This cohort study assesses differences between older Black and White patients who receive home- and community-based rehabilitation services after a traumatic brain injury.
Key Points
Question
Is race associated with differences in receipt of home- and community-based rehabilitation services after traumatic brain injury (TBI) among older adults?
Findings
In this cohort study of 19 026 Medicare beneficiaries, non-Hispanic Black (hereafter Black) beneficiaries received less outpatient rehabilitation therapy over 6 months after TBI compared with non-Hispanic White (hereafter White) beneficiaries. However, Black beneficiaries received more home health rehabilitation therapy over 6 months after TBI compared with White beneficiaries.
Meaning
Findings of this study suggest that there are relative shifts in rehabilitation use, with lower outpatient therapy use and higher home health care use among Black patients vs White patients with TBI, which may contribute to differences in recovery from TBI and long-term disability.
Abstract
Importance
Non-Hispanic Black (hereafter Black) patients with traumatic brain injury (TBI) experience worse long-term outcomes and residual disability compared with non-Hispanic White (hereafter White) patients. Receipt of appropriate rehabilitation can improve function among older adults after TBI.
Objective
To assess the association between race and receipt of home- and community-based rehabilitation among a nationally representative sample of older Medicare beneficiaries with TBI.
Design, Setting, and Participants
This cohort study analyzed a random sample of Medicare administrative claims data for community-dwelling Medicare beneficiaries aged 65 years or older who were hospitalized with a primary diagnosis of TBI and discharged alive to a nonhospice setting from 2010 through 2018. Claims data for Medicare beneficiaries of other races and ethnicities were excluded due to the small sample sizes within each category. Data were analyzed January 21 to August 30, 2022.
Exposures
Black or White race.
Main Outcomes and Measures
Monthly use rates of home-based or outpatient rehabilitation were calculated over the 6 months after discharge from the hospital. The denominator for rate calculations accounted for variation in length of hospital and rehabilitation facility stays and loss to follow-up due to death. Rates over time were modeled using generalized estimating equations, controlling for TBI acuity, demographic characteristics, comorbidities, and socioeconomic factors.
Results
Among 19 026 Medicare beneficiaries (mean [SD] age, 81.6 [8.1] years; 10 781 women [56.7%]; and 994 Black beneficiaries [5.2%] and 18 032 White beneficiaries [94.8%]), receipt of 1 or more home health rehabilitation visits did not differ by race (Black vs White, 47.4% vs 46.2%; P = .46), but Black beneficiaries were less likely to receive 1 or more outpatient rehabilitation visits compared with White beneficiaries (3.4% vs 7.1%; P < .001). In fully adjusted regression models, Black beneficiaries received less outpatient therapy over the 6 months after TBI (rate ratio, 0.60; 95% CI, 0.38-0.93). However, Black beneficiaries received more home health rehabilitation therapy over the 6 months after TBI than White beneficiaries (rate ratio, 1.15; 95% CI, 1.00-1.32).
Conclusions and Relevance
This cohort study found relative shifts in rehabilitation use, with markedly lower outpatient therapy use and modestly higher home health care use among Black patients compared with White patients with TBI. These disparities may contribute to reduced functional recovery and residual disability among racial and ethnic minority groups. Additional studies are needed to assess the association between the amount of outpatient rehabilitation care and functional recovery after TBI in socioeconomically disadvantaged populations.
Introduction
Each year in the US, traumatic brain injury (TBI) results in over 123 000 hospitalizations and 485 000 emergency department visits among adults aged 65 years and older, representing a major public health burden.1,2 Furthermore, hospitalization rates for TBI among older adults are more than double those observed in other age groups and are rapidly increasing.1,3 Compared with younger adults with similar injury severity, older adults have poor short-term and long-term outcomes after TBI, including longer length of hospital stay, increased functional limitations and disability, and higher mortality.3,4,5,6,7,8,9 In addition, racial disparities in outcomes after TBI in younger age groups have been previously reported. Younger adults who identify as belonging to racial or ethnic minority groups experience worse functional recovery and residual disability after TBI, even after controlling for injury severity and discharge functional status.10,11,12,13 Although Black older adults generally report more unmet mobility and activity needs compared with White older adults, little is known about racial disparities in rehabilitation care in home- and community-based settings among older adults after TBI.11,14
Appropriate postacute rehabilitation care is critical for improving functional outcomes and quality of life during the postacute injury period. However, in younger populations there is evidence that Black patients are less likely to receive inpatient rehabilitation after TBI compared with White patients.15 Racial disparities in receipt of rehabilitation and subsequent recovery after TBI are likely compounded by age given that older adults are less likely to receive inpatient rehabilitation and experience worse recovery compared with younger adults.16,17,18,19,20
Rehabilitation care for patients with TBI does not end at the time of hospital discharge. Access to home- and community-based rehabilitation (HCBR), such as outpatient and home health care, could improve recovery after TBI and help older adults remain in the community longer. Home health care includes skilled nursing care, physical and occupational therapy, speech-language therapy, and medical social services, which are provided by a variety of skilled health care professionals at the patient’s home. However, home care and outpatient rehabilitation are delivered in distinct rehabilitation settings and fragmented by payment system. For example, home health care is paid under the Medicare Part A benefit, and only those beneficiaries who are homebound can qualify for these services. Generally, home care focuses on mobility goals and is delivered in distinct 30- to 60-day episodes. Outpatient rehabilitation is provided under the Medicare Part B benefit, which includes a patient responsibility of 20% coinsurance for each visit. In outpatient rehabilitation, patients can focus on higher-level mobility and functional goals (such as independent community ambulation) without homebound restrictions.
Understanding access to HCBR among racial and ethnic minority groups is especially pertinent, as this population is likely to be discharged to inpatient rehabilitation but more likely to experience physical and financial barriers in accessing care.15,21,22 These services serve a critical role in the continuum of care, yet Black patients may experience barriers in access to HCBR after TBI, impacting health outcomes.10,11,12,13,15,23 One key determinant of health among Black patients with TBI is structural racism or inequities in access to walkable sidewalks, transportation, and economic resources that have been continually reinforced through biased or overtly racist housing, employment, and education policies.24 These inequities could interrupt access to home-based rehabilitation if it is perceived to be difficult or dangerous to provide services in these neighborhoods. Outpatient rehabilitation also may be disrupted, as costs associated with transportation, parking, and Medicare copayments may be challenging for those with lower incomes. Because no prior studies have examined use of HCBR after TBI among older adults, it is unknown how often Black patients who need home health or outpatient care after TBI actually receive it. Therefore, the aim of the study was to evaluate whether race was associated with receipt of HCBR rehabilitation among a nationally representative sample of older adult Medicare beneficiaries after TBI.
