Abstract
Hypertension is a major contributor to cardiovascular disease and daily deep breathing exercise (DBE) is a promising intervention to reduce blood pressure and stress in adults. DBE is simple, time-efficient, and does not require specialized equipment, allowing participation in a wide variety of settings. The workplace is an ideal setting to implement DBE at the national level for several reasons, including a large proportion of waking hours spent in the workplace, high levels of sedentary time at work, prevalence of work-related stress, and regular breaks throughout the day potentially reducing worker error. While the degree of adherence to daily workplace DBE will be the responsibility of the individual, employers and managers can (and should) do much to remove barriers to participation. Specifically, this could include: implementing regular short breaks or classes to perform DBE throughout the day, covering subscription costs for smartphone applications that guide DBE, and creating incentive programs for continuing DBE participation. Implementing DBE in the workplace is a pragmatic approach to provide a low-cost blood pressure and stress reduction therapy to a substantial portion of the adult population in the US, at least 50% of whom have high blood pressure.
Keywords: hypertension, diaphragmatic breathing, stress, workplace, blood pressure
Introduction
Daily deep breathing exercise (DBE) can lower resting blood pressure (BP) and reduce stress and anxiety (Russo et al., 2017; Zaccaro et al., 2018; Yau and Loke, 2021). Further, as an exercise that can be performed virtually anywhere without any equipment required, there are few barriers to DBE, relative to traditional exercise strategies. The workplace serves as a source of stress for many adults, while simultaneously resulting in long periods of sedentary time for a large portion of the US workforce in our increasingly automated society. Chronic stress and high levels of sedentary time contribute directly to the development and worsening of cardiovascular disease (CVD) (Diaz et al., 2017; Kivimäki and Steptoe, 2018), the leading cause of death throughout the world for the last two decades (World Health Organization, 2020). Further, CVD-related disability negatively impacts workplace productivity (Virtanen et al., 2017). Above-normal BP (i.e., ≥120/80 mmHg) is a primary modifiable risk factor for CVD (Stanaway et al., 2018), and adults with above-normal BP face annual healthcare costs that are approximately $2,000 higher on average than normotensive adults (Kirkland et al., 2018), making BP reduction a key therapeutic target. Regular exercise participation, along with other lifestyle changes (e.g., diet), is recommended to maintain optimal health as well as counter CVD progression and lower BP (Li et al., 2018). Unfortunately, less than half of US adults exercise regularly (NCHS. National Center for Health Statistics, 2017); a trend that will likely continue despite decades of national programs/initiatives to increase physical activity levels. As such, the workplace is an ideal location to implement daily DBE, both as an additive strategy for those who exercise regularly and as a gateway exercise for those who do not exercise regularly. Employers are partially responsible for their employee’s job satisfaction and wellbeing, and thus could provide resources and regular breaks for DBE to improve these outcomes. In this Perspective article we will provide a brief overview of the key physiological and psychological benefits of DBE. We will then discuss the impact of CVD and stress on workplace productivity, and the potential for DBE to reduce CVD risk, as well as acute and chronic stress. Finally, we will discuss real-world application potential of DBE in the workplace, as well as current research gaps and future directions. Our overall goal is to highlight the potential health and productivity benefits of DBE and call for additional investigations surrounding this promising lifestyle intervention. In-depth reviews of the underlying mechanisms leading to the changes discussed herein are outside the scope of this manuscript, but can be found elsewhere (Russo et al., 2017; Zaccaro et al., 2018; Yau and Loke, 2021).
Deep breathing exercise
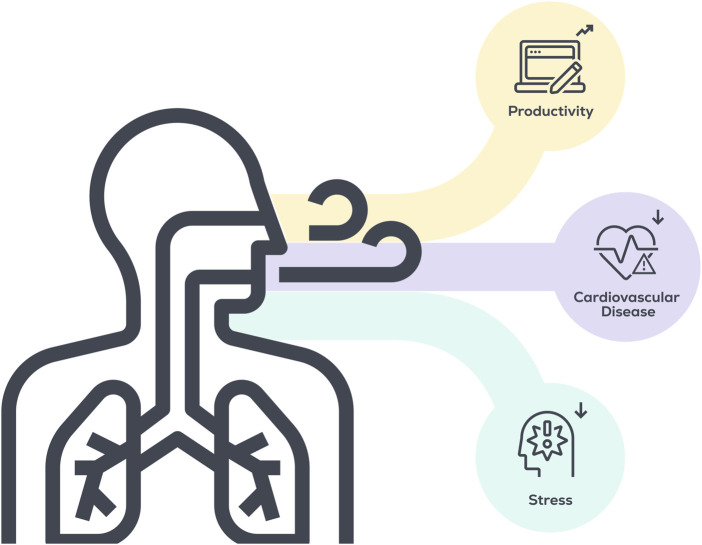
DBE is a broad term that encompasses several types of non-resisted, paced breathing strategies, including yogic breathing or Pranayama, diaphragmatic breathing, and abdominal breathing, to name a few (Bruton et al., 2011; Jayawardena et al., 2020). Along with their being differences between overall types of breathing training, there also exist significant differences in the specifics of how breathing training is employed. For example, two studies purporting to investigate “diaphragmatic breathing” may differ in the employed breathing frequency (breaths/minute), the fraction time spent inhaling and exhaling per breath, the utilization of nose or mouth breathing, the amount of time spent per day performing DBE, or the time of day that the intervention is performed, along with many other variables (Bruton et al., 2011). Given the number of variables at play, it is not surprising that current studies investigating breathing interventions have employed a wide degree of study designs, making it challenging to fully understand the potential health benefits of breathing training at the current moment. However, the preponderance of evidence does suggest DBE can improve certain important aspects of human health, including reduced BP and psychological stress (Zaccaro et al., 2018; Chaddha et al., 2019) (Figure 1), which may indirectly increase productivity through less utilization of sick time. Further, common barriers to traditional exercise strategies in non-exercising adults (e.g., lack of energy, poor health/physical disabilities, equipment/facilities access, work commitments/lack of time, cost, fear of pain/discomfort, bad weather, lack of knowledge, and low motivation (Booth, Bauman, Owen, Gore, 1997; Zunft et al., 1999; Baillot et al., 2021; Gee et al., 2012)) are minimized by DBE, and providing time and/or space for DBE in the workplace will help to overcome many of the remaining barriers. However, lack of knowledge and low motivation are two interconnected hurdles that must be addressed prior to widespread participation. Potential solutions to these barriers will be discussed in later sections.
