Abstract
Background:
Addressing patients’ social determinants of health is a national priority for cancer treatment centers. Transportation insecurity is one major challenge for patients undergoing active cancer treatment, and missing treatments can result in worse cancer treatment outcomes, including worse morbidity and mortality. How cancer treatment centers are addressing transportation insecurity is understudied.
Methods:
In January and February 2022, the NCCN Best Practices Committee conducted a survey of NCCN’s 31 Member Institutions (currently 32 member institutions as of April 2022) to assess how centers were addressing patient transportation insecurity: how they screen for transportation insecurity, coordinate transportation, and fund transportation initiatives, and their plans to address transportation insecurity in the future.
Results:
A total of 25 of 31 (81%) NCCN Member Institutions responded to the survey, of which 24 (96%) reported supporting the transportation needs of their patients through screening, coordinating, and/or funding transportation. Patients’ transportation needs were most often identified by social workers (96%), clinicians (83%), or patients self-declaring their needs (79%). Few centers (33%) used routine screening approaches (eg, universal screening of social risk factors) to systematically identify transportation needs, and 54% used the support of technology platforms or a vendor to coordinate transportation. Transportation was predominantly funded via some combination of philanthropy (88%), grants (63%), internal dollars (63%), and reimbursement from insurance companies (58%). Over the next 12 months, many centers were either going to continue their current transportation programs in their current state (60%) or expand existing programs (32%).
Conclusions:
Many NCCN Member Institutions are addressing the transportation needs of their patients. Current efforts are heterogeneous. Few centers have systematic, routine screening approaches, and funding relies on philanthropy more so than institutional dollars or reimbursement from insurers. Opportunities exist to establish more structured, scalable, and sustainable programs for patients’ transportation needs.
Background
Transportation insecurity occurs in healthcare contexts when a patient is unable to regularly participate in their healthcare in a safe and timely manner due to the lack of material, economic, or social resources. This insecurity may be due to a number of different factors, including financial stresses that preclude paying for gas, parking, and/or lodging near cancer centers; inadequate social and family support; lack of access to personal transportation; public transportation infrastructure that is not suitable for patients with cancer; and inability to access ride services.1,2 Transportation insecurity is a social risk factor3—adverse social conditions associated with poor health—that frequently co-occurs with other social risk factors, such as financial, housing, and food insecurity.4 This insecurity is a major challenge for patients undergoing active cancer treatment.5-7
Although the precise prevalence of transportation insecurity among patients with cancer is unknown, transportation challenges are common among this population,7-10 and patients undergoing cancer treatment are particularly vulnerable to transportation insecurity. First, the physical limitations that result from cancer or treatments may limit transportation options for patients (eg, the need for a wheelchair accessible vehicle or assistance ambulating from a vehicle to the examination room, or the physical inability to use public transportation).11 Second, financial toxicity is common among patients undergoing cancer treatment,12-14 resulting in constraints to transportation affordability. Third, regionalized centers of excellence are often the nexus for highly specialized cancer care, requiring some patients to travel far distances and spend significant time traveling to access necessary care.15,16 Fourth, cancer care requires frequent clinical encounters for intensive treatments, resulting in many opportunities for transportation insecurity to impact patients’ ability to access care, and compounding financial and practical barriers to accessing care. As a result, patients may miss, delay, or change their care plans.17,18 Ultimately, these disruptions in care can be associated with higher rates of cancer recurrence, worse mortality, and widened racial and income disparities in cancer treatment outcomes.19-21
Although national organizations such as the National Academies of Sciences, Engineering, and Medicine have identified transportation insecurity as a key social risk factor,22,23 how cancer care providers and treatment centers currently address patients’ transportation insecurity is largely unknown. The objective of this study is to characterize the national landscape of how cancer centers assess and manage transportation insecurity among oncology patients. Leveraging the NCCN Best Practices Committee (BPC), we conducted a national survey to identify how NCCN Member Institutions screen for transportation insecurity, coordinate transportation, and fund transportation initiatives, and their plans to address transportation insecurity in the future.
