Abstract
Premature deaths in bodybuilders regularly make headlines and are cited as evidence that bodybuilding is a dangerous activity. A wealth of research has revealed elite athletes typically enjoy lower mortality rates than non-athletes, but research on bodybuilder lifespan is surprisingly limited. Anabolic androgenic steroid (AAS) use is commonly cited as a key contributor to morbidity and premature mortality in bodybuilders, but this area of research is highly nuanced and influenced by numerous confounders unique to bodybuilding. It is quite possible that bodybuilders are at elevated risk and that AAS use is the primary reason for this, but there remains much unknown in this realm. As global participation in bodybuilding increases, and healthcare providers play a more active role in monitoring bodybuilder health, there is a need to identify how numerous factors associated with bodybuilding ultimately influence short- and long-term health and mortality rate. In this Current Opinion, we discuss what is currently known about the bodybuilder lifespan, identify the nuances of the literature regarding bodybuilder health and AAS use, and provide recommendations for future research on this topic.
Key Points
| The literature on bodybuilder health is primarily based on case studies and clinical surrogates, but there is little direct epidemiologic evidence that bodybuilders are at increased risk of adverse clinical outcomes. |
| Androgenic anabolic steroids (AAS) likely contribute to morbidity and premature mortality in bodybuilders, but it is difficult to disentangle AAS use from multiple other bodybuilding-specific risk factors which may have adverse effects on short- and long-term health. |
Introduction
“The doctors were against me—they said that working out with weights would give people heart attacks…”—Jack LaLanne, commenting on the response to his opening a fitness center in 1936 [1].
In 2021, over two dozen professional competitive bodybuilders died suddenly, along with a number of retired bodybuilders under the age of 60 years (Table 1). This spate of deaths has received much attention within the bodybuilding world, but relatively little in the medical community. This is especially concerning and relevant to healthcare providers, given that modern bodybuilders often seek guidance from medical professionals in an attempt to minimize their personal risk. Bodybuilding health and safety is an under recognized public health issue, given that the sport attracts male and female competitors of all ages and abilities from around the globe.
Table 1.
Known list of national and international level bodybuilders reported to have died seemingly premature deaths from non-accidental causes in 2021
| Initials (nationality) | Sex | Date of death | Age (years) | Reported cause of death | Notes |
|---|---|---|---|---|---|
| M.S. (UK) | M | January 18, 2021 | 50 | Not reported | |
| L.B. (USA) | F | January 22, 2021 | 52 | Suicide | History of depression |
| C.P. (South Africa) | M | January 23, 2021 | 50 | COVID-19 | |
| A.H. (USA) | M | March 19, 2021 | 54 | Pulmonary embolism following elbow surgery | Previous history of deep vein thrombosis one year earlier |
| S.K.A. (Pakistan) | M | April 7, 2021 | 41 | Heart attack | |
| M.H. (USA) | M | April 8, 2021 | 55 | Heart attack (13 days earlier) | Heart attack after workout on March 26 after days of pain in chest and arm, plus chills and fever |
| B.H. (USA) | M | April 11, 2021 | 54 | Not reported | Collapsed while playing billiards |
| J.L. (India) | M | April 30, 2021 | 34 | COVID-19 | |
| F.Z.H. (Saudi Arabia) | M | May 8, 2021 | Not reported | Not reported | History of epilepsy |
| L.M. (Trinidad and Tobago) | M | May 8, 2021 | 58 | Renal failure | History of renal failure |
| S.K. (India) | M | May 10, 2021 | 35 | Heart attack | |
| J.L (USA) | F | July 18, 2021 | 49 | Seizure during sleep | |
| S.H. (Iraq) | M | July 20, 2021 | 35 | Stroke | |
| S.G. (USA) | F | July 31, 2021 | 27 | Heart attack | Preparing for competition in 4–6 weeks |
| J.M. (USA) | M | August 8, 2021 | 49 | Pulmonary embolism | Heart attack 18 months earlier |
| A.H. (Czechoslovakia) | F | August 15, 2021 | 46 | Diuretic abuse | Hours before competition |
| O.G. (Italy) | M | August 17, 2021 | Unreported | Heart attack | Days after competition |
| P.H. (USA) | M | August 19, 2021 | 55 | Not reported | History of kidney disease |
| W.S. (USA) | M | August 22, 2021 | 56 | Not reported | |
| M.M. (USA) | F | August 24, 2021 | 28 | Not reported | |
| G.P. (USA) | M | October 6, 2021 | 37 | Not reported | 1 day before Mr. Olympia competition |
| J.H. (USA) | F | October 23, 2021 | 58 | Not reported | |
| S.R. (Jamaica / USA) | M | November 6, 2021 | 46 | Heart attack | |
| R.L. (Canada) | F | November 26, 2021 | 52 | Colon cancer | |
| T.E. (UK) | M | December 22, 2021 | 55 | Not reported |
All information was gathered via internet news sources
Competitive bodybuilding has existed for nearly a century, with the first Mr. America contest held in 1938 and the first International Federation of BodyBuilding and Fitness (IFBB) professional event (Mr. Olympia) in 1965. While mortality rates in other types of elite athletes from this era have been extensively examined and found to be favorable compared to the general population [2], the fate of bodybuilders has been largely unstudied. Theoretically, bodybuilding should benefit health since it focuses on physical activity and “optimal” nutrition. Indeed, current evidence suggests that resistance training is associated with reduced all-cause mortality rates, and likely reduces cardiovascular risk [3]. However, elite athletes in other strength-based sports do not enjoy a major benefit of longevity, especially compared to endurance athletes [4–6]. Bodybuilders engage in extremely high volume and intensity strength training exercise and adopt unusual dietary behaviors, both of which may set them apart from other strength-based athletes. It is unclear how the combination of all of these factors ultimately influences health and mortality at the population level.
While 2021 seemed to be unusual in the high number of deaths that year and is not necessarily representative of other years, reports of premature death (i.e., before the age of 50 years) in high-profile bodybuilders are common. The seemingly high rate of premature death is a common topic of discussion within the bodybuilding community but is rooted in anecdotal case series rather than epidemiology. One must also consider that many famed bodybuilders are still alive and well in their 70s and beyond (e.g., Arnold Schwarzenegger, Lou Ferrigno), while others from that era have died in their late 70s or 80s (e.g., Dave Draper [7], Chris Dickerson [8]). Regardless, anabolic androgenic steroid (AAS) abuse is commonly cited as a key contributor, if not the primary factor, in the premature deaths in bodybuilding. While this may indeed be the case, there is surprisingly limited direct evidence for this. Here, we present an overview of suspected risk factors for premature death in bodybuilders, describe the nuances of the literature, and present suggestions for future research.
The Role of Anabolic Androgenic Steroids
Bodybuilders frequently partake in drug abuse to achieve their exaggeratedly massive and lean physiques. Incidence of AAS use has been reported to be 54–76% and 10–40% in male and female competitive bodybuilders, respectively [9–11]. There is a wealth of information that AAS will increase muscle mass but will also have deleterious health effects [12].
Drug Testing in Bodybuilding (or Lack Thereof)
An apparent lack of drug testing in competitive bodybuilding has enabled a culture where bodybuilders openly engage in polypharmacy (taking various cocktails of appearance/performance enhancing drugs, e.g., [13]). This is in stark contrast to that of other sports, in which athletes generally do not admit to intentional drug use even after testing positive for banned substances [14]. The premier governing body for competitive bodybuilding, the IFBB, has policies regarding drug testing which conform to the World Anti-Doping Association (WADA) Code. However, in recent decades these rules appear to have been minimally enforced. The IFBB and its member affiliates host > 6000 competitions annually, but the most recently available WADA report (2018) indicates that they only submitted a total of 171 samples for analysis [15]. For comparison’s sake in other similar sports, the International Powerlifting Federation submitted 787 samples, and the International Weight-Lifting Federation submitted 3238 samples.
Cardiovascular Risks from AAS
A detailed review of the multi-systemic effects of AAS on surrogate measures of health is beyond the scope of this paper, since premature death is our primary outcome of interest. Nonetheless, it is important to briefly review the effects of AAS on the cardiovascular system since many of the recent deaths were cardiovascular in nature. Several studies have demonstrated that AAS unfavorably influences known cardiovascular disease risk factors. For example, AAS have been demonstrated to markedly reduce high density lipoprotein (HDL) cholesterol and increase low density lipoprotein (LDL) cholesterol in bodybuilders and powerlifters [16, 17], and increase homocysteine in bodybuilders [18]. There are numerous studies reporting that AAS abuse is associated with elevated blood pressure, but also many reports showing no effect. The nuances of these conflicting findings were reviewed by Achar et al. [19].
Cardiac Hypertrophy with Cardiac Dysfunction
The recent Health risks of Anabolic Androgenic steRoid use by maLE aMateur athletes (HAARLEM) study examined male AAS users in a gym and reported that one cycle of AAS is associated with unfavorable cardiac function, blood lipid profile, and various other risk factors [20, 21]. Though insightful, these studies lack a control group of non-AAS users [22]. These findings may not represent high-level bodybuilders. Of the 111 male AAS users initially enrolled, only 19% were competitive bodybuilders and the entire sample only performed a median of 4 training sessions per week (which is lower than most competitive bodybuilders [23]).
Cardiac hypertrophy is typically present in bodybuilders and other athletes and is suspected to be pathological when facilitated by AAS. D’Andrea et al. [24] showed that septal and posterior wall thickness, left ventricular mass and stroke volume were statistically greater in both, AAS-using (at least 5 years of use, n = 20) and non-using (n = 25), top-level bodybuilders compared to age-matched sedentary healthy controls. These parameters did not differ between AAS users and non-users. However, only the AAS-users showed evidence of subclinical systolic and diastolic dysfunction, and this was related to cumulative AAS exposure. Non-users had lower maximal systolic blood pressures and greater performance during a maximal cycle ergometry test. Likewise, Baggish et al. [25] reported cardiac dysfunction (but similar cardiac structure) in a small sample of non-competitive strength-trained AAS users (n = 12) compared to non-users (n = 7). Cardiac dysfunction in that sample was more severe than reported in other studies which examined AAS-using competitive bodybuilders [24, 26], and the authors suggested this may be due to the elite bodybuilders having greater overall health than the non-competitive sample [25]. Fyksen et al. reported AAS users had greater hematocrit, interventricular septum and left ventricular posterior wall thickness (with only AAS users having concentric hypertrophy), and reduced aerobic exercise capacity, left ventricular ejection fraction, and HDL cholesterol compared to strength-trained AAS non-users [27]. Ismail et al. [28] and Dickerman et al. [29] also reported an increase in left ventricular mass and wall thickness in AAS-using bodybuilders (Ismail et al., n = 15, Dickerman et al., n = 8) compared to non-using bodybuilders (Ismail et al., n = 8 Dickerman et al., n = 8), as well as a decreased right (but not left) ventricular ejection fraction [28] and ventricular compliance [29].
Impaired cardiac function in AAS users shares some commonalities with hypertrophic cardiomyopathy (HCM). Grandperrin et al. found that AAS-using bodybuilders had greater left ventricular wall thickness than non-using control athletes (non-bodybuilders), but less than asymptomatic athletes (non-bodybuilding) with HCM [30]. Anabolic androgenic steroid-using athletes also had many anatomic and functional characteristics in common with HCM, such as decreased cardiac work efficiency, but some key regional differences in cardiac function differentiated between the AAS users and HCM athletes [30]. However, it should be noted that many individuals from each group had considerable individual overlap in cardiac work parameters. These findings provide some interesting insights in that cardiac phenotype in AAS-using bodybuilders has similarities to HCM, but it is not clear if such would be the case for AAS non-using bodybuilders.