FIGURE 1.
Potential benefits of implementing DBE in the workplace.
Physiological effects of deep breathing exercise
Clinical efficacy studies (i.e., those performed in tightly controlled laboratory conditions) suggest breathing training can lower BP. Two meta-analyses encompassing 22 randomized controlled trials (median intervention duration 8 weeks) and 1,344 participants with CVD and/or above-normal BP reported a 6 mmHg reduction in systolic BP and a 3–6 mmHg reduction in diastolic BP, on average (Zou et al., 2017; Chaddha et al., 2019). Importantly, these reductions are similar to those seen in response to other non-pharmacological lifestyle interventions (e.g., DASH diet, sodium restriction, caloric restriction, aerobic exercise, meditation (Fu et al., 2020)). Further, a large multi-center study (21,563 participants) reported that a single bout of DBE (6 breaths over 30 s) acutely reduced systolic BP 3–4 mmHg and diastolic BP 1 mmHg, relative to a time-matched rest interval (Mori et al., 2005). However, BP reduction in response to DBE is not a universal finding, as some reviews of the literature, specifically those quantifying the effects of device-guided DBE (i.e., RESPeRATE device), have found no benefit of DBE on BP compared to active control treatments (Landman et al., 2014; Freitas Gonçalves et al., 2022). Despite these reports, a preponderance of the evidence suggests that breathing interventions, primarily slow deep breathing, can lower BP, though the extent of the reduction likely varies considerably based on intervention designs. The reductions in systolic BP (i.e., 3–6 mmHg) observed following breathing training are likely to be clinically significant, as reductions of 5 mmHg achieved with pharmacotherapy are associated with a 10% lower risk for CVD (Blood Pressure Lowering Treatment Trialists’ Collaboration, 2021), while other studies suggest that even smaller reductions (i.e., 2 mmHg) can decrease risk for stroke and heart disease by 7%–10% (Lewington et al., 2002). Additional physiological adaptations to DBE include alterations in autonomic activity, increased heart rate variability, augmentation of baroreflex sensitivity, and improved ventilation efficiency (Russo et al., 2017; Zaccaro et al., 2018; Yau and Loke, 2021). There is also limited evidence that these physiological adaptations have a beneficial effect on some common health disorders, including gastrointestinal disorders, migraines, chronic obstructive pulmonary disease, and asthma (Hamasaki, 2020), and may improve sleep quality when performed prior to going to bed (Tsai et al., 2015; Laborde et al., 2019; Kuula et al., 2020), though these investigations are few and have notable limitations.
Psychological effects of deep breathing exercise
Acutely, breathing interventions appear effective for reducing feelings of anxiety or depression (Zaccaro et al., 2018; Hopper et al., 2019; Yau and Loke, 2021), and DBE is a reliable method of controlling panic attacks by countering hyperventilation, a common symptom in adults with panic disorder (Cowley and Roy-Byrne, 1987). A single bout of DBE (5–20 min) reportedly reduces subjective feelings of anxiety in generally healthy young and older adults (Yu et al., 2011; Magnon et al., 2021) and in men with alcohol dependence (Clark and Hirschman, 1990), while also reducing feelings of depression and anger-hostility in healthy adults (Yu et al., 2011). In regard to long-term benefits, evidence from clinical trials support the chronic effects of breathing interventions for improving mental health parameters as well. For example, 20 sessions of 15 min of diaphragmatic breathing over 8 weeks reduced negative affect (i.e., negative emotions and expression) and physiological markers of stress (i.e., salivary cortisol), but did not alter positive affect (i.e., positive emotions and expression) in healthy adults (Ma et al., 2017). Other 8-week randomized controlled trials in adults with anxiety (Chen et al., 2017) or major depressive disorder (Sharma et al., 2017) demonstrated the effectiveness of DBE for improving self-reported anxiety and indices of depression, respectively, though it should be noted that in adults with depression, the experimental group performed yoga poses in addition to modified breathing (Sharma et al., 2017). In a separate non-randomized trial, those encouraged to perform 10 min of deep breathing, twice per day, for 9 months demonstrated greater reductions in self-reported stress than those in the control group (Sundram et al., 2014). Chronic stress/anxiety is an independent risk factor for hypertension (Bhelkar et al., 2018) and is associated with increased sympathetic activity (Won and Kim, 2016), and it is possible that these physiological adaptations are simply a side effect of the reduced stress seen in response to DBE.
