Abstract
Indicative evidence suggests that minoritised ethnic groups have higher risk of developing multiple long-term conditions (MLTCs), and do so earlier than the majority white population. While there is evidence on ethnic inequalities in single health conditions and comorbidities, no review has attempted to look across these from a MLTCs perspective. As such, we currently have an incomplete understanding of the extent of ethnic inequalities in the prevalence of MLTCs. Further, concerns have been raised about variations in the way ethnicity is operationalised and how this impedes our understanding of health inequalities. In this systematic review we aimed to 1) describe the literature that provides evidence of ethnicity and prevalence of MLTCs amongst people living in the UK, 2) summarise the prevalence estimates of MLTCs across ethnic groups and 3) to assess the ways in which ethnicity is conceptualised and operationalised. We focus on the state of the evidence prior to, and during the very early stages of the pandemic. We registered the protocol on PROSPERO (CRD42020218061). Between October and December 2020, we searched ASSIA, Cochrane Library, EMBASE, MEDLINE, PsycINFO, PubMed, ScienceDirect, Scopus, Web of Science, OpenGrey, and reference lists of key studies/reviews. The main outcome was prevalence estimates for MLTCs for at least one minoritised ethnic group, compared to the majority white population. We included studies conducted in the UK reporting on ethnicity and prevalence of MLTCs. To summarise the prevalence estimates of MLTCs across ethnic groups we included only studies of MLTCs that provided estimates adjusted at least for age. Two reviewers screened and extracted data from a random sample of studies (10%). Data were synthesised using narrative synthesis. Of the 7949 studies identified, 84 met criteria for inclusion. Of these, seven contributed to the evidence of ethnic inequalities in MLTCs. Five of the seven studies point to higher prevalence of MLTCs in at least one minoritised ethnic group compared to their white counterparts. Because the number/types of health conditions varied between studies and some ethnic populations were aggregated or omitted, the findings may not accurately reflect the true level of ethnic inequality. Future research should consider key explanatory factors, including those at the macrolevel (e.g. racism, discrimination), as they may play a role in the development and severity of MLTCs in different ethnic groups. Research is also needed to ascertain the extent to which the COVID19 pandemic has exacerbated these inequalities.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-022-14940-w.
Keywords: Multiple long‐term conditions, Ethnicity, Inequalities, Systematic review, Narrative synthesis, UK
Background
Long‐term conditions (e.g. chronic kidney disease, hypertension and depression) are health conditions that are currently not curable and can only be managed with medication or other therapies [1, 2]. One in four primary care patients in the United Kingdom (UK) have multiple long-term health conditions (MLTCs) i.e. the presence of two or more long-term health conditions in an individual [3, 4]. Further, the proportion of people living with four or more long-term conditions is expected to double between 2015 and 2035 [5]. Evidently, healthcare systems, which have previously focused on single conditions, will need to radically transform their approaches to meet the challenges and complexity of caring for people with MLTCs [6].
Indicative evidence suggests that the risk of developing MLTCs is higher, and with MLTCs occurring at an earlier age, for people from minoritised ethnic groups than people from the majority white group [7, 8]. Studies of single conditions provide evidence that many, but not all, people from minoritised ethnic groups in the UK experience poorer health than people from the white ethnic group [9, 10]. Much of the variation in poor health across minoritised ethnic groups is due to underlying socioeconomic inequalities which, in turn, can be attributed to life-course experiences of racism and racial discrimination [11].
With ethnic inequalities evident in single health conditions, we would expect ethnic inequalities in MLTCs to follow a similar pattern. To our knowledge, there has been one previous review that has reported on ethnicity and MLTCs in the UK [12]. However, this review narrowly focused on long-term mental health conditions (i.e. comorbid substance use in psychosis), and therefore, provides only partial evidence of the burden of MLTCs across ethnic groups. Given that having MLTCs is associated with poorer functioning, lower quality of life, higher mortality risk [4], and greater healthcare use and cost [13], developing an understanding of the variation in the burden of MLTCs across ethnic groups in the population is key to ensure efficient, and equitable policy and practice [7].
It is important to consider that there is significant variability in the way ethnicity data is operationalised, analysed and presented in the UK [14]. These variations can introduce bias resulting in incorrect conclusions being drawn, ultimately compromising our understanding of health inequalities [14]. For a complete understanding of ethnic inequalities in the prevalence of MLTCs it is crucial for researchers to carefully consider how ethnicity is best conceptualised and to assess the strengths and limitations of the approaches they adopt during its operationalisation.
Thus, the aim of the present review is 1) to identify and describe the literature that provides evidence of ethnicity and prevalence of MLTCs amongst people living in the UK, 2) to summarise the prevalence estimates of MLTCs across ethnic groups and 3) to assess how ethnicity is conceptualised and operationalised. COVID-19 and the measures adopted to curb the spread of the virus during the pandemic have disproportionately affected minoritised ethnic group people. Given emerging evidence documenting the increase in ethnic inequalities following the coronavirus pandemic, we focus on the state of the evidence prior to, and during the very early stages of the pandemic. This provides a useful benchmark for future studies to measure and understand the impact on the pandemic in further exacerbating longstanding ethnic inequalities in health.
Methods
Search strategy
As per the Preferred Reporting Items for Systematic review and Meta‐Analysis Protocols (PRISMA‐P) guidelines [15], we registered the protocol for this review on PROSPERO (CRD42020218061). We electronically searched for studies that included the prevalence of MLTCs across ethnic groups in the UK using the following databases: ASSIA (Applied Social Sciences Index and Abstracts), Cochrane Library, EMBASE (Excerpta Medica dataBASE), MEDLINE, PsycINFO, PubMed, ScienceDirect, Scopus, Web of Science core collection. To ensure that relevant grey literature was not excluded we also conducted a search on OpenGrey. We supplemented the electronic search with a manual search of the reference lists of key articles identified. Experts in the field who had recently conducted systematic reviews on multimorbidity were contacted to compare search strategies and obtain further references. When full texts were unavailable, we contacted the relevant authors.
We adhered to the conventions of each search engine and used search terms that captured the key concepts; Ethnicity (e.g. "Ethnic Groups"[Mesh] OR “BME” OR “BAME”), multiple health conditions (e.g. “Multiple Chronic Conditions” OR Comorbid* OR Multimorbidity), Health inequality (e.g. "Health Equity"[Mesh] OR “Healthcare disparit*” [MeSH] OR Inequalit*) and the geographical location (e.g. "United Kingdom"[MeSH Terms] OR “UK”) (See Supplementary file 1 for a full list of search terms).
Study inclusion and exclusion criteria
We did not restrict the start of the search to any particular period in time and included studies published up until December 2020. Only UK studies, reported in English, with estimated prevalence of MLTCs across ethnic groups of people in the UK general population, residing in the community were included. To accommodate the variety of ways in which MLTCs were defined and operationalised in the extant literature, we included studies of multimorbidity (i.e. the presence of two or more long-term health conditions [16]) and comorbidity (i.e. the presence of any distinct additional co-existing ailment in a person with an index condition under investigation [17]). We applied further restrictions to address the second objective (to summarise the prevalence estimates of MLTCs across ethnic groups). Given the role of age in patterning MLTCs [2], and the younger age profile of minoritised ethnic group people [18], we excluded studies that did not adjust for at least age as they would have provided an inaccurate representation of the prevalence of MLTCs across ethnic groups. We also excluded studies that focused on only two conditions (e.g. depression and substance abuse) and included only studies that counted more than two conditions. These studies are more likely to focus on people with overall severity of illness, greater healthcare utilisation, and complex medical needs [19, 20].
We imported the studies retrieved from the electronic search to Endnote X8 where duplicates were removed. BH and LB screened a random sample (10%) of the titles, abstracts, and full texts. The studies were divided into 3 batches. For each batch, BH and LB double screened 10% of the studies first and compared results before BH continued to independently screen the remaining studies. Disagreements were resolved by discussion.
Data extraction strategy
We extracted relevant data from the included studies using a structured form with the following items: study identifier, design, setting, recruitment/data source, sample size, population description, definitions of MLTCs, type and number of MLTCs, confounders, and the results. We denoted any missing information with the acronym NR (i.e. Not Reported). BH and LB double extracted data from a random sample of studies (10%) and reconciled differences through discussion. Thereafter, BH independently extracted data from the remaining studies.
Population and outcomes
The outcomes of interest were prevalence estimates for MLTCs for at least one minoritised ethnic group, compared to the majority white population.
Quality appraisal
We assessed the quality of all the studies that contributed to evidence on ethnic inequalities in the prevalence of MLTCs using quality appraisal prompts proposed by Dixon-Woods and colleagues [21] (Supplementary file 2). The prompts can be used to appraise different study designs and focus on aspects of research practice, allowing for the identification and exclusion of studies which are deemed to be fatally flawed [21]. In addition to the quality appraisal, we assessed the relevance of the studies for understanding ethnic inequalities in the prevalence of MLTCs. This approach considers that some papers may have some methodological limitations but may still be of high relevance. Therefore, by considering both methodological quality and relevance, we maximise the inclusion and contribution of a wide range of studies at the level of concepts [21]. This approach is especially relevant given the dearth of studies assessing ethnic inequalities in MLTCs in the UK. All reviewers were involved in the quality appraisal of the studies. MS and LB each appraised a third of the studies. BH appraised the same studies and was in agreement with the ratings allocated by MS and LB (Supplementary file 3). The remaining studies were then independently appraised by BH.
Data synthesis and presentation
Given the different ways in which MLTCs were conceptualised and operationalised, the different ethnic groups, and the range of conditions explored in the included studies, we conducted a narrative synthesis. We present the findings of the synthesis in themes, supplemented with tables and figures, in two sections. First, we provide an overview of the studies that documented the prevalence estimates of MLTCs across ethnic groups. Second, we present studies where the authors counted more than two long-term conditions and reported on at least age-adjusted prevalence estimates of MLTCs across ethnic groups. Thus far, we have used the term ‘minoritised’ ethnic group people to refer to people who do not self‐identify as belonging to the majority white ethnic group. This term emphasises how social positions are social constructions dependent on context rather than outcomes and practices that are fixed and inevitable [22]. However, as we present the results, we use the terminology used by authors to describe ethnic categories in their studies in recognition of the different labels ascribed to minoritised ethnic group people in the UK.
Results
Overview of included studies
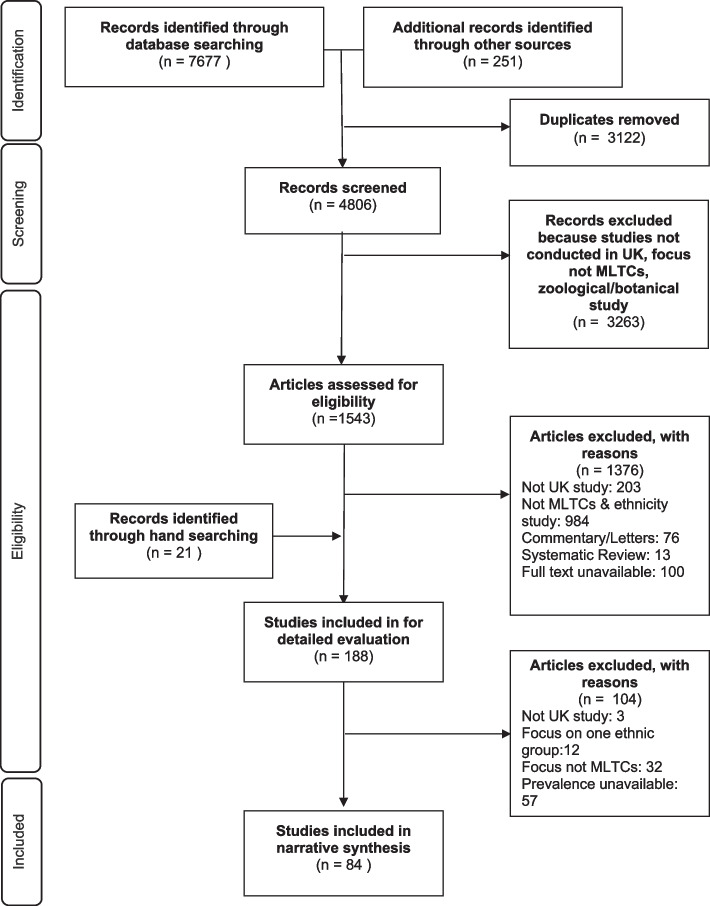
We identified 7949 titles from the electronic search, manual search and additional sources (See Fig. 1 which is based on PRISMA guidelines [23]). After removal of duplicates and studies identified as ineligible from the title or abstract, 188 papers were eligible for further evaluation. A further 104 studies were excluded, producing a final sample of 84 studies for the review. Seven of these studies contributed to the evidence of ethnic inequalities in the prevalence of MLTCs among people living in the UK. These were studies in which the authors counted more than two long-term conditions and adjusted for at least age in their analyses.