Methods
Study Sample
NCCN is a not-for-profit alliance of 32 leading cancer centers devoted to patient care, research, and education (https://www.nccn.org/home/member-institutions). NCCN Member Institutions are recognized as NCI-designated academic cancer centers. They consist of free-standing institutions as well as matrix cancer centers, and are primarily located in metropolitan areas throughout the United States. Insured and uninsured patients travel from urban, suburban, and rural locations to receive treatment at these cancer centers. NCCN Member Institutions develop resources that provide valuable information to numerous stakeholders, not only in the United States but worldwide. The BPC is comprised of one representative from each of the 32 NCCN Member Institutions. BPC members are senior physician and administrative leaders who work toward improving the effectiveness and efficiency of cancer center operations. The main objective of the BPC is to share operational best practices. This goal is achieved through the collection of cancer center data and information, the formation of workgroups, and discussions at in-person and virtual BPC meetings The BPC conducts several surveys each year on a variety of topics that are of high importance to committee members. At the time of this survey, there were 31 NCCN Member Institutions that constituted the study sample (a new member institution was added after the survey was conducted).
Survey Design
Between January 12 and February 7, 2022, NCCN conducted a patient transportation survey that was disseminated to BPC members. The 8 survey questions (Table 1) were drafted and the survey was pilot tested with 2 BPC members to assess readability and content accuracy. After the pilot, the survey was disseminated to all members of the committee via a web-based tool (SurveyMonkey). Consistent with the BPC’s typical survey process, committee members were instructed to review the survey questions and identify a content expert at their center to complete the survey. Questions focused on how centers screen for transportation insecurity, coordinate transportation, and fund transportation initiatives, and their plans to address transportation insecurity in the upcoming 12 months. The qualifications related to most respondents included titles such as Director, Supervisor, or Manager of social work, patient care services, or supportive services at their respective NCCN Member Institutions. No incentives were offered to BPC members to complete the survey; completing surveys is an expectation of committee membership. Two email reminders were sent to encourage BPC members to ensure their center completed the survey.
Table 1.
Survey Questions
| Category | Question | Number of Respondents |
Center Percentage |
|---|---|---|---|
| Transportation insecurity screening | Does your cancer center support (eg, screen, coordinate, fund) the transportation needs of patients? | 25 | Yes: 96% No: 4% |
| Transportation insecurity screening | How does your cancer center screen for the transportation needs of patients? (Please check all that apply) | 24 | Social worker referral: 96% Clinician referral: 83% Patient or client initiated: 79% Insurance coverage (eg, Medicaid or uninsured): 50% Other: 42% Routine or intermittent screening of patients (eg, annual): 33% |
| Transportation insecurity coordination | Does your cancer center coordinate transportation for its patients? | 24 | Yes, coordinated in collaboration with a ride service (eg, Uber Health, Lyft Health, or a transportation network company): 54% Yes, coordinated solely by the clinic or the cancer center: 46% |
| Transportation insecurity coordination | How does your cancer center coordinate transportation for its patients? (Please check all that apply) | 24 | Calls rides for patients: 83% Provides vouchers for transportation (eg, taxi or public transit): 75% Uses a platform operated by a technology company or vendor (eg, Uber Health, Lyft Health, or a transportation network company): 54% Other: 54% Uses a platform operated by a transportation broker (eg, ModivCare or Logisticare): 17% |
| Transportation insecurity funding | How is transportation for your cancer center patients funded? (Please check all that apply) | 24 | Philanthropy: 88% Internal, operational dollars: 63% Grants: 63% Insurance covers transportation: 58% Other: 17% |
| Transportation insecurity in the upcoming 12 months | Which of the below best describes your cancer center’s plans for patient transportation in the next 12 months? | 25 | Continuing program(s) in current state: 60% Expanding existing program(s): 32% Starting new program(s): 4% None of the above: 4% |
| Transportation insecurity in the upcoming 12 months | In the next 12 months, how important is it for your cancer center to solve transportation challenges for patients? | 25 | Extremely important: 44% Very important: 20% Moderately important: 28% Slightly important: 8% Not at all important: 0% |
| Transportation insecurity in the upcoming 12 months | What types of transportation challenges is your cancer center currently facing? | 12 | Open text box responses |
Descriptive Analysis
Survey responses were analyzed using means and proportions to characterize observed patterns. The study protocol was determined to not meet the definition of human subjects research by the University of Pennsylvania Institutional Review Board.