Methods
We conducted a retrospective cohort study using Medicare administrative claims and assessment data obtained from the Centers for Medicare & Medicaid Services Chronic Conditions Warehouse. The study sample was selected from a 5% random sample for years 2010 through 2016 and a 20% random sample for years 2017 through 2018. Claims were available for hospitals, skilled nursing facilities, home health care agencies, and both freestanding and hospital-based outpatient facilities. The University of Maryland School of Medicine Institutional Review Board deemed the study exempt from review and waived the requirement for informed consent because only deidentified data were used. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Population
The study population comprised community-dwelling Medicare beneficiaries aged 65 years and older who were hospitalized with a primary diagnosis of TBI between 2010 and 2017 and discharged alive to a nonhospice community setting. For beneficiaries who had multiple TBI claims over the observation period, only the first observation was used. Community-dwelling status before TBI was defined as those who were not long-stay residents (residence of more than 100 days in a long-term care facility before admission) as identified by using assessment dates on the Medicare Minimum Data Set 3.0. Traumatic brain injury was defined using International Classification of Diseases, Ninth Revision (ICD-9) and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes (eTable in the Supplement) on inpatient claims, and the date of TBI was assigned as the index date.1 Codes indicating TBI sequelae or subsequent encounters were excluded from our TBI definition. Study participants were required to have continuous Medicare Parts A and B coverage for at least 6 months before and for the entirety of the 12-month follow-up period or until death.
TBI Acuity and Race and Ethnicity
A major limitation in clinical and health service research using population-based data is that data are missing information on TBI acuity measures. We have addressed this important limitation by including an estimate of the Abbreviated Injury Scale (AIS) score for the head region. The AIS is a measure of anatomic injury severity associated with increased risk of mortality.25,26 It is rated on a scale from 1 to 6, with higher scores indicating greater injury severity. We excluded individuals with AIS scores of 6, as these injuries are designated as untreatable. We estimated the AIS head score using the ICD Programs for Injury Categorization in R (ICDPICR) (R Project for Statistical Computing), which converts ICD-9 and ICD-10 codes from the inpatient claim into AIS codes.27 This software has been previously used to estimate the head AIS score in patients with TBI.28,29,30 Consistent with our prior work, we also used length of hospital stay, whether the hospitalization included an intensive care unit stay, and discharge location (home vs rehabilitation) as proxies for injury severity.31,32,33 Hospital length of stay was highly skewed and was categorized for analysis based on its distribution.
Patients’ race and ethnicity were classified as non-Hispanic Black (hereafter Black) and non-Hispanic White (hereafter White) based on self-reported information obtained from the Medicare Beneficiary Summary File. Individuals identifying as another race and ethnicity were excluded because of small sample sizes within each category that precluded accurate estimation of disparities for these populations.
Home- and Community-Based Rehabilitation Services
The primary outcome was the use rate of HCBR delivered by occupational therapy or physical therapy clinicians in the 6 months after TBI admission. Although research on recovery after TBI among older adults is limited, evidence from previous studies of Medicare beneficiaries, as well as studies of patients with hip fractures, suggests that recovery plateaus by 6 months after injury.33,34,35 To calculate the numerator for the rate, we first calculated physical rehabilitation visits delivered in home health care settings under a Medicare Part A stay by extracting individual revenue codes associated with physical therapy (042x) and occupational therapy (043x) from the home health care claims file.36 Similarly, revenue codes (from the Outpatient File) or rehabilitation specialty codes (from the Carrier File) for outpatient visits were captured to identify visit counts for patients receiving outpatient rehabilitation under Medicare Part B, which can include visits received in clinics, within assisted living facilities, or at the patient’s home. These methods are consistent with those used by Warren and Shireman37 to capture variability in rehabilitation use for Medicare beneficiaries. We eliminated Medicare Part B visits delivered to patients during long-term nursing home stays, hospital observation stays, and emergency department visits by comparing the date of service on rehabilitation claims against Minimum Data Set records and outpatient claims files—this exclusion, which to the best of our knowledge is novel, more accurately identifies those receiving community-based rehabilitation care. eFigures 2 to 4 in the Supplement detail our process for identifying rehabilitation visits.
The number of days spent at home after a TBI is not equal for each patient. For example, patients discharged to inpatient rehabilitation are not at home and would not be able to receive HCBR. Therefore, the denominator for HCBR rates was the number of days per month that the patient was at home. This approach allowed us to account for differing lengths of hospital and rehabilitation facility stays and permitted inclusion of beneficiaries who did not survive the entire follow-up period. The number of days at home per month was adapted from a previous study38 and calculated by subtracting the sum of inpatient days, skilled nursing facility days, inpatient psychiatry days, inpatient rehabilitation days, hospital observation days, emergency department days, long-term nursing home stays, and long-term care hospital days from the total number of days spent alive each month.
Covariates
In addition to age and sex, the Chronic Conditions Warehouse contains annual flags and dates of first diagnosis for 27 chronic conditions that are identified using Centers for Medicare & Medicaid Services algorithms based on specific diagnosis or procedure codes.39 If the date of first diagnosis occurred before the date of TBI, that condition was considered present at baseline. In addition, we captured the Original Reason for Entitlement Code (OREC), dichotomized as age or disability (including end-stage kidney disease) and eligibility for Medicaid (dual eligibility), an indicator of low socioeconomic status.
Statistical Analysis
Data were analyzed January 21 to August 30, 2022. We described the distribution of clinical, demographic, and injury-related characteristics by race and tested differences in distributions using χ2 goodness-of-fit and t tests. We stratified the subsequent analyses by home health vs outpatient rehabilitation because evidence suggests that use of these modalities varies by race and clinical needs.40 We plotted unadjusted monthly rates of home health and outpatient rehabilitation over the 6 months after TBI.