Fig. 1.
PRISMA Flow chart
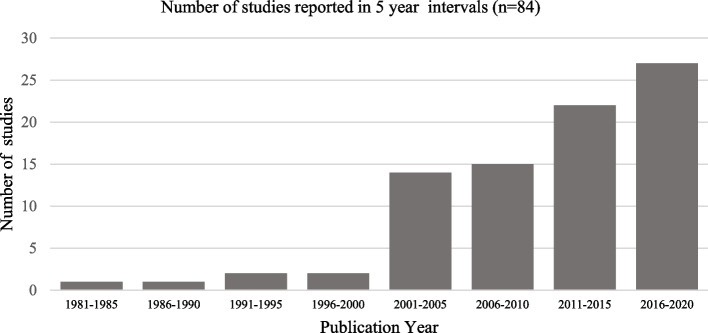
The 84 studies included were published between July 1984 and October 2020. Figure 2 below illustrates that the number of studies reporting on ethnic differences in MLTCs has increased steadily over the last four decades with a sharp increase in the number of studies published from the year 2001 onwards. The authors of the papers published before the turn of the century conceptualised MLTCs as complications [24], underlying diseases [25] or risk factors [26] for particular conditions. The term comorbidity is used from 2001 onwards to refer to MLTCs and it is not until 2010 that we start to see the use of the term multimorbidity [27].
Fig. 2.
Publication dates of included studies
In this review, 49 studies were conducted locally, 7 studies were regional, and 28 were national. Sample sizes ranged from 45 to nearly 900,000. The majority of the studies used patient records to analyse the prevalence of MLTCs in people from minoritised ethnic groups (n = 69) (Fig. 3). These studies used data from primary care (n = 19), hospital records (n = 14), specialist clinics/services (n = 19) and disease registers (n = 17). Fourteen used cross-sectional survey data (e.g. the General Practice Patient survey, Mental Health and Substance Misuse services survey, and the National tuberculosis surveys) and cohort study data (e.g. the HUSERMET Study, the Yorkshire Health Study, the Southall and Brent Revisited study, the Comorbidity Dual Diagnosis Study (n = 2), the Millennium Cohort Study (n = 2), and UK Biobank (n = 4)) [28–41]. In one study, the authors used Scotland-wide linked education and patient databases [42].
Fig. 3.
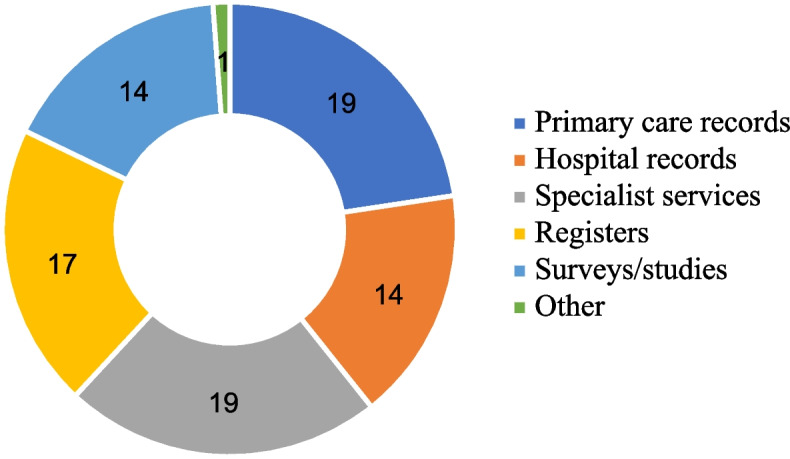
Data Sources used in included studies
Population characteristics
Ethnic group identification
Thirty-eight studies (45%) explicitly reported how ethnicity was identified. Of these, participants self-reported their ethnic identity in 23 studies (27%). One of these studies determined ethnicity based on genealogy [33]. In four studies ethnicity was assigned by interviewers [43], keyworkers [41], researchers, physicians, and nurses [25, 44, 45]. In six studies, ethnicity was both self-reported by participants and clinician assigned [46–51]. Four studies used computerised name recognition programs to identify South Asian people [52–55]. In one study, ethnicity was identified using self-reports, specialist unit ascription, and name recognition software [55].
When ethnicity data could not be identified, some authors attempted to locate the missing information in a variety of ways. One study obtained missing ethnicity data from hospital services and primary care records [56]. Another study imputed the missing participants’ ethnicity from the Census super output area using postcode of residence; where this was an area with ≥ 98% white ethnicity, they assumed the participant was of white ethnicity [55]. The authors in one study relied on the modal ethnicity of patients with the same surname in the Electronic Health Records database where possible [57].
Ethnic group categorisation
In this review, 11 studies grouped participants into six or more ethnic group categories and 12 studies used five broad ethnic group categories. The majority of studies (61 out of 84) grouped participants into four ethnic categories or fewer (Supplementary file 5). Of these studies, 19 studies compared the prevalence of MLTCs between two ethnic groups. Table 1 provides a breakdown of the ethnic groups of interest in these studies. Two studies compared Indian [26] and Punjabi people [58] with white European and English people respectively. The remaining 16 studies used broad ethnic minoritised group categories. The majority (n = 12) compared the prevalence of MLTCs between Asians/South Asians with white/British/Caucasian/European participants [24, 26, 40, 52–54, 58–63]. Three studies focused on people of Black/Afro-Caribbean and white/Caucasian ethnicity [64, 65]. Four studies categorised participants as white/Caucasian or non-white/other [30, 36, 39, 66].
Table 1.
Ethnic groups in studies comparing two ethnic group categories
| Asian/South Asian ethnicity compared with majority white ethnic group | |
|---|---|
| Asian | British [24] |
| Asian | white [59, 60] |
| Asian | Caucasian [61] |
| Indian | European [26] |
| Punjabi | English [58] |
| South Asian | Caucasian [62] |
| South Asian | European [40] |
| South Asian | Europid [63] |
| South Asian | white European [53, 54] |
| South Asian | Non-South Asians [52] |
| Black/African/Caribbean ethnicity compared with majority white group | |
| Afro-Caribbean | Caucasian [65] |
| Black | white [64, 67] |
| Unspecified ethnicity compared with majority white ethnic group | |
| Non-Caucasian | Caucasian [39] |
| Non-white | white [30, 36] |
| Other | white [66] |
In some studies, ethnic categories with small numbers were excluded from the analyses [28, 55, 64, 67–69].
We assessed whether there were changes in how ethnicity was reported over time and we found no discernible pattern. Indeed, studies published in the 80s and 90s used continent/country of origin to ascertain ethnicity [26, 70] or broad ethnic groups such as Asian, Black, Caucasian or British [25, 59, 61]. However, these labels were also observed in more recent studies. Noteworthy is that all the studies that did not specify ethnic group categories and used labels such as non-white, non-Caucasian or other were published between 2016 and 2020 [30, 36, 39, 66]. One study published in 2004 compared white, English-speaking participants self-identifying as English with Asian participants self identifying as Punjabi [58]. They excluded Irish, Scottish or Welsh participants from their analyses as they consider them to be nationally and culturally distinct with different risk profiles from English participants [58].
Missing ethnicity data
The percentage of missing ethnicity data was available in 34 studies and ranged from 0.02% [68] to 65% [69]. Missing ethnicity data was treated in various ways. In some studies, those with missing ethnicity data were excluded from the analyses [27, 33, 70] or reported as ‘unknown’ [44]. In other studies, those of unknown ethnicity were combined with those of other ethnicity [31, 37]. Whilst some studies provided the characteristics of those with unknown ethnicity data alongside other ethnic groups [71–73], only two studies specifically conducted sensitivity analyses to ascertain if there were sociodemographic differences between those with missing and complete ethnicity data and discussed the findings [74, 75].
Age
The participants’ age was reported in 82 studies. There were 75 studies that included participants aged 16 and above. Of these studies, 31 reported a mean age of 40 years and above. Three studies reported a mean age of between 30 and 39 years [35, 43, 76]. Four studies investigated the prevalence of MLTCs in children [38, 39, 42, 77], and two studies included both adults and children [69, 78].
Studies reporting on ethnicity and prevalence of MLTCs (Unspecified Index condition)
Of the 84 studies, nine studies counted the number of long-term conditions where there was no specific index condition. The number of ethnic group categories varied across the studies (Table 2).
Table 2.
Studies reporting MLTCs across ethnic groups with no index condition
| Study ID | Study design | Geographical reach | Data Source | Sample size | Age in years | %Female | Ethnic categories | Covariates adjusted for in analysis of the prevalence of multiple conditions |
|---|---|---|---|---|---|---|---|---|
| Chudasama et al., 2020 [30] | Longitudinal cohort study | National | UK Biobank | 480,940 | Age range: 38–73 | 54 | white, Non-white | none |
| Dorrington et al., 2020 [79] | Longitudinal study | Local | Lambeth Datanet | 326,415 | Age range: 16–60 | 53 | white, Black African, Asian, Black Caribbean, mixed, other, Black other | age, gender, deprivation |
| Fleming et al., 2020 [42] | Retrospective study | National | Scotland-wide databases | 766,244 | Age range: 4–19 | 49 | white, Asian, Black, mixed, other | none |
| Ashworth et al., 2019 [80] | Longitudinal study | Local | Primary care records | 332,353 | Age: ≥ 18 | 50 | white, Black, South Asian, mixed, other | age, gender, deprivation, cardiovascular risk |
| Zemedikun et al., 2018 [29] | Cross-sectional study | National | UK Biobank | 502,643 | Median Age (IQR): 58 (50–63) | 54 | white, mixed, Asian, Black, other | none |
| Hesketh et al., 2016 [38] | Longitudinal study | National | Millennium Cohort Study | 9548 | Age < 18 | 51 | white, mixed, Indian, Pakistani/Bangladeshi, Black, other | Sex, highest level of maternal education, quintiles of household income |
| Li et al.,2016 [36] | Longitudinal study | Local | Yorkshire Health Study | 27,806 | Age range:16–85 | 56 | white, non-white | none |
| Paddison et al., 2015 [32] | Cross-sectional study | National | General Practice Patient Survey | 890,427 | Age: ≥ 18 | 56 | white, mixed, Asian, Black, other | none |
| Mathur et al., 2011 [27] | Cross-sectional study | Local | Primary care records | 99,648 | Age: ≥ 18 | NR | white, South Asian, Black, other | age, sex |
Studies reporting on ethnicity and prevalence of MLTCs (Index condition specified)
The majority of studies reporting MLTCs across ethnic groups specified an index condition (n = 75) (Table 3). Measures of comorbidity were used in five studies; three of which used the Charlson Comorbidity Index [69, 71, 81], one used the Elixhauser Comorbidity score [44], and another used the Stoke comorbidity score [82]. As shown in Table 3, kidney-related conditions (n = 15), diabetes (n = 13), and mental health illnesses (n = 12) were the most frequently studied index conditions. COVID-19 was the index condition in three studies [44, 57, 70].
Table 3.
