Abstract
The presence of perinatal mood and anxiety disorders has typically been associated with decreases in the quality of mother–infant interactions. However, maternal anxiety symptoms during the postpartum period have been less studied than other mental health disorders like depression. In the current study, we examined associations among symptoms of maternal anxiety, maternal perceived stress, and mother–infant behavioral synchrony in the early postnatal period. Eighty-one mother–infant dyads participated in this study when the infants were 3 months old. Surveys were given to obtain demographic information and current maternal mental health symptoms, and dyads completed a 5-min free-play task to measure behavioral synchrony. Results indicated that maternal anxiety symptoms were positively associated with behavioral synchrony, but only for mothers reporting moderate levels of perceived stress. These findings highlight the differential impact of maternal postpartum mental health on behavioral synchrony and suggest that higher maternal anxiety symptoms during the postnatal period may play an adaptive role in fostering more dynamic mother–infant interactions.
1 ∣. INTRODUCTION
Maternal mental health is a major concern during the postpartum period. Women often develop and experience perinatal mood and anxiety disorders (PMAD) during this time due to the myriad of hormonal, neurobiological, and behavioral changes as a result of childbirth and caring for an infant. Postpartum depression has been found in 17.22% of the world's population (Wang et al., 2021), but as this disorder is oftentimes underdiagnosed (Toohey, 2012), this estimate is likely to be much higher. Studies have reported that postpartum depression may last 3–14 months after childbirth and has been linked to negative impacts on subsequent child development, most notably within the cognitive and socioemotional domains (Slomian et al., 2019).
Although most of the literature has focused on postpartum depression, rates of postpartum anxiety are reported to be much higher, with up to 50% of new moms reporting experiencing symptoms of postpartum anxiety (Wenzel et al., 2005). One important aspect of the early child environment thought to be impacted by maternal mental health is the quality of mother–infant interactions (Granat et al., 2017; Kaitz et al., 2010). Research on associations between maternal mental health and mother–infant interactions has largely focused on individual parenting behaviors, such as maternal sensitivity, described as the mother's ability to notice, interpret, and appropriately respond to infant cues (Beebe et al., 2011) rather than behavioral synchrony, which treats the mother–infant dyad as a single interdependent unit of coordinated back-and-forth exchanges of affective and behavioral cues (Feldman, 2007a). The degree of synchrony between mother and infant has been positively associated with a number of child outcomes, including self-regulation, attachment security, and measures of social and emotional wellbeing (Feldman & Eidelman, 2004; Feldman et al., 1999, 2009; Isabella & Belsky, 1991; Jaffe et al., 2001). However, disruptions in mother–infant synchrony can also serve as a risk for psychopathology later in development (Feldman, 2007a). As such, given the prevalence of maternal anxiety in the postpartum period, and the importance of mother–infant synchrony for multiple domains of development, more research is needed to clarify the associations between maternal anxiety and mother–infant behavioral synchrony specifically.
1.1 ∣. Postpartum anxiety and mother–infant interactions
Given that the focus of most research in maternal mental health and mother–infant interactions has been on postpartum depression, associations between maternal anxiety and mother–infant interactions are less well understood than associations with depression. Importantly, however, existing research has shown that anxiety and depression have differential influences on mother–infant interactions (Granat et al., 2017), highlighting the need to better understand how anxiety may influence the mother–infant relationship. Specifically, maternal depression has been associated with more withdrawn mother–infant interactions, including less maternal warmth, lower rates of maternal sensitivity, and difficulties with emotional bonding between mother and infant compared to mothers without postpartum mental illness (Slomian et al., 2019). In a study comparing the dynamics of mother–infant interactions between depressed, anxious, and control mothers and their 9-month-old infants, Granat et al. (2017) found that infants of depressed mothers showed higher rates of gaze aversion, less social gaze, the lowest rates of both gaze and touch synchrony with the mother, and did not show evidence that the mother buffered negative affect. By contrast, dyads with anxious moms showed the highest rates of gaze and touch synchrony and showed evidence of maternal buffering of negative affect. Altogether, available evidence would suggest that maternal anxiety and depression show important differences in the emotional dynamics of mother–infant interactions in the first year of life.
The research focused specifically on maternal anxiety and mother–infant interactions has yielded mixed results. Using the Coding Interactive Behavior (CIB) manual to measure mother–infant interactions, Feldman et al. (2009) reported that clinically diagnosed anxious mothers show poorer social engagement and reduced maternal sensitivity than nonanxious mothers during short free-play interactions with their 9-month-old infants (Feldman et al., 2009). Another study by Kaitz et al. (2010) used 14 parenting behaviors from the Scale of Interactional Style measure and found that although clinically anxious mothers showed more exaggerated behaviors with their 6-month-old infants during free-play interactions, they did not show deficits in sensitivity. Furthermore, some studies have suggested that mothers with anxiety symptoms are actually more attuned to their 12 months infants' arousal and emotional bids when recording vocalizations and day-long physiological fluctuations (Smith et al., 2021). These mixed findings would suggest that associations between maternal anxiety and mother–infant interactions may differ based on infant age, how mother–infant interactions are measured, and assessment of maternal mental health status (clinical diagnosis vs. symptom-based approaches). The reliance on clinical cutoffs or diagnoses limits the generalizability of previous research in this area by failing to account for individual differences within clinical and nonclinical groups, and sources of variability in mother–infant interactions related to mental health symptoms at the subclinical level. As such, more research is needed in nonclinical samples to better characterize the associations between maternal anxiety and mother–infant interactions and improve generalizability of findings to the general population.
