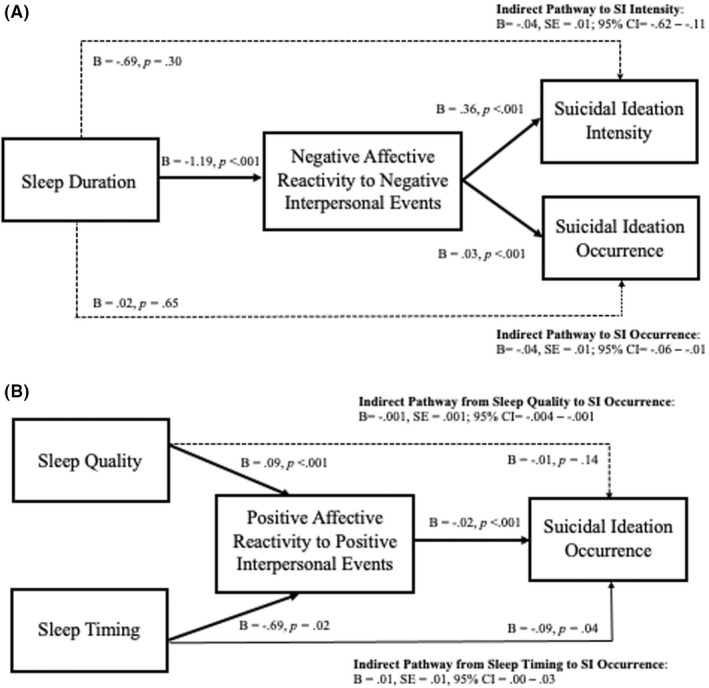
Indirect pathways linking sleep, affective reactivity, and suicidal ideation. All multilevel mediation of indirect pathways were conducted with within‐person variables, with sleep and affective reactivity reflecting within‐person fluctuations compared to each person's own mean. Solid lines reflect significant paths and dashed lines reflect non‐significant paths. Sleep duration and sleep timing reflect actigraphy‐derived measures, whereas sleep quality was self‐reported on the daily surveys in the morning
Consistent with hypotheses, within‐person fluctuations of sleep domains indirectly predicted SI via affective reactivity to interpersonal stress. Affective reactivity to negative interpersonal events was an indirect pathway between within‐person decreases in sleep duration and the occurrence of SI (B = −.04, SE = .01; 95% CI = −.06 to −.01) and SI intensity (B = −.04, SE = .01; 95% CI = −.62 to −.11). There also was a significant indirect effect between within‐person decreases in sleep quality and next‐day occurrence of SI via reduced affective reactivity to positive interpersonal events (B = −.001, SE = .001; 95% CI = −.004 to −.001). There was no significant indirect effect of sleep timing on SI through positive affective reactivity (B = .01, SE = .01, 95% CI = .00–.03). In short, there was an indirect effect through which individual decreases in sleep duration predicted next‐day heightened affective reactivity to negative interpersonal events, which, in turn was associated with the occurrence of same‐day SI and intensity. Similarly, reduced sleep quality compared to an individuals' mean predicted lower next‐day affective reactivity to positive interpersonal events, which, in turn, was associated with a greater likelihood of same‐day SI.
Discussion
This study used an intensive monitoring design to examine daily affective reactivity to positive and negative interpersonal events as a proximal mechanism through which sleep influences the presence and intensity of daily SI among adolescents and young adults at high‐risk for suicide. Consistent with hypotheses, results suggest that individual nights of shorter‐than‐usual or poorer‐than‐usual sleep quality have an indirect effect on next‐day SI through their impact on affective reactivity to interpersonal events. Specifically, shorter‐than‐usual sleep duration significantly predicted next‐day affective reactivity to negative interpersonal events, which, in turn, was associated with SI occurrence and intensity. Significant indirect effects also indicated that poorer‐than‐usual sleep quality predicted next‐day SI through blunted affective reactivity to positive interpersonal events. Overall, findings point to several proximal and modifiable targets for intervention aimed at reducing the occurrence and intensity of SI among adolescents and young adults at high‐risk for suicide: sleep and affective reactivity to negative and positive interpersonal events.