Counts of HCBR visits were modeled over the 6 months after TBI as a function of race and time using generalized estimating equations with a negative binomial distribution and log link, with the log of days at home as an offset. The correlation matrix was independent. Time was modeled as its inverse based on model fit using the quasilikelihood information criterion. Next, we successively added groups of variables (TBI acuity, demographic characteristics, comorbidities and socioeconomic indicators) to the regression model to evaluate the association of each subsequent addition with adjusted estimates for race to identify potential mechanisms associated with racial disparities. Rate ratios and 95% CIs were reported. To assess whether racial disparities in HCBR were modified by discharge location (a proxy for injury severity), we also tested the fully adjusted model with an interaction term (community vs facility). During preliminary analyses, we observed that Black beneficiaries were more likely to qualify for the Medicare entitlement due to disability or end-stage kidney disease compared with White beneficiaries. Thus, we also tested whether the OREC (age vs disability) modified the association of race on receipt of home health and outpatient rehabilitation using an interaction term. A 2-sided P < .05 was considered statistically significant.
Results
We identified 32 560 Medicare beneficiaries with TBI who met the enrollment criteria (eFigure 1 in the Supplement). Of these, 4740 (14.6%) were deceased at discharge, 5659 (17.4%) were discharged to locations other than a nonhospice community setting (eg, hospice, long-term acute care, or psychiatric hospital), 1486 (4.6%) were younger than 65 years, and 1649 (5.1%) were not Black or White, leaving 19 026 beneficiaries (58.4%) in the study sample (mean [SD] age, 81.6 [8.1] years; 10 781 women [56.7%] and 8245 men [43.3%]; and 994 Black beneficiaries [5.2%] and 18 032 White beneficiaries [94.8%]) (Table 1). Black beneficiaries were more likely to have a head AIS score of 4 or 5, indicating more severe TBI compared with White beneficiaries (59.3% vs 53.1%; P < .001). Black beneficiaries were more likely to stay in the hospital more than 5 days compared with White beneficiaries (36.8% vs 27.3%; P < .001), although there was no difference in discharge to rehabilitation between groups (50.8% vs 51.2%; P = .12).
Table 1. Baseline Characteristics of Black and White Medicare Beneficiaries Hospitalized With TBI From 2010 Through 2017 and Discharged to Rehabilitation or Home .
| Characteristic | No. (%) | P value | |
|---|---|---|---|
| Black beneficiaries (n = 994) | White beneficiaries (n = 18 032) | ||
| Age, mean (SD), y | 79.8 (8.5) | 81.7 (8.1) | <.001 |
| Sex | |||
| Female | 532 (53.5) | 10 249 (56.8) | .04 |
| Male | 462 (46.5) | 7783 (43.2) | |
| TBI acuity variables | |||
| Abbreviated Injury Scale score for heada | |||
| 1-2 | 148/986 (15.0) | 2655/17 881 (14.8) | <.001 |
| 3 | 253/986 (25.7) | 5724/17 881 (32.0) | |
| 4-5 | 585/986 (59.3) | 9502/17 881 (53.1) | |
| Length of hospital stay, d | |||
| <2 | 128 (12.9) | 2483 (13.8) | <.001 |
| 2-3 | 286 (28.8) | 6565 (36.4) | |
| 4-5 | 214 (21.5) | 4064 (22.5) | |
| >5 | 366 (36.8) | 4920 (27.3) | |
| Intensive care unit stay | 346 (34.8) | 6199 (34.4) | .78 |
| Discharge destination | |||
| Home | 489 (49.2) | 8805 (48.8) | .12 |
| Rehabilitation | 505 (50.8) | 9227 (51.2) | |
| Comorbid conditions | |||
| Acute myocardial infarction | 95 (9.6) | 1771 (9.8) | .79 |
| Alzheimer disease and related dementias | 417 (42.0) | 5965 (33.1) | <.001 |
| Anemia | 764 (76.9) | 13 101 (72.7) | .004 |
| Asthma | 187 (18.8) | 2878 (16.0) | .02 |
| Atrial fibrillation | 196 (19.7) | 5774 (32.0) | <.001 |
| Cataract | 655 (65.9) | 14 551 (80.7) | <.001 |
| Cancer | 253 (25.5) | 3915 (21.7) | .006 |
| Chronic kidney disease | 559 (56.2) | 7607 (42.2) | <.001 |
| Depression | 386 (38.8) | 8531 (47.3) | <.001 |
| Diabetes | 600 (60.4) | 7858 (43.6) | <.001 |
| Glaucoma | 375 (37.7) | 5162 (28.6) | <.001 |
| Heart failure | 515 (51.8) | 8062 (44.7) | <.001 |
| Hip fracture | 48 (4.8) | 1646 (9.1) | <.001 |
| Hyperlipidemia | 819 (82.4) | 15 558 (86.3) | <.001 |
| Hypertension | 932 (93.8) | 16 460 (91.3) | .007 |
| Hypothyroid | 232 (23.3) | 6282 (34.8) | <.001 |
| Ischemic heart disease | 680 (68.4) | 12 344 (68.5) | .98 |
| Osteoporosis | 184 (18.5) | 5834 (32.4) | <.001 |
| Rheumatoid or osteoarthritis | 681 (68.5) | 12 895 (71.5) | .04 |
| Stroke | 350 (35.2) | 5618 (31.2) | .007 |
| Socioeconomic indicators | |||
| Original reason for entitlement | |||
| Age | 793 (79.8) | 16 231 (90.0) | <.001 |
| Disability or end-stage kidney disease | 201 (20.2) | 1801 (10.0) | |
| Dual eligibility in Medicare and Medicaid | 425 (42.8) | 4127 (22.9) | <.001 |
Abbreviation: TBI, traumatic brain injury.
Some International Classification of Diseases, Ninth Revision and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes were not able to be converted into Abbreviated Injury Scale codes, and thus the numbers in this section do not add to the total beneficiaries.
Black beneficiaries were younger than White beneficiaries (mean [SD] age, 79.8 [8.5] years vs 81.7 [8.1] years; P < .001) and more likely to be male (46.5% vs 43.2%; P = .04) (Table 1). Black beneficiaries had a higher burden of most comorbidities compared with White beneficiaries, including a higher prevalence of Alzheimer disease and related dementias (42.0% vs 33.1%; P < .001), chronic kidney disease (56.2% vs 42.2%; P < .001), and heart failure (51.8% vs 44.7%; P < .001). Black beneficiaries were more likely to have initially qualified for Medicare due to disability or end-stage kidney disease compared with White beneficiaries (20.2% vs 10.0%; P < .001) and more likely to be dual eligible for Medicaid (42.8% vs 22.9%; P < .001).