1.2 ∣. Anxiety, stress, and behavioral synchrony
Recent shifts in the study of mother–infant interaction have focused on the role of synchrony within the dyad (Feldman, 2007a; Granat et al., 2017; Kaitz et al., 2010; Smith et al., 2021). Previous studies have shown that infants in highly synchronous mother–infant dyads show higher capacities for self-regulation in childhood (Feldman & Eidelman, 2004; Feldman et al., 1999), higher empathy in adolescence (Feldman, 2007b), and more secure attachment behavior (Isabella & Belsky, 1991; Jaffe et al., 2001). However, behavioral synchrony between mother and child seems to be influenced by the mother's emotional state.
When examining maternal anxiety and synchrony, some research has found that anxious mothers show more synchrony with their infants (Doba et al., 2022; Granat et al., 2017; Smith et al., 2021), while others have shown no differences between anxious and nonanxious mothers in behavioral synchrony (Kaitz et al., 2010). These mixed findings suggest that more research is needed to better understand the precise role of maternal anxiety in mother–infant behavioral synchrony. Importantly, much of the research in this area has relied upon clinical diagnosis of maternal anxiety (Kaitz et al., 2010) or extreme case designs (Granat et al., 2017), potentially obscuring how individual differences in anxiety severity may contribute to behavioral synchrony. It is important to examine subclinical anxiety symptoms as they relate to mother–infant interactions, as heightened anxiety during the postpartum period is a relatively common experience, and is tied to neurobiological changes in the maternal brain (Kim et al., 2010), but may not always amount to clinically significant anxiety. Additionally, from a Research Domain Criteria (RDoC) perspective (Cuthbert & Insel, 2013), examining individual differences in symptoms, rather than clinical diagnoses, increases translational utility of research findings by allowing for broader generalizability of findings beyond strictly clinical samples.
Previous work in the area of anxiety and mother–infant interactions has suggested a midrange model of self-reported anxiety, in which mothers reporting neither very high nor very low levels of anxiety show the most engaged and sensitive parenting (Beebe et al., 2011). This moderate anxiety is hypothesized to allow mothers to be more attuned and responsive to infant distress cues without becoming distressed themselves, whereas very high anxiety might cause mothers to become distressed, and very low anxiety might inhibit mothers' ability to detect infant distress cues. This midrange model further highlights the importance of examining subclinical anxiety symptoms, as it may be the case that clinical anxiety symptoms show a different behavioral phenotype than moderate or low subclinical anxiety symptoms (Barlow, 1991; Kaitz & Maytal, 2005). Within this context, moderate maternal anxiety may be associated with greater behavioral synchrony in a mother–infant dyad, due to heightened maternal awareness of infant cues without becoming overly distressed so as to disengage the infant.
The postpartum period is associated with changes in a number of biological and physiological systems in mothers that may predispose them to moderately heightened stress and anxiety during this time. Studies have shown that maternal stress is associated with increases in amygdala sensitivity to infant cues of distress and decreases in amygdala sensitivity to infant happy cues (Kim et al., 2017; Schechter et al., 2012). This would suggest that mothers experiencing heightened levels of stress may be more responsive to infant distress cues and less responsive to neutral or positive infant cues. Additionally, stress is known to exacerbate the behavioral and neurobiological symptoms of anxiety (Pêgo et al., 2010; Shin & Liberzon, 2010). Taken together with the midrange anxiety model, these findings would suggest that mothers experiencing heightened anxiety may show more behavioral synchrony with their infants, but that relationship might be moderated by the degree of stress the mother is experiencing. These findings highlight the importance of examining both direct and interactional effects of anxiety and stress on behavioral synchrony in the perinatal period.
1.3 ∣. The current study
The current study examines the associations among maternal anxiety symptoms, maternal perceived stress, and mother–infant behavioral synchrony during a free-play task. We seek to expand upon previous literature examining associations between maternal mental health and behavioral synchrony by specifically focusing on symptoms of maternal anxiety, including a consideration of the interaction between maternal anxiety symptoms and stress in the early postpartum period. We hypothesize that maternal anxiety symptoms will be associated with greater behavioral synchrony between mother and infant, but that this relationship will be moderated by the degree of maternal stress. Specifically, we hypothesize that at moderate levels of stress, there will be a positive association between maternal anxiety and behavioral synchrony. Expanding upon previous research, we test these associations in a nonclinical sample of mother–infant dyads when infants are 3 months old to better understand how early in development we can begin to see differences in behavioral synchrony in relation to maternal mental health.
2 ∣. METHODS
2.1 ∣. Participants
One-hundred-and-three families were recruited from community events and flyers posted around the New York City metropolitan area. Inclusion criteria for children included being 3 months old at the time of the first lab visit (range = 2.8–3.8 months), born at or after 37 weeks of gestation, and no history of neurological or developmental delays. For the purposes of the current analyses, we limit our sample to useable data from families where the mother completed all of the tasks including free play, the Edinburgh Postnatal Depression Scale (EPDS), and stress questionnaires. Our final sample consists of 81 mother–infant dyads who completed all required surveys and a 5-min free-play interaction. We examined the differences between those included and those not on the basis of income, maternal depression, and caregiver race and found no significant differences between groups. The present study was conducted according to guidelines laid down in the Declaration of Helsinki, with written informed consent obtained from a parent or guardian for each child before any assessment or data collection. All procedures were approved by the Institutional Review Board at New York University.
2.2 ∣. Measures
2.2.1 ∣. Demographic questionnaire
Families completed questionnaires during the visit to obtain demographic information including maternal and infant age, race, ethnicity, sex, and annual household income. Household income to needs ratio (INR) was measured by dividing the total annual household income by the federal poverty line for families of that size. An INR value below one indicates that the family is living in poverty, and below 2 would indicate that the family is classified as low income. The INR for this sample ranged from 0 to 23.44 and the median was 3.7.
