Abstract
The pathogenesis of gastroesophageal reflux disease (GERD) is multifactorial. The severity of abnormal reflux burden corresponds to the dysfunction of the antireflux barrier and inability to clear refluxate. The crural diaphragm is one of the main components of the esophagogastric junction and plays an important role in preventing gastroesophageal reflux. The diaphragm, as a skeletal muscle, is partially under voluntary control and its dysfunction can be improved via breathing exercises. Thus, diaphragmatic breathing training (DBT) has the potential to alleviate symptoms in selected patients with GERD. High-resolution esophageal manometry (HRM) is a useful method for the assessment of antireflux barrier function and can therefore elucidate the mechanisms responsible for gastroesophageal reflux. We hypothesize that HRM can help define patient phenotypes that may benefit most from DBT, and that HRM can even help in the management of respiratory physiotherapy in patients with GERD. This systematic review aimed to evaluate the current data supporting physiotherapeutic practices in the treatment of GERD and to illustrate how HRM may guide treatment strategies focused on respiratory physiotherapy.
Keywords: Diaphragmatic breathing training, Gastroesophageal reflux disease, High-resolution manometry
Introduction
Gastroesophageal reflux disease (GERD) is a global health issue affecting a significant part of our population. Traditionally, GERD has been considered a disease of middle-aged adults and the elderly, but in the last decade, there has been an increase in the prevalence of GERD in younger patients—probably due to the rise in obesity [1]. A combination of multiple risk factors, most of which are related to lifestyle, usually contributes to the development of reflux symptoms [2].
In addition to lifestyle changes (including dietary changes, weight reduction, and smoking cessation), antisecretory treatment with proton pump inhibitors (PPIs) remains the main therapeutic approach that improves both symptoms and quality of life in most patients with GERD—especially in those with reflux esophagitis. However, this treatment does not target the mechanisms of reflux, as it does not strengthen the antireflux barrier or promote esophageal refluxate clearance. Thus, long-term antisecretory treatment is often necessary. Patients who do not adequately respond to pharmaceutical interventions should undergo upper endoscopy and esophageal testing—specifically, pH metry with impedance to phenotype the GERD and optimize patient treatment [3]. Endoscopy and high-resolution esophageal manometry (HRM) help define the integrity of the antireflux barrier and the anatomy of the gastroesophageal flap valve. HRM may also assess peristaltic function, which is important for refluxate clearance. Currently, the only standard therapeutic procedure that results in the recovery of the antireflux barrier is antireflux surgery. Laparoscopic fundoplication not only restores the anatomical properties of esophagogastric junction (EGJ), but also reduces the frequency of transient lower esophageal sphincter relaxation (TLESr), including reflux-associated TLESr, which is considered the main pathophysiological mechanism of GERD [4, 5]. Conversely, endoscopic techniques (for example, controlled delivery of radiofrequency energy [Stretta] at the level of lower esophageal sphincter [LES] or devices intended for transoral incisionless fundoplication [Esophyx, MUSE]) mainly affect the distensibility of the EGJ and do not target hiatus hernia or the crural defect [6].
Respiratory physiotherapy to strengthen inspiratory muscles, especially the diaphragm, can improve the function of the antireflux barrier [7–9]. This approach is a comprehensive procedure leading to an improvement of chest expansivity, airway clearance, and the enhancement of respiratory muscles. Breathing exercises or diaphragmatic breathing training (DBT), using various techniques to increase the muscle tone of the diaphragm, are part of this procedure, but specific devices with controllable resistance of inhaled air can also be used. Besides DBT, effective physiotherapeutic techniques involving visceral manipulation might improve the function of myofascial tissue and respiratory muscles, as a result. However, breathing exercises are still not recognized as a standard means for GERD management because scientific evidence is lacking in this area. Moreover, the selection of patients who might benefit from respiratory physiotherapy is not well understood.
This systematic review aimed to assess the effectiveness of breathing exercises in patients with GERD and demonstrate the usefulness of HRM in GERD treatment guidance. Moreover, we characterized specific respiratory techniques, using visual documentation, which may be of practical benefit to both gastroenterologists and physiotherapists in understanding how breathing exercises affect the antireflux barrier
Role of the Diaphragm as an Antireflux Barrier
The diaphragm is a striated flat muscle separating the thoracic and abdominal cavities, and is considered to be the main inspiratory muscle. It also serves as a postural stabilizer, and the crural diaphragm (CD) is an important component of the antireflux barrier [10, 11]. Studies quantifying the CD within the EGJ concluded that approximately 85% of overall EGJ contractility is attributable to the diaphragm [12]. As a skeletal muscle, the diaphragm is partially under voluntary control and its dysfunction can be improved by various techniques of respiratory physiotherapy. Strengthening the diaphragm may also have beneficial effects on the other components of the antireflux barrier—not only the EGJ.
Ideal involvement of the diaphragm in these functions requires maintenance of the caudal position of the chest, which is ensured by the balanced activity of the abdominal and pectoral muscles, and upper chest fixators [10]. Most patients with GERD typically have an imbalance in the auxiliary respiratory muscles, with their chest taking the inspiratory position that is labeled “open scissors syndrome” among respiratory physiotherapists (Fig. 1) [11]. Open scissors syndrome posture is an example of impaired lumbar spine stabilization, with the disturbed position of the thoracic and pelvic planes. This subsequently leads to a change in breathing pattern, with reduced activity of the CD. Moreover, it may also result in LES-CD separation, which is considered a significant risk factor for GERD, further leading to the development of hiatus hernia [13]. On the other hand, all activities that increase the diaphragm’s demands on its postural function, such as coughing, the Valsalva maneuver, or lifting the limbs, may lead to a reflexive increase in LES tone [6, 14]. Additionally, due to the increased activity of the diaphragm, both EGJ competence and relaxation change. Reduced EGJ compliance forces the esophagus to exert greater contractile vigor during swallowing. Thus, improved diaphragmatic function may result in better esophageal peristalsis, which is an essential component of the antireflux barrier [15–17].
Fig. 1.