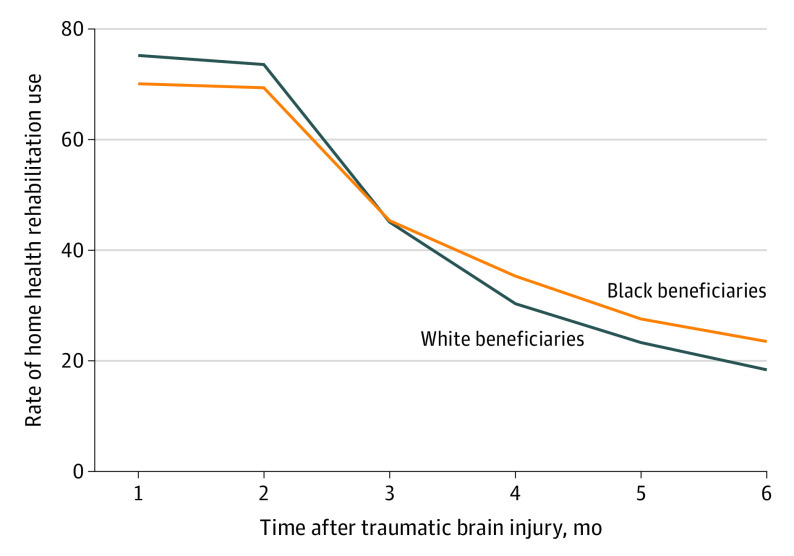
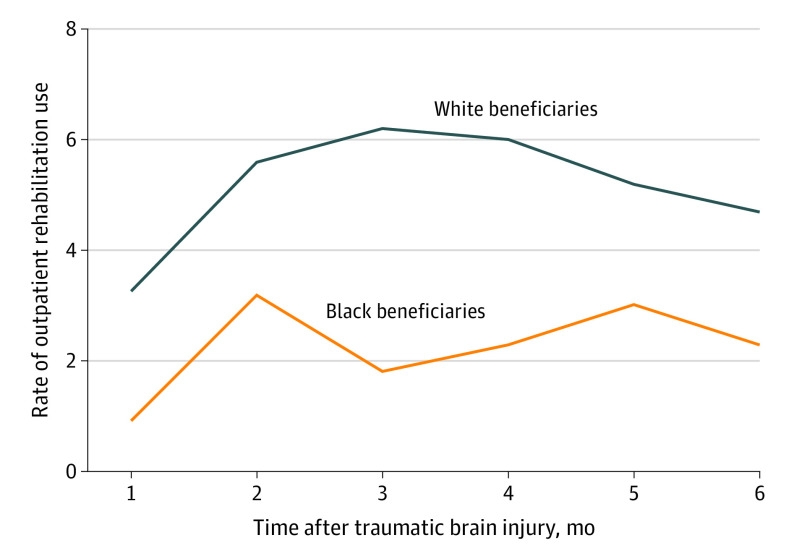
Over the 6 months after injury, almost half of beneficiaries hospitalized with TBI received at least 1 home health rehabilitation visit, with no statistically significant differences between Black and White beneficiaries (47.4% vs 46.2%; P = .46). Although receipt of outpatient rehabilitation was much less common, Black beneficiaries were less likely to receive at least 1 outpatient rehabilitation visit compared with White beneficiaries (3.4% vs 7.1%; P < .001). Unadjusted rates of home health care and outpatient rehabilitation use for the 6 months after TBI are displayed by race in Figure 1 and Figure 2.
Figure 1. Rate of Home Health Rehabilitation Visits per 1000 Days at Home During the 6 Months After Traumatic Brain Injury Among Older Medicare Beneficiaries.
Figure 2. Rate of Outpatient Rehabilitation Visits per 1000 Days at Home During the 6 Months After Traumatic Brain Injury Among Older Medicare Beneficiaries.
We observed significant differences in outpatient use between Black vs White patients (Table 2). Black beneficiaries were less likely than White beneficiaries to receive outpatient therapy over the 6 months after TBI in the unadjusted model (rate ratio, 0.47; 95% CI, 0.31-0.72). Addition of covariates was not followed by large changes to the effect estimate, which remained significant in the fully adjusted model (rate ratio, 0.60; 95% CI, 0.38-0.93). In contrast, Black beneficiaries were more likely to receive home health rehabilitation in the unadjusted (rate ratio, 1.14; 95% CI, 1.02-1.27) and fully adjusted (rate ratio, 1.15; 95% CI, 1.00-1.32; P = .04) models (Table 3). There was no statistically significant interaction between race and discharge location or race and OREC for either home health or outpatient rehabilitation rates.
Table 2. Association Between Race and Use of Outpatient Rehabilitation Services Over the 6 Months After Hospitalization for Traumatic Brain Injury Among Black and White Medicare Beneficiaries From 2010 Through 2017.
| Rate ratio (95% CI) | |
|---|---|
| Unadjusted | |
| Black beneficiaries | 0.47 (0.31-0.72) |
| White beneficiaries | 1 [Reference] |
| Adjusted, acuity variablesa | |
| Black beneficiaries | 0.47 (0.31-0.72) |
| White beneficiaries | 1 [Reference] |
| Adjusted, acuity and demographic variablesb | |
| Black beneficiaries | 0.47 (0.31-0.71) |
| White beneficiaries | 1 [Reference] |
| Adjusted, acuity, demographic, and comorbidity variablesc | |
| Black beneficiaries | 0.50 (0.33-0.77) |
| White beneficiaries | 1 [Reference] |
| Adjusted, acuity, demographic, comorbidity, and socioeconomic variablesd | |
| Black beneficiaries | 0.60 (0.38-0.93) |
| White beneficiaries | 1 [Reference] |
Length of hospital stay, Abbreviated Injury Scale score for head, intensive care unit stay, and discharge location (home vs inpatient rehabilitation).
Age and sex.
Acute myocardial infarction, Alzheimer disease and related dementias, anemia, asthma, atrial fibrillation, cataract, cancer, chronic kidney disease, chronic obstructive pulmonary disease, depression, diabetes, glaucoma, heart failure, hip fracture, hyperlipidemia, hypertension, hypothyroid, ischemic heart disease, osteoporosis, rheumatoid and osteoarthritis, and stroke.