2.2.2 ∣. Perceived Stress Scale
The Perceived Stress Scale (PSS; Cohen et al., 1983) was used to assess self-reported maternal stress. The PSS is a 14-item self-report questionnaire that assesses the degree to which the respondent has perceived situations as stressful within the last month. Items are rated on a five-point Likert scale ranging from 0 (never) to 4 (very often). A total score is the sum of scores from all items (after four items are reverse scored). Scores on the PSS can range from 0 to 40. Scores between 0 and 13 are considered low stress, 14–26 are considered moderate stress, and 27–40 are considered high stress. The range of scores in our community sample ranged from 0 to 34; however, only 2 participants had scores falling within the “high stress” range (scores of 28 and 34). As such, to reduce the influence of isolated higher stress scores, we created a dichotomous stress variable, in which all participants scoring above 13 (moderate stress) on the PSS received a score of 1 (n = 30) and all those receiving a score of 13 or below (low stress) received a score of 0 (n = 46).
2.2.3 ∣. Mother–infant interaction and behavioral synchrony
Infants were placed in an infant rocker, which is a chair for infants from 0 to 6 months that has a curved seat, enabling 3-month-old babies to sit back and allowing face to face interaction with mothers, who were seated across from them. Each dyad was given a standardized set of toys including a book, plastic cups, and a rattling ball, and were instructed to play like they normally would at home for 5 minutes. Infants were not rocked during the interaction. The interactions were video recorded and the experimenters left the room during the task. Quality of mother–infant interactions were assessed using the Coding Interactive Behavior (CIB; Feldman, 1998) measure. Each behavioral code was coded on a 5-point scale, where 1 denotes a minimal level of the specific behavior and 5 denotes a maximal level across the 5-min interaction.
From the CIB, the following dyadic scales were used to characterize behavioral synchrony:
Dyadic Reciprocity:
Describes the synchrony between mother and child in terms of frequency (moving along smoothly) and quality of the interaction (understanding, and responding to their partner's signals). It is the “serve and return” of an interaction. Dyadic reciprocity describes how well each partner participates in the joint interaction while giving something meaningful (saying something, doing something) and allowing for the space and time for the other partner to do the same. This scale focuses more on the content of the interaction—what did each person share? Did it build off of what the other person shared? Are they responding to each other? An example of an interaction high in dyadic reciprocity would be when the child vocalizes, the mother acknowledges and elaborates upon the vocalization as a response to that signal. In this scale, 1 was the minimum score, where coordination was not observed between the dyad, for example, if the mother or the infant was rejecting. The maximum score was five and it was given to those dyads that were synchronized, reading and responding to their partner's cues.
Adaptation–regulation:
This scale describes the mutual adaptation to different states and signals, and the degree to which mother and infant adapt to their partner's degree of involvement or level of stimulation. Examples include lowering one's voice when the other averts their gaze, or increasing involvement following the other's encouragement. A score of 1 was given when the mothers ignored the child signals and continued stimulating them, for example, if the infant was crying and the mother continued playing with them. The maximum score of five was given when mothers adapted to their child's signals, for example, if the baby was crying, they would try to calm them down before stimulating.
Fluency:
This is associated with the rhythm and flow of the interaction. Higher scores on this scale are achieved when the dyad keeps a continuous and consistent flow, independent of the speed of the interaction. An absence of fluency in the dyad would receive a score of 1 and a very fluent interaction would get a 5.
Three coders with CIB training coded the interactions. After CIB training, study-specific training occurred, where videos were chosen randomly from the study database (n = 20) and were used to establish overall reliability across the three coders, with inter-rater reliability of r > 0.85. Following this training phase, coders coded their own randomly assigned videos, blind to socio-demographic or maternal mental health data. Strength of agreement using Fleiss' Kappa ranged from good to very good: Dyadic Reciprocity κ = 0.857, Adaptation-Regulation κ = 0.751, and Fluency κ = 0.906.
2.2.4 ∣. Edinburgh Postnatal Depression Scale (EPDS)
The EPDS is a 10-item self-report scale assessing the common symptoms of postpartum depression and anxiety (Brouwers et al., 2001; Cox et al., 1987; Matthey, 2008; Matthey et al., 2013). Of the 10 items, 7 directly measure depression symptoms, while 3 measure anxiety symptoms (Brouwers et al., 2001; Matthey, 2008; Matthey et al., 2013).
Postpartum anxiety.
Our main measure of anxiety in this analysis is the 3-item anxiety subscale of the EPDS (EPDS-3A). The items read as follows: “I have been anxious or worried for no good reason,” “I have blamed myself unnecessarily when things went wrong,” and “I have felt scared or panicky for no good reason.” Previous studies using both exploratory (Smith-Nielsen et al., 2018) and confirmatory (Smith-Nielsen et al., 2021) factor analysis have found distinct anxiety and depression subscales within the EPDS (Kozinszky et al., 2017). This evidence suggests that the EPDS-3A is both a reliable and time-effective method of measuring anxiety during the perinatal period. The Cronbach's alpha for this subscale was 0.69, indicating acceptable internal consistency. This value is comparable to values found in previous studies using the EPDS-3A to assess anxiety (Smith-Nielsen et al., 2021).
Postpartum depression.
Our maternal depression measure consisted of items from the EPDS measuring depression symptoms (EPDS items 1, 2, 6, 7, 8, 9, 10). The items read: “I have been able to laugh and see the positive side of things as much as I used to,” “I have had a strong desire to get things done and I enjoy doing so,” “Things have been piling up and I haven't been able to keep up,” “I have been so unhappy that I have had difficulty sleeping,” “I have felt sad or miserable,” “I have been so unhappy that I have been crying,” and “The thought of harming myself has occurred to me.” This subscale had a Cronbach's alpha of 0.81, indicating good internal consistency.
