Abstract
Background
Post-intensive care unit recovery programs for survivors of critical illness related to COVID-19 remain limited, ever-evolving, and under active investigation. Mental health professionals have an emerging role within this multidisciplinary care model.
Objective
This article explores the design and implementation of an intensive care unit follow-up clinic in New Orleans during the era of COVID-19. Survivors of a critical illness due to COVID-19 were offered multidisciplinary outpatient treatment and systematic psychological screening up to 6 months after the initial clinic visit.
Methods
We implemented a prospective, observational study at a post-intensive care syndrome (PICS) clinic for survivors of a critical illness related to COVID-19 embedded within an academic Veterans Affairs hospital. Our team identified patients at high risk of PICS and offered them a clinic consultation. Patients were provided the following interventions: review of the critical care course, medication reconciliation, primary care, psychopharmacotherapy, psychotherapy, and subspecialty referrals. Patients were followed up at 1- to 3-month intervals. Psychological symptom screening was conducted with Posttraumatic Stress Disorder Checklist for the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition, 9-question Patient Health Questionnaire, and 7-item Generalized Anxiety Disorder assessments.
Results
Seventy-seven total patients were identified to be at high risk of PICS from March to November 2020, and of this cohort, 44 (57.14%) survived their COVID-19 hospitalizations. Of the surviving 44 patients contacted, 21 patients established care in the PICS clinic and returned for at least 1 follow-up visit. At initial evaluation, 66.7% of patients demonstrated clinically meaningful symptoms of post-traumatic stress disorder. At 3-month follow-up, 9.5% of patients showed significant post-traumatic stress disorder symptoms. Moderate-to-severe symptoms of anxiety were present in 38.1% of patients at initial evaluation and in 4.8% of patients at 3 months. Moderate-to-severe symptoms of depression were present in 33.4% and 4.8% of patients at initial visit and at 3 months, respectively.
Conclusions
A PICS clinic serves as a posthospitalization model of care for COVID-19 intensive care unit survivors. This type of health care infrastructure expands the continuum of care for patients enduring the consequences of a critical illness. We identified a high prevalence of post-traumatic stress, anxiety, and depression, along with other post- intensive care unit complications warranting an intervention. The prevalence of distressing psychological symptoms diminished across all domains by 3 months.
Key words: post-intensive care syndrome, COVID-19, post-traumatic stress disorder, ICU-recovery center, delirium, post-acute COVID-19
Introduction
As in-hospital mortality of critically ill patients has declined significantly over the last 30 years, interest has shifted toward long-term morbidity and posthospitalization outcomes in this high-risk group.1 The growth of intensive care unit (ICU) survivorship has led to a surging population, including family members, who suffer from the long-term consequences of a critical illness.2 , 3 Typical post-ICU symptoms include cognitive deficits, physical impairment, and mental health problems that persist long after the index hospitalization and comprise post-intensive care syndrome (PICS)—coined by the Society of Critical Care Medicine in 2010.4
Over half of ICU survivors will acquire PICS at least 3 months after hospitalization.5 , 6 Within this cohort, the prevalence of post-traumatic stress disorder (PTSD) and depressive symptoms related to the ICU is about 40% and 30%, respectively.7, 8, 9 Cognitive impairment (e.g., deficits in memory, concentration, and executive function) is identified in 40% of patients up to 6 months after hospitalization.10 The cognitive and psychological problems patients endure after a critical illness are largely associated with delirium, recognized or not, during the ICU admission.4 , 7 , 10 We expect these rates to continue climbing due to the effects of the pandemic, as unique psychological and neurocognitive disturbances have been recognized in individuals up to 2 years following infection with COVID-19.11
In 2020, ICUs experienced a surge in patients suffering from prolonged delirium, invasive mechanical ventilation, exposure to deep sedation and neuromuscular blockade, acute respiratory distress syndrome, and hypoxia—all uniquely associated with severe COVID-19 infection and strong, independent risk factors for the development of psychological and cognitive impairments related to the ICU stay.4 , 12, 13, 14 Other major risk factors for the development of PICS include sepsis, multiorgan failure, old age, physical frailty, and psychosocial frailty (e.g., pre-existing depression, poor social support, or cognitive impairment).13 , 14
Clinicians across disciplines must be equipped to understand the severity, prevalence, and emerging treatment modalities for the complications of a critical illness. PICS is generally not well understood by physicians providing long-term follow-up care of ICU survivors. The dynamic needs of this population, including psychiatric sequelae, are often distinct and require unique conceptualizations and treatment approaches by mental health care providers. As the framework for diagnosing and treating these patients may be unfamiliar to psychiatrists, PICS is underrecognized, and the much-needed clinical attention is likely diverted.