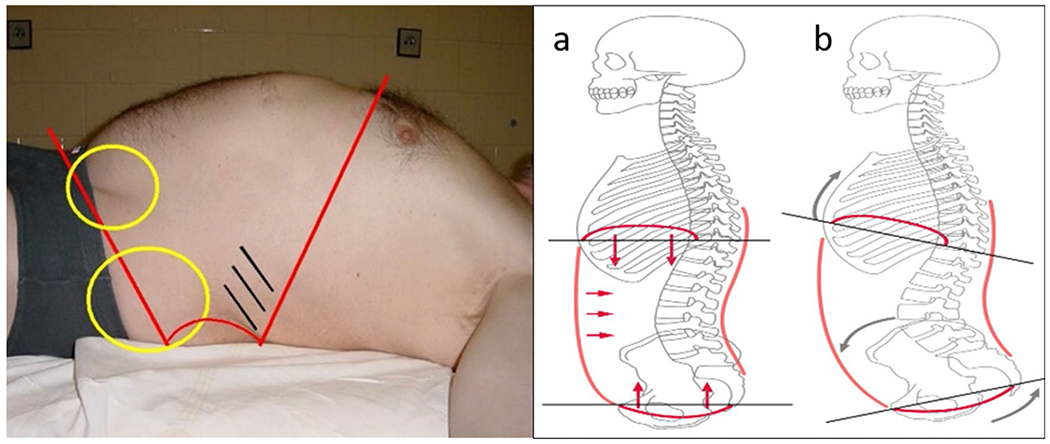
Open scissors syndrome. Left: An example of impaired lumbar spine stabilization. The red lines represent the plane of the chest (diaphragm) and pelvis (with their incorrect positions), and lordotization of the lumbar spine in the so-called “open scissors syndrome.” The yellow circles indicate a loss of abdominal muscle function. The black lines represent a defect in the position of the lower ribs. Right: Schematic representation of the ideal and disturbed positions of the planes of the chest, pelvis, and lumbar spine. a Ideal position, with the planes of the diaphragm and pelvis placed horizontally above each other; b instability of the lumbar spine, with incorrect position of individual body segments corresponding to open scissor posture (reprinted with permission of Petr Bitnar)
HRM as a Useful Tool in the Management of Respiratory Physiotherapy
HRM has become a crucial part of the diagnostic procedure in patients with PPI refractory symptoms. Evaluation of the morphology and integrity of the EGJ has become a priority in the new version of the Chicago classification [12]. HRM not only provides parameters assessing the function of the antireflux barrier, but also allows the evaluation of the esophageal reserve, using various provocation maneuvers [13, 18]. Basal LES tone, presence of LES-CD separation, or esophageal contractile vigor are the main parameters describing the integrity and function of the antireflux barrier. HRM, and especially three-dimensional HRM, has enabled detailed imaging of the EGJ and provided insight into the functional contribution of indiviual EGJ components. This reveals a number of new parameters, such as the EGJ contractile integral (EGJ-CI), which also have predictive value in assessing the severity of GERD [19, 20]. Moreover, a number of these parameters directly reflect diaphragmatic function, especially LES-CD separation or inspiratory augmentation [16], supporting the importance of focusing on the diaphragm in the therapeutic approach to GERD.
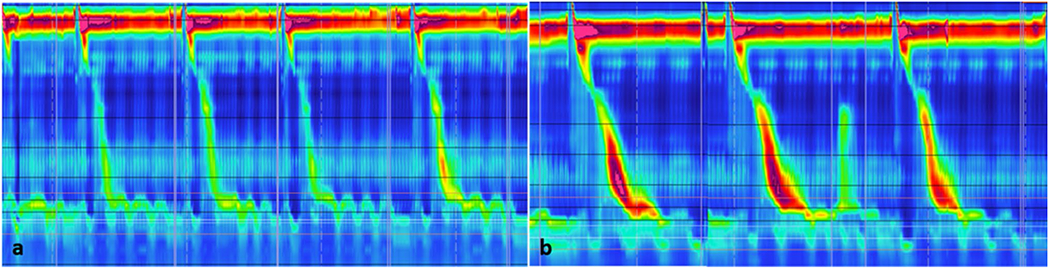
HRM may be a very useful tool in guiding respiratory physiotherapy itself, since various respiratory techniques performed during manometric examination may reveal not only EGJ dysfunction (Fig. 2), but also esophageal reserves (Fig. 3) that may not be apparent from standard assessments. This may help to understand the mechanism of reflux in a particular patient, creating a more appropriate therapeutic approach, as well as determine the appropriate load of breathing exercises. Signs indicating a more severe degree of antireflux barrier incompetence (for example, hypotensive LES or hiatus hernia), should further influence the therapeutic process. Moreover, patients who undergo DBT during treatment need to be motivated, since only regularly performed exercises have the potential to improve the antireflux barrier over time. HRM objectively and very clearly demonstrates the exact changes in EGJ function and esophageal clearence, obvious to patients themselves (Figs. 4 and 5). Therefore, HRM has the potential to be used as a method for biofeedback treatment for GERD patients. Halland and colleagues have used this approach in patients with rumination syndrome [21]. The researchers used postprandial HRM not only for diagnosis, but also for DBT in patients suffering from rumination. The study demonstrated both good tolerance of HRM during training, as well as its beneficial effect in reducing the disturbed gastroesophageal pressure gradient that is responsible for rumination.
Fig. 2.
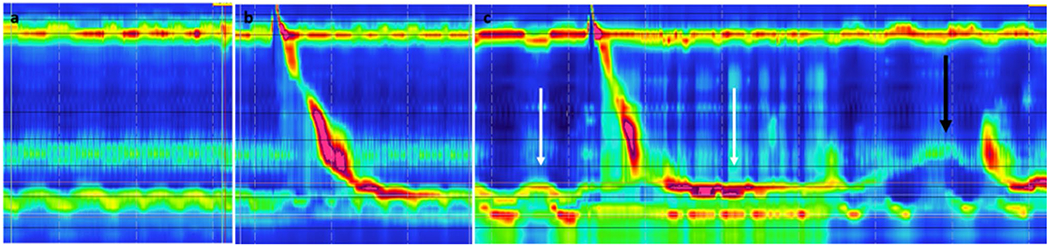
Esophagogastric junction (EGJ) dysfunction revealed during contraction of the abdominal muscles in the manometric study. Increased EGJ compliance may not be apparent until intra-abdominal pressure has increased. Various physical activities performed during manometric examination may reveal EGJ dysfunction. In this case, an abdominal strengthening exercise with leg raises showed the disruption of the EGJ (c) with lower esophageal sphincter-crural diaphragm separation of a size of 2.5 cm (white arrows), and by apparent transient lower esophageal sphincter relaxation (black arrow). EGJ dysfunction was visible neither during the resting phase (a) nor during swallowing (b)
Fig. 3.
Increase in esophageal contractility during diaphragmatic breathing training (DBT). Provocative tests such as multiple rapid swallow or rapid drink challenge are used to determine the contractile reserve of the esophageal body during manometry. An increase in the tonic activity of the crural diaphragm during DBT leads to a decrease in esophagogastric junction (EGJ) relaxation during deglutition. Reduced EGJ relaxation represents some degree of obstruction in EGJ flow that is accompanied by an increase in esophageal contractility (black arrows). Therefore, application of DBT may demonstrate contractile reserve of the esophageal body that is not apparent when using the provocative tests during standard manometry studies (white arrows indicate where we usually expect augmented peristalsis)
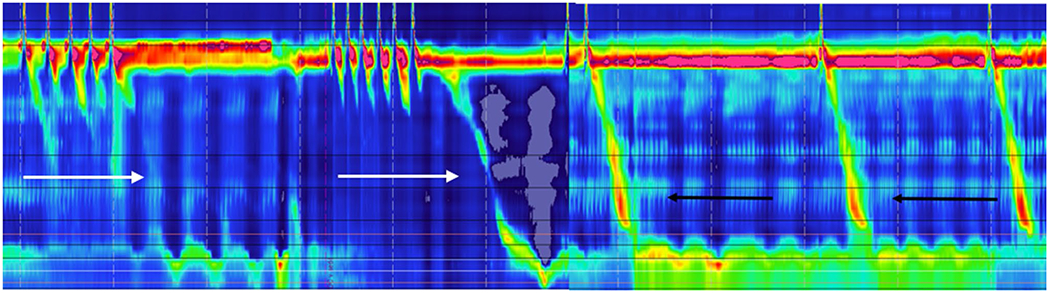
Fig. 4.