This is the first study to investigate the mechanistic pathway through which sleep may contribute to SI through affective reactivity to interpersonal events on a daily basis and using an intensive monitoring design involving both subjective and objective measures. In general, young people in our sample experienced considerable daily fluctuations in SI, sleep domains, and affective reactivity to both positive and negative interpersonal events, highlighting the importance of evaluating these proximal processes within‐person and over shorter time intervals. Adolescents and young adults in the IOP treatment endorsed SI on 22% of days per person across the day (0–43%), which is comparable to other daily studies conducted for one month following discharge from a psychiatric hospital in adolescent samples (Czyz et al., 2019). Surprisingly, there was no direct effect of actigraphic sleep duration on next‐day SI, and sleep timing was in the opposite direction as hypothesized, which is consistent with the only other study evaluating daily sleep and SI among adolescents (Glenn, Kleiman, Kearns, et al., 2021). However, findings do suggest that sleep may indirectly influence next‐day SI through heightened affective reactivity to negative interpersonal events and blunted affective reactivity to positive interpersonal events.
Building on prior research (King & Merchant, 2008; Palmer, Oosterhoff, Bower, Kaplow, & Alfano, 2018), shorter sleep duration and poorer sleep quality impair critical processes involved in affective functioning (Palmer et al., 2018), including emotional, cognitive, and social processes that affect how youth process and respond to interpersonal events in their daily lives (Ben Simon, Vallat, Barnes, & Walker, 2020). Critically, sleep disruption has been demonstrated to lead to more impulsive behaviors and impaired decision‐making (Weaver, Barger, Malone, Anderson, & Klerman, 2018), which may have dire implications when youth experience negative interpersonal events or stressors and suicidal thoughts. While within‐person changes of sleep quality did not impact next‐day negative affective reactivity, better sleep quality across the study period (mean overall levels) was associated with higher reactivity to both negative and positive events. While unexpected, better overall sleep might improve the flexibility and variability of youth's emotional responses in both affective directions, which is generally considered to be adaptive (Kashdan & Rottenberg, 2010). In general, our study contributes to a better understanding of how multiple dimensions of sleep might differentially influence affective functioning. Experiencing later sleep times than usual and worse sleep quality may have greater impact on reward responsiveness and thus regulation of positive emotions by potentially dampening positive emotional responses, which subsequently heightens SI. In contrast, not getting enough sleep compared to one's usual amount may impact individual's ability to regulate and respond to negative interpersonal events and heightened levels of emotional distress, which contributes to SI. Thus, our study points to the importance of differentiating negative and positive affective reactivity as potential mechanisms linking sleep and proximal risk for SI and as targets for suicide prevention. For instance, targeting emotion regulation and interpersonal effectiveness skills, including both managing negative emotional responses and reducing deficits in positive affective experiences (Craske, Meuret, Ritz, Treanor, & Dour, 2016), may be particularly effective in acute suicide prevention (McCauley et al., 2018).
Importantly, findings suggest unidirectional relationships of sleep to next‐day affective reactivity, but not affective reactivity to next‐day sleep. In this study, sleep predicted next‐day negative affective reactivity, but negative affective reactivity did not predict sleep the following night. Only positive affective reactivity predicted better sleep quality that night. Other studies, however, have reported that stress and heightened psychophysiological arousal impact subsequent sleep (Kalmbach et al., 2018; Lo Martire, Caruso, Palagini, Zoccoli, & Bastianini, 2020; ), and future research should explore affective and stress reactivity using more comprehensive and multimodal approaches. Regardless, findings point to the importance of targeting sleep as a means of improving affective reactivity, which may be a proximal risk factor associated with SI.