Cardiovascular disease and workplace stress
CVD has been the leading cause of death in the US for the last two decades (World Health Organization, 2020). Further, those living with CVD are likely to develop additional chronic diseases and early onset physical disability (Jin et al., 2019; Vassalle et al., 2022). CVD is prevalent in middle-age US adults, and therefore imposes substantial morbidity/mortality-related productivity costs in the workplace, including greater utilization of sick time for longer periods and time off work to recover from cardiac events (Virtanen et al., 2017). Both chronic stress and depression independently increase CVD risk (Strike and Steptoe, 2002; Kivimäki and Steptoe, 2018), and the workplace is a primary source of stress for many adults, with 85% of respondents to a 2021 survey indicating that workplace stress affects their mental health (Mental Health America, 2021), while a separate report found that 76% of working US adults reported experiencing at least one symptom of a mental health condition (i.e., burnout, depression, anxiety) due to work in the last year (Partners, 2021). One in two US adults have high BP (Whelton et al., 2018) and those adults who work ≥49 h/week have a 70% greater chance of developing hypertension (Trudel et al., 2020). Employees with chronic work stress have a 50% excess risk for coronary heart disease than those without work stress (Kivimäki et al., 2006), and acute stress events can trigger cardiac events in those with ongoing CVD, whereas chronic stress is associated with recurrent cardiac events (Steptoe and Kivimäki, 2012). As a result, a record number of adults are leaving their jobs in what is coming to be known as the “Great Resignation”, with at least half of adults who left their jobs citing mental health reasons (Partners, 2021) and ∼40% reporting feeling disrespected at work (Pew Research Center, 2022). The workplace has transformed from a strictly professional setting to a vibrant social scene where people want to connect with their coworkers and enjoy their time. If employees feel negatively about their work situation (e.g., unsupported by management, lack of growth potential, disrespect) they will find an alternative job that evokes positive feelings, or one with sufficient monetary compensation to overcome the negative aspects. It has become the responsibility of the employer to provide a working environment that is supportive for employees; a place where they want to spend a large portion of their time every day. Several private companies understand this and have invested in perks for employees, including exercise equipment on site, mental health resources, free subscriptions to mindfulness apps, and healthy food alternatives, to name a few (Glassdoor, 2019).
It is worth noting that not all individuals perceive stress in the same way and that the workplace may not necessarily be the underlying cause of stress for all people. Stress and the stress response are multifactorial processes, influenced by early life experiences, race, gender identity, socioeconomic status, and personality type, to name a few (Williams, 1999; Vollrath, 2001; LeMoult et al., 2020; Tan et al., 2020). Further, there may be workplace stressors that are too severe to be resolved with DBE (e.g., workplace harassment). With this in mind, DBE should not be seen as a replacement for established pharmacological or behavioral therapies to treat stress, anxiety, or depression. Instead, we recommend DBE be used as a stress-reduction tool to supplement any ongoing or planned mental health treatment.
Real-world application
At least two studies assessing the effectiveness of DBE in the workplace have been published to date (Alexopoulos et al., 2014; Sundram et al., 2014), neither of which reported sufficient methodological details (e.g., breathing rate) to replicate the intervention. However, what we can pull from these investigations is that lack of supervisor support and high work-load are major barriers to regular DBE participation (Sundram et al., 2014). Further, DBE can easily be paired with other relaxation activities (e.g., mindfulness, progressive muscle relaxation) as they can be performed simultaneously (Alexopoulos et al., 2014).
There is a wealth of DBE resources online and in written format. There are essentially limitless combinations of breathing factors (e.g., inhale/exhale ratios, nose or mouth breathing, exercise duration) that could be employed, yet not enough evidence to recommend one protocol over another. However, the two components of DBE that appear to be most consistent among protocols are 1) depth of breath (i.e., at least 80% of vital capacity) and 2) rate of breathing (i.e., approximately 0.1 Hz or slower, or about 6 breaths/minute or fewer). Thus, if these criteria are met, the other aspects of the protocol may become less important. Given the above, two important public health goals become 1) increasing DBE adoption on a national or international scale; and 2) promoting long-term adherence to DBE by new and current participants by removing as many barriers to DBE as possible.
As mentioned previously, there are several barriers to traditional exercise strategies that do not necessarily pertain to DBE. However, relevant barriers to DBE include lack of knowledge, low motivation, and lack of support. In fact, because of the simplicity of DBE, successful adherence strategies probably closely reflect the strategies used to increase adherence to medications, including increasing patient self-efficacy, belief in the effectiveness of the treatment, and social support (Holmes et al., 2014). Additional medication adherence strategies like having an established routine and cues as reminders (Chambers et al., 2011) (e.g., hourly smartwatch notifications) would likely be effective for DBE as well.