Cardiac Hypertrophy Without Dysfunction
The studies above provide a convincing case that AAS use has deleterious effects on cardiac function in bodybuilders and other strength-trained athletes. However, there are some conflicting findings to consider. Thompson et al. found no differences in cardiac dimensions and generally similar cardiac function between AAS-using (n = 12) and non-using (n = 11) weightlifters (with ≥ 3 years of training history) [31]. Non-significant increases in left ventricular compliance were observed in the AAS-using weightlifters compared to non-users, which conflicts Dickerman et al.’s findings [29]. Barbosa Neto et al. [32] reported statistically significantly greater interventricular septal thickness, left ventricular mass and posterior wall thickness in AAS-using versus non-using bodybuilders, but no differences in ejection fraction. Dickerman et al. [33] also reported significant left ventricular hypertrophy without diastolic dysfunction in elite strength trained athletes (bodybuilders and powerlifters). Salke et al. [34] reported no differences in cardiac dimensions between AAS using (n = 15) and non-using bodybuilders (n = 15), although both had greater ventricular and septal dimensions than sedentary controls. Systolic function during resistance training and maximal-intensity aerobic exercise did not differ between AAS using (n = 9) and non-using (n = 5) bodybuilders [35]. The acute cardiac functional responses to resistance training exercise also appear to be similar between AAS users and non-users [36].
Methodological Considerations
It is understandable that studies comparing AAS-using versus non-using bodybuilders are often limited by small sample sizes, but this is nonetheless important to consider when interpreting results. This is especially so, given that numerous, sometimes inter-related, cardiac parameters are typically examined within a given study, and many (not all) of these studies do not report if statistical adjustments to account for multiple comparisons were performed. Thus, it is uncertain if reports of statistically significant differences between AAS-users and non-users are due to chance (Type I error), and if a lack of significant differences in other studies is attributable to underpowered studies (Type II error). Conflicting results between studies may be attributed to lack of blinding [19], and also differences in measurement techniques [37]. Additionally, AAS users commonly use other drugs, which can impair cardiac function. Many (> 20%) of the participants in the HAARLEM study [22] and most of the AAS users in Fysken et al. [27] used other anabolic agents (e.g., human growth hormone (hGH)), medications (e.g., thyroxine, ephedrine), and recreational drugs (e.g., nicotine, cocaine, amphetamines). Most studies examining the effects of AAS do not account for these drugs, which makes it difficult to isolate the effects of AAS [19], as described in Sects. 3 and 4.
The magnitude of cardiac hypertrophy in bodybuilders must also be interpreted cautiously, since common normalization methods are rooted in formulae which are highly nuanced. Cardiac mass is generally reported in terms of lean body mass (or fat-free mass) and/or body surface area (BSA). Numerous methods exist to estimate body composition (e.g. skinfold testing, underwater weighing, various medical imaging procedures, bioelectrical impedance, etc.) and each is built around various assumptions and produces different results [38]. A cross-sectional study of 27 bodybuilders computed fat-free mass using eight different body composition methods and reported means ranging from 65.5 to 69.1 kg, depending on method (and 62.0 kg using estimations based on body mass index (BMI), i.e. height and weight alone) [39]. Skinfold tests and bioelectrical impedance estimated body fat percentage with approximately ± 8% difference than the reference standard four-compartment model [39]. BSA is estimated using various formulae (most commonly that published by DuBois and DuBois in 1916 [40, 41]) and is based exclusively on height and weight (and occasionally sex) from specific populations [42]. There is concern that BSA may not be appropriate for obese individuals or others with atypical anatomic proportions (e.g. obese and anorexic individuals) [43, 44]; thus it seems plausible that existing BSA calculations would not accurately translate to bodybuilders. Body surface area normalization is recognized to be problematic in cardiac measurement of athletes in general [45]. Different normalizations may provide different conclusions. For instance, a study comparing elite Olympic weightlifters (mass 62–94 kg) to weight-matched recreational controls found no statistically significant differences in left ventricular mass without scaling (4.3% greater in weightlifters, p = 0.33), with height2.7 scaling (8.6%, p = 0.11), or BSA1.5 scaling (0%, p = 0.82), but did find a significant difference between groups when using dual-energy X-ray absorptiometry (DXA) fat-free mass normalization (11.3%, p = 0.01) [37]. When comparing current AAS abusers (n = 37) versus controls (n = 30), left ventricular mass was 38.3% greater in AAS users when reported without scaling, 33.7% when scaled to BSA, and only 17% when scaled to DXA fat-free mass [46]. Thus, different scaling methods can amplify or diminish between-group differences in cardiac mass, and it is unknown how this would be affected if different BSA formulae or body composition methods were used for normalization.
Reversibility of Deleterious Effects of AAS
It is important to recognize that at least some of the unfavorable cardiovascular changes associated with AAS appear to be reversible, which calls into question their significance (or magnitude of influence) in the long-term health of bodybuilders. There are studies which report that changes in cardiac function persist for at least 9 weeks after discontinuation [47], but longer-term follow-up suggests that this time frame is too short to observe reversibility. The multiple cardiovascular changes (i.e., left ventricular hypertrophy, impaired systolic and diastolic function) observed in the HAARLEM study completely reversed to baseline levels 3–12 months following discontinuation of AAS use [21]. Moreover, baseline cardiovascular parameters did not differ between individuals who had never used AAS previously compared to those with a history of AAS use. This is consistent with other studies in which current AAS users had impaired cardiac function compared to both past AAS users and individuals who never used AAS [48]. Reversibility has also been observed in case series, such that cardiac function improved 5 months after AAS were discontinued [49]. However, Rasmussen et al. reported some indicators of systolic dysfunction persisted in former AAS users (n = 33, mean 30 months post-cessation), although left ventricular mass was similar to resistance-trained controls (n = 30), and lower than current AAS-users (n = 37) [46].
The reversibility of AAS-related cardiac changes suggests that health risks may be greatest at the time of use. As such, longer AAS cycles may be associated with greater risk. Data from HAARLEM are limited to one AAS cycle, and it is unknown how cumulative exposure to multiple cycles ultimately influences cardiovascular risk. Many of the other studies comparing AAS-using versus non-using bodybuilders and strength athletes are performed at a time of AAS use, with some even requiring confirmation with urinary metabolite quantification. Thus, it is difficult to know which deleterious changes would persist (and at what magnitude) following cessation of AAS use. Indeed, it is possible that multiple AAS exposures over the course of many years could result in progressive irreversible changes (e.g. atherosclerotic lesions, glomerular damage), and cause other non-cardiovascular pathologies (e.g., hepatocellular adenomas and carcinomas [50–54] and other cancers). For instance, impaired testosterone levels, reproductive function, and psychological health may last for months or years following cessation of AAS [55, 56]. However, indicators of liver dysfunction associated with AAS use return to normal within 1 year of AAS discontinuation in most, but not all strength-trained athletes [57]. Regardless, the lack of epidemiologic data in the AAS-using and non-using bodybuilding populations precludes an accurate assessment of long-term health risks.
AAS, Morbidity, and Mortality in the Context of Other Athletic Populations
It is tempting to attribute “heart attacks” and other seemingly untimely deaths to bodybuilding-specific practices, but sudden death in athletes can happen for various reasons [58]. Numerous case reports have attributed morbidity/mortality in bodybuilders to AAS use and/or other drugs [49, 59–65], and indeed AAS may be the culprit in many of these. There exist instances of AAS-using bodybuilders with significant cardiac morbidity who deny using anabolic agents or drugs (e.g., no growth hormone, anabolic beta agonists, etc.) [66], but these cases are rare. As such, most case reports and series do not provide: (1) information on how common these events are, and (2) definitive evidence of cause-and-effect for any one specific contributor or differentiate between contributors (e.g., AAS and/or polypharmacy practices vs extreme protein intake vs extreme resistance exercise training; see Sects. 3 and 4).
Case reports about coronary and thromboembolic events in bodybuilders generally assume that AAS were the primary contributors to such events. However, one must also consider that similar adverse outcomes can happen in presumed non-AAS using athletes. There are a number of case reports of well-trained marathon runners with a low-risk of cardiovascular disease (e.g., normal blood lipid profile, no history of smoking, etc.), having clinically significant coronary artery disease [67–70]. Likewise, thromboembolic events have been associated with AAS in bodybuilders, but have also been reported during training and following competition in healthy and fit runners with low cardiovascular disease risk [71, 72]. Numerous cases of venous thromboembolism have been identified in professional athletes in various other sports and have been attributed to various risk factors (e.g., frequent air travel, family history, trauma) [73], but AAS use has generally not been suspected in these populations. Multiple factors contribute to thromboembolism in physically active individuals, including dehydration, heat exposure, and extreme exercise [74].
It seems inappropriate to blindly assume that coronary or thromboembolic events in bodybuilders are a direct consequence of AAS, when they are well-documented in other athletes who are seemingly at low risk of cardiovascular disease. The nearly exclusive focus on AAS may distract attention from other potential modifiable health risks in bodybuilding (such as those described in Sect. 3). We must emphasize that sudden cardiac death and other cardiovascular events are relatively rare in seemingly otherwise healthy athletes, but they do occur frequently enough to be a topic of study. Indeed, it is very possible (or even likely) that AAS use is a significant contributor to cardiovascular adverse events in bodybuilders, and the rate of cardiovascular morbidity and mortality in AAS-using bodybuilders may be far higher than in these other athletic populations. However, there are currently insufficient data to determine the magnitude that AAS contribute to this, and it is therefore necessary to explore other risks.
Potential Other Health Risks for Bodybuilders
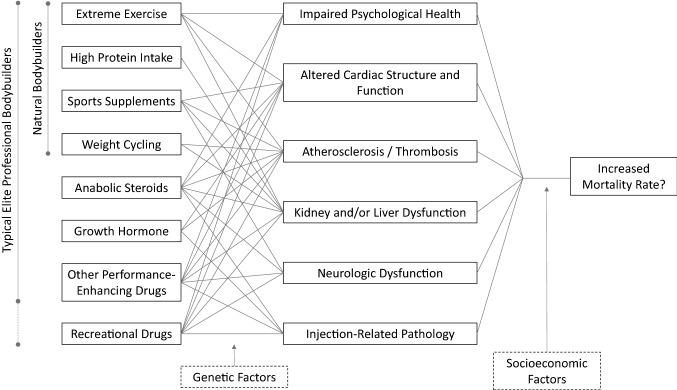
It is clear that AAS have a deleterious effect on various aspects of health and are connected with increased mortality rates in the general population. However, it is difficult to separate AAS themselves from polypharmacy practices and broader issues related to substance abuse (including unmanaged psychiatric illness and greater engagement in risk-taking behavior). While it is quite possible drug abuse is a primary factor behind the seemingly high rate of premature death in bodybuilders, focus on intentional drug use may overshadow some other important contributors to morbidity and mortality in bodybuilders. Bodybuilding represents an extreme lifestyle, and multiple aspects of it may be detrimental to health (Fig. 1).
Fig. 1.
Factors which may contribute to morbidity and premature death in bodybuilders. There is little epidemiologic research investigating significant morbidity and mortality in bodybuilders, but case reports and anecdotal evidence suggest a number of causes. These include myocardial infarction, cardiomyopathy, heart failure, pulmonary embolism, kidney failure, epilepsy, and suicide. Androgenic anabolic steroids (AAS) are commonly cited as the primary cause of morbidity and mortality in bodybuilders, but many other factors can also influence short- and long-term health and clinical outcomes in all bodybuilders. Each individual factor may contribute to pathology, and it is possible that there are additive or synergistic effects. Genetics likely modulate the magnitude of pathology/morbidity for each individual risk factor. Socioeconomic factors (e.g., education level, access to high-quality healthcare) may influence whether pathology results in premature death. It should be noted that this figure focuses on suspected pathology/health risks of bodybuilding behaviors, but it is also possible that some behaviors could be beneficial (e.g., extreme weight training might improve overall health, some supplements or drugs may provide protective effects)
Extreme Strength-Training Exercise
It must be emphasized that the health benefits of exercise training far outweigh the risks. Indeed, a 2012 systematic review (N = 7 studies, with at least three participants in one study using AAS) concluded that elite weightlifters had enhanced systolic function [75], and other studies examining highly trained weightlifters report enhanced diastolic function [76]. However, exercise can sometimes be associated with cardiovascular adverse events. There is evidence that extreme endurance exercise training is associated with cardiac abnormalities, although the clinical significance of these are unknown [77]. Less is known about the long-term effects of extreme strength training practices by bodybuilders.