Dual Medicaid and Medicare eligibility and Original Reason for Medicare Entitlement Code (age vs other).
Table 3. Association Between Race and Use of Home Health Rehabilitation Services Over the 6 Months After Hospitalization for Traumatic Brain Injury Among Black and White Medicare Beneficiaries From 2010 Through 2017.
| Rate ratio (95% CI) | |
|---|---|
| Unadjusted | |
| Black beneficiaries | 1.14 (1.02-1.27) |
| White beneficiaries | 1 [Reference] |
| Adjusted, acuity variablesa | |
| Black beneficiaries | 1.14 (1.01-1.29) |
| White beneficiaries | 1 [Reference] |
| Adjusted, acuity and demographic variablesb | |
| Black beneficiaries | 1.25 (1.10-1.42) |
| White beneficiaries | 1 [Reference] |
| Adjusted, acuity, demographic, and comorbidity variablesc | |
| Black beneficiaries | 1.19 (1.04-1.37) |
| White beneficiaries | 1 [Reference] |
| Adjusted, acuity, demographic, comorbidity, and socioeconomic variablesd | |
| Black beneficiaries | 1.15 (1.00-1.32)e |
| White beneficiaries | 1 [Reference] |
Length of hospital stay, Abbreviated Injury Scale score for head, intensive care unit stay, discharge location (home vs inpatient rehabilitation).
Age and sex.
Acute myocardial infarction, Alzheimer disease and related dementias, anemia, asthma, atrial fibrillation, cataract, cancer, chronic kidney disease, chronic obstructive pulmonary disease, depression, diabetes, glaucoma, heart failure, hip fracture, hyperlipidemia, hypertension, hypothyroid, ischemic heart disease, osteoporosis, rheumatoid and osteoarthritis, and stroke.
Dual Medicaid and Medicare eligibility, Original Reason for Medicare Entitlement Code (age vs other).
P = .04.
Discussion
Among a nationally representative sample of older Black and White Medicare beneficiaries hospitalized with TBI, we found low rates of outpatient rehabilitation use overall and racial disparities in patterns of use. Two major findings of this article warrant attention. First, fewer than half of the beneficiaries received rehabilitation from a home health care agency, and less than 1 in 10 received services from an outpatient clinician. This low rate of use is alarming given that the majority of TBI among older adults results from an injurious fall,1,3 and patients often experience physical and cognitive impairment.3,4,5,6,7,8,9 A lack of engagement with formal rehabilitation services may contribute to unmet needs for assistance with activities of daily living, leaving older adults who have these unmet needs at risk for future falls, hospitalizations, or institutionalization. Second, we found relative shifts in rehabilitation use, with markedly lower outpatient therapy use and modestly higher home health care use among Black patients with TBI. This finding is concerning because restrictions on delivery of home care therapy may not permit maximal recovery of outcomes important to patients, such as community mobility. Furthermore, a previous study41 found that patients identifying as a member of a racial or ethnic minority group were less likely to receive care from high-quality home health agencies. The present study adds new information on the disparity in outpatient rehabilitation services for high-risk and high-need socioeconomically disadvantaged patient populations. Moreover, barriers experienced by Black older adults in accessing appropriate and high-quality rehabilitation may be 1 potential mechanism explaining poorer functional outcome among Black older adults after TBI. Taken together, findings of the present study point toward a need for rehabilitation to be better integrated in care pathways for older adults recovering from a TBI.
Rehabilitation services for patients with TBI often include gait training, balance exercises, and interventions to improve activities of daily living functioning—all important services to promote aging in place after traumatic injuries. When older adults do not receive these services, it is likely that potentially addressable mobility deficits are left untreated. Mobility-related impairments that go unaddressed, especially with overlying cognitive deficits common in TBI, may be associated with an increased risk for falls, hospitalizations, or institutionalization. In this study, the fact that less than half of the sample received any home-based care is worrisome. In addition to individualized rehabilitation exercises, home-based care delivered by physical and occupational therapists includes careful inspections of the home environment, adaptation of equipment and home environment (eg, installation of grab bars) for safe mobility, and provision of caregiver training—all of which would be beneficial for older adults recovering from even uncomplicated TBIs. Failure to provide home-based care after TBI could leave potentially modifiable impairments or home environment safety concerns unaddressed.
Substantial race-based disparities were observed in the use of outpatient rehabilitation care, even after accounting for injury severity, geriatric comorbidities, and socioeconomic status. Black race was associated with lower use of outpatient rehabilitation (rate ratio, 0.60), a disparity that has not been previously documented to our knowledge. Outpatient rehabilitation care, mostly provided in centers with more equipment and resources, permits practice of high-level gait and balance tasks (eg, walking over uneven surfaces) as well as higher-level cognitive rehabilitation that may be difficult to accomplish effectively during short episodes of home health care. Lack of access to and low use of outpatient rehabilitation among older Black patients with TBI may contribute to poorer outcomes.10,11,12
Infrequent outpatient rehabilitation use is consistent with estimates from patients with stroke, of whom only 11% received these services in the early posthospitalization period in prior national studies.42 Additionally, low use of HCBR services among other older adult populations has been associated with poorer functional recovery and higher rates of hospital readmission; thus, disparities in rehabilitation use among Black beneficiaries with TBI is of concern.42,43,44 Infrequent outpatient rehabilitation use has been observed in prior studies of older adult populations without TBI and suggests that previously observed disparities in rehabilitation use may have been a factor in outpatient rather than home health rehabilitation.40,45,46
The observed racial disparities in access to outpatient rehabilitation may be manifestations of structural discrimination and social determinants of health.21,47,48 For example, structural factors, such as poor quality of housing, poorly maintained built environments (eg, cracked sidewalks), or low availability of public transportation, may impact access to physical therapy and impede functional recovery.49,50 Black older adults may be disproportionately affected by these factors as a result of historically biased urban planning policies at the local, state, and federal levels.51 A lack of therapists in certain geographic regions (eg, rural areas) has also been cited as a barrier to use.40,52 These barriers may weigh even heavier on older adults who have mobility limitations or disabilities. These results highlight the importance of understanding how the social determinants of health impact access to HCBR. Additionally, individual-level socioeconomic disadvantage may mediate racial and ethnic disparities in rehabilitation use.40,45,46 In the present study, eligibility for Medicaid, a proxy for low income, was associated with use of outpatient rehabilitation, providing evidence of intersectionality. Nonetheless, evidence on dual eligibility as a barrier to rehabilitation has been mixed. For example, among Medicare beneficiaries enrolled in the National Health and Aging Trends Study,40 lack of transportation was the largest barrier to receipt of rehabilitation over the last year. Finally, it should be noted that prevalence of Alzheimer disease and related dementias was modestly high in the study population but was disproportionately higher among Black older adults compared with White older adults (42.0% vs 33.1%). Preexisting cognitive impairment has previously been identified as a barrier to receiving inpatient rehabilitation among patients who have had strokes, although whether it would result in differential use of outpatient services is not known.53,54 Future investigation of barriers to receipt of outpatient rehabilitation among older adults after TBI could identify targets for improving rehabilitation use.