2.2.5 ∣. Covariates
All regressions control for family income-to-needs ratio, infant sex, maternal depression (to parse out potentially shared sources of variance between anxiety and depression symptoms), and first-time motherhood status. We control family income-to-needs ratio to mitigate potential sources of income-related stress as influencing the quality of mother–infant interactions, in line with the Family Stress Model (Conger et al., 2010). We control effects of infant sex, based on previous literature suggesting that male infants may be more sensitive to influences of maternal mental health than female infants (Reck et al., 2018). Finally, we control for first-time motherhood status based on previous literature suggesting that first-time mothers show different patterns of maternal self-efficacy and mental health symptoms than more experienced mothers (Kunseler et al., 2014).
2.3 ∣. Analysis plan
All analyses were conducted in R. We created composites for behavioral synchrony, maternal anxiety, and maternal depression by taking the mean of the items listed in the measures section. The behavioral synchrony composite comprised CIB items of dyadic reciprocity, adaptation–regulation, and fluency. The Cronbach's alpha of this measure was 0.72, indicating acceptable internal consistency.
First, we performed a series of bivariate correlations to determine if there were basic associations between our measures of interest. We then performed a series of regression models with behavioral synchrony as our outcome of interest and maternal anxiety symptoms and stress as our predictors, controlling for all covariates outlined above. Finally, to test for a possible moderating effect of stress, we performed a regression with an interaction between stress and anxiety symptoms, and a simple slopes test to examine if the association between anxiety symptoms and behavioral synchrony differed between our moderate stress and low stress participants. To minimize effects of multicollinearity between anxiety symptoms, stress, and depression symptoms, we standardized and mean centered all continuous predictors in our regression analyses and examined variance inflation factors for all regression terms. Missing data were accounted for using full information maximum likelihood estimation.
3 ∣. RESULTS
3.1 ∣. Descriptive statistics and correlations
Information on the demographic characteristics of our sample can be found in Table 1. Maternal anxiety symptoms, perceived stress, and behavioral synchrony were all relatively normally distributed in our sample, as described in Table 2. The mean score on the Edinburgh scale across the entire sample was 5.4 (range = 0–19), below the threshold for possible depression of 10, indicating that our sample is generally in the subclinical range for mental health symptoms as measured by the EPDS. The mean EPDS-3A score in our sample was 1.94, with possible values ranging from 1 to 4, indicating low to moderate average anxiety symptoms in our sample.
TABLE 1.
Demographic characteristics
| Mean (SD) or N (% of sample) | |
|---|---|
| Family income-to-needs ratio | 5.13 (5.27) |
| Infant sex | 50 (61.7%) male |
| First time mother status | 41 (50.6%) first time mothers |
| Maternal Race | |
| Black/African American | 15 (18.52%) |
| Asian American | 8 (9.88%) |
| White | 26 (32.10%) |
| Two or more races | 21 (25.93%) |
| Other | 8 (9.88%) |
| Did not report | 3 (3.70%) |
TABLE 2.
Descriptive statistics
| Variable | Mean (SD) | Min, Max (possible range) |
Skewness | Kurtosis |
|---|---|---|---|---|
| Maternal anxiety symptoms (EPDS-3A) | 1.94 (0.7) | 1, 3.67 (1–4) | 0.46 | −0.66 |
| Perceived Stress Scale | 12.99 (6.54) | 0, 34 (0–40) | 0.55 | 0.28 |
| Maternal depression symptoms (mean of items 1, 2, 6, 7, 8, 9, 10) | 1.5 (0.47) | 1, 3.14 (1–4) | 1.18 | 1.02 |
| Dyadic reciprocity | 3.69 (0.64) | 2, 5 (1–5) | −0.17 | −0.38 |
| Fluency | 3.51 (0.69) | 1, 5 (1–5) | −1.15 | 2.87 |
| Adaptation regulation | 3.9 (0.7) | 2, 5 (1–5) | −0.17 | −0.5 |
| Behavioral synchrony (composite) | 3.71 (0.54) | 2.33, 5 (1–5) | −0.22 | −0.03 |
A correlation matrix for all variables of interest can be found in Table 3. Upon examination of correlations, we found, as expected, strong positive correlations between maternal anxiety symptoms, depression symptoms, and stress, suggesting that these mental health symptoms are highly comorbid in our sample. There were no correlations between income-to-needs ratio and mental health symptoms or behavioral synchrony in our sample. Additionally, we found no significant correlation between maternal anxiety symptoms and behavioral synchrony (r = 0.19, p = 0.09). The correlations between our behavioral synchrony items were moderate in magnitude and in the expected direction: fluency and adaptation regulation (r = 0.34, p < 0.01), fluency and dyadic reciprocity (r = 0.43, p < 0.01), adaptation regulation and dyadic reciprocity (r = 0.64, p < 0.01).
TABLE 3.
Correlations between all measures of interest
| Maternal anxiety symptoms |
Maternal depression symptoms |
Behavioral synchrony |
Income-to- needs ratio |
Perceived Stress Scale |
|
|---|---|---|---|---|---|
| Maternal anxiety symptoms | 1 | ||||
| Maternal depression symptoms | 0.63*** | 1 | |||
| Behavioral synchrony | 0.19 | 0.05 | 1 | ||
| Income-to-needs ratio | 0.00 | −0.08 | 0.17 | 1 | |
| Perceived Stress Scale | 0.62*** | 0.66* | −0.08 | −0.07 | 1 |
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001.
3.2 ∣. Does maternal anxiety predict behavioral synchrony?
In a multiple regression model controlling for all covariates of interest, we found no significant association between maternal anxiety symptoms and behavioral synchrony (β = 0.32, p = 0.06). We then ran an analysis including maternal stress as an additional predictor of behavioral synchrony. Maternal stress was negatively associated with behavioral synchrony (β = −0.41, p = 0.001), and the addition of maternal stress in the model resulted in a significant positive association between maternal anxiety symptoms and behavioral synchrony (β = 0.36, p = 0.02).