High-resolution manometry (HRM) before and after respiratory physiotherapy in a case of hypotensive lower esophageal sphincter (LES). The finding on HRM shows an increase in the tone of the LES after respiratory physiotherapy was applied in a patient with initial hypotensive LES. Left: Evaluation in the landmark (a) and in a swallow (b) before respiratory physiotherapy (mean LES pressure 7.9 mmHg). Right: Evaluation in the landmark (c) and in a swallow (d) after respiratory physiotherapy (mean LES pressure 33.3 mmHg)
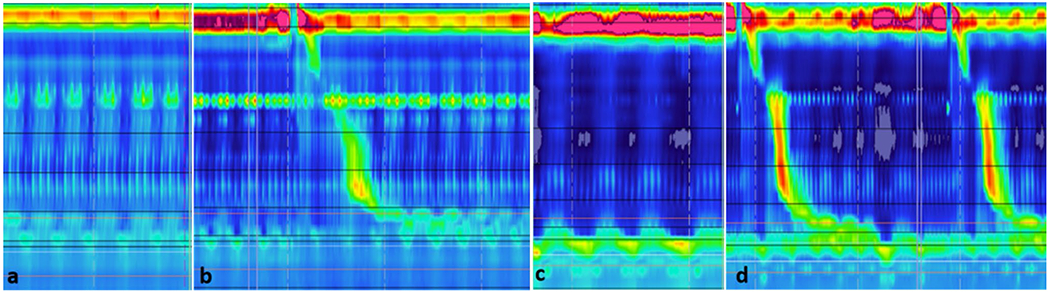
Fig. 5.
High-resolution manometry (HRM) before and after respiratory physiotherapy in a case of ineffective esophageal motility (IEM). The finding on HRM shows an increase in the contractile vigor of the esophagus after respiratory physiotherapy was applied in a patient with initial IEM (assessed according Chicago classification v3.0). a Evaluation of esophageal contractility before respiratory physiotherapy (mean distal contractile integral [DCI] 632 mmHg.cm.s; half of all swallows were weak); b Evaluation of esophageal contractility after respiratory physiotherapy (mean DCI 1620 mmHg.cm.s; no swallows were weak)
Respiratory Physiotherapy in Patients with GERD
Although respiratory physiotherapy includes various techniques focused particularly on improving diaphragmatic function, there are many ways to perform breathing exercises. The main goal is to change the breathing pattern from thoracic to abdominal, where abdominal breathing is the ideal breathing pattern. For optimal activation of the diaphragm during DBT, caudal position of the chest is necessary [10, 11]. The caudalization of the chest itself will increase the involvement of the diaphragm in the EGJ, as showed in Fig. 6. Chest caudalization may also reduce esophageal shortening—one of the key events leading to EGJ opening during TLESr [5]. The manual contact of the therapist helps not only to maintain the correct position of the chest during breathing exercises, but enables the patient to focus on activating all parts of the diaphragm, i.e., to breath into the ventral, lateral, and dorsal parts of the abdominal cavity. Greater involvement of the diaphragm is achieved by increasing diaphragmatic postural activity, through various maneuvers [6, 10]. As shown in Fig. 6, triflexion of the lower limbs, used by physiotherapists for ideal co-activation of trunk muscles, increases the postural demands on diaphragm, resulting in higher diaphragmatic involvement in EGJ pressure. Triflexion of the lower limbs also enables the gradual increase in exercise load, which is very important in patients with suspected higher order EGJ dysfunction. Despite the more severe degree of dysfunction of the antireflux barrier, DBT is a suitable form of regular physical activity that can improve physical condition, in addition to improving GERD symptoms [22]. DBT can also prevent, for example, the development of lower back pain, since this condition is highly associated with open scissor syndrome [11].
Fig. 6.
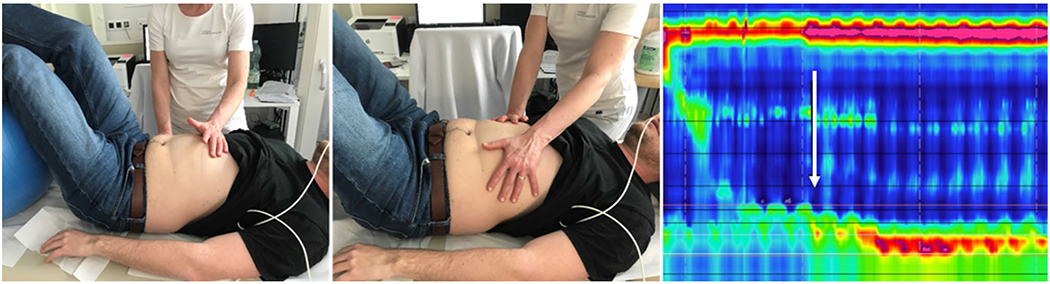
The caudalization of the chest during respiratory physiotherapy. For ideal involvement of the diaphragm during breathing exercises, manual correction of the chest to the caudal position is usually necessary before respiratory physiotherapy. The greater engagement of the diaphragm in the function of the esophagogastric junction after this adjustment is evident, using high-resolution manometry (HRM; white arrow) (photo taken with permission of the patient)
The role of physiotherapists for patients with GERD is not only in guiding physiotherapy. Physiotherapists also help treat another musculoskeletal system dysfunctions, such as reduced back muscle strength, scoliosis and kyphosis, or cervical vertebropathy, which are closely related to GERD [23–25]. Patients with GERD are generally less active than those without GERD [26]; however, strenuous physical activity in individuals with EGJ dysfunction may be predisposed to exercise-induced reflux. Increased EGJ compliance presents in GERD patients (even in those without hiatus hernia) and is likely to be partially responsible for the reflux that occurs during increased intra-abdominal pressure [27].
Methods
We performed an online search to identify relevant clinical trials regarding the effect of respiratory physiotherapy in patients with GERD. English language databases (Pubmed, Cochrane library, Google scholar) were used for the search, with the following keywords: “reflux”, “reflux disease”, “GERD”, “gastroesophageal reflux disease”, AND “diaphragmatic breathing”, “diaphragmatic breathing training”, “breathing exercises”, “respiratory physiotherapy”, abdominal breathing”, “inspiratory muscle training”. Only studies published in peer-reviewed journals since 2000 were included. Inclusion criteria were applied to adult patients diagnosed with GERD, based on typical symptoms confirmed by endoscopic examination or 24 h esophageal pH measurement. The study interventions were techniques of respiratory physiotherapy aimed at increasing the activity of diaphragmatic function, while control groups were treated only pharmacologically or underwent sham breathing exercises. The primary outcomes were reflux symptoms, quality of life (QoL) evaluated by standardized questionnaires, consumption of antireflux medication, and objective parameters of antireflux barrier function demonstrated on esophageal manometry or esophageal pH metry. The exclusion criteria included a different publication format from the clinical study (i.e., review, letter, or case report), duplicate studies, studies in the pediatric population, inappropriate study groups such as patients suffering from a disease other than GERD, and inconvenient interventions use or outcomes in the study (i.e., parameters not corresponding to GERD).