Studies reporting MLTCs across ethnic groups specifying index condition
| CANCERS | ||||||||||||||||
| Study ID | Study design | Geographical reach | Data Source | Sample size | Age in years | %Female | Ethnic categories | Index condition | Covariates adjusted for in analysis of the prevalence of multiple conditions | |||||||
| Gathani et al., 2020 [81] | Retrospective study | National | National Cancer Registration & Analysis Service data | 164,143 |
Mean Age SD): 59 (11.3) |
100 | white, Indian, Black Caribbean, Pakistani, Black African | Breast cancer | none | |||||||
| Samy et al., 2015 [71] | Retrospective study | National | The National Cancer Data Repository | 24,361 | Age: 83% of sample > 60 | 46 | white, Black, South Asian, other | Myeloma | none | |||||||
| Nimako et al., 2013 [83] | Retrospective study | Local | Specialist services | 423 | Mean Age: 64 | 35 | Western European, Afro-Caribbean, Indian Sub-Continent, South East Asian, other | Lung cancer | none | |||||||
| DIABETES | ||||||||||||||||
| Study ID | Study design | Geographical reach | Data Source | Sample size | Age in years | %Female | Ethnic categories | Index condition | Covariates adjusted for in analysis of the prevalence of multiple conditions | |||||||
| Mathur et al., 2020 [75] | Observational cohort study | National | Clinical Practice Research Datalink | 179,886 |
Age at diagnosis: 62(13) |
45 | white, South Asian, Black, other/mixed | Diabetes | age at diagnosis, sex, deprivation | |||||||
| Mathur et al., 2020b [84] | Observational cohort study | National | Clinical Practice Research Datalink | 162,238 | Age at diagnosis: 62(13) | 45 | white, South Asian, Black | Diabetes | none | |||||||
| Mathur et al., 2018 [85] | Observational cohort study (2006–2016) with nested casecontrol study | local | Primary records | 6274 |
Age range: 25–84 |
56 | white, South Asian, Black | Diabetes | none | |||||||
| Owusu Adjah et al., 2018 [86] | Matched case control | National | The Health Improvement Network | 341,626 | Age: ≥ 18 | 43 | white European, African-Caribbean, South Asia | Diabetes | age, sex | |||||||
| Malavige et al., 2013 [63] | Cross-sectional study | Local | primary care records | 510 | Mean Age(SD): 57(8) | 0 | South Asian, Europid | Diabetes | none | |||||||
| Sivaprasad et al., 2012 [56] | Cross-sectional study | Local | Diabetes register | 50,285 | Mean Age (SD): 62(15) | 47 | white European, African/Afro-Caribbean, South Asian, mixed, other | Diabetes | age, gender, region, type of diabetes | |||||||
| Mehta et al., 2011 [53] | Cross-sectional study | Local | Clinical workstation | 5664 | Mean Age (SD): 60(17) | 46 | South Asian, white European | Diabetes | none | |||||||
| Ali et al., 2009 [54] | Cross-sectional study | Local | The clinical workstation | 6230 | Age: 55% of sample ≥ 60 | 46 | South Asian, white European | Diabetes | age, gender, comorbidities and complications | |||||||
| Fischbacher et al., 2009 [52] | Retrospective study | Local | The Diabetes Audit and Research in Tayside | 9833 | Age:95% of sample > 45 | 47 | South Asian, Non-South Asian | Diabetes | age, sex | |||||||
| Baskar et al., 2006 [87] | Cross-sectional study | Local | Diabetes register | 6047 | Age: ≥ 18 | 46 | African Caribbean, Caucasian, Indo-Asian | Diabetes | age, gender, Duration of diabetes (year), BMI, Type 2 Diabetes, Ever smoked, Systolic Blood Pressure | |||||||
| Earle et al., 2001 [88] | Retrospective case note review | Local | Hospital records | 45 | Mean Age (SD): 66 (8.5) | 36 | Indo-Asian, African-Caribbean, Caucasian | Diabetes | age, gender, blood pressure, baseline proteinuria, antihypertensive treatment and smoking habit | |||||||
| Nagi et al., 1994 [61] | Cross-sectional study | Local | Specialist services | 89 | Age range: 35–70 | 24 | Caucasian, Asian | Diabetes | none | |||||||
| Hawthorne et al., 1990 [24] | Cross-sectional study | Local | diabetes register | 71 | Age: NR | 59 | Asian, British | Diabetes | none | |||||||
| CONDITIONS AFFECTING THE HEART AND BLOOD VESSELS | ||||||||||||||||
| Study ID | Study design | Geographical reach | Data Source | Sample size | Age in years | %Female | Ethnic categories | Index condition | Covariates adjusted for in analysis of the prevalence of multiple conditions | |||||||
| Lawson et al., 2020 [18] | Retrospective study | National | Clinical Practice Research Datalink | 108,638 | Mean Age (SD): 78(12) | 50 | white, South Asian, Black | Heart Failure | none | |||||||
| Gill et al., 2017 [89] | Cross-sectional study | Regional | Primary care records | 551 | Age range: 40–75 | 50 | white British, African Caribbean, South Asian | hypertension status | none | |||||||
| Gorantla et al., 2015 [90] | Retrospective study | Regional | Hospital records | 42,685 | Mean age: 74 | 49 | Caucasian, South Asian, Afro-Caribbean, Oriental, mixed, other | Atrial fibrillation | none | |||||||
| Sosin et al., 2008 [91] | Cross-sectional study | Local | Hospital records | 243 | Age: 34% of sample ≥ 65 | 28 | white European, African Caribbean, South Asian | Heart failure | age, gender, diabetes status, smoking status, or BNP vitamin B12, folate, healthy control status | |||||||
| Patel et al., 2007 [62] | Cross-sectional study | Local | Specialist services | 212 | Mean Age(SD): 61(13) | 33 | South Asian, Caucasian | Chronic Heart Failure | none | |||||||
| Conway et al., 2004 [92] | Retrospective study | Local | Hospital records | 388 | Mean Age (SD): 70(12) | 41 | Indo-Asian, Afro-Caribbean, Caucasian | Peripheral artery disease | age, gender | |||||||
| Blackledge et al., 2003 [73] | Historical cohort study | Local | Hospital records | 5789 | Age: ≥ 40 | 50 | white, South Asian, other | Heart failure | none | |||||||
| Lear et al., 1994 [26] | Retrospective study | Local | Specialist services | 403 | Age range: 33–93 | 35 | Indian, European | Myocardial infarction | none | |||||||
| Lowry et al., 1984 [59] | Retrospective study | Local | Specialist services | 102 | Mean Age (SD):50(8) | 9 | Asian, white | Coronary artery disease | none | |||||||
| CONDITIONS AFFECTING THE KIDNEY | ||||||||||||||||
| Study ID | Study design | Geographical reach | Data Source | Sample size | Age in years | %Female | Ethnic categories | Index condition | Covariates adjusted for in analysis of the prevalence of multiple conditions | |||||||
| Steenkamp et al., 2016 [48] | Retrospective study | National | UK Renal Registry | 7786 | Age: ≥ 18 | NR | white, South Asian, Black, other | Renal disease | none | |||||||
| Hull et al., 2014 [72] | Cross-sectional study | Local | Patient survey | 12,011 | Mean Age: 71 | 57 | white, South Asian, Black, other | Chronic Kidney Disease | none | |||||||
| Cole et al., 2014 [64] | Retrospective study | Local | Specialist services | 1340 | Mean Age (SD): 60(16) | 39 | white, Black | End stage Renal disease | none | |||||||
| Jesky et al., 2013 [93] | Retrospective cohort study | Local | Primary care records | 31,254 | Median age (IQR):59 (50,71) | 49 | white, South Asian, Black | Chronic Kidney Disease | none | |||||||
| Rao et al., 2013 [46] | Retrospective study | National | UK Renal Registry | 6979 | Age: ≥ 18 | NR | white, South Asian, Black, other | Renal disease | none | |||||||
| Udayaraj et al., 2013 [94] | Retrospective study | National | UK Renal Registry | 53,565 | Age: ≥ 18 | 38 | South Asian, Black, white | Renal disease | none | |||||||
| Shaw et al., 2012 [47] | Retrospective study | National | UK Renal Registry | 5783 | Age: ≥ 18 | NR | white, South Asian, Black, other | Renal disease | none | |||||||
| Webb et al., 2011 [50] | Retrospective study | National | UK Renal Registry | 4877 | Age: ≥ 18 | NR | white, South Asian, Black, other | Renal disease | none | |||||||
| Caskey et al., 2010 [49] | Observational study | National | UK Renal Registry | 12,943 | Age: ≥ 18 | NR | white, South Asian, Black, other | Renal disease | none | |||||||
| Roderick et al., 2009 [55] | Prospective cohort | National | Renal Registry | 5901 | Age:82% of sample > 45 | 38 | Caucasian, South Asian, Black | Established Renal failure | age | |||||||
| Jain et al., 2009 [82] | Prospective study | Regional | Hospital records | 755 | Age range: 16–86 | 37 | white, Black, South Asian, other | Renal disease | none | |||||||
| Udayaraj et al., 2009 [51] | Retrospective study | National | UK Renal Registry | 11,399 | Age: ≥ 18 | NR | South Asian, Black, Chinese, other, white | Renal disease | none | |||||||
| Tomson et al., 2007 [45] | Retrospective study | National | UK Renal Registry | 10,579 | Age: ≥ 18 | NR | South Asian, Black, Chinese, other, white | Renal disease | none | |||||||
| Bakewell et al., 2001 [60] | Observational study | Local | Specialist services | 120 | Age: ≥ 18 | 32 | Asian, white | End-stage renal disease | none | |||||||
| Roderick et al., 1996 [25] | Cross-sectional retrospective study | National | Specialist services | 5901 | Age: ≥ 16 | NR | white, Asian, Black | End stage renal disease | none | |||||||
| MENTAL HEALTH CONDITIONS | ||||||||||||||||
| Study ID | Study design | Geographical reach | Data Source | Sample size | Age in years | %Female | Ethnic categories | Index condition | Covariates adjusted for in analysis of the prevalence of multiple conditions | |||||||
| Downs et al., 2017 [77] | Historical cohort study | Local | Clinical Record Interactive Search system | 638 | Age range: 10–17 | 50 | white British, white Other, Black, Asian, Mixed | Psychosis | none | |||||||
| Nicholl et al., 2015 [28] | Cross-sectional study | National | UK Biobank | 144,139 | Mean age (SD): 57(8.1) | 53 | white, Asian, Black | Depression | age, sex, quintiles of Townsend score, smoking status, frequency of alcohol consumption, BMI, morbidity count | |||||||
| Bruce et al., 2012 [76] | Cross-sectional study | Local | Specialist services | 165 | Mean age (SD): 39(10) | 0 | African, Caribbean, white British | Severe mental illness | none | |||||||
| Mazzoncini et al., 2010 [95] | Retrospective study | Local | Specialist services | 511 | Age range: 16–64 | 41 | white British, white other, Black Caribbean, Black African, Asian, other | Psychosis | none | |||||||
| Pinto et al., 2010 [67] | Cross-sectional study | Local | Lambeth DataNet | 903 | Age range: 16–74 | 40 | white, Black | Psychosis | age, gender, obesity and deprivation | |||||||
| Afuwape et al., 2006 [35] | Retrospective cohort study | Local | COMO study | 213 | Mean Age: 37 | 16 | white, Black Caribbean, Black African, Black British | Psychotic illness | age | |||||||
| Bhui et al., 2004 [58] | Cross-sectional study | Local | Primary care records | 389 | Age: ≥ 16.5 | 56 | Punjabi, English | Depression | age, gender, social class, employment, marital status, number of body systems affected by physical illness | |||||||
| Kennedy et al., 2004 [96] | Epidemiologically-based study | Local | Specialist services | 246 | Age: > 16 | 54 | white European, African–Caribbean, African, other | Severe mental illness | none | |||||||
| Miles et al., 2003 [34] | Cross-sectional study | Local | COMO study | 214 |
Age range: 17–77 |
17 | white, Black, other | Psychotic illness | none | |||||||
| McKenzie et al., 2002 [43] | Cross-sectional design | Local | Hospital records | 337 |
Mean Age(SD): 33 (13) |
44 | white, African-Caribbean, Mixed African-Caribbean and white, African, South Asian, Other | Psychosis | age, sex, social class, RDC diagnosis and referral status | |||||||
| Graham et al., 2001 [41] | Cross-sectional study | Local | Mental Health and Substance Misuse services survey | 498 |
Age range: 18–71 |
22 | white UK, African-Caribbean, Asian, European, Irish, mixed, Black other, other | Severe mental illness | none | |||||||
| Weaver et al., 2001 [97] | Cross-sectional study | Local | Specialist services | 851 |
Mean Age(SD): 45(14) |
44 | white UK/European, Black, Irish, Other | Psychotic disorders | age, sex, diagnosis | |||||||
| NEUROLOGICAL CONDITIONS | ||||||||||||||||
| Study ID | Study design | Geographical reach | Data Source | Sample size | Age in years | %Female | Ethnic categories | Index condition | Covariates adjusted for in analysis of the prevalence of multiple conditions | |||||||
| Bhanu et al., 2020 [74] | Retrospective cohort study | National | The Health Improvement Network database | 10,570 | Mean Age: 80 | 64 | white, Asian, Black | Dementia | none | |||||||
| Taylor et al., 2020 [31] | Longitudinal cohort study | National | UK Biobank | 1568 | Age range: 40–69 | 72 | white, BAME, other/unknown | Multiple sclerosis | none | |||||||