Heavy resistance training exercise produces extremely high systolic and diastolic blood pressure, with measures as high as 480/350 mmHg reported in the literature [78]. High pressures likely contribute to left ventricular hypertrophy in strength-trained athletes [79]. These changes are not inherently pathologic [80–83], but it is possible that the extreme training that bodybuilders engage in could trigger some deleterious remodeling. It is also possible that individuals with pre-existing cardiovascular vulnerabilities (e.g., valvular deficiencies, abnormal coronary artery structure or function, genetic predisposition for hypercoagulability, etc.) who may not experience adverse events from typical exercise training could develop serious pathology from extreme bodybuilding training.
Bodybuilding health and risk factors have generally been studied in elite, AAS-using individuals, which makes it difficult to disentangle the effects of extreme weight training exercise from AAS use. There is some research comparing differences in cardiac risk surrogates between AAS-using versus natural bodybuilders [84], but such studies are relatively uncommon and limited by small sample size. As described in Sect. 2.2.2, Thompson [31] and D’Andrea et al. [24] both report a similar magnitude of cardiac hypertrophy in AAS user and non-user weightlifters and bodybuilders. Basic science studies have demonstrated that AAS can directly influence the myocardium, but it is also possible that AAS and other drugs simply allow for increased resistance training intensity, and such extreme training is what ultimately drives deleterious cardiac remodeling and dysfunction.
Longitudinal studies of American-style football players provide some insight on the cardiac effects of high-load resistance exercise. In a longitudinal study, players who reported not using AAS demonstrated concentric left ventricular hypertrophy and impaired left ventricular diastolic function over 3 months [85]. A similar study found significant increases in left ventricular mass, interventricular septal thickness, relative wall thickness in first-year collegiate players [both linemen (n = 64) and non-linemen (n = 49)] over a season, with none of the players testing positive for AAS during routine drug testing [86]. However, concentric left ventricular hypertrophy was almost exclusively found in the linemen (20 of 64, compared to 1 of 49 non-linemen). A 3-year longitudinal study (AAS use not specified) showed progression of concentric left ventricular hypertrophy and unfavorable changes in cardiac diastolic function and arterial function [87]. However, it is possible that other football-specific factors, such as repeated impacts, could influence cardiovascular function. These studies also attempted to control AAS use, but it is possible that AAS-using athletes may not have reported this or may not have been selected for routine drug testing. Regardless, these findings have much in common with those reported in AAS-using bodybuilders (see Sect. 2.2.1) and emphasize the need to consider that extreme resistance-training exercise itself (or perhaps high-intensity isometric loading) may be a contributor to deleterious changes in cardiac structure and function.
Extreme Dietary Practices
Competitive bodybuilders engage in extreme dietary practices, and these vary substantially between each phase of their seasonal schedules. Bodybuilding training can be divided into broad phases of off-season, pre-competition, and competition [88–90]. The off-season phase focuses on maximizing muscle hypertrophy (“bulking”) through periodized training combined with very high protein intakes [10, 88]. The pre-competition phase is designed to gradually reduce fat mass (“cutting"), which is achieved through aerobic exercise and altered macronutrient intake [10, 88]. The competition phase, known as “peak week,” optimizes bodybuilding-specific aesthetics (i.e., muscle definition) through dehydration and other techniques [89–91]. Different types of drugs and supplements may also be used to achieve the goals of each phase [88].
Dietary Protein Intake
The relationship between protein intake and kidney dysfunction or disease is a highly nuanced area of research and often involves surrogate outcomes (i.e., estimated glomerular filtration rates), which are open to interpretation [92, 93]. There is epidemiologic evidence showing high protein diets and certain types of protein (e.g., from red meat) are associated with impaired renal function [94, 95]. Large epidemiological studies have linked higher protein diets (generally 1.0–1.7 g/kg/day) to impaired renal function and kidney disease within the general population [96], but such epidemiologic investigation has not been done in strength trained athletes or bodybuilders.
Bodybuilders often consume substantial quantities of dietary protein (1.9–4.3 g/kg body mass/day for men, 0.8–2.8 g/kg/day for women) [97], which exceeds recommendations for strength-trained athletes (1.4–2.0 g/kg/day) [98–100]. Some individuals may consume even greater amounts, as exemplified in a case report of a novice bodybuilder who consumed 750 g of protein per day [101]. The unique protein requirements for elite bodybuilders have not been studied, so it is unclear if such high protein intake is excessive or necessary for success [102]. Regardless, there is concern that these high intakes adversely affect renal health in bodybuilders [93, 96]. A number of studies have found that prescription of a very high protein diet (3.0–4.4 g/kg body mass/day, for between 8 weeks and 1 year) does not adversely change biomarkers of kidney and liver function in healthy resistance-trained individuals [103–106].
Some case reports have suggested that whey protein supplementation was a causative factor for coronary events [107, 108], although the causative nature of these claims is difficult to substantiate. A case series of 5 non-AAS using otherwise healthy males describes new onset of acne following ~ 6 months of regular whey protein consumption [109], and another case series reports similar effects in five adolescent patients [110]. These acne cases do not represent severe morbidity but are provided to demonstrate undesirable effects of whey protein, which could have otherwise been attributed to AAS [111]. One high-profile case of an amateur female bodybuilder was widely attributed to excess protein supplement intake; however, she did not know that she had a rare (1 in 8000 people) genetic disorder that made her susceptible to toxic effects from a high protein intake [112].
Thus, there are indications that excessive protein can have deleterious effects on bodybuilder health, but the lack of available epidemiologic data suggests bodybuilders are not at increased risk of kidney disease. Ali et al. identified 15 bodybuilding patients who required a diagnostic kidney biopsy from 2011 through 2019 but estimated that the risk of kidney disease in bodybuilders was the same as that of the general population [113]. The one exception to this was a higher likelihood of nephrocalcinosis in bodybuilders, attributable to veterinary-grade vitamin D injection (1 case per 314 injectors) [113]. Further epidemiologic study of severe kidney disease in current and former bodybuilders is needed.
Weight Cutting and Weight Cycling
A systematic review reported that male and female bodybuilders typically lose 5–7 kg and 3–6 kg of total body mass, respectively, for competition [97]. However, there is considerable variation in weight loss reported between studies. For example, Andersen et al. [114] reported a mean loss of 8.4 ± 9.3 kg of body mass in 26 natural female bodybuilders (mean total body mass 55.5 ± 6.4 kg) over the course of a season. Fifteen percent of these female competitors reported losing > 9.5 kg at least one time, and 2% reported losing 5–9.1 kg on at least 4 occasions throughout their career [114]. Binge eating is common after these competition periods and causes athletes to gain back a similar amount of mass [114, 115]. The dangers of this are demonstrated by a case report of life-threatening hypokalemia and rhabdomyolysis in a 28-year-old bodybuilder who gained 10 kg in a 4-day eating binge shortly after a competition [116]. Another example has been reported for a different 28-year-old bodybuilder, who developed similar health issues after losing 19 kg prior to a bodybuilding contest and then consuming 800 g of carbohydrates daily for 5 days [117]. This “refeeding syndrome” might account for some of the deaths which happen within a week after a bodybuilding competition (of which there is one reported in Table 1, O.G.).
Rapid weight loss in sports is achieved through a combination of dietary practices, thermal stress, and/or diuretic usage. There are several documented cases of sudden death attributable to rapid weight loss, using a combination of intentional dehydration and thermal stress [118–120]. Severe effects of diuretic misuse have been reported in bodybuilders [121], with one case report describing a furosemide-induced 5–6 kg water loss 48 h before a competition leading to hypokalemic paralysis [122]. It is reasonable to suspect that bodybuilding deaths immediately before or after a competition could be a direct result of extreme weight cutting practices—attributable to extreme dehydration and/or major disturbances in micronutrient balance. Table 1 includes one female bodybuilder (A.H.) who died following diuretic abuse and one male (G.P.) who died 1 day before competition. However, these do not account for the deaths which occur outside of peak week or in former bodybuilders.
It is possible that repeated bouts of body mass loss and gain (“weight cycling”) can adversely affect long-term health [123], but direct evidence of this in athletes, let alone bodybuilders, is limited. Epidemiological studies examining the health effects of weight cycling generally come from obese patients and the general population and focus on surrogate outcomes (e.g. body composition, blood pressure, blood biomarkers) rather than morbidity and mortality [123]. The limited long-term research in weight cycling athletes suggests there may be some impact on metabolism and body composition [120], but findings are inconsistent. There is no research clearly showing a history of weight cycling increases the likelihood of morbidity or mortality later in life in any athletic population. Thus, there is not a convincing case for weight cycling to be a key risk factor for unexpected deaths outside of the competition phase or in retired bodybuilders.
Supplement Use
Bodybuilders typically use numerous supplements [124–127], which makes it difficult to isolate the effects of any one supplement from the interactions of multiple supplements, especially when combined with AAS. Supplementation can far exceed (i.e., > 1000%) the recommended daily allowance for various micronutrients [97, 128].
Bodybuilding supplements are commonly cited as a cause of morbidity. There is one case report of venous thromboembolism in a 24-year-old strength-trained individual who was ingesting 20 g of creatine in preparation for a bodybuilding competition [129], and other similar cases of severe renal dysfunction in otherwise healthy young adults [130–133]. Such case reports assume a cause-and-effect relationship, yet a wide body of research indicates that creatine is safe at the levels ingested [134]. Thus, it is uncertain if creatine may be unsafe under certain conditions (i.e., rare genetic risk factors) or if morbidity is related to other unrecognized factors. Branched chain amino acids (BCAA) are often used by bodybuilders and other athletes seeking to gain muscle mass, but emerging basic science [135] and clinical research suggest BCAA supplementation can promote thrombosis and other adverse effects [136]. However, there is no strong evidence to suggest BCAA supplements are causing significant adverse effects in athletes.
Bodybuilding supplements may also be contaminated with various drugs. Bodybuilders often intentionally seek out these supplements as an easy way to obtain pharmacologically active compounds, but unsuspecting fitness enthusiasts may also take such supplements hoping for a “natural” boost [137]. For example, selective androgen receptor modulators are banned by WADA, but were sold online as “green tea extract” and face moisturizers, even though the full pharmacological effects of the substances were unknown [138]. Likewise, tamoxifen (a drug used for breast cancer treatment) has been found in commercially available supplements [137]. Another study found multiple supplements sold in the USA contained stimulants such as 1,3-dimethylbutylamine (DMBA) and 1,3-dimethylamylamine (DMAA) [139]. At the time, DMBA had never been studied in humans, and DMAA had already been associated with cardiomyopathy, stroke, and death in humans (though difficult to prove a causation) [140]. The US Food and Drug Administration (FDA) has offered numerous warnings regarding contaminated bodybuilding drugs [141]. Analysis of 24 different dietary supplements targeted at bodybuilders in the UK revealed 23 contained AAS (including 12 with controlled substances) [142].
The dangers of contaminated supplements are evident in a 2004–2013 multi-state registry study, which prospectively identified 44 patients who experienced severe liver injury from bodybuilding supplements and 85 from non-bodybuilding supplements [143, 144]. Of those from bodybuilding supplements, 14 patients provided their supplements for chemical analysis; AAS were found in supplements provided by nine of these patients, but no AAS were identified in supplements from the other five patients [144]. A number of other dietary supplements have been linked to liver injury [145–148]. Thus, it seems clear that at least some dietary supplements can influence the long-term health of bodybuilders, but this is dependent upon dosage, contaminants, and interactions with other pharmacologically active substances.
Injections
Bodybuilders perform intramuscular injections for drug delivery (e.g., AAS, insulin, hGH, etc.) and for directly enhancing muscle appearance (i.e., oils to increase volume) [149], and this could increase risk of infectious disease. Prior to the introduction of recombinant hGH in 1985, hGH was only obtained from cadaver pituitaries. It was discovered that the supply was contaminated with the prion causing Creutzfeldt-Jakob disease, which left hGH-abusing athletes susceptible to infection [150]. Recombinant hGH has eliminated this risk, but poor needle-sharing practices could place bodybuilders at risk for other blood-borne diseases. Case reports in the 1980s and 1990s describe bodybuilders who became infected with HIV from sharing needles for AAS injection [151–153]. Similar cases exist for hepatitis C virus transmission in weightlifters [154].