Strengths and Limitations
Strengths of this study include a large and nationally representative sample of older Medicare beneficiaries. To our knowledge, this study is the first to examine use of HCBR services after TBI and the first to specifically focus on racial disparities in the use of rehabilitation services after TBI among older adults. Use of days at home as the denominator for the HCBR rate calculations effectively controlled for differences in hospital length of stay and inpatient rehabilitation as well as censoring due to death. Finally, we were able to control for anatomic TBI injury severity by converting diagnostic codes to AIS codes using the ICDPICR program.27
Limitations of this study should be considered when interpreting the results. First, this study focused only on beneficiaries hospitalized with TBI, meaning older adults with mild TBI may have been underrepresented. Nonetheless, based on the AIS scores, approximately 15% of the sample had mild TBI (AIS 1-2). Hospitalized beneficiaries would likely be more severely injured and in need of HCBR services. Although we used the ICDPICR software to approximate the head AIS score, there may have been some misclassification of TBI severity. Although claims data do not have information on mechanism of injury, which is related to pre-TBI function, falls are the predominant injury mechanism for more than 75% of TBIs.1,55,56 Furthermore, this study included Medicare Fee-for-Service beneficiaries; thus, individuals with Medicare Advantage plans were not represented. Finally, social support and transportation may have altered participation in outpatient rehabilitation, yet these variables were not available in the data. Lack of transportation has previously been identified as a barrier to receipt of rehabilitation among older adults,40 and both social support and transportation have been identified as barriers to receipt of psychiatric care among adults with TBI.57 Future studies should seek to address these limitations to elucidate perceptions of rehabilitation services after TBI among older adults.
Conclusions
Among older adults with TBI, we observed relative shifts in rehabilitation use, with markedly lower outpatient therapy use and modestly higher home health care use among Black patients compared with White patients with TBI, which may contribute to differences in recovery from TBI and long-term disability. The findings underscore the need to further investigate the underlying causes of racial disparities in long-term outcomes among older patients with TBI. A better understanding of the delivery of HCBR services after TBI may inform the implementation of strategies to mitigate differences in patient outcomes.
eTable. International Classification of Disease (ICD) Codes Version 9 and 10 Used to Identify Traumatic Brain Injury
eFigure 1. Study Population Flow Chart of Medicare Beneficiaries, 2010-2018
eFigure 2. Identifying Outpatient Rehabilitation Visits in Medicare Claims: Outpatient File
eFigure 3. Identifying Outpatient Rehabilitation Visits in Medicare Claims: Carrier File
eFigure 4. Identifying Home-Health Rehabilitation Visits in Medicare Claims: Home Health Claims File
References
- 1.Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR Surveill Summ. 2017;66(9):1-16. doi: 10.15585/mmwr.ss6609a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albrecht JS, Hirshon JM, McCunn M, et al. Increased rates of mild traumatic brain injury among older adults in US emergency departments, 2009-2010. J Head Trauma Rehabil. 2016;31(5):E1-E7. doi: 10.1097/HTR.0000000000000190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gardner RC, Dams-O’Connor K, Morrissey MR, Manley G. Geriatric traumatic brain injury: epidemiology, outcomes, knowledge gaps, and future directions. J Neurotrauma. 2018;35(7):889-906. doi: 10.1089/neu.2017.5371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mosenthal AC, Lavery RF, Addis M, et al. Isolated traumatic brain injury: age is an independent predictor of mortality and early outcome. J Trauma. 2002;52(5):907-911. doi: 10.1097/00005373-200205000-00015 [DOI] [PubMed] [Google Scholar]
- 5.Mosenthal AC, Livingston DH, Lavery RF, et al. The effect of age on functional outcome in mild traumatic brain injury: 6-month report of a prospective multicenter trial. J Trauma. 2004;56(5):1042-1048. doi: 10.1097/01.TA.0000127767.83267.33 [DOI] [PubMed] [Google Scholar]
- 6.Selassie AW, Zaloshnja E, Langlois JA, Miller T, Jones P, Steiner C. Incidence of long-term disability following traumatic brain injury hospitalization, United States, 2003. J Head Trauma Rehabil. 2008;23(2):123-131. doi: 10.1097/01.HTR.0000314531.30401.39 [DOI] [PubMed] [Google Scholar]
- 7.Susman M, DiRusso SM, Sullivan T, et al. Traumatic brain injury in the elderly: increased mortality and worse functional outcome at discharge despite lower injury severity. J Trauma. 2002;53(2):219-223. doi: 10.1097/00005373-200208000-00004 [DOI] [PubMed] [Google Scholar]
- 8.Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006;54(10):1590-1595. doi: 10.1111/j.1532-5415.2006.00894.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Utomo WK, Gabbe BJ, Simpson PM, Cameron PA. Predictors of in-hospital mortality and 6-month functional outcomes in older adults after moderate to severe traumatic brain injury. Injury. 2009;40(9):973-977. doi: 10.1016/j.injury.2009.05.034 [DOI] [PubMed] [Google Scholar]
- 10.Arango-Lasprilla JC, Rosenthal M, Deluca J, et al. Traumatic brain injury and functional outcomes: does minority status matter? Brain Inj. 2007;21(7):701-708. doi: 10.1080/02699050701481597 [DOI] [PubMed] [Google Scholar]
- 11.Shafi S, Marquez de la Plata C, Diaz-Arrastia R, et al. Racial disparities in long-term functional outcome after traumatic brain injury. J Trauma. 2007;63(6):1263-1268. doi: 10.1097/TA.0b013e31815b8f00 [DOI] [PubMed] [Google Scholar]