| Jordan et al., 2017 [39] | Longitudinal study | National | Millennium Cohort Study | 7224 | Age: < 18 | 49 | Caucasian, Non-Caucasian | Dyslexia | none | |||||||
| Liew et al., 2016 [98] | Retrospective study | Regional | Hospital records | 3275 | Mean Age: 71 | 53 | Caucasian, South Asian, Afro-Caribbean, Oriental, mixed, other | Transient ischemic attack | none | |||||||
| Eastwood et al., 2015 [40] | Longitudinal study | Local | The SABRE study | 4196 | Age range: 45–58 | 0 | South Asian, European | Stroke | age, smoking status, waist/hip ratio, total/HDL-cholesterol ratio, diabetes mellitus, fasting glucose, physical activity, heart rate | |||||||
| Potluri et al., 2015 [99] | Retrospective study | Regional | Hospital records | 17,415 | Mean Age: 74 | 50 | Caucasian, South Asian, Afro-Caribbean, Oriental, mixed, other | Ischaemic stroke | none | |||||||
| Sarker et al., 2008 [100] | Prospective study | Local | The South London Stroke Register | 566 | Mean Age(SD): 62(17) | 46 | white, Black, other/missing | Haemorrhagic stroke | none | |||||||
| Patel et al., 2001 [101] | Prospective study | Local | South London Stroke Register | 235 | Mean Age(SD): 71(14) | 51 | white, Black, other | Stroke | none | |||||||
| RESPIRATORY CONDITIONS | ||||||||||||||||
| Study ID | Study design | Geographical reach | Data Source | Sample size | Age in years | %Female | Ethnic categories | Index condition | Covariates adjusted for in analysis of the prevalence of multiple conditions | |||||||
| Sapey et al., 2020 [57] | Observational cohort study | Local | Hospital records | 2217 | Median Age(IQR): 73(58–84) | 42 | white, mixed, South Asian/South Asian British, Black/African/Caribbean/Black British, other | COVID-19 infection | none | |||||||
| Zakeri et al., 2020 [70] | Cohort observational study | local | Lambeth DataNet | 872 | Age: ≥ 18 | 44 | Black, white, mixed/other, Asian | COVID-19 infection | none | |||||||
| Perez-Guzman et al., 2020 [44] | Retrospective study | Local | Hospital records | 559 | Median Age(IQR): 69(25) | 38 | white, Black, Asian, other | SARS-CoV-2 infection | none | |||||||
| Marshall et al., 1999 [102] | Retrospective study | Local | Specialist services | 157 | Age:94% of sample > 20 | 34 | European, African, Asian, Americans | Tuberculosis | none | |||||||
| OTHER HEALTH CONDITIONS | ||||||||||||||||
| Study ID | Study design | Geographical reach | Data Source | Sample size | Age in years | %Female | Ethnic categories | Index condition | Covariates adjusted for in analysis of the prevalence of multiple conditions | |||||||
| Ali et al., 2020 [103] | Observational study | Regional | Specialist services | 313 | Mean Age(SD): 52(11) | 25 | Asian/Asian British, white, Black/African/Caribbean/Black British, mixed, other ethnic group | Hepatitis C infection | none | |||||||
| Eendebak et al., 2017 [33] | Cross-sectional observational study | Local | HUSERMET Study | 642 | Age range: 40–48 | 0% | South Asian, white European, African Caribbean | Reproductive hormone levels | none | |||||||
| Misra et al., 2016 [69] | Retrospective cohort study | National | Hospital records | 71,966 | Age range:2–104 | 52 | White European, Indian, Pakistani, Bangladeshi, Black, Chinese, | Ulcerative colitis | none | |||||||
| Patel et al., 2016 [66] | Cross-sectional observational study | Local | Specialist services | 299 | Mean Age(SD): 58(2) | 5 | white, other | HIV | none | |||||||
| Nisar et al., 2015 [104] | Retrospective study | Local | Specialist services | 299 | Mean Age at start of therapy:51 | 64 | Caucasian, Asian, Afro-Caribbean, Mixed | Inflammatory arthritis | none | |||||||
| Chackayil et al., 2013 [105] | Retrospective, cross-sectional study | Regional | Hospital records | 3563 | Age: NR | 59 | white, South Asian, African Caribbean | Iron deficiency Anaemia | none | |||||||
| Kitley et al., 2012 [65] | Retrospective study | Local | Specialist services | 106 | Mean Age at onset:41 | 87 | Caucasian, Afro-Caribbean, Japanese | Neuromyelitis optical | none | |||||||
| Mann et al., 2008 [106] | Retrospective | National | Hospital records | 40,488 | Mean Age(SD): 42(13) | 39 | white, Black African, Black Caribbean, Pakistani, Bangladeshi, Other, Mixed, Indian, Chinese | Hepatitis C | age, sex, year | |||||||
| Mohsen et al., 2005 [68] | Cross-sectional design | Local | Specialist services | 1017 | Median age at presentation(IQR):32.6(29–38) | 35 | white, Black African, Black Caribbean, Black Other, South Asian, Other, Oriental | HIV | gender, HIV risk group, Place of birth, History of Injecting Drug Use, Blood factor | |||||||
| Dragovic et al., 2002 [78] | Retrospective study | Local | Specialist services | 153 | Age: 97% aged ≥ 17 | 19.6 | white, Black Caribbean, Black African, | Gonococcal infection | age, sex | |||||||
| Rose et al., 2002 [37] | Retrospective study | National | National TB survey database & HIV/AIDS patient database | 3432 | Age range: 16–54 | 45 | white, Black African, Indian sub-continent, other/unknown | HIV | year, sex, geographical area | |||||||
Prevalence of multiple long-term conditions by ethnic group
Seven studies provided evidence on ethnicity and age-adjusted prevalence of multiple conditions amongst people living in the UK (Table 4). Of these, three were studies of MLTCs with no specified index condition [27, 79, 80]. All seven studies were appraised and were considered to be of high methodological quality (Table 4, Supplementary file 4). In all studies, the authors clearly specified the study designs which we deemed to be appropriate to address the aims and objectives of the research. There was a clear description of the methods of analysis and the process by which the results were produced. In addition, the interpretations and conclusions of the authors were supported by the data they presented. The findings of these studies suggest that people from minoritised ethnic groups have a higher prevalence of MLTCs when compared to people from the majority white group [27, 79, 80]. All were local studies that used patient records in their analyses. All adjusted for age and gender/sex, with two studies also adjusting for deprivation [79, 80] and one also adjusting for cardiovascular risk factors [80]. Mathur and colleagues investigated the cardiovascular multimorbidity by ethnicity in a socially deprived and multi-ethnic population in east London [27]. Their focus was on five health conditions: coronary heart disease, diabetes, heart failure, stroke, and hypertension across four ethnic groups. After adjusting for age and sex, and clustering by general practice, minoritised ethnic group people were more likely to have MLTCs than white people with adjusted odds ratios (OR) of 2.4 (95% Confidence interval (CI): 1.94–2.15) for South Asian people and 1.23 (95% CI: 1.18–1.29) for Black people [27].
Table 4.
Studies reporting adjusted prevalence of MLTCs multiple conditions across ethnic groups
| Study ID | Region | Data Source | Sample size | No. of Ethnic Categories | No. of conditions | Types of conditions | Index condition | Covariates |
Effect measure ORs/Prevalence and 95% CI Reference: White Ethnicity |
Overall Study Quality |
|---|---|---|---|---|---|---|---|---|---|---|
| Dorrington et al., 2020 [79] | Local | Lambeth Datanet | 326,415 | Asian, Black African, Black Caribbean, Black other, mixed, other, white | 13 | Epilepsy, Chronic Pain, Depression, Vascular, Cancer, Cardiac Disease, Rheumatoid Arthritis, Severe Mental Illness, Hypertension, Diabetes, Obesity, Respiratory Disease, Learning Disability | - | age, gender, deprivation |
Black African: 1.92 (1.75–2.10) Black Caribbean: 2.83 (2.56–3.14) Mixed: 1.50 (1.31–1.72) Black Other: 2.22 (1.87–2.64) |
High |
| Mathur et al., 2020 [84] | National | CPRD data | 179,886 | Black, South Asian, white | 8 | Diabetes, Hypertension, Coronary Heart Disease (Angina/Myocardial Infarction), Heart Failure, Chronic Kidney Disease, Retinopathy, Neuropathy | Diabetes | age, sex, deprivation |
South Asian: 0.88 (0.80–0.96) Black: 0.50 (0.43–0.58) |
High |
| Ashworth et al., 2019 [80] | Local | Primary care records | 332,353 | Black, mixed,other, South Asian, white | 12 | Atrial Fibrillation, Chronic Obstructive Pulmonary Disease, Chronic Pain, Chronic Kidney Disease, Coronary Heart Disease, Diabetes Mellitus, Dementia, Depression, Heart Failure, Serious Mental Illness, Stroke, Morbid Obesity | - | age, gender, deprivation, cardiovascular risk |
South Asian: 1.44 (1.29–1.61) Black: 0.86 (0.80–0.92) |
High |
| Owusu Adjah et al., 2018 [86] | National | THIN data | 341,626 | African-Caribbean, South Asian, Western European | 5 | Diabetes, Myocardial Infarction, Heart Failure, Stroke, Cancer | Diabetes | age, sex |
Normal BMI W. Europeans: 10.4% (9.5, 11.3) South Asians: 6.8% (4.8, 9.5) African-Caribbeans: 6.4% (4.0, 10.4) |
High |
| Mathur et al., 2011 [27] | Local | Primary care records | 99,648 | Black, other, South Asian, white | 5 | Hypertension, Ischaemic Heart Disease, Heart Failure, Stroke, And Diabetes | - | age, sex |
South Asian: 2.4 (1.94–2.15) Black: 1.23 (1.18–1.29) |
High |
| Roderick et al., 2009 [55] | National | UK Renal Registry data | 5901 | Black, South Asian, Caucasian | 8 | Established Renal Failure, Coronary Heart Disease, Diabetes, Any Vascular Disease, Chronic Obstructive Pulmonary Disease, Smoking, Any Malignancy, Chronic Liver Disease | Established Renal Failure | age |
South Asian: 1.26 (1.04–1.52) Black: 0.70 (0.52–0.95) |
High |
| Baskar et al., 2006 [87] | Local | Diabetes Register | 6047 | Afro-Caribbean, Caucasian, Indo-Asian | 6 | Diabetes, Retinopathy, Dipstick Proteinuria, Ischaemic Heart Disease, Cerebrovascular Disease, Peripheral Vascular Disease | Diabetes | age, gender, diabetes complication risk factors |
Microvascular complications: Afro-Caribbean: 1.29 (1.06–1.57) Macrovascular complication: Afro-Caribbean: 0.71(0.51–0.87) Indo-Asian: 0.81 (0.67–0.93) |
High |
OR Odds Ratio, CI Confidence Interval, THIN The Health Improvement Network, CPRD Clinical Practice Research Datalink
Ashworth and colleagues examined the social determinants and cardiovascular risk factors for multimorbidity and the acquisition sequence of multimorbidity [80]. Their focus was on 12 conditions across five ethnic groups. Age-sex adjusted estimates were not provided but they found that compared to white people, Black and South Asian people had higher odds of multimorbidity after adjusting for age, gender, and area level deprivation (OR 1.15 (95% CI: 1.07–1.23) and 1.19 (95% CI: 1.07–1.33) respectively). However, when hypertension, obesity, and smoking status were added to the model, only South Asian people had higher odds of multimorbidity (1.44 [95% CI: 1.29–1.61]), but not Black people (0.86 [95% CI: 0.80–0.92]) [80].
Dorrington and colleagues assessed 13 conditions across seven ethnic groups. Age-sex adjusted estimates were not provided [79]. Age, gender and area-level deprivation adjusted models showed that the odds of having two or more long-term conditions were higher in some minoritised ethnic groups; 1.92 (95% CI: 1.75–2.10) for Black African people, 2.83 (95% CI: 2.56–3.14) for Black Caribbean people, 1.50 (95% CI: 1.31–1.72) for people with mixed ethnicity and 2.22 (95% CI: 1.87–2.64) for people who self identified as Black other. When three or more long-term conditions were considered, the same minoritised ethnic group populations still had higher odds of multimorbidity than the white population (OR 3.42 [95% CI:3.05–3.83] for Black Caribbean people, 2.53 [95%CI: 2.02–3.18] for Black other people, 1.95 [95% CI 1.74–2.20] for Black African people and 1.50 [95% CI: 1.30–1.73] for people with mixed ethnicity) [79]. In the remaining four studies, an index condition was specified [55, 75, 86, 87]. Two studies, one which focused on people starting renal replacement therapy, and the other which focused on people with diabetes, reported a higher prevalence of MLTCs in people from some minoritised ethnic groups [89, 48]. The other two studies which focused on people with diabetes, reported lower prevalence of MLTCs among minoritised people [75, 86]. Three out of these four studies used national data [55, 75, 86]. All used patient records to assess MLTCs across three ethnic group categories: Black/African-Caribbean, South Asian/Indo-Asian and white ethnicity. All four studies adjusted for age, three studies additionally adjusted for sex [75, 86, 87]. One study additionally adjusted for area-level deprivation [75] and another for diabetes complication risk factors [87].