The prevalence of HIV and viral hepatitis, as well as unsafe needle-sharing behaviors, have been studied in populations which inject performance-enhancing drugs. A cross-sectional survey of 395 men who used injectable performance-enhancing drugs found 1.5% had HIV and ~ 5–10% had viral hepatitis antibodies [155]. Similarly, a study of 63 (n = 23 bodybuilders) injectable-AAS users in Australia revealed ~ 10% prevalence for hepatitis C and ~ 12% for hepatitis B antibodies; however, these users did not share needles for AAS injection (but did for other drugs) and hepatitis was attributable to other high-risk behaviors [156]. In a similar study, injectable AAS users also reported not sharing needles, but did share multi-dose vials and used syringes to partition drugs—both risk factors for hepatitis and HIV [157]. However, these findings are not specific to bodybuilders. Current literature reveals bodybuilders share needles for AAS at a drastically lower rate (at least tenfold) than intravenous drug users (e.g. heroin addicts) and generally practice good hygiene for injections [158]. Thus, the risk for blood-borne viral infection from AAS and other injectable performance enhancing drugs is likely to be relatively low for most (but not all) bodybuilders. However, injectable oils and AAS can cause severe abscesses (which, in rare cases, can lead to septic shock [159]), pain, myositis, and compartment syndrome [149, 160–166]. There is little epidemiologic information regarding significant mortality or life-threatening morbidity from bodybuilding-related injections, but it should still be considered as a potential risk factor.
Challenges of Identifying Primary Risk Factors in Bodybuilders
As described throughout, bodybuilding involves a combination of multiple extreme behaviors, and it is possible that each of these factors can influence health independently of one another. Likewise, it seems likely that the interaction of all of these practices can greatly exacerbate risk. For instance, the potential deleterious effects of a high protein diet may be exacerbated by dehydration and AAS-related cardiovascular dysfunction (e.g., hypertension, increased hematocrit, etc.). Causation is not just an academic question; while elite bodybuilders may continue to perform all of these extreme behaviors together, non-competitive recreational bodybuilders and fitness enthusiasts may only partake in a few of these behaviors (e.g., using AAS but not consuming a cocktail of supplements and other drugs, or vice versa; performing extreme resistance exercise with a high protein diet, but not using AAS or other drugs). As such, it is worthwhile to determine how each of these extreme behaviors influence health.
Much of the literature on bodybuilder morbidity and mortality consists of case series and case reports. However, it is difficult to determine if any one factor is causative. This is epitomized by a case report which describes myocardial infarction in a 26-year-old male novice bodybuilder [101]. The patient began bodybuilding training 2 months earlier, but was training 4 h per day, consuming 500 g of whey protein per day in addition to 250 g of dietary protein, while also taking an appetite suppressant (and lost 6 kg body mass in the previous 2 months), branched chain amino acids supplement, and a mixture of anabolic steroids [101]. The patient’s body mass was unreported, but his BMI was 21.5 kg/m2 – so assuming a very conservative estimate of body mass of 90 kg, he was consuming at least 8.3 g/kg protein per day. He also had hepatitis A and was treated for this. It is nearly impossible to know if his outcome would have been different if he either did not use AAS or had a lower protein diet. Another case report describes a 32-year-old competitive bodybuilder who experienced rhabdomyolysis and fulminant liver failure with nearly fatal encephalopathy, but seemingly in the absence of AAS use [167]. The patient was taking dozens of different drugs (including multiple anabolic agents, but not AAS specifically) and supplements, but not recreational drugs [167].
There are dozens of papers attributing AAS use to morbidity or mortality in bodybuilders, but numerous potential confounders specific to bodybuilding are not reported. The lack of adequate patient history reporting is demonstrated in the literature examining kidney disease in bodybuilders. A 2022 systematic review identified 13 papers (case studies and case series) which describe acute or chronic kidney injury or disease in a total of 75 bodybuilders [168]. Across studies, there is inconsistent reporting of protein intake and history of AAS, vitamins (and other supplements), diuretics, or nonsteroidal anti-inflammatory drug (NSAID) use. Though many of the cases were attributed to AAS use, two of the case reports involved young (aged 19 and 24 years) males who denied using AAS, diuretics, and NSAIDs [133, 169].
Mortality Risk
There is little high-quality research directly examining the connection between AAS and morbidity/mortality rates in bodybuilders or other competitive athletes. However, research outside of the bodybuilding population may provide some insight into the relationship between AAS and premature death.
Elevated Mortality Rates in Confirmed AAS Users
Some of the best evidence for a connection between AAS and mortality arises from research conducted in countries which routinely perform drug testing on the general public. These policies exist in Belgium, Sweden, Denmark, and Norway [170, 171]. Gym members suspected of anabolic steroid usage (e.g., unusually muscular males) are subject to anti-doping testing and further investigation regarding drug use, even if they are not competitive athletes [170]. A 2019 retrospective cohort study compared all-cause mortality rates in 545 male laboratory-confirmed anabolic steroid users (who were identified as part of these anti-doping programs) with 5450 healthy controls consisting of randomly selected age-matched individuals from the Danish population and found a threefold higher mortality rate in the anabolic steroid users [172]. This study also revealed a threefold increase in nonischemic heart disease and fivefold increase in thromboembolic conditions. However, it must be emphasized that this study was not specific to bodybuilders and did not consider potential other related factors that may accompany AAS usage (e.g., recreational drug usage, supplement usage, etc.). Additionally, these testing scenarios include selection bias (“muscle profiling"), as anti-doping officials specifically target the most muscular looking individuals (who may be using other drugs), rather than a random sampling of gym users, AAS-users, or the general public [170, 171].
Elevated mortality rates have also been associated with AAS in other studies not limited to fit individuals. A study from the Swedish general population (i.e., not restricted to fitness centers) found men who had tested positive for non-therapeutic use of AAS had double the cardiovascular morbidity and mortality of those who tested negative, and approximately 18 times greater all-cause mortality rate than the general population [173]. In a sample of patients who tested within a Swedish university hospital, which included patients receiving care for psychiatric disorders and substance abuse, AAS use was associated with a greater risk for premature death, and also convulsions in those without a history of epilepsy or other similar disorders [174].
It must be recognized that “AAS users” represent a diverse group of individuals, including recreational athletes, non-bodybuilders aiming to improve aesthetics, prisoners, military personnel, and law enforcement officers [175–177]. Thus, it is not clear if mortality outcomes from studies examining these heterogeneous populations are generalizable to the bodybuilding population.
Elevated Mortality Rates in Athletes Participating in AAS-Using Sports
Less direct evidence of mortality risk from anabolic steroid use stems from epidemiologic data involving elite strength-focused athletes who competed in an era before drug testing was a standard component of sports. Excess mortality and suicide rate were increased under the age of 50 in Swedish athletes who competed in strength-focused sports from 1960 through 1979 [178]. However, for those who survived beyond that, mortality rate was comparable to the general population. Similarly, a higher mortality and suicide rate were identified in Finnish powerlifters who competed during a similar era; however, this study had a relatively small sample size (n = 62 powerlifters, with only 8 deaths during the study period). These studies point to a possible role of AAS use in premature deaths in suspected (albeit not confirmed) AAS users. However, one must also consider that AAS were reported to have been commonly used by Tour de France cyclists in the 1970s, yet cyclists from this era seem to have a substantially lower mortality rate than the general population, which is no different to their counterparts before the AAS era [179]. Thus, one must exercise caution in attributing AAS use as a primary causative factor for increased mortality reported in studies of strength-trained athletes, and consider other possible factors, including the strength-training itself, dietary protein and supplement intake, and other sport-specific issues.
Conclusions and Recommendations for Future Research
Bodybuilding is an internationally popular activity, which includes recreational and professional participants. Reports of premature deaths in the mainstream media, combined with case reports in medical literature suggest that bodybuilding seems to be associated with an increased mortality rate, and this is mostly attributed to AAS use. However, there is currently insufficient high-quality scientific evidence to support a causal link for either claim, especially given numerous plausible confounders.
We are not advocating for AAS use or denying the possibility that premature deaths are common in bodybuilders and exacerbated by AAS abuse. Rather, we are hoping to improve the quality of research in this realm, so that athletes and clinicians can make informed decisions. We believe the following research is necessary to better understand the health risks of bodybuilding:
Survival analysis should be used to examine the mortality rate in elite bodybuilders (e.g., Mr. Olympia competitors) and control for duration of elite career (i.e., total exposure to bodybuilding). The period of competition should be considered to determine whether the mortality rate has changed over time (e.g., due to different training and polypharmacy protocols). This research should attempt to examine comparative risk in natural versus AAS-using bodybuilders. However, the relatively short history of competitive natural bodybuilding may not be of sufficient duration to assess long-term mortality in that population.
The research above can be extended to include other strength-trained athletes (e.g., weightlifters, shot putters, etc.), to determine if bodybuilding-specific culture/practices have a distinct influence on mortality. Likewise, it would be beneficial to compare bodybuilders to other athletes who undergo physiological extremes (e.g., ultra-endurance athletes, including professional tour cyclists and ultramarathoners).
Case–control studies comparing drug-using bodybuilders versus natural bodybuilders can help determine the role of polypharmacy in cardiovascular risk factors. Ideally, these studies should be extended into the long-term to determine if physiologic parameters (e.g., echocardiography parameters, laboratory values) are predictive of morbidity and/or mortality risk.
Declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of interest
No competing interests: James Smoliga, Z. Taggart Wilber, and Brooks Robinson have all completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work. Brooks Robinson is employed at a sports supplement company but does not have any conflicts which influenced this work.
Author contributions
The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. JMS led the manuscript writing and revision. ZTW and BTR contributed substantially to identifying sources of information for background research, developing the key concepts described within the editorial, and reviewing and editing this manuscript. All authors read and approved the final manuscript.
References
- 1.Goldstein R. Jack LaLanne, Founder of modern fitness movement, dies at 96. New York Times. 2011.
- 2.Antero-Jacquemin J, Rey G, Marc A, Dor F, Haïda A, Marck A, et al. Mortality in female and male French Olympians: a 1948–2013 cohort study. Am J Sports Med. 2015;43(6):1505–1512. doi: 10.1177/0363546515574691. [DOI] [PubMed] [Google Scholar]
- 3.Saeidifard F, Medina-Inojosa JR, West CP, Olson TP, Somers VK, Bonikowske AR, et al. The association of resistance training with mortality: a systematic review and meta-analysis. Eur J Prev Cardiol. 2020;26(15):1647–1665. doi: 10.1177/2047487319850718. [DOI] [PubMed] [Google Scholar]
- 4.Kettunen JA, Kujala UM, Kaprio J, Bäckmand H, Peltonen M, Eriksson JG, et al. All-cause and disease-specific mortality among male, former elite athletes: an average 50-year follow-up. Br J Sports Med. 2015;49(13):893–897. doi: 10.1136/bjsports-2013-093347. [DOI] [PubMed] [Google Scholar]
- 5.Kujala UM, Tikkanen HO, Sarna S, Pukkala E, Kaprio J, Koskenvuo M. Disease-specific mortality among elite athletes. JAMA. 2001;285(1):44–45. doi: 10.1001/jama.285.1.44. [DOI] [PubMed] [Google Scholar]
- 6.Teramoto M, Bungum TJ. Mortality and longevity of elite athletes. J Sci Med Sport. 2010;13(4):410–416. doi: 10.1016/j.jsams.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 7.Sandomir R. Dave Draper, Bodybuilding’s ‘Blond Bomber,’ dies at 79. New York Times. 2021.
- 8.Williams A. Chris Dickerson, Who broke bodybuilding barriers, dies at 82. New York Times. 2022.