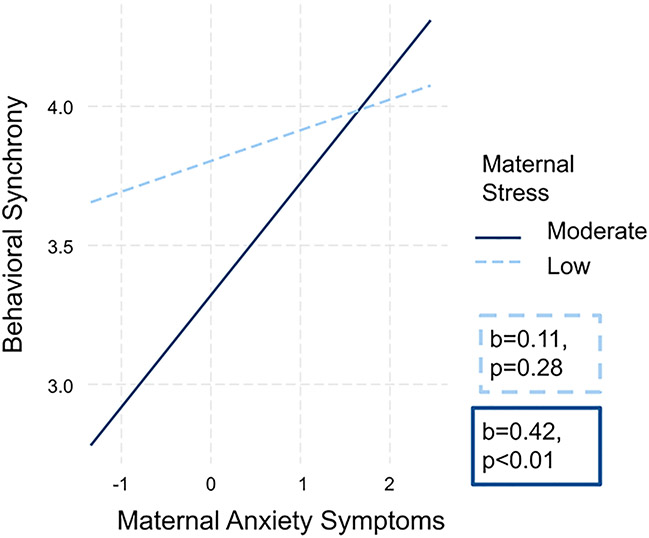
To further explore this result, we included an interaction between maternal anxiety symptoms and stress in the next regression model. The coefficient for the interaction term was significant (β = 0.34, p = 0.03). A simple slopes analysis demonstrated that for mothers scoring low on the Perceived Stress Scale (≤13), there was no association between anxiety symptoms and behavioral synchrony (b = 0.11, p = 0.28). However, for mothers scoring in the moderate range on the Perceived Stress Scale, we find a significant positive association between anxiety symptoms and behavioral synchrony (b = 0.42, p < 0.01). These findings suggest that when accompanied by a moderate degree of maternal stress, maternal anxiety symptoms are positively associated with behavioral synchrony in our sample. This association is illustrated in Figure 1. A summary of all regression results is reported in Table 4.
FIGURE 1.
Interaction plot showing significant positive association between maternal anxiety symptoms and behavioral synchrony at moderate stress, shown in the solid dark blue line
TABLE 4.
Summary of all regression results
| Model (F-value, p-value) | β | p-value | Variance inflation factor (VIF) |
|---|---|---|---|
| Model 1 (F = 1.79, p = 0.13) | |||
| Maternal anxiety symptoms | 0.32 | 0.06 | 2.42 |
| Maternal depression symptoms | −0.18 | 0.27 | 2.40 |
| Income-to-needs ratio | 0.10 | 0.42 | 1.20 |
| First-time mother status | 0.17 | 0.14 | 1.23 |
| Infant sex | 0.04 | 0.71 | 1.04 |
| Model 2 (F = 3.20, p < 0.01) | |||
| Maternal anxiety symptoms | 0.36 | 0.02 | 2.45 |
| Maternal stress (dichotomized) | −0.41 | 0.001 | 1.56 |
| Maternal depression symptoms | 0.02 | 0.92 | 2.75 |
| Income-to-needs ratio | 0.09 | 0.47 | 1.20 |
| First-time mother status | 0.12 | 0.27 | 1.23 |
| Infant sex | 0.06 | 0.57 | 1.06 |
| Model 3 (F = 3.47, p < 0.01) | |||
| Maternal anxiety symptoms | 0.18 | 0.28 | 3.10 |
| Maternal stress (dichotomized) | −0.40 | 0.001 | 1.57 |
| Maternal anxiety × maternal stress | 0.34 | 0.03 | 2.65 |
| Maternal depression symptoms | −0.10 | 0.56 | 3.10 |
| Income-to-needs ratio | 0.02 | 0.89 | 1.28 |
| First-time mother status | 0.16 | 0.16 | 1.26 |
| Infant sex | 0.03 | 0.76 | 1.07 |
4 ∣. DISCUSSION
The current study aimed to understand how anxiety and stress in the perinatal period promote behavioral synchrony in the mother–infant dyad. Our results suggest that maternal anxiety symptoms are positively associated with behavioral synchrony when infants are 3 months of age. However, these results come with important nuances. Specifically, we found that maternal anxiety symptoms were associated with behavioral synchrony only at moderate levels of maternal-reported stress, as assessed by the Perceived Stress Scale. At low levels of stress, there were no associations between maternal anxiety symptoms and behavioral synchrony. Importantly, we also found no direct effect of maternal anxiety symptoms on behavioral synchrony in our correlations. This finding, while potentially surprising, aligns with our initial hypothesis that the interaction between maternal anxiety symptoms and maternal perceived stress would be an important predictor of behavioral synchrony due to the behavioral and neurobiological changes associated with experiencing both stress and anxiety together. Stress and anxiety are relatively common experiences in the early postpartum period, and it could be the case that elevated stress may exacerbate some of the behavioral phenotypes associated with maternal anxiety, thus influencing the degree of behavioral synchrony in the mother–infant dyad.
Previous studies within the literature examining maternal anxiety, stress, and mother–infant interactions have yielded mixed results. However, these past studies have often relied on extreme case designs or case-control designs (Granat et al., 2017; Kaitz et al., 2010) between mothers with anxiety compared to mothers without anxiety. These studies provide important foundational knowledge about anxiety, stress, and parenting, but may not capture meaningful differences that arise across the spectrum of maternal mental health symptoms. Specifically, such studies often fail to account for variability in symptom severity within clinical versus nonclinical groups, thus limiting our understanding of how individual differences in mental health symptoms influence the quality of mother–infant interactions. Similarly, samples such as these are often skewed toward individuals with the social and economic resources to seek mental healthcare and thus receive clinical diagnoses, which limits generalizability of findings and fails to account for symptoms of anxiety in those without a clinical diagnosis.