Results
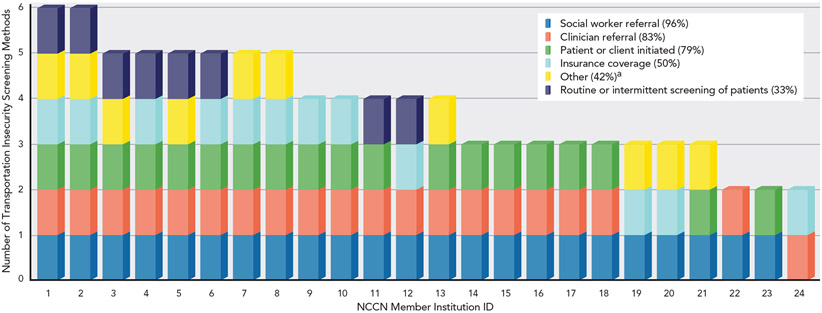
In total, 25 of 31 (81%) NCCN Member Institutions responded to the survey. Among the respondents, 24 (96%) supported the transportation needs of patients by implementing processes for screening, coordinating, or funding transportation. Patients’ transportation needs were most often identified by some combination of social workers (96%), clinicians (83%), or patients self-declaring their needs (79%) (Figure 1). Few centers (33%) used routine screening approaches to identify transportation needs, such as universally screening all patients for social risk factors at regular intervals.
Figure 1. Responses to “How does your cancer center screen for the transportation needs of its patients?,” depicting common methods of transportation insecurity (N=24).
aIncluding distress screenings, initial screening prior to first appointment, patient-reported outcomes survey through medical record, part of all outpatient nurse assessments, patient navigation screening, scheduling team obtains transportation issues and needs of patients, any medical professional can help identify the need and refer to social work.
Among the 24 centers that supported transportation needs, all of them coordinated the patients’ transportation needs, with 11 (46%) using support staff within their treatment centers to coordinate transportation, and 1 even employing a full-time transportation coordinator (4%). However, 54% of the responding centers used the support of technology platforms or a vendor to coordinate transportation, such as Uber Health, Lyft Health, or another technology-enabled transportation network company. Many centers called rides for patients (83%), provided vouchers for transportation (75%) to facilitate taxi rides or public transit, and some used community resources, insurance company processes to support nonemergency medical transportation, or contracted directly with local transportation services, such as cab companies.
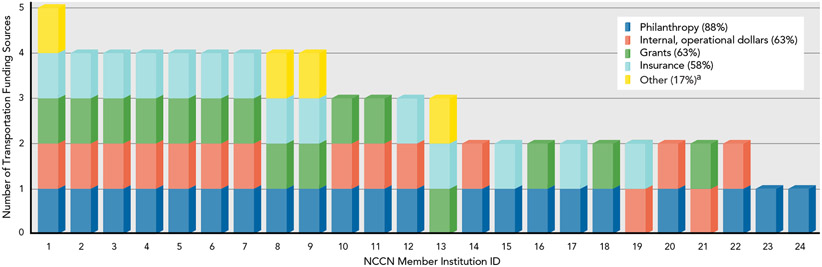
Transportation was funded through a variety of mechanisms, such as philanthropy (88%), grants (63%), internal dollars (63%), and insurance coverage (58%) (Figure 2). One site noted that the only insurance that covers transportation is Medicaid (4%).
Figure 2. Responses to “How is transportation for your cancer center patients funded?,” illustrating transportation funding sources (N=24).
aIncluding local and regional nonprofits, city programs, clinical trial sponsors, etc.
When asked about centers’ plans for the next 12 months, one center was planning to start a new program to address transportation (4%) and some stated they would expand existing programs (32%). Most centers were going to continue their transportation programs in the current state (60%). When asked how important it was for cancer centers to solve transportation challenges for their patients, 22 of 24 centers (92%) felt transportation was at least moderately important, with 44% responding that it was extremely important.