- 9.Goldfield GS. Body image, disordered eating and anabolic steroid use in female bodybuilders. Eat Disord. 2009;17(3):200–210. doi: 10.1080/10640260902848485. [DOI] [PubMed] [Google Scholar]
- 10.Hackett DA, Johnson NA, Chow C-M. Training practices and ergogenic aids used by male bodybuilders. J Strength Cond Res. 2013;27(6):1609–17. [DOI] [PubMed]
- 11.Tricker R, O'Neill MR, Cook D. The incidence of anabolic steroid use among competitive bodybuilders. J Drug Educ. 1989;19(4):313–325. doi: 10.2190/EGT5-4YWD-QX15-FLKK. [DOI] [PubMed] [Google Scholar]
- 12.Hartgens F, Kuipers H. Effects of androgenic-anabolic steroids in athletes. Sports Med. 2004;34(8):513–554. doi: 10.2165/00007256-200434080-00003. [DOI] [PubMed] [Google Scholar]
- 13.Gentil P, de Lira CAB, Paoli A, Dos Santos JAB, da Silva RDT, Junior JRP, et al. Nutrition, pharmacological and training strategies adopted by six bodybuilders: case report and critical review. Eur J Transl Myol. 2017;27(1):6247. doi: 10.4081/ejtm.2017.6247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moston S, Engelberg T. And justice for all? How anti-doping responds to ‘Innocent Mistakes’. Int J Sport Policy Polit. 2019;11(2):261–274. doi: 10.1080/19406940.2018.1550799. [DOI] [Google Scholar]
- 15.World Anti Doping Association. 2018 anti-doping testing figures.
- 16.Hurley BF, Seals DR, Hagberg JM, Goldberg AC, Ostrove SM, Holloszy JO, et al. High-density-lipoprotein cholesterol in bodybuilders v powerlifters Negative effects of androgen use. JAMA. 1984;252(4):507–513. doi: 10.1001/jama.1984.03350040037019. [DOI] [PubMed] [Google Scholar]
- 17.Lenders J, Demacker P, Vos J, Jansen P, Hoitsma A, Van't Laar A, et al. Deleterious effects of anabolic steroids on serum lipoproteins, blood pressure, and liver function in amateur body builders. Int J Sports Med. 1988;9(01):19–23. doi: 10.1055/s-2007-1024972. [DOI] [PubMed] [Google Scholar]
- 18.Ebenbichler CF, Kaser S, Bodner J, Gander R, Lechleitner M, Herold M, et al. Hyperhomocysteinemia in bodybuilders taking anabolic steroids. Eur J Internal Med. 2001;12(1):43–47. doi: 10.1016/S0953-6205(00)00131-X. [DOI] [PubMed] [Google Scholar]
- 19.Achar S, Rostamian A, Narayan SM. Cardiac and metabolic effects of anabolic-androgenic steroid abuse on lipids, blood pressure, left ventricular dimensions, and rhythm. Am J Cardiol. 2010;106(6):893–901. doi: 10.1016/j.amjcard.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smit DL, Grefhorst A, Buijs MM, de Hon O, den Heijer M, de Ronde W. Prospective study on blood pressure, lipid metabolism and erythrocytosis during and after androgen abuse. Andrologia. 2022;11:e14372. doi: 10.1111/and.14372. [DOI] [PubMed] [Google Scholar]
- 21.Smit DL, Voogel AJ, Heijer Md, Ronde Wd. Anabolic androgenic steroids induce reversible left ventricular hypertrophy and cardiac dysfunction. Echocardiography results of the HAARLEM study. Front Reproduct. Health. 2021;3:732318. doi: 10.3389/frph.2021.732318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smit DL, Buijs MM, de Hon O, den Heijer M, de Ronde W. Positive and negative side effects of androgen abuse. The HAARLEM study: a one-year prospective cohort study in 100 men. Scand J Med Sci Sports. 2021;31(2):427–438. doi: 10.1111/sms.13843. [DOI] [PubMed] [Google Scholar]
- 23.Alves RC, Prestes J, Enes A, de Moraes WMA, Trindade TB, de Salles BF, et al. Training programs designed for muscle hypertrophy in bodybuilders: a narrative review. Sports (Basel). 2020;8(11):149. doi: 10.3390/sports8110149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.D’Andrea A, Caso P, Salerno G, Scarafile R, De Corato G, Mita C, et al. Left ventricular early myocardial dysfunction after chronic misuse of anabolic androgenic steroids: a Doppler myocardial and strain imaging analysis. Br J Sports Med. 2007;41(3):149–155. doi: 10.1136/bjsm.2006.030171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baggish AL, Weiner RB, Kanayama G, Hudson JI, Picard MH, Hutter AM, Jr, et al. Long-term anabolic-androgenic steroid use is associated with left ventricular dysfunction. Circ Heart Fail. 2010;3(4):472–476. doi: 10.1161/CIRCHEARTFAILURE.109.931063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krieg A, Scharhag J, Albers T, Kindermann W, Urhausen A. Cardiac tissue Doppler in steroid users. Int J Sports Med. 2007;28(08):638–643. doi: 10.1055/s-2007-964848. [DOI] [PubMed] [Google Scholar]
- 27.Fyksen TS, Vanberg P, Gjesdal K, von Lueder TG, Bjørnerheim R, Steine K, et al. Cardiovascular phenotype of long‐term anabolic‐androgenic steroid abusers compared with strength‐trained athletes. Scand J Med Sci Sports. 2022;32(8):1170–81. [DOI] [PMC free article] [PubMed]
- 28.Ismail TF, Angell PJ, Jabbour A, Smith G, Wage R, Hewins B, et al. Cardiac effects of anabolic steroid use amongst recreational body builders—a CMR study. J Cardiovasc Magn Reson. 2012;14(1):P186. doi: 10.1186/1532-429X-14-S1-P186. [DOI] [Google Scholar]
- 29.Dickerman RD, Schaller F, Zachariah NY, McConathy WJ. Left ventricular size and function in elite bodybuilders using anabolic steroids. Clin J Sport Med. 1997;7(2):90–93. doi: 10.1097/00042752-199704000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Grandperrin A, Schnell F, Donal E, Galli E, Hedon C, Cazorla O, et al. Specific alterations of regional myocardial work in strength-trained athletes using anabolic steroids compared to athletes with genetic hypertrophic cardiomyopathy. J Sport Health Sci. 2022;S2095-2546(22)00078-3. [DOI] [PMC free article] [PubMed]
- 31.Thompson PD, Sadaniantz A, Cullinane EM, Bodziony KS, Catlin DH, Torek-Both G, et al. Left ventricular function is not impaired in weight-lifters who use anabolic steroids. J Am Coll Cardiol. 1992;19(2):278–282. doi: 10.1016/0735-1097(92)90478-6. [DOI] [PubMed] [Google Scholar]
- 32.Barbosa Neto O, da Mota GR, De Sordi CC, Resende EAMR, Resende LAPR, Vieira da Silva MA, et al. Long-term anabolic steroids in male bodybuilders induce cardiovascular structural and autonomic abnormalities. Clin Auton Res. 2018;28(2):231–244. doi: 10.1007/s10286-017-0470-2. [DOI] [PubMed] [Google Scholar]
- 33.Dickerman RD, Schaller F, McConathy WJ. Left ventricular wall thickening does occur in elite power athletes with or without anabolic steroid use. Cardiology. 1998;90(2):145–148. doi: 10.1159/000006834. [DOI] [PubMed] [Google Scholar]
- 34.Salke RC, Rowland TW, Burke EJ. Left ventricular size and function in body builders using anabolic steroids. Med Sci Sports Exerc. 1985;17(6):701–704. doi: 10.1249/00005768-198512000-00014. [DOI] [PubMed] [Google Scholar]
- 35.Riebe D, Fernhall B. Left ventricular function during exercise and creatine kinase MB levels in anabolic steroid users and nonusers. Sports Med Train Rehabil. 1993;4(1):57–65. doi: 10.1080/15438629309511967. [DOI] [Google Scholar]
- 36.Angell PJ, Green DJ, Lord R, Gaze D, Whyte G, George KP. Acute cardiovascular responses to resistance exercise in anabolic steroids users: a preliminary investigation. Sci Sports. 2018;33(6):339–346. doi: 10.1016/j.scispo.2018.05.003. [DOI] [Google Scholar]
- 37.Lalande S, Baldi JC. Left ventricular mass in elite Olympic weight lifters. Am J Cardiol. 2007;100(7):1177–1180. doi: 10.1016/j.amjcard.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 38.Barone M, Losurdo G, Iannone A, Leandro G, Di Leo A, Trerotoli P. Assessment of body composition: intrinsic methodological limitations and statistical pitfalls. Nutrition. 2022;102:111736. doi: 10.1016/j.nut.2022.111736. [DOI] [PubMed] [Google Scholar]
- 39.Lichtenbelt W, Hartgens F, Vollaard NB, Ebbing S, Kuipers H. Body composition changes in bodybuilders: a method comparison. Med Sci Sports Exerc. 2004;195(9131/04):3603–4490. doi: 10.1249/01.mss.0000117159.70295.73. [DOI] [PubMed] [Google Scholar]
- 40.DuBois D, DuBois E. A formula to estimate the approximate surface area if height and body mass be known. Arch Intern Med. 1916;17:863–871. doi: 10.1001/archinte.1916.00080130010002. [DOI] [Google Scholar]
- 41.Shuter B, Aslani A. Body surface area: Du bois and Du bois revisited. Eur J Appl Physiol. 2000;82(3):250–254. doi: 10.1007/s004210050679. [DOI] [PubMed] [Google Scholar]
- 42.Redlarski G, Palkowski A, Krawczuk M. Body surface area formulae: an alarming ambiguity. Sci Rep. 2016;6(1):27966. doi: 10.1038/srep27966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hoit BD, Litwin SE. The new normal: how should we assess cardiac chamber sizes and proportionality across the full spectrum of body sizes with varying degrees of adiposity? J Am Soc Echocardiogr. 2022;35(2):151–153. doi: 10.1016/j.echo.2021.11.013. [DOI] [PubMed] [Google Scholar]
- 44.Nabeshima Y, Takeuchi M. Is body surface area the best method to scale cardiac size? J Am Soc Echocardiogr. 2022;35(11):1193–94. doi: 10.1016/j.echo.2022.04.009. [DOI] [PubMed] [Google Scholar]
- 45.Paylik G, Olexó Z, Frenkl R. Echocardiographic estimates related to various body size measures in athletes. Acta Physiol Hung. 1996;84(2):171–181. [PubMed] [Google Scholar]
- 46.Rasmussen JJ, Schou M, Madsen PL, Selmer C, Johansen ML, Ulriksen PS, et al. Cardiac systolic dysfunction in past illicit users of anabolic androgenic steroids. Am Heart J. 2018;203:49–56. doi: 10.1016/j.ahj.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 47.De Piccoli B, Giada F, Benettin A, Sartori F, Piccolo E. Anabolic steroid use in body builders: an echocardiographic study of left ventricle morphology and function. Int J Sports Med. 1991;12(04):408–412. doi: 10.1055/s-2007-1024703. [DOI] [PubMed] [Google Scholar]
- 48.Shankara-Narayana N, Yu C, Savkovic S, Desai R, Fennell C, Turner L, et al. Rate and extent of recovery from reproductive and cardiac dysfunction due to androgen abuse in men. J Clin Endocrinol Metab. 2020;105(6):1827–1839. doi: 10.1210/clinem/dgz324. [DOI] [PubMed] [Google Scholar]
- 49.Nieminen MS, Rämö M, Viitasalo M, Heikkilä P, Karjalainen J, Mäntysaari M, et al. Serious cardiovascular side effects of large doses of anabolic steroids in weight lifters. Eur Heart J. 1996;17(10):1576–1583. doi: 10.1093/oxfordjournals.eurheartj.a014724. [DOI] [PubMed] [Google Scholar]
- 50.Kosaka A, Takahashi H, Yajima Y, Tanaka M, Okamura K, Mizumoto R, et al. Hepatocellular carcinoma associated with anabolic steroid therapy: report of a case and review of the Japanese literature. J Gastroenterol. 1996;31(3):450–454. doi: 10.1007/BF02355039. [DOI] [PubMed] [Google Scholar]
- 51.Johnson FL, Lerner K, Siegel M, Feagler J, Majerus P, Hartmann J, et al. Association of androgenic-anabolic steroid therapy with development of hepatocellular carcinoma. Lancet. 1972;300(7790):1273–1276. doi: 10.1016/S0140-6736(72)92649-9. [DOI] [PubMed] [Google Scholar]
- 52.Gorayski P, Thompson C, Subhash H, Thomas A. Hepatocellular carcinoma associated with recreational anabolic steroid use. Br J Sports Med. 2008;42(1):74–75. doi: 10.1136/bjsm.2007.03932. [DOI] [PubMed] [Google Scholar]