The workplace is an ideal venue to implement DBE at a large scale, however, there are some key considerations that employers should keep in mind. A recent qualitative analysis directed toward understanding the psychological and social influences surrounding taking breaks at work has identified some key themes that can provide insight to employers (Oliver et al., 2021). With these considerations in mind, we have created some recommendations on how to promote daily DBE at work: 1) regular DBE breaks throughout the day must become part of the culture at work and employers/manager should lead by example, 2) employers attitudes toward breaks must be perceived as positive by employees and there should not be pressure from management to work during breaks, 3) it must be clear that these short breaks are added on top of breaks already in place (e.g., lunch break) and not replacing them, 4) employees should feel that their physical and mental health is valued more than their productivity, and 5) break time should be protected (those practicing DBE should not be interrupted for work responsibilities until break time is over). While there may be concerns that frequent breaks will reduce productivity, current evidence suggests no negative effects of short, regular breaks on productivity (Waongenngarm et al., 2018), and, in fact, they can reduce perceived tiredness, stress, and job errors (Mitra et al., 2008; Taylor, 2011; Randolph, 2016).
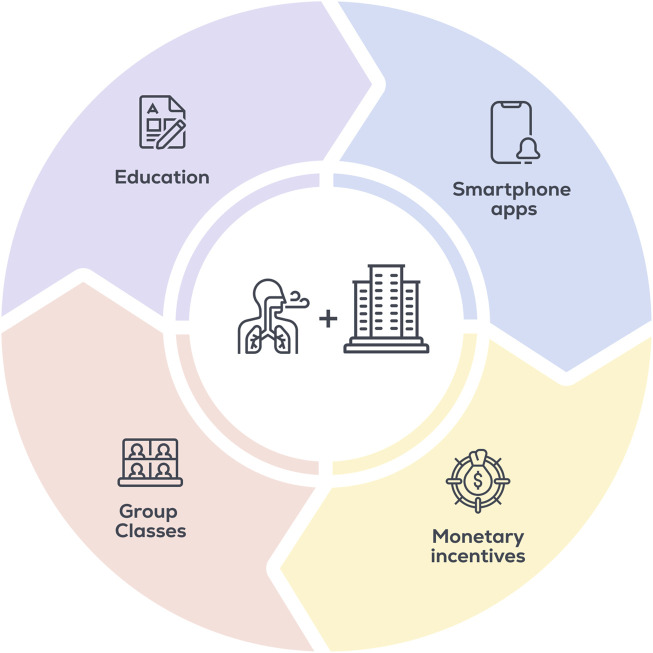
Additional solutions employers could use to overcome barriers to regular DBE include providing educational resources regarding the beneficial effects of DBE, implementing in-person deep breathing “classes” that employees can attend throughout the day, covering subscription costs for smartphone applications that guide DBE (e.g., Breathwrk, Breathe+), and/or create incentive programs for continuing DBE participation (Figure 2). Smartphone applications have been shown to increase adherence to lifestyle interventions (Carter et al., 2013), and generally contain additional features to increase engagement (e.g., tracking, leaderboards, personalization, education). Further, these applications provide multiple types of guided or self-directed breathing protocols, allowing users to choose the type of DBE they prefer and find most effective at reducing stress for themselves. As of 2021, 85% of US adults reportedly own a smartphone (Pew Research Center, 2021), making application-directed DBE accessible to the majority of adults.
FIGURE 2.
Strategies to implement DBE and increase adherence in the workplace.
Potential in other populations and future directions
While this Perspective article highlights the workplace as an ideal venue for large-scale DBE participation to impact physiological and psychological health at the national level, there are several other groups that could potentially benefit from regular DBE. High rates of acute and chronic stress/anxiety in adolescents (Merikangas et al., 2010) and young adults (Goodwin et al., 2020) highlight schools as a target for DBE participation. Similarly, individuals suffering from performance anxiety (e.g., athletes, musicians) could potentially benefit from DBE, and coaches/teachers could provide the resources suggested in this article. DBE may be particularly useful in unique clinical populations unable to perform traditional exercise strategies (e.g., individuals with orthopedic injuries, older adults with mobility limitations), as well as any population with above-normal BP (e.g., adults with obstructive sleep apnea). Indeed, there are several recently completed or ongoing clinical trials with the aim of validating DBE in distinct populations, including smokers (NCT03728530), women with pregnancy-induced hypertension (NCT04059822), adults with physical limitations (NCT05396027), post cardiac surgery patients (NCT01282671), and cancer patients undergoing radiotherapy (NCT04441827).
In addition to these disease/condition-specific investigations, larger and longer-term trials must be undertaken, ideally with adequate control groups that will help investigators to differentiate the effects of DBE from other stress-reducing therapies (e.g., mindfulness). Further, pragmatic experimental designs that take into account real-world barriers to habit forming and long-term adherence are warranted. DBE could also be compared against traditional exercise strategies or other interventions designed to decrease sedentary time. For example, whether DBE can counteract the negative effects of prolonged sitting has not been investigated to date. Recent reports indicate that just 5 min of walking, and even simply standing, every hour can counteract some of the negative effects of prolonged sitting (Benatti and Ried-Larsen, 2015; Chandrasekaran et al., 2021), and it is possible that DBE would result in similar beneficial effects. Ultimately, increased awareness and enhanced dissemination strategies will be necessary if wide-spread acceptance of DBE is to become a reality.