Evidence-based interventions for ICU survivors (such as post-intensive care recovery centers) remain limited and best studied in Europe.15, 16, 17, 18, 19 Common features among existing multidisciplinary programs include coordination among physical medicine and rehabilitation, social work, pharmacy, primary care, and psychiatry departments. Results from randomized controlled trials on PICS clinics have been mixed; methodologies are limited by small sample sizes and focused on the primary outcome measure of quality-of-life scores.16, 17, 18, 19 Meta-analyses on studies of ICU follow-up programs reveal a paucity of high-powered randomized controlled trials and highlight the heterogenous and ever-evolving post-ICU population, suggesting interventions should be focused on physical and mental health, individualized, and multimodal.20, 21, 22
Our 2020 clinical trial studied the efficacy of the bedside diary in reducing ICU-related PTSD symptoms through construction of the illness narrative.23 This novel intervention targeted risk factors for PTSD, some of which are also risk factors for PICS. Patients with poor recall of the ICU course and who endured a longer duration of sedation are at higher risk of developing post-ICU psychological sequelae.24, 25, 26 While the results of our trial did not demonstrate a benefit of ICU diaries in reducing symptoms of post-traumatic stress, we identified a high prevalence of post-intensive care PTSD.23 Our ICU diary intervention increased PICS awareness and highlighted the need for posthospitalization infrastructure for this vulnerable population.23 In response to our findings, we created a PICS clinic for comprehensive aftercare services embedded within an academic Veterans Affairs (VA) hospital.
This article describes the design and implementation of our ICU-recovery model for COVID-19 survivors with a critical illness. We also report psychiatric outcomes from patients through the first 6 months of recovery after the initial clinic evaluation.
Methods
We implemented a prospective, observational study at our PICS clinic for COVID-19 survivors embedded within an academic VA hospital between May 2021 and April 2022. The institutional review board determined our intervention, study design, and analysis as a quality-improvement process. Our team retrospectively identified ICU survivors who endured a COVID-19-related critical illness from March to November 2020 at high risk of PICS (via a systematic chart review). Eligible patients were adults aged 18 years or older who were discharged from our medical, surgical, and cardiac ICUs with a hospital diagnosis of COVID-19, along with 1 or more of the following risk factors for the development of PICS: mechanical ventilation ≥24 hours, recognized delirium, or a history of septic shock. Initial contact with the patient occurred via telephone call, where PICS education was provided, and for interested patients, initial consultation was offered.
Delirium was noted for patients if any of the following were documented during the ICU admission: a description of hallucinations or perceptual disturbances, the term “delirium” in physician clinical assessments, or a description of agitation leading to psychotropic medication use or restraints. Septic shock was defined as the presence of systemic inflammatory response symptoms with a suspected source of infection and administration of vasopressors.
In our PICS clinic, we provided patients with the following broad categories of interventions: review of the critical care course, medication reconciliation, primary care in coordination with the patient's own physician, psychopharmacotherapy, psychotherapy, further diagnostic workup (including imaging, bloodwork, or procedures), and case management and subspecialty referrals. Patients had follow-up appointments at a minimum of 3-month intervals and more frequently if clinically necessary. Psychological symptom screening was conducted every 3 months with the following validated assessments: Posttraumatic Stress Disorder Checklist for the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5), 9-question Patient Health Questionnaire (PHQ-9), and 7-item Generalized Anxiety Disorder (GAD-7).
The PCL-5 is a self-report measure of Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, symptoms of PTSD, including re-experiencing, avoidance, negative alterations in mood and cognition and hyperarousal (range, 0–80; higher scores represent greater severity). A total symptom score >30 on the PCL-5 corresponds to probable PTSD. The PHQ-9 identifies the presence and severity of depressive symptoms (range, 0–27; higher scores correspond to more severe symptoms). The GAD-7 assesses the presence and severity of anxiety symptoms (range, 0–21; higher scores indicate more severe symptoms). Moderate symptoms of depression and anxiety are defined as scores >10 on the PHQ-9 and GAD-7 scales, respectively. Severe symptoms of depression and anxiety are represented by scores >15 on the PHQ-9 and GAD-7 assessments, respectively. Ventilator days are defined as the number of hospital days the patient required mechanical ventilation in the ICU.
Categorical variables are summarized using frequencies and percentages. Continuous variables are summarized using medians and interquartile ranges. Categorical outcomes and median scores over time are presented at baseline, 3 months, and 6 months after baseline. A study timeline of 6 months captured the majority of our study participants, which demonstrated a significant dropout rate by 9–12 months (due to termination of treatment or loss to follow-up). Differences in scores from baseline over time are presented at 3 and 6 months after baseline. The associations of ventilator days with baseline PCL-5, PHQ-9, and GAD-7 and those of number of PICS interventions with PCL-5, PHQ-9, and GAD-7 were estimated and tested using linear regression. Three-month percent differences for PCL-5, PHQ-9, and GAD-7 were defined by subtracting the baseline value from the 3-month value and dividing the resulting difference by the baseline value. The association of these percent differences and ventilator days and number of PICS interventions was then tested using linear regression.
Statistical significance was defined a priori as α = 0.05. SAS 9.4 (SAS Institute, Cary, NC) was used for data management and all analyses.
Clinic Description
The PICS clinic we describe opened in May of 2021 within the VA Department of Ambulatory Mental Health. Expanding upon the existing framework for general post-ICU follow-up programs, we also incorporated novel revisions to adapt to this population of survivors of a critical illness from COVID-19 (Supplementary Table 1). As literature on COVID-19 evolves quickly, our team regularly shared the latest evidence regarding post-COVID-19 impairments, with special attention to the complexity of symptoms and their relation to psychological and cognitive factors. Maintaining a carefully coordinated, multidisciplinary treatment approach is critical in this cohort.27 , 28 Our clinic is led by dually trained physician internist-psychiatrists, which differs from existing PICS care models led by intensivists. The organization of care providers within our clinic and the greater VA system is depicted in Supplementary Figure 1. Core clinical staff participated in weekly interdisciplinary meetings to discuss updates in patient care.