Results
Our literature search (performed by LZ and KB) identified 163 studies. After examining the titles and abstracts, we excluded 146 irrelevant studies, while the remaining 17 studies underwent full text reading. Additionally, six articles were discarded due to inapproprite study group use or outcomes, or they were duplicates. Eleven eligible studies were included in our systematic review. The flow diagram of literature searching is shown in Fig. 7.
Fig. 7.
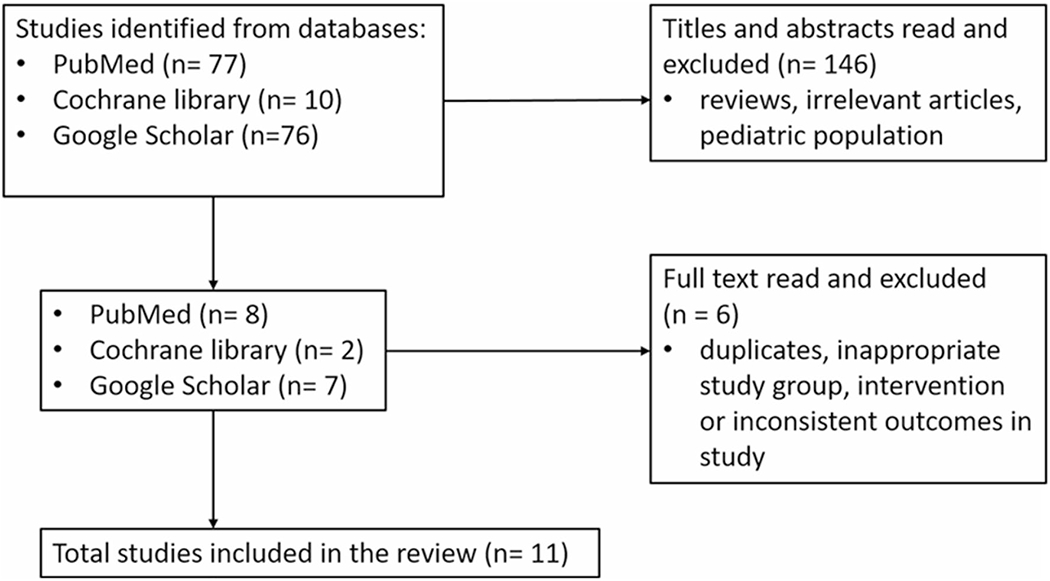
Flow diagram of literature screening
In a randomized controlled trial, Eherer and colleagues [28] studied the effect of breathing exercises in patients with nonerosive reflux disease (NERD) and healed esophagitis. QoL, pH metry, and on-demand PPI usage were assessed at baseline and after 4 weeks of training. Patients in the training group practiced abdominal breathing techniques for 30 min per day. QoL and PPI usage were also evaluated after 9 months of continual training. A significant reduction in acid exposure time (AET) was found in the trained group compared to controls. QoL also improved, and PPI use decreased to one third of the initial dose after 9 months in patients who continued practicing breathing exercises.
Da Silva et al. [29] performed a randomized controlled study using 38 patients with GERD, where 22 patients underwent osteopathic techniques and 16 were in the placebo group. The osteopathic techniques included respiratory maneuvers, using manual contact of the physiotherapist on the lower part of the thoracic cage during deep respiration. An average respiratory pressure and maximum expiratory pressure of the LES were measured by manometry before and immediately after the osteopathy. An increase of 9–27% in LES pressure was observed in patients who performed the osteopathic maneuver.
Carvalho de Miranda Chaves et al. [30] performed a prospective, sham-controlled study in GERD patients with hypotensive LES. The researchers evaluated the effect of inspiratory muscle training (IMT), using a specific device with controllable resistance of inhaled air on esophageal manometry and pulmonary function, after 8 weeks of training. Patients in the experimental group used a threshold device twice a day with progressive loading, while the threshold for sham-treated patients was stable for the whole period. The mid-respiratory pressure (MRP) increased in 75% of patients in the experimental group, with average increase of 46.6%. MRP increased in 66% of patients in the sham group, with an average increase of 26.2%. The researchers concluded that IMT increases LES pressure in patients with GERD, regardless of the resistence load.
Nobre e Souza et al. [31] prospectively assessed the impact of IMT on pH metry, manometry, and autonomic function in GERD patients. The patients entered a 5 days a week training program under progressive inspiratory resistance, using a threshold IMT device. The authors showed that IMT increased average EGJ pressure, decreased the number and cumulative duration of TLESrs, and also decreased the proximal progression of reflux. Heartburn and regurgitation scores decreased significantly after 2 months of training.
Sun et al. [32] investigated the effectiveness of diaphragm biofeedback training in 40 patients with GERD, in short-term and long-term follow-up. Patients were randomized to receive breathing exercises and PPI treatment (rabeprazole), or rabeprazole alone. The diaphragm biofeedback training/rabeprazole group showed significant improvement in reflux symptoms and EGJ pressure after 8 weeks compared to baseline values. Acid suppressing drug use significantly decreased at the 6-month mark, where 82% of patients in the study group (diaphragm biofeedback training/rabeprazole) had ceased PPI use after breathing exercises, while only 6.2% of patients in the control group (rabeprazole only) had ceased PPI use.
In a study by Ong et al. [33], the effect of diaphragmatic breathing was assessed in GERD patients who exhibited a dominant symptom of supragastric belching. Fifteen patients were enrolled in the training group, while 21 controls were placed on a waitlist. Patients underwent four weekly sessions over a period of 4 weeks. After training, 80% of participants in the treatment group, compared to only 19% of participants in the control group, had a significantly reduced belching frequency, measured via a Visual Analog Scale score. Reflux symptoms and QoL scores also significantly increased in training group, and these changes were sustained 4 months post treatment.
Moffa et al. [34] performed a prospective study in 21 patients with NERD and evaluated reflux symptoms and laryngoscopic findings before and after IMT. Nineteen patients completed the training program, which consisted of modified breathing exercises in supine and sitting positions performed twice a day for 4 weeks. The questionnaire scores of esophageal and extraesophageal symptoms (GERD esophageal symptomatology [GERDQ], extra-esophageal GERD symptomatology [RSI], GERD-Health-Related Quality of Life Questionnaire [GERD-HRQL]) significantly reduced after treatment, and laryngeal endoscopy scores greatly improved.
Martinez-Hurtado et al. [35] aimed to demonstrate whether diaphragmatic myofascial release (MFR) had any effect on the symptoms, QoL, and use of antisecretory medication in patients with NERD. The researchers randomized 30 patients into either an MFR or a sham group. Patients in the study group received MFR treatment comprising four sessions—each lasting 25 min, twice a week, for 2 weeks. The experienced physiotherapist applied a three-dimensional, low-load pressure to the fascial tissue in the corresponding area to restore the myofascial properties of the CD. The sham group received exactly the same type of contact treatment but without any fascial stimulation or pressure. All variables were assessed at the baseline, 1 week, and 4 weeks after the end of the treatment. At week 4, patients receiving MFR techniques showed significant improvements in reflux symptoms, QoL, and PPI usage compared to the sham group.