Discussion
A national priority for cancer treatment centers is to address patients’ social risk factors of health that impact treatment and outcomes. Transportation insecurity is one major challenge for many patients undergoing cancer treatment. For some patients, it is a challenge before they begin their treatment and for others it becomes a significant challenge as they undergo treatment. Missing treatments can result in worse cancer treatment outcomes, including worse morbidity and mortality. How cancer treatment centers are addressing patient transportation insecurity is understudied.
The NCCN BPC survey had 3 key findings. Many NCCN Member Institutions have begun addressing the transportation needs of their patients. Most centers have implemented processes for screening, coordinating, or funding transportation, and many believe that patient transportation issues are moderately or extremely important. However, few centers have a standardized approach to routine screening, and there is variability regarding how centers cover transportation assistance services. Most centers cite philanthropy as the main source of funding, more so than institutional dollars or payer-driven mechanisms.
On one hand, these findings highlight how NCCN Member Institutions commonly address the challenge of transportation for their patients. On the other hand, there remain opportunities to reduce transportation insecurity. How to screen for transportation issues is not standardized across cancer centers. We found that the most common methods of screening were through referrals to social workers, clinicians triggering referrals, or patients declaring their need. The accuracy of provider-initiated referral or self-referral mechanisms for detecting transportation insecurity among patients with cancer is unknown. Without systematic screening practices, patients who may benefit from transportation assistance (eg, those with financial hardship, have long distances to travel, or are physically impaired by their specific type of cancer or treatment regimen) may not be identified and linked to necessary services. Although screening for transportation insecurity and documenting how patients are connected to resources is beginning to occur in the primary care setting,24-27 only 35% of outpatient practices and 74% of hospitals routinely screen for transportation insecurity.28 Our study found that 33% of NCCN Member Institutions routinely screened for transportation insecurity, a setting where there may be an even more critical need.
Why might routine universal screening not occur? There are significant components of the screening pathway that are understudied, and optimization would likely yield better care: how to screen (eg, widely accepted, validated among patients with cancer), when to screen (eg, at home, in clinics), how frequently to screen (eg, regularly every 3 months or after a missed appointment), which screening medium (eg, through the electronic health record, phone survey, tablets), how to implement (eg, front desk screening, self-reported questionnaires, social work administered), and whether patients will find screening questions about social risk factors acceptable while undergoing cancer treatment.
Additionally, we observed significant heterogeneity across cancer centers with regard to how they addressed and funded transportation insecurity. Although a nonemergency medical transportation benefit (eg, rides to and from doctors’ appointments) is available through certain insurance plans, healthcare facilities, such as cancer centers, are not required to provide these benefits nor do they routinely screen patients for social risk factors. Therefore, patients with transportation needs are not routinely identified. As a result, studies are needed to help (1) characterize the prevalence of transportation insecurity among patients with cancer, and (2) determine the effectiveness of interventions to address transportation needs on downstream health (eg, completion of cancer-directed therapy) and economic (eg, clinical revenue) outcomes. Although some intervention studies have been published,29,30 more evidence is needed to guide how and when provider and payer organizations support transportation interventions for patients undergoing cancer treatment. Quantifying and articulating these impacts to payers, providers, and patients can inform practice and payment change toward supporting interventions that address the social risk factors of patients across the cancer care continuum.
Furthermore, we need to better understand how transportation insecurity interacts with other social risk factors. Transportation insecurity may be the result of unemployment or the consequence of an individual’s decision to avoid the financial toxicity that often ensues for patients undergoing cancer care. Transportation barriers may depend on the patient’s severity of illness. Patients who are severely ill may be unable to drive or access public transportation to attend their scheduled cancer appointments. Distance from the healthcare facility and availability, or lack thereof, of public transportation, including ride services, may factor into a patient’s transportation challenges. Inadequate social support, such as relatives or friends who can help transport patients to and from medical appointments, may also contribute to an individual’s transportation insecurity. The independent and combined effects of these different social risk factors should be studied, and multimodal interventions are likely needed.