There is a growing body of research that suggests that anxious mothers may be more attuned to infant signals and may be more responsive to those cues. In a recent study examining physiological synchrony in mother–infant dyads, Smith et al. (2021) found that dyads with anxious mothers showed a higher degree of physiological synchrony overall throughout the day compared to dyads with less anxious mothers. Specifically, this study reported that less anxious mothers were highly responsive to peak levels of arousal from their infants, but that more anxious mothers displayed more consistent responsiveness to smaller fluctuations in infant arousal. This study would suggest that maternal anxiety is positively associated with physiological synchrony, but that behavioral aspects of these mother–infant interactions may differ as a function of maternal anxiety. Importantly, however, Smith and colleagues used a median split to characterize their high and low anxiety groups, and found that their high anxiety group was more reflective of moderate anxiety, as defined by their measurement tool the GAD-7. Thus, these findings, in addition to our own, provide additional support for a midrange model of anxiety at which moderate anxiety in the postnatal period is thought to be associated with an optimal level of mother–infant interaction (Beebe et al., 2011; Smith et al., 2021).
Similarly, in a study of 72 mothers and their 6-month-old infants, Doba et al. (2022) found that higher subclinical maternal anxiety was associated with higher motor, verbal, and gaze synchrony between the mother and infant (Doba et al., 2022). Altogether, the existing research on maternal anxiety and behavioral synchrony would suggest that a certain degree of maternal anxiety in the postnatal period is an important tool for cultivating dynamic and synchronous mother–infant interactions (Beebe et al., 2011; Doba et al., 2022; Granat et al., 2017; Smith et al., 2021).
A higher degree of mother–infant behavioral synchrony is often associated with more positive infant outcomes (Leclère et al., 2014); however, in the absence of adequate stress buffering and regulation of negative arousal, this synchrony could prime the infant toward more anxious patterns of self-regulation in order to “match” that of the caregiver. In the short term, these kinds of adaptations are highly beneficial, allowing the infant to regulate their arousal in a manner most appropriate for their environment (Ellis & Del Giudice, 2019). However, in the long term these adaptations may increase the risk for later anxiety disorders (Santarelli et al., 2014). This would suggest that behavioral synchrony in the postpartum period may be an important conduit for intergenerational transmission of anxiety; however, we did not examine this possibility in this study and more longitudinal research is needed to address this possibility.
Our findings provide some support for a midrange model of anxiety (Beebe et al., 2011). A moderate degree of maternal anxiety may involve more consistent awareness of and attunement to infant emotional cues (as seen in Smith et al., 2021), whereas high anxiety might be associated with excessive awareness of infant cues (seen in Kaitz et al., 2010), and very low anxiety might be associated with intermittent awareness of and responsiveness to infant cues (Smith et al., 2021). Such a model may fit well within the context of our findings, in which we find that at moderate levels of stress, we see a positive relationship between anxiety and behavioral synchrony and at low stress we find no relationship between anxiety and synchrony. This is significant, because stress and anxiety are highly correlated in our sample (r = 0.621), indicating that mothers who report the highest levels of stress are also likely to report the highest levels of anxiety, and vice versa. This would suggest that a midrange anxiety framework may be a useful framework to interpret our findings, in which we see the highest degree of behavioral synchrony in the midrange for both anxiety symptoms and stress. Replication of these findings in a larger sample, capturing a wider range of stress and anxiety experiences, is needed to provide additional support for this model.
There are a number of methodological and conceptual strengths in this study. To begin with, our focus on individual differences in anxiety symptoms, rather than clinical diagnosis of anxiety, is especially valuable. A symptom-based approach to understanding mental health aligns well with a Research Domain Criteria (RDoc; Cuthbert & Insel, 2013) framework of examining a wider range of mental health experiences in behavioral research, rather than limiting observations to clinical versus nonclinical diagnoses. This added nuance is particularly valuable for understanding maternal mental health in the postpartum period, where heightened anxiety is common but not always chronic or detected by clinicians.
An additional strength of our approach comes in the consideration of both stress and anxiety. Our finding that higher anxiety symptoms are related to higher behavioral synchrony only among those mothers experiencing moderate stress suggests that the experience of stress plays an important role in how mothers coping with anxiety interact with their infants. Within our study, for moms reporting low stress there was no association between anxiety symptoms and synchrony, suggesting that maternal anxiety may be a less important predictor of mother–infant interactions in low stress contexts than in moderate stress contexts. These findings highlight the importance of more specifically tailored mental health services for new mothers, services that both reduce maternal stress and alleviate symptoms of maternal anxiety. More work in this area is needed to fully disentangle effects of co-occurring stress and anxiety in the postpartum period, but this study provides an important step in understanding these complex dynamics.
Despite the strengths of this study, there are limitations that merit addressing. As mentioned above, while this sample adequately represents mothers experiencing low and moderate stress, we have very few mothers reporting high levels of stress. As such, we are limited in the conclusions we can draw about how high stress may interact with symptoms of maternal anxiety. Further studies are needed to better capture a fuller range of stress experiences and fully understand these associations for mothers experiencing high levels of stress. An additional limitation comes from the sample size (n = 81) represented here. Future studies employing larger samples may be able to detect more nuances in associations between maternal stress, anxiety symptoms, and behavioral synchrony than we are able to do here due to issues of statistical power and sample size limits. Furthermore, while we examine stress as a moderating factor influencing the associations between maternal anxiety and synchrony, it could be the case that anxiety and stress contribute additive, rather than interactive, influences on the mother–infant relationship, which we have not accounted for in these analyses. A further limitation comes from our use of the EPDS-3A as a measure of maternal anxiety. While the EPDS-3A shows adequate reliability in our sample, and has been shown elsewhere to reliably detect maternal anxiety (Kozinszky et al., 2017; Smith-Nielsen et al., 2018, 2021), future studies should employ additional measures of maternal anxiety such as the State-Trait Anxiety Inventory or the GAD-7 to further assess the associations between maternal anxiety symptoms and behavioral synchrony.