The effect of osteopathic visceral treatment in patients with GERD was evaluated in a study by Eguaras et al. [36]. Sixty patients were equally randomized in a study and control group. Reflux symptoms were assessed 1 week after the first intervention, which was performed by an osteopath for 5 min. Cervical mobility and C4 spinosus process pressure pain threshold were assessed after the second intervention, after 2 weeks. The application of osteopathic manual treatment produced significant improvements in all assessed variables in the study group compared to the control group.
Halland et al. [37] studied the effect of diaphragmatic breathing in GERD patients with upright reflux and aimed to determine the impact of postprandial breathing maneuvers on reflux, LES, and gastric pressure. Thirty-three subjects were enrolled in the study. During high-resolution impedance manometry, 23 study patients received a standardized meal and were randomized to a DBT or sham group. After, patients underwent 48 h of pH-impedance monitoring, with another randomization to postprandial DBT on the second day. The postprandial breathing training reduced the number of postprandial reflux events in patients and healthy controls and decreased reflux episodes on day two compared to day one observations in all subjects. Comparing the DBT group with the sham group, total AET on day two was not significantly different, but AET in the two-hour window after standardized meal administration was significantly reduced on day two versus day one. According to the authors, DBT reduces postprandial reflux by increasing the difference between LES and gastric pressure.
Ahmadi et al. [38] compared the effect of diaphragmatic breathing and aerobic exercise (AE) on LES pressure and QoL in patients with moderate to severe GERD. Patients were randomized into three equal groups. The control group received 20 mg of omeprazole per day, while the other groups received DBT or AE in addition to antireflux medication. Patients in the DBT group performed DBT with deep respiration into the abdomen, 5 days a week and with five sessions each day. Patients in the AE group ran for 20 min per day, achieving 70% of maximum heart rate, for five sessions a week. QoL and LES pressure were measured before and after the study. DBT improved both LES pressure and QoL in patients with reflux, where DBT had more of an effect on QoL than AE did.
The results of all selected studies are summarized in Table 1.
Table 1.
Clinical studies evaluating the effect of respiratory physiotherapy in patients with GERD
| Authors Journal (Year) | Region | Study design | Patients (number/characteristics) | Therapy training/control | Exercises time/follow-up | Parameters | Results |
|---|---|---|---|---|---|---|---|
| Eherer et al. The American Journal of Gastroenterology (2012) | Austria | Prospective randomized controlled study | 19 patients with NERD or healed esophagitis (10 in training group/mean age 48 ± 4 years, mean BMI 22.0 kg/m2; 9 in control group/mean age 55 ± 4 years, mean BMI 24.9 kg/m2) | Abdominal breathing exercises + on-demand PPI/on-demand PPI | 4 weeks training/9 months | pH-metry, QoL, on-demand PPI usage | Significant decrease in pH < 4.0 (9.1 ± 1.3 to 4.7 ± 0.9), significantly improved QoL, and significant decrease in PPI usage after 9 months (98 ± 34 to 25 ± 12 mg/week)—only in study group |
| Da Silva RCV et al. Diseases of the Esophagus (2012) | Brazil | Prospective randomized controlled study | 38 patients (22 in study group/mean age 49.4 ± 15 years, mean BMI 25.7 kg/m2; 16 in placebo group/mean age 50.5 ± 16, mean BMI 23.52 kg/m2) | Osteopathy (diaphragm stretching technique)/placebo technique | ARP and MEP on esophageal manometry before and just after osteopathy | Increase of 9–27% in LES pressure only in study group (9.2% increase in ARP; 21.0% increase in MEP) | |
| Chaves RCM et al. Respiratory Medicine (2012) | Brazil | Prospective study | 29 consecutive patients (20 in study group/mean age 50.1 years; 9 in control group/mean age 51.3 years) | IMT using threshold/respiratory exercises with minimal inspiratory load | 8 weeks | MRP and EEP on esophageal manometry | Significant increase in MRP and EEP in both study group (46.6% and 34.8%, respectively) and control group (26.2% and 15.0%, respectively) |
| Souza MA et al. Am J Physiol Gastrointest Liver Physiol (2013) | Brazil | Prospective study | 12 patients with GERD and 7 healthy volunteers | IMT with threshold | 2 months | Average EGJ pressure, inspiratory EGJ pressure during respiratory maneuvers, assesment of TLESr on manometry, pH-metry, autonomic function | Improved EGJ pressures (19.7 ± 2.4 to 29.5 ± 2.1 mmHg), decreased number and duration of TLESr (8.5 to 7 events/hour, 199.1 ± 23.5 to 156.8 ± 25.9 min), reduced GERD proximal progression, decreased GERD symptoms |
| Sun et al. Diseases of the Esophagus (2016) | China | Prospective randomized controlled study | 40 patients (20 patients in training group/mean age 48.9 ± 2 years, mean BMI 27.9 kg/m2; 20 patients in control group/mean age 50.5 ± 2 years, mean BMI 26.4 kg/m2) | Diaphragm biofeedback training + PPI (Rabeprazole)/Rabeprazole only | 8 weeks/6 months | Consumption of PPI, GERD symptoms, QoL, esophageal motility on HRM | Improved GERD symptoms and QoL at 8 weeks; decreased PPI use at 6 months (82.3% of patients in the study group ceased PPI use; 6.2% of patients in control group ceased PPI use), increased CD pressure (16.81 ± 1.08 to 25.27 ± 1.31 mmHg) and EGJ pressure (23.21 ± 1.28 to 31.76 mmHg), observed only in study group |
| Ong et al. Clinical Gastroenterology and Hepatology (2018) | Singapore | Prospective study | 36 consecutive GERD patients with excessive belching (15 patients in training group/mean age 44.9 ± 15.7 years; 21 patients in control group/mean age 46 ± 10.4 years) | Diaphragmatic breathing exercises/no exercises | 4 weeks/4 months | Belching VAS score, GERD symptoms, QoL | Decreased belching VAS score, reduced GERD symptoms, increased QoL only in study group |
| Moffa et al. Acta Otorrinolaringol Esp. (2019) | Italy, Spain | Prospective study | 21 patients with NERD | Modified inspiratory muscle training | 4 weeks | GERD symptoms, QoL, laryngeal endoscopy | Improved GERD symptoms and QoL, improved laryngeal endoscopy score |
| Martinez-Hurtado et al. Scientific Reports (2019) | Spain | Prospective randomized controlled study | 30 patients with GERD (15 patients in study group/mean age 49.9 ± 14 years, mean BMI 25.6 kg/m2; 15 patients in control group/mean age 46.9 ± 15 years, mean BMI 27.3 kg/m2) | Diaphragmatic MFR techniques/gentle contact techniques | 2 weeks/4 weeks | GERD symptoms, QoL, PPI consumption | Improved GERD symptoms and QoL; reduced PPI usage by week 4 (88 mg/week to 33 mg/week), observed only in study group |
| Eguaras et al. Journal of Clinical Medicine (2019) | Spain | Randomized double-blinded controlled study | 60 patients with GERD (31 patients in experimental group/mean age 48.19 years, mean BMI 24.7 kg/m2; 29 patients in control group/mean age 49.45 years, mean BMI 24.81 kg/m2) | Osteopathic techniques for LES/manual contact mimicked the osteopathic techniques | 1 week/2 weeks | GERD symptoms, CROM, C4 PPTs | Significant improvement in GERD symptoms in 1 week; C4 PPTs and CROM improved in 2 weeks |