The Initial Clinic Consultation
The initial evaluation lasted for 90 minutes, when patients and their family members (or caregivers) review the critical illness course with a physician. This entails the integration of patients' memories of their experiences, coupled with information available from their ICU medical records. The goal is to work toward construction of a coherent illness narrative and to situate the trauma as a disruption within the context of a patient's life trajectory. Themes may arise that deal with the meaning of enduring and surviving a life-threatening experience. Patients interested in exploring meaning-making in the psychotherapeutic space are offered an adapted version of meaning-centered psychotherapy.29 , 30
After a review of the ICU course, a thorough medication reconciliation is performed, along with a comprehensive history (social, medical, and psychiatric) and physical examination. The PICS clinic physician also screens for post-COVID-19 symptoms and administers psychological surveys (detailed in the Methods section). Finally, the clinician formulates an assessment of the patient, which includes active medical problems and new difficulties in daily functioning. Subspecialty referrals are placed, and further diagnostic workup is pursued (if indicated). A clinic patient example is presented in Table 1 .
Table 1.
Clinic Patient Example
| A 76-y-old man with a history of diabetes, hypertension, diastolic heart failure, atrial fibrillation, chronic kidney disease, and COVID-19 requiring a lengthy ICU admission presents to establish care in our post-intensive care syndrome clinic 1 y following hospital discharge. His ICU stay lasted 38 d in the Spring of 2020 and was complicated by delirium, a stroke with residual motor deficits, and end-stage renal disease now requiring hemodialysis. He endured prolonged mechanical ventilation, neuromuscular blockade, and use of vasopressors. The patient remembers a workplace exposure to COVID-19 at the cash register. His cold-like symptoms worsened over a few days, as he began feeling short of breath. Upon arrival to the emergency room, he recalls having great difficulty catching his breath and gasping for air. He remembers having an intravenous catheter placed and being asked about a breathing tube, but the rest is relatively foggy. The patient recalls visions of his deceased brother at his bedside and nurses conspiring against him to keep his body locked in a room for experimentation. He also remembers intense moments of helplessness when he was unable to see his family members for extended periods of time (due to hospital visitor restrictions). After an initial evaluation, the patient appears to show significant symptoms of PTSD, with a PCL-5 score of 36—marked by nightmares, flashbacks of being back in the ICU, avoidance, hypervigilance, insomnia, and irritability. He also has moderate symptoms of depression (PHQ-9 is 11) and anxiety (GAD-7 is 10). His depressive symptoms appear tied to a sense of loss and transition since his ICU admission. Adjusting to hemodialysis has been difficult. He feels he can never get back to work as a mechanic, which enhanced his sense of meaning in life. The patient is still quite weak in his left leg and has trouble hearing from his left ear since he was discharged. Moreover, he just feels fatigued and “low in energy” throughout the day, which is out of character for him. This is all consistent with a diagnosis of PICS. |
| PICS clinic interventions |
| 1. Due to his clinically significant symptoms of PTSD, we agreed to start sertraline 50 mg/d. |
| 2. The patient set goals to alleviate depressive symptoms during dialysis sessions, including calling a few friends and completing crossword puzzles. |
| 3. Due to his risk factors, he was referred for a sleep study, diagnosed with obstructive sleep apnea, and obtained a home ventilator. We communicated this to the patient's primary care physician. |
| 4. Due to his left-sided sensorineural hearing loss, we referred the patient to otolaryngology. He is now undergoing an evaluation for a cochlear implant. |
| 5. The patient was able to establish care with outpatient physical and occupational therapy for his persistent left-sided weakness. |
| 6. We referred the patient for compensated work therapy within the VA hospital. While he may not be able to work as a mechanic anymore, the patient might find other work opportunities to contribute to his sense of meaning in life. |
This case is a deidentified composite constructed from and based on real patients we have seen in our clinic under similar circumstances.
GAD-7 = 7-item Generalized Anxiety Disorder; ICU = intensive care unit; PCL-5 = Posttraumatic Stress Disorder Checklist for the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition; PHQ-9 = 9-question Patient Health Questionnaire; PICS = post-intensive care syndrome; PTSD = post-traumatic stress disorder; VA = veterans affair.
Patients return to the PICS clinic for regular follow-up at intervals of 1–3 months with the same provider to maintain continuity, until the patient expresses a desire to end treatment or further treatment is no longer deemed beneficial. If a need for more regular or structured psychotherapy is identified (typically during the initial clinic visit), the patient is either scheduled for more frequent visits with their PICS physician or referred for adjunctive care within the VA system. The indicated psychotherapeutic modality may range from supportive, meaning-centered psychotherapy, or other manualized treatments to psychodynamic psychotherapy. Supplementary Figure 2 provides a schematic diagram and further description of the initial PICS clinic consultation.