Conclusion
Daily DBE can result in beneficial physiological adaptations, including reduced BP and sympathetic activity, and can reduce chronic stress and mitigate acute stress events. It should be noted that the evidence behind these assertions is somewhat limited. However, the simplicity of the technique, lack of negative effects, and high benefit/cost ratio (i.e., modest-moderate benefit with minimal cost/time commitment) make DBE a potential candidate for a large-scale intervention option targeted to individuals wherein BP and/or stress and anxiety could be reduced, and the workplace is an ideal setting to implement daily DBE. In contrast to traditional exercise strategies, DBE can be performed by any population and has few barriers to participation. Further, DBE can be performed essentially anywhere, has low energetic cost, and would have no negative effects on performance or productivity. The barriers that are inherent to habit-forming (e.g., lack of motivation) and thus regular DBE participation, could be mitigated by employers by providing resources for DBE and promoting a work culture that emphasizes the physical and mental health of its employees. Smartphone applications that guide users in DBE, as well as provide educational materials on the health benefits of DBE, may help to increase acceptance and adherence.
Funding Statement
This work was supported by NIH grants K01HL153326 (DC) and 5T32HL007249-45 (DT).
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
DC developed the initial concept, and DT and DC drafted and edited the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Alexopoulos E. C., Zisi M., Manola G., Darviri C. (2014). Short-term effects of a randomized controlled worksite relaxation intervention in Greece. Annals of Agricultural and Environmental Medicine. 21 (2), 382–387. 10.5604/1232-1966.1108609 [DOI] [PubMed] [Google Scholar]
- Baillot A., Chenail S., Barros Polita N., Simoneau M., Libourel M., Nazon E., et al. (2021). “Physical activity motives, barriers, and preferences in people with obesity: A systematic review,”. PLOS ONE. Editor Kumar S., 16, 6. e0253114. 10.1371/journal.pone.0253114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benatti F. B., Ried-Larsen M. (2015). The effects of breaking up prolonged sitting time: A review of experimental studies. Medicine & Science in Sports & Exercise. 47 (10), 2053–2061. 10.1249/MSS.0000000000000654 [DOI] [PubMed] [Google Scholar]
- Bhelkar S., Deshpande S., Mankar S., Hiwarkar P. (2018). Association between stress and hypertension among adults more than 30 years: A case-control study. National Journal of Community Medicine. 9 (6), 4. [Google Scholar]
- Blood Pressure Lowering Treatment Trialists’ Collaboration (2021). Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: An individual participant-level data meta-analysis. Lancet Lond England. 397 (10285), 1625–1636. 10.1016/S0140-6736(21)00590-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth M. L., Bauman A., Owen N., Gore C. J. (1997). Physical activity preferences, preferred sources of assistance, and perceived barriers to increased activity among physically inactive Australians. Preventive Medicine. 26 (1), 131–137. 10.1006/pmed.1996.9982 [DOI] [PubMed] [Google Scholar]
- Bruton A., Garrod R., Thomas M. (2011). Respiratory physiotherapy: Towards a clearer definition of terminology. Physiotherapy 97 (4), 345–349. 10.1016/j.physio.2010.12.005 [DOI] [PubMed] [Google Scholar]
- Carter M. C., Burley V. J., Nykjaer C., Cade J. E. (2013). Adherence to a smartphone application for weight loss compared to website and paper diary: Pilot randomized controlled trial. Journal of Medical Internet Research. 15 (4), e32. 10.2196/jmir.2283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaddha A., Modaff D., Hooper-Lane C., Feldstein D. A. (2019). Device and non-device-guided slow breathing to reduce blood pressure: A systematic review and meta-analysis. Complementary Therapies in Medicine. 45, 179–184. 10.1016/j.ctim.2019.03.005 [DOI] [PubMed] [Google Scholar]
- Chambers J. A., O’Carroll R. E., Hamilton B., Whittaker J., Johnston M., Sudlow C., et al. (2011). Adherence to medication in stroke survivors: A qualitative comparison of low and high adherers. British Journal of Health Psychology. 16 (3), 592–609. 10.1348/2044-8287.002000 [DOI] [PubMed] [Google Scholar]