| Halland et al. Am J Gastroenterol (2021) | USA | Randomized controlled study | 23 patients with GERD and 10 controls (GERD patients/mean age 58 ± 12 years, BMI 29.98 kg/m2; healthy controls/mean age 44 ± 10 years, mean BMI 28.32 kg/m2) | DBT/no exercises | 2 days | Effect of DBT on reflux (48 h pH-impedance monitoring), LES, and gastric pressure on HRM | Reduced postprandial reflux events on day 2 by increased LES—gastric pressure difference (percentage of acid exposure time decreased from 11.8 ± 6.4 to 5.2 ± 5.1 on day 2) |
| Ahmadi et al. Middle East Journal of Digestive Disease (2021) | Iran | Randomized controlled study | 75 patients with GERD (25 patients in aerobic group/mean age 37 ± 9 years, mean BMI 24 kg/m2; 25 patients in breathing group/mean age 42.6 ± 8 years, mean BMI 23.6 kg/m2; 25 patients in control group/mean age 40.3 ± 7 years, mean BMI 23.43 kg/m2) | AE/DBT/no exercises | 8 weeks | Effect of AE and DBT on QoL and LES pressure | After 8 weeks, DBT had more beneficial effects on LES pressure (16.6 ± 6.29 to 24.3 ± 4.61 mmHg) and QoL than did AE; AE did not change LES pressure, but improved QoL |
NERD nonerosive reflux disease, BMI body mass index, PPI proton pump inhibitor, QoL quality of life, ARP average respiratory pressure, MEP maximum expiratory pressure, LES lower esophageal sphincter, IMT inspiratory muscle training, MRP Mid-respiratory pressure, EEP end expiratory pressure, EGJ esophagogastric junction, TLESr transient lower esophageal sphincter relaxation, GERD gastroesophageal reflux disease, DBT diaphragmatic breathing training, HRM high resolution manometry, CD crural diaphragm, VAS visual analogue Scale, MFR myofascial releas, CROM cervical range of motion, PPT pressure pain threshold, AE aerobic exercise
Discussion
GERD is a global health issue with an increasing incidence. Antisecretory medications remain the main therapeutic approach to controlling reflux symptoms in most GERD patients; however, antisecretory medications do not affect reflux mechanisms. Furthermore, patients themselves become aware of the possible adverse effects of PPIs, creating reluctance in taking these medications over extended periods. The second most often applied treatment in GERD is surgical fundoplication, which is often considered too invasive a procedure. The gap between these two main treatment approaches principally consists of endoscopic methods that are not recognized as standard treatments and, moreover, are not available to patients in many countries [39].
Respiratory physiotherapy is an approach providing therapeutic relief in some GERD patients, since the diaphragm (which is the target of breathing exercises) is considered the dominant component of the antireflux barrier.
The effect of various respiratory physiotherapy techniques was evaluated in selected studies examining both GERD symptoms and QoL, with objective parameters such as EGJ function and reflux parameters. The authors mostly used validated questionnaires (GERDQ, RSI, GERD-HRQL), whose scores, in general, significantly improved in relation to reflux symptoms and QoL after the administration of respiratory physiotherapy training. Moreover, the studies assessing PPI consumption before and after breathing exercise training demonstrated a significant reduction in PPI usage after breathing exercise training. All studies assessing objective parameters showed overall improvement in GERD outcomes. The measured parameters of EGJ function included an increase in LES or EGJ pressure, decreased AET, decreased number or duration of TLESr or reduced postprandial reflux events.
The majority of patients in these studies suffered from NERD or mild reflux disease (i.e., reflux esophagitis grade A or B), but in a few studies, the GERD phenotype was undefined, or patients were diagnosed based on typical symptoms (such as responding to PPIs only). These studies may have included patients with functional heartburn or esophageal hypersensitivity—not GERD. The beneficial effect of breathing exercises found in these patients could have been the result of reduced hypersensitivity or hypervigilance. On the contrary, four studies demonstrated the effect of respiratory physiotherapy in patients with moderate to severe GERD, or an even greater degree of EGJ dysfunction (e.g., hypotensive LES and hiatus hernia), which highlights the potential of respiratory physiotherapy in a broader spectrum of patients with GERD [30, 31, 33, 38].
Conventional manometry and pH metry without impedance were used in most of the studies for objective evaluation of the EGJ and for determining the presence of reflux events. These methods could have influenced the accuracy of EGJ function assessment, since the sensitivity of conventional manometry in evaluating diaphragmatic function is not adequate [40]. Equally, pH metry is not suitable for evaluating PPI refractory patients, since weak acid reflux and proximal mixed episodes are responsible for persistent symptoms in those patiens. The majority of patients enrolled in those studies were symptomatic, despite treatment with PPIs. As impedance detects approximately 20% more reflux episodes, using pH metry with impedance would have been of greater benefit due to the increased sensitivity impedance brings [41].
Most study outcomes were evaluated after a relatively short time. Only a few studies had a long-term follow-up over several months, where long-term follow-up was better in demonstrating the changes on antireflux barrier function induced by regular breathing exercise training. Appropriate diaphragmatic function depends on the restoration of the ideal position of the body, which requires a longer time to achieve; thus, the assessment of DBT effects, after only a few weeks of use, on GERD symptoms may have been underestimated.
Besides breathing exercises, MFR was applied in two of the studies. Manipulation of the myofascial tissues, which form a network throughout the body, affects the function of muscles, bones, and visceral tissues, leading to the reduction of pain and improvement of muscle strength and range of motion. Mechanical stimulation of the diaphragm can increase its contractility and proprioception, and thus its participation in EGJ competence. Moreover, visceral manipulation releases increased tension within the abdominal cavity, which may favorably affect the abdomino-thoracic pressure gradient. This pressure gradient, together with the dysfunction of the antireflux barrier, is considered a critical point in the development of gastroesophageal reflux [42].
There were several limitations among the analyzed studies. Some studies included small numbers of patients. Most of the studies did not have blinding and lacked effective implementation control of the recommended exercises for patients. Furthermore, studies differed in terms of the specific physiotherapeutic technique under examination. Despite these limitations, the studies were prospective and controlled, and all but four were randomized. Although the studies generally showed an improvement in reflux symptoms, QoL, and EGJ contractility (including the reduction of reflux episodes after treatment), the studies were often heterogenous in their design, study outcomes, and particularly study interventions. Thus, it would be difficult to assess these the data in a meta-analysis.