- 53.Solbach P, Potthoff A, Raatschen H-J, Soudah B, Lehmann U, Schneider A, et al. Testosterone-receptor positive hepatocellular carcinoma in a 29-year old bodybuilder with a history of anabolic androgenic steroid abuse: a case report. BMC Gastroenterol. 2015;15(1):1–7. doi: 10.1186/s12876-015-0288-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Socas L, Zumbado M, Perez-Luzardo O, Ramos A, Perez C, Hernandez J, et al. Hepatocellular adenomas associated with anabolic androgenic steroid abuse in bodybuilders: a report of two cases and a review of the literature. Br J Sports Med. 2005;39(5):e27. doi: 10.1136/bjsm.2004.013599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kanayama G, Hudson JI, DeLuca J, Isaacs S, Baggish A, Weiner R, et al. Prolonged hypogonadism in males following withdrawal from anabolic–androgenic steroids: an under-recognized problem. Addiction. 2015;110(5):823–831. doi: 10.1111/add.12850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rasmussen JJ, Selmer C, Østergren PB, Pedersen KB, Schou M, Gustafsson F, et al. Former abusers of anabolic androgenic steroids exhibit decreased testosterone levels and hypogonadal symptoms years after cessation: a case-control study. PLoS ONE. 2016;11(8):e0161208. doi: 10.1371/journal.pone.0161208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Urhausen A, Torsten A, Wilfried K. Reversibility of the effects on blood cells, lipids, liver function and hormones in former anabolic–androgenic steroid abusers. J Steroid Biochem Mol Biol. 2003;84(2):369–375. doi: 10.1016/S0960-0760(03)00105-5. [DOI] [PubMed] [Google Scholar]
- 58.Maron BJ, Haas TS, Murphy CJ, Ahluwalia A, Rutten-Ramos S. Incidence and causes of sudden death in US College athletes. J Am Coll Cardiol. 2014;63(16):1636–1643. doi: 10.1016/j.jacc.2014.01.041. [DOI] [PubMed] [Google Scholar]
- 59.Ahlgrim C, Guglin M. Anabolics and cardiomyopathy in a bodybuilder: case report and literature review. J Cardiac Fail. 2009;15(6):496–500. doi: 10.1016/j.cardfail.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 60.Dufayet L, Gorgiard C, Vayssette F, Barbet JP, Hoizey G, Ludes B. Death of an apprentice bodybuilder following 2,4-dinitrophenol and clenbuterol intake. Int J Legal Med. 2020;134(3):1003–1006. doi: 10.1007/s00414-020-02268-2. [DOI] [PubMed] [Google Scholar]
- 61.Lehmann S, Thomas A, Schiwy-Bochat K-H, Geyer H, Thevis M, Glenewinkel F, et al. Death after misuse of anabolic substances (clenbuterol, stanozolol and metandienone) Forensic Sci Int. 2019;303:109925. doi: 10.1016/j.forsciint.2019.109925. [DOI] [PubMed] [Google Scholar]
- 62.Li C, Adhikari BK, Gao L, Zhang S, Liu Q, Wang Y, et al. Performance-enhancing drugs abuse caused cardiomyopathy and acute hepatic injury in a young bodybuilder. Am J Mens Health. 2018;12(5):1700–1704. doi: 10.1177/1557988318783504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dickerman RD, Schaller F, Prather I, McConathy W. Sudden cardiac death in a 20-year-old bodybuilder using anabolic steroids. Cardiology. 1995;86(2):172–173. doi: 10.1159/000176867. [DOI] [PubMed] [Google Scholar]
- 64.Lemiński A, Kubis M, Kaczmarek K, Gołąb A, Kazimierczak A, Kotfis K, et al. When bodybuilding goes wrong—bilateral renal artery thrombosis in a long-term misuser of anabolic steroids treated with angiojet rheolytic thrombectomy. Int J Environ Res Public Health. 2022;19(4):2122. doi: 10.3390/ijerph19042122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Falkenberg M, Karlsson J, Örtenwall P. Peripheral arterial thrombosis in two young men using anabolic steroids. Eur J Vasc Endovasc Surg. 1997;13(2):223–226. doi: 10.1016/S1078-5884(97)80025-1. [DOI] [PubMed] [Google Scholar]
- 66.Baumann S, Jabbour C, Huseynov A, Borggrefe M, Haghi D, Papavassiliu T. Myocardial scar detected by cardiovascular magnetic resonance in a competitive bodybuilder with longstanding abuse of anabolic steroids. Asian J Sports Med. 2014;5(4):e24058. doi: 10.5812/asjsm.24058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Katsi V, Soulaidopoulos S, Aggeli C, Latsios G, Tousoulis D, Toutouzas K, et al. Extensive coronary artery disease in a long-distance athlete: a case report. J Athl Train. 2020;56(10):1137–1141. doi: 10.4085/JAT0330-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Goel R, Majeed F, Vogel R, Corretti MC, Weir M, Mangano C, et al. Exercise-induced hypertension, endothelial dysfunction, and coronary artery disease in a marathon runner. Am J Cardiol. 2007;99(5):743–744. doi: 10.1016/j.amjcard.2006.09.127. [DOI] [PubMed] [Google Scholar]
- 69.Handler JB, Asay RW, Warren SE, Shea PM. Symptomatic coronary artery disease in a marathon runner. JAMA. 1982;248(6):717–719. doi: 10.1001/jama.1982.03330060057035. [DOI] [PubMed] [Google Scholar]
- 70.Angeli SJ, Haft JI. Severe coronary artery disease in a marathon runner. Chest. 1987;91(2):271–272. doi: 10.1378/chest.91.2.271. [DOI] [PubMed] [Google Scholar]
- 71.Tan KL, Kandasamy B. TCTAP C-001 fate of a modern day pheidippides: acute coronary thrombosis in a young marathon runner. J Am Coll Cardiol. 2018;71(16_Supplement):S69. doi: 10.1016/j.jacc.2018.03.206. [DOI] [Google Scholar]
- 72.Hull CM, Hopkins CL, Purdy NJ, Lloyd RC, Harris JA. A case of unprovoked venous thromboembolism in a marathon athlete presenting atypical sequelae: What are the chances? Scand J Med Sci Sports. 2015;25(5):699–705. doi: 10.1111/sms.12262. [DOI] [PubMed] [Google Scholar]
- 73.Bishop M, Astolfi M, Padegimas E, DeLuca P, Hammoud S. Venous thromboembolism within professional American Sport Leagues. Orthop J Sports Med. 2017;5(12):2325967117745530. doi: 10.1177/2325967117745530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hull CM, Harris JA. Venous thromboembolism in physically active people: considerations for risk assessment, mainstream awareness and future research. Sports Med. 2015;45(10):1365–1372. doi: 10.1007/s40279-015-0360-5. [DOI] [PubMed] [Google Scholar]
- 75.Dhamu H, Malliaras P, Twycross-Lewis R, Maffulli N. A systematic review of resting left ventricular systolic and diastolic function and adaptation in elite weightlifters. Br Med Bull. 2012;104(1):129–141. doi: 10.1093/bmb/lds025. [DOI] [PubMed] [Google Scholar]
- 76.Adler Y, Fisman EZ, Koren-Morag N, Tanne D, Shemesh J, Lasry E, et al. Left ventricular diastolic function in trained male weightlifters at rest and during isometric exercise. Am J Cardiol. 2008;102(1):97–101. doi: 10.1016/j.amjcard.2008.02.105. [DOI] [PubMed] [Google Scholar]
- 77.Eijsvogels TMH, Thompson PD, Franklin BA. The "Extreme Exercise Hypothesis": recent findings and cardiovascular health implications. Curr Treat Options Cardiovasc Med. 2018;20(10):84. doi: 10.1007/s11936-018-0674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.MacDougall JD, Tuxen D, Sale DG, Moroz JR, Sutton JR. Arterial blood pressure response to heavy resistance exercise. J Appl Physiol (Bethesda, Md: 1985). 1985;58(3):785–790. doi: 10.1152/jappl.1985.58.3.785. [DOI] [PubMed] [Google Scholar]
- 79.Sullivan J, Hanson P, Rahko PS, Folts JD. Continuous measurement of left ventricular performance during and after maximal isometric deadlift exercise. Circulation. 1992;85(4):1406–1413. doi: 10.1161/01.CIR.85.4.1406. [DOI] [PubMed] [Google Scholar]
- 80.Augustine DX, Howard L. Left ventricular hypertrophy in athletes: differentiating physiology from pathology. Curr Treat Options Cardiovasc Med. 2018;20(12):96. doi: 10.1007/s11936-018-0691-2. [DOI] [PubMed] [Google Scholar]
- 81.D’Ascenzi F, Solari M, Corrado D, Zorzi A, Mondillo S. Diagnostic differentiation between arrhythmogenic cardiomyopathy and athlete’s heart by using imaging. JACC Cardiovasc Imaging. 2018;11(9):1327–1339. doi: 10.1016/j.jcmg.2018.04.031. [DOI] [PubMed] [Google Scholar]
- 82.Danielian A, Shah AB. Differentiating physiology from pathology: the Gray zones of the athlete’s heart. Clin Sports Med. 2022;41(3):425–440. doi: 10.1016/j.csm.2022.02.005. [DOI] [PubMed] [Google Scholar]
- 83.Millar LM, Fanton Z, Finocchiaro G, Sanchez-Fernandez G, Dhutia H, Malhotra A, et al. Differentiation between athlete’s heart and dilated cardiomyopathy in athletic individuals. Heart. 2020;106(14):1059–1065. doi: 10.1136/heartjnl-2019-316147. [DOI] [PubMed] [Google Scholar]
- 84.Graham MR, Grace FM, Boobier W, Hullin D, Kicman A, Cowan D, et al. Homocysteine induced cardiovascular events: a consequence of long term anabolic-androgenic steroid (AAS) abuse. Br J Sports Med. 2006;40(7):644–648. doi: 10.1136/bjsm.2005.025668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Baggish AL, Wang F, Weiner RB, Elinoff JM, Tournoux F, Boland A, et al. Training-specific changes in cardiac structure and function: a prospective and longitudinal assessment of competitive athletes. J Appl Physiol. 2008;104(4):1121–1128. doi: 10.1152/japplphysiol.01170.2007. [DOI] [PubMed] [Google Scholar]
- 86.Weiner RB, Wang F, Isaacs SK, Malhotra R, Berkstresser B, Kim JH, et al. Blood pressure and left ventricular hypertrophy during American-style football participation. Circulation. 2013;128(5):524–531. doi: 10.1161/CIRCULATIONAHA.113.003522. [DOI] [PubMed] [Google Scholar]
- 87.Tso JV, Turner CG, Liu C, Galante A, Gilson CR, Clark C, et al. Association between race and maladaptive concentric left ventricular hypertrophy in American-style football athletes. Br J Sports Med. 2022;56(3):151–157. doi: 10.1136/bjsports-2021-104333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hackett DA. Training, supplementation, and pharmacological practices of competitive male bodybuilders across training phases. J Strength Cond Res. 2022;36(4):963–970. doi: 10.1519/JSC.0000000000003989. [DOI] [PubMed] [Google Scholar]
- 89.Chappell A, Simper T, Barker M. Nutritional strategies of high level natural bodybuilders during competition preparation. J Int Soc Sports Nutr. 2018;15(1):4. doi: 10.1186/s12970-018-0209-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chappell AJ, Simper TN. Nutritional peak week and competition day strategies of competitive natural bodybuilders. Sports. 2018;6(4):126. doi: 10.3390/sports6040126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Escalante G, Stevenson SW, Barakat C, Aragon AA, Schoenfeld BJ. Peak week recommendations for bodybuilders: an evidence based approach. BMC Sports Sci Med Rehabil. 2021;13(1):68. doi: 10.1186/s13102-021-00296-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schwingshackl L, Hoffmann G. Comparison of high vs. normal/low protein diets on renal function in subjects without chronic kidney disease: a systematic review and meta-analysis. PLoS ONE. 2014;9(5):e97656. doi: 10.1371/journal.pone.0097656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Marinaro M, Alexander DS, de Waal D. Do the high‐protein recommendations for athletes set some on a path to kidney injury and dialysis? Seminars in dialysis; 2021. Wiley Online Library; 2021. [DOI] [PubMed]
- 94.Jhee JH, Kee YK, Park S, Kim H, Park JT, Han SH, et al. High-protein diet with renal hyperfiltration is associated with rapid decline rate of renal function: a community-based prospective cohort study. Nephrol Dial Transplant. 2019;35(1):98–106. doi: 10.1093/ndt/gfz115. [DOI] [PubMed] [Google Scholar]
- 95.Haring B, Selvin E, Liang M, Coresh J, Grams ME, Petruski-Ivleva N, et al. Dietary protein sources and risk for incident chronic kidney disease: results from the Atherosclerosis Risk in Communities (ARIC) study. J Ren Nutr. 2017;27(4):233–242. doi: 10.1053/j.jrn.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cho E, Choi SJ, Kang D-H, Kalantar-Zadeh K, Ko G-J. Revisiting glomerular hyperfiltration and examining the concept of high dietary protein-related nephropathy in athletes and bodybuilders. Curr Opin Nephrol Hypertens. 2022;31(1):18–25. doi: 10.1097/MNH.0000000000000755. [DOI] [PubMed] [Google Scholar]