- Chandrasekaran B., Pesola A. J., Rao C. R., Arumugam A. (2021). Does breaking up prolonged sitting improve cognitive functions in sedentary adults? A mapping review and hypothesis formulation on the potential physiological mechanisms. BMC Musculoskeletal Disorders. 22 (1), 274. 10.1186/s12891-021-04136-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y. F., Huang X. Y., Chien C. H., Cheng J. F. (2017). The effectiveness of diaphragmatic breathing relaxation training for reducing anxiety. Perspectives in Psychiatric Care 53 (4), 329–336. 10.1111/ppc.12184 [DOI] [PubMed] [Google Scholar]
- Clark M. E., Hirschman R. (1990). Effects of paced respiration on anxiety reduction in a clinical population. Biofeedback and Self-regulation. 15 (3), 273–284. 10.1007/BF01011109 [DOI] [PubMed] [Google Scholar]
- Cowley D. S., Roy-Byrne P. P. (1987). Hyperventilation and panic disorder. The American Journal of Medicine. 83 (5), 929–937. 10.1016/0002-9343(87)90654-1 [DOI] [PubMed] [Google Scholar]
- Diaz K. M., Howard V. J., Hutto B., Colabianchi N., Vena J. E., Safford M. M., et al. (2017). Patterns of sedentary behavior and mortality in U.S. Middle-aged and older adults: A national cohort study. Annals of Internal Medicine. 167 (7), 465–475. 10.7326/M17-0212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freitas Gonçalves K. S., Queiroz Godoy Daniel A. C., Tatagiba Lamas J. L., Oliveira H. C., Cloutier L., De Campos Pereira Silveira R. C., et al. (2022). Device and nondevice‐guided slow breathing to reduce blood pressure in hypertensive patients: A systematic review and meta‐analysis. Health Science Reports. 5 (3), e636. 10.1002/hsr2.636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu J., Liu Y., Zhang L., Zhou L., Li D., Quan H., et al. (2020). Nonpharmacologic interventions for reducing blood pressure in adults with prehypertension to established hypertension. Journal of the American Heart Association. 9 (19), e016804. 10.1161/JAHA.120.016804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee M. E., Bienek A., Campbell N. R. C., Bancej C. M., Robitaille C., Kaczorowski J., et al. (2012). Prevalence of, and barriers to, preventive lifestyle behaviors in hypertension (from a national survey of Canadians with hypertension). The American Journal of Cardiology. 109 (4), 570–575. 10.1016/j.amjcard.2011.09.051 [DOI] [PubMed] [Google Scholar]
- Glassdoor (2019). 13 companies with cool wellness perks. Available at: https://www.glassdoor.com/blog/cool-wellness-perks/(Accessed June 9, 2022).
- Goodwin R. D., Weinberger A. H., Kim J. H., Wu M., Galea S. (2020). Trends in anxiety among adults in the United States, 2008–2018: Rapid increases among young adults. Journal of Psychiatric Research. 130, 441–446. 10.1016/j.jpsychires.2020.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamasaki H. (2020). Effects of diaphragmatic breathing on health: A narrative review. Medicines 7 (10), 65. 10.3390/medicines7100065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E. A. F., Hughes D. A., Morrison V. L. (2014). Predicting adherence to medications using health psychology theories: A systematic review of 20 years of empirical research. Value Health 17 (8), 863–876. 10.1016/j.jval.2014.08.2671 [DOI] [PubMed] [Google Scholar]
- Hopper S. I., Murray S. L., Ferrara L. R., Singleton J. K. (2019). Effectiveness of diaphragmatic breathing for reducing physiological and psychological stress in adults: A quantitative systematic review. JBI Database of Systematic Reviews and Implementation Reports. 17 (9), 1855–1876. 10.11124/JBISRIR-2017-003848 [DOI] [PubMed] [Google Scholar]
- Jayawardena R., Ranasinghe P., Ranawaka H., Gamage N., Dissanayake D., Misra A. (2020). Exploring the therapeutic benefits of “Pranayama” (yogic breathing): A systematic review. International Journal of Yoga. 13 (2), 99–110. 10.4103/ijoy.IJOY_37_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y., Tanaka T., Ma Y., Bandinelli S., Ferrucci L., Talegawkar S. A. (2019). Cardiovascular health is associated with disability among older community dwelling men and women. Journal of Aging and Health 31 (8), 1339–1352. 10.1177/0898264318778417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkland E. B., Heincelman M., Bishu K. G., Schumann S. O., Schreiner A., Axon R. N., et al. (2018). Trends in healthcare expenditures among us adults with hypertension: National estimates, 2003–2014. Journal of the American Heart Association. 7 (11), e008731. 10.1161/JAHA.118.008731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimäki M., Steptoe A. (2018). Effects of stress on the development and progression of cardiovascular disease. Nature Reviews Cardiology. 15 (4), 215–229. 10.1038/nrcardio.2017.189 [DOI] [PubMed] [Google Scholar]