There is a great deal of evidence that heightened maternal anxiety in the postpartum period is a relatively common experience, with a neurobiological basis that is often different from anxiety experienced in other time periods (Pawluski et al., 2017). Future research should continue to examine the ways in which maternal anxiety influences mother–infant interactions in the early postpartum period, particularly the extent to which neurophysiological changes following childbirth that promote anxiety may also promote positive and supportive mother–infant relationships. Integrating models of postpartum anxiety with models of behavioral synchrony and infant development will be a useful and fruitful step in understanding these complex processes in context and providing the best possible support for parents and their infants.
ACKNOWLEDGEMENTS
This publication was supported by a NICHD K99/R00 grant (R00HD086255) to NHB.
Funding information
National Institute of Child Health and Human Development, Grant/Award Number: R00HD086255-03
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest with regard to the funding source for this study.
REFERENCES
- Barlow DH (1991). Disorders of emotion. Psychological Inquiry, 2(1), 58–71. 10.1207/s15327965pli0201_15 [DOI] [Google Scholar]
- Beebe B, Steele M, Jaffe J, Buck KA, Chen H, Cohen P, Kaitz M, Markese S, Andrews H, Margolis A, & Feldstein S (2011). Maternal anxiety symptoms and mother-infant self- and interactive contingency. Infant Mental Health Journal, 32(2), 174–206. 10.1002/imhj.20274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwers EPM, van Baar AL, & Pop VJM (2001). Maternal anxiety during pregnancy and subsequent infant development. Infant Behavior and Development, 24(1), 95–106. 10.1016/s0163-6383(01)00062-5 [DOI] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). Perceived stress scale (PSS). Journal of Health and Social Behavior, 24(4), 285. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Conger RD, Conger KJ, & Martin MJ (2010). Socioeconomic status, family processes, and individual development. Journal of Marriage and Family, 72(3), 685–704. 10.1111/j.1741-3737.2010.00725.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Holden JM, & Sagovsky R (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry: Journal of Mental Science, 150(6), 782–786. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- Cuthbert BN, & Insel TR (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11(1), 126. 10.1186/1741-7015-11-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doba K, Pezard L, & Nandrino J-L (2022). How do maternal emotional regulation difficulties modulate the mother-infant behavioral synchrony? Infancy. The Official Journal of the International Society on Infant Studies, 27(3), 582–608. 10.1111/infa.12461 [DOI] [PubMed] [Google Scholar]
- Ellis BJ, & Del Giudice M (2019). Developmental adaptation to stress: An evolutionary perspective. Annual Review of Psychology, 70(1), 111–139. 10.1146/annurev-psych-122216-011732 [DOI] [PubMed] [Google Scholar]
- Feldman R (1998). Coding interactive behavior manual. Unpublished Manual. [Google Scholar]
- Feldman R (2007a). Parent–infant synchrony and the construction of shared timing; physiological precursors, developmental outcomes, and risk conditions. Journal of child Psychology and Psychiatry, and Allied Disciplines. 10.1111/j.1469-7610.2006.01701.x [DOI] [PubMed] [Google Scholar]
- Feldman R (2007b). Mother-infant synchrony and the development of moral orientation in childhood and adolescence: Direct and indirect mechanisms of developmental continuity. American Journal of Orthopsychiatry, 77(4), 582–597. 10.1037/0002-9432.77.4.582 [DOI] [PubMed] [Google Scholar]
- Feldman R, & Eidelman AI (2004). Parent-infant synchrony and the social-emotional development of triplets. Developmental Psychology, 40(6), 1133–1147. 10.1037/0012-1649.40.6.1133 [DOI] [PubMed] [Google Scholar]
- Feldman R, Granat A, Pariente C, Kanety H, Kuint J, & Gilboa-Schechtman E (2009). Maternal depression and anxiety across the postpartum year and infant social engagement, fear regulation, and stress reactivity. Journal of the American Academy of Child & Adolescent Psychiatry, 48(9), 919–927. 10.1097/chi.0b013e3181b21651 [DOI] [PubMed] [Google Scholar]
- Feldman R, Greenbaum CW, & Yirmiya N (1999). Mother–infant affect synchrony as an antecedent of the emergence of self-control. Developmental Psychology, 35(1), 223–231. 10.1037/0012-1649.35.1.223 [DOI] [PubMed] [Google Scholar]
- Granat A, Gadassi R, Gilboa-Schechtman E, & Feldman R (2017). Maternal depression and anxiety, social synchrony, and infant regulation of negative and positive emotions. Emotion, 17(1), 11–27. 10.1037/emo0000204 [DOI] [PubMed] [Google Scholar]
- Isabella RA, & Belsky J (1991). Interactional synchrony and the origins of infant-mother attachment: A replication study. Child Development, 62(2), 373–384. 10.2307/1131010 [DOI] [PubMed] [Google Scholar]
- Jaffe J, Beebe B, Feldstein S, Crown CL, Jasnow MD, Rochat P, & Stern DN (2001). Rhythms of dialogue in infancy: Coordinated timing in development. Monographs of the Society for Research in Child Development, 66(2), i–149 [PubMed] [Google Scholar]
- Kaitz M, & Maytal H (2005). Interactions between anxious mothers and their infants: An integration of theory and research findings. Infant Mental Health Journal, 26(6), 570–597. 10.1002/imhj.20069 [DOI] [PubMed] [Google Scholar]