- 12.Staudenmayer KL, Diaz-Arrastia R, de Oliveira A, Gentilello LM, Shafi S. Ethnic disparities in long-term functional outcomes after traumatic brain injury. J Trauma. 2007;63(6):1364-1369. doi: 10.1097/TA.0b013e31815b897b [DOI] [PubMed] [Google Scholar]
- 13.Gary KW, Arango-Lasprilla JC, Stevens LF. Do racial/ethnic differences exist in post-injury outcomes after TBI? a comprehensive review of the literature. Brain Inj. 2009;23(10):775-789. doi: 10.1080/02699050903200563 [DOI] [PubMed] [Google Scholar]
- 14.Berridge C, Mor V. Disparities in the prevalence of unmet needs and their consequences among Black and White older adults. J Aging Health. 2018;30(9):1427-1449. doi: 10.1177/0898264317721347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meagher AD, Beadles CA, Doorey J, Charles AG. Racial and ethnic disparities in discharge to rehabilitation following traumatic brain injury. J Neurosurg. 2015;122(3):595-601. doi: 10.3171/2014.10.JNS14187 [DOI] [PubMed] [Google Scholar]
- 16.NIH Consensus Development Panel on Rehabilitation of Persons With Traumatic Brain Injury . Rehabilitation of persons with traumatic brain injury. JAMA. 1999;282(10):974-983. doi: 10.1001/jama.282.10.974 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention . Report to Congress on traumatic brain injury in the United States: epidemiology and rehabilitation. 2015. Accessed December 8, 2022. https://www.cdc.gov/traumaticbraininjury/pubs/congress_epi_rehab.html [DOI] [PubMed]
- 18.Uomoto JM. Older adults and neuropsychological rehabilitation following acquired brain injury. NeuroRehabilitation. 2008;23(5):415-424. doi: 10.3233/NRE-2008-23505 [DOI] [PubMed] [Google Scholar]
- 19.Frankel JE, Marwitz JH, Cifu DX, Kreutzer JS, Englander J, Rosenthal M. A follow-up study of older adults with traumatic brain injury: taking into account decreasing length of stay. Arch Phys Med Rehabil. 2006;87(1):57-62. doi: 10.1016/j.apmr.2005.07.309 [DOI] [PubMed] [Google Scholar]
- 20.Dijkers M, Brandstater M, Horn S, Ryser D, Barrett R. Inpatient rehabilitation for traumatic brain injury: the influence of age on treatments and outcomes. NeuroRehabilitation. 2013;32(2):233-252. doi: 10.3233/NRE-130841 [DOI] [PubMed] [Google Scholar]
- 21.Riley WJ. Health disparities: gaps in access, quality and affordability of medical care. Trans Am Clin Climatol Assoc. 2012;123:167-172. [PMC free article] [PubMed] [Google Scholar]
- 22.Young DR, Cradock AL, Eyler AA, et al. ; American Heart Association Advocacy Coordinating Committee . Creating built environments that expand active transportation and active living across the United States: a policy statement from the American Heart Association. Circulation. 2020;142(11):e167-e183. doi: 10.1161/CIR.0000000000000878 [DOI] [PubMed] [Google Scholar]
- 23.Chun Fat S, Herrera-Escobar JP, Seshadri AJ, et al. Racial disparities in post-discharge healthcare utilization after trauma. Am J Surg. 2019;218(5):842-846. doi: 10.1016/j.amjsurg.2019.03.024 [DOI] [PubMed] [Google Scholar]
- 24.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453-1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 25.Rating the severity of tissue damage: I. The abbreviated scale. JAMA. 1971;215(2):277-280. doi: 10.1001/jama.1971.03180150059012 [DOI] [PubMed] [Google Scholar]
- 26.Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187-196. doi: 10.1097/00005373-197403000-00001 [DOI] [PubMed] [Google Scholar]
- 27.Clark DE, Black AW, Skavdahl DH, Hallagan LD. Open-access programs for injury categorization using ICD-9 or ICD-10. Inj Epidemiol. 2018;5(1):11. doi: 10.1186/s40621-018-0149-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Deynse H, Cools W, Depreitere B, et al. Traumatic brain injury hospitalizations in Belgium: a brief overview of incidence, population characteristics, and outcomes. Front Public Health. 2022;10:916133. doi: 10.3389/fpubh.2022.916133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Validation of ICDPIC software injury severity scores using a large regional trauma registry. Inj Prev. 2015;21(5):325-330. doi: 10.1136/injuryprev-2014-041524 [DOI] [PubMed] [Google Scholar]
- 30.Lilley EJ, Scott JW, Weissman JS, et al. End-of-life care in older patients after serious or severe traumatic brain injury in low-mortality hospitals compared with all other hospitals. JAMA Surg. 2018;153(1):44-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Albrecht JS, Liu X, Baumgarten M, et al. Benefits and risks of anticoagulation resumption following traumatic brain injury. JAMA Intern Med. 2014;174(8):1244-1251. doi: 10.1001/jamainternmed.2014.2534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Albrecht JS, Barbour L, Abariga SA, Rao V, Perfetto EM. Risk of depression after traumatic brain injury in a large national sample. J Neurotrauma. 2019;36(2):300-307. doi: 10.1089/neu.2017.5608 [DOI] [PubMed] [Google Scholar]
- 33.Albrecht JS, Peters ME, Smith GS, Rao V. Anxiety and posttraumatic stress disorder among Medicare beneficiaries after traumatic brain injury. J Head Trauma Rehabil. 2017;32(3):178-184. doi: 10.1097/HTR.0000000000000266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55(9):M498-M507. doi: 10.1093/gerona/55.9.M498 [DOI] [PubMed] [Google Scholar]
- 35.Albrecht JS, Kiptanui Z, Tsang Y, et al. Depression among older adults after traumatic brain injury: a national analysis. Am J Geriatr Psychiatry. 2015;23(6):607-614. doi: 10.1016/j.jagp.2014.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Falvey JR, Murphy TE, Gill TM, Stevens-Lapsley JE, Ferrante LE. Home health rehabilitation utilization among Medicare beneficiaries following critical illness. J Am Geriatr Soc. 2020;68(7):1512-1519. doi: 10.1111/jgs.16412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Warren M, Shireman TI. Geographic variability in discharge setting and outpatient postacute physical therapy after total knee arthroplasty: a retrospective cohort study. Phys Ther. 2018;98(10):855-864. doi: 10.1093/ptj/pzy077 [DOI] [PubMed] [Google Scholar]