- Kivimäki M., Virtanen M., Elovainio M., Kouvonen A., Väänänen A., Vahtera J. (2006). Work stress in the etiology of coronary heart disease: A meta-analysis. Scandinavian Journal of Work, Environment & Health 32 (6), 431–442. 10.5271/sjweh.1049 [DOI] [PubMed] [Google Scholar]
- Kuula L., Halonen R., Kajanto K., Lipsanen J., Makkonen T., Peltonen M., et al. (2020). The effects of presleep slow breathing and music listening on polysomnographic sleep measures: A pilot trial. Scientific Reports. 10 (1), 7427. 10.1038/s41598-020-64218-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laborde S., Hosang T., Mosley E., Dosseville F. (2019). Influence of a 30-day slow-paced breathing intervention compared to social media use on subjective sleep quality and cardiac vagal activity. Journal of Clinical Medicine. 8 (2), E193. 10.3390/jcm8020193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landman G. W. D., Van Hateren K. J., Van Dijk P. R., Sjj L., Houweling S. T., Groenier K. H., et al. (2014). Efficacy of device-guided breathing for hypertension in blinded, randomized, active-controlled trials: A meta-analysis of individual patient data. JAMA Internal Medicine. 174 (11), 1815–1821. 10.1001/jamainternmed.2014.4336 [DOI] [PubMed] [Google Scholar]
- LeMoult J., Humphreys K. L., Tracy A., Hoffmeister J. A., Ip E., Gotlib I. H. (2020). Meta-analysis: Exposure to early life stress and risk for depression in childhood and adolescence. Journal of the American Academy of Child and Adolescent Psychiatry 59 (7), 842–855. 10.1016/j.jaac.2019.10.011 [DOI] [PubMed] [Google Scholar]
- Lewington S., Clarke R., Qizilbash N., Peto R., Collins R., Prospective Studies Collaboration (2002). Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet Lond England. 360 (9349), 1903–1913. 10.1016/s0140-6736(02)11911-8 [DOI] [PubMed] [Google Scholar]
- Li Y., Pan A., Wang D. D., Liu X., Dhana K., Franco O. H., et al. (2018). Impact of healthy lifestyle factors on life expectancies in the US population. Circulation 138 (4), 345–355. 10.1161/CIRCULATIONAHA.117.032047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma X., Yue Z. Q., Gong Z. Q., Zhang H., Duan N. Y., Shi Y. T., et al. (2017). The effect of diaphragmatic breathing on attention, negative affect and stress in healthy adults. Frontiers in Psychology. 8, 874. 10.3389/fpsyg.2017.00874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnon V., Dutheil F., Vallet G. T. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Scientific Reports. 11 (1), 19267. 10.1038/s41598-021-98736-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mental Health America (2021). Mind the workplace report (2021). Alexandria, United States: MHA. [Google Scholar]
- Merikangas K. R., He J. P., Burstein M., Swanson S. A., Avenevoli S., Cui L., et al. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the national comorbidity survey replication–adolescent supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry 49 (10), 980–989. 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitra B., Cameron P. A., Mele G., Archer P. (2008). Rest during shift work in the emergency department. Australian Health Review 32 (2), 246–251. 10.1071/ah080246 [DOI] [PubMed] [Google Scholar]
- Mori H., Yamamoto H., Kuwashima M., Saito S., Ukai H., Hirao K., et al. (2005). How does deep breathing affect office blood pressure and pulse rate? Hypertension Research. 28 (6), 499–504. 10.1291/hypres.28.499 [DOI] [PubMed] [Google Scholar]
- Nchs. National Center for Health Statistics (2017).Report No.: 2017-1232 “Health, United States, 2016: With chartbook on long-term trends in health,”. (Hyattsville, MD. National Center for Health Statistics (NCHS). [PubMed] [Google Scholar]
- Oliver M., Rodham K., Taylor J., McIver C. (2021). Understanding the psychological and social influences on office workers taking breaks: A thematic analysis. Psychology & Health 36 (3), 351–366. 10.1080/08870446.2020.1764954 [DOI] [PubMed] [Google Scholar]
- Partners M. S. (2021). Mental health at work report (2021). San Francisco, United States: MHA. [Google Scholar]
- Pew Research Center (2021). Mobile fact sheet. Available at: https://www.pewresearch.org/internet/fact-sheet/mobile/(Accessed June 29, 2022).
- Pew Research Center (2022). Majority of workers who quit a job in 2021 cite low pay, no opportunities for advancement, feeling disrespected. Available at: https://www.pewresearch.org/fact-tank/2022/03/09/majority-of-workers-who-quit-a-job-in-2021-cite-low-pay-no-opportunities-for-advancement-feeling-disrespected/(Accessed. June 9, 2022).