DBT may be a useful therapeutic method in a large spectrum of GERD patients, as demonstrated by the presented studies. Patients who are symptomatic despite lifestyle modifications and the use of antisecretory medication should consider practicing DBT, since it may improve antireflux barrier function and thus allow reduced PPI consumption. We suggest that DBT should be part of the therapeutic approach for all GERD phenotypes, including patients with varying degrees of hiatus hernia. The use of HRM as a biofeedback therapy also allows the adjustment of ideal treatment positions or techniques in patients with more severe antireflux barrier dysfunction. Therefore, we do not assume that some groups of patients are contraindicated to practice DBT. There are no data evaluating the effect of DBT in patients who are indicated for or have undergone antireflux surgery. However, due to the possible effect of DBT on esophageal contractility, we hypothesize improved surgical outcomes in patients who practice DBT before surgery. This hypothesis must be confirmed by future clinical studies.
Conclusion
Current knowledge suggests the potential of breathing exercises in the treatment of GERD; however, long-term efficacy, patient selection, and the role of HRM in tailoring physiotherapeutic approaches requires further research. Future work should also aim to unify physiotherapeutic procedures to obtain a standardized method in GERD treatment, allowing for the better assessment of procedural effects in GERD patients.
Funding
This work was supported by the Cooperatio Program, research area Internal Disciplines and by Grant number GAUK 118221.
Footnotes
Conflict of interest The authors declare no conflict of interest or professional disclosures relevant to the synthesis of this paper.
References
- 1.Yamasaki T, Hemond C, Eisa M, Ganocy S, Fass R. The changing epidemiology of gastroesophageal reflux disease: are patients getting younger? J Neurogastroenterol Motil. 2018;24:559–69. 10.5056/jnm18140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cameron AJ, Lagergren J, Henriksson C, Nyren O, Locke GR, Pedersen NL. Gastroesophageal reflux disease in monozygotic and dizygotic twins. Gastroenterology. 2002;122:55–9. 10.1053/gast.2002.30301. [DOI] [PubMed] [Google Scholar]
- 3.Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67:1351–62. 10.1136/gutjnl-2017-314722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessing BF, Conchillo JM, Bredenoord AJ, Smout AJPM, Masclee AAM. Review article: the clinical relevance of transient lower oesophageal sphincter relaxations in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2011;33:650–61. 10.1111/j.1365-2036.2010.04565.x. [DOI] [PubMed] [Google Scholar]
- 5.Pandolfino JE, Zhang Q, Ghosh SK, Han A. Transient lower esophageal sphincter relaxations and reflux: mechanistic analysis using concurrent fluoroscopy and high-resolution manometry. Gastroenterology. 2006;131:1725–33. 10.1053/j.gastro.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Mittal RK, Goyal RK. Sphincter mechanisms at the lower end of the esophagus. GI Motil Online. 2006. 10.1038/gimo14. [DOI] [Google Scholar]
- 7.De Miranda Chaves RC, Navarro-Rodriguez T. Respiratory physiotherapy in gastroesophageal reflux disease: A review article. Worl J Respirol. 2015;5:28–33. 10.5320/wjr.v5.i1.28. [DOI] [Google Scholar]
- 8.Casale M, Sabatino L, Moffa A, Capuano F, Luccarelli V, Vitali M, Ribolsi M, Cicala M, Salvinelli F. Breathing training on lower esophageal sphincter as a complementary treatment of gastroesophageal reflux disease (GERD): a systematic review. Eur Rev Med Pharmacol Sci. 2016;20:4547–52. [PubMed] [Google Scholar]
- 9.Qiu K, Wang J, Chen B, Wang H, Ma Ch. The effect of breathing exercises on patients eith GERD: a meta-analysis. Ann Palliat Med. 2020;9:405–13. 10.21037/apm.2020.02.35. [DOI] [PubMed] [Google Scholar]
- 10.Bitnar P, Hlava S, Stovicek J, Kobesová A. Diaphragm in the role of esophageal sphincter and possibilities of treatment of esophageal reflux disease using physiotherapeutic procedures. Eur Respir J. 2018;52(Suppl 62):2446. 10.1183/13993003.congress-2018.PA2446. [DOI] [Google Scholar]
- 11.Kolar P Clinical rehabilitation, 1st edition, Prague: Galén, 2009. 713 s., ISBN 978-80-7262-657-1 [Google Scholar]
- 12.Kahrilas PJ, Mittal RK, Bor S, Kohn GP, Lenglinger J, Mittal SK, Pandolfino JE, Serra J, Tatum R, Yadlapati R. Chicago Classification update (v4.0): Technical review of high-resolution manometry metrics for EGJ barrier function. Neurogastroenterol Motil. 2021;33:e14113. 10.1111/nmo.14113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tolone S, Cassan CD, Bortoli ND, Roman S, Galeazzi F, Salvador R, Marabotto E, Furnari M, Zentilin P, Marchi S, Bardini R, Sturniolo GC, Savarino V, Savarino E. Esophagogastric junction morfology is associated with a positive impedance-pH monitoring in patiens with GERD. Neurogastroenterol Motil. 2015;27:1175–82. 10.1111/nmo.12606. [DOI] [PubMed] [Google Scholar]
- 14.Bitnar P, Stovicek J, Andel R, Arlt J, Arltova M, Smejkal M, Kolar P, Kobesova A. Leg raise increases pressure in lower and upper esophageal sphincter among patients with gastroesophageal reflux disease. J Bodyw Mov Ther. 2016;20(3):518–24. 10.1016/j.jbmt.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 15.Mittal RK, Shaffer HA, Parollisi S, Baggett L. Influence of breathing pattern on the esophagogastric junction pressure and esophageal transit. Am J Physiol. 1995;269:G577–83. 10.1152/ajpgi.1995.269.4.G577. [DOI] [PubMed] [Google Scholar]
- 16.Pandolfino JE, Kim H, Ghosh SK, Clarke JO, Zhang Q, Kahrilas PJ. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol. 2007;102:1056–63. 10.1111/j.1572-0241.2007.01138.x. [DOI] [PubMed] [Google Scholar]
- 17.Lin S, Li H, Fang X. Esophageal motor dysfunction in gastroesophageal reflux disease and therapeutic perspestives. J Neurogastroenterol Motil. 2019;25:499–507. 10.5056/jnm19081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Masuda T, Mittal SK, Kovacs B, Csucska M, Bremner RM. Simple manometric index for comprehensive esophagogastric junction barrier competency against gastroesophageal reflux. J Am Coll Surg. 2020;230:744–755.e3. 10.1016/j.jamcollsurg.2020.01.034. [DOI] [PubMed] [Google Scholar]
- 19.Nicodéme F, Pipa-Muniz M, Kahrilas PJ, Pandolfino JE. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil. 2014;26:353–60. 10.1111/nmo.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tolone S, De Bortoli N, Marabotto E, de Cassan C, Bodini G, Roman S, Furnari M, Savarino V, Docimo L, Savarino E. Esophagogastric junction contractility for clinical assessment in patients with GERD: a real added value? Neurogastroenterol Motil. 2015;27:1423–31. 10.1111/nmo.12638. [DOI] [PubMed] [Google Scholar]