This study is among the first to utilize an intensive longitudinal design with daily objective and subjective sleep measures. Our study also used an idiographic approach to disentangle the effects of sleep and affective reactivity within person (i.e. fluctuations from an individual's mean) and between people (i.e. higher or lower levels compared to others), which provides a more nuanced examination of these daily relationships. Despite our study's innovative conceptual and methodological approaches, several limitations can inform future research. Because affective reactivity and suicidal ideation were assessed simultaneously on a daily level, claims of temporal causality that can be made about these associations are limited. These items were assessed daily at the same time (just prior to bedtime), which means that experiences of SI may have preceded those of affective reactivity, or SI itself could have elicited certain negative interpersonal events, consistent with the stress generation framework (Liu & Spirito, 2019). The duration of our ambulatory assessment period (i.e. up to 3 months) limited the total number of questions that could be asked on a daily basis. Thus, the content or context of interpersonal events and full range of affective responses following interpersonal events were not captured. This may influence heterogeneity between participants in how negative and positive interpersonal events were defined. Though common in intensive monitoring studies (Myin‐Germeys & Kuppens, 2022), daily items were revised, adapted, and constructed for the current study to adhere to text limitations in our survey software, as well as to reduce participant burden of completing lengthy daily surveys for a period of up to three months. To increase transparency and inform future studies, we have provided a supplement detailing these items and item construction. Though research assistants provided training on the daily surveys (including review of item comprehension), researchers are encouraged to actively contribute to and utilize the Experience Sampling Method item bank being developed to ensure item reliability and consistency of constructs across studies (See Appendix S2 for more information). Research building on these findings should also empirically test whether targeting sleep in treatment improves both affective reactivity and SI, as well as whether medication, substance use, or other contextual factors affect the relationships between sleep, SI, and treatment response.
Although reflective of the demographics of adolescents and young adults at high‐risk for suicide in the geographic area, the results might not generalize to more diverse samples due to disparities in access to mental health care. Future studies should include representative samples of youth and across levels of care. Studies should be designed specifically around understanding the sleep–suicide risk association and associated interventions to reduce risk in individuals who identify as racial/ethnic and gender/sexual minorities. The high and increasing rates of suicide in Black youth (Goldstein, Jonassaint, Williamson, & Franzen, 2021; Ramchand, Gordon, & Pearson, 2021) and greater sleep problems (Levenson, Thoma, Hamilton, Choukas‐Bradley, & Salk, 2021; Pollitt & Mallory, 2021) and suicidality among sexual and gender minority youth (Liu, Walsh, Sheehan, Cheek, & Carter, 2020) make this a high‐priority research area. As one of the first studies to evaluate these daily and within‐person associations in a high‐risk sample of youth using subjective and actigraphic methods, our findings also should be replicated in larger samples and among young people with and without depression or suicidal behavior to better understand how, when, and for whom sleep and affective reactivity may be associated with increased proximal risk for SI and behaviors. Although our sample contains over 3,000 days of data collection and is comparable in its sample size to other studies that used intensive monitoring designs, including clinical samples (Brüdern et al., 2022; Czyz et al., 2019; Glenn, Kleiman, Kearns, et al., 2021; Kleiman et al., 2017; Littlewood et al., 2019), the nature of our sample and its relatively small size limit generalizability and the meaningful nature of effects to our samples. Of note, effect sizes for results are not provided in the current study given ongoing debate about the interpretation and meaning of effects at the within‐ and between‐person levels, and caution is advised when interpreting these effects. Further, because all participants were in a current depressive episode, this may have also influenced their sleep, affective reactivity, and SI. Thus, it is unclear whether the observed relationships are specific to a high‐risk group or will also generalize to individuals without depression. Future research should evaluate these relationships using intensive monitoring designs across different samples to compare between and within‐group effects, evaluate developmental differences in these relationships, and examine whether sleep and affective reactivity contribute to the onset of SI or suicidal behaviors among young people in community‐based and other clinical populations.