- 97.Spendlove J, Mitchell L, Gifford J, Hackett D, Slater G, Cobley S, et al. Dietary intake of competitive bodybuilders. Sports Med. 2015;45(7):1041–1063. doi: 10.1007/s40279-015-0329-4. [DOI] [PubMed] [Google Scholar]
- 98.Jäger R, Kerksick CM, Campbell BI, Cribb PJ, Wells SD, Skwiat TM, et al. International society of sports nutrition position stand: protein and exercise. J Int Soc Sports Nutr. 2017;14(1):20. doi: 10.1186/s12970-017-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kerksick CM, Wilborn CD, Roberts MD, Smith-Ryan A, Kleiner SM, Jäger R, et al. ISSN exercise & sports nutrition review update: research & recommendations. J Int Soc Sports Nutr. 2018;15(1):38. doi: 10.1186/s12970-018-0242-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Thomas DT, Erdman KA, Burke LM. Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: nutrition and athletic performance. J Acad Nutr Diet. 2016;116(3):501–528. doi: 10.1016/j.jand.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 101.Jain V, Goel G. Acute myocardial infarction in young newbie bodybuilder using multiple steroid and protein supplements. J Cardiol Cases. 2020;21(4):134–136. doi: 10.1016/j.jccase.2019.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ribeiro AS, Nunes JP, Schoenfeld BJ. Should competitive bodybuilders ingest more protein than current evidence-based recommendations? Sports Med. 2019;49(10):1481–1485. doi: 10.1007/s40279-019-01111-y. [DOI] [PubMed] [Google Scholar]
- 103.Antonio J, Ellerbroek A, Silver T, Vargas L, Peacock C. The effects of a high protein diet on indices of health and body composition—a crossover trial in resistance-trained men. J Int Soc Sports Nutr. 2016;13(1):3. doi: 10.1186/s12970-016-0114-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Antonio J, Ellerbroek A, Silver T, Orris S, Scheiner M, Gonzalez A, et al. A high protein diet (3.4 g/kg/d) combined with a heavy resistance training program improves body composition in healthy trained men and women—a follow-up investigation. J Int Soc Sports Nutr. 2015;12(1):39. doi: 10.1186/s12970-015-0100-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Antonio J, Ellerbroek A, Silver T, Vargas L, Tamayo A, Buehn R, et al. A high protein diet has no harmful effects: a one-year crossover study in resistance-trained males. J Nutr Metab. 2016;2016:9104792. doi: 10.1155/2016/9104792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Antonio J, Peacock CA, Ellerbroek A, Fromhoff B, Silver T. The effects of consuming a high protein diet (4.4 g/kg/d) on body composition in resistance-trained individuals. J Int Soc Sports Nutr. 2014;11(1):19. doi: 10.1186/1550-2783-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kayapinar O, Ozde C, Koc Ay E, Keskin M, Kaya A. Anterior myocardial infarction in a 26-year-old body builder with concomitant use of whey protein powder and amino acid capsules. Acta Cardiol Sin. 2018;34(4):359–362. doi: 10.6515/ACS.201807_34(4).20180306A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rencuzogullari I, Börekçi A, Karakoyun S, Cagdas M, Karabağ Y, Yesin M, et al. Coronary thrombosis in three coronary arteries due to whey protein. Am J Emerg Med. 2017;35(4):664e3–e4. doi: 10.1016/j.ajem.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 109.Simonart T. Acne and whey protein supplementation among bodybuilders. Dermatology. 2012;225(3):256–258. doi: 10.1159/000345102. [DOI] [PubMed] [Google Scholar]
- 110.Silverberg NB. Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes. Cutis. 2012;90(2):70–2. [PubMed] [Google Scholar]
- 111.Melnik B, Jansen T, Grabbe S. Abuse of anabolic-androgenic steroids and bodybuilding acne: an underestimated health problem. JDDG Journal der Deutschen Dermatologischen Gesellschaft. 2007;5(2):110–7. doi: 10.1111/j.1610-0387.2007.06176.x. [DOI] [PubMed] [Google Scholar]
- 112.Titelius R. Mandurah mum's use of protein shakes being blamed for contributing to her death. West Aust. 2017;12:2017. [Google Scholar]
- 113.Ali AA, Almukhtar SE, Sharif DA, Saleem ZSM, Muhealdeen DN, Hughson MD. Effects of bodybuilding supplements on the kidney: a population-based incidence study of biopsy pathology and clinical characteristics among Middle Eastern men. BMC Nephrol. 2020;21(1):164. doi: 10.1186/s12882-020-01834-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Andersen RE, Brownell KD, Morgan GD, Bartlett SJ. Weight loss, psychological, and nutritional patterns in competitive female bodybuilders. Eat Disord. 1998;6(2):159–167. doi: 10.1080/10640269808251251. [DOI] [PubMed] [Google Scholar]
- 115.Andersen RE, Barlett SJ, Morgan GD, Brownell KD. Weight loss, psychological, and nutritional patterns in competitive male body builders. Int J Eat Disord. 1995;18(1):49–57. doi: 10.1002/1098-108X(199507)18:1<49::AID-EAT2260180106>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 116.Lee TW, Bae E, Hwang K, Jang HN, Park HJ, Jeon DH, et al. Severe hypokalemic paralysis and rhabdomyolysis occurring after binge eating in a young bodybuilder: case report. Medicine (Baltimore) 2017;96(40):e8251. doi: 10.1097/MD.0000000000008251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lapinskienė I, Mikulevičienė G, Laubner G, Badaras R. Consequences of an extreme diet in the professional sport: refeeding syndrome to a bodybuilder. Clin Nutr ESPEN. 2018;23:253–5. doi: 10.1016/j.clnesp.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 118.Franchini E, Brito CJ, Artioli GG. Weight loss in combat sports: physiological, psychological and performance effects. J Int Soc Sports Nutr. 2012;9(1):52. doi: 10.1186/1550-2783-9-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Burke LM, Slater GJ, Matthews JJ, Langan-Evans C, Horswill CA. ACSM expert consensus statement on weight loss in weight-category sports. Curr Sports Med Rep. 2021;20(4):199–217. doi: 10.1249/JSR.0000000000000831. [DOI] [PubMed] [Google Scholar]
- 120.Lakicevic N, Mani D, Paoli A, Roklicer R, Bianco A, Drid P. Weight cycling in combat sports: revisiting 25 years of scientific evidence. BMC Sports Sci Med Rehabil. 2021;13(1):154. doi: 10.1186/s13102-021-00381-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Pfisterer N, Stöllberger C, Finsterer J. Severe acquired hypokalemic paralysis in a bodybuilder after self-medication with triamterene/hydrochlorothiazide. Clin J Sport Med. 2020;30(5):e172–4. doi: 10.1097/JSM.0000000000000763. [DOI] [PubMed] [Google Scholar]
- 122.Mayr FB, Domanovits H, Laggner AN. Hypokalemic paralysis in a professional bodybuilder. Am J Emerg Med. 2012;30(7):1324.e5–e8. doi: 10.1016/j.ajem.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 123.Montani J-P, Viecelli A, Prévot A, Dulloo AG. Weight cycling during growth and beyond as a risk factor for later cardiovascular diseases: the ‘repeated overshoot’theory. Int J Obes. 2006;30(4):S58–S66. doi: 10.1038/sj.ijo.0803520. [DOI] [PubMed] [Google Scholar]
- 124.Knapik JJ, Steelman RA, Hoedebecke SS, Austin KG, Farina EK, Lieberman HR. Prevalence of dietary supplement use by athletes: systematic review and meta-analysis. Sports Med. 2016;46(1):103–23. doi: 10.1007/s40279-015-0387-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Montuori P, Loperto I, Paolo C, Castrianni D, Nubi R, De Rosa E, et al. Bodybuilding, dietary supplements and hormones use: behaviour and determinant analysis in young bodybuilders. BMC Sports Sci Med Rehabil. 2021;13(1):147. doi: 10.1186/s13102-021-00378-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Karimian J, Esfahani PS. Supplement consumption in body builder athletes. J Res Med Sci. 2011;16(10):1347–1353. [PMC free article] [PubMed] [Google Scholar]
- 127.Perry PJ, Lund BC, Deninger MJ, Kutscher EC, Schneider J. Anabolic steroid use in weightlifters and bodybuilders: an internet survey of drug utilization. Clin J Sport Med. 2005;15(5):326–30. doi: 10.1097/01.jsm.0000180872.22426.bb. [DOI] [PubMed] [Google Scholar]
- 128.Kuehn BM. Bodybuilding supplements. JAMA. 2008;299(24):2847. [Google Scholar]
- 129.Lee SH, Seo JA, Park JE, Kim CH, Lee J. A case of pulmonary thromboembolism possibly associated with the use of creatine supplements. Respirol Case Rep. 2022;10(4):e0932. doi: 10.1002/rcr2.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tan CW, Tha MH, Ng HJ. Creatine supplementation and venous thrombotic events. Am J Med. 2014;127(8):e7–e8. doi: 10.1016/j.amjmed.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 131.Taner B, Aysim O, Abdulkadir U. The effects of the recommended dose of creatine monohydrate on kidney function. NDT Plus. 2010;4(1):23–24. doi: 10.1093/ndtplus/sfq177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Koshy KM, Griswold E, Schneeberger EE. Interstitial nephritis in a patient taking creatine. N Engl J Med. 1999;340(10):814–815. doi: 10.1056/NEJM199903113401017. [DOI] [PubMed] [Google Scholar]
- 133.Thorsteinsdottir B, Grande JP, Garovic VD. Acute renal failure in a young weight lifter taking multiple food supplements, including creatine monohydrate. J Ren Nutr. 2006;16(4):341–345. doi: 10.1053/j.jrn.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 134.Greenhaff P. Renal dysfunction accompanying oral creatine supplements. Lancet. 1998;352(9123):233. doi: 10.1016/S0140-6736(05)77834-X. [DOI] [PubMed] [Google Scholar]
- 135.Xu Y, Jiang H, Li L, Chen F, Liu Y, Zhou M, et al. Branched-chain amino acid catabolism promotes thrombosis risk by enhancing tropomodulin-3 propionylation in platelets. Circulation. 2020;142(1):49–64. doi: 10.1161/CIRCULATIONAHA.119.043581. [DOI] [PubMed] [Google Scholar]
- 136.Manuel M, Heckman CJ. Stronger is not always better: could a bodybuilding dietary supplement lead to ALS? Exp Neurol. 2011;228(1):5–8. doi: 10.1016/j.expneurol.2010.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Evans-Brown M, Kimergård A, McVeigh J, Chandler M, Brandt SD. Is the breast cancer drug tamoxifen being sold as a bodybuilding dietary supplement? BMJ Br Med J. 2014;348:g1476. doi: 10.1136/bmj.g1476. [DOI] [PubMed] [Google Scholar]
- 138.Thevis M, Geyer H, Kamber M, Schänzer W. Detection of the arylpropionamide-derived selective androgen receptor modulator (SARM) S-4 (Andarine) in a black-market product. Drug Test Anal. 2009;1(8):387–392. doi: 10.1002/dta.91. [DOI] [PubMed] [Google Scholar]
- 139.Cohen PA, Travis JC, Venhuis BJ. A synthetic stimulant never tested in humans, 1, 3-dimethylbutylamine (DMBA), is identified in multiple dietary supplements. Drug Test Anal. 2015;7(1):83–87. doi: 10.1002/dta.1735. [DOI] [PubMed] [Google Scholar]
- 140.Cohen PA. DMAA as a dietary supplement ingredient. Arch Intern Med. 2012;172(13):1038–1039. doi: 10.1001/archinternmed.2012.1677. [DOI] [PubMed] [Google Scholar]
- 141.United States Food and Drug Administration. Tainted products marketed as dietary supplements. 2020 [cited 2022 September 19]. Available from: https://www.fda.gov/about-fda/fda-pharmacy-student-experiential-program/tainted-products-marketed-dietary-supplements.