Our findings have limitations. The NCCN BPC survey is cross-sectional. Although our study illuminates how NCCN Member Institutions are addressing transportation challenges, there is little information about how these programs have evolved over time. Transportation network companies and ridesharing-based programs are new features to the nonemergency medical transportation landscape. How these interventions improve access to care have mixed evidence but have not been adequately studied among patients being treated for cancer. Our findings may be limited by responder bias (19% of NCCN Member Institutions did not respond) or the Hawthorne effect, as NCCN Member Institutions may not want to self-report that they are not adequately screening for or addressing the transportation needs of their patient population now or in the future. Furthermore, the findings from NCCN Member Institutions may not reflect how other cancer treatment centers or clinical practices are responding to this challenge. Yet, how NCCN Member Institutions are responding to the transportation needs of patients undergoing cancer treatment is important, because these cancer centers are important models for setting care standards in the United States and can influence how policymakers, payers, and other provider organizations choose to improve the care of patients with cancer. Furthermore, indepth qualitative and quantitative assessments studying how these cancer centers screen for transportation insecurity coordinate transportation, and fund transportation initiatives, and their plans to address transportation insecurity will be informative and further the understanding of practice gaps which, if closed, may improve clinical and patient-reported outcomes for patients undergoing cancer care.
Conclusions
In this cross-sectional study of NCCN Member Institutions, we identified that most cancer centers have mechanisms in place to screen, address, and fund initiatives to address transportation insecurity among patients with cancer. However, variability exists across cancer centers, and critical details for the development and sustainment of effective programs are not known. Understanding how NCCN Member Institutions are addressing the challenge of transportation insecurity provides a lens into the real-world implementation of transportation interventions for patients undergoing cancer treatment. Evaluating how these interventions impact patients’ access to cancer treatments and treatment outcomes remains an important next step. In addition, assessment of the practical and financial impact of missed appointments due to transportation challenges could help establish further impetus to support the needs of patients with cancer. A more structured approach can answer these questions, as well as establish the need for transportation assistance as a basic element of cancer care for many in need.
Footnotes
Disclosures: Dr. Chaiyachati has disclosed receiving grant/research support from PCORI, the RAND Corporation, Roundtrip, Inc., and Independence Blue Cross, Inc.; serving on a board for Primary Care Progress, Inc.; serving as a consultant for Verily Life Sciences, Inc.; and being employed by Verily Life Sciences, Inc. Dr. Graboyes has disclosed receiving grant/research support from and serving as a consultant for Castle Biosciences. Dr. Shulman has disclosed receiving grant/research support from the Breast Cancer Research Foundation. The remaining authors have disclosed being employed by the National Comprehensive Cancer Network.
References
- 1.Gould-Werth A, Griffin J, Murphy AK. Developing a new measure of transportation insecurity: an exploratory factor analysis. Surv Pract 2018;11:0024. [Google Scholar]
- 2.Gravity Project. Introducing the Gravity Project. Accessed on March 21, 2022. Available at: https://thegravityproject.net/
- 3.Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q 2019;97:407–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitman A, De Lew N, Chappel A, et al. Addressing Social Determinants of Health: Examples of Successful Evidence-Based Strategies and Current Federal Efforts. Washington, DC: US Department of Health and Human Services, Office of Health Policy: 2022. [Google Scholar]
- 5.Guidry JJ, Aday LA, Zhang D, et al. Transportation as a barrier to cancer treatment. Cancer Pract 1997;5:361–366. [PubMed] [Google Scholar]
- 6.Zullig LL, Jackson GL, Provenzale D, et al. Transportation: a vehicle or roadblock to cancer care for VA patients with colorectal cancer? Clin Colorectal Cancer 2012;11:60–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jazowski SA, Sico IP, Lindquist JH, et al. Transportation as a barrier to colorectal cancer care. BMC Health Serv Res 2021;21:332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang C, Deng L, Wang Q, et al. Transportation barriers to health care and mortality risk among the U.S. adults with history of cancer [abstract]. J Clin Oncol 2021;39(Suppl):Abstract 121. [Google Scholar]