Overall, findings highlight the importance of examining potential mechanisms through which sleep may impact SI. Results point to multiple areas of intervention, including improving sleep and affective regulation within interpersonal relationships. Given that sleep disruption is common among youth at high risk for suicide (Goldstein & Franzen, 2022), targeting skills in treatment that help adolescents and young adults modulate affective responses may be critical in decreasing SI risk, particularly in emotionally salient interpersonal contexts. Further, improving sleep and circadian rhythms via cognitive behavioral interventions may reduce the potential effects of affective reactivity to interpersonal events. For example, the Transdiagnostic sleep and Circadian intervention is an evidence‐based, modularized treatment that targets a range of sleep and circadian difficulties (Dong, Dolsen, Martinez, Notsu, & Harvey, 2020). Interpersonal and Social Rhythm Therapy (Frank, Swartz, & Boland, 2007) also focuses on improving sleep and wake regularity to enhance affective stability. Addressing sleep difficulties in the context of other evidence‐based treatments for youth suicide risk may further enhance their effectiveness. In conclusion, our findings indicate that several dimensions of sleep health and affective reactivity may constitute important, novel, and more precise targets for suicide prevention in adolescents and young adults.
Supporting information
Table S1. Affective reactivity to interpersonal events predicting sleep outcomes.
Appendix S1. Suicide safety protocol.
Appendix S2. EMA item selection and construction.
Acknowledgements
This research was supported by grants awarded by the American Foundation for Suicide Prevention (T.R.G.; P.L.F.) (SRG‐0‐056‐16) and University of Pittsburgh Clinical and Translational Science Institute (UL1 TR001857), as well as K01MH121584 (J.L.H.), L30MH117642 (J.L.H.), T32MH018269 (A.T.), T32MH018951 (C.J.R.S.), and R01 MH118312 (P.L.F.). The authors are grateful to the Services for Teens at Risk (STAR) clinic staff, participants, and their families in helping to conduct this study, which is supported in part by an appropriation from the Commonwealth of Pennsylvania. The authors have declared that they have no competing or potential conflicts of interest.
Key points.
Suicide is the second leading cause of death for individuals aged 15–24 years.
Sleep disturbances and interpersonal stress are risk factors for suicidal ideation.
This is the first longitudinal, prospective study to test the daily interrelations between sleep duration and timing (assessed objectively via actigraphy), sleep quality, affective reactivity, and suicidal ideation in a high‐risk sample of young people.
Affective reactivity to interpersonal events is identified as a proximal mechanism linking daily sleep and suicidal ideation.
Sleep and affective reactivity are modifiable risk factors, and thus may be key targets for suicide prevention programs and treatment of high‐risk adolescents and young adults.
Conflict of interest statement: No conflicts declared.
Note
Post‐hoc power analyses for assessing SI intensity (which had fewer observations) indicated that we have 80% power to detect large effects.
Contributor Information
Jessica L. Hamilton, Email: jessica.hamilton@rutgers.edu.
Peter L. Franzen, Email: franpl@upmc.edu.