- 21.Halland M, Parthasarathy G, Bharucha AE, Katzka DA. Diaphragmatic breathing for rumination syndrom: efficacy and mechanisms of action. Neurogastroenterol Motil. 2016;28:384–91. 10.1111/nmo.12737. [DOI] [PubMed] [Google Scholar]
- 22.Festi D, Scaioli E, Baldi F, Vestito A, Pasqui F, Di Biase AR, Colecchia A. Body weight, lifestyle, dietary habits and gastroesophageal reflux disease. World J Gastroenterol. 2009;15:1690–701. 10.3748/wjg.15.1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bordoni B, Marelli F, Morabito B, Sacconi B, Caiazzo P, Castagna R. Low back pain and gastroesophageal reflux in patients with COPD: the disease in the breath. Int J Chron Obstruct Pulmon Dis. 2018;13:325–34. 10.2147/COPD.S150401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Imagama S, Hasegawa Y, Wakao N, Hirano K, Hamajima N, Ishiguro N. Influence of lumbar kyphosis and back muscle strength on the symptoms of gastroesophageal reflux disease in middle-aged and elderly people. Eur Spine J. 2012;21:2149–57. 10.1007/s00586-012-2207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hep A, Vanakova E, Tosnerova V, Prásek J, Vízd’a J, Dite P, Ondrousek L, Dolina J. Radionuclide oesophageal transit scintigraphy: a useful method for verification of oesophageal dysmotility by cervical vertebropathy. Dis Esophagus. 1999;12:47–50. 10.1046/j.1442-2050.1999.00008.x. [DOI] [PubMed] [Google Scholar]
- 26.Martinucci I, de Bortoli N, Savarino E, Nacci A, Romeo SO, Bellini M, Savarino V, Fattori B, Marchi S. Optimal treatment of laryngopharyngeal reflux disease. Ther Adv Chronic Dis. 2013;4:287–301. 10.1177/2040622313503485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matsuzaki J, Suzuki H, Masaoka T, Tanaka K, Mori H, Kanai T. Influence of regular exercise on gastric emptying in healthy men: a pilot study. J Clin Biochem Nutr. 2016;59:130–3. 10.3164/jcbn.16-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eherer AJ, Netolitzky F, Hogenauer C, Puschnig G, Hinterleitner TA, Scheidl S, Kraxner V, Krejs GJ, Hofmann KM. Positive effect of abdominal breathing exercise on gastroesophageal reflux disease: a randomized controlled study. Am J Gastroenterol. 2012;107:372–8. 10.1038/ajg.2011.420. [DOI] [PubMed] [Google Scholar]
- 29.da Silva RCV, de Sá CC, Pascual-Vaca ÁO, de Souza Fontes LH, Herbella Fernandes FAM, Dib RA, Queiroz RA, Navarro-Rodriguez T. Increase of lower esophageal sphincter pressure after osteopathic intervention on the diaphragm in patients with gastroesophageal reflux. Dis Esophagus. 2013;26:451–6. 10.1111/j.1442-2050.2012.01372.x. [DOI] [PubMed] [Google Scholar]
- 30.de Miranda Chaves RC, Suesada M, Polisel F, de Sá CC, Navarro-Rodriguez T. Respiratory physiotherapy can increase lower esophageal sphincter pressure in GERD patients. Respir Med. 2012;106:1794–9. 10.1016/j.rmed.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 31.Souza MAN, Lima MJV, Martins GB, Nobre RA, Souza MHLP, de Oliviera RB, dos Santos AA. Inspiratory muscle training improves antireflux barrier in GERD patients. Am J Physiol Gastrointest Liver Physiol. 2013;305:G862–7. 10.1152/ajpgi.00054.2013. [DOI] [PubMed] [Google Scholar]
- 32.Sun X, Shang W, Wang Z, Liu X, Fang X, Ke M. Short-term and long-term effect of diaphragm biofeedback training in gastroesophageal reflux disease: an open-label pilot, randomized trial. Dis Esophagus. 2016;29:829–36. 10.1111/dote.12390. [DOI] [PubMed] [Google Scholar]
- 33.Ong AML, Chua LTT, Khor ChJL, Asokkumar R, Namasivayam V, Wang YT. Diaphragmatic breathing reduces belching and proton pump inhibitory refractory gastroesophageal reflux symptoms. Clin Gastroenterol Hepatol. 2018;16:407–16. 10.1016/j.cgh.2017.10.038. [DOI] [PubMed] [Google Scholar]
- 34.Moffa A, Oliveto G, Di Matteo F, Baptista P, Cárdenas A, Cassano M, Casale M. Modified inspiratory muscle training (m-IMT) as promising treatment for gastro-oesophageal reflux disease (GERD). Acta Otorrinolaringol Esp. 2020;71:65–9. 10.1016/j.otorri.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Martinez-Hurtado I, Arguisuelas MD, Almela-Notari P, Cortés X. Effects of diaphragmatic myofascial release on gastroesophageal reflux disease: a preliminary randomized controlled trial. Sci Rep. 2019;9:7273. 10.1038/s41598-019-43799-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eguaras N, Rodriguez-Lopez ES, Lopez-Dicastillo O, Franco-Sierra MA, Ricard F, Oliva-Pascual-Vaca Á. Effect of osteopathic visceral treatment in patients with gastroesophageal reflux: a randomized controlled trial. J Clin Med. 2019;8:1738. 10.3390/jcm8101738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Halland M, Bharucha AE, Crowell MD, Ravi K, Katzka DA. Effects of diaphragmatic breathing on the pathophysiology and treatment of upright gastroesophageal reflux: a randomized controlled trial. Am J Gastroenterol. 2021;116:86–94. 10.14309/ajg.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 38.Ahmadi M, Amiri M, Rezaeian T, Abdollahi I, Rezadoost AM, Sohrabi M, Bakhshi E. Different effect of aerobic exercise and diaphragmatic breathing on lower esophageal sphincter pressure and quality of life in patients with reflux: a comparative study. Middle East J Dig Dis. 2021;13:61–6. 10.34172/mejdd.2021.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weusten BLAM, Barret M, Bredenoord AJ, Familiari P, Gonzalez JM, van Hooft JE, Lorenzo-Zúñiga V, Louis H, Martinek J, van Meer S, Neumann H, Pohl D, Prat F, von Renteln D, Savarino E, Sweis R, Tack J, Tutuian R, Ishaq S. Endoscopic management of gastrointestinal motility disorders—part 2: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52:600–14. 10.1055/a-1171-3174. [DOI] [PubMed] [Google Scholar]
- 40.Mello M, Gyawali CP. Esophageal manometry in gastroesophageal reflux disease. Gastroenterol Clin North Am. 2014;43:69–87. 10.1016/j.gtc.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 41.Karamanolis G, Kotsalidis G, Triantafyllou K, Polymeros D, Gaglia A, Fessatou S, Triantafyllou M, Papanikolaou I, Ladas SD. Yield of combined impedance-pH monitoring for refarctory reflux symptoms in clinical practise. J Neurogastroenterol Motil. 2011;17:158–63. 10.5056/jnm.2011.17.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ghost SK. Biomechanics of the esophagogastric junction in gastroesophageal reflux disease. Curr Gastroenterol Rep. 2008;10:246–51. 10.1007/s11894-008-0051-6. [DOI] [PubMed] [Google Scholar]