In their study exploring the survival of patients starting renal replacement therapy across three ethnic groups, Roderick and colleagues found that compared to white patients, the age-adjusted prevalence of vascular comorbidity was higher in South Asian patients but lower in Black patients [odds ratios of 1.26 (95% CI:1.04–1.52) and 0.70 (95% CI:0.52–0.95) respectively]. However, other comorbidities were found to be generally more common in white patients [55]. Baskar and colleagues evaluated ethnic differences in the prevalence of hypertension and vascular complications in a population with diabetes [87]. They considered microvascular complications to be the documented presence of any grade of retinopathy and/or dipstick proteinuria [87]. Macrovascular complications were considered to be the documented presence of ischaemic heart disease and/or cerebrovascular disease, and/or peripheral vascular disease [87]. Age-adjusted estimates were not provided. After adjusting for age, gender, BMI, systolic blood pressure, smoking, type 2 diabetes, and duration of diabetes, Afro-Caribbean people had a higher risk of microvascular complications (odds ratios of 1.293 (95% CI: 1.063–1.573) relative to white people). However, compared to white people, both Afro-Caribbean and Indo-Asian people had significantly lower risk of macrovascular complications with odds ratios of 0.710 (95% CI: 0.581–0.866) and 0.807 (95% CI: 0.669–0.933) respectively [87].
Owusu-Adjah and colleagues examined ethnic differences in comorbidities in patients with type 2 diabetes mellitus [86]. They found that Western European patients had significantly higher baseline age-sex adjusted prevalence of cardiovascular complications compared to South Asian patients (at all levels of BMI) and African-Caribbean patients (in overweight or obese groups only). Western Europeans also had significantly higher baseline prevalence of cancer and depression [86]. Mathur and colleagues investigated ethnic differences in the severity and clinical management of type 2 diabetes at initial diagnosis. Age-adjusted estimates were not provided. Adjusting for age, sex and deprivation, and clustering by practice, the odds of having comorbid macrovascular disease (i.e. hypertension, coronary heart disease (including myocardial infarction and angina), stroke, and heart failure) at diagnosis were reduced in South Asian people (0.88, 95%CI 0.80–0.96) and halved in Black people (0.50, 95%CI 0.43–0.58) relative to white people. However, they found no ethnic differences in the odds of having diagnosed microvascular disease (i.e. chronic kidney disease, retinopathy, and neuropathy) in their sample [75].
Discussion
We identified seven studies that give insight into age-adjusted ethnic differences in the prevalence of MLTCs. The findings are indicative of ethnic inequalities in MLTCs in favour of the majority white as five of the seven studies reported that some minoritised ethnic groups have a higher prevalence of MLTCs than their white counterparts. The evidence suggests that South Asian people (three out of five studies) and Black people (two out of five studies) may be at a higher risk of MLTCs [27, 55, 79, 80, 87]. Whilst some studies adjusted for factors that may be on the explanatory pathway, including deprivation and risk factors for cardiovascular disease and diabetes complications, all studies adjusted for at least age in their analyses. As such, the evidence of ethnic inequalities in MLTCs is based on studies that considered this key confounder [2]. However, given the variation in the number and types of conditions examined in these studies and the merging of different minoritised ethnic groups, this evidence may not accurately reflect the true level of inequality.
The two studies that reported a lower prevalence of MLTCs in minoritised ethnic groups are recent studies which focused on people living with diabetes. This finding is intriguing and warrants further attention. In trying to understand these observations, we cannot rule out errors with measurement of ethnicity and data quality. We must also consider that Black and South Asian people in the UK not only have a higher prevalence of diabetes, but they also develop the condition at an earlier age [84, 107]. It is, therefore, possible that the minoritised populations included in these studies are younger than their white counterparts. Since MLTCs increase with age, the lower prevalence of MLTCs among minoritised ethnic groups observed in these studies could result from residual confounding by age. Otherwise put, there may be persistent differences in age among minoritised ethnic group people and white people even after controlling for age. Also, given that minoritised ethnic groups have a higher risk of developing diabetes, much effort might be paid to the identification and management of diabetes in this population. Mathur and colleagues, who examined the ethnic variations in the severity and management of diabetes at first diagnosis, provide support for this notion [75]. They found that when compared to white people, Black and South Asian people had better capture of risk factors, better/similar cardio-metabolic profile at diagnosis, faster initiation of anti-diabetic treatment, first National Health Service (NHS) health check and structured education [75]. These outcomes may prevent further health problems, thereby, contributing to a lower prevalence of MLTCs in minoritised people with diabetes. However, other studies report ethnic inequalities in diabetes care with Black and Asian people found to have worse glycaemic control and being less likely to be prescribed newer therapies [108]. Inequalities in diabetes care can result in higher rates of complications [108] which can increase the likelihood of MLTCs. Future work is, therefore, required to explore these findings further.
Proposed mechanisms underlying observed inequalities
Given that few studies have assessed the prevalence of MLTCs across ethnic groups, it is difficult to ascertain the reasons behind the observed ethnic inequalities in the prevalence of MLTCs in the UK. However, based on longstanding international evidence on ethnic inequalities in single conditions, we propose a number of mechanisms. We consider the impact of racism and discrimination in explaining the observed ethnic differences in the prevalence of MLTCs as they are known to influence health [109]. It is possible that racism and multiple forms of discrimination can intersect with demographic factors (e.g. age, gender, and/or sexual orientation) resulting in disadvantage in accessing key economic, physical and social resources for some, thereby, leading to socioeconomic and health inequalities [110–112]. In turn, these inequalities can result in higher prevalence of some health conditions which may then accelerate the development of MLTCs in some minoritised ethnic group populations. Racism and multiple forms of discrimination can also lead to ethnic inequalities in healthcare access, utilisation and care quality [113] through a number of pathways. For example, findings from international studies suggest that negative discriminatory practices can result in mistrust of healthcare professionals, non-compliance with treatment, delayed diagnoses and treatment and even forgone healthcare [114–116]. These outcomes are detrimental as they not only exacerbate existing health inequalities, but they can also lead to the development and/or progression of MLTCs. However, these processes have received very little investigation in the context of ethnic inequalities in the prevalence of MLTCs in the UK.
Quality of studies contributing to ethnic inequalities in MLTCs
We assessed the quality of the seven studies which contributed to the evidence on ethnic inequalities in the prevalence of MLTCs and considered the studies to be of high quality. Whilst the studies were methodologically sound, we identified limitations which potentially impede a full understanding of ethnic inequalities in the prevalence of MLTCs. For example, in one study, ethnicity, deprivation, and socially-patterned risk factors were considered in isolation [80]. Relatedly, some authors presented only fully adjusted estimates [79, 87] which doesn’t allow for the assessment of the impact of key variables on the prevalence of MLTCs. We noted the use of broad ethnic categories, patient records and a general lack a sensitivity analysis to assess the characteristics of those with and without complete ethnicity data. We discuss these limitations and their implications for understanding ethnic inequalities in MLTCs in the following section.
Broad ethnic group categories
In the seven studies that contributed to the evidence of ethnic inequalities in the prevalence of MLTCs, people from minoritised ethnic groups were often grouped into broad categories; in particular, Black/African-Caribbean, South Asian/Asian/Indo-Asian, mixed, and other. In one study, the Black ethnic group was disaggregated into three different categories, but the authors did not adopt this approach for the Asian ethnic group [79]. Categorising minoritised ethnic group people into overarching categories can be useful for identifying broad patterns as some may have shared experiences of racism, discrimination, and/or social exclusion [35]. However, the use of broad ethnic categories may obscure the extent of inequalities. For example, as reported above, South Asian people may be at particular risk of MLTCs [27, 55, 80] but studies have shown that Pakistani and Bangladeshi women report higher levels of limiting long-term illness than Indian women [9]. Yet, they are often grouped together as people of South Asian ethnicity. This issue also applies to the white other ethnic group [43] who are a diverse population with particular groups, e.g. Gypsy, Roma, and Traveller community [9, 117].
Missing ethnicity data
The availability of complete ethnicity data is crucial for studies that seek to assess ethnic inequalities not only in relation to MLTCs, but also in relation to healthcare utilisation and care [118]. Information about the different ways in which authors handled missing ethnicity data was available in all but one of the seven studies that contributed to the evidence of ethnic inequalities in the prevalence of multiple conditions [79]. Amongst these studies, people with missing ethnicity data were excluded from analyses in three studies [27, 86, 87]. In one study, the authors used the patients’ postcode and census data to determine ethnicity [55] and in another, those with unknown ethnicity were also included in the analysis [80]. Of note is that the authors of only one study compared the sociodemographic characteristics of individuals of with missing and completed ethnicity data [75]. Researchers should carefully consider the most appropriate approach to dealing with missing data and check alternative approaches using sensitivity analysis because policies based on inaccurate data may result in poor targeting of resources and services [118].
Sources of data
All seven studies analysed data from patient records. For individuals to be included in patient records, they need to be in contact with healthcare services. It has been reported that access to primary care health services is generally equitable for people from minoritised ethnic groups [119]. However, they are less likely to access other specialist services [119, 120]. Therefore, those who do not access these services or for that matter, those who do not use healthcare services at all, are excluded from analyses that employ patient records. This differential access may lead to underestimation of inequalities. It is also important to consider ethnic inequalities in care quality as studies suggest that there may be differences in how patient symptoms are recorded, diagnosed or treated [121]. Other studies have not only found data quality problems when ethnicity data is recorded in hospital records (e.g. incomplete coding, inconsistent use of codes, systematic biases), but also that these data quality issues disproportionately affect hospital records for minoritised patients [122]. Consequently, the health conditions in some minoritised people may be underreported when patient records are used in analyses, thereby, impacting on the prevalence estimates of MLTCs and impeding our understanding of ethnic inequalities.
Strengths and limitations
In presenting the state of the evidence, this review has highlighted the inconsistent ways in which MLTCs are defined and measured with the number of long-term conditions varying between studies. This lack of consensus in how MLTCs are captured has been raised by authors of other reviews of prevalence of MLTCs in the general population [123, 124]. They argue that the operational definition of multimorbidity may impact prevalence estimates and call for the standardisation of the definition and assessment of multimorbidity so as to better understand the phenomenon [123, 124]. The review has also highlighted the limitations of the studies in this area. First, many did not provide age-adjusted prevalence estimates of MLTCs. Second, not only were broad ethnic groupings used in several studies, but there were inconsistent definitions of ethnic groups. In addition, in many of these studies ethnic groups with small sample sizes and people with missing ethnicity data were often excluded from analyses. Relatedly, information on sensitivity analysis of missing ethnicity data was generally lacking. Finally, in 18% of the studies, ethnicity was assigned by practitioners, clinicians, or researchers via a combination of name recognition software and genealogy. These modes of assigning ethnicity are problematic primarily because it may be incongruent with the ways in which individuals choose to identify themselves [125]. We, therefore, have an incomplete picture of ethnic inequalities across ethnic group populations in the UK. Nonetheless, the review provides evidence of the existence of ethnic inequalities in the prevalence of multimorbidity and cardiovascular multimorbidity [27, 79, 80] prior to the COVID-19 pandemic. Studies are needed to ascertain the extent to which these inequalities have been exacerbated during the COVID19 pandemic and beyond.
A limitation of this review is that a single reviewer initially screened the titles and abstracts, and excluded irrelevant studies given the large number of studies retrieved. It is possible that some studies may have been inadvertently excluded. However, we manually searched the reference lists of key studies and relevant systematic reviews, thereby, reducing the likelihood of missing relevant studies. A strength of the review is that we conformed to the PRISMA guidelines to help transparently report the review process [23, 126] (Supplementary file 6). We also conducted the electronic search across a range of databases to identify published and unpublished studies. Not only did we assess the methodological quality, but we also assessed the relevance of the studies for understanding ethnic inequalities in the prevalence of MLTCs. Relatedly, when synthesising the results of studies that contributed to the evidence of ethnic inequalities in the prevalence of MLTCs, we only included studies that adjusted for at least age because the risk of acquiring multiple health conditions increases with age [127]. In doing so, we reduced the likelihood of presenting results that are misleading. In this review, we included studies published up until 2020 and identified three studies where COVID19 was the index condition. Whilst we do not consider COVID19 a long-term condition to be captured by definitions of multimorbidity [1, 3], we acknowledge that the pandemic has exacerbated ethnic inequalities in healthcare [128]. Our decision to focus mainly on studies published before 2020 ensures that the review sets a benchmark and provides an overview of studies that examined ethnic inequalities in the prevalence of MLTCs prior to the pandemic.
Conclusions
In this review, we have presented the state of the evidence on ethnic inequalities in the prevalence of MLTCs in the UK prior to the COVID19 pandemic. We have identified and described the literature in this area and in doing so, illuminated the scope of work required to enhance future analyses of ethnic inequalities in people with MLTCs. With the exception of two studies that focused on diabetes, the studies identified point to the existence of ethnic inequalities in the prevalence of MLTCs. These studies also suggest that Indian, Pakistani, Bangladeshi, Black African, Black Caribbean, and people who identify as Black other, other Asian, and mixed may be at higher risk of MLTCs. Our assessment of the conceptualisation and operationalisation of ethnicity has revealed that the majority of these studies used broad ethnic categories in their analyses. They also focused on different health conditions. Further, they drew on patient records, thereby, excluding those who are not in contact with healthcare services. Thus, the results provide a partial picture of ethnic inequalities in the prevalence of multiple conditions.