- 9.Jiang C, Yabroff KR, Deng L, et al. Self-reported transportation barriers to health care among US cancer survivors. JAMA Oncol 2022;8:775–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barrington WE, DeGroff A, Melillo S, et al. Patient navigator reported patient barriers and delivered activities in two large federally-funded cancer screening programs. Prev Med 2019;129(Suppl):105858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jankowski C, Berger AM, Aranha O, et al. NCCN Clinical Practice Guidelines in Oncology: Cancer-Related Fatigue. Version 2.2022. Accessed March 21, 2022. To view the most recent version, visit https://www.nccn.org [Google Scholar]
- 12.Ramsey S, Blough D, Kirchhoff A, et al. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood) 2013;32:1143–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guy GP Jr, Ekwueme DU, Yabroff KR, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol 2013;31:3749–3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhanvadia SK, Psutka SP, Burg ML, et al. Financial toxicity among patients with prostate, bladder, and kidney cancer: a systematic review and call to action. Eur Urol Oncol 2021;4:396–404. [DOI] [PubMed] [Google Scholar]
- 15.Herb JN, Dunham LN, Mody G, et al. Lung cancer surgical regionalization disproportionately worsens travel distance for rural patients. J Rural Health 2020;36:496–505. [DOI] [PubMed] [Google Scholar]
- 16.Siegel J, Engelhardt KE, Hornor MA, et al. Travel distance and its interaction with patient and hospital factors in pancreas cancer care. Am J Surg 2021;221:819–825. [DOI] [PubMed] [Google Scholar]
- 17.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013;38:976–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Etminani-Ghasrodashti R, Kan C, Mozaffarian L. Investigating the role of transportation barriers in cancer patients’ decision making regarding the treatment process. Transp Res Rec 2021;2675:175–187. [Google Scholar]
- 19.Yabroff KR, Reeder-Hayes K, Zhao J, et al. Health insurance coverage disruptions and cancer care and outcomes: systematic review of published research. J Natl Cancer Inst 2020;112:671–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheridan R, Oliver SE, Hall G, et al. Patient non-attendance at urgent referral appointments for suspected cancer and its links to cancer diagnosis and one year mortality: a cohort study of patients referred on the Two Week Wait pathway. Cancer Epidemiol 2019;63:101588. [DOI] [PubMed] [Google Scholar]
- 21.Etminani-Ghasrodashti R, Khan MA, Mozaffarian L. Modeling the structural relationships between travel distance, built environment, and cancer outcomes. J Urban Plann Dev 2022;148:05022016. [Google Scholar]
- 22.Transit Cooperative Research Program. Guidebook and Research Plan to Help Communities Improve Transportation to Health Care Services. Washington, DC: National Academies Press; 2021. [Google Scholar]
- 23.Transit Cooperative Research Program. Dialysis Transportation: The Intersection of Transportation and Healthcare. Washington, DC: National Academies Press; 2019. [Google Scholar]
- 24.Byhoff E, De Marchis EH, Hessler D, et al. Part II: a qualitative study of social risk screening acceptability in patients and caregivers. Am J Prev Med 2019;57(Suppl 1):S38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Marchis EH, Hessler D, Fichtenberg C, et al. Part I: a quantitative study of social risk screening acceptability in patients and caregivers. Am J Prev Med 2019;57(Suppl 1):S25–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gottlieb L, Fichtenberg C, Adler N. Screening for social determinants of health. JAMA 2016;316:2552. [DOI] [PubMed] [Google Scholar]
- 27.Gottlieb L, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med 2017;53:719–729. [DOI] [PubMed] [Google Scholar]
- 28.Fraze TK, Brewster AL, Lewis VA, et al. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by us physician practices and hospitals. JAMA Netw Open 2019;2:e1911514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Damico N, Deshane A, Kharouta MZ, et al. Rideshare services for patients undergoing daily radiation therapy. Int J Radiat Oncol Biol Phys 2020;108(Suppl):e388. [Google Scholar]
- 30.Manning M, Marquez R, Woodruff H, et al. The impact of rideshare transportation in radiation oncology. Int J Radiat Oncol Biol Phys 2020;108(Suppl):S99–100. [Google Scholar]