Results
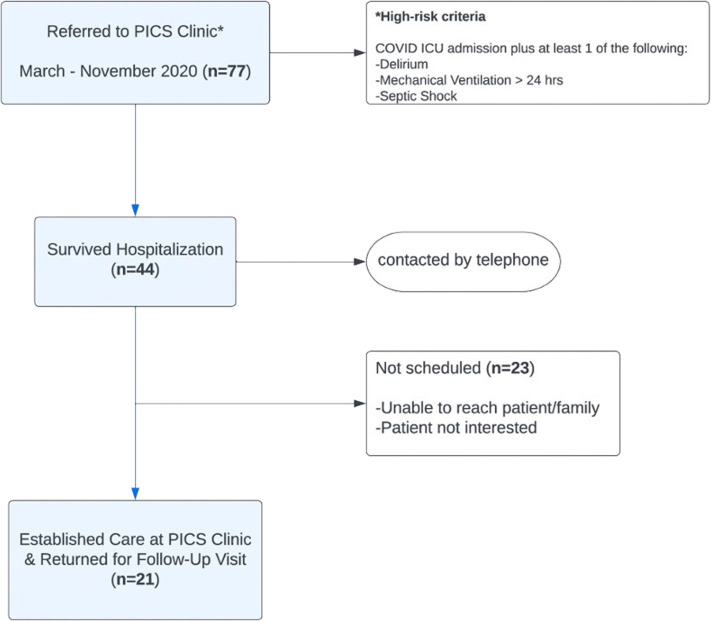
Seventy-seven total patients were identified to be at high risk of PICS from March to November 2020, and of this cohort, 44 (57.14%) survived their COVID-19 hospitalizations. Of the surviving 44 patients contacted, 21 patients established care in the PICS clinic and returned for at least 1 follow-up appointment. Most patients in this cohort continued to follow up in our clinic up to 1 year following the baseline assessment. Patient recruitment is outlined in Figure 1 .
Figure 1.
Patient Recruitment Diagram
Patient baseline demographics and clinical characteristics are presented in Table 2 . The cohort is predominantly male (95.2%), with a median age of 68 years. About 76% of our patients survived the initial COVID-19 wave of Spring 2020. The most common medical and psychiatric comorbidities include hypertension (62%), diabetes mellitus (38%), congestive heart failure (33%), chronic kidney disease (33%), and PTSD (48%).
Table 2.
Demographics and Clinical Characteristics
| Patient demographics/characteristics | Results |
|---|---|
| Age (median [Q1, Q3]) | 68 [63, 73] |
| Male sex, n (%) | 20 (95.2%) |
| COVID+, n (%) | 21 (100.0%) |
| Spring 2020 COVID wave, n (%) | 16 (76.2%) |
| Delirium, n (%) | 21 (100.0%) |
| Septic shock, n (%) | 9 (42.9%) |
| Mechanical ventilation >24 h, n (%) | 19 (90.5%) |
| ICU length of stay (d), median [Q1, Q3] | 26 [15, 35] |
| Time on ventilator (d), median [Q1, Q3] | 8 [2, 15] |
| Duration of sedation (d), median [Q1, Q3] | 7 [1, 13] |
| Medical comorbidities, n (%) | 21 (100.0%) |
| Congestive heart failure | 7 (33.3%) |
| Atrial fibrillation | 3 (14.3%) |
| Chronic kidney disease | 7 (33.3%) |
| Chronic obstructive pulmonary disease | 2 (9.5%) |
| Obstructive sleep apnea | 5 (23.8%) |
| Hypertension | 13 (61.9%) |
| Coronary artery disease | 4 (19.0%) |
| Cirrhosis | 3 (14.3%) |
| Diabetes mellitus, type II | 9 (42.9%) |
| Asthma | 1 (4.8%) |
| Obesity | 5 (23.8%) |
| End-stage renal disease | 2 (9.5%) |
| Prostate cancer | 2 (9.5%) |
| Subdural hematoma | 1 (4.8%) |
| Human immunodeficiency virus | 1 (4.8%) |
| Sarcoidosis | 1 (4.8%) |
| Stroke | 1 (4.8%) |
| Psychiatric comorbidities, n (%) | 13 (61.9%) |
| Major depressive disorder | 5 (23.8%) |
| Post-traumatic stress disorder | 10 (47.6%) |
| Opioid use disorder | 1 (4.8%) |
| Alcohol use disorder | 1 (4.8%) |
| Sedation used, n (%) | 17 (81.0%) |
| Dexmedetomidine | 4 (19.0%) |
| Fentanyl | 12 (57.1%) |
| Propofol | 13 (61.9%) |
| Midazolam | 5 (23.8%) |
| Paralytic | 4 (19.0%) |
| Inpatient COVID medications, n (%) | 19 (90.5%) |
| Antibiotics | 14 (66.7%) |
| Anticoagulation | 4 (19.0%) |
| Hydroxychloroquine | 10 (47.6%) |
| Dexamethasone | 5 (23.8%) |
| Methylprednisolone | 2 (9.5%) |
| Remdesivir | 4 (19.0%) |
| Tocilizumab | 1 (4.8%) |
The median ICU length of stay was 26 days. Eighty-one percent of patients received sedation, of which propofol was the most frequently administered one (62%). During the first COVID-19 wave, evidence for treatment was sparse and in its preliminary phase. The most common inpatient COVID-19 treatments included antibiotics (67%) and hydroxychloroquine (48%).
The median time from ICU discharge to PICS clinic visit was 12 months (Table 3 ). New psychiatric medications were initiated or changed in 19 patients (90%) at intake (Supplementary Table 2). Melatonin was the most prescribed medication (33%) in our clinic. The median number of PICS clinic visits per patient was 4. Case management or subspecialty referral services were provided for 15 patients (71%). The median number of PICS clinic interventions per patient was 5.