- Randolph S. A. (2016). The importance of employee breaks. Workplace Health & Safety. 64 (7), 344. 10.1177/2165079916653416 [DOI] [PubMed] [Google Scholar]
- Russo M. A., Santarelli D. M., O’Rourke D. (2017). The physiological effects of slow breathing in the healthy human. Breathe 13 (4), 298–309. 10.1183/20734735.009817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A., Barrett M. S., Cucchiara A. J., Gooneratne N. S., Thase M. E. (2017). A breathing-based meditation intervention for patients with major depressive disorder following inadequate response to antidepressants: A randomized pilot study. The Journal of Clinical Psychiatry 78 (1), e59–e63. 10.4088/JCP.16m10819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanaway J. D., Afshin A., Gakidou E., Lim S. S., Abate D., Abate K. H., et al. (2018). Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 392 (10159), 1923–1994. 10.1016/S0140-6736(18)32225-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A., Kivimäki M. (2012). Stress and cardiovascular disease. Nature Reviews Cardiology. 9 (6), 360–370. 10.1038/nrcardio.2012.45 [DOI] [PubMed] [Google Scholar]
- Strike P. C., Steptoe A. (2002). Depression, stress, and the heart. Heart 88 (5), 441–443. 10.1136/heart.88.5.441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundram B. M., Dahlui M., Chinna K. (2014). Taking my breath away by keeping stress at bay”: An employee assistance program in the automotive assembly plant. Iranian Journal of Public Health 43 (3), 263–272. [PMC free article] [PubMed] [Google Scholar]
- Tan K. K. H., Treharne G. J., Ellis S. J., Schmidt J. M., Veale J. F. (2020). Gender minority stress: A critical review. Journal of Homosexuality 67 (10), 1471–1489. 10.1080/00918369.2019.1591789 [DOI] [PubMed] [Google Scholar]
- Taylor W. C. (2011). Booster Breaks: An easy-to-implement workplace policy designed to improve employee health, increase productivity, and lower health care costs. Journal of Workplace Behavioral Health 26 (1), 70–84. 10.1080/15555240.2011.540991 [DOI] [Google Scholar]
- Trudel X., Brisson C., Gilbert-Ouimet M., Vézina M., Talbot D., Milot A. (2020). Long working hours and the prevalence of masked and sustained hypertension. Hypertension 75 (2), 532–538. 10.1161/HYPERTENSIONAHA.119.12926 [DOI] [PubMed] [Google Scholar]
- Tsai H. J., Kuo T. B. J., Lee G. S., Yang C. C. H. (2015). Efficacy of paced breathing for insomnia: Enhances vagal activity and improves sleep quality. Psychophysiology 52 (3), 388–396. 10.1111/psyp.12333 [DOI] [PubMed] [Google Scholar]
- Vassalle C., Xiao J., Sabatino L. (2022). Editorial: Relationship between cardiovascular disease and other chronic conditions. Frontiers in Cardiovascular Medicine. 9, 875551. 10.3389/fcvm.2022.875551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virtanen M., Ervasti J., Mittendorfer-Rutz E., Lallukka T., Kjeldgård L., Friberg E., et al. (2017). Work disability before and after a major cardiovascular event: A ten-year study using nationwide medical and insurance registers. Scientific Reports. 7 (1), 1142. 10.1038/s41598-017-01216-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollrath M. (2001). Personality and stress. Scandinavian Journal of Psychology. 42, 335–347. 10.1111/1467-9450.00245 [DOI] [PubMed] [Google Scholar]
- Waongenngarm P., Areerak K., Janwantanakul P. (2018). The effects of breaks on low back pain, discomfort, and work productivity in office workers: A systematic review of randomized and non-randomized controlled trials. Applied Ergonomics. 68, 230–239. 10.1016/j.apergo.2017.12.003 [DOI] [PubMed] [Google Scholar]
- Whelton P. K., Carey R. M., Aronow W. S., Casey D. E., Collins K. J., Dennison Himmelfarb C., et al. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of cardiology/American heart association task force on clinical practice guidelines. Journal of the American College of Cardiology. 71 (19), e127–e248. 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
- Williams D. R. (1999). Race, socioeconomic status, and health the added effects of racism and discrimination. Annals of the New York Academy of Sciences. 896 (1), 173–188. 10.1111/j.1749-6632.1999.tb08114.x [DOI] [PubMed] [Google Scholar]
- Won E., Kim Y. K. (2016). Stress, the autonomic nervous system, and the immune-kynurenine pathway in the etiology of depression. Current Neuropharmacology. 14 (7), 665–673. 10.2174/1570159x14666151208113006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2020). WHO reveals leading causes of death and disability worldwide: 2000-2019. Accessed Available at: https://www.who.int/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000-2019 June 29, 2022).
- Yau K. K. Y., Loke A. Y. (2021). Effects of diaphragmatic deep breathing exercises on prehypertensive or hypertensive adults: A literature review. Complementary Therapies in Clinical Practice. 43, 101315. 10.1016/j.ctcp.2021.101315 [DOI] [PubMed] [Google Scholar]
- Yu X., Fumoto M., Nakatani Y., Sekiyama T., Kikuchi H., Seki Y., et al. (2011). Activation of the anterior prefrontal cortex and serotonergic system is associated with improvements in mood and EEG changes induced by Zen meditation practice in novices. International Journal of Psychophysiology. 80 (2), 103–111. 10.1016/j.ijpsycho.2011.02.004 [DOI] [PubMed] [Google Scholar]
- Zaccaro A., Piarulli A., Laurino M., Garbella E., Menicucci D., Neri B., et al. (2018). How breath-control can change your life: A systematic review on psycho-physiological correlates of slow breathing. Frontiers in Human Neuroscience. 12, 353. 10.3389/fnhum.2018.00353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou Y., Zhao X., Hou Y. Y., Liu T., Wu Q., Huang Y. H., et al. (2017). Meta-analysis of effects of voluntary slow breathing exercises for control of heart rate and blood pressure in patients with cardiovascular diseases. The American Journal of Cardiology. 120 (1), 148–153. 10.1016/j.amjcard.2017.03.247 [DOI] [PubMed] [Google Scholar]
- Zunft H. J. F., Friebe D., Seppelt B., Widhalm K., De Winter A. M. R., Vaz de Almeida M. D., et al. (1999). Perceived benefits and barriers to physical activity in a nationally representative sample in the European Union. Public Health Nutrition. 2 (1), 153–160. 10.1017/s1368980099000208 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.