Future recommendations
The COVID19 pandemic has not only exposed structural inequalities in our society but it has also exacerbated them, especially among minoritised ethnic group people [129]. Therefore, reviews that explicitly examine the impact of the COVID19 pandemic on health(care) and quality outcomes are required to better understand the ways in which ethnic inequalities have been exacerbated and to identify potential solutions. Given the complexity of multiple conditions, the diversity of the minoritised ethnic group populations in the UK, and the varied pathways through which they come to develop MLTCs, future studies would benefit from conceptualising and analysing the prevalence of ethnic inequalities through an intersectional lens. This work could shed light on the extent to which key explanatory pathways, including racism and discrimination, play a role in the development of MLTCs in different ethnic group populations. It is findings of analyses such as these that could help to inform strategies to reduce ethnic inequalities in the prevalence of MLTCs.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- ASSIA
Applied Social Sciences Index and Abstracts
- BAME
Black Asian and Minority Ethnic
- BME
Black and Minority Ethnic
- BMI
Body Mass Index
- CI
Confidence Interval
- COVID-19
Coronavirus Disease 2019
- CPRD
Clinical Practice Research Datalink
- EMBASE
Excerpta Medica data base
- MLTCs
Multiple long-term conditions
- NHS
National Health Service
- OR
Odds Ratios
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- THIN
The Health Improvement Network
- UK
United Kingdom
Authors’ contributions
LB and MS devised the primary research goals and objectives of this systematic review. LB MS, and BH planned the methodological approach and developed the protocol. BH formulated the search terms together with LB and MS. BH performed the search, imported the identified studies and eliminated duplicate studies. BH and LB screened and extracted data from a random sample of studies (10%). BH screened and extracted data from the remaining studies (90%). BH, MS and LB appraised the quality of the studies that contribute to evidence of ethnic inequalities in the prevalence of MLTCs. BH narratively synthesised the findings with extensive methodological and intellectual feedback from LB and MS. BH prepared the manuscript and wrote the initial draft. LB and MS critically reviewed and commented on the initial and subsequent drafts. When reviewing the manuscripts, both LB and MS verified the data from the studies that contributed to the evidence of ethnic inequalities in the prevalence MLTCs. All authors had full access to the included studies. BH submitted the manuscript for publication. All authors have read and agreed to the published version of the manuscript.
Funding
This work is funded by The Health Foundation (AIMS 1874695).
Availability of data and materials
The data extracted from the included studies are publicly available.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
MS is employed by The Health Foundation. The authors have no competing interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Brenda Hayanga, Email: brenda.hayanga@kcl.ac.uk.
Mai Stafford, Email: mai.stafford@health.org.uk.
Laia Bécares, Email: laia.becares@kcl.ac.uk.
References
- 1.Long MJ, Conditions T. Briefing Paper. London: Race Equality Foundation; 2021. [Google Scholar]
- 2.Stafford M, Steventon A, Thorlby R, Fisher R, Turton C, Deeny S. Briefing: Understanding the health care needs of people with multiple health conditions [Online]. 2018. Available from https://www.health.org.uk/sites/default/files/upload/publications/2018/Understanding%20the%20health%20care%20needs%20of%20people%20with%20multiple%20health%20conditions.pdf. Accessed 2 June 2021.
- 3.Head A, Fleming K, Kypridemos C, Pearson-Stuttard J, O’Flaherty M. Multimorbidity: the case for prevention. J Epidemiol Community Health. 2021;75:242–244. doi: 10.1136/jech-2020-214301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multi- morbidity and implications for health care, research and medical education: a cross- sectional study. The Lancet online. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 5.Kingston A, Robinson L, Booth H, Knapp M, Jagger C. Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing. 2018;47(3):374–380. doi: 10.1093/ageing/afx201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moffat K, Mercer SW. Challenges of managing people with multimorbidity in today’s healthcare systems. BMC Fam Pract. 2015;16(1):129. doi: 10.1186/s12875-015-0344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verest W, Galenkamp H, Spek B, Snijder MB, Stronks K, van Valkengoed IGM. Do ethnic inequalities in multimorbidity reflect ethnic differences in socioeconomic status? The HELIUS study. Eur J Public Health. 2019;29(4):687–693. doi: 10.1093/eurpub/ckz012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guy’s and St Thomas’ Charity. From one to many. Exploring people’s progression to multiple long-term conditions in an urban environment [Online]. 2018. Available from https://www.gsttcharity.org.uk/sites/default/files/GSTTC_MLTC_Report_2018.pdf. Accessed 16 May 2021.
- 9.Bécares L. Which ethnic groups have the poorest health? In: Jivraj A, Simpson L, editors. Ethnic Identity and Inequality in Britain The Dynamics of Diversity. Bristol: Policy Press; 2015.
- 10.Nazroo JY. Ethnicity, Class and Health. London: Policy Studies Institute; 2001. [Google Scholar]
- 11.Nazroo JY. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. Am J Public Health. 2003;93(2):277–84. doi: 10.2105/ajph.93.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carrà G, Johnson S. Variations in rates of comorbid substance use in psychosis between mental health settings and geographical areas in the UK. a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2009;44(6):429–47. doi: 10.1007/s00127-008-0458-2. [DOI] [PubMed] [Google Scholar]
- 13.Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28(5):516–523. doi: 10.1093/fampra/cmr013. [DOI] [PubMed] [Google Scholar]
- 14.Toleikyte L, Salway S. Local action on health inequalities. Understanding and reducing ethnic inequalities in health [Online]. 2018. Available from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/730917/local_action_on_health_inequalities.pdf. Accessed 30 Sept 2022.
- 15.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Institute for Health and Care Excellence. Multimorbidity [Online]. 2018. Available from https://cks.nice.org.uk/topics/multimorbidity/. Accessed 2 June 2021.
- 17.Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chronic Dis. 1970;23(7):455–468. doi: 10.1016/0021-9681(70)90054-8. [DOI] [PubMed] [Google Scholar]
- 18.Lawson CA, Zaccardi F, Squire I, Okhai H, Davies M, Huang W, et al. Risk factors for heart failure: 20-year population-based trends by sex, socioeconomic status, and ethnicity. Circ Heart Fail. 2020;13(2):e006472. doi: 10.1161/CIRCHEARTFAILURE.119.006472. [DOI] [PubMed] [Google Scholar]
- 19.Cassell A, Edwards D, Harshfield A, Rhodes K, Brimicombe J, Payne R, et al. The epidemiology of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2018;68(669):e245–e251. doi: 10.3399/bjgp18X695465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harrison C, Britt H, Miller G, Henderson J. Examining different measures of multimorbidity, using a large prospective cross-sectional study in Australian general practice. BMJ Open. 2014;4(7):e004694. doi: 10.1136/bmjopen-2013-004694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35. doi: 10.1186/1471-2288-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dawson E. Equity, Exclusion and Everyday Science Learning: The Experiences of Minoritised Groups. Abingdon, UK: Routledge; 2019. [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hawthorne K. Asian diabetics attending a British hospital clinic: a pilot study to evaluate their care. Br J Gen Pract. 1990;40:243–247. [PMC free article] [PubMed] [Google Scholar]
- 25.Roderick PJ, Raleigh VS, Hallam L, Mallick NP. The need and demand for renal replacement therapy in ethnic minorities in England. J Epidemiol Community Health. 1996;50(3):334–339. doi: 10.1136/jech.50.3.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lear JT, Lawrence IG, Pohl JEF, Burden AC. Myocardial infarction and thrombolysis: a comparison of the Indian and European populations on a coronary care unit. J R Coll Physicians Lond. 1994;228(2):143–147. [PMC free article] [PubMed] [Google Scholar]
- 27.Mathur R, Hull SA, Badrick E, Robson J. Cardiovascular multimorbidity: the effect of ethnicity on prevalence and risk factor management. Br J Gen Pract. 2011;61(586):e262–e270. doi: 10.3399/bjgp11X572454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nicholl BI, Smith DJ, Cullen B, Mackay D, Evans J, Anderson J, et al. Ethnic differences in the association between depression and chronic pain: cross sectional results from UK Biobank. BMC Fam Pract. 2015;16:128. doi: 10.1186/s12875-015-0343-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zemedikun DT, Gray LJ, Khunti K, Davies MJ, Dhalwani NN. Patterns of multimorbidity in middle-aged and older adults: an analysis of the UK biobank data. Mayo Clin Proc. 2018;93(7):857–866. doi: 10.1016/j.mayocp.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 30.Chudasama YV, Khunti K, Gillies CL, Dhalwani NN, Davies MJ, Yates T, et al. Healthy lifestyle and life expectancy in people with multimorbidity in the UK Biobank: a longitudinal cohort study. PLoS Med. 2020;17(9):e1003332. doi: 10.1371/journal.pmed.1003332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taylor TR, Jacobs BM, Giovannoni G, Petrushkin H, Dobson R. Prevalence and demographics of multiple sclerosis-associated uveitis: a UK biobank study. Mult Scler Relat Disord. 2020;43:102209. doi: 10.1016/j.msard.2020.102209. [DOI] [PubMed] [Google Scholar]
- 32.Paddison CA, Saunders CL, Abel GA, Payne RA, Campbell JL, Roland M. Why do patients with multimorbidity in England report worse experiences in primary care? evidence from the general practice patient survey. BMJ Open. 2015;5(3):e006172. doi: 10.1136/bmjopen-2014-006172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eendebak RJ, Swiecicka A, Gromski PS, Pye SR, O'Neill TW, Marshall A, et al. Ethnic differences in male reproductive hormones and relationships with adiposity and insulin resistance in older men. Clin Endocrinol (Oxf) 2017;86(5):660–668. doi: 10.1111/cen.13305. [DOI] [PubMed] [Google Scholar]
- 34.Miles H, Johnson S, Amponsah-Afuwape S, Finch E, Leese M, Thornicroft G. Characteristics of subgroups of individuals with psychotic illness and a comorbid substance use disorder. Psychiatric Serv. 2003;54(4):554–561. doi: 10.1176/appi.ps.54.4.554. [DOI] [PubMed] [Google Scholar]
- 35.Afuwape SA, Johnson S, Craig TJK, Miles H, Leese M, Mohan R, et al. Ethnic differences among a community cohort of individuals with dual diagnosis in South London. J Ment Health. 2006;15(5):551–567. [Google Scholar]
- 36.Li J, Green M, Kearns B, Holding E, Smith C, Haywood A, et al. Patterns of multimorbidity and their association with health outcomes within Yorkshire, England: baseline results from the Yorkshire Health Study. BMC Public Health. 2016;16:649. doi: 10.1186/s12889-016-3335-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rose AMC, Sinka K, Watson JM, Mortimer JY, Charlett A. An estimate of the contribution of HIV infection to the recent rise in tuberculosis in England and Wales. Thorax. 2002;57:441–445. doi: 10.1136/thorax.57.5.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hesketh KR, Law C, Bedford H, Hope S. Co-occurrence of health conditions during childhood: longitudinal findings from the UK Millennium Cohort Study (MCS) PLoS ONE. 2016;11(6):e0156868. doi: 10.1371/journal.pone.0156868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jordan JA, Dyer K. Psychological well-being trajectories of individuals with dyslexia aged 3–11 years. Dyslexia. 2017;23(2):161–180. doi: 10.1002/dys.1555. [DOI] [PubMed] [Google Scholar]