- 38.Burke LG, Orav EJ, Zheng J, Jha AK. Healthy days at home: a novel population-based outcome measure. Healthc (Amst). 2020;8(1):100378. doi: 10.1016/j.hjdsi.2019.100378 [DOI] [PubMed] [Google Scholar]
- 39.Centers for Medicare and Medicaid Services . Chronic Conditions Data Warehouse. 2020. Accessed May 5, 2022. https://www.ccwdata.org/web/guest/condition-categories
- 40.Keeney T, Jette AM, Freedman VA, Cabral H. Racial differences in patterns of use of rehabilitation services for adults aged 65 and older. J Am Geriatr Soc. 2017;65(12):2707-2712. doi: 10.1111/jgs.15136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fashaw-Walters SA, Rahman M, Gee G, Mor V, White M, Thomas KS. Out of reach: inequities in the use of high-quality home health agencies. Health Aff (Millwood). 2022;41(2):247-255. doi: 10.1377/hlthaff.2021.01408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Freburger JK, Li D, Fraher EP. Community use of physical and occupational therapy after stroke and risk of hospital readmission. Arch Phys Med Rehabil. 2018;99(1):26-34.e5. doi: 10.1016/j.apmr.2017.07.011 [DOI] [PubMed] [Google Scholar]
- 43.Freburger JK, Li D, Johnson AM, Fraher EP. Physical and occupational therapy from the acute to community setting after stroke: predictors of use, continuity of care, and timeliness of care. Arch Phys Med Rehabil. 2018;99(6):1077-1089.e7. doi: 10.1016/j.apmr.2017.03.007 [DOI] [PubMed] [Google Scholar]
- 44.Wang J, Liebel DV, Yu F, Caprio TV, Shang J. Inverse dose-response relationship between home health care services and rehospitalization in older adults. J Am Med Dir Assoc. 2019;20(6):736-742. doi: 10.1016/j.jamda.2018.10.021 [DOI] [PubMed] [Google Scholar]
- 45.Gell NM, Mroz TM, Patel KV. Rehabilitation services use and patient-reported outcomes among older adults in the United States. Arch Phys Med Rehabil. 2017;98(11):2221-2227.e3. doi: 10.1016/j.apmr.2017.02.027 [DOI] [PubMed] [Google Scholar]
- 46.Yeboah-Korang A, Kleppinger A, Fortinsky RH. Racial and ethnic group variations in service use in a national sample of Medicare home health care patients with type 2 diabetes mellitus. J Am Geriatr Soc. 2011;59(6):1123-1129. doi: 10.1111/j.1532-5415.2011.03424.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bade E, Evertsen J, Smiley S, Banerjee I. Navigating the health care system: a view from the urban medically underserved. WMJ. 2008;107(8):374-379. [PubMed] [Google Scholar]
- 48.McCallum CA. Access to physical therapy services among medically underserved adults: a mixed-method study. Phys Ther. 2010;90(5):735-747. doi: 10.2522/ptj.20090242 [DOI] [PubMed] [Google Scholar]
- 49.Gaskin DJ, Dinwiddie GY, Chan KS, McCleary R. Residential segregation and disparities in health care services utilization. Med Care Res Rev. 2012;69(2):158-175. doi: 10.1177/1077558711420263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Probst JC, Laditka SB, Wang JY, Johnson AO. Effects of residence and race on burden of travel for care: cross sectional analysis of the 2001 US National Household Travel Survey. BMC Health Serv Res. 2007;7:40. doi: 10.1186/1472-6963-7-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Falvey JR, Murphy TE, Leo-Summers L, Gill TM, Ferrante LE. Neighborhood socioeconomic disadvantage and disability after critical illness. Crit Care Med. 2022;50(5):733-741. doi: 10.1097/CCM.0000000000005364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carvalho E, Bettger JP, Goode AP. Insurance coverage, costs, and barriers to care for outpatient musculoskeletal therapy and rehabilitation services. N C Med J. 2017;78(5):312-314. doi: 10.18043/ncm.78.5.312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hakkennes SJ, Brock K, Hill KD. Selection for inpatient rehabilitation after acute stroke: a systematic review of the literature. Arch Phys Med Rehabil. 2011;92(12):2057-2070. doi: 10.1016/j.apmr.2011.07.189 [DOI] [PubMed] [Google Scholar]
- 54.Longley V, Peters S, Swarbrick C, Rhodes S, Bowen A. Does pre-existing cognitive impairment impact on amount of stroke rehabilitation received? an observational cohort study. Clin Rehabil. 2019;33(9):1492-1502. doi: 10.1177/0269215519843984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Albrecht JS, Al Kibria GM, Greene CR, Dischinger P, Ryb GE. Post-discharge mortality of older adults with traumatic brain injury or other trauma. J Am Geriatr Soc. 2019;67(11):2382-2386. doi: 10.1111/jgs.16098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Albrecht JS, McCunn M, Stein DM, Simoni-Wastila L, Smith GS. Sex differences in mortality following isolated traumatic brain injury among older adults. J Trauma Acute Care Surg. 2016;81(3):486-492. doi: 10.1097/TA.0000000000001118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Albrecht JS, O’Hara LM, Moser KA, Mullins CD, Rao V. Perception of barriers to the diagnosis and receipt of treatment for neuropsychiatric disturbances after traumatic brain injury. Arch Phys Med Rehabil. 2017;98(12):2548-2552. doi: 10.1016/j.apmr.2017.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. International Classification of Disease (ICD) Codes Version 9 and 10 Used to Identify Traumatic Brain Injury
eFigure 1. Study Population Flow Chart of Medicare Beneficiaries, 2010-2018
eFigure 2. Identifying Outpatient Rehabilitation Visits in Medicare Claims: Outpatient File
eFigure 3. Identifying Outpatient Rehabilitation Visits in Medicare Claims: Carrier File
eFigure 4. Identifying Home-Health Rehabilitation Visits in Medicare Claims: Home Health Claims File