Table 3.
PICS Clinic Characteristics
| PICS clinic characteristics | Summary |
|---|---|
| Number of PICS clinic visits, median [Q1, Q3] | 4 [3, 5] |
| Time to first clinic visit (mo), median [Q1, Q3] | 12 [11, 14] |
| Number of interventions, median [Q1, Q3] | 5 [4, 6] |
| Number of hospital readmissions, median [Q1, Q3] | 0 [0, 1] |
PICS = post-intensive care syndrome.
Psychological outcomes over time are presented in Table 4 . At initial evaluation (baseline), 66.7% of patients demonstrated clinically meaningful symptoms of PTSD. At 3-month follow-up, 9.5% of patients showed significant PTSD symptoms. Moderate-to-severe anxiety was present in 38.1% of patients at initial evaluation and in 4.8% of patients at 3-month follow-up. Moderate-to-severe depression was present in 33.4% and 4.8% of patients at initial evaluation and at 3 months, respectively. Table 4 also depicts median psychological scores on the PCL-5, GAD-7, and PHQ-9 surveys longitudinally. We saw a 14.5-point drop in PCL-5 scores from the initial evaluation to 6 months (Supplementary Table 3). Secondary analyses revealed no significant association between the number of ventilator days, or the number of PICS clinic interventions, and psychological screening scores (Supplementary Tables 4 and 5).
Table 4.
Psychological Outcomes and Median Scores Over Time
| Psychological outcomes over time, n (%) | |||||||
|---|---|---|---|---|---|---|---|
| Time | PTSD | Anxiety |
Depression |
||||
| Mild | Moderate | Severe | Mild | Moderate | Severe | ||
| Baseline | 14 (66.7%) | 3 (14.3%) | 6 (28.6%) | 2 (9.5%) | 7 (33.3%) | 3 (14.3%) | 4 (19.1%) |
| 3 mo | 2 (9.5%) | 2 (9.5%) | 0 (0.0%) | 1 (4.8%) | 6 (28.6%) | 1 (4.8%) | 0 (0.0%) |
| 6 mo | 1 (6.3%) | 2 (12.5%) | 1 (6.3%) | 0 (0.0%) | 2 (12.5%) | 0 (0.0%) | 1 (6.3%) |
| Median PTSD, anxiety, and depression scores over time, median [Q1, Q3] | |||||||
|---|---|---|---|---|---|---|---|
| Time | PTSD (PCL-5) | Anxiety (GAD-7) | Depression (PHQ-9) | ||||
| Baseline | 21 [14, 46] | 6 [2, 11] | 8 [4, 13] | ||||
| 3 mo | 13 [5, 19] | 4 [1, 5] | 4 [2, 6] | ||||
| 6 mo |
12.5 [6.5, 18.5] | 4 [2, 5] | 4 [1, 4.5] | ||||
Five missing at 6 months.
GAD-7 = 7-item Generalized Anxiety Disorder; PCL-5 = Posttraumatic Stress Disorder Checklist for the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition; PHQ-9 = 9-question Patient Health Questionnaire; PTSD = post-traumatic stress disorder.
Discussion
The development of PICS is attributed to a range of interventional, environmental, and psychological harms, including invasive treatments such as mechanical ventilation, coupled with the distress of being in an unfamiliar environment. In particular, the persistent psychological and cognitive problems patients face after a critical illness are strongly associated with delirium during the ICU course. Although patients are increasingly surviving life-threatening illnesses, the trauma of a near-death experience and the specific circumstances of the ICU stay, including a perceived lack of control, pain and suffering, isolation and perceived abandonment, and fear and disorientation among other negative experiences, may confer long-term psychological morbidity. By identifying and studying modifiable risk factors for PICS, we may reduce its incidence and improve psychological outcomes for both patients and families.
The findings of our ICU diaries clinical trial revealed an alarming prevalence of intensive care–related PTSD (70% at 3 months) and important barriers to accessing aftercare.23 What remains clear from our work is that the psychological needs and complications of ICU survivors are chronic and prevalent and merit improved efforts at prevention, education, treatment, and access to care supported by ongoing research. This evidence fueled our desire to open a novel, clinical program to treat post-ICU complications.
Adapting the current framework of PICS clinic models to the unique needs of the post-COVID-19 ICU patient population is critical. The long-term consequences of severe COVID-19 infection requiring intensive care are yet largely unknown but likely substantial given the presence of known risk factors for PICS and the distinct circumstances of the pandemic. For instance, social isolation (due to visitor restrictions), limitations to rehabilitation services, greater need for sedation and neuromuscular blockade, and longer lengths of stay and immobility, combined with hypoxemia and coagulopathy, all compound the neuropsychiatric risk and complicated recovery process after hospitalization.27 , 31
We found utility in adapting a meaning-centered psychotherapy framework in the trauma setting with veterans who endured a critical illness from COVID-19. Logotherapy has been used as adjunctive treatment for combat-related PTSD in veterans, particularly as this population is often left with “profound existential questions related to the loss of meaning in life”.32 Our veterans frequently posed questions in clinic regaining meaning after experiencing a life-threatening illness in the ICU. Future studies should rigorously examine the specific impact of psychotherapy on mental health outcomes in patients recovering from a critical illness.