- 40.Eastwood SV, Tillin T, Chaturvedi N, Hughes AD. Ethnic differences in associations between blood pressure and stroke in South Asian and European men. Hypertension. 2015;66(3):481–488. doi: 10.1161/HYPERTENSIONAHA.115.05672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Graham HL, Maslin J, Copello A, Birchwood M, Mueser K, McGovern D, et al. Drug and alcohol problems amongst individuals with severe mental health problems in an inner city area of the UK. Soc Psychiatry Psychiatr Epidemiol. 2001;36:448–455. doi: 10.1007/s001270170023. [DOI] [PubMed] [Google Scholar]
- 42.Fleming M, Salim EE, Mackay DF, Henderson A, Kinnear D, Clark D, et al. Neurodevelopmental multimorbidity and educational outcomes of Scottish schoolchildren: A population-based record linkage cohort study. PLoS Med. 2020;17(10):e1003290. doi: 10.1371/journal.pmed.1003290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McKenzie K, Jones P, Lewis S, Williams M, Toone B, Sham P, et al. Lower prevalence of pre-morbid neurological illness in African-Caribbean than White psychotic patients in England. Psychol Med. 2002;32(7):1285–1289. doi: 10.1017/s0033291702006190. [DOI] [PubMed] [Google Scholar]
- 44.Perez-Guzman PN, Daunt A, Mukherjee S, Crook P, Forlano R, Kont MD, et al. Clinical characteristics and predictors of outcomes of hospitalized patients with COVID-19 in a multi-ethnic London NHS Trust: a retrospective cohort study. Clin Infect Dis. 2020;7:ciaa1091. doi: 10.1093/cid/ciaa1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tomson C, Udayaraj U, Gilg J, Ansell D. Comorbidities in UK patients at the start of renal replacement therapy (chapter 6) Nephrol Dial Transplant. 2007;22(Suppl 7):vii58–68. doi: 10.1093/ndt/gfm330. [DOI] [PubMed] [Google Scholar]
- 46.Rao A, Steenkamp R, Caskey F. UK Renal Registry 16th Annual Report: Chapter 5 Comorbidities and Current Smoking Status amongst Patients starting Renal Replacement Therapy in England, Wales and Northern Ireland from 2011 to 2012 [Online]. 2013. Available from https://renal.org/sites/renal.org/files/Chap%2005.pdf. Accessed 23 Mar 2021. [DOI] [PubMed]
- 47.Shaw C, Webb L, Casulaa A, Tomson C. UK Renal Registry 14th Annual Report: Chapter 4 Comorbidities and Current Smoking Status amongst Patients starting Renal Replacement Therapy in England, Wales and Northern Ireland from 2009 to 2010 [Online]. 2012. Available from https://renal.org/sites/renal.org/files/Chap04_1.pdf. Accessed 23 Mar 2021. [DOI] [PubMed]
- 48.Steenkamp R, Caskey F. UK Renal Registry 18th Annual Report: Chapter 6 Comorbidities and Current Smoking Status amongst Patients starting Renal Replacement Therapy in England, Wales and Northern Ireland from 2013 to 2014. Nephron. 2016;132 Suppl 1:145–54. [DOI] [PubMed]
- 49.Caskey F, Webb L, Gilg J, Fogarty D. UK Renal Registry 12th Annual Report (December 2009): chapter 6: comorbidities and current smoking status amongst patients starting renal replacement therapy in England, Wales and Northern Ireland from 2003 to 2008: national and centre-specific analyses. Nephron Clin Pract. 2010;115(Suppl 1):c103–c116. doi: 10.1159/000301161. [DOI] [PubMed] [Google Scholar]
- 50.Webb L, Gilga J, Feesta T, Fogarty D. Chapter 4. Comorbidities and Current Smoking Status amongst Patients starting Renal Replacement Therapy in England, Wales and Northern Ireland from 2008 to 2009 [Online]. 2011. Available from https://renal.org/sites/renal.org/files/Chap04_0.pdf. Accessed 24 Mar 2021. [DOI] [PubMed]
- 51.Udayaraj U, Tomson CR, Gilg J, Ansell D, Fogarty D. UK Renal Registry 11th Annual Report (December 2008): Chapter 6 Comorbidities and current smoking status amongst patients starting renal replacement therapy in England, Wales and Northern Ireland: national and centre-specific analyses. Nephron Clin Pract. 2009;111 Suppl 1:c97–111. [DOI] [PubMed]
- 52.Fischbacher CM, Bhopal R, Steiner M, Morris AD, Chalmers J. Is there equity of service delivery and intermediate outcomes in South Asians with type 2 diabetes? analysis of DARTS database and summary of UK publications. J Public Health (Oxf) 2009;31(2):239–249. doi: 10.1093/pubmed/fdp003. [DOI] [PubMed] [Google Scholar]
- 53.Mehta RL, Davies MJ, Ali S, Taub NA, Stone MA, Baker R, et al. Association of cardiac and non-cardiac chronic disease comorbidity on glycaemic control in a multi-ethnic population with type 1 and type 2 diabetes. Postgrad Med J. 2011;87(1033):763–768. doi: 10.1136/postgradmedj-2011-130298. [DOI] [PubMed] [Google Scholar]
- 54.Ali S, Davies MJ, Taub NA, Stone MA, Khunti K. Prevalence of diagnosed depression in South Asian and white European people with type 1 and type 2 diabetes mellitus in a UK secondary care population. Postgrad Med J. 2009;85(1003):238–243. doi: 10.1136/pgmj.2008.074641. [DOI] [PubMed] [Google Scholar]
- 55.Roderick P, Byrne C, Casula A, Steenkamp R, Ansell D, Burden R, et al. Survival of patients from South Asian and Black populations starting renal replacement therapy in England and Wales. Nephrol Dial Transplant. 2009;24(12):3774–3782. doi: 10.1093/ndt/gfp348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sivaprasad S, Gupta B, Gulliford MC, Dodhia H, Mohamed M, Nagi D, et al. Ethnic variations in the prevalence of diabetic retinopathy in people with diabetes attending screening in the United Kingdom (DRIVE UK) PLoS ONE. 2012;7(3):e32182. doi: 10.1371/journal.pone.0032182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sapey E, Gallier S, Mainey C, Nightingale P, McNulty D, Crothers H, et al. Ethnicity and risk of death in patients hospitalised for COVID-19 infection in the UK: an observational cohort study in an urban catchment area. BMJ Open Respir Res. 2020;7(1):e000644. doi: 10.1136/bmjresp-2020-000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bhui K, Bhugra D, Goldberg D, Sauer J, Tylee A. Assessing the prevalence of depression in Punjabi and English primary care attenders: the role of culture, physical illness and somatic symptoms. Transcult Psychiatry. 2004;41(3):307–322. doi: 10.1177/1363461504045642. [DOI] [PubMed] [Google Scholar]
- 59.Lowry PJ, Glover DR, Mace PJE, Littler WA. Coronary artery disease in Asians in Birmingham. Br Heart J. 1984;52:610–613. doi: 10.1136/hrt.52.6.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bakewell AB, Higgins RM, Edmunds ME. Does ethnicity influence perceived quality of life of patients on dialysis and following renal transplant? Nephrol Dial Transplant. 2001;16(7):1395–1401. doi: 10.1093/ndt/16.7.1395. [DOI] [PubMed] [Google Scholar]
- 61.Nagi DK. Cardiovascular risk factors in Asian and Caucasian subjects with and without Type 2 diabetes: studies using new highly specific assays for insulin, intact proinsulin and des 31,32 split proinsulin. London: University College London; 1994.
- 62.Patel JV, Sosin M, Lim HS, Chung I, Panja N, Davis RC, et al. Raised leptin concentrations among South Asian patients with chronic heart failure. Int J Cardiol. 2007;122(1):34–40. doi: 10.1016/j.ijcard.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 63.Malavige LS, Wijesekara P, Seneviratne Epa D, Ranasinghe P, Levy JC. Ethnic differences in sexual dysfunction among diabetic and nondiabetic males: the Oxford Sexual Dysfunction Study. J Sex Med. 2013;10(2):500–508. doi: 10.1111/j.1743-6109.2012.02911.x. [DOI] [PubMed] [Google Scholar]
- 64.Cole N, Bedford M, Cai A, Jones C, Cairns H, Jayawardene S. Black ethnicity predicts better survival on dialysis despite greater deprivation and co-morbidity: a UK study. Clin Nephrol. 2014;82(2):77–82. doi: 10.5414/CN108247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kitley J, Leite MI, Nakashima I, Waters P, McNeillis B, Brown R, et al. Prognostic factors and disease course in aquaporin-4 antibody-positive patients with neuromyelitis optica spectrum disorder from the United Kingdom and Japan. Brain. 2012;135(Pt 6):1834–1849. doi: 10.1093/brain/aws109. [DOI] [PubMed] [Google Scholar]
- 66.Patel R, Moore T, Cooper V, McArdle C, Perry N, Cheek E, et al. An observational study of comorbidity and healthcare utilisation among HIV-positive patients aged 50 years and over. Int J STD AIDS. 2016;27(8):628–637. doi: 10.1177/0956462415589524. [DOI] [PubMed] [Google Scholar]
- 67.Pinto R, Ashworth M, Seed P, Rowlands G, Schofield P, Jones R. Differences in the primary care management of patients with psychosis from two ethnic groups: a population-based cross-sectional study. Fam Pract. 2010;27(4):439–446. doi: 10.1093/fampra/cmq014. [DOI] [PubMed] [Google Scholar]
- 68.Mohsen AH, Murad S, Easterbrook PJ. Prevalence of hepatitis C in an ethnically diverse HIV-1-infected cohort in south London. HIV Med. 2005;6(3):206–215. doi: 10.1111/j.1468-1293.2005.00291.x. [DOI] [PubMed] [Google Scholar]
- 69.Misra R, Askari A, Faiz O, Arebi N. Colectomy rates for ulcerative colitis differ between ethnic groups: results from a 15-year nationwide cohort study. Can J Gastroenterol Hepatol. 2016;2016:8723949. doi: 10.1155/2016/8723949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zakeri R, Bendayan R, Ashworth M, Bean DM, Dodhia H, Durbaba S, et al. A case-control and cohort study to determine the relationship between ethnic background and severe COVID-19. EClinicalMedicine. 2020;28:100574. doi: 10.1016/j.eclinm.2020.100574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Samy EF, Ross J, Bolton E, Morris EJ, Oliver SE. Variation in incidence and survival by ethnicity for patients with myeloma in England (2002–2008) Leuk Lymphoma. 2015;56(9):2660–2667. doi: 10.3109/10428194.2014.1003060. [DOI] [PubMed] [Google Scholar]
- 72.Hull S, Mathur R, Dreyer G, Yaqoob MM. Evaluating ethnic differences in the prescription of NSAIDs for chronic kidney disease: a cross-sectional survey of patients in general practice. Br J Gen Pract. 2014;64(624):e448–e455. doi: 10.3399/bjgp14X680557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Blackledge HM, Newton J, Squire IB. Prognosis for South Asian and white patients newly admitted to hospital with heart failure in the United Kingdom: historical cohort study. BMJ. 2003;327(7414):526–531. doi: 10.1136/bmj.327.7414.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bhanu C, Jones ME, Walters K, Petersen I, Manthorpe J, Raine R, et al. Physical health monitoring in dementia and associations with ethnicity: a descriptive study using electronic health records. BJGP Open. 2020;4(4):bjgpopen20X101080. doi: 10.3399/bjgpopen20X101080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mathur R, Palla L, Farmer RE, Chaturvedi N, Smeeth L. Ethnic differences in the severity and clinical management of type 2 diabetes at time of diagnosis: a cohort study in the UK Clinical Practice Research Datalink. Diabetes Res Clin Pract. 2020;160:108006. doi: 10.1016/j.diabres.2020.108006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bruce M, Gwaspari M, Cobb D, Ndegwa D. Ethnic differences in reported unmet needs among male inpatients with severe mental illness. J Psychiatr Ment Health Nurs. 2012;19(9):830–838. doi: 10.1111/j.1365-2850.2011.01859.x. [DOI] [PubMed] [Google Scholar]
- 77.Downs JM, Lechler S, Dean H, Sears N, Patel R, Shetty H, et al. The association between comorbid autism spectrum disorders and antipsychotic treatment failure in early-onset psychosis: a historical cohort study using electronic health records. J Clin Psychiatry. 2017;78(9):e1233–e1241. doi: 10.4088/JCP.16m11422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dragovic B, Greaves K, Vashisht A, Straughair G, Sabin C, Smith NA. Chlamydial co-infection among patients with gonorrhoea. Int J STD AIDS. 2002;13(4):261–263. doi: 10.1258/0956462021925063. [DOI] [PubMed] [Google Scholar]
- 79.Dorrington S, Carr E, Stevelink SAM, Dregan A, Woodhead C, Das-Munshi J, et al. Multimorbidity and fit note receipt in working-age adults with long-term health conditions. Psychol Med. 2020:1–10. [DOI] [PubMed]
- 80.Ashworth M, Durbaba S, Whitney D, Crompton J, Wright M, Dodhia H. Journey to multimorbidity: longitudinal analysis exploring cardiovascular risk factors and sociodemographic determinants in an urban setting. BMJ Open. 2019;9(12):e031649. doi: 10.1136/bmjopen-2019-031649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gathani T, Chiuri K, Broggio J, Reeves G, Barnes I. Ethnicity and the surgical management of early invasive breast cancer in over 164 000 women. Breast Cancer Res Treat. 2020;180:1–49. doi: 10.1002/bjs.11865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jain P, Cockwell P, Little J, Ferring M, Nicholas J, Richards N, et al. Survival and transplantation in end-stage renal disease: a prospective study of a multiethnic population. Nephrol Dial Transplant. 2009;24(12):3840–3846. doi: 10.1093/ndt/gfp455. [DOI] [PubMed] [Google Scholar]