- 142.Abbate V, Kicman AT, Evans-Brown M, McVeigh J, Cowan DA, Wilson C, et al. Anabolic steroids detected in bodybuilding dietary supplements—a significant risk to public health. Drug Test Anal. 2015;7(7):609–618. doi: 10.1002/dta.1728. [DOI] [PubMed] [Google Scholar]
- 143.Navarro VJ, Barnhart H, Bonkovsky HL, Davern T, Fontana RJ, Grant L, et al. Liver injury from herbals and dietary supplements in the US Drug-Induced Liver Injury Network. Hepatology. 2014;60(4):1399–1408. doi: 10.1002/hep.27317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Stolz A, Navarro V, Hayashi PH, Fontana RJ, Barnhart HX, Gu J, et al. Severe and protracted cholestasis in 44 young men taking bodybuilding supplements: assessment of genetic, clinical and chemical risk factors. Aliment Pharmacol Ther. 2019;49(9):1195–1204. doi: 10.1111/apt.15211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kuehn BM. Dietary supplement linked to cases of acute hepatitis. JAMA. 2013;310(17):1784. doi: 10.1001/jama.2013.281868. [DOI] [PubMed] [Google Scholar]
- 146.Roytman MM, Pörzgen P, Lee CL, Huddleston L, Kuo TT, Bryant-Greenwood P, et al. Outbreak of severe hepatitis linked to weight-loss supplement OxyELITE Pro. Off J Am Coll Gastroenterol ACG. 2014;109(8):1296–8. doi: 10.1038/ajg.2014.159. [DOI] [PubMed] [Google Scholar]
- 147.Timcheh-Hariri A, Balali-Mood M, Aryan E, Sadeghi M, Riahi-Zanjani B. Toxic hepatitis in a group of 20 male body-builders taking dietary supplements. Food Chem Toxicol. 2012;50(10):3826–32. doi: 10.1016/j.fct.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 148.Villavicencio Kim J, Wu GY. Body building and aminotransferase elevations: a review. J Clin Transl Hepatol. 2020;8(2):161–167. doi: 10.14218/JCTH.2020.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Schäfer CN, Hvolris J, Karlsmark T, Plambech M. Muscle enhancement using intramuscular injections of oil in bodybuilding: review on epidemiology, complications, clinical evaluation and treatment. Eur Surg. 2012;44(2):109–115. doi: 10.1007/s10353-011-0033-z. [DOI] [Google Scholar]
- 150.Perry HM. Risk of Creutzfeldt-Jakob disease in bodybuilders. BMJ (Clin Res Ed) 1993;307(6907):803. doi: 10.1136/bmj.307.6907.803-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Scott MJ. HIV infection associated with injections of anabolic steroids. JAMA. 1989;262(2):207–208. doi: 10.1001/jama.1989.03430020049017. [DOI] [PubMed] [Google Scholar]
- 152.Henrion R, Mandelbrot L, Delfieu D. HIV contamination after injections of anabolic steroids. Presse Med. 1992;21(5):218. [PubMed] [Google Scholar]
- 153.Sklarek HM, Mantovani RP, Erens E, Heisler D, Niederman MS, Fein AM. AIDS in a bodybuilder using anabolic steroids. N Engl J Med. 1984;311(26):1701. doi: 10.1056/NEJM198412273112615. [DOI] [PubMed] [Google Scholar]
- 154.Rich JD, Dickinson BP, Merriman NA, Flanigan TP. Hepatitis C virus infection related to anabolic-androgenic steroid injection in a recreational weight lifter. Off J Am Coll Gastroenterol ACG. 1998;93(9):1598. doi: 10.1111/j.1572-0241.1998.01598.x. [DOI] [PubMed] [Google Scholar]
- 155.Hope VD, McVeigh J, Marongiu A, Evans-Brown M, Smith J, Kimergård A, et al. Prevalence of, and risk factors for, HIV, hepatitis B and C infections among men who inject image and performance enhancing drugs: a cross-sectional study. BMJ Open. 2013;3(9):e003207. doi: 10.1136/bmjopen-2013-003207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Aitken C, Delalande C, Stanton K. Pumping iron, risking infection? Exposure to hepatitis C, hepatitis B and HIV among anabolic–androgenic steroid injectors in Victoria, Australia. Drug Alcohol Depend. 2002;65(3):303–8. doi: 10.1016/S0376-8716(01)00174-0. [DOI] [PubMed] [Google Scholar]
- 157.Midgley SJ, Heather N, Best D, Henderson D, McCarthy S, Davies JB. Risk behaviours for HIV and hepatitis infection among anabolic-androgenic steroid users. AIDS Care. 2000;12(2):163–70. doi: 10.1080/09540120050001832. [DOI] [PubMed] [Google Scholar]
- 158.Underwood M. The unintended consequences of emphasising blood-borne virus in research on, and services for, people who inject image and performance enhancing drugs: a commentary based on enhanced bodybuilder perspectives. Int J Drug Policy. 2019;67:19–23. doi: 10.1016/j.drugpo.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 159.Herr A, Rehmert G, Kunde K, Gust R, Gries A. A thirty-year old bodybuilder with septic shock and ARDS from abuse of anabolic steroids. Anaesthesist. 2002;51(7):557–63. doi: 10.1007/s00101-002-0335-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Prosperi-Porta G, Oleynick C, Vaughan S. Myositis from intramuscular oil injections in a bodybuilder. CMAJ. 2020;192(18):E480. doi: 10.1503/cmaj.191500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hope VD, McVeigh J, Marongiu A, Evans-Brown M, Smith J, Kimergård A, et al. Injection site infections and injuries in men who inject image- and performance-enhancing drugs: prevalence, risks factors, and healthcare seeking. Epidemiol Infect. 2015;143(1):132–140. doi: 10.1017/S0950268814000727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.AbdullGaffar B. Illicit injections in bodybuilders: a clinicopathological study of 11 cases in 9 patients with a spectrum of histological reaction patterns. Int J Surg Pathol. 2014;22(8):688–694. doi: 10.1177/1066896914553664. [DOI] [PubMed] [Google Scholar]
- 163.Jabal TA, Ganayem M, Peretz A, Nitzan O. The undesired outcomes of bodybuilding: an intra-deltoid abscess caused by Eikenella corrodens after licking the needle. Israel Med Assoc J IMAJ. 2020;22(10):652–653. [PubMed] [Google Scholar]
- 164.Kienbacher G, Maurer-Ertl W, Glehr M, Feierl G, Leithner A. A case of a tumorsimulating expansion caused by anabolic androgen steroids in body building. Sportverletz Sportschaden. 2007;21(4):195–8. doi: 10.1055/s-2007-963708. [DOI] [PubMed] [Google Scholar]
- 165.Al-Ismail K, Torreggiani WC, Munk PL, Nicolaou S. Gluteal mass in a bodybuilder: radiological depiction of a complication of anabolic steroid use. Eur Radiol. 2002;12(6):1366–1369. doi: 10.1007/s00330-001-1169-1. [DOI] [PubMed] [Google Scholar]
- 166.Evans NA. Local complications of self administered anabolic steroid injections. Br J Sports Med. 1997;31(4):349–350. doi: 10.1136/bjsm.31.4.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Richards JR, Scheerlinck PH, Owen KP, Colby DK. Bodybuilding supplements leading to copper toxicity, encephalopathy, fulminant hepatic failure and rhabdomyolysis. Am J Emerg Med. 2020;38(11):2487.e1–e5. doi: 10.1016/j.ajem.2020.05.096. [DOI] [PubMed] [Google Scholar]
- 168.Tidmas V, Brazier J, Hawkins J, Forbes SC, Bottoms L, Farrington K. Nutritional and non-nutritional strategies in bodybuilding: impact on kidney function. Int J Environ Res Public Health. 2022;19(7):4288. doi: 10.3390/ijerph19074288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Rocha PN, Santos CS, Avila MO, Neves CL, Bahiense-Oliveira M. Hypercalcemia and acute kidney injury caused by abuse of a parenteral veterinary compound containing vitamins A, D, and E. Braz J Nephrol. 2011;33:467–471. doi: 10.1590/S0101-28002011000400013. [DOI] [PubMed] [Google Scholar]
- 170.Ven Kvd, Mulrooney KJD. Doping controls in gyms—ineffective, costly and more common than you think. 2016 [cited]. Available from: https://theconversation.com/doping-controls-in-gyms-ineffective-costly-and-more-common-than-you-think-68797.
- 171.Mulrooney KJD, Ven Kvd. ‘Muscle Profiling’: anti-doping policy and deviant leisure. 2015 [cited 2022 September 21]. Available from: https://deviantleisure.com/2015/01/21/muscle-profiling-anti-doping-policy-and-deviant-leisure/.
- 172.Horwitz H, Andersen JT, Dalhoff KP. Health consequences of androgenic anabolic steroid use. J Intern Med. 2019;285(3):333–340. doi: 10.1111/joim.12850. [DOI] [PubMed] [Google Scholar]
- 173.Thiblin I, Garmo H, Garle M, Holmberg L, Byberg L, Michaëlsson K, et al. Anabolic steroids and cardiovascular risk: a national population-based cohort study. Drug Alcohol Depend. 2015;1(152):87–92. doi: 10.1016/j.drugalcdep.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 174.Petersson A, Garle M, Granath F, Thiblin I. Morbidity and mortality in patients testing positively for the presence of anabolic androgenic steroids in connection with receiving medical care. A controlled retrospective cohort study. Drug Alcohol Depend. 2006;81(3):215–20. doi: 10.1016/j.drugalcdep.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 175.Kanayama G, Pope HG., Jr History and epidemiology of anabolic androgens in athletes and non-athletes. Mol Cell Endocrinol. 2018;464:4–13. doi: 10.1016/j.mce.2017.02.039. [DOI] [PubMed] [Google Scholar]
- 176.Sagoe D, Molde H, Andreassen CS, Torsheim T, Pallesen S. The global epidemiology of anabolic-androgenic steroid use: a meta-analysis and meta-regression analysis. Ann Epidemiol. 2014;24(5):383–398. doi: 10.1016/j.annepidem.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 177.Sagoe D, Pallesen S. Androgen abuse epidemiology. Curr Opin Endocrinol Diabetes Obes. 2018;25(3):185–194. doi: 10.1097/MED.0000000000000403. [DOI] [PubMed] [Google Scholar]
- 178.Lindqvist AS, Moberg T, Ehrnborg C, Eriksson BO, Fahlke C, Rosén T. Increased mortality rate and suicide in Swedish former elite male athletes in power sports. Scand J Med Sci Sports. 2014;24(6):1000–1005. doi: 10.1111/sms.12122. [DOI] [PubMed] [Google Scholar]
- 179.Marijon E, Tafflet M, Antero-Jacquemin J, El Helou N, Berthelot G, Celermajer DS, et al. Mortality of French participants in the Tour de France (1947–2012) Eur Heart J. 2013;34(40):3145–3150. doi: 10.1093/eurheartj/eht347. [DOI] [PubMed] [Google Scholar]