The prevalence of significant psychiatric symptoms in our small clinic population at initial evaluation appears to exceed rates of anxiety, depression, and PTSD symptoms in a large multicenter cohort of first-wave COVID-19 ICU survivors in the Netherlands at 1 year after index hospitalization.33 We noted a reduction in symptom burden across all 3 psychological domains by 3 months, particularly in symptoms of PTSD. Whether this can be attributable to our clinic intervention is questionable given the small sample size and observational nature of our analysis. VA posthospitalization clinics have been associated with decreases in death, nonelective hospital readmissions, and emergency room utilization.34, 35, 36 Generalizability of these results to the post-ICU population is uncertain yet possible. Larger, randomized studies are needed to make definitive claims regarding the efficacy of post-ICU interventions such as ours. Furthermore, qualitative studies should examine the attitudes and subjective experiences of health care professionals and patients involved in post-ICU follow-up programs; this may help streamline ongoing refinements in the design of this new care model.
Our current clinic model broadly draws from the multidisciplinary care models for chronic medical conditions affecting multiple organ systems (such as cancer or cystic fibrosis), where close collaboration among medical specialties is crucial. This serves as the framework for the approach and management of PICS. As such, we expect our PICS model is applicable to nonveteran survivors of a critical illness. Moreover, this model can be extended to include patients who suffer from post-COVID-19 complications after hospital stays that did not require intensive care. For example, the common post-COVID-19 symptoms of fatigue, dyspnea, and cognitive impairment affect (and are influenced by) both mental health and physical function and are not consistently associated with initial disease severity or ICU length of stay.27
Future systems of care deploying this model on a wider scale should evaluate outcome measures such as rehospitalization, quality of life, and specific psychiatric sequela such as downstream suicide and self-harm. Studies that capture post-ICU subpopulations (e.g., veterans who survived a critical illness from COVID-19) and investigate the efficacy of tailored interventions (e.g., psychotherapy, early mental health referrals, review of the ICU stay, and so forth) will offer significant clarity for this complex and emerging area of patient care.
Barriers to Care
We encountered noteworthy barriers in the implementation of our clinic. Mortality rates in the ICU remain high. Nearly 50% of patients we identified as candidates for ICU follow-up did not survive to hospital discharge. The referral pathway from the ICU setting to our posthospitalization clinical program still needs to be effectively integrated as part of routine patient discharge planning. Establishing contact and gaining patient trust and interest in our post-ICU intervention is challenging, not just because patient and provider awareness of PICS remains low but also for many reasons. Avoidance of health care is common among those suffering with PICS. Additionally, the stigma of receiving mental health care persists in veteran populations nationwide.37, 38, 39 We hope to continue addressing these barriers with our ongoing efforts to educate, destigmatize, and offer access to mental health services.
Limitations
Our observational pilot study has several important limitations. No claims regarding causality or efficacy of our clinic can be made due to the design of the study, small sample size, and heterogenous interventions based on individual patient characteristics and needs during clinical assessments. While most patients appeared to improve with regard to psychometric scores from intake to follow-up visits, and we would like to attribute the improvement to the interventions made as a result of our PICS clinical program, we have no comparator cohort and cannot conclude that any significant difference exists for our patients versus patients progressing with usual care, for whom time from the incident event may garner comparable benefit. Randomized studies are needed to assess any measurable difference in outcomes. The patient population for this pilot study is niche—predominantly male veterans of Southeast Louisiana who survived a COVID-19-related ICU admission. Almost half of our patients had pre-existing, chronic PTSD from the military. We observed a significant drop in symptoms of post-traumatic stress related to the index ICU stay by 6 months; yet it remains unclear if a previous diagnosis of PTSD may have conferred downstream protection (versus heightened risk) in our cohort.
Our ICU follow-up program is distant from the index hospitalization (about 1 year after discharge), due to logistics and time required to establish a novel clinic within an academic institution at the onset of the pandemic. Future comparisons will discern whether establishing care with a PICS clinic sooner after discharge alters the disease course and response to treatment. We predict that our outcomes would vary significantly, depending on the time from index hospitalization to psychological screening and clinical intervention. For instance, prevalence rates of anxiety and depression in the post-COVID-19 intensive care population appear to decline over time, from 6 to 12 months after discharge.33 , 40 , 41 This is relatively consistent with prepandemic trends of psychiatric symptoms after a critical illness.6 Multidisciplinary experts in ICU follow-up care recommend planning the initial post-ICU clinic visit at 12 weeks after discharge.42 Thus, we may have captured patients suffering with a greater symptom burden sooner after index hospitalization, when our interventions could provide even greater impact.
Conclusions
The overlap among persistent psychological, cognitive, and physical symptoms is complicated and dynamic. PICS is influenced by environmental factors, ICU interventions, the critical illness itself, the degree of patients' social support, psychological frailty, and more. Post-ICU sequelae remain poorly understood, and treatment approaches must be interdisciplinary and individualized. We need more comprehensive, multisite studies that can better characterize patients by their level of risk in developing specific features of PICS to enhance our understanding of post-ICU interventions and improve patient care.
Acknowledgements
Author Contributions: All authors have contributed sufficiently to the manuscript, and all authors have approved the final manuscript.
Footnotes
Ethical Publication Statement: The institutional review board reviewed and approved this study as a quality-improvement process. Informed consent was waived due to the use of retrospective and deidentified data. This study adhered to the guidelines set forth by the Office of Human Research Protection that is supported by the U.S. Department of Health and Human Services.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure: The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jaclp.2023.01.009.