- 83.Nimako K, Gunapala R, Popat S, O'Brien ME. Patient factors, health care factors and survival from lung cancer according to ethnic group in the south of London. UK Eur J Cancer Care (Engl) 2013;22(1):79–87. doi: 10.1111/j.1365-2354.2012.01373.x. [DOI] [PubMed] [Google Scholar]
- 84.Mathur R, Farmer RE, Eastwood SV, Chaturvedi N, Douglas I, Smeeth L. Ethnic disparities in initiation and intensification of diabetes treatment in adults with type 2 diabetes in the UK, 1990–2017: a cohort study. PLoS Med. 2020;17(5):e1003106. doi: 10.1371/journal.pmed.1003106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mathur R, Dreyer G, Yaqoob MM, Hull SA. Ethnic differences in the progression of chronic kidney disease and risk of death in a UK diabetic population: an observational cohort study. BMJ Open. 2018;8(3):e020145. doi: 10.1136/bmjopen-2017-020145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Owusu Adjah ES, Bellary S, Hanif W, Patel K, Khunti K, Paul SK. Prevalence and incidence of complications at diagnosis of T2DM and during follow-up by BMI and ethnicity: a matched case-control analysis. Cardiovasc Diabetol. 2018;17(1):70. doi: 10.1186/s12933-018-0712-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Baskar V, Kamalakannan D, Holland MR, Singh BM. Does ethnic origin have an independent impact on hypertension and diabetic complications? Diabetes Obes Metab. 2006;8(2):214–219. doi: 10.1111/j.1463-1326.2005.00485.x. [DOI] [PubMed] [Google Scholar]
- 88.Earle K, Porter K, Ostberg J, Yudkin J. Variation in the progression of diabetic nephropathy according to racial origin. Nephrol Dial Transplant. 2001;16(2):286–290. doi: 10.1093/ndt/16.2.286. [DOI] [PubMed] [Google Scholar]
- 89.Gill P, Haque MS, Martin U, Mant J, Mohammed MA, Heer G, et al. Measurement of blood pressure for the diagnosis and management of hypertension in different ethnic groups: one size fits all. BMC Cardiovasc Disord. 2017;17(1):55. doi: 10.1186/s12872-017-0491-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gorantla RS, Nimmagadda M, Potluri S, Uppal H, Chandran S, Potluri R. Ethnic variations in length of hospital stay in patients with atrial fibrillation. Int J Cardiol. 2015;187:542–544. doi: 10.1016/j.ijcard.2015.03.405. [DOI] [PubMed] [Google Scholar]
- 91.Sosin MD, Patel JV, Bhatia GS, Hughes EA, Davis RC, Lip GY. Effects of white European, African Caribbean and South Asian ethnicity on homocysteine levels in patients with systolic heart failure. Int J Cardiol. 2008;129(1):69–75. doi: 10.1016/j.ijcard.2007.04.112. [DOI] [PubMed] [Google Scholar]
- 92.Conway DS, Lip GY. Comparison of outcomes of patients with symptomatic peripheral artery disease with and without atrial fibrillation (the West Birmingham Atrial Fibrillation Project) Am J Cardiol. 2004;93(11):1422–5, A10.. doi: 10.1016/j.amjcard.2004.02.047. [DOI] [PubMed] [Google Scholar]
- 93.Jesky M, Lambert A, Burden AC, Cockwell P. The impact of chronic kidney disease and cardiovascular comorbidity on mortality in a multiethnic population: a retrospective cohort study. BMJ Open. 2013;3(12):e003458. doi: 10.1136/bmjopen-2013-003458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Udayaraj U, Pruthi R, Casula A, Roderick P. UK Renal Registry 16th Annual Report: Chapter 6 Demographics and Outcomes of Patients from Different Ethnic Groups on Renal Replacement Therapy in the UK [Online]. 2013. Available from https://renal.org/sites/renal.org/files/Chap%2006.pdf. Accessed 5 July 2021. [DOI] [PubMed]
- 95.Mazzoncini R, Donoghue K, Hart J, Morgan C, Doody GA, Dazzan P, et al. Illicit substance use and its correlates in first episode psychosis. Acta Psychiatr Scand. 2010;121(5):351–358. doi: 10.1111/j.1600-0447.2009.01483.x. [DOI] [PubMed] [Google Scholar]
- 96.Kennedy N, Boydell J, van Os J, Murray RM. Ethnic differences in first clinical presentation of bipolar disorder: results from an epidemiological study. J Affect Disord. 2004;83(2–3):161–168. doi: 10.1016/j.jad.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 97.Weaver T, Rutter D, Madden P, Ward J, Stimson G, Renton A. Results of a screening survey for co-morbid substance misuse amongst patients in treatment for psychotic disorders: prevalence and service needs in an inner London borough. Soc Psychiatry Psychiatr Epidemiol. 2001;36(8):399–406. doi: 10.1007/s001270170030. [DOI] [PubMed] [Google Scholar]
- 98.Liew I, Carter P, Reynolds J, Gollop ND, Uppal H, Chandran S, et al. Length of hospital stay is shorter in South Asian patients with transient ischemic attack. Int J Cardiol. 2016;203:607–608. doi: 10.1016/j.ijcard.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 99.Potluri R, Wasim M, Markandey B, Kapour A, Khouw N, Carter P, et al. Length of hospital stay is shorter in South Asian patients with ischaemic stroke. Int J Cardiol. 2015;187:190–191. doi: 10.1016/j.ijcard.2015.03.290. [DOI] [PubMed] [Google Scholar]
- 100.Sarker SJ, Heuschmann PU, Burger I, Wolfe CD, Rudd AG, Smeeton NC, et al. Predictors of survival after haemorrhagic stroke in a multi-ethnic population: the South London Stroke Register (SLSR) J Neurol Neurosurg Psychiatry. 2008;79(3):260–265. doi: 10.1136/jnnp.2007.129189. [DOI] [PubMed] [Google Scholar]
- 101.Patel M, Coshall C, Rudd AG, Wolfe CD. Natural history and effects on 2-year outcomes of urinary incontinence after stroke. Stroke. 2001;32(1):122–127. doi: 10.1161/01.str.32.1.122. [DOI] [PubMed] [Google Scholar]
- 102.Marshall BG, Mitchell DM, Shaw RJ, Marais F, Watkins R, Coker R. HIV and tuberculosis co-infection in an inner London hospital–a prospective anonymized seroprevalence study. J Infect. 1999;38:162–166. doi: 10.1016/s0163-4453(99)90244-x. [DOI] [PubMed] [Google Scholar]
- 103.Ali S, Ur-Rehman T, Lougher E, Mutimer D, Ali M, Paudyal V. Impact of HIV and chronic kidney disease comorbidities on hepatitis C treatment choices, drug-drug interactions and hepatitis C cure. Int J Clin Pharm. 2020;42(2):515–526. doi: 10.1007/s11096-020-00994-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nisar MK, Rafiq A, Ostor AJ. Biologic therapy for inflammatory arthritis and latent tuberculosis: real world experience from a high prevalence area in the United Kingdom. Clin Rheumatol. 2015;34(12):2141–2145. doi: 10.1007/s10067-015-3099-3. [DOI] [PubMed] [Google Scholar]
- 105.Chackathayil J, Patel JV, Gill PS, Potluri R, Natalwala A, Uppal H, et al. Cardiovascular risk profiles amongst women in a multiethnic population in inner city britain: a potential impact of anaemia. Int J Endocrinol. 2013;2013:303859. doi: 10.1155/2013/303859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mann AG, Trotter CL, Balogun MA, Ramsay ME. Hepatitis C in ethnic minority populations in England. J Viral Hepat. 2008;15(6):421–426. doi: 10.1111/j.1365-2893.2007.00958.x. [DOI] [PubMed] [Google Scholar]
- 107.Winkley K, Thomas SM, Sivaprasad S, Chamley M, Stahl D, Ismail K, et al. The clinical characteristics at diagnosis of type 2 diabetes in a multi-ethnic population: the South London Diabetes cohort (SOUL-D) Diabetologia. 2013;56(6):1272–1281. doi: 10.1007/s00125-013-2873-5. [DOI] [PubMed] [Google Scholar]
- 108.Whyte MB, Hinton W, McGovern A, van Vlymen J, Ferreira F, Calderara S, et al. Disparities in glycaemic control, monitoring, and treatment of type 2 diabetes in England: a retrospective cohort analysis. PLoS Med. 2019;16(10):e1002942. doi: 10.1371/journal.pmed.1002942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bastos JL, Harnois CE, Paradies YC. Health care barriers, racism, and intersectionality in Australia. Soc Sci Med. 2018;199:209–218. doi: 10.1016/j.socscimed.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 110.Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: Structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75(12):2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- 111.Bowleg L. The Problem With the Phrase Women and Minorities: Intersectionality— an Important Theoretical Framework for Public Health. American journal of public health. 2012;102(7):1267–73. doi: 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Nazroo JY, Bhui KS, Rhodes J. Where next for understanding race/ethnic inequalities in severe mental illness? Structural, interpersonal and institutional racism. Sociol Health Illn. 2020;42(2):262–276. doi: 10.1111/467-9566.13001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Parliamentary Office of Science and Technology. Ethnicity And Health [Online]. 2007. Available from https://www.parliament.uk/globalassets/documents/post/postpn276.pdf. Accessed 4 June 2021.
- 114.Rivenbark JG, Ichou M. Discrimination in healthcare as a barrier to care: experiences of socially disadvantaged populations in France from a nationally representative survey. BMC Public Health. 2020;20(1):31. doi: 10.1186/s12889-019-8124-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Adegbembo AO, Tomar SL, Logan HL. Perception of racism explains the difference between Blacks’ and Whites’ level of healthcare trust. Ethn Dis. 2006;16:792–798. [PubMed] [Google Scholar]
- 116.Sabbah W, Gireesh A, Chari M, Delgado-Angulo EK, Bernabé E. Racial discrimination and uptake of dental services among American adults. Int J Environ Res Public Health. 2019;16(9):1558. doi: 10.3390/ijerph16091558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Parry G, Van Cleemput P, Peters J, Walters S, Thomas K, Cooper C. health status of gypsies and travellers in England. J Epidemiol Community Health. 2007;61(3):198–204. doi: 10.1136/jech.2006.045997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Iqbal G, Johnson MRD, Szczepura A, Gumber A, Wilson S, Dunn JA. Ethnicity data collection in the UK: the healthcare professional’s perspective. Divers Equal Health Care. 2012;9:281–290. [Google Scholar]
- 119.Raleigh V, Holmes J. The health of people from ethnic minority groups in England [online]. 2021. Available from https://www.kingsfund.org.uk/publications/health-people-ethnic-minority-groups-england#Diabetes. Accessed 25 May 2021.
- 120.Livingston G, Leavey G, Kitchen G, Manela M, Sembhi S, Katona C. Accessibility of health and social services to immigrant elders: the Islington Study. Br J Psychiatry. 2002;180:369–374. doi: 10.1192/bjp.180.4.369. [DOI] [PubMed] [Google Scholar]
- 121.Molokhia M, Okoli G, Redmond P, Asgari E, Shaw C, Schofield P, et al. Uncoded chronic kidney disease in primary care: a cross-sectional study of inequalities and cardiovascular disease risk management. Br J Gen Pract. 2020;70(700):e785–e792. doi: 10.3399/bjgp20X713105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Scobie S, Spencer J, Raleig V. Ethnicity coding in English health service datasets [Online]. 2021. Available from https://www.nuffieldtrust.org.uk/files/2021-06/1622731816_nuffield-trust-ethnicity-coding-web.pdf. Accessed 14 June 2021.
- 123.Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: Toward a more uniform methodology. Annals of Family Medicine Inc. 2012;10:142–51 [DOI] [PMC free article] [PubMed]
- 124.Violan C, Foguet-Boreu Q, Flores-Mateo G, Salisbury C, Blom J, Freitag M, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS ONE. 2014;9(7):e102149. doi: 10.1371/journal.pone.0102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bradby H. Describing ethnicity in health research. Ethn Health. 2003;8(1):5–13. doi: 10.1080/13557850303555. [DOI] [PubMed] [Google Scholar]
- 126.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Department of Health. Long-term conditions compendium of Information: 3rd edition [Online]. 2012. Available from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216528/dh_134486.pdf. Accessed 14 May 2021.
- 128.Bécares L, Shaw RJ, Katikireddi SV, Irizar P, Amele S, Kapadia D, et al. Racism as the fundamental cause of ethnic inequities in COVID-19 vaccine hesitancy: A theoretical framework and empirical exploration using the UK Household Longitudinal Study. SSM - Population Health. 2022;19:101150. doi: 10.1016/j.ssmph.2022.101150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Bhui K. Ethnic inequalities in health: the interplay of racism and COVID-19 in syndemics. The Lancet. 2021;36:100953. doi: 10.1016/j.eclinm.2021.100953. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data extracted from the included studies are publicly available.