References
- Aguiar, M.R. , & Sala, O.E. (1998). Interactions among grasses, shrubs, and herbivores in Patagonian grass‐shrub steppes. Ecologia Austral, 8, 201–210. [Google Scholar]
- Ahn, C. , Heo, M. , & Zhang, S. (2015). Sample size calculations for clustered and longitudinal outcomes in clinical research. New York: CRC Press. [Google Scholar]
- Ben Simon, E. , Vallat, R. , Barnes, C.M. , & Walker, M.P. (2020). Sleep loss and the socio‐emotional brain. Trends in Cognitive Sciences, 24, 435–450. [DOI] [PubMed] [Google Scholar]
- Brüdern, J. , Hallensleben, N. , Höller, I. , Spangenberg, L. , Forkmann, T. , Rath, D. , … & Glaesmer, H. (2022). Sleep disturbances predict active suicidal ideation the next day: An ecological momentary assessment study. BMC Psychiatry, 22, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan, C.J. (2019). A preliminary validation study of two ultra‐brief measures of suicide risk: The suicide and perceived burdensomeness visual analog scales. Suicide & Life‐Threatening Behavior, 49, 343–352. [DOI] [PubMed] [Google Scholar]
- Cole, R.J. , Kripke, D.F. , Gruen, W. , Mullaney, D.J. , & Gillin, J.C. (1992). Automatic sleep/wake identification from wrist activity. Sleep, 15, 461–469. [DOI] [PubMed] [Google Scholar]
- Connor, R.C.O. , & Nock, M.K. (2014). The psychology of suicidal behaviour. The Lancet Psychiatry, 366, 1–13. [DOI] [PubMed] [Google Scholar]
- Craske, M.G. , Meuret, A.E. , Ritz, T. , Treanor, M. , & Dour, H.J. (2016). Treatment for anhedonia: A neuroscience driven approach. Depression and Anxiety, 33, 927–938. [DOI] [PubMed] [Google Scholar]
- Czyz, E.K. , King, C.A. , & Nahum‐Shani, I. (2018). Ecological assessment of daily suicidal thoughts and attempts among suicidal teens after psychiatric hospitalization: Lessons about feasibility and acceptability. Psychiatry Research, 267, 566–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czyz, E.K. , Horwitz, A.G. , Arango, A. , & King, C.A. (2019). Short‐term change and prediction of suicidal ideation among adolescents: A daily diary study following psychiatric hospitalization. Journal of Child Psychology and Psychiatry, 60, 732–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong, L. , Dolsen, M.R. , Martinez, A.J. , Notsu, H. , & Harvey, A.G. (2020). A transdiagnostic sleep and circadian intervention for adolescents: Six‐month follow‐up of a randomized controlled trial. Journal of Child Psychology and Psychiatry, 61, 653–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducasse, D. , Loas, G. , Dassa, D. , Gramaglia, C. , Zeppegno, P. , Guillaume, S. , … & Courtet, P. (2018). Anhedonia is associated with suicidal ideation independently of depression: A meta‐analysis. Depression and Anxiety, 35, 382–392. [DOI] [PubMed] [Google Scholar]
- Frank, E. , Swartz, H.A. , & Boland, E. (2007). Interpersonal and social rhythm therapy: An intervention addressing rhythm dysregulation in bipolar disorder. Dialogues in Clinical Neuroscience, 9, 325–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin, J.C. , Ribeiro, J.D. , Fox, K.R. , Bentley, K.H. , Kleiman, E.M. , Huang, X. , … & Nock, M.K. (2017). Risk factors for suicidal thoughts and behaviors: A meta‐analysis of 50 years of research. Psychological Bulletin, 143, 187–232. [DOI] [PubMed] [Google Scholar]
- Glenn, C.R. , Kleiman, E.M. , Kandlur, R. , Esposito, E.C. , & Liu, R.T. (2021). Thwarted belongingness mediates interpersonal stress and suicidal thoughts: An intensive longitudinal study with high‐risk adolescents. Journal of clinical child and adolescent psychology: The official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 51, 295–311. 10.1080/15374416.2021.1969654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn, C.R. , Kleiman, E.M. , Kearns, J.C. , Boatman, A.E. , Conwell, Y. , Alpert‐Gillis, L.J. , & Pigeon, W. (2021). Sleep problems predict next‐day suicidal thinking among adolescents: A multimodal real‐time monitoring study following discharge from acute psychiatric care. Development and Psychopathology, 33, 1701–1721. [Google Scholar]