Supplementary Data
References
- 1.Zimmerman J.E., Kramer A.A., Knaus W.A. Changes in hospital mortality for United States intensive care unit admissions from 1988 to 2012. Crit Care. 2013;17 doi: 10.1186/cc12695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jackson J.C., Pandharipande P.P., Girard T.D., et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2:369–379. doi: 10.1016/S2213-2600(14)70051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sevin C.M., Bloom S.L., Jackson J.C., Wang L., Ely E.W., Stollings J.L. Comprehensive care of ICU survivors: development and implementation of an ICU recovery center. J Crit Care. 2018;46:141–148. doi: 10.1016/j.jcrc.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mikkelsen M.E., Still M., Anderson B.J., et al. Society of critical care medicine's international consensus conference on prediction and identification of long-term impairments after critical illness. Crit Care Med. 2020;48:1670–1679. doi: 10.1097/CCM.0000000000004586. [DOI] [PubMed] [Google Scholar]
- 5.Kawakami D., Fujitani S., Morimoto T., et al. Prevalence of post-intensive care syndrome among Japanese intensive care unit patients: a prospective, multicenter, observational J-PICS study. Crit Care. 2021;25:69. doi: 10.1186/s13054-021-03501-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marra A., Pandharipande P.P., Girard T.D., et al. Co-occurrence of post-intensive care syndrome problems among 406 survivors of critical illness. Crit Care Med. 2018;46:1393–1401. doi: 10.1097/CCM.0000000000003218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rabiee A., Nikayin S., Hashem M.D., et al. Depressive symptoms after critical illness: a systematic review and meta-analysis. Crit Care Med. 2016;44:1744–1753. doi: 10.1097/CCM.0000000000001811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parker A.M., Sricharoenchai T., Raparla S., Schneck K.W., Bienvenu O.J., Needham D.M. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med. 2015;43:1121–1129. doi: 10.1097/CCM.0000000000000882. [DOI] [PubMed] [Google Scholar]
- 9.Wintermann G.B., Brunkhorst F.M., Petrowski K., et al. Stress disorders following prolonged critical illness in survivors of severe sepsis. Crit Care Med. 2015;43:1213–1222. doi: 10.1097/CCM.0000000000000936. [DOI] [PubMed] [Google Scholar]
- 10.Pandharipande P.P., Girard T.D., Jackson J.C., et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369:1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taquet M., Sillett R., Zhu L., et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. 2022;9:815–827. doi: 10.1016/S2215-0366(22)00260-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huggins E.L., Bloom S.L., Stollings J.L., Camp M., Sevin C.M., Jackson J.C. A clinic model: post-intensive care syndrome and post-intensive care syndrome-family. AACN Adv Crit Care. 2016;27:204–211. doi: 10.4037/aacnacc2016611. [DOI] [PubMed] [Google Scholar]
- 13.Desai S.V., Law T.J., Needham D.M. Long-term complications of critical care. Crit Care Med. 2011;39:371–379. doi: 10.1097/CCM.0b013e3181fd66e5. [DOI] [PubMed] [Google Scholar]
- 14.Hosey M.M., Needham D.M. Survivorship after COVID-19 ICU stay. Nat Rev Dis Primers. 2020;6:60. doi: 10.1038/s41572-020-0201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griffiths J.A., Barber V.S., Cuthbertson B.H., Young J.D. A national survey of intensive care follow-up clinics. Anaesthesia. 2006;61:950–955. doi: 10.1111/j.1365-2044.2006.04792.x. [DOI] [PubMed] [Google Scholar]
- 16.Cuthbertson B.H., Rattray J., Campbell M.K., et al. The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial. BMJ. 2009;339 doi: 10.1136/bmj.b3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walsh T.S., Salisbury L.G., Merriweather J.L., et al. Increased hospital-based physical rehabilitation and information provision after intensive care unit discharge: the RECOVER randomized clinical trial. JAMA Intern Med. 2015;175:901–910. doi: 10.1001/jamainternmed.2015.0822. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt K., Worrack S., Von Korff M., et al. Effect of a primary care management intervention on mental health-related quality of life among survivors of sepsis: a randomized clinical trial. JAMA. 2016;315:2703–2711. doi: 10.1001/jama.2016.7207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jensen J.F., Egerod I., Bestle M.H., et al. A recovery program to improve quality of life, sense of coherence and psychological health in ICU survivors: a multicenter randomized controlled trial, the RAPIT study. Intensive Care Med. 2016;42:1733–1743. doi: 10.1007/s00134-016-4522-1. [DOI] [PubMed] [Google Scholar]
- 20.Rosa R.G., Ferreira G.E., Viola T.W., et al. Effects of post-ICU follow-up on subject outcomes: a systematic review and meta-analysis. J Crit Care. 2019;52:115–125. doi: 10.1016/j.jcrc.2019.04.014. [DOI] [PubMed] [Google Scholar]
- 21.Schofield-Robinson O.J., Lewis S.R., Smith A.F., McPeake J., Alderson P. Follow-up services for improving long-term outcomes in intensive care unit (ICU) survivors. Cochrane Database Syst Rev. 2018;11 doi: 10.1002/14651858.CD012701.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geense W.W., van den Boogaard M., van der Hoeven J.G., Vermeulen H., Hannink G., Zegers M. Nonpharmacologic interventions to prevent or mitigate adverse long-term outcomes among ICU survivors: a systematic review and meta-analysis. Crit Care Med. 2019;47:1607–1618. doi: 10.1097/CCM.0000000000003974. [DOI] [PubMed] [Google Scholar]