- Kaitz M, Maytal HR, Devor N, Bergman L, & Mankuta D (2010). Maternal anxiety, mother–infant interactions, and infants’ response to challenge. Infant Behavior and Development, 33(2), 136–148. 10.1016/j.infbeh.2009.12.003 [DOI] [PubMed] [Google Scholar]
- Kim P, Capistrano CG, Erhart A, Gray-Schiff R, & Xu N (2017). Socioeconomic disadvantage, neural responses to infant emotions, and emotional availability among first-time new mothers. Behavioural Brain Research, 325(Pt B), 188–196. 10.1016/j.bbr.2017.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim P, Leckman JF, Mayes LC, Feldman R, Wang X, & Swain JE (2010). The plasticity of human maternal brain: Longitudinal changes in brain anatomy during the early postpartum period. Behavioral Neuroscience, 124(5), 695–700. 10.1037/a0020884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozinszky Z, Töreki A, Hompoth EA, Dudas RB, & Németh G (2017). A more rational, theory-driven approach to analysing the factor structure of the Edinburgh Postnatal Depression Scale. Psychiatry Research, 250, 234–243. 10.1016/j.psychres.2017.01.059 [DOI] [PubMed] [Google Scholar]
- Kunseler FC, Willemen AM, Oosterman M, & Schuengel C (2014). Changes in parenting self-efficacy and mood symptoms in the transition to parenthood: A bidirectional association. Parenting, Science and Practice, 14(3–4), 215–234. 10.1080/15295192.2014.972758 [DOI] [Google Scholar]
- Leclère C, Viaux S, Avril M, Achard C, Chetouani M, Missonnier S, & Cohen D (2014). Why synchrony matters during mother-child interactions: A systematic review. PLoS One, 9(12), e113571. 10.1371/journal.pone.0113571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthey S (2008). Using the Edinburgh Postnatal Depression Scale to screen for anxiety disorders. Depression and Anxiety, 25(11), 926–931. 10.1002/da.20415 [DOI] [PubMed] [Google Scholar]
- Matthey S, Fisher J, & Rowe H (2013). Using the Edinburgh postnatal depression scale to screen for anxiety disorders: Conceptual and methodological considerations. Journal of Affective Disorders, 146(2), 224–230. 10.1016/j.jad.2012.09.009 [DOI] [PubMed] [Google Scholar]
- Pawluski JL, Lonstein JS, & Fleming AS (2017). The neurobiology of postpartum anxiety and depression. Trends in Neurosciences, 40(2), 106–120. 10.1016/j.tins.2016.11.009 [DOI] [PubMed] [Google Scholar]
- Pêgo JM, Sousa JC, Almeida OFX, & Sousa N (2010). Stress and the neuroendocrinology of anxiety disorders. Current Topics in Behavioral Neurosciences, 2, 97–117. 10.1007/7854_2009_13 [DOI] [PubMed] [Google Scholar]
- Reck C, Tietz A, Müller M, Seibold K, & Tronick E (2018). The impact of maternal anxiety disorder on mother-infant interaction in the postpartum period. PLoS One, 13(5), e0194763. 10.1371/journal.pone.0194763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santarelli S, Lesuis SL, Wang X-D, Wagner KV, Hartmann J, Labermaier C, Scharf SH, Müller MB, Holsboer F, & Schmidt MV (2014). Evidence supporting the match/mismatch hypothesis of psychiatric disorders. European Neuropsychopharmacology: The Journal of the European College of Neuropsychopharmacology, 24(6), 907–918. 10.1016/j.euroneuro.2014.02.002 [DOI] [PubMed] [Google Scholar]
- Schechter DS, Moser DA, Wang Z, Marsh R, Hao X, Duan Y, Yu S, Gunter B, Murphy D, McCaw J, Kangarlu A, Willheim E, Myers MM, Hofer MA, & Peterson BS (2012). An fMRI study of the brain responses of traumatized mothers to viewing their toddlers during separation and play. Social Cognitive and Affective Neuroscience, 7(8), 969–979. 10.1093/scan/nsr069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin LM, & Liberzon I (2010). The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology, 35(1), 169–191. 10.1038/npp.2009.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slomian J, Honvo G, Emonts P, Reginster J-Y, & Bruyère O (2019). Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women's Health, 15, 1745506519844044. 10.1177/1745506519844044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CG, Jones EJH, Charman T, Clackson K, Mirza FU, & Wass SV (2021). Anxious parents show higher physiological synchrony with their infants. Psychological Medicine, 1–11, 1–11. 10.1017/s0033291720005085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-Nielsen J, Egmose I, Wendelboe KI, Steinmejer P, Lange T, & Vaever MS (2021). Can the Edinburgh Postnatal Depression Scale-3A be used to screen for anxiety? BMC Psychology, 9(1), 1–11. 10.1186/s40359-021-00623-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-Nielsen J, Matthey S, Lange T, & Væer MS (2018). Validation of the Edinburgh Postnatal Depression Scale against both DSM-5 and ICD-10 diagnostic criteria for depression. BMC Psychiatry, 18(1), 393. 10.1186/s12888-018-1965-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toohey J (2012). Depression during pregnancy and postpartum. Clinical Obstetrics and Gynecology, 55(3), 788–797. 10.1097/grf.0b013e318253b2b4 [DOI] [PubMed] [Google Scholar]
- Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, Xiao X, Zhang W, Krabbendam E, Liu S, Liu Z, Li Z, & Yang BX (2021). Mapping global prevalence of depression among postpartum women. Translational Psychiatry, 11(1), 543. 10.1038/s41398-021-01663-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel A, Haugen EN, Jackson LC, & Brendle JR (2005). Anxiety symptoms and disorders at eight weeks postpartum. Journal of Anxiety Disorders, 19(3), 295–311. 10.1016/j.janxdis.2004.04.001 [DOI] [PubMed] [Google Scholar]