- Glenn, C.R. , Kleiman, E.M. , Kearns, J.C. , Santee, A.C. , Esposito, E.C. , Conwell, Y. , & Alpert‐Gillis, L.J. (2022). Feasibility and acceptability of ecological momentary assessment with high‐risk suicidal adolescents following acute psychiatric care. Journal of Clinical Child & Adolescent Psychology, 51, 32–48. [DOI] [PubMed] [Google Scholar]
- Glenn, C.R. , & Nock, M.K. (2014). Improving the short‐term prediction of suicidal behavior. American Journal of Preventive Medicine, 47, S176–S180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein, T.R. , & Franzen, P.L. (2022). A comprehensive review of the literature on sleep difficulties and suicidality in youth to inform an integrative developmental model and future directions. Current Sleep Medicine Reports, 8, 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein, T.R. , Jonassaint, C.R. , Williamson, A.A. , & Franzen, P.L. (2021). Sleep health disparities: A promising target for preventing suicide in black youth? Journal of Psychiatry and Brain Science, 6, e210021. [Google Scholar]
- Hall, M. , Scherner, P.V. , Kreidel, Y. , & Rubel, J.A. (2021). A systematic review of momentary assessment designs for mood and anxiety symptoms. Frontiers in Psychology, 12, 642044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, L.M. , Huang, X. , Linthicum, K.P. , Bryen, C.P. , & Ribeiro, J.D. (2020). Sleep disturbances as risk factors for suicidal thoughts and behaviours: A meta analysis of longitudinal studies. Scientific Reports, 10, 13888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, A.F. , & Preacher, K.J. (2010). Quantifying and testing indirect effects in simple mediation models when the constituent paths are nonlinear. Multivariate Behavioral Research, 45, 627–660. [DOI] [PubMed] [Google Scholar]
- Herres, J. , Ewing, E.S.K. , & Kobak, R. (2016). Emotional reactivity to negative adult and peer events and the maintenance of adolescent depressive symptoms: A daily diary design. Journal of Abnormal Child Psychology, 44, 471–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm, S.M. , Forbes, E.E. , Ryan, N.D. , Phillips, M.L. , Tarr, J.A. , & Dahl, R.E. (2009). Reward‐related brain function and sleep in pre/early pubertal and mid/late pubertal adolescents. The Journal of Adolescent Health, 45, 326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobes, D.A. , & Joiner, T.E. (2019). Reflections on suicidal ideation. Crisis, 40, 227–230. [DOI] [PubMed] [Google Scholar]
- Kalmbach, D.A. , Cuamatzi‐Castelan, A.S. , Tonnu, C.V. , Tran, K.M. , Anderson, J.R. , Roth, T. , & Drake, C.L. (2018). Hyperarousal and sleep reactivity in insomnia: Current insights. Nature and Science of Sleep, 10, 193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan, T.B. , & Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30, 865–878. 10.1016/j.cpr.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller, M.B. , Lavori, P.W. , Friedman, B. , Nielsen, E. , Endicott, J. , McDonald‐Scott, P. , & Andreasen, N.C. (1987). The longitudinal interval follow‐up evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry, 44, 540–548. [DOI] [PubMed] [Google Scholar]
- King, C.A. , & Merchant, C.R. (2008). Social and interpersonal factors relating to adolescent suicidality: A review of the literature. Archives of Suicide Research, 12, 181–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman, E.M. (2020). Suicidal thinking as a valuable clinical endpoint. EClinicalMedicine, 23, 100399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman, E.M. , Turner, B.J. , Fedor, S. , Beale, E.E. , Huffman, J.C. , & Nock, M.K. (2017). Examination of real‐time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126, 726–738. [DOI] [PubMed] [Google Scholar]