- 23.Sayde G.E., Stefanescu A., Conrad E., Nielsen N., Hammer R. Implementing an intensive care unit (ICU) diary program at a large academic medical center: results from a randomized control trial evaluating psychological morbidity associated with critical illness. Gen Hosp Psychiatry. 2020;66:96–102. doi: 10.1016/j.genhosppsych.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Biehl M., Sese D. Post-intensive care syndrome and COVID-19 - implications post pandemic. Cleve Clin J Med. 2020 doi: 10.3949/ccjm.87a.ccc055. [DOI] [PubMed] [Google Scholar]
- 25.Jones C., Griffiths R.D., Humphris G., Skirrow P.M. Memory, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Crit Care Med. 2001;29:573–580. doi: 10.1097/00003246-200103000-00019. [DOI] [PubMed] [Google Scholar]
- 26.Karnatovskaia L.V., Johnson M.M., Benzo R.P., Gajic O. The spectrum of psychocognitive morbidity in the critically ill: a review of the literature and call for improvement. J Crit Care. 2015;30:130–137. doi: 10.1016/j.jcrc.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 27.Parker A.M., Brigham E., Connolly B., et al. Addressing the post-acute sequelae of SARS-CoV-2 infection: a multidisciplinary model of care. Lancet Respir Med. 2021;9:1328–1341. doi: 10.1016/S2213-2600(21)00385-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santhosh L., Block B., Kim S.Y., et al. Rapid design and implementation of post-COVID-19 clinics. Chest. 2021;160:671–677. doi: 10.1016/j.chest.2021.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Breitbart W.S., Breitbart W., Poppito S.R. Oxford University Press; New York, NY: 2014. Individual Meaning-Centered Psychotherapy for Patients with Advanced Cancer: A Treatment Manual. [Google Scholar]
- 30.Rosenfeld B., Saracino R., Tobias K., et al. Adapting meaning-centered psychotherapy for the palliative care setting: results of a pilot study. Palliat Med. 2017;31:140–146. doi: 10.1177/0269216316651570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vannorsdall T.D., Brigham E., Fawzy A., et al. Cognitive dysfunction, psychiatric distress, and functional decline after COVID-19. J Acad Consult Liaison Psychiatry. 2022;63:133–143. doi: 10.1016/j.jaclp.2021.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Southwick S.M., Gilmartin R., McDonough P., Morrissey P. Logotherapy as an adjunctive treatment for chronic combat-related PTSD: a meaning-based intervention. Am J Psychother. 2006;60:161–174. doi: 10.1176/appi.psychotherapy.2006.60.2.161. [DOI] [PubMed] [Google Scholar]
- 33.Heesakkers H., van der Hoeven J.G., Corsten S., et al. Clinical outcomes among patients with 1-year survival following intensive care unit treatment for COVID-19. JAMA. 2022;327:559–565. doi: 10.1001/jama.2022.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shu C.C., Hsu N.C., Lin Y.F., Wang J.Y., Lin J.W., Ko W.J. Integrated postdischarge transitional care in a hospitalist system to improve discharge outcome: an experimental study. BMC Med. 2011;9:96. doi: 10.1186/1741-7015-9-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Diem S.J., Prochazka A.V., Meyer T.J., Fryer G.E. Effects of a postdischarge clinic on housestaff satisfaction and utilization of hospital services. J Gen Intern Med. 1996;11:179–181. doi: 10.1007/BF02600273. [DOI] [PubMed] [Google Scholar]
- 36.van Walraven C., Mamdani M., Fang J., Austin P.C. Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med. 2004;19:624–631. doi: 10.1111/j.1525-1497.2004.30082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blais R.K., Renshaw K.D., Jakupcak M. Posttraumatic stress and stigma in active-duty service members relate to lower likelihood of seeking support. J Trauma Stress. 2014;27:116–119. doi: 10.1002/jts.21888. [DOI] [PubMed] [Google Scholar]
- 38.Ben-Zeev D., Corrigan P.W., Britt T.W., Langford L. Stigma of mental illness and service use in the military. J Ment Health. 2012;21:264–273. doi: 10.3109/09638237.2011.621468. [DOI] [PubMed] [Google Scholar]
- 39.Blais R.K., Renshaw K.D. Stigma and demographic correlates of help-seeking intentions in returning service members. J Trauma Stress. 2013;26:77–85. doi: 10.1002/jts.21772. [DOI] [PubMed] [Google Scholar]
- 40.Writing Committee for the COMEBAC Study Group Four-month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA. 2021;325:1525–1534. doi: 10.1001/jama.2021.3331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schandl A., Hedman A., Lyngå P., et al. Long-term consequences in critically ill COVID-19 patients: a prospective cohort study. Acta Anaesthesiol Scand. 2021;65:1285–1292. doi: 10.1111/aas.13939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Der Schaaf M., Bakhshi-Raiez F., Van Der Steen M., Dongelmans D.A., De Keizer N.F. Recommendations for intensive care follow-up clinics; report from a survey and conference of Dutch intensive cares. Minerva Anestesiol. 2015;81:135–144. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.