- Konjarski, M. , Murray, G. , Lee, V.V. , & Jackson, M.L. (2018). Reciprocal relationships between daily sleep and mood: A systematic review of naturalistic prospective studies. Sleep Medicine Reviews, 42, 47–58. [DOI] [PubMed] [Google Scholar]
- Levenson, J.C. , Thoma, B.C. , Hamilton, J.L. , Choukas‐Bradley, S. , & Salk, R.H. (2021). Sleep among gender minority adolescents. Sleep, 44, zsaa185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlewood, D.L. , Kyle, S.D. , Carter, L.A. , Peters, S. , Pratt, D. , & Gooding, P. (2019). Short sleep duration and poor sleep quality predict next‐day suicidal ideation: An ecological momentary assessment study. Psychological Medicine, 49, 403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, R.T. , & Spirito, A. (2019). Suicidal behavior and stress generation in adolescents. Clinical Psychological Science, 7, 488–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, R.T. , Steele, S.J. , Hamilton, J.L. , Do, Q.B.P. , Furbish, K. , Burke, T.A. , … & Gerlus, N. (2020). Sleep and suicide: A systematic review and meta‐analysis of longitudinal studies. Clinical Psychology Review, 81, 101895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, R.T. , Walsh, R.F.L. , Sheehan, A.E. , Cheek, S.M. , & Carter, S.M. (2020). Suicidal ideation and behavior among sexual minority and heterosexual youth: 1995–2017. Pediatrics, 145, e20192221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Martire, V. , Caruso, D. , Palagini, L. , Zoccoli, G. , & Bastianini, S. (2020). Stress & sleep: A relationship lasting a lifetime. Neuroscience and biobehavioral reviews, 117, 65–77. 10.1016/j.neubiorev.2019.08.024 [DOI] [PubMed] [Google Scholar]
- McCauley, E. , Berk, M.S. , Asarnow, J.R. , Adrian, M. , Cohen, J. , Korslund, K. , … & Linehan, M.M. (2018). Efficacy of dialectical behavior therapy for adolescents at high risk for suicide: A randomized clinical trial. JAMA Psychiatry, 75, 777–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMakin, D.L. , Dahl, R.E. , Buysse, D.J. , Cousins, J.C. , Forbes, E.E. , Silk, J.S. , … & Franzen, P.L. (2016). The impact of experimental sleep restriction on affective functioning in social and nonsocial contexts among adolescents. Journal of Child Psychology and Psychiatry, 57, 1027–1037. [DOI] [PubMed] [Google Scholar]
- Meltzer, L.J. , Montgomery‐Downs, H.E. , Insana, S.P. , & Walsh, C.M. (2012). Use of actigraphy for assessment in pediatric sleep research. Sleep Medicine Reviews, 16, 463–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer, L.J. , Walsh, C.M. , Traylor, J. , & Westin, A.M.L. (2012). Direct comparison of two new actigraphs and polysomnography in children and adolescents. Sleep, 35, 159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millner, A.J. , Lee, M.D. , Hoyt, K. , Buckholtz, J.W. , Auerbach, R.P. , & Nock, M.K. (2018). Are suicide attempters more impulsive than suicide ideators? General Hospital Psychiatry, 63, 103–110. [DOI] [PubMed] [Google Scholar]
- Monk, T.H. , Reynolds, C.F. , Kupfer, D.J. , Buysse, D.J. , Coble, P.A. , Hayes, A.J. , … & Ritenour, A.M. (1994). The Pittsburgh sleep diary. Journal of Sleep Research, 3, 111–120. [PubMed] [Google Scholar]
- Muthén, L.K. , & Muthén, B.O. (1998. –2017). Mplus user's guide (8th edn). Los Angeles: Muthén & Muthén. [Google Scholar]
- Myin‐Germeys, I. , & Kuppens, P. (Eds.). (2022). The open handbook of experience sampling methodology: A step‐by‐step guide to designing, conducting, and analyzing ESM studies (2nd edn). Leuven, Belgium: Center for Research on Experience Sampling and Ambulatory Methods Leuven. [Google Scholar]
- Nock, M.K. , Kleiman, E.M. , Abraham, M. , Bentley, K.H. , Brent, D.A. , Buonopane, R.J. , … & Pearson, J.L. (2021). Consensus statement on Ethical & Safety Practices for conducting digital monitoring studies with people at risk of suicide and related behaviors. Psychiatric Research and Clinical Practice, 3, 57–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivier, J. , May, W.L. , & Bell, M.L. (2017). Relative effect sizes for measures of risk. Communications in Statistics—Theory and Methods, 46, 6774–6781. [Google Scholar]
- Palmer, C.A. , & Alfano, C.A. (2017). Sleep and emotion regulation: An organizing, integrative review. Sleep Medicine Reviews, 31, 6–16. [DOI] [PubMed] [Google Scholar]
- Palmer, C.A. , Oosterhoff, B. , Bower, J.L. , Kaplow, J.B. , & Alfano, C.A. (2018). Associations among adolescent sleep problems, emotion regulation, and affective disorders: Findings from a nationally representative sample. Journal of Psychiatric Research, 96, 1–8. [DOI] [PubMed] [Google Scholar]
- PASS . (2020). Power analysis and sample size software (2020). NCSS, LLC: Kaysville, UT. ncss.com/software/pass [Google Scholar]
- Pollitt, A.M. , & Mallory, A.B. (2021). Mental and sexual health disparities among bisexual and unsure Latino/a and black sexual minority youth. LGBT Health, 8, 254–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner, K. , Brown, G.K. , Stanley, B. , Brent, D.A. , Yershova, K.V. , Oquendo, M.A. , … & Mann, J.J. (2011). The Columbia‐Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. The American Journal of Psychiatry, 168, 1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher, K.J. , Zyphur, M.J. , & Zhang, Z. (2010). A general multilevel SEM framework for assessing multilevel mediation. Psychological Methods, 15, 209–233. [DOI] [PubMed] [Google Scholar]
- Quante, M. , Kaplan, E.R. , Cailler, M. , Rueschman, M. , Wang, R. , Weng, J. , … & Redline, S. (2018). Actigraphy‐based sleep estimation in adolescents and adults: A comparison with polysomnography using two scoring algorithms. Nature and Science of Sleep, 10, 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . (2021). R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing. https://www.R‐project.org/ [Google Scholar]
- Ramchand, R. , Gordon, J.A. , & Pearson, J.L. (2021). Trends in suicide rates by race and ethnicity in the United States. JAMA Network Open, 4, e2111563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, M.A. , & Gajos, J.M. (2020). Annual Research Review: Ecological momentary assessment studies in child psychology and psychiatry. Journal of Child Psychology and Psychiatry, 61, 376–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schriber, R.A. , & Guyer, A.E. (2016). Adolescent neurobiological susceptibility to social context. Developmental Cognitive Neuroscience, 19, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin, N.L. , Wen, J.H. , Klaiber, P. , Buxton, O.M. , & Almeida, D.M. (2020). Sleep duration and affective reactivity to stressors and positive events in daily life. Health Psychology, 39, 1078–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart, J.G. , Shields, G.S. , Esposito, E.C. , Cosby, E.A. , Allen, N.B. , Slavich, G.M. , & Auerbach, R.P. (2019). Life stress and suicide in adolescents. Journal of Abnormal Child Psychology, 47, 1707–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver, M.D. , Barger, L.K. , Malone, S.K. , Anderson, L.S. , & Klerman, E.B. (2018). Dose‐dependent associations between sleep duration and unsafe behaviors among US high school students. JAMA Pediatrics, 172, 1187–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WISQARS (Web‐based Injury Statistics Query and Reporting System)|Injury Center|CDC . (2020). Retrieved June 28, 2021, from https://www.cdc.gov/injury/wisqars/index.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Affective reactivity to interpersonal events predicting sleep outcomes.
Appendix S1. Suicide safety protocol.
Appendix S2. EMA item selection and construction.


